1 Surgical Instrumentation
CHAPTER CONTENTS
Introduction 2
Design of Ophthalmic Instruments 2
Ophthalmic Surgical Instruments 3
Adaptations for Large Animal and Special Species
Ophthalmic Surgeries 13
Surgical Instruments for Ophthalmic Surgeries 13
Recommended Instruments for Orbital Surgeries 15
Recommended Surgical Instruments for Eyelid Surgeries 15
Recommended Surgical Instruments for Conjunctival and Corneal Surgeries 15
Recommended Surgical Instruments for Intraocular Surgeries and Cataract Extractions 16
Instruments for Vitreoretinal Surgeries 16
Ophthalmic Sutures and Needles 16
Instrument Care, Storage, and Sterilization 17
Further Reading 18
Introduction
Since the 1960s, magnification has had a major influence on the advances of ophthalmic surgery and instrumentation. With magnification of the ophthalmic surgical field, incisions previously deemed quite satisfactory were viewed as irregular and wound apposition as imperfect. The standard ophthalmic surgical instruments, as observed under 10x to 20x magnification, were too large and impaired the surgeon’s view of the surgical field. Forceps were viewed to compress and occasionally tear tissues. The standard ophthalmic needle holders grasped the smaller needles poorly, often flattening the curved needles. The working distance between the surgical field and the bottom of the operating microscope limited both the number and size of ophthalmic instruments. As a result, smaller microsurgical instruments evolved in the 1960s and 1970s.
Although some general surgical instrumentation may be used for extraocular procedures, the surgical instruments for conjunctival, corneal, and intraocular surgical procedures should be microsurgical ophthalmic instruments. These instruments are delicate in comparison to the general surgical instruments and require prudent care and use to ensure long-term use and optimal surgical results.
The investment in standard, microsurgical, or a combination of ophthalmic instrumentation varies with their predicted amount of use. The most important instruments are corneoscleral and conjunctival scissors, and needle holders; these instruments should be the best available. If microsurgical
instruments are selected, tying forceps rather than needle holders are used for handling small ophthalmic sutures, and these instruments should be of high quality.
Design of Ophthalmic Instruments
Microsurgery instruments were developed by reducing the size of standard ophthalmic instruments by approximately one third (120 to 140 mm to 90 to 100 mm). They are thinner and shorter to accommodate the working distance between the patient’s eye and the base objective lens of the operating microscope and usually have a dull or minimally reflective finish to prevent glare from the microscope light. If the instruments are too large, inadvertent contact and the resultant contamination with the bottom of the operating microscope may occur. The size of the jaws, blades, or forceps tips were reduced further to permit atraumatic handling of the tissues, needles, and suture materials.
A large assortment of standard and microsurgical instruments are available to the veterinarian contemplating corneal and intraocular surgery. Choices must be made regarding instrument length, size, angle and length of the teeth and jaws, designation of tips (sharp versus blunt, straight versus curved), configuration of handles (flat versus rounded, with either serrated, six-sided, or knurled grips), locking versus nonlocking mechanisms, inclusion or exclusion of tying platforms and pin stops, finish (dull or polished), and material (stainless steel versus titanium). Titanium is stronger and more corrosion resistant than stainless steel and will generally retain sharpness for a longer period of time. It is recommended that the surgeon purchase high-quality instruments for the most delicate tissue and tying forceps, needle holders, and scissors. Although expensive, high-quality instruments tend to last longer and perform superiorly.
The diameters of the handles of most of ophthalmic spatulas and knives are about 6 to 7 mm. The width of the handles of the larger needle holders, scissors, and forceps are usually about 10 to 12 mm. The shape of these instruments also directly influences their use. Instruments with 5 to 6 mm diameter handles often have rounded or 4 or 6 sides to permit convenient rotation or turning of the handle while grasping the instrument. Instruments that are flat or expand in only one direction, like corneoscleral scissors or the different forceps, have handles that are flat or serrated for grasping and permit only limited or no rotation. To facilitate grasping and manipulation of these small instruments without slipping, the handles are usually serrated, knurled, or 6-sided to accommodate and limit placement of the fingers on these gripping areas. If these irregular surfaces are too small, the grasp of the instrument may be less than secure.

If these serrated areas are too large, the large finger placement area may actually limit manipulation and even snag sutures during tying. All ophthalmic instruments should be constructed from high-quality stainless steel or titanium with dull surfaces to minimize light reflections.
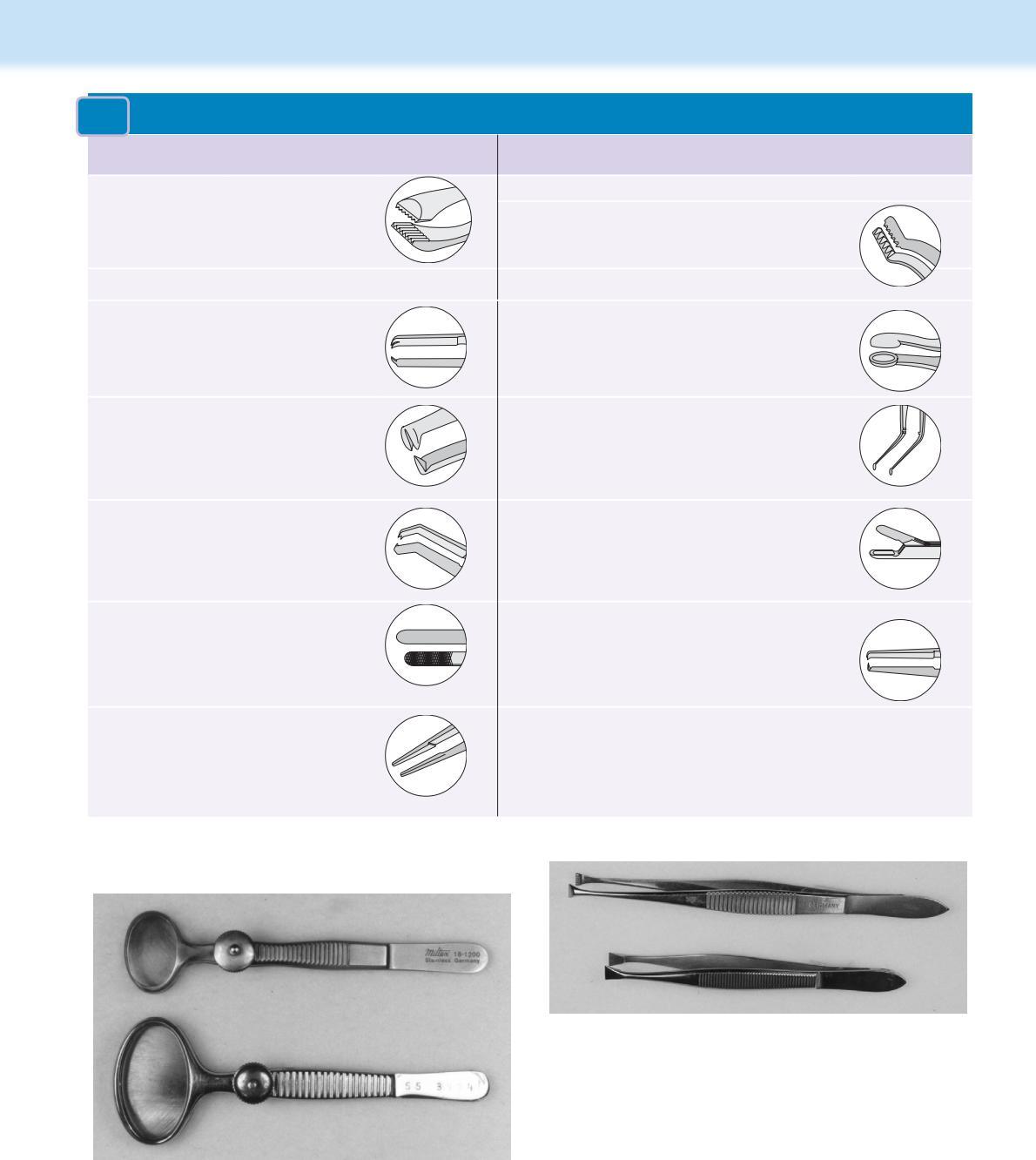
The forceps and scissors for corneal and intraocular procedures are usually hinged with different mechanisms to facilitate their opening. The three most common hinges include the x-hinge, vertical pin hinge, and the bar hinge (Fig. 1.1). The common x-hinge for scissor blades or needle holder tips are usually joined by small screws or pins, and often the handles converge to become spring mechanisms that maintain the instrument in an open position. With spring handles, as the instrument is closed, the springs straighten, a pin stop prevents overclosing, and then the springs return to the curved position opening the jaws as finger pressure is released. With vertical pin hinges, as in iris scissors, the hinge pin is deformed as the scissor blade is closed to act as a spring device to open the blades upon release. The bar hinge is typical of most forceps and consists of the junction of base of both handles; tension of these handles closes the forceps blades and release results in the forceps tips opening. All of these hinges are very delicate and, if extended too far, can easily bend or break.
Most of the standard and microsurgical ophthalmic instruments are designed for a single purpose. Hence, the standard corneal or intraocular surgical instrument pack includes several instruments. Occasionally, these instruments are designed to perform two or more functions. One example is the tying forceps. Its tip usually includes teeth (1 x 2), which permit grasping of the cornea and/or conjunctiva. Just proximal to its tip is a flat tying platform to grasp sutures during tying and construction of knots. These multiple purpose forceps are usually heavily used during corneal and intraocular surgical procedures and can become easily malaligned.
During microsurgery, the tips of the ophthalmic instruments are often the only parts of these instruments that are visible. In addition, many microsurgical instruments possess angled tips to facilitate their use at higher magnifications and minimize the obstruction of the surgical field.
OPHTHALMIC SURGICAL INSTRUMENTS
Ophthalmic surgical instruments are often developed for specific tasks and functions. As a result, a considerable choice of the standard and microsurgical ophthalmic instruments is available. A certain number of these instruments are essential and recommended for the different small and large animal ophthalmic surgeries.
For convenience, these instruments for the different ophthalmic surgical procedures are listed later in the latter section of this chapter. They include
• Table 1.2 – Instruments for orbital surgeries;
• Table 1.3 – Instruments for eyelid and conjunctival surgeries;
• Table 1.4 – Instruments for conjunctival and corneal surgeries;
• Table 1.5 – Instruments for glaucoma surgeries;
• Table 1.6 – Instruments for intraocular and cataract surgeries; and
• Table 1.7 – Instruments for vitreoretinal surgeries. These instruments are first presented in further detail.
