https://ebookmass.com/product/medical-disorders-in-
Instant digital products (PDF, ePub, MOBI) ready for you
Download now and discover formats that fit your needs...
Obstetrics and Gynecology: Maintenance of Knowledge, An Issue of Obstetrics and Gynecology Clinics, 1e Janice L. Bacon
https://ebookmass.com/product/obstetrics-and-gynecology-maintenanceof-knowledge-an-issue-of-obstetrics-and-gynecology-clinics-1e-janicel-bacon/
ebookmass.com
Management of Labor and Delivery, An Issue of Obstetrics and Gynecology Clinics 1st Edition Aaron B. Caughey
https://ebookmass.com/product/management-of-labor-and-delivery-anissue-of-obstetrics-and-gynecology-clinics-1st-edition-aaron-bcaughey/
ebookmass.com
The Pancreas Revisited, An Issue of Surgical Clinics 1st Edition Avram M. Cooperman
https://ebookmass.com/product/the-pancreas-revisited-an-issue-ofsurgical-clinics-1st-edition-avram-m-cooperman/
ebookmass.com
Nutrition for Health and Health Care 7th Edition Edition Linda Kelly Debruyne
https://ebookmass.com/product/nutrition-for-health-and-healthcare-7th-edition-edition-linda-kelly-debruyne/
ebookmass.com
Ansible for Kubernetes by Example: Automate Your Kubernetes Cluster with Ansible 1st Edition Luca Berton
https://ebookmass.com/product/ansible-for-kubernetes-by-exampleautomate-your-kubernetes-cluster-with-ansible-1st-edition-luca-berton/
ebookmass.com
Key Concepts in Geomorphology 1st Edition, (Ebook PDF)
https://ebookmass.com/product/key-concepts-in-geomorphology-1stedition-ebook-pdf/
ebookmass.com
Vilfredo Pareto: An Intellectual Biography Volume II: The Illusions and Disillusions of Liberty (1891–1898) 1st ed.
Edition Fiorenzo Mornati
https://ebookmass.com/product/vilfredo-pareto-an-intellectualbiography-volume-ii-the-illusions-and-disillusions-ofliberty-1891-1898-1st-ed-edition-fiorenzo-mornati/ ebookmass.com
Blood and Ember Isabel Cooper
https://ebookmass.com/product/blood-and-ember-isabel-cooper-3/
ebookmass.com
Dancing on Bones: History and Power in China, Russia and North Korea (2022) Katie Stallard
https://ebookmass.com/product/dancing-on-bones-history-and-power-inchina-russia-and-north-korea-2022-katie-stallard/
ebookmass.com
The Third Wish Carolyn Brown https://ebookmass.com/product/the-third-wish-carolyn-brown/
ebookmass.com
ELSEVIER
1600JohnF.KennedyBoulevard Suite1800 Philadelphia,Pennsylvania,19103-2899
http://www.theclinics.com
OBSTETRICSANDGYNECOLOGYCLINICSOFNORTHAMERICAVolume45,Number2 June2018ISSN0889-8545,ISBN-13:978-0-323-58407-4
Editor:KerryHolland DevelopmentalEditor:KristenHelm
ª 2018ElsevierInc.Allrightsreserved.
ThisperiodicalandtheindividualcontributionscontainedinitareprotectedundercopyrightbyElsevier,andthefollowingtermsandconditionsapplytotheiruse:
Photocopying
Singlephotocopiesofsinglearticlesmaybemadeforpersonaluseasallowedbynationalcopyrightlaws.Permission ofthePublisherandpaymentofafeeisrequiredforallotherphotocopying,includingmultipleorsystematiccopying, copyingforadvertisingorpromotionalpurposes,resale,andallformsofdocumentdelivery.Specialratesareavailable foreducationalinstitutionsthatwishtomakephotocopiesfornon-profiteducationalclassroomuse.Forinformation onhowtoseekpermissionvisit www.elsevier.com/permissions orcall:(+44)1865843830(UK)/(+1)2152393804 (USA).
DerivativeWorks Subscribersmayreproducetablesofcontentsorpreparelistsofarticlesincludingabstractsforinternalcirculation withintheirinstitutions.PermissionofthePublisherisrequiredforresaleordistributionoutsidetheinstitution. PermissionofthePublisherisrequiredforallotherderivativeworks,includingcompilationsandtranslations(please consult www.elsevier.com/permissions).
ElectronicStorageorUsage PermissionofthePublisherisrequiredtostoreoruseelectronicallyanymaterialcontainedinthisperiodical,including anyarticleorpartofanarticle(pleaseconsultwww.elsevier.com/permissions).Exceptasoutlinedabove,nopartofthis publicationmaybereproduced,storedinaretrievalsystemortransmittedinanyformorbyanymeans,electronic, mechanical,photocopying,recordingorotherwise,withoutpriorwrittenpermissionofthePublisher.
Notice NoresponsibilityisassumedbythePublisherforanyinjuryand/ordamagetopersonsorpropertyasamatterof productsliability,negligenceorotherwise,orfromanyuseoroperationofanymethods,products,instructionsorideas containedinthematerialherein.Becauseofrapidadvancesinthemedicalsciences,inparticular,independent verificationofdiagnosesanddrugdosagesshouldbemade.
Althoughalladvertisingmaterialisexpectedtoconformtoethical(medical)standards,inclusioninthispublicationdoes notconstituteaguaranteeorendorsementofthequalityorvalueofsuchproductoroftheclaimsmadeofitbyits manufacturer.
ObstetricsandGynecologyClinics (ISSN0889-8545)ispublishedquarterlybyElsevierInc.,360ParkAvenueSouth,New York,NY10010-1710.MonthsofissueareMarch,June,September,andDecember.PeriodicalspostagepaidatNew York,NY,andadditionalmailingoffices.Subscriptionpriceperyearis$313.00(USindividuals),$652.00(USinstitutions), $100.00(USstudents),$393.00(Canadianindividuals),$823.00(Canadianinstitutions),$225.00(Canadianstudents), $459.00(internationalindividuals),$823.00(internationalinstitutions),and$225.00(internationalstudents).Toreceive student/residentrate,ordersmustbeaccompaniedbynameofaffiliatedinstitution,dateofterm,andthesignature ofprogram/residencycoordinatoroninstitutionletterhead.Orderswillbebilledatindividualrateuntilproofofstatus isreceived.Foreignairspeeddeliveryisincludedinall Clinics subscriptionprices.Allpricesaresubjecttochange withoutnotice.POSTMASTER:Sendaddresschangesto ObstetricsandGynecologyClinics,ElsevierHealthSciences Division,SubscriptionCustomerService,3251RiverportLane,MarylandHeights,MO63043. CustomerService: Telephone:1-800-654-2452(U.S.andCanada);314-447-8871(outsideU.S.andCanada).Fax:314-447-8029. E-mail: journalscustomerservice-usa@elsevier.com (forprintsupport); journalsonlinesupport-usa@elsevier. com (foronlinesupport).
Reprints. Forcopiesof100ormoreofarticlesinthispublication,pleasecontacttheCommercialReprintsDepartment, ElsevierInc.,360ParkAvenueSouth,NewYork,NewYork10010-1710.Tel.:212-633-3874;Fax:212-633-3820; E-mail: reprints@elsevier.com
ObstetricsandGynecologyClinicsofNorthAmerica isalsopublishedinSpanishbyMcGraw-HillInteramericana EditoresS.A.,P.O.Box5-237,06500,Mexico;inPortuguesebyReichmannandAffonsoEditores,RiodeJaneiro, Brazil;andinGreekbyPaschalidisMedicalPublications,Athens,Greece.
ObstetricsandGynecologyClinicsofNorthAmericaiscoveredinMEDLINE/PubMed(IndexMedicus),Excerpta Medica,CurrentConcepts/ClinicalMedicine,ScienceCitationIndex,BIOSIS,CINAHL,andISI/BIOMED. PrintedintheUnitedStatesofAmerica.
