CONTRIBUTORS
Douglas G. Adler, MD, FACG, AGAF, FASGE
Professor of Medicine
Director of Therapeutic Endoscopy
Director of GI Fellowship Program
Gastroenterology and Hepatology
University of Utah School of Medicine
Huntsman Cancer Center
Salt Lake City, Utah
Sushil K. Ahlawat, MD, FACP, FASGE, AGAF
Associate Professor of Medicine
Director of Endoscopy
Program Director, Gastroenterology and Hepatology Fellowship
Program Director, Advanced Endoscopy Fellowship
Division of Gastroenterology and Hepatology
Rutgers New Jersey Medical School
Newark, New Jersey
Jawad Ahmad, MD, FRCP, FAASLD
Professor of Medicine
Division of Liver Diseases
Icahn School of Medicine at Mount Sinai
New York, New York
Firas H. Al-Kawas, MD
Professor of Medicine
Division of Gastroenterology and Hepatology
Johns Hopkins University
Baltimore, Maryland
Director of Johns Hopkins Endoscopy Program
Sibley Memorial Hospital
Washington, District of Columbia
Michelle A. Anderson, MD
Associate Professor of Medicine
Taubman Center
University of Michigan
Ann Arbor, Michigan
Everson Luiz de Almeida Artifon, MD, PhD, FASGE
Coordinator of Pancreatic Biliary Endoscopy Unit
GI Endoscopy Service
Hospital de Clinicas of the University of Sao Paulo
Associate Professor of Surgery
University of Sao Paulo
Sao Paulo, Brazil
João Guilherme Guerra de Andrade
Lima Cabral, MD
Endoscopist
Advanced Endoscopy Unit
A.C. Camargo Cancer Center
São Paulo, Brazil
John Baillie, MD
Professor of Medicine
Chief of Endoscopy
Virginia Commonwealth University School of Medicine
Richmond, Virginia
Rupa Banerjee, MD, DTM
Consultant
Gastroenterologist
Asian Institute of Gastroenterology
Hyderabad, India
Todd H. Baron, MD, FASGE
Professor of Medicine
Division of Gastroenterology and Hepatology
University of North Carolina School of Medicine
Chapel Hill, North Carolina
Omer Basar, MD
Gastrointestinal Unit
Pancreas Biliary Center
Massachusetts General Hospital
Boston, Massachusetts
Professor of Medicine
Department of Gastroenterology
Hacettepe University Medical School
Ankara, Turkey
Petros C. Benias, MD
Director of Endoscopic Surgery
Division of Gastroenterology
Northwell Health System
Hofstra Zucker School of Medicine
Manhasset, New York
Ivo Boškoski, MD, PhD
Digestive Endoscopy Unit
Cattolic University of Rome
Rome, Italy
Michael J. Bourke, MBBS, FRACP
Clinical Professor of Medicine
Director of Endoscopy
Gastroenterology and Hepatology
Westmead Hospital
Sydney, Australia
Brian C. Brauer, MD
Associate Professor of Medicine
University of Colorado School of Medicine
Aurora, Colorado
William R. Brugge, MD
Professor of Medicine
Harvard Medical School
Director of Gastrointestinal Unit
Pancreas Biliary Center
Massachusetts General Hospital
Boston, Massachusetts
Jonathan M. Buscaglia, MD
Associate Professor and Division Chief
Gastroenterology and Hepatology
Stony Brook University School of Medicine
Stony Brook, New York
David L. Carr-Locke, MD, FRCP, FASGE, FACG
Clinical Director
Center for Advanced Digestive Care
Division of Gastroenterology and Hepatology
Weill Cornell Medicine
Cornell University
New York, New York
Prabhleen Chahal, MD
Physician
Department of Gastroenterology and Hepatology
Cleveland Clinic
Cleveland, Ohio
Sujievvan Chandran, MBBS, FRACP
Therapeutic Endoscopy Fellow
Gastroenterology
St. Michaels’s Hospital
Toronto, Ontario, Canada
Yen-I Chen, MD
Assistant Professor of Medicine
Division of Gastroenterology and Hepatology
McGill University Health Center
Montreal, Quebec, Canada
Anthony J. Choi, MD
Resident Physician
Department of Medicine
Weill Cornell Medicine
Cornell University
New York, New York
Jonah Cohen, MD
Clinical Fellow in Advanced Endoscopy
Division of Gastroenterology
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Guido Costamagna, MD, FACG
Digestive Endoscopy Unit
Catholic University
Gemelli University Hospital
Rome, Italy
Chair of Digestive Endoscopy
USIAS Strasbourg University Strasbourg, France
Gregory A. Coté, MD
Associate Professor of Medicine
Division of Gastroenterology and Hepatology
Department of Medicine
Medical University of South Carolina Charleston, South Carolina
Peter Cotton, MD, FRCS, FRCP
Professor of Medicine
Digestive Disease Center
Medical University of South Carolina Charleston, South Carolina
Koushik K. Das, MD
Assistant Professor of Medicine Division of Gastroenterology
Washington University School of Medicine St. Louis, Missouri
Jacques Devière, MD, PhD
Professor of Medicine
Head
Department of Gastroenterology, Hepatology, and Digestive Oncology
CUB Erasme
Université Libre de Bruxelles Brussels, Belgium
Steven A. Edmundowicz, MD
Professor of Medicine
University of Colorado School of Medicine Aurora, Colorado
Ihab I. El Hajj, MD, MPH
Assistant Professor of Medicine
Division of Gastroenterology and Hepatology
Indiana University Indianapolis, Indiana
Douglas O. Faigel, MD, FACG, FASGE, AGAF
Professor of Medicine
Department of Gastroenterology and Hepatology
Mayo Clinic Scottsdale, Arizona
Pietro Familiari, MD, PhD
Fondazione Policlinico Gemelli
Digestive Endoscopy Unit
Rome, Italy
Paul Fockens, MD, PhD, FASGE
Professor and Chair
Gastroenterology and Hepatology
Academic Medical Center Amsterdam, Netherland
Evan L. Fogel, MD
Professor of Medicine
Division of Gastroenterology and Hepatology
Indiana University School of Medicine Indianapolis, Indiana
Victor L. Fox, MD
Associate Professor of Pediatrics
Harvard Medical School
Director of GI Procedure and Endoscopy Unit
Division of Gastroenterology, Hepatology, and Nutrition
Boston Children’s Hospital Boston, Massachusetts
Martin L. Freeman, MD Professor of Medicine
Division of Gastroenterology, Hepatology, and Nutrition
University of Minnesota Minneapolis, Minnesota
S. Ian Gan, MD
Department of Gastroenterology
Virginia Mason Medical Center Seattle, Washington
Andres Gelrud, MD, MMSc, FASGE
Director
Pancreatic Disease Center
Miami Cancer Institute Miami, Florida
Gregory G. Ginsberg, MD
Professor of Medicine
Department of Medicine
Division of Gastroenterology
Hospital of the University of Pennsylvania Philadelphia, Pennsylvania
Michael Gluck, MD
Past Chief of Medicine
Department of Gastroenterology
Virginia Mason Medical Center
Seattle, Washington
Khean-Lee Goh, MBBS, FRCP, MD Professor
Gastroenterology and Medicine
University of Malaya
Kuala Lumpur, Malaysia
Robert H. Hawes
Professor of Medicine
University of Central Florida College of Medicine
Medical Director
Florida Hospital Institute for Minimally Invasive Therapy
