Retinal Degenerative Diseases XIX
Mechanisms and Experimental Therapy
Editors
John D. Ash
Department of Ophthalmology
University of Pittsburgh School of Medicine
Pittsburgh, PA, USA
Robert E. Anderson
Health Sciences Center
University of Oklahoma Health Sciences Center
Oklahoma City, OK, USA
Joe G. Hollyfeld
Department of Ophthalmology
Cleveland Clinic Lerner College of Medicine
Cleveland, OH, USA
Eric Pierce
Ocular Genomics Institute
Department of Ophthalmology
Massachusetts Eye and Ear Infrmary
Harvard Medical School Boston, MA, USA
Catherine Bowes Rickman
Department of Ophthalmology
Duke Medical Center Durham, NC, USA
Christian Grimm
Laboratory for Retinal Cell Biology
Department of Ophthalmology
University Hospital Zurich University of Zurich Schlieren, Switzerland
ISSN 0065-2598
ISSN 2214-8019 (electronic)
Advances in Experimental Medicine and Biology
ISBN 978-3-031-27680-4 ISBN 978-3-031-27681-1 (eBook) https://doi.org/10.1007/978-3-031-27681-1
© The Editor(s) (if applicable) and The Author(s), under exclusive license to Springer Nature Switzerland AG 2023
This work is subject to copyright. All rights are solely and exclusively licensed by the Publisher, whether the whole or part of the material is concerned, specifcally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microflms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifc statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors, and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, expressed or implied, with respect to the material contained herein or for any errors or omissions that may have been made. The publisher remains neutral with regard to jurisdictional claims in published maps and institutional affliations.
This Springer imprint is published by the registered company Springer Nature Switzerland AG The registered company address is: Gewerbestrasse 11, 6330 Cham, Switzerland
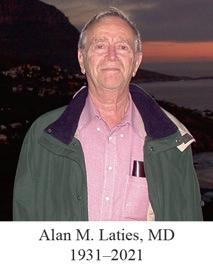
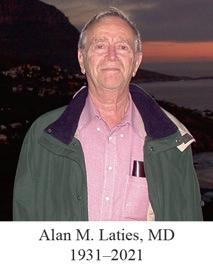
The editors are pleased dedicate this publication to the memory of our long-time friend and colleague, Alan M. Laties. Except for the most recent years, Alan attended each of these biennial retinal degeneration meetings since they began in 1984. Early on Alan recognized the importance of our attempt to provide a continuing international platform for discussions and scientifc exchange to take place among investigators focused on retinal degeneration research. Through his scientifc leadership at the Foundation Fighting Blindness (formerly the Retinitis Pigmentosa Foundation), we received the frst meeting grant to partially cover some of the expenses of the RD meeting held in San Francisco in 1988. The Foundation has provided continuing support for each of the subsequent meetings in the form of travel grant support for young investigators.
Born in Beverly, Massachusetts, the son of Russian immigrants, he attended Harvard College (BA, 1954) and completed medical school at Baylor College of Medicine (MD, 1959), followed by a residency in ophthalmology in the Hospital of the University of Pennsylvania (1961–63). A United States Public Health Service Special Research Fellowship supported his
research training in the Institute of Neurological Sciences at the University of Pennsylvania (1963–64). He joined the faculty at the University of Pennsylvania in 1965 where he moved through the academic ranks until retiring as Emeritus Professor of Ophthalmology at the Perelman School of Medicine in 2020. He held joint appointments in Ophthalmology and Neurology where he was the Irene Heinz Given and John LaPorte Given Research Professor and the Harold G. Scheie Research Professor in Ophthalmology. He served as neuro-ophthalmologist at the Hospital of the University of Pennsylvania while pursuing basic research on the autonomic innervation of the eye, eye growth, and therapeutic approaches to eye diseases. He has published 140 original research papers, 30 review articles, and presented numerous invited lectures at major university medical centers around the world on a variety of topics critical to the treatment of diseases of the eye. He was an inventor holding multiple patents in the area of ophthalmology.
In the early 1970s, Alan was approached by the Retinitis Pigmentosa Foundation to help them develop a scientifc plan to support targeted research that would lead to an understanding of the causes of retinitis pigmentosa. At the time, it was recognized that these diseases were inherited, but only in a very limited way (autosomal dominant, recessive or X-linked). At the time, no mutations causing RP had been identifed and the Human Genome Project would not be initiated for another 20 years. Alan agreed and organized the frst Scientifc Advisory Board for this Foundation and served as Chairman. In this leadership role, Alan helped identify and direct funding to the frst laboratory focused on degenerative retinal disease research, the Berman-Gund Laboratory at the Massachusetts Eye and Ear Infrmary, Harvard University. Research Centers focused on retinal degeneration would later be expanded to many medical centers in North America, England, and Europe. Alan recognized the importance and need for animal models with these inherited retinal diseases and directed funds from the Foundation to support the development of the dog models with RP identifed by Dr. Gustavo Aguirre at the College of Veterinary Medicine. In the early 1980s, Alan initiated a scientifc plan for the Foundation to identify the major genes responsible for RP. This led in 1989 to the discovery of a mutation in the rhodopsin gene
responsible for an autosomal dominant form of retinitis pigmentosa. Discovery of mutations in other genes causing retinitis pigmentosa quickly followed. With the discovery of RP-65, a gene that causes a recessive form of RP, gene therapy in a dog model with this recessive disorder could be quickly initiated because of Dr. Laties’ early support from the Foundation of these dog model lines. Dr. Laties’ early leadership was hugely important to gene therapy clinical trials and a number of other therapies related to these inherited retinal diseases. To honor Dr. Laties, the Foundation Fighting Blindness named their physicians’ and physician-scientists’ career development award the Alan Laties Career Development Program and honored him with the inaugural Llura Liggett Gund Lifetime Achievement Award.
