1 SynopsisofAdultCardiac SurgicalDisease
Itisessentialthatallindividualsinvolvedintheassessmentandmanagementofpatients withcardiacsurgicaldiseasehaveabasicunderstandingofthediseaseprocessesthatare beingtreated.Thischapterpresentsthespectrumofadultcardiacsurgicaldiseasethatis encounteredinmostcardiacsurgicalpractices.Thepathophysiology,indicationsfor surgery,specificpreoperativeconsiderations,andsurgicaloptionsforvariousdiseasesare presented.Diagnostictechniquesandgeneralpreoperativeconsiderationsarepresentedin thenexttwochapters.Issuesrelatedtocardiacanesthesiaandpostoperativecarespecificto mostofthesurgicalprocedurespresentedinthischapterarediscussedinChapters4and8, respectively.Themostcurrentguidelinesfortheevaluationandmanagementofpatients withcardiacdiseasecanbeobtainedfromtheAmericanCollegeofCardiologywebsite (www.acc.org).
I.CoronaryArteryDisease
A Pathophysiology.Coronaryarterydisease(CAD)resultsfromprogressiveblockageof thecoronaryarteriesbyatherothromboticdisease.Significantriskfactorsinclude hypertension,dyslipidemia(especiallyhighLDLandlowHDLlevels),diabetes mellitus,cigarettesmoking,andobesity.Clinicalsyndromesresultfromanimbalance ofoxygensupplyanddemandresultingininadequatemyocardialperfusiontomeet metabolicdemand(ischemia).Progressivecompromiseinluminaldiameterproducing supply/demandimbalanceusuallyproducesapatternofchronicstableangina.Plaque rupturewithsuperimposedthrombosisisresponsibleformostacutecoronarysyndromes (ACS),whichincludeclassic“unstableangina”,non-ST-elevationmyocardialinfarctions(NSTEMI),andST-elevationinfarctions(STEMI).Interestingly,plaquerupture commonlyoccursincoronarysegmentsthatarenotseverelystenotic.Endothelial dysfunctionhasbecomeincreasinglyrecognizedasacontributingfactortoworsening ischemicsyndromes.Generalizedsystemicinflammation,indicatedbyelevated C-reactiveproteinlevels,isusuallynotedinpatientswithACS,andappearstobe associatedwithadverseoutcomes.1
B Managementstrategies
1.Symptomaticcoronarydiseaseisinitiallytreatedwithmedicaltherapy,including aspirin,nitrates,and b-adrenergicblockers.Calciumchannelblockers(CCBs)are consideredif b-blockersarecontraindicated.Statinsshouldbegiventocontrol dyslipidemiasandareeffectiveforplaquestabilization.Angiotensin-converting
enzyme(ACE)inhibitorsareusedforcontrolofhypertension,especiallyinpatients withcompromisedleftventricularfunction.Clopidogrelgenerallydoesnotprovide benefittopatientswithchronicstableangina,exceptinselectedsubsets,butis beneficialinpatientswithanACS.2–6
2.STEMIsarepreferentiallytreatedbypercutaneouscoronaryintervention(PCI) (angioplastyandstenting),althoughthrombolytictherapymaybeconsideredwhen PCIcannotbeperformedwithinafewhours.Clinicalbenefitistime-related(“timeis myocardium”),andthebestresultsareobtainedwith“doortoballoon”timeslessthan 90minutes.However,myocardialsalvagemaystilloccurifreperfusioncanbe accomplishedwithin6hoursoftheonsetofchestpain.7,8
3.PatientspresentingwithanACSshouldbetreatedwithaspirinandunfractionatedor low-molecular-weightheparin(LMWH),aswellasthestandardtherapylisted above(nitrates, b-blockers,statins).9,10 Clopidogrelmayprovideclinicalbenefitto thesepatientsiftheyaretobetreatedmedically,anditmaybegivenifanearly invasivestrategyisproposed.The2007ACC/AHArecommendationswerethatit shouldnotbegivenifurgentsurgeryisconsideredlikely,butthiscanbedifficultto predictandthereforeitisgivenroutinely.Moststudieshaveshownthat30-day outcomesarebetterinpatientsundergoingcoronaryarterybypassgraft(CABG) surgerywhoinitiallyreceivedclopidogrel.2–6 However,onestudyshowedthatthere wasnodifferenceinoutcomeswhetherclopidogrelwasgivenornotifpatientshad surgerywithin5days,butoutcomewasbetterifitwasinitiallygivenonpresentation, thenstoppedforatleast5daysbeforesurgery.11 ThisstudysupportstheACC/AHA recommendationthatclopidogrelbestoppedatleast5daysbeforesurgeryexceptin urgentoremergentsituations.9 IfprasugrelisgiveninanticipationofPCI,but CABGisrecommendedinstead,itshouldbestoppedatleast7dayspriortosurgery.
4.Inpatientswithcontinuingischemiaandhigh-riskfeatures(crescendoanginaover 48hours,restpain,ECGchangesatrest,congestiveheartfailure[CHF],hemodynamicinstability,oranelevatedtroponinlevel),plateletglycoproteinIIb/IIIa inhibitors,suchastirofibanoreptifibatide,maybeaddedtotheregimenwithplans toproceedtoanearlyinvasivestrategyofcatheterization.Atthattime,the appropriatemeansofintervention(PCIvs.CABG)canbedetermined.IfaIIb/ IIIainhibitorisusedandaclopidogrelloadisnotgivenpriortoPCI,itwillprovide antiplateletactivityuntiltheinitialdosingofclopidogrelachievesadequateplatelet inhibition(afewhoursaftera600mgload).Numeroustrialsareevaluatingtheroleof variousplateletinhibitorsandtheuseofbivalirudinratherthanheparinduringPCI.
C. Selectionofaninterventionalprocedure
1.Anassessmentofthepatient’sclinicalpresentation,theextentandnatureofcoronary disease,degreeofinducibleischemiaonstresstesting,andstatusofventricular functionaretakenintoconsiderationwhendeterminingwhetherthepatientisan appropriatecandidateforaninterventionalprocedure.12 Inpatientswithconvincing evidenceofanACS,stresstestsarenotindicatedpriortocardiaccatheterization.The primaryobjectiveofanyinterventionisthereliefofischemiatopreventorminimize theextentofmyocardialdamage.
2.PCIhasseenwideapplicabilitybeyonditsprovenbenefitinearlyrandomizedtrials, whichgenerallyhadveryselectiveinclusioncriteria.Itisoftenpreferabletosurgeryin patientspresentingwithSTEMIsorwithongoingischemiawithNSTEMIsbecause
itcanmorepromptlysalvagemyocardium–unlesstheanatomyissuchthatCABGis preferable(seebelow).ThebenefitsofPCIinpatientswithchronicstableanginaare notaswelldefined.13,14
3.TheindicationsforPCIinmultivesseldiseasearecontroversial.Althoughseveral studiessuggestthatCABGimproveslong-termsurvivalbetterthanPCI,othertrials indicatethatsurvivaliscomparable,althoughmorepatientsundergoingPCIrequire reintervention.15–20 TherationaleisthatPCIonlyaddressesfocallesionsdespite CADbeingamultifocaldisease,whereasCABGbypassestheentireproximal segment.Thus,repeatintervention,usuallyinsitesotherthantheoriginalstent location,ismuchmorelikelyifPCIisutilized.Evidence-basedguidelineshavebeen establishedbymajororganizationstoidentifywhenPCIand/orCABGisindicated (Figures1.1and1.2).12 Theseguidelineswillcontinuetoevolvewhentheresultsof additionaltrialsincludingmultivesselandleftmaindisease,21–23 reoperativesituations,varyingpatientsubpopulations,andnewerstenttechnologiesbecomeavailable. OneapproachtodecisionmakingisuseoftheSYNTAXscore(accessibleatwww. syntaxscore.com),whichassessestheextentandnatureofcoronaryarterydisease andprovidescomparativemajoradversecardiacevent(MACE)ratesforPCIand CABGformultivesselaswellasleftmaindisease.23–25 Useofsuchdatacanprovide patientswithadequateevidence-basedclinicalinformationtogiveinformedconsent foranyinterventionalprocedure.
