TranslationalEpigeneticsSeries
TrygveTollefsbol-SeriesEditor
TransgenerationalEpigenetics
EditedbyTrygveO.Tollefsbol,2014
PersonalizedEpigenetics
EditedbyTrygveO.Tollefsbol,2015
EpigeneticTechnologicalApplications
EditedbyY.GeorgeZheng,2015
EpigeneticCancerTherapy
EditedbyStevenG.Gray,2015
DNAMethylationandComplexHumanDisease
ByMichelNeidhart,2015
EpigenomicsinHealthandDisease
EditedbyMarioF.FragaandAgustinF.FFerna ´ ndez,2015
EpigeneticGeneExpressionandRegulation
EditedbySumingHuang,MichaelLittandC.Ann Blakey,2015
EpigeneticBiomarkersandDiagnostics
EditedbyJoseLuisGarcı´a-Gimenez,2015
DrugDiscoveryinCancerEpigenetics
EditedbyGerdaEggerandPaolaBarbara Arimondo,2015
MedicalEpigenetics
EditedbyTrygveO.Tollefsbol,2016
ChromatinSignalingandDiseases
EditedbyOlivierBindaandMartinFernandez-Zapico,2016
GenomeStability
EditedbyIgorKovalchukandOlgaKovalchuk,2016
ChromatinRegulationandDynamics
EditedbyAnitaGondor,2016
NeuropsychiatricDisordersandEpigenetics
EditedbyDagH.Yasui,JacobPeedicayilandDennisR. Grayson,2016
PolycombGroupProteins
EditedbyVincenzoPirrotta,2016
EpigeneticsandSystemsBiology
EditedbyLeonieRingrose,2017
CancerandNoncodingRNAs
EditedbyJayprokasChakrabartiandSangaMitra,2017
NuclearArchitectureandDynamics
EditedbyChristopheLavelleandJean-MarcVictor,2017
EpigeneticMechanismsinCancer
EditedbySabitaSaldanha,2017
EpigeneticsofAgingandLongevity
Editedby AlexeyMoskalevandAlexander M.Vaiserman, 2017
TheEpigeneticsofAutoimmunity
EditedbyRongxinZhang,2018
EpigeneticsinHumanDisease,SecondEdition
EditedbyTrygveO.Tollefsbol,2018
EpigeneticsofChronicPain
EditedbyGuangBaiandKeRen,2018
EpigeneticsofCancerPrevention
EditedbyAnupamBishayeeandDeepakBhatia,2018
ComputationalEpigeneticsandDiseases
EditedbyLooKeatWei,2019
Pharmacoepigenetics
EditedbyRamo ´ nCacabelos,2019
EpigeneticsandRegeneration
EditedbyDanielaPalacios,2019
ChromatinSignalingandNeurologicalDisorders
EditedbyOlivierBinda,2019
TransgenerationalEpigenetics,SecondEdition
EditedbyTrygveTollefsbol,2019
NutritionalEpigenomics
EditedbyBradleyFerguson,2019
PrognosticEpigenetics
EditedbyShilpySharma,2019
EpigeneticsoftheImmuneSystem
EditedbyDieterKabelitz,2020
StemCellEpigenetics
EditedbyEranMeshorerandGiuseppeTesta,2020
EpigeneticsMethods
EditedbyTrygveTollefsbol,2020
HistoneModificationsinTherapy
EditedbyPedroCastelo-BrancoandCarmenJeronimo,2020
EnvironmentalEpigeneticsinToxicologyandPublicHealth
EditedbyRebeccaFry,2020
DevelopmentalHumanBehavioralEpigenetics
EditedbyLivioProvenziandRosarioMontirosso,2020
SeriesEditor
TrygveTollefsbol
ComprehensiveCancerCenter,ComprehensiveCenterforHealthyAging, UniversityofAlabamaatBirmingham,Birmingham,AL,UnitedStates
Editedby
YvanDevaux
Head,CardiovascularResearchUnit,LuxembourgInstituteofHealth,Strassen,Luxembourg
SchoolofMedicine,DivisionofCardiology,UniversityofColoradoDenver, AnschutzMedicalCampus,Aurora,CO,UnitedStates
CARIMSchoolforCardiovascularDiseases,FacultyofHealth,MedicineandLifeSciences, MaastrichtUniversity,Maastricht,TheNetherlands
EmmaLouiseRobinson
AcademicPressisanimprintofElsevier 125LondonWall,LondonEC2Y5AS,UnitedKingdom 525BStreet,Suite1650,SanDiego,CA92101,UnitedStates 50HampshireStreet,5thFloor,Cambridge,MA02139,UnitedStates TheBoulevard,LangfordLane,Kidlington,OxfordOX51GB,UnitedKingdom
Copyright©2021ElsevierInc.Allrightsreserved.
Nopartofthispublicationmaybereproducedortransmittedinanyformorbyanymeans,electronicor mechanical,includingphotocopying,recording,oranyinformationstorageandretrievalsystem,without permissioninwritingfromthepublisher.Detailsonhowtoseekpermission,furtherinformationaboutthe Publisher’spermissionspoliciesandourarrangementswithorganizationssuchastheCopyrightClearance CenterandtheCopyrightLicensingAgency,canbefoundatourwebsite: www.elsevier.com/permissions.
ThisbookandtheindividualcontributionscontainedinitareprotectedundercopyrightbythePublisher(other thanasmaybenotedherein).
Notices
Knowledgeandbestpracticeinthisfieldareconstantlychanging.Asnewresearchandexperiencebroadenour understanding,changesinresearchmethods,professionalpractices,ormedicaltreatmentmaybecome necessary.
Practitionersandresearchersmustalwaysrelyontheirownexperienceandknowledgeinevaluatingandusing anyinformation,methods,compounds,orexperimentsdescribedherein.Inusingsuchinformationormethods theyshouldbemindfuloftheirownsafetyandthesafetyofothers,includingpartiesforwhomtheyhavea professionalresponsibility.
Tothefullestextentofthelaw,neitherthePublishernortheauthors,contributors,oreditors,assumeanyliability foranyinjuryand/ordamagetopersonsorpropertyasamatterofproductsliability,negligenceorotherwise,or fromanyuseoroperationofanymethods,products,instructions,orideascontainedinthematerialherein.
LibraryofCongressCataloging-in-PublicationData
AcatalogrecordforthisbookisavailablefromtheLibraryofCongress
BritishLibraryCataloguing-in-PublicationData
AcataloguerecordforthisbookisavailablefromtheBritishLibrary
ISBN:978-0-12-822258-4
ForinformationonallAcademicPresspublications visitourwebsiteat https://www.elsevier.com/books-and-journals
Publisher: AndreGerhardWolff
AcquisitionsEditor: PeterB.Linsley
EditorialProjectManager: MeganAshdown
ProductionProjectManager: SreejithViswanathan
CoverDesigner: MarkRogers
TypesetbySPiGlobal,India
Contributors
BenceA ´ gg
CardiometabolicandMTA-SESystemPharmacologyResearchGroup,Departmentof PharmacologyandPharmacotherapy,SemmelweisUniversity,Budapest;PharmahungaryGroup, Szeged;HeartandVascularCenter,SemmelweisUniversity,Budapest,Hungary
ParisaAghagolzadeh
ExperimentalCardiologyUnit,DivisionofCardiology,DepartmentofCardiovascularMedicine, UniversityofLausanneMedicalSchool,Lausanne,Switzerland
ChukwuemekaGeorgeAnene-Nzelu
GenomeInstituteofSingapore;CardiovascularDiseaseTranslationalResearchProgramme, NationalUniversityHealthSystem,NationalUniversityofSingaporeYongLooLinSchoolof Medicine,Singapore,Singapore
JohannesBacks
InstituteofExperimentalCardiology,UniversityofHeidelberg;DZHK(GermanCentrefor CardiovascularResearch),PartnerSiteHeidelberg/Mannheim,Heidelberg,Germany
FerranBarbe
TranslationalResearchinRespiratoryMedicine,UniversityHospitalArnaudeVilanovaandSanta Maria,IRBLleida,Lleida;CIBERofRespiratoryDiseases(CIBERES),InstituteofHealthCarlosIII, Madrid,Spain
FayBetsou
IBBL(IntegratedBiobankofLuxembourg),Dudelange,Luxembourg
StephanieBezzinaWettinger
DepartmentofAppliedBiomedicalScience,FacultyofHealthSciences,UniversityofMalta,Msida, MSD2080,Malta
AndreiCodreanu
HospitalCenterofLuxembourg,Strassen,Luxembourg
YvanDevaux
CardiovascularResearchUnit,LuxembourgInstituteofHealth,Luxembourg,Luxembourg
ChristophDieterich
GermanCenterforCardiovascularResearch(DZHK)—PartnersiteHeidelberg/Mannheim; SectionofBioinformaticsandSystemsCardiology,KlausTschiraInstituteforIntegrative ComputationalCardiologyandDepartmentofInternalMedicineIII,UniversityHospitalHeidelberg, Heidelberg,Germany
JavierDura ´ n
InstituteofExperimentalCardiology,UniversityofHeidelberg;DZHK(GermanCentrefor CardiovascularResearch),PartnerSiteHeidelberg/Mannheim,Heidelberg,Germany
RosienneFarrugia
