Respiratory Care Exam Review
Gary Persing, BSRT, RRT
Retired Program Director
Respiratory Care Program
Tulsa Community College Tulsa, Oklahoma
Respiratory Review Workshops, Inc. Director
TMC/Clinical Simulation Exam Review Workshops
Please do not contact Gary for issues you may be having with the Evolve website portion of the textbook. Direct any concerns to Evolve Technical Support at 800-222-9570.
Elsevier
3251 Riverport Lane
St. Louis, Missouri 63043
RESPIRATORY CARE EXAM REVIEW, FIFTH EDITION
Copyright © 2020, 2016, 2010, 2005, 2000 by Saunders, an imprint of Elsevier Inc. All rights reserved.
ISBN: 978-0-323-55368-1
All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the Publisher. Details on how to seek permission, further information about the Publisher’s permissions policies, and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency can be found at our website: www.elsevier.com/permissions
This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein).
Notices
Knowledge and best practice in this field are constantly changing. As new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary.
Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. In using such information or methods, they should be mindful of their own safety and the safety of others, including parties for whom they have a professional responsibility.
With respect to any drug or pharmaceutical products identified, readers are advised to check the most current information provided (i) on procedures featured or (ii) by the manufacturer of each product to be administered to verify the recommended dose or formula, the method and duration of administration, and contraindications. It is the responsibility of practitioners, relying on their own experience and knowledge of their patients, to make diagnoses and to determine dosages and the best treatment for each individual patient, and to take all appropriate safety precautions.
To the fullest extent of the law, neither the Publisher nor the authors, contributors, or editors assume any liability for any injury and/or damage to persons or property as a matter of products liability, negligence, or otherwise or from any use or operation of any methods, products, instructions, or ideas contained in the material herein.
Library of Congress Control Number: 2019952407
Executive Content Strategist: Yvonne Alexopoulos
Content Development Manager: Ellen Wurm-Cutter
Content Development Specialist: Melissa Rawe
Project Manager: Bharat Narang
Designer: Patrick Ferguson
To Debbie, Lindsey, Kenton and Maddie, and all the students who have used my exam review books over the years. Also, to Buddy, our lovable golden retriever, and to the memory of Buddy Sr., our golden retriever and retired service dog whom we recently lost to cancer.
And as always, to my Lord and Savior Jesus Christ, who has continued to bless me in so many ways.
This page intentionally left blank
1
5. Given the following data, what is the patient’s total arterial O2 content?
pH 7.41
PaCO2 37 mm Hg
PaO2 88 mm Hg
HCO3 26 mEq/L
SaO2 95%
Hb 14 g/dL
A. 12 mL/dL
B. 14 mL/dL
C. 16 mL/dL
D. 18 mL/dL
6. The respiratory therapist receives an order to set up a moderate level of O2 on a patient who arrives in the ED breathing at a rate of 35 breaths/min. Which of the following O2 delivery devices is most appropriate to use in this situation?
A. Simple O2 mask at 10 L/min
B. Nasal cannula at 4 L/min
C. Nonrebreathing mask at 15 L/min
D. Air-entrainment mask at 40% O2
7. A severe COPD patient arrives in the emergency department on a 2 L/min nasal cannula. Arterial blood gas results follow:
pH 7.32
PaCO2 67 mm Hg PaO2 62 mm Hg HCO3 38 mEq/L
Which of the following is the most appropriate recommendation?
A. Increase the liter flow to 4 L/min.
B. Maintain the current O2 level.
C. Institute noninvasive positive pressure ventilation (NPPV).
D. Place on a nonrebreathing mask at 12 L/min.
8. The physician has ordered O2 to be set up on a patient who has a spontaneous tidal volume of 500 mL and an inspiratory time of 1 second. Which of the following O2 delivery devices will deliver a flow that meets or exceeds this patient’s inspiratory flow?
A. 35% air-entrainment mask at 6 L/min
B. 60% aerosol mask at 12 L/min
C. Nonrebreathing mask at 15 L/min
D. Simple O2 mask at 10 L/min
9. A patient breathing 50% oxygen has a PaO2 of 248 torr. Which of the following should the respiratory therapist recommend?
A. Discontinue oxygen therapy.
B. De crease the oxygen to 30%.
C. Titrate oxygen to maintain an SpO2 .93%.
D. Repeat the blood gases because the PaO2 is not possible on this FiO2
10. A patient is receiving 30% oxygen via an airentrainment mask at a flow of 5 L/min. The total flow delivered by this device is which of the following?
A. 36 L/min
B. 45 L/min
C. 54 L/min
D. 60 L/min
See answers and rationales at the back of the text.
REVIEW
I. STORAGE AND CONTROL OF MEDICAL GASES
A. Storage of Medical Gases and Cylinder
Characteristics
1. Cylinders are constructed of chrome molybdenum steel.
2. Gas cylinders are stored at high pressures; a full O2 cylinder contains 2200 psig pressure.
3. Cylinders are constructed in various sizes. The most common sizes for O2 storage are the H cylinder and the E cylinder.
a. The H cylinder holds 244 cu ft (6900 L) of O2.
b. The E cylinder used for transport holds 22 cu ft (622 L) of O2
There are 28.3 L in 1 cu ft.
4. Valves on the cylinder allow attachment of regulators that release the gas at various flow rates. Cylinder and regulator safety systems dictate that the valves be constructed to allow the connection of only one type of gas regulator. For example, an O2 regulator cannot be attached to a helium cylinder.
a. Large cylinders use the American Standard Safety System. Each type of gas cylinder valve has a different number of threads per inch and a different thread size, and the cylinder may
require either a right- or left-hand turning motion for attachment to the regulator.
b. Small cylinders use the Pin Index Safety System. Each cylinder valve has two holes drilled in unique positions that line up with corresponding pins on the appropriate regulator. There are six different hole placement positions.
