Approachtoapatientwith headache
SeyedEhsanMohammadianinejad
IranianCenterofNeurologicalResearch,NeuroscienceInstitute,TehranUniversityofMedicalSciences, Tehran,Iran
Introduction
Headache(HA)isacommonsymptominmanysystemicandneurologicdisorders.ThethirdeditionofInternationalClassificationofHeadache Disorders(ICHD-3)listsmorethan200primaryandsecondaryHA disordersthatcanbedifferentiatedmostlybyhistoryandphysicalexamination[1].
ICHDclassifiesHAdisordersintotwotypes
1. PrimaryHAsthatlackanunderlyingstructuraldisorder.Thecornerstone ofdiagnosisisagoodhistorytaking,sinceneurologicalexaminationand paraclinicalinvestigationsarecharacteristicallynormal.PrimaryHAs consistoffourgroups,includingmigraine,tension-typeHA(TTH), trigeminalautonomiccephalalgias(TACs),andotherprimaryHA disorders.Thesebenignconditionscanbemimickedbysecondary causes.ThereisnodefinitivediagnostictestforprimaryHAs;therefore, secondarycausesshouldbeexcludedtomakeadiagnosis.
2. SecondaryHAsthathaveanunderlyingcausethatshouldbediscovered byred flagsfoundinhistoryorphysicalexaminationorarelevantabnormalityfoundininvestigationsincludingimagingorlaboratorytests. Therefore,anormalexaminationalonedoesnotexcludesecondaryHA disorder.Inpractice,approximately90%ofpatientswithHAhaveprimaryHAs[2].
HeadacheandMigraineinPractice
ISBN:978-0-323-99729-4
https://doi.org/10.1016/B978-0-323-99729-4.00010-7
https://t.me/medicalRobinHood
© 2022ElsevierInc. Allrightsreserved. 1 j
Therefore,thediagnosisofaprimaryHAdisordersrequiresthe followingstages:
1. Therearenored flagsorbetterexplanationsforthesymptoms.Thisis actuallyanimportantnegativepointforthediagnosisofaprimaryHA.
2. Therearetypicalfeaturessupportingthediagnosisaccordingtocriteria. Thisisactuallyanimportantpositivepointforthediagnosisofaprimary HA.
• ThesymptomsofmigraineHAsuchasnausea,vomiting,photophobia,orphonophobiaarenotspecificandseveralprimaryand secondaryHAdisorderscansuperficiallymimicmigraineHA (Table1.1)[3,4].
• HAsresemblingTTHareacommonphenotypeinbraintumors.
• Inalmostallofthesemimickers,thereisoneormoreatypicalfeatures indetailedhistorytakingorphysicalexaminationthatisnot compatiblewithtypicalprimaryHA[4].Meanwhile,theprimary andsecondaryHAdisorderscouldoccursimultaneouslyinapatient.
Inconclusion,allpatientswithHA,eventhosethatseemtohaveaprimarybenigndisorderinitially,should firsthaveanegativediagnosisby excludingsecondarycauses.Thisismainlyperformedbydetailedhistory takingandcompletedbyatargetedsystemicandneurologicexamination tosearchforred flags(Table1.2).Imagingandlaboratoryworkupcompletestheinvestigationincaseswhereasecondarycauseisinconsideration (Algorithm1.1).Thepresenceofred flags,asshownin Table1.2,mandatespatientevaluationforasecondaryHAdisorder[5 9].
Table1.1 HAdisordersthatmimicmigraineHA.
PrimaryHAdisordersSecondaryHAdisorders
Hemicraniacontinua
ClusterHA
Vascularmalformations
Cerebralveinthrombosis
Cervicalarterydissection
Giantcellarteritis
Hypertension
Braintumors
Hydrocephalus
Pseudotumorcerebrisphenoidsinusitis
CADASIL
Table1.2 Red flagsthatmayindicateasecondaryHAdisorder.
AcuteonsetsevereHA
TheworstHAoflife
ThunderclapHA
Split-secondonsetHA
The firstoccurrenceofanewtypeofHA
AchangeinthepatternofHA
ProgressiveorworseningHA
OnsetofHAatage50ormore
ChronicdailyHAthathasaclearlyrememberedonset(NDPH)
HAthatremainsfocalovertime
Recentonsetofaside-lockedHA
HApresentimmediatelyaftersleep
HAthatawakenspatientfromsleep(nocturnalheadache)
VomitingprecedesHA
Neurologicsymptomsand/orsigns
Systemicsymptomsand/orsigns
HAwithchangesinbehavior/personality
AcuteHAfollowingcough,sneeze,strainingoranyvalsalvamaneuver
AcuteHAafterbending
AcuteHAafterexercise
AcuteHAduringsexualintercourse
AcuteHAinpregnancyorpostpartumperiod
Underlyingcancer,diabetesorimmunocompromisedstate
HAinpatientsonanticoagulants
HAinpatientswithdementia
HAoccurringorexacerbatingwithposturalchanges
HAdoesnotrespondadequatelytotreatment
Recenthistoryofheadornecktrauma
OnsetofHA < 6years
MostofthepatientswithHAcanbediagnosedwithhistoryalone. Obviously,moretimeisusuallygiventohistorytakingcomparedto physicalexaminationinpatientswithHA.ItisnotpossibletodiagnoseprimaryHAdisorderswithouthistorytaking.Historytakingrevealsmanyred fl agsforsecondaryHAsandalsoguidesthephysicianastotheorderofimagingorlaboratoryinvestigations.Italsoprovidesabackgroundfortreatmentplans.
