Acknowledgments
DeWit’s Fundamental Concepts and Skills for Nursing is the result of the creative efforts of many people. First of all, I owe a deep debt of gratitude to Susan de Wit for being a wonderful mentor and passing along such a ine textbook and entrusting me with its future. You set the bar very high and have taught me so very much over the past several years.
I am especially grateful to the contributors, consultants, and reviewers for their expertise, suggestions, and inished work. Their perspectives from the various geographic areas of the United States and Canada have lent a broader viewpoint of current nursing practice.
The dedicated staff at Elsevier has provided tireless support and expertise from the initial concept of the book to the cohesive inished product. I am very grateful to Nancy O’Brien, Senior Content Strategist, who helped guide this project from start to inish and was never too busy to answer any question no matter how small. Bill Drone, Production Manager, made certain that problems were solved and skillfully attended to all aspects of production and printing of the text. Becky Leenhouts, Senior Content Development Specialist, was simply amazing with her creativity, diligence, and attention to detail. Brittany Clements, Marketing Manager, applied her creative ideas to promote the book
and announce its presence to students and instructors. The design of the book, following the Threads design of other Elsevier LPN/LVN texts, was provided by Renee Duenow. Thanks for all the efforts of these diligent, creative, professional people.
The artistry, many hours, and creative eye of Jack Sanders, our photographer, lent the visual appeal and clinical detail needed to illustrate the concepts and skills of much of this edition, as well as the previous editions. Ginger Navarro, RN, did a wonderful job coordinating the photography shoots, facilities, and models at PeaceHealth for the past three editions of the book.
Many thanks also to PeaceHealth Southwest Washington Medical Center, the De Anza College Nursing Skills and Simulation Lab, and Bay Area Surgical Specialists Surgery Center for the opportunity to photograph within the facilities. Thanks to the many employeesandnursingstudentswhocontributedtheirtimeand talents to the ifth edition as models. Much appreciation to all my nursing colleagues who comprise my e-mail network across the country and who contributed expertise and encouragement throughout the project.
Patricia Williams, MSN, RN, CCRN
UNIT I INTRODUCTION TO NURSING AND THE HEALTH CARE SYSTEM, 1
1 Nursing and the Health Care System, 1
Historical Overview, 1
Nursing in England and Europe, 1
Nursing in North America, 2
The Art and Science of Nursing, 3
Evidence-Based Practice, 4
Current Nursing Practice, 6
Nursing Education Pathways, 7
Practical Nursing, 7
Registered Nursing, 7
Advanced Practice Nursing, 8
Delivery of Nursing Care, 8
Practice Settings, 9
Today’s Health Care System, 9
Health Maintenance Organizations, 10
Preferred Provider Organizations, 10
The Patient Protection and Affordable Care Act, 11
2 Concepts of Health, Illness, Stress, and Health Promotion, 14
Health and Illness, 14
Traditional Views of Health and Illness, 15
Stages of Illness, 15
Current Views of Health and Illness, 16
Implications of Current Views, 17
The Consumer Concept of Health and Illness, 17
Health and Illness Behaviors, 17
Cultural Inluences on Concepts of Health and Illness, 17
The Holistic Approach, 19
Maslow’s Theory of Basic Needs, 19
Homeostasis, 22
Adaptation, 22
The Effects of Stress, 26
Defense Mechanisms, 26
Stress-Reduction Techniques, 26
Health Promotion and Illness Prevention, 26
3 Legal and Ethical Aspects of Nursing, 30
Source of Law, 31
Civil and Criminal Law, 32
Laws Related to Nursing Practice and Licensure, 32
Nurse Practice Act, 32
Scope of Practice, 32
Licensure, 32
Professional Accountability, 33
Professional Discipline, 33
Continuing Education, 33 Laws and Guidelines Affecting Nursing Practice, 33
Occupational Safety and Health Administration, 33
Child Abuse Prevention and Treatment Act, 34 Discrimination, 34
Sexual Harassment, 34
Good Samaritan Laws, 35 Patient’s Rights, 35
National Patient Safety Goals, 35 Legal Documents, 36
The Medical Record, 36 Health Insurance Portability and Accountability Act, 37
Consents and Releases, 38 Witnessing Wills or Other Legal Documents, 39 Advance Directives, 39 Violations of Law, 39 Negligence and Malpractice, 39
Common Legal Issues, 40
Decreasing Legal Risk, 42 Ethics in Nursing, 43 Codes of Ethics, 43 Ethics Committees, 45 Ethical Dilemmas, 45
UNIT II THE NURSING PROCESS, 48
4 The Nursing Process and Critical Thinking, 48
The Nursing Process, 48 Critical Thinking, 50
Problem Solving and Decision Making, 50 Skills for Critical Thinking, 51 Critical Thinking in Nursing, 51 Priority Setting and Work Organization, 53 Application of Problem Solving and Clinical Reasoning, 53
5 Assessment, Nursing Diagnosis, and Planning, 57 Assessment (Data Collection), 57
The Interview, 59
Medical Records (Chart) Review, 59
Physical Assessment, 62
Assessment in Long-Term Care, 63
Assessment in Home Health Care, 63 Analysis, 63
Nursing Diagnosis, 64
Etiologic Factors, 65
Deining Characteristics, 65
Prioritization of Problems, 65
Nursing Diagnosis in Long-Term Care, 66
Nursing Diagnosis in Home Health Care, 66 Planning, 66
Expected Outcomes (Goals), 66
Planning in Long-Term Facilities, 68
Planning in Home Health Care, 68
Interventions (Nursing Orders), 68
Documentation of the Plan, 69
6 Implementation and Evaluation, 73 Implementation, 73
Priority Setting, 73
Considerations for Care Delivery, 74 Interdisciplinary Care, 74
Implementing Care, 75
Documentation of the Nursing Process, 75 Evaluation, 76
Evaluation in Long-Term Care, 77 Evaluation in Home Health Care, 77
Revision of the Nursing Care Plan, 77
Quality Improvement, 77
Constructing a Nursing Care Plan, 78
UNIT III COMMUNICATION IN NURSING, 84
7 Documentation of Nursing Care, 84
Purposes of Documentation, 84
Documentation and the Nursing Process, 86
The Medical Record, 86
Methods of Documentation (Charting), 86
Source-Oriented or Narrative Charting, 88
Problem-Oriented Medical Record Charting, 88
Focus Charting, 89
Charting by Exception, 90
Computer-Assisted Charting, 90
Case Management System Charting, 94
The Documentation Process, 95
Accuracy in Documentation, 95
Brevity in Documentation, 95
Legibility and Completeness in Documentation, 95 What to Document, 98
8 Communication and the Nurse-Patient Relationship, 101
The Communication Process, 101
Factors Affecting Communication, 102 Communication Skills, 103