5. Safety relief devices on cylinder valves allow escape of excess gas if the pressure in the cylinder increases. There are two types of safety relief devices:
a. Frangible disk—breaks at 3000 psig
b. Fusible plug—melts at 208° to 220° F (caused by high ambient temperature or high pressure, which increases the temperature)
6. The Compressed Gas Association (CGA) developed a color code system for cylinders to distinguish the various gases.
Gas Color of Cylinder
O2 Green; white (internationally)
Helium Brown
Carbon dioxide Gray
Nitrous oxide Light blue
Cyclopropane Orange
Ethylene Red
Air Yellow
CO2/O2 Gray and green
He/O2 Brown and green
7. Cylinder markings
8. Cylinder testing
a. Cylinders are visually tested by lowering a light bulb inside to look for corrosion.
b. Cylinders are hydrostatically tested every 5 or 10 years, depending on the cylinder marking. A star next to the latest test date means the next test must be done 10 years from that date. Hydrostatic testing determines the amount or number of:
(1) Wall stress
(2) Cylinder expansion
(3) Leaks
9. Liquid gas systems
a. 1 cu ft of liquid O2 expands to 860 cu ft as it changes to a gas. Liquid O2 is much more economical than gas.
b. The liquid O2 is stored in Thermos containers at a pressure not to exceed 250 psig and at a temperature below 297° F (the boiling point of O2).
c. Liquid O2 is most commonly produced by the process of fractional distillation.
B. Control of Medical Gases
1. Re gulators are devices attached to the cylinder valve to regulate flow and reduce cylinder pressure to working pressure (i.e., 50 psig).
2. Types of reducing valves
a. Single stage, which reduces the cylinder pressure directly to 50 psig and has one safety relief device
b. Double stage, which reduces the cylinder pressure to approximately 150 psig and then to 50 psig and has two safety relief devices
c. Triple stage, which reduces the cylinder pressure to approximately 300 psig, then to 150 psig, and finally to 50 psig and has three safety relief devices
