PediatricCardiology
Contents
Foreword:GenerationsofDedicatedResearchersResultinginGenerationsof ConstantProgress:PediatricCardiologyxv BonitaF.Stanton
Preface:PediatricCardiology:FromBasicstoInnovationxvii Pei-NiJone,D.DunbarIvyandStephenR.Daniels
EvaluatingChestPainandHeartMurmursinPediatricandAdolescentPatients783
ChristopherA.SumskiandBenjaminH.Goot
Chestpainandheartmurmursarecommonissuesprimarycareproviders mustevaluateandmanage.Bothareasourceofanxietyforpatients,parents,andproviders,necessitatingevaluationandunderstandingtoensure appropriatemanagement.Mostpediatricchestpaincanbetreatedsymptomaticallyandwithreassurance.Thisarticleexaminestheapproachto pediatricchestpainincludingidentificationofkeyhistoricalpoints,commoncausesofchestpain,andwhentorefer.Thearticlealsodelineates ourapproachtoauscultation,describescommonbenignmurmurs,andofferssuggestionsonwhentoreferforfurtherevaluation.
SyncopeandPalpitations:AReview801
JohannesC.vonAlvensleben
Syncopeandpalpitationsarecommoncomplaintsforpatientspresenting totheirprimarycareprovider.Theyrepresentsymptomsthatmostoften haveabenignetiologybutrarelycanbethefirstwarningsignofaserious condition,suchasarrhythmias,structuralheartdisease,ornoncardiac disease.Thehistory,physicalexamination,andnoninvasivetestingcan, inmostcases,distinguishbenignfrompathologiccauses.Thisarticleintroducessyncopeandpalpitations,withemphasisonthedifferentialdiagnoses,initialpresentation,diagnosticstrategy,andvariousmanagement strategies.
UpdateontheManagementofKawasakiDisease811
KevinG.FriedmanandPei-NiJone
TreatmentofKawasakidisease(KD)withintravenousimmunoglobulin (IVIG)administeredwithintheinitial10daysoffeveronsetdecreasesthe riskofcoronaryarteryaneurysms(CAAs)from w 25%tolessthan5%. However,patientswithIVIGresistance,younginfants,men,highlyinflamedpatients,and/orthosewithcoronarychangesatdiagnosisremain athighriskforCAA.High-riskpatientsmaybenefitfromacute,adjunctive antiinflammatorytreatmentinadditiontoIVIG.Optimaltherapyremains unknown.Thisarticlereviewstheacutepharmacologicmanagementof patientswithKD,focusingonadjunctiveprimarytherapyoptionsand treatmentofpatientswithIVIGresistance.
CommonLeft-to-RightShunts821
DaleA.Burkett
Videocontentaccompaniesthisarticleat http://www.pediatric.theclinics. com.
Left-to-rightshuntsrepresentasignificantportionofcongenitalheartdisease.Suchlesionsarecommoninisolation,butarefrequentlyseenin conjunctionwithother,oftenmorecomplex,congenitalheartdisease. Thisreviewcoversbasicanatomy,physiology,physicalexaminationfindings,diagnosisandmanagementforatrialseptaldefects,ventricular septaldefects,andpatentductusarteriosa.
UpdateonPreventionandManagementofRheumaticHeartDisease843 CraigSable
Rheumaticheartdisease(RHD)remainsthemostcommoncauseofcardiovascularmorbidityandmortalitygloballyinchildrenandyoungadults. ThisarticlefocusesonpreventionandmanagementofRHD.Pregnancy canunmaskpreviouslyundiagnosedRHDandposeshighriskformother andfetus.Managementofanticoagulationisimportant.Definitivecatheter andsurgicalinterventionaretheonlytreatmentsthatcanimproveoutcomesofpatientswithmoderateorsevereRHD.AccesstointerventionremainsverylimitedinRHDendemicregions.Thereareongoingglobal effortstoincreaseawareness,publicpolicyadoption,andgreateraccess totreatment.
Diagnosis,Evaluation,andTreatmentofMyocarditisinChildren855
AdamPutschoeglandScottAuerbach
Myocarditisinthepediatricpopulationcanbeachallengingdiagnosisto makeandoftenrequiresutilizationofmultiplediagnosticmodalities.The causeisoftenduetoaviralinfectionwithactivationoftheinnateandacquiredimmuneresponsewitheitherrecoveryordiseaseprogression.Laboratorytestingoftenincludesinflammatorymarkers,cardiactroponin levels,andnatriureticpeptides.Noninvasivetestingshouldincludeelectrocardiogram,echocardiogram,andpossiblyanMRI.Treatmentof myocarditisremainscontroversialwithmostprovidersusingimmune modulatorswithintravenousimmunoglobulinandcorticosteroids.
PediatricInfectiveEndocarditis:AClinicalUpdate875
DanielA.CoxandLloydY.Tani
Thisarticlepresentsupdatesandanoverviewofpediatricinfectiveendocarditis.Itincludesadiscussionofpresentationofillness,diagnosisofthis disorder,differentialdiagnosis,treatmentrecommendation,andassociatedmorbidityandmortality.
UpdateofPediatricHeartFailure889
KaeWatanabeandRenataShih
Pediatricheartfailure(PHF)affects0.87to7.4per100,000children.Ithas a5-yearmortalityorhearttransplantrateof40%.Diagnosisoftenis
delayedbecauseinitialsymptomsaresimilartocommonpediatricillnesses.Diseaseprogressionistrackedbysymptoms,echocardiogram, andbiomarkers.Treatmentisextrapolatedfrommostlyadultheartfailure (HF)literature.Recentstudiesdemonstratedifferencesbetweenpediatric andadultHFpathophysiology.IncreasedcollaborationamongPHFprogramsisadvancingthemanagementofPHF.Unfortunately,therearepatientswhoultimatelyrequirehearttransplantation,withincreasing numberssupportedbyaventricularassistdeviceasabridgeto transplantation.
PediatricPulmonaryArterialHypertension903
BenjaminS.FrankandD.DunbarIvy
Pulmonaryhypertension(PH),thesyndromeofincreasedpressureinthe pulmonaryarteries,isassociatedwithsignificantmorbidityandmortality foraffectedchildrenandisassociatedwithavarietyofpotentialunderlying causes.Severalpulmonaryarterialhypertension–targetedtherapieshave becomeavailabletoreducepulmonaryarterypressureandimprove outcome,butthereisstillnocureformostpatients.Thisreviewprovides adescriptionofselectcausesofPHencounteredinpediatricsandanupdateonthemostrecentdatapertainingtoevaluationandmanagementof childrenwithPH.AvailableevidenceforspecificclassesofPH-targeted therapiesinpediatricsisdiscussed.
UpdateonPreventiveCardiology923
SarahB.ClaussandSarahD.deFerranti
Althoughprogresshadbeenmadeinreducingcardiovasculardisease (CVD)mortality,thepositivetrendhasreversedinrecentyears,and CVDremainsthemostcommoncauseofmortalityinUSwomenand men.YouthrepresentthefutureofCVDprevention;emergingevidence suggestsexposuretoriskfactorsinchildrencontributestoatherosclerosis andresultsinvascularchangesandincreasedCVDevents.ThecontributorstoCVDincludethosecommonlyseeninadults.Thisarticlereviews hypercholesterolemia,hypertension,obesity,diabetes,andsmoking.It discussestheprevalenceofeachdisease,diagnosis,treatment,andcardiovascularcomplications.
OutcomesinHypoplasticLeftHeartSyndrome945
MeghanKileyMetcalfandJackRychik
Hypoplasticleftheartsyndrome(HLHS)isacomplexformofcongenital heartdiseasedefinedbyanatomicandfunctionalinadequacyoftheleft sideoftheheartwithnonviabilityoftheleftventricletoperformsystemic perfusion.Lethalifnottreated,astrategyforsurvivalcurrentlyiswellestablished,withcontinuingimprovementinoutcomesoverthepast30 years.Prenataldiagnosis,goodnewborncare,improvedsurgicalskills, specializedpostoperativecare,anduniquestrategiesforinterstagemonitoringallhavecontributedtoincreasinglikelihoodofsurvival.Theunique lifewithasinglerightventricleandaFontancirculationisafocusedarea ofinvestigation.
