https://ebookmass.com/product/breast-cancer-and-gynecologiccancer-rehabilitation-1st-edition-adrian-cristian-md-editor/
Instant digital products (PDF, ePub, MOBI) ready for you
Download now and discover formats that fit your needs...
Breast Cancer Sourcebook, 6th Edition Williams
https://ebookmass.com/product/breast-cancer-sourcebook-6th-editionwilliams/
ebookmass.com
Cancer Rehabilitation: Principles and Practice 1st Edition, (Ebook PDF)
https://ebookmass.com/product/cancer-rehabilitation-principles-andpractice-1st-edition-ebook-pdf/
ebookmass.com
Breast Cancer Sourcebook: Health Reference Series 6th Edition Angela Williams
https://ebookmass.com/product/breast-cancer-sourcebook-healthreference-series-6th-edition-angela-williams/ ebookmass.com
Dane Kate Oliver
https://ebookmass.com/product/dane-kate-oliver/
ebookmass.com
https://ebookmass.com/product/marketing-management-indian-casesprachi-gupta/
ebookmass.com
Eyes of the Void (Final Architecture 2) 1st Edition Adrian Tchaikovsky
https://ebookmass.com/product/eyes-of-the-void-finalarchitecture-2-1st-edition-adrian-tchaikovsky-2/
ebookmass.com
Works of John Dryden. Volume 10 Plays: The Tempest. Tyrannick Love. An Evening’s Love Maximillian E. Novak (Editor)
https://ebookmass.com/product/works-of-john-dryden-volume-10-playsthe-tempest-tyrannick-love-an-evenings-love-maximillian-e-novakeditor/
ebookmass.com
Sports Marketing: A Strategic Perspective, 5th edition 5th Edition, (Ebook PDF)
https://ebookmass.com/product/sports-marketing-a-strategicperspective-5th-edition-5th-edition-ebook-pdf/
ebookmass.com
Imaging Anatomy Brain and Spine Anne G. Osborn
https://ebookmass.com/product/imaging-anatomy-brain-and-spine-anne-gosborn/
ebookmass.com
Governing California in the Twenty-First Century (Seventh Edition)
https://ebookmass.com/product/governing-california-in-the-twentyfirst-century-seventh-edition/
ebookmass.com
BreastCancer andGynecologic Cancer Rehabilitation
EDITEDBY
ADRIANCRISTIANMDMHCMFAAPMR
Chief,CancerRehabilitation,MiamiCancerInstitute,Miami,FL,UnitedStates
Professor,FloridaInternationalUniversity,HerbertWertheimCollegeofMedicine, Miami,FL,UnitedStates
BreastCancer andGynecologic Cancer Rehabilitation
Elsevier
Radarweg29,POBox211,1000AEAmsterdam,Netherlands TheBoulevard,LangfordLane,Kidlington,OxfordOX51GB,UnitedKingdom 50HampshireStreet,5thFloor,Cambridge,MA02139,UnitedStates
Copyright©2021ElsevierInc.Allrightsreserved.
Nopartofthispublicationmaybereproducedortransmittedinanyformorbyanymeans,electronicormechanical,including photocopying,recording,oranyinformationstorageandretrievalsystem,withoutpermissioninwritingfromthepublisher.Detailson howtoseekpermission,furtherinformationaboutthePublisher’spermissionspoliciesandourarrangementswithorganizationssuch astheCopyrightClearanceCenterandtheCopyrightLicensingAgency,canbefoundatourwebsite: www.elsevier.com/permissions
ThisbookandtheindividualcontributionscontainedinitareprotectedundercopyrightbythePublisher(otherthanasmaybenoted herein).
Notices
Knowledgeandbestpracticeinthisfieldareconstantlychanging.Asnewresearchandexperiencebroadenourunderstanding, changesinresearchmethods,professionalpractices,ormedicaltreatmentmaybecomenecessary.
Practitionersandresearchersmustalwaysrelyontheirownexperienceandknowledgeinevaluatingandusinganyinformation, methods,compounds,orexperimentsdescribedherein.Inusingsuchinformationormethodstheyshouldbemindfuloftheirown safetyandthesafetyofothers,includingpartiesforwhomtheyhaveaprofessionalresponsibility.
Tothefullestextentofthelaw,neitherthePublishernortheauthors,contributors,oreditors,assumeanyliabilityforanyinjuryand/or damagetopersonsorpropertyasamatterofproductsliability,negligenceorotherwise,orfromanyuseoroperationofanymethods, products,instructions,orideascontainedinthematerialherein.
BritishLibraryCataloguing-in-PublicationData
AcataloguerecordforthisbookisavailablefromtheBritishLibrary
LibraryofCongressCataloging-in-PublicationData AcatalogrecordforthisbookisavailablefromtheLibraryofCongress
ISBN:978-0-323-72166-0
ForInformationonallElsevierpublications visitourwebsiteat https://www.elsevier.com/books-and-journals
Publisher: CathleenSether
AcquisitionsEditor: HumayraRahman
EditorialProjectManager: MeganAshdown
ProductionProjectManager: KiruthikaGovindaraju
CoverDesigner: AlanStudholme
TypesetbyMPSLimited,Chennai,India
LISTOFCONTRIBUTORS xiii
PREFACE xvii
SECTIONI
1. CascadeofDisabilityinBreast andGynecologicCancer 1
AdrianCristian,MD,MHCM
Introduction 1
AssessmentofBreastandGynecologicCancer PatientwithaFocusonPhysicalImpairments andLossofFunction 2
CascadeofDisability 4
ReturntoWorkinBreastandGynecologic Cancers 5
RehabilitationofBreastandGynecologicCancer Patients AHolisticApproach 6
Conclusion 7
References 7
2. PracticeImplementation,Clinical Assessment,andOutcomes Measurement 9
NicoleL.Stout,DPT,CLT-LANA,FAPTA, ShanaE.Harrington,PT,PhDandMerylJ. Alappattu,PT,PhD
Introduction 9
ProspectiveSurveillanceModel 9
Breast 10
PelvicFloor 11
CommonCancerTreatment Related Impairments 12
PracticeImplementation 12
Summary 15
KeyResearchQuestions 15
References 15
3. ExerciseWhileLivingWithBreast andGynecologicalCancers 19
CarlyRothman,DOandSusanMaltser,DO
Introduction 19
TypesofExercise 19
ExercisePositivelyInfluencesBreastand GynecologicalCancerPrevention,Treatment, SurvivalandRecurrence 19
ExerciseGuidelines 22
GeneralSafetyConsiderations 23
BarrierstoExercise/Adherence 24
MedicalandSurgicalComplicationsofBreast Cancer:ExerciseBenefits, SafetyConsiderations,andBarriers 24
BoneHealth 27
Osteopenia/Osteoporosis 28
ArmandShoulderDysfunction 30
AxillaryWebSyndrome 32
Conclusion 33
PatientResources 34
References 34
4. Cancer-RelatedFatigueinBreast andGynecologicCancers 39
JasmineZheng,MDandBettyChernack,MD
Introduction 39 Definitions 39 Mechanisms 40 RiskFactors 41 Screening 41 ApproachtoPatientWithCancer-Related Fatigue 42
PhysicalExam 42 LaboratoryStudies 43
OtherDiagnosticTesting 43 Treatment 43
Nonpharmacologic 44
Exercise 44
Nutrition 44
ComplementaryandAlternative Medicine 45
Pharmacologic 45
Cancer-RelatedFatigueand Prehabilitation 46
Cancer-RelatedFatigueandHospice/Endof Life 46
ProposedMultidimensionalApproach 47
Conclusion 47
References 47
5. NutritionalRehabilitationof BreastandGynecologicCancer Patients 51
KarlaOtero,MS,RDN,LDN,CSO,CDE, ClaudiaFerri,MS,RD,CSO,LDNandCarlaAraya, MPH,RDN,LDN
NutritionScreeningandAssessmentinBreastand GynecologicalCancers 51
EstimatingEnergyNeedsforCancerPatients 52
ObesityandCancerRisk 52
DietaryInterventionsforOverweightandObese CancerPatientandSurvivors 52
DietComposition 53
CounselingStrategies 53
TheRoleofBariatricSurgeryinWeight ManagementforBreastandGynecological Cancers 54
DietandInflammation 55
HowCanWeFightInflammationThrough Food? 55
MediterraneanDietAsanAntiinflammatoryDiet 57
DietaryRecommendationsforCancerPatientsand Survivors 57
TheLinkBetweenEthanolandBreastCancer 58
Conclusion 58
References 59
6. AComprehensiveApproachto PsychosocialDistressandAnxietyin
BreastandGynecologicalCancers 63
LynnKim,OTD,OTR/L,VinitaKhanna,LCSW,MPH, ACHP-SW,OSW-C,VanessaYanez,MOT, OTR/LandSherryHite,MOT,OTR/L
Background 63
DefinitionofDistressandAnxiety 63
DistressandAnxietyintheBreastandGynecological CancerPopulations 64
TheImportanceofPsychosocialScreeningand Intervention 64
PsychosocialNeedsintheBreastandGynecological CancerPopulations 64
