LIST OF CONTRIBUTORS
The editor(s) acknowledge and offer grateful thanks for the input of all previous editions’ contributors, without whom this new edition would not have been possible.
Bassel W. Abou-Khalil, MD
Professor of Neurology Director of Epilepsy Division, Neurology Vanderbilt University Medical Center Nashville, TN, USA
Peter Adamczyk, MD Neurosciences Department Chair Eden Medical Center Castro Valley, CA, USA
Bela Ajtai, MD, PhD
Attending Neurologist DENT Neurologic Institute Amherst, NY, USA
Jeffrey C. Allen, MD Director, Pediatric Neuro-oncology and Neurofibromatosis Programs
Department of Pediatrics, Division of Pediatric HematologyOncology
NYU Langone Medical Center New York, NY, USA
Brandon Ally, PhD
Assistant Professor Department of Neurology Vanderbilt University Nashville, TN, USA
Andrea A. Almeida, MD BA Sports Neurology Fellow Clinical Lecturer, Neurology University of Michigan Ann Arbor, MI, USA
Anthony A. Amato, MD Vice-Chairman Neurology
Brigham and Women’s Hospital; Professor of Neurology Harvard Medical School Boston, MA, USA
Michael J. Aminoff, MD, DSc, FRCP
Distinguished Professor Department of Neurology School of Medicine University of California San Francisco, CA, USA
Nicolaas C. Anderson, DO, MS
Assistant Professor Department of Neurology
Baylor College of Medicine Houston, TX, USA
Tetsuo Ashizawa, MD Professor
Department of Neurology
Houston Methodist Research Institute Houston, TX, USA
Hatim Attar, MD
Assistant Professor of Neurology Department of Neurology
Medical College of Wisconsin and Zablocki VA Medical Center, Milwaukee, WI Milwaukee, WI, USA
Alon Y. Avidan, MD, MPH
Director, UCLA Sleep Disorders Center Director, UCLA Neurology Clinic
University of California at Los Angeles
David Geffen School of Medicine at UCLA
Los Angeles, CA, USA
Joachim M. Baehring, MD, DSc
Associate Professor
Departments of Neurology, Neurosurgery and Medicine
Chief
Section of Neuro-Oncology
Yale Cancer Center
Yale School of Medicine
New Haven, CT, USA
Asim K. Bag, MD
Associate Member
Department of Diagnostic Imaging, St. Jude Children’s Research Hospital Memphis, TN, USA
Laura J. Balcer, MD, MSCE
Professor of Neurology and Population Health
Vice Chair, Department of Neurology
NYU Langone Medical Center
New York, NY, USA
Leomar Y. Ballester, MD, PhD
Assistant Professor
Co-Director, Molecular Diagnostics Laboratory
Department of Pathology and Laboratory Medicine
Department of Neurosurgery
University of Texas Health Science Center at Houston, TX, USA
Robert W. Baloh, MD
Professor, Department of Neurology
Division of Head and Neck Surgery
University of California School of Medicine
Los Angeles, CA, USA
Elizabeth Barkoudah, MD
Program Director, Neurodevelopmental Disabilities Residency
Program Director, Children with Disabilities HMS Student Clerkship
Co-Director Cerebral Palsy and Spasticity Center
Department of Neurology Boston, MA, USA
Roger A. Barker, BA, MBBS, MRCP PhD Professor of Clinical Neuroscience
Honorary Consultant Neurologist
Department of Clinical Neurosciences
University of Cambridge Addenbrooke’s Hospital Cambridge, UK
Ryan Barmore, MD
Adjunct Clinical Postdoctoral Associate Neurology
University of Florida Gainesville, FL, USA
J.D. Bartleson, MD, FAAN
Emeritus Professor of Neurology
Mayo Clinic
College of Medicine and Science Rochester, MN, USA
Amit Batla, MBBS MD DM (Neurology) FRCP
Honorary Consultant Neurologist
National Hospital for Neurology and Neurosurgery and Royal Free London Hospital
UCL Queen Square Institute of Neurology, London, UK
John David Beckham, MD
Associate Professor Departments of Medicine, Neurology, and Immunology and Microbiology University of Colorado Anschutz Medical Campus Aurora, CO, USA
Leigh Beglinger, PhD Neuropsychologist Elks Rehab System Boise, ID, USA
David H. Benninger, PD Dr Senior Consultant and Lecturer in Neurology Department of Clinical Neurosciences University Hospital of Lausanne (CHUV) Lausanne, Switzerland
Joseph R. Berger, MD, FACP, FAAN, FANA
Professor of Neurology and Associate Chief of the Multiple Sclerosis Division Perelman School of Medicine University of Pennsylvania Philadelphia, PA, USA
José Biller, MD, FACP, FAAN, FAHA, FANA
Professor and Chairman Department of Neurology Loyola University Chicago Stritch School of Medicine Maywood, IL, USA
David F. Black, MD Assistant Professor of Neurology and Radiology Mayo Clinic Rochester, MN, USA
Nicholas Boulis, MD Associate Professor Department of Neurosurgery, Emory University Atlanta, GA, USA
Michael P. Bowley, MD, PhD Staff Neurologist Massachusetts General Hospital Instructor Harvard Medical School Boston, MA, USA
Sherri A. Braksick, MD Assistant Professor Department of Neurology Senior Associate Consultant Neurosciences ICU Mayo Clinic Rochester, MN, USA
Helen M. Bramlett, PhD Professor, Neurological Surgery
University of Miami Miller School of Medicine
Research Health Scientist, Research Service
Bruce W. Carter Department of Veterans Affairs Medical Center Miami, FL, USA
Steven M. Bromley, MD Director
Bromley Neurology Audubon, NJ, USA
Joseph Bruni, MD, FRCPC Consultant Neurologist
St. Michael’s Hospital; Associate Professor of Medicine
University of Toronto Toronto, ON, Canada
John C.M. Brust, AB, MD Professor of Neurology
Columbia University College of Physicians and Surgeons
New York, NY, USA
W. Bryan Burnette, MD, MS Associate Professor
Pediatrics and Neurology
Vanderbilt University School of Medicine, Nashville, TN, USA
Carol Camfield, MD
Professor Emeritus Pediatrics
Dalhousie University Halifax, NS, Canada
Peter Camfield, MD Professor Emeritus Pediatrics
Dalhousie University Halifax, NS, Canada
Alan Carson, MB, ChB, MD, FRCPsych, FRCP, MPhil Consultant Neuropsychiatrist
Senior Lecturer in Psychological Medicine Department of Clinical Neurosciences University of Edinburgh Edinburgh, United Kingdom
Dimitri Cassimatis, MD Associate Professor of Medicine
Emory University School of Medicine Atlanta, GA, USA
Robert Cavaliere, MD Assistant Professor
The Ohio State University Columbus, OH, USA
David A. Chad, MD Staff Neurologist
Reliant Medical Group
Saint Vincent Hospital Worcester, MA, USA
Vijay Chandran, MBBS, DM Clinical Fellow
Pacific Parkinson’s Research Centre University of British Columbia Vancouver, BC, Canada
Gisela Chelimsky, MD Professor of Paediatrics
The Medical College of Wisconsin Milwaukee, WI, USA
Thomas Chelimsky, MD Professor of Neurology
The Medical College of Wisconsin Milwaukee, WI, USA
Tanuja Chitnis, MD Professor of Neurology
Harvard Medical School Boston, MA, USA
Sudhansu Chokroverty, MD, FRCP Professor and Co-Chair Program Director of Clinical Neurophysiology and Sleep Medicine
NJ Neuroscience Institute at JFK Clinical Professor, Robert Wood Johnson Medical School
New Brunswick, NJ, USA
Ugonma N. Chukwueke, MD Center for Neuro-Oncology
Dana-Farber Cancer Institute Boston, MA, USA
Paul E. Cooper, MD, FRCPC, FAAN Professor of Neurology, Schulich School of Medicine and Dentistry and University Hospital, London Health Sciences Centre, London, ON, Canada
Dany Cordeau, RN, PhD(c) Registered Nurse Department of Sexology
Université du Québec à Montréal Montreal, QC, Canada
Frédérique Courtois, PhD Chair, Full Professor Department of Sexology
Université du Quéébec à Montréal Montreal, QC, Canada
Claire J. Creutzfeldt, MD
Harborview Comprehensive Stroke Center University of Washington Seattle, WA, USA
Josep Dalmau, MD, PhD
ICREA Research Professor Hospital Clinic, IDIBAPS/University of Barcelona
Barcelona, Spain, Adjunct Professor Neurology University of Pennsylvania Philadelphia, PA, USA
Robert B. Daroff, MD
Professor and Chair Emeritus Department of Neurology
Case Western Reserve School of Medicine University Hospitals Case Medical Center Cleveland, OH, USA
Ranan DasGupta, MBBChir, MA, MD, FRCS(Urol)
Consultant Urological Surgeon Department of Urology
Imperial College Healthcare NHS Trust London, UK
Mariel B. Deutsch, MD
Behavioral Neurology and Neuropsychiatry Fellow
V.A. Greater Los Angeles Healthcare System
David Geffen School of Medicine at UCLA Los Angeles, CA, USA
Michael W. Devereaux, MD Professor of Neurology University Hospitals Case Medical Center Case Western Reserve University Cleveland, OH, USA
Melissa DiBacco, MD
Postdoctoral Clinical Research Fellow Department of Neurology – Epilepsy Division
Boston Children’s Hospital Boston, MA, USA
W. Dalton Dietrich, PhD Scientific Director