Thefollowingpartsofthischapterdiscusstheuseoftargetedhistorytaking,physicalexamination,and finallyimagingandlaboratoryinvestigations toapproachapatientwithHA.Elementsofhistorytakingareshownin Table1.3 andexplainedinthefollowingsections.
Table1.3 Historytakinginapatientwithheadache.
1WhatwasyouragewhenHAstarted?
2Temporalpro fileofHAepisode(s)
a. HowlonghaveyoubeenhavingHA?
b. Howdoesitstartandhowlongdoesittakefromonsettopeak?
c. Whatisthedurationandfrequencyofepisodes?
d. Hastherebeenachangeinthepatternofepisodesrecentlyorisyour recentHAlikeyourpreviousones?
3HaveyoueverhadsimilarHAbefore?
4Whereisthelocationofpainandwheredoesitradiate?
5Howisthepainquality?
6Howdoyouscoretheseverityofpainfrom1to10?
7Whataretheaccompanyingsymptoms?
8DoyouexperiencepremonitorysymptomsbeforetheonsetofHA?
9Howdoyoubehaveduringtheattack?
10DoHAepisodesoccurinparticulartimes?
11Dotheattacksawakenyoufromsleep?
12Whatareexacerbatingandrelievingfactors?
13IstheHArelatedtoposturalchange?
14Isthereachangeinbehaviorandpersonality?
15Doesthepatienthaveafamilyhistoryofmigraineorneurologicdisorder?
16Isthereoneormoretypesofheadache?
17Isthereahistoryofheadornecktrauma?
18IsthereacutepainfollowingValsalva(cough,straining,lifting)?
20Isthereacutepainafterexercise?
21IsHArelatedtosexualactivityandhow?
22Isthereahistoryofanysystemicdiseaselikehypothyroidism,connective tissuedisorder(CTD),hypertension,glaucoma,HIV,cancer, immunosuppression.
23Whatistheamountofanalgesicsyouconsumeinaweek?
24Whatarepersonalhabits?
25DidtheHAstartduringpregnancyorinthepostpartumperiod?
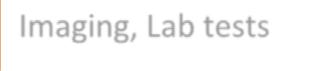
Algorithm1.1. Primaryapproachtopatientwithheadache.
Patient with headache
Targeted history taking & physical examination
Are there any red flags? (See Table 2)
Possible primary HA disorder
Supportive features for diagnosis of primary HA disorder
YES
Determine the type of primary HA disorder
Migraine HA Tension HA TACs
Other primary p y HA disorders YES
Imaging, Lab tests Rule out Medication overuse? NO
Determine if secondary HA disorder present
Historytakinginpatientswithheadache
WhatwasyouragewhenHAstarted?
Thepatient’sagehassignificantdiagnosticandtherapeuticimplicationsinHA.
• HAisthemostcommonneurologiccomplaintinchildren.Mostcases areduetoprimarybenigndisorders,butconcernsdoexistfor
secondarydisorders.TheSNOOOPPPPYred flagshaverecentlybeen suggestedtodeterminechildrenwithHAwhorequireevaluationfor secondarycauses(Table1.4)[9,10].Althoughthereisgeneralagreement aboutmostoftheincludedfeatures,thereisnoconsensusforsome, includingageandoccipitalpain[11,12].
TheonsetofHAinlessthan6yearsisconsideredared flag,becausethe historyandphysicalexaminationmaynotbeveryreliableinthisagegroup. However,itprobablydependsonthecase.Obviouslyifthepatient’ sage doesnotallowanadequateevaluation,furtherevaluationseemsreasonable.
TheICHD-3considersthatoccipitalpainisrareinchildhoodmigraine andcallsformoreevaluation.However,arecentstudyshowedthatoccipital HAastheonlysymptominchildrenwithoutassociatedwarningfeaturesis rarelyrelatedtobraintumorsandthereforemaybeinvestigatedsimilarto thepaininotherlocations[11,12].