OutcomesinAdultCongenitalHeartDisease:NeurocognitiveIssuesandTransition
RoniM.Jacobsen
Thereisagrowingpopulationofpatientslivingwithcongenitalheartdisease(CHD),nowwithmoreadultslivingwithCHDthanchildren.Adults withCHDhaveuniquehealthcareneeds,requiringathoughtfulapproach tocardiac,neurocognitive,mental,andphysicalhealthissues.Theyhave increasedriskofanxiety,depression,pragmaticlanguageimpairment, limitedsocialcognition,worseeducationalattainmentandunemployment, anddelayedprogressionintoindependentadulthood.Asaresult,itis importanttoestablishanindividualizedapproachtoobtainsuccessful transitionandtransferofcarefromthepediatrictoadulthealthcareworld inthispatientpopulation.
InnovationsinCongenitalInterventionalCardiology973
JennyE.ZablahandGarethJ.Morgan
Thisarticleaimstosummarizesomeofthekeyadvancesincongenitalinterventionalcardiologyoverthepastfewyears,fromnovelimagingtechnologies,suchasvirtualreality,fusionimaging,and3-dimensionalprinted models,tonewlyavailabledevicesandtechniquestofacilitatecomplex proceduresincludingpercutaneouspulmonaryvalvereplacementand hybridprocedures.Itisanexcitingtimeforthefield,withrapiddevelopmentoftechniques,devices,andimagingtoolsthatallowaminimallyinvasiveapproachformanycongenitalcardiacdefectswithprogressivelyless radiationandcontrastdoses.
TheNextFrontierinPediatricCardiology:ArtificialIntelligence995
SharibGaffar,AddisonS.Gearhart,andAnthonyC.Chang
Artificialintelligence(AI)inthelastdecadecenteredprimarilyarounddigitizingandincorporatingthelargevolumesofpatientdatafromelectronic healthrecords.AIisnowpoisedtomakethenextstepinhealthcareintegration,withprecisionmedicine,imagingsupport,anddevelopmentofindividualhealthtrendswiththepopularizationofwearabledevices.Future clinicalpediatriccardiologistswilluseAIasanadjunctindeliveringoptimumpatientcare,withthehelpofaccuratepredictiveriskcalculators, continualhealthmonitoringfromwearables,andprecisionmedicine.Physiciansmustalsoprotecttheirpatients’healthinformationfrommonetizationorexploitation.
Foreword
GenerationsofDedicated ResearchersResultingin GenerationsofConstantProgress:
EvaluatingChestPainand HeartMurmursinPediatric
andAdolescentPatients
ChristopherA.Sumski, DO*,BenjaminH.Goot, MD
KEYWORDS
KEYPOINTS
Historyandphysicaloftenidentifythecauseofchestpaininpediatrics,whichisrarelycardiacinorigin.
Chestpainassociatedwithexercise,syncope,orpalpitationsshouldbefurtherevaluated. Vibratory,quiet,intermittentsystolicmurmursinotherwisehealthychildrenrarelyneed furtherevaluation.
Loud,harsh,ordiastolicmurmurs,murmursaccompaniedbyathrill,orotherabnormal findingsshouldbeevaluatedbypediatriccardiology.
CHESTPAIN
Introduction
Chestpainaccountsfor0.3%to0.6%ofpediatricvisitstotheemergencydepartmentoroutpatientclinic.1,2 Therearemanyetiologies,butcardiacpathologytypicallyremainstheprimaryconcern.1 ,3 Distressandfearregardingchestpainislikely causedbypublicawarenessoftherelationshipbetweenthissymptomandheart disease,andthepublicityofrarecasesofpediatricsuddencardiacdeath. 1 ,4–6 Additionally,withthepopularityofactivitymonitorstrackinghealthstatistics,peoplearemorekeenlyawareoftheirheart.Thisconfluenceleadstoconcernsthat affectqualityoflifeandcanleadtomissingschoolandself-limitationfrom exercise.1
Chestpaininpediatricsisrarelycardiacinnature.Saleebandcolleagues6 reviewed 3700patientswithoutpreviouslyknowncardiovasculardisease,representingnearly 18,000patient-years,andfoundlowincidenceofcardiacpathology(1%)andnomortalitysecondarytocardiacdiseasefollowingassessment.Conversely,inaseparate
HermaHeartInstitute,Children’sWisconsin&MedicalCollegeofWisconsin,9000WestWisconsinAvenue,Milwaukee,WI53226,USA
*Correspondingauthor.
E-mailaddress: csumski@wustl.edu
PediatrClinNAm67(2020)783–799 https://doi.org/10.1016/j.pcl.2020.05.003
pediatric.theclinics.com 0031-3955/20/ª 2020ElsevierInc.Allrightsreserved.
Box1
Commonnoncardiacdifferentialdiagnosis
Musculoskeletal
Idiopathic
Musclestrain
Costochondritis
Slippedrib
Chestwallabnormalities
Trauma
Precordialcatchsyndrome
Pulmonary
Pneumonia
Pleuritis
Pneumothorax
Asthma
Pulmonaryembolus
Pulmonarycontusion
Pleuraleffusion
Chroniccough
Gastrointestinal
Gastroesophagealrefluxdisease
Pepticulcerdisease
Gastritis
Esophagealspasm
Esophagitis
Psychogenic
Anxiety
Depression
Bullying
Miscellaneous
Herpeszoster
Toxin/drugexposure
Breasttenderness
studybythesamegroupevaluatingthosewithprovencardiacdisease,mostpatients withseriouscardiacpathologypresentedwithchestpainwithexertion,suggesting thiscomplaintisnotonetotakelightly.3
DifferentialDiagnosis
Practitionersevaluatingayoungpatientwithchestpainshouldremainopen-minded. Considerationscovermanysystems(Box1)includingcardiac,gastrointestinal, musculoskeletal,pulmonary,andpsychogenicsources.6,7 Thissectionprovidesan overviewofsomecommonsourcesanddiagnosticclues.
Musculoskeletal
Musculoskeletalcausesofchestpainarecommonandcanarisefrombone,cartilage, muscles,tendons,orligaments.1,7,8 Oftentheanswerisfoundinthehistoryalone.For example,excessiveexercise,asthma,orarecentcoughingillnesssuggestsa muscularstrain,whereasaboneyabnormalityisaconsiderationwithrecenttrauma.
Idiopathicchestpainiscommonandpresentsassharp,unilateralpainlasting severalsecondstominutes.Itisusuallyleftsidedandnotreproducibleonpalpation. Thepainisintermittentandusuallywithoutanycleartriggers.Notreatmentisrequired
otherthanreassurance.Idiopathicchestpainoftenself-resolvesinweeksto months.1,9
Costochondritisrepresentsinflammationofcostochondraljoints.Painoccursatthe jointsandinvolvesmultiplecostalcartilages.Thecauseisnotalwaysknown,but inflammationisoftenprecededbyrespiratoryillness.Thererarelyisredness,warmth, orindurationbutthepainisusuallyreproduciblewithpalpation.Costochondritisis oftenself-limited;however,treatmentwithnonsteroidalanti-inflammatorydrugs maybenecessary.
Verybrief,sharp,stabbingpainworsebydeepinspirationissuggestiveofprecordialcatch.Thecauseisnotunderstood.Painisusuallyovertheleftsternalborderand canbeintense.Usuallypatientsreportneedingtotakeshallowbreathswhileawaiting resolution.Thepainusuallyself-resolves,requiringonlyreassurance.
Slippingribsyndromeiscausedbyincreasedmobilityofthefloatingribs.This hypermobilityallowstheribstoslipupwardputtingpressureontheintercostal nerve.10 Theremaybeahistoryoftrauma,andpainisworsewithcoughing,stretching, oractivity.Thehookingmaneuver,wheretheproviderelicitsaslippingoftheribsby retractingthecostalmarginanteriorlyandsuperiorly,isdiagnostic.Treatmentisusuallysymptomatic,butcouldrequiresurgeryforrelief.
