Visit to download the full and correct content document: https://ebookmass.com/product/photographic-manual-of-regional-orthopaedic-and-ne urologic-tests-5th-edition-ebook-pdf/
More products digital (pdf, epub, mobi) instant download maybe you interests ...
Manual of Cardiovascular Medicine 5th Edition, (Ebook PDF)
https://ebookmass.com/product/manual-of-cardiovascularmedicine-5th-edition-ebook-pdf/
DeLee & Drez’s Orthopaedic Sports Medicine E Book 5th Edition, (Ebook PDF)
https://ebookmass.com/product/delee-drezs-orthopaedic-sportsmedicine-e-book-5th-edition-ebook-pdf/
Greenmanu2019s Principles of Manual Medicine 5th Edition, (Ebook PDF)
https://ebookmass.com/product/greenmans-principles-of-manualmedicine-5th-edition-ebook-pdf/
Davis’s Comprehensive Manual of Laboratory and Diagnostic Tests with Nursing Implications (Davis’s Comprehensive Handbook of Laboratory & Diagnostic Tests With Nursing Implications) 8th Edition, (Ebook PDF)
https://ebookmass.com/product/daviss-comprehensive-manual-oflaboratory-and-diagnostic-tests-with-nursing-implications-davisscomprehensive-handbook-of-laboratory-diagnostic-tests-with-
Dutton's orthopaedic examination, evaluation, and intervention 5th Edition Mark Dutton
https://ebookmass.com/product/duttons-orthopaedic-examinationevaluation-and-intervention-5th-edition-mark-dutton/
Netter Atlas of Human Anatomy-Classic Regional Approach, 8e (Mar 29, 2022)_(0323793738)_(Elsevier) NOT TRUE PDF Frank H. Netter
https://ebookmass.com/product/netter-atlas-of-human-anatomyclassic-regional-approach-8e-mar-29-2022_0323793738_elsevier-nottrue-pdf-frank-h-netter/
Manual of Perioperative Care in Adult Cardiac Surgery 5th Edition, (Ebook PDF)
https://ebookmass.com/product/manual-of-perioperative-care-inadult-cardiac-surgery-5th-edition-ebook-pdf/
Landscape Architecture, Fifth Edition: A Manual of Environmental Planning and Design 5th Edition, (Ebook PDF)
https://ebookmass.com/product/landscape-architecture-fifthedition-a-manual-of-environmental-planning-and-design-5thedition-ebook-pdf/
Laboratory Manual for Anatomy & Physiology (Anatomy and Physiology) 5th Edition, (Ebook PDF)
https://ebookmass.com/product/laboratory-manual-for-anatomyphysiology-anatomy-and-physiology-5th-edition-ebook-pdf/
2010
Lippincott Williams & Wilkins
Philadelphia
Two Commerce Square, 2001 Market Street, Philadelphia, PA 19103
978-1-60547-595-0
© 2010 by LIPPINCOTT WILLIAMS & WILKINS, a WOLTERS KLUWER business
Two Commerce Square, 2001 Market Street, Philadelphia, PA 19103, LWW.com
All rights reserved. This book is protected by copyright. No part of this book may be reproduced in any form or by any means, including photocopying, or utilized by any information storage and retrieval system without written permission from the copyright owner.
The publisher is not responsible (as a matter of product liability, negligence, or otherwise) for any injury resulting from any material contained herein. This publication contains information relating to general principles of medical care that should not be construed as specific instructions for individual patients. Manufacturers' product information and package inserts should be reviewed for current information, including contraindications, dosages, and precautions.
Printed in China
Acquisitions Editor: Robert Hurley
Product Manager: Elise M. Paxson
Production Manager: Alicia Jackson
Senior Manufacturing Manager: Benjamin Rivera
Marketing Manager: Lisa Lawrence
Design Coordinator: Doug Smock
Production Service: Aptara, Inc.