Contributors CONSULTINGEDITOR WILLIAMF.RAYBURN,MD,MBA
AssociateDean,ContinuingMedicalEducationandProfessionalDevelopment, DistinguishedProfessorandEmeritusChair,ObstetricsandGynecology,Universityof NewMexicoSchoolofMedicine,Albuquerque,NewMexico
EDITORS
ERIKAPETERSON,MD
AssociateProfessor,DepartmentofObstetricsandGynecology,Director,Divisionof Maternal-FetalMedicine,Co-DirectorFetalConcernsCenterofWisconsin,Medical CollegeofWisconsin,Milwaukee,Wisconsin
JUDITHU.HIBBARD,MD
ProfessorEmeritus,Professor,ViceChair,DepartmentofObstetricsandGynecology, DivisionofMaternal-FetalMedicine,MedicalCollegeofWisconsin,Milwaukee,Wisconsin
AUTHORS
KASSIEJ.BOLLIG,MD
ResidentPhysician,DepartmentofObstetrics,GynecologyandWomen’sHealth, UniversityofMissouriSchoolofMedicine,Columbia,Missouri
JOANBRILLER,MD
ProfessorofMedicine,DirectoroftheHeartDiseaseinWomenProgram,Divisionof Cardiology,Professor,DepartmentofObstetricsandGynecology,UniversityofIllinoisat Chicago,Chicago,Illinois
SABRINACRAIGO,MD
ProfessorofObstetricsandGynecology,DirectorofMaternal-FetalMedicine,Tufts UniversitySchoolofMedicine,TuftsMedicalCenter,Boston,Massachusetts
MEREDITHO.CRUZ,MD,MPH,MBA
AssistantProfessor,DepartmentofObstetricsandGynecology,DivisionofMaternal-Fetal Medicine,MedicalCollegeofWisconsin,Milwaukee,Wisconsin
JEFFREYM.DENNEY,MD,MS,FACOG
AssistantProfessor,DepartmentofObstetricsandGynecology,Sectionof Maternal-FetalMedicine,WakeForestUniversitySchoolofMedicine,Winston-Salem, NorthCarolina
CARAD.DOLIN,MD
DivisionofMaternal-FetalMedicine,DepartmentofObstetricsandGynecology,NewYork UniversityLangoneHealth,NewYork,NewYork
JENNIFERE.DOMINGUEZ,MD,MHS
AssistantProfessor,DepartmentofAnesthesiology,DivisionofWomen’sAnesthesia, DukeUniversityMedicalCenter,Durham,NorthCarolina
MAURICEDRUZIN,MD
ProfessorofObstetrics,ObstetricsandGynecology,StanfordUniversity,Stanford Hospital,Stanford,California
MEGANE.FOELLER,MD
Maternal-FetalMedicineFellow,ObstetricsandGynecology,StanfordUniversity, StanfordHospital,Stanford,California
TIMOTHYM.FOELLER,MD
ClinicalInstructor,InternalMedicine,StanfordHealthCare–Valleycare,Pleasanton, California
KIMBERLYB.FORTNER,MD
AssociateProfessor,DepartmentofObstetricsandGynecology,DivisionDirector, Maternal-FetalMedicine,TheUniversityofTennesseeMedicalCenter,Knoxville, Tennessee
LORIEM.HARPER,MD,MSCI
AssociateProfessor,DepartmentofObstetricsandGynecology,Divisionof Maternal-FetalMedicine,TheUniversityofAlabamaatBirmingham,WomenandInfants Center,Birmingham,Alabama
SARAHHARRIS,MS
UniversityofNorthCarolinaatChapelHillSchoolofMedicine,ChapelHill,NorthCarolina
JUDITHU.HIBBARD,MD
ProfessorEmeritus,Professor,ViceChair,DepartmentofObstetricsandGynecology, DivisionofMaternal-FetalMedicine,MedicalCollegeofWisconsin,Milwaukee, Wisconsin
DANIELL.JACKSON,MD,MS
AssistantProfessor,DepartmentofObstetrics,GynecologyandWomen’sHealth, UniversityofMissouriSchoolofMedicine,Columbia,Missouri
AMANDAJ.JOHNSON,MD
DepartmentofObstetricsandGynecology,DivisionofMaternal-FetalMedicine,Medical CollegeofWisconsin,Milwaukee,Wisconsin
CRESTAW.JONES,MD
DepartmentofObstetrics,GynecologyandWomen’sHealth,DivisionofMaternal-Fetal Medicine,UniversityofMinnesotaMedicalSchool,Minneapolis,Minnesota
SARAHJ.KILPATRICK,MD,PhD
Chair,DepartmentofObstetricsandGynecology,DivisionofMaternal-FetalMedicine, Cedars-SinaiMedicalCenter,LosAngeles,California
DIANAKOLETTIS,MD
Maternal-FetalMedicineFellow,TuftsMedicalCenter,Boston,Massachusetts
MICHELLEA.KOMINIAREK,MD,MS
DivisionofMaternal-FetalMedicine,DepartmentofObstetricsandGynecology, NorthwesternUniversity,Chicago,Illinois
JUDETTELOUIS,MD,MPH
AssociateProfessor,DepartmentofObstetricsandGynecology,Divisionof Maternal-FetalMedicine,MFMDivisionChief,FellowshipDirector,UniversityofSouth Florida,Tampa,Florida
ANNAMCCORMICK,DO
DepartmentofObstetricsandGynecology,MedicalCollegeofWisconsin,Milwaukee, Wisconsin
CLAUDIANIEUWOUDT,MD
ResidentPhysician,DepartmentofObstetricsandGynecology,TheUniversityof TennesseeMedicalCenter,Knoxville,Tennessee
JOHNA.OZIMEK,DO,MS
StaffPhysicianI,DepartmentofObstetricsandGynecology,DivisionofMaternal-Fetal Medicine,Cedars-SinaiMedicalCenter,LosAngeles,California
ERIKAPETERSON,MD
AssociateProfessor,DepartmentofObstetricsandGynecology,Director,Divisionof Maternal-FetalMedicine,Co-DirectorFetalConcernsCenterofWisconsin,Medical CollegeofWisconsin,Milwaukee,Wisconsin
KRISTENH.QUINN,MD,MS,FACOG
AssistantProfessor,DepartmentofObstetricsandGynecology,Sectionof Maternal-FetalMedicine,WakeForestUniversitySchoolofMedicine,Winston-Salem, NorthCarolina
CALLIEF.REEDER,MD
ResidentPhysician,DepartmentofObstetricsandGynecology,TheUniversityof TennesseeMedicalCenter,Knoxville,Tennessee
LINDASTREET,MD
AssistantProfessor,DepartmentofObstetricsandGynecology,Divisionof Maternal-FetalMedicine,MedicalCollegeofGeorgia,AugustaUniversity,Augusta, Georgia
RONANSUGRUE,MD,MPH
ClinicalFellow,DepartmentofObstetricsandGynecology,BrighamandWomen’s Hospital,HarvardMedicalSchool,Boston,Massachusetts
AMELIAL.M.SUTTON,MD,PhD
AssistantProfessor,DepartmentofObstetricsandGynecology,Divisionof Maternal-FetalMedicine,TheUniversityofAlabamaatBirmingham,WomenandInfants Center,Birmingham,Alabama
GEETAK.SWAMY,MD
SeniorAssociateDeanClinicalResearch,AssociateProfessor,DepartmentofObstetrics andGynecology,Director,ObstetricsClinicalResearch,DukeUniversityMedicalSystem, Durham,NorthCarolina
ALANT.N.TITA,MD,PhD
Professor,DepartmentofObstetricsandGynecology,DivisionofMaternal-Fetal Medicine,TheUniversityofAlabamaatBirmingham,WomenandInfantsCenter, Birmingham,Alabama
NEETAL.VORA,MD DivisionofMaternal-FetalMedicine,DepartmentofObstetricsandGynecology, UniversityofNorthCarolinaatChapelHillSchoolofMedicine,ChapelHill,NorthCarolina
CHLOEZERA,MD,MPH
AssistantProfessor,DivisionofMaternal-FetalMedicine,BrighamandWomen’s Hospital,HarvardMedicalSchool,Boston,Massachusetts
Contents Foreword:Team-BasedCareofPregnantWomenwithChallenging MedicalDisorders xiii
WilliamF.Rayburn
Preface:MedicalDisordersinPregnancyxv ErikaPetersonandJudithU.Hibbard
MaternalMortalityintheTwenty-FirstCentury175
JohnA.OzimekandSarahJ.Kilpatrick
Maternalmortalityplaguesmuchoftheworld.Therewere303,000maternal deathsin2015representinganoverallglobalmaternalmortalityratioof216 maternaldeathsper100,000livebirths.IntheUnitedStates,thematernal mortalityratiohadbeendecreasinguntil1987,remainedstableuntil1999, andthenbegantoincrease.Racialdisparitiesexistintheratesofmaternal mortalityintheUnitedStates,withmaternaldeathaffectingahigherproportionofblackwomencomparedwithwhitewomen.Toreducematernal mortality,nationalorganizationsintheUnitedStateshavecalledforstandardizedreviewofcasesofmaternalmorbidityandmortality.
CancerinPregnancy187
AnnaMcCormickandErikaPeterson
Thisarticlereviewssomeofthemorecommontypesofcancerthatmaybe encounteredduringpregnancy.Itreviewstheuniquechallengeswiththe diagnosisandtreatmentofbreast,cervical,hematologic,andcoloncancersinpregnantpatients.
OpioidUseDisordersandPregnancy201
AmandaJ.JohnsonandCrestaW.Jones
Opioidusedisorderpresentsanincreasedriskofcomplicationsinpregnancy,particularlywhenuntreated.Tooptimizeoutcomes,medicationassistedtreatmentusingmethadoneorbuprenorphineasapartofa comprehensivecaremodelisrecommended.Neonatalabstinencesyndromeandpoorfetalgrowthremainsignificantcomplicationsofthisdisorderdespitematernaltreatment.
PregnancyinWomenwithObesity217 CaraD.DolinandMichelleA.Kominiarek
Pregnancyinwomenwithobesityisanimportantpublichealthproblemwith short-andlong-termimplicationsformaternalandchildhealth.Obesity complicatesalmostallaspectsofpregnancy.Giventhegrowingprevalence ofobesityinwomen,obstetricprovidersneedtounderstandtherisksassociatedwithobesityinpregnancyandtheuniqueaspectsofmanagementfor
womenwithobesity.Empathicandpatient-centeredcare,alongwithknowledge,canoptimizeoutcomesforwomenandchildren.