Eyelid Specula
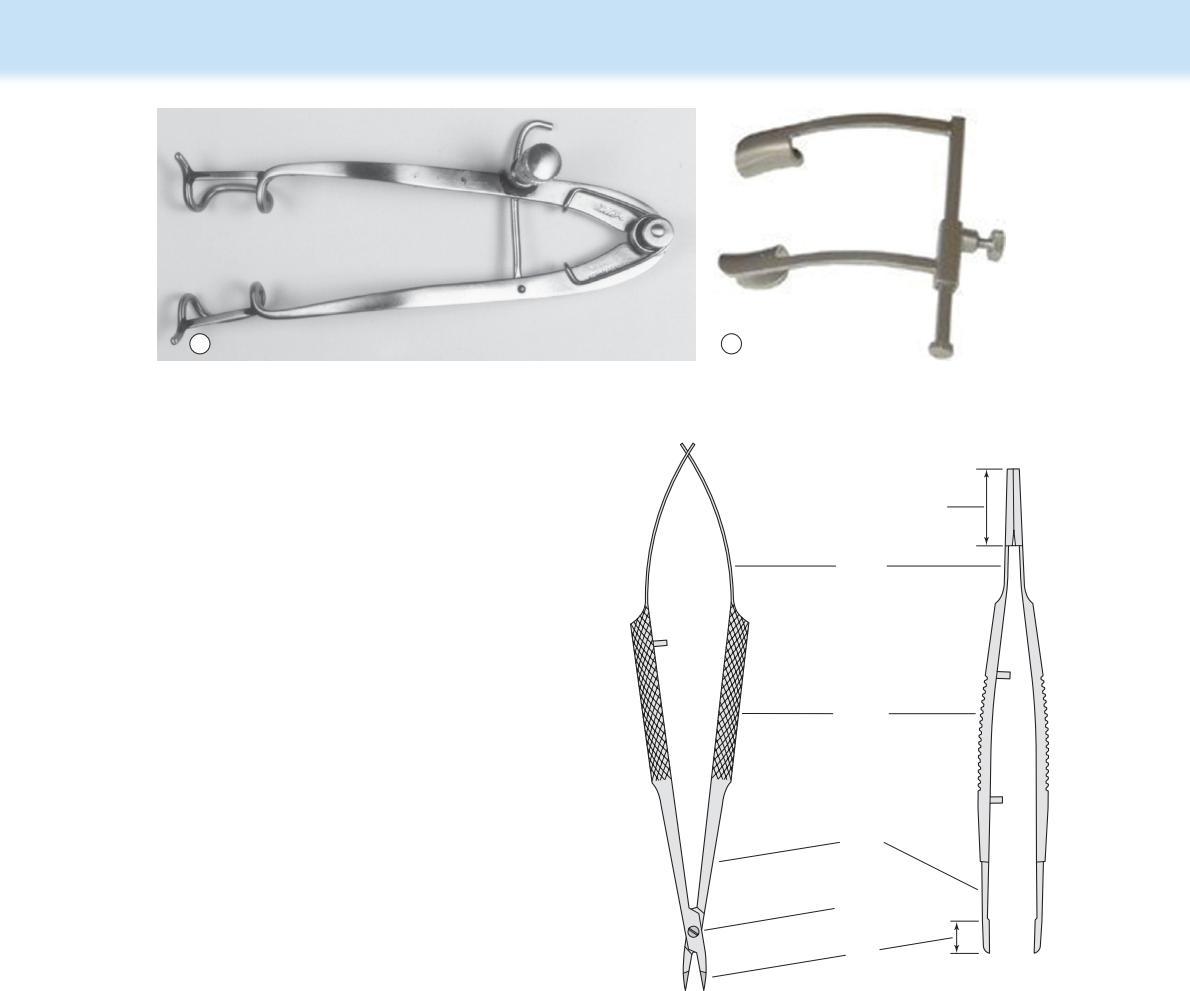
Eyelid specula are used to retract the eyelids and enhance exposure of the conjunctiva, cornea, and the globe. The ideal eyelid speculum should be strong enough to retract the eyelids to the maximal amount possible but sufficiently lightweight to prevent direct pressure on the cornea and globe. The most versatile and inexpensive eyelid speculums for small animals are fashioned of wire. For most breeds of dogs and cats, the Barraquer wire speculum with 14 mm blades and an overall length of 40 mm is preferred (Fig. 1.2). The pediatric size Barraquer speculum may be useful in young and smaller animals; its blades are 11 mm and overall length is 34 mm. The stainless steel Cook speculum™ with its locking screw mechanism (10 mm blades, 22 mm blade spread, and 52 to 55 mm overall length) is also particularly helpful in small animals with short palpebral fissures (see Fig. 1.3b).
In large dogs and large animals, a heavier eyelid speculum may be necessary. Eyelid speculums, such as the Guyton-Park (14 mm blades and overall length of 85 mm), Castroviejo (15 or 16 mm blades and overall length of 75–82 mm), and Williams (10 mm blades and overall length of 90 mm), can provide maximum exposure of the palpebral fissure (Fig. 1.3a and b). Sometimes, for the lid speculum to conform to the eyelid and palpebral curvatures of the horse and cow, the arms of the specula are bent slightly. With all eyelid specula, the blades should extend beneath the eyelid margins for several millimeters to
A B C
Fig. 1.1 The different hinge mechanisms used for ophthalmic instruments (from left to right: x-type, vertical pin, and bar hinge).
Fig. 1.2 The pediatric and adult size wire eyelid specula by Barraquer. These inexpensive lid specula are the most versatile and durable for small animals.
adequately retract the eyelids and reduce the possibility of dislodgement. In some species, like the avian species, the palpebral fissures and eyelids are very small, and a single 4-0 to 6-0 silk suture may be placed in each eyelid to retract the lids open.
Tissue Forceps
The different types of ocular tissues have resulted in the development of a large selection of tissue forceps with specialized tips. These tissue forceps vary by tips, shaft, handles, springs, and bar hinge (Fig. 1.4). The handles of these forceps are usually flat, with serrations or knurling on the handles to facilitate their grasp. The microsurgical forceps usually have angled tips and are about two-thirds the total length of the standard ophthalmic instruments. The arms of these forceps are hinged at the base, and this hinge provides sufficient tension to maintain the tips about 5 to 10 mm apart. Upon digital compression, the tissue forceps tips should completely and perfectly contact each other. The tips of many forceps are angulated to prevent blockage of the surgeon’s view during surgery.
The major difference of the ophthalmic tissue forceps is their tips, which have highly specialized indications (Table 1.1). In selecting these tissue forceps, one should handle them individually and use those forceps that feel the most comfortable to the surgeon.
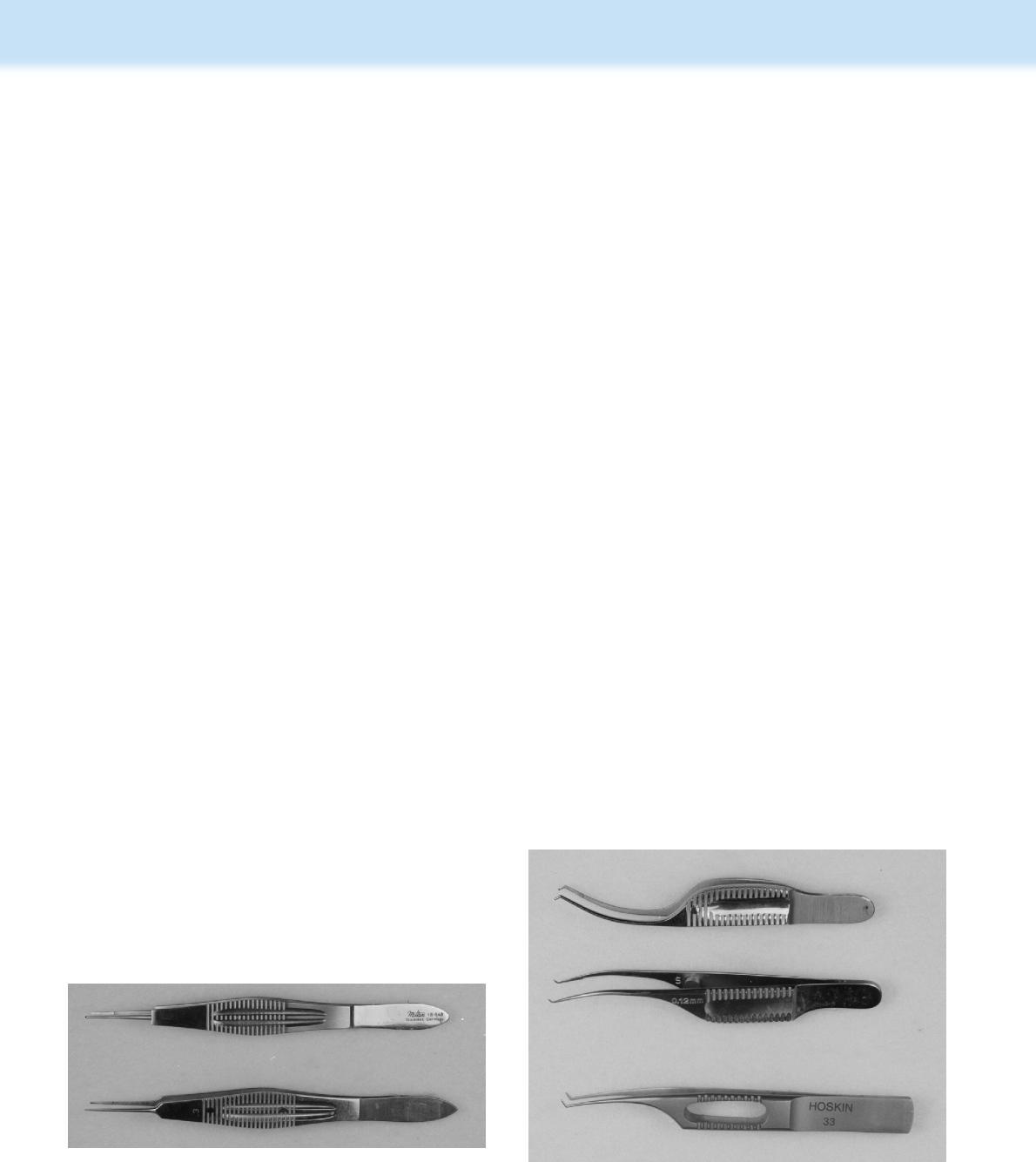
Eyelid/Chalazion Forceps
Highly specialized forceps have been developed for entropion and chalazion surgery. The chalazion forceps have an open and a solid or a ring plate on the opposite tips (Fig. 1.5). These tips may be either circular or oval; the latter tips are more versatile as they can be inserted in the palpebral fissure with the oval is either the vertical or horizontal axis. With the forceps clamped to the eyelid, a small lid tumor or chalazion can be excised while pressure from the special plates maintains hemostasis and exact positioning of the eyelid margins and mass.
