New Concepts in Glaucoma Surgery Series: Volume 1
Editors
John R. Samples
Iqbal
Ike K. Ahmed
Kugler Publications/Amsterdam/The Netherlands
New Concepts in Glaucoma Website
Visit our website at newconceptsinglaucoma.com for access to the videos discussed in this book, captured content from our annual congress, and clinical science and research articles published within the series.
Videos
Videos can be accessed directly through: newconceptsinglaucoma.com/surgery1/videos/chapter-number
e.g. for chapter 10 go to to newconceptsinglaucoma.com/surgery1/videos/10)
New Concepts in Glaucoma Surgery Series - Volume 1
ISSN 2589-7632
ISBN 978-90-6299-276-8
Kugler Publications
P.O. Box 20538
1001 NM Amsterdam, The Netherlands www.kuglerpublications.com
© 2020 Kugler Publications, Amsterdam, The Netherlands
All rights reserved. No part of this book may be translated or reproduced in any form by print, photoprint, microfilm, or any other means without prior written permission of the publisher.
Kugler Publications is an imprint of SPB Academic Publishing bv, P.O. Box 20538, 1001 NM Amsterdam, The Netherlands
Cover design by: Willem Driebergen, Rijnsburg, The Netherlands
Haiyan Gong, David L. Swain
William Noonan
3. Which minimally
Jithin Yohannan, E. Randy Craven
4.
5. On the use of curcumin as a multimodal antifibrotic agent
Nicholas M. Pfahler, Michael C. Giovingo, Paul A. Knepper
6. The future of MIGS ........................................................................
Thiago A. Moulin, Arsham Sheybani
7. Gonioscopy-assisted transluminal trabeculotomy (GATT)
Ronald L. Fellman, Davinder S. Grover
8. Hydrus® microstent ......................................................................
Thiago A. Moulin, Arsham Sheybani
9. The iStent devices: iStent, iStent inject, and iStent Supra ......................................
Antonio M. Fea, Simona Scalabrin, Carlo Lavia
10. Ab interno trabecular meshwork incision, ablation, and disruption ............................. 137 Hamed Esfandiari, Si Chen, Ralitsa T. Loewen, Susanna Waxman, Kevin Kaplowitz, Nils A. Loewen
11. iTrack™ ab interno c anal-based glaucoma surgery: the next evolution in MIGS ...................
Mahmoud Khaimi, David Lubeck
12. XEN: the evolution of the stent and technique ...............................................
Vanessa Vera, Daniel Lee, Natasha N. Kolomeyer, M. Reza Razeghinejad, Jonathan S. Myers
13. An ab externo minimally invasive aqueous shunt comprised of a novel biomaterial ............... 181 Leonard Pinchuk, Isabelle Riss, Juan F. Batlle, Henny Beckers, Ingeborg Stalmans
14. Laser trabeculoplasty and micropulse: evolution from trabecular photocoagulation, to trabecular photothermolysis, to trabecular photostimulation .................................
193
Giorgio Dorin, Ted S. Acott, Antonio M. Fea, John R. Samples
15. Cyclophotocoagulation .................................................................. 211
Michael Giovingo, Shyam Patel, Shweta Chaudhary, Amar Mannina, Thomas Patrianakos
16. Excimer laser trabeculostomy: the laser-based MIGS procedure for open-angle glaucoma ........ 231
Michael S. Berlin, Marc Töteberg-Harms, Jonathan Shakibkhou, Alyssa Francesca Ahorro, Ryan Lamrani, Antonio Moreno Valladares, Ulrich Giers
17. Mixing and combining MIGS procedures ....................................................
Steven R. Sarkisian, Jr.
18. Trabeculectomy with suprachoroidal derivation.............................................
Rodolfo A. Pérez-Grossmann, Daniel Grigera, Alan Wenger, Rodolfo A. Pérez-Simons
19. Modern retinal laser for neuroprotection in open-angle glaucoma .............................
Jeffrey K. Luttrull, David Kent
20. What is the ideal conjunctival bleb and how to achieve it?
Learning from the Microfistula-XEN procedure .................................................
Dao-Yi Yu, Stephen John Cringle, William H. Morgan, Er-Ning Su
21. Special considerations for pediatric glaucoma ..............................................
Peter A. Netland, John R. Samples
About the authors
Ted Acott, MD, PhD
Dr. Acott is Research Professor of Ophthalmology and of Biochemistry & Molecular Biology at the Casey Eye Institute, Oregon Health & Science University, OR, USA. His team’s long-term research interests are centered on identifying therapeutic targets to treat glaucoma via lowering intraocular pressure. They have recently identified the homeostatic mechanism of intraocular pressure, which normally maintains the aqueous humor outflow resistance at the appropriate levels, protecting most people from ever developing glaucoma. In addition, they have been studying the molecular and biomechanical properties that are responsible for this homeostatic mechanism and for maintaining the highly segmental nature of aqueous humor outflow. Their work has recently demonstrated that the IOP homeostatic mechanism is compromised in glaucoma, and both high and low segmental flow regions exhibit different biomechanical and flow properties. The team has also identified individual extracellular matrix proteins that may be important therapeutic targets in the treatment of glaucoma.
Alyssa Francesca Ahorro, BA
Alyssa Francesca Ahorro received a Bachelor of Arts in Psychology at the University of California, Riverside in June of 2018. Currently, she is conducting research at the Glaucoma Institute of Beverly Hills and Cedars-Sinai Medical Center in Los Angeles, CA, USA. Her current interests lie within the scopes of Ophthalmology and Oncology. Upon gaining further research experience, she will pursue a medical degree.