4.Althoughdrug-elutingstents(DES)areassociatedwithalowerriskofrestenosis thanbare-metalstents(BMS),moststudieshavenotshownasignificantimpacton theriskofmyocardialinfarctionordeath.26 Infact,theriskofstentthrombosisis greaterwithDES,andthisisaccentuatedinpatientswhoareresistanttothe antiplateleteffectsofaspirinand/orclopidogrel.27 Plateletfunctiontestingmaybe beneficialindeterminingwhichpatientsareresistanttotheirantiplateleteffects.To minimizetheriskofstentthrombosis,itisrecommendedthatpatientsreceiving BMStakeaspirinandclopidogrelforatleast1month,andthosereceivingDEStake thesemedicationsforatleast1year.28
5.OneshouldnotconsidereitherPCIorCABGanexclusiveapproachtoapatient’s coronaryarterydisease.Forexample,onehybridapproachistoperformaPCIofthe culpritlesioninanunstablepatientintheinterestofmyocardialsalvageandthenrefer thepatientforsurgicalrevascularizationofotherlesions.29 Ithasevenbeenproposed thatplacingaleftinternalthoracicartery(LITA)totheleftanteriordescending artery(LAD)inapatientwiththree-vesseldiseaseprovidestheessentiallong-term benefitofaCABGandconvertsthepatient’sanatomytotwo-vesseldiseasewhich canbemanagedmedicallyorwithPCI.30
D. Indicationsforsurgery.Thejustificationforproceedingwithaninterventionisbased primarilyuponanassessmentofwhetherthepatientisatincreasedriskforanadverse cardiacevent.Studieshaveshownthatsurgeryisveryeffectiveinrelievingangina,in manycasesisabletodelayinfarction,andinmostcasescanimprovesurvivalcompared withcontinuedmedicalmanagement.CABGcanbedeemedappropriatebasedonan assessmentofthepatient’ssymptomstatus,non-invasiveimagingstudies,andthe degreeofanatomicdisease(Figure1.1).12 ItshouldbeconsideredwhenPCIisnot feasibleorwhentheshort-andlong-termbenefitsofCABGaresuperiortothoseof PCI(Figure1.2).
Two vessel coronary artery disease with proximal LAD stenosis
Three vessel coronary artery disease
Isolated left main stenosis
Laft main stenosis and additional coronary artery disease
Figure1.2 . Recommendedmethodofrevascularizationbasedonextentofcoronarydisease. A,appropriate;U,uncertain;I,inappropriate.(ReproducedwithpermissionfromSmith, Ann ThoracSurg 2009;87:1328–31.)19
1. Clinicalscenarios.Thepatientwithrefractoryanginaoralargeamountof myocardiuminischemicjeopardyhasanindicationforaninterventionrelatively independentoftheextentofcoronaryinvolvement:
a.ClassIII–IVchronicstableanginarefractorytomedicaltherapy
b.Acutecoronarysyndromes,includingunstableanginaandNSTEMIs
c.AcuteischemiaorhemodynamicinstabilityfollowingattemptedPCI,whichmay includedissectionandcompromisedfloworcoronaryperforationwithtamponade
d.AcuteevolvingSTEMIwithin4–6hoursoftheonsetofchestpainorlaterif thereisevidenceofongoingischemia(earlypostinfarctionischemia)
e.Markedlypositivestresstestpriortomajorintra-abdominalorvascularsurgery–butnotnecessarilyifthepatienthaschronicstableangina
f.Ischemicpulmonaryedema
2. Anatomy.Asecondgroupofpatientsincludesthosewithoutdisablinganginaor refractoryischemiainwhomtheextentofcoronarydisease,thestatusofventricular function,andthedegreeofinducibleischemiaonstresstestingaresuchthatsurgery mayimprovelong-termsurvival.Thisispresumedtooccurbypreventinginfarction andpreservingventricularfunction.Surgeryisespeciallybeneficialforpatientswith impairedventricularfunctionandinducibleischemia,inwhomthemedicalprognosis isunfavorable.Thefollowingrecommendationsforsurgery,basedontherandomizedcontrolledtrialsofprimarilychronicstableanginaintheearly1980’shavebeen incorporatedintothe2009appropriatenesscriteriaguidelinesnotedinFigure1.2. ForpatientswithACS,theyareallclassIindicationsforsurgery,andforpatients
Figure1.1 . Appropriatenessratingsforcoronaryarterybypassgrafting.Thegridincorporates CanadianCardiovascularSociety(CCS)class,extentofcoronarydisease,andresultsofnoninvasivetestingindeterminingwhetherCABGisanappropriateprocedure.A,appropriate; U,uncertain;I,inappropriate.(ReproducedwithpermissionfromPateletal., JAmCollCardiol 2009;53:530–53.)12
withfewersymptomsormoderatedegreesofischemia,theyareclassIIaandIIb indications(seeAppendix1).
a.Leftmainstenosis >50%
b.Three-vesseldiseasewithejectionfraction(EF) <50%
c.Three-vesseldiseasewithEF >50%andsignificantinducibleischemiaonstress testing
d.Two-vesseldiseasewithinvolvementofproximalLADandEF <50%or significantinducibleischemiaonstresstesting
e.One-andtwo-vesseldiseasenotinvolvingtheLADwithextensivemyocardium injeopardybutlesionsnotamenabletoPCI
Althoughsurgeryisappropriateinthesepatients,mostpatientswithone-ortwo-vessel diseasearepreferentiallytreatedbyPCI.Furthermore,althoughthe2009guidelines considerPCIforleftmaindiseasetobe‘‘inappropriate’’andforthree-vesseldiseasetobe ‘‘uncertain’’,useoftheSYNTAXscore,theMayoClinicriskscore,andotherrisk modelsforPCImaymodifythisapproach.23–25
3 Otherconditions.Athirdgroupofpatientsshouldundergobypasssurgeryfor coronarystenosesexceeding50%whenotheropen-heartproceduresareindicated:
a.Valveoperations,septalmyectomy,etc.
b.Surgeryforpostinfarctionmechanicaldefects(leftventricularaneurysm,ventricularseptalrupture,acutemitralregurgitation)
c.Coronaryarteryanomalieswithriskofsuddendeath(vesselpassingbetweenthe aortaandpulmonaryartery)
E. Preoperativeconsiderations
1.Preoperativeautologousblooddonationhasbeenconsideredtoreducetherequirementforhomologoustransfusion.Thismaybefeasibleinpatientswithchronicstable angina,butnotinthosewithacutecoronarysyndromesorleftmaindisease.Withthe increasingsafetyofblood,theuseofantifibrinolyticdrugs,andtheperformanceof off-pumpsurgery,thisisnolongeracommonpractice.31
2. Anemia.Preoperativebloodtransfusionsshouldbeconsideredinpatientswithan ACSandahematocrit <28%.Thismaynotonlyimprovetheischemicsyndromebut willminimizehemodilutionduringsurgery.Lowpreoperativehematocritsmay increaseoperativemortalityfollowingCABG,oftenbecauseofanassociationwith otheradverseriskfactorsformortality,anditisnotknownwhethertransfusionscan reducethatrisk.32 Certainly,indiscriminateuseoftransfusionsmustbeavoided becauseoftheirassociationwithadverseoutcomesfollowingcardiacsurgery.33–35
a.Inadditiontobloodwithdrawalforpreoperativelabtests,itisnotuncommonfor thehematocrittofallseveralpointsafteracardiaccatheterizationfrombothblood lossandhemodilutionwithhydration.Onestudyshowedthatcoronaryangiographywasassociatedwithafallinhemoglobinof1.8g/dL(equivalenttoabouta 5.4%fallinhematocrit).36
b.Hemodilutiononcardiopulmonarybypass(CPB)toahematocrit <20%maybe associatedwithanincreasedriskofrenaldysfunction,stroke,opticneuropathy,and death.37–40 Lowhematocritsloweroncoticpressureandviscosity,increasefluid requirements,whichcontributestoextracellularedema,andmakeitmoredifficult tomaintainanadequatebloodpressureduringandafterCPB.Patientswith
profoundanemiatendtobleedandrequiremorebloodcomponenttransfusions. Thus,preoperativetransfusionstoanadequatelevelmaybeconsideredtoreduce patientmorbidity,possiblyreducetheoverallnumberoftransfusionsrequired intra-andpostoperatively,andpotentiallydecreasemortality.