3. Regulators may be preset or adjustable.
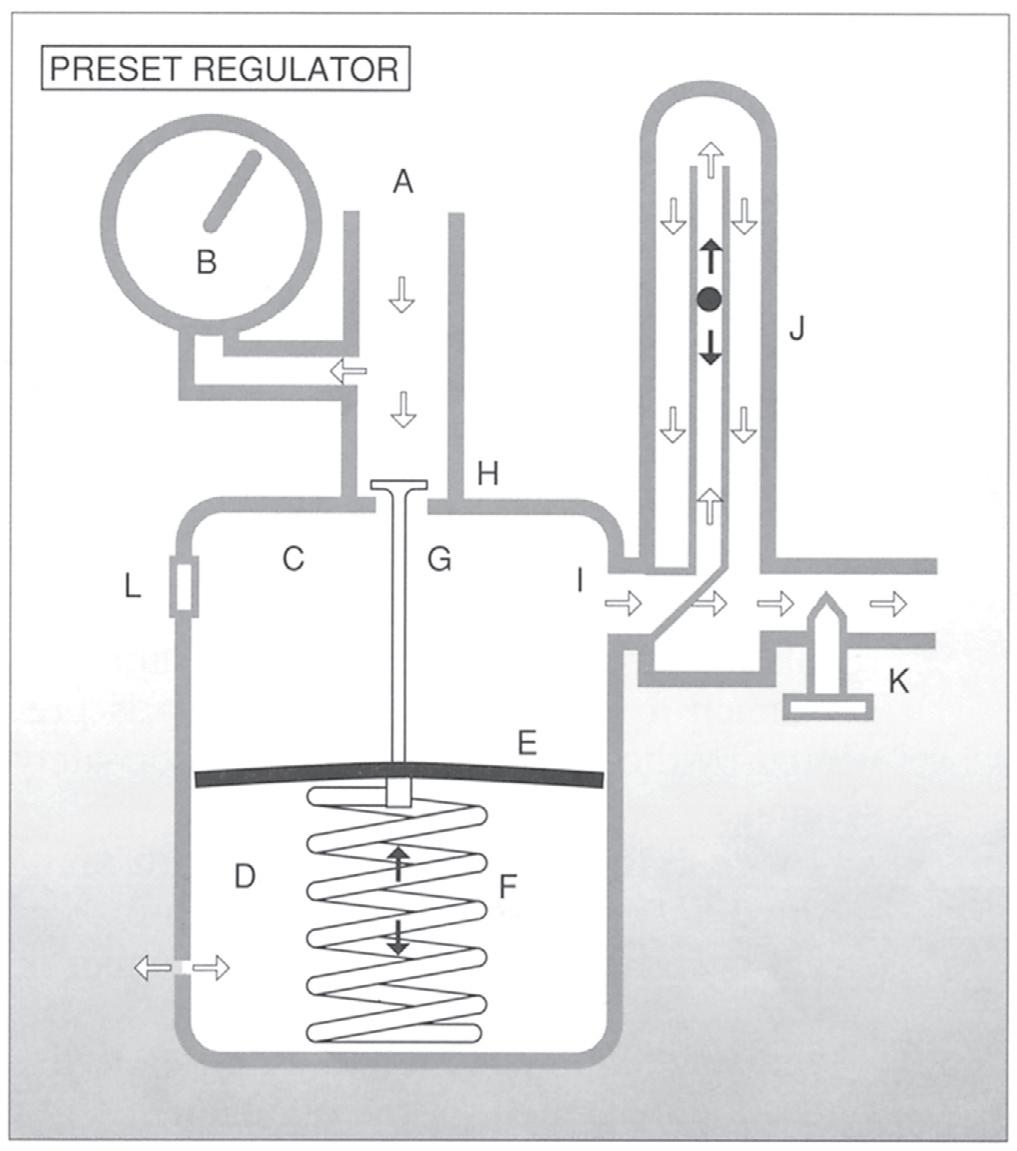
a. Mechanics of a preset regulator
b. Adjustable regulator
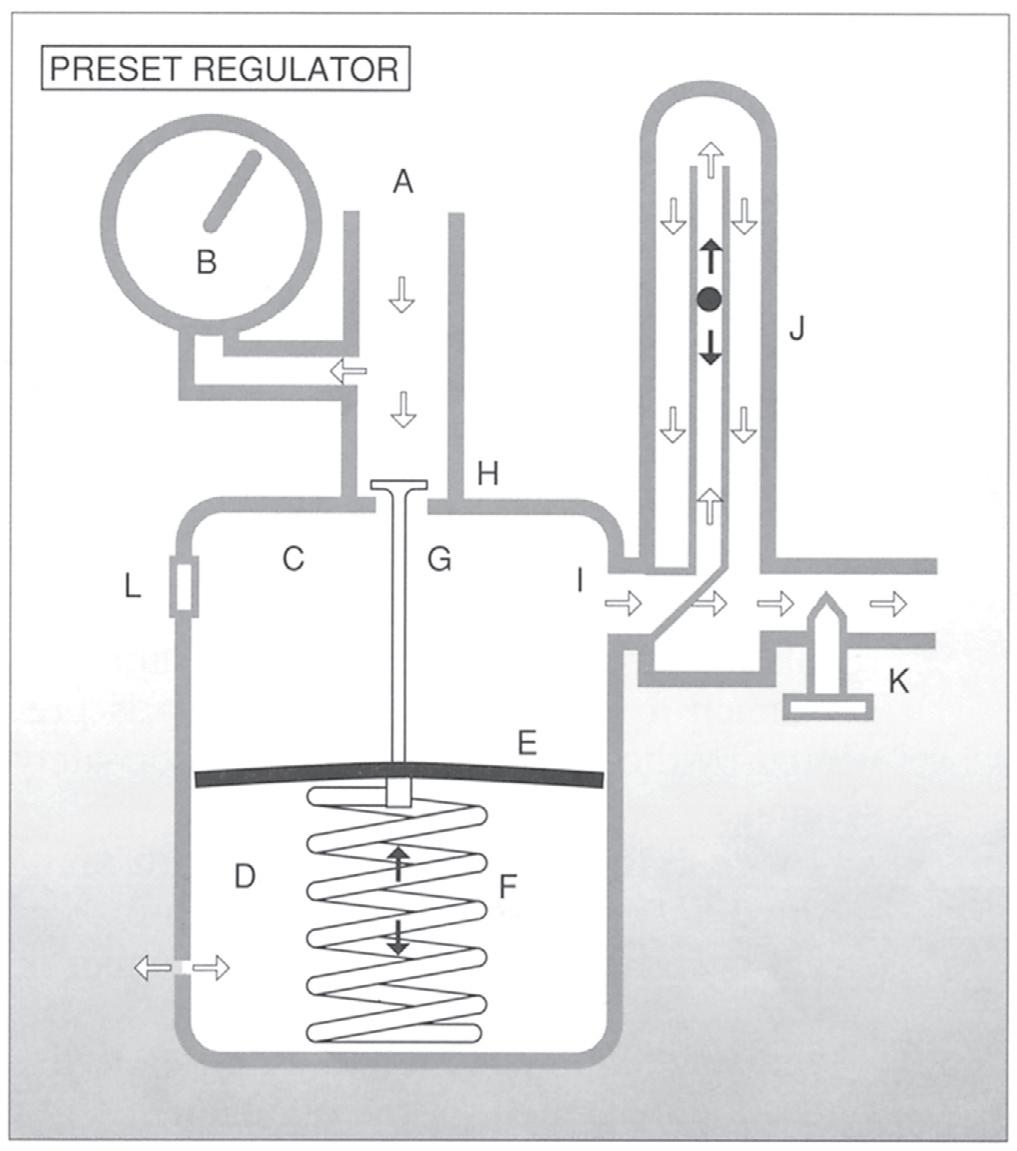
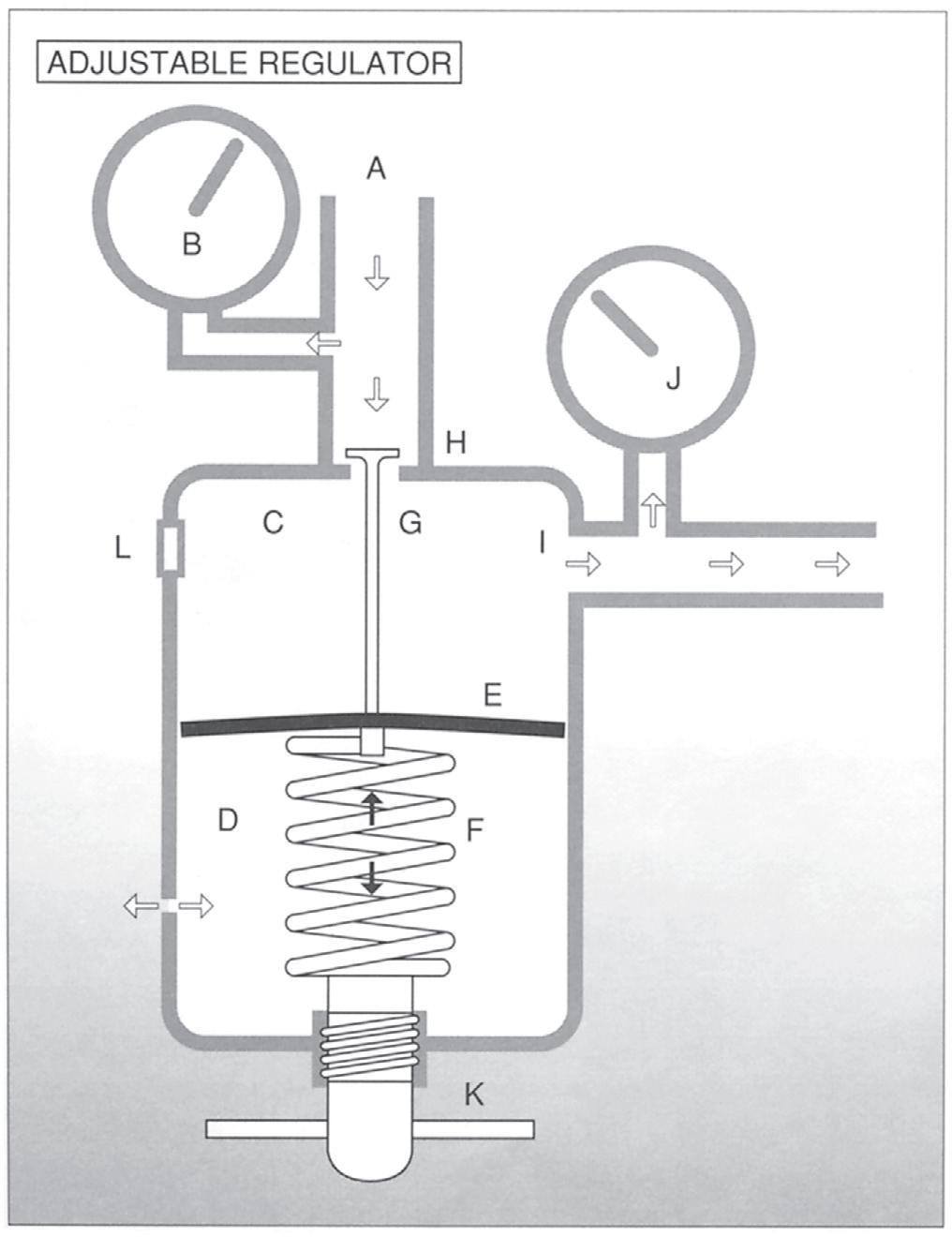
FIGURE 1-2 Gas under high pressure from the cylinder enters the inlet (A) of the reducing valve, where cylinder pressure is read on the Bourdon gauge (B). Gas then passes through the inlet valve (H) into the pressure chamber (C) and pushes down on the diaphragm (E), spring (F), and valve stem (G) assembly, closing the valve and cutting off gas flow into the pressure chamber. At the moment the valve closes, the gas pressure is equal to the spring pressure in the ambient chamber (D). Then, as gas exits the pressure chamber through the outlet (I), pressure drops in the pressure chamber and the diaphragm assembly moves upward, which allows gas to enter the chamber again. In fact, the diaphragm assembly moves continually up and down, opening and closing the valve repeatedly as gas passes through the chamber flowmeter (J) and needle valve (K). Excessive pressure in the pressure chamber is vented through a pressure relief valve (L). The spring tension on this regulator is preset at 50 psig.
4. Technical problems associated with reducing valves and regulators
a. Dust or debris entering the regulator from the cylinder valve may rupture the diaphragm. Always “crack” the cylinder before attaching a regulator. This is accomplished by turning the cylinder on and back off quickly to blow out the debris from the cylinder outlet.
b. Constant pressure trapped in the pressure chamber after the cylinder is turned off may rupture the diaphragm. Always vent pressure in the regulator by turning the flowmeter back on after the cylinder is turned off.
c. A hole in the diaphragm will result in a continuous leak into the ambient chamber and out the vent hole (see Figure 1-2), causing failure of the regulator.