Juan F. Batlle, MD
Dr. Batlle is founder and President of the multi-specialty private practice Centro Laser in Santo Domingo, Dominican Republic. He is a Distinguished Member of Vision 2020/International Agency for the Prevention of Blindness, Chief of Ophthalmology at the charity clinic Elias Santana Hospital, and Medical Director of one of the most prestigious residency training programs of ophthalmology in Latin America associated with Instituto Tecnológico de Santo Domingo. He has dedicated his professional life to the prevention of blindness in Latin America, with an interest in cataract, glaucoma, cornea, and refractive surgery. Dr. Batlle has more than 20 years of experience in research and collaborates with well-known ophthalmic companies for the development and design of ophthalmic devices and medications, supporting submissions and approvals to world-wide regulatory agencies in his areas of interest.
Henny J.M. Beckers, MD, PhD, FEBOphth
Dr. Beckers is Associate Professor, Head of the Glaucoma Clinic, and Director of the Ophthalmology Residency Program at the University Eye Clinic of the Maastricht University Medical Center+ in the Netherlands. She is the Secretary of the Dutch Glaucoma Group, an active committee of Dutch ophthalmologists with a special interest in glaucoma. Her main research interest is glaucoma surgery, with a focus on studying new glaucoma devices. Research lines also include progression of glaucoma, prognostic factors in glaucoma, diagnosis of narrow-angle glaucoma, glaucoma treatment and adherence, and cost-effectiveness studies.
Michael S. Berlin, MD, MSc
Dr. Michael Berlin is a Professor of Clinical Ophthalmology at the UCLA Stein Eye Institute. His professional contributions are in laser surgery and in the research and treatment of glaucoma. He is the founder and director of the Glaucoma Institute of Beverly Hills (GIBH) in Los Angeles, CA, USA, where he has maintained a private clinical practice for over 30 years and is the director of the GIBH Research Foundation. Dr. Berlin received his bachelor’s degree, medical degree, and his Master of Sciences degree in ophthalmology from the University of Michigan. He completed an internship in Internal Medicine at the Harbor –UCLA Medical Center, followed by an ophthalmology residency at the University of Michigan and subsequent subspecialty glaucoma fellowship training at the Mount Sinai Medical Center in New York. His research interests focus on the development of novel therapies for the treatment of glaucoma. He holds multiple patents for innovative laser and surgical procedures, publishes extensively and lectures internationally.
Shweta Chaudhary, MD
Shweta Chaudhary is an ophthalmology resident at Cook County Health and Hospitals, Chicago, IL, USA. She has completed an ophthalmology residency in India and a corneal neurobiology research fellowship at the University of Illinois at Chicago. Her research interests include surgical and laser inventions in the field of glaucoma, especially mechanisms of action of different types of glaucoma lasers and minimally invasive glaucoma surgery.
Si Chen, MD
Si Chen is a PhD student from Central South University, Xiangya School of Medicine, Changsha, China. She is currently a visiting international scholar in the Loewen Lab in the Department of Ophthalmology at the University of Pittsburgh, PA, USA. Her research interests involve the role of microincisional glaucoma surgeries in the cause, treatment, and prevention of glaucoma. Her PhD is concerned with factors that influence outflow in the distal outflow tract.
E. Randy Craven, MD
Dr. Craven specializes in glaucoma and complex anterior segment cases, such as iris problems and lens issues. He is an Associate Professor at Johns Hopkins University School of Medicine (Baltimore, MD, USA). Dr. Craven is currently also the Medical Director of the Wilmer Eye Institute Bethesda (Bethesda, MD, USA) and serves as the Vice-Chair for the Wilmer Eye Institute Practice Network.
From 2013 to 2016, Dr. Craven served as the Chief of Glaucoma and Glaucoma Fellowship Director at the King Khaled Eye Specialist Hospital in Riyadh, Saudi Arabia. He also served as the Residency Coordinator there.
Dr. Craven was involved with the development and implementation of risk-management programs for ophthalmologists while serving on the Board of Directors for the Ophthalmic Mutual Insurance Company in the USA. He participated in over 120 clinical research trials and was the first US surgeon in the US Food and Drug Administration (FDA) trial to implant the iStent, as well as the first US surgeon to implant the CyPass; as a result, he is active in expanding and educating about the role of minimally invasive glaucoma surgeries throughout Europe, the Middle East, Africa, and the USA. He has extensive experience with optical coherence tomography for glaucoma and served as an advisor for the development of imaging in glaucoma.
Stephen John Cringle, BSc, PhD
Dr. Cringle is Professor of the Lions Eye Institute, Center for Ophthalmology and Visual Science at The University of Western Australia in Nedlands, Australia. His research involves basic studies of retinal oxygen metabolism, vascular biology, laser applications in ophthalmic research, and the development of new diagnostic and therapeutic techniques in glaucoma and retinal diseases. He has worked with Professor Yu and made a significant contribution to the XEN Gel Stent technology for glaucoma filtration surgery that is now in clinical use. Dr. Cringle has a background in physics and 35 years of experience in ophthalmic research.
Giorgio Dorin
Giorgio Dorin has been devoted to the development of clinical laser systems for the treatment of glaucoma, retinal, and refractive disorders since 1969. In 1983, in recognition of his contributions to the ocular applications of lasers, he was awarded with the Honorary Membership by the Italian Society of Laser in Ophthalmology (S.I.L.O.).
During the past two decades, he has developed micropulse laser emission techniques to master the control of the photothermal effects during ocular laser treatments, to the end of minimizing and avoiding the treatment’s iatrogenic damage and collateral complications, while maintaining and optimizing both clinical outcomes and therapeutic benefits.
