Guide to the Canadian Family Medicine Examination, Second Edition Visit to download the full and correct content document: https://ebookmass.com/product/guide-to-the-canadian-family-medicine-examination-s econd-edition/
More products digital (pdf, epub, mobi) instant download maybe you interests ...
Batesu2019 Nursing Guide to Physical Examination and History Taking Second,
https://ebookmass.com/product/bates-nursing-guide-to-physicalexamination-and-history-taking-second/
Graber and Wilbur's Family Medicine Examination and Board Review, Fifth Edition Brigit Ray
https://ebookmass.com/product/graber-and-wilburs-family-medicineexamination-and-board-review-fifth-edition-brigit-ray/
Graber and Wilbur’s Family Medicine Examination and Board Review 5th Edition Edition Jason K. Wilbur
https://ebookmass.com/product/graber-and-wilburs-family-medicineexamination-and-board-review-5th-edition-edition-jason-k-wilbur/
Wasps of the World: A Guide to Every Family (A Guide to Every Family, 8) Noort
https://ebookmass.com/product/wasps-of-the-world-a-guide-toevery-family-a-guide-to-every-family-8-noort/
Seidel’s Guide to Physical Examination – E-Book (Mosby’s Guide to Physical Examination) 9th Edition –Ebook PDF Version
https://ebookmass.com/product/seidels-guide-to-physicalexamination-e-book-mosbys-guide-to-physical-examination-9thedition-ebook-pdf-version/
Bates’ Guide to Physical Examination and History Taking (Bates Guide to Physical Examination and History Taking) 12th Edition, (Ebook PDF)
https://ebookmass.com/product/bates-guide-to-physicalexamination-and-history-taking-bates-guide-to-physicalexamination-and-history-taking-12th-edition-ebook-pdf/
Physical Examination and Health Assessment - 3rd Canadian Edition Carolyn Jarvis
https://ebookmass.com/product/physical-examination-and-healthassessment-3rd-canadian-edition-carolyn-jarvis/
The Infographic Guide to Medicine Neeral L. Shah
https://ebookmass.com/product/the-infographic-guide-to-medicineneeral-l-shah/
Bates’ Guide to Physical Examination and History-Taking – Eleventh Edition
https://ebookmass.com/product/bates-guide-to-physicalexamination-and-history-taking-eleventh-edition/
Hyperlipidemia
Diabetes
IschemicHeartDisease
CongestiveHeartFailure
Fatigue
CHAPTER8:PREVENTATIVEMEDICINE
PeriodicHealthAssessment
Men’sGenitourinaryHealth
Osteoporosis
SmokingCessation
CHAPTER9:SEXUALHEALTH
Gender-SpecificIssues
Infertility
Sex
SexuallyTransmittedInfections
BreastLump
CHAPTER10:WOMEN’SHEALTH
Contraception
Pregnancy
VaginalBleeding
Vaginitis
Menopause
CHAPTER11:MUSCULOSKELETALMEDICINE
Fractures
JointDisorders
LowBackPain
NeckPain
Lifestyle
CHAPTER12:CAREOFTHEELDERLY
Elderly
MultipleMedicalProblems
Dementia
MentalCapacityandCompetency
Disability
PalliativeCare
CHAPTER13:TRAVELMEDICINE
TravelMedicine
Hepatitis
ImmigrantHealth
CHAPTER14:SOCIALMEDICINE/PSYCHOLOGY
DomesticViolence
Rape/SexualAssault
Violent/AggressivePatient
Stress
CrisisManagement
FamilyIssues
BadNews
DifficultPatient
CHAPTER15:PREPARATIONFORTHESOO TheSOO Overview,NineHelpfulQuestionsandHowtoAttackIt
CHAPTER16:SHORTANSWERMANAGEMENTPROBLEMS(SAMPs)
Index
Contributors MalyhaAlibhai,BMedSci,MBBS(Hons),CCFP
ClinicalAssistantProfessor
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter5:Pediatrics
AngelaArnold,BASc,MEng,MD,CCFP(EM)
FamilyMedicineandEmergencyMedicine
UniversityofSaskatchewan,Regina
Regina,Saskatchewan,Canada
Chapter14:SocialMedicine/Psychology
Chapter15:PreparationfortheSOO
WilliamBaldwin,MD
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter16:SAMPs
LeanneBaumgartner,MD
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter4:Surgery
LourensBlignaut,MBChB,MCFP
FamilyPhysician
ClinicalAssistantProfessor
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter2:InternalMedicine
MatthewButz,MD
FamilyMedicineResident
UniversityofSaskatchewan
PrinceAlbert,Saskatchewan,Canada
Chapter6:Psychiatry
MeganClark,MD,CCFP
AssistantProfessorofMedicine
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter13:TravelMedicine
DanielleCutts,BA,MD,CCFP,FCFP
AssistantClinicalProfessor UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter9:SexualHealth
MeganDash,BSc,MD,CCFP(SEM),DipSportMed
FamilyMedicineandEnhancedSkills:SportandExerciseMedicine UniversityofSaskatchewan,Regina
Regina,Saskatchewan,Canada
Chapter11:MusculoskeletalMedicine
Chapter14:SocialMedicine/Psychology
TaegenFitch,MD
FamilyMedicineResident UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter7:ChronicDisease
LisaHarasen,MD,CCFP
FamilyMedicineResident UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter8:PreventativeMedicine
AndrewHoumphan,MD
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter10:Women’sHealth
ElliottHui,MD,CCFP
CommunityFamilyPhysician
Regina,Saskatchewan,Canada
Chapter12:CareoftheElderly
KaalynHumber,MD,CCFP
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter7:ChronicDisease
Chapter11:MusculoskeletalMedicine
WilliamDenovanJohnston,MD,BSc
AssociateClinicalProfessor
UniversityofSaskatchewan
SwiftCurrent,Saskatchewan,Canada
Chapter6:Psychiatry
BradleyJoss,MD,BSc
