Radiology-Nuclear Medicine Diagnostic Imaging Ali Gholamrezanezhad
Visit to download the full and correct content document: https://ebookmass.com/product/radiology-nuclear-medicine-diagnostic-imaging-ali-gh olamrezanezhad/
More products digital (pdf, epub, mobi) instant download maybe you interests ...

Core Radiology: A Visual Approach to Diagnostic Imaging
https://ebookmass.com/product/core-radiology-a-visual-approachto-diagnostic-imaging/

Diagnostic Imaging: Interventional Radiology 3rd Edition Brandt C. Wible
https://ebookmass.com/product/diagnostic-imaging-interventionalradiology-3rd-edition-brandt-c-wible/

Essentials of Nuclear Medicine and Molecular Imaging 7th Edition
https://ebookmass.com/product/essentials-of-nuclear-medicine-andmolecular-imaging-7th-edition/
Grainger & Allison’s Diagnostic Radiology. A Textbook of Medical Imaging 7th Edition Andreas Adam
https://ebookmass.com/product/grainger-allisons-diagnosticradiology-a-textbook-of-medical-imaging-7th-edition-andreas-adam/
Nuclear
Medicine and Molecular Imaging: the Requisites
5th
Edition
Janis P. O'Malley
https://ebookmass.com/product/nuclear-medicine-and-molecularimaging-the-requisites-5th-edition-janis-p-omalley/

Coronavirus Disease 2019 (Covid-19): A Clinical Guide
1st Edition Ali Gholamrezanezhad
https://ebookmass.com/product/coronavirusdisease-2019-covid-19-a-clinical-guide-1st-edition-aligholamrezanezhad/
Grainger &
Allison’s
Lee Alexander Grant
Diagnostic Radiology. Essentials
https://ebookmass.com/product/grainger-allisons-diagnosticradiology-essentials-lee-alexander-grant/
Textbook of Radiology And Imaging, Vol 2 Bharat Aggarwal
https://ebookmass.com/product/textbook-of-radiology-and-imagingvol-2-bharat-aggarwal/
Diagnostic Imaging Genitourinary 4th Edition Ganeh Fananapazir
https://ebookmass.com/product/diagnostic-imaginggenitourinary-4th-edition-ganeh-fananapazir/
Radiology-Nuclear Medicine Diagnostic
Imaging: A Correlative Approach
Radiology-Nuclear Medicine Diagnostic Imaging: A Correlative Approach
Edited by Ali Gholamrezanezhad, MD
AssociateProfessorof Clinical Radiology, Keck School of Medicine Universityof SouthernCalifornia Los Angeles, CA, USA
Majid Assadi, MD, MSc
Professor, Department of Radiology, School of Medicine
Director, Nuclear Medicine and Molecular Imaging Research Center
Bushehr University of Medical Sciences Bushehr, Iran
Hossein Jadvar, MD, PhD, MPH, MBA
Professor of Radiology, Urology, and Biomedical Engineering
Keck School of Medicine and Viterbi School of Engineering University of Southern California Los Angeles, CA, USA
This edition first published 2023 © 2023 John Wiley & Sons Ltd
All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by law. Advice on how to obtain permission to reuse material from this title is available at http://www.wiley.com/go/permissions.
The right of Ali Gholamrezanezhad, Majid Assadi, and Hossein Jadvar to be identified as the authors of the editorial material in this work has been asserted in accordance with law.
Registered Offices
John Wiley & Sons, Inc., 111 River Street, Hoboken, NJ 07030, USA
John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK
For details of our global editorial offices, customer services, and more information about Wiley products visit us at www.wiley.com.
Wiley also publishes its books in a variety of electronic formats and by print-on-demand. Some content that appears in standard print versions of this book may not be available in other formats.
Trademarks: Wiley and the Wiley logo are trademarks or registered trademarks of John Wiley & Sons, Inc. and/or its affiliates in the United States and other countries and may not be used without written permission. All other trademarks are the property of their respective owners. John Wiley & Sons, Inc. is not associated with any product or vendor mentioned in this book.
Limit of Liability/Disclaimer of Warranty
The contents of this work are intended to further general scientific research, understanding, and discussion only and are not intended and should not be relied upon as recommending or promoting scientific method, diagnosis, or treatment by physicians for any particular patient. In view of ongoing research, equipment modifications, changes in governmental regulations, and the constant flow of information relating to the use of medicines, equipment, and devices, the reader is urged to review and evaluate the information provided in the package insert or instructions for each medicine, equipment, or device for, among other things, any changes in the instructions or indication of usage and for added warnings and precautions. While the publisher and authors have used their best efforts in preparing this work, they make no representations or warranties with respect to the accuracy or completeness of the contents of this work and specifically disclaim all warranties, including without limitation any implied warranties of merchantability or fitness for a particular purpose. No warranty may be created or extended by sales representatives, written sales materials or promotional statements for this work. The fact that an organization, website, or product is referred to in this work as a citation and/or potential source of further information does not mean that the publisher and authors endorse the information or services the organization, website, or product may provide or recommendations it may make. This work is sold with the understanding that the publisher is not engaged in rendering professional services. The advice and strategies contained herein may not be suitable for your situation. You should consult with a specialist where appropriate. Further, readers should be aware that websites listed in this work may have changed or disappeared between when this work was written and when it is read. Neither the publisher nor authors shall be liable for any loss of profit or any other commercial damages, including but not limited to special, incidental, consequential, or other damages.
Library of Congress Cataloging-in-Publication Data applied for ISBN: 9781119603610 (hardback)
Cover Design: Wiley
Cover Images: © semakokal/iStock/Getty Images, wenht/iStock/Getty Images
Set in 9.5/12.5pt STIXTwoText by Straive, Pondicherry, India
Dedicated to Mojgan, Donya, and Delara, with love. . .