ScreeningforDistressandAnxiety 66 ImplementationofPsychosocialScreeningof DistressandAnxiety 68
InterventionsforManagementofDistressand Anxiety 68
OvercomingChallenges 72
Conclusion 73
References 73
7. PrehabilitationinBreastand GynecologicOncology 75
JuliaM.Reilly,MD,AlexandraI.Gundersen,MDand SashaE.Knowlton,MD
Introduction 75
GoalsofPrehabilitation 75
BreastCancerPrehabilitation 75
GynecologicCancerPrehabilitation 77
RecommendationsforPrehabilitationandFuture
Directions 79
References 79
SECTIONII
8. SystemicTherapyfortheTreatmentof BreastCancer 81
AnaCristinaSandovalLeon,MDandAngelique EllerbeeRichardson,MD,PhD
Introduction 81
ClinicalPresentationandDiagnosticWorkup 81
NonmetastaticVersusMetastaticBreastCancer 81
SystemicTreatmentbyReceptorStatus 82
HormoneReceptor PositiveBreastCancer 82
HumanEpidermalGrowthFactorReceptor 2 PositiveBreastCancer 84
Triple-NegativeBreastCancer 85
Conclusion 86
PatientResources 86
References 86
9. PrinciplesofRadiationTherapyin BreastCancer 89
Maria-AmeliaRodrigues,MD
Introduction 89
RadiationTherapyintheTreatmentofBreast Cancer 89
TypesofRadiationTherapyforBreastCancer 90
PartialBreastIrradiation 90
WholeBreastIrradiation 91
BreastorChestWallIrradiation,IncludingRegional LymphNodes 93
ThePatientExperienceintheRadiationOncology Department 93
RadiationTherapyAdverseEffects 94
RadiationEffectsontheSkinandBreast 94
MyositisandShoulderDysfunction 95
ImplicationsforRehabilitationMedicine 96
Conclusion 96
References 96
FurtherReading 97
10. BreastCancerSurgery 99
JaneMendez,MD
Introduction 99
LifestyleandDietaryFactors 100
RoleofSurgeryintheTreatmentofBreast Cancer 101
DescriptionofHowtheSurgeriesAre Performed 103
Conclusion 106
PatientResources 106
References 106
11. ReconstructiveSurgeryand PostoperativeCareforBreast Cancer 109
MiguelA.MedinaIII,MD,AustinJ.Pourmoussa,Erin M.Wolfe,BSandHarryM.Salinas,MD
Introduction 109
Anatomy 109
PreoperativeEvaluationandPatientAssessment 111
Procedures 111
PostoperativeCareandPatientEducation 114
Conclusion 115
PatientResources 116
References 116
FurtherReading 118
12. RehabilitationoftheCancerPatient WithSkeletalMetastasis 119
TheresaPazionis,MD,MA,FRCSC,RachelThomas andMirzaBaig,BS
Introduction 119 Background 119
OrthopedicOncologyProcedures 120
RecommendationsforPhysicalMedicineand Rehabilitation 121
Conclusion 124
References 124
13. ShoulderDysfunctioninBreast Cancer 127
DianaMolinares,MDandAdrianCristian,MD, MHCM
Introduction 127
AnatomyandBiomechanics 127
PatientAssessment 128
Tumor-RelatedImpairments 131
Surgical-RelatedImpairments 131
RadiationImpairments 133
Imaging 134
ShoulderRehabilitation 136
Conclusion 137
References 137
14. RoleofInterventionalPain ManagementinBreastCancer 141
AshishKhanna,MD
Introduction 141
PostmastectomyPainSyndrome 141
RadiationFibrosisSyndrome 141
PostreconstructionPain 144
InterventionalPainTechniques 145
Conclusion 147
References 147
15. AromataseInhibitorMusculoskeletal Syndrome 149
MonicaGibilisco,DOandJonasM.Sokolof,DO
Introduction 149
EtiologyandPathogenesisofAromataseInhibitor MusculoskeletalSyndrome 149
Conclusion 152
References 152
SECTIONIII
16. SystemicTherapyforGynecologic Malignancies 155
JohnP.Diaz,MD,FACOG
Introduction 155
OvarianCancer 155
RelapsedDisease 156
PlatinumResistance 157
BRCAMutation 157
UterineCancer 157
CervicalCancer 158
VaginalandVulvarCancer 158
UterineSarcomas 158
Conclusion 158
References 159
17. PrinciplesofRadiationTherapyin GynecologicCancer 161
AllieGarcia-Serra,MD
GeneralOverviewofRadiationTherapy 161
CancerSurveillance 168
References 169
18. SurgicalGynecologicOncology 171
NicholasC.Lambrou,MDandAngelAmadeo,BS
Introduction 171
Anatomy 171
EndometrialCarcinoma 172
Conclusion 185
References 185
19. PelvicFloorDysfunctionin GynecologicCancer 189
LouiseV.Gleason,MSPT,PRPC
Introduction 189
PelvicFloorEvaluation:AssessingSystems 190
Rehabilitation:TreatingPelvicFloor Dysfunction 199
CommunicatingTherapyGoals 207
Summary 207
References 208
SECTIONIV
20. Cancer-RelatedCognitiveImpairment: Diagnosis,Pathogenesis,and Management 211
AileenM.Moreno,LCSW,RichardA.Hamilton,PhD andM.BeatrizCurrier,MD
Introduction 211
StructuralandFunctionalNeuroanatomical CorrelatesofCancer-RelatedCognitive Impairment 213
RiskFactorsandPathogenesisofCancer-Related CognitiveImpairmentinPatientsWithBreastor GynecologicalCancer 213
AssessmentoftheCancerPatientWithCognitive Impairment 216
TreatmentofCognitiveImpairmentinBreastand GynecologicalCancerPatients 217
AreasofFutureResearch 220
Conclusion 220
PatientResources 220
References 220
FurtherReading 222
21. LymphedemainBreastand GynecologicOncology 225
MaryCrosswellPTDPTCLTandAdrianCristian, MD,MHCM
Introduction 225
AnatomyoftheLymphaticSystem 226
PathophysiologyofLymphedema 227
RiskFactors 227
TheAssessmentofthePatientWith Lymphedema 228
StagingandDiagnosis 229
Treatment 235
SurgicalTreatmentforLymphedema 243
Education 243
RiskReductionBehaviors 244
Conclusion 245
References 246
22. PeripheralNervousSystem InvolvementinBreastandGynecologic Cancers 253
FranchescaKönig,MDandChristianM.Custodio,MD
Introduction 253
DirectNeuromuscularEffects 253
ParaneoplasticSyndromes 255
TreatmentRelated 256
IndirectNerveInjuries 259
Conclusion 260
References 260
23. InpatientRehabilitationforBreastand GynecologicCancerPatients 263
TerrenceMacArthurPugh,MD,VishwaS.Raj,MD andCharlesMitchell,DO
Introduction 263
Epidemiology 263
ReasonforAdmissiontoAcuteInpatient Rehabilitation 263
InpatientRehabilitationManagement 265
OtherCommonImpairments 267
TherapeuticInterventions 268
Conclusion 271
References 271
24. PalliativeCareandSymptom ManagementinBreastand GynecologicalCancers 275
SuleykiMedina,MD
andMarianaKhawand-Azoulai,MD
ComprehensivePatientAssessment 276
PainManagement 277
GeneralGuidelinesforPharmacologicalPain Management 278
Nausea 280
Constipation 281
MalignantBowelObstruction 281
AnorexiaCachexiaSyndrome 282
DepressionandAnxiety 283
MedicalCannabis 284
SpiritualIssuesandExistentialDistress 284
AdvanceCarePlanningandEnd-of-Life 285
TheRoleofRehabilitationinthePalliativeCare
Setting 286
Conclusion 286
PatientResources 286
References 287
25. FertilityPreservationintheSettingof BreastandGynecologicCancersand CancerTreatment 289
ElinaMelik-Levine,ARNP andJohnP.Diaz,MD,FACOG
Introduction 289
HowDoesCancerTherapyAffectFertility? 290
SystemicTreatments:Chemotherapy,Targeted TherapyandImmunotherapy,Antihormonal Therapy 290
OptionsforFertilityPreservation 291
EndometrialCancer 291
CervicalCancer 292
OvarianCancer 293
SexualEducationDuringandPostcancer Treatment 294
Conclusion 295
References 295
26. OncologyMassageTherapyin BreastandGynecologic Cancers 297
KristenM.Galamaga,LMT andAdrianCristian,MD,MHCM
Introduction 297
History 297
ComplementaryVersusAlternativeTherapy 298
BenefitsofOncologyMassageTherapy 298
ContraindicationstoMassageTherapy 298
MassageTechniques 299
PatientAssessment 299
PrecautionsinOncologyMassageTherapy 299
MassageTreatmentSession 300
Conclusion 300
References 300
INDEX 303
ToEliane,mywifeandbestfriend,forherunwaveringlove, support,encouragement,andbeliefthatwehavethepower tomaketheworldabetterplace, Tomychildren,AlecandChloefortheirlove,support,and boundlessoptimism,
TomycolleaguesattheMiamiCancerInstitutefortheir dedicationtothecompassionatecareofourpatients, Tomypatients,fortheprivilegeofallowingmetobepartof theirlifeandforteachingmeaboutstrength,resilience,and dignityinthefaceofadversity.
