https://ebookmass.com/product/respiratory-physiology-mosbyphysiology-series-2nd-edition-edition-michelle-m-cloutier/
Instant digital products (PDF, ePub, MOBI) ready for you
Download now and discover formats that fit your needs...
Gastrointestinal Physiology (Mosby Physiology Series) 9th Edition Edition Leonard R. Johnson
https://ebookmass.com/product/gastrointestinal-physiology-mosbyphysiology-series-9th-edition-edition-leonard-r-johnson/ ebookmass.com
Nunn and Lumb's Applied Respiratory Physiology, 9th Edition Andrew B. Lumb
https://ebookmass.com/product/nunn-and-lumbs-applied-respiratoryphysiology-9th-edition-andrew-b-lumb/
ebookmass.com
Physiology Sixth Edition Costanzo
https://ebookmass.com/product/physiology-sixth-edition-costanzo/ ebookmass.com
Recovering Scottish History: John Hill Burton and Scottish National Identity in the Nineteenth Century Craig Beveridge
https://ebookmass.com/product/recovering-scottish-history-john-hillburton-and-scottish-national-identity-in-the-nineteenth-century-craigbeveridge/ ebookmass.com
Hill Country Promise Kit Hawthorne
https://ebookmass.com/product/hill-country-promise-kit-hawthorne/
ebookmass.com
Circuit Theory and Networks Analysis and Synthesis 2nd Edition Ravish R. Singh
https://ebookmass.com/product/circuit-theory-and-networks-analysisand-synthesis-2nd-edition-ravish-r-singh/
ebookmass.com
Reverie Ryan La Sala
https://ebookmass.com/product/reverie-ryan-la-sala-2/
ebookmass.com
Essentials of Anatomy & Physiology, 2nd Edition Kenneth S. Saladin
https://ebookmass.com/product/essentials-of-anatomy-physiology-2ndedition-kenneth-s-saladin/
ebookmass.com
Honey Hill Ranch 13: Schmetterlinge im Bauch (German Edition) Elea Meyer
https://ebookmass.com/product/honey-hill-ranch-13-schmetterlinge-imbauch-german-edition-elea-meyer/
ebookmass.com
https://ebookmass.com/product/102-things-to-do-before-you-are-duedawn-dais/
ebookmass.com
PREFACE
I wrote this book to help teach medical students and other students of medicine. I have been gratified by the many positive responses from students about how they have used this book to learn respiratory physiology, and also by how many pulmonary fellows and new pulmonologists have used this book to prepare for certification and recertification—in particular, in pulmonary medicine. In this revised edition, I have included many more clinical vignettes to help students fill the gaps between respiratory physiology
and its application to respiratory disease. The vignettes were chosen to demonstrate how respiratory physiology is used in medicine to guide diagnosis and treatment. I hope students will find this book especially useful in understanding difficult concepts. I encourage your feedback and comments.
Michelle M. Cloutier
Fig. 1.2 Airway generations and approximate dimensions in the human lung. In the adult, alveoli can be found as early as the 10th airway generation and as late as the 23rd generation. (Redrawn from Weibel ER. Morphometry of the Human Lung. Berlin: Springer Verlag; 1963. Data from Bouhuys A. The Physiology of Breathing. New York: Grune & Stratton; 1977.)
terminal bronchioles, there can be as few as 10 or as many as 20 generations (Fig. 1.2). With each airway generation, the airways become smaller and more numerous (Fig. 1.3) as they penetrate deeper into the lung parenchyma.
Both the right and the left lung are encased by two membranes—the visceral pleura and the parietal pleura. The visceral pleural membrane completely envelops the lung except at the hilum where the bronchus, pulmonary vessels, and nerves enter the lung parenchyma. The parietal pleural membrane lines the inner surface of the chest wall, mediastinum, and diaphragm and becomes continuous with the visceral pleura at the hilum. Under normal conditions, the space between the two pleuras contains a small amount of clear, serous fluid that is produced by filtration from the parietal pleural capillaries and is resorbed by the visceral pleural capillaries. This fluid facilitates the smooth gliding of the lung as it expands in the chest and creates a potential space that can be involved in disease. Air can
enter this potential space between the visceral and parietal pleuras because of trauma, rupture of a weakened area at the surface of the lung, or surgery producing a pneumothorax. Fluid can also enter this space, creating a pleural effusion. Because the pleuras of the right and left lung are separate, a pneumothorax involves only the right or the left hemithorax.