DepartmentofAppliedBiomedicalScience,FacultyofHealthSciences,UniversityofMalta,Msida, MSD2080,Malta
KyriacosFelekkis
DepartmentofLifeandHealthSciences,SchoolofSciencesandEngineering,UniversityofNicosia, Nicosia,Cyprus
PeterFerdinandy
CardiometabolicandMTA-SESystemPharmacologyResearchGroup,Departmentof PharmacologyandPharmacotherapy,SemmelweisUniversity,Budapest;PharmahungaryGroup, Szeged,Hungary
RogerS-YFoo
GenomeInstituteofSingapore;CardiovascularDiseaseTranslationalResearchProgramme, NationalUniversityHealthSystem,NationalUniversityofSingaporeYongLooLinSchoolof Medicine,Singapore,Singapore
EleftheriaGalatou
DepartmentofLifeandHealthSciences,SchoolofSciencesandEngineering,UniversityofNicosia, Nicosia,Cyprus
DaviddeGonzalo-Calvo
TranslationalResearchinRespiratoryMedicine,UniversityHospitalArnaudeVilanovaandSanta Maria,IRBLleida,Lleida;CIBERofRespiratoryDiseases(CIBERES),InstituteofHealthCarlosIII, Madrid,Spain
SimonaGreco
MolecularCardiologyLaboratory,IRCCSPoliclinicoSanDonato,Milan,Italy
JohannesGrillari
TAmiRNAGmbH;AustrianClusterforTissueRegeneration,MedicalUniversityofVienna;Ludwig BoltzmannInstituteforExperimentalandClinicalTraumatology,Vienna,Austria
HakanGunes
FacultyofMedicine,DepartmentofCardiology,KahramanmarasSutcuImamUniversity, Kahramanmaras,Turkey
MatthiasHackl
TAmiRNAGmbH;AustrianClusterforTissueRegeneration,MedicalUniversityofVienna,Vienna, Austria
NazhaHamdani
DepartmentofMolecularandExperimentalCardiology;DepartmentofCardiology,St.JosefHospitalandBergmannsheil;DepartmentofClinicalPharmacology;InstituteofPhysiology,Ruhr UniversityBochum,Bochum,Germany
LutzHein
InstituteofExperimentalandClinicalPharmacologyandToxicology,FacultyofMedicine;BIOSS CentreforBiologicalSignallingStudies,UniversityofFreiburg,Freiburg,Germany
CarlosHermenegildo
DepartmentofPhysiology,FacultyofMedicineandDentistry,UniversityofValencia,andINCLIVA BiomedicalResearchInstitute,Valencia,Spain
EduardoIglesias-Gutierrez
DepartmentofFunctionalBiology,Physiology,UniversityofOviedo;HealthResearchInstituteof thePrincipalityofAsturias(ISPA),Oviedo,Spain
BenedettaIzzi
DepartmentofEpidemiologyandPrevention,IRCCSNEUROMED,Pozzilli,IS,Italy
KorneliaJaquet
DepartmentofMolecularandExperimentalCardiology;DepartmentofCardiology,St.JosefHospitalandBergmannsheil;DepartmentofClinicalPharmacology,RuhrUniversityBochum, Bochum,Germany
AmelaJusic
DepartmentofBiology,FacultyofNaturalSciencesandMathematics,UniversityofTuzla,Tuzla, BosniaandHerzegovina;CardiovascularResearchUnit,LuxembourgInstituteofHealth, Luxembourg,Luxembourg
KanitaKarad-uzovic-Hadz ˇ iabdic
DepartmentofEngineering,InternationalUniversityofSarajevo,Sarajevo,BosniaandHerzegovina
GabrielaM.Kuster
DepartmentofBiomedicine,UniversityHospitalBaselandUniversityofBasel;Departmentof Cardiology,UniversityHospitalBasel,Basel,Switzerland
AlisiaMade `
MolecularCardiologyLaboratory,IRCCSPoliclinicoSanDonato,Milan,Italy
FedericaDeMajo
DepartmentofMolecularGenetics,FacultyofScienceandEngineering;CARIMSchoolfor CardiovascularDiseases,FacultyofHealth,MedicineandLifeSciences;MaastrichtUniversity, Maastricht,TheNetherlands
FabioMartelli
MolecularCardiologyLaboratory,IRCCSPoliclinicoSanDonato,Milan,Italy
AndreasM€ ugge
DepartmentofMolecularandExperimentalCardiology;DepartmentofCardiology,St.JosefHospitalandBergmannsheil,RuhrUniversityBochum,Bochum,Germany
VivienNgo
InstituteofExperimentalandClinicalPharmacologyandToxicology,FacultyofMedicine,University ofFreiburg,Freiburg,Germany
SusanaNovella
DepartmentofPhysiology,FacultyofMedicineandDentistry,UniversityofValencia,andINCLIVA BiomedicalResearchInstitute,Valencia,Spain
AnaBelenPaes
DepartmentofPhysiology,FacultyofMedicineandDentistry,UniversityofValencia,andINCLIVA BiomedicalResearchInstitute,Valencia,Spain
ChristosPapaneophytou
DepartmentofLifeandHealthSciences,SchoolofSciencesandEngineering,UniversityofNicosia, Nicosia,Cyprus
ThierryPedrazzini
ExperimentalCardiologyUnit,DivisionofCardiology,DepartmentofCardiovascularMedicine, UniversityofLausanneMedicalSchool,Lausanne,Switzerland
AntjePeters
DepartmentofGeneticEpidemiology,InstituteofHumanGenetics,UniversityofMunster,Munster, Germany
Lucı´aPinilla
TranslationalResearchinRespiratoryMedicine,UniversityHospitalArnaudeVilanovaandSanta Maria,IRBLleida,Lleida;CIBERofRespiratoryDiseases(CIBERES),InstituteofHealthCarlosIII, Madrid,Spain
EmmaLouiseRobinson
SchoolofMedicine,DivisionofCardiology,UniversityofColoradoDenver,AnschutzMedical Campus,Aurora,CO,UnitedStates
ElisabethSemmelrock
TAmiRNAGmbH,Vienna,Austria
JustusStenzig
DepartmentofExperimentalPharmacologyandToxicology,UniversityMedicalCentreHamburgEppendorf,Hamburg,Germany
MaartenVanhaverbeke
CardiovascularMedicine,UniversityHospitalsLeuven,Leuven,Belgium
MirkoVolkers
GermanCenterforCardiovascularResearch(DZHK)—PartnersiteHeidelberg/Mannheim; DepartmentofInternalMedicineIII,UniversityHospitalHeidelberg,Heidelberg,Germany
LeonJ.DeWindt
DepartmentofMolecularGenetics,FacultyofScienceandEngineering;CARIMSchoolfor CardiovascularDiseases,FacultyofHealth,MedicineandLifeSciences;MaastrichtUniversity, Maastricht,TheNetherlands
JohannesWinkler
DepartmentofCardiology,MedicalUniversityofVienna,Vienna,Austria
AngelaXuerebAnastasi
DepartmentofAppliedBiomedicalScience,FacultyofHealthSciences,UniversityofMalta,Msida, MSD2080,Malta
MehmetBirhanYilmaz
FacultyofMedicine,DepartmentofCardiology,DokuzEylulUniversity,Izmir,Turkey
Preface
YvanDevauxa andEmmaLouiseRobinsonb,c
CardiovascularResearchUnit,LuxembourgInstituteofHealth,Strassen,Luxembourga SchoolofMedicine,Divisionof Cardiology,UniversityofColoradoDenver,AnschutzMedicalCampus,Aurora,CO,UnitedStatesb CARIMSchoolfor CardiovascularDiseases,FacultyofHealth,MedicineandLifeSciences,MaastrichtUniversity,Maastricht, TheNetherlandsc
OnbehalfoftheEU-CardioRNACOSTActionCA17129.
Theburdenofcardiovasculardisease
Cardiovasculardisease(CVD)remainsamajorcauseofdisabilityanddeathworldwide.Accordingto the2019statisticsoftheWorldHealthOrganization(WHO),17.9millionpeopledieeachyearfrom CVD,whichrepresentsalmostathirdofalldeathsglobally.1 Despitesignificantimprovementsin healthcare,CVDcontinuestorepresentamajorsocioeconomicburden.RiskfactorsforCVDareeither modifiable,suchastobaccouse,physicalinactivity,excessivefoodintake,oracquired.GeneticpredispositionstoCVDhavebeenextensivelyinvestigated,yetmostlargeassociationstudiesremainat theDNA(genomic)level,searchingforassociationsbetweennucleotidepolymorphismsandtheriskof developingaCVDorhavingapoorclinicaloutcomeafteranacutecardiovascularevent(e.g.,worseningofanacutecondition,developingcomorbiditiesaffectingotherorgans,ordeath).Morerecently, abetterknowledgeofthemechanismsregulatinggeneandproteinexpressionallowedadiversification oftheseassociationstudies,nowfocusingalsoonmodificationsoccurringattheDNA,chromatin,and RNAlevels.Thosemodificationsnotalteringnucleicacidsequenceshavebeengroupedundertheterm “epigenetics,”derivedfromtheGreek“epi”meaning“over,around,ontop.”Itisnowacceptedthat epigeneticmodificationsplayamajorroleinregulatingcardiovascularhomeostasis,CVD development,andprogression.