Therapeutic Communication Techniques, 104
Using Silence, 105
Asking Open-Ended Questions, 105
Restating, 106
Clarifying, 106
Using Touch, 106
Using General Leads, 106
Offering of Self, 106
Encouraging Elaboration, 106
Providing Patient Education, 106
Looking at Alternatives, 107
Summarizing, 107
Blocks to Effective Communication, 107
Changing the Subject, 107
Offering False Reassurance, 110
Giving Advice, 110
Using Defensive Comments, 110
Asking Prying or Probing Questions, 110
Using Clichés, 110
Listening Inattentively, 110
Interviewing Skills, 110
The Nurse-Patient Relationship, 111 Empathy, 111
Becoming Nonjudgmental, 112
Maintaining Hope, 112
Nurse-Patient Communication, 112
Communicating with the Hearing-Impaired Patient, 113
Communicating with an Aphasic Patient, 113
Communicating with Older Adults, 113 Communicating with Children, 114
Communication Within the Health Care Team, 114 End-of-Shift Report, 114
Telephoning Primary Care Providers, 115
Assignment Considerations and Delegating, 115 Computer Communication, 117 Communication in the Home and Community, 117
9 Patient Education and Health Promotion, 120
Purposes of Patient Education, 120 Modes of Learning, 121 Assessment of Learning Needs, 121 Factors Affecting Learning, 122
The Patient Education Plan, 124 Resources for Patient Education, 125
Implementing the Plan, 125 Evaluation, 126 Documentation, 127
Coordination with Discharge Planning, 127
10 Delegation, Leadership, and Management, 129
The Chain of Command, 130 Leadership Styles, 130
Keys to Effective Leadership, 130
Effective Communication and Relationships, 130
Clinical Competence and Conidence, 132 Organization, 132
Delegation, 132
Leadership Roles, 133
Beginning Leadership Roles, 133
Advanced Leadership Roles, 134 Management Skills for the Licensed Practical Nurse/Licensed Vocational Nurse, 134 Time Management, 135
Using the Computer, 135
Receiving New Orders, 137
Taking Verbal Orders, 137
Documenting for Reimbursement, 138 Risk Management, 138
UNIT IV DEVELOPMENTAL, PSYCHOSOCIAL, AND CULTURAL CONSIDERATIONS,
141
11 Growth and Development: Infancy Through Adolescence, 141
OVERVIEW OF STRUCTURE AND FUNCTION, 142
Prenatal Development, 142
What Happens in the Germinal Stage of Prenatal Development? 142
What Happens in the Embryonic Stage of Prenatal Development? 142
What Happens in the Fetal Stage of Prenatal Development? 142
What Causes Multiple Births? 142
Adolescent Development, 143
How Does a Girl Mature into a Woman? 143
How Does a Boy Mature into a Man? 143
Age Groups, 143
Theories of Development, 143 Principles of Growth and Development, 145
Prenatal Development, 145
Events in Prenatal Development, 145
Maternal Inluences, 146 Infants, 146
Nutrition, 146
Appearance and Capabilities of Newborns, 147
Physical Development, 147
Motor Development, 147
Cognitive Development, 148
Psychosocial Development, 148
Young Children, 149
Physical Development, 149
Motor Development, 150
Cognitive Development, 150
Psychosocial Development, 151
Day Care and Early Education, 152
Middle and Older Children, 152
Physical Development, 152
Cognitive Development, 152
Psychosocial Development, 153
Parenting, 153
Child Abuse, 154
Adolescents, 154
Physical Development, 154
Sexuality, 155
Cognitive Development, 155
Psychosocial Development, 155
Tasks of Adolescence, 156
Concerns in Adolescent Development, 156
12 Adulthood and the Family, 160
Adulthood as Continuing Change, 160
Theories of Development, 161
Schaie’s Theory of Cognitive Development, 161
Erikson’s Stages of Adult Psychosocial Development, 161 Families, 161
Types of Families, 161
Historical Changes in Families, 162
Divorce and Families, 162
Young Adults, 162
Physical Development, 163
Health Concerns of Young Adults, 163
Cognitive Development, 164
Psychosocial Development, 164
Developmental Tasks, 165
Middle Adulthood, 166
Physical Development, 166
Health Concerns, 167
Cognitive Development, 167
Psychosocial Development, 168
13 Promoting Healthy Adaptation to Aging, 172
Overview of Aging, 172
Theories of Aging, 173
Longevity, 173
Demographics, 174
Physical Changes, 174
Health Concerns, 176
Health Promotion Behaviors, 176
Cognitive Aspects of Aging, 177
Wisdom and Learning, 177
Memory Issues, 177
Employment and Retirement, 178
Health Promotion Behaviors, 178
Psychosocial Aspects of Aging, 178
Life Review, 178
Family Relationships, 178
Social Activity, 179
Living Arrangements, 179
Health Promotion Behaviors, 179
When a Parent Needs Help, 180
Planning Ahead, 180
Observing Changes, 180
Resources for Families, 180
14 Cultural and Spiritual Aspects of Patient Care, 183
Transcultural Care, 184 What Is Culture? 184
Understanding Spirituality, 185
Major Religions in the United States and Canada, 185 Christianity, 185 Islam, 186
Judaism, 188
Hinduism, Buddhism, and Taoism, 188
Developing Cultural Competence, 189
Barriers to Cultural Competence, 190 Cultural Differences, 190 Communication, 191 View of Time, 191
Family Organization and Structure, 191
Nutritional Practices, 191
Death and Dying, 192
Health Care Beliefs, 192
Susceptibility to Disease, 194
Nursing Process in Transcultural Nursing, 194 Assessment (Data Collection), 194
Nursing Diagnosis, 195 Planning, 195 Implementation, 195 Evaluation, 196
15 Loss, Grief, and End-of-Life Care, 198
Nurses’ Attitudes Toward End-of-Life Care, 199 Change, Loss, and Grief, 199 Change, 199 Loss, 199
Grief, 200
Stages of Grief, 200 Death and Dying, 201
End-of-Life Care Within the Health Care System, 201
Hospice and Palliative Care, 201
The Dying Process, 203 Nursing and the Dying Process, 204 Application of the Nursing Process, 205 Assessment (Data Collection), 205
Nursing Diagnosis, 205 Planning, 205 Implementation, 206 Evaluation, 208
Signs of Impending Death, 208
Physical Signs, 208
Psychosocial and Spiritual Aspects of Dying, 208
Legal and Ethical Aspects of Life-and-Death Issues, 209 Advance Directives, 209 Euthanasia, 209
Adequate Pain Control, 210
Organ and Tissue Donation, 210 Postmortem (After Death) Care, 210
16 Infection Prevention and Control: Protective Mechanisms and Asepsis, 216
Infectious Agents, 217 Bacteria, 217 Prions, 219 Viruses, 219 Protozoa, 219 Viruses, 219 Rickettsia, 219 Fungi, 219 Helminths, 219
Other Infectious Agents, 219 Process (Chain) of Infection, 219
Causative Agent (Link One), 219 Reservoir, 220
Mode of Transfer, 220 Portal of Entry, 220
Susceptible Host, 221 Body Defenses Against Infection, 223 Inlammatory Response, 224
Immune Response, 224
Asepsis and Control of Microorganisms, 226
Medical Asepsis and Surgical Asepsis, 226 Hand Hygiene, 227
Standard Precautions, 231