Dr. Laties was a gifted scientist, outstanding leader, and compassionate human who enriched the lives of his contemporaries. He played a key role in nurturing and expanding research in inherited retinal diseases. He is survived by his wife Deena Gu, a distinguished artist, daughter Jane Laties, sons Alex P. Laties and Nicholas P. Robinson, and a brother, David.
Preface
The XIX International Symposium on Retinal Degeneration was held from September 26 to October 2, 2021. The symposium was initially planned for October of 2020 in Mendoza, Argentina. However, the global pandemic made this meeting impossible. With the availability of vaccines, we decided in March of 2021 that it would be possible to organize the meeting for late September of 2021. From the beginning, we planned the meeting as an inperson meeting with the capability of switching to a hybrid or fully online meeting depending on the state of the pandemic, and we moved the in-person meeting to the United States to reduce travel complications for most attendees. As the delta variant began to surge in the weeks leading up to the meeting, we had to activate the hybrid meeting. The meeting platform we established allowed both in-person and virtual platform talks as well as both in-person and virtual attendance. The platform was organized so that all presentations were live and all participants were able to ask questions. All presentations, including posters, were recorded and made available 4 months after the meeting. The in-person sessions were held in the Sonesta Nashville Airport Hotel in Nashville, TN. Because of COVID concerns, the in-person attendance was small (118 scientists) compared to previous meetings (~250 scientists), but the overall attendance increased to 344 attendees. The virtual option was the main driver for the increase in attendance. The meeting program included four outstanding keynote presentations from Michael Chiang, Director of the National Eye Institute on Artifcial intelligence for clinical care and research; Douglas Wallace, National academy of Science member and Professor at the University of Pennsylvania on Mitochondria and the etiology of disease; David Gamm, Professor at the University of WisconsinMadison on Ultrathin micromolded 3D scaffolds for outer retina reconstruction; Valeria Canto-Soler, Professor at the University of Colorado on Human iPSC-derived 3D retinal tissue for stem cell-based therapies for retinal degenerative diseases. Drs Chiang and Wallace presented via the virtual platform, while Drs Gamm and Canto-Soler presented from the podium. The program also included 41 platform talks, with 28 presented in person from the podium and another 13 presented virtually. In addition, 143 posters were presented as short talks on the virtual platform. Seventy-three of the posters were also presented in person during two well-attended poster sessions. New and important data were presented at the meeting, and we were mentioned in a written article published on NPR, and several attendees were interviewed by reporters from Science and other journals.
The RD2021 Travel award competition was highly successful at attracting qualifed applicants. We received a 35% increase in TA applications for a total of 196. The applications were reviewed by a panel of 14 expert reviewers, including 6 women, 8 men, and sceintists from a recognized underrepresented minority (URM). Since funding from European sources is dedicated to European early career scientists, we included three reviewers from Europe. Many of the panel members have been prior travel awardees. Each application was assigned four reviewers, and reviewers independently scored applications on a 1–9 scale. Based on scores, the applications are ranked and slotted into funding sources based on funding agency criteria. We were able to support full travel awards for 60 in-person early career scientists and another 41 virtual early-career scientists. This is the largest pool of awardees at an RD meeting. The awards were balanced between men and women. In addition, we implemented a new diversity and inclusion policy and dedicated a minimum of six awards to underrepresented minorities (URM). In the end, we were able to fund 11 URMs to attend the RD meeting.
Although the pandemic made the RD2021 meeting more complex and more challenging to organize, the RD2021 meeting was, by all accounts, a terrifc success.