Pulmonary
Respiratoryillnessesorbronchospasmcanleadtostrainoroveruseoftheaccessorymusclesofrespirationandpain.Wiensandcolleagues11 reportedahigher thananticipatedincidenceofexercise-inducedasthmainpatientswithchestpain. Physicalexaminationmaybenormal,buthistoryofshortnessofbreath,coughing, chesttightness,orwheezingwouldbepresent.Withexercise-inducedbronchospasm,symptomscouldbereplicatedwithexercisetestingandimprovedwith b -agonists.
Pneumoniamaypresentwithchestpainfrommusclestrainorpleuralirritation. Althoughnotuniversallypresent,fever,cough,andrespiratorysymptomsmaybeconcurrentwiththechestpain.Supportingphysicalexaminationfindingsincludefocal decreasedbreathsounds,crackles,andtachypnea.Chestradiographmaybeuseful inthediagnosis.
Pneumothoraxrepresentsairbetweenthechestwallandlungparenchyma.Multiple mechanismscancausepneumothorax.Commonetiologiesincludetraumaorspontaneouspneumothoraxinthosewithconnectivetissuedisease.Symptomsinclude suddenonsetchestpain,shortnessofbreath,and/orincreasedworkofbreathing. Evaluationdemonstratesdecreasedbreathsoundsandassociatedabsenceoflung markingsonradiograph.Itisimportanttoevaluateforrespiratorycompromiseinpatientspresentingwithpneumothorax.
Pulmonaryembolismisararecauseofchestpaininchildren;however,becauseof itsseriousnature,at-riskpatientswhopresentwithchestpain,shortnessofbreath, andcyanosisshouldpromptassessment.12 Riskfactorsincludepatientorfamilyhistoryofclottingdisorder,malignancy,recentsurgery,periodofimmobilization,ororal contraceptiveuse.
Gastrointestinal
Themostcommongastrointestinalcauseofchestpainisgastroesophagealreflux,but otherconsiderationsincludepepticulcerdisease,esophagealspasm,esophagealor gastricinflammation,orcholecystitis.Diagnosisisprimarilymadebyhistory,basedon relationshipstoeating,diet,andpainquality(eg,burningpainassociatedwithreflux). Treatmentistypicallyconservativewithdietadjustmentand,ifnecessary,medication.
Psychogenic
Adiagnosisofexclusion,psychogenicchestpainshouldbeaconsiderationonce othercausesareruledout.1,7 Historymayidentifyanacutestressorathomeorschool. Withincreasingconcernsovercyberbullyingandschoolviolenceonemustbevigilant toassessforthis.13 Onceidentified,treatmentislargelyconservativeandincludes reassuranceandcopingstrategies.Psychiatricevaluation,counseling,anddirected therapymaybenecessary.
Miscellaneous
Miscellaneouscausesincludepainassociatedwithbreastdevelopmentorabnormal thoracicshape,suchaspectusabnormalitiesorscoliosis.Herpeszosterofthechest wallmaycausepainorburningbeforearashdevelops.Toxiningestionshouldbe considered,especiallyifthepatienthasapositivehistoryorclinicalsignsofabuse. Drugabusewithamphetaminesandcocainehasbeenlinkedtochestpainandacute myocardialinfarction.14,15
Cardiac
Cardiacchestpainisdividedintoanatomicabnormalities,myocardial/pericardialabnormalities,andarrhythmias.Potentialcausesarelistedin Box2
Hypertrophiccardiomyopathycausesasymmetricmyocardialhypertrophyandaffects1:500individualsintheUnitedStates.AccordingtoMaronandcolleagues4 it isthemostcommoncardiaccauseofsuddendeathamongyoungcompetitiveathletes.16 Hypertrophycancauseleftventricularoutflowobstruction.17 Furthermore, theincreasedmassincreasesoxygendemand,especiallywithexercise,whereas theobstructioncancausedecreases(insteadofthenormalincrease)inbloodpressureandcoronaryperfusion.Thiscanleadtoischemia,arrhythmia,anddeath.Chest painisnotthetypicalpresentingsymptom,buthasbeendescribed,alongwithpalpitations,syncope,andsuddendeath.1 Becauseofincreasedscreeningpractices,patientsmayalsobeidentifiedduetoanaffectedfamilymember.18 Onexamination patientshaveasystolicejectionmurmurifthereisobstruction,louderwithstanding orValsalva.Theelectrocardiogram(EKG)canbenormal,orfindingsincluding increasedvoltagesandischemicchangesmaybepresent.
Aorticstenosiscanalsoleadtoleftventricularoutflowtractobstructionandcause chestpain.Stenosiscanoccurbelow,atthelevelof,orabovetheaorticvalve.
Box2
Commoncardiaccausesofchestpain
Anatomicabnormalities
Anomalouscoronaries
Coronaryinsufficiencysecondarytonarrowingorcompression
Coronaryaneurysm
Leftventricularoutflowobstruction(aorticstenosis,hypertrophiccardiomyopathy)
Aorticdissection
Myocardial/pericardial
Cardiomyopathy
Myocarditis
Pericarditis
Pericardialeffusion
Arrhythmogenic
Supraventriculartachycardia
Ventriculartachyarrhythmia
Frequentectopy(oftendescribedaspainbyyoungerpatients)
Obstructionleadstoincreasedworkloadfortheleftventricle,resultinginhypertrophy, increasedoxygendemand,anddiminishedcoronaryreserve.Thesechanges(inadditiontolimitedcardiacoutputduringexercise)canleadtoischemiaand arrhythmia.19,20 Aorticstenosisisoftenprogressive,andsymptomsmaybeabsent untillateinthedisease.Ifpresenttheyincludedyspneawithexertion,angina,andsyncope.Asystolicejectionmurmurthatradiatestothecarotidsandalaterallydisplaced pointofmaximumimpulsebecauseofhypertrophymaybefoundonexamination.
Ifpainoccursduringtimesofincreasedmyocardialoxygendemand,suchasexertion,coronaryinsufficiencyshouldbeaconsideration.Repeatischemiceventscan leadtomyocardialscar,anidusforpotentiallydangerousarrhythmias.Thisinsufficiencycanbecausedbyanatomicabnormalitiesofthecoronaries,suchasan abnormalvesseloriginoranatypicalcoursethatresultsinintraluminalnarrowing.21,22
Autopsystudieshavesuggestedanomalousaorticoriginofthecoronaryarteryaccountsforapproximately15%ofallsuddendeathinyoungcompetitiveathletesbut trueincidenceisunknownbecausenotallpatientsaresymptomatic.4,21,22 Furthermore,coronaryvasospasm,congenitalheartdiseaserelatedanomalies,andstenosis oraneurysmfollowingvasculitis(ie,Kawasakidisease)shouldalsobeconsidered.8,22–24 Exertionalsymptoms,palpitations,presyncope,orsyncopeassociated withchestpainshouldallpromptassessmentofthecoronaries.
Inflammatoryprocessesofthemyocardiumorpericardiumcancausechestpain. Etiologiesincludeviral,bacterial,andautoimmunecauses.Theextentofinflammation existsonaspectruminvolvingthepericardium,myocardium,orboth(myopericarditis).Typicallymyopericarditisisapericardialprocessextendingintothemyocardium, whereasmyocarditisisprimarilywithinthemyocardium,althoughthisisnotalways clearlydefined.25,26 Importantly,myocarditisshouldbetreatedaggressivelybecause thereispotentialforfurthersequelaeincludingcardiacarrest.4 Inflammatorydisease mostoftenpresentswithacute,sharporsqueezing,substernalchestpain.Withpericardialinvolvementthepainisworsewithsupinepositioningleadingpatientstolean forward.Paincanbeworsewithinspirationormovement.Onauscultationapericardialfrictionrubmaybeappreciated.Effusion,ifpresent,canleadtotamponadeand hemodynamiccompromise,thereforepulsusparadoxus,jugularvenousdistention,or profoundtachycardiashouldpromptechocardiography.Pericarditistreatmentistypicallyconservativewithnonsteroidalanti-inflammatorydrugsunlessthereisalarge effusionormyocardialinvolvementbecausethesescenariosmayrequireadmission andexpertconsultation.