• Childhoodmigraineisdifferentfromadultsinsomeclinicalaspects[13]. Itaffectsboysmoreoftenthangirlsbeforepuberty.Attacksaretypically shorterinchildren(30min 2h).Theyaremoreoftenbilateral,nonthrobbing,andlocatedinfrontalortemporalareascomparedtoadults. Vomitingmaybemoreprominentandsymptomssuchasnauseaand sensitivitytolightandsoundmaybemoreobviousfromthefunction andbehaviorofthepatientthandirectquestionsinthehistory.Migraine equivalentsarecharacteristicallymorecommoninchildren.
Migrainemostcommonlystartsat15 25yearsandattenuatesafter50.It shouldnotbeconsideredasa firstdiagnosisinheadachesstartingafterage50.
• TTHdoesnotrespecttoanyperiodoflife.Itismorecommonin middle-agedpeoplebutisalsothemostcommoncauseofHAin
Table1.4 SNOOOPPPPYred flagsforheadacheinchildren.
Systemicsymptomorillness
Neurologicsymptomorsigns
Acuteonset
Recentonset
Occipitallocation
PrecipitatedbyValsalva
Positional
Progressive
Parentsnotinvolved(negativefamilyhistory)
Year < 6
elderly,whilechildren,especiallyadolescents,arenotuncommonly affected.Adolescentswithintractableprimaryheadachesandnormal investigationswhodonotrespondadequatelytotreatmentprobably sufferfromTTHandbenefitfromapsychiatricconsultation[14,15].
• HAinolderadults(practicallyafterage50)ismostcommonlycausedby primaryHAssuchasTTHormigraine,buttheriskofsecondarydisordersincreasesinthisagegroup(Table1.5)[16,17].Thisiswhynew onsetHAafterage50isared flagandmandatesevaluationforsecondary causes.
• Giantcellarteritis(GCA)startsafter50andshouldbeexcludedinevery olderadultpatientwithnewonsetHA.
• Ischemicstrokes,particularlywhentheyoccurintheposteriorcirculation,arecommonlyassociatedwithheadaches.Asevereheadache withanacuteonsetmaybeduetoanischemicinfarctofthecerebellum oroccipitallobe.Focalneurologicdeficitsareoftenpresent.
• ICHshouldbeconsideredinanolderadultpresentingwithacutesevere HA.Itcouldbeintheformofintraparenchymal,subduralorepidural hematoma.Alteredconsciousnessandvomitingareoftenassociated.This diagnosisshouldbeparticularlyconsideredinhypertensivepatientsor thoseonanticoagulants.
• BraintumorsdonothaveacharacteristictypeofHA;mostpatientshave aclinicalpicturelikeaTTH.Thereisared flagofteninhistoryandless ofteninphysicalexaminationtoguidethephysician.
• Inolderadults,especiallythosewithvascularriskfactors,HAthatoccurs uponexerciseandisrelievedbyrestmaybeduetocardiacischemia. UnlikeotherHAs,cardiaccephalalgiaisuniquelyrelievedby nitroglycerine.
• CervicogenicHAismorecommoninolderadults.Thepainistypically unilateral,startswithneckpain,andextendstotheheadonthesame
Table1.5
Primarycauses:
TensiontypeHA,Migraine,HypnicHA
Secondarycauses: Giantcellarteritis,intracranialhemorrhage,subduralhematoma,ischemicstroke, braintumors,cervicogenicHA,posttraumaticHA,glaucoma,hypertension, cardiaccephalalgia,sleepapnea,medicationoveruseHA
CommoncausesofHAinolderadults.
side.Neckstiffnessandlimitedrangeofmotionarecommonlypresent. Neckmovementorpressureonthegreateroccipitalnervemayprovoke thepain.Migrainefeaturessuchasnausea,vomiting,photophobia,or phonophobiamaybepresentalthoughtoalesserextentcomparedto migraine[18].
• SleepapneamaypresentwithmorningorwakeupHAinolderpatients. Thisshouldnotbeforgotteninthisagegroup,sincetheprevalenceof sleepapneaincreaseswithage.
• Acuteangleclosureglaucomaiseasilydiagnosedbecauseoftheprominenteyesymptomssuchasredeyeandblurredvision,whileitisnotthe casewithsubacuteangle-closureglaucomathattypicallypresentswith noredeye.ItmaypresentwithintermittentshortHAepisodes.Theylast usuallylessthan4h(usuallylessthan1h)andareoftenassociatedwith blurredvision.Theepisodestypicallyoccurintheeveningwhendim lightresultsinmydriasisleadingtoincreasesintraocularpressure[19].It needsahighindexofsuspicionasacauseofintermittentunilateralHAin olderpeople.