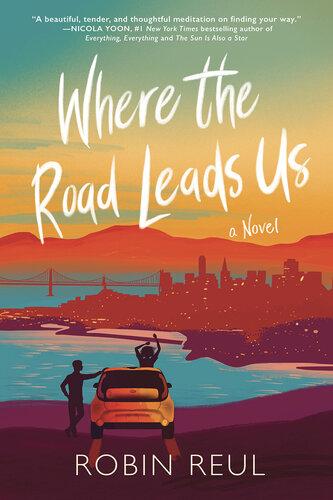
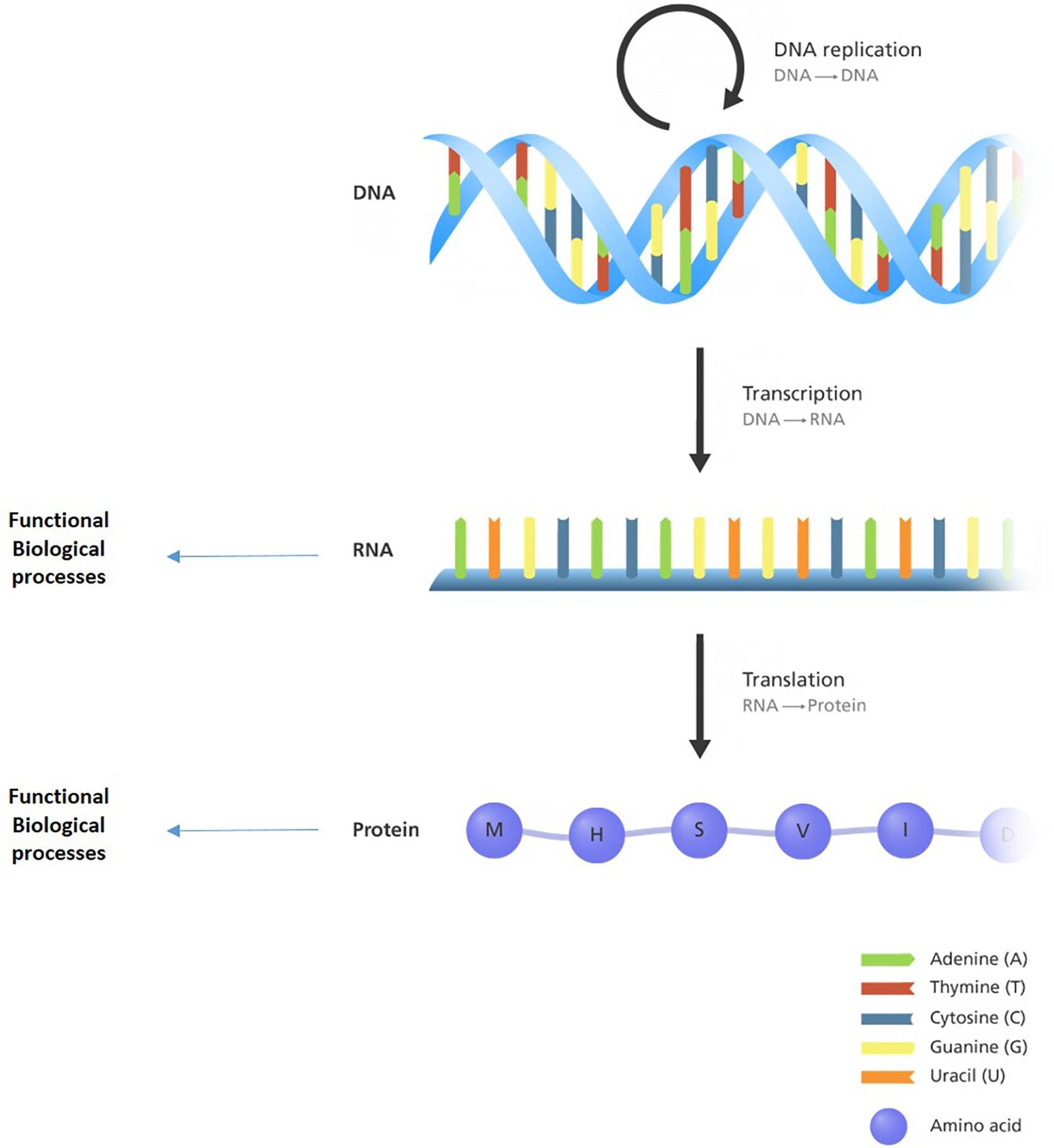
Centraldogmaofmolecularbiology
Cellularandtissuestructure,morphology,biochemistry,andfunctionaredeterminedbytheprofileof proteinsandRNAmoleculespresent.Theoriginalcentraldogmaofmolecularbiology—asdefinedby SirFrancisCrickin1957—statesthatDNAiscopiedintoRNAinaprocesscalledtranscription,with RNAthenbeingexportedfromthenucleusforproteinsynthesisattheribosomes,inaprocesscalled translation(Fig.1).However,wenowknowthatsomeRNAmoleculesarefunctionalasRNAmoleculesintheirownrightandarenotusedtoencodeproteins,accountingforatleast80%ofthetranscribedgenome.2 ThisfamilyofRNAsisknownasnoncodingRNAs(ncRNAs).Theexpressionof protein-codingRNAs(messengerRNAs)andncRNAsisdeterminedbytherateoftranscription. Thetranscriptionisunderthecontrolofepigeneticmechanisms.Epigeneticmechanismsinvolve
FIG.1
Anillustrationofthecentraldogmaofmolecularbiology,theflowofbiochemicalinformationfromDNAtoRNA andprotein.
AdaptedfromGenomeResearchLimited.
chemicalmodificationeithertotheDNAorRNAbasesthemselvesortotheproteins(histones)that packageDNAintochromatin.
Epigeneticmechanismsinclude:
– DNAcytosinemethylationanditsderivatives, – Covalentmodificationsonaminoacidsofhistones, – NoncodingRNAsthatmediatechromatinstructureandregulateotherepigeneticmodifiers, – Higher-orderchromatinstructureandscaffolding,and – CovalentmodificationsonRNAnucleotides(knownspecificallyastheepitranscriptome).
TheseepigeneticmodificationsactinconcertwitheachothertodeterminetheproteinandRNAprofilesatanygivenpointintime.3
Epigeneticmechanisms
Epigeneticmechanismsregulatedifferentiation,development,homeostasis,aging,anddisease.Epigeneticmarksarelaiddownindifferentiationanddevelopmenttoprogramthetranscriptomefrompluripotencytodeterminecellfateanddefinethedifferentiatedcellstate.Bothinareplication-dependent aswellasreplication-independentmanner,theepigeneticlandscapeisnotstatic(unlikethegenome) butisdynamicthroughoutreplicativeandchronologicalaging.Importantly,theepigenomeisresponsivetoenvironmentalcuessuchasredoxandmetabolicorneurohumoralsignaling.WholesaleremodelingofDNAmethylation,histonemodification,noncodingRNA,andRNAmodificationprofileshas beendescribedintheheartandvasculatureinCVD.4–7
Epigeneticmarks(DNA,RNA,andchromatinmodifications)aremediatedbyepigeneticmodifiers.Epigeneticmodifierscanbefurtherdescribedaccordingtotheirfunction—epigeneticwriters, erasers,andreaders.Thesearealsodynamicallyregulatedindiseaseprocesses.Theadditionorremovalofepigeneticmarks,accompaniedbybindingofepigeneticreadersandncRNAs,inturnregulatesgeneexpression.Itdoessobyalteringthechromatinstructureataparticularlocationinthe genome;affectingtheaccessibilityofenhancers,promoters,andgenebodiestotranscriptionfactors andRNApolymerases;aswellascreatingplatformsforlong-distanceregulatorygenomicinteractions. Inthecaseoftheepitranscriptome,RNAstability,localization,andfunctioncanbemodulated.
Thisbookaddressesthecurrentknowledgeandunderstandingofhowepigeneticmodificationsand modifiersregulategeneexpressionanddifferentbiologicalprocessesintheinitiationandprogression ofCVDintheheartandvasculature.Italsoevaluatestheuseofepigeneticmarksindiagnosticand epigeneticmodifiersemergingastherapeutictargets.
EpigeneticmechanismsasbiomarkersandtreatmenttargetsinCVD
Biomarkersaremoleculesthatcanbeeasilyandquantitativelymeasuredinbiologicalsamplesand giveinformationonthepresence(diagnosticbiomarkers)oforevolution(prognosticbiomarkers) ofdiseases.Traditionally,mostbiomarkershavebeensearchedforinthebloodstreamandbelong
tothefamilyofproteins.Asanexample,troponins—contractileproteinscontainedincardiomyocytes, thecellsresponsibleforheartcontractility—areusedasdiagnosticbiomarkersofacutemyocardial infarction,sincetheyarereleasedintheblooduponthedamageofthecardiactissuefollowingrupture ofbloodsupplyduetoobstructionofacoronaryartery(alsoknownasheartattackormyocardialinfarction).Diversificationofbiomarkerstudiesledtothediscoverythatnotonlyproteins(orpeptides) canbeusedasbiomarkers,butalsochangesaffectingepigeneticmechanismsthatcanbequantifiedin biologicalfluidsortissuebiopsies.NoncodingRNAsforinstance,manyofwhichcanbefoundinthe bloodstream,areemergingaspotentialnovelbiomarkersofCVD.Themostwidelyinvestigatedhave beenshort21–25nucleotidencRNAs,calledmicroRNAs(miRNAs),andtheirpotentialtohelpinpersonalizinghealthcarehasbeenproposed.8 Othertypesofepigeneticmechanismswillalsobeaddressed inthisbook,forboththeirbiomarkervalueandtheirtherapeuticpotential.Indeed,sincebiomarkers reflectdiseaseprogression,theymayalsohavetherapeuticpotential,asrecentlydiscussed.9
Theuseofepigeneticmechanismstodesignnoveldrugstotreatpatients,almostastheiruseas biomarkers,isonlyinitsinfancy,andfurtherworkandstudiesareneededtofullyaddresstheirpotentialtobeusedinprecisionmedicine.Hopesandlimitationsoftheuseofepigeneticmechanisms tohelpinimplementingpersonalizedmedicineinthecardiovascularfieldwillbediscussedin thisbook.
