Morrey’s The Elbow and Its Disorders
FIFTH EDITION
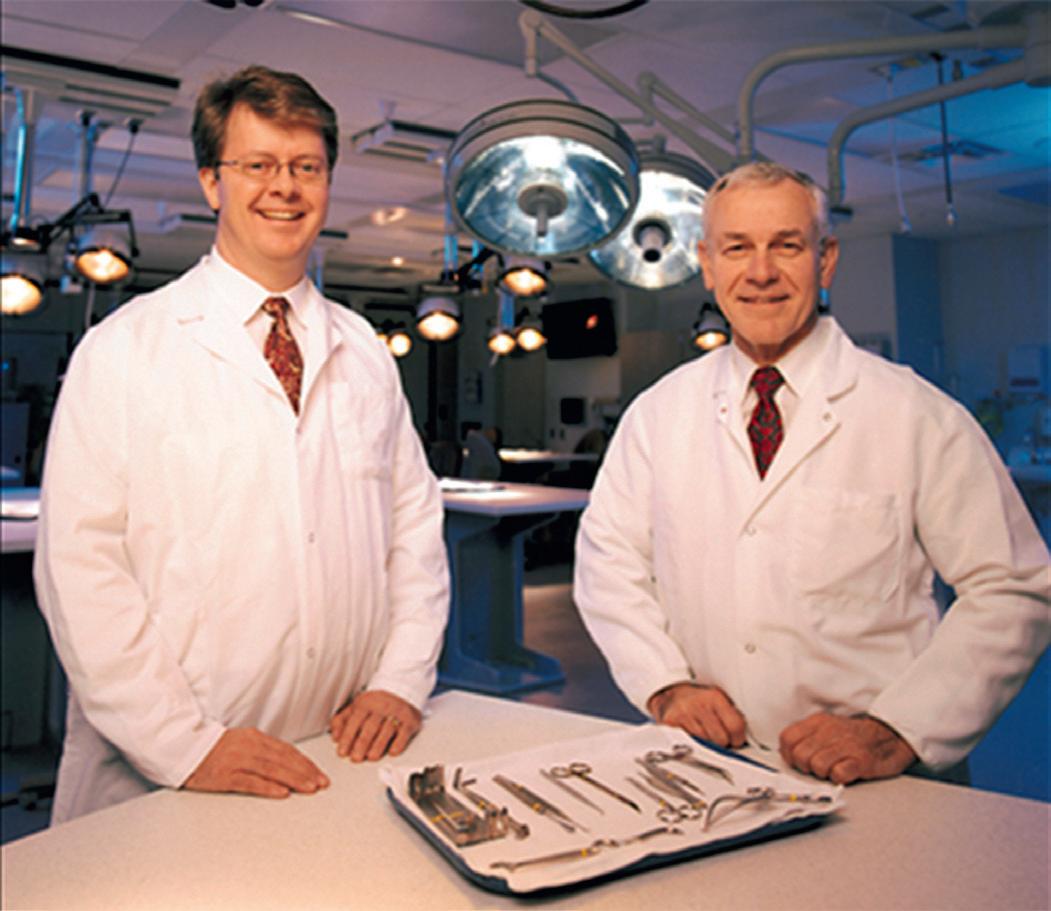
Bernard F. Morrey, MD
Professor
Department of Orthopedic Surgery
Mayo Clinic Rochester, Minnesota; Professor of Orthopedics
University of Texas Health Science Center San Antonio, Texas
Joaquin Sanchez-Sotelo, MD, PhD
Professor
Department of Orthopedic Surgery
Mayo Clinic College of Medicine
Consultant
Division of Adult Reconstruction
Department of Orthopedic Surgery
Mayo Clinic Rochester, Minnesota
Mark E. Morrey, MD, MSc
Assistant Professor of Orthopedics
Department of Orthopedic Surgery
Mayo Clinic Rochester, Minnesota
Anatomic dissections: Manuel Llusá-Pérez, MD, PhD, and José R. Ballesteros-Betancourt, MD
1600 John F. Kennedy Blvd.
Ste 1800 Philadelphia, PA 19103-2899
MORREY’S THE ELBOW AND ITS DISORDERS, FIFTH EDITION
ISBN: 978-0-323-34169-1
Copyright © 2018 Mayo Foundation for Medical Education and Research. Published by Elsevier Inc. All rights reserved.