3. Ischemia.Aggressivemanagementofongoingorpotentialischemiaisindicatedin patientswithcriticalcoronarydiseasetoreducesurgicalrisk.Thismayinclude adequatesedationandanalgesia,antiischemicmedicationstocontrolheartrateand bloodpressure(intravenousnitratesand b-blockers),antiplateletandanticoagulant medications(aspirin,clopidogrel,heparin,IIb/IIIainhibitors),and/orplacementof anintra-aorticballoonpump(IABP)forrefractoryischemia.Itcannotbeoveremphasizedthatjustbecauseapatienthasbeencatheterizedandacceptedforsurgery doesnotmeanthatmedicalcareshouldnotbeaggressiveuptothetimeofsurgery!If thepatienthaspersistentischemiadespiteallofthesemeasures,emergencysurgeryis mandatory.
a.Allantianginalmedicationsshouldbecontinueduptoandincludingthemorning ofsurgery.Studieshavedemonstratedthebenefitofpreoperative b-blocker therapyinloweringperioperativemortalityincardiacsurgerypatients.41 Patients beingadmittedthemorningofsurgeryshouldberemindedtotaketheir medicationsbeforecomingtothehospital.
b. Unfractionatedheparin (UFH)isoftenusedinpatientswithacutecoronary syndromes,leftmaincoronarydisease,orapreoperativeIABP.Theheparin shouldgenerallybecontinueduptothetimeofsurgery.Centrallinescanusually beplacedsafelywhilethepatientisheparinized.Patientsreceivingheparinshould havetheirplateletcountrecheckeddailytobevigilantforthedevelopmentof heparin-inducedthrombocytopenia(HIT).Notethatpreoperativeassessment forHITantibodiesisnotindicatedintheabsenceofaclinicalindication.42
c. Low-molecular-weightheparin (LMWH)isoftenusedinpatientspresenting withanACSandmaybeusedinthecathlabaswell.Itmustbestoppedatleast 18–24hourspriortosurgerytominimizetheriskofperioperativebleeding. Fondaparinux,oftenusedroutinelyforvenousthromboembolismprophylaxis, hasahalf-lifeof17–21hoursandmustbestoppedatleast48hourspriorto surgery.
d Aspirin isroutinelyusedinpatientswithknowncoronarydiseaseorgivenupon presentationtothehospital.Plateletfunctiongenerallyreturnstonormalwithin 3daysofcessationofaspirin,soitcanbestoppedatthattimefortrulyelective cases.43,44 Otherwise,aspirin81mgshouldbecontinueduptothetimeofsurgery inpatientswithanACSorcriticalcoronarydisease,sinceitmayimprove outcomeswithoutasignificantincreaseintheriskofbleeding.44–47
e.Preoperativeuseof clopidogrel hasgenerallybeenshowntosignificantlyincrease theriskofbleedingandreexplorationforbleeding.5,44,47,48 Thus,ithasbeen recommendedthatitshouldbestopped5–7daysbeforeelectivesurgery,although stoppingitforonly3daysmaybeacceptablepriortooff-pumpsurgery.49 Prasugrel isamorepotentADPinhibitorthatcanachieve80%plateletinhibitionwithin30 minutesofadministration.Becauseofitseffectivenessandcomparablehalf-lifeto clopidogrel,itmaycontributetoanevengreaterriskofperioperativebleedingand shouldbestoppedatleast7dayspriortosurgery,ifpossible.
i.Aloadingdoseofclopidogrel(300–600mg)isfrequentlygiventopatients presentingwithanACSintheemergencyroomorinpreparationforaPCI. Alternatively,aloadingdoseofprasugrel(60mg)maybegiveninthecathlab. IfPCIisnotfeasibleorfails,thepatientwillthenbeathigherriskfor bleedingfollowingCABG.
ii.Insomecases,emergencystentingofaculpritlesioncausinganevolving infarctionmaybeperformedwithsubsequentreferralforurgentsurgeryto achievecompleterevascularization.Inthissituation,itispreferabletousea IIb/IIIainhibitortominimizestentthrombosisasabridgetosurgery.It shouldbestopped4hourspriortosurgery,sothatbythetimesurgerystarts, 80%ofplateletactivitywillhaverecovered.
iii.Inpatientswithpriorstenting(<1monthforaBMSand <1yearforaDES), thereisanincreasedriskofstentthrombosisifclopidogrelisstopped.28 Either surgerymustbeperformedwiththepatientstilltakingclopidogrelorone mightpossiblystoptheclopidogrelforonly3daystohavesomeresidual protectiveantiplateletactivity,yethopefullylessintraoperativebleeding.
4.Otherpreoperativemedicationstobeconsidered
a. Amiodarone isbeneficialinreducingtheincidenceofpostoperativeatrial fibrillation(AF).Onerespectedrandomizedtrialshowedabenefittogiving 10mg/kgdailystarting6dayspriortosurgery,althoughashortercoursemaybe justaseffective.50
b Statins havebeendemonstratedtoreduceoperativemortality,theriskofstroke, andtheoccurrenceofAFwhenusedinhighdoses(atorvastatin40mg).51–53
c Steroids havebeenevaluatedasameansofreducingthesystemicinflammatory responseofsurgeryandhavebeenshowntoimprovemyocardialfunctionand possiblyreducetheincidenceofAF.54–57 However,improvementinpulmonary functionhasnotbeenclearlyshown,andsteroidsdoworsenpostoperative hyperglycemia.Sincethebenefitsarecontroversial,steroidshavenotseen widespreadusage.