The Miami Project to Cure Paralysis Professor of Neurological Surgery, Neurology, Cell Biology and Biomedical Engineering University of Miami
Leonard M. Miller School of Medicine Center Miami, FL, USA
Pradeep Dinakar, MD, MS, MBA, FAAP Director, Interventional Pain Program
Boston Children’s Hospital
Pain Management Center
Mass General Brigham
Assistant Professor of Anesthesiology
Harvard Medical School Boston, MA, USA
Bruce H. Dobkin, MD Professor of Neurology
University of California Los Angeles Los Angeles, CA, USA
Richard L. Doty, BS, MA, PhD
Director, Smell and Taste Center
Hospital of the University of Pennsylvania Professor, Otorhinolaryngology: Head and Neck Surgery
University of Pennsylvania, Perelman School of Medicine
Philadelphia, PA, USA
Gary R. Duckwiler, MD
Professor and Director Interventional Neuroradiology
Director, INR Fellowship Program
Co-Director UCLA HHT Center of Excellence
David Geffen School of Medicine at UCLA Los Angeles, CA, USA
Ronald G. Emerson, MD
Attending Neurologist and Director Intraoperative Monitoring Program
Hospital for Special Surgery
New York, NY, USA
Michelle T. Fabian, MD
Assistant Professor
Icahn School of Medicine at Mount Sinai
New York, NY, USA
Alireza Faridar, MD
Assistant professor Neurology
Houston Methodist Houston, TX, USA
Conor Fearon, BE, MB, BCh, BAO
Clinical Fellow
Department of Neurology
University of Toronto Toronto, ON, Canada
Marcia V. Felker, MD
Clinical Assistant Professor of Pediatric Neurology
Indiana University School of Medicine
Riley Hospital for Children Indianapolis, IN, USA
Richard D. Fessler, MD, PhD
Neurosurgery Resident
Rush University Medical Center Chicago, IL, USA
Richard G. Fessler, MD, PhD Professor, Neurosurgery
Rush University Medical Center, Chicago, IL, USA
Kathryn C. Fitzgerald, ScD
Assistant Professor of Neurology and Epidemiology, Johns Hopkins University, Baltimore, MD, USA
Laura Flores-Sarnat, MD
Adjunct Research Professor of Clinical Neurosciences and Paediatrics University of Calgary and Alberta Children’s Hospital Research Institute Calgary, AB, Canada
Brent L. Fogel, MD, PhD
Associate Professor of Neurology and Human Genetics
David Geffen School of Medicine University of California, Los Angeles Los Angeles, CA, USA
Brent P. Forester, MD, MSc
Associate Professor of Psychiatry Chief, Division of Geriatric Psychiatry McLean Hospital, Harvard Medical School, Belmont, MA, USA
Jennifer E. Fugate, DO
Assistant Professor of Neurology Divisions of Critical Care and Cerebrovascular Neurology Mayo Clinic Rochester, MN, USA
Martin J. Gallagher, MD, PhD
Associate Professor of Neurology
Vanderbilt University School of Medicine Nashville, TN, USA
Sharon L. Gardner, MD
Associate Professor, Pediatrics
Stephen D Hassenfeld Childrens Center For Cancer and Blood Disorders
New York University Langone Medical Center
New York, NY, USA
Jarred Garfinkle, MDCM, MSc, FRCPC
Neonatologist, Department of Pediatrics
McGill University/Montreal Children’s Hospital Montreal, QC, Canada
Ivan Garza, MD
Assistant Professor of Neurology Department of Neurology Mayo Clinic Rochester, MN, USA
Claudio Melo de Gusmao, MD Clinical Director, Movement Disorders Program Neurology Boston Children’s Hospital Boston, MA, USA
Carissa Gehl, PhD
Clinical Associate Professor Department of Psychiatry University of Iowa Iowa City, IA, USA
Christopher D. Geiger, DO
Assistant Professor Department of Neurology Case Western Reserve School of Medicine University Hospitals Cleveland Medical Center Cleveland, OH, USA
David S. Geldmacher, MD Professor Department of Neurology University of Alabama at Birmingham Birmingham, AL, USA
Carter Gerard, MD
Neurosurgery Resident Rush University Medical Center Chicago, IL, USA
Daniel H. Geschwind, MD, PhD David Geffen School of Medicine University of California, Los Angeles Los Angeles, CA, USA
Michael D. Geschwind, MD, PhD, FAAN, FANA
Professor, Michael J. Homer Family Chair in Neurology Department of Neurology, Memory and Aging Center University of California, San Francisco San Francisco, CA, USA
Katherine A. Gifford, PhD
Assistant Professor of Neurology Vanderbilt University Medical Center Nashville, TN, USA
K. Michael Gibson, PhD Professor of Pharmacotherapy College of Pharmacy and Pharmaceutical Sciences
Washington State University Spokane, WA, USA
Meredith R. Golomb, MD, MSc
Associate Professor Division of Child Neurology Department of Neurology
Indiana University School of Medicine Indianapolis, IN, USA
Rachel Goode, MD
Assistant Professor of Pediatrics Department of Pediatrics
Vanderbilt University Medical Center Nashville, TN, USA
Jonathan Graff-Radford, MD
Assistant Professor of Neurology Mayo Clinic College of Medicine Rochester, MN, USA
Olivia Groover, MD
Assistant Professor of Neurology
Emory University Atlanta, GA, USA
Jeffrey T. Guptill, MD, MA, MHS
Professor of Neurology
Director, Duke University School of Medicine, Faculty
Duke Clinical Research Unit Durham, NC, USA
Cecil D. Hahn, MD, MPH
Associate Professor Paediatrics (Neurology) University of Toronto Director
Critical Care EEG Monitoring Program The Hospital for Sick Children Toronto, ON, Canada
Christine Hall, PhD
Adjunct Professor Department of Psychology Emory University Atlanta, GA, USA
Mark Hallett, MD Chief, Human Motor Control Section National Institute of Neurological Disorders and Stroke
National Institutes of Health Bethesda, MD, USA
Aline I. Hamati, MD
Clinical Assistant Professor of Pediatric Neurology
Indiana University School of Medicine
Riley Hospital for Children Indianapolis, IN, USA
David Hart, MD
Director, Neurosurgery Spine
The Neurological Institute
University Hospitals Case Medical Center
Associate Professor of Neurological Surgery
Department of Neurological Surgery
Case Western Reserve University Cleveland, OH, USA
Sabine Hellwig, MD Neurologist
Assistant in Psychiatry Department of Psychiatry and Psychotherapy
University Hospital Freiburg Freiburg, Germany
Karl Herholz, MD Professor in Clinical Neuroscience Division of Neuroscience and Experimental Psychology University of Manchester Manchester, UK
Alan Hill, MD, PhD Professor, Pediatrics University of British Columbia Child Neurologist
British Columbia’s Children’s Hospital Vancouver, BC, Canada
Benjamin D. Hill, PhD Assistant Professor Psychology Department/CCP University of South Alabama Mobile, AL, USA
Fred H. Hochberg, MD Visiting Scientist, Neurosurgery University of California at San Diego San Diego, CA, USA
Kristin Huntoon, PhD, DO University of Texas MD Anderson Cancer Center Houston, TX, USA
Jason T. Huse, MD, PhD
Associate Professor Departments of Pathology and Translational Molecular Pathology
University of Texas MD Anderson Cancer Center Houston, TX, USA
Monica P. Islam, MD, FAES, FACNS
Associate Professor of Clinical Pediatrics
Section of Child Neurology
Nationwide Children’s Hospital
The Ohio State University College of Medicine Columbus, OH, USA
Michael Iv, MD
Clinical Associate Professor, Radiology Stanford University Stanford, CA, USA
Reza Jehan, MD Professor Department of Radiological Sciences
David Geffen School of Medicine at UCLA Los Angeles, CA, USA
Joseph Jankovic, MD
Professor of Neurology
Distinguished Chair in Movement Disorders Director of Parkinson’s Disease Center and Movement Disorders Clinic Department of Neurology Baylor College of Medicine Houston, TX, USA
S. Andrew Josephson, MD
Carmen Castro Franceschi and Gladyne K. Mitchell
Neurohospitalist Distinguished Professor and Chair
Department of Neurology University of California, San Francisco San Francisco, CA, USA
Tudor G. Jovin, MD Neurology Cooper University Hospital Camden, NJ, USA
Min K. Kang, MD
Assistant Clinical Professor Department of Neurology University of California, San Francisco San Francisco, CA, USA
Matthias A. Karajannis, MD, MS Chief, Pediatric Neuro-Oncology Service Attending Physician Department of Pediatrics Memorial Sloan Kettering Cancer Center New York, NY, USA
Carlos S. Kase, MD Professor of Neurology
Emory University School of Medicine Atlanta, GA, USA
Bashar Katirji, MD Director, Neuromuscular Center and EMG Laboratory
University Hospitals Cleveland Medical Center Professor Department Neurology Case Western Reserve University School of Medicine Cleveland, OH, USA
Kevin A. Kerber, MD
Professor
University of Michigan Health System
Ann Arbor, MI, USA
Geoffrey A. Kerchner, MD, PhD
Global Development Leader Product Development Neuroscience F. Hoffman-La Roche, Ltd.