Evaluationforanarrhythmiamaybewarrantedwhenassessingchestpaininapediatricpatient.Tachyarrhythmias,suchassupraventriculartachycardia,canbeinterpretedaspain,especiallyinyoungerchildren.1 Ventriculararrhythmiascanpresent withchestpain,althoughthesepatientsarelikelytoalsoreportsyncope,exercise intolerance,orabortedsuddencardiacdeath.Tachycardiaitselfcancausedemand ischemiaand/orventriculardysfunction,butthisisrare,dependsontypeof arrhythmia,andusuallyrequiresprolongedepisodes.Moretypicallysymptoms includeself-limitedpalpitationsalongsidechestdiscomfort.Ifarrhythmiaisongoing orthereispredispositiontoarrhythmia,EKGwillbediagnostic.
ApproachtothePatientwithChestPain
Theevaluationofapatientwithchestpainshouldfocusonadetailedhistoryandphysicalexaminationbecausethesefrequentlydeterminecause.1,6 Itisunusualforapatientwithisolatedchestpaintopresentascriticallyill,thereforethereisoftentime forinvestigation.
Box3
Importantquestions
Whatwereyoudoingwhenthepainstarted/stopped?
Howlongdidthepainlast?
Wheredidthepainhurtthemost?
Couldyoudoanythingtomakethepainworseorbetter?
Didyoupassoutwhenthechestpainhappened?
Didyouhavepainanywhereelse?
Didyouexperiencetroublebreathingassociatedwiththepain?
Didyoufeellikeyourheartwasskippingbeatswhenyouwerehavingpain?
Howoftendoyouhavethepain?
History
Box3 highlightssomeimportanthistoricalfeatures.Ofprimaryimportanceisidentifyingentitiesneedingacutemanagement. Box4 identifiesfeaturessuggestingcardiac disease.Suchfeaturesaschronicityorreproducibilityargueagainstcardiacischemia oracutephenomena,suchaspneumothoraxorpulmonaryembolus.Symptomsof palpitationsorshortnessofbreathareoftendescribedaschestpaininchildren,thereforeclarificationofthispointisnecessary.Identifyingassociationwithactivities(eg, eating,exertion,orstress)isimportant,asiswhatfollowsthepain(eg,vomiting,syncope,headache).Historyshouldincludeareviewofsystemswithattentiontosymptomsofindigestion,coughordyspnea,fatigue,activitytolerance,jointpainsor redness,edema,fevers,associatedillnesses,orrecenttrauma.
Itisimportanttoobtainfamily,social,medication,andpersonalmedicalhistories wheninvestigatingchestpain.Familyhistoryoffrequentsyncope,suddencardiac death(includingsuddendeathduringexerciseorsuddeninfantdeathsyndrome), congenitalheartdisease,cardiomyopathy,andarrhythmiaareimportantbecauseentitiesmaybefamilial.4 Socialhistorycoulduncoverdrugabuseoruseofe-cigarettes, whichhasbeenassociatedwithlunginjuryandchestpain.27–30 Amedicalhistory includingconnectivetissuedisease,autoimmunedisease,orKawasakidiseasemay directonetoruleoutcoronaryinsufficiency,aorticdissection,pericardialeffusion, orpneumothorax.
Box4
Cardiac“redflags”
Chestpainwithexerciseorassociatedwithphysicalactivity
Chestpainassociatedwithpalpitations
Chestpainassociatedwithsyncope
Familyhistory(firstdegree)ofsuddencardiacdeathorcardiomyopathy
Knownhistoryofcongenitalheartdisease
KnownhistoryofKawasakidisease
Knownhistoryofconnectivetissuedisease
ChestpainassociatedwithEKGabnormalities
Physicalexamination
Physicalexaminationisalwaysindicatedwhenassessingchestpain,butmostpediatriccaseshavenormalexaminations.6 Fevermaysupportaninfectiousorinflammatoryprocess,whereasdesaturationortachypneashouldprompturgentassessment foranintrapulmonaryprocess,suchaspneumoniaorpulmonaryembolus.Tachycardiaisassociatedwithanoncardiaccause,suchasanxiety,ormoreseriouspathology,suchasarrhythmia,myocarditis,orcompensatedheartfailure.Thegeneral appearanceofapatientlendsinformationincludingdegreeofcurrentdistressorfeaturesofchronicdisease.Thechestshouldbeexaminedfordeformityortrauma, includingpalpationofthecostochondraljoints,sternum,andribs.Tendernessof breasttissue,regardlessofgender,canoccur,especiallyinadolescents.Lungexaminationhelpsevaluateforpulmonaryetiologies.Cardiacexaminationshouldinclude palpationforahyperdynamicprecordiumordisplacementofthePMI.Patientswith chestpainandaheartmurmurshouldpromptconsiderationforreferraltoapediatric cardiologist.Systolicejectionqualitymurmursmaybeconsistentwithaorticvalvestenosis,whereassystolicmurmursthatdisappearwhenthepatientissupineorbecome louderwithValsalvacanoccurinhypertrophiccardiomyopathy.Heartsoundsshould beevaluatedforclicks,gallops,rubs,orforaccentuatedP2 suggestingpulmonaryhypertension.Dependingonclinicalhistoryandexaminationfindings,oneshould considerconnectivetissuedisease,suchasMarfansyndrome.31
Diagnostictesting
Studieshaveshownthatintheabsenceofspecificindications,testingbeyondthehistoryandphysicalisoftennothelpful.1,32 Therearesomepatients,however,inwhom furthertestingisindicated.
Chestradiograph Achestradiographisusefultoevaluateforpneumonia,pneumothorax,orskeletalabnormality.Cardiomegalyshouldbefurtherevaluated,but becausepericardialeffusionorenlargedthymusmasqueradesascardiomegaly, twoviewsshouldbeobtained.
Electrocardiogram EKGisusefulbecauseST-segmentchangesinaspecificcoronary distributionsuggestmyocardialischemia,whereasdiffuseST-segmentabnormalities aresuspiciousforpericarditis.Nonspecificrepolarizationabnormalitiesmaybeseen incardiomyopathyormyocarditis.Lastly,hypertrophyispresentinsomecardiomyopathiesorstructuralabnormalities.AnEKGmayalsoprovideevidenceofheritable arrhythmias(eg,longQTsyndrome)orpredispositiontoarrhythmia(eg,WolffParkinson-Whitesyndrome),althoughpediatricEKGinterpretationrequirescaution becausefindingscanbenonspecificandrelatedtoage,bodyhabitus,orlead placement.
Exercisestresstest Anexercisestresstestallowsfordynamicassessmentofheart rhythmandevaluationforischemiaduringexercise.Exercisestresstestisusedforpatientswithexertionalsymptomsandismostusefulwhenpatientsareoldenoughto cooperatewhileprovidingmaximaleffortandsymptomsarereproducedduringthetest.
Echocardiogram Echocardiographyallowsforvisualizationofthemyocardium,ventricularsizeandfunction,andanatomicabnormalities.Echocardiographycanalso beexpensive,lowyield,andidentifyincidentalfindingsthatleadtoclinicaldilemmas,6,33 suchasidentifyingananomalousrightcoronaryarteryarisingfromthe leftsinusofValsalva(itisunclearifanatomyalwayspresentsanidusforischemia).21 Wethereforehighlyrecommendthatechocardiographybeobtainedinconsultation withacardiologist.
Laboratoryexamination Laboratorytestsareinfrequentlyusefulinthework-upof chestpain.Troponintestingshouldbeusedjudiciouslygivenfalse-positiverates, butishelpfulwhenmyocarditisorischemiaareprimaryconcerns.34
Management
Patientswithisolatedchestpainandanunremarkablehistoryandphysicalexaminationoftenrequirereassuranceonly.Initialevaluationisimportant,becauseanextensivework-upandreferralsleadstoincreasedpatientanxiety.Kadenandcolleagues35 reportedthatintheirsurvey37%oftheadolescentswithchestpainweremore anxiousaftervisitingtheirprimarydoctor.Forpatientsreferredtocardiologyonly abouthalfwerethenreassureddespitenopathology.Patientswithanidentified organiccausetotheirpainrequireappropriatemedicaltreatmentandreferralas necessary.Inparticularpatientswitharedflagforcardiacdisease(see Box4)should promptcardiacevaluation.
