Little Lovely Things Maureen Joyce Connolly
https://ebookmass.com/product/little-lovely-things-maureen-joyceconnolly/
ebookmass.com
Western Civilization: A Brief History, Volume II: Since 1500 8th Edition, (Ebook PDF)
https://ebookmass.com/product/western-civilization-a-brief-historyvolume-ii-since-1500-8th-edition-ebook-pdf/
ebookmass.com
Endangered Species and Fragile Ecosystems in the South China Sea: The Philippines v. China Arbitration 1st ed. 2020 Edition Alfredo C. Robles
https://ebookmass.com/product/endangered-species-and-fragileecosystems-in-the-south-china-sea-the-philippines-v-chinaarbitration-1st-ed-2020-edition-alfredo-c-robles/
ebookmass.com
The Island Home: The book making life brighter in 2021 Libby Page
https://ebookmass.com/product/the-island-home-the-book-making-lifebrighter-in-2021-libby-page/
ebookmass.com
An Epistemic Theory of Democracy Robert E Goodin
https://ebookmass.com/product/an-epistemic-theory-of-democracy-roberte-goodin/
ebookmass.com
The 1 Day Refund: Take Back Time, Spend it Wisely Donna Mcgeorge
https://ebookmass.com/product/the-1-day-refund-take-back-time-spendit-wisely-donna-mcgeorge/
ebookmass.com
ELSEVIER
3251 lllverport Lane
St. Louis, Mbsouri 63043
ECGt MADE EASY, SIXTH EDITION
Copyright c 2018, lllsevier IDe. All r!pta raene4. Prnloue e4itloall copyrlpted 2013,2011, 2006, 2002, uull995.
ISBN: 978-0-32340130-2
No part ofthil publication may be reproduced or transmitted in any form or by any mean1, electronk or mechanical, including photocopying, .recording. or any in!ormali.on stDrap and Rtrieval. systmn. without permilaion in writing from the publiaher. Details on how to 1eek penniasion. further information about the Publither's permi.lsi.OIIJ policies and our arrangements with organi2al:ian.t such as the Copyright Clearance Center and the Copyright Licenalng Agency, can be fuWld at our webalte: www.ellevier.com/permiaaiona.
This book and the lndlvldual contributl01111 contained In It are protected Wlder copyright by the Publilher (other than u may be noted herein).
Notices
Knowledge and best practice in this field aR constantly changing. N new research and experience broaden our undemanding, changes in research method.t, profesrional practices, or medical treatment may become neceuary.
and researchers must alwaya rely on their own aperlence and knowledge In evaluating and uaing any Information, methods, compound&, or aperlmentl described herein. In usiDg tuc.h information or method. they should be mindful of their own takty and the takty of others, including parties fur whom they have a professional Rtpoll8ibility.
With respect. to any drug or pharmaceutical pmduct& ident:ified. reader• are adviled to check the mo1t information provided (i) on procedURS fealuRd or (ii) by the manufacturer of each product to be administered. to verify the .recommended dose or formula, the method and duration ofadminiltration, and contnindlcatiOIIJ. It is the responsibility of practitioners, relying on their own experience and knowledge of their patients, to make to determine doaget and the belt t.reatment for each individual patienl, and to take all appropriate sarety precautionl.
To the fulli:st ment of the law, neither the Publisher nor the alrthon, contributors, or editor1, UNme any liability fur any injury and/or damage to peraom or property u a matter of produculiabllity, nesJigence or otherwile, or from any uae or operation of any method&, product., imtruction1, or ideu contained in the m:rterial herein.
Name.: Aehlert, Barbara, author.
Title: ECGa made easy I Barbara Aehlert, MSEd, BSPA, RN.
Description: Sixth edition. I Phoenix, Arizona : Southwest EMS Education, Inc., [2018liindudes blhllographical refuences and lnda. I Identifiers: LCCN 2017015081 (print) I LCCN 2017026543 (ebook) I ISBN 9780323479059 () I ISBN 9780323401302 (pbk. : a1k. paper)
Subjecu: LCSH: Electrocardiography--Handboob. manuals. etc.
Cl.ulifi.c:ation: LCC RC683.5.F.5 (ebook) I LCC RC683.5.E5 A39 2018 (print) I DDC 616.1/207547--dc23
LC record available at httpt:!/ka1loc.gov/2017015081
Executive Contel!t Stmteglst: Sandra Clark
Content Developmettt SpeclalUU: Laura SeltlrtiMelissa. Kinsey
Publishing Semcu Manager. Deepthi Unni
SenWr Project MaMpr. Umarani Na1arajan
Dirmton: Brian Saliabury
in Canada Last digit is the print number: 9 8 7 6 5 4 3 2 1
Many years ago, as a green but enthusiastic nurse preparing to shift from medical-surgical nursing to critical care, I signed up for a course in basic ECG recognition. It was an intimidating experience. My i.nst:ructor was extremely knowledgeable and kind. and I studied diligently throughout the course, yet I struggled to crack the code of heart rhythm interpretation. To make matters worse, I couldn't find any resources in which these complex concepts were presented in a practical, useful way. Although I passed the course. I decided to repeat it a few months later because I simply coulchlt recall and apply the infonnation I needed to help my patients
After successfully completing the second course, I promised myself that I would someday present these concepts in a simpler way. 'Ihat promise became my life's work. Ever since then, I have been looking for better ways in which to present the skill of basic ECG recognition to those who will apply that knowledge every working day:
• Paramedics
• Nursing and medical students
• ECG monitor technicians
• Nurses and other allied health personnel world.ng in emergency departments, critical care units, postanesthesia care units, operating rooms, and telemetry units
'!his book can be used alone or as part of a formal course of instruction in basic dysrhythmia recognition. 1he book'• content focuses on the essentials of ECG interpretation. Each ECG rhythm is described and accompanied by a sample rhythm strip. 1hen the discussion turns to possible signs and symptoms related to each rhythm and. where appropriate, current recommended treatment. At the end of each chapter, additional rhythm strips and their description.s are provided for practice. (All rhythm strips shown in this text were recorded in lead n unless otherwise noted.) 1he Stop 8c Review exerci!es at the end of each chapter are self-usessment activities that allow you to check your learning.
In addition, resources to aid the in.stru.ctor in teaching this content can be found on Evolve at http://evolve.elsevier.com/Aehlert/ecgl 1hese resources include:
• Image Collection
• PPTSlide.
• PPT Practice Slides
• TEACH2.4
• Test Bank
I have made every attempt to supply content consistent with current literature, including current resuscitation guidelines. However, medicine is a dynamic field. Recommendations change as medical research evolves, technology improves, and new medications, procedures, and devices are developed. As a result, be •ure to learn and follow local protocols as defined by your medical advisors. Neither I nor the publisher can assume responsibility or liability for loss or damage resulting from the use of information contained within.
I genuinely hope this book is helpful to you, and I wish you success in your studies and clinical practice.
Best regards, Barbara
Aehlert
I would like to thank the manuscript reviewers foc their commenb and suggestiom. Areu of this text were rewritten, reorganized, and clarified because of your effom.
I would also like to thank the following health care professionals, who provided many of the rhythm strips used in this book: Andrew Baird, CEP; James Bratcher; Joanna Burgan, CEP; Holly Button, CEP; Gretchen Chalmers, CEP; 'Ihomas Cole, CEP; Brent Haines, CEP; Paul Honeywell, CEP; Timothy Klatt. RN; Bill Loughran. RN; Andrea Lowrey, RN; Joe Martinez, CEP; St.ephanos Orphanidis, CEP; Jason Payne, CEP; Steve Ruehs, CEP; Patty Seneski, RN; David Stockton, CEP; Jason Stodghill, CEP; Dionne Socie, CEP; Kristina Tellez, CEP; and Fran Wojculewicz, RN.
A special thanks to Melissa Kinsey for her humor, guidance, advice, and impeccable attention to detail throughout this project.
To Deepak C. Patel, MD
whose knowledge, humor, and genuine compassion for his patients are unparalleled.