ListofContributors
MerylJ.Alappattu,PT,PhD
DepartmentofPhysicalTherapy,Universityof Florida,Gainesville,FL,UnitedStates
AngelAmadeo,BS
BachelorofScience(BS),UniversityofCentral Florida,Orlando,FL,UnitedStates
CarlaAraya,MPH,RDN,LDN
ClinicalNutritionSpecialist,MiamiCancerInstitute, Miami,FL,UnitedStates
MirzaBaig,BS
HerbertWertheimCollegeofMedicineatFlorida InternationalUniversity,Miami,FL,UnitedStates
BettyChernack,MD
DepartmentofPhysicalMedicineandRehabilitation, UniversityofPennsylvania,Philadelphia,PA,United States
AdrianCristian,MD,MHCM
CancerRehabilitation,MiamiCancerInstitute, Miami,FL,UnitedStates;Professor,Departmentof TranslationalMedicineHerbertWertheimSchoolof Medicine,FloridaInternationalUniversity,Miami,FL, UnitedStates
MaryCrosswell,PTDPTCLT
SupervisorofRehabilitationServices,SouthMiami Hospital,BaptistHealthSouthFlorida,Miami,FL, UnitedStates
M.BeatrizCurrier,MD
MiamiCancerInstitute,CancerPatientSupport CenteratBaptistHealthSouthFlorida,Miami,FL, UnitedStates
ChristianM.Custodio,MD
MemorialSloanKetteringCancerCenter,NewYork, NY,UnitedStates;WeillCornellMedicine,NewYork, NY,UnitedStates
JohnP.Diaz,MD,FACOG
DirectorofMinimallyInvasiveGynecologicSurgery, LeadPhysicianResearchGynecologicOncology, DivisionofGynecologicOncology,MiamiCancer Institute,BaptistHealthSouthFlorida,Miami,FL, UnitedStates
ClaudiaFerri,MS,RD,CSO,LDN
BaptistHealthSouthFlorida,MiamiCancerInstitute, Miami,FL,UnitedStates
KristenM.Galamaga,LMT
MiamiCancerInstitute,Miami,FL,UnitedStates
AllieGarcia-Serra,MD
RadiationOncologist,InnovativeCancerInstitute, Miami,FL,UnitedStates
MonicaGibilisco,DO
NYITCollegeofOsteopathicMedicine
LouiseV.Gleason,MSPT,PRPC
PelvicHealth&ContinenceTestingDepartment, CenterforWomenandInfants:SouthMiami Hospital,Miami,FL,UnitedStates
AlexandraI.Gundersen,MD
HarvardMedicalSchool,Boston,MA,UnitedStates; DepartmentofPhysicalMedicineandRehabilitation, SpauldingRehabilitationHospital,Boston,MA, UnitedStates
RichardA.Hamilton,PhD
MiamiCancerInstitute,CancerPatientSupport CenteratBaptistHealthSouthFlorida,Miami,FL, UnitedStates
ShanaE.Harrington,PT,PhD
PhysicalTherapyProgram,UniversityofSouth Carolina,Columbia,SC,UnitedStates
SherryHite,MOT,OTR/L
DepartmentofRehabilitation,CityofHopeNational MedicalCenter,Duarte,CA,UnitedStates
AshishKhanna,MD
CancerRehabilitationMedicine,TheKesslerInstitute forRehabilitation,WestOrange,NJ,UnitedStates; DepartmentofPhysicalMedicine&Rehabilitation, RutgersNewJerseyMedicalSchool,WestOrange,NJ, UnitedStates
VinitaKhanna,LCSW,MPH,ACHP-SW,OSW-C DepartmentofClinicalSocialWork,USCNorris ComprehensiveCancerCenter,LosAngeles,CA, UnitedStates
MarianaKhawand-Azoulai,MD
Medicine/PalliativeCare;UniversityofMiami/Jackson HospiceandPalliativeMedicine;MedicalDirectorPalliativeMedicineServicesUhealth
LynnKim,OTD,OTR/L
DepartmentofRehabilitation,CityofHopeNational MedicalCenter,Duarte,CA,UnitedStates
SashaE.Knowlton,MD
AssistantDirectorofCancerRehabilitation,Instructor inPhysicalMedicineandRehabilitation,Harvard MedicalSchool,Boston,MA,UnitedStates
FranchescaKönig,MD
MemorialSloanKetteringCancerCenter,NewYork, NY,UnitedStates;WeillCornellMedicine,NewYork, NY,UnitedStates
NicholasC.Lambrou,MD
MiamiCancerInstitute,Miami,FL,UnitedStates; BaptistHealthSouthFlorida,SouthMiami,FL, UnitedStates
SusanMaltser,DO
DonaldandBarbaraZuckerSchoolofMedicineat Hofstra/Northwell,Manhasset,NY,UnitedStates; GlenCoveHospital,GlenCove,NY,UnitedStates
MiguelA.Medina,III,MD
PlasticandReconstructiveSurgery;Directorof MicrosurgeryMiamiCancerInstituteatBaptistHealth SouthFlorida,Miami,FL,UnitedStates
SuleykiMedina,MD
PalliativeMedicinePhysician,Symptom ManagementandPalliativeMedicine,Miami CancerInstitute,Baptis tHealthSouthFlorida, Miami,FL,UnitedStates
ElinaMelik-Levine,ARNP
MiamiCancerInstitute,BaptistHealthSouthFlorida, Miami,FL,UnitedStates
JaneMendez,MD
ChiefBreastSurgery,MiamiCancerInstitute,Baptist HealthSouthFlorida,FL,UnitedStates
CharlesMitchell,DO
DepartmentofPhysicalMedicineandRehabilitation, AtriumHealthCarolinasRehabilitation,Charlotte, NC,UnitedStates;DepartmentofSupportiveCare Oncology,LevineCancerInstitute,Charlotte,NC, UnitedStates;AtriumHealth,Charlotte,NC,United States
DianaMolinares,MD
CancerRehabilitationMedicineDirectorforSylvester CancerCenter,DepartmentofPhysicalMedicineand Rehabilitationm,UniversityofMiami-MillerSchoolof Medicine,Miami,FL,UnitedStates
AileenM.Moreno,LCSW
MiamiCancerInstitute,CancerPatientSupportCenter atBaptistHealthSouthFlorida,Miami,FL,UnitedStates
KarlaOtero,MS,RDN,LDN,CSO,CDE
SupervisorofClinicalNutritionCancerPatient SupportCenter,MiamiCancerInstitute,Miami, FL,UnitedStates
TheresaPazionis,MD,MA,FRCSC
AssistantProfessor,OrthopedicSurgeryandSports Medicine,LewisKatzSchoolofMedicineatTemple University,Philadelphia,PA,UnitedStates
AustinJ.Pourmoussa
MedicalStudentHerbertWertheimSchoolof MedicineFloridaInternationalUniversity,Miami,FL, UnitedStates
TerrenceMacArthurPugh,MD
DepartmentofPhysicalMedicineandRehabilitation, AtriumHealthCarolinasRehabilitation,Charlotte,
NC,UnitedStates;DepartmentofSupportiveCare Oncology,LevineCancerInstitute,Charlotte,NC, UnitedStates;AtriumHealth,Charlotte,NC,United States;UniversityofNorthCarolinaSchoolof Medicine,ChapelHill,NC,UnitedStates
VishwaS.Raj,MD
Vice-ChairforClinicalOperations,Departmentof PhysicalMedicineandRehabilitation,AtriumHealth CarolinasRehabilitation,Charlotte,NC,United States;Chief,SectionofRehabilitation,Departmentof SupportiveCareOncology,LevineCancerInstitute, Charlotte,NC,UnitedStates;AtriumHealth, Charlotte,NC,UnitedStates;MedicalDirector, DirectorofOncologyRehabilitation,Carolinas Rehabilitation,Charlotte,NC,UnitedStates
JuliaM.Reilly,MD
AttendingPhysiatrist,MemorialSloan-Kettering CancerCenter,NewYork,NY,UnitedStates