Cleaning and Disinfection, 236
Sepsis in the Home Environment, 237
Infection Control Surveillance, 237
17 Infection Prevention and Control in the Hospital and Home, 242 Infection, 242
Stages of Infection, 242
Health Care–Associated Infections, 243
Infection Prevention and Control, 243 Personal Protective Equipment, 245 Needle Stick Injuries, 246
Application of the Nursing Process, 246 Assessment (Data Collection), 246
Nursing Diagnosis, 246 Planning, 247 Implementation, 247 Evaluation, 260
18 Safely Lifting, Moving, and Positioning Patients, 267
OVERVIEW OF THE STRUCTURE AND FUNCTION OF THE MUSCULOSKELETAL SYSTEM, 268
Which Structures Are Involved in Positioning and Moving Patients? 268
What Are the Functions of Bones for Positioning and Moving Patients? 268
What Are the Functions of Muscles for Positioning and Moving Patients? 268
What Changes in the System Occur with Aging? 268
Principles of Body Movement for Nurses, 269
Obtain Help Whenever Possible, 269
Use Your Leg Muscles, 269
Provide Stability for Movement, 270
Use Smooth, Coordinated Movements, 270
Keep Loads Close to the Body, 270
Keep Loads near the Center of Gravity, 270 Pull and Pivot, 271
Principles of Body Movement for Patients, 271
Hazards of Improper Alignment and Positioning, 271
Application of the Nursing Process, 271 Assessment (Data Collection), 271
Nursing Diagnosis, 272 Planning, 272 Implementation, 272 Evaluation, 288
19 Assisting with Hygiene, Personal Care, Skin Care, and the Prevention of Pressure Injuries, 295
Overview of the Structure and Function of the Integumentary System, 296
What Is the Structure of the Skin? 296
What Are the Functions of the Skin and Its Structures? 296
What Changes in the System Occur with Aging? 296
Application of the Nursing Process, 296 Assessment (Data Collection), 296
Nursing Diagnosis, 301 Planning, 301 Implementation, 301 Evaluation, 319
20 Patient Environment and Safety, 321
Factors Affecting the Environment, 321
Temperature, 321
Ventilation, 322
Humidity, 322
Lighting, 322
Odor Control, 322
Noise Control, 322
Interior Design, 323 Neatness, 323
Privacy, 323
Patient Unit, 323 Beds, 323
Bed Positions, 323
Bed Making, 324
Safety, 329
Hazards, 329
Hazardous Materials, 332
Protective Devices, 335
Legal Implications of Using Protective Devices, 335
Alternatives to Protective Devices, 335
Principles Related to the Use of Protective Devices, 336
Documentation of the Use of Protective Devices, 339
21 Measuring Vital Signs, 343
Overview of Structure and Function Related to the Regulation of Vital Signs, 344
How Is Body Heat Produced? 344
What Factors Affect Body Heat Production? 344
How Is Body Temperature Regulated? 344
How Does Fever Occur, and What Are Its Physiologic Effects? 345
What Physiologic Mechanisms Control the Pulse? 345
What Is Respiration? 345
What Are the Organs of Respiration? 346
How Is Respiration Controlled? 347
What Is Blood Pressure? 347
What Physiologic Factors Directly Affect the Blood Pressure? 347
What Changes Occur in Vital Signs with Aging? 347
Measuring Body Temperature, 347
Factors Inluencing Temperature Readings, 348 Problems of Temperature Regulation, 349
Measuring Body Temperature, 350 Glass Thermometers, 351
Electronic Thermometers, 352
Disposable Thermometers, 355
Application of the Nursing Process, 355 Assessment (Data Collection), 355
Nursing Diagnosis, 355 Planning, 355 Implementation, 356 Evaluation, 356
Measuring the Pulse, 357 Common Pulse Points, 357 Pulse Rate, 358 Pulse Characteristics, 360
Application of the Nursing Process, 361 Measuring Respirations, 361
Respiratory Patterns, 362
Measuring Oxygen Saturation of the Blood, 364
Measuring the Blood Pressure, 364
Equipment Used for Measuring Blood Pressure, 365
Korotkoff Sounds, 369
Hypertension, 369
Hypotension, 370
Application of the Nursing Process, 370 Pain, the Fifth Vital Sign, 371 Automated Vital Sign Monitors, 371
Documenting Vital Signs, 371
Recording Temperature Measurements, 371
Recording Pulse Measurements, 372
Recording Respiration Measurements, 372
Recording Blood Pressure Measurements, 372
Evaluating Vital Sign Trends, 372
22 Assessing Health Status, 375
Data Collection and Assessment, 375
Application of the Nursing Process, 376 Assessment (Data Collection), 376
Nursing Diagnosis, 388 Planning, 388 Implementation, 388 Evaluation, 396
23 Admitting, Transferring, and Discharging Patients, 398
Types of Admissions, 398
Routine Admissions, 398
Emergency Admissions, 399 Admission Process, 399
Preadmission Procedures and Requirements, 399 Day of Admission, 399 Reactions to Admission, 402 Plan of Care, 402
Patient Transfer to Another Hospital Unit, 402
Discharging the Patient, 403
Discharge to an Extended-Care or Rehabilitation Facility, 403
Discharge Home, 403
Death of a Patient, 404
Providing Support for Signiicant Others, 404
Pronouncement of Death, 404
Autopsies, 405 Organ Donation, 405
24 Diagnostic Tests and Specimen Collection, 407
Diagnostic Tests and Procedures, 408
Application of the Nursing Process, 408 Assessment (Data Collection), 408
Nursing Diagnosis, 408 Planning, 408 Implementation, 408 Evaluation, 430
UNIT VI MEETING BASIC PHYSIOLOGIC NEEDS, 436
25 Fluid, Electrolyte, and Acid-Base Balance, 436
Composition of Body Fluids, 436
Water, 436
Electrolytes, 438
Nonelectrolytes, 438
Blood, 438
Distribution of Body Fluids, 438
Movement of Fluid and Electrolytes, 438
Fluid and Electrolyte Imbalances, 440
Deicient Fluid Volume, 441
Excess Fluid Volume, 442
Electrolyte Imbalances, 442
Acid-Base Balance, 447
pH, 447
Bicarbonate, 447
Control Mechanisms, 447
Acid-Base Imbalances, 447
Respiratory Acidosis, 449
Metabolic Acidosis, 449
Respiratory Alkalosis, 449
Metabolic Alkalosis, 450
Application of the Nursing Process, 450 Assessment (Data Collection), 450
Nursing Diagnosis, 451
Planning, 451
Implementation, 451 Evaluation, 455
26 Concepts of Basic Nutrition and Cultural Considerations, 458
Overview of the Structure and Function of the Gastrointestinal System, 459
Which Structures Are Involved in the Gastrointestinal (Digestive) System? 459
What Are the Functions of the Organs of the Gastrointestinal System? 459
What Changes in the Digestive System Occur with Aging? 460
Dietary Guidelines, 460
USDA Myplate and the 2015 Dietary Guidelines for Americans, 460
Protein, 462
Functions of Protein, 462
Food Sources of Protein, 462
Dietary Reference Intakes of Protein, 462
Protein Deiciency, 463
Protein Excess, 463
Vegetarian Diets, 463
Carbohydrates, 464
Functions of Carbohydrates, 464
Simple Carbohydrates, 464
Complex Carbohydrates (Starches), 464
Recommendations for Intake, 464
Fiber, 465
Fats (Lipids), 465