• OlderpatientswithHAmostoftensufferfromTTHcomparedto migraine.TheclinicalprofileofTTHinolderadultsisthesameas youngerpeoplebutthismaynotbetrueformigraine.Interestingly, symptomssuchasnausea,vomiting,photophobia,andphonophobiaare lessprominentinolderadultswithmigrainebutneckpainismore common[20].
• HypnicHAisaparticulartypeofprimaryHAdisorderthattypicallyoccursafterage50.Itoccursexclusivelyatnightandawakensthepatient fromnocturnalsleep.Thebilaterallocationandabsenceofautonomic featuresdifferentiateitfromclusterHA[21,22].
WhatisthetimecourseofHA?
ThisisactuallythemostinformativepartofhistoryinapatientwithHA.It shouldbeaskedindetailveryaccurately.
HowlonghaveyoubeenhavingHA?
ArecentonsetHAismorelikelytobesecondarytoaseriousdiseasethana stablepatternofachronicheadache.ThelongerthetimeHAhasbeenpresent(>12months),thegreaterthechancethatitisaprimarybenigntype. ThisiswhilethemorerecenttheHAonset(<6months),thehigheristhe riskofaworrisomecause.
Howdoesitstartandhowlongdoesittakefromonsettopeak?
• AcuteHAwithmaximalseveritywithinsecondstominutesofonset shouldalwaysbeconsideredserious,particularlyifnotexperienced before.
TheonsettopeaktimeofHAisveryimportant.Theshorteristhetime, thehigheristheriskofaseriousdisease.IftheHApeaksinlessthan1minute,itisreferredtoasathunderclapHA(TCH),whichisaseriousred flag, withavascularcauseinmostsecondarycases.Althoughaperiodof1minis proposedfordefiningTCH,everysevereHAthatstartsacutelyandpeaksin ashorttime(notnecessarily1min)isconsideredasared flag[23].Thisis particularlytruewhenitisdescribedas “theworstHAoflife.”
CommoncausesofTCHareshownin Table1.6.ThesamelistisconsideredforsuddenonsetsevereHAregardlessoftheproposed1minute.The detailsarediscussedinthenextchapters.
• Subarachnoidhemorrhage(SAH)isactuallythemostimportantcauseof TCH.Timelytreatmentcanpreventrebleeding,whichisassociatedwith amortalityrateofupto70%[24].IsolatedHAisthemostcommon presentation.NothingischaracteristicforHAtodifferentiatefromother conditionsexcepttheseverityandacuteness.Thedurationofpainis usuallymorethan2handthepaintypicallylastsforhourstodays[25].
AnunrupturedaneurysmmayalsoproduceaseveresuddenonsetHAin theformofTCH.ThissentinelHA,whichisseenin10% 43%,mayoccur daystoweeks(usuallywithin2weeks)beforetheruptureofaneurysmand SAH.Itisprobablyduetoacuteexpansionoraneurysmleak[26].Sentinel HAisofutmostimportancesinceitisanalarmforaneurysmruptureinthe
Table1.6 CausesofthunderclapHA. VascularcausesNonvascularcauses
SAH
Unrupturedintracranialaneurysm
Dissectionofcervico-cerebral arteries
Cerebralvenousthrombosis
RCVS
Pituitaryapoplexy
Cerebralinfarct
Intracranialhemorrhage
PRES
Acutehypertensivecrisis
Spontaneousintracranial hypotension
Colloidcystofthirdventricle
Cardiaccephalalgia
PrimarycoughHA
PrimaryexertionalHA
PrimaryHAwithsexualactivity
PrimaryTCH
nearfuture.AspecifictimecourseforpatientswithSAHas “split-second onsetHA” probablyresultsfromsuchascenario.Thepatientexperiences asevereandtransientsentinelHA,enjoysremissionforashorttime(may behourstodays)unexpectedly,andthenagainsuffersfromamorepersistent severeHAresultingfromtheaneurysmrupture.
• Dissectionofcervicalarteriesincludinginternalcarotidartery(ICA)or vertebralartery(VA)iseasilymisdiagnosedduetovariableandsometimesnonspecificpresentations.HAandneckpainarethemostcommon andoftentheonlysymptoms.Mostpatientsexperienceischemicevents intheterritoryofthedissectedarteryduringoraftertheHAphase.Upto 80%ofdissectionsfollowatraumatotheheadorneck,whichmaybe minorandnotsignificant[27].Dissectionusuallyoccursimmediately aftertraumabutmayoccurwithalatencyof1week[28].
ICAdissectionpresentstypicallywithHA(mainlyfrontotemporal)and/ orfacialpain.Neckpainintheanterolateralareauptothejawmaybepresent.PartialHornersyndrome(ptosisandmiosiswithoutanhydrosis)ispresentin1/3ofthecases[29].Ischemicstrokeintheterritoryofthemiddleor anteriorcerebralarteriesmayfollow.