Krlaten Bon:IWt, llN, MSN, PNP, Nll-P, CPN Care Coordinator Cincinnati Childrms Hospital Medical Center Cincinnati, Ohio
Joshua BorkoU:.y, BS, pp.c EMS Education Manager University of Cincinnati College of Medicine Cincinnati, Ohio
Angela McConachie, DNP, MSN-PNP, RN Assistant Professor Goldfarb School ofNursing at Barnes-Jewish College St Louis, Missouri
BiB Miller Paramedic Crew Chief St. Louis Fire Department-HEMS St. Louis, Missouri
Mark.Nootena, MD, PACC Cardiologist. Private Practice Munster, Indiana
Ruth C. Tamulonis, MS, RN Nursing Professor Yuba College Marysville, California
Barbara Aehlert, MSBd, BSPA, RN, has been a registered nurse for more than 40 years. with clinical experience in medicallsurgical nursing. critical care nursing, prehotpital education, and nursing education. Barbara i.s an active CPR and Advanced Cardiovascular Life Support (ACLS) instructor with a special interest in teaching basic dysrhythmia recognition and ACLS to nurses and paramedics.
1 ANATOMY AND PHYSIOLOGY, 1
Location. SJu, and Shape of the Heart. 2
Surfaca ofthe Heart. 2
Coverinp of the Heart, 2
Structure of the Heart, 5
Layers ofthe Heart WalL 5 Heart Chambers, 6 Heart Valves, 8
The Heart's Blood Supply, 11
The Heart's Nerve Supply, 16
The Heart aa a Pump, 19
Cardiac Cycle, 19
Blood PreS3Ul't, 20
R£ferenca, '1.7
2 BASIC ELECTROPHYSIOLOGY, 28
Cardiac Cella, 30
Types of Cardiac Cells, 30
Propertia of Cardiac Cells, 30
Cardiac Action Potmtial, 30
Polarization, 31
Depolarization, 31
Repolarization, 32
Phases of the Cardiac Action Potential, 32
Refractory Periods, 34
Conduction Syatem, 35
Sinoatrial Node, 35
Atrioventricular Node and Bundle, 37 Right and Left Bundle Branches, 38
Purkinje Fibers, 38
Cauaea of Dyarhythmiaa, 39
Disorders of Impulse Formation, 39
Disorders of Impulse Conduction, 39
The Ela:trocardiogr, 41 Electrodes, 41 Leads, 42
Ambulatory Cardiac Monitoring, 46
Blectrocanliopaphy Paper, 47
Waveforms, 48
Segments, 53 Intervals, 55 Artifact. 56
Symmatic Rhythm J:nterpretation. 57
Asseas Regularity, 57
Asseas Rate, 58
Identify and Examine Waveforms, 60
Asseaslntervals and Examine Segments, 60
Interpret the Rhythm, 60
Re&renca, 74
3 SINUS MECHANISMS, 78
Introdudlon. 76
Sinua Rhythm, 77
How Do I Recognize It? 77
Sinua Bradycardia. 78
How Do I Recognize It? 78 What Causes m 78 What Do I Do About It? 79
Sinua Tadlyardia, 80
How Do I Recognize It? 80 What Causes It? 80 What Do I Do About It? 81
Sinua Arrbytbmia, 81
How Do I Recognize It? 81 What Causes It! 81 What Do I Do About It? 82
Sinoatrial Block. 82
How Do I Recognize It? 82 What Causes It? 82
What Do I Do About It? 83
Sinua Arrest, 83
How Do I Recognize It? 83
What Causes It? 83
What Do I Do About It? 84
Referencea,IOI
4 ATRIAL RHYTHMS, 102
Introduction, 103
Atrial Dyar.bythmiaa: 103
Abnormal Automaticity, 103
Tnggered Activity, 103 Reentry, 104
Premature Atrial Compleea, 104
How Do I Recognize It? 104
Noncompensatory versus Compensatory Pause, 105
Aberrantly Conducted Premature Atrial Complexes, 106
Nonconducted Premature Atrial Complexes, 106
What Do I Do About Them? 107
Wuuleriq Atrial Pacemaker, 107
How Do I Recognize It? 107 What Causes It? 107
What Do I Do About It? 107
Mal.tifoc:al Atrial Tachycanlia, 108
How Do I Recognize It? 108 What Causes It? 108
What Do I Do About It? 108
Supraventricular 'Thchycardia, 108
Atrial Tachycardias, 109
Atrioventricular Nodal Reentrant Tachycardia, 113
Atrioventricular Reentrant Thchycardia, 114
Atrial Flutter, 117
How Do I Recognize It? 117
What Causes It? 118
What Do I Do About It? 118
Atrial Fibrillation, 119
How Do I Recognize It? 119
What Causes It? 121
What Do I Do About It? 121 References, 140
5 RHYTHMS, 141
Introduction, 141
Premature Juncticmal Compleus, 142
How Do I Recognize 142
What Causes 1hem? 143
What Do I Do About Them? 143
Junctional Escape Beau or Rhythm, 144
How Do I Recognize It? 144
What Causes It? 145
What Do I Do About It? 146
Accelerated Junctional Rhythm, 146
How Do I Recognize It? 146
What Causes It? 146
What Do I Do About It? 146
Junctional Tachyardia. 146
How Do I Recognize It? 146 What Causes It? 147
What Do I Do About It? 147 References, 164
6 VENTRICULAR RHYTHMS, 165
Introductlon,166
Premature Ventricular Complexes, 166
How Do I Recognize 166
What Causes 1hem? 170
What Do I Do About Them? 170
Ventricular .Escape Beats or Rhythm,170
How Do I Recognize It? 170
What Causes It? 172
What Do I Do About It? 172
Accelerated Idlovmtrl<:Ular :Rhythm. 172
How Do I Recognize It? 172 What Causes It? 172
What Do I Do About It? 173
Ventricnlar Tachycardia, 173
How Do I Recognize It? 173
Ventricular Fibrillation, 176
How Do I Recognize It? 176
What Causes It? 177
What Do I Do About It? 177
How Do I Recognize It? 177 What Causes It? 178
What Do I Do About It? 178 References, 193
7 ATRIOVENTRICULAR BLOCKS, 194
Introduction, 194
First-Degree Atrioventricalar Block, 195
How Do I Recognize It? 195
What Causes It? 196
What Do I Do About It? 197
Second-Degree Atrioventricular Blocks, 197
Second-Degree Atrioventricular Block Type I, 197
How Do I Recognize It? 197
What Causes It? 198
What Do I Do About It? 199
Second-Degree Atrioventricular Block Type ll, 199
How Do I Recognize It? 199
What Causes It? 200
What Do I Do About It? 200
2:1 Atriovmtricalar moa, 200
How Do I Recognize It? 200
Advanced Second-Degree Atriovent:rkular Block. 201 'Ihird-Degree Atrioventricu1ar Block, 202.
How Do I Recognize It? 202
What Causes It? 203
What Do I Do About It? 203
Reference8, 221
B PACEMAKER RHYTHMS, 222
Pacemaker Systema. 223
Permanent Pacemakers and hnplantable CardioverterDefibrillators, 223
Temporary Pacemakers, 224
Pacing Lead Symms, 225
Padng Chamben and Modes, 226
Single-Chamber Pacemakers, 226
Dual-Chamber Pacemakers, 227
Biventricular Pacemakers, 227
Fixed-Rate Pacemakers, 227
Demand Pacemakers, 227
Pacemaker Codes, 228
Pacemaker Malfunction.l28
Failure to Pace, 228
Failure to Capture, 229
Failure to Sense, 230
Analyzing Pacemaker Fund:ion on the ECG, 230
Reference., 240
9 INTRODUCTION TO THE 12-LEAD ECG, 241
Introduction, 141
Layout of the 12-Lead Electrocardiogram, 242 Vedors,242
Axis,243
.Acute Coronary Syndromes, 244
Anatomic Location of a Myocardial Infarction, 246
Intraventricular Conduction Delays, 254
Structures of the Intraventricular Conduction System,254
Bundle Branch Activation, 254
How Do I Recognize It? 254
What Causes It? 257
What Do I Do About It? 257
Chamber Enlargement, 257
Atrial .Abnormalities, 258
Ventricular Abnormalities. 259
Electrolyte Disturbances, 260
Sodium, 261
Potassium, 261
Calcium, 262
Magnesium, 263
ADalyzing the 12-Lead EledJ:ocanUogram, 263 References, 277
10 POSlTEST, 278
INDEX, 321
LEARNING OBJECTIVES
After reading this chapter, you should be able to:
1. Describe the location of the heart.
2. Identify the surfaces of the heart.
3. Describe the structure and function of the coverings of the heart.
4. Identify the three cardiac muscle layers.
5. Identify and describe the chambers of the heart and the vessels that enter or leave each.
6. Identify and describe the location of the atrioventricular and semilunar valves.
7. Explain atrial kick.
8. Name the primary branches and areas of the heart supplied by the right and left coronary arteries.
KEY TERMS
acute coronary syndrome (ACS): A term used to refert o distinct conditions caused by a similar sequence of pathologic eventsa temporary or permanent blockage of a coronar_y artery. These conditions are characterized by an excessive dem nd or inadequate supply of oxygen and nutrients to the heart muscle associated with plaque disruption, thrombus formation, and vasoconstriction. ACSs consist of three major syndromes: unstable angina, nonST-elevation myocardial infarction, and ST elevation myocardial infarction.
afterload: The pressure or resistance against which the ventricles must pump to eject blood.
angina pectoris: Chest discomfort or other related symptoms of sudden onset that may occur because the increased oxygen demand of the heart temporarily exceeds the blood supply.
apex of the heart: Lower portion of the heart that is formed by the tip of the left ventricle.
atria: Two upper chambers of the heart (singular, atrium).
atrial kick: Blood pushed into the ventricles because of atrial contraction. atrioventricular (AV) valve: The valve located between each atrium and ventricle; the tricuspid separates the right atrium from the right ventricle, and the mitral (bicuspid) separates the left atrium from the left ventricle.
atypical presentation: Uncharacteristic signs and symptoms perceived by some patients experiencing a medical condition, such as an ACS.
9. Define and explain acute coronary syndromes.
10. Discuss myocardial ischemia, injury, and infarction, indicating which conditions are reversible and which are not.
11. Compare and contrast the effects of sympathetic and parasympathetic stimulation of the heart.
12. Identify and discuss each phase of the cardiac cycle.
13. Beginning with the right atrium, describe blood flow through the normal heart and lungs to the systemic circulation.
14. Identify and explain the components of blood pressure and cardiac output.
base of the heart: Posterior surface of the heart.
blood pressure: Force exerted by the blood against the walls of the arteries as the ventricles of the heart contract and relax.
cardiac output (CO): The amount of blood pumped into the aorta each minute by the heart; defined as the stroke volume multiplied by the heart rate.
chordae tendineae (tendinous cords): Thin strands of fibrous connective tissue that extend from the AV valves to the papillary muscles that prevent the AV valves from bulging back into the atria during ventricular systole (contraction).
chronotropy: A change in (heart) rate.
diastole: Phase of the cardiac cycle in which the atria and ventricles relax between contractions and blood enters these chambers. When the term is used without reference to a specific chamber of the heart, ventricular diastole is implied.
dromotropy: Refers to the speed of conduction through the AV junction.
dysrhythmia: Any disturbance or abnormality in a normal rhythmic pattern; any cardiac rhythm other than a sinus rhythm.
ejection fraction: The percentage of blood pumped out of a heart chamber with each contraction.
endocardium: Innermost layer of the heart that lines the inside of the myocardium and covers the heart valves.
epicardium: Also known as the visceral pericardium; the external layer of the heart wall that covers the heart muscle.
hBart failure: Acondition In whlctl the heart Is unable tD pump enough blood to meet the metabolic needs of the body; It may result from any that impairs preload, afterload, cardiac contractility, or heart rare.
inDtropy: Refers to a change in myocardial contractility.
ischemia: Decreased supply of oxygena1ed blood tn a body part or organ.
mediastinum: Middle area of the thoracic cavity; contains the heart, great vessels, trachea, and esophagus, among other structures; extends from the sternum to the vertebral column.
mltochondrta: The energy-producing parts of a cell.
mvocardlallnfarctlon Death of some mass of the heart muscle caused by an Inadequate blood supply.
mvocardlum: Middle and thickest layer of the heart; contains the cardiac muscle fibers that cause contraction of the heart and contal ns the conduction system and blood supply.
myofibril: Slender striated strand of muscle tissue.
papillary muscles: Muscles attached to the chordae mndineae of the AV valves and the ventricular muscle of the heart that help prevent the AV valves from bulging too far intn the abia.
pericardium: A double-walled sac thai erdoses the heart and helps protect It from trauma and Infection.
peripheral resistance: Resistance to the flow of blood determined by blood vessel diameter and the tone of the vascular musculature. preload: Force exerted by the blood on the walls of the venb1cles at the end of diastole.
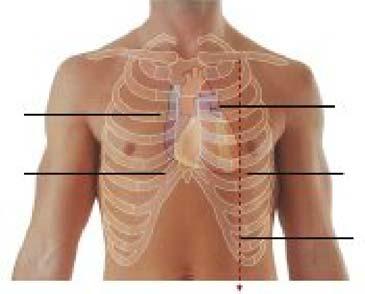
LOCATION, SIZE, AND SHAPE OFTHEHEART
[Oblectlve 1]
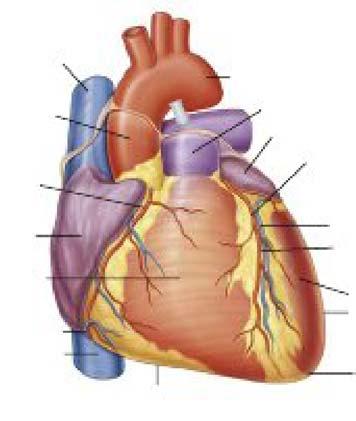
The heart is a hollow muscular organ that lies in the space between the lungs (i.e., the mediastinum) in the middle of the chest (Pig. 1.1). It sits behind the stemwn and just above the diaphragm. About two thirds of the heart lies to the left ofthe midline ofthe stemwn. The remaining third lies to the right of the sternum.
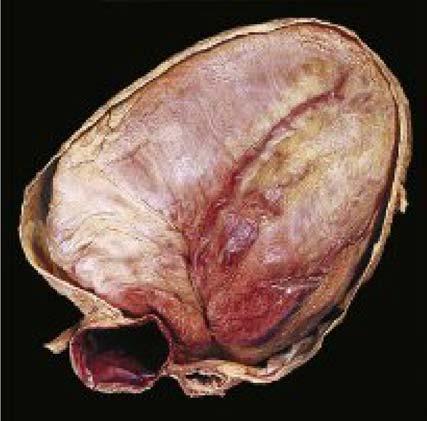
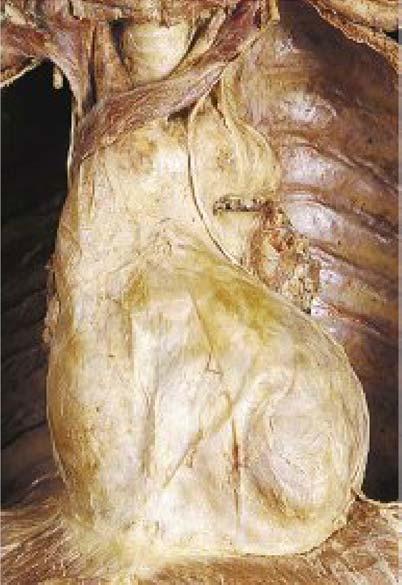
The adult heart is about 5 inches (12 an) long, 3.5 inches (9 em) wide, and 2.5 inches (6 em) thick (Fig_ 1.2). It typically weighs between 250 and 350 g (about 11 oz) and is about the size of its owner's fist The weight of the heart is about 0.4596 ofa man's body weight and about 0.40% of a woman's, A person's heart size and weight are influenced by his or her age, body weight and build. frequency of physical exercise, and heart disease.