Center for Interventional Endoscopy
Florida Hospital Orlando Orlando, Florida
Jennifer T. Higa, MD
Advanced Endoscopy Fellow
Department of Gastroenterology
Virginia Mason Medical Center Seattle, Washington
Jordan D. Holmes, MD
Gastroenterologist
Iowa Digestive Disease Center Clive, Iowa
Shayan Irani, MBBS, MD
Department of Gastroenterology
Virginia Mason Medical Center Seattle, Washington
Takao Itoi, MD, PhD, FASGE, FACG Professor and Chair
Department of Gastroenterology and Hepatology
Tokyo Medical University
Tokyo, Japan
Priya A. Jamidar, MD Professor of Medicine
Director of Endoscopy
Section of Digestive Diseases
Yale University
New Haven, Connecticut
Michel Kahaleh, MD
Professor of Medicine
Division of Gastroenterology and Hepatology
Department of Medicine
Weill Cornell Medicine
Cornell University
New York, New York
Anthony N. Kalloo, MD
The Moses and Helen Golden Paulson Professor of Gastroenterology
Director of Division of Gastroenterology and Hepatology
The Johns Hopkins Hospital Baltimore, Maryland
Mouen A. Khashab, MD
Director of Therapeutic Endoscopy
Associate Professor of Medicine
Department of Gastroenterology and Hepatology
The Johns Hopkins Hospital Baltimore, Maryland
Michael L. Kochman, MD
Wilmott Family Professor of Medicine
Division of Gastroenterology
Department of Medicine
Perelman School of Medicine
University of Pennsylvania Philadelphia, Pennsylvania
Tadashi Kodama, MD, PhD
Advisor
Department of Gastroenterology
Iwasaki Hospital
Mitoyo City, Kagawa, Japan
Andrew Korman, MD
Division of Gastroenterology and Hepatology
Saint Peter’s University Hospital New Brunswick, New Jersey
Paul Kortan, MD, FRCPC, FASGE, AGAF
Department of Medicine
St. Michael’s Hospital University of Toronto Toronto, Ontario, Canada
Tatsuya Koshitani, MD, PhD
Director of Department of Gastroenterology
Japan Community Healthcare Organization
Kobe Central Hospital Kobe City, Hyogo, Japan
Richard A. Kozarek, MD, FASGE
Executive Director
Digestive Disease Institute
Department of Gastroenterology
Virginia Mason Medical Center
Seattle, Washington
Michael Larsen, MD
Gastroenterologist
Digestive Disease Institute
Virginia Mason Medical Center
Seattle, Washington
James Y.W. Lau, MD
Chairman and Yao Ling Sun Professor of Surgery
The Chinese University of Hong Kong
Shatin, Hong Kong, China
Ryan Law, DO
Clinical Lecturer
Division of Gastroenterology
University of Michigan
Ann Arbor, Michigan
Glen Lehman, MD
Professor of Medicine
Division of Gastroenterology
Department of Medicine
Indiana University
Indianapolis, Indiana
Joseph W. Leung, MD, FRCP, FACP, MACG, FASGE
Mr. and Mrs. C.W. Law Professor of Medicine
Division of Gastroenterology and Hepatology
University of California Davis School of Medicine
Sacramento, California
Section Chief of Gastroenterology
Veterans Affairs Northern California Health Care System
Mather, California
Dario Ligresti, MD
Endoscopy Service
Department of Diagnostic and Therapeutic Services
IRCCS ISMETT (Instituto Mediterraneo per i Trapianti e Terapie ad Alta Specializzazione)
Palermo, Italy
Eugene Lin, MD
Attending Radiologist
Virginia Mason Medical Center
Seattle, Washington
Simon K. Lo, MD, FACP
Director of Endoscopy
Head of Pancreatic Diseases Program
Division of Digestive Diseases and Hepatology
Cedars-Sinai Medical Center
Clinical Professor of Medicine
David Geffen School of Medicine at UCLA
Los Angeles, California
Michael X. Ma, MBBS, FRACP
Advanced Endoscopy Fellow
Gastroenterology and Hepatology
Westmead Hospital
Sydney, Australia
John T. Maple, DO
Associate Professor of Medicine
Division of Digestive Diseases and Nutrition
University of Oklahoma
Oklahoma City, Oklahoma
Alberto Mariani, MD
Pancreato-Biliary Endoscopy and Endosonography Division
Pancreas Translational and Clinical Research Center
San Raffaele Scientific Institute
Vita Salute San Raffaele University
Via Olgettina
Milan, Italy
Gary May, MD, FRCPC, FASGE
Division of Gastroenterology
Department of Medicine
The Center of Advanced Therapeutic Endoscopy and Endoscopic Oncology
St. Michael’s Hospital
University of Toronto Faculty of Medicine
Toronto, Ontario, Canada
Lee McHenry, MD
Professor of Medicine
Division of Gastroenterology
Department of Medicine
Indiana University
Indianapolis, Indiana
Meir Mizrahi, MD
Director of Advanced Endoscopy
Internal Medicine
Division of Gastroenterology
University of South Alabama College of Medicine
Mobile, Alabama
Rawad Mounzer, MD
Assistant Professor of Medicine
Digestive Institute
Banner-University Medical Center
University of Arizona
Phoenix, Arizona
Thiruvengadam Muniraj, MD, PhD, MRCP(UK)
Assistant Professor of Medicine
Director of Yale Center for Pancreatitis
Section of Digestive Diseases
Yale University School of Medicine
New Haven, Connecticut
Horst Neuhaus, MD
Professor of Medicine
Chief of the Department of Internal Medicine
Evangelisches Krankenhaus Düsseldorf Düsseldorf, Germany
Ian D. Norton, MBBS, PhD
Associate Professor Department of Gastroenterology
Royal North Shore Hospital Sydney, Australia
Manuel Perez-Miranda, MD, PhD
Head of Gastroenterology and Hepatology
Hospital Universitario Rio Hortega
Associate Professor of Medicine
Valladolid University Medical School Valladolid, Spain
Bret T. Petersen, MD Professor of Medicine
Department of Gastroenterology and Hepatology
Mayo Clinic Rochester, Minnesota
Douglas Pleskow, MD
Associate Clinical Professor Department of Medicine
Harvard Medical School
Chief of Clinical Gastroenterology
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Tugrul Purnak, MD
Associate Professor of Medicine Gastroenterology and Hepatology
Hacettepe University Medical School Ankara, Turkey
G. Venkat Rao, MS, MAMS, FRCS
Director and Chief of Gastrointestinal and Minimally Invasive Surgery
Asian Institute of Gastroenterology Hyderabad, India
Anthony Razzak, MD Gastroenterologist
Oregon Clinic
Portland, Oregon
D. Nageshwar Reddy, MBBS, MD, DM Director and Chief Gastroenterologist
Asian Institute of Gastroenterology Hyderabad, India
Andrew S. Ross, MD
Section Head of Gastroenterology
Medical Director
Therapeutic Endoscopy Center of Excellence
Virginia Mason Medical Center
Seattle, Washington
Alexander M. Sarkisian, MD
Resident Physician
Internal Medicine
Tulane University School of Medicine
New Orleans, Louisiana
Beth Schueler, PhD
Professor of Medical Physics
Department of Radiology
Mayo Clinic
Rochester, Minnesota
Dong Wan Seo, MD, PhD
Professor Gastroenterology