Pittsburgh, PA, USA
John D. Ash Boston, MA, USA Eric Pierce Oklahoma City, OK, USA
Robert E. Anderson Durham, NC, USA
Catherine Bowes Rickman Cleveland, OH, USA
Joe G. Hollyfeld Schlieren, Switzerland Christian Grimm
Part I Age-related Macular Degeneration
High-Resolution Imaging Mass Spectrometry of Human
Donor Eye: Photoreceptors Cells and Basal Laminar
Deposit of Age-Related Macular Degeneration
David M. G. Anderson, Ankita Kotnala, Jeffrey D. Messinger, Nathan Heath Patterson, Jeffrey M. Spraggins, Christine A. Curcio, Richard M. Caprioli, and Kevin L. Schey
3
The Noncanonical Role of Complement Factor H in Retinal Pigment Epithelium (RPE) Cells and Implications for Age-Related Macular Degeneration (AMD) 9
Angela Armento, David Adrian Merle, and Marius Ueffng
Macular Pigment Carotenoids and Bisretinoid A2E 15
Ranganathan Arunkumar and Paul S. Bernstein
Disturbed Matrix Metalloproteinases Activity in Age-Related Macular Degeneration
Beatriz Martins and Rosa Fernandes
Current Views on Chr10q26 Contribution to Age-Related Macular Degeneration 27
Navdeep Gogna, Lillian F. Hyde, Gayle B. Collin, Lisa Stone, Jurgen K. Naggert, and Patsy M. Nishina
Untargeted Lipidomic Profiling of Aged Human Retina With and Without Age-Related Macular Degeneration (AMD) . . . . . 37
Ankita Kotnala, David M. G. Anderson, Jeffrey D. Messinger, Christine A. Curcio, and Kevin L. Schey
Decoding Race and Age-Related Macular Degeneration: GPR 143 Activity Is the Key
Dorothy Tung and Brian S. McKay
Peroxisome Proliferator-Activated Receptor Gamma
Coactivator-1Alpha (PGC-1α): A Transcriptional Regulator at the Interface of Aging and Age-Related Macular Degeneration? 49
Freya M. Mowat
Regulation of ABCA1 by miR-33 and miR-34a in the Aging Eye 55
Florian Peters and Christian Grimm
The Role of Gene Expression Regulation on Genetic Risk of Age-Related Macular Degeneration
Rinki Ratnapriya
Elastin Layer in Bruch’s Membrane as a Target for Immunization or Tolerization to Modulate Pathology in the Mouse Model of Smoke-Induced Ocular Injury
Bärbel Rohrer, Nathaniel Parsons, Balasubramaniam Annamalai, Crystal Nicholson, Elisabeth Obert, Bryan Jones, and Andrew D. Dick
Repurposing Drugs for Treatment of Age-Related Macular Degeneration
Sarah G. Francisco and Sheldon Rowan
Part II Extracellular Vesicles
Extracellular Vesicle RNA Contents as Biomarkers for Ocular Diseases
Heran Getachew and Eric Pierce
Proteomics of Retinal Extracellular Vesicles: A Review into an Unexplored Mechanism in Retinal Health and AMD Pathogenesis
Adrian V. Cioanca, Riccardo Natoli, and Yvette Wooff
Part III Gene Editing
Prime Editing Strategy to Install the PRPH2 c.828+1G>A Mutation
Salvatore Marco Caruso, Yi-Ting Tsai, Bruna Lopes da Costa, Masha Kolesnikova, Laura A. Jenny, Stephen H. Tsang, and Peter M. J. Quinn
61
67
73
87
Analysis of CRB1 Pathogenic Variants Correctable with CRISPR Base and Prime Editing 103
Bruna Lopes da Costa, Laura A. Jenny, Irene H. Maumenee, Stephen H. Tsang, and Peter M. J. Quinn
Generation of an Avian Myeloblastosis Virus (AMV)
Reverse Transcriptase Prime Editor .
Yi-Ting Tsai, Bruna Lopes da Costa, Salvatore Marco Caruso, Nicolas D. Nolan, Sarah R. Levi, Stephen H. Tsang, and Peter M. J. Quinn
109
Part IV Gene Therapy
Preexisting Neutralizing Antibodies against Different Adeno-Associated Virus Serotypes in Humans and Large Animal Models for Gene Therapy.
Divya Ail and Deniz Dalkara
Optimization of Capillary-Based Western Blotting for MYO7A
Kaitlyn R. Calabro, Sanford L. Boye, and Shannon E. Boye
AAV Serotypes and Their Suitability for Retinal Gene Therapy
Lynn J. A. Ebner and Christian Grimm
Gene Augmentation for Autosomal Dominant CRX-Associated Retinopathies
Chi Sun and Shiming Chen
Txnip Gene Therapy of Retinitis Pigmentosa Improves Cone Health
Yunlu Xue
Part V Human Retinal Degeneration
Factors Affecting Readthrough of Natural Versus Premature Termination Codons
Avigail Beryozkin, Kerstin Nagel-Wolfum, Eyal Banin, and Dror Sharon
Integrating Computational Approaches to Predict the Effect of Genetic Variants on Protein Stability in Retinal Degenerative Disease
Michelle Grunin, Ellen Palmer, Sarah de Jong, Bowen Jin, David Rinker, Christopher Moth, John A. Capra, Jonathan L. Haines, William S. Bush, and Anneke I. den Hollander
Network Biology and Medicine to Rescue: Applications for Retinal Disease Mechanisms and Therapy