VAdissectionhasamorestereotypedclinicalprofile.Ittypicallypresents withunilateralposteriorneckpainoroccipitalpaincommonlyfollowedby lateralmedullaryinfarction.
Thediagnosisofcervicalarterydissectionshouldbeconsideredwhena combinationofacuteneckpain,HA,andfacialpainoccursshortlyatrauma. ThisisparticularlythecasewhencompleteHornersyndrome,transient monocularblindness,orischemiceventsaccompanyorfollowthepain. Obviously,thisdiagnosisiseasilymissedincaseswithisolatedpainwhen thereisnoorminortraumaortheHAisofasubacuteormorechronic coursesimilartopreviousmigraineepisodes.
• Cerebralveinthrombosis(CVT)mostcommonlypresentswithasubacuteprogressiveHAbutmaylesscommonlypresentwithacuteHA. AsignificantminorityofthepatientspresentwithTCHthatissimilarto SAH[30].HAisthemostcommonsymptomofCVT.Itmaybethe onlysymptomsbutisoftenassociatedwithotherCVTsuggestivefeatures(seechapvascular).
• Reversiblecerebralvasoconstrictionsyndrome(RCVS)ischaracterized byaspecificpatternofrecurrentshort-livedTCHs.Thepatient experiencesanacutesevereHAthatpeaksrapidlyinlessthanaminute, makingthepatientagitatedforminutestofewhours.Thepatient experiencesatemporaryremissionandthensuffersfromfurtherepisodes.
Itisauniphasicdisorderwithaspectrumofclinicalmanifestations rangingfromisolatedHAepisodestoischemicorhemorrhagic complications,alllastinglessthan3months[31].
• Pituitaryapoplexyresultsfromaninfarctorhemorrhageinthepituitary gland.Mostcasesoccurinthesettingofpituitaryadenomaalthoughthey maynotbeawareoftheadenomaatthetimeofpresentation.AcuteonsetsevereHAisthemainsymptom.Itissometimesassociatedwith varyingdegreesofvisualimpairmentandophthalmoplegia.Pituitary dysfunctionmayoccurtoavariableextent.
• Cerebralinfarcts,mainlyintheposteriorcirculation,maypresentwith acutesevereHA.ThesameistruefordifferenttypesofICHs.
• AcutehypertensivecrisismaybeassociatedwithacutesevereHA,mainly inthebackofthehead.Itmaybeassociatedwithsymptomssuchas dizziness,agitation,chestpain,dyspnea,epistaxis,andevenfocal neurologicdeficits,whicharereversibleuponbloodpressurecontrol.
• Posteriorreversibleencephalopathysyndrome(PRES)occursinthe settingofacutehypertension,eclampsia,oradministrationofsome drugs.ItpresentswithacutesevereHAassociatedwithnausea,vomiting, confusion,blurredvision,seizure,and/orfocaldeficits.Itisconfirmedby reversibleclinicalandMRI findings.
• AmongnonvascularcausesofTCH,spontaneousintracranialhypotension(SIH)requiresahighindexofsuspicion.Ittypicallypresentsas orthostaticHA;however,itpresentsasTCH,whichisverysimilarto ruptureofaneurysm,inalmost15%ofcases[32].ItoftenfollowsValsalva maneuversuchaslifting,straining,cough,bendingover,orsportactivities.ThepatternoforthostaticHAmaybecomelessobviousafterthe initialphase.
• Patientswithcolloidcystsofthethirdventriclemayexperienceacute HAfollowingbendingover.ThisisduetoobstructionoftheMonro foramenandacutereversibleobstructivehydrocephalusfollowinga positionchange.Itmayevenresultinalteredconsciousnessthatimproves uponpositionchange.
• Myocardialinfarctionshouldbeconsideredasararebutimportantcause ofTCH.ItshouldbesuspectedinacuteonsetsevereHAinolderpatientswithvascularriskfactors.
• CoughHA,exertionalHA,andHAassociatedwithsexualactivityhave primaryandsecondarytypesandallmaypresentwithTCH.Theyare discussedin Chapter5
• AmongprimaryHAdisorders,TACshavetheshortestonsettopeak time.Theycanlastforonlysecondstominutes.Cranialneuralgias, especiallytrigeminalneuralgia(TN),alsohaveaveryshortonsettopeak time.
• MigraineHAusuallypeaksin1 2h.However,migraineepisodesmay haveanonsettopeaktimeofminutes[33].Thediagnosisofmigraine shouldnotbeacceptedeasilyinthisunusuallyacuteconditionunlessa similarhistoryispresentandthereisnootherred flagintheassessment.
