About the Authors
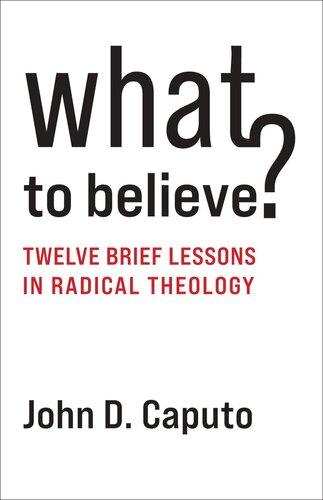
Tania Killian
Tania Killian, BScN, BEd, MEd, CCN, CHSE, began her nursing career at Lakehead University in Thunder Bay, Ontario. Graduating in 1998, she continued her educational pursuits at Lakehead University, subsequently completing a Bachelor and then a Masters of Education. Tania supplemented her studies with practical field experience, spending her summers working Search and Rescue for the Canadian Coast Guard. It was the combination of academics and experiential learning that served to solidify her love for prehospital and emergency care. Tania parlayed this passion into a profession providing essential service as an emergency/trauma nurse throughout the evolution of her career. The student turned teacher in 2002 when Tania became a full-time professor at Seneca College. Now, almost 20 years later, Tania continues to be a valued and respected faculty member of Seneca’s School of Health Sciences. Her college portfolio includes a variety of course curriculum development and delivery. In addition to her classroom leadership, Tania also manages simulation and virtual reality programs for numerous faculties within Seneca College. Within her roles, she has secured several funding initiatives and established and continues to maintain partnerships within the international community to grow numerous projects that enhance student learning.
An advocate of innovation, Tania has advanced cross-disciplinary experiential learning in the various responsibilities she holds at the college. She has served as a Seneca Ambassador internationally and has hosted international delegations at the college to share best practices in nursing studies. Combining her medical training with her love of sports, Tania has added new capacities and ‘personal bests’ to her career. She is proud to have served professionally at several Olympic, Paralympic, Pan Am, and national games. Closer to home, Tania is a member of several Team Ontario sport teams where she has the privilege of working with sector allies to provide high-quality health care to elite athletes.
Tania’s other love is animals, and she is often seen with her loyal dog, Lucy, by her side.
Deborah C. Gray Morris
Deborah C. Gray Morris, RN, BSN, MA, LNC, began her nursing education at Bronx Community College, graduating in 1971. In 1973, Deborah earned a bachelor of science in nursing (BSN) from the City College of the City University of New York, followed by a master (MA) in nursing from New York University in 1978. In 1998, Deborah pursued her interest in the legal aspects of nursing and graduated with certification as a legal nurse consultant from Long Island University’s Legal Nurse Consultant Program in 1999. Deborah has also earned 12 credits from John Jay College of the City University of New York, including credits in criminal justice and forensic science.
Deborah is currently a full professor and the chairperson of the Department of Nursing and Allied Health Sciences at Bronx Community College, where she teaches dosage calculations in the Registered Nursing and Licensed Practical Nursing Programs. Deborah has held the position of chairperson since 2010; first as acting, then elected to the position in 2011. Prior to becoming chairperson, Deborah served as deputy chairperson for 13 years and as course coordinator for Pharmacology Computations. Her second term as
chairperson began in July 2015. Deborah is also a program evaluator for the Accreditation Commission for Education in Nursing (ACEN). Upon request, Deborah provides consultant services to nursing programs in the area of dosage calculation.
Deborah’s interest in dosage calculation started with her career at Bronx Community College of the City University of New York in 1978. Her original position at the college was in the capacity of providing nursing students with tutoring in the area of dosage calculation, which had been identified as an area of difficulty for students. She began with the development of a manual to assist students with the subject matter and later developed a course titled Pharmacology Computations, which was approved through the college governance bodies and is currently a required course for students in the Associate Degree Nursing Program. Deborah’s very first edition of Calculate with Confidence was published in 1994. Calculate with Confidence is currently in its 7th U.S. edition and ranks among the top books published by Elsevier in this area.
Deborah is married.