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter5:Pediatrics
RejinaKamrul,MBBS,CCFP
AssociateProfessor
AcademicFamilyMedicine(Regina)
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter7:ChronicDisease
AaronKastelic,MD,BComm
FamilyMedicineResident UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter3:InfectiousDiseases
JenniferKuzmicz,MD,CFPC,FCFP
AssistantProfessorofFamilyMedicine UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter8:PreventativeMedicine
TaraLee,MD,BSc(Hons),CCFP
ClinicalAssociateProfessor UniversityofSaskatchewan
SwiftCurrent,Saskatchewan,Canada
Chapter3:InfectiousDiseases
M.AntoinetteleRoux,MBChB,MPraxMed,CCFP
ClinicalAssistantProfessor DepartmentofFamilyMedicine UniversityofSaskatchewan
Saskatoon,Saskatchewan,Canada
Chapter13:TravelMedicine
SarahLiskowich,MD,CCFP
AssistantProfessorofMedicine UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter7:ChronicDisease
KishLyster,MD,CCFP(EM)
ClinicalAssistantProfessor UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter1:EmergencyMedicine
Chapter2:InternalMedicine
KyleMacDonald,MD
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter6:Psychiatry
SallyMahood,MD,CCFP,FCFP
AssociateProfessorFamilyMedicine
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter10:Women’sHealth
RaenelleNesbitt,MD,CCFP
EmergencyMedicinePhysician/FamilyPhysician
ClinicalAssistantProfessor
DepartmentofAcademicFamilyMedicine
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter1:EmergencyMedicine
StephanieNyberg,MD
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter9:SexualHealth
JaredOberkirsch,MD,CCFP
ClinicalAssistantProfessor
UniversityofSaskatchewan
Weyburn,Saskatchewan,Canada
Chapter2:InternalMedicine
TiannO’Carroll,MD,CCFP(EM)
Faculty,DepartmentofEmergencyMedicine
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter6:Psychiatry
JeremyReed,MD,FRCSC
OrthopaedicSportsSurgeon
ClinicalAssociateProfessorofSurgery
AdjunctProfessorofGraduateStudies
UniversityofSaskatchewan
ATLSCourseDirector
Regina,Saskatchewan,Canada
Chapter1:EmergencyMedicine
Chapter11:MusculoskeletalMedicine
OliviaReis,MD,CFCP
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter2:InternalMedicine
BabakSalamati,MD,CCFP
FamilyMedicineResident
UniversityofSaskatchewan
NorthBattleford,Saskatchewan,Canada
Chapter14:SocialMedicine/Psychology
SheilaSmith,MD,CCFP(EM),FCFP
ClinicalAssistantProfessor
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter4:Surgery
AndreaVasquez,MD
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter12:CareoftheElderly
RobertWeitemeyer,BSc,BA,BMBS
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter1:EmergencyMedicine
ChristopherYoung,MD
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter1:EmergencyMedicine
CherylZagozeski,BSc,MD,CCFP,FCFP
FamilyPhysician
ReginaCommunityClinic
Regina,Saskatchewan,Canada
Chapter2:InternalMedicine
LucasZahorski,CCFP
FamilyMedicineResident
UniversityofSaskatchewan
Regina,Saskatchewan,Canada
Chapter2:InternalMedicine
Preface “Thelifesoshort,thecraftsolongtolearn” Hippocrates Dr Arnold and I feel this quote encompasses the never-ending learning process medicine We have collaborated with many for this book, with the idea to assist individuals in studying for what may be the biggest exam of their life It is not intended to be the only resource, but to aid in relieving some of the stress thatthisexamcan,andlikelywill,create
This book has been originated from handwritten notes, scribbled in the wee hours of the night, while Angela and I prepared for our exam. When finished we placed the notes in a giant orange binder, thus it was appropriately nicknamed The Orange Book My original copy is sitting in the drawer at my office desk and I still pull it out every once in a while I still remember the day Angela told me she thought we should submit ournotesforpublication.Ilaughedskeptically,butsaidIwasupforthechallenge.Andnowhereweare!The book is no longer orange and has glossy pages and fancy tables, but the content and purpose of the book is largelyunchanged
The second edition has been updated to make sure that all the information is aligned with current practice guidelines,andachapterofexampleSAMPscreatedtohelpyouinyourpreparationsfortheCanadianfamily medicineexamination.We’vealsotriedtoleavealotofmarginspacesoyouhaveroomtoannotate. Thankstoallthedoctorsandresidentswhogavetheirtimetoassistintheeditingofthissecondedition Your expertiseandeffortishighlyvalued.
Tothereader,wehopeyoufindthisresourceasusefulasitwasforus.Happystudying!
Acknowledgements SpecialthankstoAngela,forputtingupwithmeandstudyingwithmeallthoselatenights,myhusbandDr Jeremy Reed for all your advice and support, and to our new little one Kendall Grace, for letting me edit this new edition whilebreastfeeding!
ThankstoMeganforagreeingtothesecondedition We’vecomealongwayandIalwaysappreciatethecollaboration and how the book keeps us connected! I also want to acknowledge that being able to practice medicine is truly a privilegeandIamgratefulforallmycolleaguesandthepeoplewhohavehelpedinthisnever-endinglearningprocess.