Hossein Jadvar
To my family especially my mother, Maryam, my wife, Moloud, my sons, Arian and Aiden. For their endless sacrifices they have made to make my life most rewarding Majid Assadi
To those contributed to my education and excellence, especially my mother (the best teacher I have ever had), Fatemeh, my brother, Hadi, my wife, Farzaneh, and my son, Adrian and
To my patients, those who I served with the deepest gratitude and appreciation. Ali Gholamrezanezhad
Contents
List of Contributors x Preface xvii
1 Introductionto CorrelativeImaging:WhatRadiologistsand NuclearMedicinePhysiciansShould Know on HybridImaging 1
Prathamesh V. Joshi, Alok Pawaskar, and Sandip Basu
2 BasicPrinciplesof HybridImaging 30
Leda Lorenzon, M. Bonelli, A. Fracchetti, and P. Ferrari
3 Cross-sectionalCorrelatefor IntegrativeImaging(AnatomicalRadiology) 52
Antonio Jesús Láinez Ramos-Bossini, Ángela Salmerón-Ruiz, José Pablo Martínez Barbero, José Pablo
Martín Molina, José Luis Martín Rodríguez, Genaro López Milena, and Fernando Ruiz Santiago
4 Radiopharmaceuticals 133
Ferdinando Calabria, Mario Leporace, Rosanna Tavolaro, and Antonio Bagnato
5 Diseasesof theCentralNervousSystem 163
Hiroshi Matsuda, Eku Shimosegawa, Yoko Shigemoto, Noriko Sato, Hiroyuki Fujii, Fumio Suzuki, Yukio Kimura, and Atsuhiko Sugiyama
6 PETImaginginGliomas:ClinicalPrinciplesandSynergieswithMRI 194
Riccardo Laudicella, C. Mantarro, B. Catalfamo, P. Alongi, M. Gaeta, F. Minutoli, S. Baldari, and Sotirios Bisdas
7 Diseasesof theHeadand Neck 219
Florian Dammann and Jan Wartenberg
8 TheRoleof NoninvasiveCardiacImagingin theManagementof Diseases of theCardiovascularSystem 257
Ahmed Aljizeeri and Mouaz H. Al-Mallah
9 VascularSystem 285
Ahmad Shariftabrizi, Khalid Balawi, and Janet H. Pollard
10Diseasesof thePulmonarySystem 308
Murat Fani Bozkurt and Bilge Volkan-Salanci
11ThoracicMalignancies 333
Sanaz Katal, Thomas G. Clifford, Kanhaiyalal Agrawal, and Ali Gholamrezanezhad
12ACorrelativeApproachto BreastImaging 351
Shabnam Mortazavi, Sonya Khan, Kathleen Ruchalski, Cory Daignault, and Jerry W. Froelich
13CorrelativeImagingof BenignGastrointestinalDisorders 383
Mariano Grosso, Michela Gabelloni, Emanuele Neri, and Giuliano Mariani
14GastrointestinalMalignancies 407
Janet H. Pollard, Paul A. DiCamillo, Ayca Dundar, Sarah L. Averill, and Yashant Aswani
15HepatobiliaryImaging 456
Janet H. Pollard
16CorrelativeImagingin EndocrineDiseases 485
Sana Salehi, Farshad Moradi, Doina Piciu, Hojjat Ahmadzadehfar, and Ali Gholamrezanezhad
17CorrelativeImagingin NeuroendocrineTumors 512
Ameya Puranik, Sonal Prasad, Indraja D. Devi, and Vikas Prasad
18Nephro-urinaryTractPathologies:ACorrelativeImagingApproach 521
Salar Tofighi, Thomas G. Clifford, Saum Ghodoussipour, Peter Henry Joyce, Meisam Hoseinyazdi, Maryam Abdinejad, Saeideh Najafi, Fahad Marafi, and Russell H. Morgan
19CorrelativeApproachto ProstateImaging 533
Soheil Kooraki and Hossein Jadvar
20CorrelativeImagingof theFemaleReproductiveSystem 554
Sanaz Katal, Akram Al-Ibraheem, Fawzi Abuhijla, Ahmad Abdlkadir, Liesl Eibschutz, and Ali Gholamrezanezhad
21MusculoskeletalImaging 577
George R. Matcuk, Jr., Jordan S. Gross, Dakshesh B. Patel, Brandon K. K. Fields, Dorian M. Lapalma, and Daniel Stahl
22SpineDisorders:CorrelativeImagingApproach 625
Azadeh Eslambolchi, Amit Gupta, Jay Acharya, Christopher Lee, and Kaustav Bera
23Osteoporosis:DiagnosticImagingand Valueof MultimodalityApproachin DifferentiatingBenignVersus PathologicCompressionFractures 659
Daniela Garcia, Shambo Guha Roy, and Reza Hayeri
24EmergencyRadiology 671
Sean K. Johnston, Russell Flato, Peter Hu, Peter Henry Joyce, and Andrew Chong
25CorrelativeImaging of PediatricDiseases 693
Seth J. Crapp, Rachel Pevsner Crum, Nolan Altman, Jyotsna Kochiyil, Eshani Sheth, and Caldon J. Esdaille
26Infection/InflammationImaging 717
Christopher J. Palestro and Charito Love
27Imagingthe LymphaticSystem 747
Girolamo Tartaglione, Marco Pagan, Francesco Pio Ieria, Giuseppe Visconti, and Tommaso Tartaglione
28Lymphomaand MyelomaCorrelativeImaging 772
Pavel Gelezhe, Sergey Morozov, Anton Kondakov, and Mikhail Beregov
29ClinicalApplicationof PET/MRI 788
Laura Evangelista, Paolo Artoli, Paola Bartoletti, Antonio Bignotto, Federica Menegatti, Marco Frigo, Stefania Antonia Sperti, Laura Vendramin, and Diego Cecchin
30 68Ga-FAPI,aTwinTracer for 18F-FDGintheEra of EvolvingPETImaging 814
Reyhaneh Manafi-Farid, GhasemAli Divband, HamidReza Amini, Thomas G. Clifford, Ali Gholamrezanezhad, Mykol Larvie, and Majid Assadi
31ArtificialIntelligencein DiagnosticImaging 826
Martina Sollini, Daniele Loiacono, Daria Volpe, Alessandro Giaj Levra, Elettra Lomeo, Edoardo Giacomello, Margarita Kirienko, Arturo Chiti, and Pierluca Lanzi
32RadionuclideTherapiesand CorrelativeImaging 838
Ashwin Singh Parihar and Erik Mittra
Index 871
List of Contributors
Maryam Abdinejad
Department of Radiology, Namazi Hospital, Shiraz, Iran
Department of Nuclear Medicine, Namazi Hospital, Shiraz, Iran
Ahmad Abdlkadir
Department of Nuclear Medicine, King Hussein Cancer Center, Amman, Jordan
Fawzi Abuhijla
Department of Radiation Oncology, King Hussein Cancer Center, Amman, Jordan
Jay Acharya
Radiology, Keck School of Medicine of USC, HCCII Lower Level Radiology, Los Angeles, CA, USA
Kanhaiyalal Agrawal
Department of Nuclear Medicine, All India Institute of Medical Sciences, Bhubaneswar, India
Hojjat Ahmadzadehfar
Department of Nuclear Medicine, Klinikum Westfalen, Dortmund, Germany
Akram Al-Ibraheem
Department of Nuclear Medicine, King Hussein Cancer Center, Amman, Jordan
Ahmed Aljizeeri
King Abdulaziz Cardiac Center, Riyadh, Saudi Arabia
King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
Mouaz H. Al-Mallah
Houston Methodist DeBakey Heart & Vascular Center, Houston Methodist Hospital, Houston, TX, USA
P. Alongi
Unit of Nuclear Medicine, Fondazione Istituto G. Giglio, Cefalù, Italy
Nolan Altman
Nicklaus Children’s Hospital, Miami, FL, USA
HamidReza Amini
Khatam PET-CT Center, Khatam Hospital, Tehran, Iran
Paolo Artoli
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Majid Assadi
Department of Radiology, School of Medicine, Nuclear Medicine and Molecular Imaging Research Center Bushehr University of Medical Sciences Bushehr, Iran
Yashant Aswani
University of Iowa, Carver College of Medicine, Iowa City, IA, USA
Sarah L. Averill
University of Iowa, Carver College of Medicine, Iowa City, IA, USA