Basel, Switzerland
Ryan Khanna, MD Neurosurgery Resident
Rush University Medical Center Chicago, IL, USA
Samia J. Khoury, MD
Director of Abou-Haider Neuroscience Institute
Professor of Neurology
American University of Beirut Medical Center Beirut, lebanon; Visiting Professor of Neurology Harvard Medical School Boston, MA, USA
Howard S. Kirshner, BA, MD Professor and Vice Chairman Department of Neurology Vanderbilt University Medical Center Nashville, TN, USA
Stefan Klöppel, MD Head of Memory Clinic Department of Psychiatry and Psychotherapy University Medical Center Freiburg Freiburg, Germany
Anita A. Koshy, MD Assistant Professor Department of Neurology Department of Immunobiology University of Arizona, College of Medicine Tucson, AZ, USA
Stephen C. Krieger, MD
Associate Professor of Neurology Corinne Goldsmith Dickinson Center for MS
Icahn School of Medicine at Mount Sinai New York, NY, USA
Abhay Kumar, MD
Assistant Professor Neurology Saint Louis University Saint Louis, MO, USA
John F. Kurtzke, MD, FACP, FAAN
Professor Emeritus, Neurology Georgetown University; Consultant, Neurology Veterans Affairs Medical Center Washington, DC, USA
Jeffrey S. Kutcher, MD, FAAN Director, Kutcher Clinic for Sports Neurology Brighton, Michigan Park City, UT, USA
Sheng-Han Kuo, MD
Assistant Professor Department of Neurology College of Physicians and Surgeons Columbia University New York, NY, USA
Anthony E. Lang, MD, FRCPC Professor
Department of Medicine, Neurology University of Toronto Director of Movement Disorders Center and the Edmond J. Safra Program in Parkinson’s Disease Toronto Western Hospital Toronto, ON, Canada
Patrick J.M. Lavin, MB, BCh, BAO, MRCPI
Professor, Neurology and Ophthalmology Department of Neurology
Vanderbilt University Medical School Nashville, TN, USA
Alice Lawrence, PT, MD
Assistant Professor of Pediatrics Department of Pediatrics
Vanderbilt University Medical Center Nashville, TN, USA
Marc A. Lazzaro, MD
Assistant Professor of Neurology and Neurosurgery Director, Neurointerventional Fellowship Training Program
Medical Director, Telestroke Program
Medical College of Wisconsin and Froedtert Hospital Milwaukee, WI, USA
Sönke Langner
Department of Diagnostic Radiology and Neuroradiology, University Medicine, Greifswald, Germany
David S. Liebeskind, MD, FAAN, FAHA Professor of Neurology Neurology Director, Stroke Imaging Co-Director, UCLA Cerebral Blood Flow Laboratory
Director, UCLA Vascular Neurology Residency Program; Associate Neurology Director, UCLA Stroke Center
UCLA Department of Neurology Los Angeles, CA, USA
Chih-Chun Lin, MD, PhD Movement Disorders fellow Department of Neurology College of Physicians and Surgeons Columbia University New York, NY, USA
Eric Lindzen, MD, PhD
Jacobs Neurological Institute School of Medicine and Biomedical Sciences State University of New York at Buffalo Buffalo, NY, USA
Alan H. Lockwood, MD, FAAN, FANA Emeritus Professor Neurology and Nuclear Medicine University at Buffalo Buffalo, NY, USA
Glenn Lopate, MD Professor of Neurology Department of Neurology Washington University School of Medicine Saint Louis, MO, USA
Fred D. Lublin, MD
Saunders Family Professor of Neurology; Director, The Corinne Goldsmith Dickinson Center for MS
Icahn School of Medicine at Mount Sinai New York, NY, USA
Michael J. Lyerly, MD
Associate Professor Director, Birmingham VA Medical Center Stroke Center Department of Neurology University of Alabama at Birmingham Birmingham, AL, USA
Robert L. Macdonald, MD, PhD Professor of Neurology Vanderbilt University Medical Center Nashville, TN, USA
Devin D. Mackay, MD
Associate Professor of Neurology, Ophthalmology and Neurosurgery Director of Neuro-Ophthalmology
Indiana University School of Medicine Indianapolis, IN, USA
Robert Mallery, MD
Assistant Professor Neurology
Brigham and Women’s Hospital Boston, MA, USA
Joseph C. Masdeu, MD, PhD
Graham Family Distinguished Chair in Neurological Sciences
Director, Nantz National Alzheimer Center and Neuroimaging
Houston Methodist Neurological Institute
Houston Methodist Hospital Houston, TX, USA
John C. Mazziotta, MD, PhD
Vice Chancellor of UCLA Health Sciences
Dean, David Geffen School of Medicine
CEO UCLA Health
University of California, Los Angeles Los Angeles, CA, USA
Mario F. Mendez, MD, PhD Director, Behavioral Neurology Program, and Professor Neurology and Psychiatry
David Geffen School of Medicine at UCLA Director, Neurobehavior
V.A. Greater Los Angeles Healthcare System Los Angeles, CA, USA
Philipp T. Meyer, MD, PhD
Medical Director and Professor
Department of Nuclear Medicine
Medical Center - University of Freiburg
Faculty of Medicine, University of Freiburg Freiburg, Germany
Dominique S. Michaud, ScD
Professor, Department of Public Health and Community Medicine
Tufts University School of Medicine Boston, MA, USA
Amanda Miller, LMSW
Social Worker
University of Iowa Huntington’s Disease Society of America Center of Excellence
University of Iowa Carver College of Medicine
Iowa City, IA, USA
Karl E. Misulis, MD, PhD
Professor of Clinical Neurology and Clinical Biomedical Informatics
Director of Neurology Hospitalist Service
Vanderbilt University School of Medicine Nashville, TN, USA
Hiroshi Mitsumoto, MD, DSc
Director
Eleanor and Lou Gehrig MDA/ALS Research Center
The Neurological Institute
New York, NY, USA
Brian Murray, MB, BCh, BAO, MSc
Consultant Neurologist
Hermitage Medical Clinic
Old Lucan Road
Dublin, Ireland
E. Lee Murray, MD, FACP
Clinical Assistant Professor of Neurology
University of Tennessee Health Science Center
Memphis, TN, USA
Attending Neurologist
West Tennessee Neuroscience Jackson, TN, USA
Evan D. Murray, MD
Assistant in Neurology/ Instructor in Neurology
Department of Neurology
McLean Hospital/ Massachusetts General Hospital/ Harvard Medical School
Belmont, MA, USA;
Director, Traumatic Brain Injury Service
Manchester VA Medical Center
Manchester, NH, USA
Fadi Nahab, MD
Associate Professor of Neurology and Pediatrics
Emory University Atlanta, GA, USA
Ruth Nass, MD
Professor of Child Neurology, Child and Adolescent Psychiatry, and Pediatrics