Functions of Fat, 465
Food Sources of Fat, 466
Vitamins, 466
Minerals, 467
Water, 469
Factors that Inluence Nutrition, 469
Age, 472
Illness, 472
Emotional Status, 472
Economic Status, 472
Religion, 472
Culture, 472
Food Safety, 472
Cultural Inluences on Nutrition, 473
African American, 473
Hispanic American, 473
Asian American, 473
Middle Eastern American, 473
Nutrition Counseling, 473
Nutritional Needs Throughout the Life Span, 473
Infants, 473
Toddlers and Preschool Children, 475
School-Age Children, 475
Adolescents, 475
Adults, 475
Older Adults, 476
Application of the Nursing Process, 477 Assessment (Data Collection), 477
Nursing Diagnosis, 479 Planning, 479
Implementation, 479 Evaluation, 480
27 Nutritional Therapy and Assisted Feeding, 484
The Goals of Nutritional Therapy, 485
The Postoperative Patient, 487
Health Issues Related to Nutrition, 487
Feeding and Eating Disorders, 487
Obesity, 489
Pregnancy, 490
Substance-Related and Addictive Disorders, 490
Disease Processes That Beneit from Nutritional Therapy, 491
Cardiovascular Disease, 491
Diabetes Mellitus, 491
HIV/AIDS, 493
Assisted Feeding, 494
Nasogastric and Enteral Tubes, 495
Percutaneous Endoscopic Gastrostomy or Jejunostomy Tubes, 496
Feeding Tubes and Pumps, 500
Total Parenteral Nutrition, 504
Application of the Nursing Process, 505 Assessment (Data Collection), 505
Nursing Diagnosis, 505 Planning, 505 Implementation, 505 Evaluation, 505
28 Assisting with Respiration and Oxygen Delivery, 508
Overview of the Structure and Function of the Respiratory System, 508
Which Structures Are Involved in Respiration? 508
What Are the Functions of the Respiratory Structures? 509
What Changes Occur with Aging That Affect Respiration? 509
Hypoxemia, 510
Symptoms of Hypoxia, 510
Pulse Oximetry, 511
Airway Obstruction and Respiratory Arrest, 511
Clearing Respiratory Secretions, 513
The Effective Cough, 513
Postural Drainage, 518
Oxygen Administration, 518
Cannula, 522
Masks, 522
Artiicial Airways, 522
Nasopharyngeal Suctioning, 524
Tracheobronchial Suctioning, 526
Tracheostomy, 529
Chest Drainage Tubes, 529
Application of the Nursing Process, 530
Assessment (Data Collection), 530
Nursing Diagnosis, 532
Planning, 532
Implementation, 533
Evaluation, 539
29 Promoting Urinary Elimination, 541
Overview of Structure and Function of the Urinary System, 542
Which Structures Are Involved in Urinary Elimination? 542
What Are the Functions of the Urinary Structures for Elimination? 542
What Factors Can Interfere with Urinary Elimination? 543
What Changes in the System Occur with Aging? 543
Normal Urinary Elimination, 543
Factors Affecting Normal Urination, 543
Characteristics of Normal Urine, 543
Alterations in Urinary Elimination, 544
Application of the Nursing Process, 545
Assessment (Data Collection), 545
Nursing Diagnosis, 547
Planning, 548
Implementation, 548
Evaluation, 570
30 Promoting Bowel Elimination, 572
Overview of the Structure and Function of the Intestinal System, 573
Which Structures of the Intestinal System Are Involved in Waste Elimination? 573
What Are the Functions of the Intestines? 573
What Effect Does Aging Have on the Intestinal Tract? 574
Characteristics of Stool, 574
Normal Characteristics of Stool, 574
Abnormal Characteristics of Stool, 574
Hypoactive Bowel and Constipation, 574
Hyperactive Bowel and Diarrhea, 576
Fecal Incontinence, 577
Application of the Nursing Process, 577 Assessment (Data Collection), 577
Nursing Diagnosis, 577 Planning, 577
Implementation, 578 Evaluation, 580
Rectal Suppositories, 580
Enemas, 580
Types of Enemas, 580
Amount and Temperature of Solution, 580
Recommended Position, 581
Rectal Tube, 581
Fecal Impaction, 583
Bowel Training for Incontinence, 584
Bowel Ostomy, 585
Ostomy Care, 587
31 Pain, Comfort, and Sleep, 593
Pain and Discomfort, 594
Theories of Pain, 594
Types of Pain, 595
Application of the Nursing Process, 597 Assessment (Data Collection), 597
Nursing Diagnosis, 599 Planning, 599
Implementation, 599 Evaluation, 608
Sleep, 608
Functions of Sleep, 609
Stages of Sleep, 609
Normal Sleep Requirements, 609
Factors Affecting Sleep, 610
Sleep Disorders, 610
Application of the Nursing Process, 611 Assessment (Data Collection), 611
Nursing Diagnosis, 611 Planning, 611
Implementation, 611 Evaluation, 612
32 Complementary and Alternative Therapies, 614
Complementary and Alternative Medicine, 614
Mind and Body Interventions, 615
Acupuncture, 615
Yoga, 615
Chiropractic, 616
Massage Therapy, 616
Relaxation Therapy, 616
Imagery, 616
Meditation, 616
Biofeedback, 616
Bioield Therapies, 616
Hypnotherapy, 617
Music, Art, and Dance Therapy, 617
Humor, 617
Prayer, 617
Natural Products, 617
Herbal Therapy and Dietary Supplements, 617
Aromatherapy, 619
Other Complementary Interventions, 619
Homeopathic Medicine, 619
Naturopathic Medicine, 619
Traditional Chinese Medicine, 619
Ayurveda, 619
Shamanism, 619
Folk Medicine, 620
American Indian Medicine, 620
The Nurse’s Role in Complementary and Alternative Therapies, 620
UNIT VII MEDICATION ADMINISTRATION, 622
33 Pharmacology and Preparation for Drug Administration, 622
Pharmacology, 622
Classiication of Drugs, 623
Legal Control of Drugs, 625
Basic Concepts of Pharmacology, 626
Medication Administration and Safety, 629
Considerations for Infants and Children, 631
Considerations for the Older Adult, 632
Considerations for Home Care, 633
Problems of Nonadherence, 633
Application of the Nursing Process, 634
Assessment (Data Collection), 634
Nursing Diagnosis, 636
Planning, 636
Implementation, 637 Evaluation, 641
34 Administering Oral, Topical, and Inhalant Medications, 644
Nursing Responsibilities in Medication Administration, 645
Medication Orders, 645
Types of Orders, 646
Regularly Scheduled or Routine Medication Orders, 647
Dosage of Medications, 647
Routes of Oral and Topical Medication Administration, 647
Medication Administration and Technology, 648
Medication Administration Record, 649
Medication Administration Systems, 649
Unit-Dose System, 649
Prescription System, 650
Preparation of Oral Controlled Substances from a Dispenser, 650
Topical Drugs, 652
Application of the Nursing Process, 652
Assessment (Data Collection), 652
Nursing Diagnosis, 652
Planning, 653
Implementation, 653 Evaluation, 669
Medication Errors, 669
35 Administering Intradermal, Subcutaneous, and Intramuscular Injections, 673
Principles of Parenteral Injections, 674
Routes for Parenteral Medication, 674
Intradermal Route, 675
Subcutaneous Route, 675
Intramuscular Route, 675
Injection Equipment, 676
Types of Syringes, 676
Measurement Scales, 676
Needle Gauge and Length, 676
Preventing Needle Sticks, 677