Whatisthefrequencyanddurationofepisodes?
• ThefrequencyanddurationofHAepisodesishelpfulfordiagnosticand therapeuticpurposes.
• HAsarearbitrarilydividedintoshortduration(lessthan4h)andlong duration(morethan4h).MigraineHAlasts4 72hifuntreatedand isoflongduration,butTACsarecharacteristicallyofshortduration.
• SubacuteclosedangleglaucomamaypresentwithintermittentshortepisodesofHAintheeveningasdiscussedbefore.New-onsetpaininolder adultsandpaindurationaremaindifferentiatingfeaturesfrombenign primaryHAs.
• SubacuteprogressionorworseningofHAintermsofthefrequencyor durationofepisodesoverweekstomonthsisared flagindicatingan intracranialpathologysuchasspaceoccupyinglesions,cerebralvenous thrombosis,intracranialhypertension,andgiantcellarthritis.
• Chronicdailyheadache(CDH)isdefinedasHAepisodesin15ormore dayspermonthforthreeormoreconsecutivemonths.
• Chronicmigraine(CM)isconsideredwhenapatientwithCDHhasHA withmigrainefeaturesforeightormoredaysinthemonth.Medication overuseisseeninmanycasesofCM.Prognosisandtreatmentstrategyare differentfromepisodicmigraine.
• ChronicTension-TypeHeadache(CTTH)isdefinedasaCDHthat ful fillsthecriteriaforTTH.Itiscommonlyassociatedwithpsychiatric comorbiditiesandrequiresmultidisciplinarymanagement.
• InchronicclusterHA(CH),CHepisodescontinueformorethan1year withoutremissionorwithremissionsoflessthan3months.ThetreatmentmayberatherdifferentfrompatientswithepisodicCH.
• NewdailypersistentHA(NDPH)isaCDHwithaclearlyremembered onset.ThepatientrememberstheexacttimeofHAonset,whichbecomesdailyandcontinuousinlessthan24h.Itisared flag,evenifthe HAhasmigraineortension-typefeatures[34].Ithasdifferentcauses,the
mostimportantofwhichincludeintracranialhypertension,intracranial hypotensionfromCSFleak,dissectionofcervicalarteries,and posttraumaticheadache.Thisemphasizestheimportanceofasking specificallyhowtheHAstartedfromonset.
HaveyouexperiencedarecentchangeinthepatternofHAs?
Inapatientwithastablepatternofheadacheformorethan6months,a seriouscauseislesslikely.ArecentchangeinthepatternofapreviouslystableHAisared flagandrequiresinvestigation.Thischangecanbeinthe temporalcourse,quality,duration,severity,location,and/oraccompanying symptomsofHA.
• AnexamplewouldbeapatientwithapreviousmigraineHAthatexperiencesacutetosubacuteprogressiveHAofdifferentdurationand severityafteracourseoforalcontraceptive(OCP)use.Itmaybe wronglyattributedtoexacerbationofmigrainefromOCPuse,butCVT oralternativepossibilitiesshouldberuledout first.
• Anotherexampleisapatientwithaprevioushistoryofoccasionalsevere attacksofmigrainewhoisreferredwithseverepersistentHAinfrontal andvertexareassince10daysago;imagingshowssphenoidsinusitis. Forheadachesthathavebegunrecently,particularlywhenthepatternis unstableandepisodesareprogressiveintermsoffrequencyandorseverity, furtherevaluationismandatory.
HaveyoueverhadsimilarHAsbefore?
Iftheanswertothequestionis “No,” theHAshouldbeinterpretedwith caution.Thisisnotnecessarilyconsideredared flagbutthepatientshould beinterpretedmorecautiouslyaccordingtoassociatedclinicalfeaturesand thesettinginwhichthepainhasstarted.
• Anexampleisapatientwithanewsevereandpersistentpainintheneck andbackofheadfor10daysfollowingtraumaandmoreinvestigation revealsdissectionoftheVA.
Whereisthelocationofpainandwheredoesitradiateto?
MigraineHAismostcommonlylocatedintheeyeorfrontalortemporal areas,butitcaninvolveanypartofheadsuchasthevertex,backofthe head,theneck,orthewholeahead.Painintheoccipitalorneckeachoccurs inalmost40%ofthepatientswithmigraine[35].Episodesofmigraineare oftenunilateral,butbilateralpainisnotuncommon.Tensionheadaches
aretypicallygeneralizedandbilateralormaybefeltinthebackofthehead, vertex,orneck.TACsareside-lockedHAsthatarecenteredmostseverely intheV1territoryoftrigeminalnerve(orbitandnearbyaround).They commonlyradiatetothetempleorface.