ManagementofObstructiveSleepApneainPregnancy233 JenniferE.Dominguez,LindaStreet,andJudetteLouis
Thespectrumofsleep-disorderedbreathing(SDB)rangesfrommildsnoringtoobstructivesleepapnea,themostsevereformofSDB.Currentrecommendationsaretotreatthesewomenwithcontinuouspositiveairway pressuredespitelimiteddata.SDBinearlyandmidpregnancyisassociatedwithpreeclampsiaandgestationaldiabetes.Pregnantwomenwitha diagnosisofobstructivesleepapneaatdeliverywereatsignificantly increasedriskofhavingcardiomyopathy,congestiveheartfailure,pulmonaryembolism,andin-hospitaldeath.Theseeffectswereexacerbatedin thepresenceofobesity.Postpartum,thesewomenareatriskforrespiratorysuppressionandshouldbemonitored.
MaternalGeneticDisordersinPregnancy249 SarahHarrisandNeetaL.Vora
Thelifeexpectancyandqualityoflifeofwomenwithgeneticdisorders continuestoimprove,resultinginmorewomenreachingreproductive ageanddesiringfertility.Itisbecomingincreasinglyimportantthatobstetriciansbecomefamiliarwithcommongeneticdisordersandtheirassociatedrisksinpregnancy.Theauthorsreviewpregnancyinwomenwith variousgeneticdisorders,includingreviewofpregnancyoutcomes,managementrecommendations,andgeneticriskassessment.Mostdataon pregnanciesinwomenwithgeneticconditionsarebasedoncasereports andliteraturereviews.Additionalstudies,includingpregnancyregistries, areneededtoimproveourunderstandingandcareofthispatient population.
MaternalCongenitalHeartDiseaseinPregnancy267 MeganE.Foeller,TimothyM.Foeller,andMauriceDruzin
Congenitalheartdiseasecomprisesmostmaternalcardiacdiseasesin pregnancyandisanimportantcauseofmaternal,fetal,andneonatal morbidityandmortalityworldwide.Pregnancyisoftenconsideredahighriskstateforindividualswithstructuralheartdiseaseasaconsequenceof alimitedabilitytoadapttothemajorhemodynamicchangesassociated withpregnancy.Preconceptioncounselingandevaluationareofutmost importance,aspregnancyiscontraindicatedincertaincardiacconditions. Pregnancycanbesafelyaccomplishedinmostindividualswithcareful riskassessmentbeforeconceptionandmultidisciplinarycarethroughout pregnancyandthepostpartumperiod.
NewInsightsinPeripartumCardiomyopathy281 MeredithO.Cruz,JoanBriller,andJudithU.Hibbard
Significantprogressinunderstandingthepathophysiologyofperipartum cardiomyopathy,especiallyhormonalandgeneticmechanisms,has beenmade.Specificcriteriashouldbeusedfordiagnosis,butthedisease
remainsadiagnosisofexclusion.Bothlong-termandrecurrentpregnancy prognosesdependonrecoveryofcardiacfunction.Datafromlargeregistriesandrandomizedcontrolledtrialsofevidence-basedtherapeuticshold promiseforfutureimprovedclinicaloutcomes.
GestationalDiabetes:UnderpinningPrinciples,Surveillance,andManagement299
JeffreyM.DenneyandKristenH.Quinn
Gestationaldiabetesmellitus(GDM)iscarbohydrateintoleranceresulting inhyperglycemiawithonsetduringpregnancy.Thisarticleprovides clinicianswithaworkingframeworktominimizematernalandneonatal morbidity.Landmarkhistoricalandrecentdataarereviewedandpresentedtoprovideclinicianswithaquick,easyreferenceforrecognition andmanagementofGDM.Datapresentedtieininsightswithunderlying pathophysiologicprocessesleadingtoGDM.Screeninganddiagnostic thresholdsarediscussedalongwithmanagementupondiagnosis.Good clinicalpracticeregardingscreening,diagnosis,andmanagementof GDMeffectivelyreducesriskandimprovesoutcomesofwomenandfetusesinaffectedpregnancies.
PregestationalDiabetesinPregnancy315 RonanSugrueandChloeZera
Diabetesisacommonchronicconditioninwomenofreproductiveage.Preconceptioncareiscrucialtoreducingtheriskofadversematernalandfetal outcomes,suchashypertensivedisorders,abnormalfetalgrowth,traumatic delivery,andstillbirth,associatedwithpoorglycemiccontrol.Insulinisthe preferredmedicationtooptimizeglucosecontrolinwomenwithpregestationaldiabetes.Frequentdoseadjustmentsareneededduringpregnancy toachieveglycemicgoals,andteam-basedmultidisciplinarycaremay help.Postpartumcareshouldincludelactationsupport,counselingoncontraceptiveoptions,andtransitiontoprimarycare.
HypertensiveDisordersinPregnancy333 AmeliaL.M.Sutton,LorieM.Harper,andAlanT.N.Tita
Hypertensivedisordersofpregnancyareaheterogeneousgroupofconditionsthatincludechronichypertension,gestationalhypertension,preeclampsia,andpreeclampsiasuperimposedonchronichypertension. Thesedisordersaccountforasignificantproportionofperinatalmorbidity andmortalityandnearly10%ofallmaternaldeathsintheUnitedStates. Giventhesubstantialhealthburdenofhypertensivedisordersinpregnancy,thereisincreasinginterestinoptimizingmanagementoftheseconditions.Thisarticlesummarizesthediagnosisandmanagementofeachof thedisordersinthespectrumofhypertensioninpregnancyandhighlights recentupdatesinthefield.
SeizuresinPregnancy349 KassieJ.BolligandDanielL.Jackson
Seizuresareamongthemostseriousneurologiccomplicationsencounteredinpregnancy.Thisarticleprovidesafoundationfortheinitial
diagnosis,evaluation,classification,andmanagementofseizuresduring pregnancy.
InfectionsinPregnancyandtheRoleofVaccines369
KimberlyB.Fortner,ClaudiaNieuwoudt,CallieF.Reeder,andGeetaK.Swamy
Pregnantwomenareatriskforinfectionandmayhavesignificant morbidityormortality.Influenza,pertussis,zika,andcytomegalovirusproducemildorasymptomaticillnessinthemotherbuthaveprofoundimplicationsforherfetus.Maternalimmunizationcanpreventormitigate infectionsinpregnantwomenandtheirinfants.TheAdvisoryCommittee ofImmunizationPracticesrecommends2vaccinesduringpregnancy:inactivatedinfluenza,andtetanustoxoid,reduceddiphtheriatoxoid,and acellularpertussisduringpregnancy.ThebenefitsofMMR,varicella, andothervaccinesarereviewed.Novelvaccinestudiesforuseduring pregnancyforpreventionofillnessareexplored.
ThromboprophylaxisinPregnancy389
DianaKolettisandSabrinaCraigo
Venousthromboembolismisaleadingcauseofmaternalmorbidityand mortalityworldwide.Identifyingwomenwhoareatgreatestriskforvenous thromboembolismandmanagingtheirpregnancieswithappropriate thromboprophylaxisisessentialtodecreasingthislife-threateningcondition.Thoseatgreatestriskarepatientswiththrombophilias,patients withapersonalorfamilyhistoryofvenousthromboembolism,andthose undergoingcesareandelivery.Currentinternationalguidelinesonthromboprophylaxisvaryindetails,butallstrategiesrelyonriskfactoridentificationandthromboprophylaxisforthehighest-riskpatients.Allguidelines requireclinicianstothinkcriticallyaboutindividualpatient’sriskfactors throughoutpregnancyandthepostpartumperiod.
OBSTETRICSANDGYNECOLOGYCLINICS FORTHCOMINGISSUES
September2018
PerinatalMentalHealth
ConstanceGuilleandRogerB.Newman, Editors
December2018
ReproductiveAging
NanetteSantoroandHowardKravitz, Editors
March2019
GynecologicCancerCare
CarolynY.Muller, Editor
RECENTISSUES March2018
ReproductiveGenetics
LorraineDugoff, Editor
December2017
ManagementofLaborandDelivery
AaronB.Caughey, Editor
September2017
EvaluationandManagementofVulvar Disease
ArunaVenkatesan, Editor
ISSUEOFRELATEDINTEREST RheumaticDiseaseClinicsofNorthAmerica, May2017(Vol.43,No.2)
ReproductiveHealth
LisaR.SammaritanoandElizaF.Chakravarty, Editors Availableat: http://www.rheumatic.theclinics.com/
Accessyoursubscriptionat: www.theclinics.com
Foreword Team-BasedCareofPregnant WomenwithChallengingMedical Disorders WilliamF.Rayburn,MD,MBA ConsultingEditor
Ithasbeennineyearssinceourlastupdateonmedicaldisordersinpregnancyin the ObstetricsandGynecologyClinicsofNorthAmerica.WeappreciateDrJudith U.HibbardforundertakingthisupdateagainwithhernewcoeditorDrErikaPeterson. Botheditorsbringtothereaderanunderstandableandlogicalapproachtotheevaluationandmanagementofpregnantwomenwhoareafflictedwithoneormoremedical conditionsdescribedinthisissue.Thewell-regardedauthorsalsopresentanyupdates inthediagnosisoftheseconditionsduringpregnancy.