He has pioneered the clinical use of sub-visible-threshold nondamaging micropulse laser procedures for the treatment of retinovascular disorders and glaucoma. This has led to new subthreshold laser micropulse photostimulation (SLMP) treatment protocols that have been fine-tuned in pilot studies and validated in prospective randomized clinical trials, which have provided the evidence that SLMP is at least as effective as the conventional destructive threshold laser photocoagulation and can result in superior outcomes and unprecedented functional benefits thanks to the absence of the treatment’s morphologic and functional damage. This evidence is now leading a pivotal swing from laser photocoagulation to laser photostimulation, a seminal paradigm-shift with intrinsic unprecedented safety profile and benefit-to-risk ratio. He is now advocating the ban of destructive photocoagulation and the use of photostimulation for the treatment of ocular chronic degenerative progressive neurotrophic disorders.
He has been granted three patents on sub-threshold laser applications by the US Patent Office, has authored/coauthored numerous publications in peer-reviewed medical journals, has contributed with chapters in ophthalmology books, and has presented posters and given podium presentations at ophthalmology meetings, congresses, and courses throughout the world. He is currently serving as the Senior Development Scientist and COO for ALeyeGN Technologies, Saratoga, CA, USA.
Hamed Esfandiari, MD
Hamed Esfandiari is an Assistant Professor of Ophthalmology at Shahid Beheshti University of Medical Science in Tehran, Iran. He completed a research fellowship with Dr. Loewen at the University of Pittsburgh (PA, USA) focusing on the clinical outcomes of novel techniques to increase conventional outflow. He is now on the Pediatric Ophthalmology service at the Northwestern University in Chicago, IL, working extensively in the field of childhood glaucoma. His research interests encompass success factors in traditional and new glaucoma surgeries and how they relate to recent insights into the conventional aqueous outflow tract. He has also conducted studies on pediatric glaucoma, optic neuropathies, and novel glaucoma medications.
Antonio Maria Fea, MD, PhD
Dr. Antonio Maria Fea is an Aggregate Professor at the University of Turin, Italy and an adjunct scientist at SERI. He holds a PhD in electrophysiology. He developed and propagated the use of several psychophysical techniques to test visual function in infants and children. Dr. Fea was part of several humanitarian missions in Madagascar, Namibia and, India. In recent years, he has been involved in the development and clinical evaluation of several minimally invasive techniques for the treatment of glaucoma. He has been part of several multicenter trials performing and teaching MIGS surgery in Armenia, India, Colombia, and Chile, and is part of the Advisory Board of several companies involved in the development of novel and minimally invasive methods for the treatment of glaucoma. He serves as reviewer and is part of the editorial board of several peer-reviewed journals.
Ronald L. Fellman, MD
Ronald Fellman is an Attending Surgeon and Clinician at Glaucoma Associates of Texas in Dallas, Adjunct Professor of Ophthalmology at North Texas Eye Research Institute (NTERI) University of North Texas Health Science Center Fort Worth and Associate Clinical Professor Emeritus, Department of Ophthalmology, University of Texas Southwestern Medical Center, Dallas (UTSWMC) in TX, USA. Dr. Fellman attained his medical degree from Tulane University, residency at University of Texas Southwestern Medical Center, and glaucoma fellowship at Wills Eye Hospital. He is involved in clinical research concerning the surgical management of glaucoma including wound healing, new devices and techniques for canal surgery and the factors associated with canalogenesis. Dr. Fellman serves on the board of Cure Glaucoma, a foundation dedicated to translational research in glaucoma and the reduction of blindness from glaucoma on a global level and is active in various roles for the American Glaucoma Society.
Ulrich Giers, MD
Dr. Ulrich Giers is the Founder, Director, and Head of the anterior segment surgery department of the OWL Eye Clinic in Detmold, Germany. He graduated and earned his medical doctorate degree from Marburg University. He then completed his residency and fellowship at the University Eye Hospital in Ulm, Germany. His research interests focus on clinical outcomes of refractive and glaucoma procedures.
Michael Giovingo, MD
Michael Giovingo is the director of Glaucoma Service for Cook County Health and Hospital System in Chicago, IL, USA. He is a board-certified ophthalmologist and fellowship trained glaucoma specialist. His research interests include the pathophysiology of glaucoma, development of new medical interventions for glaucoma, and minimally invasive glaucoma surgery and lasers. Dr. Giovingo is also active in training medical and surgical management of glaucoma to the Ophthalmology residents at Cook County Health and Hospital System.