Syringe and Needle Selection, 678
Preparing the Syringe for Use, 678
Parenteral Solutions, 678
Using a Medication Ampule, 678
Using a Medication Vial, 680
Reconstitution of a Drug, 681
Compatibility of Medications, 681
Application of the Nursing Process, 683
Assessment (Data Collection), 683
Nursing Diagnosis, 683
Planning, 684
Implementation, 684
Evaluation, 696
36 Administering Intravenous Solutions and Medications, 699
Intravenous Therapy, 700
Licensed Practical Nurse/Licensed
Vocational Nurse’s Role in Intravenous Therapy, 700
Types of Intravenous Solution, 700
Equipment for Intravenous Administration, 703
Administration Sets, 703
Infusion Pumps and Controllers, 705
Venous Access Devices, 707
Complications of Intravenous Therapy, 709
Iniltration, 709
Extravasation, 709
Phlebitis, 710
Bloodstream Infection, 710
Other Complications, 710
Application of the Nursing Process, 710
Assessment (Data Collection), 710
Nursing Diagnosis, 711
Planning, 711
Implementation, 712
Evaluation, 731
UNIT VIII CARE OF THE SURGICAL AND IMMOBILE PATIENT, 733
37 Care of the Surgical Patient, 733
Reasons for Surgery, 734
Patients at Higher Risk for Surgical Complications, 734
Perioperative Nursing, 735
Enhancements to Surgical Technique, 735
Laser Surgery, 735
Fiberoptic Surgery, 735
Robotic Surgery, 736
Anesthesia, 736
General Anesthesia, 736
Regional Anesthesia, 736
Procedural (Moderate) Sedation Anesthesia, 736
Local Anesthesia, 736
Preoperative Procedures, 737
Surgical Consent, 737
Surgical Site Identiication, 737
Physical Examination, 737
Application of the Nursing Process, 738
Preoperative Care, 738
Assessment (Data Collection), 738
Nursing Diagnosis, 739
Planning, 739
Implementation, 739
Evaluation, 743
Intraoperative Care, 747
Role of the Scrub Person and Circulating Nurse, 748
Postanesthesia Immediate Care, 748
Postanesthesia Care in the Same-Day Surgery Unit, 748
Postoperative Care, 749
Assessment (Data Collection), 749
Nursing Diagnosis, 749
Planning, 750 Implementation, 751
Evaluation, 755
38 Providing Wound Care and Treating Pressure Injuries, 759
Types of Wounds and the Healing Process, 760
Phases of Wound Healing, 761
Factors Affecting Wound Healing, 762
Age, 762
Nutrition, 762
Lifestyle, 762
Medications, 765
Infection, 765
Chronic Illness, 765
Complications of Wound Healing, 765
Hemorrhage, 765
Infection, 765
Dehiscence and Evisceration, 766
Treatment of Wounds, 766
Wound Closure, 766
Drains and Drainage Devices, 767
Débridement, 768
Dressings, 769
Binders, 770
Negative Pressure Wound Therapy, 771
Treatment of Pressure Injuries or Vascular Ulcers, 772
Application of the Nursing Process, 772
Assessment (Data Collection), 772
Nursing Diagnosis, 773
Planning, 773
Implementation, 773 Evaluation, 787
39 Promoting Musculoskeletal Function, 789
Systemic Effect of Immobilization, 790
Psychosocial Effects of Immobilization, 791
Types of Immobilization, 792
Splints, 792
Traction, 792
Casts, 794
External Fixators, 795
Devices Used to Prevent Problems of Immobility, 796
Specialty Beds, 796
Pressure Relief Devices, 796
Continuous Passive Motion Machine, 797
Therapeutic Exercise, 797
Application of the Nursing Process, 798
Assessment (Data Collection), 798
Nursing Diagnosis, 799 Planning, 799
Implementation, 800 Evaluation, 812
UNIT IX CARING FOR THE ELDERLY, 815
40 Common Physical Care Problems of the Older Adult, 815
Getting Older, 815
Immobility, 815
Nursing Interventions to Promote Mobility, 816
Preventing Falls, 818
Alteration in Elimination, 819
Urinary Incontinence, 819
Constipation and Fecal Impaction, 820
Alteration in Nutrition, 820
Nursing Interventions for Nutritional Support, 821
Sensory Deicits, 821
Vision Deicits, 821
Hearing Deicit, 823
Sexuality, 823
Polypharmacy, 824
Nursing Interventions for Polypharmacy, 825
41 Common Psychosocial Care Problems of the Older Adult, 830
Changes in Cognitive Functioning in Older Adults, 830
Assessment of Cognitive Changes in Older Adults, 831
Common Cognitive Disorders in Older Adults, 831
Confusion, 831
Delirium, 831
Dementia, 832
Alzheimer Disease, 834
Safety for the Cognitively Impaired, 835
Behaviors Associated with Cognitive Disorders, 835
Depression, Alcoholism, and Suicide, 837
Interventions for Depression, Alcoholism, and Suicide Prevention, 838
Crimes Against Older Adults, 839
Elder Abuse, 839
Scams and White-Collar Crime, 840
Future Issues of Concern to Older Adults, 840 Planning for the Future, 841
APPENDIXES
A Standard Steps for All Nursing Procedures, 843
B NFLPN Nursing Practice Standards for the Licensed Practical/Vocational Nurse, 845
C American Nurses Association Code of Ethics for Nurses, 847
D Standard Precautions, 848
E Most Common Laboratory Test Values, 851
F NANDA-I Approved Nursing Diagnoses, 2015-2017, 854
Reader References, 857
Glossary, 866
Index, 882
Selected Nursing Theories
THEORISTGOAL OF NURSINGPRACTICE FRAMEWORK
Virginia Henderson (1955)To help patients gain independence in meeting their needs as quickly as possible
Dorothy Johnson (1968)To reduce stress, allowing the patient to recover as quickly as possible
Fourteen fundamental needs
Seven behavioral subsystems in an adaptation model
Martha Rogers (1970)To achieve maximum level of wellnessConcept of “unitary man” evolving along the life process
Dorothea Orem (1971)To care for and help patients with various needs attain self-care
Betty Neumann (1972)To help individuals, families, and groups attain and maintain maximum levels of total wellness through purposeful interventions
Sister Callista Roy (1976)To identify types of demands placed on the patient and the patient’s adaptation to them
Jean Watson (1979)To promote health, restore patients to health, and prevent illness
Rosemarie Parse (1987)To assist the patient in interaction with the environment and in co-creating health. To sustain a safe and protective environment
Patricia Benner and Judith Wrubel (1989)
Self-care deicits
Systems model with stress reduction as its goal; nursing care occurs on various levels: primary prevention, secondary prevention, or tertiary prevention
Four adaptive modes: physiologic, psychological, sociological, and independence
“Carative” factors, with caring as an interpersonal process used to meet human needs
Human becoming: patients are open, mutual, and constantly interacting with the environment. Health is constantly changing
To care about the patient as an individualPrimacy of caring: caring is central and allows for the giving and receiving of help. Caring extends to all aspects of care of the patient