Conjunctival Forceps
Forceps to manipulate the bulbar and palpebral conjunctiva generally possess teeth. Small splay-tooth or dog-tooth tips with 1 × 2 teeth are most useful to grasp the conjunctiva during most manipulations. A variety of forceps that differ by the measured space between the teeth ranging from 0.12 mm to 1.0 mm
Shafts
x-hinge
Tips
are available. The smaller the distance in these instruments, the finer and more delicate is the grasp. Excessive tension of the conjunctival tissues with the small tips will often create small tears or ‘button-holes’ of the conjunctival mucosa. These small breaks in the conjunctival mucosal surface are not usually important but may be significant in certain grafting procedures. The tips of the von Graefe tissue forceps possesses 10 to 14 fine teeth and generally accommodate a considerable tension of the conjunctival mucosa or the leading edge of the nictitans before tearing is evident (Fig. 1.6). Unfortunately, the von Graefe tips are too large for microsurgical procedures but useful for orbit, eyelids, and orbital surgeries. The conjunctival tissues can also be manipulated with serrated tips, devoid of any teeth; however, slippage of the tips from the mucosa is likely. These forceps are
A B
Fig. 1.3 (a) The Williams eyelid speculum is reserved to retract the eyelids of large breeds of dogs and other large species. (b) The Cook speculum™ has a locking screw mechanism and short retractors is also useful in small animals with short palpebral fissures.
Bar hinge Springs
Handles
Fig. 1.4 Components of ophthalmic forceps include tips, shaft, handles, springs, and bar/x hinge.
TABLE 1.1
Tips of Tissue Forceps Used for Corneal and Intraocular Surgery
Tip Design Designated Tissue(s) or Use
von Graefe
Conjunctiva/nictitans
Appearance Tip Design Designated Tissue(s) or Use Appearance
Lens capsule
Extracapsular
Grasp/tear anterior lens capsule
1 x 2 teeth
Cornea/conjunctiva
Splay Intracapsular Grasp/hold anterior lens capsule
Dog-toothed
Colibri-style tip angulation
Cornea/conjunctiva
Utrata
Intraocular
Anterior capsulorrhexis
Grasp/remove lens capsule and fragments
Serrations Cornea/conjunctiva
Tying platforms Tying small sutures
Combination 1 x 2 teeth tying platform
Cornea/conjunctiva & tying sutures
Fig. 1.5 The Francis chalazion (top) and Desmarres entropion (bottom) forceps have specialized tips consisting of an oval to round ring and a solid oval to circular tip. The ring base is used to surround the surgical site, and the solid base is used to protect deeper tissues, including the eye.
Fig. 1.6 Graefe fixation (top) and cilia (bottom) forceps. The Graefe forceps have wide jaws with multiple fine teeth that can grasp the eyelid and conjunctiva without tearing. The cilia forceps have smooth surface jaws that permit grasping of fine cilia.
generally unsuitable for manipulating or tying the very fine ophthalmic sutures.
Corneal, Limbal, and Scleral Forceps
The cornea, sclera, and limbus represent the fibrous tunic of the globe and are remarkedly tough tissues to incise, manipulate, and suture in many animal species. As a result, the tips of the
corneal or corneoscleral forceps generally possess some type of teeth. Generally, the tips consist of either splay-tooth or dogtooth designs. These types of tips successfully grasp and hold these tissues. Modifications of these tips, such as the closedcups (von Mandach forceps) open-cups (Pierse type) are less traumatic to the cornea but permit limited lateral slippage. The finest forceps with the smallest intratooth distance, such as 0.12 mm, are recommended for manipulation of the corneal tissues. The forceps may be straight or shaped according to the Colibri fashion; either are appropriate with the choice based upon the surgeon’s preference. Some corneal forceps will have a tying platform to facilitate not only placement of sutures but also securing of subsequent knots.
Suture and Tying Forceps
Special forceps have been developed to facilitate suture manipulation and tying during microsurgery. In fact, most ophthalmic surgeons prefer these forceps for tying of small-diameter sutures. The standard or microsurgery needle holder often allows these very small-diameter sutures to easily slip within the needle holder jaws. The surgeon’s fingers cannot be used because the sutures are too small and often too short. The standard suture-tying forceps are either the straight or curved model with 1 × 2 teeth or without teeth. The smooth platforms of both tips have rounded edges to accommodate the sutures and prevent any suture breakage or etching (Fig. 1.7). The platforms must meet perfectly flush to permit suture manipulation and grasp during tying. These forceps are designed for the very small size ophthalmic sutures (6-0 to 12-0). The addition of 1 x 2 teeth to the tip of the Harm-type suture-tying forceps permits these forceps to both grasp corneal or conjunctival tissues and assist in the tying of sutures, and decreases the time and effort during wound apposition.
A unique design, the Colibri style, has been used with many tissue forceps to incorporate a tying platform. Often, these Colibri-type forceps, with a characteristic angled shaft, have tips with teeth to assist in the grasping of corneal and conjunctival tissues (Fig. 1.8). The tips with different types of teeth are used to grasp tissues; the knee or angle portion can be used as smooth forceps.
Iris Forceps
The animal iris and ciliary body tissues are highly friable and vascular. Excessive traction with tissue forceps on the iris results
in frequent tearing and hemorrhage. Iris forceps may be straight or curved; their tips are serrated or possess very small teeth. To facilitate anterior chamber manipulations, the tips and shafts of these forceps are quite slender and delicate.
Anterior Lens Capsule Forceps
Special forceps have been developed to grasp and hold or grasp and tear the anterior lens capsule during cataract surgery in the dog and cat. Intracapsular lens forceps are used to grasp and hold the anterior lens capsule during removal of the entire lens with its capsules (see Table 1.1). The forceps have slender shafts and tips to enter the anterior chamber and pupil. The shafts are also curved or angled to traverse the pupil and facilitate grasping the anterior lens capsule. Within the tip is a 2.0 to 2.5 mm cup to grasp, not tear, the central anterior lens capsule.
The extracapsular forceps are very similar in design, but their tips possess either 4 to 5 or 5 to 6 fine teeth to grasp and tear a central portion of the anterior lens capsule (see Table 1.1). Through the defect in the anterior lens capsule, the reminder of the lens cortex and nucleus are expressed or removed by phacoemulsification.
Phacoemulsification has largely replaced the standard extracapsular cataract techniques in most animal species in most countries, and circular tearing of the anterior capsule sufficiently large to accommodate the insertion of an intraocular lens (IOL) has become standard. The most frequently used forceps for the continuous anterior capsulectomy or capsulorrhexis is the Utrata instrument. The Utrata forceps has variable lengths tips and very small single teeth pointing down from the two tips to grasp the anterior lens capsule. Additional information on the Utrata forceps may be found in Chapter 12 on surgery of the lens and cataract.
IOL Instrumentation
With the advent of intraocular lenses (IOLs) in humans and animals, special IOL forceps shaped as either tissue forceps or scissors have been and continue to be developed. These forceps are used
Fig. 1.7 Typing forceps have shaft with smooth platforms to provide flat surfaces to grasp fine suture material during tying. Some tying forceps have a combination shaft with distal 1 x 2 teeth to grasp tissues, and a more proximal smooth tying platform to grasp sutures. Top: Ogawa–Castroviejo tying forceps; bottom: Castroviejo suturing forceps.
Fig. 1.8 The distinct Colibri forceps have a characteristic angled shaft. Top: Troutman–Barraquer corneal fixation forceps (0.5 mm 1 x 2 teeth with a 6 mm tying platform); middle: Troutman–Barraquer corneal fixation forceps (0.5 mm 1 x 2 teeth); and bottom: Pierse-type Colibri forceps (0.03 mm Pierse-type tips).
to grasp the IOL or its haptic loop and to facilitate the placement of the IOL within the capsular bag or in the posterior chamber. It is important that these tips do not damage the IOL or its surface during insertion. Both hard (polymethylmethacrylate [PMMA] and acrylic) and foldable (silicone and hydrogels) IOLs have been available for the dog and cat for several years, but only recently for the horse and rabbit. IOLs may be custom made for exotic species if globe measurements and desired refractive power can be determined. With introduction of soft or foldable IOLs (which permit a smaller corneal incision), new forceps to fold or roll the IOL during insertion through the corneal incision and into the capsular bag or a specific injector or insertor are necessary. The foldable or ‘soft’ IOLs have become the most popular option for dogs.
Several IOL instruments have been developed to position and manipulate IOLs within the anterior chamber, posterior chamber, and the capsular bag. Most IOLs in the dog are placed in the capsular bag after all cataractous material has been removed. Placement of the IOL within the capsular bag requires a special forceps or injector; another instrument is used to rotate or dial the IOL into its final position. The IOL hook and lens manipulator possess different tips, with single or forked prongs, that
can push the IOL haptics into final position. Other instruments include iris hook, intraocular suturing hook, insertion hooks, suture assist hook, lens manipulator, push or pull iris hook, capsular support hook, lens dialer, no-hole manipulator, and others.
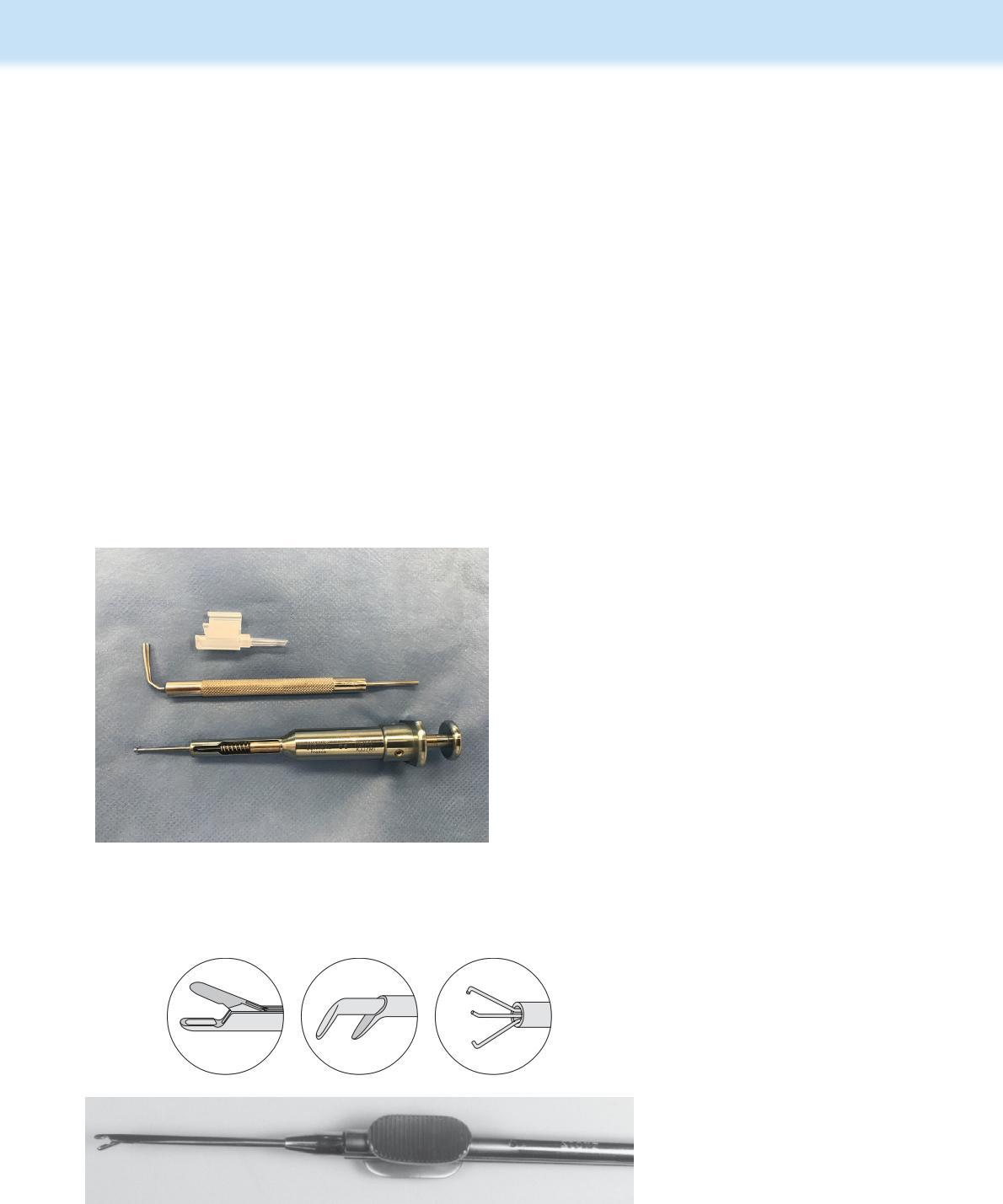
Within increased popularity of the soft intraocular lenses, several different inserters have been developed and may be used only for specific manufacturers’ IOLs (Fig. 1.9). They are loaded just before use, then inserted through the small corneal incisions and directed toward the capsular bag and anterior capsulectomy. The soft lens is injected very slowly, being careful to place the IOL properly into the capsular bag. Other instruments are used to rotate and adjust the IOL within the bag.
