https://ebookmass.com/product/encyclopedia-of-respiratorymedicine-laurent-g/
Instant digital products (PDF, ePub, MOBI) ready for you
Download now and discover formats that fit your needs...
Encyclopedia of Cardiovascular Research and Medicine 1st Edition Douglas B. Sawyer
https://ebookmass.com/product/encyclopedia-of-cardiovascular-researchand-medicine-1st-edition-douglas-b-sawyer/
ebookmass.com
Murray & Nadel's Textbook of Respiratory Medicine 7th Edition Various Authors
https://ebookmass.com/product/murray-nadels-textbook-of-respiratorymedicine-7th-edition-various-authors/
ebookmass.com
International Encyclopedia of Transportation Roger Vickerman
https://ebookmass.com/product/international-encyclopedia-oftransportation-roger-vickerman/
ebookmass.com
Without Saying Goodbye Laura Jarratt
https://ebookmass.com/product/without-saying-goodbye-laura-jarratt/
ebookmass.com
Kingsbane Claire Legrand https://ebookmass.com/product/kingsbane-claire-legrand/
ebookmass.com
Fundamentals of congenital minimally invasive cardiac surgery Stellin
https://ebookmass.com/product/fundamentals-of-congenital-minimallyinvasive-cardiac-surgery-stellin/ ebookmass.com
Down the Hill Susan Hendricks
https://ebookmass.com/product/down-the-hill-susan-hendricks/
ebookmass.com
Lavinu2019s Radiography for Veterinary Technicians E Book 6th Edition, (Ebook PDF)
https://ebookmass.com/product/lavins-radiography-for-veterinarytechnicians-e-book-6th-edition-ebook-pdf/ ebookmass.com
Promise Boys Nick Brooks
https://ebookmass.com/product/promise-boys-nick-brooks-2/ ebookmass.com
https://ebookmass.com/product/investments-13e-13th-internationaledition-zvi-bodie/
ebookmass.com
INTRODUCTION Respiratorydiseasesrepresentoneofthelargesthealthproblemswordwide.Diseasessuchasasthmaand thesmokingrelateddiseasesarealreadycommonandincreasingsoweurgentlyneedbetterapproaches totreatorcurethesediseases.Atthesametime,newrespiratorydiseasessuchasthoseassociatedwithviruses threatenpandemicsthatchallengeournationalhealthsystems.
Withthesecontinuedchallengesfornewtreatmentwithbetterpatientcare,clinicalandrespiratoryresearchers havesoughtbetterapproachestoallaspectsofpatientcarefromimproveddiagnosestosuperiortherapies. Thishasleadtoanexplosionofnewresearchwithanincreasinglybetterunderstandingofhowtodiagnose diseasesandthendevelopnewtherapies.Thus,forexampleeverimprovingtechnologiesforimaginglung diseasehaveleadtoincreasinglybetterdiagnoses,althoughchallengesremainasweseektofurtherimprove resolution.Atthesametime,therevolutioninmolecularbiology,culminatingwiththepublicationofthe completehumangenome,hasleadtohopesforfindingmoreprecisecluestodiseasesusceptibilitypathogenesis ingeneticanalysis.Thisisleadingtonewconceptsinpharmacogenomicsaswestarttousenewdrugs, includingthoseusedforlungcancers,beingdirectedatmutationsassociatedwithdisease.
ThisisthefirstEncyclopaediaofRespiratoryMedicine.Itisourhopethatitiscomprehensiveandcaptures thekeyaspectsofcurrentpatientcare,aswellastheexcitingdevelopmentsinrespiratorysciencethatweall believewilleventuallyleadtobetterpatientcareinthetwentyfirstcentury.
Thisencyclopaediaiscomprehensiveinscopeandprovidesclinicianandresearcherwithasnapshotofthe currentstateofknowledgeinrespiratorymedicine.Allentrieshaveadheredtoastructuredlayout,starting withanabstractcrystallizingthekeyfactsandfinishingwithreadinglistsforthosewhowanttodelvefurther intothesubject.Inaddition,mostentrieshaveacolourdiagramdesignedtohelpunderstandingandprovidea valuableaidforundergraduateandpost-graduateteaching.
Theseareexcitingtimesforrespiratorymedicine.Wehopethisencyclopediawillbecomeavalubletoolfor cliniciansandresearchesatallstagesoftheircareersfromthosebeginningtheircarreerstothoseestablished butwantingtoupdatethemselvesonthenewdevelopments.
Finally,wewouldliketothankourAdvisoryEditorialBoardwhohelpedsomuchinshapingthecontentsof thisworks,aswellastheauthorswhowrotethearticlesandfacedthechallengeofcondensingareasof respiratorymedicine,oftenthesubjectofentiretextbooks,intoashortarticleof4000wordsorless.
FOREWORD Animalslivebytwoprincipalthings,foodandbreath.Ofthese,byfarthemostimportantistherespiration,forifitisstopped,theman willnotendurelong,butimmediatelydies.–AretaeustheCappocian(150–200AD)
Ofcourse,notallmedicalspecialistswouldagreewiththisstatement,andthosewhodisagreewouldbe quicktopositthatitisthefailureof‘‘their’’particularorganthattendstocauseimmediatedeath. However,thatisnottheissue.Thepointofthisquotationistoillustratethattheproperfunctioningofthelung hasbeenasubjectofgreatinterestforcenturies.TheGreekphysicianAretaeusdevotedmanyofhis observationstodiabetes,buthismanuscript‘‘OntheCausesandIndicationsofAcuteandChronicDiseases’’ alsodiscussedlungdiseases,suchaspneumonia.Sincehistime,greatnumbersofphysiciansfromallcontinentsandcultureshavecontributedtoourknowledgeofrespiratorydiseases.
Whileacknowledgingourrichhistoryofdiscoveriesaboutpulmonaryandrespiratorymedicine—discoveriesthatweremadebymenandwomenwhosenamessymbolizethegreatjourneyofthisspecialty—one mustconcedethatthefieldexperiencedanextraordinarygrowthspurtbeginninginthe1940s.Knowledgeof respiratoryphysiology,whichdevelopedveryfastduringWorldWarII,createdatidalwaveofinterestthat continuedforyearsafterward.Theabilitytomeasureandunderstandrespiratoryphysiologyanditsalterationsbecameadiagnostictool,anditopenedthedoortotherapeuticorrespiratorysupportprocedures.
But,then,inthe1950sand1960scellbiologyandsubcellularresearchenteredthescene.Thepotentialof molecularbiologyandgeneticswasquicklyrecognized,andrespiratorymedicineappreciatedthatabetterunderstandingofnormalanddisorderedbiologicalrespiratoryprocesseshingedonuseofthesenewapproaches. Lungandrespiratoryresearchers,impelledinpartbytheever-increasingpublichealthburdensofrespiratory diseases,seizedtheopportunity.Thestagewassetforprogresstooccur.Thearchitectsofthis‘‘revolution’’in respiratorymedicinearewellknown;itisourgoodfortunethatmanyhavecontributedtothesefourvolumes.
Fourvolumes! Encyclopedia! Indeed,thesefourvolumestrulyconstituteanencyclopediaofpulmonarybiologyandrespiratorymedicine!
Respiratorymedicineisstillgrowing.Becauseitissuchadynamicandexcitingfield,newinvestigatorswill almostsurelywanttobepartofit.However,todosotheywillneedtoknowabouttheestablishedstateof knowledgethatwillbethebasisoftheirwork.Newinvestigatorsinthescienceofrespiratorymedicine, whetherinterestedinfundamentalresearchorclinicalresearchorapplication,willfindideasandinspirationin thesevolumes.Allofthetoolsofthetradeareassembledtherein.
Asnoted,respiratorymedicinehasbeenaprogressiveandexpandingfieldbut,asisthecasewithmanyfields ofmedicine,thetransferofwhatweknowtothegeneralpracticeofmedicinehasbeenslowandlimited. Translation,asitiscalled,isanemergingdisciplineinneedofassistance;fortunately,thebreadthofthe knowledgepresentedinthesevolumesprovidestoolstofacilitatethistranslationprocess.
Thisfour-volumeencyclopediais,atonce,bothatributetothecenturiesofpioneeringinvestigationsinthe fieldofrespiratorymedicineandafoundationforevengreateraccomplishmentsinthefuture.Thepresentation ofallthisknowledgeintheseexcellentandcomprehensivevolumescanonlyservetostimulatefurtherworkof equalorsurpassingsignificance.Theeditorsandtheauthorsaretobecommendedfortheircontributionsto thissingulareffort.Becauseoftheirwork,respiratoryscienceandmedicinewilladvancefasterandpatients worldwidewillbethebeneficiaries.
ClaudeLenfant,MD Gaithersburg,Maryland
NotesontheSubjectIndex Tosavespaceintheindex,thefollowingabbreviationshavebeenused:
ALIacutelunginjury
ARDSacuterespiratorydistresssyndrome
BALbronchoalveolarlavage
BPDbronchopulmonarydysplasia
CAPcommunity-acquiredpneumonia
CFTRcysticfibrosistransporterregulation
COPcryptogenicorganizingpneumonia
COPDchronicobstructivepulmonarydisease
CWPcoalworkers’pneumoconiosis
G-CSFgranulocytecolony-stimulatingfactor
GERDgastroesophagealrefluxdisease
GM-CSFgranulocyte-macrophagecolony-stimulatingfactor
HUVShypocomplementemicurticarialvasculitissyndrome
ILinterleukin
IPFidiopathicpulmonaryfibrosis
IPHidiopathicpulmonaryhemosiderosis
MCPmonocytechemoattractantprotein
M-CSFmacrophagecolony-stimulatingfactor
MIPmacrophageinflammatoryprotein
MMPmatrixmetalloproteinase
NSCLCnon-smallcelllungcarcinoma
PPARperoxisomeproliferator-activatedreceptor
SCLCsmall-celllungcarcinoma
SPsurfactantprotein
TGFtransforminggrowthfactor
TIMPtissueinhibitorofmetalloproteinases
TNFtumornecrosisfactor
VEGFvascularendothelialgrowthfactor
EditorialAdvisoryBoard KennethB.Adler, NorthCarolinaStateUniversity,Raleigh,NC,USA
PeterJ.Barnes, ImperialCollegeLondon,UK
PaulBorm, ZuydUniversity,Heerlen,TheNetherlands
ArnoldR.Brody, TulaneMedicalSchool,NewOrleans,LA,USA
RachelC.Chambers, UniversityCollegeLondon,UK
AugustineM.K.Choi, UniversityofPittsburgh,PA,USA
JackA.Elias, YaleUniversitySchoolofMedicine,NewHaven,CT,USA
PatriciaW.Finn, UniversityofCaliforniaSanDiego,LaJolla,CA,USA
StephenT.Holgate, UniversityofSouthampton,Southampton,UK
StevenIdell, TheUniversityofTexasHealthCenteratTyler,TX,USA
SebastianL.Johnston, NationalHeartandLungInstitute,ImperialcollegeLondon,UK
TalmadgeE.King,Jr, UniversityofCalifornia,SanFrancisco,CA,USA
StellaKourembanas, Children’sHospitalBoston,HarvardMedicalSchool,Boston,MA,USA
Y.C.GaryLee, UniversityCollegeLondon,UK
RichardMarshall, UniversityCollegeLondon,UK
SadisMatalon, UniversityofAlabama,Birmingham,AL,USA
JoelMoss, NationalInstitutesofHealth,Bethesda,MD,USA
WilliamC.Parks, UniversityofWashington,Seattle,WA,USA
CharlesG.Plopper, UniversityofCalifornia,Davis,CA,USA
BruceW.S.Robinson, TheUniversityofWesternAustralia,Nedlands,Australia
NeilSchluger, ColumbiaUniversityCollegeofPhysiciansandSurgeons,NewYork,NY,USA
EdwinK.Silverman, BrighamandWomen’sHospitalBoston,MA,USA
EricS.Silverman, BrighamandWomen’sHospital,Boston,MA,USA
PeterSly, InstituteforChildHealthResearch,WestPerth,Australia
KingmanStrohl, CaseWesternReserveUniversity,Cleveland,OH,USA
TeresaD.Tetley, ImperialCollegeLondon,UK
JohnB.West, UniversityofCalifornia,SanDiego,CA,USA
Editors GeoffreyJLaurent, RoyalFreeandUniversityCollegeMedicalSchool,London,UK
StevenDShapiro, BrighamandWoman’sHospital,Boston,USA
Dedication Tomyfamily,Lal,Guy,DavidandGabrielle(GJL).