TheEU-CardioRNACOSTAction:networkingtoadvancescience
Networkingandsharingofcomplementaryexpertiseisessentialinbiomedicalresearch.OnlysynergisticmulticenterinvestigationshavethepotentialtodecipherthemechanismsofcomplexandmultifactorialdiseasessuchasCVD.Inthiscontext,researchersfromdifferenthorizonsteamedupina networkinginitiativefundedbyCOST.COST(EuropeanCooperationinScienceandTechnology; https://www.cost.eu)isaH2020-fundedorganizationforresearchandinnovationnetworks.COST networkingtools—knownasActions—areresearchinitiativesacrossEuropeandbeyond.Theyhelp researcherstogrowtheirideasinanyscienceandtechnologyfield,suchasbiomedicalresearch.The EU-CardioRNACOSTActionCA17129(https://cardiorna.eu)startedinOctober2018foraduration offouryears.ThemaingoalofthisActionistocatalyzetheresearchontheroleoftranscriptomicsin CVDthroughnetworkingactivitiesandcollaborativeexchangeofexpertise.TheActionaimsatabetterknowledgeofhowepigeneticsandmorepreciselyregulatoryRNAmoleculesaffectCVDdevelopment.10 Ultimately,thisgainofknowledgeisexpectedtoallowthedevelopmentofnovel biomarkersanddrugstoimprovehealthcareofCVDpatients.TheActionorganizesyearlymeetings todiscussthemostrecentscientificsignsofprogressinthefield.ThroughthefundingofShort-Term ScientificMissions(STSMs)betweenpartnerlaboratories,theActionaimstofavorstaffmobility, technologytransfer,andthesetupofsynergisticmulticenterresearchprojects.TheActionprovides InclusivenessTargetCountry(ITC)grantstohelpyounginvestigatorsfromlessresearch-intensive countriestoattendscientificconferencesanddiscusstheirdatawiththeirpeers.DisseminationactivitiesaswellasscientificcommunicationoutreachactivitiesarekeycomponentsoftheAction.AnoverallpresentationofEU-CardioRNA’sActiongoalsandorganizationhasbeenpublished.11 Thisbookon EpigeneticsinCardiovascularDiseaseisaconcreteexampleofsuchdisseminationactivities,which hasbeenpossiblebyajointeffortofmorethan25EU-CardioRNApartnersfrom15countries.
Theever-growingburdenof cardiovasculardisease 1
MehmetBirhanYilmaza andHakanGunesb
FacultyofMedicine,DepartmentofCardiology,DokuzEylulUniversity,Izmir,Turkeya FacultyofMedicine,Department ofCardiology,KahramanmarasSutcuImamUniversity,Kahramanmaras,Turkeyb
1.1 Introduction
Cardiovasculardiseases,whichcompriseischemiccardiacdisease,stroke,heartfailure,peripheral arterydisease,andothervasculardiseases,arealeadingcauseofmortalityandmorbidityintheworld andcontributesignificantlytoimpairedqualityoflife.In2017,CVDresultedin17.8milliondeathand 35.6million-yeardisabilityworldwide.AwarenessofprevalenceandincidenceofCVDandrisk factorscanprovideuswiththeopportunityforpreventionandmanagementofthediseaseandcanlead toimprovedsurvival.1
1.2 Financialloadofcardiovasculardisease
Cardiovasculardisease(CVD),asamultifaceteddiseasewithmultiplestages,isthemajorcontributor ofearlydeathallovertheworld,asaboutone-thirdofalldeathsareattributabletoCVD,andthismeasureisforeseentorisefurtherinthisdecade.2 ThereareatleastthreesignificantdomainsofCVD: epidemiologicalburden,whichconsidersfrequencyinoverallpopulationandproductiveages;economicburden,whichconstitutesdirectandindirectcosts;anddisabilityburden,whichaccountsfor severalconsequencesofthesediseases.Cardiovascularhealthservicesconstituteasignificantpart oftheoverallhealthbudgetofmembercountriesoftheEuropeanSocietyofCardiology(ESC). TheoverallburdenofhealthexpendituresrelatedtoCVDcanbebroughtundertwosubheadingsof fiscalandeconomicburden.ESCcountriesdivergesignificantlywhenitcomestoCVD-relatedfiscal burdensincehealthsystems,structuralorganizations,andpercapitaincomedifferbetweenthesecountriessignificantly.Accordingto2016reports,healthexpenditureperpersoninKirghizstanwas reportedtobe240USDollars,whereasinSwitzerland,thismeasurereached7900USDollars.2
AccordingtotheESCAtlasreport,in2016,theratioofcurrenthealthexpendituretogrossdomestic product(GDP)rangedfrom3.5%to12.2%intheESCcountrieswithGermany,France,andSwitzerlandleadingthelistandwithRomania,Turkey,Egypt,andKazakhstanatthebottomofthelistby reserving <5%ofGDPonhealthcare.2
Simplybyconsideringeconomicstrengthandlo calpurchasingpower,healthexpendituresof high-incomecountriesquadruplethatoflow-incomecountries.ThefiscalburdenofCVD,evaluated EpigeneticsinCardiovascularDisease. https://doi.org/10.1016/B978-0-12-822258-4.00008-0 Copyright # 2021ElsevierInc.Allrightsreserved.
bythedataderivedfromEurostatandtheOrganizationforEconomicCooperationandDevelopment (OECD),wasshowntoyieldmorethan10%oftotalhealthexpendituresin2016.2 Ofnote,majority wasshowntoberelatedtohospitalizationsandph armacologicaltherapy.InHealthExpendituresby DiseasesandConditions(HEDIC) Project,whichincludesseveralEuropeancountriesin2013,CVD wasshowntocoverthehighestratioofallhealth expenditures,yieldingalmost16%ofallexpendituresbyverifyingOECDmeasures.Theratioofh ealthexpendituresreservedforCVDwasnotified tobeanimportantpartoftotalexpendituresalthoughthereisadecreasingtrendinrecentyears. WhenitcomestotheeconomicburdenofCVD,itw ascalculatedtobe169b illionEurosaccounting for62%ofallhealthexpenditures.2 In2015,thiswascalculatedtoriseto210billionEuros,andof thiscost,53%wenttohealthcosts,26%wenttopr oductivitylosses,and21%wenttooff-the-record care. 2 Amonghealthcarecosts,in-hospitalcareofC VDpatientsaccountsfor51%andthemedicationcostsaccountfor21%.Onthecontrary,thetotalcostofischemicheartdiseasewascalculatedto beapproximately59billionEurosandthiswasfollowedupbycerebrovascular disease-relatedcosts of45billionEuros. 2 IntheENHstudy,percapitacostforCVDwasconsideredthoroughlyanditwas shownthatitwas48,000EuroinBulgariaand365,000EuroinFinland.2 Inthelightofthesefindings, itcouldbestatedthatCVDaccountsforasignifi cantportionofhealthcareexpendituresofESC countrieswithregardtofinancialsituationandeconomicpower.Cardiovasculardiseaseaccounts forasignificantpartofhealthcareexpendituresintheUSA,quitesimilartothatinESCcountries. In2015,102.7millionpeople(41.5%ofthewhole population)werenotedtosufferfromCVDand thisnumberisexpectedtoriseto131.2millionpeoplebytheyear2035.Withhalfofitspopulation sufferingfromCVD,theUSAwascalculatedtos pend318billionUSDollarsin2015,andthisis expectedtoriseto749billionUSDollarsbytheyea r2035.Cardiovasculardiseasehasimportant consequencesallovertheworldconsideringindividuals,healthcaresystems,andpopulationlevel. WorldHeartFederationestimated thatthe963billionUSDollarsofthetotalglobalfinancialburden ofCVDtorise1044billionUSDollarsby2030.2 Hence,itisanimportantsubsistenceasitgives shapetoepidemiologicalandeconomicfuture.