Introduction to Evidence-Based Validity and Reliability of Physical Examination Procedures
Orthopedic and neurological physical examination procedures are an integral part of the clinical examination. Musculoskeletal and neurological complaints are common problems that are seen frequently in many practitioners' offices. Comprehensive history taking and physical examination procedures are the mainstay of any musculoskeletal and neurological evaluation. Advanced imaging is also an integral part of the evaluation process. Due to the rise of advanced imaging such as magnetic resonance imaging (MRI), physical examination procedures have garnered less research than advanced diagnostic testing. If more research was conducted on clinical examination procedures, much of today's diagnostic testing may become unnecessary.
Due to this lack of research, validity and reliability of many common orthopedic and neurological tests are undocumented. The literature is full of descriptions of various tests but little exists for guidance of validity and reliability of most testing procedures. When literature is available for validity and reliability of common tests, the results greatly vary from study to study1. Unfortunately, there is no true gold standard in which to assess the validity and reliability of physical examination procedures. This being said, these procedures should not be discounted, but rather more research is needed to better understand each test and ultimately come to a standardization of physical examination procedures.
Diagnostic Accuracy
Research that is available and address diagnostic accuracy of physical examination procedures should be well-designed and of
high quality. The quality of studies concerning physical examination procedures varies greatly. The scientific community has produced some tools to aid in the critique and quality of publications concerning physical examination procedure research2,3,4. One of the methods used is by Whiting et al.5 Called quality assessment of diagnostic accuracy studies (QUADAS) (Table 1), this was developed to assess the quality of research studies involving diagnostic accuracy. QUADAS involves the scoring of 14 components of individual studies. Each step is scored as a “yes”, “no” or “unclear.” A score of seven or greater registered “yes” responses indicates a high-quality study; those scores below 7 indicate lowquality studies. The QUADAS tool provides a format in which the reader can evaluate the validity of studies that attempt to evaluate physical diagnostic testing procedures.
Table 1. Quality Assessment of Diagnostic Accuracy Studies (QUADAS) Tool
1. Was the spectrum of patients representative of the patients who received the test in practice? Y N UNCLEAR
2. Were selection criteria clearly described? Y N UNCLEAR
3. Is the reference standard likely to classify the target condition correctly?
Y N UNCLEAR
4. Is the period between reference standard and index test short enough to be reasonably sure that the target condition did not change between the two tests?
Y N UNCLEAR
5. Did the whole sample or a random selection of the sample receive verification using a reference standard of diagnosis?
Y N UNCLEAR
6. Did patients receive the same reference standard regardless of the index test result?
Y N UNCLEAR
7. Was the reference standard independent of the index test (i.e., the index test did not form part of the reference standard)?
Y N UNCLEAR
8. Was the execution of the index test described in sufficient detail to permit replication of the test?
Y N UNCLEAR
9. Was the execution of the reference standard described in sufficient detail to permit replication of the test?
Y N UNCLEAR
10. Were the index test results interpreted without knowledge of the results of the reference standard?
Y N UNCLEAR
11. Were the reference standard results interpreted without knowledge of the results of the index test?
Y N UNCLEAR
12. Were the same clinical data available when the test results were interpreted as would be available when the test is used in practice?
Y N UNCLEAR
13. Were uninterpretable/intermediate test results reported?
Y N UNCLEAR
14. Were withdrawals from the study explained?
Y N UNCLEAR
Once the study quality is evaluated based on criteria such as QUADAS, we can then look at validity, reliability, specificity and sensitivity.
Validity
Validity of physical examination procedures is assessed in two ways. First is the internal validity of the test or procedure. This would include the conclusions from research data obtained from a study that correctly represents and validates the clinical question being researched.
External validity is outside of the research setting and in the clinical setting, based on real-world clinical practice. Can the conclusions of the study be transferred into the clinical setting and are the outcomes the same? Many factors such as errors in design study, oversimplified research, measurement errors, clinical characteristics and demographics of the study population may influence the accuracy and validity of both internal and external validity.