University of Ulsan College of Medicine
Asan Medical Center
Seoul, South Korea
Raj J. Shah, MD, FASGE, AGAF
Professor of Medicine
Division of Gastroenterology
University of Colorado School of Medicine
Director of Pancreaticobiliary Endoscopy
Division of Gastroenterology
University of Colorado Anschutz Medical Campus
Aurora, Colorado
Reem Z. Sharaiha, MD, MSc
Assistant Professor of Medicine
Division of Gastroenterology and Hepatology
Weill Cornell Medicine
Cornell University
New York City, New York
Stuart Sherman, MD
Professor of Medicine and Radiology
Glen Lehman Professor in Gastroenterology
Division of Gastroenterology and Hepatology
Indiana University
Indianapolis, Indiana
Chan Sup Shim, MD, PhD, FASGE, AGAF
Professor
Department of Gastroenterology
Kunkuk University Medical Center
Seoul, South Korea
Ajaypal Singh, MD
Director of Advanced Endoscopy
Rush University Medical Center
Chicago, Illinois
Adam Slivka, MD, PhD
Professor of Medicine
Associate Chief of Clinical Services
Division of Gastroenterology, Hepatology, and Nutrition
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania
Sanjeev Solomon, MD
Howard University Hospital
Washington, District of Columbia
Tae Jun Song, MD, PhD
Associate Professor
Gastroenterology
University of Ulsan College of Medicine
Asan Medical Center
Seoul, South Korea
Indu Srinivasan, MD
Advanced Endoscopy Fellow
Maricopa Integrated Health System Chandler, Arizona
Joseph J.Y. Sung, MD, PhD
President and Vice Chancellor
Mok Hing Yiu Professor of Medicine
The Chinese University of Hong Kong
Shatin, Hong Kong, China
Ilaria Tarantino, MD
Endoscopy Service
Department of Diagnostic and Therapeutic Services
IRCCS ISMETT (Instituto Mediterraneo per i Trapianti e Terapie ad Alta Specializzazione)
Palermo, Italy
Paul R. Tarnasky, MD
Physician
Methodist Dallas Medical Center
Dallas, Texas
Pier Alberto Testoni, MD, FASGE
Director of Division of Gastroenterology and GI Endoscopy
San Raffaele Scientific Institute
Vita Salute San Raffaele University
Via Olgettina
Milan, Italy
Catherine D. Tobin, MD
Associate Professor of Anesthesiology
Department of Anesthesia
Medical University of South Carolina
Charleston, South Carolina
Mark Topazian, MD
Professor of Medicine
Department of Gastroenterology and Hepatology
Mayo Clinic Rochester, Minnesota
Sachin Wani, MD
Associate Professor of Medicine
Division of Gastroenterology and Hepatology
University of Colorado Anschutz Medical Campus Aurora, Colorado
John C.T. Wong, MD
Clinical Professional Consultant
Institute of Digestive Disease
The Chinese University of Hong Kong
Shatin, Hong Kong, China
Andrew W. Yen, MD, MAS, FACG, FASGE
Associate Chief of Gastroenterology
Veterans Affairs Northern California Health Care System
Mather, California
Assistant Clinical Professor of Medicine
Division of Gastroenterology and Hepatology
University of California Davis School of Medicine
Sacramento, California
What a difference 10 years makes. Since the first edition of ERCP published in 2008, it seems like there has been a cosmic shift in the practice of gastrointestinal medicine and endoscopy. Diagnostic ERCP has given way to continued improvements in computed tomography and magnetic resonance imaging, as well as to endoscopic ultrasound (EUS), which provides information not only about the diameter, contents, and contours of the pancreaticobiliary ducts but also about the pancreatic and liver parenchyma, contiguous organs, relevant vasculature, and lymph nodes. Additionally, EUS has been shown to have improved sensitivity for the diagnosis of pancreatic malignancy compared with brushing or biopsy done at time of ERCP. Moreover, as technology and EUS experience have expanded, therapeutic procedures previously relegated to ERCP (or interventional radiology) are increasingly being done with an echoendoscope: gallbladder and bile duct access for cholecystoduodenal, hepatobiliary, and choledochoduodenal stenting; endoscopic anastomosis of obstructed afferent limbs; gastroenterostomy for bypass of malignant duodenal obstruction; PD imaging and duct decompression in difficultto-access anatomy; and imaging and treatment of pancreatic fluid collections, many of which were previously imaged and variably treated with ERCP. The barbarians are at the gate!
Or are they? ERCP with sphincterotomy and/or balloon dilation remains the treatment of choice for choledocholithiasis and for many cases of pancreatic stones. Moreover, it maintains primacy for the treatment of benign pancreaticobiliary strictures and most malignancies causing obstructive jaundice. In contrast, therapeutic EUS has evolved to allow access in complex postoperative anatomy, duodenal obstruction, or after failed ERCP. In fact, we are the barbarians who often employ both echoendoscopes and duodenoscopes in the same patient under a single anesthesia to stage a patient with malignant obstructive jaundice, obtain a definitive tissue diagnosis, and render appropriate palliative
therapy. Alternatively, we may use EUS to access the pancreaticobiliary tree as part of a rendezvous procedure to improve the success rate of ERCP. The third edition of this text acknowledges the expanded role that EUS has come to play in patients previously undergoing diagnostic or therapeutic ERCP alone. Utilizing one procedure without access to the other is a disservice to our patients and encourages the overuse of one of the (potentially) more dangerous therapeutic endoscopic procedures we perform.
What a difference 10 years makes. Look for the new chapters, including one on endoscope disinfection. This should not come as a surprise to anyone as both the lay press and medical literature have been awash in cases of antibiotic resistant bacterial infections, which can be traced back to duodenoscopes contaminated with the same organism. What else is new in the third edition of ERCP? Almost everything: new images, updated videos, and multiple chapters that incorporate EUS and place it into the perspective of modern ERCP practice. However, there is much that has not changed in the current edition of this text. Most notably we have retained the world’s premier clinicians and endoscopic researchers to share their ERCP experience, their wisdom, and their cautions to us all.
ACKNOWLEDGMENT
The Editors thank our medical colleagues and support staff for their outstanding contributions to our patients’ care and the authors of this textbook for their new or updated contributions.