1.3 Riskfactorsandhealth(y)behaviors
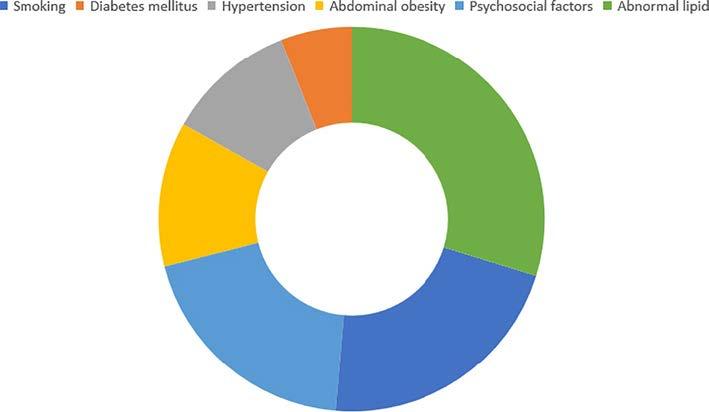
IntheFraminghamHeartStudy,sign ificantpredisposingfactorsareidentifiedforthedevelopment ofCVD.3 Theseriskfactorsarevalidatedinmanyotherstudiesand,hence,ge neratefrequentlyused predictivemodels.IntheINTERHEARTstudy, itwasshownthattherewereriskfactors(Fig.1.1) andlifestylehabitsthatleadto acutemyocardialinfarctionand eliminationorcontrolofthese riskfactorswasshowntoyieldasignifi cantdecreaseincardiovascularevents.4 WorldHealth Organizationtargetedtodecreasetheriskfactors,suchashypertension,dyslipidemia,obesity, smoking,alcohol,diet,andsedentarylifestyletill2025. 2 Controllingriskfactorsandlifestyleis ofgreatimportancewithregardtothepreventionofCVD.Whentheprevalenceoftheseriskfactors andlifehabitsisthoroughlytakenintoconsideration,itisnotabigsurprisetoseemorbidityand mortalityofCVDremainsonthetoplistinthefollowingdecadesoftheESCcountries.Riskfactors andlifestylehabitsforthede velopmentofCVDarereviewedi ndividuallyinthefollowing.
PopulationattributableriskforCVD.
1.3.1 Riskfactors
1.3.1.1 Hypertension
Hypertensionisdefinedasofficesystolicbloodpressureofmorethanandequalto140mmHgordiastolicbloodpressureofmorethanandequalto90mmHgontwooccasionsortakingantihypertensive medication.Hypertensionisoneofthemostfrequentchronicmedicalconditionsthatincreasetherisk ofimpairmentinthefunctionofheart,brain,kidney,eye,andotherorgans.TheWorldHealthOrganizationstatesthat1in4menand1in5womenintheworldhavehypertensionthatcontributesto prematuremortalityworldwide.
Itiswellestablishedthatthereisacontinuousandlinearrelationshipbetweenincreasingblood pressurelevelsandmyocardialinfarctionandstroke.5 Internationalsurveysdesignatedthatbetween 1990and2015,theprevalenceofhypertensionwasshowntoincreasesignificantlyandcontributed notonlytomortalitybutalsotomorbidity.6 IntheINTERHEARTstudy,itwasshownthat22%of allacutemyocardialinfarctioncasesarerelatedtohypertensionanditwasalsonotedthatthepresence ofhypertensionincreasedtheriskofmyocardialinfarctionatleasttwofold.7 Theprevalenceofhypertensiondiffersaccordingtogenderandincomelevelsofcountries.In2015,medianage-standardized (MAS)hypertensionprevalencealloverESCcountrieswascalculatedtobe24.8%.2 Ofnote,thehighestprevalencewasreportedinCroatiaandthelowestwasreportedintheUK(32.4%versus15.2%).It isalsoimportanttonotethattheprevalenceofhypertensioninwomenislowerthaninmeninESC countries(22.3%versus27%).Income-basedcomparisonofESCcountriesalsoyieldedinteresting resultssuchthattheprevalenceofhypertensionwashigherinlow-to-middle-incomecountriescomparedtohigh-incomecountries(23.8%versus15.7%).2 Thisfindingwasprimarilydrivenbythefact
FIG.1.1
thattheprevalenceofhypertensiondecreasedfrom1980to2015inallESCcountries(35.3%versus 24.2%)althoughitwasmuchmorestrikinginhigh-incomecountries.2 Asanimportantcontributorof CVD-relatedmorbidityandmortality,hypertensionhasnotonlybeenbetterrecognizedandmanaged inhigh-incomecountries,butalsoachievedconsiderableprogressinlow-to-middle-incomecountries.7 Inlightofthesefindings,WHOannounceditswishtodecreasetheprevalenceofhypertensionby25% bytheyear2025.2 Managementofhypertensionhasacriticalroleintheprimaryandsecondary preventionofCVD.Thisisparticularlyvalidforpatientswithdiabetesmellitus,renalfailure,and vasculardiseasebyachievingstrictcontrolofbloodpressure.Ofnote,thisachievementcanyielda significantdecreaseintheprevalenceofCVD.
1.3.1.2 Cholesterol
Cholesterol,particularlyLDLcholesterol,isasignificantpredictorofCVD,andincreasedserumconcentrationofLDLcholesterolislinearlyrelatedtoincreasedriskforCVD.8 Amongpeoplewithouta historyofCVD,i.e.,inprimaryprevention,statin-related1mmol/LdecreaseinLDLcholesterolcan decreaseCVDriskby15%.9 Justlikehypertension,theprevalenceofhighcholesterol(i.e.,hypercholesterolemia)alsodiffersbygenderorincomelevelsofcountries.Hightotalcholesterolisreportedin morethan50%ofhigh-incomeEuropeancountries,whereasitislessthan30%inAsianorAfrican countries.In2008,MAShypercholesterolemiaprevalencewas15.6%inwomenversus14.3%in menintheESCcountries.Theprevalenceofhypercholesterolemiainwomenfromhigh-incomecountriesraisedto18.8%(IQR16.5%–20.8%),comparedto11.8%(IQR9.6%–13%)prevalenceofwomen fromlow-incomecountries.Besides,theprevalencewas18.1%amongmenfromhigh-incomecountries,andamongmenfromlow-incomecountries,hypercholesterolemiaprevalencewasjust8.7%.2 Of note,similardecreasingtrendsintheprevalenceofhypercholesterolemiawasobservedinbothhighincomeandlow-incomecountries.Effectivemanagementofhyperlipidemia,notsurprisingly,can decreasenotonlytheprevalencebutalsotheincidenceofCVD.
1.3.1.3 Diabetesmellitus
Diabetesmellitusisdefinedasfastingplasmaglucosemorethanandequalto126mg/dLorcasual plasmaglucosemorethanandequalto200mg/dLtogetherwithdiabetessymptomsorHbA1clevel ofmorethanandequalto6.5%.10 Therearesixtymillionpatientswithdiabetesmellitus(DM)in Europeand422millionpatientswithDMintheworld,withthemajorityoftype2DMaccording toWHO.11 Inthelast30years,irrespectiveofgender-andincome-baseddistribution,theprevalence ofDMhasbeensignificantlyincreasingallovertheworld.Thisincreaseislinkedtoanincreasedprevalenceofobesityandoverweightpeopleinassociationwithhighcaloricnutritionandphysicalinactivityleadingtoasedentarylifestyle.ThemedianprevalenceofDMin2017is6.8%acrossESC membercountries,withthelowestfrequencyinEstonia,Ireland,andLithuaniaandthehighest frequenciesinSerbia,Albania,NorthMacedonia,Montenegro,BosniaandHerzegovina,Turkey,Lebanon,Egypt,andLibya.2 MortalityriskofpatientswithDMistraditionallyknowntobetwiceasmuch asthosewithoutDMalthoughdisparityhasbeenreportedtobelessapparentrecently.12 Morethanhalf ofthesedeathsbelongtocardiovascularsystemdiseases,particularlyischemiccardiacdiseaseand cerebrovasculardiseases.Hence,despitethedecreasingprevalenceofhypertensionandhypercholesterolemia,anincreaseinDMprevalenceseemstocompensateforanybenefitandevenfurtherincrease inCVDandassociatedoutcomes.
1.3.1.4 Obesity
Obesity,inthegeneralpopulation,iscalculatedasthebodymassindex(BMI),inwhichanindividual’s weightinkilogramsisdividedbythesquareofheightinmeters.Obesityispresentwhenbodymass indexismorethan30kg/m2,reportedbyWHOalongwithincreasingBMIcategoriesincreasingthe severityofobesity.Ofnote,apersonwithaBMImorethanandequalto25kg/m2 isconsideredoverweight.Theprevalenceofobesityisrisingnotonlyindevelopedbutalsoindevelopingcountries. Liberalisminglobaltrading,rapidurbanization,sedentarylifestylechanges,andincreasedconsumptionofanimal-derivedoilsandsugarhasbroughtaboutobesityastheepidemicofthenewcentury.13 In theworld,thenumberofobesepeopleexceededthenumberofleanpeople.InESCcountries,everyone infiveindividualsisobese.IntheESCcountries,MASBMIisreportedtobe26.6kg/m2 (IQR 26.1–27.1)withsimilarnumbersinbothgenders.GlobalBMIMortalityCollaborationreportedin 2016thatevery5kg/m2 increaseinBMIamongpeoplewithBMI 25.0kg/m2 increasedtheriskof deathby1.39-folds.14 Althoughtheprevalenceofobesityinhigh-incomecountriesishigherthanthat inlow-incomecountries,bothgroupsyieldedasignificantincreaseintheprevalenceofobesity.In 1980,obesityprevalencewas9.6%(IQR8.2%–11.9%),andthisnumberin2016hasraisedto 22.6%(IQR20.9%–25.8%).2 AnincreaseintheprevalenceofobesityalongwithDMsignificantly contributestoanuncontrollableincreaseinCVD.