Structurally, the trachea is supported by C-shaped (sometimes referred to as U-shaped) cartilage anteriorly and laterally that prevents tracheal collapse and by smooth muscle posteriorly, which can invaginate and markedly decrease the cross-sectional area of the trachea. Like the trachea, cartilage in large bronchi is also semicircular, but as the bronchi enter the lung parenchyma, the cartilage rings disappear and are replaced by plates of cartilage. As the airways further divide, these plates of cartilage decrease in size and eventually disappear around the 11th airway generation. Airways beyond the 11th generation are
in
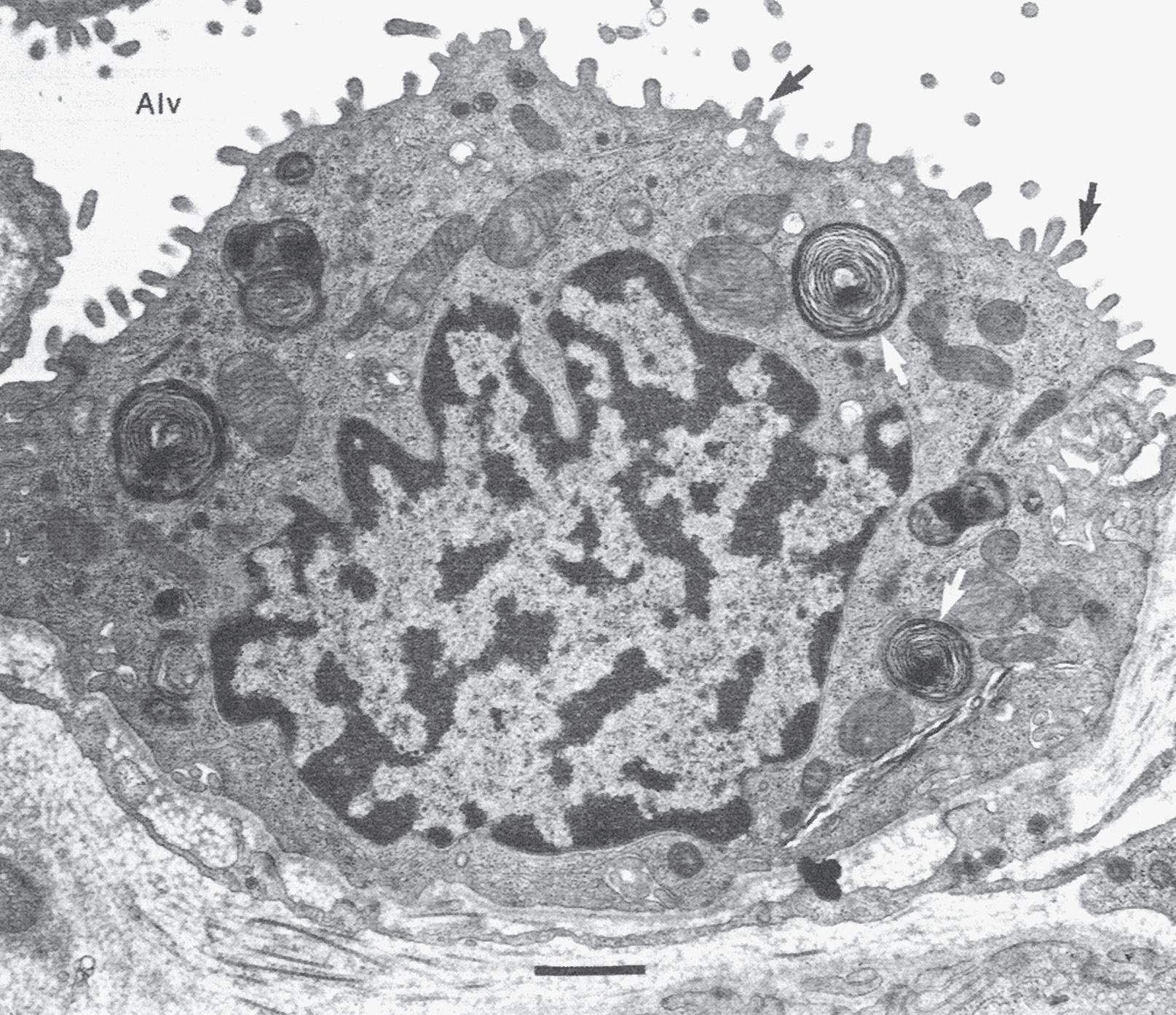
Fig. 1.6 Structure of the normal alveolus.
The type I cell, with its long thin cytoplasmic processes, lines most of the alveolar surface, whereas the cuboidal type II cell, which is more numerous, occupies only about 7% of the alveolar surface. Capillaries (C) with red blood cells (RBC) are also shown. A, alveolar surface; IS, interstitial space; L, lamellar body, source of surfactant. (Modified from Weinberger S, Cockrill, BA, Mandel J. Principles of Pulmonary Medicine, 5th ed. Philadelphia: W.B. Saunders; 2008.)
Alveolar Surface
The alveolar epithelium is a continuous layer of tissue composed primarily of type I cells or squamous pneumocytes. These cells have broad, thin extensions that cover approximately 93% of the alveolar surface (Fig. 1.6). They are highly differentiated cells that do not divide, which makes them particularly susceptible to injury from inhaled or aspirated toxins and from high concentrations of oxygen (see Chapter 11). They are joined into a continuous sheet by tight junctions that prevent large molecules such as albumin from entering the alveoli, resulting in pulmonary edema. The thin cytoplasm of the type I cell is ideal for optimal gas diffusion.