F. Surgicalprocedures
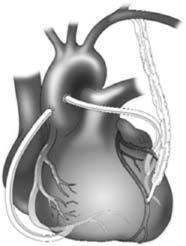
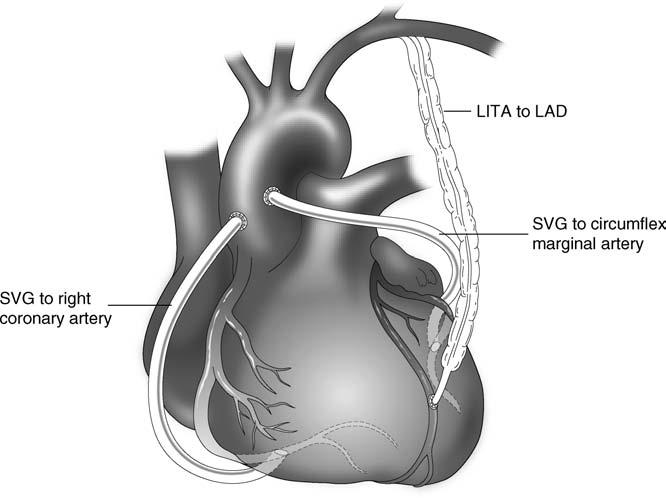
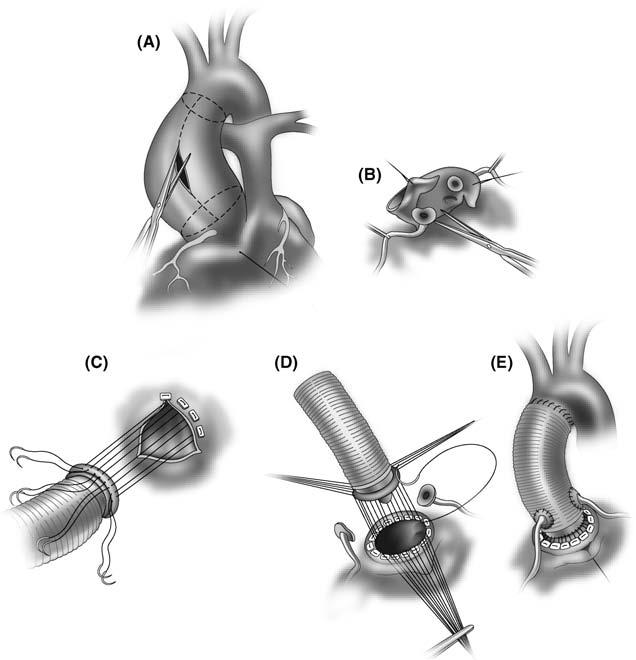
1 Traditionalcoronaryarterybypassgrafting isperformedthroughamedian sternotomyincisionwithuseofCPB.Myocardialpreservationisusuallyprovided bycardioplegicarrest.Theprocedureinvolvesbypassingthecoronaryblockageswith avarietyofconduits.Theleftinternalthoracic(ormammary)artery(ITA)isusually usedasapedicledgrafttotheLADandissupplementedbyeitherasecondITAgraft orradialarterygrafttotheleftsystemand/orsaphenousveingraftsinterposed betweentheaortaandthecoronaryarteries(Figure1.3).
a.Thesaphenousveinshouldbeharvestedendoscopicallytominimizepatient discomfort,reducetheincidenceoflegedemaandwoundhealingproblems,and optimizecosmesis.58 Therearesomeconcernsthatendoscopicharvestingcould produceendothelialdamagethatmightcompromiselong-termpatencyand reducelong-termsurvival.59,60
b.Useofadditionalarterialconduits(bilateralITAs,radialartery)canberecommendedtoimproveevent-freesurvival,61–63 althoughonestudyofstatinuse showedcomparablesurvivalofpatientsreceivingoneortwoITAs.64 Theradial arterycanbeharvestedendoscopicallyusingatourniquettominimizebleeding
Figure1.3 . Coronaryarterybypassgrafting.Aleftinternalthoracicartery(LITA)hasbeen placedtotheleftanteriordescendingartery(LAD)withaortocoronarysaphenousveingrafts (SVG)tothecircumflexmarginalandrightcoronaryarteries.
duringtheharvestwithplacementofadrainafterwardstopreventblood accumulationwithinthetract.65–67 Withradialarterygrafting,avasodilatoris initiatedduringsurgerytominimizespasm(eitherIVdiltiazem0.1mg/kg/h (usually5–10mg/h)orIVnitroglycerin10–20 mg/min(0.1–0.2 mg/kg/min).68 ThisiscontinuedintheICUandthenconvertedtoeitheramlodipine5mgpoqd orImdur20mgpoqdforseveralmonths.Thebenefitofsuchpharmacologic managementtopreventspasmhasbeenuniversallyaccepted,butnotproven.
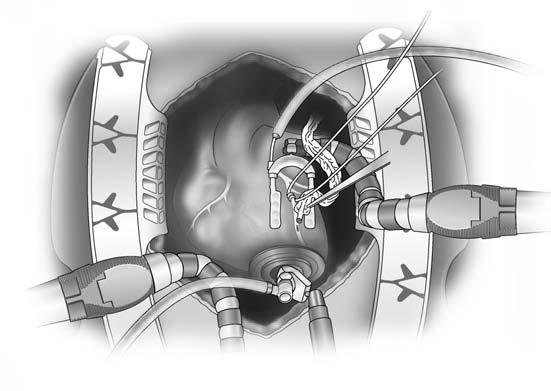
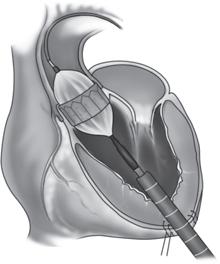
2.ConcernsabouttheadverseeffectsofCPBspurredthedevelopmentof “off-pump” coronarysurgery(OPCAB),duringwhichcompleterevascularizationshouldbe achievedwiththeavoidanceofCPB.Deeppericardialsuturesandvariousretraction devicesareusedtopositiontheheartforgraftingwithouthemodynamiccompromise. Astabilizingplatformminimizesmovementatthesiteofthearteriotomy (Figure1.4).Intracoronaryoraortocoronaryshuntingcanminimizeischemiaafter anarteriotomyisperformed.69
a.Conversiontoon-pumpsurgerymaybenecessaryinthefollowingcircumstances:
i.Coronaryarteriesareverysmall,severelydiseasedorintramyocardial.
ii.LVfunctionisverypoor,orthereisseverecardiomegalyorhypertrophythat precludesadequatecardiactranslocationwithouthemodynamiccompromise orarrhythmias.
iii.Theheartisextremelysmallandverticalinorientation.
Figure1.4 . Off-pumpbypassgraftingrequiresdisplacementoftheheartusingtechniquesto avoidhemodynamiccompromise.Thesemayincludeplacementandelevationofdeeppericardialsuturesortheuseofanapicalsuctiondevice.Astabilizingdeviceisusedtominimize motionandaproximalvesselloopisplacedtominimizebleedingatthesiteoftheanastomosis.
iv.Uncontrollableischemiaorarrhythmiasdevelopwithvesselocclusionthat persistsdespitedistalshunting.
v.Intractablebleedingoccursthatcannotbecontrolledwithvesselloopsoran intracoronaryshunt.
b.OPCABsreducetransfusionrequirements,andarguablylowermortalityand reducetheriskofstroke,renaldysfunction,andatrialfibrillation.70–73 Despite thesepotentialadvantages,enthusiasmforthistechniqueismodest,anditis estimatedthatfewerthan20%ofCABGsareperformedoff-pump.Many surgeonsreserveitsuseforpatientswithlimiteddisease.Itsmajoradvantage maybeintheveryhigh-riskpatientwithmultiplecomorbiditiesinwhomitis criticaltoavoidCPB.
c.Insomepatientswithsevereventriculardysfunction,theheartwillnottoleratethe manipulationrequiredduringoff-pumpsurgery.Inthiscircumstance,right ventricularassistdevicescanbeusedtoimprovehemodynamics.Alternatively, surgerycanbedoneon-pumponanemptybeatinghearttoavoidtheperiodof cardioplegicarrest.Thistechniquemaybebeneficialinpatientswithascending aorticdiseasethatpreventssafeaorticcross-clamping,butdoesallowforsafe cannulationanduseofaorticpunches,suchastheHEARTSTRINGproximal sealsystem(MaquetCardiovascular),toperformtheproximalanastomoses.