FIGURE 1-1 A Cylinder markings. B, Cylinder markings.
Vent hole
FIGURE 1-3 This is an example of a Bourdon gauge regulator. It works just as a preset regulator does, except the spring tension is adjustable by the user. The second gauge (J) indicates the pressure exerted by the spring. If a flowmeter or high-pressure hose leading to a ventilator is attached to the outlet of the regulator, the spring should be adjusted to 50 psig. The gauge may also be calibrated in L/min to read flow. This is called a Bourdon gauge flowmeter.
d. A weak spring can result in diaphragm vibration and inadequate flows that are caused by premature closing of the inlet valve.
e. When attaching a regulator to a small cylinder, make sure the plastic washer is in place, or gas will leak audibly around the cylinder valve outlet and regulator inlet.
5. Calculating how long cylinder contents will last
EXAMPLE:
Calculate how long a full H cylinder will last running at 8 L/min.
Exam Note
To simplify the math, use 0.3 for the E cylinder factor and 3 for the H cylinder factor. Then select the answer that is closest to what you calculated. The answers are far enough apart on the exam that you can still get the correct answer.
EXAMPLE:
An E cylinder of O2 contains 1800 psig. If the respiratory therapist runs the cylinder at 4 L/min through a nasal cannula, how long will it take for the cylinder to reach a level of 200 psig?
6. Calculating the duration of flow for a liquid O2 system
One liter of liquid O2 weighs 2.5 lb (1.1 kg).
Gasremaining
EXAMPLE:
A liquid O2 tank contains 5 lb of liquid O2. The patient is receiving O2 at 3 L/min through a nasal cannula. How long will the liquid O2 last?
Gasremaining 5lbs 860
Math shortcut: Because 860 and 2.5 are constants in the equation, cancel them out by dividing 860 by 2.5. The answer is 344. Now simply multiply 344 by the pounds of liquid O2. The answer will be the same as when you use the longer equation.