MycontributiontothisworkwouldnothavebeenpossiblewithouttheloveandsupportfrommywifeNicole andmydaughtersCalli,Tess,Skylar,andEllery.Ialsothankmymentorsandtraineesformycontinual educationandtheDivisionofPulmonaryandCriticalCareMedicineatBrighamandWomen’sHospitalwho tookcareofourpatientsallowingmethetimetoundertakethisproject(SDS)
PermissionAcknowledgments ThefollowingmaterialisreproducedwithkindpermissionofLippincottWilliamsandWilkins
Figure4and8ofARTERIALBLOODGASES
Table1ofARTERIESANDVEINS
Figure2and3ofBREATHING|BreathingintheNewborn
Figure2a,2b,3,4and5ofDRUG-INDUCEDPULMONARYDISEASE
Table1,2and3ofDRUG-INDUCEDPULMONARYDISEASE
Figure2ofENVIRONMENTALPOLLUTANTS|Dieselexhaustparticles
Figure4ofEXERCISEPHYSIOLOGY
Figure2ofFLUIDBALANCEINTHELUNG
Figure2ofGASTROESOPHAGEALREFLUX
Figure2ofGENEREGULATION
Figure2ofHIGHALTITUDE,PHYSIOLOGYANDDISEASES
Figure2and3ofIDIOPATHICPULMONARYHEMOSIDEROSIS
Table1ofIDIOPATHICPULMONARYHEMOSIDEROSIS
Figure1,2and3ofOXYGEN-HEMOGLOBINDISSOCIATIONCURVE
Figure10a,10band11aofSYSTEMICDISEASE|EosinophilicLungDiseases http://www.lww.com
ThefollowingmaterialisreproducedwithkindpermissionofNaturePublishingGroup
Figure2ofCOAGULATIONCASCADE|iuPA,tPA,uPAR
Figure1ofCOAGULATIONCASCADE|TissueFactor
Figure1aofMATRIXMETALLOPROTEINASES
Figure1ofMYOFIBROBLASTS
Figure1ofVESICULARTRAFFICKING
http://www.nature.com/natureandhttp://www.nature.com/reviews
ThefollowingmaterialisreproducedwithkindpermissionofTaylor&FrancisLtd
Figure2ofAUTOANTIBODIES
Table1ofBASALCELLS
Figure1ofNEUROPHYSIOLOGY|NeuroendocrineCells
Table1ofNEUROPHYSIOLOGY|NeuroendocrineCells
Figure1and2ofSURFACANT|Overview
Tables1,2,3and4ofSURFACANT|Overview
http://www.tandf.co.uk/journals
A ACETYLCHOLINE JZaagsmaandHMeurs,UniversityofGroningen, Groningen,TheNetherlands & 2006ElsevierLtd.Allrightsreserved.
Abstract
Intheairways,acetylcholineisaneurotransmitterinparasympatheticgangliaandinpostganglionicparasympatheticnerves, aswellasanonneuralparacrinemediatorinvariouscellsinthe airwaywall.Ganglionictransmissionbyacetylcholineismediatedbynicotinicreceptors,whichareligand-gatedinchannels, whereaspostganglionictransmissionisthroughG-protein-coupledmuscarinicreceptors.Ofthefivemammalianmuscarinic receptorsubtypes,mainlyM1,M2,andM3 receptorsareinvolvedinairwayfunctions.Gq-coupledM1 receptorsfacilitate ganglionictransmissionmediatedbynicotinicreceptorsand modulatesurfactantproductionandfluidresorptioninthealveoli.PrejunctionalGi/o-coupledM2 receptorsinparasympatheticnerveterminalsattenuateacetylcholinereleaseuponnerve stimulation.M2 receptorsarealsoabundantlypresentinairway smoothmuscle;however,themajorfunctionofthesepostjunctionalM2 receptorsisunknown.PostjunctionalGq-coupledM3 receptorsmediateairwaysmoothmusclecontractionandmucus secretion.DysfunctionoftheprejunctionalM2 autoreceptorinducedbyallergicairwayinflammationhasbeenimpliedinexaggeratedvagalreflexactivityandairwayhyperresponsiveness inasthma.Inflammation-inducedincreasedM3 receptorstimulationmaybeinvolvedinairwayremodelinginchronic asthma.Possiblemechanismsincludepotentiationofgrowth factor-inducedproliferationofairwaysmoothmusclecellsand inductionofacontractilephenotypeofthesecells.Exaggerated M3 receptorstimulationmayalsocausereducedresponsivenessto b2-adrenoceptoragonistsbytransductionalcross-talk betweenphosphoinositidemetabolismandadenylylcyclase, whichinvolvesproteinkinaseC-induceduncouplingofthe b2adrenoceptorfromtheeffectorsystem.Muscarinicreceptorantagonistshavebeenshowntobeeffectiveinairwaydiseaseslike asthmaand,especially,chronicobstructivepulmonarydisease. Ofthese,tiotropiumbromideisparticularlyuseful,duetoits longdurationofactionaswellasitskineticselectivityforthe M3 receptor.
Introduction
Acetylcholineisaneurotransmitterinthecentraland peripheralnervoussystemwhereitplaysamajorrole intheafferentneuronsofboththeautonomic andsomatic(voluntary)branches.Asachemical transmitter,ithasbeenidentifiedas‘Vagusstoff’in 1921byOttoLoewishowingitsreleasefrom anisolatedfrogheartfollowingstimulationofthe
vagosympathetictrunk;whenappliedtoasecond, unstimulatedheart,theperfusatesloweditsrate, resemblingtheeffectofvagusstimulation.In 1926Loewiprovidedevidenceforidentificationof Vagusstoffasacetylcholine.Acetylcholineisthe neurotransmitterofallsympatheticandparasympatheticautonomicgangliaandofthepostganglionic parasympatheticnerves.Intheairways,theparasympatheticgangliaarelocatednearorwithintheairway wall.Ganglionictransmissionmediatedbyacetylcholineisthroughnicotinicreceptorswhichbelongto thefamilyofligand-gatedionchannels.Postganglionictransmissionbyacetylcholine,releasedfrom parasympatheticnerveterminals,isthroughmuscarinicreceptorsofwhichfivedifferentsubtypes havebeenidentified,allbeingG-protein-coupled receptors.Duringperiodsofairwayinflammation vagalreleaseofacetylcholinemaybeincreasedby variousmechanisms.Hence,bothinasthmaand (particularly)inchronicobstructivepulmonarydisease(COPD)blockadeofpostjunctionalmuscarinic receptorsisthekeytoreversingairwayobstructions.
Synthesis,Storage,andRelease AcetylcholineissynthesizedfromcholineandacetylcoenzymeA(acetyl-CoA)inthecytoplasmofthe nerveterminalthroughtheenzymecholineacetyltransferase(ChAT).Cholineistakenupbythenerve terminalfromtheextracellularfluidthroughasodium-dependentcarrier;thistransportistheratelimitingprocessinacetylcholinesynthesis.Acetyl-CoA issynthesizedinmitochondriawhichareabundantly presentinthenerveendings.Mostofthesynthesized acetylcholineisactivelytransportedfromthecytosol intosynapticvesiclesbyaspecifictransporter;this vesicular(‘quantal’)packageofacetylcholinereaches upto50000moleculespervesicle.
Releaseofacetylcholineisinitiatedbyinfluxof Ca2 þ ionsthroughvoltage-operatedN-orP-typecalciumchannels.TheincreasedintracellularCa2 þ ions bindtoavesicle-associatedprotein(synaptotagmin) whichfavorsassociationofasecondvesicleprotein (synaptobrevin)withoneormoreproteinsinthe plasmamembraneofthenerveterminal.Following
thisvesicle-dockingprocess,fusionbetweenvesicle membraneandplasmamembraneoccurs,followedby exocytosis.Aftertheexpulsionofacetylcholinethe emptyvesicleisrecapturedbyendocytosisandcanbe reused.Inthesynapticcleft,thereleasedacetylcholine willassociatewithpost-andprejunctionalreceptors andisalsosubjecttorapidhydrolysisbytheenzyme acetylcholinesteraseintocholineandacetate.Over 50%ofthecholineformedwillbetakenupagainby thenerveterminalandreusedforneurotransmitter synthesis.
Acetylcholineisalsopresentinnonneuronalcells. Inrecentyearsithasbecomeclearthatintheairways themajorityofcellsexpressChATandcontain acetylcholine,includingepithelialcells,smoothmusclecells,mastcells,andmigratedimmunecellssuch asalveolarmacrophages,granulocytes,andlymphocytes.However,theregulatoryroleofthisnonneuronalacetylcholineininflammatoryairways diseaseshasyettobeestablished.
RegulationofSynapticTransmission andActivity Ganglionic
Preganglionicnervesinnervatingtheparasympathetic gangliaintheairwaysevokeactionpotentialsduring normalbreathingwithrelativelyhighfrequencies,in therangeof1–20Hz.Asaresult,basalairway smoothmuscletone invivo ismediatedtoasignificantextentbycholinergicnerveactivity.Thepattern ofganglionicactionpotentialburstscoincideswith respiration,suggestingthattherespiratorycentersin thebrainstemgovernpreganglionicnerveactivity. However,inadditiontothiscentraldrive,reflex stimulationthroughmechanicallysensitiveafferent nerveterminalsinthelungsduringrespirationis importantlyinvolvedaswell.Thefidelitybywhich preganglionicimpulsesaretranslatedintoaction potentialsinthepostganglionicneuronsisrelatively lowinparasympatheticairwayganglia,implyinga filteringfunctionoftheseganglia.Thisfiltering functioncanbediminishedbyvariousinflammatorymediators.Thus,histamine,prostaglandinD2 (PGD2),andbradykininareabletoenhanceganglioniccholinergictransmissionandthesameistruefor tachykinins(substanceP,neurokininA)releasedby nonmyelinatedsensoryC-fibersintheairways.
Postganglionic
Thereleaseofacetylcholinefromparasympathetic nerveterminalsisregulatedbyavarietyofprejunctionalreceptors,whichmayinhibitorfacilitate transmitteroutflow.Intheairways,autoinhibitory
muscarinicM2 receptors,activatedbyacetylcholine itself,representanimportantnegativefeedback, limitingfurtherrelease,athigherfiringratesin particular.Inanimalmodelsofallergicairwayinflammationandasthmaaswellasinhumanasthma, dysfunctionoftheseM2 autoreceptorshasbeen foundtocontributetoexaggeratedacetylcholinereleasefromvagalnerveendings,toincreasedcholinergicreflexactivityinresponsetoinhaledstimuli, andtocontributetoairwayhyperresponsiveness. Mostofthisreceptordysfunctionisthoughttobe causedbyactivatedeosinophilsthatmigrateto cholinergicnervesandreleasemajorbasicprotein (MBP)whichactsasanallostericantagonistofmuscarinicM2 receptors.SinceeosinophilicinflammationisfarlessprominentinCOPDandsinceM2 autoreceptorsaremoreprominentinlargerairways, itisnosurprisethatthesereceptorsarestillfunctionalinpatientswithstableCOPD;however, thisdoesnotexcludeadysfunctionduringacute exacerbations.