Todd H. Baron, MD, FASGE Richard A. Kozarek, MD, FASGE David L. Carr-Locke, MD, FRCP, FASGE, FACG
SECTION I General Topics
1. Approaching 50 Years: The History of ERCP, 1
Lee McHenry and Glen Lehman
2. The ERCP Room, 7
Brian C. Brauer and Steven A. Edmundowicz
3. Radiologic Issues and Radiation Safety During ERCP, 14
Eugene Lin and Beth Schueler
4. Endoscopes, Guidewires, and Accessories, 30
Sushil K. Ahlawat and Firas H. Al-Kawas
5. Duodenoscope Reprocessing, 44
Jennifer T. Higa, Michael Gluck, and Andrew S. Ross
6. Sedation in ERCP, 49
Catherine D. Tobin and Gregory A. Coté
7. Indications for and Contraindications to ERCP, 54
Sanjeev Solomon and John Baillie
8. Adverse Events of ERCP: Prediction, Prevention, and Management, 59
Indu Srinivasan and Martin L. Freeman
9. ERCP Training, 68
Rawad Mounzer and Sachin Wani
10. Preparation of the Patient for ERCP, 80
John T. Maple
11. Principles of Electrosurgery, 86
Petros C. Benias and David L. Carr-Locke
12. Quality Issues and Measures in ERCP, 93
Jordan D. Holmes and Douglas O. Faigel
13. Medicolegal Issues in ERCP, 99
Peter Cotton
SECTION II Techniques
14. Cannulation of the Major Papilla, 108
Michael J. Bourke and Michael X. Ma
15. Access (Precut) Papillotomy, 123
Sujievvan Chandran, Gary May, and Paul Kortan
16. Sphincter of Oddi Manometry, 132
Tugrul Purnak and Evan L. Fogel
17. Biliary Sphincterotomy, 137
Horst Neuhaus
18. Balloon Dilation of the Native and Postsphincterotomy Papilla, 148
Chan Sup Shim
19. Stone Extraction, 160
Andrew W. Yen and Joseph W. Leung
20. Pancreatic Sphincterotomy, 171
Jonathan M. Buscaglia and Anthony N. Kalloo
21. Minor Papilla Cannulation and Sphincterotomy, 182
Pier Alberto Testoni and Alberto Mariani
22. Plastic Pancreaticobiliary Stents and Nasopancreaticobiliary Tubes: Concepts and Insertion Techniques, 196
Ryan Law and Todd H. Baron
23. Biliary Metal Stent Insertion: Indications and Insertion Techniques, 206
Koushik K. Das and Gregory G. Ginsberg
24. Pancreaticobiliary Stent Retrieval, 216
Anthony Razzak, Everson Luiz de Almeida Artifon, and Richard A. Kozarek
25. Papillectomy and Ampullectomy, 230
Shayan Irani and Richard A. Kozarek
26. Pancreatoscopy, 242
Tadashi Kodama and Tatsuya Koshitani
27. Cholangioscopy, 249
Raj J. Shah and Takao Itoi
28. Endomicroscopy in the Pancreaticobiliary Tree, 259
Anthony J. Choi and Michel Kahaleh
29. ERCP in Children, 263
Victor L. Fox
30. ERCP in Pregnancy, 282
Thiruvengadam Muniraj and Priya A. Jamidar
31. ERCP in Surgically Altered Anatomy, 288
Simon K. Lo
32. Endoscopic Ultrasonography–Guided Biliary Drainage, 308
Manuel Perez-Miranda
33. Endoscopic Ultrasound and EUS-Guided Endotherapy, 321 S. Ian Gan
SECTION III Approach to Clinical Problems
34. Pancreaticobiliary Disorders: What Are the Roles of CT, MRCP, and EUS Relative to ERCP?, 328
Andres Gelrud and Ajaypal Singh
35. Pancreas Divisum, Biliary Cysts, and Other Congenital Anomalies, 335
Mark Topazian
36. Dilated Bile Duct and Pneumobilia, 346
Koushik K. Das and Michael L. Kochman
37. The Dilated Pancreatic Duct, 354
Douglas G. Adler and Michelle A. Anderson
38. Ampullary Neoplasia, 361
Paul Fockens and Ian D. Norton
39. Malignant Biliary Obstruction: Distal, 372
Meir Mizrahi, Jonah Cohen, João Guilherme Guerra de Andrade
Lima Cabral, and Douglas Pleskow
40. Malignant Biliary Obstruction of the Hilum and Proximal Bile Ducts, 385
Alexander M. Sarkisian and Reem Z. Sharaiha
41. Indeterminate Biliary Stricture, 394
Bret T. Petersen
42. Endoscopic Approaches to Concomitant Malignant Biliary Obstruction and Gastric Outlet Obstruction, 405
Yen-I Chen, Todd H. Baron, and Mouen A. Khashab
43. Benign Biliary Strictures, 417
Guido Costamagna, Ivo Boškoski, and Pietro Familiari
44. Biliary Surgery Adverse Events, Including Liver Transplantation, 422
Ilaria Tarantino, Todd H. Baron, and Dario Ligresti
45. ERCP and EUS for Acute and Chronic Adverse Events of Pancreatic Surgery and Pancreatic Trauma, 432
Prabhleen Chahal and Todd H. Baron
46. Choledocholithiasis, 441
John C.T. Wong, James Y.W. Lau, and Joseph J.Y. Sung
47. Pancreaticobiliary Pain and Suspected Sphincter of Oddi Dysfunction, 449
Paul R. Tarnasky and Robert H. Hawes
48. Sclerosing Cholangitis, 457
Jawad Ahmad and Adam Slivka
49. Tropical Parasitic Infestations, 464
D. Nageshwar Reddy, G. Venkat Rao, and Rupa Banerjee
50. Recurrent Pyogenic Cholangitis, 469
Tae Jun Song, Dong Wan Seo, and Khean-Lee Goh
51. Cystic Lesions of the Pancreas, 480
Omer Basar and William R. Brugge
52. Unexplained Acute Pancreatitis and Acute Recurrent Pancreatitis, 486
Ihab I. El Hajj and Stuart Sherman
53. Biliary Intervention in Acute Gallstone Pancreatitis, 499
Andrew Korman and David L. Carr-Locke
54. Pancreatic Interventions in Acute Pancreatitis: Ascites, Fistulae, Leaks, and Other Disruptions, 506
Michael Larsen and Richard A. Kozarek
55. Chronic Pancreatitis: Stones and Strictures, 516
Jacques Devière, Todd H. Baron, and Richard A. Kozarek
56. Endoscopic Drainage of Pancreatic Pseudocysts, Abscesses, and Walled-Off (Organized) Necrosis, 525
Ryan Law and Todd H. Baron
Chapter 8 Adverse Events of ERCP: Prediction, Prevention, and Management
Video 8.1 Postsphincterotomy Oozing
Video 8.2 Postampullectomy Bleeding: Hemoclip
Video 8.3 Guidewire Perforation of the Bile Duct
Video 8.4 Retroperitoneal Perforation
Video 8.5 Retroperitoneal Perforation
Video 8.6 Retroperitoneal Sphincterotomy Perforation
Chapter 14 Cannulation of the Major Papilla
Video 14.1 Wire Lead Technique of Cannulation
Video 14.2 Wire Lead Technique of Cannulation
Video 14.3 Needle-Knife Sphincterotomy
Video 14.4 Needle-Knife Sphincterotomy
Video 14.5 Needle-Knife Sphincterotomy
Video 14.6 Pancreatic Cannulation
Chapter 15 Access (Precut) Papillotomy
Video 15.1 Fistulotomy in a Diverticulum
Video 15.2 Impacted Stone Fistulotomy
Chapter 16 Sphincter of Oddi Manometry
Video 16.1 Sphincter of Oddi Manometry
Chapter 17 Biliary Sphincterotomy
Video 17.1 Biliary Sphincterotomy: Biliary Cannulation
Video 17.2 Biliary Sphincterotomy: EST Double-Wire Biliary Cannulation
Video 17.3 Biliary Sphincterotomy and Prophylactic Pancreatic Duct
Stenting in Sphincter of Oddi Dysfunction
Video 17.4 Biliary Sphincterotomy
Video 17.5 Biliary Sphincterotomy
Chapter 18 Balloon Dilation of the Native and Postsphincterotomy
Papilla
Video 18.1 Balloon Dilation of the Major Papilla in Billroth II Gastrojejunostomy and Extraction of the Bile Duct Stone
Video 18.2 Sphincterotomy and Balloon Dilation of the Major Papilla
Video 18.3 Postsphincterotomy Large Balloon Dilation of the Major Papilla and Extraction of a Huge (4.5- × 2.0-cm) Stone
Video 18.4 Balloon Dilation of the Major Papilla and Extraction of Multiple Bile Duct Stones
Chapter 19 Stone Extraction
Video 19.1 Papillotomy and Basket Stone Extraction
Video 19.2 Papillotomy- and Papillotome-Assisted Stone Extraction Followed by Basket Stone Extraction
Video 19.3 Papillotomy, Balloon Sphincteroplasty, and Stone Extraction With Balloon
Video 19.4 Impacted Ampullary Stone