No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Details on how to seek permission, further information about the Publisher’s permissions policies and our arrangements with organizations such as the Copyright Clearance Center and the Copyright Licensing Agency, can be found at our website: www.elsevier.com/permissions
This book and the individual contributions contained in it are protected under copyright by the Publisher (other than as may be noted herein).
Notices
Knowledge and best practice in this field are constantly changing. As new research and experience broaden our understanding, changes in research methods, professional practices, or medical treatment may become necessary.
Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds, or experiments described herein. In using such information or methods they should be mindful of their own safety and the safety of others, including parties for whom they have a professional responsibility.
With respect to any drug or pharmaceutical products identified, readers are advised to check the most current information provided (i) on procedures featured or (ii) by the manufacturer of each product to be administered, to verify the recommended dose or formula, the method and duration of administration, and contraindications. It is the responsibility of practitioners, relying on their own experience and knowledge of their patients, to make diagnoses, to determine dosages and the best treatment for each individual patient, and to take all appropriate safety precautions.
To the fullest extent of the law, neither the Publisher nor the authors, contributors, or editors, assume any liability for any injury and/or damage to persons or property as a matter of products liability, negligence or otherwise, or from any use or operation of any methods, products, instructions, or ideas contained in the material herein.
Previous editions copyrighted 2009, 2000, 1993, 1985 by The Mayo Clinic Foundation.
Library of Congress Cataloging-in-Publication Data
Names: Morrey, Bernard F., 1943- editor. | Sanchez-Sotelo, Joaquin, editor. | Morrey, Mark E., editor. Title: Morrey’s the elbow and its disorders / [edited by] Bernard F. Morrey, Joaquin Sanchez-Sotelo, Mark E. Morrey.
Other titles: Elbow and its disorders.
Description: Fifth edition. | Philadelphia, PA : Elsevier, [2018] | Preceded by Elbow and its disorders / [edited by] Bernard F. Morrey, Joaquin Sanchez-Sotelo. 4th ed. c2009. | Includes bibliographical references and index.
Identifiers: LCCN 2017013655 | ISBN 9780323341691 (hardcover : alk. paper)
Subjects: | MESH: Elbow Joint | Elbow Joint—injuries | Joint Diseases
Classification: LCC RD686 | NLM WE 820 | DDC 617.472044—dc23 LC record available at https://lccn.loc .gov/2017013655
Senior Content Strategist: Kristine Jones
Senior Content Development Specialist: Ann Ruzycka Anderson
Publishing Services Manager: Catherine Jackson
Book Production Specialist: Kristine Feeherty
Design Direction: Bridget Hoette
Akin Cil, MD
Franklin D. Dickson Associate Professor of Orthopaedics
University of Missouri-Kansas City
Truman Medical Centers
Kansas City, Missouri
John E. Conway, MD
Team Orthopedic Consultant
Texas Christian University and University of Texas at Arlington Medical Director
Texas Health Ben Hogan Sports Medicine
Orthopedic Specialty Associates
Texas Health Physicians Group Fort Worth, Texas
Roger Cornwall, MD
Associate Professor
Department of Orthopaedic Surgery and Department of Developmental Biology
Cincinnati Children’s Hospital Medical Center
Cincinnati, Ohio
Omkar H. Dave, MD
Omkar Dave MD PLLC
Orthopedic Surgery, Sports Medicine, and Arthroscopy
Houston, Texas
Joshua S. Dines, MD
Sports Medicine and Shoulder Service Hospital for Special Surgery
New York, New York
Karan Dua, MD
Research Fellow
Department of Orthopaedics University of Maryland Baltimore, Maryland
Thomas R. Duquin, MD
Assistant Professor
Department of Orthopaedics University at Buffalo Buffalo, New York
Anil K. Dutta, MD
Associate Professor
Orthopedic Surgery
University of Texas Health Science Center at San Antonio
San Antonio, Texas