InadditiontoM2 autoreceptors,avarietyof heteroreceptorsmodulatingacetylcholinerelease havebeenidentifiedoncholinergicnerveendings. Catecholaminesmayinhibitorfacilitateacetylcholineoverflowthroughprejunctional a2-and b2-adrenoceptors,respectively.Neurokininslikesubstance Pmayenhancecholinergictransmissionthrough facilitatoryneurokinin1(NK1)and/or2(NK2)receptors.Interestingly,substancePmayalsoinduce MBPreleasefromeosinophils,causingM2 receptor dysfunction,whichcouldactsynergisticallytodirect facilitation.Allergicinflammation-derivedprostanoids,includingPGD2,PGF2a,andthromboxane A2,aswellashistamine,canalsoaugmentacetylcholinereleasethroughprejunctionalreceptors.
Takentogether,theaboveobservationsindicate thatparasympatheticacetylcholinereleaseisgovernedbyvariousregulatorysystems,theset-pointof whichissubjecttoenvironmentalmodulations.Duringperiodsofairwayinflammationthesemodulations oftenresultinenhancedcholinergictransmission.
ReceptorsandBiologicalFunction Intheganglia,acetylcholineinteractswithnicotinic receptors.Thesereceptorsconsistoffivepolypeptide subunits,togetherformingacylindricstructureof about8nmdiameter,whichactsasanionchannel. Eachsubunitpassesthemembranefourtimes,so thecentralporeissurroundedby20membranespanninghelices.Thesubunitshavebeensubdivided intofiveclasses,designated a, b, g, d,and e.Ofthe a and b subunits,10and4differentsubtypeshave beenidentified,respectively.Peripheralganglionic
receptorsconsistofonly a and b subunits,themain subtypebeing(a3)2(b4)3.Each a subunitpossessesa bindingsiteforacetylcholine;theyneedtobeoccupiedbothtoinducechannelopening,whichwill enhanceNa þ andK þ permeability.Thisresultsin aninwardfluxofmainlyNa þ ions,causingdepolarizationandactionpotentialgenerationinthe postganglioniccell(providedtheacetylcholineconcentrationishighenough).
Acetylcholinereleasedbypostganglionicparasympatheticnervesmaychoosebetweenfivemuscarinic receptorsubtypes,designatedM1 toM5,tointeract with.Mostorgansandtissuesexpressmorethanone subtypeandthisistrueformanyindividualcellsas well.Thefivesubtypescanbesubdividedintotwo mainclasses,theodd-numberedreceptors(M1,M3, M5),whichcouplepreferentiallytoheterotrimericGqproteins,andtheeven-numbered(M2,M4)receptors whichshowselectivityforGi/o typeofG-proteins.
TheprincipalsignalingrouteofGq-coupledreceptorsistheactivationofphospholipaseC,mediating hydrolysisofphosphatidylinositol4,5-bisphosphate intoinositol1,4,5-trisphosphate(IP3)and1,2-diacylglycerol(DAG)(Figure1,left).IP3 mobilizesCa2 þ ionsfromintracellularstores,whichgeneratesarapid andtransientriseofthefreeCa2 þ concentrationin thecytosol.DAGtriggersthetranslocationandactivationofproteinkinaseC(PKC)whichisableto phosphorylateavarietyofdifferentproteinsubstrates.
ThemainsignaltransductionofGi/o-coupled receptorsistoinhibitadenylylcyclaseactivity,which reducestheintracellularcyclicAMPconcentration.
Inairwaysmoothmuscle,activationofGi/o byM2 receptorsmayalsodiminishopeningofcalcium-activatedpotassiumchannels(KCa ormaxi-Kchannels) inducedby(Gs-coupled) b-adrenoceptors.Thus,K þ efflux,membranehyperpolarization,andsubsequent smoothmusclerelaxation,initiatedby b-agonist administration,isunderrestraintofacetylcholine throughthismechanism.
Intheairwaysofmostmammalianspecies,includinghuman,M1,M2,andM3 receptorsarethe mostimportantones.Sofar,M4 receptorshaveonly beendetectedconvincinglyinbronchiolarsmooth muscleandalveolarwallsoftherabbit,whereas muscarinicM5 receptors,nowknowntomediate dilatationofcerebralarteriesandarterioles,are absentinthelungs.
M1 receptorshavebeenfoundinalveolarwalls, parasympatheticganglia,andsubmucosalglands. Ratandguineapiglungstudieshaveindicatedtheir presenceintypeIIalveolarcells,mediatingsurfactantproductionandfluidreabsorption,respectively. Inparasympatheticairwaygangliaofseveralspecies, includinghuman,M1 receptorstimulationisableto facilitateganglionictransmissionmediatedbynicotinicreceptors.Thus,vagalbronchoconstriction, inducedbyinhalationofSO2,hasbeenfoundespeciallysensitivetoinhaledpirenzepine,aM1-selective antagonist.Insubmucosalglands,M1 receptorsare notinvolvedinmucussecretion,whichappearstobe mediatedsolelybyM3 receptors.
M2 andM3 receptorsrepresentthemajorreceptorpopulations,bothinintra-andextrapulmonary
Figure1 Cross-talkbetweenM3 muscarinicreceptorsand b2-adrenoceptorsinairwaysmoothmuscle.Generationof1,2-diacylglycerol(DAG)byM3 receptor-inducedphosphoinositide(PIP2)metabolismcausesactivationofproteinkinaseC(PKC).PKCmayphosphorylatethe b2-adrenoceptoraswellasGs,causinguncouplingofthereceptorfromtheeffectorsystem.Moreover,PKCmay phosphorylate b-adrenoceptorkinase(s)(bARK),whichamplifies b-agonist-induceddesensitizationmediatedby bARK-inducedphosphorylationofthereceptor.AC,adenylylcyclase;cAMP,cyclicadenosine30 ,50 -monophosphate;IP3,inositol1,4,5-trisphosphate;PLC, phospholipaseC.
airways.Asalreadydiscussed,inhibitoryM2 autoreceptorslocatedatparasympatheticnerveterminals haveanimportantregulatoryroleinlimitingacetylcholinerelease.Postjunctionalmuscarinicreceptor populationsinairwaysmoothmuscleareamixture ofM2 andM3 receptors,theM2 subtypebeingpredominant,particularlyinthelargeairways.
Contraction,however,isprimarilymediatedby M3 receptors(eveninthosesmoothmusclepreparationswheretheratioofM2 :M3 receptorsis90: 10),theM2 receptorpopulationhavingatmosta minorsupportingrole.Thisisconfirmedinairway preparationsfromM2 receptorknockoutmice, inwhichcarbachol,amuscarinicagonist,was hardlylesspotentthaninpreparationsfromwildtypemice.
Cross-talkbetweenGi-coupledM2 receptorsand Gs-coupled b-adrenoceptors(havingopposingeffects oncyclicAMPaccumulationormaxi-Kchannel opening)hasnomajoreffectsinmodulatingmuscarinicagonistinducedcontractionor b-agonist inducedrelaxation,atleastunderphysiologicalcircumstances.However,ininflammatoryconditions suchasasthma,inwhichGi-proteinsmaybeupregulated,thesituationmaychange.
IncontrasttoM2 receptors,Gq-coupledM3 receptors,generatingIP3 andDAGbystimulating phosphoinositidemetabolism,mayhaveamajor influenceon b2-adrenoceptorfunction,eveninnoninflamedairways.ThisisduetoDAG-inducedactivationofPKCwhichmay(1)phosphorylatethe b2-adrenoceptoraswellasGs,causingreceptoruncouplinganddesensitization,and(2)phosphorylate andactivate b-adrenoceptorkinase(s)(bARKs, whicharemembersoftheG-proteinreceptorkinase (GRK)family),amplifyinghomologous, b-agonist induceddesensitization(Figure1).Theseprocesses mayexplainthewell-knownattenuationof b-agonist efficacyduringepisodesofseverebronchoconstriction,forexample,duringexacerbations.
AirwayRemodeling Inadditiontophosphoinositidemetabolism,inhibitionofadenylylcyclaseandmaxiK-channelactivation,stimulationofM3 and/orM2 receptorsin airwaysmoothmusclecellshasbeenshowntoactivatedifferentpromitogenicsignalingpathways, includingthep42/p44mitogen-activatedproteinkinase,Rho/Rhokinase,andPI3kinasepathways. In vitro studieshaverevealedthatmuscarinicagonists donotinduceairwaysmoothmusclecellproliferationbythemselves,butenhancetheproliferative responseinducedbypeptidegrowthfactors.This effect,whichissolelymediatedbytheM3 receptor,
indicatesthatacetylcholinemaycontributetoairway remodelingasobservedinasthmaandCOPD. Indeed,inananimalmodelofchronicasthmait wasrecentlydemonstratedthatthelong-acting muscarinicantagonisttiotropiumbromideinhibited increasedairwaysmoothmusclemass,enhanced airwaysmoothmusclecontractility,andincreased expressionofcontractileproteinsinthelungupon repeatedallergenchallenge.Thisimpliesthat,inadditiontotheirbronchodilatingproperties,muscarinic receptorantagonistscouldbebeneficialinthe treatmentofasthmabypreventingchronicairway hyperresponsivenessanddeclineoflungfunction. Althoughnotfullyestablished,amoreextensive roleofacetylcholineinairwayremodeling,including airwaysmoothmuscleproliferation,contractileproteinexpression,promitogenicsignaling,andregulationofsecretoryfunctionsaswellascellmigration, hasrecentlybeenproposed(Figure2).
AcetylcholineinRespiratoryDiseases Asindicatedabove,theparasympatheticnervous systemrepresentsamajorconstrictorypathwayof theairways;evenbasalbronchomotortoneispartly governedbyacetylcholine.Bothitsreleaseandits postjunctionaleffects,includingsmoothmusclecontractionandmucussecretion,areregulatedand mediated,respectively,bymuscarinicreceptors.So far,noevidenceforupregulationofpostjunctional M3 andM2 receptorshasbeenfoundinhyperresponsiveairwaysofpatientswithasthmaandCOPD. Incontrast,dysfunctionalautoreceptors,leading toexaggeratedvagalreflexesintheairways,arewell establishedinallergicasthma.M1 receptors,facilitatingnicotinicneurotransmissioninparasympatheticairwayganglia,donotappeartocontribute significantlytobronchomotortoneinhumans,either withorwithoutobstructiveairwaydiseases.Hence, theprincipletherapeuticmuscarinicreceptortarget inasthmaandCOPDistheM3 receptor.InCOPD, muscarinicreceptorantagonistslikeipratropium, aquarternarynonselectiveantagonist,arevery effectiveincausingbronchodilatation.Arecentlyintroducedantagonististiotropium,whichacutely occupiesbothM2 andM3 receptors;however,while itdissociatesrapidlyfromM2 receptorsduring washout,blockadeofM3 receptorspersistsfor hours.ThiskineticallybasedM3 receptorsubtype selectivitycouldbeoftherapeuticadvantagesince blockadeofprejunctionalM2 receptorsenhances acetylcholineoutflow.BothinCOPDand,particularly,inallergicasthma,inwhichM2 autoreceptors arealreadydysfunctional,thisisanunwantedside effect.
Figure2 Proposedmechanismsbywhichacetylcholine(ACh)couldaffectairwaysmoothmuscleremodeling.Acetylcholinehasbeen showntoaffectairwaysmoothmusclecontractility,contractileproteinexpression,promitogenicsignaling,andproliferation.Inaddition, likeseveralotherG-protein-coupledreceptoragonists,acetylcholinecouldalsobeinvolvedinairwaysmoothmusclecellmigration, extracellularmatrixproteinproduction,andsecretionofcytokinesandchemokines.Altogether,theseeffectscouldcontributetoairway remodelinginasthmaandCOPD.ReproducedfromGosensR,ZaagsmaJ,GrootteBromhaarM,NelemansSA,andMeursH(2004) Acetylcholine:anovelregulatorofairwaysmoothmuscleremodelling. EuropeanJournalofPharmacology 500:193–201,withpermissionfromElsevier.
