MÜLLER’S IMAGING OF THE CHEST
1600 John F. Kennedy Blvd.
Ste 1600 Philadelphia, PA 19103-2899
MÜLLER’S IMAGING OF THE CHEST, SECOND EDITION
Copyright © 2019 by Elsevier, Inc. All rights reserved.
ISBN: 978-0-323-46225-9
No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions
This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein).
Notices
Knowledge and best practice in this field are constantly changing. As new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary.
Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. In using such information or methods they should be mindful of their own safety and the safety of others, including parties for whom they have a professional responsibility.
With respect to any drug or pharmaceutical products identified, readers are advised to check the most current information provided (i) on procedures featured or (ii) by the manufacturer of each product to be administered, to verify the recommended dose or formula, the method and duration of administration, and contraindications. It is the responsibility of practitioners, relying on their own experience and knowledge of their patients, to make diagnoses, to determine dosages and the best treatment for each individual patient, and to take all appropriate safety precautions.
To the fullest extent of the law, neither the Publisher nor the authors, contributors, or editors, assume any liability for any injury and/or damage to persons or property as a matter of products liability, negligence or otherwise, or from any use or operation of any methods, products, instructions, or ideas contained in the material herein.
Previous editions copyrighted 2008 by Saunders, an imprint of Elsevier Inc.
Library of Congress Control Number: 2018953443
Publisher: Russell Gabbedy
Senior Content Development Specialist: Ann Ruzycka Anderson
Publishing Services Manager: Catherine Albright Jackson
Senior Project Manager: Claire Kramer
Design Direction: Ryan Cook
To Eunhee, thank you for your constant support and pushing me to take on this project. You truly make me a better man.
To Elsie, thank you for always loving me and making me aware of the things that matter most in life.
To Lillian, thank you for always making me laugh and giving the biggest hugs a dad could ever ask for.
CMW
To my parents, Kyu Youl and Bok Hee: Thank you for endlessly encouraging my curiosity.
To my daughter, Alexandra: Thank you for always being so excited to see me when I come home; it is the only time I have felt like a rock star.
And to my loving wife, Aimee-Sue: Thank you for being the backbone of our family. Your unending support and love always inspire me.
JHC
Bradley S. Sabloff, MD Professor
Department of Diagnostic Radiology
The University of Texas MD Anderson Cancer Center Houston, Texas
Jean M. Seely, MDCM, FCRPC
Associate Professor
University of Ottawa Head of Breast Imaging Section
Department of Medical Imaging
The Ottawa Hospital Clinician Investigator Ottawa Hospital Research Institute Ottawa, Ontario, Canada
Phillip A. Setran, MD
Radiology Resident
Department of Diagnostic Radiology
Oregon Health and Science University Portland, Oregon
Girish S. Shroff, MD
Associate Professor Department of Diagnostic Radiology
The University of Texas MD Anderson Cancer Center Houston, Texas
Justin T. Stowell, MD
Resident Department of Radiology
University of Missouri–Kansas City Kansas City, Missouri
Nicola Sverzellati, MD, PhD Professor of Radiology Department of Medicine and Surgery University of Parma Parma, Italy
Mylene T. Truong, MD Professor
Department of Diagnostic Radiology
The University of Texas MD Anderson Cancer Center Houston, Texas
Emily B. Tsai, MD
Department of Radiology
Stanford University Stanford, California
Chitra Viswanathan, MD Professor
Department of Diagnostic Radiology Division of Diagnostic Imaging
The University of Texas MD Anderson Cancer Center Houston, Texas
Christopher M. Walker, MD
Associate Professor of Radiology
University of Kansas Medical Center Kansas City, Kansas
Charles S. White, MD Professor
Department of Diagnostic Radiology University of Maryland Baltimore, Maryland
Carol C. Wu, MD
Associate Professor Department of Diagnostic Radiology
The University of Texas MD Anderson Cancer Center Houston, Texas
The aim of this second edition of Imaging of the Chest is to provide a succinct, state-of-the art overview of imaging of the thorax. We congratulate Drs. Christopher Walker and Jonathan Chung in achieving this goal by combining their outstanding talents as editors and their ability to obtain the collaboration of an exceptional team of internationally renowned chest radiologists to write chapters in their fields of expertise. The new edition includes a truly up-to-date review of the clinical, radiologic, and pathologic manifestations of lung diseases and several hundred new images that provide excellent illustrations of the latest technologic advances.