Intraocular Forceps
Special intraocular forceps have been developed to grasp and remove tissues or foreign bodies within the anterior chamber, posterior chamber, and the vitreous (Fig. 1.10). The intraocular forceps have 1.5 to 2.0 mm jaws and long shafts. The shafts are also small in diameter (20 g needle diameter; 0.89 mm) to accommodate insertion into the different compartments of the globe. The Rappazzo intraocular forceps has smooth, cusp or dusted jaws with a 45-° angulation. The Storz intraocular forceps has 1.5 mm cup-shaped oval jaws. Both of these intraocular forceps are used in animals to grasp and remove portions of the anterior lens capsule and portions of the lens cortex and nucleus.
Scissors
Several specific types of scissors have been developed to address the variety of different types of ocular tissue. No single scissors can perform adequately on the wide range of ocular tissues that one commonly confronts. As a result, specific-use scissors have been designed for the conjunctiva, cornea, corneosclera, iris, and intraocular tissues. The corneal and corneoscleral scissors are available as either standard size or microsurgical scissors. The overall length of the scissors’ ring handles is about 100 to 110 mm, and the blades are about 18 to 20 mm long.
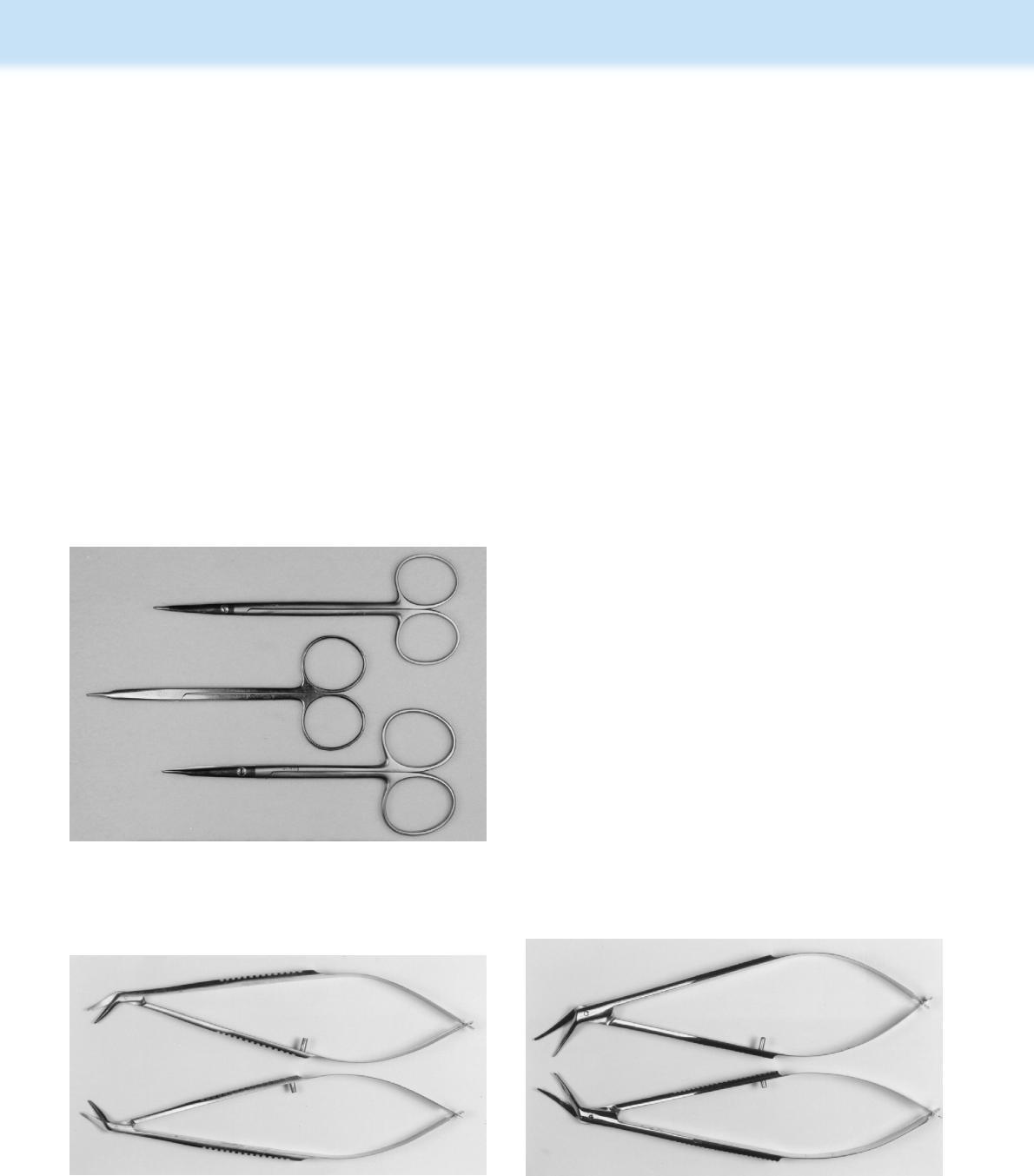
Conjunctival Scissors Conjunctival scissors include tenotomy, strabismus, eye, conjunctival, and utility types, and are available with either straight or curved tips (Fig. 1.11). The tips are also varied as both sharp (pointed), blunt, or a combination of both.
Fig. 1.10 The intraocular forceps is designed to be inserted through a very small opening. Insert shows the different available tip types.
Fig. 1.9 Instruments for injection of the soft intraocular lens (IOL). There are several injectors or inserters for the canine intraocular lenses (IOLs). Often, use of these injectors is limited to only a single manufacturers’ IOLs.
The handles are either ribbon-style, ring-type, or flat serrated spring-type handles; the latter types are more expensive. The versatile Stevens tenotomy scissors with slightly curved blunttipped blades is commonly favored. Conjunctival scissors with blunt tips tend to reduce the likelihood of producing ‘buttonholes’ or small full-thickness defects in the bulbar conjunctiva during preparation of conjunctival flaps.
These scissors may also be used to cut sutures. As most types of ophthalmic sutures are very small, one scissors within each surgical pack reserved for the express purpose of cutting sutures is recommended. The scissors to cut sutures often have pointed and sharp tips and can be easily distinguished from conjunctival tissue scissors.
Corneal Scissors The corneal scissors are available as either standard size or microsurgical types. Because dog and cat corneas are difficult to cut, these scissors should be of high quality to ensure precise incisions and minimal tissue trauma.
Periodic sharpening of these scissors may ensure long-term use. A large selection of corneal scissors is available (Fig. 1.12). These scissors can be used as a universal type or as pairs (right and left).
1.11 Selected scissors for conjunctival tissues with either straight or curved blades with sharp or blunt tips. Top: Knapp straight strabismus scissors; middle: Stevens straight tenotomy scissors; and bottom: Stevens curved tenotomy scissors.
The mirror-image pair types of corneal scissors complement each other, and are used to extend corneal incisions in opposite directions. The standard scissors range in total length is from about 100 to 120 mm long. The blades of these scissors are more curved than the corneoscleral scissors.
The microsurgical corneal scissors are usually approximately 90 mm long. The tips may be straight, slightly curved, or angled. Both tips may be of equal length, or the longer bottom tip that is inserted beneath the cornea is 0.5 to 1.0 mm longer to maintain the scissor tip within the anterior chamber as multiple cuts are performed. The corneal scissors used for keratoplasty possess tips that are quite curved (5 mm radius) and short as the standard full-thickness corneal graft for humans is usually 6 to 8 mm diameter. The corneal scissors used at the limbus have longer tips. These scissors may cut either vertically or obliquely. For most corneal incisions, vertical rather than oblique incisions are preferred, unless the incision is close to the limbus. To achieve a vertical cut, the lower blade of the corneal scissors is hinged to contact the inside of the concavity of the upper blade.
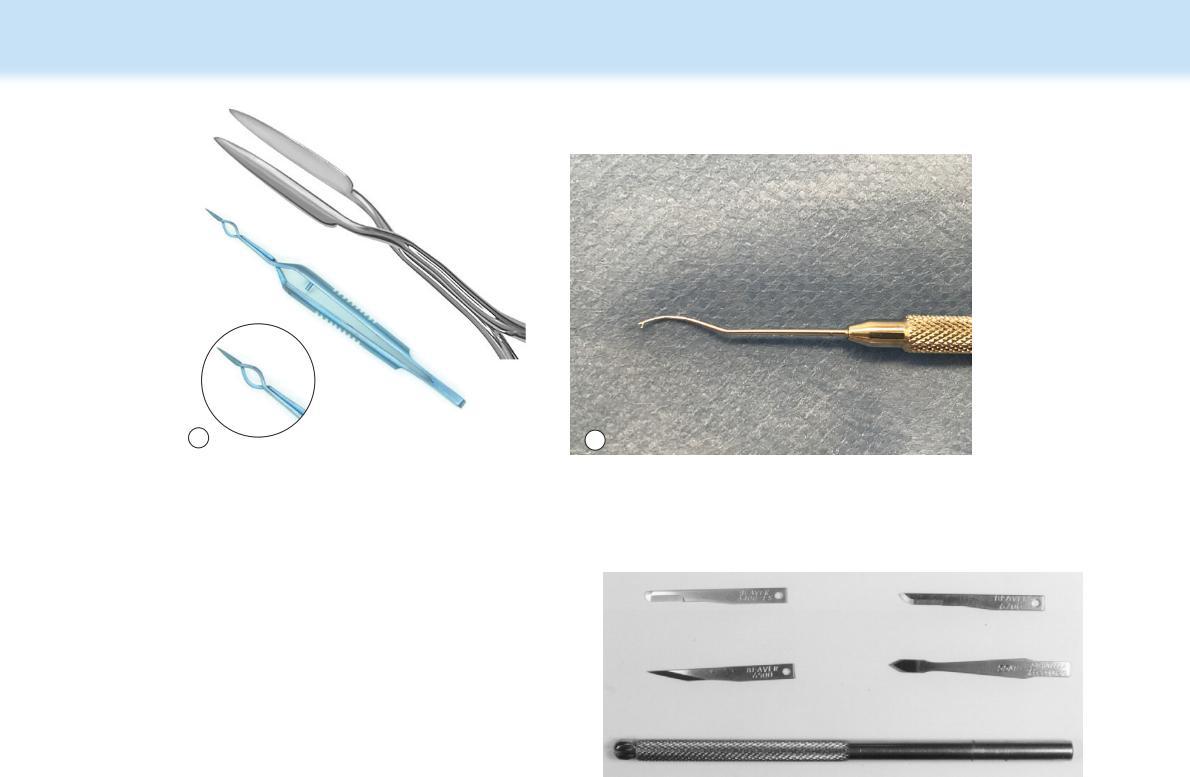
Corneoscleral or Corneal Section Cataract Scissors
Corneoscleral scissors are larger corneal scissors that are used at the limbus. Like corneal scissors, these are available as either standard or microsurgical types (Fig. 1.13). These scissors are usually self-opening with the flexible handles functioning as springs and loosely connected at their ends. Some types of these scissors have one rigid handle and the opposite flexible handle to maintain the scissors blades in an open position. Still other models look like regular scissors with straight handles.