AngeliqueEllerbeeRichardson,MD,Phd UniversityofCaliforniainSanDiego,CA,United States
Maria-AmeliaRodrigues,MD
DepartmentofRadiationOncology,MiamiCancer Institute,BaptistHealthSouthFlorida,Florida,FL, UnitedStates
CarlyRothman,DO
DonaldandBarbaraZuckerSchoolofMedicineat Hofstra/Northwell,Manhasset,NY,UnitedStates
HarryM.Salinas,MD
PlasticandReconstructiveSurgery,MiamiCancer Institute,BaptistHealthSouthFlorida,Miami,FL, UnitedStates
AnaCristinaSandovalLeon,MD MedicalOncologist,MiamiCancerInstitute,Miami, FL,UnitedStates
JonasM.Sokolof,DO
ClinicalAssociateProfessorofRehabilitation MedicineNYUGrossmanSchoolofMedicineDirector ofOncologicalRehabilitationatNYU-LangoneHealth
NicoleL.Stout,DPT,CLT-LANA,FAPTA
WestVirginiaUniversityCancerInstitute, Morgantown,WV,UnitedStates
RachelThomas
MedicalStudentLewisKatzSchoolofMedicineat TempleUniversity,Philadelphia,PA,UnitedStates
ErinM.Wolfe,BS
MillerSchoolofMedicine,UniversityofMiami, Miami,FL,UnitedStates
VanessaYanez,MOT,OTR/L DepartmentofRehabilitation,CityofHopeNational MedicalCenter,Duarte,CA,UnitedStates
JasmineZheng,MD
DepartmentofPhysicalMedicineandRehabilitation, UniversityofPennsylvania,Philadelphia,PA,United States
Preface
Advancesinearlierdetectionandimprovedtreatment optionshaveledtoincreasedsurvivalratesforpersonsdiagnosedwithbreastandgynecologiccancer. Yet,inspiteoftheseincreasedsurvivalrates,people oftendevelopvariousphysicalandpsychological impairmentsthathaveanadverseimpactontheir leveloffunctioninperformingself-careaswellas engaginginwork,school,oravocationalactivities.
Rehabilitationmedicinehasavitalroleinminimizingimpairmentsandmaximizingthequalityof life.Tobesuccessful,itoftenrequiresacollaborative effortamongphysiatrists,medical,surgical,orthopedicandradiationoncologists,palliativecarephysicians,nutritionists,physicaltherapists,occupational therapists,psychologists,psychiatrists,socialworkers, massagetherapists,andadvancedcareproviders.
Thisbookismeanttoprovidethereaderwitha multidisciplinaryandholisticapproachtothecareof thepersonwithbreastcancerand/orgynecologic
cancer.Itisseparatedintotwobroadsectionsthat providecontentforeachofthesetypesofcancer.This includescancertreatmentusingmedical,surgical,and radiationtherapyinterventionsfollowedbycontent oncommonlyseenimpairmentsandtheirtreatment.
Iamextremelygratefultotheauthorsfortheir importantcontributiontothisbookandhelpinmakingitareality.Myhopeisthathealth-careproviders readingitwillhaveabetterappreciationofthecomplexitiesinvolvedinthecareofpeopleaffectedby thesetypesofcancersandsubsequentlyprovidecompassionateandeffectivecaretothem.
AdrianCristian CancerRehabilitation,MiamiCancerInstitute, Miami,FL,UnitedStates
CascadeofDisabilityinBreastand GynecologicCancer
ADRIANCRISTIAN,MD,MHCM
INTRODUCTION
AccordingtotheAmericanCancerSociety,asof January1,2019,therewere3,861,520womenliving withbreastcancer;807,860womenlivingwithuterinecancer;283,120womenlivingwithcervicalcancer;and249,320womenlivingwithovariancancer. The5-yearsurvivalratesare91%forbreastcancer, 65.8%forcervicalcancer,81.2%foruterine cancer,and47.6%forovariancancer.1 3 Aswomen aresurvivingbreastandgynecologiccancerslonger,it isperhapsnotsurprisingthattheprojectionforpeoplelivingwithbreastandgynecologiccancersistosee thesenumbersincrease.Theprojectionisthatby 2030therewillbe4,957,960livingwithbreastcancer; 1,023,290livingwithuterinecancer;297,580living withovariancancer;and288,710livingwithuterine cervixcancer.Womenarealsolivingsubstantiallylongerpostdiagnosisaswell.Forexample,19%of womenareliving20 1 yearssincediagnosedwith breastcancer,29%sincediagnosedwithovariancancer,49%sincediagnosedwithcervicalcancer,and 22%withuterinecancer.Thenumberofwomenlivingwithmetastaticbreastcancerisgreaterthan 150,000.Womenarealsodiagnosedwithbreastor gynecologiccancermoreoftenlaterinlife.Forexample,ageatprevalenceforwomendiagnosedwith breastcancerinthe65 84age-groupwas51%for breastcancer,47%forovariancancer,39%foruterine cancer,and56%foruterinecorpus.
Thesestatisticsillustratethatthereareasignificant numberofwomendiagnosedwithbreastandgynecologiccancers,oftenlaterinlifeandlivinglonger posttreatmentsfortheircancer.Themostcommontreatmentsforthesetypesofcancersincludea
combinationofsurgery,radiationtherapy,chemotherapy,andantihormonaltherapy.Whereasthese treatmentscanbeverysuccessfulintreatingthecancer,theycanalsohaveanadverseimpactonhealthy tissuessuchasmuscle,nerve,andconnective.The adverseimpactonhealthytissuescanattimesbevery closetotheonsetofthetreatment;however,these adverseeffectsoftendevelopslowlyovertimeleading toagraduallossoffunctionthatcanbeimperceptible toboththeindividualandthetreatmentteam.Often thelossoffunctioncannotbedirectlylinkedtoany onetreatment,butrathertoacombinedeffectofseveraltreatmentsaswellthepatient’sownprecancer stateofhealth,nutritionalstatus,andpreexistingdiseasessuchasdiabetesmellitus.
Rehabilitationmedicineshouldbeanintegralpartof thecareofthepersonwithbreastorgynecologiccancer fromtimeofdiagnosis,throughactivetreatmentandin thesurvivorshipperiod.Followingdiagnosisandprecancertreatment,physiatristscanassessthepatientforany preexistingphysicalimpairmentsofkeybodystructures thatwouldbesubjectedtotheeffectsofmultimodality cancertreatment.Forthepersonwithnewlydiagnosed breastcancer,thiscanincludeshoulderdysfunction, assessmentofpreexistingperipheralneuropathy,preexistingpainfuljointconditionsaffectingthehands,knees, andlowerback,andlymphedema.Forthepersonwith newlydiagnosedgynecologiccancer,thiscaninclude assessmentofpreexistingperipheralneuropathy,preexistinglymphedemaofleg,impairedbalance,decreased finemotorskillsandstrengthinhands,andhistoryof pelvicfloordysfunction.Inaddition,anassessmentof nutritionalstatus,preexistingcognitiveimpairment, depression,andanxietyisalsoveryimportant.
