Atlas of Abdominal Wall Reconstruction
Second Edition
Michael J. Rosen, MD, FACS Professor of Surgery
Lerner
College
of
Medicine; Director,
Cleveland Clinic Comprehensive Hernia Center Cleveland Clinic Foundation Cleveland Ohio
I would like to dedicate this atlas to all of my patients. It is through their surgical treatment that we constantly improve and find the best surgical approaches for their disorders.
Eduardo Parra-Davila, MD, FACS, FASCRS
Director of Minimally Invasive and Colorectal Surgery Director of Hernia and Abdominal Wall Reconstruction Celebration Health Florida Hospital Celebration, Florida
Eric M. Pauli, MD
Assistant Professor of Surgery Director of Endoscopic Surgery Department of General Surgery
Penn State Milton S. Hershey Medical Center Hershey, Pennsylvania
Clayton C. Petro, MD General Surgery Resident University Hospitals Case Medical Center Cleveland, Ohio
Ajita S. Prabhu, MD
Assistant Professor Department of Surgery University Hospitals Case Medical Center Cleveland, Ohio
Michael J. Rosen, MD, FACS Professor of Surgery Lerner College of Medicine; Director, Cleveland Clinic Comprehensive Hernia Center
Cleveland Clinic Foundation Cleveland Ohio
Steven Rosenblatt, MD, FACS Staff Surgeon General Surgery Cleveland Clinic Cleveland, Ohio
J. Scott Roth, MD, FACS Professor of Surgery and Chief, Gastrointestinal Surgery Department of Surgery University of Kentucky Lexington, Kentucky
Christopher J. Salgado, MD Professor Division of Plastic Surgery Department of Surgery University of Miami Miami, Florida
Carley E. Schroering Medical Student University of Kentucky Lexington, Kentucky
Nathaniel F. Stoikes, MD, FACS
Assistant Professor of Surgery University of Tennessee Health Science Center Memphis, Tennessee
Jeffrey Ustin, MD, MS, FACS Acute Care Surgeon General Surgery Cleveland Clinic Cleveland, Ohio
Guy R. Voeller, MD, FACS Professor of Surgery University of Tennessee Health Science Center Memphis, Tennessee
David L. Webb, MD, FACS
Assistant Professor Department of Surgery University of Tennessee Health Science Center Memphis, Tennessee
Joshua S. Winder, MD Research Fellow Department of General Surgery Penn State Milton S. Hershey Medical Center Hershey, Pennsylvania
Benjamin Zendejas-Mummert, MD Resident in Surgery Mayo Clinic Rochester, Minnesota
Martin D. Zielinski, MD, FACS
Associate Professor Department of Surgery Mayo Clinic Rochester, Minnesota
Xiphoid process
Costal margin
Parietal peritoneum
Extraperitoneal (subserosa) fascia
Transversalis fascia
Transversus abdominis muscle
Posterior rectus sheath (above arcuate line)
• Transversalis fascia
• Internal oblique fascia
Internal oblique muscle
External oblique muscle
Anterior rectus sheath (above arcuate line)
• Internal oblique fascia
• External oblique fascia
Superficial fascia
• Camper fascia
• Scarpa fascia
Fascia lata
Superficial epigastric and circumflex iliac arteries
Femoral vessels
Intercrural fibers
Pectoralis major muscle
Serratus anterior muscles
Rectus abdominis muscles
Linea alba
Linea semilunaris
Tendinous inscriptions
Midaxillary line
External oblique muscle and aponeurosis
Iliac crest
Anterior superior iliac spine (ASIS)
Umbilicus
Arcuate line
Inguinal ligament
Pubic tubercle Pyramidalis muscle
Symphysis pubis
Pectoralis major muscle
Serratus anterior muscles
Midaxillary line
Iliac crest
Anterior superior iliac spine (ASIS)
Inguinal ligament
External oblique aponeurosis
External oblique muscle
Xiphoid process
Costal margin
Linea alba
Rectus abdominis muscles
Umbilicus
Tendinous inscriptions
Linea semilunaris
Arcuate line
Pubic tubercle
Fig. 1.1
Latissimus dorsi muscle
Fig. 1.2
Pearls and Pitfalls
s Scarpa fascia is usually a visible and durable structure and is closed separately during various surgeries on the abdominal wall to achieve an optimal scar result.