New York University Langone Medical Center
New York, NY, USA
Lakshmi Nayak, MD
Assistant Professor of Neurology, Harvard Medical School
Center for Neuro-Oncology, Dana-Farber/ Brigham and Women’s Cancer Center
Boston, MA, USA
Nancy J. Newman, MD
LeoDelle Jolley Professor of Ophthalmology
Professor of Ophthalmology and Neurology
Instructor in Neurological Surgery, Emory University School of Medicine
Director, Section of Neuro-Ophthalmology
Emory Eye Center
Emory University
Atlanta, GA, USA
Thanh N. Nguyen, MD
Neurology, Radiology
Boston Medical Center
Boston University School of Medicine
Boston, MA, USA
Raul G. Nogueira, MD Neurology
Marcus Stroke and Neuroscience Center
Grady Memorial Hospital
Emory University School of Medicine Atlanta, GA, USA
John G. Nutt, MD Professor of Neurology
Oregon Health & Science University Portland, OR, USA
Marc R. Nuwer, MD, PhD
Department Head, Clinical Neurophysiology
Ronald Reagan UCLA Medical Center; Professor, Neurology
David Geffen School of Medicine at UCLA
Los Angeles, CA, USA
D. David O’Banion, MD FAAP
Assistant Professor of Pediatrics, Developmental and Behavioral Pediatrics, Neurology
Emory University School of Medicine
Children’s Healthcare of Atlanta Pediatrics Institute Atlanta, GA, USA
Michael S. Okun, MD
Adelaide Lackner Professor of Neurology and Neurosurgery
UF Center for Movement Disorders and Neurorestoration
Gainesville, FL, USA
Justin J.F. O’Rourke, PhD
Clinical Neuropsychologist
South Texas Veterans Healthcare System
San Antonio, TX, USA
Claudia R. Padilla, MD
Behavioral Neurology and Neuropsychiatry Fellow
David Geffen School of Medicine
University of California at Los Angeles Neurobehavior Unit
VA Greater Los Angeles Healthcare System
Los Angeles, CA, USA
Jalesh N. Panicker, MD, DM, MRCP(UK)
Consultant and Honorary Senior Lecturer Department of Uroneurology
The National Hospital for Neurology and Neurosurgery and UCL Institute of Neurology London, UK
Leila Parand, MD
Behavioral Neurology Fellow
David Geffen School of Medicine
University of California at Los Angeles
V.A. Greater Los Angeles Healthcare System
Los Angeles, CA, USA
Jane S. Paulsen, PhD
Professor
Department of Neurology
University of Wisconsin-Madison Madison, WI, USA
Phillip L. Pearl, MD
Director of Epilepsy and Clinical Neurophysiology
William G. Lennox Chair, Department of Neurology
Boston Children’s Hospital Professor of Neurology, Harvard Medical School Boston, MA, USA
Zhongxing Peng-Chen, MD Neurologist
Movement Disorder Specialist Neurología
Universidad del Desarrollo, Hospital Padre Hurtado
Facultad de Medicina Clínica Alemana Santiago, Chile
David L. Perez, MD, MMSc
Assistant Professor of Neurology Departments of Neurology and Psychiatry
Massachusetts General Hospital
Harvard Medical School Boston, MA, USA
Ronald C. Petersen, PhD, MD Professor of Neurology
Cora Kanow Professor of Alzheimer Disease Research
Department of Neurology
Mayo Clinic College of Medicine Rochester, MN, USA
Ronald F. Pfeiffer, MD Professor
Department of Neurology
Oregon Health & Science University Portland, OR, USA
Robert D.S. Pitceathly, MBChB, PhD
MRC Clinician Scientist and Honorary Consultant Neurologist
Department of Neuromuscular Diseases
University College London Queen Square Institute of Neurology and The National Hospital for Neurology and Neurosurgery London, UK
Scott L. Pomeroy, MD, PhD
Bronson Crothers Professor of Neurology Director, Intellectual and Developmental Disabilities
Research Center
Harvard Medical School
Chair, Department of Neurology Neurologist-in-Chief
Boston Children’s Hospital Boston, MA, USA
Sashank Prasad, MD
Associate Professor of Neurology
Harvard Medical School
Chief, Division of Neuro-Ophthalmology
Brigham and Women’s Hospital Director, Harvard-Brigham and Women’sMassachusetts
General Hospital Neurology Residence Program Boston, MA, USA
Bruce H. Price, MD
Chief, Department of Neurology McLean Hospital
Associate Neurologist
Massachusetts General Hospital Associate Professor of Neurology
Harvard Medical School Boston, MA, USA
Raymond S. Price, MD
Associate Professor of Clinical Neurology and Neurology Residency Program Director
Perelman School of Medicine University of Pennsylvania Philadelphia, PA, USA
Louis J. Ptáček, MD
Distinguished Professor Department of Neurology University of California, San Francisco San Francisco, CA, USA
Alejandro A. Rabinstein, MD Professor
Department of Neurology Consultant
Neurosciences ICU Mayo Clinica Rochester, MN, USA
Vijay Ramaswamy, MD, PhD, FRCPC
Assistant Professor and Staff NeuroOncologist
Division of Haematology/Oncology
Departments of Medical Biophysics and Paediatrics
Hospital for Sick Children and University of Toronto Toronto, ON, Canada
Tyler Reimschisel, MD, MHPE
Founding Associate Provost for Interprofessional Education Research and Collaborative Practice Case Western Reserve University and Cleveland Clinic Cleveland, OH, USA
Bernd F. Remler, MD Professor of Neurology and Ophthalmology Departments of Neurology and Ophthalmology Medical College of Wisconsin Chief, Section of Neurology, Zablocki VA Medical Center, Milwaukee, WI Milwaukee, WI, USA
Michel Rijntjes, MD Department of Neurology and Neuroscience University Medical Center Freiburg Freiburg, Germany
E. Steve Roach, MD Professor of Neurology University of Texas Dell Medical School Austin, TX, USA
Carrie E. Robertson, MD Assistant Professor Department of Neurology Mayo Clinic Rochester, MN, USA
Maisha T. Robinson, MD, MS Departments of Neurology and Family Medicine Mayo Clinic Jacksonville, FL, USA
Michael Ronthal, MbBCh, FRCP, FRCPE, FCP(SA) Professor of Neurology Emeritus Department of Neurology Beth Israel Deaconess Medical Center Harvard Medical School Boston, MA, USA
Karen L. Roos, MD
John and Nancy Nelson Professor of Neurology Department of Neurology Indiana University School of Medicine Indianapolis, IN, USA
Ashley M. Roque, MD Assistant Professor Department of Neuro-Oncology Mount Sinai Hospital New York, NY, USA
Gary A. Rosenberg, MD
Professor of Neurology
Director, UNM Center for Memory and Aging