Reliability
Reliability is the concept of reproducibility. Can the results of the study be replicated and reproduce consistently the same conclusion found in the study? Precision, which is part of the reliability factor, is the uniformity and consistency of the data and is affected by random error. If random error in the study is high, then the precision of the study is low (5m).
Reliability must take into account intra- and inter-observer reproducibility. Intra-observer reproducibility requires that repeated measurements be reproducible by a single observer. Inter-observer reproducibility requires that repeated measurements be reproduced by separate observers of the same event.
After determining the validity and reliability, the next step is to ascertain the sensitivity/specificity of the procedure.
Sensitivity/Specificity
Sensitivity and specificity is determined by data that include true positives, true-negatives, false-positives and false-negatives.
A. A true-positive indicates that the test or procedure is positive and the patient truly has the pathology that the maneuver is attempting to discover.
B. A false-positive indicates that the test or procedure is positive and that the patient does not have the pathology that the maneuver is attempting to discover.
C. A false-negative indicates that the test or procedure is negative and the patient truly has the pathology.
D. A true-negative indicates that the test or procedure is negative but the patient truly does have the pathology.
Sensitivity indicates the ability of the test to identify the injury or disease. For the test to be highly sensitive for presence of the injury or disease, a positive test would have an outcome that includes a true-positive (a) and a false-negative (c).
Sensitivity = (a) + (c).
Specificity indicates the ability of the test to identify the absence of the injury or disease.
For the test to be highly specific for the absence of injury or disease, a negative test would have an outcome that includes a false-positive (b) and a true-negative (d).
Specificity = (b) + (d).
Summary
Evaluating physical examination procedures through high-quality studies gives us better clinical evidence as to the value of individual tests and
procedures. This will lead the clinician to pick tests that will support more accurately the given diagnosis.
Evidence-based practice should combine clinical expertise with best available clinical evidence. This should include a literature search, appraisal of the literature, integration of the literature with your clinical expertise and unique patient circumstances, implementation of the findings and outcome assessment.
Obtaining an accurate diagnosis requires a systemic logical approach that is based on the knowledge, experience and interpersonal skills of the clinician. The goal of the clinician is to accurately diagnose the patient's condition and effectively treat the condition based on sound evidence-based parameters.
References
1. Sackett DL, Rennie D. The science and the art of clinical examination. JAMA. 1992;267:2650–2652.
2. Deeks JJ. Systematic reviews in health care: systematic reviews of evaluations of diagnostic and screening tests. BMJ. 2001;323:157–162.
3. Lijmer JG, Mol BW, Heisterkamp S, et al. Empirical evidence of design-related bias in studies of diagnostic tests. JAMA. 1999;282: 1061–1066.
4. Reid, MC, Lachs MS, Feinstein AR. Use of methodological standards in diagnostic test research: getting better but still not good. JAMA. 1995;274:645–651.
5. Whiting P, Rutjes AW, Dinnes J, Reitsma J, Bossuyt PM, Kleijnen J. Development and validation of methods for assessing the quality of diagnostic accuracy studies. Health Technol Assess. 2004;1–234.
Functional testing
During the clinical assessment, it is necessary to document findings. The most common method to record the outcome of the assessment is through a problem-oriented records method that uses a SOAP (subjective, objective, assessment, plan) note format (Box 1-2).
Box 1-2 Soap Notes
Subjective The subjective portion is evaluated by taking the patient's history
Objective The objective portion is evaluated by observation and special tests that measure an objective component.
Assessment The assessment is based on the compilation of the subjective and objective findings and the examination
Plan The plan may include further testing and/or treatment options
The clinical assessment protocol is a comprehensive, organized, and reproducible system. This protocol is an essential tool for evaluating musculoskeletal and neurologic disorders.
Patient History
A complete history is one of the most important aspects of the clinical assessment protocol. A complete and thorough history is invaluable in assessing the patient's condition. At times, a history alone may lead to a proper diagnosis. The examiner should place emphasis on the aspect of the patient's history with the greatest clinical significance. Although concentrating on the area of greatest clinical significance, the examiner must not forget to acquire all of the patient's history, whether or not it seems relevant at the time. There may come a time during the clinical assessment that the information that seemed irrelevant is quite useful. History may also help to determine the personality type of the patient and his or her ability or willingness to follow directions. Patients who have a history of using an inordinate number of clinicians for the same disorder and receiving little or no help from them may be
unwilling or unable to perform certain functions to better their condition.