Type II cells, or granular pneumocytes, are more numerous than type I cells; however, because of their cuboidal shape, they occupy only approximately 7% of the alveolar surface and are located in the corners of the alveolus (see Fig. 1.6). The hallmarks of the type II cell are their microvilli and their osmiophilic lamellar inclusion bodies that contain surfactant, a compound with a high lipid content that acts as a detergent to reduce the surface tension of the alveoli (Fig. 1.7; also see Chapter 2). The type II cell is the progenitor cell of the alveolar epithelium. When there is injury to the type I cell, the type II cell multiplies and eventually differentiates into a type I cell. In a group of diseases that result in pulmonary fibrosis, the type I cell is injured and the alveolar epithelium is now lined entirely by type II cells, a condition that is not conducive to optimal
gas exchange. This repair system is an example of phylogeny recapitulating ontogeny, because the epithelium of the alveolus is composed entirely of type II cells until late in gestation.
The lumen of the alveolus is covered by a thin layer of fluid composed of a water phase immediately adjacent to the alveolar epithelial cell and covered by surfactant. Within the alveolar epithelium there are also a small number of macrophages, a type of phagocytic cell that patrols the alveolar surface and ingests (phagocytizes) bacteria and inhaled particles (see Chapter 11).
Pulmonary Circulation
The lung has two separate blood supplies (see Chapter 6 ). The pulmonary circulation brings deoxygenated blood from the right ventricle to the gas-exchanging units (alveoli). Pulmonary perfusion (Q ) refers to pulmonary blood flow, which equals the heart rate multiplied by the right ventricular stroke volume. The lungs receive the entire right ventricular cardiac output and are the only organ in the body that functions in this manner. The bronchial (or lesser) circulation arises from the aorta and provides nourishment to the lung parenchyma. The dual circulation to the lung is another of the unique features of the lung.
The pulmonary capillary bed is the largest vascular bed in the body, with a surface area of 70 to 80 m2. It is best
AB C
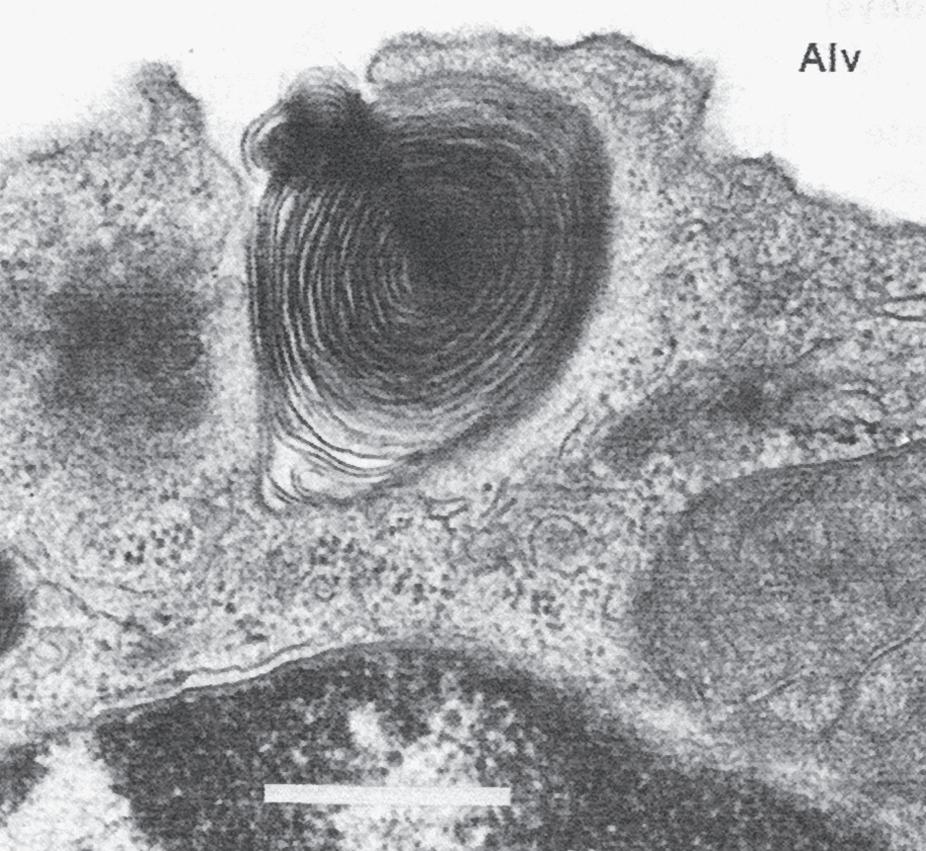
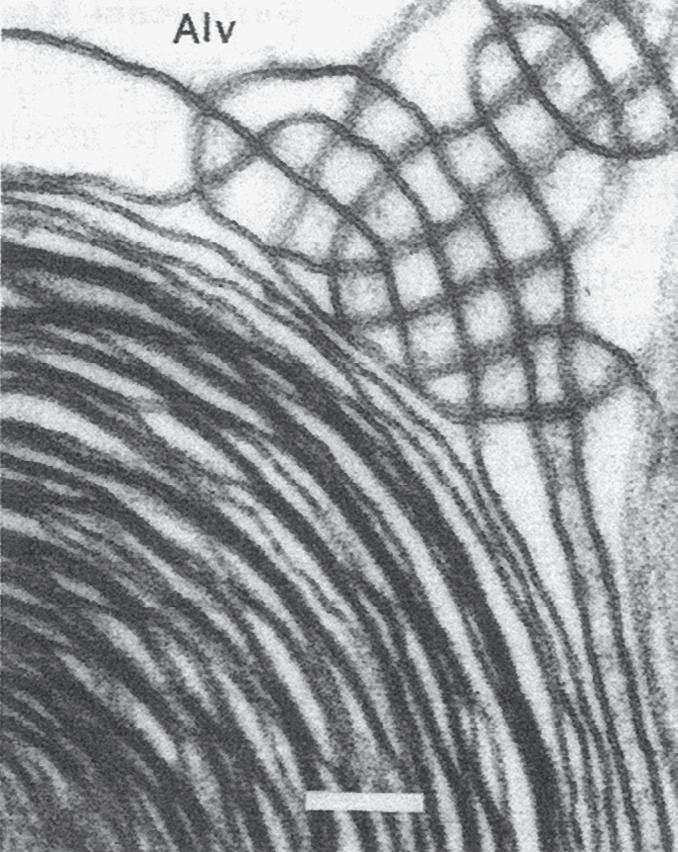
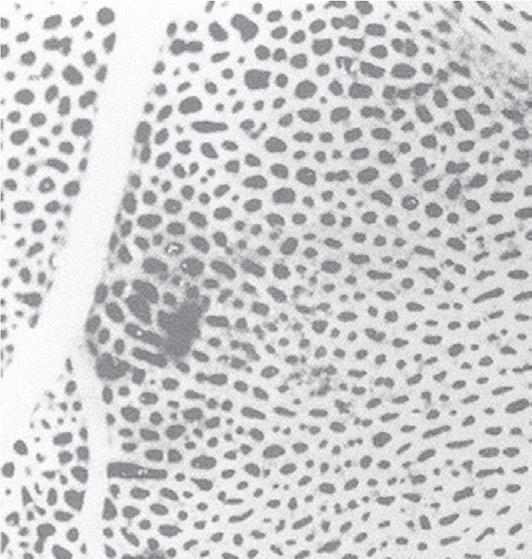