SURFACES OF THE HEART
[Obiactiva 2]
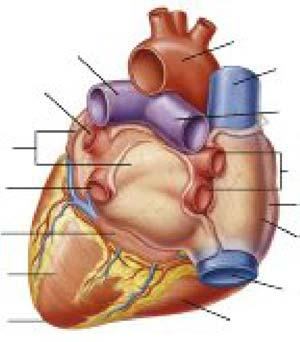
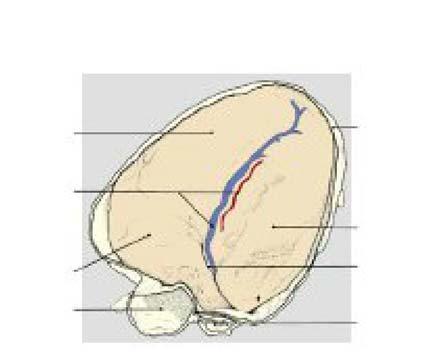
The base, or posterior surface, ofthe heart is formed by the left atrium, a small portion of the right atrium, and proximal portions of the superior and inferior venae cavae and the pulmonary veins (Fig. 1.3). The front (anterior) surface ofthe heart lies behind the sternum and costal cartilages. It is
pi'Oldmal: Location nearer to the midline of the body or the point of attachment than something else Is.
sarcolemma: Membrane that covers smooth, striated, and cardiac muscle fibers.
sarcomere: Smallest functional of a myofibril.
sarcoplasm: SemWiuid cytnplasm of muscle cells.
sarcoplasmic reticulum: Network of tubules and sacs that plays an important role in muscle contraction and relalration by releasing and storing calcium Ions.
semilunar (SL) valves: Valves shaped like half-moons that separate the ventricles from the aorta and pulmonary artery.
septum: An lntBmal wall of connective tissue.
stroke volume {SV): The amount of blood e]eclBd from a ventricle with each heartbeat
sulcus: Groove.
systole: Contraction of the heart (usually refarri ng to ventricular contraction), during which blood is propelled intn the pulmonary artery and aorta; when the tenn is used without reference to a specific chamber of the heart, ventricular systole is implied.
tone: A term that may be used when referring to the normal state of balanced tension In body tissues.
venous return: Amount of blood flowing lntn the right atrium each minute from the syslemlc c1 rculatlon.
venb1cles: The two lower chambers of the heart
formed by portions of the right atrium and the left and right vmtrides (Fig. 1.4). However, because the heart is tilted slightly toward the left in the chest, the right ventricle is the area of the heart that lies most directly behind the sternum. The apa, or lower portion, ofthe heart is formed by the tip of the left ventricle. The apex lies just above the diaphragm at about the level of the fifth intercostal space in the midclavicular line.
The heart's left side (i.e., left lateral surface) faces the left lung and is made up mostly of the left ventricle and a portion of the left atrium. The right lateral surface faces the right lung and consists of the right atrium. The heart's bottom (i.e., inferior) surface is formed primarily by the left ventricle, with small portions of the right ventricle and right atrium. The right and left ventricles are separated by a groove containing the posterior interventricular vessels. Because the inferior surface of the heart rests on the diaphragm, it is also called the diaphragmatic surface (Fig. 1.5).
COVERINGS OF THE HEART
[Obiactive 3)
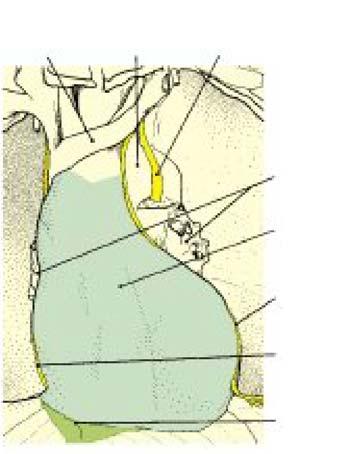
The periQU'dium is a double-walled sac that encloses the heart and helps protect it from trauma and infection. The tough outer layer of the pericardia! sac is called the fibrous parietal pericardium (Fig. 1.6). It anchors the heart to some
Mldclavlcular line
Fig. 1.1 Antar1or v1aw of tha chest wall of a man lhM!rg skslalal structullls and the surface projactlon of the heart (From Draka R, Vogl AW, Mlb:hall AWM: Gtay's 8II8JDmy for studsnts, ed 3, New York, 2015, Churchill LMngstooe.)
1.3 The base af the heart. (Ffm1 Drake R, 'ql A.W, Milcrell A."WM: &ay's anaiDmy for stJJdents, ed 3, New York, 2015, Churchill
The right and left phrenic nerves, which innervate the diaphragm, pass through the fibrous pericardium as they descend to the diaphragm. Because these nerves supply sensory fibers to the fibrous pericardium, the parietal serous pericardium, and the mediastinal pleura, discomfort related to conditions affecting the pericardium may be felt In the areas above the shoulders or lateral neck.
of the structures around it. such as the sternum and diaphragm, by means of ligaments. This helps prevent excessive movement of the heart in the chest with changes in body position.
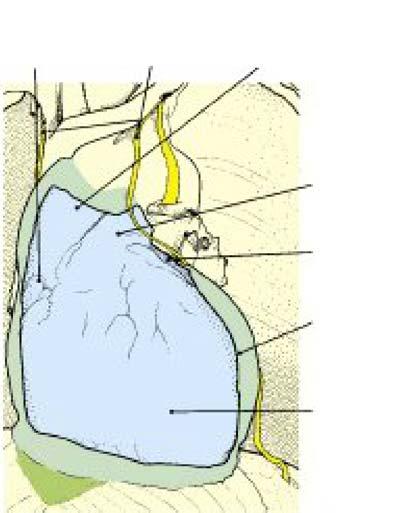
The inner layer of the pericardium, the serous pericardium, consists of two layers: parietal and visceral (Fig. 1.7). the parietal. layer lines the inside of the fibrous pericardium. The visceral layer attaches to the large vessels that enter and exit the heart and covers the outer surface ofthe heart muscle (ie., the epicardium).
Between the visceral and parietal layers is a space (the pericardia! space) that normally contains about 20 mL of serous (pale yellow and transparent) fluid. This fluid acts as a lubricant, preventing friction as the heart beats.
If the pericardium becomes Inflamed (pericarditis), excess pericardia! fluid can be quickly generated in response to the inflammation. Pericarditis can result from a bacterial or viral infection, rheumatoid arthritis, tumors, destruction of the heart muscle in a heart attack, among other causes.
Heart surgery or trauma to the heart, such as a stab wound, can cause a rapid buildup of blood in the pericardia! space. The buildup of excess blood or fluid in the pericardia! space compresses the heart. This can affect the heart's abiily to relax and fill with blood between heartbeats. Ifthe heart cannot adequately
Fig.
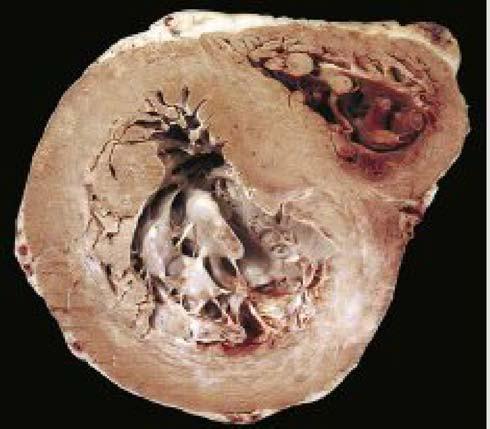
Fig. 1.2 of 1h& heart. This pho!Dgraph shows a living human heart p111pered for transplan1al!on Into a paUent. NoiB liB slza llllaUveiD 1he hands that Rill hading 1t. (From PaiiDn KT, Thlbolil&u GA: Anatomy& physiology. &d 9, St. Louis. 2016, Mosby.)
Anlartor branch of left coronary artery Greal canlac vein
Obtuee mergln
Fig. 1.4 Th& ant:&r1or surface of the haart. (From Drake R, Vogl AW, Mitchell AWM: Gray's anatomy frJr stJJd6nts, &d 3, Naw York, 2015, Churchill L.Mrgstona.)