It is important that the examiner keep the patient focused on the problem and discourage wandering from the presenting condition. To achieve a good history it is essential to listen carefully to the patient's concerns about his or her problem and the expectations for diagnosis and treatment. When acquiring information from the patient the examiner must not lead the patient into answering questions, such as, “Is this movement painful?” Instead the examiner should say something like, “What do you feel with this movement?”
This history should concentrate on, but not be limited to, the patient's chief complaint, past history, family history, occupational history, and social history. History taking should be accomplished in two steps:
Closed-Ended History
The first step is a closed-ended question and answer format in which the patient answers direct, pointed questions. This step can be accomplished in a written form that the patient fills out.
Open-Ended History
After the closed-ended history is complete, the patient and examiner should engage in an open dialog to discuss the patient's condition. A closed-ended history may lead the examiner to the patient's problem but may not address the patient's fears or concerns regarding this condition. The patient may also have other problems either directly or indirectly related to the presenting complaint that may not be addressed by a closed-ended history.
An open-ended history may take on a discussion format in which the examiner and patient ask questions of each other. In this way, the examiner acquires extra needed information about the patient and the patient's complaint. All aspects of the patient's complaint should be explored and evaluated to its fullest. The examiner should develop a good rapport with the patient, keeping the patient focused on the presenting problem and discouraging irrelevant topics. The pneumonic OPQRST (onset, provoking or palliative concerns, quality of pain,
radiating, site and severity, time) may be incorporated into this evaluation (Box 1-3).
Box 1-3 Opqrst Mnemonic
Onset of complaint
Provoking or palliative concerns
Quality of pain
Radiating to a particular area
Site and severity of complaint
Time frame of complaint
Once the examiner has determined all aspects of the presenting complaint, it is time to focus on the history. Has the patient had prior problems with this or any other complaint? This information may assist with both assessment of the problem and insight on how to treat the problem.
Family history can give a clue about the patient's propensity of inheriting familial diseases. A significant number of neurologic problems and many orthopaedic problems can be traced to family members.
Occupational and social histories are also important because they may lead to a factor causing the patient's problem, such as an overuse syndrome. They can also help to determine whether the patient's condition will respond more favorably if the patient refrains from performing certain work or social functions. For example, lifting, bending, and playing tennis or golf may be contraindicated. The patient may also need to be retrained for other types of work.
Observation/Inspection
Observe the patient for general appearance and functional status. Note the body type, such as slim, obese, short, or tall, and postural deviations for general appearance, gait, muscle guarding, compensatory or substitute movements, and assistive devices for functional status.
Inspection should be divided into three layers: skin, subcutaneous soft tissue, and bony structure. Each layer has its own special characteristics for determining underlying pathology or dysfunction.
Skin
Skin assessment should begin with common and obvious findings, such as bruising, scarring, and evidence of trauma or surgery. Then look for changes in color, either from vascular changes accompanying inflammation or from vascular deficiency, such as pallor or cyanosis. Large, brownish, pigmented areas and/or hairy regions, especially on or near the spine, may indicate a bony defect such as spina bifida. Changes in texture may accompany reflex sympathetic dystrophies. Open wounds should be evaluated for either traumatic or insidious origin, which may accompany diabetes.
Subcutaneous Soft Tissue
Subcutaneous soft tissue abnormalities usually involve either inflammation and swelling or atrophy. When evaluating for an increase in size, attempt to identify edema, articular effusion, muscle hypertrophy, or other hypertrophic changes. Also note any nodules, lymph nodes, or cysts. Establish any inflammation by comparing bilateral symmetry for the torso and circumferential measurements for the extremities.