Anupam K. Mondal and Anand Swaroop
Non-syndromic Retinal Degeneration Caused by Pathogenic Variants in Joubert Syndrome Genes 173 Riccardo Sangermano, Egle Galdikaité-Braziené, and Kinga M. Bujakowska
Exonic Variants that Affect Splicing – An Opportunity for “Hidden” Mutations Causing Inherited Retinal Diseases . . . . . . . 183
Yogapriya Sundaresan, Eyal Banin, and Dror Sharon
Enhanced S-cone Syndrome, a Mini-review
Yiyi Wang, Jessica Wong, Jacque L. Duncan, Austin Roorda, and William S. Tuten
Part VI Infammation
The Role of Microglia in Inherited Retinal Diseases . . . . . . . . . . . . . . 197
Asha Kumari and Shyamanga Borooah
CD68: Potential Contributor to Inflammation and RPE
Cell Dystrophy
Mayur Choudhary and Goldis Malek
Gene Expression of Clusterin, Tissue Inhibitor of Metalloproteinase-1, and Their Receptors in Retinal Pigment Epithelial Cells and Müller Glial Cells Is Modulated by Inflammatory Stresses
Mengmei Zheng, Eun-Jin Lee, Shinwu Jeong, and Cheryl Mae Craft
Part VII Mechanisms of Degeneration
207
215
Axonal Transport Defects in Retinal Ganglion Cell Diseases . . . . . . . 223
Iskalen Cansu Topcu Okan, Fatma Ozdemir, and Cavit Agca
Connexins Biology in the Pathophysiology of Retinal Diseases . . . . . 229
Alejandro Ponce-Mora, Andrea Yuste, Giuliana Perini-Villanueva, María Miranda, and Eloy Bejarano
Role of Nuclear NAD+ in Retinal Homeostasis
Emily E. Brown, Michael J. Scandura, and Eric Pierce
235
Retinal Pigmented Epithelium-Derived Ectopic Norrin Does Not Promote Intraretinal Angiogenesis in Transgenic Mice 241
Andrea E. Dillinger and Ernst R. Tamm
Caveolin-1 in Müller Glia Exists as Heat-Resistant, High Molecular Weight Complexes
Eric N. Enyong, Jami Gurley, Virginie Sjoelung, and Michael H. Elliott
Role of VLC-PUFAs in Retinal and Macular Degeneration
249
257 Aruna Gorusupudi, Uzoamaka Nwagbo, and Paul S. Bernstein
Ocular Amyloid, Condensates, and Aggregates – Higher-Order Protein Assemblies Participate in Both Retinal Degeneration and Function 263
Michael H. Hayes, DaNae R. Woodard, and John D. Hulleman
Photoreceptor Ion Channels in Signaling and Disease
Shivangi M. Inamdar, Colten K. Lankford, and Sheila A. Baker
The Role of Peripherin-2/ROM1 Complexes in Photoreceptor Outer Segment Disc Morphogenesis
Tylor R. Lewis, Muayyad R. Al-Ubaidi, Muna I. Naash, and Vadim Y. Arshavsky
269
277
Human Mutations in Arl3, a Small GTPase Involved in Lipidated Cargo Delivery to the Cilia, Cause Retinal Dystrophy . . .
Amanda M. Travis and Jillian N. Pearring
Genotype–Phenotype Association in ABCA4-Associated Retinopathy 289
Maximilian Pfau, Wadih M. Zein, Laryssa A. Huryn, Catherine A. Cukras, Brett G. Jeffrey, Robert B. Hufnagel, and Brian P. Brooks
Retinal Pathoconnectomics: A Window into Neurodegeneration 297
Rebecca L. Pfeiffer and Bryan W. Jones
The Role of Ceramide in Inherited Retinal Disease Pathology
Xinye Qian, Tanmay Srinivasan, Jessica He, and Rui Chen
Extracellular Matrix: The Unexplored Aspects of Retinal Pathologies and Regeneration
Dmitri Serjanov and David R. Hyde
Role of TFEB in Diseases Associated with Lysosomal Dysfunction .
Hsuan-Yeh Pan and Mallika Valapala
Retinoic Acid Receptor-Related Orphan Receptors (RORs) in Eye Development and Disease
Felix Yemanyi, Kiran Bora, Alexandra K. Blomfeld, and Jing Chen
Part VIII Mechanisms of Degeneration – Animal Models
A Novel Mouse Model for Late-Onset Retinal Degeneration (L-ORD) Develops RPE Abnormalities Due to the Loss of C1qtnf5/Ctrp5
Shyamanga Borooah, Anil Chekuri, Shikha Pachauri, Bhubananda Sahu, Marina Vorochikhina, John J. Suk, Dirk-Uwe Bartsch, Venkata R. M. Chavali, Monica M. Jablonski, and Radha Ayyagari
Comparison of Mouse Models of Autosomal Dominant Retinitis
Pigmentosa Due to the P23H Mutation of Rhodopsin
Shannon R. Barwick and Sylvia B. Smith
Compensatory Cone-Mediated Mechanisms in Inherited Retinal Degeneration Mouse Models: A Functional and Gene Expression Analysis
Alicia A. Brunet, David M. Hunt, Carla Mellough, Alan R. Harvey, and Livia S. Carvalho
309
341
347
Inhibition of Ryanodine Receptor 1 Reduces Endoplasmic Reticulum (ER) Stress and Promotes ER Protein
Degradation in Cyclic Nucleotide-Gated Channel Deficiency 353
Fan Yang, Hongwei Ma, Rekha Garg, Alfred Lewin, and Xi-Qin Ding
Mouse Choroid Proteome Revisited: Focus on Aging