3. Deep Fascial Layers (see Figs. 1.1 and 1.2)
s The rectus sheath is found in the midline.
s Laterally, layers of the abdominal wall deep to superficial fascia include external oblique, internal oblique, transversus abdominis, and parietal peritoneum.
s The arcuate line (see Fig. 1.3) is located midway between the umbilicus and symphysis pubis and is a transition point where the posterior rectus sheath transitions from being the fusion of part of internal oblique fascia and transversalis fascia superiorly to only transversalis fascia inferiorly.
s Above the arcuate line, the anterior rectus sheath consists of external oblique fascia and part of internal oblique fascia. The posterior rectus sheath consists of internal oblique fascia and transversalis fascia. The anterior and posterior layers of the rectus fascia invest the rectus abdominis muscles.
s Below the arcuate line, the external oblique and internal oblique fasciae merge to form the anterior rectus sheath. The posterior rectus sheath consists of transversus abdominis fascia, making this only a thin layer with minimal strength.
Tendinous inscriptions
Linea semilunaris
Linea alba
Fig. 1.4
External oblique fascia release
Fig. 1.5
Fig. 1.6
s Zone III comprises the lateral abdominal wall (flank region) and is supplied by the musculophrenic, lower intercostals (Fig. 1.8A), and lumbar arteries (Fig. 1.8B).
Vascular Supply
s Knowledge of these zones of blood supply to the anterior abdominal wall is important when planning incisions for surgical procedures. A previous subcostal incision can compromise the circulation to Huger’s zone III of the abdominal wall. In transverse rectus abdominis myocutaneous flap harvest, the presence of a subcostal scar was found to increase donor site complications, with a significantly higher incidence of abdominal wall skin necrosis (25%) compared with patients without abdominal wall scars (5%).