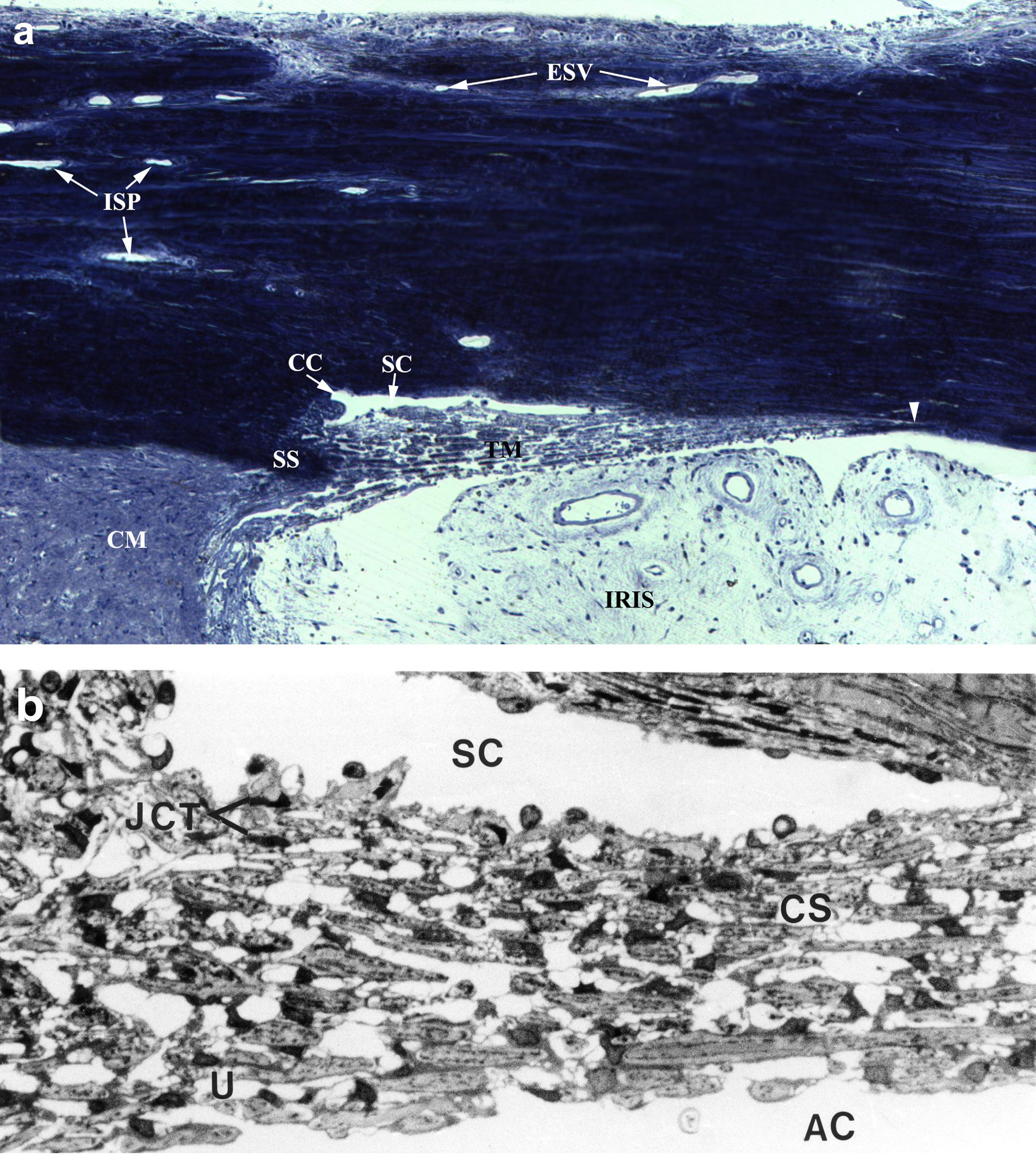
Haiyan Gong, MD, PhD, FARVO
Dr. Gong is Professor of Ophthalmology, Anatomy, and Neurobiology at Boston University School of Medicine (MA, USA). Her research is focused on understanding the mechanisms that regulate aqueous humor outflow resistance in normal eyes and how this resistance is increased in eyes with primary open-angle glaucoma, using physiological and morphological methods to provide new insights for the development of new therapeutic strategies to treat this disease. Dr. Gong’s current research is supported by National Institutes of Health/ National Eye Institute, BrightFocus Foundation, Aerie Pharmaceuticals, Inc., and Massachusetts Lions Eye Research Fund.
Daniel Grigera, MD
Dr. Grigera earned his medical degree from the University of Buenos Aires, Buenos Aires, Argentina. He currently serves as a consultant in the Glaucoma Service at Santa Lucía Eye Hospital and as Assistant Professor of Ophthalmology at the Faculty of Medicine of Salvador University in Buenos Aires, Argentina.
He is a former President of the Latin American Glaucoma Society and the Pan American Glaucoma Society, member of the World Glaucoma Association Council, and founding member and first president of the Argentine Association of Glaucoma. Dr. Grigera has participated as coordinator or speaker in more than 90 congresses and symposiums in Argentina, America, and Europe. He is a reviewer of Journal of Glaucoma and has published 23 works on glaucoma in Argentinian and international peer-reviewed publications.
Davinder S. Grover, MD, MPH
Dr. Grover is Attending Surgeon and Clinician at Glaucoma Associates of Texas, Dallas, Adjunct Assistant Professor at North Texas Eye Research Institute (NTERI), University of North Texas Health Science Center, Fort Worth, and Clinical Assistant Professor at University of Texas Southwestern Medical School in Dallas, TX, USA. His interests include innovative glaucoma surgeries, complex glaucoma, cataract, and anterior segment surgeries, as well as clinical research outcomes in medical and surgical glaucoma. He is widely published and has helped develop innovative surgical techniques and has designed several novel surgical instruments.
Dr. Grover received his medical degree from the Johns Hopkins School of Medicine, residency at the Wilmer Eye Institute, and glaucoma fellowship at the Bascom Palmer Eye Institute. Additionally, he received a Master of Public Health degree at the Harvard University School of Public Health. He also serves on the Board of Directors for the Cure Glaucoma Foundation, a charitable organization with a mission to improve access to quality care, fund transformational research, and disseminate knowledge through global outreach efforts.
Leon W. Herndon, Jr., MD
Dr. Herndon is Professor of Ophthalmology at Duke University Medical Center in Durham, NC, USA. He currently serves as Chief of the Glaucoma Division at the Duke University Eye Center, where he has trained 74 clinical fellows. Dr. Herndon is the recipient of the Distinguished Medical Alumnus Award from the UNC School of Medicine, and was the Surgery Day Lecturer at the American Glaucoma Society Annual Meeting in 2019.
Dr. Herndon’s research interests include studying novel treatment approaches in the diagnosis and management of glaucoma. He has ongoing research projects evaluating the high prevalence of primary open-angle glaucoma in Ghana, West Africa.
Kevin Kaplowitz, MD
Kevin Kaplowitz is an Associate Professor in the Department of Ophthalmology at the VA Loma Linda with Loma Linda University, CA, USA. One of his main research interests is evaluating the outcomes and success factors for glaucoma surgery.
David Kent, FRCOphth
Dr. Kent is a vitreoretinal surgeon practicing in The Vision Clinic, Kilkenny, Ireland. His research interests include the therapeutic use of light to modulate and promote repair in the aging retina. He has been a member of ARVO since 1996 and currently serves as a director of LIGHT: The International Retinal Laser Society.