Donita Garland, James Harnly, and Radha Ayyagari
359
Morphological and Functional Comparison of Mice Models for Retinitis Pigmentosa 365 Prakadeeswari Gopalakrishnan, Avigail Beryozkin, Eyal Banin, and Dror Sharon
Current Advancements in Mouse Models of Retinal Disease 371 T. J. Hollingsworth, Xiangdi Wang, Raven N. Simpson, William A. White, Robert W. Williams, and Monica M. Jablonski
Single-Cell Transcriptomic Profiling of Müller Glia in the rd10 Retina
Duygu Sigurdsson and Christian Grimm
Methods for In Vivo Characterization of Proteostasis in the Mouse Retina
Yixiao Wang and Ekaterina S. Lobanova
Absence of PRCD Leads to Dysregulation in Lipid Homeostasis Resulting in Disorganization of Photoreceptor Outer Segment Structure
Sree I. Motipally and Saravanan Kolandaivelu
Expansion Microscopy of Mouse Photoreceptor Cilia
Abigail R. Moyel, Michael A. Robichaux, and Theodore Wensel
Rod Photoreceptor-Specific Ablation of Metformin Target, AMPK, in a Preclinical Model of Autosomal Recessive Retinitis Pigmentosa
Nicholas D. Nolan, Laura A. Jenny, Stephen H. Tsang, and Xuan Cui
377
383
389
395
403
TLR2 Is Highly Overexpressed in Retinal Myeloid Cells in the rd10 Mouse Model of Retinitis Pigmentosa 409 Alonso Sánchez-Cruz, Enrique J. de la Rosa, and Catalina Hernández-Sánchez
Environmental Light Has an Essential Effect on the Disease Expression in a Dominant RPE65 Mutation 415 Wenjing Wu, Yusuke Takahashi, Xiang Ma, Gennadiy Moiseyev, and Jian-Xing Ma
Microglia Preserve Visual Function in a Mouse Model of Retinitis Pigmentosa with Rhodopsin-P23H Mutant
Chen Yu and Daniel R. Saban
Part IX Mechanisms of Degeneration – Metabolism
Measuring the Release of Lactate from Wild-Type and rd1 Mouse Retina
Yiyi Chen, Laimdota Zizmare, Christoph Trautwein, and François Paquet-Durand
421
Aerobic Glycolysis in Photoreceptors Supports Energy Demand in the Absence of Mitochondrial Coupling 435
Daniel T. Hass, Celia M. Bisbach, Martin Sadilek, Ian R. Sweet, and James B. Hurley
Redox Status in Retinitis Pigmentosa
L. Olivares-González, S. Velasco, I. Campillo, J. M. Millán, and R. Rodrigo
Perspectives on Retinal Dolichol Metabolism, and Visual Deficits in Dolichol Metabolism-Associated Inherited Disorders
Sriganesh Ramachandra Rao, Steven J. Pittler, and Steven J. Fliesler
Retinal Metabolic Profile on IMPG2 Deficiency Mice with Subretinal Lesions
Rong Xu, Yekai Wang, Jianhai Du, and Ezequiel M. Salido
Part X Neuroprotection
Glutathione Coating of Liposomes Enhances the Delivery of Hydrophilic Cargo to the Inner Nuclear Layer in Retinal Cultures 467
Gustav Christensen and François Paquet-Durand
Modification of Müller Glial Cell Fate and Proliferation with the Use of Small Molecules
Marcus J. Hooper
A Potential Neuroprotective Role for Pyruvate Kinase 2 in Retinal Degeneration
Jiaming Zhou, Michel Rasmussen, and Per Ekström
Part XI Photoreceptors
Critical Role of VEGF as a Direct Regulator of Photoreceptor Function 487
Jianyan Hu, Meili Zhu, Dai Li, Qiang Wu, and Yun-Zheng Le
Lysine Ubiquitylation Drives Rhodopsin Protein Turnover 493
Allen P. F. Chen, Leon Chea, Eun-Jin Lee, and Jonathan H. Lin
In Silico Prediction of MYO1C-Rhodopsin Interactions and Its Significance in Protein Localization and Visual Function 499
Glenn P. Lobo, Rakesh Radhakrishnan, Matthias Leung, Andrew Gruesen, Hans-Joachim Knölker, Frederik J. van Kuijk, and Sandra R. Montezuma
A Ciliary Branched Actin Network Drives Photoreceptor Disc Morphogenesis 507
William J. Spencer and Vadim Y. Arshavsky
Part XII RPE
Revisiting the Daily Timing of POS Phagocytosis 515
Antonio E. Paniagua, Harjas S. Sabharwal, Kausalya Kethu, Andrew W. Chang, and David S. Williams
Inhibition of Bacterial Peptidoglycan Cytopathy by Retina Pigment Epithelial PGRP2 Amidase .
Marlyn P. Langford, Laura A. Perilloux-Lyons, and A. Scott Kavanaugh
521
Understanding Ischemic Retinopathies: The Role of Succinate and Its Receptor in Retinal Pigment Epithelium 527
Bilge Esin Ozturk
The Amphipathic Helix in Visual Cycle Proteins: A Review 533
Sheetal Uppal, Eugenia Poliakov, Susan Gentleman, and T. Michael Redmond
The Retinal Pigment Epithelium: Cells That Know the Beat! . . . . . . 539
Elora M. Vanoni and Emeline F. Nandrot
Part XIII Stem Cell Models and Therapies
Retinal Organoids: A Human Model System for Development, Diseases, and Therapies .