Reviewers
Jennifer Black, RN, BScN, MN Professor & Coordinator
Practical Nursing Program
Fanshawe College—Woodstock/Oxford Regional Campus Woodstock, Ontario
Julie Duff Cloutier, RN, BScN, MSc, PhD(c)
Assistant Professor School of Nursing
Laurentian University
Sudbury, Ontario
Michelle Earl, BSN, PID
Team Leader and Placement Coordinator
Practical Nursing
Sprott Shaw College—Kelowna Campus; Clinical Nursing Instructor University of British Columbia—Okanagan Campus
Kelowna, British Columbia
Andrea Gretchev, RN, BScN, MN, CCNE
BSN Curriculum Coordinator
Douglas College, Health Sciences
Coquitlam, British Columbia
(Amy) Phuong Thi Dieu Hoang, BSc Mathematics, BEd Professor
Department of Mathematics
Niagara College
Welland, Ontario
Kelly Kidd, RN, BScN, MN Professor Nursing Studies
Coordinator Year 1 Practical Nursing Program
Coordinator Clinical Education
Health and Community Studies
Algonquin College
Pembroke, Ontario
Allison McFadden-Squire, BScN, RN, MEd(c)
Curriculum Lead
Practical Nurse Program
NorQuest College Edmonton, Alberta
Dennise Morgan, RN, BScN, MN, CON(c)
Clinical Supervisor
Seneca-York Collaborative BScN Program
Practical Nursing Program
Seneca College of Applied Arts and Technology Department of Health Sciences Toronto, Ontario
Pammla Petrucka, RN, PhD Professor
College of Nursing University of Saskatchewan Saskatoon, Saskatchewan
Crystal Schauerte, BscN, MscN
Nursing Professor
Department of Nursing
Algonquin College Ottawa, Ontario
Ruth Swart, EdD, MHS, RN, BN, BSc
Senior Instructor
Faculty of Nursing University of Calgary Calgary, Alberta
Selena Talbot, RN, MAEd Instructor III
Faculty of Nursing University of Regina Regina, Saskatchewan
Andrea Tannahill, RN, MSN
Nursing Instructor
School of Health Sciences
University of Alberta BScN Collaborative Program at Red Deer College Red Deer, Alberta
Barbara Thompson, RN, BScN, MScN Professor of Nursing, Coordinator Practical Nursing Program
Health Programs
Sault College
Sault Ste. Marie, Ontario
Lorna Walsh, BN, MEd, RN
Nurse Educator/Year 1 and 2 Coordinator
Centre for Nursing Studies
Memorial University of Newfoundland St. John’s, Newfoundland
With special thanks to Terri Burrell RN, BScN, MSN Faculty
Saskatchewan Collaborative Bachelor of Science in Nursing (SCBScN)
Saskatchewan Polytechnic—Regina Campus Regina, Saskatchewan
Preface to the Instructor
The culture of safety continues to be a priority in the delivery of health care. To advance patient safety and its importance in health care delivery worldwide, several organizations continue to promote patient safety, which includes an emphasis on improving safety in medication administration. Canadian organizations include Health Canada, the Canadian Institute for Health Information (CIHI), the Institute for Safe Medication Practices Canada (ISMP Canada), and the Canadian Patient Safety Institute (CPSI). These organizations also collaborate on the Canadian Medication Incident Reporting and Prevention System (CMIRPS). This pan-Canadian program encourages reporting, sharing, and learning about medication incidents in order to help reduce their reoccurrence and create a safer health care system.
The second Canadian edition of Gray Morris’s Calculate with Confidence continues to emphasize safety in medication administration and is written to meet the needs of current and future practitioners of health care at any level. This book can be used as a resource for any education program or practice setting that involves dosage calculation and medication administration by health care providers.
Gray Morris’s Calculate with Confidence, Second Canadian Edition, primarily uses the metric system in calculating dosages, but it presents examples that incorporate imperial system (household, apothecary) measurements where applicable. Specifically, you will see the conversion of pounds to kilograms in some examples because weight is still sometimes measured in pounds in the community at large. Therefore it is prudent to include imperial units of measurement in this book.