Thisissuefocusesonateam-basedapproachtopatientswithmedicaldisorders thatfrequentlyantedatethepregnancy.Theincreasedprevalenceofobesityandthe delayofmorewomeninconceivingaddtoadditionalmorbidityduringgestation. Despitechronicillness,mostreproductive-agedwomenareabletoconceive.Apatient withanewlydiagnosedpregnancyandanactivemedicaldisorderispredisposedto acomplexityofproblemsthatmayfurthercomplicatepregnancy.Forexample, obstructivesleepapneaisbeingencounteredmoreoftenduetoone-thirdormore ofallpregnantwomenbeingobese.Manyconditionsdiscussedinthisissueareassociatedwithagreaterriskofpreeclampsia,fetalloss,pretermdelivery,andfetalgrowth restriction.Thromboembolism,cardiomyopathy,andothercardiovasculardiseases togetheraccountforaboutone-thirdofallmaternaldeaths.
Mostobstetriciansarefamiliarwiththedisordersdescribedinthisissue:cancer, opiateuse,congenitalcardiacdisease,diabetes,seizuresandotherneurologicconditions,andhypertensivedisease.However,lessfrequentconditionsencounteredinan obstetrician’spracticecancausethepractitionertofeel“rusty”astowhatisimportant forcontinuoussurveillanceandtreatment.Whilemanymayrelyononeormany qualifiedsubspecialists,itremainsessentialthattheobstetricianbeabletolookat
ObstetGynecolClinNAm45(2018)xiii–xiv https://doi.org/10.1016/j.ogc.2018.02.004
obgyn.theclinics.com 0889-8545/18/ª 2018ElsevierInc.Allrightsreserved.
the“bigpicture”andfunctionaseitherateammemberoraleadertoprovideoptimal caretothemother,fetus,andfamily.
Eacharticleoftheissueconsidersthesocialdeterminantsandriskfactors, screening,andtreatmentofeverymedicaldisorder.Certainconditions,suchas cardiomyopathyorcancer,areofprincipalconcernstothemother,whileothers, suchaspregestationaldiabetes,maternalgeneticdisorders,andopiateuse,posea risktothefetus,newborn,andmother.Infectiousdiseaseisperhapsthesingle mostcommonmedicalconditionencounteredbytheobstetrician,yetthiswaswell coveredintheDecember2014issue.Therefore,thisissueprovidesabriefupdate ofcertaininfectionsandemphasizestheimportantroleofvaccineswhenapplicable. Iappreciatehowpreventivehealthiscoveredinmanyarticles,especiallywiththromboprophylaxis,vaccines,andchallengesofobesity.
DrHibbardandDrPetersonselectedaverycapablegroupofaccomplished maternal-fetalmedicineauthors.Eachprovidedrelevantinformationtooffercontemporarystrategiesontheirsubject.Theirexpertiseandcommitmenttoqualitycareand advancementofpatientsafetyarenoteworthy.Itisourhopethatthissinglereference willaidprovidersinnavigatingtheseoftencomplexandchallengingissueswhilealso understandingthemostcurrentstate-of-the-scienceandrecommendations.
WilliamF.Rayburn,MD,MBA ContinuingMedicalEducationand ProfessionalDevelopment UniversityofNewMexicoSchoolofMedicine MSC105580 1UniversityofNewMexico Albuquerque,NM87131-0001,USA
E-mailaddress: wrayburn@salud.unm.edu
Preface MedicalDisordersinPregnancy ErikaPeterson,MD JudithU.Hibbard,MD Editors
Wearebothprivilegedtohavetheopportunitytoeditthisimportantissueof Obstetrics andGynecologyClinicsofNorthAmerica onthetopicofMedicalDisordersinPregnancy.Recentmedicaladvanceshaveledwomenwithcomplexmedicalproblems tobeabletochoosepregnancyandbemanagedsuccessfullythroughanoftenchallenginggestation.However,theearlytwenty-firstcenturyhasalsoseenanunprecedentedincreaseinmaternalmortalityandmorbidityintheUnitedStates.Thismaybe duetosickerpatientsnowbeingabletoconceive,oraresultofincreasedratesof obesity,advancingmaternalage,andotherfactorsleadingtogreatermorbidityfrom pregnancy.
WehaveinvitedagroupofeminentMaternalFetalMedicinephysicianstoauthorarticlesthatarebothcuttingedgeandpertinenttochangingobstetricpractice.Theynot onlyreviewtimelydataoncomplexconditionsthathavebecomeprominentinthelast severaldecadesbutalsoaddressmorecommonmedicalcomplicationsofpregnancy.
Ourissuebeginswithanimportantarticlefocusingonmaternalmortalityinthe twenty-firstcentury,anexcellentstartingpointthatputsinperspectivehowchallengingthemanagementofpregnancyhasbecome.Thisisfollowedbyseveralarticles targetinganunderstandingofdiseasesthathaverecentlycometothefore.Managementofcancerinpregnancyisupdated,whileanotherarticlehighlightstheopioid epidemicandsupervisionofdependentwomeninpregnancy.Wethenturnourfocus toobesityinpregnancy,yetanotherproblemofepidemicproportionsforwhichallobstetriciansmustbeprepared,reviewingnotonlygeneralcomplicationsbutalsoweight andsurgicalmanagementoftheobesegravida.Thisisfollowedbyaverytimelyreview ofsleepapneainpregnancy,aproblemthathasriseninparallelwiththeobesityrate. Sleepapneaisfrequentlyoverlooked,sowearefortunatetoincludethisappraisalof diagnosisandtreatmentduringpregnancy.
Thenextseveralarticlesareallrelatedtomedicalconditionsthatdecadesagowere uncommoninpregnancy,asmanyofthesewomenwereoftennothealthyenoughto
ObstetGynecolClinNAm45(2018)xv–xvi https://doi.org/10.1016/j.ogc.2018.02.003
obgyn.theclinics.com 0889-8545/18/ª 2018PublishedbyElsevierInc.
reproduce.Anexaminationofmaternalgeneticconditionshighlightsseveraldiseases, includinghereditaryhemorrhagictelangiectasiaandmyotonicdystrophyamong others.Wetakeafreshlookatmanagementofmaternalcongenitalcardiacdisease, nowmostoftensurgicallycorrectedwithimprovedoutcomes.
Wethenshiftfocustomorewell-knownmedicaldisorders,includingarenewed assessmentofperipartumcardiomyopathy,andtimelyreportsonbothgestational andpregestationaldiabeteshighlightingrecommendationsondiagnosisandmanagement.Thesurveyonhypertensivedisordersisacurrent,concisesinglereferencefor managementofallhypertensionduringgestation.Comprehensiveinformationon managementofseizuredisordersinpregnancyaswellasrecentinformationon antiseizuremedicationisincluded.
Ourlasttwopiecesfocusonpreventionofdiseaseinpregnancy.Thefirsttargets commoninfectionsinpregnancy,includingcurrentdataonZikainpregnancy,as wellasthemostrecentinformationonvaccinationsinpregnancy.Wefinishwitha reviewofthromboprophylaxis,includingthemostrecentrecommendationsonantepartum,postpartum,andpost–cesareandeliverythromboprophylaxis.
Theopportunitytoeditthisissueof ObstetricsandGynecologyClinicsofNorth America hasbeenchallenging,rewarding,andalearningexperience.Wehopeyou willfindthesearticlesasinterestingandvaluableaswehave.
ErikaPeterson,MD DivisionofMaternalFetalMedicine FetalConcernsCenterofWisconsin MedicalCollegeofWisconsin 9200WestWisconsinAvenue Milwaukee,WI53226-3522,USA
JudithU.Hibbard,MD MedicalCollegeofWisconsin 9200WestWisconsinAvenue Milwaukee,WI53226-3522,USA
E-mailaddresses: epeterson@mcw.edu (E.Peterson) jhibbard@mcw.edu (J.U.Hibbard)
MaternalMortalityinthe Twenty-FirstCentury JohnA.Ozimek, DO,MS*,SarahJ.Kilpatrick, MD,PhD
KEYWORDS
Maternalmortality Severematernalmorbidity Racialdisparities
Maternalmortalityratio Pregnancy-relateddeath
KEYPOINTS
Maternalmortalityplaguesmuchoftheworld,with303,000maternaldeathsin2015.This numberrepresentsaglobalmaternalmortalityratioof216maternaldeathsper100,000 livebirths.
TheWorldHealthOrganizationhascreatedagoaltodecreasetheglobalmaternalmortalityratioto70maternaldeathsper100,000livebirthsbytheyear2030.
ThematernalmortalityratioishigherintheUnitedStatesthaninanyotherdeveloped nationandhasincreasedoverthelastseveralyears. SignificantracialdisparitiesexistintheratesofmaternalmortalityintheUnitedStates.
INTRODUCTION
Maternaldeathwasquitecommoninthenineteenthcenturywithasmanyas7deaths per100birthsinsomehospitalsintheUnitedStates.1 Bytheearlytwentiethcentury, maternalmortalitiesimprovedbutplateauedatapproximately6to9maternaldeaths per1000livebirths.2 Mostmaternaldeathsduringthistimeweresecondarytopoor obstetriceducationanddeliverypractices,andmostofthemwerepreventable.2 In the1920s,mostdeliveriesoccurredathomeunderthecareofmidwivesorgeneral practitioners.Deliveriesduringthistimewereoftenperformedwithoutfollowingprinciplesofaseptictechnique,resultingininfection,withsepsiscausing40%ofmaternal deaths.2 Thelargemajorityoftheremainingmaternaldeathsweresecondarytohemorrhageorpreeclampsia/eclampsia.2 Inthe1930s,alinkwasdemonstratedbetween poorasepticpractice,excessiveoperativedeliveries,andhighmaternalmortality. Thesedatawerepublishedinthe1933WhiteHouseConferenceonChildHealthProtection,Fetal,Newborn,andMaternalMortalityandMorbidityreport.2 Statemedical
Theauthorshavenofinancialdisclosures. DepartmentofObstetricsandGynecology,DivisionofMaternal-FetalMedicine,Cedars-Sinai MedicalCenter,8635West3rdStreet,Suite160-W,LosAngeles,CA90048,USA
*Correspondingauthor.