Sangeetha Kandoi and Deepak A. Lamba
549
Modeling Retinitis Pigmentosa with Patient-Derived iPSCs . . . . . . . 555
Yeh Chwan Leong and Jane C. Sowden
Primary Retinal Cell Cultures as a Model to Study Retina Biology 565
Germán A. Michelis, Luis E. Politi, and S. Patricia Becerra
Generation of CRB1 RP Patient-Derived iPSCs and a CRISPR/Cas9-Mediated Homology-Directed Repair Strategy for the CRB1 c.2480G>T Mutation
Bruna Lopes da Costa, Yao Li, Sarah R. Levi, Stephen H. Tsang, and Peter M. J. Quinn
Inducing Neural Regeneration from Glia Using Proneural bHLH Transcription Factors
Levi Todd
Index
Part I
Age-related Macular Degeneration
High-Resolution Imaging Mass Spectrometry of Human Donor Eye: Photoreceptors Cells and Basal Laminar Deposit of Age-Related Macular Degeneration
David M. G. Anderson, Ankita Kotnala, Jefrey D. Messinger, Nathan Heath Patterson, Jefrey M. Spraggins, Christine A. Curcio, Richard M. Caprioli, and Kevin L. Schey
Abstract
Pathologies of the retina are clinically visualized in vivo with OCT and ex vivo with immu-
D. M. G. Anderson · N. H. Patterson · R. M. Caprioli
· K. L. Schey (*)
Department of Biochemistry, Vanderbilt University, Nashville, TN, USA
Mass Spectrometry Research Center, Vanderbilt University School of Medicine, Nashville, TN, USA e-mail: k.schey@vanderbilt.edu
A. Kotnala
Department of Biochemistry, Vanderbilt University, Nashville, TN, USA
Department of Ophthalmology and Visual Sciences, University of Alabama at Birmingham, Birmingham, AL, USA
J. D. Messinger · C. A. Curcio
Department of Ophthalmology and Visual Sciences, University of Alabama at Birmingham, Birmingham, AL, USA
J. M. Spraggins
Mass Spectrometry Research Center, Vanderbilt University School of Medicine, Nashville, TN, USA
Department of Ophthalmology and Visual Sciences, University of Alabama at Birmingham, Birmingham, AL, USA
Department of Cell and Developmental Biology, Vanderbilt University School of Medicine, Nashville, TN, USA
nohistochemistry. Although both techniques provide valuable information on prognosis and disease state, a comprehensive method for fully elucidating molecular constituents present in locations of interest is desirable. The purpose of this work was to use multimodal imaging technologies to localize the vast number of molecular species observed with matrix-assisted laser desorption ionization imaging mass spectrometry (MALDI IMS) in aged and diseased retinal tissues. Herein, MALDI IMS was utilized to observe molecular species that reside in photoreceptor cells and also a basal laminar deposit from two human donor eyes. The molecular species observed to accumulate in these discrete regions can be further identifed and studied to attempt to gain a greater understanding of biological processes occurring in debilitating eye diseases such as age-related macular degeneration (AMD).
Keywords
Age-related macular degeneration · Macula · Retinal pigment epithelium · Photoreceptors · Basal lamina deposit · MALDI IMS
© The Author(s), under exclusive license to Springer Nature Switzerland AG 2023 J. D. Ash et al. (eds.), Retinal Degenerative Diseases XIX, Advances in Experimental Medicine and Biology 1415, https://doi.org/10.1007/978-3-031-27681-1_1
D. M. G. Anderson et al.
Introduction
Matrix-assisted laser desorption ionization imaging mass spectrometry (MALDI IMS) can localize and display the tissue distributions of hundreds to thousands of molecules, at cellular resolution, without the need for antibodies or radioisotopes [1]. With effective co-registration to multimodal optical imaging and optical coherence topography (OCT) microscopy, these distributions can be accurately correlated to very small histological features of the neural retina and retinal pigment epithelium (RPE). MALDI IMS methods have been used to examine eye tissues including the retina [2–4], optic nerve [4–6], lens [7, 8], and cornea [9]. Distinct cell and synaptic layers of the retina have unique layer-specifc lipid and metabolite signatures distinguished by IMS [4, 10, 11]. By applying multimodal optical imaging technologies with accurate registration and incorporating data-rich IMS images [12], cellular and subcellular localization of specifc molecules informative to cellspecifc biochemistry can be observed. Human retinal lipid composition studies have been performed in the past. The results, while valuable, provide limited information on cellular origin, as experiments require dissections followed by solvent extractions. MALDI IMS offers a “molecular microscope” that localizes tissue components in situ by molecular weights [11], simultaneously providing hundreds to thousands of spatially resolved signals. In this study, we used a newly developed method of highaccuracy registration [12] to co-register high spatial resolution IMS images with OCT autofuorescence and histological images of the same tissue to examine subcellular localizations and molecular features of photoreceptors and AMD pathology.
2 Methods
This section has been summarized from Anderson et al. [3]; for detailed explanations, please see this reference.
2.1
Tissue Acquisition and Characterization
Whole eyes were obtained from deceased human donors via Advancing Sight Network (formerly the Alabama Eye Bank) by the UAB authors.
2.2 Tissue Handling and Ex Vivo Imaging
Methods were optimized for multimodal ex vivo clinical imaging of the ocular fundus [13]. Globes with lens and iris in place were immersed in buffered 4% paraformaldehyde overnight. Iris and lens were removed before imaging.
For imaging with OCT and scanning laser ophthalmoscopy, globes were immersed in buffer facing frontward within a custom-built chamber with a 60-diopter lens [13]. Spectral domain OCT images were captured with a Spectralis (HRA&OCT, HRA2; Heidelberg Engineering).
Tissues were embedded in 2.5% carboxymethyl cellulose (Sigma C9481), and serial 10 μm cryosections were collected on Superfrost glass slides and on large, 45 × 45 mm in-house, polylysine-coated indium-tin-oxide (ITO) slides (Delta Technologies Loveland, CO, USA).