AngelaArnold
MeganDash
Abbreviations < lessthan
A1C glycatedhemoglobin
AAA abdominalaorticaneurysm
ABPM ambulatorybloodpressuremeasurement(24-hourbloodpressuremonitoring)
ACE-I angiotensinconvertingenzymeinhibitor
AE adverseeffects
AFib atrialfibrillation
AIS adenocarcinomainsitu
ALP alkalinephosphatase
ALT alaninetransaminase
ARB angiotensinreceptorblocker
ASA acetylsalicylicacid
ASC-US atypicalsquamouscellsofundeterminedsignificance
AST Aspartatetransaminase
BCC basalcellcarcinoma
BMI bodymassindex
BNP B-typenatriureticpeptide
BP bloodpressure
BPH benignprostatichyperplasia
BPM bloodpressuremeasurement
BSA bodysurfacearea
C&M crossandmatch
CAD coronaryarterydisease
CAROC comprehensivefractureriskassessmenttool
CDA CanadianDermatologyAssociation
CHF congestiveheartfailure
CI contraindicated
CKD chronickidneydisease
CN cranialnerve
CNS centralnervoussystem
COMT catechol-O-methyltransferase
COPD chronicobstructivepulmonarydisease
CRP C-reactiveprotein
CT computedtomography
CVD cerebrovasculardisease
CVS cardiovascularsystem
D&C dilationandcurettage
DM diabetesmellitus
DVT deepvenousthrombosis
DWI diffusionweightedimaging
ECG electrocardiogram
Eg forexample
EM erythemamultiforme
ENT ear,nose,andthroat
FH familyhistory
FIT fecalimmunochemicaltest
FNA fineneedleaspiration
FOBT fecaloccultbloodtest
FPG fastingplasmaglucose
FRAX FractureRiskAssessmentTool
FT4 freethyroxine
GBS groupBstreptococcus
GDM gestationaldiabetesmellitus
GERD gastroesophagealrefluxdisease
GGT gamma-glutamyltransferase
GHTN gestationalhypertension
HAART highlyactiveantiretroviraltherapy
HBV hepatitisBvirus
HF heartfailure
HIDAscan hepatobiliaryscintigraphy
HIV humanimmunodeficiencyvirus
HOCM hypertrophicobstructivecardiomyopathy
HR heartrate
HRT hormonereplacementtherapy
HSIL high-gradesquamousintraepitheliallesion
HTN hypertension
IUGR intrauterinegrowthrestriction
IV intravenous
LLDP leftlateraldecubitusposition
LOC lossofconsciousness
LSIL low-gradesquamousintraepitheliallesion
LT4 l-thyroxine,levothyroxine
MAO-I monamineoxidaseinhibitor
MCV meancorpuscularvolume
MDD majordepressivedisorder
MI myocardialinfarction
MMI methimazole
MRI magneticresonanceimaging
MS multiplesclerosis
NNT numberneededtotreat
NSAIDs non-steroidalanti-inflammatorydrugs
OGTT oralglucosetolerancetest
OH orthostatichypotension
OSA obstructivesleepapnea
PCOS polycysticovariansyndrome
PD Parkinsondisease
PE pulmonaryembolism
PG plasmaglucose
PHQ-9 preventativehealthquestionnaire9;ascreeningquestionnairefordepression
PMH pastmedicalhistory
PNS peripheralnervoussystem
PO oralroute
PPD postpartumdepression
PPG post-prandialplasmaglucose
PPROM PretermPROM(lessthan37weeks)
PPT postpartumthyroiditis
PROM premature(beforetheonsetoflabour)ruptureofmembranes
PTU propylthiouracil
PV pervaginum
QOL qualityoflife
R/O ruleout
RAI radioactiveiodine
RAIU radioactiveiodineuptakescan
RCT randomizedcontrolledtrial
RS respiratorysystem
rTPA RecombinantTissuePlasminogenActivator
RUQ rightupperquadrant
Rx treatment
SCC squamouscellcarcinoma
SE sideeffects
SERM selectiveestrogenreceptormodulator
SES socio-economicstatus
SJS Stevens-Johnsonsyndrome
SSRI selectiveseretoninreuptakeinhibitor
STI Sexuallytransmittedinfection
T3 triiodothyronine
T4 thyroxine
TCA tricyclicantidepressants
TDaP tetanus,diptheria,andacellularpertussis
TEN toxicepidermalnecrolysis
TIA transientischemicattach
TOP terminationofpregnancy
TPO thyroidperoxidase
TRAP tremor,rigidity,akinesia,posturalinstability
TRH thyrotropinreleasinghormone
TSH thyroidstimulatinghormone
TSI thyroidstimulatingimmunoglobulin
U/S ultrasound
UE upperextremities
VZV varicellazostervirus
WBC whitebloodcells
TopTenTipsforWritingSAMPs 1 Ensurethatyoureadthequestionsthoroughly Sometimestheanswerisgivenwithinthequestion
2 CBC is not an appropriate answer You must state hemoglobin, white blood cell count, etc This is the sameforalllaboratoryinvestigations
3 Takeyourtime Youwillhaveplentyoftimetocompleteallthequestions
4 Be aware of the environment in which the question places you Your answer may be different if you are in yourofficeversustheemergencyroom
5 Know classes of medications and ensure that you know a few options for each condition For example, classes of medications to treat hypertension include calcium channel blockers, diuretics, beta blockers, and soon.