Eric W. Edmonds, MD
Associate Professor of Orthopaedic Surgery
University of California San Diego; Director, 360 Sports Medicine
Rady Children’s Hospital San Diego San Diego, California
Neal S. ElAttrache, MD
Associate Clinical Professor Department of Orthopaedics
Keck School of Medicine
University of Southern California; Director, Sports Medicine Fellowship, Kerlan-Jobe Orthopaedic Clinic Los Angeles, California
Bassem T. Elhassan, MD
Mayo Clinic Rochester, Minnesota
Larry D. Field, MD
Orthopaedic Physician
Mississippi Sports Medicine and Orthopaedic Center Jackson, Mississippi
Antonio M. Foruria, MD, PhD
Shoulder and Elbow Reconstructive Surgery Unit
Head, Orthopedic Surgery Department
Fundación Jiménez Díaz University Hospital Associate Professor of Orthopedics
Surgery Department
Autonoma University Madrid, Spain
Hillary W. Garner, MD
Assistant Professor
Department of Radiology
Mayo Clinic
Jacksonville, Florida
Robert U. Hartzler, MD, MS
Assistant Clinical Professor
University of the Incarnate Word School of Osteopathic Medicine
Shoulder and Elbow Surgeon
The San Antonio Orthopaedic Group
San Antonio, Texas
John W. Hinchey, MD
Assistant Chief of Orthopaedic Surgery
Shoulder & Elbow Fellowship, VA Site Director
South Texas Veterans’ Health Care System; Adjunct Associate Professor, Orthopaedic Surgery
University of Texas Health Science Center at San Antonio
San Antonio, Texas
E. Rhett Hobgood, MD
Mississippi Sports Medicine and Orthopaedic Center Jackson, Mississippi
Justin L. Hodgins, MD
Orthopaedic Surgeon
Rouge Valley Health System
Toronto, Ontario, Canada
Terese T. Horlocker, MD
Professor of Anesthesiology and Orthopaedics
Department of Anesthesiology
Mayo Clinic Rochester, Minnesota
Jeffery S. Hughes, MBBS, FRACS
Orthopaedic Consultant
North Shore Private Hospital
Sydney, Australia
Carrie Y. Inwards, MD
Professor of Pathology
Department of Laboratory Medicine
Division of Anatomic Pathology
Mayo Clinic College of Medicine Rochester, Minnesota
In-Ho Jeon, MD, PhD
Professor
Department of Orthopaedic Surgery
Asan Medical Centre, School of Medicine, University of Ulsan
Seoul, South Korea
Srinath Kamineni, MD, FRCS-Orth Professor of Bioengineering
Brunel University School of Engineering and Design;
Consultant Elbow, Shoulder, Upper Limb Surgeon, and Clinical Lead Upper Limb Unit
Cromwell Hospital
London, United Kingdom
Graham J.W. King, MD, MSc, FRCSC Professor
Department of Surgery
Western University; Director
St. Joseph’s Health Centre
Roth McFarlane Hand and Upper Limb Centre
London, Ontario, Canada
Jeffrey C. King, MD
Clinical Associate Professor
Western Michigan University
Homer Stryker MD School of Medicine
Kalamazoo, Michigan
Rick Papandrea, MD
Partner
Orthopedic Associates of Wisconsin Pewaukee, Wisconsin; Assistant Clinical Professor Orthopaedic Surgery
Medical College of Wisconsin Milwaukee, Wisconsin
Hamlet A. Peterson, MD, MS
Emeritus Professor of Orthopedic Surgery
Mayo Medical School; Emeritus Consultant in Orthopedic Surgery
Emeritus Chair Pediatric Orthopedics
Mayo Clinic Rochester, Minnesota
Samantha Lee Piper, MD
Orthopedic Hand and Upper Extremity Surgery
Southern California Permanente Medical Group San Diego, California
Adam M. Pourcho, DO
Instructor of Sports Medicine
Physical Medicine and Rehabilitation Swedish Medical Group Seattle, Washington
Matthew L. Ramsey, MD
Professor Orthopaedic Surgery
Thomas Jefferson University and Rothman Institute Philadelphia, Pennsylvania
Nicholas G. Rhodes, MD
Senior Associate Consultant Department of Radiology
Mayo Clinic Rochester, Minnesota
David Ring, MD, PhD
Associate Dean for Comprehensive Care
Professor of Surgery and Perioperative Care
The University of Texas at Austin–Dell Medical School
Austin, Texas
Joaquin Sanchez-Sotelo, MD, PhD Professor
Department of Orthopedic Surgery
Mayo Clinic College of Medicine Consultant
Division of Adult Reconstruction
Department of Orthopedic Surgery
Mayo Clinic Rochester, Minnesota
Felix H. “Buddy” Savoie III, MD
Ray J. Haddad Professor and Chair of Orthopaedic Surgery
Tulane University School of Medicine
New Orleans, Louisiana
Olga D. Savvidou, MD