NeckpainisacommoncomplaintinpatientswithHAandisnotspecific forcervicogenicHA.ItiscommoninprimaryHAssuchasTTHand migraineandisseeninmanysecondaryHAdisorders.However,acute neckpainassociatedwithHAshouldbeconsideredimportant,particularly followingtrauma,sincedissectionofcervicalarteriesmaybethecause.
ThetermsinusHAisusedbypatientsandsometimesgeneralphysicians tonotepainovertheparanasalsinusesinthefaceandfrontalareas.Itisassociatedwithnausea,vomiting,photophobia,orphonophobiamostofthe timeandisactuallyduetomigraine.Nasalsymptomssuchasnasalstuffiness orrhinorrheaarenotuncommoninmigraineandshouldnotbesimply attributedtorhinogenicpain.
HAisnonspecificinbraintumors.Itisnotlocatedinaspecificpartofthe headexceptforinfratentorialtumors,whichmostlypresentwithoccipital pain.TumorHAismoreoftenlikeTTHthanothertypesofHA[36,37].
SphenoidsinusitisisanunderdiagnosedcauseofHA.Thepainisoftenin thevertexandorretro-orbitalareabutmaybefeltinotherpartsofthehead includingthefrontaloreventheneckregion.Itrequiresahighindexofsuspicionbecausethenasalsymptomsareoftenabsent[38].Oneshouldthink ofthisdiagnosiswhenthereisasubacuteprogressiveHAinthevertexand/ orretroorbitalarea.
Side-lockedHAisdefinedasanHAthatisalwaysonthesameside. Someexpertsdefineitwhenmorethan90%ofepisodesoccuronthe sameside.TwothirdsofthecaseshaveprimaryHAdisorders,whileabout 1/3sufferfromasecondarydisorderorcranialneuralgia.Itisconsideredasa red flagrequiringinvestigationtoruleoutsecondarycauses[39].
TACsarecharacteristicallyside-locked,whichisamandatoryfeaturefor diagnosis.Migraineisrarelyside-locked,butitisadiagnosisbyexclusion. Side-lockedHAwithorwithoutneckpainwithanacutetosubacutecourse shouldbetakenseriously,sincecervico-cerebralarterialdissectionisa possibility.
HAsthatremainfocalwithoutanychangesinthelocationovertheexpectedtimeareared flagrequiringmoreevaluation.Primaryheadachesdo notusuallyremainfocalovertimeandtypicallyshifttoadjacentareasorto theotherside.
UnilateraloroccipitalHAthatbecomesgeneralizedaftertheValsalva maneuverissuggestiveofintracraniallesionsandincreasedintracranialpressure(ICP).
Whatisthequalityofpain?
Throbbingorpulsatingheadacheischaracteristicformigraineandisa featureofmigraineinICHD;however,thefollowingpointsshouldbe considered:
1. NonthrobbingHAisnotuncommoninmigraine.Therefore,ICHDallowsadiagnosisofmigraineintheabsenceofpulsatilepainwhenother criteriaarefulfilled.
2. ManyotherHAtypes(includingseriouscauses)mayalsopresentwith throbbingpain.Therefore,thethrobbingqualityofpainisnotareliablesymptomtodifferentiateprimaryfromsecondaryHAsandshould beinterpretedusingaccompanyingsymptomsandtheclinicalsetting.
TTHisdescribedasapressing,pressurelike,orbandlikepain,feeling somethingheavyonthehead,oradullheadache.
Briefsharppainindifferentpartsoftheheadisreferredtoasicepickor stabbingpain.Itiscommonlyreportedbypatientswithmigraineormaybe anidiopathicentityknownas “idiopathicstabbingHA.”
PatientswithTACs,particularlyclusterHA,mayexperienceaveryseveredeep,boring,orburningpainthatmaybedescribedasahotpokerin oneeye.Thepatientisusuallyagitatedandrestlessduringtheepisode.
TNischaracterizedbyparoxysmalsharpandjab-likepainepisodesthat thepatientdescribesasrepeatedshockstotheface.
Persistentdullpaininthemid-facewithoutanyobjective findingsis compatiblewithpersistentidiopathicfacialpain,previouslyknownasatypicalfacialpain.Itmightbeduetounderlyingpsychopathologiesalthough othercausessuchasposttraumaticpainorcomorbidpainconditionsshould alsobeconsidered.
Howdoesthepatientscorethepainseverity?
TheseverityofHAisassessedbyanumericratingscalefrom0to10in which0meansnopainand10indicatestheworstpain.ClusterHAorseveremigraineepisodesareusuallygivenascoreof8 10,butpatientswith TTHusuallygiveascoreoflessthan5;hence,thepaindoesnottypically interferewithroutinephysicalactivities.