2.3 MALDI IMS Analysis
The matrices 2,5-dihydroxyacetophenone (DHA) and 1,5-diaminonaphthalene (DAN) (Sigma Aldrich, St. Louis, MO, USA) were applied to tissue sections by sublimation [14]. MALDI IMS data were acquired with a laser spot size of 10–15 μm in full scan mode using a Bruker SolariX 9.4T FTICR mass spectrometer (Bruker Daltonics Billerica, MA, USA). Following data acquisition, an advanced image registration workfow [12] was performed. More detailed information of the image registration process can be found in publications by Patterson et al. [12] and Anderson et al. [3]. Molecular identifcations were made using LC-MS of chloroform-methanol extracts from adjacent tissue sections.
Results
3.1 Signals Specifc to Photoreceptors and RPE
Figure 1a shows MALDI IMS and optical microscopy focusing on photoreceptors and their support cells. The RPE sends delicate processes in the apical direction to contact photoreceptor outer segments, near the RPE cell body for rods and 10–15 μm above the cell body, to contact cone outer segments, which are shorter. Figure 1a is color-coded depiction of photoreceptor and RPE compartments associated with IMS signals in Fig. 1b (blue ONL, red inner segments, yellow outer segments, green RPE).
Figure 1b shows MALDI IMS images overlaid with H&E images from this donor. The photoreceptors on the left side of the image are attached to the RPE and detached from the RPE on the right side, a common artifact which can occur during sample preparation. In Fig. 1a, the signal at m/z 818.575 was observed with high abundance in the ONL and was identifed as PE(20:0_22:6) (blue). This region is comprised of the photoreceptor cell bodies and processes of Müller (radial) glia. A highly localized signal can be observed with high abundance along a narrow band aligned with photoreceptor inner segments at m/z 1426.0 (red). This signal was identifed as
a cardiolipin CL(70:5). Cardiolipins are highly abundant in mitochondria, which are abundant in the ellipsoid portion of photoreceptor inner segments. At the distal part of the photoreceptor cells, outer segments are highly interleaved with apical processes of RPE cells. A DHA-containing PE(18:0_22:6) is observed at m/z 790.539 (yellow) in panel D which can be observed with high abundance in the outer segments, while a signal observed at m/z 728.596 (green) is localized above and within the RPE.
3.2 Signals Specifc to Basal Laminar Deposit
Figure 2 shows multimodal imaging of a 93-yearold donor tissue with the imaging modalities separated into panels. Figure 2a displays ex vivo OCT hyperrefective foci (yellow arrowhead) and an RPE elevation (green arrowhead) near the fovea. Figure 2b shows that retinal layers are visible in H&E-stained sections after IMS data acquisition. The inset magnifes BLamD (PASH staining of an alternate section), clearly indicating thickened extracellular matrix between the RPE plasma membrane and its native basal lamina. Figure 2c shows autofuorescence of the elevated RPE layer and anteriorly migrated RPE cells, which account for high-risk-indicating

Fig. 1 MALDI IMS signals consistent with localization to photoreceptor and RPE compartments. (a) Schematic diagram of outer retina, excerpted from Fig. 1a. Blue, pink, yellow, and green bands indicate layers formed by highly compartmentalized and vertically aligned photoreceptors and RPE cells in panels b, c. Layers: OPL outer plexiform layer, ONL outer nuclear layer, ELM external limiting membrane, RPE retinal pigment epithelium, BrM Bruch’s membrane, R rod, C cone photoreceptors. (b–f)
MALDI IMS images and H&E-stained tissue images overlaid in perifoveal retina displaying signals from multiple lipid classes that localize to subcellular compartments of the photoreceptor cells. (b) Overlay showing four separate signals. (c) Localized to ONL. (d) Localized to photoreceptor inner and outer segments. (e) Localized to mitochondria-rich photoreceptor inner segments. (f) Localized to RPE apical processes
Fig. 2 Imaging mass spectrometry (IMS) for molecularly informed optical coherence tomography (OCT) and tissue-level target discovery. Asterisk, foveal pit; RPE, retinal pigment epithelium. Color-coded arrowheads represent corresponding structures across modalities, in a 93-year-old human donor eye. (a) OCT B-scan shows subretinal hyperrefective material (yellow) and an RPE elevation (green). (b) H&E stained cryosection shows
hyperrefective foci of clinical OCT. Figure 2d shows that a sphingomyelin-related lipid (PE-Cer-NMe2(42:1)) at m/z 799.671 [15] is highly abundant and localizes to BLamD and RPE, building on previous histochemical and chromatography fndings of lipids in this deposit [16, 17].
pigmented debris (yellow) and dysmorphic RPE overlying BLamD. Insert, BLamD with basal mound (arrow). Basal mounds contain soft druse material. Layers: GCL ganglion cell, INL inner nuclear, HFL Henle fber, ONL outer nuclear. (c) Autofuorescent, pigmented debris (yellow) and dysmorphic RPE (green). (d) IMS reveals an m/z signal at 799.673, restricted to BLamD and not detected in the RPE
4 Conclusions
MALDI IMS combined with multimodal imaging methods and ex vivo OCT provides a powerful tool to elucidate the molecular composition and localization of molecular species in key regions and pathology associated with ocular dis-
D. M. G. Anderson et al.
ease. Understanding molecular processes occurring in BLamD in early AMD is important as they are early-identifed histologic risk factors for AMD progression [18] and are just now being recognized clinically [19, 20].