The second Canadian edition of Gray Morris’s Calculate with Confidence illustrates the standard methods of dosage calculation: the ratio and proportion method, the formula method, and the dimensional analysis method. With the inclusion of all three, instructors have the freedom to decide which method(s) best suit their program, and students have the same freedom to choose the method that facilitates correct dosage calculations.
This second Canadian edition responds to evidence-informed practices as they relate to safe medication practices at all levels. Highlights include best practices for the labelling, dispensing, preparing, and administering of medications. With the nursing student in mind, emphasis is placed on critical thinking and clinical reasoning in the prevention of medication errors. Principles of competence and safety are integrated throughout.
Answers to the Practice Problems include rationales to enhance the understanding of principles. In response to the increased need for competency in basic math as an essential prerequisite for dosage calculation, many Practice Problems are included in the basic math section.
The once controversial use of calculators is now a more accepted practise, and they are used in many nursing exams, including when writing licensure exams such as the NCLEX. Critical care areas in some health care institutions have policies that require the use of calculators to verify calculations to avoid medication errors. A basic calculator is usually sufficient for dosage calculations. Calculator use is not encouraged in the basic math section of this book due to the expectation that students should be able to perform calculations proficiently and independently without their use.
Despite decreased errors in calculating medication dosages due to the availability of better technology, health care providers must continue to use sound clinical reasoning in problem solving to minimize the risk to patient safety.
The second Canadian edition of Gray Morris’s Calculate with Confidence embodies all the standards of nursing practice. It clearly delineates the nurse’s responsibility in medication practices, including accurate dosage calculation to optimize safe patient outcomes.
Organization of Content
The second Canadian edition is organized in a progression from simple topics to more complex ones, making content relevant to the needs of students and using realistic Practice Problems and Clinical Reasoning Questions to enhance learning and make material clinically applicable.
The 23 chapters are arranged into 5 units.
Unit One includes Chapters 1 through 4. This unit provides a review of basic math skills, including fractions, decimals, ratio and proportion, and percentages. A pre-test and posttest are included. This unit allows students to determine their weaknesses and strengths in math and provides a review. Academic institutions using this book may use these units as independent study for students to review basic math concepts before venturing on to actual dosage calculations.
Unit Two includes Chapters 5 through 7. Chapter 5 introduces students to the metric and imperial (household, apothecary) systems of measurement. Canada’s health care providers use the metric system. However, some units of household measurement are discussed because of their continued use, albeit limited. These measurements are pound, ounce, teaspoon, tablespoon, and cup. In Chapter 6, students learn to convert measurements. Chapter 7 presents conversions relating to temperature, length, weight, and international time.
Unit Three includes Chapters 8 through 14. This unit provides essential information that is needed as a foundation for dosage calculation and safe medication administration. Chapter 8 includes an expanded discussion of medication errors, routes of medication administration, equipment used in medication administration, the rights of medication administration, and the nursing role in preventing medication errors. Chapter 9 presents the abbreviations used in medication administration and discusses how to interpret medication orders. Chapter 10 introduces students to medication administration records and the various medication distribution systems. Chapter 11 provides students with the skills necessary to read medication labels to calculate dosages. Chapters 12 through 14 introduce students to the various methods used for dosage calculation followed by Practice Problems illustrating each method.
Unit Four includes Chapters 15 through 18. In Chapter 15, students learn the principles and calculations related to oral medications (solid and liquids). In Chapter 16, students learn about the various types of syringes and skills needed for calculating injectable medications. Chapter 17 introduces students to the calculations associated with reconstituting solutions for injectable and noninjectable medications. Calculations associated with the preparation of noninjectable solutions such as nutritional feedings include determining the strength of a solution and determining the amount of the desired solution. Chapter 18 introduces students to insulin types, insulin equipment, and Canadian Diabetes Association 2018 Clinical Practice Guidelines for the prevention and management of diabetes in Canada.