1.3.2 Healthbehaviors
1.3.2.1
Smoking
Smokingortobaccousehasbeendefinedasthesinglemostpreventablehealthriskbyeveryauthority intheworld.SmokinghasbeenassociatedwithmanytypesofcancerandCVDandremainsasthe majorindicatorofmortality,particularlyprematuremortalityintheEuropeancountries.15 Everyyear, about6millionpeoplesuccumbedtodeathsecondarytosmoking-relateddiseases.Smoking prevalencein2014wasreportedtobe21%inmenandwomenwithagemorethan15yearsinthe ESCcountries.2 TheprevalenceintheESCcountriesrangesfrom11.9%inSwedento36.1%inLithuania.Smokinghasbeenmoreprevalentinmenthaninwomen.Theprevalenceofmalesmokersis higherinlow-incomecountriescomparedtohigh-incomecountries,whereastheprevalenceoffemale smokersishigherinthehigh-incomecountriescomparedtolow-incomecountries.IntheESC countries,smokingprevalencedecreasedfrom28%to21%byabout25%.2
1.3.2.2 Alcohol
Alcoholconsumptionisdefinedasthepercapitaconsumptionofpurealcoholinlitersperyearandisa EuropeanCoreHealthIndicatorandtargetofWHO.16 Excessivealcoholconsumptionisresponsible foroneineverytendeathsamongadultsand,hence,isanimportantreasonofprematuredeathinthe USA.IntheEUcountries,excessivealcoholconsumptionisalsoanimportantcontributortopremature deathaftersmokingandalcohol-abuse-relatedhypertensionisresponsiblefor60%ofallalcoholrelateddeaths.In2016,66.6%ofadultsintheESCcountriesreportedtoconsumealcoholinthelast yearwithamedianalcoholconsumptionof10.2L/capita/year.2 Ofnote,significantdifferencesexistin differentcountrieswiththehighestconsumptioninPortugal,Belgium,Bulgaria,France,Germany, Latvia,RepublicofMoldova,Romania,andSlovenia,andthelowestconsumptioninAlgeria, Azerbaijan,Egypt,Israel,Lebanon,Libya,Morocco,Syria,Tunisia,andTurkey.Ofnote,thereis nolevelatwhichchronicalcoholconsumptioncanbebeneficial,accordingtoGBD2016Alcohol
Collaboratorspaper,publishedinLancetin201817 althoughpreviousreportsdenotethatmoderationof alcoholconsumptionorlowalcoholintakeisrecommendedovernoalcohol.
1.3.2.3 Physicalinactivity
Insufficientphysicalactivitymeansapopulationwhocannotachievestrenuousexercisemorethan 75minperweekormorethan150minperweekofmoderateexercise.Physicalinactivityisassociated withaheightenedriskofischemiccardiacdisease,diabetesmellitus,andsomecancers,andisresponsiblefornearly10%ofalldeathsworldwide.18 Althoughitismorefrequentlyencounteredinfemales andhigh-incomecountries,theprevalenceofphysicalinactivityamongtheadultpopulationisreported tobe31%intheESCcountries.2
Riskfactorsandunhealthyhabitsarepotentiallyreversible.Unopposedgrowthofthecardiovasculardiseaseinseveralcountriescanonlybemitigatedbystrictcontrolofriskfactors.Otherwise,cardiovascularinterventionswiththehighcostalongwithalifelongtherapyisnotarationalapproach giventhatthepreventionisalwaysmuchcheaperthantreatment.
1.3.2.4 Vegetableandfruitconsumption
Lowfruitandvegetableconsumptioniscountedinthelistofriskfactorsfornoncommunicable diseases(NCDs)suchascancerandCVD.Inasystematicreviewof95prospectivestudies,dailyconsumptionof800goffruitandvegetablesyieldedasignificantandgradualdecreaseinCVD-related outcomes.19 InESCcountries,52.2%ofthepopulationwasnotedtoconsumeonevegetableand 55%wasnotedtoconsumeonefruitperday.2 Invegetableconsumption,Israelleadsby81%and theNetherlandsisthelowestby35%.Infruitconsumption,IsraelandItalyleadby71%.2 Vegetable andfruitconsumptionbringsaboutlessfrequentconsumptionofanimalfatandsugar.Itisclearthat fightingagainstobesity,whichisasignificantcontributortoCVD,isimportantinthismillennium, sinceincreasingvegetablesandfruitinthedietprovidesnotonlydirectbutalsoindirectbenefits forhealth.
1.4 Cardiovascularmorbidity
Morbidityisdefinedasthenumberofpatientswhosufferfromaspecificdiseasewithinatimewindow andaspecificgroup.Morbiditymeasureshavesignificantrolesindefiningepidemiologicalmetricsas theyidentifytheaffectedindividualsfromaspecificdiseaseinagivenpopulation.ForCVDmorbidity metrics,theprevalenceandincidencearemostfrequentlyutilized.Prevalencemeasuresdesignateall ofthenumberofindividualswithanexistingdiseaseinagivenpopulation.InthecaseofacuteCVD eventssuchasacutemyocardialinfarctionorstroke,theprevalenceindicatesthenumberofindividuals whosufferedfromtheseeventsinagivenpopulation.However,theincidencedesignatesindividuals withneweventsinagivenperiodandhenceprovidesametricfornewdiseaseoccurrence.
Indiseaseswithveryhighfatalityratessuchasacutemyocardialinfarctionandstroke,morbidityis ascriticalasmortalitysincethosepatientswhosurviveddiseaseswithhighmortalitybringabouta significanttreatmentburdenirrespectiveofthehealingstatusofthepatients.Hence,morbiditystatisticsaretheimportantdeterminantsofcountryreflexesthatareexecutedtopreventandmanagethe diseases.
1.4.1 Incidenceandprevalenceofcardiovasculardisease
Currentstateofknowledgeindicatesthatin2017therewere19.9millionnewcasesin54ESCcountries.2 Ofnote,MASincidenceofCVDwas1133per100,000populationofeachmembercountry, rangingfromthecountrieswiththelowestnumberssuchasArmenia,Kyrgyzstan,Lebanon,and TurkeytothosewiththehighestnumberssuchasAustria,CzechRepublic,Finland,Luxembourg, Romania,andSlovenia.2
However,whenitcomestogender-basedcomparison,newcasesofCVDalloverESCcountriesare morefrequentinfemalescomparedtomales(10.3millionvs.9.6million);however,theagestandardizedmedianrateinwomenis1006per100,000people,thatislowerthan1291per 100,000peoplethemedianrateofmen.2
Theincome-basedcomparisonyieldsasignificantdifferencebetweenthelow-to-middle-income countries(1039per100,000inhabitants)andhigh-incomecountries(1224per100,000inhabitants) andwiththelatteronehavingmorefrequentCVDincidence.Incomparisonwith1990versus2017 data,CVDincidenceisnotedtoslightlydecrease(1186versus1133per100,000inhabitants),driven by43countriesalthough11countrieswerereportedtohavesomeincrease.2 Onthecontrary,CVD prevalenceisreportedtobe108.7millionpatientsintheESCcountrieswithaMASprevalenceof 6595per100,000inhabitantsalongwiththelowestprevalenceof5254per100,000inhabitantsin Norwayandwiththehighestprevalenceof8766per100,000inhabitantsinBulgaria.Ofnote,theoverallcomparisonofcountryincomelevelsyieldedthatCVDprevalence,justlikeincidence,wasmore frequentinlow-to-middle-incomecountriescomparedtohigh-incomecountries(7022versus6245per 100,000inhabitants).ThecomparisonofCVDprevalencebetween1990and2017yieldedsimilardecreasingtrendslikeincidence(7155versus6595per100,000inhabitants).However,thisdecreasedoes notseemtocompensatefortheincreasedfinancialburdenofCVD.Itisinterestingtonotethatthereare morefemaleswithCVD(i.e.,prevalence)comparedtomalesintheESCcountries(55.7millionversus 52.9millionconsecutivelyoutof108.7million).2
1.4.1.1
IncidenceandPrevalenceofischemicheartdisease
IschemicheartdiseasehasthehighestincidenceamongalloftheCVDby3.6millioncasesintheESC countries.IntheESCcountries,MASrateofischemicheartdiseaseis176.3per100,000inhabitantsin bothgendersand132and235.9per100,000inhabitantsinfemalesandmales,respectively.Ofnote,the rateswerenotedtobethehighestinEgypt,Morocco,andBelarusinfemalesandinAzerbaijan,Belarus,andEgyptinmales,andthelowestinPortugal,Cyprus,Malta,Spain,andLuxembourg.2 Onthe contrary,theincidenceofischemicheartdiseaseisdecreasingfrom1990to2017intheESCcountries (273to176.3per1000.000inhabitants).TheprevalenceofischemicheartdiseaseintheESCcountries isreportedtobe34.9millionandmorefrequentlyencounteredinmalesthanfemales.Contrarytoincidence,theprevalenceofischemicheartdiseaseismorefrequentinhigh-incomecountriescompared tolow-to-middle-incomecountries(2503vs.1527per1000.000inhabitants).Temporaltrendof1990 to2017designatedthatprevalencehasalsodecreasedinparalleltoincidence(2482vs2270per100 0.000inhabitants).2
1.4.1.2
Incidenceandprevalenceofstroke
Strokeremainsthesecondafterischemicheartdiseaseby2.3millionnewcasesinESCcountriesin 2017.Medianage-standardizedincidencewas143.4per100,000inhabitantsforallESCcountries.2 AmongESCcountries,strokenumbersforbothgenderswerehighthrougheasternEuropeandNorth