E-mailaddress: john.ozimek@cshs.org
ObstetGynecolClinNAm45(2018)175–186 https://doi.org/10.1016/j.ogc.2018.01.004
obgyn.theclinics.com 0889-8545/18/ª 2018ElsevierInc.Allrightsreserved.
boardstooknoteofthisandpreviousreports,whichleadtoanewfocusonmaternal healthatthestatelevel.2 Thiscalltoactionledtotheestablishmentofthefirsthospital andstatematernalmortalityreviewcommitteesinthe1930sand1940s.Overthe followingyears,thesecommitteesdevelopedinstitutionalpracticeguidelinesand definedminimumphysicianqualificationsneededtogainhospitaldeliveryprivileges. Overthesameperiod,hospitaldeliveriesbecamefavoredoverhomedeliveries throughoutthecountry,increasingfrom55%to90%from1938to1948.2 Deliveries inhospitalswereperformedunderasepticconditionsandallowedforcareofthe poorbystate-providedservices.Thesechangesledtodecreasesinmaternalmortality after1930.Declinesinratesofmaternalmortalitybecameevenmorepronouncedwith medicaladvances,includingtheuseofantibiotics,oxytocin,improvedbloodtransfusiontechnique,andbettermanagementofhypertensiveconditionsofpregnancy.2 Theseadvancesandchangesinpracticeledtoafurtherdecreaseinmaternalmortalityof71%overa10-yearperiodfrom1939to1948.2 From1950to1973,deathsfrom septicabortiondecreasedby89%,whichislikelypartiallyattributabletothelegalizationofinducedabortionbeginninginsomestatesin1967,followedbylegalizationin allstatesin1973.2,3
Despitetheimprovementsmadeinthetwentiethcentury,maternalmortalitycontinuestoplaguemuchoftheworld,disproportionatelyaffectingdevelopingnations. AccordingtotheUnitedNationsMaternalMortalityEstimationInter-AgencyGroup, therewere303,000maternaldeathsin2015.4 Thisnumberrepresentsanoverall globalmaternalmortalityratio(MMR)of216maternaldeathsper100,000livebirths, a44%decreaseovertheprior25years.4 TheMMRvariedgreatlybyregionranging from12deathsper100,000livebirthsindevelopedregionsto546deathsper 100,000livebirthsinsub-SaharanAfricaandashighas1100deathsper100,000 livebirthsinSierraLeone.4 Currenttrendsinworldwidematernalmortalitydemonstratearangeofannualreductionfrom1.8%intheCaribbeanto5.0%forEastern Asia.4 Althoughthesereductionsinglobalmaternalmortalityrepresentatrendin therightdirection,thisdecreasefellshortoftheUnitedNationsMillenniumDevelopmentGoalofareductionof75%intheMMRbetween1990and2015.5 TheWorld HealthOrganization(WHO)haspresentednewSustainableDevelopmentGoalswith theobjectiveofreducingtheglobalMMRtolessthan70deathsper100,000livebirths from2015to2030.6 Inordertoachievethisambitiousgoal,countrieswillneedto decreasetheirMMRatanannualrateofreductionofatleast7.5%,afaraccelerated ratecomparedwiththelast25years.4 Reasonscitedforthedecreaseinmaternal mortalitiesoverthelast25yearsincludeadecreaseinthetotalfertilityrate,increased maternaleducation,andincreasedaccesstoskilledbirthattendantsamongvarious otherimprovements.7 Strategiesforongoingreductionoftheglobalmaternal mortality,asoutlinedintheWHOSustainableDevelopmentGoals,includeahuman rights–basedapproachtomaternalandnewbornhealth,whichincludeseliminatinginequitiesthatleadtodisparitiesinaccess,quality,andoutcomesofcarewithinandbetweencountries.Theneedforimprovementsincare,includingsexualand reproductivehealth,familyplanning,andnewbornandchildsurvival,arealsocited asneededstrategiestocontinuetoimprovematernalmortalities.6
Ofthe171countriesstudiedbytheUnitedNationsMaternal-MortalityEstimation Inter-AgencyGroup,158demonstratedareductioninmaternalmortalityoverthe 25yearsstudied.4 Alarmingly,thereare13countriesthathaveincreasingratesof maternalmortality.ThesecountriesincludeBahamas,Georgia,Guyana,Jamaica, NorthKorea,St.Lucia,Serbia,SouthAfrica,Suriname,Tonga,UnitedStates, Venezuela,andZimbabwe.TheUnitedStatesistheONLYdevelopednationwith anincreasingMMR,and,infact,thecurrentMMRintheUnitedStatesisalmost2
timesgreaterthanthatoftheUnitedKingdomandmorethan2timesgreaterthanthe MMRinCanada.4,8
MATERNALMORTALITYINTHEUNITEDSTATES TounderstandcurrentmaternalmortalitiesandtrendsintheUnitedStates,itisimportant torecognizetheterminologythatisused.Thereareseveralterms,eachwithaslightly differentdefinitionandresultantdifferentratesofmaternalmortality.Theuseofmultiple termsoftenleadstodifferingreportsofmaternalmortalityinbothpopularandscientific literature.Currentfrequentlyusedterminologyanddefinitionsincludethefollowing:
Pregnancy-RelatedDeath(CentersforDiseaseControlandPrevention[CDC]): thedeathofawomanwhilepregnantorwithin1yearofpregnancytermination, regardlessofthedurationorsiteofthepregnancy,fromanycauserelatedtoor aggravatedbythepregnancyoritsmanagement,butnotfromaccidentalorincidentalcauses.9
Pregnancy-RelatedDeath(WHO):thedeathofawomanwhilepregnantorwith 42daysofterminationofpregnancy,irrespectiveofthecauseofdeath.10
MaternalDeath(WHO):thedeathofawomanwhilepregnantorwithin42daysof terminationofpregnancy,irrespectiveofthedurationandsiteofthepregnancy oritsmanagementbutnotfromaccidentalorincidentalcauses.10
Pregnancy-RelatedMortalityRatio(CDC):anestimateofthenumberof pregnancy-relateddeathsforevery100,000livebirths.TheCDCreportsthat therewere17.3pregnancy-relateddeathsper100,000livebirthsintheUnited Statesin2014.9
MaternalMortalityRatio(WHO):thenumberofmaternaldeathsper100,000live births.10 TheWHOreportsthatthematernalmortalityratiointheUnitedStates was14deathsper100,000livebirthsin2015.4
TheMMRisthemostcommonlyusedmeasureofmaternalmortality.IntheUnited States,theMMRhadbeensteadilydecreasinguntilreachingitsnadirin1987at6.6.8 After1987,theMMRremainedfairlystableatbetween7and8maternaldeaths/ 100,000livebirthsuntil1999whentheMMRbegantosteadilyincrease,resultingin themostrecentreportof14deaths/100,000livebirthsin2015.4 Itispostulatedthat someofthereportedincreaseintheMMRintheUnitedStatesissecondarytoimprovementsinmethodsforidentificationofpregnancy-relateddeathsandchanges incodingandclassificationofmaternaldeaths.Otherfactorsthatarethoughtto contributetotheincreasingrateofmaternalmortalityincludeincreasingmaternal age,increasingmaternalbodymassindex,andincreasedincidenceofmedical comorbidities.11–13 Alargepopulation-levelanalysis,whichanalyzeddatafromthe CentersforDiseaseControlandPreventionNationalCenterforHealthStatisticsdatabase(CDCWONDER),demonstratedthattherewasasignificantcorrelationbetween mortalityandthepercentageofnon-Hispanicblackwomeninthedeliverypopulation, furtherillustratingknownracialdisparitiesinoverallmaternaloutcomesintheUnited States.14 Theinvestigatorsalsoconcludedthatcesareandeliveries,unintendedbirths, unmarriedstatus,and4orlessprenatalvisitsweresignificantlyassociatedwith increasedMMR.14
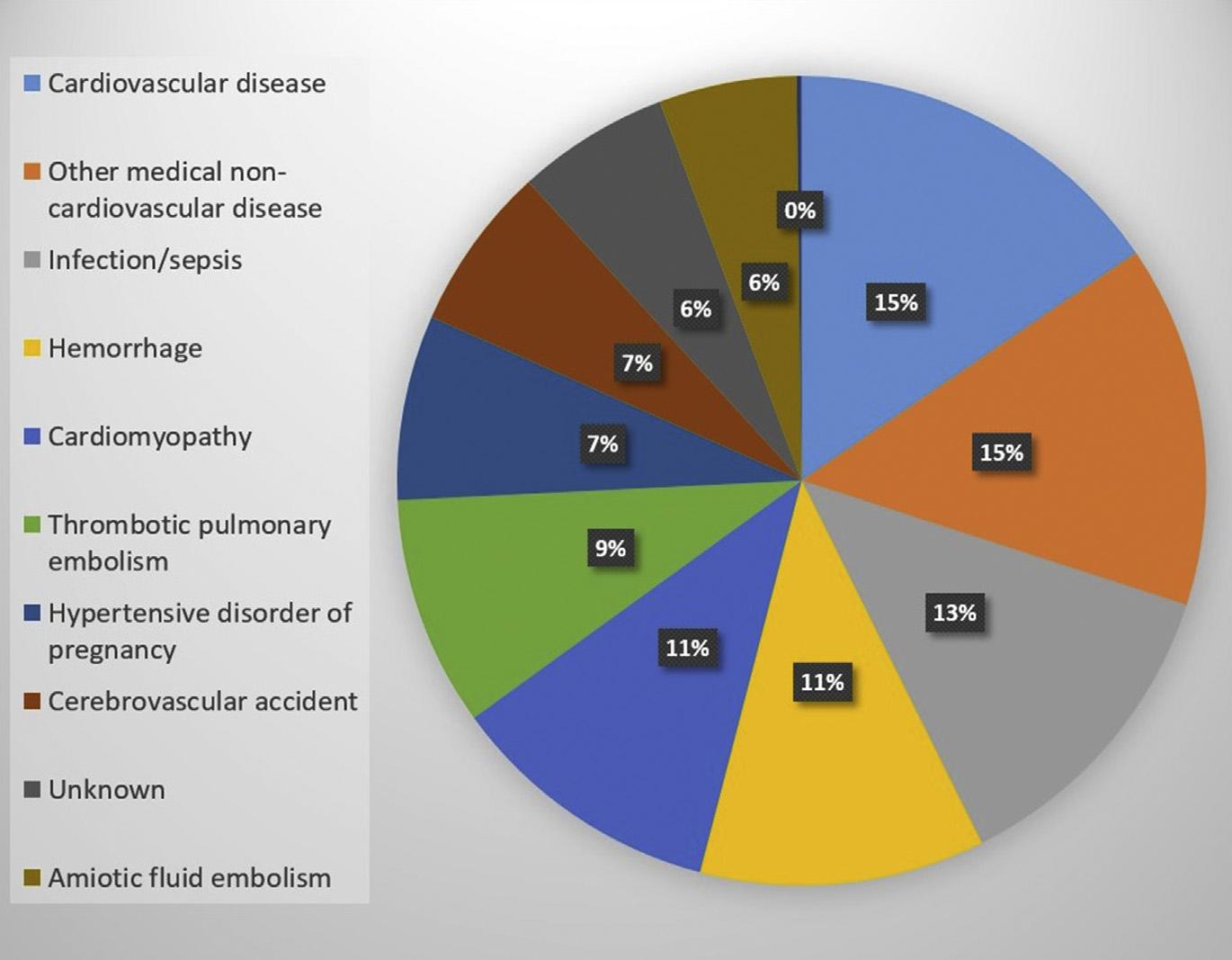