The emphasis of this book, similar to daily practice, is on chest radiography and computed tomography (CT). However, as is also required in clinical practice, it includes the indications and characteristic findings on magnetic resonance imaging and, when applicable, scintigraphy, positron emission tomography (PET), integrated PET-CT imaging, and ultrasound. The book also provides a summary of the clinical manifestations and pathologic findings. The clinical history is always helpful and often essential for an accurate diagnosis or appropriate differential
diagnosis, while knowledge of the pathologic findings allows a better understanding of the patterns of abnormalities seen on the radiologic images.
As the editors, we were delighted with the quality of the first edition and very thankful to the numerous authors who were responsible for its success. There have been, however, many major changes and new developments since the publication of that edition in 2008, which led to the need for a major revision and update. We chose to pass on the new edition to a young team of editors with the talent, energy, and dedication required in planning, organizing, and completing this monumental endeavor. We are very pleased to see that they managed to improve the quality of the book and believe that it will be extremely useful to radiology residents, chest radiology fellows, pulmonary physicians, thoracic surgeons, and general radiologists with an interest in chest imaging.
Nestor L. Müller
C. Isabela Silva Müller
30 Acute Interstitial Pneumonia 456
JONATHAN H. CHUNG | CHRISTOPHER M. WALKER
31 Sarcoidosis 461
JONATHAN H. CHUNG | CHRISTOPHER M. WALKER
32 Hypersensitivity Pneumonitis 478
ANDREA L. MAGEE | CHRISTOPHER M. WALKER | JONATHAN H. CHUNG
33 Pulmonary Langerhans Cell Histiocytosis 494
STEPHEN B. HOBBS
34 Smoking-Related Interstitial Lung Disease 502
STEPHEN B. HOBBS
35 Lymphangioleiomyomatosis and Tuberous Sclerosis 513
NICOLA SVERZELLATI
36 Idiopathic Pleuroparenchymal Fibroelastosis 524
ROBERT M. DEWITT | STEPHEN K. FRANKEL
37 Eosinophilic Lung Diseases 527
MELISSA PRICE | CAROL C. WU | MATTHEW D. GILMAN
38 Metabolic and Storage Lung Diseases 535
CHRISTOPHER M. WALKER | JONATHAN H. CHUNG
SECTION 8 Connective Tissue Diseases
39 Rheumatoid Arthritis 552
STEPHEN B. HOBBS
40 Systemic Sclerosis (Scleroderma) 561
BRENT P. LITTLE
41 Systemic Lupus Erythematosus 565
BRENT P. LITTLE
42 Polymyositis/Dermatomyositis 571
STEPHEN B. HOBBS
43 Sjögren Syndrome 576
STEPHEN B. HOBBS
44 Mixed Connective Tissue Disease 581
BRENT P. LITTLE
45 Interstitial Pneumonia With Autoimmune Features 585
MICHAEL A. KADOCH | JUSTIN M. OLDHAM
SECTION 9 Vasculitis and Granulomatosis
46 Antineutrophil Cytoplasmic Antibody–Associated Vasculitis 592
STEPHANE L. DESOUCHES | CHRISTOPHER M. WALKER |
JONATHAN H. CHUNG
47 Goodpasture Syndrome (Anti–Basement Membrane Antibody Disease) 606
JONATHAN H. CHUNG | CHRISTOPHER M. WALKER
48 Behçet Disease 611
JONATHAN H. CHUNG | CHRISTOPHER M. WALKER
49 Takayasu Arteritis 616
CHRISTOPHER M. WALKER | JONATHAN H. CHUNG
SECTION 10 Pulmonary Embolism, Hypertension, and Edema
50 Acute Pulmonary Embolism 622
CAROL C. WU | MATTHEW D. GILMAN
51 Chronic Pulmonary Thromboembolism 633
BRENT P. LITTLE
52 Nonthrombotic Pulmonary Embolism 642
CHRISTOPHER M. WALKER | JONATHAN H. CHUNG
53 Pulmonary Arterial Hypertension 658
VEDANT GUPTA | STEPHEN B. HOBBS
54 Hydrostatic Pulmonary Edema 674
CHRISTOPHER M. WALKER | JONATHAN H. CHUNG
55 Permeability Pulmonary Edema 685
STEPHEN B. HOBBS
SECTION 11 Diseases of the Airways
56 Tracheal Diseases 694
BRENT P. LITTLE
57 Bronchiectasis and Other Bronchial Abnormalities 713
BRENT P. LITTLE
58 Asthma 733
JONATHAN H. CHUNG | CHRISTOPHER M. WALKER
59 Bronchiolitis 745
SHERIEF GARRANA | CHRISTOPHER M. WALKER | JONATHAN H. CHUNG
60 Emphysema 765
STEPHEN B. HOBBS
SECTION 12 Inhalational Diseases and Aspiration
61 Asbestos-Related Disease 775
STEPHEN B. HOBBS
62 Silicosis and Coal Workers’ Pneumoconiosis 793
STEPHEN B. HOBBS
63 Uncommon Pneumoconioses 809
STEPHEN B. HOBBS
64 Aspiration 822
TOMÁS FRANQUET
SECTION 13 Iatrogenic Lung Disease and Trauma
65 Drug-Induced Lung Disease 836
SARAH T. KURIAN | CHRISTOPHER M. WALKER | JONATHAN H. CHUNG
MÜLLER’S IMAGING OF THE CHEST
Fig. 1.2 Properly centered chest radiograph. A view from a frontal radiograph shows that the medial ends of the right and left clavicles (highlighted in black) are equidistant to the spinous process (arrow) of the vertebra at the same level, thus indicating that the radiograph is properly centered.