The standard corneoscleral scissors are generally 100 to 120 mm long and have slightly angled and curved tips. The tips are about 12 to 20 mm long and often the bottom blade is 0.5 to 1.5 longer to maintain the scissor tip within the anterior chamber during repeated cuts of the limbus. In most corneoscleral or cataract section scissors, the lower blade cuts against the convex curve of the upper blade producing an oblique cut.
These scissors are used to cut the cornea, limbus, and sclera to perform keratoplasty, often in animals to enter the anterior chamber during cataract surgery. For maximum flexibility,
Fig.
Fig. 1.12 Castroviejo corneal section scissors (right and left) for keratectomy and keratoplasty. These scissors have more curved blades to cut the cornea or limbus; this curvature approaches the smaller corneal transplant diameters
Fig. 1.13 Castroviejo corneal section cataract scissors (right and left) for entry into the anterior chamber at the periphery cornea or limbus. The lower blade is longer, permitting the scissors to remain in the anterior chamber while cutting.
a slightly angled curved right and left pair of corneal section scissors is recommended. As most cataract surgery in animals uses a clear corneal incision for entry into the anterior chamber, these scissors should be of high quality for maximum durability.
Iris Scissors The animal iris is a very friable and vascular tissue that, upon incision, will often hemorrhage extensively. As a result, incision of the iris often necessitates light cautery before or after cutting to seal these vessels in most animal species. Iris scissors are small and delicate and are designed to cut the iris on a flat surface. These scissors must be very sharp, and their use should be limited to cutting only iridal tissues. Iris scissors include types by Vannas, DeWecker, and Barraquer, as well as the traditional ophthalmic scissors with ring or curled handles (Fig. 1.14). Their tips are usually pointed, variable in length, and slightly angled. The specialized Vannus and Barraquer iris scissors are quite small (54 mm long); the DeWecker iris scissors is 114 mm long. They can be easily inserted into the anterior chamber to perform a dorsal iridectomy or sphincterotomy. Because of the pronounced vascularity of most animal basal irides, incision/excision of the iris is usually performed with the section of interest extended from the anterior chamber or avoids the basal iris altogether. Limited electrocautery may be necessary to obtain complete hemostasis after incision of the iris and before repositioning into the anterior chamber.

Intraocular Scissors With refinement of intraocular surgical techniques, small scissors were developed to cut intraocular tissues, often through small corneal, limbal, or scleral incisions. There are two basic types: 1) standard ophthalmic scissors that can be inserted through a complete corneal or corneoscleral incision with very slender blades that are 10 to 15 mm long, and 2)intraocular scissors constructed like the intraocular forceps with a shaft diameter of about 1.0 mm (the outside diameter of a 20 g hypodermic needle). The handles of intraocular scissors may be spring type, barrel-squeeze handle, or the traditional rigid curled handles (Fig. 1.15). The tips are usually pointed and close as regular scissors or in a guillotine fashion. The blades of scissors inserted through 2 or 3 mm corneal or limbal incisions range from 1 to 3 mm long.
More recently, a subtype of intraocular scissors has been developed to insert through limbal or corneal incisions to cut the anterior lens capsule. These microsurgical capsulotomy scissors possess either straight or slightly angled pointed blades of 5 to 11 mm long. These scissors tips must be very sharp and their function limited to anterior capsulotomies or capsulectomies.
Instruments Used During Phacoemulsification
When phacoemulsification was first introduced in the 1970s by Kelman, the surgery involved one larger corneoscleral incision for the phaco handpiece (which provided the ultrasonic energy and aspiration) and a separate smaller incision approximately 90° to the larger incision to insert the infusion needle (balanced salt solution for the anterior chamber was provided by gravity from a bottle on an IV stand). Today’s phaco tips possess all three of these functions: 1) aspiration to remove lens material and aqueous humor, 2) infusion to regulate the amount of irrigating solution delivered to the phaco site, and 3) phaco (ultrasonic) energy to fragment and break down the lens material through a single incision.
A variety of instruments (quick chopper, nucleus segmenter, prechopper, etc.) are available for cracking or manipulating the lens before or during phacoemulsification. They may stabilize or chop (incise and divide) a hard lens nucleus. These instruments may be inserted through a second smaller corneal incision reminiscent of bimanual phacoemulsification of the 1970s. They are also inserted into the lens nucleus to lift and support lens fragments toward the phaco tip for fragmentation (Fig. 1.16a and b). An example is the Steinert nuclear chopping instrument that
Fig. 1.14 Special scissors for cutting the iris. Top: Barraquer iris scissors; bottom: McPherson–Vannas curved iris scissors. These scissors must be very sharp and never used to cut sutures.
Fig. 1.15 Intraocular scissors: Storz intraocular scissors; the straight blades are 3.0 mm long and pointed. Insert shows close-up of the cutting blades.
A B
Fig. 1.16 Instruments to assist during phacoemulsification. There are several instruments that can be inserted through the small corneal incisions and into the capsular bag to manipulate and rotate parts of the lens as well as divide (choppers) hard lens fragments. (a) Prechopper to divide hard lens fragments and reduce phaco time (insert shows the long blades that can reach the capsular bag from the corneal incision); (b) Probe to rotate or manipulate lens fragments. There are several differently shaped tips for these instruments.
possesses an angular tip with a wedge like end (1.5 mm) sharpened on its inner edge. This creates the chop of the nucleus while maintaining contact of the chopper with the nucleus; deep penetration of the nucleus is avoided to prevent posterior capsule penetration. Another intralens instrument is similar to a wire hook. Other examples include the Kavanagh nucleus sustainer and chopper, or the Jewelewicz Rosen chopper, which is used to stabilize the cataractous nucleus to chop the nucleus horizontally; their rounded tips offer some protection to the posterior lens capsule. Another example is the AW Brown nucleus cracker, which looks like scissors but its reverse action divides and ‘cracks’ the nucleus with the tips that look like tiny paddles. The Akahoshi prechopper has sharp tipped jaws that once inserted into the core of the lens nucleus will crack or divide the nucleus without sculpting, which reduces phaco time and energy. This instrument has a cross action mechanism that allows the jaws to fully open for cracking without stretching the incision or the capsule excessively.
Warren modified the Nagahara technique used in humans for the dog. This procedure uses the phaco tip to impale and with high vacuum, hold the lens nucleus while a chopper is hooked at the lens equator and pulled centrally, splitting the nucleus along its natural cleavage planes. By dividing the nucleus into quadrants or smaller parts using the chop technique and combined with the phacoemulsification ‘divide and conquer’ technique, phaco time and energy are significantly reduced, as is corneal endothelial cell damage.
Because the dog’s lens is larger than the human’s, Warren recommends using the human instrument for small dogs (1 to 2 mm tip) and has modified the Chang combination chopper for medium and large dogs (4 mm tip). For safety, the chopper’s tip is inserted into the nucleus to only one-half thickness. Some canine cataract cortices and nuclei are too hard to ‘chop’ or possess insufficient room for the instrument to pass between the anterior lens capsule and adjacent cortex, and are not amenable to this technique. Additional information on the chop techniques is found in Chapter 12 (Surgery of the Lens and Cataract).
Knives
The dog and cat cornea, limbus, and sclera are very tough tissues, and they will dull most stainless steel knives after only a few incisions. As a result, disposable blades are usually employed to ensure a sharp and atraumatic incision. The Beaver No. 64, 65, 67, and 69 blades are the most often used (Fig. 1.17). The Beaver No. 64 blade with the traditional shape is used to incise the cornea, limbus, and sclera. As an alternate, the Beaver blade No. 67 has a more pointed tip and is used for the same incisions. The Beaver No. 65 blade is pointed and used to incise the full-thickness of the cornea, limbus, and sclera. The Beaver No. 69 blade is configured similar to the No. 64 blade but has cutting surfaces on both sides of the blade. The Beaver keratomes are the preferred instrument with which to incise the cornea and the anterior lens capsule during cataract surgeries in small animals. This blade is arrow shaped, and as it is pushed through the cornea or limbus, both of its sides incise the full-thickness corneal, limbal, or scleral tissues. The incisions tend to self-seal, but in animals, they are often apposed by sutures.
The larger Bard-Parker Nos. 11 (pointed) and 15 scalpel blades and handle are not designed as microsurgical instruments. They are reserved for eyelid and orbital surgeries in both small and large animals. Even though these surgeries are not generally performed under an operating microscope, some
Fig. 1.17 Beaver disposable surgical blades: From Left to Right, top row (No. 64 and No. 67), middle row (No. 65 and keratome) and bottom row (Beaver scalpel handle).
magnification (2.5x to 6x) such as that achieved with surgical head loupes is recommended.
Diamond knives were introduced several years ago as a reusable scalpel blade and handle (see Chapter 4). This knife is used for corneal, limbal, and scleral incisions. A micrometer has been added to some types of the diamond knives to control the length of the blade and to perform corneal refractive surgery. The diamond blade shape ranges from an angle, spear like to rounded, and is 1.0 to 3.0 mm wide. These high-cost blades are very sharp and must be carefully used, cleaned, and stored.
Although a corneal dissector and restricted depth knife are not scalpel blades per se, these instruments are used to bluntly separate the corneal stromal layers. The corneal separators, like the Martinez and Gill corneal dissector knives, are used to bluntly dissect the different layers of the corneal stroma and reduce greatly the risk for progressive deeper separation of the cornea and corneal penetration. Disposable versions such as the crescent knife as available as well.