Thetop3causesofmaternalmortalityintheUnitedStateshavehistoricallybeen hemorrhage,hypertensivedisease,andthrombosis. 15 However,overtime,the contributionofthesecausestopregnancy-relateddeathdeclined,andby2010, deathssecondarytocardiovascularconditionsandinfectionincreasedwithcardiovascularconditionsrankedastheleadingcause.15 RecentdatafromtheCDC
corroboratethisshiftincauseofdeathandlistthetop3causesintheUnitedStates from2011to2013ascardiovasculardisease(15.5%),othermedicalnoncardiovasculardisease(14.5%),andinfection/sepsis(12.7%).Hemorrhageisstilllisted amongthetopcauses,rankingasthefourthleadingcauseat11.4%of pregnancy-relateddeathsduringthistime(Fig.1)16 Multiplestudiesconducted overasimilarperioddemonstrateacorollarytrendinincreasedincidenceofchronic heartdisease,17 hypertensivedisorders,18 obesity,19 anddiabetes,20 amongpregnantwomenofferingadditionalinsightintothechangingtrendsinmaternalmortality intheUnitedStates.RacialdisparitiesinmaternalmortalitypersistintheUnited Statesaswell.15
Animportantcauseofdeathamongpregnantwomenistrauma.Traumaisestimatedtoaffect1in12pregnantwomenandistheleadingnonobstetriccauseofdeath amongreproductive-agedwomenintheUnitedStates.21 Theeffectoftrauma-related maternalmortalityisnotwelldescribed.Standarddefinitionsofmaternalmortality fromtheWHOandCDCexcludetrauma-relateddeathsfromnationalmaternalmortalityreports.21 Astrauma-relateddeathsarenotincludedinnationalreports,this limitsopportunitiesforfurtherstudyandpreventionoftrauma-relateddeathsinpregnancy.Arecentstudyanalyzedmorethan1100traumaeventsamongpregnant womencomparedwith43,600traumaeventsamongage-matched,nonpregnant women.21 Theinvestigatorsfoundthatpregnantwomenweremorelikelytoexperienceviolenttrauma,were1.6timesmorelikelytodie,andweremorelikelytobe deadonarrivaltothehospitalortodieduringtheirhospitalcoursecomparedwith nonpregnantwomen.Thefindingspersisteddespitepregnantpatientshavingan
Fig.1. Causesofpregnancy-relateddeathintheUnitedStates:2011to2013.(Datafrom CentersforDiseaseControlandPrevention(CDC).Pregnancymortalitysurveillancesystem. Availableat: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html.)
overalllowerinjuryseverityscore.Theinvestigatorsshowedthatpregnanttraumavictimswerelesslikelytoundergosurgeryandmorelikelytobetransferredtoanother facility.21 Anotherimportantfindingshowedthatpregnantwomenweretwiceaslikely toexperienceviolenttraumaandmorethan3timesmorelikelytodieofviolenttrauma comparedwiththeirnonpregnantcounterparts.21 Thesefindingsunderscoretheneed forcontinuedscreeningforviolenceinpregnancyandongoingstudiesoftraumaand violenceamongpregnantwomen.
RACIALDISPARITIESANDMATERNALMORTALITYINTHEUNITEDSTATES Inananalysisofpregnancy-relateddeathintheUnitedStatesfrom2006to2010,significantracialdisparitiesinpregnancy-relatedmortalityratiosweredemonstrated.15 It wasfoundthatasignificantlyhigherproportionofnon-Hispanicblackwomenexperiencedpregnancy-relateddeathcomparedwithnon-Hispanicwhitewomen.Although womeninallracialgroupswerefoundtobeatincreasedriskofpregnancy-related deathwithincreasingage,thisfindingwasparticularlypronouncedamongnonHispanicblackwomen.15 Teenagedblackwomenwere1.4timesmorelikelytodie thantheirwhitecounterparts;blackwomenaged20to24yearswere2.8times morelikelytodie,andblackwomeninallotheragegroupsweremorethan4times morelikelytodiefrompregnancy-relatedcomplications.Forfurtherperspective, thepregnancy-relatedmortalityratioforblackwomenaged40orolderinthiscohort approached150maternaldeathsper100,000livebirthsversusapproaching40 deathsper100,000livebirthsamongwhitewomeninthesameagegroup.Thestudy alsofoundthatblackwomenwhodiedofpregnancy-relatedcomplicationswere younger,lesseducated,morelikelytobeunmarried,morelikelytobelatetoprenatal care,andmorelikelytodieofectopicpregnancy–relatedcomplicationsthanwhite women.15
Therealsoappeartobelocation-specificdisparitiesintheMMRacrossthe UnitedStates,whichmaybesecondarytotheracialdisparitiesdescribedabove.14 Inalargepopulation-levelanalysisstudyexaminingdatafromtheCDCNational CenterforHealthStatisticsdatabaseandtheDetailedMortalityUnderlyingCause ofDeathdatabase(CDCWONDER),MMRsfrom2005to2014werecomparedat astatelevel.13 Thestudydemonstratedthattherewassignificantvariabilityofthe MMRfromstatetostateandthatthesedifferencestendedtocorrelatewiththepercentageofnon-Hispanicblackwomeninthepopulation.Massachusettshadthe lowestMMRat5.6maternaldeathsper100,000livebirthsandranked25thfor thepercentageofnon-Hispanicblackbirths.TheDistrictofColumbiahadthehighestMMRat38.8deathsper100,000livebirthsandalsoranksfirstwiththehighest percentageofnon-HispanicblackbirthsandlastwiththelowestpercentageofnonHispanicwhitebirths.TheinvestigatorsnotethatalthoughtheDistrictofColumbia hasthehighestMMRintheUnitedStates,italsohasthelowestMMRfornonHispanicwhitebirths. 13 Althoughithasbeenpostulatedinthepastthatsomeof thelocation-specificdisparitiesinmaternaloutcomesaresecondarytopoverty, immigration,orruralstatus,datafromthisstudyfoundnocorrelationbetween maternalmortalityandanyofthesevariables.13 Statewidedifferencesinmedical factors,suchashypertensivedisease,diabetes,tobaccouse,andobesity,were analyzedaswellandwerenotfoundtobesignificantlycorrelatedwithmortalityratios.ThisstudydemonstratedthatthevariationinMMRwasmostcloselyassociatedwithsocialfactors,suchasunintendedpregnancy,unmarriedstatus,and non-Hispanicblackrace,furtherdemonstratingthesignificantracialdisparitiesin theUnitedStates.14
PREVENTABILITY Multiplestudieshavedemonstratedthatalmosthalfofpregnancy-relateddeathsin theUnitedStatesarepreventable.22,23 Inaretrospectivestudyofmaternaldeaths inNorthCarolina,108pregnancy-relateddeathswerereviewedbytheNorthCarolina Pregnancy-RelatedMortalityReviewCommittee.22 Theyfoundthat40%of pregnancy-relateddeathswerepotentiallypreventableandthatpreventabilityvaried bycause.Theyreportedthat93%ofhemorrhage-relateddeaths,60%of hypertension-relateddeaths,43%ofinfection-relateddeaths,and40%of cardiovascular-relateddeathswerepotentiallypreventable.Itwasalsosurmisedby theinvestigatorsthatimprovedqualityofmedicalcarewastheleadingfactorthat couldhaveledtoprevention.22 Otherstudieshavereportedsimilarfindingswith onestudyinMassachusettsreportingthat54%ofpregnancy-associateddeaths weredeemedpreventable.23 AlthoughtheMMRintheUnitedStatesisrising,luckily absolutenumbersremainlow,makingitdifficulttostudystrategiestopreventmortality.Paststudieshaveplacedmaternalmortalityattheendofacontinuumrangingfrom healthypregnancy,tomaternalmorbidity,toseverematernalmorbidity,to death.22,24–26 Ithasbeensuggestedthat,givenseverematernalmorbidityisafar morecommonoccurrencethanmaternaldeath,strategiesshouldbedevelopedto recognizeandpreventseverematernalmorbidity,therebyinterruptingthecontinuum leadingtoanddecreasingratesofmaternalmortality.