Physiatristscanalsoprovideusefulandtimelyinformationtomedical,surgical,andradiationoncologists withrespecttopotentialimpactofcancertreatmenton lossoffunction,whichcantheninturnbeusefulin theplanningofthecancertreatment.Thisisbasedon theirknowledgeoffunctionalanatomyofthemusculoskeletalandnervoussystemsaswellasassessmentof functionalloss.Thisinformationwouldideallybediscussedatmultidisciplinarytumorboards.Anotherrole thatphysiatristscanhaveintheplanningofcancer treatmentistoassessthepatientforfrailtysincefrailty canhaveanadverseimpactonaperson’sabilitytotoleratecancertreatments.
Oncethesepreexistingimpairmentsareidentified, acoordinatedeffortofvariousteammemberssuchas physicaltherapy,occupationaltherapy,psychology, andnutritiontominimizethemiscritical.Attimes,it isnotrealistictoaddressalloftheseimpairments priortostartoftreatmentsincethepatient’sfocusas wellasthatofthecancertreatmentteamisoninitiatingtreatmentassoonaspossible,thereforeprioritizationiskey.Forexample,apatientwithapreexisting reductioninrangeofmotionoftheshoulderwould needthislimitationtobeaddressedtohelpher undergoradiationtherapy.Rehabilitativeinterventionscanbecontinuedduringactivecancertreatment; however,thisdependsonthepatient’sabilitytotoleratebothcancertreatmentandrehabilitativeinterventionsconcurrently.Periodicsurveillanceforsubjective andobjectiveevidenceoflossofphysicalfunction becomesimportantattimesduringactivetreatment aswellasduringsurvivorship.
ASSESSMENTOFBREASTAND
GYNECOLOGICCANCERPATIENTWITHA FOCUSONPHYSICALIMPAIRMENTSAND LOSSOFFUNCTION
Thephysiatristshouldapproachtheassessmentofthe personwithbreastorgynecologiccancerbyhavinga goodworkingknowledgeofthecommonphysical, cognitive,andpsychologicimpairmentsaffectingthe breastandgynecologiccancerpatientsandutilizing appropriateclinicalassessmenttools.
Areviewofpertinentpastmedicalhistoryandpast surgicalhistorycanhelpidentifytheareasofpotential lossoffunction.Forexample,preexistingperipheral neuropathyfromdiabetesmayworsenoncethe patientistreatedwithchemotherapy,thereby adverselyaffectinghandfunctionandbalance. Anotherexampleisapatientwithahistoryoflimited shoulderfunctionduetoadhesivecapsulitisthat
couldpotentiallyleadtoaworseningofthecondition followingtreatmentofbreastcancerwithsurgeryand radiationtherapy.
ReviewofpriorimagingstudiessuchasPET/CT scans,bonescans,MRIs,andplainX-rayscanhelp identifytheareaswithmetastaticdisease.Resultsof echocardiogramsandpulmonaryfunctionstudies,if available,canprovideinformationaboutheartand lungfunction,respectively.Thatknowledgecanthen beusedinsettingprecautionsduringrehabilitationto minimizetheriskofharmforthepatient.Reviewof laboratorystudiessuchashemoglobin,platelet,and whitebloodcellcountscanyieldimportantinformationthatcanbeusedingeneratingadditional hematologicalprecautionsintherehabilitationprescription.Thisinformationaswellasreviewofliver andrenalfunctiontestsandmedicationsforpertinent drug druganddrug diseaseinteractionscanbevery usefulwhenprescribingmedicationsforthetreatment ofpainfulconditions.
Thereviewofsystemscanserveasauseful“checklist”ofareasofpotentialconcernwithrespecttoloss offunctionpostbreastandgynecologiccancertreatment. Table1.1 providesanexampleofsuchachecklistaswellaspossibletreatmentinterventions.In additiontothoselisted,otherareasofinterestinclude symptomspertainingtothecardiovascular,pulmonary,andnervoussystemsaswellaschangesin weightandappetite.
Itisalsoimportanttoassessthepatient’slevelof functionintheirhome,community,andworksettings.Pertinentquestionsabouttheperson’sabilityto performself-careactivitiessuchasbathinganddressingandlimitationsorneedforadditionalassistance areimportant.Householdandcommunitymobility, needforassistivedevicesforwalking,abilitytodrive, shopforfood,andmanagingfinancescanallyield importantinformationaboutfunctionalloss.
Ifthepatientisworking,itisimportanttoinquire aboutthespecifictasksinvolvedintheirworkand anycurrentlimitationsintheirabilitytoperform theirwork.Forexample,apersonwithbreastcancer whoworksasahairdressermayhavedifficultyraising herarmoverheadfollowingbreastcancersurgery, whichcanadverselyaffectherabilitytoperformher job.Anotherexampleisapersonwithgynecologic cancerthatdevelopslymphedemaofthelower extremityaswellasperipheralneuropathy,bothof whichcanmakeitdifficultforhertomaintainher balanceandwalk.Thisinturncanhaveanadverse effectonherjobasaflightattendantforexample.It isalsoimportanttoaskthepersonaboutany
TABLE1.1
BreastandGynecologicCancerImpairmentChecklist
ImpairmentSampleInterventions
FatigueMedicationreview
Treatunderlyinganemiaandhypothyroidismifpresent
Treatdepressionifpresent Exerciseprogram
GeneralweaknessExerciseprogram
ObesityNutritionreferral,exercise
ShoulderdysfunctionPhysicaltherapy
Nonsteroidalantiinflammatorydrugs
AromataseinhibitormusculoskeletalsymptomsPhysicalandoccupationaltherapy
Nutritionreferralifobesityispresent Nonsteroidalantiinflammatorydrugs Injections
LymphedemaLymphedematherapy,compressionsleeve,compressionpump,patient education
Nutritionreferralifobese
Arm-strengtheningexercises
PeripheralneuropathyPhysicaltherapy
Occupationaltherapy
Medications—duloxetine,pregabalin,gabapentin Topicalmedications
CognitiveimpairmentNeuropsychologicalevaluation
Occupationalandspeechtherapy
PsychosocialdistressPsychiatry,psychology,socialworkreferral
AdverseimpactofimpairmentsonworkPhysicalandoccupationaltherapy Drivertraining
Ergonomicevaluation,functionalcapacityevaluation
problemswithconcentration,memoryloss,ordifficultyperformingactivitiesthatrequiretheuseof executivefunctioningskillsforeitherwork,school, hobbies,orfamilylife.
Lastly,inquiringaboutthepatient’sabilitytofunctionintheirvariousliferolessuchasspouseorpartner,daughter,and/orparentcanyielduseful informationaboutadditionalfunctionallimitations. Forexample,aretheredifficultieswithchildrearing duetoshoulderorotherjointpainsorimpairedbalanceassociatedwithneuropathy?Anotherexample,is theresexualdysfunctionassociatedwithtreatmentfor gynecologiccancerthatincludedsurgeryandradiationtherapy?
Sinceexerciseisanimportantpartofthelivesof manypatientswithbreastandgynecologiccancers,it isusefultoinquireaboutanylimitationsintheperson’sabilitytoengageindifferentformsofexercise
duetotheircancerandcancertreatment.Forexample, apersonmaybereluctanttoparticipateduetojoint painsorconcernsaboutsafelyexercisingiftheyhave metastaticbonedisease.
Thephysicalexaminationofthebreastandgynecologiccancerpatientsshouldincludeathorough assessmentofthenervousandmusculoskeletalsystem thatincludesinspection,palpation,rangeofmotion, aswellasspecialdiagnostictestsofinterest. Inspectionandpalpationofsurgicalscarscanyield usefulinformationaboutstructuresthatcanbea sourceofpain.