Chapter 20 Pancreatic Sphincterotomy
Video 20.1 Pancreatic Sphincterotomy
Chapter 21 Minor Papilla Cannulation and Sphincterotomy
Video 21.1 Minor Papilla Cannulation and Sphincterotomy
BOX 1.1 History of ERCP: Five Decades, Decade by Decade
1970s: Diagnosis and Therapy
• Locating the ampulla
• Biliary and pancreatic duct cannulation
• Interpretation of cholangiography and pancreatography, identifying pathology
• First reports of biliary sphincterotomy
• Developing the instruments: balloon extraction of bile duct stones and stent placement
1980s: Slowly Shifting from Surgery to Endoscopic Management of Pancreaticobiliary Disorders
• Refinement of accessories, improvements in radiographic imaging
• Reporting adverse events of sphincterotomy
• Biliary stent placement for obstructive jaundice and shift from palliative surgery
• Introduction of the teaching head: “seeing is believing”
• Acceptance of ERCP by the medical community
• Management of CBD stones shifts from surgery to endoscopy
• ERCP training gets its start for physicians and ERCP nurses
• Basic threshold numbers for competence
1990s: Training and Expanding Our Therapies
• More emphasis on advanced training
• Endoscopic photography and videography: sharing images with others
• Referring MDs, patients, and industry
• Comparison of one procedure to another
• Teaching and training
• “Theater presentations” of ERCP
• Therapies for pancreatic disorders: chronic pancreatitis, pseudocysts, and necrosis
• Era of laparoscopic cholecystectomy and bile duct injuries
• Safer sphincterotomy: monofilament wires and computer-regulated blended current
• Self-expandable metallic stents
• Complementary pancreaticobiliary techniques developed
• Endoscopic ultrasonography (EUS) and magnetic resonance cholangiopancreatography (MRCP)
2000s: Prevention, Pulverizing, and Peculiar Pancreas Diseases
• Pancreatic stents and post-ERCP pancreatitis prevention
• Improved techniques for extraction of “large” bile duct stones are implemented
• Papillary balloon dilation
• Single-operator system for intraductal lithotripsy
• Intraductal papillary mucinous neoplasm (IPMN) and autoimmune pancreatitis (AIP) recognized
• “Hands-on” courses
• EUS and ERCP therapeutic interface
2010s: Refinements of ERCP Techniques and New Treatments
• Pharmacologic agents (rectal NSAIDs) for post-ERCP prevention
• Revised recommendations for sphincter of Oddi dysfunction diagnosis and therapy
• ERCP scope infections are revisited and rigorous cleaning processes of ERCP scopes are revised
• Novel ERCP treatments for cholangiocarcinoma, including photodynamic therapy and radiofrequency ablation, are introduced
• Charge-coupled device (CCD) imaging improves intraductal cholangioscopy and pancreatoscopy
TABLE 1.1 ERCP in Its Infancy: Cannulation Rates Around 1972
541 86
145 94 Vennes 80 75
*Generally defined as entry into either duct.
From Cotton PB. Progress report: cannulation of the papilla of Vater by endoscopy and retrograde pancreatography (ERCP). Gut 1972;13:1014–1025.
Canine experiments ensued and demonstrated that a papillotomy could be performed safely without bleeding or perforation. An added benefit of the Demling-Classen probe was that contrast dye could be instilled while the catheter was in place. In Japan, Kawai developed a papillotomy device consisting of two separate 2-mm-long diathermy knives that protruded from the catheter tip and could be used to incise the papillary sphincter, similar to the present-day needle knife technique.15 This device was particularly useful in patients with impacted stones at the papilla. The Erlangen probe, because of a perceived reduction in the risk of perforation, was more accepted in the West, and sphincterotomy as a technique was born. The initial concern of postsphincterotomy scarring was postulated, but the incidence was found to be infrequent. The first
therapeutic application during ERCP, with incumbent well-chronicled risks, was gradually adopted by endoscopists around the world. Bile duct stones were accurately diagnosed at the time of cholangiography, biliary sphincterotomy was performed, and the stones were left in the bile duct to pass on their own. This clinical problem needed a solution, and as is true with the many endoscopic techniques, the fundamental elements for major endoscopic technological advances were borrowed heavily from other fields (i.e., urology: basket, stent, and balloon technology; radiology: catheter and guidewire technology; cardiology: catheters and metallic stents). To solve the clinical problem of removing stones from the bile duct, in 1975 Zimmon and colleagues18 in New York reported removal of bile duct stones with balloon-tipped catheters, a
technique that further expanded the endoscopist’s therapeutic armamentarium. Long, flexible balloon-tipped catheters, basket catheters, stone-grasping forceps, and endoscopic laser or ultrasound stone disintegrators were miniaturized to fit through the endoscope working channel, and removal of bile duct stones no longer required surgical laparotomy and open choledochotomy.

FIG 1.1 One year after Dr. William McCune successfully performed the first ERCP at George Washington University, in Japan Dr. Itaru Oi, with his chief, Dr. Takemoto, performed endoscopic cholangiopancreatogram (ECPG), as it was called, with a Machida scope in 1969.5 The method used was almost the same as Dr. McCune’s method of using a prolonged gastrofiberscope. In close collaboration with the Machida and Olympus corporations, Oi developed a side-viewing fiberoptic duodenoscope with a channel and an elevator lever to enable manipulation of the cannula. (Photo courtesy Dr. Peter Cotton, Medical University of South Carolina.)
The 1970s were an exciting time for ERCP, but many physicians (gastroenterologists and surgeons) were appropriately concerned about the dangers of the procedure, particularly PEP, bleeding, and biliary sepsis. In 1976, Bilbao and colleagues19 surveyed 402 U.S. owners of side-viewing duodenoscopes who had collectively performed 10,435 ERCPs. The procedure failed in 30%, adverse events occurred in 3%, and death occurred in 0.2%. Pancreatitis was associated with injection into the pancreatic duct and sepsis with injection into an obstructed bile duct. Inexperience led to a fourfold increase in failures (62%) and twice the rate of adverse events (7%). ERCP was the riskiest procedure for the endoscopist, yet was gradually embraced, and the physicians who had the willingness and ability to perform ERCP forged ahead. In looking back in ERCP history over the past 5 decades, the gastroenterology community was aware of the high incidence and potentially severe adverse events associated with ERCP; however, the absolute requirement of advanced training and expertise before subjecting patients to this potentially lethal procedure was understated, minimized, and inadequately addressed. These should serve as reminders and lessons for the future as new endoscopic procedures are introduced.