SEVEREMATERNALMORBIDITY Likematernalmortality,severematernalmorbidityisincreasingintheUnited States.11,27,28 Itiscurrentlyestimatedtoaffectatleast50,000womenperyearwith anoccurrenceof0.5%to1.3%ofpregnanciesintheUnitedStates.27,28 Becauseseverematernalmorbiditylieswithinacontinuumrangingfromhealthypregnancyto death,effortstoidentifyandpreventcausesofseverematernalmorbidityarethought toultimatelydecreasemorbidityand,hence,maternalmortality.22,24–26 Nationalorganizationshaverecognizedthatseverematernalmorbidityisincreasingandhaveadvocatedforaprocessinwhichcasesofseverematernalmorbidityarereviewedata hospitallevel.29,30 Similartomaternaldeathreviewcommittees,thegoalistofind whereopportunitiesforimprovementincareofsuchpatientscouldhaveprevented morbidityfromoccurring,orprogressingtoasevereevent,hencereducingboth morbidityandmortality.
Identifyingspecificcasesofseverematernalmorbidityforreviewhasbeenchallengingbecausetheconceptisdifficultto defineinabsoluteterms.However,publishedguidelineshavebeensetforthandvalidatedtoallowforsensitivemethods toscreenforseverematernalmorbidity.30–32 Althoughseveralmethodsof screeningforseverematernalmorbidityhavebeenused,recentreportsrecommendusingthefollowing2screeningcriteria:pregnantorpostpartumpatients whohavebeenadmittedtotheintensivecareunitand/orhavereceived 4units ofpackedredbloodcellsbecauseoftheirhighsensitivityandspecificityforidentificationofcasesofseverematernalmorbidity.30–32 Definitive“gold-standard” guidelinestoselectcasesoftrueseverematernalmorbidityfromthosethat screenedpositiveforpossiblemor bidityhavealsobeenestablished. 33 These guidelinesarelistedinanextensiveanddetailedsystems-basedformattohelp providersdetermineiftruesevere maternalmorbidityhasoccurred. 33 Following identificationoftruecasesofseverematernalmorbidity,ithasbeenrecommended thatcasesinallhospitalsthatprovideobstetriccarebereviewedandpresentedto amultidisciplinarycommitteeinastandardizedfashiontoidentifywhere
opportunitiesforimprovementincarema yhaveexistedthatcouldhaveaverted severemorbidity. 28,30
Arecent,large,retrospectivecohortstudyusedtherecommendedscreening methods,gold-standardguidelinestoidentifytruecasesofseverematernal morbidityandrecommendedmultidisciplinaryreviewcommitteeapproachto determinetheincidenceofandcharacterizeopportunitiesforimprovementin maternalcareatalarge,academicmedicalcenter.34 Theinvestigatorsfoundthat opportunitiesforimprovementincareexistedin44%ofwomenwhoexperienced severematernalmorbidity.Thesefindingsareconcordantwithpreviousstudieson preventablematernalmortality,whichreportthatnearlyhalfofthematernaldeaths intheUnitedStatesarepreventableandunderscoredtheneedforcontinuedprovidereducationtoreducemorbidityandmortality.22,23 Thisstudyalsodemonstratedthefeasibilityoftherecommendedreviewprocessofseverematernal morbidity.
STRATEGIESFORREDUCTIONOFMATERNALMORTALITY TheCDCestablishedthepregnancymortalitysurveillancesystemin1986,whichcollectsdatafrom52reportingareas(50states,NewYorkCity,andWashington,DC).9 TheCDCrequeststhattheseareasvoluntarilysubmitcopiesofdeathcertificates forallwomenwhodiedduringpregnancyorwithin1yearofpregnancyalongwith copiesofthematchingbirthorfetaldeathcertificates.9 Thisinformationyieldsvaluableepidemiologicdataregardingcausesandriskfactorsassociatedwithmaternal deaths.Althoughthisinformationisvaluableintermsofa“bigpicture”ofmaternal mortalityintheUnitedStates,manystatesstilllackstandardizedcommitteestoreviewindividualmaternaldeaths,whichwouldallowforanopportunitytoidentify preventablecausesandstrategiesforimprovementincare.35 Perthemostrecent statisticslistedinadocumentprovidedbytheAmericanCollegeofObstetricsandGynecology,only28statescurrentlyhaveorareformingamaternalmortalityreview committee.35
TheUnitedStateslagsinitssystemofstandardizedmaternalmortalityreview comparedwithotherdevelopednationswithlowermaternalmortalities.Forexample, theUnitedKingdomhasusedanationalsystem,ConfidentialEnquiriesintoMaternal Deaths,toreviewmaternaldeathsformorethan60years.36 Inthissystem,all maternaldeathsintheUnitedKingdomarereportedtotheMothersandBabies: ReducingRiskthroughAuditsandConfidentialEnquiriesacrosstheUnitedKingdom database.37 Thesereporteddeathsarethencross-checkedforverificationand confirmed.Fullmedicalrecordsareobtainedandmadeanonymousbeforeundergoingconfidentialreview.Therecordisfirstreviewedbyapathologistandanobstetriciantodetermineacauseofdeath.Eachwoman’scareisthenreviewedbya multidisciplinarypanelof10to15expertreviewers,includingobstetricians,anesthesiologists,midwives,pathologists,andotherspecialistsasdeterminedtobeappropriate.Thesummaryofcareisthenexaminedbyamultidisciplinarywritinggroupto elucidatethemainthemesforlearningtobehighlightedinthereport.37 Thissystem iscreditedwithdecreasingthealreadylowmaternalmortalityintheUnitedKingdom viaimplementationofrecommendedclinicalguidelines.Morerecently,thesystemhas alsobeencreditedwithnarrowingthegaprelatedtopregnancyoutcomesandracial disparities,significantlyloweringthematernalmortalityamongblackAfricanwomen. ThesepositivechangesoccurredwhilethematernalpopulationintheUnitedKingdom facessimilarhealthchallengesthatfacetheUnitedStates,includinganolderandless healthymaternalpopulation.36
AlthoughtheUnitedStatesmaybelaggingintermsofstandardizedreview,efforts areunderwaytodevelopstrategiestoreducematernalmorbidityandmortality.38–40 Forexample,inresponsetothesteadilyincreasingmaternalmortality,theCalifornia DepartmentofPublicHealth,incollaborationwiththeCaliforniaMaternalQuality CareCollaborative(CMQCC),developedtheCaliforniaPregnancy-AssociatedMortalityReviewprojectin2006.38,39 Thegoalofthisundertakingwastoidentifypregnancyrelateddeaths,causation,andcontributingfactorsatastatelevelandsubsequently makerecommendationsonqualityimprovementstomaternitycare.Sincethattime, thestateofCaliforniahasreduceditsMMRby55%from16.9in2006to7.3in 2013,wellbelowthenationalmaternalmortality,whichcontinuedtoincreaseover thesameperiod.38,39 TheCMQCC(https://www.cmqcc.org)wasestablishedin 2006inresponsetorisingmaternalmortalityandmorbidityrateswiththegoalof endingpreventablemorbidity,mortality,andracialdisparitiesinCalifornia.39 Inadditiontodecreasingthematernalmortality,theCMQCChassucceededindecreasing thepretermbirthrateandreducingmaternalmorbidityby21%amongthe126hospitalsthatparticipatedinprojectstoreducehemorrhageandpreeclampsia.39 The CMQCCreportsthesesuccessesaresecondarytomultiplefactors,includingthe following:
Theestablishmentofamaternaldatacentermakingreal-timedataavailablefrom morethan200hospitalsrepresenting90%ofbirthsinCalifornia. Creatingqualityimprovementinitiatives,includingtoolkitsregardingearlyelectivedelivery,hemorrhage,preeclampsia,andreducingprimarycesareans. ResearchcollaborationwiththestateofCaliforniatopublishtheCalifornia Pregnancy-AssociatedMortalityreviewtoidentifyqualityimprovementopportunitiesinmaternitycare.