AUSCULTATIONANDHEARTMURMURS
Introduction
Advancesindiagnostictestinghavede-emphasizedexaminationskillsandmanyprovidersarenotconfidentintheirauscultationskills.36 Earlyultrasoundeducationand theexpansionofpoint-of-careultrasoundhasmadeiteasyforlearnerstobypass theintricaciesofphysicalexamination.37–41 Theresultisthemystificationofauscultation.Furthermore,inhealthcaretodayexpensivetestingishighlyscrutinized,and thereispressuretousemedicalresourcesinaresponsiblemannerwhileavoiding anxietycreatedbyreferraltosubspecialists.42–44 Physicalexaminationandauscultationarecost-effective,safe,andaccurateinthehandsofaskilledpractitioner.45,46 Herewereviewtheskillsandpracticeofcardiacauscultationwithemphasisonthe evaluationofmurmurs.
Sound
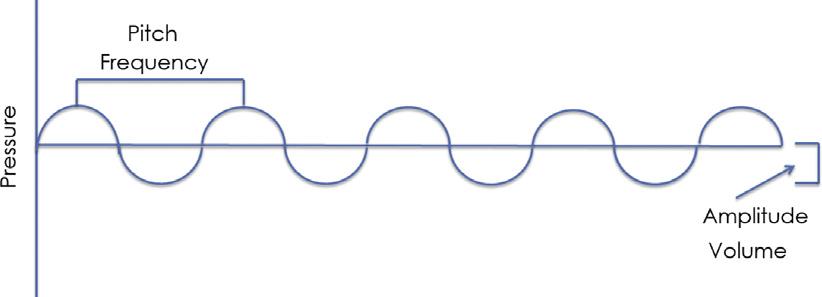
Soundsrepresentpressurechangestransmittedthroughamediumandorganizedina sinusoidalwave(Fig.1)thatisdescribedintermsofwavelengthandamplitude. Shorterwavelengthcauseshigherpitchandhigheramplitudecausesloudervolume.47 Whenwavesofsoundcausevibrationofthetympanicmembrane,theyaresummated andinterpretedbythebrainassound.47 Soundwavesthataccompanytheprimary wavearereferredtoasovertonesorundertones.Ifthesetonesarerelatedinapredictablepattern,theresultis“musical”or“harmonic.”Iftheyarechaotic,thenyouhear “harsh”sound.47
Thecardiaccycle
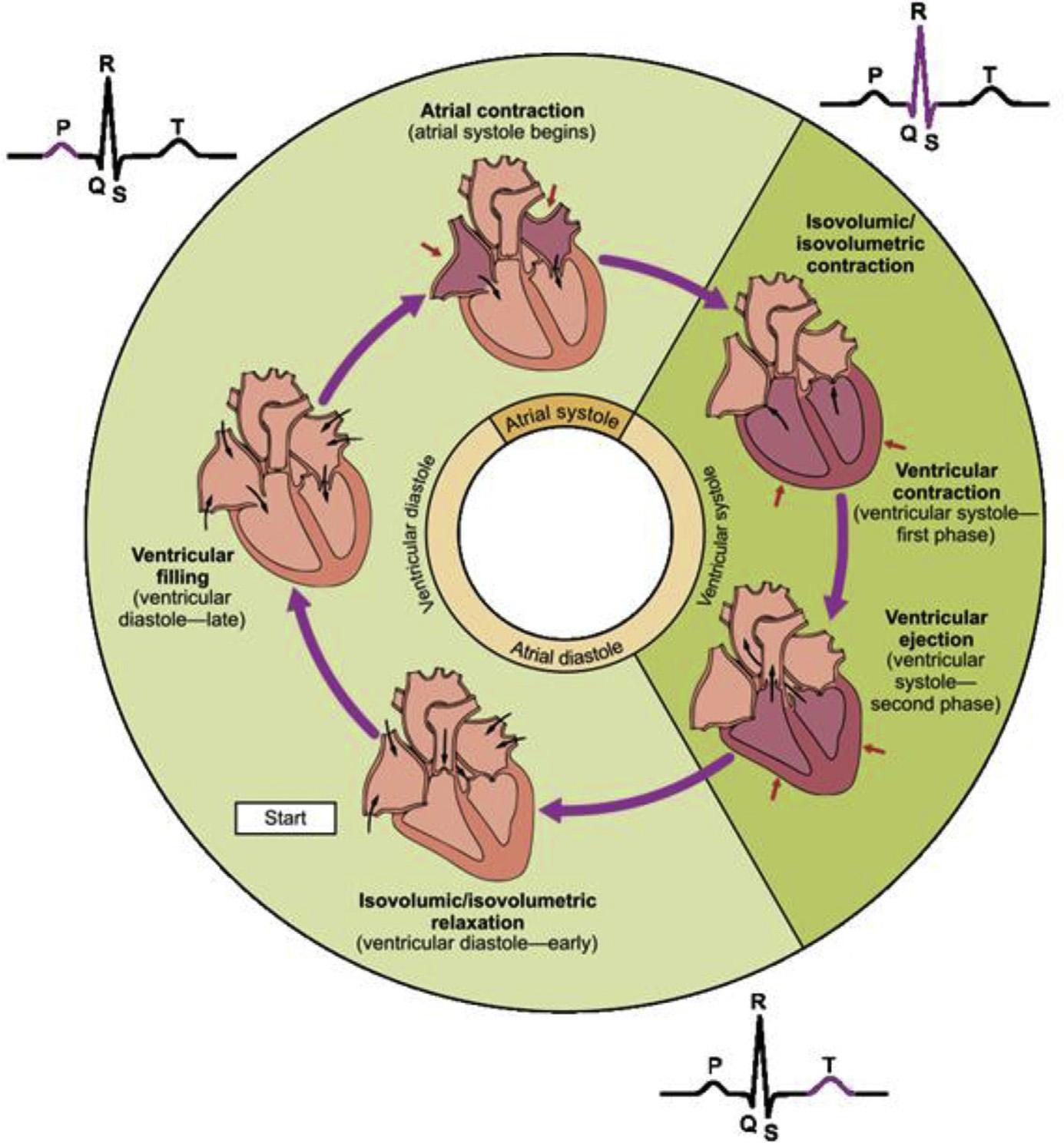
Interpretationofauscultatoryfindingsrequiresanunderstandingofthecardiaccycle (Fig.2).Thecyclebeginswithdepolarizationandactionpotentialpropagationthrough
Fig.1. Soundispressurechangeovertime.Increasedamplituderelatestovolume,whereas shorterwavelengthtohigherpitch.(Courtesyof ChristopherA.Sumski,DO,Milwaukee, WI.)
Fig.2. Thecardiaccycle.(From OpenStaxCollege.Anatomy&physiology–cardiaccycle. Availableat: https://openstax.org/books/anatomy-and-physiology/pages/19-3-cardiac-cycle. License: https://creativecommons.org/licenses/by/4.0/legalcode)
themyocardium,causingcontraction.Thisincreasesthepressureintheventricular cavitycausingatrioventricularvalveclosureandthensemilunarvalveopeningand ventricularejection.Afterejection,relaxationbeginswithadecreaseinventricular pressure.Whenpressurefallslowerthanthatofthegreatarteriesthesemilunarvalves close.Diastolebeginswithatrioventricularvalvesopeningandtheventricularfilling. Afterthe“atrialkick”attheendofdiastolethecyclerepeats.