patient care. Question the way things are done for patient care, and ask what does not make sense or what needs clariication. Ask yourself, Is there a better way to perform this procedure? An example of such a question would be, Is this the best solution to use for mouth care for this patient undergoing chemotherapy? Research the question topic and gather the best evidence available for an answer to the question. Critically look at the research for signs of validity of the data. Integrate the best evidence with your clinical expertise. Consider the patient’s preferences and values when deciding on a course of action. Evaluate the outcome of the new action(s). Resources for research and guidelines for evidencebased practice include evidence-based journals, systematic reviews of studies, centers for evidence-based nursing, and evidence-based practice guidelines. A list of resources for evidence-based nursing is available from Virginia Commonwealth University at http://guides.library.vcu.edu/ebpsteps. A tutorial on understanding evidence-based practice is available at that website.
Evidence-based nursing is used to help determine “best practices.” “Best practice means the use of care concepts, interventions, and techniques that are grounded in research and known to promote higher quality of care and living” (University of Iowa College of Nursing, 2015a, 2015b). Clinical ield experience and evidence-based research are used to establish the best practices for patient care. Best practices are often provided in the form of clinical practice guidelines.
FIGURE 1.6 Evidence-based nursing.
Clinical practice guidelines are the product of evidencebased research, and they serve as a way for nurses to implement the evidence-based practices. For example, instead of performing catheter care a certain way “because we’ve always done it this way,” the nursing staff adheres to a speciic guideline that is evidencebased—has been shown with scientiic evidence—to be safer and more effective. To sum up, evidence-based nursing is where the best research evidence, patient values and preferences, and professional nursing expertise come together (Fig. 1.6).
Think Critically
Which role of the nurse appeals to you the most?
The licensed practical/vocational nurse:
1. Shall accept assigned responsibilities as an accountable member of the health care team.
2. Shall function within the limits of educational preparation and experience as related to the assigned duties.
3. Shall function with other members of the health care team in promoting and maintaining health, preventing disease and disability, caring for and rehabilitating individuals who are experiencing an altered health state, and contributing to the ultimate quality of life until death.
4. Shall know and utilize the nursing process in planning, implementing, and evaluating health services and nursing care for the individual patient or group.
a. Planning: the planning of nursing includes:
1) assessment/data collection of health status of the individual patient, the family, and community groups
2) reporting information gained from assessment/ data collection
3) the identiication of health goals
b. Implementation: The plan for nursing care is put into practice to achieve the stated goals and includes:
1) observing, recording, and reporting signiicant changes, which require intervention or different goals
2) applying nursing knowledge and skills to promote and maintain health, to prevent disease and
CURRENT NURSING PRACTICE
As nursing has grown and changed to meet the needs of society, laws have been made and standards set that govern the practice of the profession. In 2015, the American Nurses Association (ANA) revised the Standards of Nursing Practice, which contains 17 standards of national practice of nursing, describing all facets of nursing practice: who, what, when, where, and how. These standards for the professional RN protect the nurse, the patient, and the health care agency where nursing care is given. Additionally, the ANA revised and updated the Code of Ethics for Nurses with Interpretive Statements, including areas addressing social media, the importance of intra-professional collaboration, and consideration of social justice (Epstein & Turner, 2015). The National League for Nursing published a vision statement describing the practical nurse’s role in advancing the nation’s health, emphasizing the importance of the practical nurse’s contribution as professional partners in the health care team (National League for Nursing, 2014). The practical nurse follows standards written by the National Federation of Licensed Practical Nurses to deliver safe, knowledgeable nursing care (Box 1.1, Appendix B). The National Association for Practical Nurse Education and Service (NAPNES) has formulated an additional set of standards for practical nurses (see Chapter 3). In Canada, a set of similar standards guides the practice of nursing. Nurse practice acts have been established in each of
disability, and to optimize functional capabilities of an individual patient
3) assisting the patient and family with activities of daily living and encouraging self-care as appropriate
4) carrying out therapeutic regimens and protocols prescribed by personnel pursuant to authorized state law
c. Evaluations: The plan for nursing care and its implementations are evaluated to measure the progress toward the stated goals and will include appropriate persons and/or groups to determine:
1) the relevancy of current goals in relation to the progress of the individual patient
2) the involvement of the recipients of care in the evaluation process
3) the quality of the nursing action in the implementation of the plan
4) a re-ordering of priorities or new goal setting in the care plan
5. Shall participate in peer review and other evaluation processes.
6. Shall participate in the development of policies concerning the health and nursing needs of society and in the roles and functions of the LP/VN.
the US states and in the provinces of Canada to regulate the practice of nursing. Each state has a regulatory body that makes and enforces rules and regulations for the nursing profession. The practice acts generally deine activities in which nurses may engage, state the legal requirements and titles for nursing licensure, and establish the education needed for licensure. The practice acts are designed to protect the public, and they deine the legal scope of practice. Policy and procedure books are established by each facility that hires nurses. These books deine which procedures each professional can perform in that facility and specify step-by-step guidelines for the way that facility wants a procedure performed.