Bony Structure
Bony structure should be evaluated, especially when the patient presents with a functional abnormality, such as a gait deviance or an altered range of motion. Bony inspection in the spine should focus on items such as scoliosis, pelvic tilt, and shoulder height. Note and possibly measure malformations in the extremities that may be congenital or traumatic. Two examples of congenital malformations are genu varus and genu valgus. Traumatic malformations include a healed Colles' fracture with residual angulation. All bony structures should be visually assessed for abnormalities and documented.
Gait
Gait analysis is important in assessing neurological and/or musculoskeletal dysfunction. Gait is an important aspect of inspection which may lead you to specific diagnostic conclusions. Gait is particular to each individual, although there are normal characteristics of gait, deviation of normal may not necessarily be pathologic. Dysfunctional gait patterns noted during inspection may lead to an expedited diagnosis.
A complete gait cycle is a functional event that occurs between the time one foot contacts the ground to the point where the same foot contacts the ground again. The gait cycle consists of two time periods. One is the stance phase which includes the heel strike and flatfoot. This is where the heel strikes the ground and then the forefoot is in contact with the ground resulting with the limb weight bearing. The end of this phase results in the opposite foot leaving the ground. The next time period, is called the swing phase. The swing phase begins with the foot lifted from the ground and ends with the initial contact of the opposite foot striking the ground. Approximately 60% of the gait cycle is in the stance phase and approximately 40% of the gait cycle is in the swing phase. Most gait abnormalities are produced during the stance phase because this is the phase that produces weight bearing.
Palpation
Palpate the patient in conjunction with inspection; the structures being inspected are the same ones that should be palpated. The layers are the same for palpation as for inspection, skin, subcutaneous soft tissue, and bony structures.
When palpating the skin, begin with a light touch, especially if nerve pressure is suspected. Pressure on a nerve may result in dysesthesia, which may feel like an exaggerated burning sensation to the patient.
Skin
Evaluate skin temperature first. High skin temperature may indicate an underlying inflammatory process. Low skin temperature may indicate a vascular deficiency. Also, evaluate skin mobility for adhesions, especially after surgery or trauma.
Subcutaneous Soft Tissue
The subcutaneous soft tissue consists of fat, fascia, tendons, muscles, ligaments, joint capsules, nerves, and blood vessels. Palpate these structures with more pressure than for skin. Tenderness is a subjective complaint that should be noted. It may be caused by (a) injury; (b) pathology that correlates directly to the tenderness, such as tenderness at the supraspinatus ligament for supraspinatus tendinitis; or (c) a referred component, such as tenderness in the buttock area from a lumbar injury or pathology. Determine tenderness by applying pressure to the area and grade it according to the patient's response (Box 1-4).
Evaluate swelling or edema according to its origin. Determine if the inflammation is intra-articular or extra-articular. In intra-articular effusion, the fluid is confined to the joint capsule. In extra-articular effusion, the fluid is in the surrounding tissues. Various palpation techniques are discussed in detail in the chapters on specific areas of the body.
Box 1-4 Tenderness Grading Scale
Grade I Patient complains of pain.
Grade II Patient complains of pain and winces.
Grade III Patient winces and withdraws the joint.
Grade IV Patient will not allow palpation of the joint.
There are different types of swelling or edema, according to onset and palpation feel. If swelling occurs immediately after an injury and feels hard and warm, the swelling contains blood. If the swelling occurs 8 to 24 hours after an injury and feels boggy or spongy, the swelling contains synovial fluid. If the swelling feels tough and dry, it is most likely a callus. If the feeling is thickened or leathery, it is most likely chronic swelling. If the swelling or edema is soft and fluctuating, it is most likely acute. If the feeling is hard, it is most likely bone. If the feeling is thick and slow moving, it is most likely pitting edema.
Pulse
Pulse amplitude in certain arteries is important. It is used to assess the vascular integrity of an area and plays an integral part in certain tests for thoracic outlet syndrome, arterial insufficiency, and vertebrobasilar compromise.