Malignant bile duct obstruction posed a problem to the ERCP physician in the 1970s. Endoscopic cannulation of the bile duct introduced bacteria-laden contrast dye into an obstructed biliary tree, and endoscopic sphincterotomy alone would not provide adequate biliary drainage except in the most distal bile duct or ampullary cancers. Percutaneous transhepatic methods for biliary drainage were commonly employed preoperatively in patients with deep jaundice or for palliation, and the first report of a percutaneous transhepatic cholangiography (PTC)-guided internal bile duct prosthesis was reported by Burcharth et al. in 1979.20 In 1980, the ERCP groups in England (Laurence and Cotton21) and Germany (Soehendra and Reynders-Frederix22) reported the early cases of internal decompression of malignant biliary obstruction by ERCP-directed biliary endoprosthesis placement (Fig. 1.4). The initial methods relied on “borrowed” technology and reported the uses of a 7-Fr nasobiliary drain fashioned from an angiographic catheter and a “pigtail” stent cut from a 7-Fr Teflon catheter. Over the next 30 years, with the aid of industry and ingenuity, biliary endoprosthesis design continued to advance from the back table of the craftsman/endoscopist to the precision engineering of multisized polyethylene stents and

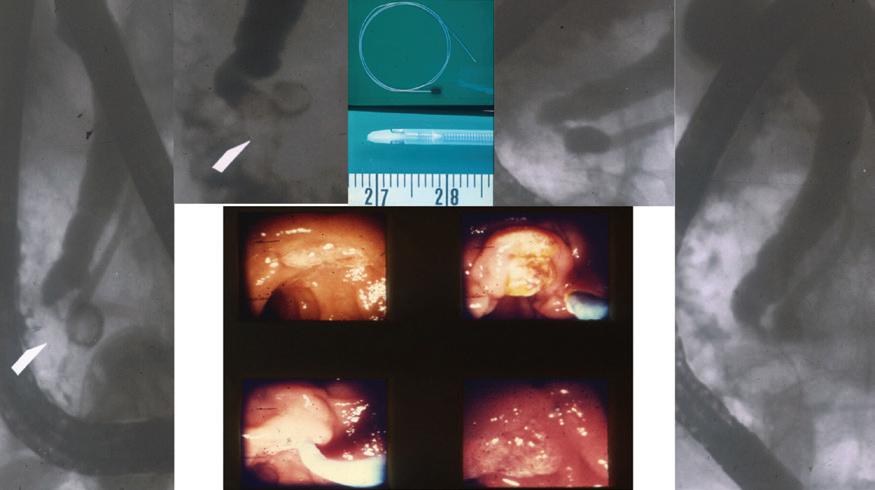
FIG 1.2 In the early days: First ERCP by Dr. Ogoshi at the Niigata Cancer Center Hospital, Japan, in 1970. Radiographs showing complete pancreatography (left) and the distal bile duct (right). Note the long scope position to obtain pancreatography. (Photo courtesy Dr. Peter Cotton, Medical University of South Carolina.)
In the bottom middle is the limited field of view of the duodenal papilla on the left and the papilla after sphincterotomy on the right. (Photo courtesy Dr. Peter Cotton, Medical University of South Carolina.)
self-expandable metallic stents. Effective palliation of malignant biliary obstruction was wrestled from the surgeon and radiologist, and planted for good into the endoscopist’s hands.
THE SECOND DECADE: 1980 TO 1990
Over the next 10 years from 1980 to 1990, medicine witnessed an explosion in the number of ERCPs performed throughout the world. However, this explosion did not occur in a vacuum and was fueled by burgeoning technology in other medical disciplines such as radiology, anesthesia, pathology, and surgery. In 1979, the Nobel Prize in Medicine was awarded jointly to Godfrey N. Hounsfield (U.K.) and Allan McLeod Cormack (Tufts University, Medford/Somerville, MA) for independently inventing the computerized axial tomography (CAT) scanner. Assessment of the patient with pancreatobiliary disease was transformed from physical examination, ultrasound, and plain radiographs, and their inherent limitations to precise computed tomography (CT) characterization and localization of the problem at hand. Improved perioperative management and anesthesia care made the ERCP procedure more acceptable to patients. Pathologic interpretation of endoscopic biopsies and cytologic assessment of brushings continued to improve, with increased number of specimens and physician experience allowing tissue diagnosis to be made nonoperatively. The surgeon’s role evolved from exploration for diagnosis with its inherent morbidity and mortality to a more focused therapeutic operation that would lead to improved patient outcomes.
Industry played a major role in the close collaboration with endoscopists in designing improved versions of ERCP accessories, including cannulas, sphincterotomes, and endoscopic stents, which led to improved therapeutics and improved patient outcomes. Companies such as Wilson-Cook (now Cook Endoscopy, Winston-Salem, NC), Olympus (Center Valley, PA, and Tokyo, Japan), Bard (now ConMed, Utica, NY), and Microvasive (now Boston-Scientific, Marlborough, MA) and many
others forged tight, long-lasting relationships with the pioneers in ERCP, which accelerated innovation in the field (Fig. 1.5). Both ERCP endoscopists and patients benefited from increased cannulation rates, improved sphincterotomies, and reliable prostheses. The domain of bile duct stones and palliation of malignancies shifted from surgeons to endoscopists. One of the recurring themes in endoscopic advances is the importance of close collaboration of engineers and clinicians to attempt to solve clinical problems.
Fiberoptic endoscopy was the platform for the ERCP gastroenterologist in the 1970s and posed a challenge for performance of and training and reporting in ERCP. Documenting endoscopic findings was limited in quality, as the camera head attachment was bulky and, when affixed, precluded real-time visualization of the endoscopy image. To share the endoscopy experience, a teaching head apparatus would connect to the endoscope to allow a second observer (an ERCP trainee or procedural nurse) to visualize the endoscopic image. The major drawbacks were halving of the light transmitted through the fibers to the eyepiece, allowing only one observer on the teaching head, and limiting the nurse to the use of only one hand to perform important functions such as wire advancement while holding the teaching head with the other hand. The first videoendoscope had a small television camera in the tip of the endoscope (charge-coupled device [CCD]) and was connected to a computer capable of transforming electronic signals into a recognizable image. Sivak and Fleischer23 in the United States and Classen and Phillip24 in Germany reported on their first experiences in 1984. Videoendoscopy had transformed the ERCP experience for the performing physician, the trainees, and the ERCP nurses to a more dynamic, less solitary experience and launched ERCP training to a new level.
THE THIRD DECADE: 1990 TO 2000
In the decade of 1990 to 2000, several breakthrough technologies in radiology, endoscopy, and surgery were introduced that would impact
FIG 1.3 The endoscopic and fluoroscopic images from the first sphincterotomy performed by Drs. Nakajima and Kawai in Kyoto, Japan, in 1974. Clockwise from left: The fluoroscopic images on the left show the distal bile duct calculus (arrow) with upstream filling of the bile duct. The catheter was used for cannulation and sphincterotomy. On the right, the cholangiogram and pancreatogram revealing bile duct clear of filling defect.
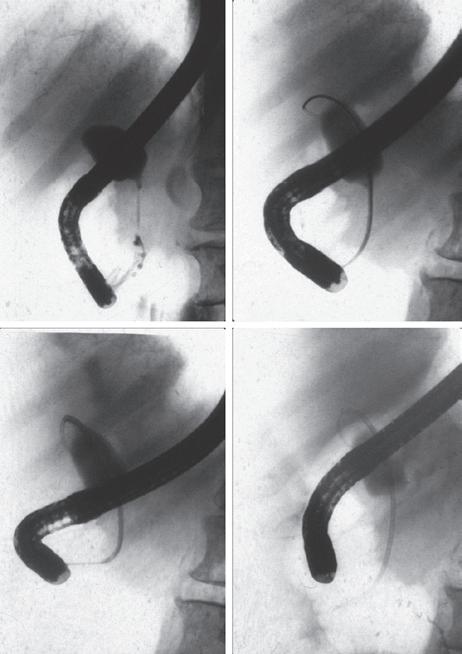
FIG 1.4 ERCP-directed bile duct drainage using biliary stents was introduced by Soehendra and Reynders-Frederix from Hamburg, Germany, in 1979, adding to the armamentarium of therapeutic ERCP. The team used a 20-cm-long, 7-Fr radioopaque angiographic catheter with 12 side holes inserted over a guidewire with a single pigtail that allowed it to be fixed inside the bile duct. (Photo courtesy Dr. Peter Cotton, Medical University of South Carolina.)