6 Bespecific Answersusuallyrequireonlyafewwords
7 Gowithyourgut Thequestionsarenottryingtotrickyou
8 Usegenericnamesofmedications,nottradenames
9 A table of normal laboratory values is provided on the exam, so do not waste your time memorizing those ranges
10 Visit the CFPC Web site at http://wwwcfpcca/EvaluationObjectives to review the objectives for the exam
CHAPTER1 EmergencyMedicine ACLS PriorityTopic1
PleaserefertoACLSguidelinesforacomprehensivereviewofACLSalgorithmsforACS,cardiacarrest, andarrhythmias(AmericanHeartAssociation,2015).
Arrhythmiasareafrequentproblemencounteredintheemergencyroom(ER) Ageneralapproachto arrhythmiasisessential(Tables1-1and1-2).
TABLE1-1 Arrhythmias ApproachandCharacteristics PATHOLOGY RHYTHM/CAUSE CHARACTERISTICS MANAGEMENT
Tachycardia (HR>100)
Afib
•Narrowcomplex
•Irregularlyirregular
•NoPwaves
•Withorwithoutrapid ventricularresponse
SVT
VTach
VFib
Bradycardia (HR<60)
Various: Searchforcauses=6
Hsand5Ts
•Narrowcomplex(<0.12 s)
•Aberrantpacemakercan beatrial,AVnode, ectopic
•VariousPwave anomalies(varied timing,morphology)
•Wide(>012s) complexes
•Greaterthanthree ventricularcomplexes withrate>100
•NoclearQRScomplexes
•Nopulse(too disorganized)
•Heartrate<60
•Mayormaynotbe symptomatic
ACLSprotocol
•ifhemodynamicallyunstableelectricalcardioversion
•ifstablemedicalrateconversion
•followwithexpertconsultation
•Vagalmanoeuvres
•Adenosine6mgIVpush;then12mg(onlyifregular)
•Ifdoesnotconvert,considerbeta-blockerordiltiazem (Expert consultation)
•Ifunstablesynchronizedcardioversion
•Withpulse;consideradenosine(asabove)onlyifmonomorphicand regular Giveamiodarone150mgIVover10min Ifunstable synchronizedcardioversion (Expertconsultation)
•Ifpulseless;FollowPEAprotocol.CPR,Epinephrine1mgq3-5min. Ifrefractoryamiodarone300mgIVmayreplaceseconddoseof epinephrine Mayrepeatamiodaroneonetimeof150mg
•StartCPRimmediately,defibrillate
•Epinephrine1mgIVq3-5min
•Amiodarone300mgIV(mayreplaceseconddoseofepinephrine), mayrepeatamiodaroneonetimeof150mg
•Transcutaneouspacing(titratemAto10%overmechanicalcapture confirmedbyfemoralpulse)
•Atropine05mgIV
Asystole/PEA Various: Searchforcauses=6 Hsand5Ts(see Table1-3)
Metabolic/drugs Cocainetoxicity
Hyperkalemia
•Rxonlyifclinically inadequateperfusion
•ECGflat.Norhythm. (Orarhythmbutno pulseisabletobe palpated.)
•Tachycardia+/ ischemicchanges
•PeakedTwaves, slurred/elongatedQRS, lossofPwave
Digoxintoxicity
*Opioid
•STdepressionwith invertedTwaves(V5V6)
•ShortQTsegment
•Cardiac/respiratory arrest
(*includedin2015ACLS protocol)
•Considerepinephrine(2-10mcg/min)ordopamine(2-20 mcg/kg/min)infusion
•Definitive(transvenous)pacing
•CPR.
•Donotdefibrillateunlessshockablerhythm(VForVT)
•Epinephrine1mgIV/IOq3-5min
•Maygivevasopressin40UIV/IOtoreplacefirstorseconddose epinephrine
•Mayconsideratropine1mgIV/IOq3-5min
•Donotgivebeta-blocker
•Cardio-protectionwithcalciumgluconate10%10mgover2min (willnormalizeECG)
•Decreasepotassiumwithinsulin+dextrose,betaagonist(salbutamol), diuretic
•DigoxinimmuneFab(Digibind)
•BeginCPR
•AdministerNaloxone04mgIM/2mgintranasalq4min
Abbreviations:Afib,atrialfibrillation;PEA,pulselesselectricalactivity;SVT,supraventriculartachycardia;VFib,ventricularfibrillation;V Tach,ventriculartachycardia
TABLE1-2 HeartBlocks
RHYTHM CHARACTERISTICS TREATMENT
1st-degreeAVblock LongPRinterval(>200ms) Notreatment
2nd-degreeAVblockMobitz1 ProgressiveincreaseinPRintervaluntiladroppedbeat,PRthenresets Stopoffendingdrugs
2nd-degreeAVblockMobitz2 NochangeinPRwithpatterneddroppedQRSbeats(2:1or3:1) Pacemaker
3rd-degreeAVblock NorelationshipbetweenPwaveandQRScomplex Pacemaker
TABLE1-3 6Hsand5Ts(UnderlyingCausesforBradycardicandTachycardic Arrhythmias)
Hypovolemia
Hypoxia
Hydrogenion(acidosis)
Hypo/Hyperkalemia
Hypoglycemia
Hypothermia
Bibliography
Toxins
Tamponade(cardiac)
Tensionpneumothorax
Thrombosis(coronaryorpulmonary)
Trauma(hypovolemia,increasedICP)
2015;18(2):132
ASA AmericanHeartAssociationguidelinesforcardiopulmonaryresuscitationandemergencycardiovascularcare Circulation2010:122
LossofConsciousness PriorityTopic59
Definition
Theoccurrenceofalossoftheabilitytoperceiveandrespond.