radiation, the intensity of which corresponds to the absorbed x-ray energy. The resultant luminescence is measured and recorded digitally.6
Digital Radiography
DR uses a flat-panel x-ray detector or an array of detectors to directly capture the radiographic image numerically, thus
eliminating the step of reading out the detector. The detectors in DR are selenium based and provide the additional advantage of having considerably greater quantum efficiency than conventional screen-film systems and photostimulable phosphor detectors do,7,8 which results in an image quality superior to that of screen-film systems and existing storage phosphor detectors at a comparable or lower radiation dose.9
Normal Anatomy of the Chest
AIRWAYS
Trachea and Bronchi
The trachea is a midline structure, and the tracheal walls are parallel except on the left side just above the bifurcation, where the aorta commonly causes a smooth indentation (Fig. 1.3). The trachea measures 10 to 12 cm in length and has 16 to 20 C-shaped cartilage rings on its lateral and anterior aspects and a fibromuscular posterior margin. Calcification of the cartilage rings is a common normal finding in patients older than 40 years, particularly women, but it is seldom evident on radiographs (Fig. 1.4). The upper limits of normal for coronal and sagittal
Fig. 1.1 Normal chest radiograph. (A) Posteroanterior projection. (B) Lateral projection.
Fig. 1.5 Anterior segmental bronchus of the right upper lobe seen end-on. A view from a frontal radiograph shows a ring shadow (curved arrow) corresponding to the anterior segmental bronchus of the right upper lobe seen end-on and the adjacent anterior segmental pulmonary artery (straight arrow). The outer diameter of the bronchus on the upright chest radiograph is slightly larger than that of the adjacent artery.

Fig. 1.6 Normal anatomy of the central pulmonary arteries. (A) A maximum-intensity projection image obtained from a CT scan demonstrates that the main pulmonary artery (MPA) courses posteriorly and branches into the right (RPA) and left (LPA) pulmonary arteries. The right pulmonary artery branches shortly after its origin into the truncus anterior, which courses cephalad to supply most of the right upper lobe, and a larger right interlobar pulmonary artery (RI), which courses just anterior and then lateral to the bronchus intermedius (BI). (B) Coronal image from a CT scan demonstrating the orientation of the RPA and LPA in the same projection as the frontal radiograph. The right pulmonary artery and the central portion of the left pulmonary artery are in the mediastinum and therefore cannot be identified on the chest radiograph. The right pulmonary artery branches into the truncus anterior (TA) and RI. (C) Sagittal image demonstrating the orientation of the right and left pulmonary arteries that corresponds to the lateral chest radiograph. The MPA originates from the right ventricle (RV) and courses cephalad and posteriorly. AA, Aortic arch; asterisk, aortopulmonary window.

1.7
right interlobar artery visualized on a frontal chest radiograph. The upper limit of normal of the transverse diameter of the interlobar artery measured from its lateral aspect to the air column of the bronchus intermedius (black bar) is 16 mm in men and 15 mm in women.
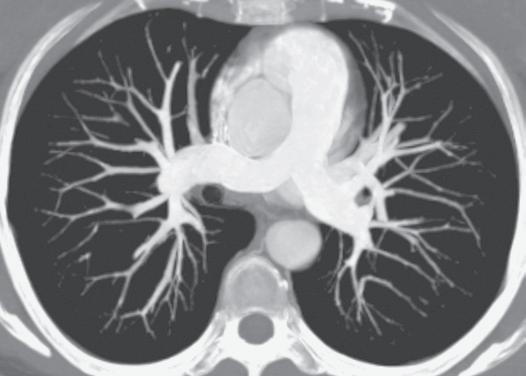
Measurements of pulmonary arterial diameter can be helpful in the assessment of pulmonary vascular disease, although in conventional radiography, it is limited to the measurement of the right interlobar artery. The upper limit of normal of the transverse diameter of the right interlobar artery (measured from its lateral aspect to the air column of the bronchus intermedius) is 16 mm in men and 15 mm in women (Fig. 1.7).12 Dilation of the interlobar pulmonary artery may result from increased pressure (e.g., pulmonary arterial hypertension), increased flow (e.g., left-to-right shunts), or aneurysm formation (e.g., Behçet disease) (Fig. 1.8).