Heartsounds
Heartsoundsresultfromvibrationsinthebloodresonatingthroughoutthechest.The firstheartsound(S1)occurswithatrioventricularvalveclosure.GenerallyS1 issingle, becausemitralandtricuspidvalveclosureoccurscoincidentally. Thesecondheartsound(S2)representstheclosureoftheaorticandpulmonary valves.HigherpressureintheaortacausesthefirstcomponentofS2 (aorticvalve
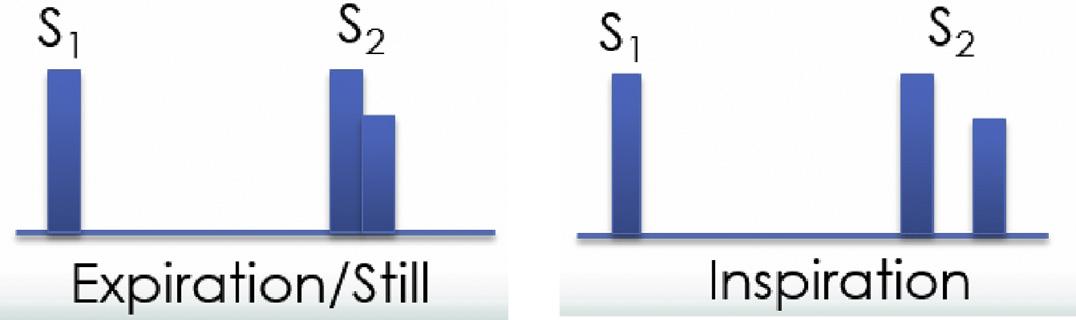
closure,A2)tobeearlierandlouderthanthesecondcomponent(pulmonaryvalve closure,P2).Thisisknownas“splitting”ofS2.Splittingiswidenedoraccentuatedundersomecircumstances(Fig.3).Increasedpulmonarybloodflow,suchaswithatrial septaldefectswithlefttorightshunting,producessplittingthatdoesnotvary(fixed splitS2).
ApproachtoMurmurs
Murmursarethemostcommonreasonforreferraltopediatriccardiology.47–49 They arelargelybenign,onlyapproximately1%representingpathology.47 Evaluation shouldincludecompletehistory,includingpersonal,family,andsocialhistory.History, inadditiontopatientage,presenceofsymptoms,andexaminationfindings,hasbeen helpfulinpredictingthepresenceofheartdiseasewithoutimaging.45
Auscultationmethod
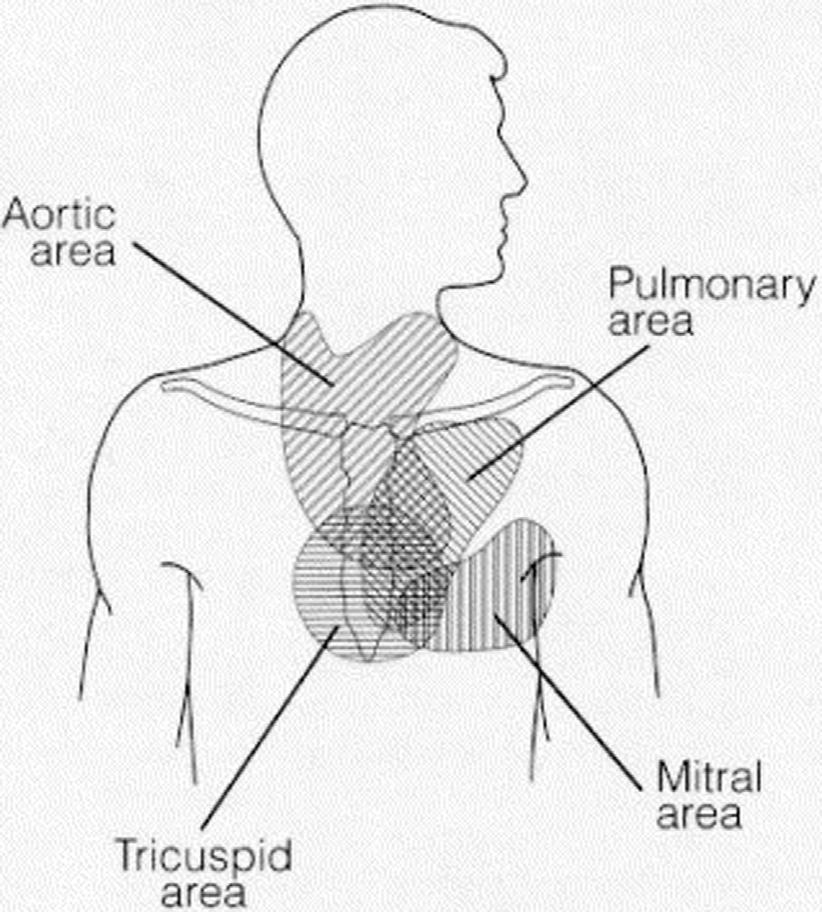
Therearefourclassic“listeningposts”(Fig.4)thatcorrespondtolocationswherethe cardiacvalvesarebestheard.Thesedistinctionsarelesshelpfulinchildren,inparticularchildrenwithcongenitalheartdisease.Thereforewhenevaluatingpatientswith murmurs,practitionersshouldlistenthroughouttheprecordium.
Auscultationshouldbeperformedwiththestethoscope’sdiaphragm(highfrequencysounds)andthebell(lowfrequencysounds).Listenforonesoundatatime. Justasitisdifficulttocharacterizeasingleinstrumentinasymphony,itisdifficult tointerpretasinglemurmurorsoundinthecontextofmany.Abnormalfindingsshould becharacterizedwiththepatientsupine,sitting,andstandingtoevaluatechanges withposition.
Descriptionofheartsounds
Descriptionisacrucialtaskinmurmurevaluation.Itallowsforbettercommunication withothersandaccurateserialevaluation.Completedescriptionincludesseven characteristics.
1.Timing:Referstotimingwithinthecardiaccycle;systolicordiastolic,andearly, mid,orlate.Amurmuriscontinuousifappreciatedthroughoutthecardiaccycle.
2.Volume:Systolicmurmursaregraded1to6.Diastolicmurmursaregraded1to4 (Box5).
3.Location:Whereamurmurisloudestandwhereitradiates.Commonplacesforradiationincludetheback,axillae,orneck.
4.Duration:Murmurscanbeshortorlong,orheardthroughoutthecycle.
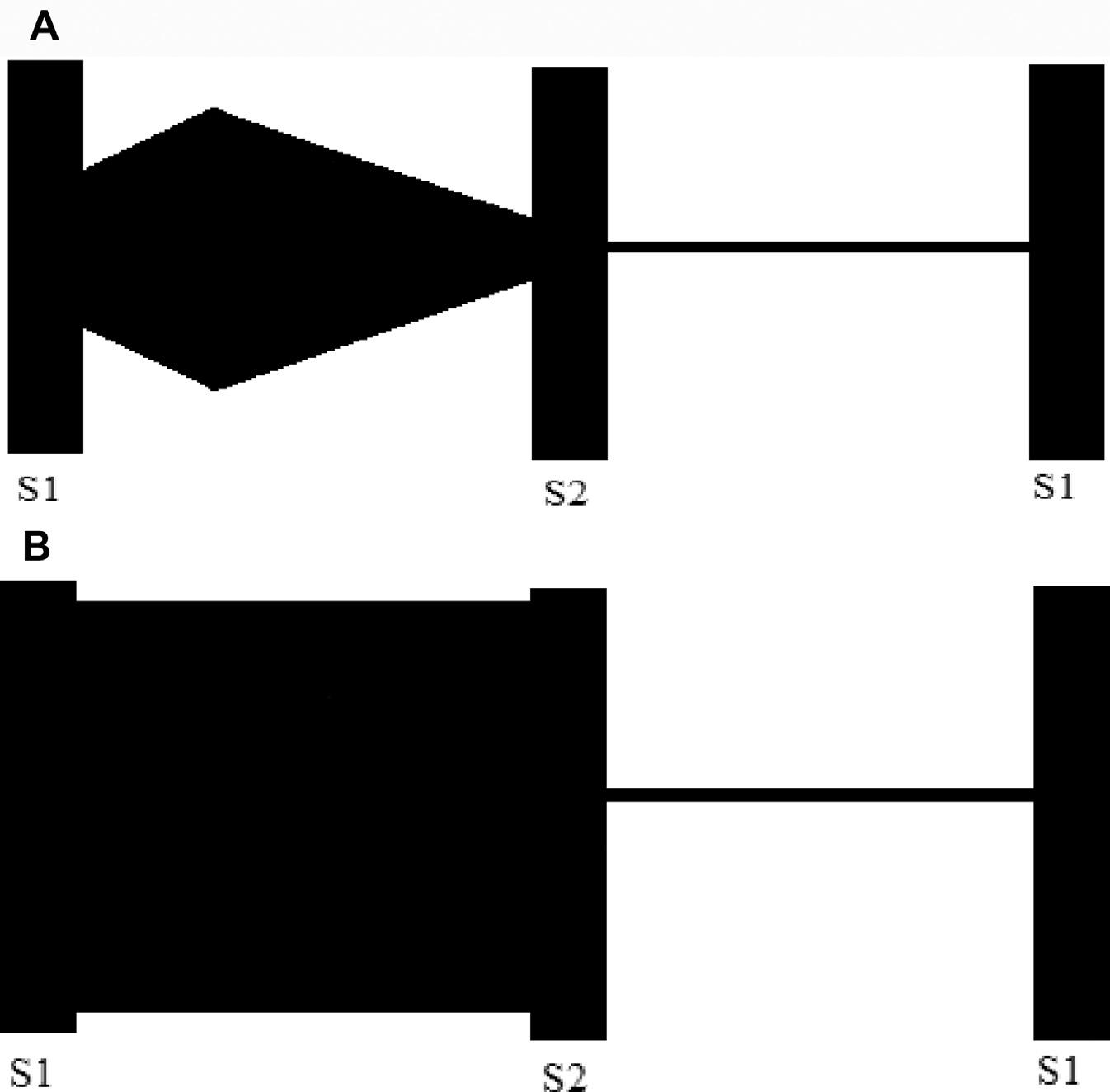
5.Shape:The“shape”ofamurmurisadescriptionofthesound.Commonshapes includeejection(crescendo-decrescendo),crescendo,decrescendo,andholosystolic(Fig.5).