Seealso: Asthma:Overview. ChronicObstructive PulmonaryDisease:Overview. Neurophysiology: NeuralControlofAirwaySmoothMuscle;Neuroanatomy;NeuronsandNeuromuscularTransmission.
FurtherReading BergeREten,SantingRE,HamstraJJ,RoffelAF,andZaagsmaJ (1995)DysfunctionofmuscarinicM2 receptorsaftertheearly allergicreaction:possiblecontributiontobronchialhyperresponsivenessinallergicguinea-pigs. BritishJournalofPharmacology 114:881–887.
BillingtonCKandPennRB(2002)M3 muscarinicacetylcholine receptorregulationintheairway. AmericanJournalofRespiratoryCellandMolecularBiology 26:269–272.
CoulsonFRandFryerAD(2003)Muscarinicacetylcholinereceptors andairwaydiseases. PharmacologyandTherapeutics 98:59–69.
GosensR,BosST,ZaagsmaJ,andMeursH(2005)Protective effectoftiotropiumbromideintheprogressionofairway
ACID–BASEBALANCE OSiggaard-Andersen,UniversityofCopenhagen, Copenhagen,Denmark & 2006ElsevierLtd.Allrightsreserved.
Abstract
Theacid–basebalanceorneutralityregulationmaintainsapH around7.4intheextracellularfluidbyexcretingcarbondioxide (carbonicacidanhydride)inthelungsandnoncarbonicacidor baseinthekidneys.Theresultisanormalacid–basestatusin bloodandextracellularfluid,i.e.,anormalpH,anormalcarbondioxidetension(pCO2 ),andanormalconcentrationof
smoothmuscleremodeling. AmericanJournalofRespiratory andCriticalCareMedicine 171:1096–1102.
GosensR,ZaagsmaJ,GrootteBromhaarM,NelemansSA,and MeursH(2004)Acetylcholine:anovelregulatorofairway smoothmuscleremodelling. EuropeanJournalofPharmacology 500:193–201.
Racke KandMatthiesenS(2004)Theairwaycholinergicsystem: physiologyandpharmacology. PulmonaryPharmacologyand Therapeutics 17:181–198.
WessJ(2004)Muscarinicacetylcholinereceptorknockoutmice: novelphenotypesandclinicalimplications. AnnualReviewof PharmacologyandToxicology 44:423–450.
WesslerI,KilbingerH,BittingerF,UngerR,andKirkpatrick CJ(2003)Thenonneuralcholinergicsysteminhumans: expression,functionandpathophysiology. LifeSciences 72: 2055–2061.
ZaagsmaJ,MeursH,andRoffelAF(eds.)(2001) Muscarinic ReceptorsinAirwaysDiseases.Basel:BirkhauserVerlag. ZaagsmaJ,RoffelAF,andMeursH(1997)Muscariniccontrolof airwayfunction. LifeSciences 60:1061–1068.
titratablehydrogenion(ctH þ ).ApH,log pCO2 chartillustratestheacid–basestatusofthearterialblood.Thechartshows normalvaluesaswellasvaluestobeexpectedintypicalacid–basedisturbances,i.e.,acuteandchronicrespiratoryacidosis andalkalosis,andacuteandchronicnonrespiratory(metabolic) acidosisandalkalosis.ThechartallowsestimationoftheconcentrationoftitratableH þ oftheextendedextracellularfluid (includingerythrocytes), ctH þ Ecf.Thisquantityisalsocalled standardbasedeficitbutthetermbasedoesnotdirectlyindicate thatthequantityreferstotheexcessordeficitofhydrogenions. ctH þ Ecfisthepreferredindicatorofanonrespiratoryacid–base disturbancebeingindependentofacutechangesin pCO2 invivo.WhilepHand pCO2 aredirectlymeasured, ctH þ Ecf
iscalculatedfrompHand pCO2 usingtheHenderson–HasselbalchequationandtheVanSlykeequation.
Description
Theacid–basebalanceorneutralityregulationmaintainsapHaround7.4intheextracellularfluidby excretingcarbondioxide(carbonicacidanhydride) inthelungsandnoncarbonicacidorbaseinthe kidneys.Theresultisanormalacid–basestatusin bloodandextracellularfluid,i.e.,anormalpH,a normalcarbondioxidetension(pCO2 ),andanormal concentrationoftitratablehydrogenion(ctH þ ). Figure1 illustratestheacid–basestatusoftheblood, especiallytherelationshipsamongthethreekey variables.
pHandtheHydrogenIonConcentration(cH þ )
pHand cH þ oftheplasmaarebothindicatedon theabscissaof Figure1.pHisthenegativedacadic logarithmofmolalhydrogenionactivity.Concentrationoffreehydrogenion(cH þ )iscalculatedas 109 pH nmoll 1.pHandpOHarecloselyrelated: pH þ pOH ¼ pKw ¼ 13.622at371C,where Kw isthe ionizationconstantofwater.IfH þ isconsidereda keycomponentofanaqueoussolution,thenOH is aderivedcomponent.AccountingforH þ andH2O indirectlyaccountsforOH aswell.Itistheauthor’sconvictionthattherelevantcomponentisthe hydrogenion,nothydrogenionbindinggroups (base)norhydroxylions.
TheCarbonDioxideTensionoftheBlood(pCO2 ) pCO2 ,i.e.,thepartialpressureofcarbondioxidein agasphaseinequilibriumwiththeblood,isshown ontheordinateonalogarithmicscalein Figure1. When pCO2 increases,theconcentrationofdissolved carbondioxideandcarbonicacidincreases,and hencethehydrogenionconcentrationincreases:
withcations)anddoesnotdirectlyindicatethatthe relevantchemicalcomponentisthehydrogenion. ThetermhydrogenionexcessoracronymHXmay alsobeused.Note:bydefinition, ctH þ ofbloodreferstotheactualhemoglobinoxygensaturation,not thefullyoxygenatedblood.
Acidandbasearedefinedbytheequilibrium:
Acidz # Hþ þ Basez 1
whereAcidz andBasez 1 isaconjugateacid–base pair.Thechargenumber z maybepositive,zero,or negative.Astrongacid,e.g.,HCl,dissociatescompletely:HCl-H þ þ Cl .Theanionthatfollowsthe hydrogenioniscalledanaprote,nonbuffering,or stronganion.AtphysiologicalpH,evenlacticacidis astrongacidandlactateanaproteanion.Abaseisa moleculecontainingahydrogenion-bindinggroup. Astrongbase,e.g.OH ,associatescompletelywith hydrogenion:OH þ H þ -H2O.Thecationthat followsthehydroxylioniscalledanaprote,nonbuffering,orstrongcation,e.g.,Na þ orK þ
Aweakacid(bufferacid)isinequilibriumwithits conjugateweakbase(bufferbase),e.g.:
TheConcentrationofTitratableHydrogenIon (ctH þ )
ctH þ isindicatedonthescaleintheupperleftcorner of Figure1. ctH þ isameasureofaddednoncarbonic acidorbase.Theamountofhydrogenionaddedor removedinrelationtoareferencepHof7.40may bedeterminedbytitrationtopH ¼ 7.40at pCO2 ¼ 5:33kPa( ¼ 40mmHg)and T ¼ 371Cusingstrong acidorbase,dependingupontheinitialpH.Titratablehydrogenionisalsocalledbasedeficit,orwith theoppositesignbaseexcess.Unfortunately,theterm ‘base’isambiguous(ithaspreviouslybeenassociated
Theconcentrationoftitratablehydrogenionmay bedeterminedforplasma(P),wholeblood(B),ora modeloftheextendedextracellularfluid,i.e.,blood plusinterstitialfluid(Ecf).Themodelconsistsof blooddilutedthreefoldwithitsownplasmatogeta hemoglobinconcentrationsimilartotheoneobtainediftheredcellswereevenlydistributedinthe wholeextracellularvolume.Anacuteincreasein pCO2 invivo causesarisein ctH þ Bandafallin ctH þ Pwhile ctH þ Ecfremainsconstant.Forexample,anacuterisein pCO2 from5.33to10.66kPa (40–80mmHg)causesariseinwholeblood ctH þ of about5mmoll 1,afallinplasma ctH þ ofabout 3mmoll 1,whiletheextracellular ctH þ remains independentofacutechangesin pCO2 .Thecauseisa redistributionofhydrogenionswithintheextended extracellularvolume.Thehydrogenionconcentrationincreasesmoreinthepoorlybufferedinterstitial fluidthaninthebloodplasma,whereitincreases morethaninsidetheerythrocytes,wherehemoglobin bindsthehydrogenions.Hydrogenionsdiffusefrom thepoorlybufferedinterstitialfluidintotheblood plasmaandfurtherintotheerythrocytes.Verylittle transferofhydrogenionsoccursbetweentheintracellularspaceandtheextracellularspace,so ctH þ Ecfremainsvirtuallyconstantduringacute
CO2 þ H2 O-H2 CO3 -Hþ þHCO3
H2 CO3 # Hþ þ HCO3
hemoglobinz # Hþ þ hemoglobinz 1
Figure1 Acid–basechartforarterialbloodwithnormalandpathophysiologicalreferenceareas.Theacid–basestatusisshownasa pointwiththreecoordinates:pH(abscissa), p CO2 (ordinate),and c tH þ (obliquecoordinate).Thebandsradiatingfromthenormalarea (thecentralellipse)showreferenceareasfortypicalacuteandchronic,respiratoryandnonrespiratory,acid–basedisturbances.Hyper-and hypocapniaarealsocalledrespiratoryacidosisandalkalosis,respectively.Hydrogenionexcessanddeficit,i.e.,increasedanddecreased c tH þ ,arealsocallednonrespiratory(ormetabolic)acidosisandalkalosis,respectively.ReproducedfromSiggaard-AndersenO(1971)An acid-basechartforarterialbloodwithnormalandpathophysiologicalreferenceareas. ScandinavianJournalofClinicalandLaboratory Investigation 27:239–245.Copyright & 1970,1974byRadiometerCopenhagenA/S,A ˚ kandevej21,Brønshøj,Denmark.
changesin pCO2 invivo. ctH þ Ecfisalsocalled standardbasedeficit(SBD),orwiththeoppositesign standardbaseexcess(SBE),butthetermbaseisdeprecatedbytheauthor.Itisimportanttouse ctH þ Ecf
ratherthan ctH þ B(wholebloodtitratablehydrogen ion)asameasureofanonrespiratoryacid–basedisturbance,especiallyinneonatologywherehighhemoglobinconcentrationsandhigh pCO2 valuesmaybe
encountered.The ctH þ Bmaythenbeconsiderably higherthan ctH þ Ecf(asmuchas4mmoll 1)causinganerroneousdiagnosisofmetabolicacidosis, whenthesituationismerelyaredistributionofhydrogenionswithintheextendedextracellularvolume.
Projectionstothe ctH þ scaleintheupperleft cornerof Figure1 shouldbemadealongtheslanting so-called vivo-CO2 titrationcurves,whicharevirtuallystraightlines(slightlyconvexupwards).The slopeofthelinesdependsontheconcentrationof nonbicarbonatebuffers,i.e.,mainlyhemoglobin.In thechart,theslopecorrespondstoahemoglobin concentrationof3mmoll 1 correspondingtothe hemoglobinconcentrationoftheextendedextracellularfluid.Variationsintheslopeduetovariationsin bloodhemoglobinconcentrationaresmallandgenerallywithoutclinicalsignificance.Variationsinthe concentrationofotherbuffers,e.g.,albumin,are evenlesssignificant.
Insummary,thehydrogenionstatusoftheblood isdescribedbyapointintheacid–basechart:the x,y coordinatesindicate cH þ and pCO2 ,theoblique coordinateis ctH þ Ecf.