Mahmoud A. Khaimi, MD
Dr. Khaimi is Clinical Professor and Glaucoma Fellowship Director of the Dean McGee Eye Institute at the University of Oklahoma in Oklahoma City, OK, USA. His clinical focus lies in the field of glaucoma, with special emphasis in innovations in MIGS, glaucoma filtration and drainage surgery, and complex cataracts. His research interests also include clinical pharmacology studies and glaucoma clinical trials.
Paul A Knepper, MD, PhD
Dr. Knepper is Associate Professor of Ophthalmology at the Feinberg School of Medicine, Northwestern University Medical School, IL, USA, as well as a Research Scientist at the University of Illinois at Chicago, IL, USA. His research interests focus on improved diagnostic modalities and treatment of primary open-angle glaucoma, Alzheimer’s disease, and age-related macular degeneration.
Natasha N. Kolomeyer, MD
Dr. Kolomeyer is a glaucoma specialist at Wills Eye Hospital, Philadelphia, PA, USA. She has published 20 peer-reviewed papers and has served on committees for the Association for Research in Vision and Ophthalmology (ARVO) and The American Academy of Ophthalmology (AAO). Dr. Kolomeyer’s research interests include clinical outcomes, public health, imaging, big data, and telemedicine.
Ryan Lamrani, BS
Ryan Lamrani started working at the Glaucoma Institute of Beverly Hills in Los Angeles, CA, USA after graduating in May 2018 from New York University with a BS degree in Public Health and Chemistry. He will be applying to medical school in the summer of 2019 with the intent of becoming an ophthalmologist. His research interests include the glaucomatous eye, epidemiology, and stem cells.
Carlo A Lavia, MD
Dr. Lavia completed his five-year residency at the Department of Ophthalmology of the University of Turin, Italy in 2018. During his residency, he took part in several clinical trials in the field of medical retina and glaucoma, with Professor Antonio Fea as main researcher. Dr. Lavia spent six months pursuing a research fellowship in medical retina, subsequently working for a year as a retina specialist at the Department of Ophthalmology of the Lariboisiere Hospital in Paris, France. He is a fellow of the European Board of Ophthalmology. Dr. Lavia has published approximately twenty original articles and reviews in peer-reviewed journals. His current interests involve MIGS and the clinical applications of OCT angiography. He currently works in the Department of Ophthalmology of the ASL TO5, Chieri-Carmagnola-Moncalieri-Nichelino, Italy.
Daniel Lee, MD
Dr. Lee is an Assistant Professor and the Director of the Glaucoma Research Center at the Wills Eye Hospital, Philadelphia, PA, USA. After obtaining his medical degree from Rutgers University’s Robert Wood Johnson Medical School, ophthalmology residency at the Yale School of Medicine, and glaucoma fellowship at the Wills Eye Hospital, Dr. Lee serves as an assistant attending surgeon on the Glaucoma Service. Dr. Lee has authored and coauthored numerous articles and lectured at local and national meetings. He is actively involved in teaching residents and fellows at Wills Eye Hospital. His current research interests include novel glaucoma treatments and the role of ocular perfusion in glaucoma pathogenesis.
Nils A. Loewen, MD, PhD
Nils Loewen is an Associate Professor in the Department of Ophthalmology at the University of Pittsburgh, PA, USA. Clinically, he is specialized in glaucoma and cataract care and microincisional glaucoma procedures that are bleb-free. He has comprehensive experience with Trabectome surgery and published extensively on factors and outcomes. In his basic research, his laboratory is focused on bioengineering of the ocular outflow system with a particular interest in the distal outflow tract.
Ralitsa Loewen, MD
Ralitsa Loewen is a physician-scientist who investigates aqueous humor outflow both clinically and in the laboratory, based in the Department of Ophthalmology at the University of Pittsburgh, PA, USA. She has developed porcine ex vivo eye models for lentiviral transduction, established methods to visualize and measure aqueous humor flow, and generated techniques to visualize microscopic aspects of the distal outflow system at high resolution and in 3D.
David Lubeck, MD
David Lubeck is a founder and world-renowned surgeon at Arbor Centers for EyeCare (IL, USA), specializing in cataract, cornea and refractive surgery. Dr. Lubeck is passionate about surgery, teaching and innovation. Dr. Lubeck teaches cataract and refractive surgery to ophthalmologists all over the world, focusing on new technologies and safe and efficient eye surgery. He is regularly a first to perform complex procedures providing patients with outstanding surgical outcomes.
In addition to a busy clinical practice, Dr. Lubeck is an Assistant Clinical Professor of Ophthalmology at the University of Illinois, Chicago and lectures regularly worldwide. He has developed curricula that have been integrated into surgical teaching programs across the USA and abroad. He has hosted and participated in live surgery programs in China, India, Vietnam, Korea, Australia, the Philippines, and the USA.
Jeffrey K. Luttrull, MD
Dr. Luttrull is a vitreoretinal surgeon and clinical researcher practicing in Ventura, CA, USA. His interests and publications include medical and surgical retina, with a special interest in retinal laser therapy. He is founder and director of LIGHT: The International Retinal Laser Society.
Ryan Machiele
Ryan Machiele is a 4th-year medical student at Campbell University, NC, USA. His research interests include evidence-based treatment modalities for various types of glaucoma. Other research interests include the relationship between intraocular pressure and systemic illness as well as eliminating barriers to care in disease-burdened areas. He will start his residency training in 2020.
Amar Mannina, MD
Amar Mannina is an ophthalmology resident at Cook County Health and Hospital Systems in Chicago, IL, USA. His research interests include treatment modalities for glaucoma, including micropulse trans-scleral diode and minimally invasive glaucoma surgery.