Iowa City Veterans Administration Healthcare System, Iowa City, IA, USA
Antonio Bagnato
Department of Nuclear Medicine and Theranostics, “Mariano Santo” Hospital, Cosenza, Italy
Khalid Balawi
University of Iowa Carver College of Medicine, Iowa City, IA, USA
S. Baldari
Department of Biomedical Sciences and Morphological and Functional Imaging, Nuclear Medicine Unit, University of Messina, Messina, Italy
José Pablo Martínez Barbero
Department of Radiology, Virgen de las Nieves University Hospital, University of Granada, Granada, Spain
Paola Bartoletti
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Sandip Basu
Radiation Medicine Centre, Bhabha Atomic Research Centre, Tata Memorial Centre Annexe, Parel, Mumbai, Maharashtra, India
Homi Bhabha National Institute, Mumbai, Maharashtra, India
Kaustav Bera
Case Western Reserve University School of Medicine, University Hospital Cleveland Medical Center, Cleveland, OH, USA
Mikhail Beregov
Federal Center for Cerebrovascular Pathology and Stroke, Department of Radiology and Functional Diagnostics, Moscow, Russia
Antonio Bignotto
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Sotirios Bisdas
Department of Brain Repair and Rehabilitation, UCL
Queen Square Institute of Neurology, University College London, London, UK
Lysholm Department of Neuroradiology, The National Hospital for Neurology and Neurosurgery, UCLH NHS Foundation Trust, London, UK
M. Bonelli
Department of Medical Physics, Central Hospital of Bolzano, Bolzano, Italy
Ferdinando Calabria
Department of Nuclear Medicine and Theranostics, “Mariano Santo” Hospital, Cosenza, Italy
B. Catalfamo
Department of Biomedical Sciences and Morphological and Functional Imaging, Nuclear Medicine Unit, University of Messina, Messina, Italy
Diego Cecchin
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Arturo Chiti
Department of Biomedical Sciences, Humanitas University, Milan, Italy
IRCCS Humanitas Research Hospital, Milan, Italy
Andrew Chong
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Thomas G. Clifford
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Seth J. Crapp
Pediatric Teleradiology Partners, Miami, FL, USA
Rachel Pevsner Crum
Nicklaus Children’s Hospital, Miami, FL, USA
Cory Daignault
Minneapolis VA Medical Center, Minneapolis, MN, USA
Florian Dammann
Department of Diagnostic, Interventional and Pediatric Radiology, Inselspital, University Hospital Bern, Switzerland
Indraja D. Devi
Department of Nuclear Medicine, Tata Memorial Hospital, Homi Bhabha National Institute (HBNI), Mumbai, Maharashtra, India
Paul A. DiCamillo
University of Iowa, Carver College of Medicine, Iowa City, IA, USA
GhasemAli Divband
Nuclear Medicine Center, Jam Hospital, Tehran, Iran
Khatam PET-CT Center, Khatam Hospital, Tehran, Iran
Ayca Dundar
University of Iowa, Carver College of Medicine, Iowa City, IA, USA
Liesl Eibschutz
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Caldon J. Esdaille
Howard University College of Medicine, Washington, DC, USA
Azadeh Eslambolchi
Pediatric Radiology Section, Mallinckrodt Institute of Radiology, Washington University in St Louis, School of Medicine, St. Louis, MO, USA
Laura Evangelista
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Murat Fani Bozkurt
Department of Nuclear Medicine, Hacettepe University Faculty of Medicine, Ankara, Turkey
P. Ferrari
Department of Medical Physics, Central Hospital of Bolzano, Bolzano, Italy
Brandon K. K. Fields
Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Russell Flato
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
A. Fracchetti
Department of Medical Physics, Central Hospital of Bolzano, Bolzano, Italy
Marco Frigo
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Jerry W. Froelich
Radiology, University of Minnesota, Minneapolis, MN, USA
Hiroyuki Fujii
Department of Radiology, National Center of Neurology and Psychiatry, Kodaira, Japan
Michela Gabelloni
Diagnostic and Interventional Radiology, Department of Translational Research and Advanced Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy
M. Gaeta
Section of Radiological Sciences, Department of Biomedical Sciences and Morphological and Functional Imaging, University of Messina, Messina, Italy
Daniela Garcia
Department of Radiology, Mercy Catholic Medical Center, Darby, PA, USA
Pavel Gelezhe
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of the Moscow Health Care Department, Moscow, Russia
European Medical Center, Radiology Department, Moscow, Russia
Saum Ghodoussipour
Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ, USA
Section of Urologic Oncology, Rutgers Cancer Institute of New Jersey, New Brunswick, NJ, USA
Ali Gholamrezanezhad
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Edoardo Giacomello
Dipartimento di Elettronica, Informazione e Bioingegneria, Politecnico di Milano, Milano, Italy
Jordan S. Gross
Department of Radiology, University of California, Los Angeles, Los Angeles, CA, USA
Mariano Grosso
Regional Center of Nuclear Medicine, Department of Translational Research and Advanced Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy
Amit Gupta
Radiology, Medicine and Biomedical Engineering, Case Western Reserve University School of Medicine, Cleveland, OH, USA
Cancer Imaging Program, Case Comprehensive Cancer Center, Cleveland, OH, USA
Diagnostic Radiography, University Hospital Cleveland Medical Center, Cleveland, OH, USA
Reza Hayeri
Department of Radiology, Mercy Catholic Medical Center, Darby, PA, USA
Meisam Hoseinyazdi
Shiraz University of Medical Sciences, Shiraz, Iran
Department of Radiology, Namazi Hospital, Shiraz, Iran
Peter Hu
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Hossein Jadvar
Professor of Radiology, Urology, and Biomedical Engineering, Keck School of Medicine and Viterbi School of Engineering, University of Southern California, Los Angeles, CA, USA
Sean K. Johnston
Department of Radiology, Division of Emergency Radiology, Keck School of Medicine of USC, LAC+USC Medical Center, Los Angeles, CA, USA
Prathamesh V. Joshi
Department of Nuclear Medicine & PET- CT, Kamalnayan Bajaj Hospital, Aurangabad, Maharashtra, India
Radiation Medicine Centre, Bhabha Atomic Research Centre, Tata Memorial Centre Annexe, Parel, Mumbai, Maharashtra, India
Peter Henry Joyce
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Sanaz Katal
Nuclear Medicine Fellow, Medical Imaging Department, St Vincent’s Hospital Melbourne, Australia
Sonya Khan