7. Flowmeters
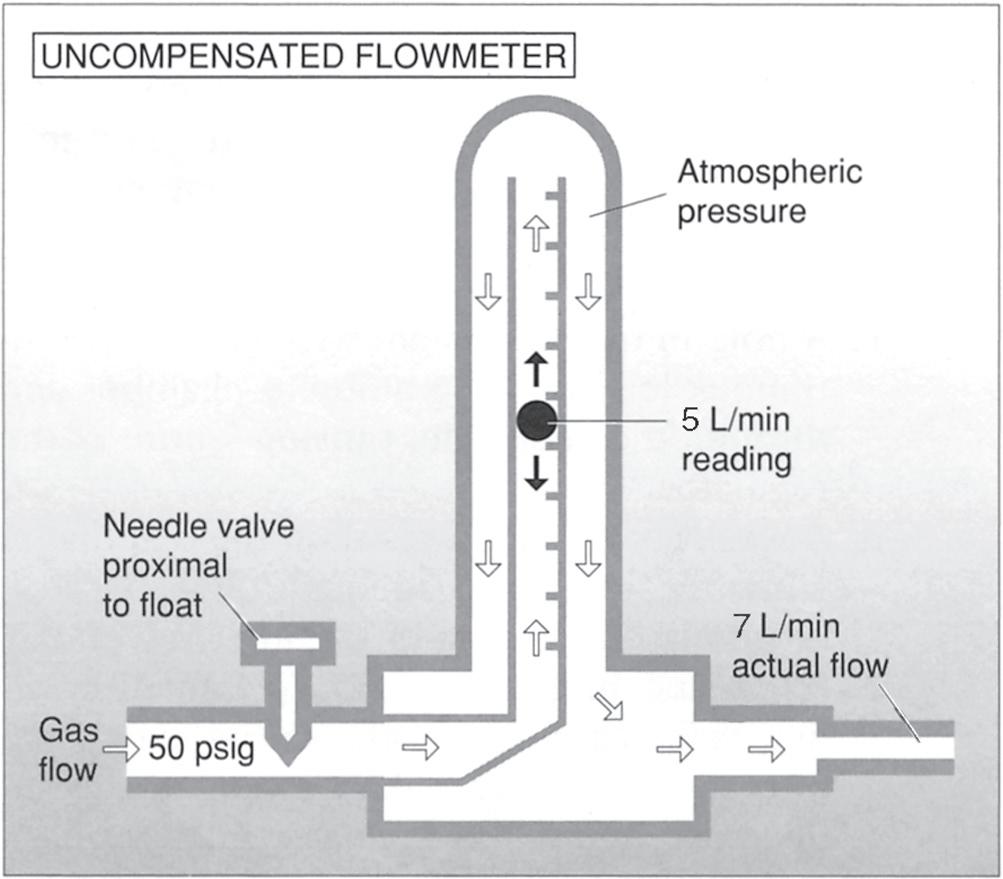
a. Uncompensated flowmeter (1) The needle valve is located proximal to (before) the float; therefore atmospheric pressure is in the Thorpe tube. Any back pressure in the tube affects the rise of the float.
1-4
(1) The needle valve is located distal to (after) the float; therefore 50 psig is in the tube. Only back pressure that exceeds 50 psig will affect the rise of the float.
(2) The flowmeter reads accurately with an attachment, such as a humidifier or nebulizer on the outlet, or with any obstruction downstream. If the O2 tubing is completely obstructed with no gas flowing to the patient, the flowmeter will reflect that with a flow reading of near 0.
(2) When a restriction, such as a humidifier or a nebulizer, is attached to the outlet, back pressure into the tube forces the float down and compresses the gas molecules closer together so that more molecules go around the float than are indicated by the float. Therefore the flowmeter reading is lower than the amount the patient is actually receiving.
(3) Uncompensated flowmeters should not be used clinically.
b. Compensated flowmeter
(3) There are three ways to determine whether a flowmeter is compensated for pressure
(a) It is labeled as such on the flowmeter.
(b) The needle valve is located after the float.
(c) The float jumps when the flowmeter, while it is turned off, is plugged into a wall outlet.
(4) Flowmeter outlets use the Diameter Index Safety System, as do all gas-administering equipment that operates at less than 200 psig, so that attachment to the wrong gas source is avoided.
FIGURE
FIGURE 1-5
FIGURE 1-6
(5) If the flowmeter is turned off completely but gas is still bubbling through the humidifier or is heard coming from the flowmeter, the valve seat is faulty and the flowmeter should be replaced.
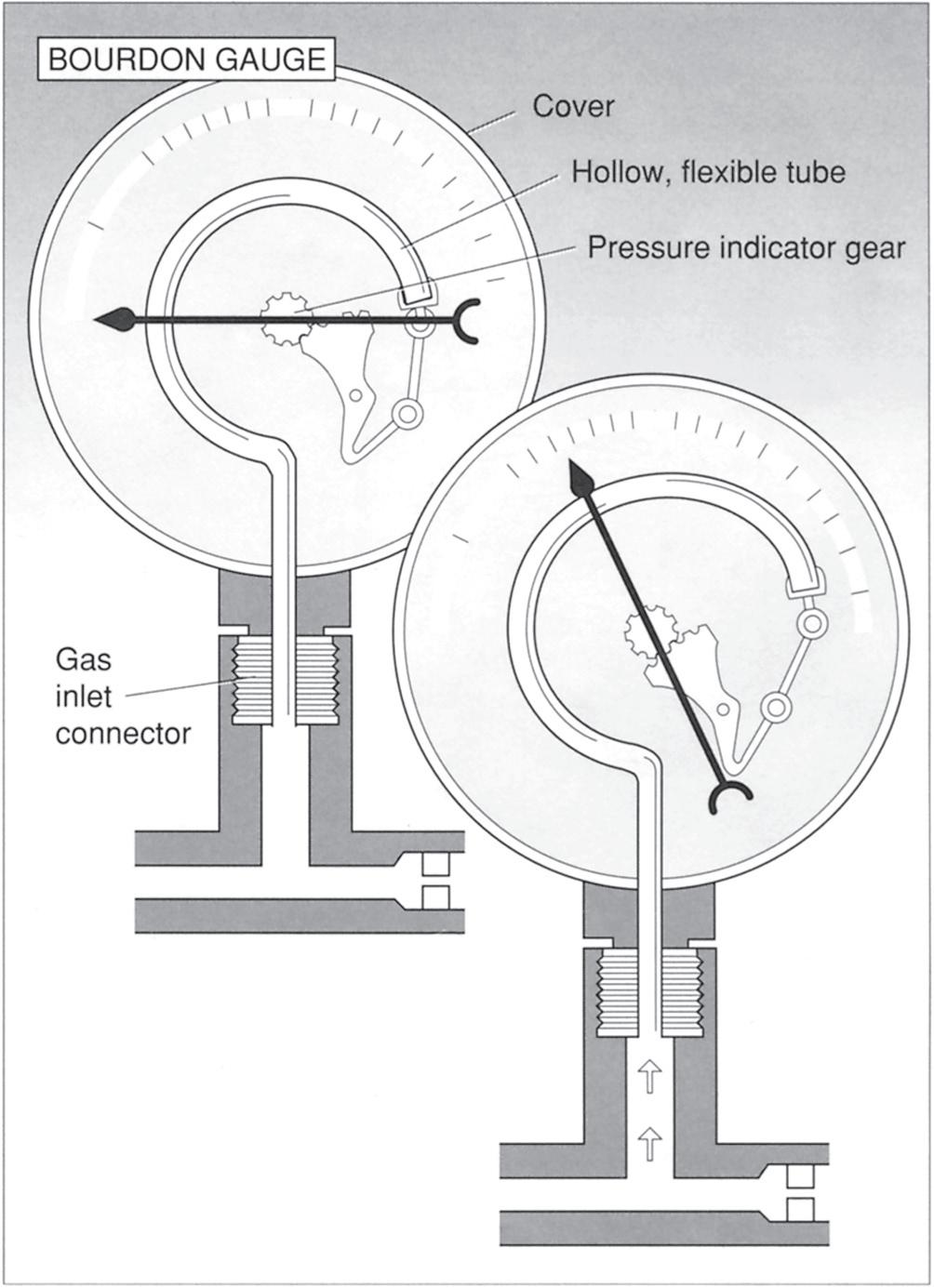
c. Bourdon gauge flowmeter