William Morgan, MBBS, PhD, FRANZCO
Dr. Morgan is Professor of the Lions Eye Institute, Center for Ophthalmology and Visual Science at The University of Western Australia in Nedlands, Australia. His research involves basic studies of pressure gradients in and around the optic nerve, with specific interest in the effect of cerebrospinal fluid (CSF) pressure. Derived from this, he has been recently pursuing a greater understanding of retinal venous pulsation and its relationship to CSF pressure and glaucoma. Dr. Morgan was involved with Professor Yu’s team in the development of gelatin microfistula surgery for glaucoma therapy, the XEN Gel Stent, which is currently being widely used internationally. He has a clinical and research interest in glaucoma surgery.
Thiago A. Moulin, MD
Dr. Moulin holds a medical degree from the University of São Paulo, Brazil. He is currently working with Dr. Arsham Sheybani from Washington University in St. Louis, MO, USA in the statistical modeling of glaucoma patients’ outcomes using large datasets. Since his graduation in 2015, he has also worked with big data analyses in the Saint Louis University Center for Outcomes Research. He is interested in advancing the specialty through data science, which includes the implementation of sophisticated analyses and also the proper use of machine-learning techniques in ophthalmology.
Jonathan S. Myers, MD
Dr. Myers is the Chief of the Glaucoma Service at Wills Eye Hospital and an Associate Professor of Ophthalmology, Sidney Kimmel Medical Center in Philadelphia, PA, USA. Dr Myers has participated in research involving many aspects of the diagnosis and management of glaucoma, but has particular interests in investigations involving surgical procedures, pharmaceutical options, and perimetry. .
Peter A. Netland, MD, PhD
Dr. Netland received his undergraduate degree at Princeton University, his PhD from Harvard University, and his medical degree from the University of California, San Francisco. He completed his residency in Ophthalmology, followed by a clinical fellowship in glaucoma, at the Massachusetts Eye and Ear Infirmary, Harvard Medical School. Currently, Dr. Netland is the Vernah Scott Moyston Professor and Chair, Department of Ophthalmology, University of Virginia School of Medicine, Charlottesville, VA, USA. He has written numerous peer-reviewed publications and delivered numerous named and invited lectures on clinical and surgical management of glaucoma. He has received the Life Achievement Honor Award from the American Academy of Ophthalmology and was elected to the American Ophthalmological Society.
William D. Noonan, MD, JD
Dr. Noonan is both a physician and a patent attorney who specializes in the protection of medical inventions. During his postgraduate training he participated in an ophthalmology residency. He is a partner and the Chair of the Life Sciences Patent Group at Klarquist Sparkman, LLP in Portland, OR, USA. During a 37-year career he has represented corporations, research institutes, universities, and individuals in both patent litigation and prosecution matters. For the last 20 years he has also represented the National Institutes of Health and other government agencies, making his firm the second largest supplier of legal services to the United States government over the last decade. He is listed in the Best Lawyers in America (2014-2019), IAM Patent 1000 World’s Leading Patent Practitioners (20152019), and Chambers USA Best Patent Practitioners (2010-2019).
Makena Parker, BA
Makena Parker holds a BA from the University of North Carolina at Chapel Hill (NC, USA). She is currently a second year Master of Physiology student at North Carolina State University and works as a clinical lead technician at a retina practice. Her research interests include ophthalmology with a focus on increased surgical success rates for glaucoma patients and retinal diseases.
Shyam Patel, MD
Shyam Patel is currently a cornea and external disease fellow at the Eye Consultants of Atlanta (GA, USA). He completed medical and business school at the University of Alabama at Birmingham (AL, USA), followed by ophthalmology residency at Cook County Health in Chicago, IL, USA. In addition to glaucoma, his previous research interests have included retina, oculoplastics, and pediatric ophthalmology.
Thomas Patrianakos, DO
Thomas D. Patrianakos is the Chair of Ophthalmology for Cook County Health and Hospitals System in Chicago, IL, USA. He is a board-certified ophthalmologist and a fellowship-training glaucoma specialist. His research interests include optic nerve head imaging techniques, microinvasive glaucoma surgery, and glaucoma laser surgery.
Rodolfo A. Pérez-Grossmann, MD
Dr. Perez-Grossmann graduated in Ophthalmology from the National Institute of Ophthalmology (Instituto Nacional de Oftalmología) in Lima, Perú. He completed a glaucoma fellowship at the Glaucoma Research and Education Group in San Francisco, CA, USA. He currently serves as Medical Director of the Glaucoma and Cataract Institute (Instituto de Glaucoma y Catarata) in Lima, Perú.
He is former President of the Pan American Glaucoma Society and the Latin American Glaucoma Society, founding member and first president of the Peruvian Glaucoma Society, and a member of the Steering Committee of the World Glaucoma Association. Dr. Perez-Grossmann has participated as coordinator or speaker in numerous congresses and symposiums worldwide. He holds a US patent involving the method and apparatus for trabeculectomy and suprachoroidal shunt surgery. He was one of the founders of the Hospital de la Familia volunteer group in Guatemala.
Rodolfo A. Pérez-Simons
Rodolfo A. Perez Simons is a medical student at the Scientific University of the South (Universidad Científica del Sur) in Lima, Perú. He volunteers at the the Glaucoma and Cataract Institute (Instituto de Glaucoma y Catarata) in Lima, Perú. He also took part in the foundation of the Hospital de la Familia volunteer group in Guatemala. His research interests involve medical and surgery treatments of glaucoma.
Nicholas M. Pfahler, BS
Nicholas M. Pfahler holds a BS from the University of Illinois at Chicago, IL, USA and is currently a Research Associate at the same university. His research interests include cellular mechanisms of neurodegeneration, identification of therapeutic targets in Alzheimer’s disease, primary open-angle glaucoma, and age-related macular degeneration, as well as visual processing.