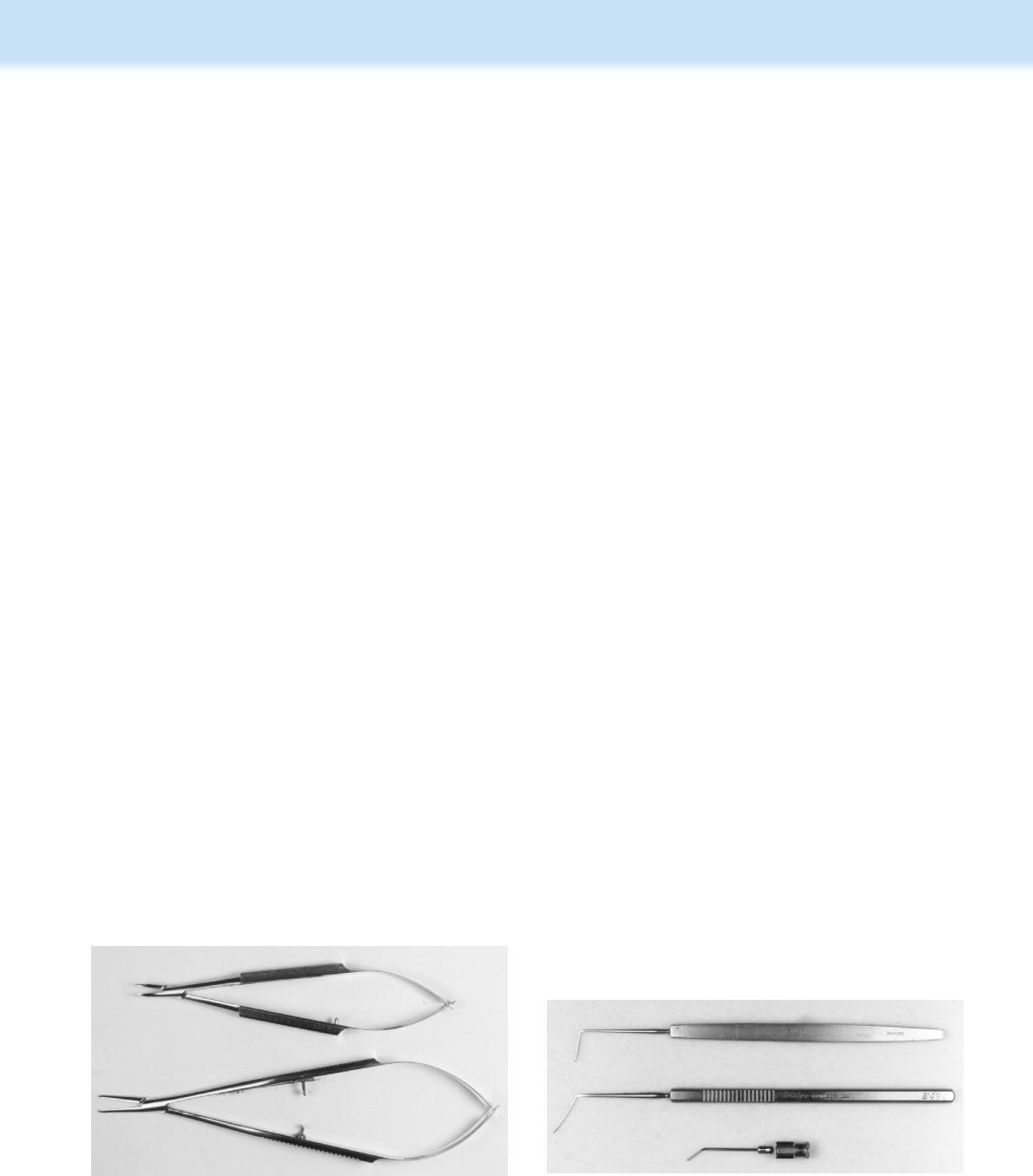
Needle Holders
Needle holders are very important in ophthalmic surgery because considerable time is consumed during the apposition of surgical incisions. Needle holders are available as either the standard models or the smaller microsurgical types (Fig. 1.18). Their tips are also divided into delicate, fine, medium, and heavy duty. The standard size needle holders are about 120 to 130 mm long, and the microsurgical types are about 100 mm long. The most common shape is similar to the corneal and corneoscleral scissors with flexible serrated or knurled handles are joined to provide a spring mechanism that automatically maintains the needle holder tips in the open position. Ophthalmic needle holders are designed to be held as a pencil.
For general extraocular surgery, the Castroviejo needle holder with flat serrated handles and a lock is often used. The jaws are about 9 mm long and may be straight or gently curved. For microsurgery involving the cornea, the Storz or Barraquer needle holder with curved jaws and no locks are preferred. All of the ophthalmic needle holders are designed for use only with small ophthalmic needles and sutures. Large needles and sutures larger than 4-0 will gradually distort these
needle holder’s jaws, rendering the instrument useless; hence, these instruments are not useful for tying the very fine ophthalmic sutures (special tying forceps are used instead). The straight to curved tips are 7 to 16 mm long, and their surfaces may be smooth or serrated.
Microneedle holders vary by the size of the jaw (delicate, fine, medium, heavy), straight or curved jaw, smooth or serrated jaw, locking or nonlocking, and the style of the handle. It is essential that the size of the instruments, specifically the jaw of the needle holder, used to grasp the needle correspond in size to match the needle selected. If the jaws of the needle holder are too large, they will deform and flatten the needle when compressed, straightening the needle and weakening it, resulting in breaking of the needle and/or inaccurate depth of suture placement and dehiscence. In contrast, if a microneedle holder is used to grasp a large needle, the converse is true, with the delicate needle holder jaws and hinge being damaged and sprung such that they will no longer hold the microneedles they were designed for. Microsurgical needles should be grasped slightly anterior of the midpoint. Grasping behind the midpoint (toward the swaged-on suture) will result in bending of the needle as it is advanced. Grasping too far forward of the midpoint may damage and dull the tip. When using a curved needle holder, the needle is grasped with the jaws curving upward. Although novice surgeons may prefer a locking needle holder, nonlocking needle holders are best for most ophthalmic procedures to avoid the jerking movement of the needle associated with release of the locking mechanism. Curved, nonlocking, round-handled Barraquer or Castroviejo-type needle holders are typically preferred for ophthalmic needles.
Spatulas/Retractors/Loops
These instruments are essential for specific functions during intraocular surgery. They include the cyclodialysis spatula, iris and extraocular muscle hooks, and the lens loop. The cyclodialysis spatula is used to bluntly create a space between the sclera and the underlying iris and ciliary body for the treatment of the glaucomas (Fig. 1.19). This instrument is about 120 to 140 mm long with a round to square serrated or knurled handle. Its tip is about 0.5 to 1.0 mm wide and 10 to 15 mm long with a blunt, rounded, or sharp end. This same design has also been incorporated into a cannula. This instrument can also be used to manipulate the iris, lens capsules, and vitreous.
Fig. 1.18 Top: Smaller microsurgical needle holder (made of titanium and 109 mm long) with no lock and curved 9 mm fine jaws; bottom: Standard Castroviejo needle holder (130 mm long) with lock and curved 9 mm jaws.
Fig. 1.19 Top: Two different cyclodialysis spatulas used for glaucoma and lens surgeries. The flat blade should be about 10 mm long and 1 mm wide, and has different angulations. Bottom: Cyclodialysis spatula combined with a cannula for injection into the anterior chamber.
The iris hook is designed to retract the pupillary aspects of the iris. These hooks are about 120 to 140 mm long and are constructed of either stainless steel or a nylon-like material (Delrin). These hook tips have a 1 to 3 mm curved end that is 1 to 4 mm wide and dull. Sharp or pointed iris hooks are not recommended, as tearing of the dog and cat iris will usually cause hemorrhage.
The muscle or strabismus hook is similar to the iris hooks with a much larger tip (Fig. 1.20). The instrument tip is angulated at 90° to facilitate placement under the extraocular muscles. These instruments are also used to rotate the globe.
The lens loop is another vital instrument for lens and cataract removal in small animals. The lens loop is positioned to slide the cataract and lens material from the corneal or corneoscleral wound. With its handle shaped like the iris and muscle hooks, the lens loop’s tip is designed as a circular to oval solid spoon or loop (Fig. 1.21). The overall size of these tips ranges from 0.3 to 6 mm wide and 7 to 15 mm long.
Cannulae for Intraocular Injections
Special cannulas are necessary for corneal and intraocular surgery. With a reusable silicone bulb or anterior chamber irrigator and cannula, lactated Ringer’s or saline solution is occasionally sprayed on the corneal and conjunctival surfaces to provide essential moisture (Fig. 1.22). These cannula range in size from 19 to 27 g. This same system is also used to reinflate the anterior chamber with air or fluids once the corneal or limbal surgical wound has been apposed (Fig. 1.23). The cannulas may also be shaped as cyclodialysis spatulas, providing for two functions. Special cannulas to inject air or solutions have specially constructed ends, such as olive tips, side ports, and hooks. To inject the more viscid viscoelastic solutions, a slightly larger diameter cannula may be necessary.
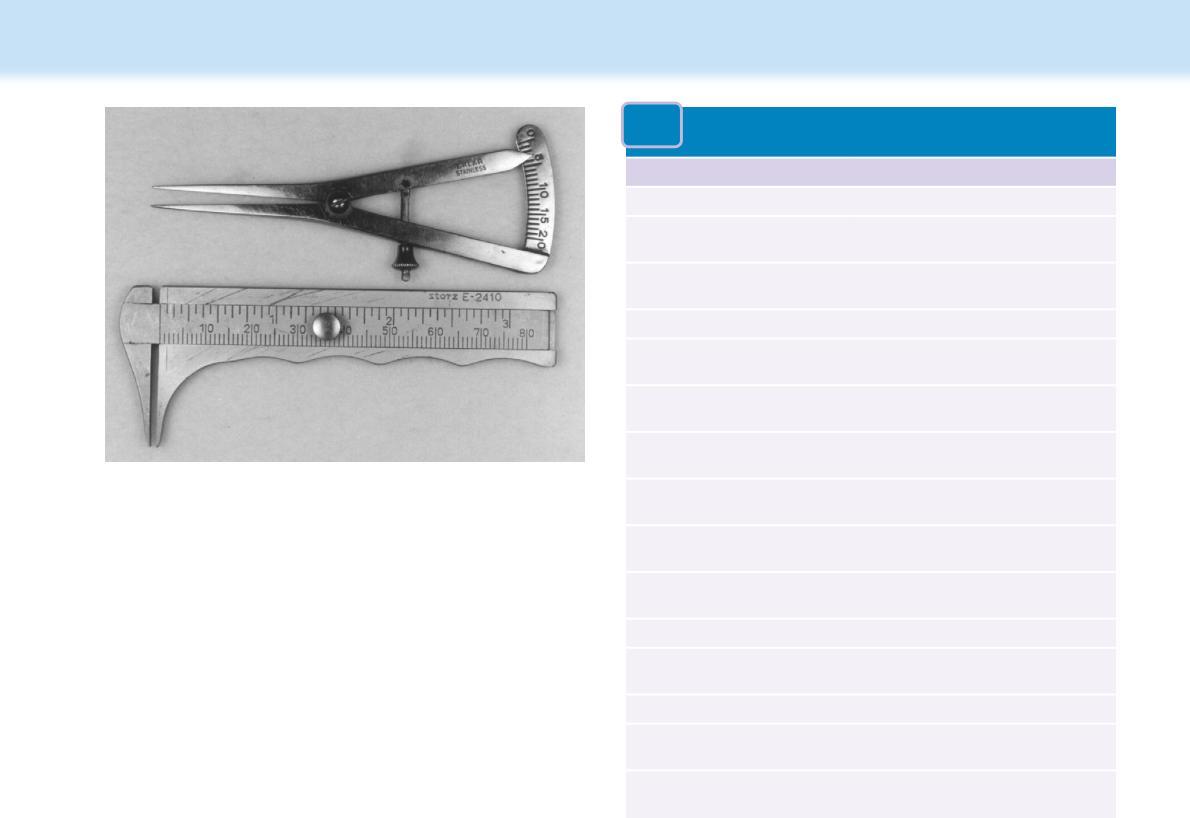
Calipers
During corneal, transscleral laser cyclophotocoagulation, cyclocryothermy, intraocular surgeries, intravitreal injections, and retinal detachment surgeries, it is very important to have precise size and distance measurements between intraocular tissues. Several types of calipers are available that can be sterilized and should be part of the standard ophthalmic surgery instrument pack. These instruments permit measurements up to 800 mm in 1 mm or 0.5 mm increments. The Jameson and Castroviejo calipers are the most frequently used (Fig. 1.24).