(1) The Bourdon gauge flowmeter is a pressure gauge that has been calibrated in liters per minute. It is uncompensated for back pressure.
(2) When a humidifier or nebulizer is attached to the outlet of the Bourdon gauge, back pressure is generated into the gauge (which measures pressure), and the gauge reading is higher than the amount the patient is actually receiving.
(3) Gas enters the hollow, flexible question mark–shaped tube, which tends to straighten as pressure fills it. A gear mechanism is attached to the tube, and as the tube straightens, it rotates a needle indicator that shows the pressure (flow).
(4) The advantage of the Bourdon gauge is that, unlike Thorpe tube flowmeters, it is not position dependent. It reads just as accurately in a horizontal position as it does in a vertical position. This makes it the flowmeter of choice when transporting a patient with an oxygen tank.
(5) Because this gauge actually measures pressure, an obstruction to flow through the tubing attached to a Bourdon gauge flowmeter resulting in back pressure will cause the gauge reading to increase slightly. In other words, the gauge will indicate flow to the patient, whereas the patient is receiving little or no O2.
8. Air compressors are used to provide medical air through either portable compressors or large medical air piping systems. Two types of air compressors are generally used
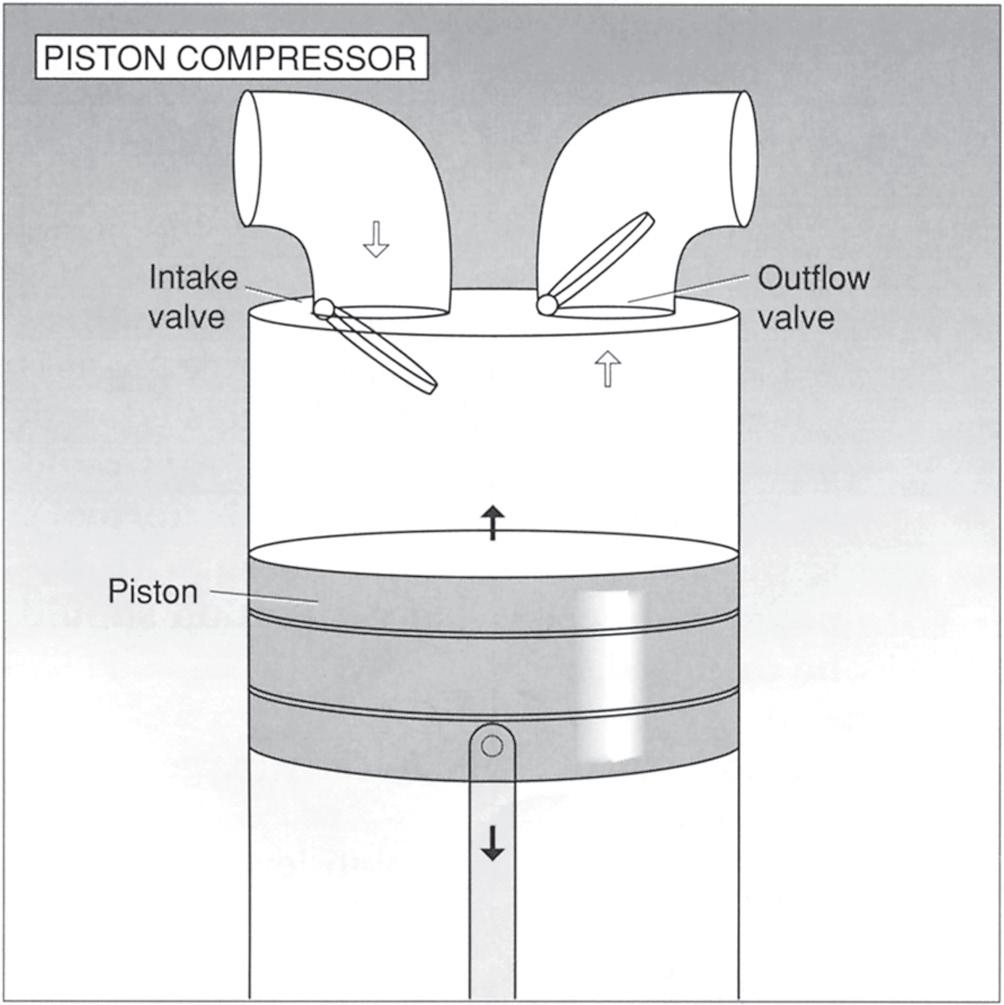
a. Piston air compressor: Air is drawn into the compressor, where it travels to a reservoir tank. From this tank, the air passes through a dryer to remove moisture and on to a pressure-reducing valve, which reduces the pressure to 50 psig to power a compressed-air wall outlet. As the piston drops, gas is drawn in through a one-way intake valve. On the upstroke, the intake valve closes and gas exits through a one-way outflow valve. Piston air compressors are seen most commonly on large medical air piping systems.