Chapter 1 Anatomy and Physiology
fill with blood, the amount of blood the ventricles can pump out to the body output) will be decreased. As a result, the amount of blood returning to the heart is also decreased. These changes can result in a life-threatening called C8ldiac temponade. The amount of blood or fluid in the pericardia! space needed to impair the heart's ability to fill depends on the rate at which the buildup of blood or fluid occurs and the ability of the pericardium to stretch and accommodate the increased volume of fluid.
The rapid buildup of as little as 100 to 150 ml of fluid or blood can be enough to result in signs and symptoms of
shock. Conversely, 1000 mL of fluid may build up over a longer period without any significant effect on the heart's ability to fill. This is because the pericardium accommodates the increased fluid by stretching over time.
The symptoms of cardiac tamponade can be relieved by removing the excess fluid from the pericardia! sac. Pericardiocentesis is a procedure in which a needle is inserted into the pericardia! space and the excess fluid is sucked out (aspirated) through the needle. If scarring is the cause of the tamponade, surgery may be necessary to remove the affected area of the pericardium.
Right
Rbrous ventricle pericardium
Postertor {cut;)
lnt8rventrlcu lar art8ly and vein
Right
Inferior vena cava
Left verrtricla
Coronary atrium sulcus
Fig. 1.15 The Inferior surface ot the heart The part ot the fibrous urn has been removed v.tlh the dlapluagm. (From Gosling JA: Human anaJDmy: color atlas and text. ad 4, L..ordcn, 2002, Mosby.)
Laft Left oaphalil: Aortic vagus vein arch narve
Lung roots Left phrenic nerve
Cenlral tendon of diaphragm
Fig. 1 .& The fibrous pericanium and phrenic nerves revealed after reiTlCJ\Iill of the lungs. {From Gosling J&.: Human anafDmy: color afias and text. ed 4, Lllndon, 2002, Mosby.)
Left and llgtrt phrenic Alcendng aorta
Pulmonary trunk
Fibrous pertcardium (cut)
V-.1
MI'OUS pertcardium
Fig. 1.7 The fbrous pericardium has been opened to expose the visceral pericardium lhe anterior surface of the heart. (From Gosling JA: HumaiJ anatomy: color atlas and tert; eel 4, London, 2002, Mosby.)
STRUCTURE OF THE HEART
Layers of the Heart Wall
[Oblactlve 4]
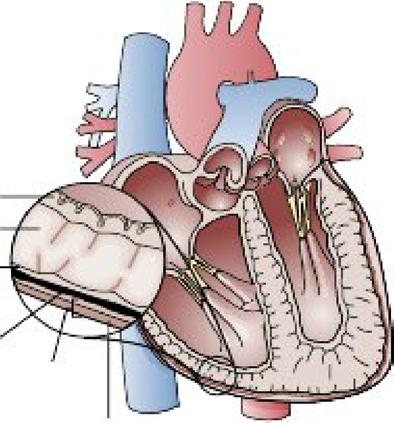
lhe walls of the heart are made up of three tissue layers: the endocardium, myocardium, and epicardium (Fig. 1.8 and Table 1.1). The heart's innennost layer, the endocardium, is made up of a thin, smooth layer of epithelium and connective tissue and Unes the heart's inner chambers, valves, chordae tendineae (tendinous cords), and papillary muscles. The terminal components of the heart's specialized conduction system can be found within this layer (Anderson & Roden. 2010). The endocardium is continuous with the innennost layer ofthe arteries, veins, and capillaries ofthe body, thereby creating a continuous, closed circulatory system.
1he .myocarclium (middle layer) is a thick. muscular layer that consists of cardiac muscle fibers (cells) responsible for the pumping action ofthe heart The myocardium makes up about 30% ofthe total left. ventrkular mass (Anderson &Roden, 2010). lhe innermost halfofthe myocardium is called the subendocar1&1 area. The outermost halfis called the subepicardial area. 1he muscle fibers of the myocardium are separated by connective tissues that have a rich supply ofcapillaries and nerve fibers.
Did You Know?
VIsceral pericardium (epicardium)
layer
Flf. 1.8 The parlcardlal sac Is aJIIliOSIId af 1:\W layn separaiBd by a narrow ftuld-fllled Sjlllllll. The v1scaral part:anllum (aplcmdklm) Is attached dlractly 1D 1ha heart's surface, and the parlelal pertardlum fcnns the llJIEr layer af the sac. (from L, Blnlslk JL: PBthoplrys/rJ/o ad 5, 2013, Elakr.)
The thickness of a heart chamber is related to the amount of pressure or resistance that the muscle of the chamber must overcome to eject blood.
The heart's outennost layer is called the epicardium. The epicardium is continuous with the inner lining of the pericardium at the heart's apex. The epicardium contains blood capillaries, lymph capillaries, nerve fibers, and fat. 1he main coronary arteries lie on the epicardial surface of the heart.
Myocardium
Perlcardlal apace
Abrous
lrJ:ll¥81 Layers of the Heart Wall
Heart Layer
Description
Epicardium
Myocardium
Endocardium
• External layer of 1he heart
• Coronary arteries, blood capillaries, lymph capillaries, nerve fibers, and fat are found in this layer
• Middle and thickest layer of the heart
• Muscular component of the heart; responsible for the heart's pumping action
• Innermost layer of the heart
• Lines heart's inner chambers, valves, chordae tendineae, and papillary muscles
• Continuous with the innermost layer of arteries, veins. and capillaries of the body
IThey feed this area first before entering the myocardium and supplying the heart's inner layers with oxygenated blood. Ischemia is a decreased supply of oxygenated blood to a body part or organ. The heart's subendocardial area is at the greatest risk ofischemia because this area has a high demand for oxygen and it is fed by the most distal branches of the coronary arteries.
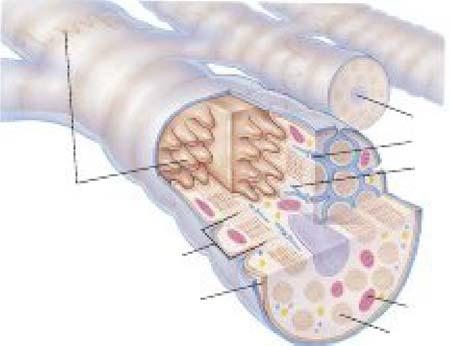
CARDIAC MUSCLE
Cardiac muscle fibers make up the walls of the heart. These fibers have striations, or stripes, similar to that of skeletal muscle. Each muscle fiber is made up of many muscle cells (Fig. 1.9). Each muscle cell is enclosed in a membrane called a sarcolemma. Within each cell (as with all cells) are mitocho.odria, the energy-producing parts of a cell, and hundreds of long, tube-like structures called myoflbrlls. Myofibrils are made up of many merea, the basic protein units responsible for contraction. The process of contraction requires adenosine triphosphate (ATP) for energy. The mitochondria that are interspersed between the myofibrils are important sites of ATP production.
The sarcolemma has holes in it that lead into tubes called T (transverse) tubules. T tubules are extensions of the cell membrane. Another system of tubules, the sarcoplasmic: reticulum (SR), stores calcium. Muscle cells need calcium in order to contract. Calcium is moved from the sarcoplasm of the muscle cell into the SR by means of "'pumps" in the SR.
There are certain places in the cell membrane where sodium (Na+), potassium (K+), and calcium (Ca++) can pass. These openings are called pores or channels. There are specific channels for sodium (sodium channels},
Fig. 1.8 cardiac muscle filar. lklllke ather types a! muscle fibers, 1he cardiac muscle flbar Is t)Pically branchoo and foiTI'IS junc1!oos, called lntaroalllled with adjacent cardiac muscle fibers. (From PatiDn KT, Thltxxfeau GA: Anthony's IIJXtbook of 8fi/J/Dmy & phys/okJgy, ad 20, St Louis, 2013,
potassium (potassium channels), and calcium (calcium channels). When the muscle is relaxed, the calcium channels are closed. As a result, calcium cannot pass through the membrane of the SR. This results in a high concentration of calcium in the SR and a low concentration in the sarcoplasm, where the muscle cells (sarcomeres) are found. If the muscle cells do not have calcium available to them, contraction is inhibited (the muscle stays relaxed). The force of cardiac muscle contraction depends largely on the concentration of calcium ions in the extracellular fluid.