Unit Five includes Chapters 19 through 23. Chapters 19 and 20 provide students with a discussion of intravenous (IV) fluids and associated calculations related to IV therapy. The recalculation of IV flow rate includes an alternative method to determining the percentage of variation. IV labels have been added throughout the chapter, with a discussion of additives to IV solutions. Chapter 21 focuses on heparin and uses the new heparin labelling. Sample heparin weight-based protocols are used to adjust IV heparin based on activated partial thromboplastin time (aPTT). Chapter 22 discusses the principles of calculating pediatric and adult dosages, with emphasis on calculating dosages based on body weight and body surface area as well as verifying the safety of dosages. Chapter 23 provides students with the skills necessary to calculate critical care IV medications. Determining the titration of IV flow rates for titrated medications includes developing a titration table.
Safety Alerts, Practice Problems, Clinical Reasoning scenarios, and Points to Remember are included throughout the book. A Comprehensive Post-Test is included at the end of the book and covers all 23 chapters.
Features of the Second Canadian Edition
• Objectives at the beginning of each chapter to emphasize content to be mastered.
• Canadian medication labels.
• Integration of ISMP Canada recommendations in the book to alert students to the importance of patient safety and reducing medication errors.
• Content related to preventing medication errors, such as the use of Tall Man Lettering, verification of the rights of medication administration, and an examination of the nursing role in preventing medication errors.
• Discussions on preventing medication errors in chapters dealing with high-alert medications (heparin and insulin).
• An up-to-date insulin chapter that reflects the Canadian Diabetes Association 2018 Clinical Practice Guidelines on insulin therapy, which features basal + bolus + correction insulin dosing as well as IV insulin therapy.
• An IV chapter, including IV labels and a discussion of IV additives. Recalculation of IV therapy includes an alternative approach to determining the variation of change using percentages.
• Safety Alert boxes that direct students to common errors and how to avoid them.
• Clinical Reasoning questions in Chapters 15 to 22 to allow students to critically think through more complex questions.
• Inclusion of heparin weight-based protocol and problems on adjusting the flow rate based on PTT.
• Critical care discussion on IV flow rates for titrated medications, including how to develop a titration table.
• Calculation of fluid resuscitation for patients with burns as well as daily pediatric fluid maintenance.
• Practice Problems and Chapter Review problems in each chapter.
• An Answer Key at the end of each chapter to provide immediate feedback on solutions to problems.
• NEW! A-Z medication index referencing page numbers where the drug labels can be found.
Ancillaries
Evolve Resources for Gray Morris’s Calculate with Confidence, Second Canadian Edition, are available to enhance student instruction. This online resource can be found at http:// evolve.elsevier.com/Canada/GrayMorris/. It corresponds with the chapters of the main book and includes the following:
• TEACH for Nurses
• Test Bank
• PowerPoint Slides
• Image Collection of Drug Labels
• Answer Key from Textbook
• Student Review Questions
• NEW! Tips for Clinical Practice easy reference
• NEW! Next Generation NCLEX Case Studies (both generic and book-specific)
• NEW! Elsevier’s Interactive Drug Calculation Application, version 1: This interactive drug calculation application provides hands-on, interactive practice for the user to master drug calculations. Users can select the mode (Study, Exam, or Comprehensive Exam) and then the category for study and exam modes. There are eight categories that cover the main drug calculation topics. Users are also able to select the number of problems they want to complete and their preferred drug calculation method. A calculator is available for easy access within any mode, and the application also provides history of the work done by the user. There are 750 practice problems in this application.
We hope that this book provides clear concept review, practice questions, detailed explanations and clinical reasoning questions to help you master the dosage calculations you need to correctly administer medications safely.
This book is not only for the beginner health care provider but is meant to also benefit the experienced health care provider as a useful reference.
Tania Killian
Acknowledgements
First and foremost, I must thank Theresa Fitzgerald for guiding me throughout this process. Without her patience and continued encouragement, I would not have completed this book.
Thank you to Roberta A. Spinosa-Millman and Rachel McMullen of Elsevier for giving me the opportunity to write this book and their support throughout the process.