Fig. 1.7 Surfactant release by type II epithelial cells. Alv, alveolus. A, Type II epithelial cell from a human lung showing characteristic lamellar inclusion bodies (white arrows) within the cell and microvilli (black arrows) projecting into the alveolus. Bar = 0.5 μm. B, Early exocytosis of lamellar body into the alveolar space in a human lung. Bar = 0.5 μm. C, Secreted lamellar body and newly formed tubular myelin in alveolar liquid in a fetal rat lung. Membrane continuities between outer lamellae and adjacent tubular myelin provide evidence of intraalveolar tubular myelin formation. Bar = 0.1 μm. (Courtesy Dr. Mary C. Williams.)
viewed as a sheet of blood interrupted by small vertical supporting posts (Fig. 1.8). When the capillaries are filled with blood, about 75% of the surface area of the alveoli overlies the red blood cells. The capillaries allow red blood cells to flow through in single file only; this greatly facilitates gas exchange between the alveoli and the red blood cells. Once gas exchange is complete, the oxygenated blood returns to the left side of the heart through pulmonary venules and veins and is ready for pumping to the systemic
circulation. In contrast to the systemic circulation, the pulmonary circulation is a highly distensible, low-pressure system capable of accommodating large volumes of blood at low pressure. This is another unique feature of the lung.
Pulmonary arteries that contain deoxygenated blood follow the bronchi in connective tissue sheaths, whereas pulmonary veins cross segments on their way to the left atrium (Fig. 1.9). Bronchial arteries also follow the bronchi and divide with them. In contrast, one-third of the blood
Fig. 1.8 Pulmonary capillary surface of the lung. View of alveolar wall (in a frog) demonstrating the dense network of capillaries. A small artery (left) and vein (right) can also be seen. The individual capillary segments are so short that the blood forms an almost continuous sheet. (From Maloney JE, Castle BL. Pressure-diameter relations of capillaries and small blood vessels in frog lung. Respir Physiol. 1969;7:150–162.)
Fig. 1.9 The anatomic relation between the pulmonary artery, the bronchial artery, the airways, and the lymphatics. A, alveoli; AD, alveolar ducts; RB, respiratory bronchioles; TB, terminal bronchioles. (From Berne RM, Levy ML, Koeppen BM, Stanton BA (eds.). Physiology, 7th ed. St. Louis: Mosby; 2018.)