The National Council of State Boards of Nursing (NCSBN) has a proposal to enact rules for transition to practice for all newly licensed nurses. All newly licensed nurses will be required to complete a transition to practice program that meets the board criteria if the rule becomes a criterion for license renewal. The program would involve a minimum 6-month preceptorship with ongoing support through the irst year of practice.
The nursing process emerged during the 1970s and 1980s as an organized, deliberate, systematic way to deliver nursing care. The nursing process provides a way to implement (to put into action) caregiving, and it combines the science and the art of nursing. The nurse focuses on the patient as an individual, identiies
health care needs and strengths of the patient, establishes and implements a plan of action to meet those needs, and evaluates the outcomes of the plan. It is a circular process involving ongoing assessment, nursing diagnosis, planning, implementation, and evaluation. The nursing process is presented in depth in Unit II: The Nursing Process.
NURSING EDUCATION PATHWAYS
Formal education has been another way to build a professional image for nursing. Nursing education has been mostly moved from hospital training schools into institutions of higher learning. There are two levels of entry into nursing: practical (or vocational) nursing and registered nursing. Often a student studies to become a certiied nursing assistant before going up the “ladder” to practical/vocational training. Each educational program produces graduates with skills for a particular level of entry into practice. A nursing assistant program is short, averaging 6 to 8 weeks. Basic personal care and basic nursing skills are taught. The practical nursing program generally takes 12 to 18 months to complete. The registered nursing program (RN) requires 2 to 5 years of education, depending on the type of degree sought (Fig. 1.7). If the student has already obtained a practical/vocational nursing license, the program may require only 1 more year to become an RN.
PRACTICAL NURSING
Practical nursing was created to ill a gap left by nurses who enlisted in the military services during World War II. Programs were developed to train practical nurses to care for well people and those who were mildly or chronically ill or past the acute stage of illness. RNs could then concentrate on the acutely ill. A need for
Advanced Practice Nurse
PhD
Nurse Practitioner
Nurse Anesthetist
Clinical Nurse Specialist
Nurse-Midwife
MSN
Registered Nurse
Baccalaureate
Associate Degree
Diploma
Practical/Vocational Nurse
practical nurses continued after the war, and NAPNES was formed to standardize practical nurse education and to establish licensure criteria for graduates. Practical nursing programs are offered in vocational schools, hospitals, proprietary schools, and community colleges. Graduates take the National Council Licensure Examination for Practical Nurses (NCLEX-PN) after program completion. Successfully passing the examination and obtaining licensure allows the use of the initials LPN or LVN after one’s name. Practical nurses provide direct patient care under the supervision of an RN, advanced practice RN, physician assistant, physician, dentist, or podiatrist. Many community colleges have structured the practical nurse curriculum so that graduates can easily enter the second year of the registered nursing program. This type of curriculum is considered a “ladder program.” Many LPN/ LVN programs require that the entering student be a certiied nursing assistant (Fig. 1.8).
After completion of an LPN/LVN curriculum and/ or licensure, the graduate can seek certiication by NAPNES in pharmacology, long-term care, and/or IV therapy. The pharmacology examination can be taken online. Each of the three certiications is valid for 3 years and can then be renewed.
REGISTERED NURSING
Graduates of three different educational programs are qualiied to take the RN licensure examination (NCLEX-RN): a hospital-based diploma program, a 2-year associate degree program at a community college, or a 4-year baccalaureate nursing program at a college or university. RNs may provide bedside care or care in the community or supervise others in managing care of multiple patients.
Diploma schools continue to decrease as the desire to improve the professional image of nursing through
FIGURE 1.7 Students in modern day simulation lab.
Certified Nursing Assistant
FIGURE 1.8 Nursing education ladder.
more formal education occurs and many diploma programs have been dissolved or absorbed into collegeor university-based educational systems because of mergers. Hospitals could no longer afford to provide the expensive diploma programs. Diploma nurses are more extensively trained in skills compared with the students of other programs. They spend a far greater number of clinical hours working directly with patients, but they do not get as broad a base of scientiic knowledge as college-educated nurses receive. Fewer than 10% of RN programs are diploma programs.
Associate degree programs attract the majority of RN students. The associate degree nurse is considered a technical nurse and is not speciically prepared to work in a management position, although many do. Graduates of these programs have 2 years of clinical experience along with their academic classes.
Baccalaureate nursing programs prepare nurses who have managerial skills, as well as bedside nursing skills. The push toward professionalism, uniication, and higher educational standards/consistencies for nursing has caused the ANA to propose that the baccalaureate degree be necessary for entry into professional nursing practice. There has been considerable controversy over this proposal because the many RNs who graduated from diploma or associate degree programs believe that their jobs may be threatened by such a proposal. To date, only some employers distinguish among the various educational programs of the RN. Magnet hospitals require that 100% of the nursing managers hold a Bachelor of Science in nursing degree (BSN), and although they make no speciic recommendation for staff nurses, the typical hospital with Magnet designation tends to have about half of employed bedside RNs holding a BSN degree (Hawkins & Shell, 2012). In most facilities, however, graduates of all three RN programs are viewed the same. Another concern is that, if the more expensive and longer program were required to become a professional RN, employers would have to pay higher salaries. Differentiation of salaries based on educational degree primarily occurs only at the managerial level, not the bedside level. The nursing shortage tempered the push for all nurses to be baccalaureate prepared because the program is twice as long, but the ANA is again pressing for the BSN to be required for entry into RN practice.
Think Critically
What are three educational differences between the practical nurse and the RN?