TheexampleandsuccessesoftheeffortstheCaliforniaDepartmentofPublic HealthandtheCMQCCcanserveasmodelsforotherstatestoemulateinaneffort tolowermaternalmortalityintheUnitedStates.ResourcessuchastoolkitsandpatientsafetybundleslikethoseimplementedbytheCMQCCofferstandardizedapproachestopatientmanagementandhavebeenshowntoreducematernal morbidityandpresumablymortality.41 Therearevariousresourcesavailablethatoffer patientsafetybundlesfreetothepublic.Oneofthemostcomprehensiveresourcesfor maternalpatientsafetybundlescanbefoundattheWebsitefortheCouncilonPatient SafetyinWomen’sHealthcare(https://www.safehealthcareforeverywoman.org ).41 TheCouncilonPatientSafetyinWomen’sHealthCareisamultidisciplinarycollaborationcomposedofseveralprofessionalorganizations,includingtheAmericanBoard ofObstetricsandGynecology,SocietyforMaternalFetalMedicine,SocietyforObstetricAnesthesiaandPerinatology,andapproximately20otherprofessional organizations.
Aselectionofavailablebundlesincludethefollowing:
Obstetrichemorrhage
Maternalvenousthromboembolism
Reductionofperipartumracial/ethnicdisparities
Severehypertensioninpregnancy
Intermsofnationalefforts,TheAmericanCollegeofObstetriciansandGynecologistsandTheSocietyforMaternal-FetalMedicinepublishedaconsensusdocument callingforthecreationofasystemofuniformdesignationsforlevelsofmaternalcare inanefforttoreducematernalmorbidityandmortality(Table1).42 Thisdocument highlightsthesuccessesofimprovedneonataloutcomesfollowingtheregionalization
Table1
Levelsofmaternalcare
BirthcenterPeripartumcareoflow-riskwomenwithuncomplicatedsingleton termpregnancieswithavertexpresentationwhoareexpectedto haveanuncomplicatedbirth
LevelI(basiccare)Careofuncomplicatedpregnancieswiththeabilitytodetect, stabilize,andinitiatemanagementofunanticipatedmaternal-fetal orneonatalproblemsthatoccuruntilthepatientcanbe transferredtoafacilityatwhichspecialtymaternalcareisavailable
LevelII(specialtycare)LevelIfacilitypluscareofappropriatehigh-riskconditions,both directlyadmittedandtransferredfromanotherfacility
LevelIII(subspecialty care)
LevelIV(regional perinatalhealth carecenters)
LevelIIfacilitypluscareofmorecomplexmaternalmedical conditions,obstetriccomplications,andfetalconditions
LevelIIIfacilitypluson-sitemedicalandsurgicalcareofthemost complexmaternalconditionsandcriticallyillpregnantwomenand fetuses
Adaptedfrom AmericanCollegeofObstetriciansandGynecologistsandSocietyforMaternal–Fetal Medicine,MenardMK,KilpatrickS,SaadeG,etal.Levelsofmaternalcare.AmJObstetGynecol 2015;212(3):259–71;withpermission.
ofneonatalcareviarisk-appropriatematernaltransportnetworks,butreviewsthatthis systemfocusesalmostentirelyontheneedsofthenewbornandnotnecessarilythe mother.Theinvestigatorshavecreated4objectivesincludingcreationofuniformdesignationsforlevelsofmaternalcareavailableatfacilities,todevelopstandardizeddefinitionsforfacilitiesthatprovideeachlevelofmaternalcare,toprovideconsistent guidelinesperlevelofmaternalcareforuseinqualityimprovementandhealthpromotion,andtofosterthedevelopmentandequitablegeographicdistributionoffullservicematernalcarefacilities.42 Throughtheseefforts,itishopedthatmaternalcare canbeimprovedandnationalratesofmorbidityandmortalityaredecreasedand broughtinlinewithotherdevelopednations.
SUMMARY Despiteimprovementsinratesofglobalmaternalmortalityoverthelastcentury,it remainsaproblemthatcontinuestoplaguemuchoftheworld.Ratesofmaternal mortalityareincreasingintheUnitedStateswithsignificantracialdisparitiesthat disproportionatelyaffectnon-Hispanicblackwomen.UptohalfofpregnancyrelateddeathsintheUnitedStateshavebeenfoundtobepreventable. 14,21,22 There arestrategiesthathavebeenshowntoreducetheratesofseverematernal morbidityandmaternalmortalit yinregionsoftheUnitedStates. 36,38 Itisimperative thattheseeffortsareadoptedonanationalleveltodecreasetheratesofmaternal mortality.
REFERENCES 1. LoudonI.Deathinchildbirth:aninternationalstudyofmaternalcareandmaternal mortality,1800–1950.Oxford:ClarendonPress;1992.
2. CentersforDiseaseControlandPrevention(CDC).Healthiermothersand babies.MMWRMorbMortalWklyRep1999;48(38):849–58[Erratumappearsin MMWRMorbMortalWklyRep1999;48(39):892]
3. CatesWJr,GrimesDA,SchulzKF.AbortionsurveillanceatCDC:creatingpublic healthlightoutofpoliticalheat.AmJPrevMed2000;19(1S):12–7
4. AlkemaL,ChouD,HoganD,etal,UnitedNationsMaternalMortalityEstimation Inter-AgencyGroupCollaboratorsandTechnicalAdvisoryGroup.Global, regional,andnationallevelsandtrendsinmaternalmortalitybetween1990 and2015,withscenario-basedprojectionsto2030:asystematicanalysisby theUNMaternalMortalityEstimationInter-AgencyGroup.Lancet2016; 387(10017):462–74
5.UNGeneralAssembly.UnitedNationsMillenniumDeclaration,ResolutionAdoptedbytheGeneralAssembly;2000;A/RES/55/2.
6. Strategiestowardendingpreventablematernalmortality(EPMM).Geneva (Switzerland):WorldHealthOrganization;2015
7. HoganMC,ForemanKJ,NaghaviM,etal.Maternalmortalityfor181countries, 1980-2008:asystematicanalysisofprogresstowardsMillenniumDevelopment Goal5.Lancet2010;375(9726):1609–23.
8.Organisationforeconomicco-operationanddevelopment.Availableat: http://stats. oecd.org/index.aspx?DataSetCode5HEALTH_STAT#.AccessedJune5,2017.
9.CentersforDiseaseControlandPrevention.Availableat: www.cdc.gov/ reproductivehealth/maternalinfanthealth/pmss.html.AccessedJune5,2017.
10.WorldHealthOrganization,Healthstatisticsandinformationsystems.Availableat: www.who.int/healthinfo/statistics/indmaternalmortality/en/.AccessedJune5,2017.
11. KassebaumNJ,Bertozzi-VillaA,CoggeshallMS,etal.Global,regional,andnationallevelsandcausesofmaternalmortalityduring1990-2013:asystematic analysisfortheGlobalBurdenofDiseaseStudy2013.Lancet2014;384(9947): 980–1004
12. BergCJ,ChangJ,CallaghanWM,etal.Pregnancy-relatedmortalityintheUnited States,1991-1997.ObstetGynecol2003;101(2):289–96
13. MacKAyAP,BergCJ,LiuX,etal.Changesinpregnancymortalityascertainment: UnitedStates,1999-2005.ObstetGynecol2011;118(1):104–10
14. MoaddabA,DildyGA,BrownHL,etal.Healthcaredisparityandstate-specific pregnancy-relatedmortalityintheUnitedStates,2005-2014.ObstetGynecol 2016;128(4):869–75.
15. CreangaAA,BergCJ,SyversonC,etal.Pregnancy-relatedmortalityinthe UnitedStates,2006-2010.ObstetGynecol2015;125(1):5–12
16.CentersforDiseaseControlandPrevention,PregnancyMortalitySurveillanceSystem.Availableat: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/ pmss.html.AccessedJune5,2017.
17. KuklinaE,CallaghanW.Chronicheartdiseaseandsevereobstetricmorbidity amonghospitalisationsforpregnancyintheUSA:1995-2006.BJOG2011; 118(3):345–52
18. KuklinaEV,AyalaC,CallaghanWM.Hypertensivedisordersandsevereobstetric morbidityintheUnitedStates.ObstetGynecol2009;113(6):1299–306
19. HinkleSN,SharmaAJ,KimSY,etal.Prepregnancyobesitytrendsamonglowincomewomen,UnitedStates,1999-2008.MaternChildHealthJ2012;16(7): 1339–48.
20. AlbrechtSS,KuklinaEV,BansilP,etal.DiabetestrendsamongdeliveryhospitalizationsintheU.S.,1994-2004.DiabetesCare2010;33(4):768–73.
21. DeshpandeNA,KucirkaLM,SmithRN,etal.Pregnanttraumavictimsexperience nearly2-foldhighermortalitycomparedtotheirnonpregnantcounterparts.AmJ ObstetGynecol2017;217(5):590.e1–9
22. BergCJ,HarperMA,AtkinsonSM,etal.Preventabilityofpregnancy-related deaths:resultsofastate-widereview.ObstetGynecol2005;106(6):1228–34