Pulmonary
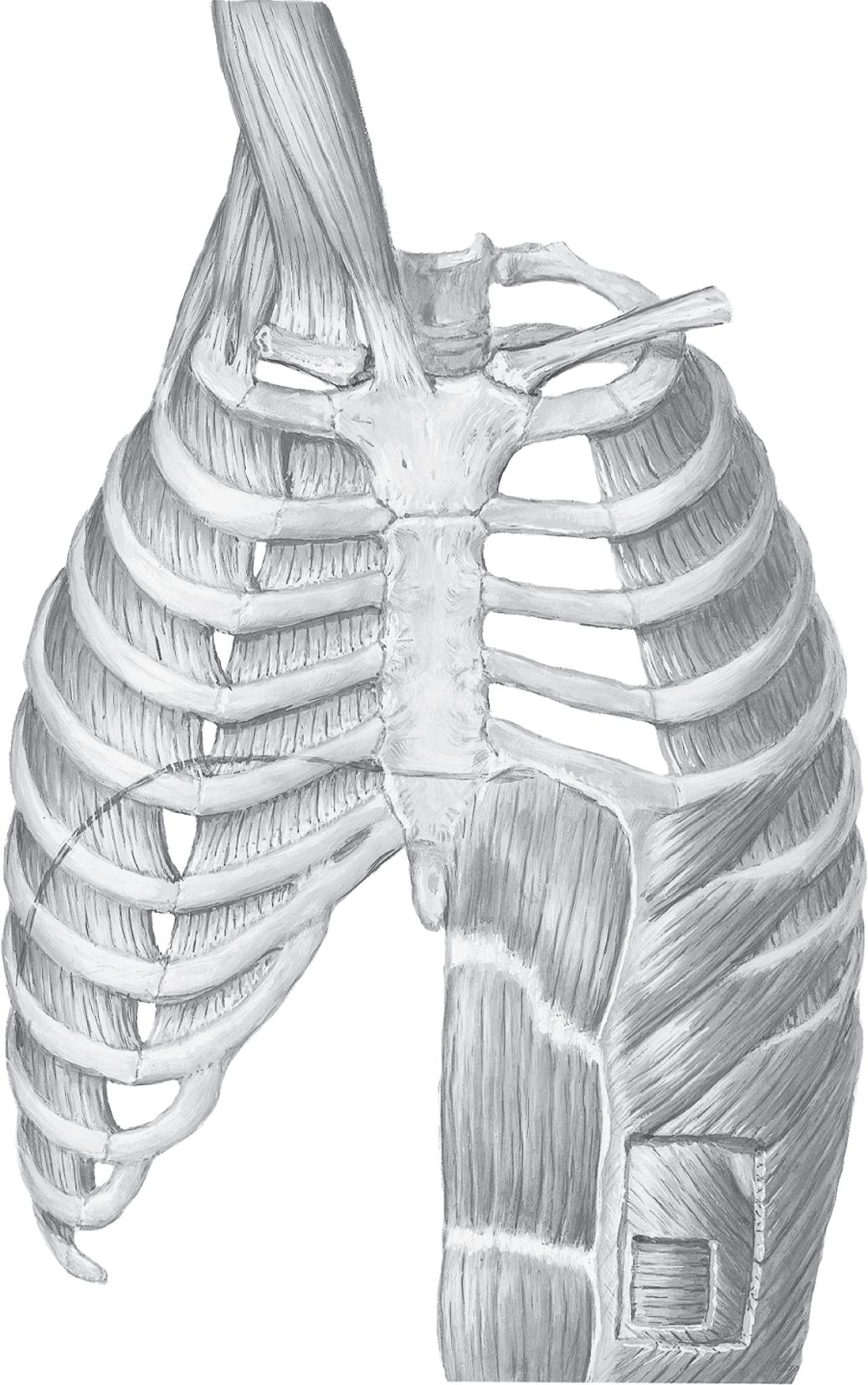
Muscles of inspiration
Accessory
Sternocleidomastoid (elevates sternum)
Scalenes
Anterior Middle Posterior (elevate and fix upper ribs)
Principal
External intercostals (elevate ribs, thus increasing width of thoracic cavity)
Interchondral part of internal intercostals (also elevates ribs)
Diaphragm (domes descend, thus increasing vertical dimension of thoracic cavity; also elevates lower ribs)
MUSCLES OF RESPIRATION
Muscles of expiration
Quiet breathing
Expiration results from passive recoil of lungs and rib cage
Active breathing
Internal intercostals, except interchondral part
Abdominals (depress lower ribs, compress abdominal contents, thus pushing up diaphragm)
Rectus abdominis
External oblique
Internal oblique
Transversus abdominis
Fig. 1.12 Muscles of respiration. Diagram of the anatomy of the major respiratory muscles. Left side, inspiratory muscles; right side, expiratory muscles. (Kaminsky D. The Netter Collection of Medical Illustrations: Respiratory System, vol. 3, 2nd ed. Philadelphia: Elsevier; 2011.)