I wish to acknowledge the valuable contributions of my reviewers. Thank you for your notes regarding the improvement of quality, coherence, and presentation of the content of the book. I am grateful for the combined insight they provided. I would also like to thank Marcia Brown for her work on the first edition.
And most importantly, to my family, friends, colleagues, and the “Coffee Club” who inspired me to take a chance at writing.
Tania Killian
UNIT ONE Math Review 1
PRE-TEST 2
1 Fractions, 6
Types of Fractions, 7
Converting Fractions, 8
Comparing Fractions, 8
Reducing Fractions, 10
Adding Fractions, 11
Subtracting Fractions, 12
Multiplying Fractions, 14
Dividing Fractions, 15
2 Decimals, 23
Reading and Writing Decimals, 24
Comparing the Value of Decimals, 26
Adding and Subtracting Decimals, 27
Multiplying Decimals, 29
Dividing Decimals, 31
Rounding Off Decimals, 32
Changing Fractions to Decimals, 34
Changing Decimals to Fractions, 34
3 Ratio and Proportion, 40
Ratios, 40
Proportions, 41
Solving for x in Ratio and Proportion, 42
Applying Ratio and Proportion to Dosage Calculation, 44
4 Percentages, 51
Percentage Measures, 51
Converting Percentages to Fractions, Decimals, and Ratios, 52
Converting Fractions, Decimals, and Ratios to Percentages, 54
Comparing Percentages and Ratios, 56
Determining the Percentage of a Quantity, 57
Determining What Percentage One Number Is of Another, 57
Calculating the Percentage of Change, 59
UNIT TWO Systems of Measurement 69
5 Standardizing Measurement Systems, 70
Metric System, 71
Rules of the Metric System, 73
Units of Measurement, 74
Conversions Between Metric Units, 75
Apothecary System (Imperial), 77
Roman Numeral System (Imperial), 78
Household System (Imperial), 78
Other Measurements Used in Dosage Calculation, 79
6 Converting Within and Between Systems, 85
Equivalents Among Metric and Household Systems, 85
Converting, 85
Methods of Converting, 86
Converting Within the Same System, 89
Converting Between Systems, 91
Calculating Intake and Output, 93
7 Additional Conversions Useful in the Health Care Setting, 103
Converting Between Celsius and Fahrenheit, 103
Converting Measures of Length, 106
Converting Between Units of Weight, 107
Converting Between Traditional and Military (International) Time, 109
Calculating Completion Times, 111
UNIT THREE Methods of Administration and Calculation 117
8 Medication Administration, 118
Medication Errors, 118
Critical Thinking and Medication Administration, 120 Factors That Influence Medication Dosages and Action, 121
Special Considerations for Older Adults, 121
The Rights of Medication Administration, 122
Medication Reconciliation, 127
Routes of Medication Administration, 129
Equipment Used for Medication Administration, 130
9 Understanding and Interpreting Medication Orders, 136
Verbal Orders, 136
Transcription of Medication Orders, 137
Writing a Medication Order, 139
Components of a Medication Order, 139
Interpreting a Medication Order, 143
10 Medication Administration Records and Drug Distribution Systems, 151
Medication Orders, 151
Medication Administration Record, 151
Essential Components of a Medication Administration Record, 153 Documentation of Medication Administration, 154 Computers and Medication Administration, 156 Medication Distribution Systems, 156
Advantages and Disadvantages of Technology, 159
11
Reading Medication Labels, 163
Reading Medication Labels, 163
12 Dosage Calculation Using the Ratio and Proportion Method, 203 Using Ratio and Proportion to Calculate Dosages, 203
13 Dosage Calculation Using the Formula Method, 237 Formula for Calculating Dosages, 237 Applying the Formula, 238
14 Dosage Calculation Using the Dimensional Analysis Method, 263
Understanding the Basics of Dimensional Analysis, 263 Dosage Calculation Using Dimensional Analysis, 266
UNIT FOUR Oral and Parenteral Dosage Forms and Insulin 287
15 Oral Medications, 288
Forms of Solid Medication, 288
Calculating Dosages of Tablets and Capsules, 292 Calculating Dosages of Oral Liquids, 306 Measuring Oral Liquids, 307