Associate Professor
First Department of Orthopaedics
Athens University Medical School
Attikon University General Hospital Athens, Greece
Erin M. Scanlon, MD
Rheumatology
Mayo Clinic Rochester, Minnesota
Alberto G. Schneeberger, MD Consultant
Privatdozent at University of Zurich Endoclinic Zurich, Klinik Hirslanden Zurich, Switzerland
Benjamin W. Sears, MD
Orthopaedic Surgeon Western Orthopaedics Denver, Colorado
Adam J. Seidl, MD
Assistant Professor Orthopedic Surgery University of Colorado Aurora, Colorado
William J. Shaughnessy, MS, MD
Pediatric Orthopedics and Scoliosis Surgery Department of Orthopedic Surgery
Mayo Clinic Rochester, Minnesota
Alexander Y. Shin, MD Professor of Orthopedic and Neurologic Surgery
Mayo Clinic College of Medicine
Consultant, Division of Hand Surgery Department of Orthopedic Surgery
Mayo Clinic Rochester, Minnesota
Thomas C. Shives, MD Professor
Department of Orthopedic Surgery
Mayo Clinic Rochester, Minnesota
Juan P. Simone, MD
Shoulder and Elbow Surgeon Orthopedic Surgery
Hospital Alemán
Buenos Aires, Argentina
Jarrod R. Smith, MD President
Smith Orthopedics & Sports Medicine, PSC
Ashland, Kentucky
Jay Smith, MD
Professor of Physical Medicine & Rehabilitation
Departments of Physical Medicine and Rehabilitation
Radiology and Anatomy
Mayo Clinic College of Medicine Rochester, Minnesota
Jeremy S. Somerson, MD
Assistant Professor
Department of Orthopaedic Surgery and Rehabilitation
University of Texas Medical Branch
Galveston, Texas
Robert J. Spinner, MD
Chairman
Department of Neurologic Surgery
Burton M. Onofrio Professor of Neurosurgery
Professor of Orthopedics and Anatomy
Mayo Clinic School of Medicine Rochester, Minnesota
Anthony A. Stans, MD
Chair, Division of Pediatric Orthopedics Department of Orthopedic Surgery
Mayo Clinic Rochester, Minnesota
Scott P. Steinmann, MD
Professor of Orthopedic Surgery
Mayo Clinic and Mayo Clinic Health System
Rochester, Minnesota Austin, Minnesota
Matthew T. Stepanovich, MD Clinical Fellow
Pediatric Orthopaedic and Scoliosis Fellowship
Rady Children’s Hospital San Diego San Diego, California
Philipp N. Streubel, MD
Assistant Professor
Orthopaedic Surgery
University of Nebraska Medical Center Omaha, Nebraska
Jo Suenghwan, MD, PhD
Assistant Professor Department of Orthopaedics
Chosun University Gwangju, South Korea
VIDEO CONTENTS
PART I Fundamentals and General Considerations
4 History and Physical Examination of the Elbow
4-1 Ulnar Nerve Subluxation
4-2 Resisted Terminal Extension
4-3 Arm Bar Examination
4-4 Localizing the Interval Between the Brachial Radialis and Extensor Carpi Radialis Longus for Palpation of the Posterior Interosseous Nerve
4-5 Percussion of the Lateral Antebrachial Cutaneous Nerve
4-6 Posterior Plica Examination
4-7 Tennis Elbow Shear Test
4-8 Range of Motion Examination
4-9 Radiocapitellar Load Test
4-10 Posterior Lateral Rotatory Drawer Test
4-11 Elbow Examination Under Anesthesia With Fluoroscopy
4-12 Moving Valgus Stress Test
4-13 Gravity-Assisted Varus Posterior Medial Rotatory Instability Grind Test
PART II Elbow Arthroscopy
20 Arthroscopic Management of Elbow Plica and Loose Bodies
20-1 Elbow Plicae and Loose Bodies
22 Arthroscopic Management of Osteochondritis
Dissecans of the Capitellum
22-1 Microfracture of Contained Osteochondritis Dissecans Lesion
PART III The Child and Adolescent Elbow
33 Osteochondritis Dissecans
33-1 Treatment of Osteochondritis Desiccans Elbow Lesions
33-2 Osteochondral Allograft Transfer for Osteochondritis Dissecans
PART IV Acute Trauma
39 Prosthetic Radial Head Replacement
39-1 rHead LATERAL Implant
39-2 rHead RECON Bipolar Replacement
39-3 rHead Extended Stem Replacement
43 Coronoid Fractures
43-1 Lateral Approach to the Elbow for Radial Head Fixation or Replacement and Coronoid Fixation
45 Distal Humerus Fractures: Fractures of the Columns With Articular Involvement
45-1 Open Reduction and Internal Fixation for Distal Humerus Fractures
48 Hinged External Fixators of the Elbow
48-1 Application of the Dynamic Joint Distractor
PART V Complications of Trauma and Elbow Stiffness
49 Persistent Elbow Instability