Leonard Pinchuk PhD, DSc (h.c.), NAE
Dr. Pinchuk is a Distinguished Research Professor of Biomedical Engineering at the University of Miami (FL, USA). He is also the founder, Chairman Emeritus, and Chief Scientific Officer of InnFocus, Inc., a Santen Company (FL, USA). Dr. Pinchuk is a biomaterials scientist with seminal patents in the area of angioplasty balloons, coronary stents, stent grafts, drug-eluting stents, biomaterials (including polycarbonate urethane and SIBS), the PRESERFLO MicroShunt, and the next-generation intraocular lens materials. He is also the 2019 Russ Prize Laureate. His current interests involve the interpretation of clinical results of the PRESERFLO MicroShunt, developing new methods of preserving the bleb, reinterpreting the drainage system from the glaucomatous eye based upon new information gleaned from MIGS and OCT, and other ocular devices.
M.
Reza Razeghinejad, MD
Dr. Razeghinejad currently serves as Associate Professor of Ophthalmology at Wills Eye Hospital, Sidney Kimmel Medical College, Thomas Jefferson University in Philadelphia, PA, USA, and Co-Director of glaucoma fellowship of the Glaucoma Service. Dr. Razeghinejad’s research focuses on the medical and surgical management of glaucoma. His research has been published in over 100 peer-reviewed publications, including major ophthalmology journals, and several book chapters.
Isabelle Riss, MD
Professor Riss is Director of the Ophthalmology Department at Clinique Mutualiste de Pessac in Pessac, France. Her research interests focus on glaucoma surgical techniques, methods of maintaining blebs, and clinical trials, as well as studies involving new glaucoma devices, including Alcon’s ExPress Shunt and the PRESERFLO MicroShunt.
Steven R. Sarkisian, Jr., MD
Dr. Sarkisian is founder and CEO of Oklahoma Eye Surgeons in Oklahoma City, OK,Dr. Sarkisian is founder and CEO of Oklahoma Eye Surgeons in Oklahoma City, OK,USA. He has an active clinical practice with a particular interest in surgical innovation for the treatment of glaucoma and cataracts, with extensive research involvement in numerous FDA clinical trials, particularly involving MIGS. He was part of pivotal FDA trials for the CyPass, iStent Inject, iStent Supra, and iDose.
Simona Scalabrin, MD
Dr. Scalabrin is currently a Resident in the Ophthalmology Unit at the Department of Surgical Sciences of the City of Health and Science University Hospital of Turin (Italy). She received her summa cum laude medical degree from the University of Turin in 2015 and attended the Scuola di Studi Superiori “Ferdinando Rossi”, an elite Italian institution of higher education. Her current interests involve the etiopathogenesis of optic nerve disorders, with particular attention to the impact of sex hormones, medical and surgical glaucoma therapy, and stem-cell treatment of eye disease.
Jonathan Shakibkhou
Jonathan Shakibkhou graduated from UCLA and is the research manager at the Glaucoma Research Institute of Beverly Hills in Los Angeles, CA, USA. Mr. Shakibkhou is interested in the development and efficacy of novel surgical methods in the treatment glaucoma. He was worked with Dr. Michael Berlin on excimer laser trabeculectomy research, testing the efficacy of this procedure in comparison to other surgical and non-surgical treatment options. Further, he has been actively involved in raising awareness about glaucoma and presenting data that is comprehensible to the general population.
Arsham Sheybani, MD
Dr. Arsham Sheybani completed his medical degree at Washington University School of Medicine in St. Louis, MO, USA. He then completed his residency in Ophthalmology at Washington University in St. Louis and was selected to remain on faculty as Chief Resident. During that year, Dr. Sheybani was responsible for ophthalmologic trauma and emergencies as well as all adult inpatient ophthalmology consultations at Barnes Jewish Hospital. He was the primary surgical teacher for the beginning residents and implemented a didactic system that is still used at Washington University. He then completed a fellowship with Ike Ahmed in Glaucoma and Advanced Anterior Segment Surgery in Toronto, Canada. Dr. Sheybani subsequently returned to Washington University School of Medicine as faculty in the Department of Ophthalmology and Visual Sciences where he serves as Residency Program Director and Assistant Professor of Ophthalmology. He has presented research internationally and is currently involved in device design aiming to make glaucoma surgery safer amongst many other endeavors. He is an avid surgical teacher, winning the resident selected faculty teaching award early in his career. He has also helped create one of the highest volume surgical glaucoma fellowships in the country serving as the fellowship director.


Ingeborg Stalmans, MD, PhD
Professor Dr. Ingeborg Stalmans heads the Laboratory of Ophthalmology at the Catholic University of Leuven (KU Leuven), as well as the Glaucoma Unit of the University Hospitals in Leuven (UZ Leuven) in Belgium. The subject of her PhD was the role of vascular endothelial growth factor (VEGF) in retinal angiogenesis and in the pathogenesis of DiGeorge syndrome. This work resulted in several high-impact papers published in journals such as Nature, Cell, and PNAS, and was rewarded by the prestigious GlaxoSmithKline prize. The current focus of her basic and clinical research work is medical glaucoma therapy, glaucoma surgery, and retinal imaging as a biomarker for systemic diseases. She has published in Cell, Ophthalmology, Journal of Glaucoma, IOVS, etc. Her work has been awarded with prizes from the Funds for Research in Ophthalmology (FRO) and the Pfizer Glaucoma Research Award. As a glaucoma specialist and researcher, she frequently lectures both nationally and internationally, including at ARVO, WGC, ISGS, EVER, EGS, ESCRS, SOE, and ESASO. Within the European Glaucoma society, she is a member of the Executive Committee, treasurer, chair of the Communication Committee, as well as co-chair of the program-planning committee. She also serves on the Board of Governors of the World Glaucoma Association (WGA) and in the Glaucoma Expert Committee of the European Vision Institute Clinical Research Network (EVICR.net). She is the Treasurer of the Belgian Glaucoma Society and a member of the Royal Academy of Medicine of Belgium.