Rings
Two types of rings are available for ophthalmic surgery. These include the external Flieringa and modified stainless steel single and double rings and internal capsular rings to insert within the capsular bag to expand the equatorial capsule. Although the
1.20 The strabismus or muscle hook is placed under the extraocular muscle to facilitate identification of their insertions as well as rotate the globe. Top: von Graefe strabismus hook; bottom: Jameson muscle hook has 6 mm hook with a 2 mm bulbous tip and a flat serrated handle. The tip may also be used for scleral depression during examination of the peripheral fundus.
Fig. 1.22 Silicone bulb and cyclodialysis cannula to irrigate the anterior chamber with lactated Ringer’s solution, balanced salt solution, or saline.
1.21 The lens loop is used to facilitate sliding the lens from the eye. The loop may be different sizes and shapes. Top: New Orleans lens spoon has a 3 mm wide by 14 mm long slightly curved spoon on a 134 mm long flat serrated handle; bottom: Gills–Welsh modified lens loop with a 6 x 7 mm loop.
Fig. 1.23 Ophthalmic cannulas may vary in diameter, length, shape, and purpose. Top: Air injection cannula (27 gauge); middle: Castroviejo cyclodialysis cannula (21 gauge); and bottom: Bracken anterior chamber cannula. The latter two cannulas are used to inject solutions; for viscoelastics larger bore (18–19 g) needles are necessary.
Fig.
Fig.
TABLE 1.2
human elliptical cornea is about 7 × 8 mm in diameter, the dog and cat corneas are considerably larger (dog: 16 × 15 mm, and cat: 17 × 16 mm). Larger Flieringa rings can be used for dogs and cats, with 20 to 22 mm diameter recommended.
Flieringa rings are attached around the cornea or limbus with 4 to 6 nonabsorbable simple interrupted sutures to prevent globe and anterior chamber collapse as during full-thickness or penetrating keratoplasty. These rings are removed once the corneal wound has been apposed.
Capsular tension rings have been introduced to expand the capsular bag after phacoemulsification and facilitate insertion of an IOL. U-shaped, capsular tension rings are available in 12.5, 13.5, and 14.5 mm diameters for the dog.
Adaptations for Large Animal and Special Species Ophthalmic Surgeries
Because the veterinary ophthalmologist may be confronted with animal species that range in size from an elephant to a parakeet or sometimes even smaller, surgical instrumentation is often determined by the size of the patient’s eye and the availability of anesthesia. Fortunately, the elephant’s eye is similar in size to the horse’s, but for the parakeet, even a 25- or 27-gauge needle is very large.
For the larger animal species, the standard soft tissues surgical instruments are used for orbital and eyelid surgeries. For conjunctival grafts, corneal and intraocular surgeries, either the standard ophthalmic or microsurgical instruments are used. If the operation microscope is used, microsurgical ophthalmic instruments are recommended. Needle type and suture selection is similar for all species. The very smallest of species will require the smallest of sutures.
Surgical Instruments for Ophthalmic Surgeries
Because ophthalmic surgeries are generally confined to certain ocular tissues, the development of specific surgical packs is
General Surgical Instruments for Orbital Surgeries
Instrument Purpose
Allis tissue forceps To hold and position tissues
Bard–Parker handle and blades Incise the eyelids
Bishop–Harmon forceps, toothed To grasp nictitans and conjunctiva
Cannula: 19 g For irrigation of the external eye
Enucleation scissors, large, curved To incise the optic nerve
Eyelid speculum, wire To retract the lids and maintain the palpebral fissure
Wet field or disposable cautery
Hemostasis
Jameson muscle hook To manipulate the extraocular muscles
Metzenbaum scissors, medium
Mosquito forceps, (2 curved, 2 straight)
To incise and separate the orbital tissues
To grasp tissues and for hemostasis
Needle holder, medium To grasp and manipulate needle
Saline bowel, small Hold saline for moistening of tissues
Silicone bulb for irrigation To irrigate the external eye
Tenotomy scissors, curved To incise the conjunctiva and nictitans
Towel clamps, (4 large, 4 small)
To maintain the surgical drapes
recommended. Surgical packs are designed to limit the number of instruments anticipated for a surgery and to reduce the number times an instrument requires cleansing, autoclaving, and nonsurgical manipulations. Highly specialized ophthalmic instruments are best individually wrapped and sterilized, and used with care and precision.
The instrumentation used in ophthalmic microsurgery begins with a basic ophthalmic microsurgical pack for eyelids, orbit, and other adnexal procedures (Table 1.2) but will then expand to include specialized microsurgical packs for cornea, cataract, or posterior segment work (Table 1.3). Phacoemulsification, irrigation/aspiration and vitrectomy, cryosurgery, laser, wet field cautery, and vitreoretinal instruments will often have their own surgical packs. The particular style of a specific instrument is often a matter of surgeon preference. Most surgeons will have several basic or minor ophthalmic surgical packs that will be used for adnexal and orbital procedures, and several major ophthalmic microsurgical packs designed for cornea, cataract, and other anterior segment procedures. A basic ophthalmic pack will typically contain an eyelid speculum (Barraquer wire in several sizes), forceps (Brown–Adson, Colibri, Bishop–Harmon, scleral fixation, tying), scissors (Stevens and Westcott tenotomy), needle holders (large and small curved, nonlocking Barraquer type, and Derf or Alabama-Green type), Desmarres chalazion
Fig. 1.24 Calipers for measurements during corneal and ocular surgeries. Top: Castroviejo; bottom: Jameson calipers.
TABLE 1.3 Surgical Instruments for Eyelid Surgeries
Instrument Purpose
Towel forceps (4-large/4-small)
Wire eyelid speculum (Barraquer)
Small curved Mayo scissors (Mayo/Metzenbaum)
To secure the drapes to the patient
To retract the lids and expose the conjunctiva/nictitans
To perform lateral canthotomy
Stainless steel cup Hold saline/lactated Ringer’s solution for ocular irrigation
Silicone bulb and cannula Periodically moisten the eye
Entropion/chalazion forceps
With oval to round ring and solid base plate. Designed to clamp and stabilize the lid.
Cilia forceps With smooth tips designed to epilate cilia
Bishop–Harmon forceps
Tissue forceps-1 x 2 teeth (0.3 mm)
Lid plate
Both serrated and 1 x 2 teeth tips. Good general tissue forceps.
Grasp conjunctiva
Plastic or stainless steel. Holds the lids taunt and protects the cornea from surgical manipulations.
Beaver scalpel handle Use No. 64, No, 67, or No. 69 Beaver blades; to incise eyelid skin/conjunctiva
Standard needle holder (Castroviejo/Barraquer)
Tenotomy scissors (Stevens) Curved/straight
Fine mosquito hemostatic forceps
Standard size recommended to accommodate the larger needles and suture sizes. Some prefer holders with a lock device.
Two different sizes recommended. Blunt tips preferred.
Hemostasis
clamp Jaeger eyelid plate, calipers (Jameson, Castroviejo), Carter sphere introducer, muscle hooks, irrigating cannulas, and Beaver and Bard-Parker blade handles. Additional instruments may include mosquito hemostats, Martinez corneal dissector, serrefine clamps, cyclodialysis spatula, and other specific instruments according to the surgeon’s preference. For a microsurgical corneal/intraocular pack, many of the same instruments will be included but will have more delicate teeth and jaws. Additional instruments in a microsurgical pack may include intraocular scissors and forceps such as the Vannas scissor and Utrata forceps, lens loop, intraocular lens (IOL) forceps, IOL manipulators, phaco choppers, or other specific instruments according to surgeon preference. In addition, a drape pack containing towel clamps, drapes, scissors, and a sterile bowl are used so that these instruments are not wrapped with the more delicate ophthalmic instruments. If vitreoretinal procedures are performed, this may require an additional set of microsurgical instruments. In addition, specialized packs for phacoemulsification or other procedures requiring specialized instrumentation may be indicated.
All microsurgical instruments should be stored in a specialized tray with a lid to protect them from damage and prevent them from contacting each other. Surgical packs should be
organized so that the fewest possible instruments will be used and subsequently cleaned and sterilized. Instruments that are not used on a routine basis should be wrapped and sterilized individually to minimize wear and tear on the instrument associated with cleaning and autoclaving. Repeated cleaning and sterilization, while necessary, is damaging over time to instruments. Immediately before initiating surgery, all instruments that will be required for the procedure should be selected, removed from the microsurgical tray, and arranged on the surgical table in the order they will be used. Once used, they should be returned to the surgical table in the same order so both the surgeon and assistant surgeon can find them quickly.
A pack designated for surgery of the external eye and adnexa is used to drape the surgical area, expose the globe, and perform and repair lateral canthotomies. The external instrument packet should contain small towel clamps, small saline bowl, silicone irrigator for solutions to maintain the cornea and conjunctiva moist, a few small hemostats, ophthalmic tissue forceps, strabismus, utility or tenotomy scissors for ocular tissues and sutures, small serrated and 1 x 2 teeth thumb forceps, knife handle and blades, and one or more eyelid specula.
A minor intraocular surgical pack should provide the essential surgical instruments for corneal, glaucoma, and iris-ciliary body surgeries. The instruments in this packet can also be used to perform conjunctival grafts, superficial keratectomies, and primary closure of corneal ulcerations, and to treat partial to full-thickness corneal lacerations with an iris prolapse. This pack is exclusively ophthalmic instruments with small serrated, 1 x 2 teeth corneal utility forceps and tying forceps; curved and straight ocular scissors (Wescott scissors); cyclodialysis spatula; standard and micro ophthalmic needle holder; and corneal and anterior chamber irrigators. Special ophthalmic instruments, such as a corneal dissectors, handheld cautery units and iris scissors, and intraocular forceps and scissors, should be individually wrapped, sterile and ready for use, and easily accessible within the operating room.