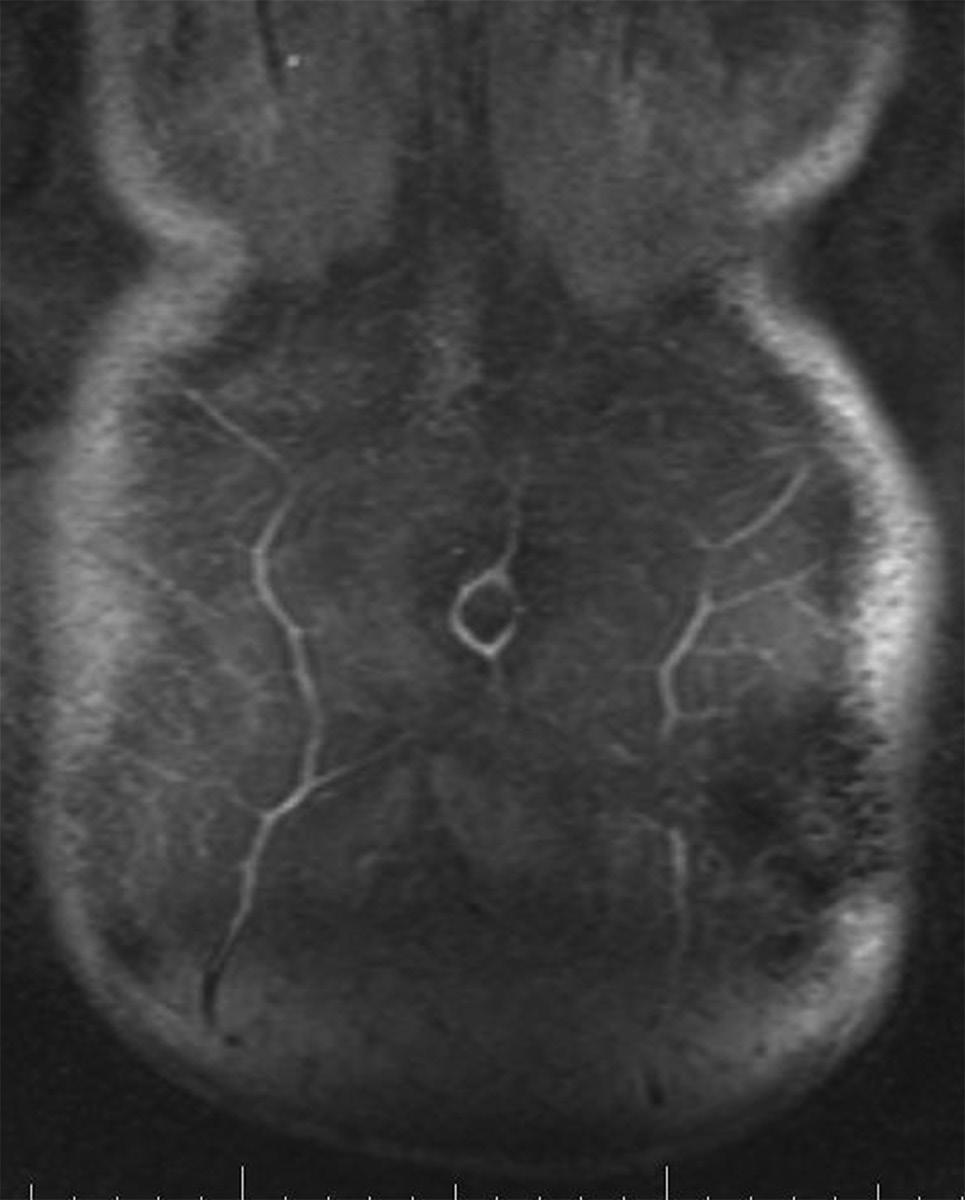
s The superior epigastric artery (SEA) and deep inferior epigastric artery (DIEA) lie on the posterior aspect of the rectus abdominis muscles and supply the muscle and overlying skin and subcutaneous tissue through musculocutaneous perforators (Fig. 1.9).
s A study by Saber et al. (2004) provided guidelines for location of the epigastric vessels based on computed tomography scan data in 100 patients. At the xiphoid process, the SEA was 4.41 ± 0.13 cm from the midline on the right and 4.53 ± 0.14 cm from the midline on the left. Midway between the xiphoid and umbilicus, the SEA was 5.50 ± 0.16 cm from the midline on the right and 5.36 ± 0.16 cm from the midline on the left. At the umbilicus, the epigastric vessels were 5.88 ± 0.14 cm from the midline on the right and 5.55 ± 0.13 from the midline on the left. Midway between the umbilicus and symphysis pubis, the inferior epigastric artery was 5.32 ± 0.12 cm from the midline on the right and 5.25 ± 0.11 cm from the midline on the left. At the symphysis pubis, the inferior epigastric artery was 7.47 ± 0.10 cm from the midline on the right and 7.49 ± 0.09 cm from the midline on the left.
s The DIEA is dominant in the vascular supply of the abdominal muscles compared with the SEA. The two arborizing vascular systems converge within the rectus abdominis muscle at a point between the xiphoid process and umbilicus. In a study by Taylor (2003), the mean diameter of the DIEA at its point of origin was 3.4 mm compared with 1.6 mm for the SEA, perhaps explaining the dominant arterial supply of the DIEA.