0ECG Pear1
The heart consists of two syncytia: atrial and ventricular. The atrial syncytium consists of the walls of the right and left atria. The ventricular syncytium consists of the walls of the right and left ventricles. Normally, impulses can be conducted from the atrial syncytium into the ventricular syncytium only by means of the atrioventricular (AV) junction. The AV junction is a part of the heart's electrical system. This allows the atria to contract a short time before ventricular contraction.
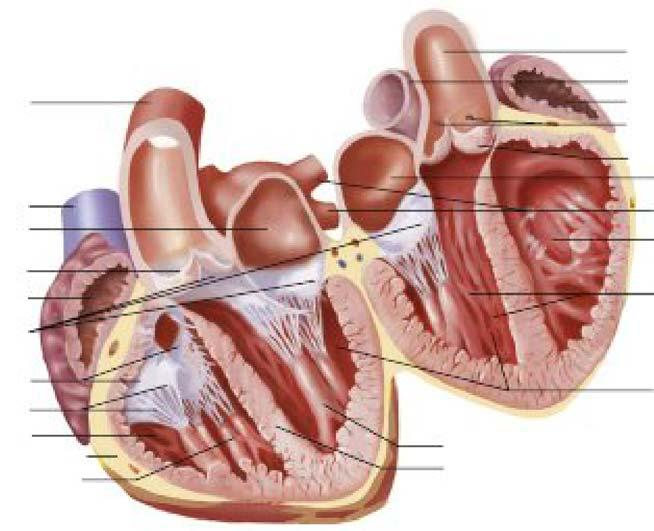
Heart Chambers
The heart has four chambers, two atria and two ventricles. The outside surface of the heart has grooves called sulci. The coronary arteries and their major branches lie in these grooves. The coronary sulcus (groove) encircles the outside of the heart and separates the atria from the ventricles. It contains the coronary blood vessels and epicardial fat.
L--lrrtercalallld dlskB
,....,_-- Pulmonary tnlnk Right atrium to coronary arteries
Aortic (SL) valve Laftatrlum
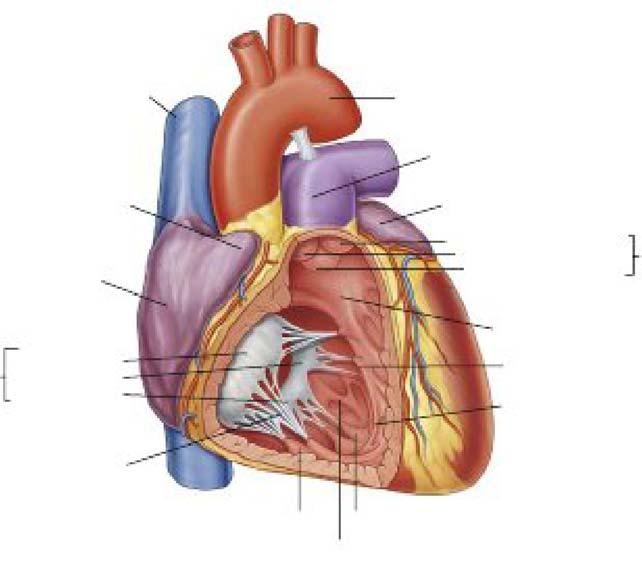
F1g. 1.10 lntartor of the heart. This Illustration shows the heart as It would appear If It were a.Jt along a lronllll plane and opened Ilks a book. The fnlnt portion of the heart lies ID 1hll reader's the back portion of the heart lias ID the reader's Iaft. ThB four chambers Ill 1hll heart-two a and two easily seen. st.. semilunar. [From Patton KT, Thllodeau GA: Anatomy & physiology, ad 9, St. llluls, 2016, Mosby.)
ATRIA
[Obiactive 5]
The two upper chambers of the heart are the right and left atria (singular, atrium) (Fig. 1.10). An earlike flap called an auricle (meaning "little ear·) protrudes from each atrium.
The purpose of the atria is to receive blood. The right atrium receives blood low in oxygen from the superior vena cava (which carries blood from the head and upper extremities), the inferior vena cava (which carries blood from the lower body), and the coronary sinus (which is the largest vein that drains the heart). The left atrium receives freshly oxygenated blood from the lungs via the right and left pulmonary veins.
1he four chambers of the heart vary in muscular wall thickness, reflecting the degree of pressure each chamber must generate to pump blood. For example, the atria encounter little resistance when pumping blood to the ventricles. As a result, the atria have a thin myocardial layer. The wall of the right atrium is about 2 mm thick. and the wall of the left atrium is about 3 m.m thick. Blood is pumped from the atria through an atrioventricular (AV) valve and into the ventricles. The valves ofthe heart are discussed later in this chapter.
Think of the atria as holding tanks or reservoirs for blood.
VENTRICLES
(Obiactive 5]
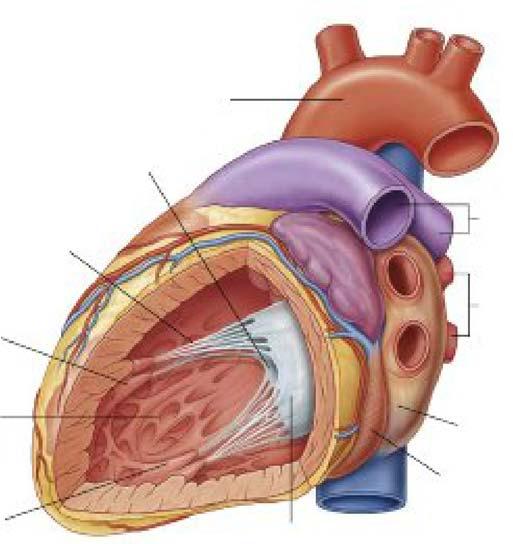
The heart's two lower chambers are the right and left ventricles. Their purpose is to pump blood. The right ventricle pumps blood to the lungs. The left ventricle pumps blood out to the body. Because the ventricles must pump blood either to the lungs (the right ventricle) or to the rest of the body (the left ventricle), the ventricles have a much thicker myocardial layer than the atria. Because the right ventricle moves blood only through the blood vessels ofthe lungs and then into the left atrium, it has one sixth of the muscle mass and one third ofthe wall thickness of the left ventricle, which must propel blood to most vessels of the body (Hutchison &: Rudakewich, 2009) (Fig. 1.11).
When the left ventricle contracts, it normally produces an impulse that can be felt at the apex of the heart (apical impulse). This occurs because as the left ventricle con· tracts, it rotates forward. In a normal heart, this causes the apex of the left ventricle to hit the chest wall. You may be able to sea the apical impulse in thin individuals. The apical impulse is also called the point of maximal impulse because it is the site where the left ventricular contraction is most strongly felt.
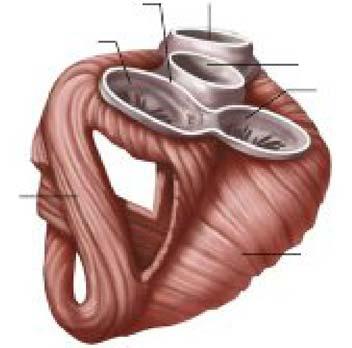
Heart Valves
The heart has a skeleton, which is made up of four rings of thick connective tissue. This tissue surrounds the bases of the pulmonary trunk, the aorta, and the heart valves. The inside of the rings provides secure attachments for the heart valves. The outside of the rings provides for the attachment of the cardiac muscle ofthe myocardium (Fig. 1.12). The heart's skeleton also helps form the partitions (septa) that separate the atria from the ventricles.