Musclestrengthtestingofkeymusclegroupsofthe upperandlowerextremities,testingofmusclestretch reflexesoftheupperandlowerextremities,aswellas sensorytestingoftheextremitiesutilizingtestsfor lighttouch,pinprick,vibration,proprioception,cold testing,andmonofilamenttestingtonameafewcan
beuseful.Assessmentforthepresenceoflymphedema shouldincludeobtainingcircumferentialmeasurementsofthearmsorlegsasnecessarytoeitherestablishabaselinelevelforthepatientpriortostartof breastorgynecologiccancertreatment,respectively,as wellasposttreatment.
Functionalexaminationintheclinicsettingcan provideusefulinformationaboutstrength,fallrisk, aswellaspresenceoffra ilty.Sampletestsinclude (1)TimedUpandGoTest,(2)sit-to-standtest,(3)balancetest,and(4)gripstrength.Self-reportedoutcome measurescanalsoprovideusefulinformationabout generalphysicalfunctionandfatigue.
CASCADEOFDISABILITY
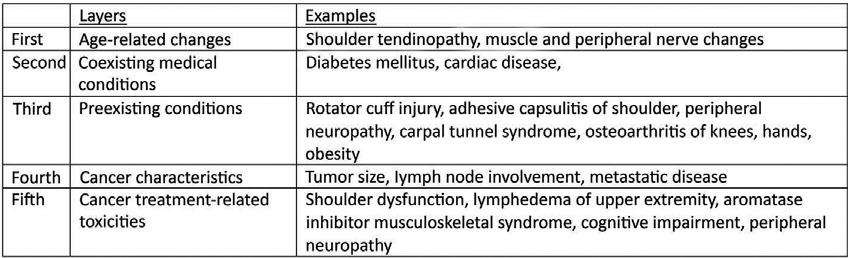
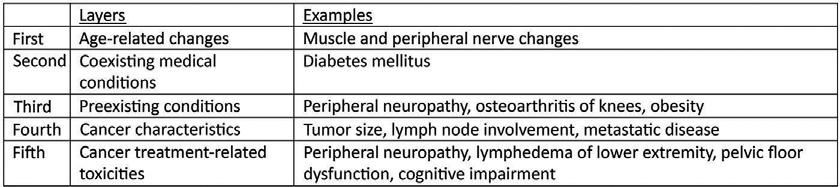
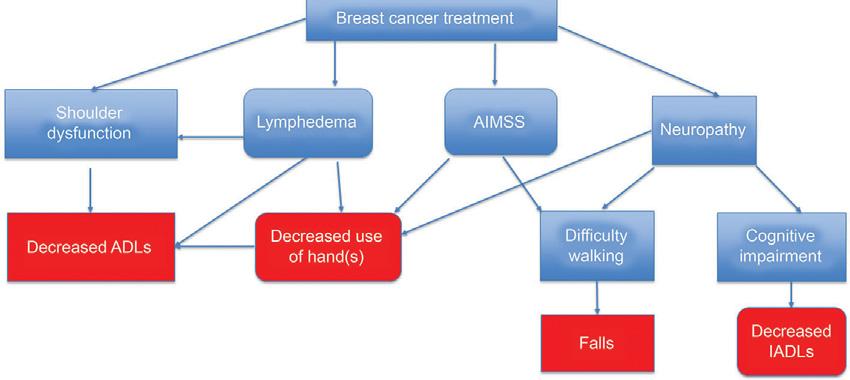
Treatmentsforbreastandgynecologiccancerscan havesignificantadverseeffectsontheindividual affectedbythesecancers.Onewaytothinkaboutthis isthrougha layeringofimpairments. Thereareseveral layersofpotentialissuesaffectingthepersonwith breastorgynecologiccancer:(1)aging-related changes;(2)presenceofcomorbidconditionssuchas diabetes,cardiacdisease,andconnectivetissuedisorders;(3)cancercharacteristicssuchastumorsizeand location,lymphnodeinvolvement,andpresenceof metastaticdisease;and(4)cancertreatment related injurytohealthytissuesfromsurgery,chemotherapy, radiationtherapy,antihormonaltherapies(Figs.1.1 and 1.2).
Thecombinationoffactorssuchasapreexisting sedentarylifestyle,obesity,preexistingperipheralneuropathyassociatedwithdiabetesmellitusandjoint painsfromdegenerativechangesinkneescaneach leadtophysicalimpairmentsandagraduallossof function.Thediagnosisandtreatmentofbreastor
gynecologiccancercanleadtoadditionalimpairmentsthatwhensuperimposedonexistingimpairmentscanleadtoasignificantfunctionaldecline,ora cascadeofdisability.
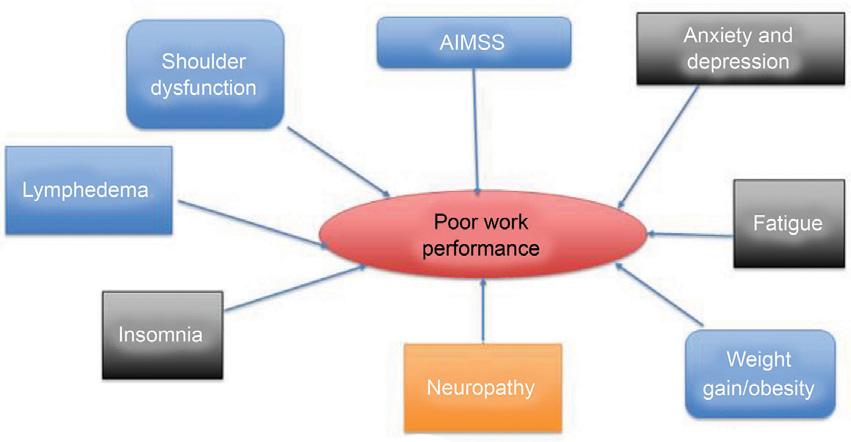
Oneexampleofthiscascadeofdisabilitycouldbe seeninlossofarmfunctioninbreastcancer.Surgery andradiationtherapyforbreastcancercanleadto shoulderdysfunctionandlymphedemaoftheipsilateralarmtherebylimitingtheuseoftheaffectedarm forself-careactivitiessuchasbathinganddressing. Theuseofaromataseinhibitorcanalsocontributeto shoulderandhandpainleadingtofurtherreduction inuseofarm.Chemotherapytreatmentwithcarboplatinorcisplatincanleadtoneuropathicpaininthe handsaswellasdecreasedhandstrengthandsensation,furtherlimitingtheuseofthehands.Thisin turncanimpactontheperson’sabilitytousetheir handsforwork.Chemotherapy-relatedperipheral neuropathycanalsocausepainandalteredsensation inthefeet.Thealteredordiminishedsensationcan adverselyaffectbalance,whichcaninturncontribute tofalls.Paininthejointsofthefeet,knees,andhips duetosideeffectsassociatedwiththeuseofaromataseinhibitorscanalsomakeitdifficultfortheperson towalkmakingthemmoresedentary,whichcanin turncontributetoincreasedweightgain.Paininthe legs,coupledwithimpairedsensationandweakness aswellasdecreaseduseofhands,canalsoaffectthe person’sabilitytodrive.Fatiguecanalsocontributeto lossoffunction.Thiscanbesecondarytochemotherapy,radiationtherapy,anemia,impairedsleepfrom paininshouldersandotherjoints,andpainmedications,allofwhichcanaffectdaytimefunctionat work,school,andinvariousliferolesmentionedearlier.Cognitiveimpairment,anxiety,anddepression canallalsoleadtoalossoffunctionaswell (Fig.1.3).
Thefatigue,diminishedmobilityinhomeand community,impairedbalance,anddecreaseduseof ipsilateralarmandhandscanalladverselyaffectthe person’sabilitytowork.Ifthepersoncannotwork, thereisthepotentialforadropinincome,lossofor significantreductionofhealthinsurancebenefits,and subsequentworseningofhealth.Theperson’sability tofunctionasaparent,spouse,andcaregivertofamilymembersandengageinhobbiescanalsobe diminished.