3. Minimallyinvasivedirectcoronaryarterybypass(MIDCAB) involvesbypassing theLADwiththeLITAwithoutuseofCPBviaashortleftanteriorthoracotomy incision.74 Anadditionalincisionintherightchestcanbeusedtobypasstheright coronaryartery.CombiningaLITAtotheLADwithstentingofothervessels (“hybrid”procedure)hasalsobeendescribed.29,30
4
Robotic or totallyendoscopiccoronaryarterybypass(TECAB) canbeusedto minimizetheextentofthesurgicalincisionsandreducetraumatothepatient. RoboticscanbeusedforbothITAtakedownandgraftingtoselectedvesselsthrough smallports.TheseprocedurescanbedonewithoutCPBorusingCPBwithfemoral cannulation.Generally,TECABisusedforlimitedgrafting,butwiderapplicability iscertainlyfeasible.75
5. Transmyocardialrevascularization(TMR) isatechniqueinwhichlaserchannels aredrilledintheheartwithCO2 orholmium-YAGlaserstoimprovemyocardial perfusion.Althoughthechannelsoccludewithinafewdays,theinflammatoryreactioncreatedinducesneoangiogenesisthatmaybeassociatedwithupregulationof variousgrowthfactors,suchasvascularendothelialgrowthfactor.Thisprocedurecan beusedasasoleprocedureperformedthroughaleftthoracotomyforpatientswith inoperableCADinregionsofviablemyocardium.Alternatively,itcanbeusedasan adjuncttoCABGinviableregionsoftheheartwherebypassgraftscannotbeplaced.76
II.LeftVentricularAneurysm
A. Pathophysiology.Occlusionofamajorcoronaryarterymayproduceextensivetransmuralnecrosiswhichconvertsmuscleintothinscartissue.Thisresultsinformationofa leftventricularaneurysm(LVA)whichexhibitsdyskinesiaduringventricularsystole.In contrast,earlyreperfusionofanoccludedvesselmaylimittheextentofmyocardial damagewithpreservationofepicardialviability,resultinginanareaofakinesia.This willresultinanischemiccardiomyopathywithadilatedventriclethatremodelswith alteredsphericalgeometrybutdoesnotproduceananeurysm.
B Presentation.ThemostcommonpresentationofLVAsandischemiccardiomyopathiesisCHFduetosystolicdysfunction.WithLVAs,thereisareductionofstroke volumecausedbygeometricremodelingoftheaneurysmalsegmentduetolossof contractiletissueandanincreaseinventriculardimensions.Anginamayalsooccurdue totheincreasedsystolicwallstressofadilatedventricleandthepresenceofmultivessel CAD.Systemicthromboembolismmayresultfromthrombusformationwithinthe dyskineticorakineticsegment.Malignantventriculararrhythmiasorsuddendeathmay resultfromthedevelopmentofamacroreentrycircuitattheborderzonebetweenscar tissueandviablemyocardium.
C. Indicationsforsurgery.Surgeryisusuallynotindicatedforthepatientwithan asymptomaticaneurysmbecauseofitsfavorablenaturalhistory.Thisisincontrastto theunpredictableprognosisandabsoluteindicationforsurgeryinapatientwithafalse aneurysm,whichiscausedbyacontainedruptureoftheventricularmuscle.Surgerymay bebeneficialintheasymptomaticpatientwithanextremelylargeaneurysmorwhen extensiveclotformationispresentwithintheaneurysm.Surgeryismostcommonly indicatedtoimprovesymptomsandprolongsurvivalwhenoneofthefourclinical syndromesnotedabove(angina,CHF,embolization,orarrhythmias)ispresent. Arrhythmiasmaybetreatedbyanon-guidedendocardialresectionthroughthe aneurysmwith/withoutcryosurgeryalongwithsubsequentplacementofatransvenous implantablecardioverter-defibrillator(ICD).
D. Preoperativeconsiderations
1.Abiplaneleftventriculogramishelpfulinidentifyingregionsofakinesiaand dyskinesiaandassessingthefunctionofnoninfarctedsegments.Echocardiography
isbestforassessingventricularsizeanddimensions,wallmotionofthenoninfarcted segments,thepresenceofthrombus,andmitralvalvefunction,whichisoften abnormalwithdilatedcardiomyopathies.
2.Thepatientshouldbemaintainedonheparinuptothetimeofsurgeryifleft ventricularthrombusispresent.
E Surgicalprocedures
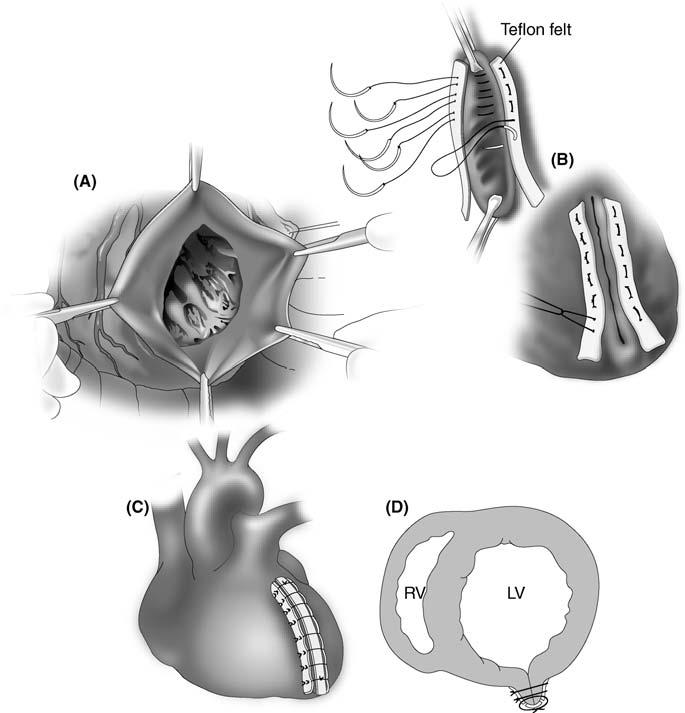
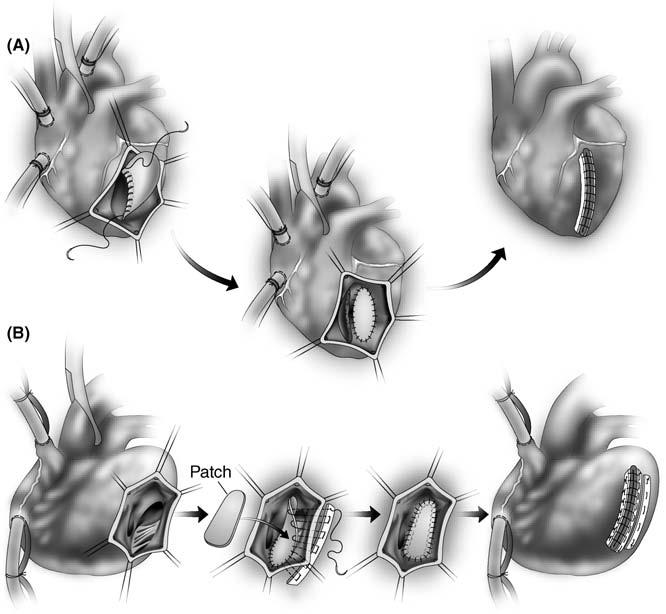
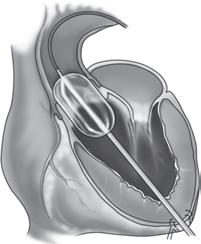
1.Standardaneurysmectomyentailsaventriculotomythroughtheaneurysm,resection oftheaneurysmwall,includingpartoftheseptumifinvolved,andlinearclosureover feltstrips(Figure1.5).77
Figure1.5 . Repairofaleftventricularaneurysmusingthelinearclosuretechnique.(A)The thinned-outscartissueisopenedandpartiallyresected.Anyleftventricularthrombusisremoved. (B)Theaneurysmisthenclosedwithmattresssuturesoverfeltstrips.(C)Anadditionalover-andoversutureisplacedoverathirdfeltstrip.(D)Cross-sectionofthefinalrepair.
2.Endoventricularreconstructiontechniquesareapplicabletolargeaneurysmsor akineticsegmentswiththeintentofreducingventricularvolumeandrestoringan ellipticalshape.