TheHenderson–HasselbalchEquation
Oftenadescriptionofacid–basebalanceisbasedon theHenderson–Hasselbalchequation,derivedfrom thelawofmassaction:
pH ¼ pK þ log10 ðcHCO3 =ðaCO2 pCO2 ÞÞ
wherepK ¼ 6.10and aCO2 ¼ 0.23mmoll 1 kPa 1
¼ 0.0306mmoll 1 mmHg 1 (solubilitycoefficient ofcarbondioxideinplasmaat371C). aCO2 pCO2 givestheconcentrationofH2CO3 plusCO2.pHis determinedbytwovariables, pCO2 and cHCO3 ,
representingrespiratoryandmetabolicdisturbances. cHCO3 isshownin Figure1 onahorizontallogarithmicscalealongthe pCO2 ¼ 5 33kPaline.Projectionstothescaleshouldbemadeatanangleof 451.However, cHCO3 isnotindependentof pCO2 .Forthisreason,standardbicarbonatewas introduced,i.e.,thebicarbonateconcentrationin plasmaofwholebloodequilibratedwithagasmixturewithanormal pCO2 (5.33kPa ¼ 40mmHg)at 371C.However,eventhestandardbicarbonateisnot completelyindependentofacutechangesin pCO2 in vivo,decreasingslightlyinacutehypercapnia.Tobe independent,theequilibrationshouldbeperformed withamodeloftheextendedextracellularfluid. Projectingfromagivenpointinthecharttothe bicarbonatescalealongtheslanting vivo-CO2 equilibrationlinesgivesthestandardbicarbonateconcentrationoftheextendedextracellularfluid.
TheVanSlykeEquation BloodgasanalyzersmeasurepHwithaglasselectrodeand pCO2 withamembrane-coveredglass electrode(Stow-Severinghauselectrode). ctH þ Ecfis calculatedfrompH, pCO2 ,and cHb(concentration ofhemoglobin)usingamodelofthetitrationcurve calledtheVanSlykeequation(Table1).Theequationcalculatesthechangeinbufferbaseconcentration(bicarbonateplusproteinanionplusphosphate) fromthevalueatthereferencepoint:
pHPy ¼ 7 40; Py CO2 ¼ 5 33kPa; and T y ¼ 37 C
Bufferbase(BB)isthedifferencebetweentheconcentrationsofbufferanionsandbuffercations(the latterbeingvirtuallyzeroatphysiologicalpH). Strongiondifference(SID)isthedifferencebetween
Table1 VanSlykeequationforcalculationoftheconcentrationoftitratablehydrogenionintheextendedextracellularfluid, c tH þ Ecf
c tH þ Ecf ¼ ð1 c HbEcf=c Hby Þ ðDc HCO3 P þ bHþ Ecf Dp HPÞ
c HbEcf ¼ c HbB V B/V Ecfconcentrationofhemoglobinintheextendedextracellularfluid
V B/V Ecf ¼ 1/3(defaultvalue)ratiobetweenthevolumeofbloodandvolumeofextendedextracellularfluid
c Hby ¼ 43mmoll 1 empiricalparameteraccountingforanunequaldistributionofhydrogenionsbetweenplasmaanderythrocytes
Dc HCO3 P ¼ c HCO3 P c HCO3 Py
c HCO3 Py ¼ 24.5mmoll 1 concentrationofbicarbonateinplasmaatpHPy ¼ 7.40, P y CO2 ¼ 5 33kPa, T y ¼ 37 0 C
DpHP ¼ pHP pHPy
bHþ Ecf ¼ bm Hby c HbEcf þ bP
bm Hby ¼ 2.3apparentmolarbuffercapacityofhemoglobinmonomerinwholeblood
bP ¼ 7.7mmoll 1 (defaultvalue)buffervalueofnonbicarbonatebuffersinplasmaforanormalplasmaprotein(albumin)concentration
c HbB ¼ rHbB/MmHb(substance)concentrationofhemoglobininblood(unit:mmoll 1)asafunctionofthemassconcentration, rHbB (unit:gl 1)
MmHb ¼ 16114gmol 1 molarmassofhemoglobinmonomer
Ecfreferstotheextendedextracellularfluid,Btowholeblood,Ptoplasma.Replacing c HbEcfby c HbBgives c tH þ B;replacing c HbEcf byzerogives c tH þ P.
Note:if c HbB ¼ 9.0mmoll 1 3 rHbB ¼ 14.5gdl 1,thentheVanSlykeequationsimplifiesto c tH þ Ecf ¼ 0.93 (Dc HCO3 P þ
DpHP 14.6mmoll 1).
theconcentrationsofnonbuffercationsandnonbufferanions(see Figure2).Accordingtothelawof electroneutrality,thevalueofBBandSIDmustbe identical.Bufferbaseisnotasuitableindicatorofa nonrespiratoryacid–basedisturbance;althoughindependentof pCO2 ,itvarieswiththealbuminand hemoglobinconcentrations,whichareunrelatedto acid–basedisturbances.
NormalAcid–BaseBalance Acid–basebalancereferstothebalancebetweeninput(intakeandproduction)andoutput(elimination) ofhydrogenion.Thebodyisanopensystemin equilibriumwiththealveolarairwherethepartial pressureofcarbondioxide pCO2 isidenticaltothe carbondioxidetensionintheblood. pCO2 isdirectly proportionaltotheCO2 productionrate(atconstant
alveolarventilationandCO2 freeinspiredair)and inverselyproportionaltothealveolarventilation(at constantCO2 productionrateandCO2 freeinspired air).CO2 isconstantlyproducedintheoxidative metabolismatarateofabout10mmolmin 1 ( ¼ 224mlmin 1)andeliminatedinthelungsatthe sameratesothatthe pCO2 remainsatabout 5.33kPa( ¼ 40mmHg).Hydrogenionsassociated withanyanionotherthanbicarbonateorexchanging withacationareeliminatedbythekidneys.Inthe oxidativemetabolismofsulfur-containingaminoacids,hydrogenionsareproducedtogetherwithsulfate ionsatarateofabout70mmolday 1 depending upontheproteinintake.Aminoacidsareoxidizedto carbondioxideandwater,andtheaminonitrogen, liberatedasNH3,combineswithcarbondioxidein theliverviatheKrebsureacycletoformneutral urea.Therefore,thereisnoproductionofbase(ammonia)exceptinthekidneys,whereammonia formedfromglutaminediffusesintotheurinewhere itbindsahydrogenion(NH3 þ H þ -NH4þ )thereby preventinganexcessivelylowurinepH.
Figure2 Electrolytebalanceofarterialplasmashowingcolumnsofcationsandanionsofequalheight(lawofelectroneutrality).Theequalityofthestrongiondifference(SID)and bufferbase(BB)isillustrated.Thechangeinconcentrationof bufferbasefromnormal(atpH ¼ 7.40, p CO2 ¼ 5 3kPa,and T ¼ 371C)withoppositesignequalstheconcentrationoftitratable hydrogenion.
Normalvaluesfortheacid–basestatusofarterial bloodaregivenin Table2.Thelower pCO2 in womenthanmenisprobablyaprogesteroneeffecton therespiratorycenter.Thevaluesareindependentof ageexceptatbirth,wherebabiestendtohavehigher pCO2 ,lowerpH,andslightlyincreased ctH þ Ecf, approachingnormalvaluesforadultsinthecourseof afewhours.Inthelasttrimesterofpregnancy,the pCO2 islower(about1kPa ¼ 7.5mmHg),compensatedbyaslightlyincreased ctH þ Ecf.Aprotein-rich dietcausesahigher ctH þ Ecf(1–2mmoll 1)anda slightlylowerpHduetoproductionofsulfuricacid fromsulfur-containingaminoacids.Adietrichin vegetablesandfruitcausesalower(negative) ctH þ EcfandaslightlyhigherpHduetoorganicanionsbindingH þ inthemetabolismtocarbondioxide andwater.High-altitudehypoxiastimulatesventilation;at5kmabovesealevel, pCO2 isdecreasedto about3.3kPa ¼ 25mmHg.Thehypocapniaiscompensatedbyincreased ctH þ Ecf,sopHisonlyslightly elevated.Thevaluesfallintheareaofchronichypocapniaintheacid–basechart(Figure1).
c H þ P36.3–41.7nmoll 1 (pH:7.38–7.44)37.2–42.7nmoll 1 (pH:7.37–7.43)
c tH þ Ecf 2.3to þ 2.7mmoll 1 3.2to þ 1.8mmoll 1
p CO2 4.59–5.76kPa(33.8–42.4mmHg)4.91–6.16kPa(36.8–46.2mmHg)
c HCO3 P21.2–27.0mmoll 1 22.2–28.3mmoll 1
c H þ P:conc.of(free)hydrogenioninplasma; c tH þ Ecf:conc.oftitratablehydrogenioninextracellularfluid(alsocalledstandardbase deficit,SBD); p CO2 :tensionofcarbondioxide; c HCO3 P:conc.ofbicarbonateinplasma.
Table2 Referencevaluesforarterialblood
Acid–BaseDisturbances RespiratoryAcid–BaseDisturbances Acuterespiratoryacid–basedisturbancesarecharacterizedbyanacutechangein pCO2 associatedwith anacutechangeinpHbutwithunchanged ctH þ Ecf. Therelationshipbetween pCO2 andpHisillustrated bytheoblique invivo CO2 equilibrationlinesinthe acid–basechart(Figure1).Primaryincreaseanddecreasein pCO2 arecompensatedbysecondaryrenal decreaseandincreasein ctH þ Ecf,respectively.The acid–basechartshowstheexpectedvaluesinchronic hypercapniaandchronichypocapnia.Theeffectof thecompensationisareturnofpHabouttwo-thirds towardsnormal,slightlymoreinacutehypocapnia.
NonrespiratoryAcid–BaseDisturbances Primaryincreaseanddecreasein ctH þ Ecfarecompensatedbysecondarydecreaseandincreasein pCO2 .Averyacuterisein ctH þ Ecf,forexample, duetoanaerobicexercisewithlacticacidformation, isonlypartlycompensatedbecauseonlyperipheral chemoreceptorsreactpromptlytoafallinbloodpH. IttakesaboutanhourbeforeH þ equilibriumbetweenbloodandbrainextracellularfluidisachieved andthecentralchemoreceptorsaremaximallystimulated.Theacid–basevaluesinacutenonrespiratory acidemiaareillustratedin Figure1 bythearealabeled‘acutehydrogenionexcess’.Theoutlineofthe areaisdottedbecauseitislesswell-definedthanthe otherareasofthechart.Thecompensationsinmore slowlydevelopingnonrespiratoryacidemiaoralkalemiaareillustratedbytheareaslabeled‘chronic hydrogenionexcess’and‘deficit’,respectively.The effectoftherespiratorycompensationisareturnof pHone-thirdtohalfwaytowardsnormal.
Onceanincreasein ctH þ Ecfhasbeendetected, thequestionis:whatcausedthemetabolicacidosis? Itmaybeaproductionoflacticacidduetoanaerobic metabolismoracetoaceticacid(ketoacidosis)dueto diabetesmellitusorstarvation.Inbothcasesthediagnosismaybeverifiedbydirectmeasurementof bloodlactateoracetoacetate.Whentheseanalyses areunavailable,calculationoftheconcentrationof undeterminedanionsmaybeuseful,i.e.,thesumof theconcentrationsofmeasuredcations(Na þ and K þ )minusthesumoftheconcentrationsofmeasuredandcalculatedanions(Cl andHCO3 ).This equalsthesumoftheconcentrationsofunmeasured anions(mainlyProtein ,SO4 2 ,HPO4 2 ,fattycarboxylate,lactate,acetoacetate)minusthesumof theconcentrationsofunmeasuredcations(Ca2 þ andMg2 þ ).Ametabolicacidosiswithamajorincreaseinundeterminedanionsusuallyindicates
organicacidosis.Ahyperchloremicacidosismaybe arenalacidosiswithretentionofH þ andCl oran intestinallossofNa þ þ HCO3 withsubsequent intakeofsaline(Na þ þ Cl ).Ahypochloremic alkalosismaybeduetolossofH þ andCl by vomiting.Hypokalemicalkalosisisduetoinability ofthekidneystoretainhydrogenionsinthepresence ofpotassiumdepletion.