FIG 1.5 Industry played a pivotal role in the field of ERCP. The Olympus duodenoscope model JF (pictured here with camera attached) was introduced in 1971. The JF duodenoscope was fiberoptic, had a 65-degree view angle, and was fitted with an elevator. The channel size was <2 mm diameter, limiting the size of catheters that could be used and making suctioning around the catheter problematic. (Photo courtesy Dr. David Barlow, Olympus Corporation.)
resonance cholangiopancreatography (MRCP) to image noninvasively the bile and pancreatic ducts.26,27 Endoscopic ultrasonography (EUS), originally described in 1980 by DiMagno et al.,28 was introduced with the radial scanning echoendoscope, which became a staple for clinical care in the late 1980s. Linear endosonography followed in 1994 and had the added advantage of diagnostic fine-needle aspiration. Laparoscopic cholecystectomy was first performed in 1987 by Mouret (unpublished) and reported in 1989 in Europe by Dubois et al.29 and Perissat et al.30 and in the United States by Reddick and Olsen.31 Laparoscopic cholecystectomy transformed the practice of ERCP, with more reliance on endoscopists to remove bile duct stones preoperatively or postoperatively.32
ERCP IN THE NEW MILLENNIUM
In the fourth and fifth decades, ERCP as an endoscopic procedure was widely available and practiced by many gastroenterologists in nearly every hospital with more than a 50-bed capacity. In the earlier decades of ERCP, the technique was adopted initially based on logic and began to grow based on cannulation success and eventually therapeutic success. There were few prospective, controlled, randomized, outcome-based studies in the early years, in part because of the excitement and enthusiasm of innovation and the lack of funding (and applications for funding) for endoscopic studies. The growth of ERCP decade by decade was in part attributable to the continued refinement of techniques and introduction of new innovations. In the new millennium, the “science of ERCP” has now become the focus. Prospective scientific studies have flourished since the year 2000, including studies evaluating the role of ERCP in gallstone pancreatitis,33 malignant biliary obstruction (preoperative endoscopic drainage followed by pancreaticoduodenectomy compared with primary pancreaticoduodenectomy alone),34 and sphincter of Oddi dysfunction (National Institutes Health–sponsored EPISOD trial) comparing sham therapy to manometrically directed sphincterotomy),35 and studies using pancreatic stents and pharmacologic agents to prevent PEP.36 Comparative trials evaluating novel therapies for cholangiocarcinoma, including photodynamic therapy (PDT) and radiofrequency ablation (RFA), emerged.
the field of pancreaticobiliary disease and the ERCP endoscopist. These technologies blossomed and ultimately transformed the indications for ERCP from a diagnostic/therapeutic procedure to a predominately therapeutic one.25 This transformation was driven in part by the introduction of magnetic resonance imaging (MRI)/magnetic
With the benefit of hindsight, in the 5-decade history of ERCP we could pose the following: What were the shortcomings of the incorporation of this technology into standard clinical practice? The risks of ERCP were underrecognized and underreported, particularly with respect to pancreatitis and perforation.37 An attempt to stratify patients at the greatest risk for PEP was not addressed until the fourth decade by Freeman and colleagues in 2001.38 Informed consent for ERCP was cursory, and in many instances, full disclosure of the potential risks and severity of adverse events was not provided to patients. Self-training was the norm in the first decade of ERCP, but advanced training became more readily available in the 1980s and 1990s. The endoscopy societies were lax in guiding ERCP training programs and community hospitals in the number of ERCPs necessary to attain a base level of competence. The Gastroenterology Core Curriculum of the Gastroenterology Leadership Council (joint effort of the American Association for the Study of Liver Diseases [AASLD], American College of Gastroenterology [ACG], American Gastroenterological Association [AGA], and American Society for Gastrointestinal Endoscopy [ASGE]) in 1996 did not recommend a specific number of ERCPs necessary to assess competence. An early ASGE guideline recommended 100 ERCP procedures (75 diagnostic and 25 therapeutic) as the minimum number of ERCPs before one could assess competency. The threshold still remains unclear, with the suggestion that at least 180 procedures are necessary.39 Yearly ERCP volume by the endoscopist practicing ERCP has not been established to guide credentialing agencies.
A “shift” of high-risk, complicated ERCP procedures to referral centers is reflected in the growing number of ERCPs performed at our institution over the past 15 years (Fig. 1.6). Hands-on training opportunities for practicing gastroenterologists to improve ERCP skills are scarce, and real-life simulators for ERCP are still not available.
KEY POINTS
• In the early years of ERCP in the 1970s, pioneers such as McCune, Oi, Classen, Kawai, Cotton, Vennes, Silvis, Geenen and others established a new technology.
• Close collaboration was vital between the endoscopist and industry to design new instrumentation, leading to higher cannulation rates, improved sphincterotomy, more effective drainage techniques, and improved outcomes.
• The early adopters of ERCP were self-taught, and subsequent trainees were schooled using the apprentice model. Training accelerated with
THE FUTURE OF ERCP
As we look back at the history of ERCP, we can take time to speculate about ERCP in the future. Capsule cameras and remote-guided cameras may complement or replace handheld gastroscopy, enteroscopy, and colonoscopy, but we foresee that endoscopic cannulation of the pancreaticobiliary system will remain the standard. Improvements with CCDs, even smaller-diameter choledochoscopes, and pancreatoscopes are eagerly awaited and should soon become a practical reality. However, optimal view, steerability, and durability remain as challenges. Hands-free manipulation of endoscopes, similar to robotic-assisted surgery, is anticipated with the advantages of reduced endoscopist fatigue, improved ability to train endoscopists, and more refined movement of accessories. Pancreaticobiliary tumor diagnosis and tissue sampling will undoubtedly improve with advances in intraductal endoscopy. Endoscopic pancreatic cancer screening of high-risk groups may become a reality. Pancreatitis management may benefit from a more defined endoscopic role. Dissolution of intraductal pancreatic stones may be possible with the aid of endoscopically placed catheters. Studies of pancreatic juice may provide predictors of recurrent pancreatitis, pancreatic cancer risk, and response to chemotherapy. Continued effort is needed to make ERCP safer and more effective. Advanced training programs must continue to ensure that ERCP endoscopists are adequately trained and skilled in the performance of this procedure.
The complete reference list for this chapter can be found online at www.expertconsult.com
introduction of videoendoscopy. Minimum qualifications for ERCP competency were poorly defined.
• In the new millennium, ERCP endoscopists have emphasized scientific rigor with several prospective, outcome-based studies. Newer techniques such as prophylactic pancreatic stent placement were adopted to make ERCP safer in high-risk patients.
FIG 1.6 ERCP case volume over 25 years at the Indiana University Division of Gastroenterology.
REFERENCES
1. Tsuchiya Y. A further study of percutaneous transhepatic cholangiography. Jpn J Gastroenterol. 1972;69:1163.
2. Redeker AG, Karvountzis GG, Richman RH, et al. Percutaneous transhepatic cholangiography: an improved technique. JAMA 1975;231:386–388.
3. Rabinov KR, Simon M. Peroral cannulation of the ampulla of Vater for direct cholangiography and pancreatography: preliminary report of a new method. Radiology. 1965;85:693–697.
4. McCune WS, Shorb PE, Moscowitz H. Endoscopic cannulation of the ampulla of Vater: a preliminary report. Ann Surg. 1968;167:752–756.
5. Oi I, Takemoto T, Kondo T. Fiberduodenoscope: direct observation of the papilla of Vater. Endoscopy. 1969;3:101–103.
6. Oi I. Fiberduodenoscopy and endoscopic pancreatocholangiography. Gastrointest Endosc. 1970;17:59–62.
7. Vennes JA, Silvis SE. Endoscopic visualisation of bile and pancreatic ducts. Gastrointest Endosc. 1972;18:149–152.
8. Cotton PB. Progress report: cannulation of the papilla by endoscopy and retrograde cholangiography (ERCP). Gut. 1972;13:1014–1024.