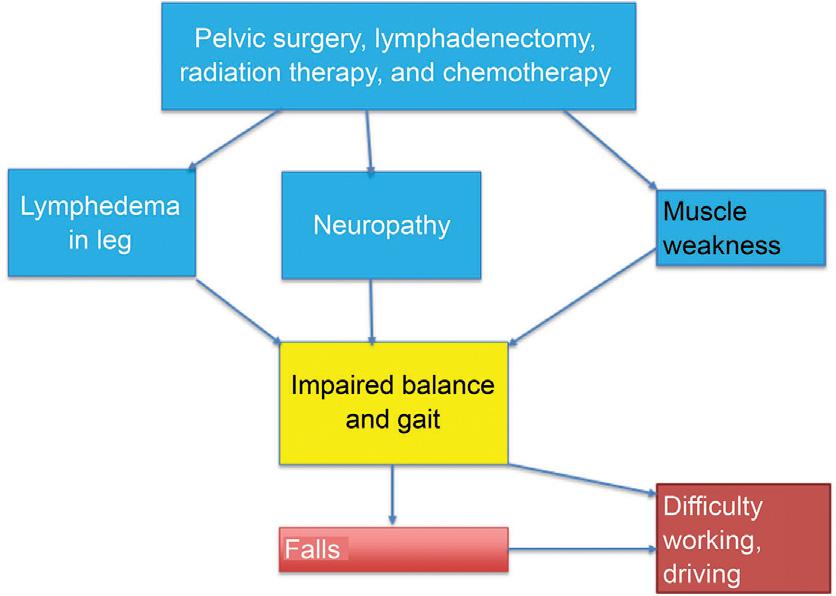
Anotherexampleofthecascadeofdisabilityasit appliestothepersonwithgynecologiccancerisinthe combinationofchemotherapy-inducedperipheral neuropathyassociatedwithlymphedemaoftheleg. Thiscancontributetoimpairedbalanceandan
FIGURE1.1 Layersofimpairments breastcancer.
FIGURE1.2 Layersofimpairments gynecologiccancer.
increasedriskoffalls,whichcanalsoaffectabilityto workinjobsorengageinliferolesthatrequirean intactbalance.Handusecanalsobeaffectedas describedpreviouslyforbreastcancerpatients. Fatigue,cognitiveimpairment,andpsychosocialdistresscanalsobepresentandadverselyaffectquality oflife.Inaddition,gynecologicsurgeryandradiation therapycanadverselyaffectpelvicfloorfunction potentiallycontributingtobowel,bladder,andsexual dysfunction—allofwhichcanhaveaprofoundeffect ontheindividual’squalityoflife(Fig.1.4).
Anyoftheabovementionedcancer-relatedimpairmentscanhaveanadverseeffectonanindividual’s leveloffunction.Whatisstrikingisthatthebreast andgynecologiccancerpatientsfacemanyofthemat thesametimeduringandaftercancertreatmentis completed.Thelossoffunctioncanbeverydramatic suchasthepersonwhocannotlifttheirarmafter
FIGURE1.3 Cascadeofdisabilityinbreastcancer. ADLs,Activitiesofdailyliving; AIMSS,aromataseinhibitor musculoskeletalsyndrome; IADLs,instrumentalactivitiesof dailyliving.Eachofthearrowsalsorepresentspointswhere rehabilitativeinterventionscanbeusedtoeitherprevent impairmentorminimizetheirfunctionalimpactontheindividualiftheyshoulddevelop.
FIGURE1.4 Cascadeofdisabilityingynecologiccancer.
breastcancersurgery,orthedevelopmentoflymphedemainthelegfollowinggynecologicsurgeryand radiationtherapyforgynecologiccancer;however,in manyinstancesthelossoffunctionisgradualsothat thepersonneedstolearntocompensateandaccepta newnormalthatislessthantheirpriorlevelof function.
RETURNTOWORKINBREASTAND GYNECOLOGICCANCERS
Workisanimportantpartoflifewithsubstantial physicalandmentalhealthbenefits.Asmentioned before,personswithbreastandgynecologiccancers facesignificantbarriersinabilitytoreturntowork.In additiontophysicalimpairmentsassociatedwiththe canceranditstreatment,therearetheadditional challengesassociatedwithworkinterruptionsuchas chemotherapyandradiationtherapytreatmentsessions,doctorvisits,aswellastreatmentsideeffects (Fig.1.5).
Inthegeneralcancerpopulation,ithasbeen reportedthat63.5%ofcancersurvivorsreturnto workandthatmeandurationofabsencefromworkis 151days.Around26% 53%ofcancersurvivorslose theirjoborquitworkingovera72-monthperiod postdiagnosis.4 Forsurvivorsofbreastcancerand canceroffemalereproductiveorgans,unemploymentratesarehighercomparedtohealthycontrol participants.5
Noeresetal.reportedonreturntoworkfollowing breastcancerinGermany.Itwasnotedthat1year afterprimarybreastcancersurgery,patientswere almostthreetimesmorelikelytoleavetheirjob comparedtoareferencegroup.At6yearsthepossibilityofreturningtoworkwasonly50%thatofa referencegroup.Factorsassociatedwiththisincluded alowerlevelofeducation,part-timeemployment,
FIGURE1.5 Factorsadverselyaffectingworkperformanceinpersonswithbreastandgynecologiccancer. AIMSS,Aromataseinhibitormusculoskeletalsyndrome.
work-relateddifficulties,age,tumorstage,andseverityofsideeffects.6 Schmidtetal.reportedthat1year followingbreastcancersurgery,57%ofsurvivors workedwiththesameworkingtimeand22%worked withreducedworkingtimecomparedtoprediagnosis. Significantassociationwithrespecttoreturntowork 1yearlaterincludedthepresenceofdepressivesymptoms,armmorbidity,cognitiveimpairment,lower education,youngerage,andpersistentfatigue. Cessationofworkafterbreastcancerwasassociated withaworsequalityoflife.7 Ahistoryofuseofpsychiatricmedicationspriortothediagnosisofbreast cancerledtoasmallyetstatisticallysignificantreductioninreturntowork1yearafterbreastcancerdiagnosis.Factorssuchashighincomeandolderagehad apositivecorrelationwithreturningtowork.8
Stergiou-Kitaetal.reportedthatinassessing whetherornotacancersurvivorcanreturntowork, keyareasthatneedtobefocusedoninclude (1)assessmentoftheperson’sfunctionalabilitiesin relationtojobdemands,(2)identifyingthecancer survivorsindividualstrengthsandbarriersastheypertaintotheirwork,and(3)identifyingsupportsystems intheworkplaceforthesurvivor.Theyconcluded thatcliniciansshoulddetermineifthecancersurvivor is“physically,cognitively,andemotionally”readyto returntoworkandiftheirworkplacehasthenecessarysupportsysteminplacetohavethemreturnto work.9 Forgynecologiccancerpatients,lesshasbeen reportedtodateonreturntoworkcomparedtobreast cancer;however,inJapan,onestudyfoundthat 71.3%ofpatientsreturnedtoworkinthesameworkplaceand83.9%ofpersonswhohadworkedpriorto thegynecologiccancerdiagnosiswereabletoreturn towork.Amongthosewhocouldnotreturntowork, 9.7%wereself-employed,5.9%wereregularly employed,and30.5%werenonregularlyemployed. Nonregularemploymentwasthemostcommonvariabletohaveanegativeeffectonreturntoworkand jobchange.Authorsconcludedthatpreventingnot returningtoworkandchangingjobswereimportant toaddress.10
REHABILITATIONOFBREASTAND GYNECOLOGICCANCERPATIENTS —A HOLISTICAPPROACH
Thegoalofthecancerrehabilitationphysicianisto preventand/orminimizeimpairments,activitylimitationsandparticipationrestrictionsthroughaholistic multidisciplinaryapproachthatfocusesonwhatis trulyimportanttothewomanbeingcaredforand
neverlosingsightofthepersonbehindthediagnosis. Itisimportanttobeopenandreceptivetolearning hergoalsandthephysicallimitationsthatarepreventingherfromlivingherlifetoitsfullest.This requiresanunderstandingofthecomplexinteractions describedearlierandcanserveasafoundationofa treatmentplanthatideallypreventsimpairments fromoccurringinthefirstplaceorminimizesthem oncetheyoccur.
Thesuccessfulrehabilitationofthebreastand gynecologiccancerpatientsshouldideallystarteven beforethebeginningofcancertreatment.Aprerehabilitationprogramemphasizingexercise,nutrition, smokingcessationaswellasassessmentandtreatmentofpreexistingphysicalimpairmentssuchas shoulderdysfunction,jointpain,andpsychosocial distressisparamount.Therehabilitationteamshould workonimprovingthebreastandgynecologiccancer patients’physicalandmentalstrengthforthetreatmentthatisabouttostart.