University of New Mexico Health Sciences Center Albuquerque, NM, USA
Myrna R. Rosenfeld, MD, PhD
Senior Investigator Neuroimmunology Program
Hospital Clinical/IDIBAPS Barcelona, Spain
Adjunct Professor, Neurology University of Pennsylvania Philadelphia, PA, USA
Janet C. Rucker, MD
Bernard A. and Charlotte Marden Professor Departments of Neurology and Ophthalmology
New York University School of Medicine
New York, NY, USA
Sean D. Ruland, DO Professor
Department of Neurology Loyola University Chicago Stritch School of Medicine
Maywood, IL, USA
Delaram Safarpour, MD, MSCE Assistant Professor of Neurology Department of Neurology
Oregon Health and Science University Portland, OR, USA
Donald B. Sanders, MD Professor of Neurology
Duke University Medical School Durham, NC, USA
Harvey B. Sarnat, MS, MD, FRCPC Professor
Departments of Paediatrics, Pathology (Neuropathology) and Clinical Neurosciences
University of Calgary, Cumming School of Medicine
Calgary, AB, Canada
Jeffrey L. Saver, MD, FAHA, FAAN, FANA
Professor of Neurology
Senior Associate Vice Chair for Clinical Research
Department of Neurology
Director, UCLA Comprehensive Stroke and Vascular Neurology Program
David Geffen School of Medicine at UCLA
Los Angeles, CA, USA
Komal T. Sawlani, MD
Assistant Professor Department of Neurology
Case Western Reserve University School of Medicine Cleveland, OH, USA
Anthony H.V. Schapira, MD, DSc, FRCP, FMedSci
Chairman and Professor of Clinical Neurosciences
Department of Clinical and Movement Neurosciences
University College London Queen Square Institute of Neurology London, UK
David Schiff, MD
Harrison Distinguished Teaching Professor Departments of Neurology, Neurological Surgery, and Medicine
University of Virginia School of Medicine Charlottesville, VA, USA
Michael J. Schneck, MD, FACP, FAAN, FAHA, FANA
Professor Department of Neurology Loyola University Chicago
Stritch School of Medicine
Maywood, IL, USA
Kirsten M. Scott, MRCP, PhD Neurology Registrar Department of Neurology
Addenbrooke’s hospital Cambridge, UK
Meagan D. Seay, DO
Assistant Professor
Department of Ophthalmology and Visual Sciences
Assistant Professor
Department of Neurology
University of Utah
Moran Eye Center UT, USA
D. Malcolm Shaner, MD, FAAN
Clinical Professor of Neurology Department of Neurology
David Geffen School of Medicine, UCLA
Kaiser Permanente West Los Angeles Medical Center
Los Angeles, CA, USA
Kaveh Sharzehi, MD, MS
Assistant Professor of Medicine Department of Medicine
Division of Gastroenterology and Hepatology
Oregon Health & Science University Portland, OR, USA
Ashkan Shoamanesh, MD, FRCPC
Assistant Professor of Medicine (Neurology) Director, Hemorrhagic Stroke Research Program
Marta and Owen Boris Chair in Stroke Research and Care McMaster University / Population Health Research Institute Hamilton, ON, Canada
Reet Sidhu, MD Director, Developmental Neurology Program
Assistant Professor of Pediatrics, Neurology
Emory University School of Medicine Children’s Healthcare of Atlanta Pediatrics Institute Atlanta, GA, USA
Jonathan H. Smith, MD, FAHS Associate Professor of Neurology Department of Neurology Mayo Clinic Scottsdale, AZ, USA
Laura A. Snyder, MD, FAANS Attending Neurosurgeon Barrow Neurological Institute Phoenix, AZ, USA
Yuen T. So, MD, PhD Professor of Neurology School of Medicine
Stanford University Palo Alto, CA, USA
Marylou V. Solbrig, MD Formerly Professor Departments of Medicine (Neurology) and Medical Microbiology University of Manitoba Winnipeg, MB, Canada
Siddharth Srivastava, MD Instructor of Neurology Department of Neurology Boston Children’s Hospital Harvard Medical School Boston, MA, USA
Martina Stippler, MD, AANS, FACS Director of Neurotrauma Department of Neurosurgery Harvard Medical School
Beth Israel Deaconess Medical Center Boston, MA, USA
Jon Stone, MB ChB FRCP PhD
Honorary Professor (University of Edinburgh)
Department Clinical Neurosciences Western General Hospital Edinburgh, UK
Jerry W. Swanson, MD, MHPE Professor of Neurology Department of Neurology
Mayo Clinic College of Medicine and Science Rochester, MN, USA
Viktor Szeder, MD, PhD, MSc
Associate Clinical Professor
Department of Radiological Sciences
David Geffen School of Medicine at UCLA Los Angeles, CA, USA
Lee A. Tan, MD
Assistant Professor
Department of Neurosurgery
UCSF Medical Center
San Francisco, CA, USA
Satoshi Tateshima, MD, DMSc Professor
Division of Interventional Neuroradiology
Department of Radiological Sciences
Ronald Reagan UCLA Medical Center
David Geffen School of Medicine at UCLA Los Angeles, CA, USA
Boon Lead Tee, MD, MSc
Assistant Professor Department of Neurology Memory and Aging Center
University of California, San Francisco San Francisco, CA, USA
Stefan J. Teipel, MD
Head of Section for Gerontopsychosomatic and Dementia Diseases
Deputy DZNE Site Speaker Rostock Greifswald and Head of the Section for Clinical Research
Clinic for Psychosomatic and Psychotherapeutical Medicine
Section of Gerontopsychosomatic Universitiy Medicine Rostock
German Center for Neurodegenerative Diseases, Site Rostock/Greifswald Rostock, Germany
Reena P. Thomas, MD PhD
Clinical Assistant Professor
Division of Neuro-Oncology
Department of Neurology
Stanford University Stanford, CA, USA
Philip D. Thompson, MBBS PhD FRACP
Emeritus Professor of Neurology Department of Medicine
University of Adelaide Adelaide, SA, Australia
Matthew J. Thurtell, MBBS, MSc, FRACP
Associate Professor, Ophthalmology and Neurology
Director, Neuro-Ophthalmology Service
Department of Ophthalmology and Visual Sciences
Department of Neurology
University of Iowa Iowa City, IA, USA
Robert L. Tomsak, MD, PhD Professor of Ophthalmology and Neurology
Wayne State University School of Medicine
Specialist in Neuro-ophthalmology Kresge Eye Institute Detroit, MI, USA
Bryan Tsao, MD, MBA, FAAN, FANA
Professor and Chair
Department of Neurology
Loma Linda University Health School of Medicine
Loma Linda, CA, USA
Chris Turner, FRCP PhD Consultant Neurologist
Queen Square Centre for Neuromuscular Diseases
The National Hospital for Neurology and Neurosurgery