Bony Structures
Bony structure palpation is critical for the detection of alignment problems, such as dislocations, luxations, subluxations, and fractures. When you palpate bony structures, you must also identify the ligaments and tendons that attach to those structures. Tenderness is a major finding in bony palpation. It may indicate periosteoligamentous sprain. It also may indicate fracture. Bony enlargements usually are associated with healing of fractures and degenerative joint disease.
Range of Motion Evaluation
Range of motion evaluation is not only a measurement of function but also an important part of biomechanical analysis. Range of motion is evaluated for three separate types of functions: passive motion, active motion, and resisted motion.
Passive Range of Motion
In passive motion, the examiner moves the body part for the patient without the patient's help. It can yield a significant amount of information about the underlying pathology. The goal obviously depends on which joint is being tested and what pathology or injury is suspected. In evaluating such motion, first note whether the movement is normal, increased, or decreased and in which planes. Second, note any pain. Classically, pain on passive range of motion indicates a capsular or ligamentous lesion on the side of movement and/or a muscle lesion on the opposite side of movement. Various other problems may be detected, depending on the degree of mobility and pain. Six possible variations of range of motion pain are shown in Box 1-5.
Box 1-5 Six Range of Motion and Pain Variations
1. Normal mobility with no pain indicates a normal joint with no lesion.
2. Normal mobility with pain elicited may indicate a minor sprain of a ligament or capsular lesion.
3. Hypomobility with no pain may indicate an adhesion of a particular tested structure.
4. Hypomobility with pain elicited may indicate an acute sprain of a ligament or capsular lesion. When an injury is severe, hypomobility and pain may also be a sign of muscle spasm caused by guarding or by muscle strain opposite the side of movement.
5. Hypermobility with no pain suggests a complete tear of a structure with no fibers intact where pain can be elicited. It may also be normal if other joints in the absence of trauma are also hypermobile.
6. Hypermobility with pain elicited indicates a partial tear with some fibers still intact. Normal pressure by the weight of structure that is attached to the ligament or capsule is being exerted. This pressure on the intact fibers can elicit pain.
After you determine the degree of passive range of motion and evaluate for pain, evaluate for an end feel. To determine end feel, passively move the joint to the end of its range of motion and then apply slight overpressure to the joint. The quality of the feeling that this elicits is the end feel, assessed as either normal (physiologic) or abnormal (pathologic) (Table 1-1).
Active Range of Motion
Active range of motion evaluates the physical function of a body part. This type of range will yield general information regarding the patient's general ability and willingness to use the part. If a patient is asked to
move a joint through a full arc of movement and cannot, it is impossible to distinguish whether the loss of function is caused by pain, weakness caused by a neurologic motor dysfunction, stiffness, or the conscious unwillingness of the patient to perform the full function. Therefore, the assessment value of active range of motion in and of itself is vague and limited. Active motion is a basic test for the integrity of the muscle or muscles used in the action and the nerve supply attached to the muscle. Obviously, the integrity of the joint being tested must be intact to evaluate muscular or neurologic dysfunction. This integrity is best evaluated by passive range of motion.
When evaluating active motion, note the degree of motion in the tested plane as well as any pain associated with the movement. The pain should be correlated with the movement, such as pain in the full arc or only in the extreme range of motion. Crepitus should also be noted when performing active range of motion. Crepitus is a crackling sound that usually indicates a roughening of joint surfaces or increased friction between a tendon and its sheath (caused by swelling or roughening).