Therefore,theseverityofHAperseisnotareliableindicatorfordifferentiatingbenignfromseriousheadachessincethemostcommonprimary HAsmaybeassevereasthepaininSAH.Itisthemodeofonset,evolution ofpain(onsettopeaktime),historyofsimilarepisodes,associatedsymptoms, andtheclinicalsettingthataremuchmorediagnostic.AnacutesevereHA thatpeaksinashorttimerequiresinvestigationwhenoccurringforthe first time,butitmightbetakenasaprimaryHAdisorderwhenthereisahistory ofsimilarpreviousepisodes.Ontheotherhand,amildtomoderateintensity ofHAdoesnotguaranteeabenigncause.Mostpatientswithbraintumors presentwithHAofmildtomoderateintensitythatmayrespondwelltoanalgesicsinearlystages.
WhataretheaccompanyingsymptomswithHA?
SymptomsthatareassociatedwithHAarekeytodiagnosis.Migraineisa complexdiseasewithmanyassociatedsymptomssuchasnausea,vomiting, andsensitivitytolight,sound,orodor.
Onthecontrary,TTHisfamousforlackofassociatedsymptomsandis thereforeknownasfeaturelessHA.ICHDhasproposedthepresenceof photophobiaorphonophobia(notboth)foradiagnosisofTTH.Nausea orvomitingisnotcompatiblewithTTH,butnauseaofmildseverityis acceptedfordiagnosisofTTH.
TACsarecharacterizedbyatleastonecranialautonomicsymptomipsilateraltotheHAalthoughICHD-3allowsadiagnosisofclusterHAand hemicraniascontinua(twotypesofTACs)intheabsenceofautonomic symptomwhenthereisagitationorrestlessness.
TACs(especiallyclusterHAandparoxysmalhemicranias)andsidelockedmigrainemaymimiceachother.Migrainepatientsmayexperience cranialautonomicsymptomssuchaslacrimation,conjunctivalinjection, facialoreyelidedema,andnasalcongestionorrhinorrheamimicking TAC[40].Migrainefeaturessuchasnausea,vomiting,photophobia,or phonophobiahavealsobeenreportedwithclusterHA[41].Itissometimes difficulttodifferentiateatthe firstglance,buttherearesomereliabledifferentiatingfeatures(Table1.7).
Photophobiaandphonophobiaarenotspecificformigraineandmaybe presentinmanyHAdisorders,includingsomeseriouscausessuchasSAH andmeningitisinadditiontoprimaryHAdisorders.Vomitingismost commonlyassociatedwithmigraine,butintracraniallesionsshouldberuled
Table1.7 Comparingside-lockedmigrainewithclusterHA. FeatureSide-lockedmigraineClusterHA
SexMorefemalesMoremales CircadianrhythmAbsentPresent AutonomicsymptomsMaybepresent(usually bilateral) Prominent(ipsilateral)
PhotophobiaProminentMaybepresent DurationofattackLonger(4 72h)Shorter(< 3h)
Behaviorduringthe attack Restinadark,quiet room Agitationand restlessness
Lateralityof photophobia BilateralUnilateral
outbyclinicaljudgment.Thisisparticularlytrueforvomitingwithoutprecedingnausea(projectilevomiting)orwhenvomitingproceedsHA,which arebothconsideredasred flags.
Tinnitusandtransientvisualobscuration(TVO)mayheraldincreased ICPinapatientwithrecentHA.UnilateralorbilateralTVO,especially withbendingorValsalvamaneuver,maybeasignofincreasedICP,which canbeduetointracraniallesionsorpseudotumorcerebrisyndrome(PTCS). AcutetosubacuteunilateralsevereHAwithipsilateraltransientmonoocularblindnessorHornersyndromeishighlysuggestiveofdissectionof craniocervialarteries.
DoyouhavepremonitorysymptomsbeforetheonsetofHA?
Auraisareversibleneurologicaldisturbancethatmayprecedeoraccompany migraineHA.Itmaylastfrom5minto1h,butitusuallylasts10 30min [42].Prolongedauraisdefinedasauraofmorethan1hourbutlessthana weekandisusuallyintheformofnonvisualsymptoms[43].Auratypically evolvesandfadeswithinminutesandhaspositivefeatures.Visualauraisthe mostcommontype,withpositive,negative,orbothtypesofvisualphenomena.Itusuallyinvolvesbotheyesandissometimesinblackandwhite. Ifitismulticoloredandofashorterduration(usuallylessthan3minutes),an occipitallobeseizureshouldbeconsidered[44].Patientswithmigrainewith auramayexperiencemorethanonetypeofaura.Inthissetting,symptoms usuallyoccurinasequentialorderandarenotsimultaneous(forexample, visualaurafollowedbysomatosensoryaura).