Africawiththelowestnumberof82.8per100,000inhabitantsinItalyandwiththehighestnumberof 213.4per100,000inhabitantsinEgypt.TheoverallstrokeincidenceinESCmembercountries remainedsimilarbetweentwogenders(femalesversusmalesand1.2millionversus1.1million, respectively).However,MASrateper100,000peoplewaslowerinfemalesthanmales(130.3vs. 159.9).2 Strokeincidencewashigherinlow-incomecountriesjustlikeanischemiccardiacdisease. Furthermore,acomparisonof1990versus2017yieldedthatstrokeincidenceisdeclining(172.9vs 143.4per100.000inhabitants).StrokeprevalenceinESCcountrieswasreportedto20.4millionwith 11.4millionmalesand9.06millionfemales.Justlikeincidence,theprevalenceofstrokeishigherin low-incomecountriescomparedtohigh-incomecountries(1542vs.942per1000.000inhabitants).2 Althoughthereisadecliningtrendforstrokeprevalencebyyears(1405versus1276per100,000 inhabitants),low-incomecountrieslikeAzerbaijanandBosniaandHerzegovinareportanincrease intheprevalenceofstrokeovertime.2
1.4.1.3 Incidenceandprevalenceofperipheralvasculardisease
PeripheralarterydiseaseremainsinthethirdpositionamongallCVDbyannual2.2millionnewcases. Herein,MASnumberofnewcasesper100,000inhabitantswerereportedtobe132.2withthelowest incidenceinNorwayandthehighestinDenmark.2 Theincidenceofperipheralarterydiseaseremains similaraccordingtogenderandcountryincomelevels.From1990to2017,theincidenceofperipheral arterydiseasewasshowntodecreasefrom136.8to132.2per100,000inhabitants.Despitedecreasing trendsinincidence,age-standardizedincidenceseemedtoincreasein54ESCcountrieswiththeUKin theleadingposition.2 In2017,therewere25.8millionpeoplelivingwithperipheralarterydiseasein the54ESCcountries.2 Ofnote,MASprevalenceofperipheralarterydiseasewas1460per100,000 inhabitantswiththelowestnumberof1061inNorwayandthehighestnumberof2204inDenmark.2 Thereweremorefemalesthanmaleslivingwithperipheralarterydisease(13.8millionvs.12.0million)throughESCcountries.2 However,MASprevalenceforperipheralarterydiseasewassimilarin bothgenders.From1990to2017,MASprevalenceofperipheralarterydiseaseremainedrelatively stableinESCcountries(1468per100,000inhabitantsin1990and1460per100,000inhabitantsin 2017).2 Ofnote,37countriesreportedsmalldeclinesmorethan20%inItaly,Norway,andtheUK intheage-standardizedprevalenceofperipheralarterydiseasealthough17countriesinESCreported smallincreasesinprevalencenotexceeding8%.2
1.4.1.4 Incidenceandprevalenceofheartfailure:growingproblem
Heartfailure(HF)asaprogressiveclinicalsyndromeisconsideredasthelatemanifestationofdifferent phenotypicexpressionsofCVD.Itishemodynamicallycharacterizedbyimpairedcardiaccontractility and/orrelaxation.Ithasbeenreportedindifferentepidemiologicalstudiesrangingfrom1%to3%of thewholepopulation.Bygrowingincidenceofsurvivorsoflong-termhypertension,diabetesmellitus, acutecoronarysyndromeswiththehelpofbetterimplementationofevidence-basedmedicine,andrevascularizationstrategies,despitedecreasingtrendsinsomeoftheCVdiseases,HFaschronicandlate phaseofseveralCVproblemssecondarytomanyetiologiesisexpectedtorisebyprevalenceglobally (Fig.1.2).
Heartfailurehasatleastthreephenotypes,asdefinedbyESCHFguidelines:Heartfailurewith reducedejectionfraction(HFrEF),heartfailurewithmid-rangeejectionfraction(HFmrEF),andheart failurewithpreservedejectionfraction(HFpEF).20 IntheESCHFlong-termregistry,distributionof HFrEFversusHFmrEFversusHFpEFwasasfollows:59.8%vs.24.2%vs.16%althoughitranged
Contributionofriskfactorstoheartfailure. ACS,acutecoronarysyndrome; CCS,chroniccoronarysyndrome.
from40.6%to70.6%vs11.8%to45.6%vs10.6%to18.4%.21 Ofnote,1-yearmortalityrateswere reportedtobe8.8%inpatientswithHFrEF,7.6%inpatientswithHFmrEF,and6.4%inpatientswith HFpEFinESCHFregistry.21 Onthecontrary,epidemiologicaldatafromtheUSAtellsadifferentstory withincreasingtrendsinHFpEFprevalence.22,23
Accordingtoonestudy,theincidenceofHFrEFandHFpEFforaperiodof20yearsrangingfrom 1990to2009wasthoroughlyevaluatedanditwasfoundthatinthefirsthalfofthe20-yearfollow-up, 1367incidentHFeventswerereported(2524inthewhole20-yearfollow-up).23 Outof1367,491 (33%)werereportedtobeHFrEFand309(29%)werereportedtobeHFpEF.Foreach1-year follow-up,age-andsex-adjustedstandardizedincidenceratesforthefirsthalfandthesecondhalfwere calculatedtobe19.7and18.9per1000persons,respectively.23 Thispracticallymeanstheoverall incidenceofHFremainedstableduring20-yearfollow-up.However,whenphenotypesofHFwere concerned,incidencerateofHFpEFwas1.53(P < 0.0001)althoughtheincidencerateratioofHFrEF wasfoundtobe0.80(P ¼ 0.0029).23 Hence,thisphenotype-basedresultpracticallymeansthereisa declineintheincidenceofHFrEFduring20-yearfollow-up,alongwiththeapparentincreaseinHFpEF incidence,compensatingforthedecreasingincidenceofHFrEF,overthisperiod.Ofnote,itseems thereisadeclineintheincidenceofHFrEF,particularlyinmen,andariseintheincidenceofHFpEF inbothgenders.23
InESCHFregistry,thepatientswithHFrEFwereyoungerthanthepatientswithHFpEF,as frequentlyreported.21 ContrarytoHFpEF,whichmainlyaffectsfemaleelderly,malesweremorelikely tosufferfromHFrEF,sinceischemicetiologywasmorecommonlyreportedinHFrEFthaninHFpEF. Onthecontrary,hypertension,diabetes,andAFweremorefrequentlyreportedinHFpEF.21
Heartfailureyieldssignificantmorbidityandmortalityandbringsasubstantialburdentothe healthcaresystemallovertheworld.Ofnote,HFisaleadingcauseofhospitalizationamongadults andtheelderly.24 HoweveralthoughthelifetimeHFdevelopingriskisreportedtobe20%between40 and80yearsofageforbothgenders,25 HFburdenincreasesbyincreasingageamongtheadultsand elderlypopulation.24 Firstofall,theprevalenceofHFisnotedtobedoubledbyeachdecadeoflife.
FIG.1.2
Hence,theprevalenceofHFislessthan1%amongpeoplewith <40yearsand10timesmorefrequent by80yearsofage.26 Weareallawarethatimprovementsinmedicaltherapyandrevascularizationand healthylifestyledelayedthedevelopmentofHF,andbyprolongingthelivesofthosewhohadCVD, theburdenofHFhasbecomemoreapparentbyincreasingage.ThispracticallymeansgeriatricmedicineshouldbeanintegralpartofHFmanagement.Secondly,halfofthepatientshospitalizedwithHF areolderthan75years.26 Hence,managementinthehospitalshouldalsoconsidergeriatricprinciples. However,contrarytoregistries,drugtrialshavetendedtoexcludetheseelderlypopulations,further researchinthisgeriatriccohortisstillneeded.26
GlobalfinancialburdenofHFisreallyhardtoaccuratelyestimateduetolimiteddata.Withthehelp ofknownnationalhealthexpenditures,someestimationsareprovidedintheliterature.IntheUSA,HF prevalenceofHFisexpectedtoincreaseby46%,totalmedicalcostsareexpectedtorisefrom20.9 billionUSDollarsto53.1billionUSDollarsfrom2012to2030andthemajorityoftheseexpenses arelinkedtoincreasedhospitalizations.27 HeartfailureistheleadingprimarydiagnosisforhospitalizationintheUSA,andthenumberofhospitalizationsthatincludedHFasaprimaryorsecondary reasontripledintwodecadesalthoughtheaveragelengthofstayshortenedconsiderably.27
Ofnote,indirectcostsinrelationtodisabilitiesandprematuremortalityareestimatedtoincreaseto asimilarextent.Eventhoughhigh-incomecountriesconstitute18%oftheworldpopulation,morethan two-thirdsoftheworldwideexpenditureforHFwasconsumedinhigh-incomecountries.28 Furthermore,inhigh-incomecountries,HFisthemostfrequentdiagnosisinthehospitalizedgeriatricpatients andHFhospitalizationrepresents1%–2%ofallhospitaladmissions.28
SimilartrendsarealsoreportedinESCcountries.IntheUK,HFaccountedfor5%ofallhospital admissionsfromtheemergencydepartment.29 HFhospitalizationsareexpectedtoriseby >50%bythe year2035,duetotheagingpopulation.29 Heartfailurehospitalizationrateswerestablebetween2000 and2010althoughinpatientmortalitydecreasedby3.3%peryearonaverageinFranceasanexample inEurope.30,31 Ofnote,therewasadecreaseinmalepatientshospitalizedforHFalongwithareductioninmortalityalthoughtherewasasignificantdecreaseinHFmortalityinfemales.31 Heartfailurerelatedhospitaladmissionswerethehighestinthe1990sintheNetherlands,Scotland,andSweden, thenadeclinewasnoted.30
1.4.1.5 Incidenceandprevalenceofatrialfibrillation
Intheyear2017,therewere0.75millionnewcasesofatrialfibrillation(AF).2 MASnumberofnew caseswas44.3per100,000inhabitants.TheincidenceofAFissimilarinbothgendersanditismore prevalentinhigh-incomecountries.Herein,MASincidenceofAFlookssimilarincomparisonwith 1990and2017(44.7versus44.3per100,000inhabitants).2 StabilityoftheincidenceofAFcontributes toanincreaseinCVDsignificantlysinceatrialfibrillationisprognosticallyimportantmainlyby thromboemboliccomplications.