Duringactivetreatment,prioritizationofrehabilitationinterventionsisimportantascancer-related impairmentsoftenstarttodevelopatthistime. Interventionsthatcanminimizelossoffunctionto theshoulderforexamplecanhelpthepatientcompletecancertreatmentssuchasradiationtherapy, whereadequateshoulderrangeofmotionisessential topositionthepatientforthetreatmentsessions. Psychosocialsupport,massagetherapy,andacupuncturecanbeusefulinterventionsasarejudiciousgeneralconditioningexercisestomaintaingeneral strengthandendurance.
CreativeArtTherapies(art,music,anddance)can helppatientsexploreandexpressdifficultfeelingsand thoughtsrelatedtotheirdiagnosisandexperienceasa cancerpatient.Patientsmayappreciatethechanceto create,reflect,andsharetheirpersonalstoriesregardingtheirillness.Thiscantakemanyforms,including drawing,painting,photography,sculpture,collage, craftwork,anddesignwithtechnology.Itcanbea meaningfulwaytoconnectwithothersandgain strengthandunderstandingfromfellowpatients.Art therapycanincreaseself-esteemandserveasatherapeuticdistractionfromtheillnessandsideeffects.It canalsohelpapersonadjusttoachangingbody imageandcanbebeneficialtothosewhoaredealing withseriousphysicalchallengesaswellandmaypreferthiscreativeoutletaspartoftheirtreatmentplan orwhentheyfeelreadytoreturntowork.
Inthepostcancertreatmentandsurvivorshipstage, itisimportanttoidentifyphysicalimpairments, activitylimitations,andparticipationrestrictionsand
introduceinterventionstominimizefunctionallossas earlyaspossible.Atthisstage,therecanbeseveral disciplinescalledupontoassisttheindividual.Return toworkissuescanrequiretheservicesofphysical therapy,lymphedematherapist,occupationaltherapy, physiatrist,psychology,drivertraining,andevena pelvicfloortherapistiftherearebowelorbladder dysfunctionissues.
CONCLUSION
Byunderstandingthelayersofimpairmentsandhow theycontributetoacascadeofdisability,therehabilitationteamcanworktoaddressthematseverallevels before,during,andaftercancertreatment.Aproactive approachemployedbyrehabilitationclinicianswith timelyandearlyinterventionsastheneedsariseand surveillanceforcancer-relatedimpairmentsatregularlyscheduledoutpatientclinicvisitsarerecommended.Integratingstandardizedfunctionaloutcome toolsusingbothself-reportedandobjectivetesting canprovidemeasurablebenchmarkstoassessthesuccessofrehabilitativeinterventions.
REFERENCES
1.Surveillance,EpidemiologyandEndResults(SEER)programoftheNationalCancerInstitute. ,http://seer.cancer.gov/statfacts/html/cervix.html. Accessed21820.
2.Surveillance,EpidemiologyandEndResults(SEER)programoftheNationalCancerInstitute. ,http://seer.cancer.gov/statfacts/html/corp.html. Accessed21820.
3.Surveillance,EpidemiologyandEndResults(SEER)programoftheNationalCancerInstitute. ,http://seer.cancer.gov/statfacts/html/ovary.html. Accessed21820.
4. MehnertA.Employmentandworkrelatedissuesincancersurvivors. CritRevOncolHematol.2011;77:109 130.
5. DeBoerAG,etal.Cancersurvivorsandunemployment: ameta-analysisandmetaregression. JAMA 2009;301:753 762.
6. NoeresD,Park-SimonTW,GrabowJ,etal.Returnto workaftertreatmentforprimarybreastcanceroverasix yearperiod:resultsfromaprospectivestudycomparing patientswiththegeneralpopulation. SupportCare Cancer.2013;(7)1901 1909.
7. SchmidtM,SchererS,WiskermannJ,SteindorfK.Return toworkafterbreastcancer:theroleoftreatmentrelated sideeffectsandpotentialimpactonqualityoflife. EurJ CancerCare(Engl).2019;28(4).N.PAG-N.PAG.
8. JensenLS,OvergaardC,GameJP,BogglidH,FonagerK. Theimpactofpriorpsychiatricmedicaltreatment onreturntoworkafteradiagnosisofbreastcancer:a registrybasedstudy. ScandJPublicHealth.2019;47 (5):519 527.
9. Stergiou-KitaM,PritloveC,HolnessDL,etal.AmI readytogobacktowork?Assistingcancersurvivorsto determineworkreadiness. JCancerSurvivorship.2016;10 (4):699 710.
10. NakamuraK,MasuyamaH,NishidaT,etal.Returnto workaftercancertreatmentofgynecologiccancerin Japan. BMCCancer.2016;16:1 9.
PracticeImplementation,Clinical Assessment,andOutcomes Measurement
NICOLEL.STOUT,DPT,CLT-LANA,FAPTA • SHANAE.HARRINGTON,PT, PHD
• MERYLJ.ALAPPATTU,PT,PHD
INTRODUCTION
Thecancercarecontinuumisaprotractedtime periodwithmultiplemedicaltreatmentsintroduced atvaryingtimepointsthroughthatcontinuum.Each medicaltreatmentbringswithittheriskfordifferent sideeffectsthatimpactvariousbodysystems.1 Implementingamodelofcarethatoptimallyserves womenduringandaftercancertreatmentrequiresan understandingofthetimingofonsetofcommon impairmentsthroughthecontinuumofcareandrecognitionofthemeasurementtoolsthataremost appropriateforscreeningandassessmenttoidentify impairmentandensurethatevidence-basedinterventionsarethenintroduced.2 Thischapterwillpresent theframeworkoftheprospectivesurveillancemodel (PSM)asaconstructforrehabilitationofpatients withbreastandgynecologicalcancersandwillreview theevidenceforscreeningandassessmentmeasures mostappropriateforthesepopulations.
PROSPECTIVESURVEILLANCEMODEL
Breastandgynecologicalcancertreatments related impairmentsareprevalentandcommonlyincitefunctionalmorbidity.Duetothehighriskofimpairment throughoutthecontinuumofcancercare,itisreasonablethatarehabilitationmodelofcareshouldparallel medicallydirectedtreatment.ThePSMencouragesthe implementationofrehabilitationservicesintothecancercarecontinuumfromthepointofdiagnosisto encourageongoingintervalsurveillanceoffunction, identifyimpairmentearly,andintroduceintervention toamelioratefunctionaldecline.3 Fig.2.1 illustrates thePSManditsnaturalparallelwiththecancer continuum.
Priortotheonsetofcancertreatments,thePSM encouragestheassessmentofanindividual’sbaseline leveloffunction.Assessingcomorbiditiesalsoprovidesinsightonfunctionalcapabilitiesatbaseline. Forsomepopulationsaprehabilitationplanofcare maybeindicated.4 Prehabilitationprovidestargeted interventionstoprepareanindividualforcancertreatmentswiththegoalofoptimizingphysicalfunction priortotheinitiationoftreatment.5 ThePSMthen proceedswithfollow-upassessmentsatintervals throughoutthecarecontinuum.Thepremiseofthe PSMisthatrepeatedintervalassessmentwillenable earlyidentificationofclinicallymeaningfulchanges infunctionalmeasures,comparedtothebaseline, thatwillpromoteearlyidentificationofemerging impairmentsandenablesintroductionofrehabilitationservicesproactively.6,7
Uponcompletionofcancertherapies,ongoing follow-up,screening,andmonitoringforemerging lateeffectsoftreatmentiswarranted.4 Lateeffects maypresentmonthsoryearsfollowingthecompletionofmedicaltreatmentsandincitefunctional decline.ThePSMisahighlyregarded,evidencebasedmodelthatprovidesaclinicalpathwayfor optimalintegrationofrehabilitationservicesintothe cancercarecontinuum.8 Useofproactiverehabilitationservices,asenabledbythePSM,isconsideredto beanimportantcomponentofhigh-qualitycancer care.
ScreeningandAssessmentMeasures
Inherentinasurveillancemodelistheneedforongoingintervalscreeningfortreatment-relatedsymptoms indicativeofemergingimpairmentandassessmentof variousdomainsofphysicalfunction.Thesemeasures