History
MustdifferentiatebetweentraumaticLOCandnontraumaticLOC.
SAMPLEhistoryisimportant
•S signsandsymptoms
•A allergies
•M medication
•P pastmedicalhistory
•L lastmeal
•E event,thedetailsofwhathappened
Historyfromwitnessesisveryimportant
Seekinformationon:
•Trauma
•Medications(Rx,over-the-counter,andsupplements)
•Toxins(illicitdrugs,poisons)
•Seizureactivity
•Psychologicalhistory
PhysicalExamination
This is a critical care scenario! Switch into ACLS/ATLS/ICU mode Do your ABCs Do a thorough examinationanddonotskipanysteps UsecollateralhistoryviaEMS,bystanders,andfamily ABCDEs
•Ensureapatentairway;intubateifnecessary
•Ensureairismovingappropriately
•Attainafullsetofaccuratevitalsincludingglucose,lookforsignsofshock.
•CheckpupilsandcalculateGlasgowComaScoring(GCS) (seeTable1-4)
TABLE1-4
GlasgowComaScoring
IfGCSlessthan8,intubate!(usually).Considerintubationforhypopnoea,pulmonarytoilet,delayin transportorexpecteddeteriorationinclinicalcourse
•Checkfor,andmanagehypothermiaviawarmedfluids,warmblankets,increasingroomtemperature,etc.
Performasystematicheadtotoeexamination.
•Lookforsignsoftrauma
•Checkforlocalizingneurologicsigns(seeTable1-5)
TABLE1-5
NeurologicSigns
Injuryaboveanteriorhorncellofspinalcord
Plantarreflexupgoing
Toneincreased,secondarytounregulatedspinalcordreflexarcs
DTRsincreased
•Notesmellofalcoholorketones
•Lookforasterixis,indicatingrenalorhepaticfailure.
ConsidervariouscausesofLOC(seeTables1-6and1-7).
TABLE1-6
Injurybelowanteriorhorncellofspinalcord
Plantarreflexdowngoing
Toneflaccid,secondarytolostmuscleinnervation
DTRsdecreased,normal,orabsent
Atrophy,fasciculationsinlongterm
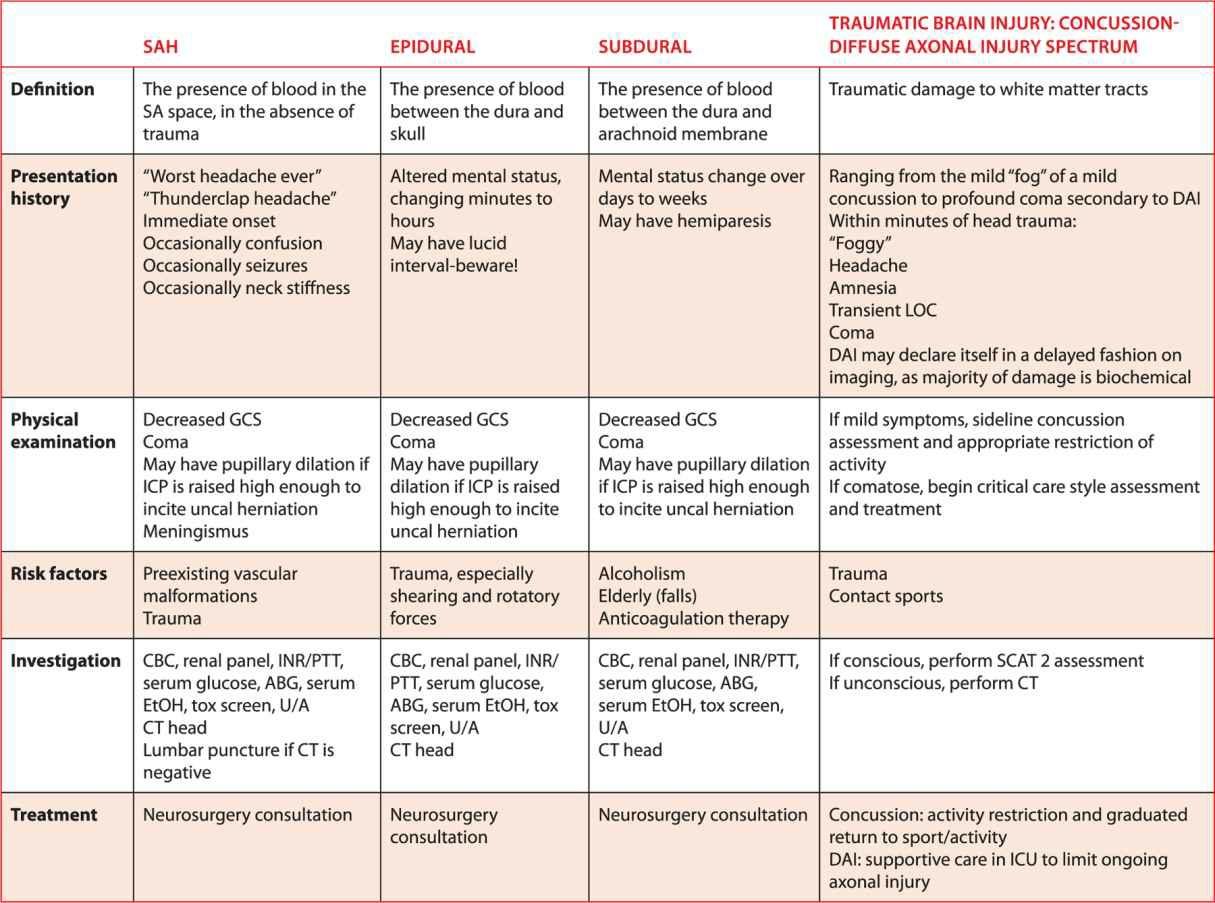
DifferentialDiagnosis TraumaticHeadInjury
TABLE1-7 DifferentialDiagnosis NontraumaticHeadInjury Definition
Presentation
Physicalexamination
Theoccurrenceofalossoftheabilitytoperceiveandrespond,intheabsenceofatraumaticevent
Stupor,confusion,unconscious
Recognizeasickpatient,recordvitals,performfocused,thoroughhead-to-toeexaminationasdiscussedearlier
Etiologies “The6Hsandthe5Ts”
Hypovolemia
Hypoxia
Hydrogenion(acidosis)
Hypo/HyperK+
Hypoglycemia
Hypothermia
Toxins
Tamponade
Tensionpneumothorax
Thrombosis
Trauma
Investigation
CBC,renalpanel,INR/PTT,serumglucose,ABG,serumEtOH,toxscreen,U/A,CThead
Treatment Appropriaterecognitionofacriticallyillpatient
Supportivecriticalcaremanagementasneeded
•ABCDE
•Warming
•Fluidresuscitation
Correctionofbiochemicalabnormalitiesandcoagulopathies
Intubation
Rapidsequenceinduction “OBLASTHIM”topreparepriortointubation
TheuseofanAirwayChecklistshouldbemandatory3
O O2 availableandworking(useApneicOxygenationtechnique;NRBplushigh-flownasalat15L/min priortointubationattempttosaturatewithoxygen.Forbag-valve-maskventilationusetwopersonsanda PEEPvalve)
B Bladeandbag(blade2-3formostadults)
L Laryngoscopeavailableandworking
A Airway(oropharyngeal/guedelairway measureangleofmouthtoangleofjawtochoosesize