In2017,therewere10.0millionpeoplelivingwithAFinthe54ESCmembercountries.2 Acrossall ESCmembercountries,MASprevalenceofAFwas571.8per100,000inhabitantswiththelowest numberof265.7inTurkeyandthehighestnumberof806.1inSweden.2 Therewerefewerwomen thanmenlivingwithAF(4.6millionvs.5.4million)inESCcountries.TheMASprevalencefor AFwaslowerforwomenthanmen(436.8versus752.5per100,000inhabitants).TheMASprevalence ofAFwaslowerinmiddle-incomecountriescomparedtohigh-incomecountries(531.3versus608.7 per100,000inhabitants)inbothfemalesandmales.2 MASprevalenceofAFremainedstablefrom1990 to2017(589.5in1990and571.75in2017per100,000inhabitants).2 12Chapter1
1.5 Disability-adjustedlifeyearsduetocardiovasculardisease
ItisalsowellestablishedthattheburdenofCVDappearsatanearlyage,notonlyasprematuremortality,whichcouldbedefinedasmortalitybeforetheageof70years,2 butalsoasmorbidity,definedas disability-adjustedlifeyears(DALYs)measure.In2017,themedianage-standardizedDALYsdueto CVDwascalculatedtobe4530per100,000inhabitantsofESCcountries,withthehighestDALYs numberinUkraineandEgyptandwiththelowestDALYsnumberinSwitzerland,Israel,andFrance.2
Ischemiccardiacdiseaseandstrokeareresponsibleformorethantwo-thirdsofDALYsdueto CVD.IntheESCcountries,ischemiccardiacdiseaseandstrokeareresponsibleformorethantwothirdsofDALYsduetoCVD.2 Onthecontrary,peripheralarterydiseaseandAFcorrespondto3% lessofDALYsofischemiccardiacdisease.2 DALYsdifferbygenderandincomelevelsofdifferent countries.Formales,MASDALYsnumbersper100,000inhabitantsduetoCVDwere5925per 100,000inhabitantswiththelowestDALYsnumberof1938inSwitzerlandandwiththehighest DALYsnumberof15,077inUkraine.Themedianage-standardizedDALYsnumberswere3219 per100,000inhabitantsforfemalesduetoCVDwiththelowestDALYSnumberby1114inFrance andwiththehighestDALYsnumberof7657inMorocco.2 AlthoughDALYswereclosetoeachother betweenthegendersat951forfemalesversus1255per100,000inhabitantsformalesforstroke,ischemicheartdiseasecreatedamajordifferencebetweenmalesandfemaleswithanearlythreefold differenceinmedianvaluesforDALYs:3145versus1384per100,000inhabitants,respectively.2 Whenitcomestoincomecomparison,themediannumberofage-standardizedDALYsduetoCVD was7160per100,000inhabitantsinmiddle-incomecountriescomparedto2235per100,000inhabitantsinhigh-incomecountries.Ofnote,MASDALYsduetoischemiccardiacdiseasewas3910per 100,000inhabitantsinmiddle-incomecountriescomparedto1042per100,000inhabitantsinhighincomecountries.2 Forstroke,thedifferencewas2183DALYsper100,000inhabitantsversus546 DALYsper100,000inhabitantsinmiddle-incomecountriesandhigh-incomecountries,respectively.2 However,from1990to2017,age-standardizedDALYsduetoCVDper100,000inhabitantsofESC countriesdecreasedfrom7542to4530withsignificantdeclinesinNorway,Denmark,Ireland,Portugal,andIsraelandwithanincreaseinAzerbaijanandBelarus.Notonlyischemicheartdiseasebutalso strokecontributedsignificantlytothedecreasedratesinDALYsduetoCVD.Medianage-standardized DALYsforischemicheartdiseasewentdownto2186DALYsper100,000inhabitantsfrom4069in ESCcountries.Ofnote,Azerbaijan,Belarus,Kyrgyzstan,Libya,andUkrainerecordedanincreasein age-standardizedDALYsduetoischemicheartdisease.Furthermore,age-standardizedDALYswent downto1141forstrokefrom2035per100,000inhabitantsalthoughAzerbaijanreportedanincreasein DALYsduetostroke.2
Globally,all-causeDALYsinallagesis2.3billion.Comparedto2007,in2017,all-causeDALYs inallageswerereportedtodecreaseslightlyby1.5%.Globally,thelargestcontributiontoDALYsis derivedfromNCDs.Thiswasfollowedby27%ofinfectious,maternal,neonatal,andnutritionaldiseases,andtheninjurieswith10.1%came.NoncommunicablediseasesincreasedDALYsrateby40.1% althoughage-standardizedDALYsratedecreasedby18%.32
Ofnote,asanimportantdimensionofall kindsofdiseasestates,leadingcausesofDALYsgloballyhadbeenreportedtobeneonataldisordersin 1990,2007,and2017amongfemaleswithischemicheartdiseasebecomingthesecondin2017. Amongmales,leadingcausesofDALYswereneonataldisordersin1990,neonataldisordersin 2007withischemicheartdiseasebeingthesecondmostcommon,andin2017ischemicheartdisease istheleadingcauseofDALYs.32
TheWorldHealthOrganization(WHO)hasbroadcastNCDtargetsinrelationtoglobalcardiovascularhealthandpointedoutthatwithreferenceto2010,by2025,a25%relativereductioninCVD mortalityisplannedontopofotherNCDssuchascancer,hypertension,diabetes,obesity,orchronic respiratorydiseases.33 Ofnote,ifachieved,themajorityofreductionisexpectedtoderivefromlow-tomiddle-incomecountries33 sinceNCD-relatedmortalityisstillhighinlow-to-middle-income countries,andamongpeoplewithlowersocioeconomicstatusinhigh-incomecountries.34
1.6 Mortalityincardiovasculardisease
Mortalitystatisticsarefrequentlyutilizedindiseasesurveillance.Deathsecondarytoadisease,particularlyasinthecaseofCVD,canbeusedasamarkerofaburdentoapopulation.Althoughitis dependentoncountry-basedregistration,mortalityisthemostaccrediteddata,whichcanreadilybe obtained.Mortalityinrelationtoadiseasedesignatestheabsoluteburdenofthatdiseaseinthepopulation.CardiovasculardiseaseisthemostfrequentreasonforprematuremortalityintheEuropean countriesalthoughtheprevalenceofithasbeensteadilydecreasing.35 AlthoughCVD-relatedmortality exceedsmortalityrelatedtocancer,cancer,inthesedays,leadtomoredeaththanCVDinmanycountries.Cancer-relatedfemaledeathsaremorecommonthanCVD-relateddeathsinDenmark,Israel, Netherland,SanMarino,andtheUK.Besides,inBelgium,Denmark,France,Ireland,Luxembourg, Netherland,Norway,Portugal,SanMarino,Slovenia,Spain,Switzerland,andtheUK,cancer-related maledeathsexceededCVD-relatedmaledeaths.2 ItisimportanttonotethatcountriesinwhichcancerrelateddeathexceedsCVD-relateddeathsarethosewithhighincome.
CardiovasculardisordersarethemostfrequentreasonfordeathinESCcountries,accountingfor 2.2milliondeathsinwomenand1.9milliondeathsinmen,inthemostrecentyearofavailabledata thesenumbersdesignate47%and39%ofalldeathsinwomenandmen,respectively.2 Onthecontrary, ischemicheartdiseaseaccountsfor38%ofCVD-relateddeathsinwomenand44%inmen.Strokeis thesecondmostfrequentreasonforCVD-relateddeaths,responsiblefor26%ofallCVDdeathsin womenand21%inmen.2
Inbothwomenandmen,CVDisresponsibleformoredeathsinmiddle-incomecountriescompared tohigh-incomecountries.
1.7 Prematurecardiovascularmortality
Cardiovasculardiseaseriskincreasesbyagingandasthepopulationgetsolder,aging-relateddiseases areexpectedtoincrease.36 Prematuremortalityisaworrisomeconsequenceofpreventablediseases. PrematureCVDmortalityisareflectionofuncompletedlifeexpectancy,andhence,significanteffort hastobeputonforprevention.37 Althoughitlacksconsensusdefinition,prematuremortalityisdefined asdeathinpeoplelessthan65to75yearsofage.Onthecontrary,WHOaccepts70yearsofageto defineprematuremortality.38 IncomparisonwithmortalityofallagecategoriesintheESCcountries, CVDaccountsforasmallportionofdeathinbothwomen(30%)andmen(33%).Thisnumerically means323,000deathsinwomenand699,000deathsinmen.2 Althoughitisasmallportion,thismortalityratesecondarytopreventablecausesremainsconcerning.