49-1 Reconstructive Options for Persistent Elbow Instability
49-2 Allograft Reconstruction of the Coronoid
50 Nonunion and Malunion of Distal Humerus Fractures
50-1 Open Reduction and Internal Fixation for Distal Humerus Nonunion
54 Extrinsic Contracture: Lateral and Medial Column Procedures
54-1 Open Contracture Release: Medial and Lateral Column
55 Elbow Stiffness: Arthroscopic Contracture Release
55-1 Arthroscopic Osteocapsular Arthroplasty for Primary Osteoarthritis
PART VI Sports and Soft Tissue Injuries
60 Percutaneous Ultrasound Tenotomy Treatment of Epicondylitis
60-1 Percutaneous Ultrasonic Tenotomy
63 Elbow Tendinopathies: Acute Distal Biceps Tendon Ruptures
63-1 Mayo Two-Incision Biceps Tendon Repair
67 Articular Injuries in the Athlete
67-1 Capitellar Osteochondritis Dissecans Lesion Treated With Microfracture
PART VIII Joint Replacement Arthroplasty
87 Radiocapitellar Prosthetic Arthroplasty for Isolated Radiocapitellar Arthritis
87-1 UNI_Elbow Radio-Capitellum Replacement
90 Linked Elbow Arthroplasty: Rationale, Design Concept, and Surgical Technique
90-1 Coonrad-Morrey Total Elbow Arthroplasty
90-2 Highlights of the Zimmer Nexel Total Elbow Surgical Procedure
92 Distal Humeral Fractures
92-1 Total Elbow Arthroplasty for Distal Humerus Fractures
93 Total Elbow Arthroplasty for Distal Humerus Nonunion
93-1 Total Elbow Arthroplasty for Distal Humerus Nonunions
PART IX Complications and Salvage of Failed Arthroplasty
104 Isolated Polyethylene Wear and Elbow Replacement 104-1 Fluoroscopic Examination for Bushing Wear
108 Revision of Failed Total Elbow Arthroplasty With Osseous Deficiency: Impaction Grafting 108-1 Revision Techniques for Total Elbow Arthroplasty
109 Revision of Failed Total Elbow Arthroplasty With Osseous Deficiency: Humeral Replacement and Allograft Prosthetic Composite Reconstruction 109-1 Allograft Prosthetic Composite Reconstruction
PART X Nonprosthetic Alternatives and Salvage Procedures
110 Synovectomy of the Elbow 110-1 Arthroscopic Synovectomy of the Elbow
113 Anconeus Interposition Arthroplasty 113-1 Anconeus Interposition Arthroplasty
114 Interposition Arthroplasty of the Elbow 114-1 Interposition Arthroplasty With Achilles Tendon Allograft and the Application of the Dynamic Joint Distractor
PHYLOGENY
Hominoid primate (chimpanzee)
Graviportal mammal (elephant)
Cursorial mammal (gazelle)
Partly terrestrial mammal (bear)
Generalized mammal (tree shrew)
Prototherian
Cretaceous ~100 mya
Jurassic mammal ~155 mya
Late Triassic mammal ~215 mya
Cynodont Early Triassic ~250 mya
Pelycosaur Late Paleozoic ~300 mya
FIG 1.1 The major evolutionary stages in the development of the elbow joint from pelycosaurs to advanced mammals. The distal ends of the humeri are shown on the left, and the corresponding radius and ulna are on the right. The form of the pelycosaur elbow was designed to maximize stability. Subsequent evolutionary stages show accommodations to increasing mobility. (Adapted from Jenkins FA Jr: The functional anatomy and evolution of the mammalian humeroulnar articulation, Am J Anat 137:281, 1973.)
olecranon fossa, providing resistance to varus and internal rotation in extension.20,21
The trochlear notch of the ulna generally mirrors the shape of the humeral trochlea. In humans and apes, the notch has medial and lateral surfaces separated by a ridge that ar ticulates w ith the trochlear groove (Fig. 1.3).20,21
The differences seen in the configuration of the humeroulnar joint across primate species reflect contrasting requirements for stabilization w ith different forms of limb use. In most monkeys, the humeroulnar joint is in its most stable configuration in a par tially flexed position owing to the development of the medial trochlear keel anterodistally and the lateral keel posteriorly.20
It is not surprising that this position of maximum stability is the one assumed by the forelimb during the weight-bearing phase of quadrupedal locomotion. The anterior orientation of the trochlear notch is a direct adaptation to weight bearing w ith a par tially flexed limb. However, such an orientation does limit elbow extension to some degree.