CLINICAL BOX
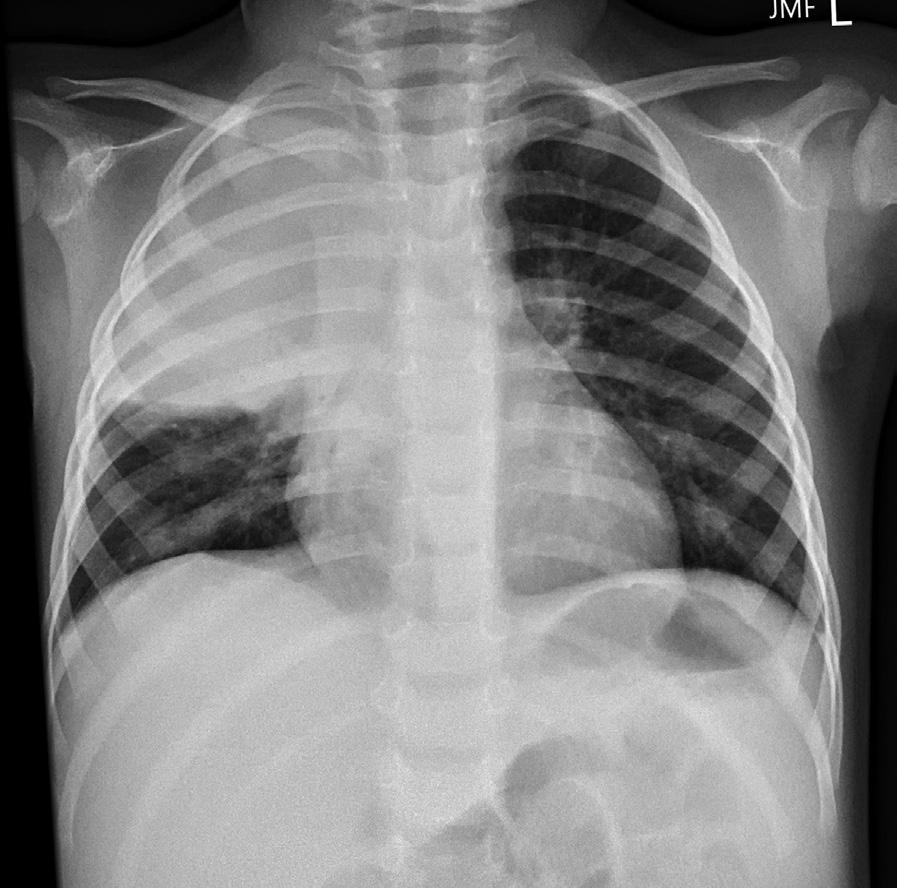
Understanding lung topography is useful in both diagnosing and localizing disease. For example, a 2-year-old boy presents with a 2-day history of fever, cough, and recent onset of tachypnea (an increased respiratory rate). On examination, there are intercostal muscle retractions and nasal flaring, and the child appears ill. On auscultation, breath sounds are decreased over the right upper lobe anteriorly.
A chest x-ray reveals opacification (known as consolidation) over the right upper lobe anteriorly consistent with lobar (specifically right upper lobe) pneumonia.
SUMMARY
1. The principal function of the respiratory system is gas exchange. Other functions include acid–base balance, host defense and metabolism, and the handling of bioactive materials.
2. Gas exchange occurs in the alveolar–capillary unit, the basic physiologic unit of the lung.
3. The bronchopulmonary segment is the segment of the lung supplied by a segmental bronchus. It is the functional anatomic unit of the lung.
4. The alveolar surface is lined by type I and type II cells. The thin cytoplasm of the type I cell is ideal for optimal gas diffusion, whereas the type II cell is important for the production of surfactant, which decreases the surface tension of the alveolus.
5. The lung has two separate circulations. The pulmonary circulation brings deoxygenated blood from the right ventricle to the gas-exchanging units. The
bronchial circulation arises from the aorta and nourishes the lung parenchyma.
6. The circulation to the lung is unique in its dual circulation and in its ability to accommodate large volumes of blood at low pressure.
7. The anatomic dead space is composed of all of the airways that do not participate in gas exchange—that is, the airways to the level of the respiratory bronchioles.
8. The cells of the conducting airways include the pseudostratified, ciliated, columnar epithelial cells, surface secretory cells, Clara cells, and submucosal tracheobronchial gland cells.
9. The diaphragm is the major muscle of respiration.
10. Breathing is both voluntary and automatic.
11. The lung demonstrates both anatomic and physiologic unity—that is, each unit is structurally identical and functions just like every other unit.
Mechanical Propertiesof the Lung and Chest Wall
OBJECTIVES
1.Describestaticlungmechanicsandthemeasurement oflungvolumes.
2.Definelungcomplianceanditsmeasurement.
3.Relatelungandchestwallcompliancetolungvolumes.