Seealso: ArterialBloodGases CarbonDioxide PeripheralGasExchange Ventilation:Overview.
FurtherReading AstupPandSeveringhausJW(1986) TheHistoryofBloodGases AcidsandBases.Copenhagen:MunksgaardInternationalPublishers.
DavenportHW(1969) TheABCofAcid–BaseChemistry,5thedn. Chicago:TheUniversityofChicagoPress.
GrogonoAW(1986)Acid–basebalance. InternationalAnesthesiologyClinics,ProblemsandAdvancesinRespiratoryTherapy 24(1).
HalperinMLandGoldsteinMB(1988) Fluid,Electrolyte,and Acid–BaseEmergencies.Philadelphia:Saunders.
HillsAG(1973) Acid–BaseBalance.Chemistry,Physiology,and Pathophysiology.Baltimore:Williams&Wilkins. InternationalFederationofClinicalChemistryandInternational UnionofPureandAppliedChemistry(1987)Approved Recommendation(1984)onPhysico-ChemicalQuantitiesand UnitsinClinicalChemistry. JournalofClinicalChemistryand ClinicalBiochemistry 25:369–391.
MasoroEJandSiegelPD(1971) Acid–BaseRegulation.ItsPhysiologyandPathophysiology.Philadelphia:Saunders.
NahasGandSchaeferKE(eds.)(1974) CarbonDioxideandMetabolicRegulations.NewYork:Springer.
RoothG(1975) Acid–BaseandElectrolyteBalance.Lund:Studentlitteratur.
SeveringhausJWandAstrupP(1987) HistoryofBloodGasAnalysis.Boston:Little,BrownandCompany.
ShapiroBA,PeruzziWT,andTemplinR(1994) ClinicalApplicationofBloodGases,5thedn.StLouis:Mosby–YearBook.
Siggaard-AndersenO(1971)Anacid-basechartforarterialblood withnormalandpathophysiologicalreferenceareas. ScandinavianJournalofClinicalandLaboratoryInvestigation 27: 239–245.
Siggaard-AndersenO(1974) TheAcid–BaseStatusoftheBlood, 4thedn.Copenhagen:MunksgaardandBaltimore:Williams& WilkinsCompany.
Siggaard-AndersenO(1979)Hydrogenionsandbloodgases.In: BrownSS,MitchellFL,andYoungDS(eds.) Chemical DiagnosisofDisease,pp.181–245.London:Elsevier,NorthHollandBiomedicalPress.
Siggaard-AndersenOandFogh-AndersenN(1995)Baseexcessor bufferbase(strongiondifference)asmeasureofanon-respiratoryacid–basedisturbance. ActaAnaesthesiologicaScandinavica 39(supplement107):123–128.
ThomsonWST,AdamsJF,andCowanRA(1997) ClinicalAcid–BaseBalance.NewYork:OxfordUniversityPress.
WestJB(1974) RespiratoryPhysiology,theEssentials.Oxford: Blackwell.
WestJB(2001) PulmonaryPhysiologyandPathophysiology.An Integrated,Case-BasedApproach.Philadelphia:Lippincott Williams&Wilkins.
AcuteExacerbations see Asthma:AcuteExacerbations. ChronicObstructivePulmonaryDisease: AcuteExacerbations.
AcuteLungInjury see AcuteRespiratoryDistressSyndrome
ACUTERESPIRATORYDISTRESSSYNDROME GBellingan,UniversityCollegeLondon,London,UK SJFinney,ImperialCollegeLondon,London,UK & 2006ElsevierLtd.Allrightsreserved.
Abstract
Theacuterespiratorydistresssyndrome(ARDS)isthedevastatingmanifestationofthediffusepulmonaryinflammationthat mayoccurfollowingawiderangeoflife-threateningsystemic illnesses.Therapidonsetofinflammationandbilateralnonhydrostaticalveolaredemaresultsinseverehypoxemiaandreducedpulmonarycomplianceoftenmandatingmechanical ventilation.Theclinicalfeatures,radiology,andpathogenesis arereviewedinthisarticle.Themanagementofpatientscomprisesprimarilyofventilatorysupportwhilethelunginjuryresolves.Thetechniquesofventilatorysupportcanpropagatethe lunginjuryandadverselyaffectoutcome;thetechniquesare discussedindetailhere.Bycontrast,pharmacotherapyhasaless clearroleinARDS.Corticosteroidsmaybebeneficialafterthe acutephases,whilstotheranti-inflammatoryagentshavenot provedbeneficial.MortalityisdeterminedprimarilybytheunderlyingtriggerforARDS,butisapproximately30–40%.Follow-upofsurvivorshasdemonstratedthatlungfunctionoften improvesconsiderably,whereasnonpulmonarymorbiditiespersisteven12monthsafterdischargefromtheintensivecareunit.
Introduction Theacuterespiratorydistresssyndrome(ARDS)and itslessextrememanifestation,acutelunginjury (ALI),aredevastatingconditionsthatresultinsuddenbilateralnonhydrostaticalveolaredemaandseverehypoxemia.Pulmonaryfailureisusuallyso severethatpatientsrequiremechanicalventilationof theirlungs.ARDSandALIaretheconsequenceof thediffusepulmonaryinflammationthatcanbetriggeredbyaninsulteithertothelungitselformore commonlyatadistantsite.Assuch,theyformpart ofthespectrumofsystemicinflammationthatcan occurfollowingmanylife-threateninginsults(see Table1).
Theconstellationofsevererespiratorydistress,refractoryhypoxemia,decreasedpulmonarycompliance,
EtiologyPercentage
Sepsis(includingpulmonarysepsis)43–52
Aspirationofgastriccontents22–36 Pulmonarycontusion8–26 Bacteremia4–12 Headinjury6–11 MultiplebonyfracturesrequiringICUadmission5–12 Bloodtransfusionexceeding10unitsin24h5–8 Cardiopulmonarybypass2 Burns(includingsmokeinhalation)2 Acutepancreatitis1 Lungreperfusioninjury(e.g.,posttransplant) Near-drowning
Thefiguresinthiswerebasedonstudiesattheuniversityof WashingtonandColorado.
anddiffuseradiologicalchangeswasfirstappreciated byAshbaughandco-workersin1967.Theyreferredto theclinicalscenarioastheadultrespiratorydistress syndrome.Sinceanidenticalconditioncanalsooccur inchildren,itisnowreferredtoastheacuterespiratorydistresssyndrome.Subsequently,theclinicalsyndromehasbeenincreasinglyrecognizedandestimates oftheannualincidenceofARDSrangefrom8to70 casesper100000populationindevelopedcountries. Overall,mortalityinpatientswithARDSisapproximately30–40%,althoughdeathisusuallyattributabletotheunderlyingetiologyratherthanpulmonary failure perse
Etiology ThemanypossibletriggersforARDSareoutlinedin Table1.Sepsisaccountsforthemajorityofcasesin generalintensivecareunits(ICUs).PatientswithmultipleriskfactorsaremorelikelytodevelopARDS. Intriguingly,ARDSonlyoccursinasubsetofpatients whosufferapparentlysimilarinsults.Itisnot clearwhatexplainsaparticularindividualgoingon
Table1 ClinicaltriggersofARDS
todevelopARDS.Althoughenvironmentalfactors suchasage,sex,smokinghistory,andintercurrent pulmonarydiseasemaybeimportant,itiswidely consideredthatgeneticfactorsarecritical.Candidate genesforwhichassociationshavebeendescribedincludethosethatencodetumornecrosisfactoralpha (TNF-a),angiotensin-convertingenzyme,interleukin-6 (IL-6),surfactantproteinB,andToll-likereceptors. Nevertheless,ithasnotbeenpossibletodrawdefinitiveconclusionssincetheseassociationsarecomplicatedbytightlinkagedisequilibriumtoothergenes, lackofclearfunctionaleffects,andsmallpatientnumbers.Moreover,theheterogeneityofARDSsuggests thatmanygeneswithvaryingphenotypesandpenetrancemayunderpinanindividual’ssusceptibility. Functionalgenomicapproachesmayhelpelucidate thesecomplexgenotypes.
Pathology Traditionally,thehistologicaldevelopmentofARDS hasbeendescribedashavingthreesequentialphases whichaffectthelungsinadiffusemanner:exudative, proliferative,andfibrotic.Itisnowevidentthatthese stagesoverlapconsiderablyandfibroticchangesare initiatedveryearly.
Withinthefirst24h,thelungsappearmacroscopicallyedematousandcongested.Atthispoint,light microscopyrevealsedemawithintheairspaces, alveolarwalls,andseptae.TypeIalveolarepithelial cellsareswollen,necrotic,andoftendetachedfrom theunderlyingbasementmembrane.Pulmonary endothelialcellsmayalsobeswollen,withfibrin thrombioccludingalveolarcapillaries.Neutrophils arealsoinitiallyobservedwithinalveolarcapillaries, butinflammatorycellsthenaccumulaterapidlyinthe edematousalveoli.Overthenextfewdays,thelungs becomemoreuniformlyredasalveolarwallandairspaceedemaincreaseandredcellsleakintotheairspaces.Histologically,hyalinemembranesformfrom fibrin-richedemafluidandlinethealveoli.The numberofneutrophilsincreasesrapidlyastheymove viatheinterstitiumintotheairspaceandthereisincreaseddisruptionofvascularstructureswithfurther neutrophilandfibrinplugsoccludingcapillaries.
Aftertheinitialinjury,myofibroblastsareobserved intheinterstitiumandthentheairspace,andstartto producenewmatrixsubstance.Indeed,thelungcollagencontentcandoubleby2weeks.Withtime,type IIalveolarepithelialcellsincreaseinnumberand mayrepresentastemcellpopulationofthelung;they differentiateintotypeIalveolarepithelialcellsand repopulatethedenudedalveolarbasementmembraneduringhealing.
Pulmonaryfunctionandcomputedtomography (CT)suggestthatmanypatientssubsequentlyreturn tohavestructurallynormallungsalthoughthiscan takemonths.Somepatientshoweverdevelopsevere fibrosisinvolvingboththealveolarspaceandinterstitium.Atitsmostextreme,the‘honeycomb’ofadvancedfibroticlungdiseasemayform.Manyofthese patientssuccumbtointercurrentinfectionassociated withaprolongedICUstay.Afewcanrecoverwith incompleteresolutionofpulmonarydamage.
ClinicalFeatures Definition ThediagnosisofARDSisbasedonthecriteriadevelopedatthe1992American–Europeanconsensus conferenceandisillustratedin Table2.Sincethe definitiondoesnotconsidercurrentmanagement strategies,therelevanceofscenariosinwhichsuboptimalmechanicalventilationandmanagementcan influencewhethercriteriaaremetornotisnotclear. Thecutoffsforseverityofhypoxemiaarearbitrary, thedefinitionof‘acute’onsetlacksclarityandthe useofthechestX-rayopensthewayforindividual interpretation.Furtherlimitationsofthedefinition includetheinclusionofotherconditionsthatprobablyhavedifferentpathologicalprocesses(suchas severepneumocystiscariniiinfection,diffusealveolar hemorrhage),andexclusionofunilateraldiseasethat mayoccurfollowingpulmonarylobectomy.Nevertheless,thedefinitionissimpletouseandissupportedbyextensiveliterature.Post-mortemstudies havedemonstratedthatthedefinitionis84%sensitiveand94%specificfordiffusealveolardamage;its performanceinpatientswhosurviveisnotclear.