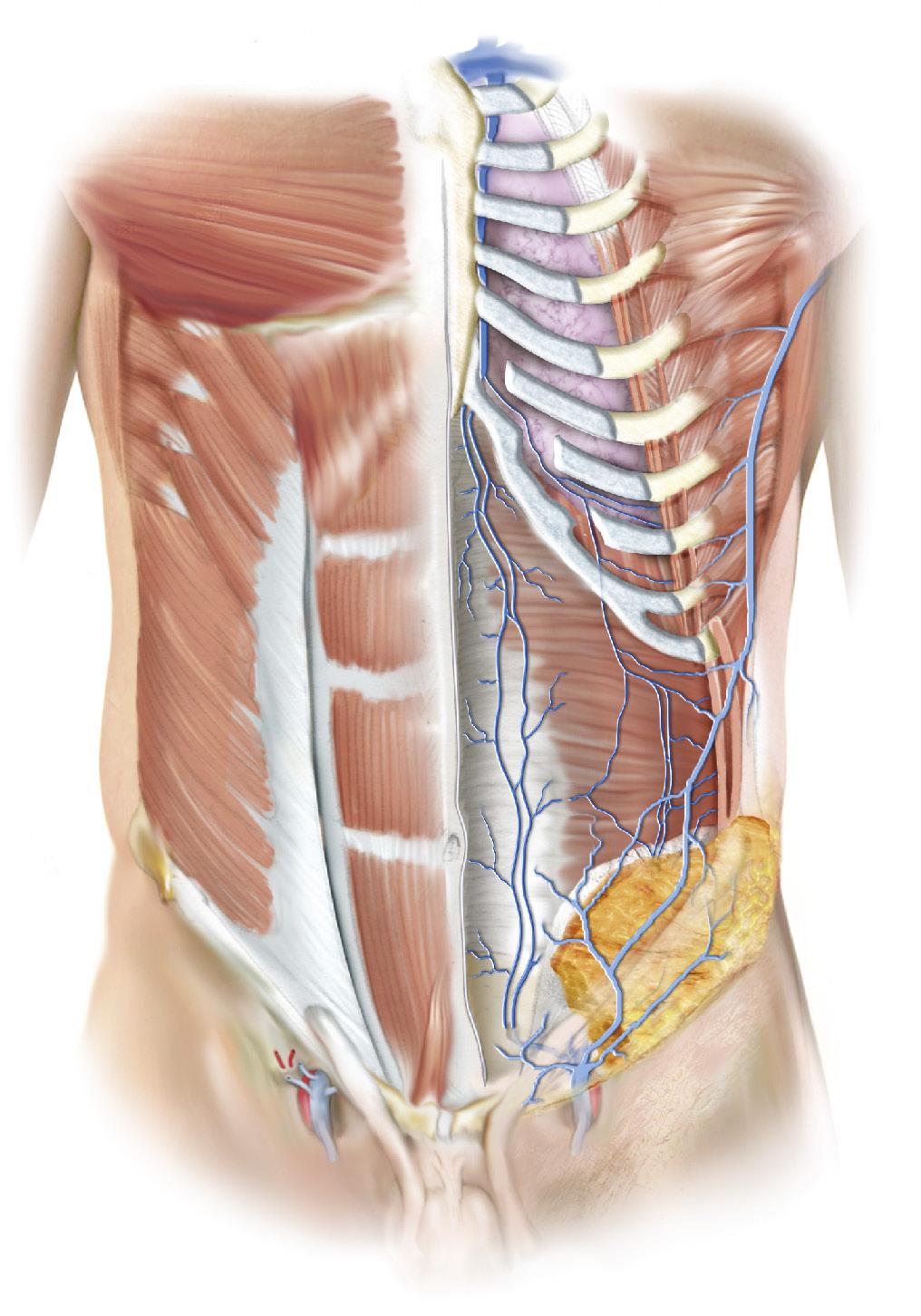
Left subclavian vein
Internal thoracic (mammary) artery
Musculophrenic vein
Superior epigastric veins
Thoracoepigastric vein
Overlying semilunaris
Lower intercostal veins
Transversus abdominis muscle
Lumbar veins
External oblique muscle (removed)
Internal oblique muscle (removed)
Deep circumflex iliac vein tributaries
Scarpa’s fascia
Camper’s fascia
Thoracoepigastric vein
Inferior epigastric veins
Inguinal ligament
Superficial circumflex veins
Superficial epigastric veins
External iliac vein
Femoral vein
Fig. 1.11