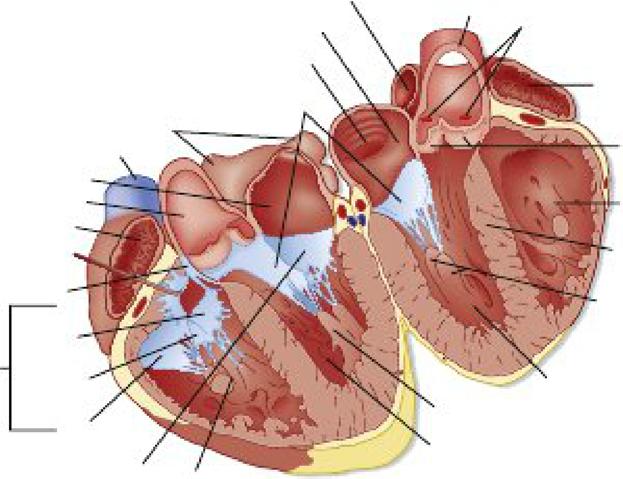
There are four one-way valves in the heart: two sets ofAV valves and two sets of &emilUIW' (SL) valves. The valves open and close in a specific sequence and assist in producing the pressure gradient needed between the chambers to ensure a smooth :flow of blood through the heart and prevent the bacldl.ow of blood.
ATRIOVENTRICULAR VALVES
[Oblectlves 6, 7]
Atrioventricular valves separate the atria from the ventricles. The two AV valves consist of tough. fibrous rings (annuli :6.brosi); :flaps (lea11.ets or cusps) of endocardium; chordae tendineae; and papillary muscles.
1he tricuspid valve is the AV valve that lies between the right atrium and right ventricle. It consists of three separate cusps or flaps (Fig. 1.13). It is larger in diameter and thinner than the mitral valve. The mitral valve, which is also called the bicuspid valve, has only two cusps and lies between the
Fig. 1.12 Skeleton of the heart. This IX)Stel1or view shows part of the venll1cular myooardlum with 1he heart valves 81111 attached. The rim of each heart valve Is supported by a fibrous structure, called the sk8/stonofth6 h6art, which encircles all four valves. AV. Atrlovenll1cular. (From PatiDn KT, Thibodeau GA: Anatmny & ed 9, St Louis, 201 6, Mosby.)
left atrium and left ventricle (Fig. 1.14). The mitral valve is so named because of its resemblance to a miter, which is a double-cusp bishop's hat, when open.
The AV valves open when a forward pressure gradient forces blood in a forward direction. They close when a ba.ck.ward pressure gradient pushes blood backward. The
Antarlor lntarvenb1cuJar Right vantrk:ular artery wall / Left Papillary Intel'" Trabeculae Marginal ventricular mUICia Y811lrtcular camaae arl8ry -11 saptum
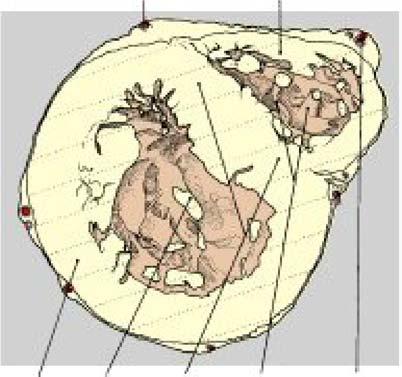
Fig. 1.11 Section through the heart shi7Mng 1he &Peal porUn of the left and venll1clas. (From Gosling JA: Human anatumy: oo1or atlas and t8Xt, ed 4, London, 2002, Mosby.)
Superior vena
Right
Trtcuspld G Anterior cusp Septal cusp
valve Posterior cusp
Septal papllluy miiiiCie
Septom•rgln•l trabecul•
Fig. 1.13 Internal view of 1he right venll1cle. (From Drake R, Vogl AW, Mitchell AWM: snatrHny frJr si1Jdenls. ed 3, New Yorll, 2015, Churchill Uvlngstone.)
MHral val¥8 antartor cuep
Pulmonary arteries
Pulmonary veins
Coronary sinus
valve poeterlor cuap
Fig. 1.14 Internal view of 1he left ventriCle. (From Drake R, Vcgl AW, MitChell AWM: anatomy for students, ed 3, New Ya'k, 2015, Chu I'Ch ill Livingstone.)
Chapter 1 Anatomy and Physiology
AV valves require almost no backflow to cause closure (Hall, 2016).
The flow of blood from the superior and inferior venae cavae into the atria is normally continuous. About 70% of this blood flows directly through the atria and into the ventricles before the atria contract; this is called passi'o'e filling. & the atria fill with blood, the pressure within the atrial chamber rises. This pressure forces the tricuspid and mitral valves open, and the ventricles begin to fill, gradually increasing the pressure within the ventricles. When the atria contract, an additionallO% to 30% of the returning blood is added to filling of the ventricles. This additional contribution of blood resulting from atrial contraction is called atrial kick. On the right side of the heart, blood low in oxygen empties into the right ventricle. On the left side of the heart, freshly oxygenated blood empties into the left ventricle. When the ventricles then contract (i.e., systole), the pressure within the ventricles rises sharply. The tricuspid and mitral valves completely close when the pressure within the ventricles exceeds that of the atria.
Chordae tendineae (tendlnoua cords) are thin strands of connective tissue. On one end, they are attached to the underside of the AV valves. On the other end, they are attached to small mounds of myocardium called papillary maades. Papillary muscles project inward from the lower portion ofthe ventricular walls. When the ventricles contract and relax, so do the papillary muscles. The papillary muscles adjust their tension on the chordae tendineae, preventing them from bulging too far into the atria. For example, when the right ventricle contracts, the papillary muscles of the right ventricle pull on the chordae tendineae. 1he chordae tendineae prevent the flaps of the tricuspid valve from bulging too far into the right atrium. 1hus, the chordae tendineae and papillary muscles serve as anchors. Because the chordae tendineae are thin and string-like, they are sometimes called "heart strings."
SEMILUNAR VALVES
[OIJiactlve B]
The pulmonic and aortic valves are SL valves. 1he SL valves prevent the bacldlow ofblood from the aorta and pulmonary arteries into the ventricles. 1he SL valves have three cusps shaped like half-moons. 1he openings ofthe SL valves are smaller than the openings ofthe AV valves, and the flaps ofthe SL valves are smaller and thicker than the AV valves. Unlike the AV valves, the SL valves are not attached to chordae tendineae. When the ventricles contract, the SL valves open, allowing blood to flow out of the ventricles. When the right ventricle contracts, blood low in oxygen flows through the pulmonic valve into the pulmonary trunk. which divides into the right and left pulmonary arteries. When the left ventricle contracts, freshly oxygenated blood flows through the aortic valve into the aorta and out to the body (Fig. 1.15). The SL valves close as ventricular contraction
ends and the pressure in the pulmonary artery and aorta exceeds that of the ventricles.
Improper valve function can hamper blood flow through the heart. Valvular heart disease is the term used to describe a malfunctioning heart valve. Types of valvular heart disease include the following:
• vaJvular prolapse. If a valve flap inverts, it is said to have prolapsed. Prolapse can occur if one valve flap is larger than the other. It can also occur if the chordae tendineae stretch markedly or rupture.
• vaJvutar regurgitation. Blood can flow backward, or regurgitate, if one or more of the heart's valves does not close properly. Valvular regurgitation Is also known as valvular incompetence or valvular insufficiency.
• Valvular stenosis. If a valve narrows, stiffens, or thickens, it is said to be stenosed. The heart must work harder to pump blood through a stenosed valve. Papillary muscles receive their blood supply from the coronary arteries. If a papillary muscle ruptures because of an inadequate blood supply (as in myocardial infarction), the attached valve cusps will not completely close and may result in a murmur. If a papillary muscle in the left ventricle ruptures, the leaflets of the mitral valve may invert Q.e., prolapse). This may result in blood leaking from the left ventricle into the left atrium (e.g., regurgitation} during ventricular contraction. Blood flow to the body o.e., cardiac output) could decrease as a result.
HEART SOUNDS
Heart sounds occur because of vibrations in the tissues of the heart caused by the closing of the heart's valves. Vibrations are created as blood flow is suddenly increased or slowed with the contraction and relaxation of the heart chambers and with the opening and closing of the valves.