16 Parenteral Medications, 348
Packaging of Parenteral Medications, 348 Syringes, 351
Reading Parenteral Labels, 360
Calculating Parenteral Dosages, 370 Calculating Injectable Medications According to the Syringe, 371
Calculating Dosages for Medications in Units, 376
Mixing Medications in the Same Syringe, 378
17 Reconstitution of Solutions, 420
Basic Principles of Reconstitution, 421
Reconstituting Medications With More Than One Direction for Mixing (Multiple Strength), 430
Reconstituting Medications From Package Insert Directions for Different Routes of Administration, 433
Medication Labels With Instructions to “See Accompanying Literature” (Package Insert) for Reconstitution and Administration, 433
Calculating Dosages of Reconstituted Medications, 435
Reconstituting Noninjectable Solutions, 438
18 Insulin, 473
Labels, 474
Types of Insulin and Their Action, 475
Appearance of Insulin, 479
Insulin Administration Methods, 479
Insulin Orders, 485
Preparing a Single Dose of Insulin in an Insulin Syringe, 488
Measuring Two Types of Insulin in the Same Syringe, 489
Intravenous Insulin, 492
Calculating an Intravenous Insulin Infusion, 492
Hypoglycemia, 493
UNIT
FIVE
Intravenous and Heparin Calculations, Pediatric Dosage Calculations, and Critical Care Calculations 509
19 Intravenous Solutions and Equipment, 510
Intravenous Delivery Methods, 510
Intravenous Solutions, 511
Administration of Intravenous Solutions, 516
20 Intravenous Calculations, 528
Intravenous Flow Rate Calculation, 528
Calculating Flow Rates for Infusion Pumps in Millilitres per Hour, 528
Calculating Flow Rates in Drops per Minute, 532
Intravenous Tubing, 532
Calculating Flow Rates in Drops per Minute
Using a Formula, 535
Determining Infusion Time and Volume, 545
Recalculating an Intravenous Flow Rate, 547
Charting Intravenous Therapy, 550
Labelling Solution Bags, 550
Administration of Medications by Intravenous Push, 550
21 Heparin Calculations, 562
Heparin, 562
Heparin Errors, 562
Heparin Dosage Strengths, 563
Reading Heparin Labels, 564
Calculating Subcutaneous Heparin Dosages, 565
Calculating Intravenous Heparin Dosages, 566
Calculating Heparin Dosages Based on Weight, 568
22 Pediatric and Adult Dosage Calculations Based on Weight, 590
Principles of Pediatric Dosage Calculation, 591
Calculating Dosages Based on Body Weight, 592
Calculating Adult Dosages Based on Body Weight, 599
Calculating Pediatric Dosages Using Body Surface Area, 604
Calculating Body Surface Area Using a Formula, 607
Calculating Dosages Based on Body Surface Area, 609
Fluid Resuscitation After a Burn Injury, 612
Intravenous Therapy and Children, 616
Calculating Pediatric Intravenous Fluid Maintenance, 618
Calculating Intravenous Medications by Burette, 619
Determining Whether a Pediatric Intravenous Dosage Is Safe, 622
Pediatric Oral and Parenteral Medications, 624
23 Critical Care Calculations, 653
Calculating the Intravenous Flow Rate in Millilitres per Hour, 654
Calculating Critical Care Dosages per Hour or per Minute, 655
Medications Ordered in Milligrams per Minute, 656
Calculating Dosages Based on Micrograms per Kilogram per Minute, 657
Intravenous Flow Rates for Titrated Medications, 658
Developing a Titration Table, 660
COMPREHENSIVE POST-TEST 682
Appendix A: Arabic Equivalents for Roman Numerals, 705
Appendix B: Diabetes Management Record: Subcutaneous Insulin, 706
References, 709
Drug Label Credits, 711
Drug Index, 712
Index, 717
CHAPTER 1 Fractions
Objectives
After reviewing this chapter, you should be able to:
1. Compare the size of fractions
2. Add fractions
3. Subtract fractions
4. Divide fractions
5. Multiply fractions
6. Reduce fractions to lowest terms
Health care providers need to have an understanding of fractions. Fractions may be seen in medical orders, patient records, prescriptions, documentation relating to care given to patients, and literature related to health care. Nurses often encounter fractions in dosage calculation.