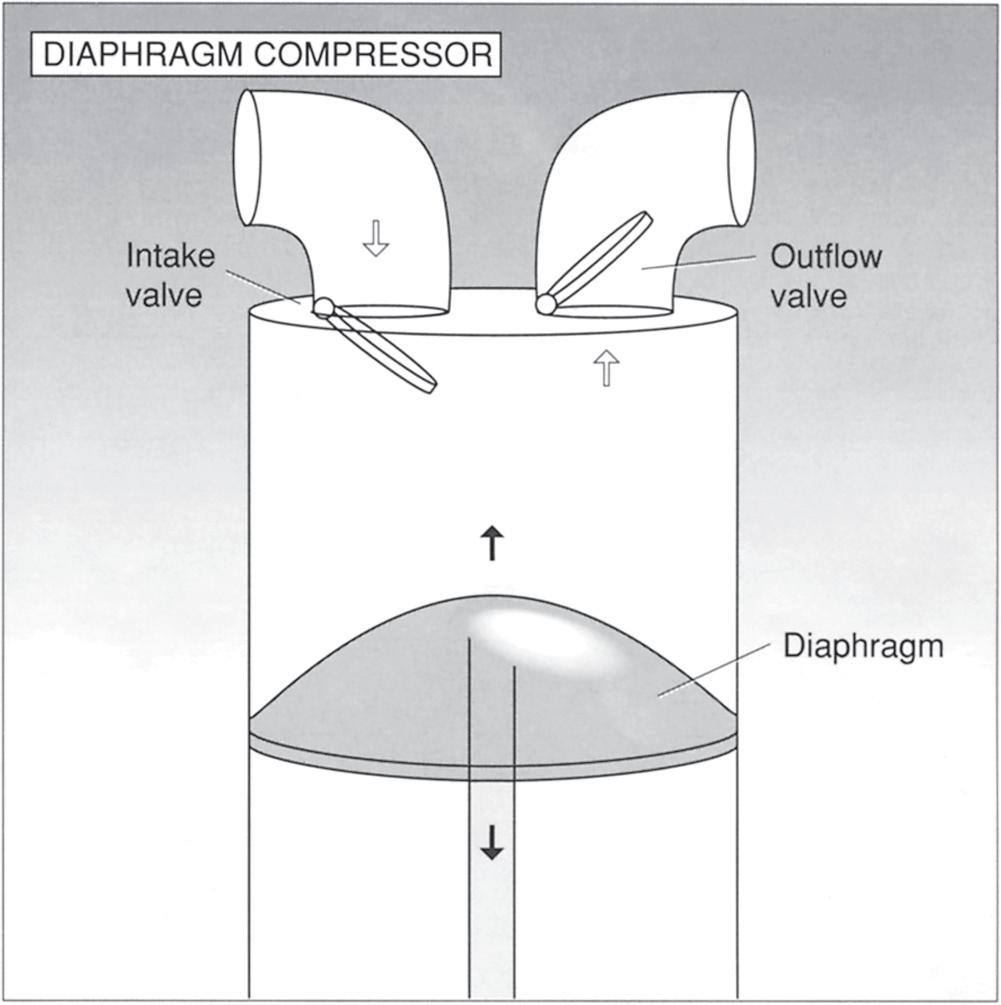
b. Diaphragm air compressor:
A diaphragm is used instead of a piston. On the downstroke, the flexible diaphragm bends
1-7
1-8
downward, drawing air through a one-way intake valve. On the upstroke, air is forced out the one-way outflow valve. Diaphragm air compressors are commonly used on O2 concentrators and portable air compressors.
II. O2 THERAPY
A. Indications for O2 Therapy
1. Hypoxemia
2. Labored breathing or dyspnea
3. Increased myocardial work
FIGURE
FIGURE
B. Signs and Symptoms of Hypoxemia
1. Tachycardia
2. Dyspnea
3. Cyanosis (unless anemia is present)
4. Impairment of special senses
5. Headache
6. Mental disturbance
7. Slight hyperventilation
C. Complications of O2 Therapy
1. Respiratory depression: The patient with chronic obstructive pulmonary disease (COPD) who is chronically hypoxic is most affected. Maintain PaO2 between 50 and 65 mm Hg for these patients.
2. Atelectasis: High O2 concentrations in the lung can wash out nitrogen in the lung and reduce the production of surfactant, which may lead to atelectasis. Maintain FiO2 below 0.60.
3. O2 toxicity: High O2 concentrations result in increased O2 free radicals and therefore lung tissue toxicity. This may lead to acute respiratory distress syndrome (ARDS). Maintain FiO2 below 0.60.
4. Reduced mucociliary activity: Maintain FiO2 below 0.60. The beating of the cilia in the mucociliary blanket is not as active when high FiO2 levels are used.
5. Retinopathy of prematurity (ROP): This is caused by high PaO2 levels in infants and results in blindness. It is more common in premature infants. Maintain PaO2 below 80 mm Hg. The normal level of PaO2 in infants is 50 to 70 mm Hg.