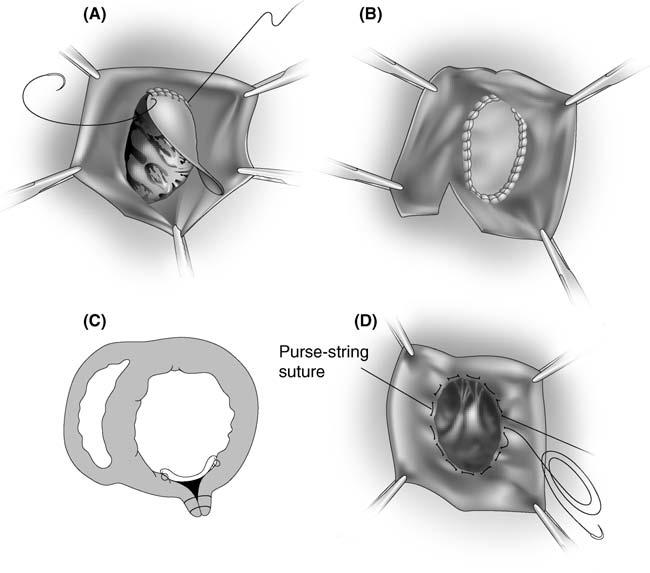
a.The“endoaneurysmorrhaphy”techniqueisusedforlargeaneurysms.ApericardialorDacronpatchissewntotheedgesofviablemyocardiumatthebaseofthe aneurysmandtheaneurysmwallisreapproximatedoverthepatch(Figure1.6). Thispreservesleftventriculargeometryandimprovesventricularfunctiontoa greaterdegreethanthelinearclosuremethod.
b.AslightlymoreelaborateendoventricularreconstructioninvolvestheendoventricularcircularpatchplastytechniqueofDor,whichistermed“surgical ventricularrestoration”(SVR).Thiscanbeappliedtoleftventricularaneurysms aswellascasesofischemiccardiomyopathywithanteriorakinesis (Figure1.6D).78,79 Theprocedureinvolvesplacementofanencirclingsuture atthejunctionofthecontractingandnoncontractingsegments,andthen
Figure1.6 . Repairofaleftventricularaneurysmusingtheendoaneurysmorrhaphytechnique. (A,B)Apericardialpatchissewnatthebaseofthedefectatthejunctionofscarandnormal myocardiumtobetterpreserveventriculargeometry.Theresectededgesoftheleftventricleare closedinasimilarfashiontothelineartechnique.(C)Cross-sectionofthefinalrepair.(D)TheDor procedureisamodificationofthistechniqueinwhichacircumferentialpursestringsutureis placedatthebaseofthedefecttorestoreanormalorientationtotheventricle.Apatchisthen sewnoverthedefect.
exclusionofthenoncontractingsegmentwithapatch.Thisproducesanelliptical contouroftheheartandresultsinsignificantimprovementinventricularsizeand function.Thisprocedureisgenerallydoneonabeatinghearttoallowforbetter differentiationofakineticandnormalsegmentsoftheheart.
c.AlthoughSVRisassociatedwithareductioninLVvolume,clinicalimprovementisnotuniform.SeveralstudieshavesuggestedthattheadditionofSVRtoa CABGimprovesclinicalstatusandlong-termsurvival.80,81 However,the STICHtrialofpatientswithCAD-relatedanteriorakinesiaordyskinesiawith EF <35%wasunabletodemonstratethatreductioninLVsizewasassociated withanimprovementinsymptomsorareductioninmortalityafter4years(see alsopage62).82
3.Coronarybypassgraftingofcriticallydiseasedvesselsshouldbeperformed.Bypass oftheLADanddiagonalarteriesshouldbeconsideredifseptalreperfusioncanbe accomplished.
4.Mitralvalverepairwithacompleteannuloplastyringisindicatedwhentheseverityofmitralregurgitation(MR)is2þ orgreater.MRisusuallyrelatedtoapical tetheringoftheleafletsduetoventriculardilatationormayresultfromannular dilatation.
. CorrelationofEchocardiographicMeasurementswiththe SeverityofAorticStenosis
.Atcatheterization,thedegreeofvalvestenosis(effectivevalvearea)isassessedbya measurementoftransvalvularflow(essentiallythecardiacoutputorstrokevolume) withacalculationofthepeakormeanpressuregradientacrossthevalve calculatedfrompressuresobtainedonacatheterpull-backfromtheleftventricle intotheaorta(Figure2.4,page97).AvalveareaiscalculatedusingtheGorlin formula: AVA ¼
where:
AVA ¼ aorticvalveareaincm2 (normal ¼ 2.5–3.5cm2)
CO ¼ cardiacoutputinmL/min
SEP ¼ systolicejectionperiod/beat
HR ¼ heartrate
Sincethepressuregradientisrelatedtoboththeorificeareaandthetransvalvular flow,lowgradientsmaybenotedinlowcardiacoutputstatesdespitesevereAS; conversely,highgradientsmaybenotedinhighoutputstatesintheabsenceof severeAS.Thisconceptmayaccountforapparentinconsistenciesinthedegreeof ASusingdifferentmeasurementsandindifferentclinicalstates.
3.Assessingtheseverityofaorticstenosisinapatientwithalowgradientandpoor ventricularfunctioncanbeproblematic.Apatientmayhaveacalculatedvalvearea consistentwithsevereAS,althoughthedegreeofASmaynotbesignificant. Dobutaminestressechocardiography(DSE)canbeusedinthiscircumstanceto determinewhetherpoorventricularfunctionwithalowstrokevolumeisprimarily relatedtoafterloadmismatchfromtruesevereASorisduetocontractile dysfunction.
a.Ifdobutamineproducesanincreaseinstrokevolumeandcardiacoutputwith littleincreaseingradient,thevalveareawillincrease,indicatingthattheseverity ofvalvestenosiswasoverestimatedandsurgeryisnotindicated.
b.Incontrast,ifdobutamineincreasesboththestrokevolumeandthegradient, thevalveareawillremainthesame,confirmingthattrueaorticstenosisis presentthatwillbenefitfromsurgery.
c.Ifdobutaminefailstoproduceanincreaseinstrokevolume,thepatienthaspoor contractilereserveandisapoorcandidateforsurgery.88,94,95 However,despitea highoperativemortality,patientswithpoorcontractilereserve(<20%increase instrokevolumewithDSE)stillhaveabetterlong-termprognosiswithsurgery thanwithmedicalmanagement.Inthesepatients,analternativeapproachto aorticvalvereplacement(AVR),suchasatranscathetervalvereplacement,may bepreferable.95
d.Interestingly,studieshavesuggestedthatanelevatedB-typenatriureticpeptide (BNP)level(>550)isaverystrongpredictorofoperativemortality,evenmore importantthancontractilereservedocumentedbyDSE.96
D. Indicationsforsurgery.Thegradingofindicationsforsurgeryandthelevelsof evidenceforalltypesofvalvesurgerylistedinthenextfewsections(seeAppendix1) arebasedon2008ACCguidelines88 andareavailableatwww.acc.org.
1.Thepresenceofsymptoms(angina,CHF,syncopeorresuscitationfromsudden death)withsevereASisaclassIindicationforsurgery,becauseoncesymptomsare present,theaveragesurvivalisonlyabout2yearswithalessthan20%chanceof surviving5years.88,97 Generally,meansurvivalis1yearforpatientswithCHF,2 yearswithsyncope,and4yearswithangina.97 Surgerywillimprovesurvivalevenin patientswithLVdysfunctionnotcausedbyexcessiveafterload,althoughLV dysfunctionandsymptomsmaynotcompletelyresolve.