Considernasopharyngealairwayasadjunct measurenarestothelobeoftheear)
S Suctionandstylet
T Tube;ETtube(size7-8)orlaryngealmaskairway(size3-4)
H HELP(getsome)/hinder(identifyanysignsofdifficultairway)
I IVaccess
M Medications
Medications
InductionOptions
Ketamine1to15mg/kgiseffectiveforinductionwithlessriskofhypotension
Propofol15to3mg/kgasaninductionbolus 1 Highriskofhypotension
Fentanyl1to2mcg/kgidealbodyweight 1
•bolusasabove,followedby10mcg/kg/h
Midazolam0.05to0.1mg/kg(maximum5mg)foramnesiaandinduction1,2
ParalyticOptions
1.Succinylcholine1to1.5mg/kgforparalysis
Intubateoncefasciculationsstop
Contraindicatedifstateofhighpotassium(eg;burns,renalfailure,polytrauma)
ExpectsuccinylcholinetoincreaseKby10mmol/L bewareinarenalfailurepatient
Expectbradycardia!
2.Rocuronium1mg/kgforparalysis.
ManagementofBloodPressure Phenylephrine Forhypotension
Purealpha(vasoconstrictive)effect
Norepinephrine Forhypotension
Strongalpha(vasoconstriction)andweakerbetaeffects(chronotropyand inotropy)
Epinephrine Forhypotensionandbradycardia
Potentalphaandbetaactivity
RSICheatSheet 1 Establishairway(chinlift,jawthrust)+/ in-lineC-spinestabilization
2 Preoxygenate100%high-flowO2 for2to3minutes
100-200mcg/doseq10-15minPRN
Dosingisalmostalwaysbolususe
Infusion001-1mcg/kg/min
Inpractice,maximumdoseusually05 mcg/kg/min
Infusion001-1mcg/kg/min
Inpractice,maximumdoseusually05 mcg/kg/min
3 IVaccessandgivefluids**note:ifableto,doyourneuroexaminationpriortoparalysis!**
4.Medications(exampleofpossibleoptions).
Midazolam01mg/kg(maximum5mg)
Fentanyl2mcg/kg
Succinylcholine1to15mg/kg
5 Expectbradycardia:haveatropine05mgq3to5min(maximum3mg)
Expecthypotension:havephenylephrine100to500mcgreadytopush.
6 WATCHforfasciculationtocease,indicatingparalysis(roughly45seconds)
7 Laryngoscopew/size2to3bladeformostadults
Headinthesniffingposition
Observelipsandteethcarefully
THENlookintothebladeandPUSHthetongueforwardandslightlyupuntilyouseechords. NEVER,EVER,rotateyourwrist,orleverageontheupperteeth
Visualizetheepiglottis
IntroduceETT(+/ styletorbougie)
Inflatecuffwithabout10ccofairandcheckforleak.
Toconfirmappropriatetubeplacement,lookfor:
a multipleoccurrencesofmistintube(thestomachcangiveyouapuffortwoofsteamandCO2), b bilateralairentrywithnobreathsoundsinepigastrium, c.endexpiratoryCO2 onindicatorstriporcapnograph.Capnographyisthestandardofcare.
Once tube placement is confirmed, care should be taken to match minute ventilation (rate and volume) of patient pre-intubation until an ABG can be obtained Keep oxygen on high-flow with bag or 100% on ventilatoruntilconsultationisobtained
**Chooseanagentthatyouarefamiliarwith,andissuitedforthesituation Takeanairwaycourse!Takingcontrolofanairwayislifesavingbut highrisk Youneedtobecomfortablewiththeskillordelegatetosomeonewhois
Bibliography AHSCriticalCareMCGs RSIPalgorithm https://wwwahsemscom/public/protocols/templates/desktop/#set/13/browse/3663/view/ 31311/Algorithm.AccessedJan182017.