D. Normal PaO2 Values by Age
Exam Note
To determine what a normal PaO2 is while any oxygen percentage is being breathed, multiply the percentage by 5. For example, a normal PaO2 for a patient breathing 40% oxygen would be approximately 200 torr (40 3 5). This is an approximation but can be helpful on the exam. If a patient on 40% has a PaO2 of 300 torr, this represents a laboratory error because it’s not possible to have a PaO2 that high on 40%. If the PaO2 is approximately five times the O2% that the patient is breathing, titrate the oxygen level or discontinue the oxygen if titration is not a choice.
E. Four Types of Hypoxia (low O2 level in the tissues)
1. Hypoxemic hypoxia
a. Caused by lack of O2 in the blood as a result of (1) Inadequate O2 in the inspired air: Administering O2 is beneficial.
(2) Alveolar hypoventilation: Administering O2 alone will not be beneficial.
(3) Diffusion defects (e.g., pulmonary edema, atelectasis, and pulmonary fibrosis): Administering O2 alone may not be beneficial.
(4) A ventilation/perfusion mismatch: Administering O2 may be beneficial.
(5) An anatomic right-to-left shunt: Administering O2 is not beneficial.
b. If a normal PaO2 level cannot be maintained with a 60% O2 mask, a large shunt is probable and should not be treated with higher O2 concentrations. CPAP should be administered provided that the PaCO2 is at normal or below normal levels. If the PaCO2 level is elevated in a patient with hypoxemia, mechanical ventilation should be initiated.
Exam Note
When given a patient using 60% O2 or higher who is ventilating adequately (normal or low PaCO2) but has hypoxemia, place the patient on CPAP. The exception to this rule is if the question states that the patient has hypotension, a low cardiac output, or an elevated intracranial pressure. Positive pressure should not be administered because the increased intrathoracic pressure may worsen these conditions. Thus in these situations, increase the FiO2
2. Anemic hypoxia
a. The blood’s capacity to carry O2 is reduced as a result of
(1) A decreased hemoglobin (Hb) level.
(a) Normal Hb level is 12 to 16 g/dL of blood.
(b) The PaO2 level may be normal, but because of the reduced capacity of the blood to carry O2, the tissues may be deprived of O2. The Hb value must be determined to assess the patient’s oxygenation status.
(c) The Hb content may be increased by administering packed red blood cells (RBCs).
(2) CO poisoning
(a) CO affinity for Hb is 200 to 250 times faster than that of O2 and therefore occupies the iron-binding sites on Hb before O2 can. This causes tissue hypoxia.
(b) Because Hb releases the CO more readily when levels of PaO2 are high, the patient should immediately be
given 100% O2, usually via a nonrebreathing mask, which delivers high O2 concentrations.
Exam Note
If the question states that the patient has been exposed to CO, always select the device that provides 100% O2, whether it is a nonrebreather, CPAP, or endotracheal (ET) tube flow-by.
(c) Elevating the PaO2 even higher to further increase the dissociation of Hb from CO may be achieved with hyperbaric O2 therapy (discussed later in this chapter).
(d) Patients who have been involved in fires or who have been breathing car fumes must be treated immediately for CO poisoning.
(e) PaO2 and Hb saturation (SaO2) readings (discussed later in this chapter) may be within a normal range even though the patient has severe hypoxia.
(f) The level of CO bound to Hb (carboxyhemoglobin) may be determined with CO oximetry (discussed later in this chapter).
(g) The patient usually presents with a normal PaO2 level and a low or normal PaCO2 level. The pH level is usually low as a result of lactic acidosis (metabolic acidosis), caused by severe hypoxia. Lactic acid is produced as the body goes into anaerobic metabolism trying to provide more O2 to the tissues.
(h) The following blood gas results on 100% O2 may be observed with patients exposed to CO:
pH 7.24
PaCO2 26 mm Hg PaO2 255 mm Hg
HC O3 15 mEq/L
B.E. 10 mEq/L
SaO2 60%
CoHb 40%
It is tempting in this situation to want to decrease the O2 level because the PaO2 is 255 mm Hg, but the saturation level is only 60%. This patient is experiencing severe hypoxemia. The reason the SaO2 is so low and the PaO2 is so high is that O2 is not able to combine with Hb because it is already carrying CO. Therefore the O2 dissolves in the
plasma, thereby increasing the PaO2. O2 levels should not be decreased until the SaO2 level is around 95%.
(3) Excessive blood loss also may result in anemic hypoxia. Administering blood (RBCs) is the appropriate treatment.
(4) Methemoglobin may cause anemic hypoxia and is most commonly a result of nitrite poisoning. Treat by administering ascorbic acid or methylene blue, which removes the chemical (nitrite) from the system.
(5) Iron deficiency leads to anemia and is treated by increasing iron intake and administering blood.
b. The blood carries O2 in two ways:
(1) Bound to Hb: 1 g of Hb is capable of carrying 1.34 mL of O2. To determine the milliliters of O2 carried by Hb, use this formula: (1.34 3 Hb 3 SaO2).
(2) Dissolved in plasma: 0.003 mL of O2 dissolves in plasma for every 1 mm Hg of O2 tension (PaO2), or (0.003 3 PaO2).
Exam Note
The sum of these two mechanisms equals the total arterial O2 content in mL/dL of blood, which is the most effective method for determining the O2-carrying capacity of a patient’s blood.
EXAMPLE:
Given the following information, calculate the patient’s total arterial O2 content.
Arterial Blood Gas Study Results
pH 7.42
PCO2 41 mm Hg
PO2 90 mm Hg
SaO2 98% Hb 15 g/dL
Exam Note
When calculating total O2 content on the exam, it is not necessary to calculate O2 dissolved in the plasma. The amount is always less than 1 mL. So take the answer you get after calculating the amount of O2 bound to Hb and pick the answer that is closest to that number but just above it. The answers are far enough apart to determine the correct answer.