Los Angeles and Veterans Administration, Greater Los Angeles Healthcare Systems, University of California, Los Angeles, CA, USA
Yukio Kimura
Department of Radiology, National Center of Neurology and Psychiatry, Kodaira, Japan
Margarita Kirienko
Department of Nuclear Medicine, Istituto Nazionale per lo Studio e la Cura dei Tumori, Milano, Italy
Jyotsna Kochiyil
Mount Sinai Medical Center, Miami Beach, FL, USA
Anton Kondakov
Central Clinical Hospital of the Russian Academy of Sciences, Nuclear Medicine Department, Moscow, Russia
Pirogov Russian National Research Medical University, Department of Radiology and Radiation Therapy, Moscow, Russia
Soheil Kooraki
Department of Molecular and Medical Pharmacology, David Geffen School of Medicine at UCLA, University of California, Los Angeles, CA, USA
Pierluca Lanzi
Dipartimento di Elettronica, Informazione e Bioingegneria, Politecnico di Milano, Milano, Italy
Dorian M. Lapalma
Department of Radiology, University of Southern California, Los Angeles, CA, USA
Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Mykol Larvie
Department of Radiology, Cleveland Clinic, Cleveland, OH, USA
Riccardo Laudicella
Department of Biomedical Sciences and Morphological and Functional Imaging, Nuclear Medicine Unit, University of Messina, Messina, Italy
Christopher Lee
Keck School of Medicine of USC, HCCII Lower Level Radiology, Los Angeles, CA, USA
Mario Leporace
Department of Nuclear Medicine and Theranostics, “Mariano Santo” Hospital, Cosenza, Italy
Alessandro Giaj Levra
IRCCS Humanitas Research Hospital, Milan, Italy
Daniele Loiacono
Dipartimento di Elettronica, Informazione e Bioingegneria, Politecnico di Milano, Milano, Italy
Elettra Lomeo
IRCCS Humanitas Research Hospital, Milan, Italy
Leda Lorenzon
Department of Medical Physics, Central Hospital of Bolzano, Bolzano, Italy
Charito Love
Radiology, Albert Einstein College of Medicine, Bronx, NY, USA
Reyhaneh Manafi-Farid
Research Center for Nuclear Medicine, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran
C.Mantarro
Department of Biomedical Sciences and Morphological and Functional Imaging, Nuclear Medicine Unit, University of Messina, Messina, Italy
Fahad Marafi
Jaber Al-Ahmad Center for Molecular Imaging, Kuwait City, Kuwait
Giuliano Mariani
Regional Center of Nuclear Medicine, Department of Translational Research and Advanced Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy
José Pablo Martín Molina
Department of Radiology, San Cecilio University Hospital, University of Granada, Granada, Spain
George R. Matcuk, Jr.
Department of Imaging, Cedars-Sinai Medical Center, Los Angeles, CA, USA
Hiroshi Matsuda
Integrative Brain Imaging Center, National Center of Neurology and Psychiatry, Kodaira, Japan
Federica Menegatti
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Genaro López Milena
Department of Radiology, Virgen de las Nieves University Hospital, University of Granada, Granada, Spain
F. Minutoli
Department of Biomedical Sciences and Morphological and Functional Imaging, Nuclear Medicine Unit, University of Messina, Messina, Italy
Erik Mittra
Department of Diagnostic Radiology, Division of Nuclear Medicine & Molecular Imaging, Oregon Health & Science University, Portland, OR, USA
Farshad Moradi
Department of Radiology, Division of Nuclear Medicine, Stanford, CA, USA
Russell H. Morgan
Department of Radiology and Radiological Science, Johns Hopkins Medical Institution, Baltimore, MD, USA
Sergey Morozov
Chief innovation officer, Osimis S.A., Belgium
Shabnam Mortazavi
Radiology, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA
Saeideh Najafi
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Emanuele Neri
Diagnostic and Interventional Radiology, Department of Translational Research and Advanced Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy
Marco Pagan
Nuclear Medicine, Cristo Re Hospital, Rome, Italy
Christopher J. Palestro
Radiology, Donald & Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY, USA
Nuclear Medicine & Molecular Imaging, Northwell Health, New Hyde Park, NY, USA
Ashwin Singh Parihar
Department of Nuclear Medicine, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Mallinckrodt Institute of Radiology, Washington University School of Medicine, St Louis, MO, USA
Dakshesh B. Patel
Department of Radiology, University of Southern California, Los Angeles, CA, USA
Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Alok Pawaskar
Radiation Medicine Centre, Bhabha Atomic Research Centre, Tata Memorial Centre Annexe, Parel, Mumbai, Maharashtra, India
Department of Nuclear Medicine & PET- CT, Shri Siddhivinayak Ganapati Cancer Hospital, Miraj, Maharashtra, India
Doina Piciu
Department of Endocrine Tumors and Nuclear Medicine, Institute of Oncology Ion Chiricuta and University of Medicine Iuliu Hatieganu, Cluj-Napoca, Romania
Francesco Pio Ieria
Nuclear Medicine, Cristo Re Hospital, Rome, Italy
Janet H. Pollard
University of Iowa Carver College of Medicine, Iowa City, IA, USA
Sonal Prasad
Berlin Experimental Radionuclide Imaging Center, Berlin, Germany
Department of Nuclear Medicine, CharitéUniversitaetsmedizin, Berlin, Germany
Vikas Prasad
Department of Nuclear Medicine, University Hospital, Ulm, Germany
Ameya Puranik
Department of Nuclear Medicine, Tata Memorial Hospital, Homi Bhabha National Institute (HBNI), Mumbai, Maharashtra, India
Antonio Jesús Láinez Ramos-Bossini
Department of Radiology, Virgen de las Nieves University Hospital, University of Granada, Granada, Spain
José Luis Martín Rodríguez
Department of Radiology, San Cecilio University Hospital, University of Granada, Granada, Spain
Shambo Guha Roy
Department of Radiology, Mercy Catholic Medical Center, Darby, PA, USA
Kathleen Ruchalski
Radiology, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA
Sana Salehi
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Ángela Salmerón-Ruiz
Department of Radiology, Virgen de las Nieves University Hospital, University of Granada, Granada, Spain
Fernando Ruiz Santiago
Department of Radiology, Virgen de las Nieves University Hospital, University of Granada, Granada, Spain
Neuro-traumatology Hospital, Virgen de las Nieves University Hospital, School of Medicine, University of Granada, Granada, Spain
Noriko Sato
Department of Radiology, National Center of Neurology and Psychiatry, Kodaira, Japan
Ahmad Shariftabrizi
University of Iowa Carver College of Medicine, Iowa City, IA, USA
Veterans Affair Medical Center, Iowa City, IA, USA