Fig. 1.10
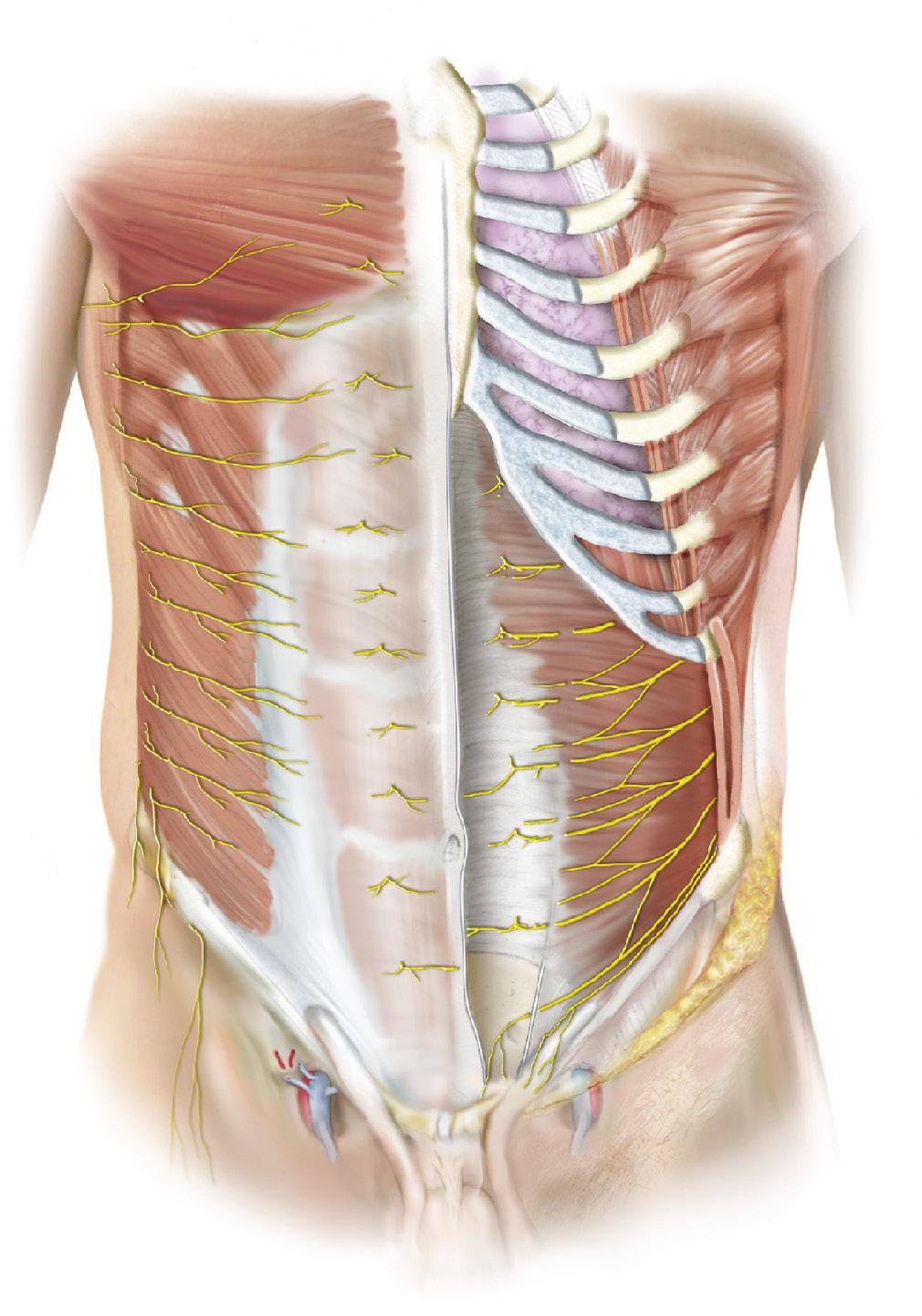
Ventral rami of intercostal nerves T2–11
Lateral cutaneous branches of intercostal nerves T2–11
Lateral cutaneous branch of subcostal nerve T12
Lateral cutaneous branch of iliohypogastric nerve L1
Lateral femoral cutaneous nerve
Ventral rami of subcostal nerve T12
Posterior layer of rectus sheath
Transversus abdominis muscle
Internal oblique muscle
External oblique muscle
Anterior branch of subcostal nerves T12
Iliohypogastric nerve L1
Ilioinguinal nerve L1
Overlying semilunaris
Fig. 1.13
Fig. 1.12