The great apes (chimpanzees, gorillas, and orangutans) and the lesser apes (gibbons) move about in a much less stereotypical fashion than do monkeys. To accommodate this more varied form of limb use, the hominoid humeroulnar joint, w ith its deeply socketed ar ticular surfaces and well-developed medial and lateral trochlear ridges all around the joint margins, is designed to provide maximum stability throughout the flexion-extension range.20–22 The use of overhead suspensory postures and locomotion in apes has led to the evolution of the capacity for complete elbow extension. Apes even keep their elbows extended during quadrupedal locomotion. The ideal joint configuration for resistance of transarticular stress w ith fully extended elbows during quadrupedal postures would be to have a trochlear notch that was proximally directed. It could then act as a cradle to support the humerus during locomotion. However, a proximal orientation of the trochlear notch would severely limit elbow flexion by impingement of the coronoid process w ithin its fossa. The anteroproximal orientation of the trochlear notch in apes thus represents a compromise that safely supports the humerus on the ulna in
1.7 Frontal view of an arm-swinging gibbon showing the skeletal structure of the forelimb. The carrying angle of the elbow brings the center of mass (i.e., center of gravity [cg]) more nearly directly under the supporting hand. (Adapted from Sarmiento EE: Functional Differences in the Skeleton of Wild and Captive Orang-Utans and Their Adaptive Significance Ph.D. Thesis, New York University, 1985.)
epicondyle and a less well-developed supracondylar crest than is seen in the apes, reflecting diminished leverage of the w rist extensors and brachioradialis.23–25 Humans have no bowing of the ulna that is related to enhancing the leverage of the forearm pronators and supinators in apes.1 Finally, a diminution in the prominence of the trochlear ridges and steep lateral margin of the olecranon fossa in humans can be related to the overall reduction in stresses at the human elbow and the concomitant relaxation on the demands for strong stabilization in all positions.20,21
When exactly did the basic pattern for the hominoid elbow arise, and how old is the morphology of the modern human elbow? For answers to these questions we must turn to the fossil record.
FOSSIL EVIDENCE
Dendropithecus macinnesi, Limnopithecus legetet, and Proconsul heseloni (all from Africa) are among the earliest known hominoid species dated to the early par t of the Miocene epoch (23 to 16 mya) for which postcranial material is known. Overall, the distal humeri of the first two of these forms resemble generalized New World monkeys such as Cebus (capuchin monkeys). The trochlea does not display a prominent lateral ridge, and the zona conoidea is relatively flat. The trochlear notch faces anteriorly, and the head of the radius is oval in outline w ith a well-developed lateral lip These features generally are considered to be primitive for higher primates (monkeys, apes, and humans).8,9,20
P. heseloni, on the other hand, does display some features characteristic of extant hominoids. It has a globular capitellum, well-developed medial and lateral trochlear ridges, and a deep zona conoidea forming the medial wall of a recessed gutter between the capitellum and trochlea.20 In general, the elbow region of Proconsul resembles that of extant hominoids in features related to general stability and range of pronosupination, yet full pronation remains a position of par ticular stability.20
of mass of the body during the single limb support phase of walking (Fig. 1.7).
All of these features have been retained in humans because of their continued advantages for tool use and other behaviors. Powerful flexion is clearly important. The continued importance of the carrying angle is perhaps less obvious, but one advantage that it does offer is that flexion of the elbow is accompanied by adduction of the forearm, thus bringing the hands more in front of the body, where most manipulatory activities are undertaken.