Somemethods of solving dosage calculations rely on expressing relationships in a fraction format. Therefore, proficiency with fractions can be beneficial in a variety of situations.
A fraction is used to indicate a part of a whole number (Figure 1-1). It is a division of a whole into units or parts (Figure 1-2). A fraction is composed of two parts: an upper number referred to as the numerator and a lower number called the denominator. The numerator and denominator are separated by a horizontal line. A fraction may also be read as the numerator divided by the denominator.
Example: 1 2 is a whole divided into two equal parts.
Numerator
Denominator
how many parts of the whole are consid : e ered how many equal parts the whole is divided into
Example: In the fraction 5 6 , the whole is divided into 6 equal parts (denominator), and five parts (numerator) are considered.
5 6 = 5 parts of 6 parts, or 5 6 of the whole.
The fraction 5 6 may also be read as 5 divided by 6.
Figure 1-1 Diagram representing fractions of a whole. Five parts shaded out of the six parts represent: 5 6 Numerator Denominator .
Types of Fractions
Proper Fraction: Numerator is less than the denominator, and the fraction has a value of less than 1.
Examples: 1 8 5 6 7 8 1 150 ,, ,
Improper Fraction: Numerator is larger than, or equal to, the denominator, and the fraction has a value of 1 or greater than 1.
Examples: 3 2 7 5 300 150 4 4 ,, ,
Mixed Number: Whole number and a proper fraction in which the total value of the mixed number is greater than 1.
Examples: 35 925 1 3 1 8 1 6 7 8 ,, ,
Complex Fraction: Numerator, denominator, or both are fractions. The value may be less than, greater than, or equal to 1.
Examples: 3 2 2 1 2 1 2 1 3 1 2 1 4 1 150 ,, ,
Whole Numbers: Have an unexpressed denominator of one (1).
Examples:
Figure 1-2 Fraction pie charts.
Converting Fractions
An improper fraction can be changed to a mixed number or whole number by dividing the numerator by the denominator. If there is a remainder, that number is placed over the denominator, and the answer is reduced to lowest terms.
A mixed number can be changed to an improper fraction by multiplying the whole number by the denominator, adding it to the numerator, and placing the sum over the denominator.
Comparing Fractions
Comparing the size of fractions is important in the administration of medications. It helps the new practitioner learn the value of medication dosages early on. Fractions can be compared if the numerators are the same by comparing the denominators or if the denominators are the same by comparing the numerators. These rules are presented in Box 1-1.
BOX 1-1 Rules for Comparing the Size of Fractions
Here are some basic rules to keep in mind when comparing fractions.
1. If the numerators are the same, the fraction with the smaller denominator has the greater value.
Example: 1 2 is larger than 1 3
Example: 1 150 is larger than 1 300
2. If the denominators are the same, the fraction with the larger numerator has the greater value.
Example: 3 4 is larger than 1 4
Example: 3 100 is larger than 1 100
Two or more fractions with different denominators can be compared by changing both fractions to fractions with the same denominator (see Box 1-1). This is done by finding the lowest common denominator (LCD), or the lowest number evenly divisible by the denominators of the fractions being compared.
Example: Which is larger, 3 4 or 4 5 ?
Solution: The LCD is 20, because it is the smallest number that can be divided by both denominators evenly. Change each fraction to the same terms by dividing the LCD by the denominator and multiplying that answer by the numerator. The answer obtained from this is the new numerator. The numerators are then placed over the LCD.
For the fraction 3 4 , 20 ÷ 4 = 5; 5 × 3 = 15; therefore 3 4 becomes 15 20
For the fraction 4 5 , 20 ÷ 5 = 4; 4 × 4 = 16; therefore 4 5 becomes 16 20 Therefore () 4 5 16 20 is larger than () 3 4 15 20
Box 1-2 presents fundamental rules of fractions.