9. Ogoshi K, Tobita Y, Hara T. Endoscopic observation of the duodenum and pancreatocholedochography using duodenofiberscope under direct vision. Gastrointest Endosc. 1970;12:83–96.
10. Kasugai T, Kuno N, Aoki I, et al. Fiberduodenoscopy: analysis of 353 examinations. Gastrointest Endosc. 1971;18:9–16.
11. Classen M, Koch H, Fruhmorgen P, et al. Results of retrograde pancreaticography. Acta Gastroenterol Jpn. 1972;7:131–136.
12. Blackwood WD, Vennes JA, Silvis SE. Post-endoscopy pancreatitis and hyperamylasuria. Gastrointest Endosc. 1973;20:56–58.
13. Safrany L, Tari J, Barna L, et al. Endoscopic retrograde cholangiography: experience of 168 examinations. Gastrointest Endosc. 1973;19:163–168.
14. Demling L. Operative endoskopie. Med Welt. 1973;24:1253.
15. Kawai K, Nakajiama M. Preliminary report on endoscopic papillotomy. J Koyoto Pref Univ Med. 1973;82:353.
16. Classen M, Demling L. Endoskopische sphinkterotomie der papilla vateri und steinextracktion aus dem ductus choledochus. Dtsch Med Wochenscher. 1974;99:496–497.
17. Demling L, Koch H, Classen M, et al. Endoscopic papillotomy and removal of gall-stones: animal experiments and first clinical results. Dtsch Med Wochenscher. 1974;99(45):2233–2237.
18. Zimmon DS, Falkenstein DB, Kessler RE. Endoscopic papillotomy for choledocholithiasis. N Engl J Med. 1975;293(23):1181–1182.
19. Bilbao MK, Dotter CT, Lee TG, et al. Complications of endoscopic retrograde cholangiopancreatography (ERCP): a study of 10,000 cases. Gastroenterology. 1976;70:314–320.
20. Burcharth F, Jensen LI, Olesen K. Endoprosthesis for internal drainage of the biliary tract. Gastroenterology. 1979;77:133–137.
21. Laurence BH, Cotton PB. Decompresson of malignant biliary obstruction by duodenoscope intubation of the bile duct. Br Med J. 1980;I:522–523.
22. Soehendra N, Reynders-Frederix V. Palliative bile duct drainage: a new endoscopic method of introducing a transpapillary drain. Endoscopy 1980;12:8–11.
23. Sivak MJ, Fleischer DE. Colonoscopy with a video-endoscope: a preliminary experience. Gastrointest Endosc. 1971;18:66.
24. Classen M, Phillip J. Electronic endoscopy of the upper GI tract: initial experience with a new type of endoscope that has no fiberoptic bundle for imaging. Endoscopy. 1984;16:16.
25. Sherman S, Lightdale CJ, editors. Endoscopic therapy of pancreatic disease. Gastrointest Endosc Clin North Am. 1998;8:1–272.
26. Wallner BK, Schumacher KA, Weidenmaier W, et al. Dilated biliary tract: evaluation with MR cholangiography with a T2-weighted contrastenhanced fast sequence. Radiology. 1991;181:805–808.
27. Fulcher AS, Turner MA, Capps GW, et al. Half-Fourier RARE MR cholangiopancreatography: experience in 300 subjects. Radiology 1998;207:21–32.
28. DiMagno EP, Buxton JL, Regan PT, et al. Ultrasonic endoscope. Lancet. 1980;1:629–631.
29. Dubois F, Berthelot G, Levard H. Cholecystectomies par coelioscopie. Presse Med. 1989;18:980–982.
30. Perissat J, Collet DR, Belliard R. Gallstones: laparoscopic treatment, intracorporeal lithotripsy followed by cholecystostomy or cholecystectomy—a personal technique. Endoscopy 1989;21(suppl):373–374.
31. Reddick EJ, Olsen DO. Laparoscopic laser cholecystectomy: a comparison with mini-lap cholecystectomy. Surg Endosc. 1989;3:131–133.
32. NIH Consensus Conference. Gallstones and laparoscopic cholecystectomy [review]. JAMA. 1993;269:1018–1024.
33. Attasanaranya S, Fogel EL, Lehman GA. Choleledocholithiasis, ascending cholangitis, and gallstone pancreatitis. Med Clin North Am. 2008;92:925–960.
34. van der Gaag NA, Rauws EA, van Eijck MD, et al. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 2010;362:129–137.
35. Cotton PB, Durkalski V, Orrell KB, et al. Challenges in planning and initiating a randomized clinic study of sphincter of Oddi dysfunction. Gastrointest Endosc. 2010;72:986–991.
36. Elmunzer BJ, Scheiman JM, Lehman GA, et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012;366:1–9.
37. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–391.
38. Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc 2001;54:425–434.
39. Jowell PS. Quantitative assessment of procedural competence: a prospective study of training in ERCP. Ann Intern Med. 1996;125: 937–939.
The ERCP room can range from very basic to state-of-the-art. Whereas smaller institutions with low ERCP volumes often perform ERCP in the radiology department or operating room, most centers with a larger ERCP volumes perform ERCP in dedicated rooms within the endoscopy unit. The basic ERCP room requires a quality fluoroscopy unit with still-image capability in addition to standard endoscopic equipment. Major innovations in the field of interventional endoscopy have led to the development of multipurpose interventional rooms with the ability to combine endoscopic ultrasonography (EUS), cholangioscopy, pancreatoscopy, confocal endomicroscopy, and other interventions in combination with ERCP. A well-designed ERCP room is needed to accommodate this expansion in the procedural intensity of ERCP. In addition, changes in the patient population have led to the necessity to be able to perform ERCP on morbidly obese patients and those with altered anatomy using deep enteroscopy instruments. Many centers have moved to have anesthesia support for all ERCPs. The cumulative effect of these changes in the practice of ERCP has led to significant changes in the design of the typical ERCP room with the incorporation of new technology to benefit the patient, physician, and staff.
EVOLUTION OF THE ERCP ROOM
The basic intent of ERCP has not changed. Endoscopic visualization of the ampulla and cannulation of the desired ductal system with high-quality radiographic imaging guiding the appropriate therapy is still the goal. In the great majority of cases the basic equipment is all that is needed to remove a stone or place a stent across uncomplicated strictures. What has changed is the potential complexity of ERCP, especially at tertiary referral centers. The need for high-quality radiographic imaging of focal pathology in larger patients has led to modified digital fluoroscopy equipment with improved resolution, reduced radiation exposure, and the ability to function continuously for long procedures without overheating. In addition, wider tables (>30 inches) capable of accommodating larger, heavier patients (≥450 lbs.) and space for anesthesia to assist in these procedures have become essential. Additional room space is also needed to accommodate larger beds and stretchers to allow for bariatric patients (Fig. 2.1). The use of a mobile or fixed C-arm system is often employed to improve visualization of the biliary tree by allowing the plane of examination to be altered to profile the bifurcation and selected ductal systems. Additional space for supplemental equipment for cholangioscopy, EUS, laser lithotripsy, electrohydraulic lithotripsy, deep enteroscopy, and other adjuvant techniques has increased the size of the typical advanced ERCP room. Space for anesthesia equipment has further increased the need for additional space at the patient’s head. All this, in combination with the need to accommodate morbidly obese patients and store a large variety of devices in close proximity to the patient, has increased the size of well-designed, advanced interventional endoscopy rooms to greater than 500 square feet.