Normal heart sounds are called Sl and S2. 1he first heart sound ("lubb,.) occurs during ventricular contraction when the tricuspid and mitral (AV) valves are closing. The second heart sound ("dupp) occurs during ventricular relaxation as the pulmonic and aortic (SL) valves close. A third heart sound is produced by ventricular filling. In those younger than 40 years ofage, the left ventricle normally permits rapid filling. The more rapid the ventricular filling, the greater the likelihood of hearing a third heart sound. A third heart sound (S3) heard in people older than 40 years ofage is considered abnormal An abnormal third heart sound is frequently associated with heart failure. An Sl-S2-S3 sequence is called a ventricular gallop or gallop rhythm. It sounds like "Kentucky"-Ken (Sl) -tuck (S2) -y (S3). The location of the
Superior vena
Left Aorta
Tricuspid valve
Mitral valv&posterior cusp
Right ventricle
Aortic valve cusps
Right venlr1cle lntervemrtcular septum
Fig. 1.1& Drawing of a heart split perpendicular to the interventriCular septum to illustrate the anatomic relationships of the leaflets of the atroventricular and aortiC valveS. (From Koeppen BM, Stanton BA: Beme & LevyJJ/1YSiOlOgY. ed 6, St. L.Duis, 2010, Mosby.)
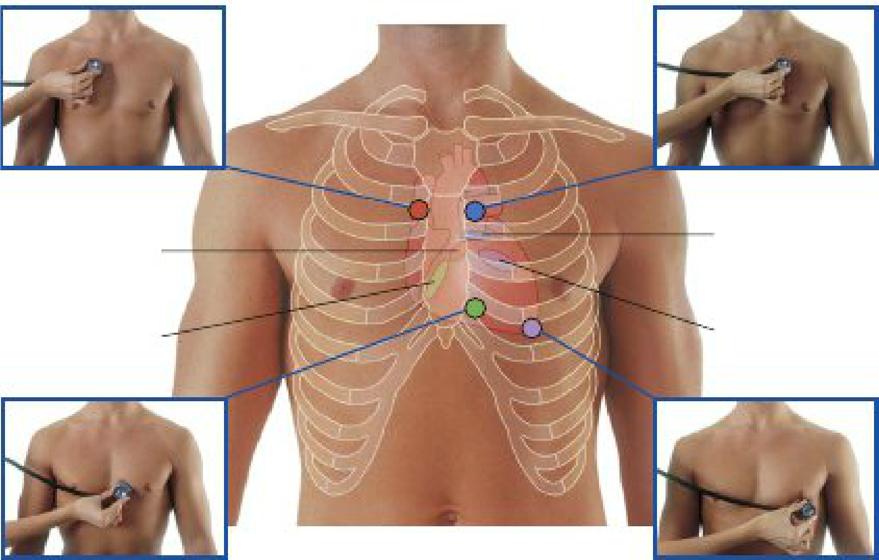
heart's AV and SL valves for auscultation is shown in Fig. 1.16. A summary ofthe heart's valves and auscultation points for heart sounds appears in Table 1.2
In people younger than 40 years of age, the left ventricle normally permits rapid filling. The more rapid the ventricular filling, the greater the likelihood of hearing a third heart sound. A third heart sound (S3) heard in those older than 40 years of age is considered abnormal. An abnormal third heart sound is frequently associated with heart failure. An S 1-32-33 sequence Is called a ventricular gallop or gallop rhythm. It sounds like Ken (S1) -tuck (S2) -y (S3).
Turbulent blood flow within the cardiac chambers and vessels can produce heart murmurs. An inflamed pericardium can produce a peric8rdial friction rub, which sounds like rough sandpaper.
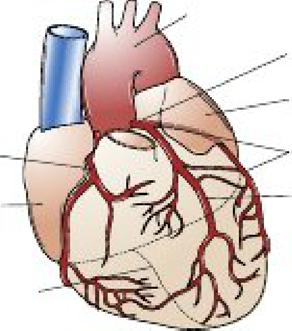
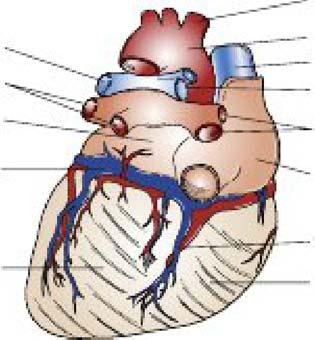
The Heart's Blood Supply
lhe coronary circulation consists of coronary arteries and veins. The right and left coronary arteries encircle the myocardium like a crown. or corona.
CORONARY ARTERIES
[Oblectlve 8]
lhe main coronary arteries lie on the outer (epicardial) surface ofthe heart. Coronary arteries that run on the surface of
the heart are called epicardial coronary arteries. They branch into progressively smaller vessels, eventually becoming arterioles, and then capillaries. Thus, the epicardium has a rich blood supply to draw from. Branches of the main coronary arteries penetrate into the heart's muscle mass and supply the subendocardium with blood. lhe diameter of these "feeder branches" (i.e., collateral circulation) is much narrower. The tissues supplied by these branches get enough blood and oxygen to survive, but they do not have much extra blood flow.
lhe work of the heart is important To ensure that it has an adequate blood supply, the heart makes sure to provide itself with a fresh supply of oxygenated blood before supplying the rest ofthe body. This freshly oxygenated blood is supplied mainly by the branches of two vessels: the right and left coronary arteries.
lhe right and left coronary arteries are the very first branches offthe base ofthe aorta. The openings to these vessels lie just beyond the cusps of the aortic SL valve. When the left ventricle contracts (systole), the force of the pressure within the left ventricle pushes blood into the arteries that branch from the aorta. 'Ihis causes the arteries to fill However, the heart's blood (ie., the coronary arteries) are compressed during ventricular contraction, reducing blood fl.ow to the tissues of the heart. Thus, the coronary arteries fill when the aortic valve is closed and the left ventricle is relaxed (i.e., diastole).
lhe three major epicardial coronary arteries include the left anterior descending (LAD) artery, circumflex (Cx) artery, and right coronary artery (RCA). A person is said to have coronary
Pulmonary valve
Auscultation position for tr1cuspld valve
if;1:Jii Q
AuscultaUon position for mitral valve
Fig. 1.18 An!Brlor view ot 1he chest r.owlng the heart, the looatlon of the heart's valves, and where to listen to heart sounds. (From Drake R, Vogl AW, Mitchell AWM: Glay'unatomyfurstWents, ad 3, New York. 2015, Churchill LMngstone.)
Heart Valves and Auscultation Points
Yalve Name Yalve 1W»e IJicatlon
Tricuspid Atrioventricular
Mitral (bicuspid) Atrioventricular
Pulmonic (pulmonary) Semilunar
Aortic Semilunar
Separates the right atrium and right ventricle
Separates the left atrium and left ventricle
Between the right ventricle and pulmonary artery
Between the left ventricle and aorta
artery disease (CAD) if there is more than 5096 diameter narrowing (i.e., stenosis) in one or more ofthese vessels.
(ill CLINICAL CORRELAT10NS
Because a heart attack, which is also called a myocardial Infarction, Is usually caused by a blocked coronary artery, it is worthwhile to become familiar with the arteries that supply the heart. When myocardial ischemia or infarction is suspected, an understanding of coronary artery anatomy and the areas of the heart that each vessel supplies helps you predict which coronary artery is blocked and anticipate problems associated with blockage of that vessel.
Auscultation Point
Just to the left of the lower part of the sternum near the fiHh intercostal space
Heart apex in the left fifth intercostal space at the midclavicular line
Left second intercostal space close to the sternum
Right second intercostal space close to the sternum
Right Coronary Artary
The RCA orlginates from the right side of the aorta (Fig. 1.17). It travels along the groove between the right atrium and right ventricle. A branch of the RCA supplies the following structures:
• Right atrium
• Right ventricle
• Inferior surface of the left ventricle in about 85% of individuals
• Posterior surface of the left ventricle in 85%
• Sinoatrial (SA) node in about 60%
• AV bundle in 8596 to 90%
Poalllllar diHicendng
nncn of riGht
c:oranary artery
Left Wiell appendage
Ci-'lex lnncto of laft main c;orvnuy ar1Bry
Luft enterlor d-ndlng lnnch of Ifill GOIIlllllry artery