STATIC LUNG MECHANICS
Airmovementinandoutofthelungiscontrolledbythe mechanicalpropertiesofthelungandchestwall.Static lungmechanicsisthestudyofthemechanicalproperties ofthelungandchestwallwhosevolumeisnotchanging withtimeandisdiscussedinthischapter.Dynamiclung mechanics,whichisthestudyofthelungandchestwallin motion(i.e.,changingvolume),isdiscussedinChape
Themechanicsofthelungarecomposedofthecombinedmechanicalpropertiesoftheairways,lungpar@:chyma,interstitialmatrix(composedoffibrin,collagen, andafewcells),alveolarsurface,andpulmonai:rcirculation.Themechanicalpropertiesofthechestwallinclude thepropertiesofallofthestructuresoutsideofthelungs thatmoveduringbreathing,includingtheribcage,diaphragm,abdominalcavity,andanteriorabdominalmuscles.TheinteractionbetweentBelungandthechestwall determineslungvolumes,andstaticlungvolumesplaya majorroleingasexchangeandintheworkofbreathing. Theycanbemeasuredandareabnormalinmanylung diseases.
LUNG VOLUMES
ThestaticvolumesofthelungsareshowninFig.2.1.All lungvolumesaresubdivisionsofthetotallungcapacity (TLC)andaremeasuredinliters.Theyarereportedeither asvolumes(e.g.,residualvolume)orcapacities(e.g.,vital capacity).Acapacityiscomposedoftwoormorevolumes.
4.Characterizelungandchestwallinteractionsin termsofpressuregradientsandpressurevolume relationships.
5.Describesurfactantanditsroralteringsurfacetension.
Thetotalvolmeofairthatiscontainedinthelungis calledthe'fLG.Itiscomposedofthevolumeofairthat anindividu�anexhalefromamaximuminspirationto amaximumexhalation,knownasthevitalcapacity(VC), andthevolumeofairthatisleftinthelungafteramaximalexhalation,knownastheresidualvolume(RV).Two otherimportantlungvolumesarethetidalvolume(TV, or,VT)andthefunctionalresidualcapacity(FRC).TheTV ·sthevolumeofairthatisbreathedintoandoutofthe lungduringquietbreathing.TheFRCisthevolumeofair containedinthelungafteranormalexhalation.TheFRC iscomposedoftheresidualvolumeandthevolumeofair thatcanbeexhaledfromtheendofanormalexhalation toresidualvolume.Thislattervolumeiscalledtheexpiratoryreservevolume(ERV).TheFRCrepresentstheresting volumeoftherespiratorysystem,inwhichtheforcesof thechestwalltoincreaseinsizeandtheforcesofthelung todecreaseinsizeareequalbutopposite(seelaterinthis chapter).
Togetasenseoftheimportanceoflungvolumesinrespiration,breathequietlyclosetoTLC(takeadeepbreath in,andbreatheatthishighlungvolumeforafewminutes).Nowbreatheoutuntilyoucannotforceanymore airout,andtrybreathingatthisvolume,whichiscloseto yourRV.Bothofthesemaneuversshouldbeuncomfortableandassociatedwithincreasedwork;bothincreases anddecreasesinlungvolumeoccurinlungdiseaseasa resultofachangeinlungmechanics.Themeasurementof lungvolumesisusedtodetectandfollowtheprogression oflungdiseaseandisdiscussedinChapter4.
Fig. 2.1 The various lung volumes and capacities. ERV, expiratory reserve volume; FRC, functional residual capacity; FVC, forced vital capacity; IC, inspiratory capacity; IRV, inspiratory reserve volume; RV, residual volume; TLC, total lung capacity; VC, vital capacity; VT, tidal volume. (From Koeppen BM, Stanton BA, eds. Berne and Levy’s Physiology, 7th ed. Philadelphia: Elsevier; 2018.)
USING AND INTERPRETING RESULTS OF LUNG VOLUME MEASUREMENTS
Two major types of pathophysiologic abnormalities involving the lung and chest wall can be described using lung volumes. One group of diseases is called obstructive pulmonary disease (OPD). In OPD, during exhalation the airways close (premature airway closure, the hallmark of OPD) trapping air behind them (see Chapter 3). This results in an increase in TLC, RV, and FRC. In contrast, in restrictive pulmonary disease, the other major pathophysiologic abnormality involving the lung and chest wall, lung volumes are reduced.
One of the most useful tests for distinguishing obstructive and restrictive types of lung disease is the measurement of the RV/TLC ratio. In normal individuals, the RV/TLC ratio is less than 0.25, that is, approximately 25% of the air in the lungs is trapped and cannot be exhaled. An elevated RV/TLC ratio, characterized by an increase in RV out of proportion to any increase in TLC, is due to air trapping secondary to airway obstruction and is seen in individuals with OPD. An elevated RV/TLC ratio due to a decrease in TLC out of proportion to any change in RV is seen in individuals with restrictive types of pulmonary disease.