ATLSSubcommittee AmericanCollegeofSurgeons’Committeeontrauma;InternationalATLSworkinggroup Advancedtraumalife support(ATLS®):theninthedition JTraumaAcuteCareSurg2013;74(5):1363-1366 doi:101097/TA0b013e31828b82f5
CardoD InductionAgentsforRapidSequenceIntubationinAdults In:WallsRM,GrayzelJ,eds,UpToDate;2016 Retrievedfrom http://wwwuptodatecom/ HardyG,HornerD BET2:Shouldrealresucitationistsuseairwaychecklists?EmergMedJ2016;33(6):439-441 StrayerR,WeingartS,AndreusP,ArntfieldR EmergencyDepartmentintubationchecklist,MountSinaiSchoolofMedicine,v13,updated 7/8/2012,accessed10/11/2016 http://emupdatescom/2012/07/08/emergency-department-intubation-checklist-v13/
CanadianHeadCTRules
AskyourselfisaheadCTindicated?
UsemnemonicBEANDASH CTifanyoneofthefollowingispresent:
•Basalskullfracture(hemotympanum,racooneyes,CSFotorrhea/rhinorrhea,Battlesign)
•Emesis≥2
•Age≥65
•Neurosymptoms(GCS<15at2hoursafterinjury)
•Dangerousmechanism(pedestrianstruckbyavehicle,occupantejectedfrommotorvehicle,fallfrom≥3 feet,etc)
•Amnesia(≥30minutesprior)
•Skullfracturesuspected(openordepressed)
GeneralManagement
1 ABCDEs Thesepeoplemaywellhaveveryseriousassociatedinjuries
Managecriticalcareissuesasneeded
2.Supportivemanagement preventionoffurtherinjuryisallyoucanofferthem. ICPmanagement:Neutralheadposition;headofbedat30degrees.
Preventhypoxemia
Preventhypotension(remembercerebralperfusion=ICP meanarterialpressure) Ifpossibleaimfor MAPsabove80mmHg
Preventhypothermia/hyperthermia
Preventseizureactivity
3.Begincorrectionofbiochemicalandcoagulationabnormalities.
4.Criticalcareandneurosurgicalconsultationsasneededfordefinitivemanagement.
Bibliography
StiellIG,WellsGA,VandemheenK,etalfortheCCCStudyGroup TheCanadianCTHeadRuleforpatientswithminorheadinjury Lancet2001;357(9266):1391-1396
Trauma PriorityTopic92
Traumaisoneoftheleadingcausesofmorbidityandmortalityinyoungagegroups. AllprimarycareprovidersshouldconsidertakinganATLScourse ATLSprovideseveryonewithasystematicwaytobringcalmtoachaotic scenario,optimizepatientoutcomes,andattimes,savealife Formoreinformationsee:http://wwwtraumacanadaorg
OVERVIEW Beprepared Knowyourfacilityandyourteam’scapabilities
Reviewwhatisavailable,andensurethatnecessaryequipmentisavailable
•WarmedIVfluids
•Warmblankets
•Chesttubetray
•Intubationset
•Cricothyroidotomyset
•Appropriatedrugs
•ABroselowtapeforpeds
•Fabricpelvicbinders notjustasheetifatallpossible
•Blood,iffeasible
•Appropriatemonitoring
MANAGEMENT Beaspreparedaspossible
Uponarrival:
•EnsureC-spineimmobilization
•Applyoxygen,monitors,andstarttwolargeboreIVs definedas16gorlarger
•Attainacompleteandaccuratesetofvitals
HR
Respiratoryrate
SaO2
Bloodpressure
Temperature
Glucose
PRIMARYSURVEY Airway Isitpatent?Willitremainpatent?Isintubationrequired?
Breathing Isairmovinginbothlungfields?
Circulation Isthereapulse?WhatistheBP?Skincolour?Anyactivebleeding?
Disability AssesspupillaryresponsesandcalculateGCS(seeLOCsectionforGCS)
Exposure Completelyuncoverthepatient Ensureyouarewarmingthemasmuchaspossible via warmedIVfluidandcoveringthepatientwithwarmblanketsassoonaspossible.
Recheck your ABCDEs constantly. If there is a change in condition, immediately revert to “A.” “A” is your safezone,your“happyplace”ifyouwill….
ADJUNCTSTOTHEPRIMARYSURVEY Monitors
•ECG,pulseoximeter,BP,ventilatoryrate
Urinarycatheter
Traumalabs
•CBC,electrolytes,bloodtypeandcrossmatch,urinalysis,toxicologyscreen,serumEtOH,arterialblood gas
X-rays
•APpelvis
•CXR
•InmostcasesalateralC-spineviewisnotrequired LeavepatientinC-spineprecautionsifconcerned
SECONDARYSURVEY Doesnotbeginuntiltheprimarysurveyiscompleted,resuscitativeeffortsareunderway,andthe normalizationofvitalfunctionshasbeendemonstrated.
RecheckABCDEs.
Athoroughandsystematicexaminationfromheadtotoe(includinglogrollandrectalexamination)istobe performed
Thismeansafullhistoryandphysicalexamination.