2.Incontrast,surgeryhastraditionallynotbeenconsideredfortheasymptomatic patient,nomatterhowseverethedegreeofstenosis,becausetheriskofsudden deathisconsideredtobelow(estimatedat <1%/year),andtheriskoftheAVRmay exceedthepotentialbenefitofsurgery.98 However,patientswithsevereASneedto befollowedcarefullyforthedevelopmentofsymptomsorrapidlyprogressivevalve stenosis.Failuretoperformsurgeryoncepatientsbecomesymptomaticisthemost importantriskfactorforlatemortality.99
a.Itisestimatedthatupto40%ofpatientswithsevereASwillbecome symptomaticwithin2yearsandabout67%willbesymptomaticby5years.100,101 However,inpatientswithhighjetvelocities,LVhypertrophy,orseverevalve calcification,therateofprogressionofvalvestenosisisfasterandthesymptomfreeintervalisshorter.101
b.Ontheaverage,theannualincreaseinjetvelocityis0.3m/sec,theincreasein meangradientis7mm,andthedecreaseinvalveareais0.1cm2.However,the rateofprogressionofAScanbequitevariable,andserialDopplerechosshould beusedtoassesstherateofhemodynamicprogressionoftheAS,whichis predictiveofclinicaloutcome.
3.Indicationsforsurgeryintheasymptomaticpatientare:
a.ClassI:LVsystolicdysfunction(EF <50%)
b.ClassIIb
i.Abnormalresponsetoexercise(hypotension,symptoms)–notethatstress testingiscontraindicatedinthesymptomaticpatientwithsevereAS
ii.SevereASwithhighlikelihoodofprogression(elderlypatients,calcified valve,presenceofCAD)oriftherewillbeapotentialdelayfromsymptom onsettosurgery
iii.ExtremelysevereAS(AVA <0.6cm2,meangradient >60mmHg,jet velocity >5.0m/s)
4.AVRisgenerallyindicatedforpatientsundergoingothercardiacsurgeryifthe AVAis <1.2cm2,andpossiblyashighas1.4cm2.Invariably,anativevalvewithat leastmoderatestenosiswillrequiresurgerywithinafewyearsforprogressive obstruction,thusmandatingareoperativeprocedureathigherrisk.Clearly,itis essentialthattheprostheticvalvebeingplacedhavehemodynamicsasgoodasand hopefullybetterthanthevalvebeingreplaced.Nonetheless,onemustremember thatplacingaprostheticvalveintroducesatleasta1–2%annualriskforeachofthe prosthetic-relatedcomplications,includingendocarditis,thromboembolism,and bleeding.
5.Whenindicationsforaorticvalvesurgeryaremetandanenlargedaorta 4.5cm ispresent,theascendingaortashouldalsobereplaced.Althoughthisisa standardcriterionforbicuspidvalves,itisnotinappropriateforpatientswith trileafletvalves.
E Preoperativeconsiderations
1.Coronaryangiographyshouldbeperformedinanypatientovertheageof40orina youngerpatientwithcoronaryriskfactors,angina,orapositivestresstest.
2.IschemicsyndromesinpatientswithASrequirejudiciousmanagement.Medicationsthatmustbeusedverycautiouslyarethosethatcanreducepreload (nitroglycerin),afterload(calciumchannelblockers),orheartrate(b-blockers), becausetheymaylowercardiacoutputandprecipitatecardiacarrestinapatient withcriticalAS.Theventricularresponsetoatrialfibrillationmustbecontrolled, andcardioversionshouldbeperformedifthisrhythmispoorlytolerated.
3.Dentalworkshouldbeperformedbeforesurgerytominimizetheriskofprosthetic valveendocarditisunlessitisfelttobeaprohibitiverisk.
4.Selectionoftheappropriateprocedureandvalvetypedependsonanumberof factors,includingthepatient’sage,contraindicationstolong-termanticoagulation,andthepatient’sdesiretoavoidanticoagulation.
F Surgicalprocedures
1.Aorticvalveproceduresmaybeperformedthroughafullmediansternotomy incisionorthroughaminimallyinvasiveincision.Theseincludeanupperorlower sternotomywitha“J”or“T”incisionintothethirdorfourthintercostalspace,oran anteriorrightsecondorthirdinterspaceincision.102,103 CannulationforCPBfor minimallyinvasiveapproachescanbeperformedeitherthroughtheincisionor usingthefemoralvessels.
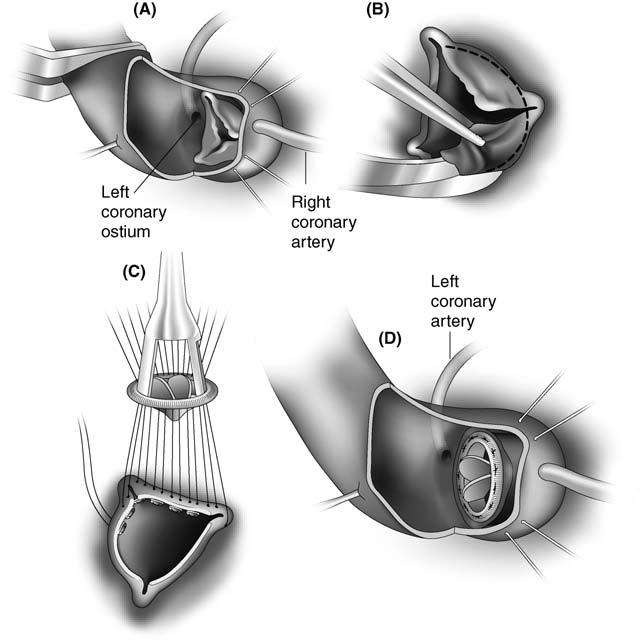
2.Aorticvalvereplacementwitheitheratissueormechanicalvalveisthestandard treatmentforAS(Figure1.8).
a.Ingeneral,tissuevalvesareselectedforpatients >age65toavoiduseofwarfarin. Current-generationtissuevalveshaveanticalcificationtreatmenttoreducethe riskofstructuralvalvedeterioration,andthusthesevalvesarebeingusedmore commonlyinyoungerpatients.
b.Astentlessvalvemaybeselectedtoprovidealargereffectiveorificeareaand maybeplacedinthesubcoronarypositionorasarootreplacement.104 Significantclinicalbenefitsofthisvalvearecontroversial,andtheoperation ismorecomplex(Figure1.9).
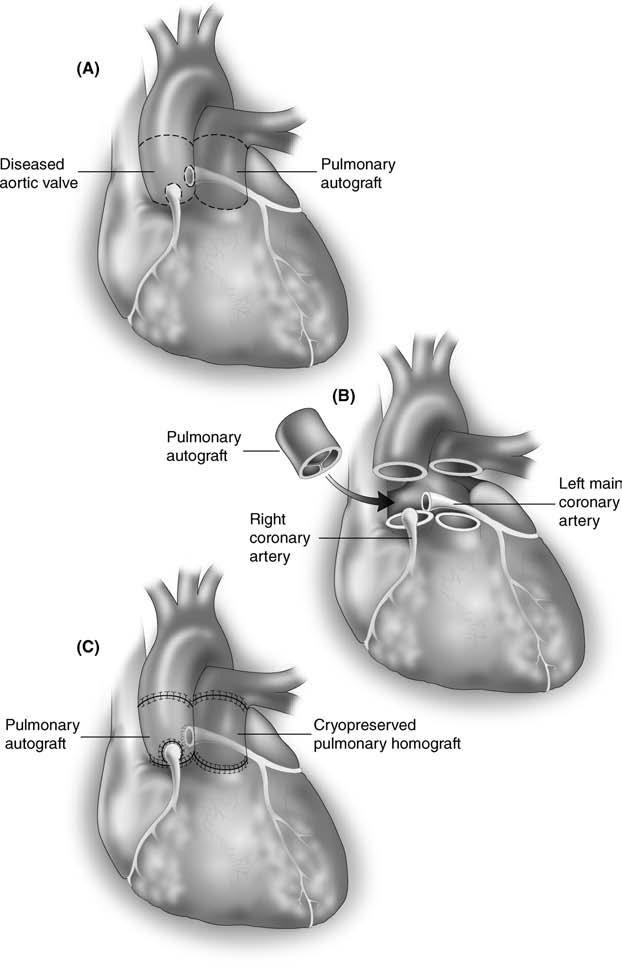
c.TheRossprocedure,inwhichthepatient’sownpulmonaryvalveisusedto replacetheaorticroot,withthepulmonaryvalvereplacedwithahomograft
Figure1.8 . Aorticvalvereplacement.(A)Atransverseaortotomyincisionismadeandholding suturesareplaced.(B)Thevalveisexcised,andtheannulusisdebridedandsized.(C,D) Pledgetedmattresssuturesareplacedthroughtheannulusandthroughthesewingringofthe valve,whichistiedintoposition.Theaortotomyisthenclosed.