The morphology of the modern human elbow is not identical to that of the ape elbow, however. In some cases, the differences are simply a matter of degree. For example, although both apes and humans are distinguished from other primates in the medial orientation of the radial tuberosity, it is more extreme in position in the ape; in the human it is typically slightly anterior to true medial. In addition, although the olecranon is short in both humans and apes compared w ith most monkeys, it is slightly longer in humans than in apes and also shaped to maintain this length throughout the range of flexion—both of which are advantageous for powerful manipulatory activities.6
Other differences between the elbow morphology of humans and that of apes can be related to the fact that the human forelimb has no role in locomotion. These differences include a less robust coronoid process and a relatively narrower, proximally oriented trochlear notch in humans, indicating relative stability in flexion rather than the need to support the weight of the body during quadrupedal locomotion in extension.1,13 Humans possess a smaller and more distally placed lateral
The limited fossil material that is available from the late Miocene epoch (16 to 5 mya) suggests that many hominoid species, including members of the genera Dryopithecus (from Europe), Sivapithecus (from Europe and Asia), and Oreopithecus (from Europe), displayed the features characteristic of the modern hominoid elbow. Although it is possible that these features arose in parallel in different genera, the more parsimonious explanation is that they inherited this morphology from an early to middle Miocene common ancestor, possibly similar to P. heseloni 16,29,31 Assuming that the characteristic features of the hominoid elbow are shared derived traits—that is, traits inherited from a single common ancestor—we can say that the elbow morphology of modern apes and humans can be dated to roughly 15 to 20 mya.
The majority of paleoanthropologists agree that humans are most closely related to the African apes (chimpanzees and gorillas) and that the two lineages arose in the late Miocene or earliest Pliocene period (between 10 and 4 mya).8 The earliest known fossils of the human lineage (hominids) date from the early Pliocene era, approximately 4 to 5 mya. There are three genera of these earliest hominids currently recognized, Ardipithecus, Paranthropus, and Australopithecus. The latter is the best known and most w idespread genus, and includes the famous “Lucy” skeleton from Hadar, Ethiopia (Australopithecus afarensis).7,12 The genus Homo, to which our own species belongs, first appeared about 2.5 to 2 mya in East Africa w ith its earliest member species, Homo habilis
All of the hominids from the Pliocene period were bipedal, although some probably spent significant time climbing trees.23–26,28 The development of bipedalism freed the upper extremity from the requirements of locomotion, placing greater emphasis on increasing mobility. The ability to supinate and pronate was an immense advantage to hominids
FIG
Anatomy of the Elbow Joint
Bernard F. Morrey, Manuel Llusá-Pérez, and José R. Ballesteros-Betancourt
This chapter discusses the normal anatomy of the elbow region. Abnormal and surgical anatomy is addressed in subsequent chapters of this book dealing w ith the pertinent condition.
TOPICAL ANATOMY AND GENERAL SURVEY
The contours of the biceps muscle and antecubital fossa are easily observed anteriorly. Laterally, the avascular interval between the brachioradialis and the triceps, the so-called column, is an important palpable landmark for surgical exposures (Fig 2.1). Laterally, the tip of the olecranon, the lateral epicondyle, and the radial head also form an equilateral triangle and provide an important landmark for joint aspiration and elbow ar throscopy (see Chapters 39 and 80). The flexion crease of the elbow is in line w ith the medial and lateral epicondyles and thus actually reflects the joint axis and is 1 to 2 cm proximal to the joint line when the elbow is extended (Fig. 2.2). The inverted triangular depression on the anterior aspect of the extremity distal to the epicondyles is called the cubital (or antecubital) fossa.
The superficial cephalic and basilic veins are the most prominent superficial major contributions of the anterior venous system and communicate by way of the median cephalic and median basilic veins to form an “M” pattern over the cubital fossa (Fig 2.3).2
The extensor forearm musculature originates from the lateral epicondyle and was termed the mobile wad by Henry.37 This forms the lateral margin of the antecubital fossa and the lateral contour of the forearm and comprises the brachioradialis and the extensor carpi radialis longus and brevis muscles. The muscles comprising the contour of the medial anterior forearm include the pronator teres, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris. Henry has demonstrated that their relationship and location can be approximated by placing the opposing thumb and the index, long, and ring fingers over the anterior medial forearm. The dorsum of the forearm is contoured by the lateral extensor musculature, consisting of the anconeus, extensor carpi ulnaris, extensor digitorum quinti, and extensor digitorum communis.
Dermal innervation about the proximal elbow is quite variable, being provided by the lower lateral cutaneous (C5, C6) and medial cutaneous (radial nerve, C8, T1, and T2) nerves of the arm. The forearm skin is innervated by the medial (C8, T1), lateral (musculocutaneous, C5, C6), and posterior (radial nerve, C6–C8) cutaneous nerves of the forearm (Fig 2.4).19
OSTEOLOGY
Humerus
The distal humerus consists of an arch formed by two condyles that support the ar ticular elements of the trochlea and capitellum (Fig 2.5).