AttainAMPLEhistoryfrompatient,family,orEMS
•A allergies
•M medications
•P pastmedicalhistory
•L lastmeal
•E events,whathappened?Askaboutthemechanismofinjury
ADJUNCTSTOTHESECONDARYSURVEY NGorOGtubes ifyouarecertainthereisnosignofbasalskullfracture
•NoBattlesign,nootorhinorrhea
Foleycatheter ifyouarecertainthereisnobladderorurethraltrauma
•Nobloodatmeatus,normalrectalexamination
ECGifindicated thatis,ifcardiacischemiaorcontusionissuspected
Additionalimaging
•X-raysofextremities,CTscanifindicated ONLYIFPATIENTISSTABLE
DEFINITIVEMANAGEMENT Stabilizethepatienttothebestofyour,andyourfacilities,ability.
Seekhelpandadviceearlyfromatraumatologist
Discussmostappropriatemodeoftransfer groundversusairplaneversushelicopter
“Packageup”thepatientfortransfer:
•Intubationandplacementofchesttubesinanambulanceisveryunpleasant It’salsounpleasantonthe sideofabusyhighway It’salmostimpossibleinaplaneorhelicopter Anticipatewhatyourpatientmight needbeforetransferring.
•Iftransferringviaair,rememberthatapneumothoraxwillprogressfasterasaltitudeincreasesduring flight.Also,rememberthatFiO2 decreaseswithaltitude.Ifapatientisnotmaintainingsatsatground level,thiswillbemadeworseduringflight
But
•Donottakeextratimewithproceduresordiagnostics(ie,CTscans)unlesstheycontributeappropriately tothepatient’sstabilityinpreparationfortransfer Donotundertakediagnosticsthatyourfacilityisnot equippedtoactupon(ie,ifyoudonothavesurgicalcoverage,don’tdoaCTscan)
•Travelwiththepatientintheambulance/plane/helicopterifthereisongoinghemodynamicinstability Earlyconsultationwithatransportserviceisimportantassoonasyourecognizethatthepersonwill outstripyoufacilitiescapabilities.
LIFE-THREATENINGTRAUMAEMERGENCYSCENARIOSTHATFAMILYPHYSICIANS SHOULDKNOW
TensionPneumothorax
Signs/symptoms:Hemodynamicinstability,respiratorydistress,increasedHR,asymmetricalchestwall motion,trachealdeviation,hyperresonancetopercussion,unilateralabsenceofbreathsounds
Rx:Needlethoracostomyatsecondintercostalspaceatmid-clavicularline DonotdelayforX-ray Follow withchesttubeatfifthintercostalspaceatanterioraxillaryline
CardiacTamponade Signs/symptoms:Usuallywithpenetratingchestwound Becktriad(hypotension,distendedneckveins, muffledheartsounds),pulsusparadoxus(abnormallylargedropinSBPoninspiration),Kussmaulsign(rise inJVPoninspiration)
Rx:ConfirmwithECHOorbedsideU/Sifpossible;pericardiocentesis(atxiphoid,aimneedleat45 degreestowardsnipple)
Bibliography
AmericanCollegeofSurgeonsCommitteeonTrauma AdvancedTraumaLifeSupportforDoctors 9thed Chicago,IL:AmericanCollegeof Surgeons;2012.
ChenYA,TranC TorontoNotes–ComprehensiveMedicalReference&ReviewforMCCQEIandUSMLEII Toronto,Canada:TorontoNotes forMedicalStudents;2013
TintinalliJE,StapczynskiJS,ClineDM,MaOJ,YealyDM,MecklerGD,eds Tintinalli’sEmergencyMedicine:AComprehensiveStudyGuide 8thed NewYork,NY:McGraw-Hill;2015
Shock
SupplementaryTopic
Definition
Inadequateend-organperfusionresultinginlossofaerobiccellularfunction
The“endorgans”are
Brain(signs alteredconsciousness,lossofconsciousness)
Kidneys(signs decreasedurineoutput)
Skin(signs cool,clammy,dusky,pale)
Heart(signs myocardialischemia,decreasedcardiacoutput,hypotension)
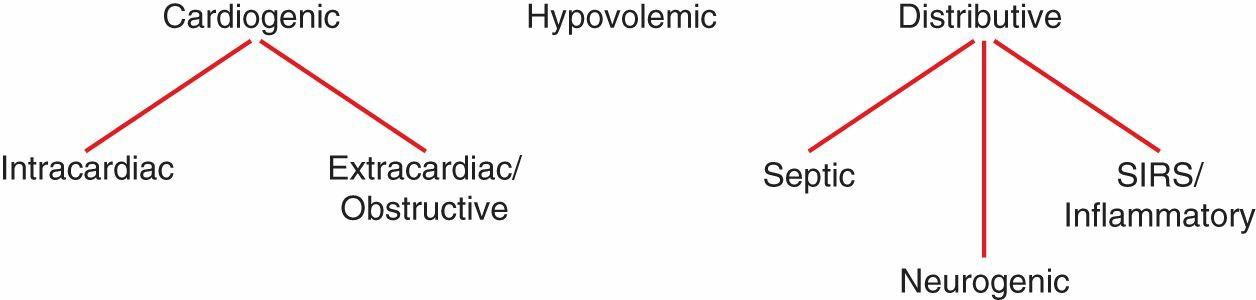
TYPESOFSHOCK HypovolemicShock
Definition
Lackofeffectivecirculatingbloodvolume
Beware:
•Bleedingmightnotbeexternal meaninggastrointestinal(GI)bleed,rupturedovariancyst,femur fracture,pelvicfracture,etc
•“Blood”isn’tjusttheredstuff.Largeserumlosses,suchasinburnpatients,nauseaandvomiting,high outputileostomy,andpancreatitiscanalsoleadtohypovolemia
Signs
Tachycardia; peripheral vasoconstriction leading to cool, clammy skin; acidosis; tachypnea; altered mental status