KEY POINTS: PULMONARY ARTERIES
• The pulmonary trunk or main pulmonary artery is not normally visualized on radiography in adults.
• Normal diameter of the right interlobar pulmonary artery is <16 mm.
Pulmonary Veins
The pulmonary veins arise from venules that drain the alveolar capillaries and the capillary network of the pleura. In contrast to the pulmonary arteries, they are not associated with the airways. Although their final course is variable, there are usually two main superior and two main inferior vessels, the former draining the middle and upper lobes on the right and the upper lobe on the left and the latter draining the lower lobes (Fig. 1.9).
PULMONARY HILA
The anatomic structures rendering the hila visible on radiographs are primarily the pulmonary arteries and veins, with lesser
contributions from the bronchial walls, surrounding connective tissue, and lymph nodes (Fig. 1.10).
On a PA radiograph the main shadow of the right hilum is formed by the vertically oriented interlobar artery. Right hilar structures immediately cephalad to the interlobar artery include the ascending pulmonary artery (truncus anterior) and superior pulmonary vein (Fig. 1.11). The end-on opacity and radiolucency of the contiguous anterior (and occasionally posterior) segmental artery and bronchus can be identified in approximately 80% of normal individuals (see Fig. 1.5).13
On the left the upper hilar opacity is formed by the distal left pulmonary artery, the proximal portion of the left interlobar
Fig.
Normal
Fig. 1.8 Enlarged central pulmonary arteries from severe pulmonary arterial hypertension. A frontal radiograph shows markedly enlarged central pulmonary arteries.
Fig. 1.9 Inferior pulmonary veins. A maximum-intensity projection image obtained from a CT scan shows two main right and left inferior pulmonary veins as they drain into the left atrium (LA). AA, Ascending aorta; DA, descending aorta; RA, right atrium.
Fig. 1.10 Normal hila. A view from a frontal radiograph shows that the main shadow of the right hilum is formed by the vertically oriented interlobar artery (arrowhead) and that of the left hilum by the distal left pulmonary artery (right arrow) and descending left pulmonary artery. Because the left pulmonary artery arches above the left main and left upper lobe bronchi, the left hilum is normally 1–2 cm higher than the right hilum.
artery and its segmental arterial branches, and the left superior pulmonary vein and its major tributaries. Because the left pulmonary artery arches over the left main and left upper lobe bronchi, the left hilum is typically 1 to 2 cm higher than the highest point of the right hilum (right interlobar artery) (see Fig. 1.10).
Surrounding the hilar vessels and bronchi are small amounts of fat and small lymph nodes, which cannot normally be distinguished from other structures on the radiograph. Enlargement of the hilar lymph nodes leads to increased size and opacity of the hilum, a lobulated contour, and obscuration of the interlobar artery. Hilar fullness from lymphadenopathy can be differentiated from hilar fullness from pulmonary arterial enlargement by carefully examining the adjacent hilar vessels. In lymphadenopathy the vessels will be visible through the region of hilar fullness (Fig. 1.12), whereas the vessels will converge on the margins of the hilar fullness in the setting of pulmonary arterial enlargement (see Fig. 1.8). This finding is known as the hilar convergence sign (see Fig. 1.12).
The radiographic anatomy of the hila on a lateral projection is complex because the right and left hilar components are to a large degree superimposed (Fig. 1.13).14,15 The trachea is usually well seen down to the level of the carina, where the air column can be seen to taper. At the level of the carina the left pulmonary artery can be seen as a curved structure as it courses above the left main bronchus and continues as the descending left pulmonary artery; consequently, the left upper lobe bronchus is seen in about 75%15 because it is completely surrounded by vessels (the left pulmonary artery above, the descending artery behind, and the mediastinal component of the left superior pulmonary

Fig. 1.11 Normal hilar anatomy. A coronal image from a CT scan demonstrates the hilar anatomy as seen on a radiograph. The right pulmonary artery (RPA) is in the mediastinum and therefore not visible on the frontal radiograph. On a frontal radiograph the main shadow of the right hilum is formed by the vertically oriented interlobar artery (RI). Right hilar structures immediately cephalad to the interlobar artery include the ascending pulmonary artery (truncus anterior) (curved arrow) and the right superior pulmonary vein (straight arrow). Most of the left hilum is formed by the distal left pulmonary artery (LPA) and left descending pulmonary artery. LA, Left atrium.