Eshani Sheth
Mount Sinai Medical Center, Miami Beach, FL, USA
Yoko Shigemoto
Department of Radiology, National Center of Neurology and Psychiatry, Kodaira, Japan
Eku Shimosegawa
Department of Molecular Imaging in Medicine, Osaka University Graduate School of Medicine, Suita, Japan
Martina Sollini
Department of Biomedical Sciences, Humanitas University, Milan, Italy
IRCCS Humanitas Research Hospital, Milan, Italy
Stefania Antonia Sperti
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Daniel Stahl
Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Atsuhiko Sugiyama
Department of Neurology, Graduate School of Medicine, Chiba University, Chiba, Japan
Fumio Suzuki
Department of Radiology, National Center of Neurology and Psychiatry, Kodaira, Japan
Girolamo Tartaglione
Nuclear Medicine, Cristo Re Hospital, Rome, Italy
List of Contributors
Tommaso Tartaglione Radiology, IDI-IRCCS, Rome, Italy
Rosanna Tavolaro
Department of Nuclear Medicine and Theranostics, “Mariano Santo” Hospital, Cosenza, Italy
Salar Tofighi
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Laura Vendramin
Nuclear Medicine Unit, Department of Medicine, University of Padua, Padua, Italy
Giuseppe Visconti
Plastic Surgery, Lymphedema Center, A. Gemelli Hospital, Sacro Cuore Catholic University, Rome, Italy
Bilge Volkan-Salanci
Department of Nuclear Medicine, Hacettepe University Faculty of Medicine, Ankara, Turkey
Daria Volpe
Department of Biomedical Sciences, Humanitas University, Milan, Italy
IRCCS Humanitas Research Hospital, Milan, Italy
Jan Wartenberg
Department of Nuclear Medicine, Inselspital, University Hospital Bern, Switzerland
Preface
Medical imaging has come a long way since the discovery of X-rays by Wilhelm Rontgen, for which he received the Nobel Prize in 1901. For over a century, medical imaging has evolved remarkably with discoveries and the development of innovative technologies which in combination with major strides in understanding the biology of health and disease have contributed significantly to the concept of precision health and precision medicine. These milestones include, but are not limited to, the discovery of radioactivity and positron and technical developments of the radiotracer concept, cyclotron, computed tomography (CT), ultrasonography (US), magnetic resonance imaging (MRI), single photon computed tomography (SPECT), and positron emission tomography (PET). Advances in computer technology have also provided opportunities for sophisticated incorporation of radiomics, artificial intelligence, and deep learning (AI/DL) algorithms in medical imaging. Over the past decade, it has become clear that hybrid imaging (e.g. PET/CT, PET/MRI, SPECT/CT) provides a broader view of disease that was unavailable previously. For example, it is now recognized that a small lymph node may harbor a tumor while a large lymph node may be benign. Another example is visualization of tumor infiltration in marrow space without concordant structural abnormalities. Such comprehensive information provides opportunities for enhanced imaging assessment of the patient, which has been demonstrated to impact clinical management and improve patient outcome.
The editors of this book have assembled an international team of expert imaging specialists to compile comprehensive coverage of correlative imaging in the domains of
diagnostic radiology and nuclear medicine, addressing all major organ systems and major diseases (cardiovascular, neurologic, oncologic, infection, and inflammation, in both adults and children). In all chapters, there is emphasis on correlative imaging and how one imaging modality complements another in a synergistic way. As appropriate, the reader is introduced to the relevant anatomy and physiology. Modern topics of radiomics, AI/DL, and theranostics are discussed. This image-rich book will appeal to physicians, allied healthcare professionals, and trainees (medical students, residents, fellows). The editors regret any potential errors and omissions and commit to remedy any shortcomings in any future editions.
We dedicate this book to the memory of Sanjiv “Sam” Gambhir, MD, PhD, Chair of Radiology at Stanford University. Sam was our mentor, friend, and colleague. He was larger than life with deep intellect, contagious generosity, and remarkable humility. The entire scientific community and indeed humanity itself lost a glorious soul from his untimely passing in July 2020.
Ali Gholamrezanezhad Clinical Radiology, University of Southern California, Los Angeles, CA, USA
Majid Assadi
Nuclear Medicine, Bushehr University of Medical Sciences, Bushehr, Iran
Hossein Jadvar Radiology, Urology, and Biomedical Engineering, University of Southern California, Los Angeles, CA, USA
Introduction to Correlative Imaging
What Radiologists and Nuclear Medicine Physicians Should Know on Hybrid Imaging
Prathamesh V. Joshi1,2, Alok Pawaskar 2,3, and Sandip Basu2,4
1 Department of Nuclear Medicine & PET-CT, Kamalnayan Bajaj Hospital, Aurangabad, Maharashtra, India
2 Radiation Medicine Centre, Bhabha Atomic Research Centre, Tata Memorial Centre Annexe, Parel, Mumbai, Maharashtra, India
3 Department of Nuclear Medicine & PET-CT, Shri Siddhivinayak Ganapati Cancer Hospital, Miraj, Maharashtra, India
4 Homi Bhabha National Institute, Mumbai, Maharashtra, India
Introduction
Correlation is defined as a connection or relationship between two or more things that are not caused by chance [1]. Medical research is naturally based on finding the relationship between the known and the unknown [2]. Correlation has been an integral part of medicine. A clinician correlates signs and symptoms with the results of medical imaging, pathology or laboratory investigations. A nuclear medicine physician or radiologist correlates findings of medical imaging with another imaging modality or laboratory investigation such as tumor marker levels, hormone levels etc. Correlative imaging comprises combining complimentary information provided by different imaging techniques for better interpretation of pathology.
In this chapter, our aim is to familiarize readers with the basics of correlative imaging, the strengths and shortcomings of various imaging modalities, and how the correlation among them leads to better understanding of pathologies. The main emphasis of this chapter will be on “fusion imaging”, which has proved to be the best available form of correlative imaging at present.