Fig.3. SplittingofS2 withinspirationrepresentsanincreaseofvenousreturnandanincreaseinthebloodejectedthroughthepulmonaryvalve,delayingclosure.(Courtesyof ChristopherA.Sumski,DO,Milwaukee,WI.)
Fig.4. Primaryauscultatingareasarebestthoughtofasgeneralareas,andnotspecific discretelocations.(From PelechAN.Thecardiacmurmur.whentorefer?PediatrClinNorth Am1998;45(1):114;withpermission.)
6.Pitch:Pitchisgenerallyhighorlow.Thisisrelatedtothepressuregradientcausing theturbulenceandthereforemurmur.
7.Quality:Examplesofmurmurqualityincludemusical/vibratory,harsh,andmachinery-like.
CommonInnocentMurmurs
Stillmurmur
AStillmurmurisasystolicmurmuroftennotedinchildrenages2to6years;however, ithasbeendescribedininfantsandadolescents.47 Thecauseisdebatedbutthought toberelatedtovibrationofchordae,relativenarrowingoftheoutflowtractsduring
Box5
Murmurgrading
Systolicmurmurs
1/6–quieterthanS1 andS2
2/6–aboutthesamevolumeasS1 andS2
3/6–louderthanS1 andS2
4/6–thrillpresent,audiblewithonlystethoscopefullyonthechest 5/6–thrillpresent,audiblewithstethoscopepartiallyliftedoffchest 6/6–thrillpresent,audiblewithstethoscopeoffchest Diastolicmurmurs
1/4–quiet,barelyaudible 2/4–quietbutaudible
3/4–clearlyaudible 4/4–loud
systole,orsemilunarvalveleafletvibration.47,48,50–53 AStillmurmurisvibratory,low frequency,andsystolic,loudestattheleftlowersternalborderandapex.Generally graded1to2/6andwithoutradiation,itislouderwithmovingfromstandingorsitting tosupine,whereaslesseningordisappearingwithValsalva.51
Peripheralpulmonarystenosis
Peripheralpulmonarystenosis(PPS)typicallyoccursininfantsuntil6to9monthsof age.PPSissecondarytoturbulentbloodflowinthebranchpulmonaryarteries.In utero,thereislessbloodflowtothelungssecondarytotheductusarteriosusandforamenovale.Giventhereducedflow,thebranchpulmonaryarteriesareoftensmall. Theyarealsoangledacutelyinneonates.Withtheincreaseinpulmonaryblood flowafterbirth,turbulencecanoccur.54 APPSmurmurisgraded1to2/6,systolic ejectionquality,andmoderatelypitched.Itisloudestovertheleftuppersternalborder (LUSB)andradiatestotheaxillaeandback.Persistencepast1yearoramurmurthat getslouderonre-examinationshouldpromptreferraltopediatriccardiology.
Pulmonaryflowmurmurs
Abenignpulmonaryflowmurmurisheardinmanyinfants,children,andadolescents. ThemurmurissimilartothatofPPSwithoutmuchradiation.Typicallyitisheardover Fig.5. Examplesoftheshapesofasystolicejectionmurmur(A)andholosystolicmurmur(B). (Courtesyof ChristopherA.Sumski,DO,Milwaukee,WI.)
theLUSBandisloudestwhensupine,diminishingwhenholdinginspirationorupright positioning.Themurmurisdifferentiatedfrompulmonaryvalvestenosisbecausevalvarstenosisishigherpitch,louder,andoftenaccompaniedbyaclick.Thepulmonary flowmurmurislouderwhenthereisahigheroutputstate,suchaswithfever,anemia, orrecent b-agonisttherapy.
Fig.6. Decision-makingalgorithmformurmurevaluation.
Venoushum
Avenoushumisalow-pitched,continuousmurmurinchildrenlocatedovertheanteriorneckextendingtojustinferiortotheclavicle.Usuallyitisloudestonthepatient’s rightside.Itisthoughttobecausedbytheconvergenceofvenousstreamsfromthe internaljugularandsubclavianveins.55 Themurmurislouderwiththepatientsitting upright,lookingawayfromtheexamineranddiminishedwithjugularcompression orturningtheheadtowardthesidewiththemurmur.
PathologicMurmurs
Whenputtingabnormalmurmurfeaturestogether,onecancreateadifferential.Aholosystolicshapetypicallyrepresentsatrioventricularvalveinsufficiencyoraventricular septaldefect.Ifaccompaniedbyathrillthenthismayrepresentaventricularseptal defectwithsignificantpressuregradient.Earlydecrescendosystolicmurmursmay representtinymuscularventricularseptaldefects.Acrescendo-decrescendosystolic murmurrepresentssystolicejection,andmayreflectpathologyintheoutflowtractsor semilunarvalves.Murmursofsemilunarvalvestenosisoftenincludeaclick,asharp noiseduringsystolecausedbystenoticleafletmotion.Furthermore,anassociated thrillsuggestsadvancedstenosis.Lowerfrequencymachinery-like,continuousmurmursareoftenassociatedwithapatentductusarteriosus.
Management
Evaluationofanychildwithaheartmurmurshouldincludeathoroughhistoryand physicalexamination.Decision-makingshouldbedoneinaholisticcontext.Thriving childrenarelesslikelytohavecardiacdisease.Murmursthataremusical,vibratory, systolicejection,varywithposition,and1to2/6arelikelyinnocentandgenerally needonlyreassessmentatallvisits.43,47,56 Aconcerninghistory,suchasfailureto thrive,poorfeeding,orfrequentrespiratoryinfections,shouldlowerthethreshold forreferral.
Concerningmurmurs(Fig.6)includeharsh,highergrade,diastolic,ormurmursthat radiatetotheneck/carotids.Murmursquieterwithsupinepositioningandlouderwith standingareabnormal.Murmurs(eveninnocentmurmurs)occurringinthesettingof otherabnormalexaminationfindingswarrantfurtherevaluation.
DISCLOSURE
Theauthorshavenothingtodisclose.
Funding:None.