Queen Square London, UK
Kenneth L. Tyler, MD
Louise Baum Endowed Chair
Chairman of the Department of Neurology University of Colorado School of Medicine Aurora, CO, USA
Stan H.M. Van Uum, MD, PhD, FRCPC Professor of Medicine, Schulich School of Medicine and Dentistry, St. Joseph’s Health Care London, ON, Canada
Ashok Verma, MD, DM, MBA, FAAN, FANA
Professor of Neurology
Staff Neurologist, Miami VA Medical Center Director, Neuromuscular Medicine
Fellowship Training Program
Medical Director, Bruce W. Carter VAMC
ALS Program
Department of Neurology
University of of Miami Miller School of Medicine
Miami, FL, USA
Michael Wall, MD
Professor of Ophthalmology and Neurology University of Iowa, College of Medicine
Iowa City, IA, USA
Mitchell T. Wallin, MD, MPH
Associate Professor of Neurology, Department of Neurology, George Washington University & University of Maryland Washington, DC, USA
Leo H. Wang, MD, PhD
Associate Professor of Neurology Department of Neurology University of Washington School of Medicine Seattle, WA, USA
Karin Weissenborn, MD, FRCP Associate Professor Clinic for Neurology Hannover Medical School Hannover, Germany
Cornelius Weiller, MD Director and Chair Department of Neurology and Clinical Neuroscience Medical Faculty University Hospital Freiberg Freiberg, Germany
Patrick Y. Wen, MD Center for Neuro-Oncology Dana-Farber Cancer Institute Boston, MA, USA
Mark A. Whealy, MD Assistant Professor of Neurology Department of Neurology Mayo Clinic Rochester Rochester, MN, USA
Eelco F.M. Wijdicks, MD PhD Professor of Neurology Consultant Neurosciences intensive Care Unit
Division of Neurocritical Care and Hospital Neurology Mayo Clinic Rochester, MN, USA
Stephen M. Wilson, PhD Associate Professor
Department of Hearing and Speech Sciences Vanderbilt University Medical Center Nashville, TN, USA
Daniel Winkel, MD
Assistant Professor of Neurology Department of Neurology Emory University School of Medicine Atlanta, GA, USA
Oleg Y. Yerstein, MD Director Center for Memory and Cognitive Disorders Lahey Hospital and Medical Center Los Angeles, CA, USA
Osama O. Zaidat, MD, MS Neuroscience Institute Bon Secours Mercy Health System St Vincent Hospital Toledo, OH, USA
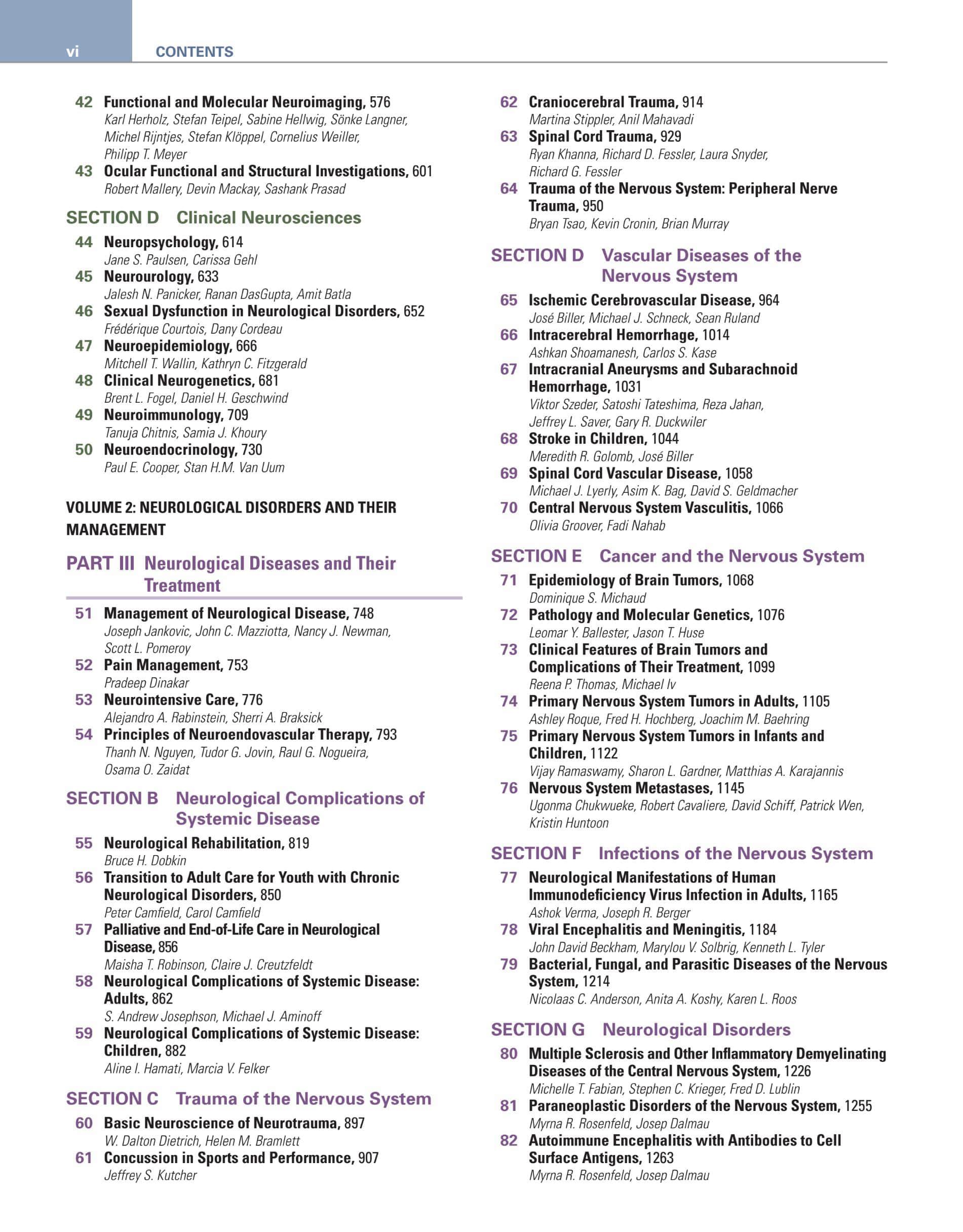
VIDEO TABLE OF CONTENTS
Chapter 8
Chapter 8
Video 1a Infant Social Skills: Social Smile
Video 1b Infant Motor Skills: Prone Position
Chapter 8 Video 2a Infant Social Skills: Social Laugh
Chapter 8
Video 2b Resolved Head Lag in Infant
Chapter 8
Video 2c Infant Motor Skills: Bears Weight
Chapter 8
Video 2d Infant Motor Skills: Rolling
Chapter 8
Video 3a Infant Motor Skills: Tripod Sit
Chapter 8
Video 3b Infant Motor Skills: Hands to Feet
Chapter 8
Video 3c Infant Motor Skills: Prone Extension
Chapter 8
Video 3d Infant Motor Skills: Pivot in Prone
Chapter 8 Video 3e Infant Motor Skills: Raking Grasp
Chapter 8 Video 3f Motor Skills: Hand Transfer
Chapter 8 Video 4a Infant object Permanence
Chapter 8 Video 4b Infant Motor Skills: Pull to Stand
Chapter 8
Video 4c Infant play: Banging Cups
Chapter 8
Video 4d Infant Motor Skills: Crawling
Chapter 8
Video 4e Infant Motor Skills: 3-Finger Grasp
Chapter 8
Video 5a Infant Motor Skills: Reciprocal Crawl
Chapter 8
Video 5b Toddler Motor Skills: Early Walker
Chapter 8
Video 5c Toddler Social Skills: Response to Name
Chapter 8 Video 6a Toddler Motor Skills: Mature Pincer
Chapter 8 Video 6b Toddler Social Skills: Pointing for Interest
Chapter 8 Video 6c Toddler Motor Skills: Transition to Stand
Chapter 8 Video 6d Toddler Motor Skills: Stoop and Recover
Chapter 8 Video 6e Toddler Language Skills: Functional Sign Language
Chapter 8 Video 7 Toddler Cognitive Skills: Pellet in Bottle
Chapter 8 Video 8a Toddler Motor Skills: Kicking
Chapter 8 Video 8b Toddler Motor Skills: Nonreciprocal Stair Pattern
Chapter 8 Video 8c Toddler Motor Skills: Normal Gait
Chapter 8 Video 9a Toddler Cognitive Skills: Block Copy
Chapter 8 Video 9b Toddler Motor Skills: Imitates Circle
Chapter 8 Video 9c Toddler Cognitive Skills: Matching Colors
Chapter 8 Video 9d Toddler Motor Skills: Jumping
Chapter 8 Video 9e Toddler Motor Skills: Toddler Run
Chapter 8 Video 9f Toddler Cognitive Skills: Unscrew Bottle Top
Chapter 8 Video 9g Toddler Language Skills: 3-Word Phrase
Chapter 8 Video 9h Toddler Language Skills: Labeling
Chapter 8 Video 10a Toddler Cognitive Skills: Block Tower
Chapter 8 Video 10b Toddler Motor Skills: Tip Toe Gait
Chapter 8 Video 11a Toddler Cognitive Skills: Block Copy
Chapter 8 Video 11b Toddler Motor Skills: Alternating Stairs
Chapter 8 Video 11c Toddler Cognitive Skills: Concept of One
Chapter 8 Video 11d Toddler Motor Skills: Tricycle
Chapter 8 Video 11e Toddler Cognitive Skills: Big/Little
Chapter 8 Video 12a Childhood Motor Skills: Broad Jump
Chapter 8 Video 12b Childhood Motor Skills: 1-Legged Balance/Hop
Chapter 8 Video 12c Childhood Motor Skills: Scissor Use
Chapter 8 Video 12d Childhood Cognitive Skills: Person Picture <10 parts
Chapter 8 Video 13a Childhood Language Skills: Counting
Chapter 8 Video 13b Childhood Motor Skills: Dynamic Grasp
Chapter 8 Video 13c Childhood Cognitive skills: Person Picture >10 parts
Chapter 8 Video 13d Childhood Motor Skills: Skipping
Chapter 8 Video 13e Childhood Motor Skills: In-Hand Manipulation of Object
Chapter 8 Video 13f Childhood Motor Skills: In-Hand Rotation of Pencil
(Clips 8-1a-8-13f Video Contributors: Alice Lawrence, Rachel Goode)
Chapter 18 Video 1 Forced Ductions
Chapter 18 Video 2 Eyelid Signs of Myasthenia Gravis
Chapter 18 Video 3 Internuclear Ophthalmoplegia
Chapter 18
Video 4 Horizontal Supranuclear Saccadic Gaze Palsy
Chapter 18 Video 5 One and A Half Syndrome
Chapter 18 Video 6 Dorsal Midbrain Syndrome
Chapter 18 Video 7 Oculopalatal Myoclonus
Chapter 18 Video 8 Downbeat Nystagmus
Chapter 18 Video 9 Upbeat Nystagmus
Chapter 18 Video 10 Gaze-Evoked Nystagmus
Chapter 18 Video 11 Square Wave Jerks
Chapter 18 Video 12 Ocular Flutter
Chapter 18 Video 13 Opsoclonus
(Clips 18.1, 18.3, 18.8 - 18.13 © Patrick J. M. Lavin, All rights reserved; Clips 103.3 - 103.7 © Janet C. Rucker, All rights reserved.)