Correlative Imaging
Medical imaging has come a long way since Roentgen first discovered the X-ray in 1895 [3]. Today X-ray, fluoroscopy, computed tomography (CT), ultrasonograpy, single-photon emission tomography (SPECT), positron emission tomography (PET), magnetic resonance imaging (MRI), PET- CT, SPECT-CT, and PET-MRI form the gamut of medical
imaging. Table 1.1 provides a brief review of the different tomographic imaging modalities which form the crux of correlative imaging.
Each imaging modality has its own strengths and shortcomings. The utilization of an individual modality depends on multiple factors:
1) Patient-related factors: age of patient, organ of interest, claustrophobia, contrast allergy, pregnancy etc.
2) Modality-related factors: availability, radiation exposure, resolution, need of morphological versus functional information
3) Physician-related factors: expertise of radiologist/ nuclear medicine physician or preference of referring physician
4) Miscellaneous: financial burden of examination, insurance coverage etc.
Depending on these multiple factors, an imaging modality is utilized as the investigation of choice during workup of a particular patient. However, it is not uncommon that imaging findings are nonspecific and rather than leading to a definitive diagnosis they lead to a spectrum of differential diagnoses. Through “fusion imaging” or “hybrid imaging” radiologists/nuclear physicians frequently utilize correlative imaging with the intent to narrow down the differentials and/or pinpoint the diagnosis.
Correlative imaging can be defined as “imaging the same sample (field of view [FOV] or subject) sequentially or simultaneously with different imaging modalities to obtain complimentary/additive information.”
Radiology-Nuclear Medicine Diagnostic Imaging: A Correlative Approach, First Edition. Edited by Ali Gholamrezanezhad, Majid Assadi, and Hossein Jadvar.
2023 John Wiley & Sons Ltd. Published 2023 by John Wiley & Sons Ltd.
Table 1.1 Overview of the salient attributes of important tomographic imaging modalities.
PrincipleThree-dimensional distribution of positron-emitting labeled radiotracers
The tracer/ contrast used
Positron-emitting radio-pharmaceuticals
Computer-generated image of local radioactive tracer distribution in tissues produced through the detection of single-photon emissions from radionuclides introduced into the body in the form of SPECT radiotracers
Gamma-ray-emitting radio-pharmaceuticals
Combined X-ray transmission source and detector system rotating around the subject to generate tomographic images
Iodine-containing contrast medium
Strong magnetic field and radio waves to create detailed images of the organs and tissues within the body
Gadolinium-based contrast agents
Resolution++ + +++ +++
Functional assessment +++ ++ + ++
Radiation exposure ++ + +++ None
Allergy/acute side effects No No Yes Yes
Measurable parameter/ quantification unit
PET tracer uptake/standardized uptake value
Attenuation value/ Hounsfield unit
Apparent diffusion coefficient/mm2/s
CT, computed tomography; MRI, magnetic resonance imaging; PET, positron emission tomography; SPECT, single-photon emission tomography.
Correlative imaging has been in practice in the form of comparative imaging for many years, a typical example of this being the “hot spot” observed in bone scans interpreted as metastatic or degenerative based on comparing it with MRI or CT of the same bone. However, now fusion imaging techniques such as SPECT-CT, PET-CT, and PET-MRI have emerged as most widely accepted form of correlative imaging. Conventionally, SPECT and PET had been domains of nuclear physicians while CT and MR had been the radiologist’s forte. With the advent and rapid success of fusion imaging there is a need for combined knowledge of both nuclear medicine and radiology for accurate interpretation of fusion imaging findings. In the next section, we aim to familiarize nuclear physicians and radiologists with the basic principles of tomographic techniques utilized in correlative/fusion imaging.
Positron Emission Tomography–Computed Tomography
PET-CT: What a Radiologist Should Know about PET
Basics of PET-CT
Positron Emission Tomography
PET is a tomographic technique that measures the threedimensional distribution of positron-emitter labeled radiotracers. PET allows noninvasive quantitative assessment of biochemical and functional processes. The most commonly
used tracer at present is the 18F-labeled glucose analogue fluorodeoxyglucose (FDG), and it is the workhorse of PET- CT imaging at present.
Though most commonly utilized in oncological imaging, FDG-PET has many other nononcological applications now: dementia, myocardial viability, and infection imaging to name a few. Hence FDG is utilized here as example to demonstrate PET tracer characteristics to radiologists.
● Principle of FDG PET imaging
Enhanced glucose metabolism of cancer cells (primarily dependent on anaerobic glycolysis or the Warburg effect) forms the fundamental basis of FDG PET/CT imaging of malignancies. The increased glucose utilization by the malignant cells is characterized by high expression of glucose transporters (GLUTs, namely GLUT1 and GLUT3) and upregulation of hexokinase activity [4].
Glucose is taken up by tumor cells by facilitated transport (via GLUT) and then undergoes glycolysis with the formation of pyruvate under aerobic conditions. However, under hypoxic conditions (such as in a necrotic tumor), glucose is metabolized under anaerobic conditions with resultant increased tumor lactate levels. FDG is a radiopharmaceutical (RP) analog of glucose that is taken up by metabolically active tumor cells using facilitated transport similar to that used by glucose (Figure 1.1). Despite the chemical differences, cellular uptake of FDG is similar to that for glucose. FDG passes the cellular membrane through facilitated transport mediated by the GLUTs, of which more than 14
F-18 FLUORODEOXYGLUCOSE (FDG)
Glusose-6phosphatase hexokinase
GLUCOSE-6-PO4
Glusose-6phosphatase
different isoforms have been identified in humans, differing in their tissue distribution and affinity for glucose. GLUT1 is the most common glucose transporter in humans and is, together with GLUT3, overexpressed in many tumors [5–7].
Like glucose, it undergoes phosphorylation to form FDG-6phosphate; however, unlike glucose, it does not undergo further metabolism. At the same time, expression of the enzyme glucose-6-phosphatase is usually significantly decreased in the malignant cells, and FDG-6-phosphate thus undergoes only minimal dephosphorylation, hence becoming “metabolically trapped” in cancer cells [8]. The distribution of FDG in normal organs and pathological lesions is detected by PET scanners.
● Preparation for FDG-PET and scan acquisition
Patients are advised to fast and not consume beverages, except for water, for at least 4–6hours before the administration of FDG to decrease physiologic glucose levels and to reduce serum insulin levels to near basal levels. Oral hydration with water is encouraged. Intravenous fluids containing dextrose or parenteral feedings also should be withheld for 4–6hours [9]. FDG is injected intravenously and the PET scan is typically acquired 50–90minutes after FDG injection.