A more complete intraocular surgical pack provides the instrumentation for cataract and lens removal and surgeries of the posterior segment. The instruments in this pack include corneal section scissors, different types of tissue and tying forceps, lens loop, cyclodialysis spatula, two or more cannula, extracapsular lens forceps, forceps for tearing of the anterior lens capsule (capsulorrhexis) such as Utratas, and one or two different size needle holders. Other instruments, individually wrapped and sterile, should include iris scissors, intraocular scissors, and intraocular forceps. Some backup instruments should be available in case contamination or malfunction of instruments occurs during the surgical procedure.
Additional ophthalmic microsurgical instrumentation may include a cryosurgical unit for eyelid and lens luxation procedures; phacoemulsification machine with irrigation, aspiration, phacoemulsification, and vitrectomy abilities; wet-field cautery; diode laser with indirect, transscleral, microscope, intraocular, and endocyclocoagulation attachments; CO2 laser; fluid–gas exchange pumps for vitreoretinal surgery; viscous oil injection and aspiration; corneal donor and recipient trephine devices for corneal transplantation; and other additional instrumentation depending on the surgeon’s interest and capabilities.
RECOMMENDED INSTRUMENTS FOR ORBITAL SURGERIES
Although the majority of the extraocular surgical procedures can be performed with general soft tissue instruments, the investment in ophthalmic surgical instruments will not only rapidly repay the surgeon the initial purchase costs but also provide greater success rates for all patients. General soft tissue surgical instruments are used for most of the orbital surgical procedures and some of the more extensive eyelid surgeries (see Table 1.2). Orbital surgery may also require some orthopedic instruments to transect and reappose the zygomatic arch when an orbitotomy is planned. Small Allis tissue forceps can be used to grasp and retract the orbital and eyelid tissues. Small Halsted mosquito forceps with straight and curved jaws are used for hemostasis by control of point bleeders, especially of the orbit, eyelids, and conjunctivae. Larger Kelly and Crile hemostatic forceps with either straight or curved jaws permit grasping larger areas of tissues and are especially useful for orbital surgery. The curved Metzenbaum scissors, especially the smaller types, are indicated for delicate orbital and eyelid tissue dissections. The Metzenbaum scissors should not be used to cut sutures. The heavy-duty Mayo dissecting scissors are useful for the cutting of dense connective tissues of the orbit in large dogs. Straight Mayo scissors, usually 6" long, are indicated for cutting sutures, especially sutures larger than 4-0. A good quality Mayo-Hegar needle holder is excellent for needles and suture sizes (4-0 to 3-0) that are used for the majority of the orbital and eyelid surgical procedures.
The Semkin and Adson tissue forceps may be used for orbital, eyelid, and conjunctival tissues, but the smaller ophthalmic fixation forceps may be less traumatic for these tissues. The Bard-Parker scalpel handle, with number 10 and 15 surgical blades, is used to incise orbital and eyelid tissues in small and large animals. The Beaver knife handle with several types of surgical blades (usually the No. 64, No. 65, and No. 69) is the most common knife for the ocular tissues of animals.
A few general surgical instruments are usually part of any corneal or intraocular surgical instrument pack. At least four small or bulldog towel clamps, and four larger towel clamps, small thumb forceps, small curved Metzenbaum scissors, and a small needle holder, such as a Derf, are used initially to improve exposure of the cornea and globe, and to perform the lateral canthotomy. Microsurgical instruments should not be used for the eyelids; these large tissues will eventually bend and disable these delicate instruments.
RECOMMENDED SURGICAL INSTRUMENTS FOR EYELID SURGERIES
Although most eyelid and nictitans surgeries can be performed with general surgical instrumentation, several instruments have been developed for specific lid surgical manipulations. As a result, a special eyelid surgery pack may be used using the standard size ophthalmic surgical instruments (see Table 1.3 ).
RECOMMENDED SURGICAL INSTRUMENTS FOR CONJUNCTIVAL AND CORNEAL SURGERIES
For conjunctival, corneal, and intraocular surgery in small animals, a number of instruments is essential. Often, a combination of the standard and microsurgical ophthalmic instruments are included into a standard surgical pack. The corneal instrument pack should have a limited numbers of instruments. Additional infrequently used but essential ophthalmic instruments are individually packaged and sterilized, and can be used as needed. As the basic pack instruments are repeatedly cleaned and sterilized, these instruments can be subjected to considerable wear. A list of surgical instruments for a typical corneal surgical pack is summarized in Table 1.4. These instruments
TABLE 1.4
Surgical instruments for Conjunctival and Corneal
Surgeries
Instrument
Purpose
INSTRUMENTS FOR BOTH SURGERIES
Towel clamps (8) Secure surgical drapes
Small curved Mayo scissors (Mayo/ Metzenbaum) Lateral canthotomy
Stainless steel cup Hold saline/lactated Ringer’s/ balanced salt solution
Silicone bulb and cannula Periodically moisten the eye
Wire lid speculum (adult/pediatricBarraquer, several sizes) Retract eyelid/expose cornea
Small needle holder Suture lateral canthotomy
Tissue forceps-1 x 2 teeth (0.5 mm, 0.3 mm & 0.12 mm) Grasp conjunctiva/cornea
Beaver scalpel handle (Blades No. 64, No. 65, No. 69) Incise cornea
Tenotomy (Stevens) scissors Cut conjunctiva/sutures
Wescott tenotomy scissors (blunt, curved) Incise conjunctiva
Castroviejo needle holder (nonlocking) Use with 5-0 to 10-0 sutures
Fine mosquito hemostatic forceps To grasp tissues, separate Tenon’s/hemostasis
FOR CORNEAL SURGERIES
Corneal section scissors (right/left pair) Cut cornea, limbus, or sclera
Martinez or Gill dissector Bluntly separate corneal stromal layers
Crescent knife Separate corneal stromal layers
Calipers
Operative measurements
Cyclodialysis spatula Manipulate iris, lens, vitreous
Disposable ophthalmic cautery or wet-field cautery
Hemostasis/cut iris
Corneal trephines (5–9 mm) For keratoplasty
Microsurgery needle holder For keratoplasty
accommodate all of the surgical procedures, except for partial and full-thickness corneal grafts (keratoplasty), including bulbar and palpebral conjunctival grafts, corneoconjunctival and corneoscleral transpositions, superficial and deeper keratectomies, partial- and full-thickness corneal lacerations, removal of partial- and full-thickness corneal foreign bodies, and limbal surgeries. The instrumentation for corneal grafts is not extensive but very specific. Because the dog and cat corneas are very tough, the corneal scissors and trephines must be very sharp.
RECOMMENDED SURGICAL INSTRUMENTS FOR INTRAOCULAR SURGERIES AND CATARACT EXTRACTIONS
The instrumentation to perform all iris–ciliary body, glaucoma, cataract, and lens removal surgical procedures is summarized in Table 1.5. More instruments are necessary for lens and cataract surgeries than for glaucoma and anterior uveal surgical procedures. The selection of these instruments should serve only as a guide; individual preferences for specific instruments, based on shape and size, vary.
Instruments for Vitreoretinal Surgeries
Vitreoretinal surgeries require additional training for veterinary ophthalmologists. With a limited number of veterinary vitreoretinal surgeons available, this type of surgery represents a new and exciting frontier for veterinary ophthalmology. For vitreoretinal surgeries, highly specialized instruments, which are expensive, are necessary (Table 1.6). Additional information of these instruments and their use is available in Chapter 13 (Vitreoretinal Surgeries). In general, vitreoretinal instruments are classified by gauge (20, 23, or 27; the first two gauges are now used in veterinary ophthalmology. The smallest gauge (27 g) was introduced several years ago, and continues to grow in popularity in human retinal surgeries. The smaller the gauge, the more delicate instruments are preferred as the experience of the surgeon grows. The smaller the instrument, the more delicate.
Ophthalmic Sutures and Needles
The general rule stating that the strength of the suture should approximate the surrounding tissues also pertains to ophthalmic sutures. With improvements in suture material and their needles, progressively smaller sizes have evolved. For surgery of the orbit, suture size approximates that of general soft-tissue surgery, with 3-0 to 5-0 absorbable sutures used for ligation and closure of the deeper orbital fascia tissues. Skin closure is usually with nonabsorbable 4-0 to 5-0 nylon, polypropylene, polyester, Dacron, or silk.
For surgery of the eyelids, 4-0 to 6-0 sutures are recommended with the absorbable sutures buried and the skin apposed with nonabsorbable 4-0 to 5-0 single interrupted sutures. Most conjunctival and corneal sutures are absorbable (to eliminate
TABLE 1.5
List of Surgical Instruments for Intraocular Surgeries
Instrument Purpose
Towel clamps (4 large/4 small)
Small curved Mayo scissors
Saline cup/bowl
Silicone bulb and cannula (cannula-19 g/25 g)
Secure surgical drapes
Lateral canthotomy
Hold saline/lactated Ringer’s/ balanced salt solution
Periodically moisten the eye
Eyelid speculum (adult/pediatric) Retract eyelid/expose cornea
Small needle holder
Tissue forceps-tooth/smooth (0.3 mm & 0.12 mm)
Tying forceps
Beaver scalpel handles (blades No. 64, No. 65, No. 67 and keratome)
Suture lateral canthotomy
Grasp conjunctiva/cornea
Grasp sutures
Incise cornea/limbus/sclera
Tenotomy scissors (Stevens) Cut conjunctiva
Utility scissors
Wescott tenotomy scissors (curved, blunt)
Corneoscleral scissors (right/left pair)
Iris scissors
Extracapsular lens forceps
Capsulectomy forceps (Utrata)
Lens loop
Cyclodialysis spatula
Cut sutures
Harvest conjunctiva
Incise cornea/limbus/sclera
Incise iris
Grasp anterior lens capsule
Tear/remove anterior lens capsule (capsulorrhexis)
Slide lens from eye
Separate tissues
Muscle hook (Jameson) Rotate globe/expose muscle insertions
Needle holder (Castroviejo)
OTHER
Calipers
Disposable cautery (sterile)
Wet field cautery
Intraocular forceps
Intraocular scissors
Vannas capsulotomy scissors
IOL forceps/hook
Suturing
Operative measurements
Hemostasis/cut iris
Hemostasis/cut iris
Grasp/remove lens capsule/ fragments or foreign bodies
Cut anterior lens capsule
Cut anterior lens capsule
Position or dial intraocular lens
the need for suture removal), and 6-0 to 8-0 in size to minimize tissue reaction.
The different ophthalmic sutures and their characteristics are listed in Table 1.7 (also see Chapter 4). Often, the choice of the skin sutures is personal preference and nearly always the nonabsorbable type. However, in some exotic small animals, skin suture removal may be impractical because of restraint, and absorbable subcutaneous or skin sutures are employed. For fractious patients or those in which a large number of sutures