LUNG COMPLIANCE AND LUNG ELASTIC PROPERTIES
Lung compliance (Cl) is a measure of the elastic properties of the lung and is a reflection of lung distensibility. These distensibility properties of the lung are seen in the pressure
volume relaxation curve for the lung that is called the compliance curve of the lung Compliance of the lungs is defined as the change in lung volume resulting from a change in the distending pressure of the lung equal to 1 cm H2O. The units of compliance are mL (or L)/cm H2O. A lung with high lung compliance refers to a lung that is easily distended. A lung with low compliance or a “stiff” lung is the one that is not easily distended. Thus the compliance of the lung (Cl) is: CL = ΔV/ΔP
where ΔV is the change in volume and ΔP is the change in pressure.
The compliance of the isolated lung is measured in animals by removing the lung and measuring the changes in lung volume that occur with each change in the pressure between the inside of the lung and the outside (also known as transpulmonary or translung pressure). As transpulmonary pressure increases, lung volume increases (Fig. 2.2A). The line that is generated, however, is curvilinear, not linear. That is, at low lung volumes, the lung distends easily, but at high lung volumes, larger increases in transpulmonary pressure are needed to produce only small changes in lung volume. This is in part because at high lung volumes all of the elastic fibers in the alveolar units and airways have been maximally stretched. More important than elastic recoil in the determination of compliance is the surface tension at the air–water interface lining the alveoli due to surfactant (see later in this chapter).
CLINICAL BOX: CLINICAL USE OF COMPLIANCE
The compliance of the lung is not altered by airflow per se, but the compliance of the lung and chest wall is affected by a number of respiratory disorders. In emphysema, the lung is more compliant because of destruction of lung elastic tissue; that is, for every 1 cm of H2O pressure increase, there is a larger increase in volume than in the normal lung. In contrast, a proliferation of connective tissue in the lung called pulmonary fibrosis can be seen in lung diseases such as interstitial pneumonitis and sarcoidosis or in association with chemical or thermal lung injury. The lungs in these diseases are “stiff,” or noncompliant; that is, for every 1 cm H2O pressure change, there is a smaller change in volume. Similarly, in diseases associated with increased fluid in the interstitial spaces such as pulmonary edema or in diseases associated with fluid, blood, or infection in the intrapleural space (pleural effusion, hemothorax, or empyema, respectively), lung compliance is reduced. The compliance of the chest wall is decreased in individuals with obesity in whom adipose tissue results in an additional load on the chest wall muscles and the diaphragm. Individuals with decreased mobility of the rib cage such as in kyphoscoliosis or other types of musculoskeletal diseases that affect chest wall movement also have decreased chest wall compliance.
Individuals with decreased compliance must generate greater transpulmonary pressures to produce changes in lung volume than individuals with normal compliance. This results in increased work associated with breathing (see Chapter 3).
Fibrosis/emphysema pressure–volume curve. TLC, total lung capacity.
(cm H2O)
From Koeppen BM, Stanton BA, eds. Berne and Levy’s Physiology, 7th ed. Philadelphia: Elsevier; 2018.
FACTORS DETERMINING LUNG VOLUME
Why can’t we inspire above TLC or exhale beyond RV? The answers lie in the properties of the lung parenchyma and in the interaction between the lungs and the chest wall. Both the lungs and the chest wall have elastic properties. Both have a resting volume (or size) that they would assume if there were no external forces or pressures exerted on them. Both expand when stresses are applied and recoil passively when stresses are released. If the lungs were removed from the chest and no external forces were applied, they would become almost airless. To expand, these lungs would require either the exertion of a positive pressure on the alveoli and airways or the application of a negative pressure from outside the lungs. Either would result in a positive transpulmonary pressure. These situations are analogous to the balloon and the vacuum canister. A balloon is airless until positive pressure is exerted at the opening to distend the balloon walls (positive-pressure “ventilation”). In the case of the vacuum, negative external pressure is applied and results in sucking materials (air) into the canister (negative-pressure “ventilation”).
The lungs are enclosed by the chest wall, which expands during inspiration. The lungs and chest wall always move together in healthy individuals. Lung volumes are determined by the balance between the lung’s elastic recoil properties and the properties of the muscles of the chest wall. TLC occurs when the forces of inspiration decrease because of chest wall muscle lengthening and are insufficient to overcome the increasing force required to distend the lung and chest wall (see Fig. 2.4). Thus TLC is limited by the distensibility of both the lungs and the chest wall and the amount of force that the inspiratory muscles can generate. Disease that affects any of these three components will affect TLC.
At RV, a significant amount of gas remains within the lung. As RV is approached, the chest wall becomes so stiff that additional effort by the expiratory chest wall muscles to contract is unable to further reduce the volume. Thus RV occurs when the expiratory muscle force is insufficient to cause a further reduction in chest wall volume (see Fig. 2.4). As the chest wall is squeezed by the expiratory muscles, the recoil pressure of the chest wall (the chest wall wanting to increase in size) increases. The expiratory muscles