● Normal biodistribution and physiological variants
Physiological FDG uptake is seen in the brain, myocardium, liver, spleen, stomach, intestines, kidneys and
FDG-6-PO4
urine, lymphoid tissue, bone marrow, salivary glands, and testes (Figure 1.2). Breast, uterus, ovary, and thymus can show variable FDG uptake.
Causes of Physiological FDG Uptake and Normal Variants Mimicking Pathology
As increased FDG uptake is not limited to malignant tissues alone, for the appropriate interpretation of FDG PET- CT imaging the interpreting radiologist needs to be aware of the physiological causes of FDG uptake as well as commonly encountered physiological variants [10–15].
Table 1.2 summarizes and enumerates the different physiological causes and sites of FDG uptake that can mimic disease and the suggested interventions to reduce them.
● Quantification of FDG uptake and SUV
While interpreting a PET-CT scan, it is the relative tissue uptake of FDG (or any other PET RP) that is of interest to the reporting physician. Visual analysis is sufficient in most cases, but the standardized uptake value (SUV) is a commonly used measure of FDG uptake and it is routinely mentioned in PET-CT reports. The basic expression for SUV is [16]

Figure 1.2 A typical example of the physiological distribution of FDG uptake in a conventional vertex-to-mid thigh whole-body PET study. (a) Maximum intensity projection (MIP) image of a PET scan. (b) Three columns depicting (left to right) trans-axial PET only, trans-axial CT only, and trans-axial fused PET-CT images of physiological distribution.
where r is the radioactivity activity concentration (kBq/ml) measured by the PET scanner within a region of interest (ROI), a is the decay-corrected amount of injected radiolabeled FDG (kBq), and w is the weight of the patient (g), which is used as a surrogate for distribution volume of tracer. If all the injected FDG is retained and uniformly distributed throughout the body, the SUV everywhere will be 1g/ml regardless of the amount of FDG injected or patient size [17, 18]. Commonly SUVmax of lesions (maximum SUV) is provided in reports, which is the SUV of most avid voxel in ROI.
The reproducibility of SUV measurements depends on the reproducibility of clinical protocols, for example dose infiltration, time of imaging after 18F-FDG administration, type of reconstruction algorithms, type of attenuation maps, size of the ROI, and changes in uptake by organs other than the tumor [9]. SUV or SUVmax values are often
utilized as a marker of change in the metabolic activity of pathology and hence it is important to reproduce the scan conditions during the follow-up PET-CT scan performed for response evaluation.
What Nuclear Medicine Physicians Need to Know about CT
PET alone is limited by poor anatomic detail, and correlation with some other form of imaging, such as CT, is desirable for differentiating normal from abnormal radiotracer uptake [8]. Hence PET-CT morpho-metabolic imaging emerged as an ideal single investigation for oncology practice. However, this also mandates the nuclear physician to have adequate knowledge of the CT component of imaging as well as the various interventions employed in CT acquisition.
Table 1.2 Characteristics and causes of physiological uptake of FDG and methods to circumvent them.
Causes/sites of FDG uptakePhysiology behind FDG uptake PET-CT appearance
Brown adipose tissue (BAT)
Nonshivering thermogenesis requires glucose for glycolysis as a source of adenosine triphosphate, which in turn is utilized in fatty acid oxidation
BAT is innervated by the sympathetic nervous system and expresses beta-adrenergic receptors, which are stimulated by cold
Vocal cordsPhonation-related laryngeal muscle contraction
MyocardiumGlucose as substrate for energy (GLUT1 and insulin-sensitive GLUT4)
FDG uptake in fat density (−150 to −50HU) in neck, shoulder, and paraspinal regions (Figure 1.3)
Less common in perirenal, perigastric regions
FDG uptake in BAT is more common in younger patients, females>males
Symmetrically increased FDG uptake in both vocal cords (Figure 1.4)
Variable, focal or diffuse without corresponding morphologic abnormality on CT
Interventions to reduce uptake
Making patients wear warm clothing and providing a blanket in the waiting suite to avoid cold-induced BAT activation.
Premedication with beta-blockers or diazepam
If the region of interest is the larynx, the patient should be instructed to avoid talking after FDG injection
Fasting before FDG PET- CT (4–12hours)
High-fat, low-carbohydrate diet before scan
Premedication with unfractionated heparin before FDG injection
Thymus Physiological uptake in pediatric patients (especially in postchemotherapy setting, known as “thymic rebound”)
Lactating breasts Due to secretory hyperplasia and the increased expression of GLUT-1
Urinary systemFDG excretion in urine
Inverted V-shaped/butterfly pattern of anterior mediastinal uptake on the transaxial view and absence of lesion on corresponding CT (Figure 1.5)
Bilateral breast reveal diffuse FDG uptake, but if infant is suckling unilateral breast only that side can show diffuse FDG uptake (Figure 1.6)
Usually does not affect scan interpretation Focal retention in kidneys/ureter/ urinary bladder can mimic pathology
Ovary FDG uptake in corpus luteal cystOvoid FDG uptake with smooth margins or a rim of FDG uptake with a photopenic center (Figure 1.7)
EndometriumFDG in menstrual flow
Colon Related to bowel motility The uptake in cecum and right colon could be result of higher lymphocytes in these regions
FDG uptake in endometrium in a diffuse uniform pattern (Figure 1.8)
Typically heterogeneous and can vary in distribution from mild focal to diffuse uptake
Often, there is higher uptake within the cecum and right colon
The uptake has a diffuse characteristic pattern: no specific intervention
The uptake has a diffuse characteristic pattern: no specific intervention
Dual point/delayed postvoid imaging with or without diuretic intervention
Correlation with menstrual history
If being evaluated for gynecological pathology, PET- CT scan should be scheduled in the postmenstrual phase
Uptake pattern: no interventions (Continued)
Table 1.2 (Continued)
Causes/sites of FDG uptakePhysiology behind FDG uptake PET-CT appearance
Spinal cordInadequate clearance of FDG from the artery of Adamkiewicz, which originates on the left side of the aorta between the T9 and T11 vertebral segments
Increased cross-sectional area of the spinal cord
Skeletal muscles
Exercise induces glucose uptake in skeletal muscles
Labored breathing can increase FDG uptake in intercostal muscles and diaphragm
In postmeal state, insulin increases GLUT (GLUT-4) mediated skeletal muscle glucose uptake
The physiological FDG uptake is visualized in the cervical spinal cord peaking at C4 level, and in the lower thoracic spinal cord peaking at the T11–T12 segments (Figure 1.9)
If related to exercise, usually symmetrical FDG uptake in muscles with no abnormal enhancement or lesion on CT
If related to meal/insulin diffuse FDG uptake in skeletal muscles (usually also accompanied with cardiac FDG uptake)
If related to labored breathing, intercostal muscles and diaphragm reveal symmetrical increased FDG uptake (Figure 1.10)
Interventions to reduce uptake
Patients should avoid strenuous exercise for 48–72hours before scheduled scan
Fasting status should be confirmed before FDG injection

(a) FDG uptake in brown adipose tissue in bilateral cervical (red arrows), paraspinal, and perirenal regions as shown in MIP image, (b) transaxial PET-only image of the neck region, (c) transaxial CT-only image, and (d) fused PET-CT image.