ChestradiographyBilateralairspaceshadowing ClinicalscenarioAcuteonsetandassociatedwithaconditionknowntocauseALI/ARDS LeftatrialpressureNodirectorclinicalevidenceofleftatrialhypertension(PAOP o18mmHg) OxygenationPaO2/FiO2 o39.9kPa(300mmHg)PaO2/FiO2 o26.6kPa (200mmHg)
PAOP,pulmonaryarteryocclusionpressure.
Table2 American–EuropeanconsensuscriteriafordiagnosingALIandARDS
NaturalHistory TheclinicalpictureofARDSisdominatedinitially byseverehypoxemiaduetomismatchingofventilationandperfusion.Indeed,intrapulmonaryshunting mayresultinoxygensaturationsthatarerelatively refractorytoincreasesintheinspiredoxygencontent.Decreasedpulmonarycomplianceincreasesthe workofbreathingandmostpatientsrequireendotrachealintubationandmechanicalventilation.
Fromapulmonaryperspective,thehighoxygen requirementspersistforsometime.Furtherincreases inthealveolar–arterialoxygengradientoccurwith ongoingpulmonaryinflammation,particularlyinthe settingofapositivefluidbalance,butmayalsoreflect asuperimposedventilatorypneumoniaorpneumothorax.Pneumothoracestendtooccurafterthefirst weekandmaytensionrapidly.Sincetheinflamed lungmaytethertothechestwall,pneumothoraces canbeloculatedandanterior,andthuseasilymissed onplainchestradiography.ThoracicCTmaybe requiredtolocatepneumothoracesaccurately. Surprisingly,despitedevastatingpulmonaryfailure, oxygenationoftenslowlyimprovesallowingwithdrawalofmechanicalventilation;formany,thismay takeweeksormonthsandoftennecessitatetemporarytracheostomy.Althoughdiseasecanremain compartmentalizedwithisolatedlungfailure,ARDS isusuallypartofthespectrumofsystemicinflammation;hence,patientsoftendemonstrateperipheral vasodilation,increasedcardiacoutputs,andsystemic hypotensionwhichmayrequiretheadministration ofvasopressorssuchasnorepinephrine.Secondary pulmonaryhypertensioncanoccurandresultin acuterightventricularfailure.Renaldysfunctionis alsocommonasistheneedforacuterenalsupport. Otherorganscanalsofailaspartofthisprocessand outcomeisrelatedtothenumberoffailingorgans. ThecourseofARDSisnotasmoothwaveofdeteriorationandrecovery.Rather,itisinterspersedby episodesofdeterioration(commonlylinkedwith intercurrentinfectionsuchasventilator-associated pneumoniaorline-relatedsepsis)andmanypatients needrepeatedepisodesofinotropeandotherorgan supportpriortofinalrecovery(ordemise).
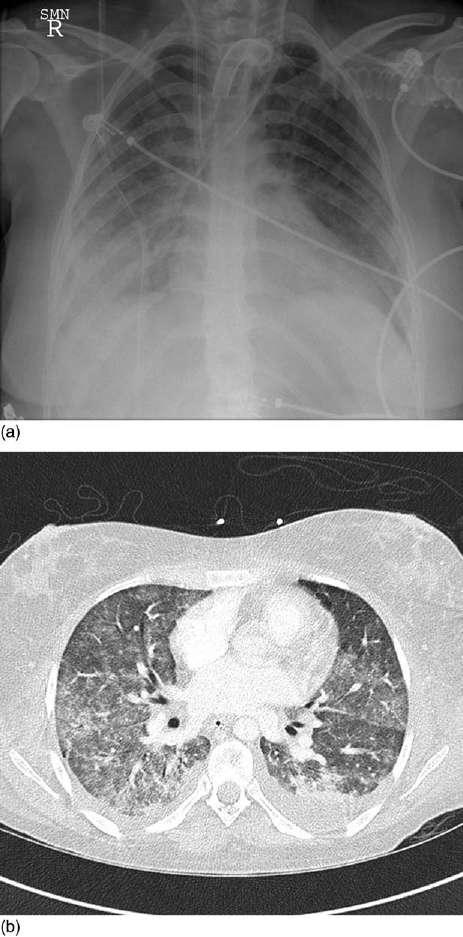
Radiology Theappearanceoftheplainchestradiograph,althoughformingpartoftheconsensusdefinitionfor ARDS,canberelativelynon-specific.CluesdistinguishingARDSfromcardiogenicpulmonaryedema includenormalcardiacdimensions,anormalvascularpediclewidth,aperipheraldistributionofairspaceshadowing,andtheabsenceofseptallines.
ChestCTdemonstratesthatthelungsareaffected inaheterogenousmanner.Typically,thereisagradientofopacificationfromapparentlynormally aeratedlung,throughground-glassappearances,to denselyconsolidatedlung.Inthesupinepatient,this gradientoccursbothinventrodorsalandcephalocaudaldirections.Thesegradientstypicallyreverse withinafewminutesifthepatientismovedtothe proneposition.Sincealveolaredemawouldnotredistributesoquickly,someoftheseappearanceare notduetoincreasededemaindependentzonesbut duetocollapseoftheseareasduetotheweightofthe overlyinglung.Thusground-glassappearancesmost likelyrepresentairspaceedema,withdenselyopacifiedareasrepresentingcollapsededematouslung. Regionsofdenseopacificationinnondependentareasmaysignifycollapse/consolidationduetoinfectionorretainedsecretions.Atlaterstages,groundglassappearancesmaybeaccompaniedbybronchial dilatationwhichpersistsintorecovery,suggesting establishedfineintralobularfibrosis(Figure1).
OtherPulmonaryInvestigations Bronchoalveolarlavagesamplesaredominatedbythe granulocyticcellpopulationinitially.Asthedisease evolves,theproportionofgranulocytesdeclinesanda greaterproportionofmacrophagesisseen.Persistent neutrophiliaoftenportendsapoorprognosis.
Sincemostpatientsaremechanicallyventilated, therearefewdataaboutclassicalpulmonaryfunctiontestsinpatientswithARDS.Re-breathingtechniqueshavebeenusedduringpositivepressure ventilationandhavedemonstratedmarkedreductionsinthefunctionalresidualcapacity,carbon monoxidediffusingcapacity(DLCO),anddiffusing coefficient(KCO).LowervaluesofDLCO and KCO tendtobeassociatedwithnonsurvival.
DiseaseSeverity Thereareseveralscoringsystemsthatevaluatethe severityofARDS.Althoughthesesystemshaveonly limitedclinicalutilityinindividuals,theydescribe wellthedegreeofphysiologicaldisturbanceandact asusefuldescriptorsofdiseaseseverityinclinical studies.ThescoringsystemsincludetheacutephysiologyandchronichealthevaluationIIandthelung injuryscore.TheformerisusedtoevaluateallcriticallyillpatientswhereasthelatterisspecificallydesignedforpatientswithARDS.
Pathogenesis Sinceneutrophilsappearearlyinhistologicalspecimensanddominateinbronchoalveolarfluidsamples,
ithasbeenconsideredthattheyareimportantinthe pathogenesisofARDS.Itispossiblethatactivated andthusrigid7.5 mmneutrophilsmaygetstuckin pulmonarycapillarieswheretheyreleaseaplethora ofinflammatorymediatorsthatincludechemokines, cytokines,andproteases.Activationmayoccurat remotesitesand/orbycirculatingcytokines.However,sinceARDScanoccurinneutropenicpatients, neutrophilscannotbeabsolutelyrequiredforthe developmentofARDS.Circulatinginflammatory mediators(e.g.,TNF-a,IL-1b,IL-6,IL-8,leukotrienes)alongwiththechangesthatoccurwithinthe coagulationsystemduringsystemicinflammationare
alsokeyinitiatorsofpulmonaryinflammationin ARDS.StudiesofpatientgroupsatriskofARDS whodoordonotprogresstodeveloprefractory hypoxemiasuggestcompartmentalizedintrapulmonaryinflammatorychanges(e.g.,increasedIL-8)may precedeasystemicinflammatoryresponse.
Thereiswidespreadactivationand/ordysfunction ofmanycelltypeswithinthelungwhichresultsin theclinicalmanifestationsofARDS(Figure2).Thus endothelialdysfunctionandlossofepithelialintegrityreducethebarrierfunctionofthealveolarwall andresultinalveolaredema.Alveolaredemaisfurtherexacerbatedbythelossofepithelialcellswhich normallypromotefluidtransportoutofthealveolus throughapicalsodiumpumps.Surfactantislostearly duringARDSduetoreducedproductionbydamaged epithelialcellsalongwithneutralizationofpreexistingsurfactantbytheprotein-richedemafluid. Surfactantlosscontributestoalveolarcollapse,intrapulmonaryshunt,andhypoxemia.Endothelial andsmoothmusclecelldysfunctionresultinimpairedhypoxicpulmonaryvasoconstrictionand, alongwithmicrothrombi,contributetothedevelopmentofsecondarypulmonaryhypertensionandalso impactsonoutcome.
AnimalModels AnimalmodelsallowthestudyofthepathophysiologyofARDSandtheeffectsofinterventionswhilst tightlycontrollingbothinsultsandgeneticbackground.However,themultiplemodelsthatexistfor ARDS/ALIillustratethatnoneareideal.Modelsin whichthelungisinjureddirectlyincludehyperoxia, hightidal-volumemechanicalventilation,andinstillationofoleicacid,bleomycin,orthiourea.Alternatively,modelsmimicsystemicsepsisinwhichthe lungisalsoinjured;theseincludesystemicinjections oflipopolysaccharideandcaecalligationandpuncture.Someauthorssuggestthattwo-hitmodelsare moreclinicallyappropriateandcombinemodelsof sepsiswithhypovolemia,burns,orhightidal-volume ventilation.
ManagementandCurrentTherapy Theprimarymanagementaimsforapatientwith ARDSaretomaintainadequateoxygenationand tosupportanyotherfailingorganswhilstthelung injuryresolves.Ingeneral,respiratoryfailureis sufficientlyseveretomandatemechanicalventilation, thetechniquesofwhichsignificantlyinfluencemortality.Bycontrast,few,ifany,therapiesdirectedat modifyingthepathogenesisandevolutionofARDS, havebeendemonstratedtoeffectoutcome.Adetailed
Figure1 TypicalappearancesofARDSwith(a)plainradiology and(b)computedtomography.
E.g., bacterial sepsis, massive transfusion
cell signaling
E.g., cytokines, chemokines, coagulation factors, eicosanoids, ROS
descriptionofoptimalmechanicalventilationalong withthepharmacotherapeuticapproachesthathave beenexploredareoutlinedbelow.
ConventionalMechanicalVentilation Themannerinwhichtheinjuredlungisventilated influencesmortalityandmayperpetuatelunginjury. Theoriginsofsuchventilator-inducedlunginjury (VILI)aremultifactorialbutincludetheshear stressesexertedonalveoliduringoverdistension andcyclicalcollapse/re-inflation,andoxygentoxicity.VILIisillustratedbychestCTofthosepatients whohavesurvivedARDS:relativelynormallungarchitectureisoftenpresentinpreviouslydenselyconsolidatedareas,whereasareticularpatternoffibrosis isseeninthoseregions(oftennondependent)that wereexposedtomechanicalventilation.VILIresults intheongoingreleaseofinflammatorymediators thatmayspilloverintothecirculationandpropagate systemicinflammation,therebyinfluencingmortality. Indeed,increasedplasmalevelsofcytokineshave beendemonstratedinanimalmodelsandinpatients receivinginjuriouslylargetidal-volumeventilation. Thistheoryhasstimulatedthedevelopmentofsocalled‘protective’strategiesformechanicalventilationwhichminimizeVILI.