Medial to the trochlea, the prominent medial epicondyle serves as a source of attachment of the medial ulnar collateral ligament and the flexor-pronator group of muscles. Laterally, the lateral epicondyle is located just proximal to the capitellum and is much less prominent than the medial epicondyle. The lateral ulnar collateral ligament and the supinator-extensor muscle group originate from the flat, irregular surface of the lateral epicondyle.
Anteriorly, the radial and coronoid fossae accommodate the radial head and coronoid process during flexion. Posteriorly, the olecranon fossa receives the tip of the olecranon.
In approximately 90% of individuals,85 a thin membrane of bone separates the olecranon and coronoid fossae. The medial supracondylar column is smaller than the lateral and explains the vulnerability of the medial column to fracture caused by trauma and some surgical procedures.56 The posterior aspect of the lateral supracondylar column is flat, allowing ease of application of contoured plates for fractures involving this structure. The prominent lateral supracondylar ridge serves as a site of attachment for the brachioradialis and extensor carpi radialis longus muscles anteriorly and for the triceps posteriorly (Fig. 2.6). It is also an important landmark for many lateral surgical approaches, especially for the “column procedure” (see Chapters 11 and 54).
Proximal to the medial epicondyle, approximately 5 to 7 cm along the medial intramuscular septum, a supracondylar process may be observed in 1% to 3% of individuals.44,48,80 A fibrous band termed the ligament of Struthers sometimes originates from this process and attaches to the medial epicondyle.38 When present, this spur serves as an anomalous insertion of the coracobrachialis muscle and an origin of the pronator teres muscle.34 Various pathologic processes have been associated w ith the supracondylar process, including fracture44 and median4 and ulnar nerve38 entrapment (see Chapter 72).
Radius
The radial head ar ticulates w ith the capitellum. It exhibits a cylindrical symmetrical shape w ith a depression in the midportion to accommodate the capitellum. The osseous contour of the radial head, on the other hand, actually is more elliptical in shape, w ith a major and minor axis. The disk-shaped head is secured to the ulna by the annular ligament (Fig. 2.7). Distal to the radial head, the bone tapers to form the radial neck, which, along w ith the head, is vulnerable to fracture.82 The radial tuberosity marks the distal aspect of the neck and has two distinct par ts (Fig 2.8). The anterior surface is covered by a bicipitoradial bursa protecting the biceps tendon during full pronation. However, it is the rough posterior aspect that provides the site of attachment of the biceps tendon. During full pronation the tuberosity is in a dorsal position; this allows repair of a ruptured biceps tendon through a posterior approach11 (see Chapter 63) and is helpful to determine axial alignment of proximal radial fractures.26 In addition to the bicipital


FIG 2.5 (A) The bony landmarks of the anterior aspect of the distal humerus. Note the 6-degree valgus angulation of the flexion axis and long axis of the humerus. (B) The prominent medial and lateral supracondylar bony columns as well as other landmarks of the posterior aspect of the distal humerus.
characteristic configuration.
radial bursa, several other potential bursae have also been described about the elbow (Fig 2.9).
Ulna
The proximal ulna provides the greater sigmoid notch (incisura semilunaris), which serves as the major ar ticulation of the elbow that is responsible for its inherent stability (Fig 2.10). The cortical surface of the coronoid process serves as the site of insertion of the brachialis muscle and of the oblique cord. Medially, the sublime tubercle serves
as the insertion site of the medial ulnar collateral ligament. The triceps tendon attaches to the posterior aspect of the olecranon process.
On the lateral aspect of the coronoid process, the lesser semilunar or radial notch ar ticulates w ith the radial head and is oriented roughly perpendicular to the long axis of the bone. Distal to this, the supinator crest serves as the site of attachment to the supinator muscle. On this crest, a tuberosity occurs that is the site of insertion of the lateral ulnar collateral ligament.51,56,65
ELBOW JOINT STRUCTURE
Articulation
The elbow joint ar ticulation is classified as a trochoginglymoid joint.76 The ulnohumeral joint resembles a hinge (ginglymus), allowing flexion
FIG 2.6 Typical supracondylar process located approximately 5 cm proximal to the medial epicondyle with its
FIG 2.7 The elliptical radial head is stabilized to the lesser sigmoid notch of the ulna. Note the symmetrical, circular portion that articulates with the capitellum.