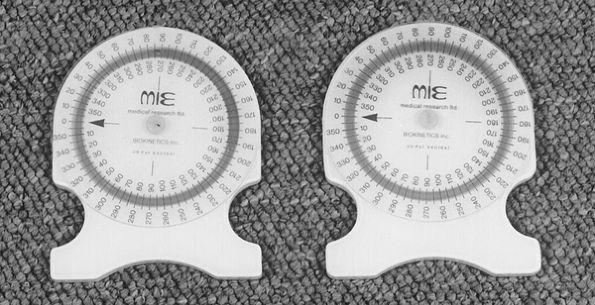
Joint range of motion should be measured and recorded by commonly accepted reproducible means. To measure the range of motion of the spine, the most accurate instrument is the inclinometer (Fig. 1-1). This instrument measures angular displacement relative to gravity as opposed to arcs. The reason for inclinometer measurement of the spine is that the spine is composed of multiple joints that function in unison to produce movement. A device that measures arcs, such as a goniometer (Fig. 1-2), cannot distinguish the difference between sacral flexion and lumbar flexion in the lower back when the patient is bending forward. In this particular instance, the inclinometer can distinguish between true lumbar flexion and sacral or hip flexion (see inclinometer range of motion in Chapters 3, 9, and 10). Goniometers are best suited to measure extremity range of motion.
Table 1-1 End Feel Evaluation
Category Normal Physiologic End Feels
Hard Abrupt hard to stop movement when bone contacts bone Example: passive elbow extension. Olecranon process contracts the olecranon fossa
Soft When two body surfaces come together, a soft compression of tissue is felt. Example: Passive elbow flexion. Anterior aspect of the forearm approximates the biceps muscle.
Firm A firm or spongy sensation that has some give when a muscle, ligament, or tendon is stretched. Example: Passive wrist flexion, passive external shoulder rotation.
Springy, block
Abnormal Pathologic End Feels
Abrupt stopping movement before normal expected passive movement. Example: Cervical flexion hard end feel due to severe degenerative joint disease.
A soft boggy sensation resulting from synovitis or soft tissue edema.
Example: Ligamentous sprain.
A firm springy sensation to movement with a slight amount of give in capsular joints.
Example: Frozen shoulder.
Rebound effect with limited motion; usually in joints with a meniscus.
Example: Torn meniscus.
Empty
An empty feel in a joint with severe pain when passively moved. The movement cannot be performed because of the pain.
Example: Fracture, subacromial bursitis, neoplasm, joint inflammation.
Figure 1-1
Figure 1-2
Resisted Range of Motion
Resisted range of motion is useful in assessing musculotendinous and neurologic structures. It is primarily used to test neurologic function (see nerve root lesions). The tests are graded 5 to 0, a scale that has been adopted by the American Academy of Orthopaedic Surgeons (Box 16).
Musculotendinous injuries are generally more painful than they are weak. Neurologic lesions are generally more weak than they are painful. The four general pain-related reactions to resisted range of motion testing are listed in Box 1-7.
Box 1-6 Muscle Grading Scale
5 Complete range of motion against gravity with full resistance
4 Complete range of motion against gravity with some resistance
3 Complete range of motion against gravity
2 Complete range of motion with gravity eliminated (movement in the horizontal plane)
1 Evidence of slight contractility
0 No evidence of contractility
Box 1-7 Resistant Range of Motion Reactions
1. Strong with no pain elicited is normal and not indicative of any lesions.
2. Strong with pain elicited may indicate a minor lesion of the muscle or tendon.
3. Weak and painless may indicate a neurologic lesion, which must be evaluated with the previous chart. It may also indicate a complete rupture of a tendon or muscle because there are no fibers intact from which pain can be elicited.
4. Weak and painful may indicate a partial rupture of a muscle or tendon because intact fibers may be stressed to produce pain. Fracture, neoplasm, and acute inflammation are also possibilities.
Special Physical, Orthopaedic, and Neurologic Testing
Special physical, orthopaedic, and neurologic testing is designed to place functional stress on isolated tissue structures in terms of the underlying pathology. Positive physical testing is not diagnostic in itself but rather a biomechanical assessment to be used as part of a complete clinical evaluation.
Before performing certain special tests, you must ascertain that they will not be detrimental to the patient's condition. Box 1-8 lists the conditions for which care must be taken when performing either range of motion testing or special physical orthopaedic and neurologic testing.