ADVANCED PRACTICE NURSING
Graduate programs are available in nursing for both master’s and doctorate degrees. Nurses who pursue higher education are prepared as specialists in the various clinical branches of nursing, in research, or in administration. Another form of advanced education
is the nurse practitioner program. RNs continue their training in a specialty such as family practice, pediatrics, maternity, psychiatry, adult health nursing, acute care, or geriatrics; once licensed, they can practice more independently than as an RN. Nurse practitioners (NPs) provide care in a hospital, outpatient, ambulatory care, or community-based setting. In many states, they can treat patients on their own and write prescriptions under the direction of a physician. NPs are one of the four types of advanced practice nurse. The other three include the titles certiied nurse-midwife (CNM), certiied registered nurse anesthetist (CRNA), and clinical nurse specialist (CNS). Each type of advance practice RN requires speciic certiication and training.
The ANA set up a separate American Nurses Credentialing Center to enhance the professional image of nursing. RNs who have experience in a particular specialty may take a comprehensive examination. Passing the examination provides the nurse with certiication of expertise in that specialty. Certiication is also available for the practical nurse under a program developed by NAPNES.
DELIVERY OF NURSING CARE
Various systems of delivering nursing care have been tried through the years. Today various adaptations are devised to meet the speciic needs of the patients and nurses. Functional nursing care was the irst care delivery system for the practical nurse. Practical nurses performed a series of tasks such as administration of medication and treatments. Care was rather fragmented; however, it was cost effective. Team nursing evolved in the 1950s and extended into the mid-1970s. An RN was the team leader who coordinated care for a group of patients. Work tasks were assigned to the other members of the team, the practical nurses and the nurses’ aides. This system worked fairly well as long as there was excellent communication among the members and the team leader evaluated care delivered. Total patient care came next, in which one nurse carried out all nursing functions for the patient, including medication administration. This was an effort to provide less fragmented care for the patient. Of course, total patient care is more expensive.
Primary nursing appeared in the late 1960s and 1970s. In this system, one nurse plans and directs care for a patient over a 24-hour period. This method eliminated fragmentation of care between shifts. When the primary nurse is off duty, an associate nurse takes over the care and planning. Today, primary nursing is often modiied with the use of cross-trained personnel assigned to help with duties. To increase the level of productivity, ancillary workers supervised by the RN are trained in multiple functions, such as clerical and housekeeping tasks, vital sign measurement, and phlebotomy. This system has not been entirely satisfactory.
Currently, because research is showing better patient outcomes with more of the care being delivered by nurses, there is a trend back to total patient care.
Relationship-based care appeared in the early 2000s (Koloroutis et al., 2004). It emphasizes three critical relationships: (1) the relationship between caregivers and the patients and families they serve; (2) the caregiver’s relationship with him- or herself; and (3) the relationship among health team members (UCLA Department of Nursing, 2015). The motivation behind relationshipbased care was to promote a cultural transformation by improving relationships to foster care for the patient. Some schools of nursing have adopted relationshipbased care as the foundation of their nursing education curriculum.
Patient-centered care has been described since the 1950s, but it came to the forefront in 2001 when the Institute of Medicine (IOM) targeted six areas for improvement in the US health care system, including safety, effectiveness, patient-centeredness, timeliness, eficiency, and equitableness (Cliff, 2012). Patientcentered care has been fully embraced by the nursing community, and it is identiied as one of the seven QSEN competencies (QSEN.org, 2015).
PRACTICE SETTINGS
Practical nurses work in health care organizations under the supervision of an RN, advanced practice RN, physician assistant, physician, dentist, or podiatrist. Traditionally, many LPN/LVN positions were found in the hospital setting, whereas community nursing, school nursing, and public health nursing were primarily the arena of the professional RN. Recent trends have changed, however, and expanded the employment landscape for the practical nurse. Hospitals now tend to hire primarily RNs, yet practice settings for the LPN/LVN remain plentiful and include the following health care organizations:
• Hospitals: Restorative care is provided to ill or injured patients.
• Subacute and extended care facilities: In facilities for subacute, intermediate, or long-term care; personal care and skilled care are provided for those requiring rehabilitation or custodial care.
• Assisted-living facilities: In facilities that provide housekeeping, prepared meals, and varying degrees of nursing care.
• Physicians’ ofices: Ambulatory patients receive preventive care or treatment of an illness or injury.
• Ambulatory clinics: Ambulatory patients come for preventive care or treatment of an illness or injury; often treatment by specialty groups is available on site. Numerous specialty clinics that employ LPNs/ LVNs include cardiology, dermatology, allergy, immunology, pulmonology, and many others.
• Renal dialysis centers: Patients with kidney failure receive renal dialysis treatments.
• Hospiceandpalliativehomecare: Supportive treatment is provided for patients who are terminally ill, improving quality of life and ease of suffering.
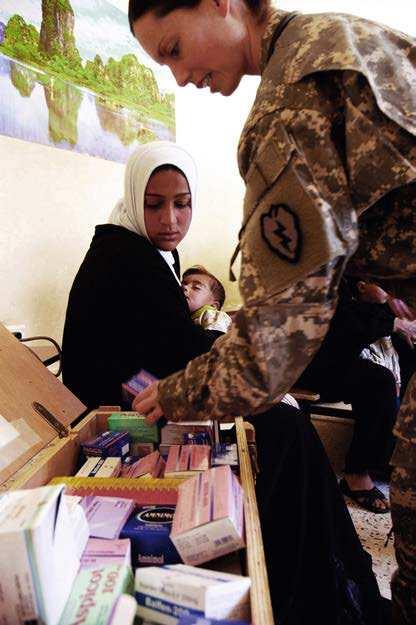
• Home health agencies: In-home care is provided to patients by nurses who visit the home (Fig. 1.9).
• Neighborhood emergency centers/urgent care clinics: Minor emergency care is provided to patients within the community setting.
• Correctional facilities: Care is rendered to incarcerated individuals, assisting with physical examinations, administering medications, and performing medical treatments.
• School nurse: Triage, medication administration, irst aid, and some care of students with diabetes.
• Surgical centers: These centers perform same day surgeries on typically healthier individuals than those found in a typical hospital operating room (OR). The LPN/LVN is often employed as the preoperative nurse in this setting.
As the role of the practical nurse expands, employment in other practice settings is possible.
TODAY’S HEALTH CARE SYSTEM
In times past, most medical care was provided by physicians in private practice. With the technological advances in medicine and the lood of new drugs on the market, health care costs have risen dramatically. Although the use of magnetic resonance imaging (MRI) and computed tomography (CT) provides much more data than a standard radiograph dose, both are very expensive. Microsurgical techniques allow procedures that would not have been possible 40 years ago. Older adults are living longer and needing more years of medical care and numerous prescription drugs.
Diagnosis-related groups (DRGs) were created by Medicare in 1983 as an attempt to contain rising health care costs. The DRG system means that a hospital receives a set amount of money for a patient who is hospitalized with a certain diagnosis. If a patient is admitted with pneumonia, only a certain number of days of hospitalization are allowed and will be paid for
FIGURE 1.9 Home health nursing. (Photo copyright istock.com.)