REFERENCES
1. CavaJR,SaygerPL.Chestpaininchildrenandadolescents.PediatrClinNorth Am2004;51(6):1553–68
2.GesueteV,FregolentD,ContornoS,etal.Follow-upstudyofpatientsadmittedto thepediatricemergencydepartmentforchestpain.EurJPediatr2019. https:// doi.org/10.1007/s00431-019-03495-5
3. KaneDA,FultonDR,SaleebS,etal.Needlesinhay:chestpainasthepresenting symptominchildrenwithseriousunderlyingcardiacpathology:chestpainas presentingsymptominchildren.CongenitHeartDis2010;5(4):366–73
4. MaronBJ,HaasTS,AhluwaliaA,etal.Demographicsandepidemiologyofsuddendeathsinyoungcompetitiveathletes:fromtheUnitedStatesNationalRegistry.AmJMed2016;129(11):1170–7
5. HarmonKG,AsifIM,KlossnerD,etal.IncidenceofsuddencardiacdeathinNationalCollegiateAthleticAssociationathletes.Circulation2011;123(15): 1594–600
6. SaleebSF,LiWYV,WarrenSZ,etal.Effectivenessofscreeningforlife-threatening chestpaininchildren.Pediatrics2011;128(5):e1062–8
7. PantellRH,GoodmanBW.Adolescentchestpain:aprospectivestudy.JAm AcadChildPsychiatry1983;22(5):510.
8. VeeramReddySR,SinghH.Chestpaininchildrenandadolescents.PediatrRev 2010;31(1):e1–9
9. DriscollDJ,GlicklichL,GallenW.Chestpaininchildren:aprospectivestudy.Pediatrics1976;57(5):648–51
10. McMahonLE.Slippingribsyndrome:areviewofevaluation,diagnosisandtreatment.SeminPediatrSurg2018;27(3):183–8
11. WiensL,PortnoyJ,SabathR,etal.Chestpaininotherwisehealthychildrenand adolescentsisfrequentlycausedbyexercise-inducedasthma.Pediatrics1992; 90(3):350–3
12. DiNisioM,vanEsN,Bu ¨ llerHR.Deepveinthrombosisandpulmonaryembolism. Lancet2016;388(10063):3060–73
13.NixonC.Currentperspectives:theimpactofcyberbullyingonadolescenthealth. AdolescHealthMedTher2014;143. https://doi.org/10.2147/AHMT.S36456
14. WestoverAN,NakoneznyPA,HaleyRW.Acutemyocardialinfarctioninyoung adultswhoabuseamphetamines.DrugAlcoholDepend2008;96(1–2):49–56
15. QureshiAI,SuriMFK,GutermanLR,etal.Cocaineuseandthelikelihoodof nonfatalmyocardialinfarctionandstroke:datafromthethirdnationalhealth andnutritionexaminationsurvey.Circulation2001;103(4):502–6
16. ShahM.Hypertrophiccardiomyopathy.CardiolYoung2017;27(S1):S25–30
17. KluesHG,SchiffersA,MaronBJ.Phenotypicspectrumandpatternsofleftventricularhypertrophyinhypertrophiccardiomyopathy:morphologicobservations andsignificanceasassessedbytwo-dimensionalechocardiographyin600patients.JAmCollCardiol1995;26(7):1699–708
18. GeskeJB,OmmenSR,GershBJ.Hypertrophiccardiomyopathy.JACCHeartFail 2018;6(5):364–75
19. CarabelloB,PaulusW.Aorticstenosis.Lancet2009;373:956--66
20. FrankS,JohnsonA,RossJ.Naturalhistoryofvalvularaorticstenosis.Heart 1973;35(1):41–6.
21. AngeliniP.Coronaryarteryanomalies:anentityinsearchofanidentity.Circulation2007;115(10):1296–305
22. MolossiS,SachdevaS.Anomalouscoronaryarteries:whatisknownandwhat stillremainstobelearned?CurrOpinCardiol2020;35(1):42–51
23. TakahashiM.Cardiacischemiainpediatricpatients.PediatrClinNorthAm2010; 57(6):1261–80.
24. PicardF,SayahN,SpagnoliV,etal.Vasospasticangina:Aliteraturereviewofcurrentevidence.ArchCardiovascDis2019;112(1):44–55
25. KobayashiD,AggarwalS,KheiwaA,etal.Myopericarditisinchildren:elevated troponinIleveldoesnotpredictoutcome.PediatrCardiol2012;33(7):1040–5
26. ImazioM,TrincheroR.Myopericarditis:etiology,management,andprognosis.Int JCardiol2008;127(1):17–26.
27. SommerfeldCG,WeinerDJ,NowalkA,etal.Hypersensitivitypneumonitisand acuterespiratorydistresssyndromefromE-cigaretteuse.Pediatrics2018; 141(6):e20163927
28. SiegelDA,JatlaouiTC,KoumansEH,etal.Update:interimguidanceforhealth careprovidersevaluatingandcaringforpatientswithsuspectede-cigarette,or vaping,productuseassociatedlunginjury—UnitedStates,October2019. MMWRMorbMortalWklyRep2019;68(41):9
29.ThakrarPD,BoydKP,SwansonCP,etal.E-cigarette,orvaping,productuseassociatedlunginjuryinadolescents:areviewofimagingfeatures.PediatrRadiol2020. https://doi.org/10.1007/s00247-019-04572-5
30. KalininskiyA,BachCT,NaccaNE,etal.E-cigarette,orvaping,productuseassociatedlunginjury(EVALI):caseseriesanddiagnosticapproach.LancetRespir Med2019;7(12):1017–26
31. LoeysBL,DietzHC,BravermanAC,etal.TherevisedGhentnosologyforthe Marfansyndrome.JMedGenet2010;47(7):476–85
32. DriscollDJ,GlicklichL,GallenW.Chestpaininchildren:AprospectiveStudy.Pediatrics1976;57(5):648–51
33. EpsteinS,GerberL,BorerJ.Chestwallsyndrome:acommoncauseofunexplainedcardiacpain.JAmMedAssoc1979;241(26):2793–7
34. HarrisTH,GossettJG.Diagnosisanddiagnosticmodalitiesinpediatricpatients withelevatedtroponin.PediatrCardiol2016;37(8):1469–74.
35. KadenG,ShenkerR,GootmanN.Chestpaininadolescents.JAdolescHealth 1991;12(3):251–5.
36. MangioneS.Theteachingandpracticeofcardiacauscultationduringinternal medicineandcardiologytraining:anationwidesurvey.AnnInternMed1993; 119(1):47
37. KimuraBJ.Point-of-carecardiacultrasoundtechniquesinthephysicalexamination:betteratthebedside.Heart2017;103(13):987–94
38. PatelSG,BenningerB,MirjaliliSA.Integratingultrasoundintomodernmedical curricula.ClinAnat2017;30(4):452–60
39. DolaraA.Thedeclineofcardiacauscultation:‘theballofthematchpointis poisedonthenet’.JCardiovascMed2008;9(11):1173–4
40. CardimN,FernandezGolfinC,FerreiraD,etal.Usefulnessofanewminiaturized echocardiographicsysteminoutpatientcardiologyconsultationsasanextension ofphysicalexamination.JAmSocEchocardiogr2011;24(2):117–24
41. MehtaM,JacobsonT,PetersD,etal.Handheldultrasoundversusphysicalexaminationinpatientsreferredfortransthoracicechocardiographyforasuspected cardiaccondition.JACCCardiovascImaging2014;7(10):983–90
42. GeggelRL,HorowitzLM,BrownEA,etal.Parentalanxietyassociatedwith referralofachildtoapediatriccardiologistforevaluationofaStill’smurmur. JPediatr2002;140(6):747–52.
43. CampbellRM,DouglasPS,EidemBW,etal.ACC/AAP/AHA/ASE/HRS/SCAI/ SCCT/SCMR/SOPE2014Appropriateusecriteriaforinitialtransthoracicechocardiographyinoutpatientpediatriccardiology.JAmSocEchocardiogr2014; 27(12):1247–66.
44. DanfordDA,NasirA,GumbinerC.Costassessmentoftheevaluationofheart murmursinchildren.Pediatrics1993;91(2):365–8
45. NewburgerJ,RosenthalA,WilliamsR,etal.Noninvasivetestsintheinitialevaluationofheartmurmursinchildren.NEnglJMed1983;308(2):61–4
46. FusterV.Thestethoscope’sprognosis.JAmCollCardiol2016;67(9):1118–9
47. PelechAN.Thephysiologyofcardiacauscultation.PediatrClinNorthAm2004; 51(6):1515–35
48. SmytheJF,TeixeiraOHP,DemersP.Initialevaluationofheartmurmurs:arelaboratorytestsnecessary?Pediatrics1990;86(4):497–500