Er-Ning Su, MD, PhD
Dr. Su is Associate Research Professor of the Lions Eye Institute, Center for Ophthalmology and Visual Science at The University of Western Australia in Nedlands, Australia. Her research mostly involves in vitro studies of vasoactivity of retinal arteries and veins. Dr. Su has developed a microperfusion system that allows vasoactivity to be assessed in real time whilst perfusing or bathing the vessels with putative vasoactive compounds. The aim is to better understand the mechanisms of blood flow control in the eye and look for potential vasoactive compounds that could be useful clinically. She has also developed a custom-built system to produce a bioengineered cross-linked gelatin microfistula for experimental use in new forms of glaucoma filtration surgery.
David L. Swain, BA
David L. Swain holds a BA in Biology and English from Boston University (MA, USA). During his undergraduate studies he participated in the investigation of morphological differences in the scleral spur between normal and glaucoma eyes. Currently, he is an MD/PhD candidate in the department of Anatomy and Neurobiology at Boston University School of Medicine, and is completing his PhD thesis in the laboratory of Dr. Gong. His research interests include mechanisms of increased resistance in the aqueous outflow pathway of eyes with primary open-angle glaucoma, and the structure and function of the inner wall endothelial cells of Schlemm’s canal.
Marc Töteberg-Harms, MD, FEBO
Dr. Töteberg-Harms is a glaucoma specialist and attending physician at the University Hospital Zurich, Department of Ophthalmology and a clinical instructor and lecturer (Privatdozent) with the University of Zurich in Switzerland. He went to Charité Medical School, Humboldt University Berlin, Germany and to the University of Kiel, Germany, where he graduated from. He earned his medical doctorate degree and the venia legendi at University of Zurich Medical School. Later, he completed clinical and basic research glaucoma fellowships at the Massachusetts Eye and Ear Infirmary, Boston, MA, and Case Western Reserve University, Cleveland, OH, in the United States. His research interests focus on glaucoma diagnosis (OCT, visual field testing, and different tonometry techniques) and efficacy and safety of surgical procedures, especially MIGS procedures.
Vanessa Vera, MD
Dr. Vera is a glaucoma specialist and a surgical consultant for Kelotec, Fs-Eye, and Allergan. She has published numerous peer-reviewed papers and book chapters, and has over ten patents and patent applications in the USA. Her research interests include novel medical and laser treatments, as well as new devices and surgical options for glaucoma.
Susannah Waxman, BA
Susannah Waxman is the Laboratory Manager of the Loewen Lab for Outflow Tract Engineering at the Department of Ophthalmology of the University of Pittsburgh, PA, USA. Her research interest is the conventional outflow tract. Her background in plant physiology and food safety has led to increasingly translational research interests in human physiology. She is set to start a PhD in the Interdisciplinary Biomedical Graduate Program at the University of Pittsburgh.
Alan Wenger, MD
Dr. Wenger is Chief of the Glaucoma Service at Hospital San Juan de Dios in Santiago, Chile. He graduated in Ophthalmology from the National Institute of Ophthalmology (Instituto Nacional de Oftalmología) in Lima, Perú and then completed a fellowship in Clinical and Surgical Glaucoma at Hadassah University Medical Center in Jerusalem, Israel. His current interests involve glaucoma clinical research and development of novel glaucoma surgeries.
Jithin Yohannan, MD, MPH
Jithin Yohannan is an Assistant Professor of Ophthalmology at the Wilmer Eye Institute, Johns Hopkins University School of Medicine (Baltimore, MD, USA). His practice specializes in medical, laser, and surgical treatment of glaucoma, with a focus on minimally invasive glaucoma surgery and new glaucoma surgical devices. He also performs both routine and complex cataract surgery. Furthermore, Dr. Yohannan specializes in the surgical management of complex problems of the anterior segment; these problems include issues that arise after trauma or prior surgery gone wrong, such as dislocated intraocular lenses, or iris and pupil defects.
Dr. Yohannan earned his bachelor’s degree in biochemistry from New York University, where he graduated summa cum laude. He then received his medical and Master of Public Health degrees from Johns Hopkins University and completed an ophthalmology residency at the Wilmer Eye Institute, Johns Hopkins University School of Medicine. From there, he served as a fellow in glaucoma and advanced anterior-segment surgery at the University of Toronto, Canada, with Ike Ahmed. Subsequently, he returned to serve as Assistant Chief of Service at the Wilmer Eye Institute.
Dr. Yohannan’s research focuses on using artificial-intelligence algorithms to improve the tests that are used to diagnose and monitor glaucoma. His background in biostatistics, epidemiology, and mathematics enables this effort. The ultimate goal of this research is to detect glaucoma and determine when it is worsening more accurately. The results of this work will ultimately help guide doctors who are managing glaucoma to make better treatment decisions. Dr. Yohannan also has a clinical and research interest in novel surgical devices used to treat glaucoma. These devices hold the promise of making glaucoma surgery safer and easier to recover from.
Dao-Yi Yu, MD, PhD
Dr. Yu is Professor of the Lions Eye Institute, Center for Ophthalmology and Visual Science at The University of Western Australia in Nedlands, Australia. His research interests cover many fields in ophthalmology, including glaucoma, retinal diseases, vascular biology, and retinal metabolism. He leads a highly innovative team and has established more than ten laboratories performing experimental research and transferring to clinical therapeutics and diagnostics. As lead inventor, he has worked with his team to develop a new glaucoma surgery including a crossed-linked gelatin microfistula, an ab interno implantation and needle type implanter to perform MIGS, now in clinical use under the name XEN Gel Stent. Currently, the team is interested in further improving the outcomes of glaucoma filtration surgery.