Tidalvolume Deliveryofanormaltidalvolumeto extensivelyconsolidatedlungsinevitablyresultsin overdistensionoftheremaininglungunits.ExperimentalworkdemonstratedthatthismaybeasignificanttriggerforVILI,andresultedintheNational InstitutesofHealth(NIH)-sponsoredstudyoflow tidal-volumeventilationin861patients.Thislandmarkstudyshowedthatmortalitycouldbereduced bytheuseoflowertidalvolumes(4–6mlkg 1,ideal bodymass)oratleasttheavoidanceofmore‘traditional’tidalvolumes(10–12mlkg 1).Thecorrespondingplateauinspiratorypressureswere25and 35cmH2O,respectively.Plasmaandbronchoalveolar lavagecytokineandchemokineslevelsweregreater inthosepatientsreceivinghighertidalvolumes.The studyprotocolhasbeenadoptedbysomeasthedefinitiveventilatorystrategy.Morecorrectly,itprovidedexcellentevidenceforVILIandshouldform thebasisoflung-protectivestrategies.Indeed,ithas beensuggestedthattargetinglower-endexpiratory alveolarpressuresmaybemoresensible,sincethe specificpulmonarycompliance(compliancecorrectedforaccessiblelungvolume)hasbeenreported asnormalinpatientswithALI/ARDS.
SmallertidalvolumesmayreduceVILIbyvirtueof thereducedcyclicalvolume perse,orthroughareductionintheend-inspiratoryvolume.Itisnotclear
Activated neutrophils
Endothelial cells Soluble mediators
ventilation Epithelial cells Smooth muscle cells
edema
hypertension Alveolar collapse
Vascular dysfunction
dysfunction
Figure2 PathogenesisofARDSandALI.HPV,hypoxicpulmonaryvasoconstriction;ROS,reactiveoxygenspecies.
whichistheimportantfactoralthough invitro experimentsonmechanicallydeformedepitheliallayers havedemonstratedthatcyclicalchangesaremore damagingthanconstantstretchtoahighvolume. Howtheseresultstranslatetothe invivo scenariois notclear.
Intheabsenceofincreasedrespiratoryrates, reductionsintidalvolumewillreducealveolarventilationandresultinahypercapnicacidosis.Permissivehypercapniaisgenerallywelltoleratedexceptin thesettingofamarkedmetabolicacidosisandincreasedintracranialpressure.Hypercapniamayalso reducemyocardialcontractility,andpossiblyincreasetheneedforsedationand/orparalysis.The effectsontheimmuneresponsearestillunclear.The degreeofhypercapnicacidosisallowableisunclear althoughmanycliniciansacceptarterialpHvalues notlessthan7.20.Whentitratingrespiratoryrateto pCO2 ,itmustberememberedthatincreasesinrespiratoryratewillhavelessinfluenceonalveolarventilationinARDSduetotheincreaseddeadspace, andthatreductionsinrespiratoryratecanparadoxicallyincreaseCO2 clearancewheninspiratorytimes areparticularlyprolonged.Trachealinsufflationof oxygenandadministrationofweakbasesaresometimesusedtocombattheacidosis.
Fractionalinspiredoxygen Highfractionsofinspiredoxygen(FiO2)causeabsorptionatelectasis andmaybecytotoxictothelung perse.ThestandardpracticeistotitratetheFiO2 toarterialsaturationsof88–92%,ratherthanaspecificpO2 which maybelessrelevanttooxygendelivery.Lowertargetsmaybeappropriateinthosepatientswhose cardiacoutputishighorwhereanimprovement ofSaO2 wouldrequireanunacceptablyinjurious patternofventilation(e.g.,throughahigherFiO2, positiveendexpiratorypressure(PEEP),ortidalvolume).ThebenefitsoffurtherreductionsinFiO2 affordedbytheuseofinhalednitricoxide(iNO), pronepositioning,andrelatedmaneuversareunknownandstillsubjecttoreview(videinfra).Intrapulmonaryshuntingmayresultinarterialoxygen saturationsbeingrelativelyindependentofFiO2 between0.8and1.0.
Positiveendexpiratorypressure Theapplicationof PEEPduringmechanicalventilationincreasesFRC andthuspreventsthecollapseofalveoliatendexpiration.Thiswillreduceintrapulmonaryshuntand improveoxygenation.Furthermore,theshearforces requiredtorepeatedlyopencollapsedalveoliduring inspirationareconsiderableandmostlikelycontributetoVILI.Thus,bykeepingthesealveoliopen throughouttherespiratorycycle,PEEPcanlimit
VILI.Sincethelungisheterogeneouslyaffectedin ARDS,excessivelyhighlevelsofPEEPcanleadto overexpansionofthoseregionswhosecomplianceis higher,aneffectthatmayexacerbateVILI.Other detrimentaleffectsofPEEPincludereducedcardiac preloadandcerebralperfusion.
Themethodtodeterminetheoptimallevelof PEEPinARDSisstillnotestablished.Arandomized multicentertrialin549patients,titratingPEEPaccordingtotherequiredFiO2,foundnooutcomedifferencesbetweenalowerandhigherPEEPalgorithm. ManyclinicianssetPEEPbyinferringtheregionof maximalslopeonthepressure–volumecurvebyassessingmaximaltidalvolumeasPEEPisadjusted withaconstantpressurecontrol.Mathematical modelingsuggeststhatthisisbestdeterminedusing adecrementalratherthananincrementalPEEPtrial.
Ventilatorymodes TheNIHtrialoflowertidal-volumeventilationusedamandatoryconstantflow,volumecontrolmodeofmandatoryventilation.Thereis considerableinterestintheroleofdescendingflow/ pressurecontrolmodessincethesemaypromotemore evendistributionofgas,asflowisslowerattheendof expirationandthusmorelikelytobelaminar.Pressure-controlmodesdonotinfluencepeakalveolar pressure,althoughpeakairwaypressuresmaybereduced.Themostlikelyadvantageaffordedbypressurecontrolventilationandinverseratioventilationis thatthesemaybeassociatedwithagreaterproportionoftherespiratorycyclespentatplateauinspiratorypressure.Greaterplateautimespromotemore homogenousventilationbyallowingslow-fillingregionstointer-fillfromareaswithfastertimeconstants.Therecruitmentofpreviouslycollapsedor partiallycollapsedslow-fillingalveolireducesshunt andimprovesoxygenation.ProlongationofinspirationcanalsoimproveCO2 clearancebyforcingexpirationtobedelayedtoapointwherealveolarpCO2 hasrisentoamaximum.Fasterrespiratoryratesreducetheefficacyofinverseratioventilationbyshorteningtheinspiratorytime.Excessiveprolongationof inspirationmayreduceexpiratorytimetoapointat whichexpirationisnotcompleted.Thismayresultin dynamichyperinflationandthegenerationofautoPEEP.Mostcliniciansconsiderauto-PEEPundesirablesincelevelsmaybeunpredictablethusleadingto cardiovascularcompromise.
Therearetheoreticaladvantagestomodesthatallowspontaneousventilationsuchasbiphasicpositive airwaypressureandairwaypressurereleaseventilation.Thesemodesallowcontinueddiaphragmatic andintercostalfunctionandtheventilationofdependent,better-perfusedregions.Althoughpressure supportmodesalsoallowspontaneousventilation,
someargueagainstthemastheyprecludeanyplateautime.
Nostudytodate,excludingthoseexamining weaning,hasdemonstratedanyoutcomedifferences accordingtoventilatorymode.
Drainageofpneumothoraces MultiplepneumothoracesmaycomplicatemechanicalventilationofpatientswithARDS.Pneumothoracescanbecomplex andlocalizedastheinflamedlungmaytethertothe chestwall.Indeed,localizationcanbedifficultbyconventionalradiographyanditmaybenecessarytoinsertdrainsundertheguidanceofCT.Intercostaldrains aregenerallyleft insitu untilthepatientiswellestablishedonaspontaneousventilatoryweaningprogram.
SupplementalTechniquesforMechanical Ventilation Pronepositioning Ventilationintheproneposition improvesoxygenationinapproximately70%ofpatients.Itisnotpossibletopredictwhichpatientswill respond,andnonrespondersmayimproveonsubsequentturns.Experiencedteamscaneasilyturn patients,evenwithmultipleintercostaldrainsand intravascularcatheters,withfewcomplications.Improvementsinoxygenationcontinuein50%ofpatientsaftertheyarereturnedtothesupineposition andareprobablytheconsequenceofexpansionof previouslycollapsedlung.Morehomogenousventilationmaypreventregionaloverdistensionandlimit VILI.Improvedsecretiondrainageandaltereddiaphragmaticmechanicsmayalsocontributetoclinical improvement.Despiteimprovementsinoxygenation, pronepositioninghasnotbeendemonstratedtoimproveoutcomeinARDS.
Recruitmentmaneuvers Sustainedandhighairway pressuresofupto60cmH2Omayberequiredto open(orrecruit)someregionsofcollapsedlung. Therehasbeenconsiderableenthusiasmfortheuse ofsuchrecruitmentmaneuverswhich,incombinationwiththeapplicationofPEEP,maykeepthese newlyrecruitedlungunitsopen.Techniquesvary fromsophisticateddeterminationofrecruitmentand derecruitmentbystepwisealterationofventilatory pressuresandrepeatedbloodgassamplingthrough tosimplytemporarilyincreasingPEEPto30cmH2O for30s.Improvementsinoxygenationhaveoften beendemonstrated,althoughthesemaynotbesustained.Suchhighintrathoracicpressuresareoften accompaniedbybriefepisodesofreducedcardiac outputandhypotension,butrarelybarotrauma.The roleofrecruitmentmaneuversstillhastobeclarified inARDS.
Partialliquidventilation Partialliquidventilation hasbeenproposedtoimproveoxygenationandlimit VILI.Perfluorocarbonsaredenseliquidsthathave littlebiologicalactivitybutverylowsurfacetension andexceptionallyhigh-solubilitycoefficientsforoxygenandcarbondioxide.Thelungisfilled(partially orfully)withtheperfluorocarbonandthennormal mechanicalventilationappliedsimultaneously.Since theperfluorocarbonisvolatile,itevaporatesover timethroughtheventilatorcircuit.Animalstudies suggestthatperfluorocarbonsreduceatelectasis, improveperfusionmatching,andimprovesecretion clearance.Somestudiessuggesttheymayalsobe anti-inflammatory,reducingpermeabilityrisesand neutrophilactivation.Humanstudieshaverevealed anincreaseintheincidenceofpneumothoraces,mucusplugging,andadisruptionofthenormalsurfactantsystem.Theyareingestedbymacrophagesand theireffectonimmunefunctionisunclear.Aphase II/IIIstudyofpartial-liquidventilationisunderway inFrancecurrently.
Extracorporealgasexchange Traditionally,extracorporealgasexchange(ECGE)hasonlybeenused asalastresortinpatientsinwhomoxygenation cannotbemaintainedbyanyothermeans.Devices varyfromthosewhichoxygenateandsupportthe wholecardiacoutput,tothosethatprovidepartial oxygenation,andcarbondioxideremovaltosupplementconventionalventilationatlowerpressures (extracorporeallungassist,ECLA).Hemorrhageand coagulopathieshavebeenthemostsignificantcomplications,occurringinabout67%ofadultpatients. Althoughnomortalityadvantagehaseverbeen shownforECGE,newtechnologysuchasheparinbondedcircuits,nonocclusiverollerpumps,pumplesscircuits,andbetteranticoagulationcontrol,that mayreducecomplicationsisleadingtoare-evaluationofthismodality.
Surfactantadministration Alveolarsurfactantis lostearlyinARDS.Theadministrationofexogenous surfactanteitherviaabronchoscopeornebulizer mayreducesurfacetensionwithinalveoliandpreventcyclicalcollapse,improvingoxygenation,and amelioratingVILI.Multipleadministrationsappear necessaryduetotheneutralizationofsurfactantby edemafluid.Despiteimprovementsinoxygenation andphaseI/IIsurvivalbenefits,nolargestudiesof surfactanthavedemonstratedanymortalityadvantageandthusitisnotadministeredtopatientswith ARDS.However,therearemanyoutstandingquestionsregardingtheoptimalformulation,patient selection,anddosingregimen.