(basicallyadoublevalveoperationforsinglevalvedisease),isanevenmore complicatedproceduregenerallyreservedforpatientsyoungerthanage50who wishtoavoidanticoagulation(Figure1.10).105
d.Homograftsareusuallyreservedforpatientswithaorticvalveendocarditis, althoughothertypesofprosthesesarguablyprovidecomparableresults.106–109
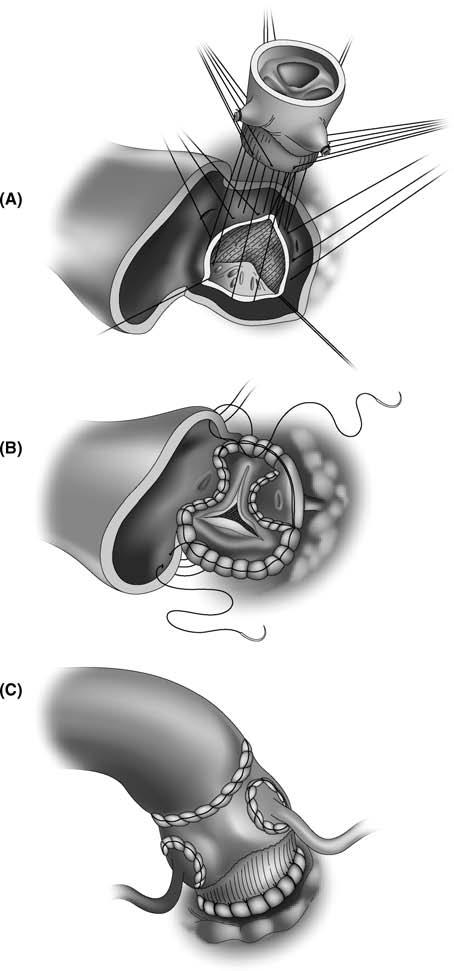
e.Anaorticrootreplacement,usuallyasavalvedconduit,isindicatedwhenthe ascendingaortamustalsobereplaced(Figure1.11).110 IfthesinusesofValsalva arenotdilated,replacingtheaorticvalveandusingasupracoronarygraft simplifiestheprocedure.
3.Reparativeprocedures,suchascommissurotomyordebridement,havelittlerole inthemanagementofcriticalaorticstenosis.However,debridementmaybe
Figure1.9 . Stentlessvalveshavealargereffectiveorificethanstentedvalves,allowingformore regressionofLVhypertrophy.(A)TheproximalsuturelinesewsthelowerDacronskirtofthe prosthesistotheaorticannulus.(B)SubcoronaryimplantationofaMedtronicFreestylevalve. Thisrequiresscallopingoftwosinuseswiththedistalsuturelinecarriedoutbelowthecoronary ostia.(C)Astentlessvalvecanbeusedasarootreplacement,requiringreimplantationofbuttons ofthecoronaryostia.Thedistalsuturelineisanend-to-endanastomosistotheaorticwall.
Figure1.10 . Rossprocedure.(A)Theaortaisopenedandthediseasedaorticvalveisremoved. Thepulmonicvalveandmainpulmonaryarteryarecarefullyexcisedandthecoronaryarteriesare mobilized.(B)Thepulmonaryautograftisthentransposedtotheaorticroot.(C)Thecoronary arteriesarereimplantedandtheRVoutflowtractisreconstructedwithacryopreserved pulmonaryvalvedhomograft.
Figure1.11 . Bentallprocedure.(A)Theaortaisopenedlongitudinallyandthendivided proximallyanddistally.(B)Coronaryostialbuttonsaremobilized.(C,D)Avalveincorporatedinto theproximalendoftheconduitisthensewntotheaorticannulus.(E)Thecoronaryostialbuttons arereimplantedandthedistalsuturelineiscompleted.
consideredinthepatientwithmoderateASinwhomthevalvediseaseisnotsevere enoughtowarrantvalvereplacement,butinwhomdecalcificationmaydelay surgeryforanumberofyears.
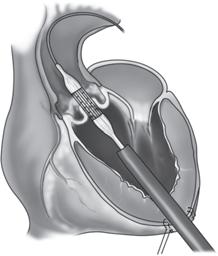
4.Transcatheteraorticvalveimplantation(TAVI)involvesplacementintheaortic rootofatissuevalvemountedonacatheterthatisadvancedeitherantegrade throughtheLVapex(viaaleftthoracotomy)orretrogradethroughthefemoral vessels(Figure1.12).Usingrapidventricularpacing,thedeviceispositioned fluoroscopicallyattheleveloftheaorticannulusamidstthediseasedvalveandthen inflatedmanually.Potentialseriouscomplicationsincludemigration,coronary obstruction,andstroke.Technicalcomplicationsnotedduringapicalimplantation includeacuteaorticandmitralregurgitation,septalhematomas,andapicalrupture. Earlytrialshavelimitedinclusioncriteriaprimarilytopatientsconsideredtoohigh
Figure1.12 . Transcatheteraorticvalveimplantation(TAVI).(A)Usingthetransapical approach,awireisplacedthroughtheaorticvalveoverwhichaballoonisusedtodilatethevalve. (B)Usingfluoroscopicimaging,thecatheterispositionedacrossthevalve,and(C)thevalveis inflated.
riskforsurgery,witharesultantmortalityrateconsistentlyexceeding10%.The rolefortranscatheterAVRinpatientswhoaresurgicalcandidateshasyettobe defined.111–115 Matchedforannularsize,percutaneousvalveshavebeenshownto besuperiorinhemodynamicperformancetobothstentedandstentlessbioprostheticvalves.116
V.AorticRegurgitation
A. Pathophysiology.88 Aorticregurgitation(AR)resultsfromabnormalitiesintheaortic valveleaflets(calcificdegeneration,bicuspidvalves,destructionfromendocarditis)or fromaorticrootdilatationthatpreventsleafletcoaptation(idiopathicrootdilatation causingannuloaorticectasia,aorticdissectionwithcuspprolapse).
1.AcuteARusuallyresultsfromendocarditisoratypeAdissection.Theventricleis unabletodilateacutelytohandlethesuddenincreaseinregurgitantvolumewhich increasestheLVend-diastolicvolume(LVEDV)andpressure(LVEDP),resulting inacuteLVfailure,cardiogenicshock,andpulmonaryedema.Dramaticelevations infillingpressuresmayoccurifacuteARissuperimposedonahypertrophic ventricle.Acutemyocardialischemiamayresultfromincreasedafterload(LV dilatation),compensatorytachycardia,andareductioninperfusionpressureasthe LVEDPapproachestheaorticdiastolicpressure.Asaresult,suddendeathmay occur.
2.ChronicARproducespressureandvolumeoverloadoftheleftventricle,resultingin progressiveLVdilatation(increaseinLVEDV)withanincreaseinwallstress,an increaseinventricularcompliance,andprogressivehypertrophy.Mostpatients remainasymptomaticfordecades,evenwithsevereAR,becauserecruitmentof preloadreserveandcompensatoryhypertrophymaintainanormalEFdespitethe increasedafterload.Theincreasedstrokevolumemaintainsforwardoutputandis manifestbyanincreaseinpulsepressurewithboundingperipheralpulses.Eventually,increasedafterloadandimpairedcontractilityleadtoLVsystolicdysfunction andafallinEF.Usuallyatthispoint,thepatientbecomessymptomaticwith