Acknowledgments This project was supported by the National Institutes of Health P41 GM103391 (R.M.C.) and R01 EY027948 (C.A.C.). Support was also received by a Research to Prevent Blindness Catalyst Award for Innovative Research Approaches for Age-Related Macular Degeneration to K.L.S.
References
1. Caprioli RM, Farmer TB, Gile J. Molecular imaging of biological samples: localization of peptides and proteins using MALDI-TOF MS. Anal Chem. 1997;69(23):4751–60.
2. Bowrey HE, Anderson DM, Pallitto P, Gutierrez DB, Fan J, Crouch RK, et al. Imaging mass spectrometry of the visual system: advancing the molecular understanding of retina degenerations. Proteomics Clin Appl. 2016;10(4):391–402.
3. Anderson DMG, Messinger JD, Patterson NH, Rivera ES, Kotnala A, Spraggins JM, et al. Lipid landscape of the human retina and supporting tissues revealed by high resolution imaging mass spectrometry. bioR xiv:2020:2020.04.08.029538.
4. Zemski Berry KA, Gordon WC, Murphy RC, Bazan NG. Spatial organization of lipids in the human retina and optic nerve by MALDI imaging mass spectrometry. J Lipid Res. 2014;55(3):504–15.
5. Anderson DM, Spraggins JM, Rose KL, Schey KL. High spatial resolution imaging mass spectrometry of human optic nerve lipids and proteins. J Am Soc Mass Spectrom. 2015;26(6):940–7.
6. Stark DT, Anderson DMG, Kwong JMK, Patterson NH, Schey KL, Caprioli RM, et al. Optic nerve regeneration after crush remodels the injury site: molecular insights from imaging mass spectrometryoptic nerve regeneration imaging mass spectrometry. Invest Ophthalmol Vis Sci. 2018;59(1):212–22.
7. Grey AC, Schey KL. Age-related changes in the spatial distribution of human lens alpha-crystallin products by MALDI imaging mass spectrometry. Invest Ophthalmol Vis Sci. 2009;50(9):4319–29.
8. Stella DR, Floyd KA, Grey AC, Renfrow MB, Schey KL, Barnes S. Tissue localization and solubilities of alphaA-crystallin and its numerous C-terminal truncation products in pre- and postcataractous ICR/f rat lenses. Invest Ophthalmol Vis Sci. 2010;51(10):5153–61.
9. Chen Y, Jester JV, Anderson DM, Marchitti SA, Schey KL, Thompson DC, et al. Corneal haze phenotype in Aldh3a1-null mice: in vivo confocal microscopy and tissue imaging mass spectrometry. Chem Biol Interact. 2017;276:9–14.
10. Anderson DM, Ablonczy Z, Koutalos Y, Spraggins J, Crouch RK, Caprioli RM, et al. High resolution MALDI imaging mass spectrometry of retinal tissue lipids. J Am Soc Mass Spectrom. 2014;25(8):1394–403.
11. Anderson DMG, Ablonczy Z, Koutalos Y, Hanneken AM, Spraggins JM, Calcutt MW, et al. Bis(monoacylglycero)phosphate lipids in the retinal pigment epithelium implicate lysosomal/endosomal dysfunction in a model of Stargardt disease and human retinas. Sci Rep. 2017;7(1):17352.
12. Patterson NH, Tuck M, Van de Plas R, Caprioli RM. Advanced registration and analysis of MALDI imaging mass spectrometry measurements through autofuorescence microscopy. Anal Chem. 2018;90(21):12395–403.
13. Pang CE, Messinger JD, Zanzottera EC, Freund KB, Curcio CA. The onion sign in neovascular age-related macular degeneration represents cholesterol crystals. Ophthalmology. 2015;122(11):2316–26.
14. Hankin J, Barkley R, Murphy R. Sublimation as a method of matrix application for mass spectrometric imaging. J Am Soc Mass Spectrom. 2007;18(9):1646–52.
15. Liu A, Chang J, Lin Y, Shen Z, Bernstein PS. Longchain and very long-chain polyunsaturated fatty acids in ocular aging and age-related macular degeneration. J Lipid Res. 2011;51:3217–29.
16. Curcio CA, Presley JB, Malek G, Medeiros NE, Avery DV, Kruth HS. Esterifed and unesterifed cholesterol in drusen and basal deposits of eyes with age-related maculopathy. Exp Eye Res. 2005;81(6):731–41.
17. Wang L, Li C-M, Rudolf M, Belyaeva OV, Chung BH, Messinger JD, et al. Lipoprotein particles of intraocular origin in human Bruch membrane: an unusual lipid profle. Invest Ophthalmol Vis Sci. 2009;50(2):870–7.
18. Sarks SH. Ageing and degeneration in the macular region: a clinico-pathological study. Br J Ophthalmol. 1976;60(5):324–41.
19. Tan ACS, Astroz P, Dansingani KK, Slakter JS, Yannuzzi LA, Curcio CA, et al. The plateau, an optical coherence tomographic signature of geographic atrophy: evolution, multimodal imaging, and candidate histology. Invest Ophthalmol Vis Sci. 2017;58(4):2349–58.
20. Sura AA, Chen L, Messinger JD, Swain TA, McGwin G Jr, Freund KB, et al. Measuring the contributions of basal laminar deposit and Bruch’s membrane in agerelated macular degeneration. Invest Ophthalmol Vis Sci. 2020;61(13):19.