Chapter 21 Video1 Bilateral Internuclear Ophthalmoplegia (INO) in a Patient with Multiple Sclerosis
Chapter 22 Video 1 Acute Peripheral Vestibular Nystagmus
Chapter 22 Video 2 Ocular Flutter
Chapter 22 Video 3 Gaze-Evoked Nystagmus and Impaired Smooth Pursuit
Chapter 22 Video 4 Gaze-Evoked Downbeating Nystagmus
Chapter 22 Video 5 Hypermetric Saccades
Chapter 22 Video 6 Head-Thrust Tests
Chapter 22 Video 7 Benign Paroxysmal Positional Vertigo
Chapter 22 Video 8 Epley Maneuver
Chapter 23 Video 1 Neurological Exams of a Case of SCA1
Chapter 23 Video 2 Different gait difficulties in ataxia patients
Chapter 23 Video 3 Various Eye Movement Abnormalities in Cerebellar Ataxia
Chapter 23 Video 4 A Case of SCA2
Chapter 23 Video 5 A Case of SCA7
Chapter 23 Video 6 A Case of Multiple System Atrophy
Chapter 28 Video 1 Grip Myotonia in a Patient with Myotonic Dystrophy Type 1
Chapter 28 Video 2 Myokymia
Chapter 28 Video 3 Percussion Myotonia in Delayed Onset Radiation-Induced Injury Following Treatment of Squamous Cell Carcinoma of the Oropharynx
Chapter 35 Video1 Seizure 1
Chapter 35 Video2 Seizure 2
Chapter 35 Video3 Seizure 3
Chapter 36 Video 1 End-Plate Noise
Chapter 36 Video 2 End-Plate Spikes
Chapter 36 Video 3 Fibrillation Potential
Chapter 36 Video 4 Fasciculation Potential
Chapter 36 Video 5 Myotonic Discharges
Chapter 36 Video 6 Myokymic Discharge
Chapter 36 Video 7 Complex Repetitive Discharge
Chapter 36 Video 8 Clinical Electromyography: Neuromyotonic Discharge
Chapter 36 Video 9 Clinical Electromyography: Cramp Discharge
Chapter 36 Video 10 Normal potential at Slight Concentration
Chapter 36 Video 11 Polyphasic Motor Unit Action Potential with Satellite Potentials
Chapter 36 Video 12 Chronic Reinnervation—Long Duration and Increased Amplitude
Chapter 36 Video 13 Moderately Decreased Recruitment
Chapter 36 Video 14 Unstable Motor Unit Action Potentials
Chapter 36 Video 15 Brief Duration, Short Amplitude, and Polyphasic Motor Unit Action Potentials
Chapter 36 Video 16 Poor Activation
(Clips 36.1–16 From Preston D. C., Shapiro B. E. Electromyography and Neuromuscular Disorders: Clinical–Electrophysiologic Correlations, 3rd edn. © 2013, Elsevier Inc.)
Chapter 38 Video 1 “Off” Stimulation Evaluation in Parkinson Disease
Chapter 38 Video 2 “On” Stimulation Evaluation in Parkinson Disease
Chapter 38 Video 3 Pre-surgical Evaluation in Essential Tremor
Chapter 38 Video 4 Post-surgical Evaluation in Essential Tremor
Chapter 55 Video 1 AKFO to Control Snap Back and Toe Catch
Chapter 96 Video 1 Patient with Parkinson’s Disease and Extreme Flexion of the Trunk (Camptocormia)
Chapter 96 Video 2 Patient with Parkinson’s Disease and Anterocollis and Camptocormia
Chapter 96 Video 3 Patient with Parkinsonism and Striatal Hand Deformities
Chapter 96 Video 4 Parkinson’s Disease; Patient with Young-Onset Parkinson’s Disease and Gait Difficulty Due to Freezing (Motor Blocks)
Chapter 96 Video 5 Patient with Dementia with Lewy Bodies and Visual Hallucinations
Chapter 96 Video 6 Parkinson’s Disease; Levodopa-Induced Dyskinesia
Chapter 96 Video 7 Progressive Supranuclear Palsy; Typical Worried, Frowning Facial Expression (Procerus Sign), Apraxia of Eyelid Opening, Although Vertical (Downward) Gaze is Preserved, Vertical Optokinetic Nystagmus is Absent
Chapter 96 Video 8 Patient with Progressive Supranuclear Palsy and Vertical Ophthalmoplegia, Marked Postural Instability, and Perseveration of Visual Gaze
Chapter 96 Video 9 Patient with Progressive Supranuclear Palsy Showing Square Wave Jerks, Slow Saccades and Abnormal Gait
Chapter 96 Video 10 Progressive Supranuclear Palsy; Deep Facial Folds, Vertical Ophthalmoplegia, Marked Postural Instability, Slumps into a Chair
Chapter 96 Video 11 Patient with Progressive Supranuclear Palsy, Procerus Sign, Deep Facial Folds, and Apraxia of Eyelid Opening
Chapter 96 Video 12 Multiple System Atrophy; Patient Describes Symptoms of Dysautonomia, Demonstrates Flexion of the Neck and Apraxia of Eyelid Opening, Typical of MSA
Chapter 96 Video 13 Corticobasal Degeneration; Patient Describes Apraxia of Left Leg, Demonstrates Ideomotor Apraxia in Left More than Right Hand and Marked Left Leg and Foot Apraxia
Chapter 96 Video 14 Patient with Corticobasal Degeneration Describing the Alien Hand Phenomenon and Manifesting Asymmetric Apraxia, Hand Myoclonus and Cortical Sensory Deficit (Graphesthesia)
Chapter 96 Video 15 Corticobasal Degeneration; Evoked Hand and Arm Myoclonus
Chapter 96 Video 16 Patient with Corticobasal Degeneration and Myoclonus
Chapter 96 Video 17 Vascular Parkinsonism; Broad-Based Gait, Freezing on Turning (Lower Body Parkinsonism) Associated with Binswanger’s Disease (See Head MRI)
Chapter 96 Video 18 Vascular Parkinsonism; Gait Initiation Failure (Pure Freezing)
Chapter 96 Video 19 Essential Tremor; Marked Improvement in Right Hand Tremor with Contralateral Deep Brain Stimulation of the VIM Thalamus
Chapter 96 Video 20 Cerebellar Outflow Tremor Because of Multiple Sclerosis; Markedly Improved with Deep Brain Stimulation of the VIM Thalamus
Chapter 96 Video 21 Patient with Orthostatic Tremor Manifested by High Frequency Tremor Upon Standing
Chapter 96 Video 22 Wilson’s Disease; Slow Tremor (Myorrhythmia) in the Left Hand
Chapter 97 Video 1 Herditary Spastic Paraparesis
Chapter 97 Video 2 Fasciculations
Chapter 97 Video 3 Kennedy Disease (X-Linked Recessive Bulbospinal Neuronopathy)
Chapter 97 Video 4 Amyotrophic Lateral Sclerosis
Chapter 97 Video 5 C9orf72 Mutation
(Clip 97.5 Adapted from Movement Disorders, 2012; http://www.ncbi. nlm.nih.gov/pmc/articles/PMC3516857/)
Chapter 100 Video 1 Focal Impaired Awareness Seizure of Right Mesial Temporal Origin
Chapter 100 Video 2 Right Hand RINCH Motions During a Left Temporal Ictal Discharge
Chapter 100 Video 3 Hyperkinetic Automatisms–Hypermotor Seizure of Frontal Lobe Origin
Chapter 100 Video 4 Gelastic seizure in a patient with hypothalamic hamartoma
Chapter 100 Video 5 Focal to bilateral tonic-clonic seizure in a patient with left temporal seizure origin
Chapter 100 Video 6 Frontal Lobe Seizure of Right Anterior Cingulate Origin
Chapter 100 Video 7 Generalized Absence Seizure with Immediate Return of Responsiveness Postictally
Chapter 100 Video 8 Generalized Absence Seizure Evolving to Bilateral Tonic-Clonic Seizure
Chapter 100 Video 9 Myoclonic Seizures in a Patient with Juvenile Myoclonic Epilepsy
Chapter 100 Video 10 Myoclonic Atonic Seizure
Chapter 100 Video 11 Cluster of Myoclonic Seizures Leading to Tonic-Clonic Seizure
Chapter 100 Video 12 Brief Tonic Seizure
Chapter 101 Video 1 Circadian Oscillators in the Epithalamus
(From Guilding, C., Hughes, A.T.L., Piggins, H.D. Circadian oscillators in the epithalamus. Neuroscience, Vol.169, Issue 4. Pages 1630-1639. Copyright © 2010 IBRO. Published by Elsevier Ltd.)
Chapter 101 Video 2 Thirty-Five Years of Undiagnosed Narcolepsy
(From Kryger, M. H. Gallery of Patient Interview Chapters. Atlas of Clinical Sleep Medicine,Second Edition. Copyright © 2014, 2010 by Saunders, an imprint of Elsevier Inc., Chapter 20, 478-482.)