Box 1-8 Physical Examination Precautions
Dislocation
Unhealed fracture
Myositis ossificans/ectopic ossification
Joint infection
Marked osteoporosis
Bony ankylosis
Newly united fracture
After surgery
If it is determined that special physical testing may indeed harm the patient, structural and/or functional testing, such as radiography, CT, MRI, or electromyography (EMG), should be employed before any physical testing.
The subsequent chapters contain a collection of special physical orthopaedic and neurologic tests organized anatomically and subcategorized by diagnostic entity. This system is best suited for expedient evaluation of musculoskeletal and orthopaedic neurologic conditions. Each test illustrates and discusses the procedures for correct performance of the test. Each test is accompanied by an explanation that indicates the positive indicators for that test and what they may mean in terms of an underlying pathology or injury. Biomechanical considerations that may not be evident in the classical interpretation of a particular test are also explored.
Best Practice Utility Scale (Bpus)
In this edition, I have changed the sensitivity/reliability scale to a Best Practice Utility Scale (BPUS) in order to evidence new research. I have added a BPUS to each of the tests described in this text. For each diagnosis presented, there are multiple tests. Some of those tests are more diagnostically valuable than others. I have attempted to rate each test based on currently available research. The scale is numbered from 0 to 4, with 1 to 2 being poorly diagnostically valuable, 2 to 3 being moderately diagnostically valuable, and 3 to 4 being very diagnostically
valuable. Those tests that are very diagnostically valuable should be performed first. This will help in evaluating the patient's condition more expeditiously.
Diagnostic Imaging and Other Specialized Structural Testing
Diagnostic imaging or structural testing entails the use of specialized equipment to visualize certain anatomic structures. The most common diagnostic imaging procedures include plain film radiology (x-ray), CT, MRI, and skeletal scintigraphy (bone scan). Each type of structural test may be best suited to visualize various structures in specific ways.
Plain Film Radiology
Plain film radiology dates to 1895, and its fundamentals are still used in practice today. X-rays are a form of radiant energy that have a short wavelength and can penetrate many substances (Fig. 1-3).
The x-ray is produced by bombarding a tungsten target with an electron beam in an x-ray tube. Plain film radiography demonstrates five basic densities: air, fat, subcutaneous tissue, bone, and metal. Anatomic structures are seen on radiographs as outlines in whole or as part of different tissue densities. These differences in densities are the key to determining the normal or pathologic state of tissues shown on radiographic film. Bone is the best-seen tissue on plain film radiography.
1-3
Computed Tomography
Computed tomography is a cross-sectional imaging technique that uses x-ray as its energy (Fig. 1-4). A computer is used to reconstruct a crosssectional image from measurements of x-ray transmission. Most CT units allow for a slice thickness between 1 and 10 mm and are generally limited to the axial plane. CT is best used for bone detail and demonstration of calcifications. Intervertebral disc defects may also be visualized on CT, but not as well as with MRI.
Figure
1-4
Magnetic Resonance Imaging
MRI is also a cross-sectional imaging technique (Fig. 1-5). It uses magnetic fields and radio waves instead of x-rays to produce its images. MRI is based on the ability of the body to absorb and emit radio waves when the body is in a strong magnetic field. The absorption and release of this energy is different and detectable in each individual type of tissue. Hence, MRI is invaluable in contrasting soft tissue structures in many planes without the use of ionizing radiation. It poorly demonstrates bone density detail or calcifications; this is the advantage of CT. MRI is superior in visualizing an intervertebral disc or other soft tissue structure for pathology.
Patients with any metallic implants or metal fragments (e.g., cardiac pacemakers, insulin pumps, vascular clips, skin staples, bullets, or shrapnel) are advised not to undergo MRI because of the strong magnetic field emitted by the scanner. This field may move or dislodge metallic implants or objects in an individual whose body is being scanned.
Figure
1-5
Myelography
Myelography introduces a small amount of water-soluble contrast medium into the subarachnoid space (Fig. 1-6). Standard x-ray films of the spine are then taken to evaluate and defects of the spinal canal, such as spinal stenosis, spinal cord lesions, and dural tears.
Figure