Chapter 101 Video 3 Diagnosis, Disease Course, and Management of Patients with Kleine-Levin Syndrome
(From Arnulf, I., Rico, T. J, BS, Mignot, E. The Lancet Neurology. 201210-01, Vol. 11, Issue 10, Pages 918-928, Copyright © 2012 Elsevier Ltd.)
Chapter 101 Video 4 Cheyne-Stokes Respiration and Obstructive Sleep Apnea with Heart Failure
(From Kryger, M. H. Gallery of Sleep Laboratory Chapter Findings. Atlas of Clinical Sleep Medicine,Second Edition. Copyright © 2014, 2010 by Saunders, an imprint of Elsevier Inc., Chapter 21, 483-495.)
Chapter 101 Video 5 Middle-Aged Woman with Restless Legs Syndrome
(From Kryger, M. H. Gallery of Patient Interview Chapters. Atlas of Clinical Sleep Medicine,Second Edition. Copyright © 2014, 2010 by Saunders, an imprint of Elsevier Inc., Chapter 20, 478-482.)
Chapter 101 Video 6 Restless Legs Syndrome with Periodic Limb Movements During Sleep (x25)
(From Kryger, M. H. Gallery of Sleep Laboratory Chapter Findings. Atlas of Clinical Sleep Medicine,Second Edition. Copyright © 2014, 2010 by Saunders, an imprint of Elsevier Inc., Chapter 21, 483-495.)
Chapter 101 Video 7 Periodic Limb Movements in Sleep
(From Sleep Medicine Pearls, 3rd Edition, 3rd edn, Berry, Richard B., MD; Wagner, Mary H., MD. Copyright © 2015, 2003, 1999 by Saunders, an imprint of Elsevier Inc.)
Chapter 101 Video 8 Parasomnias and Nocturnal Frontal Lobe Epilepsy (NFLE): Lights and Shadows – Controversial points in the differential diagnosis
(From Bisulli, F. et al, Sleep Medicine Volume 12. Copyright © 2011 Elsevier B.V.)
Chapter 101 Video 9 Fatal Familial Insomnia
(From Chokroverty, S., Thomas, R. J. (eds). Atlas of Sleep Medicine, Copyright © 2014 by Saunders, an imprint of Elsevier Inc.)
Chapter 101 Video 10 Bruxism
(From Berry, R. B., Wagner, M. H . Sleep Medicine Pearls, 3rd Edition. © 2015 Elsevier. All Rights Reserved.)
Chapter 101 Video 11 NREM Parasomnia (Confusional Arousal)
(From Pincherle, A. et al. Epilepsy and NREM-parasomnia: A complex and reciprocal relationship. Sleep Medicine. 13(4), 2012. Pages 442–444. © Elsevier. doi:10.1016/S1389-9457(12)00144-X.)
Chapter 101 Video 12 NREM Parasomnia (Confusional Arousal)
(From Pincherle, A. et al. Epilepsy and NREM-parasomnia: A complex and reciprocal relationship. Sleep Medicine. 13(4), 2012. Pages 442–444. © Elsevier. doi:10.1016/S1389-9457(12)00144-X)
Chapter 101 Video 13 REM Sleep Behavior Disorder 1
(From Berry, R. B., Wagner, M. H . Sleep Medicine Pearls, 3rd Edition. © 2015 Elsevier. All Rights Reserved.)
Chapter 101 Video 14 REM Sleep Behavior Disorder 2
(From Berry, R. B., Wagner, M. H . Sleep Medicine Pearls, 3rd Edition. © 2015 Elsevier. All Rights Reserved.)
Chapter 101 Video 15 Willis-Ekbom Disease Foundation Revised Consensus Statement on the Management of Restless Legs Syndrome
(From Silber, M. H., et al. Mayo Clinic Proceedings, 2013-09-01, Volume 88, Issue 9, Pages 977-986, Copyright © 2013 Mayo Foundation for Medical Education and Research.)
Chapter 101 Video 16 Explaining the Results
(From Kryger, M. H. Gallery of Patient Interview Chapters. Atlas of Clinical Sleep Medicine,Second Edition. Copyright © 2014, 2010 by Saunders, an imprint of Elsevier Inc., Chapter 20, 478- 482.)
Chapter 101 Video 17 A 58-Year-Old Man With PositionDependent Nocturnal Dyspnea
From Schertel, A. et al. Chest, Volume 152, Issue 2 Copyright © 2017 American College of Chest Physicians.
Chapter 101 Video 18 A 12-Year-Old Boy with Sleep Apnea and Restless Sleep
(From Kryger, M. H. Gallery of Sleep Laboratory Chapter Findings. Atlas of Clinical Sleep Medicine,Second Edition. Copyright © 2014, 2010 by Saunders, an imprint of Elsevier Inc., Chapter 21, 483- 495.)
Chapter 101 Video 19 Pediatric Sleep Surgery
(From Resnick, C. M. Atlas of the Oral and Maxillofacial Surgery. Clinics of North America. Published March 1, 2019. Vol. 27, Issue 1. Pages 67-75. Copyright © 2018 Elsevier Inc.)
Chapter 101 Video 20 70-Year-Old Male Patient With a 15Year History of Parkinson’s Disease, Severe Depression and Longstanding RBD Displaying Marked Episodes of Laughter During REM Sleep
(From Siclari, F. et al. Parkinsonism and Related Disorders, Vol. 17, Issue 5. Copyright © 2011 Elsevier Ltd.)
Chapter 101 Video 21 Ictal Bruxism Treated with Temporal Lobectomy
(From Guaita, M.et al. Sleep Medicine, Volume 16, Issue 11, Copyright © 2015 Elsevier B.V.)
Chapter 101 Video 22 Familial Idiopathic Rapid Eye Movement Sleep Behavior Disorder
(From Aurélie, P-J., Lannuzel, A., Arnulf, I. Sleep Medicine, 2017-0201, Volume 30, Pages 29-30, Copyright © 2016 Elsevier.)
Chapter 103 Video 1 Large Left Hypertropia Secondary to Right Oculomotor Nerve Palsy
Chapter 103 Video 2 Left Appendicular Ataxia
Chapter 103 Video 3 Prominent Left Ptosis
Chapter 103 Video 4 Cranial Neuropathies/Impaired Adduction, Elevation, and Depression with Intact Abduction of the Left Nerve
Chapter 103 Video 5 Bilateral Abduction Deficits Secondary to Demyelinating Bilateral Abducens Palsies
Chapter 103 Video 6 Esotropia
Chapter 103 Video 7 Facial Nerve Function in a Patient with a History of Right Facial Palsy Two Years Ago and Current Left Facial Palsy
Chapter 103 Video 8 Other Babinski Sign
(Clips 103.1–2 from Leigh R. J., Zee, D. S. The Neurology of Eye Movements, 5th Edition, 2015. © Oxford University Press; Clips 103.2 - 103.7 © Janet C. Rucker, All rights reserved; Clip 103.8 Courtesy of Joseph Jankovic, MD)
Chapter 108 Video 1 Ocular Examination in MG
Chapter 108 Video 2 Pseudo-INO in MG
Chapter 108 Video 3 “Curtain Sign”
Chapter 108 Video 4 Edrophonium Test
Chapter 108 Video 5 Triple Timed Up-and-Go Test in LEM
Chapter 109 Video 1 Myotonic Dystrophy
Chapter 111-1 This 11-Year-Old Boy Has Dyskinetic Cerebral Palsy Secondary to Kernicterus
Chapter 111-2 This 5-Year-Old Girl Has Dyskinetic Cerebral Palsy Secondary to Hypoxic Ischemic Injury
Chapter 113 Video 1 Patient Describing Dissociation at Onset of Functional Left Hemiparesis and Functional Left Facial Spasm
Chapter 113 Video 2 Longstanding Functional Left Arm and Leg Weakness and Sensory Disturbance
Chapter 113 Video 3 Right Sided Functional Leg Weakness with a Positive Hoover Sign
Chapter 113 Video 4 Functional Facial Spasm Showing Contraction of Platysma on the Right with Jaw Deviation to the Right
Chapter 113 Video 5 Bilateral Functional Ankle/Foot Dystonia Showing Fixed Nature of Deformity During Gait
Chapter 113 Video 6 Sedation Used Therapeutically for Treatment of Functional Paralysis and dystonia
(Clip 113.6 From Stone J, Hoeritzauer I, Brown K, Carson A. Therapeutic Sedation for Functional (Psychogenic) Neurological Symptoms. J Psychosom Res 2014; 76:165–8.)