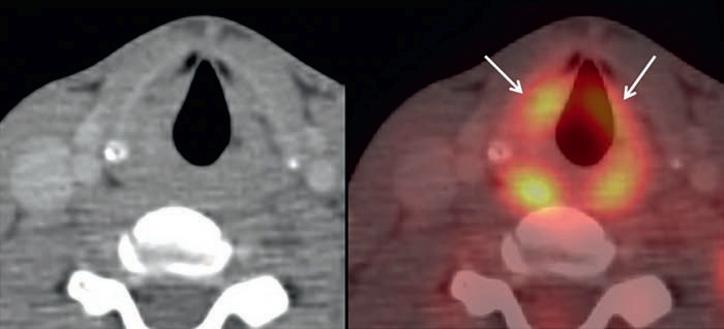
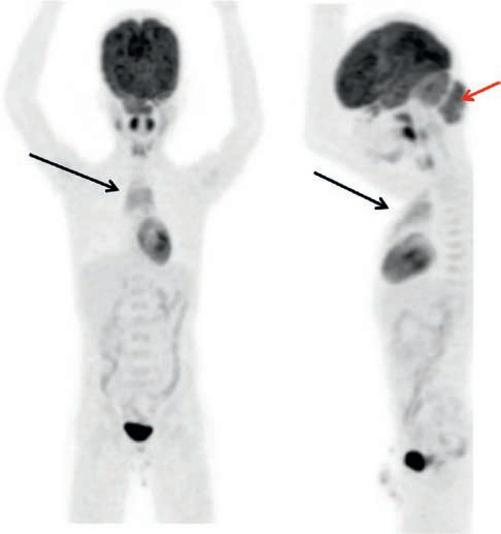
Figure 1.5 (a) MIP image of PET-CT of a 10-year-old boy showing physiological FDG uptake in the thymus (black arrows). (b) Hypermetabolism in the soft tissue neoplasm in the occipital region (red arrow).
Computed Tomography
Although the potential applications of X-rays in medical imaging diagnosis were clear from the beginning, the implementation of the first X-ray CT system was made in 1972 by Godfrey Newbold Hounsfield (Nobel prize winner in 1979 for Physiology and Medicine), who constructed the prototype of the first medical CT scanner and is considered the father of CT. After this, CT was immediately welcomed by the medical community and has often been referred to
as the most important invention in radiological diagnosis since the discovery of X-rays [19, 20].
Principle of CT
The CT scanner creates cross-sectional images by projecting a beam of X-rays through one plane of an object (patient) from defined angle positions performing one revolution. These X-rays are generated by a rotating X-ray tube (Figure 1.11). As the X-rays pass through the patient‚ some of them are absorbed, while some are scattered and others are transmitted. The process of X-ray attenuation refers to the intensity reduction involving those X-rays which are scattered or absorbed. X-rays which are attenuated due to the interactions with the object do not reach the X-ray detector. Photons transmitted through the object at each angle are collected on the detector and visualized by computer, creating a complete reconstruction of the patient. The three-dimensional (3D) gray value data structure gained in this way represents the electron density distribution in the area of interest [19].
The ability of matter to attenuate X-rays is measured in Hounsfield units (HU). By definition, water is assigned a density value of 0HU and air a value of −1000HU. Attenuation values for most soft tissues fall within 30–100HU. Notable exceptions are lungs, with attenuation values approaching −1000HU (due to high air content), and mineralized tissues such as bone, with attenuation values of approximately 1000HU [21].
Intravenous and Oral Contrast in CT Scanning
Intravenous Contrast
Differences in the CT attenuation of healthy tissue and pathology can improve the quality of the images
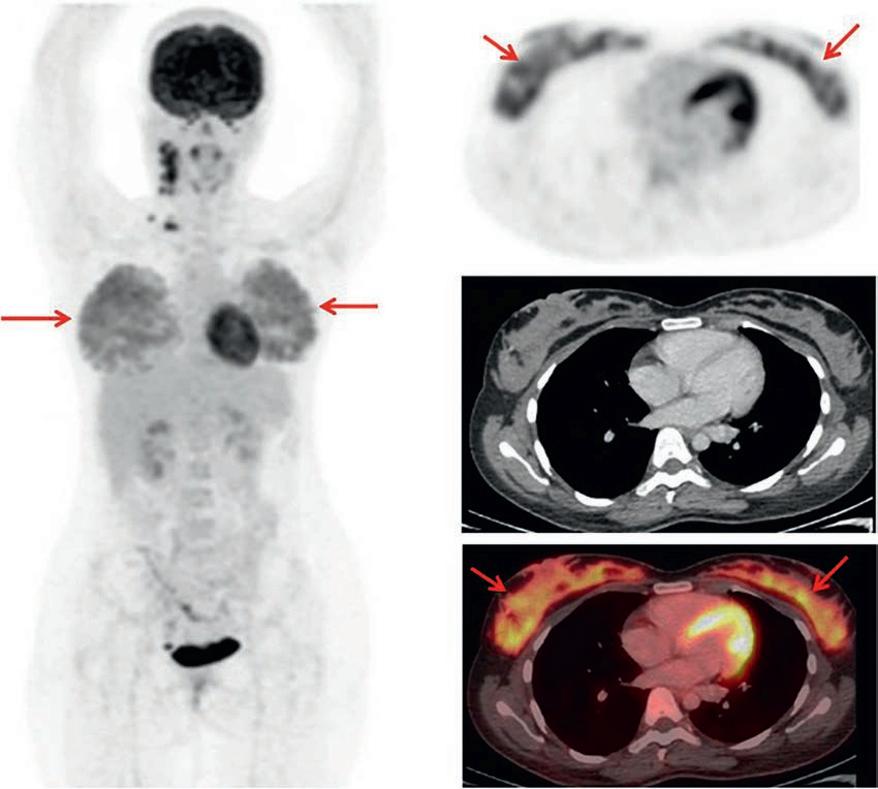
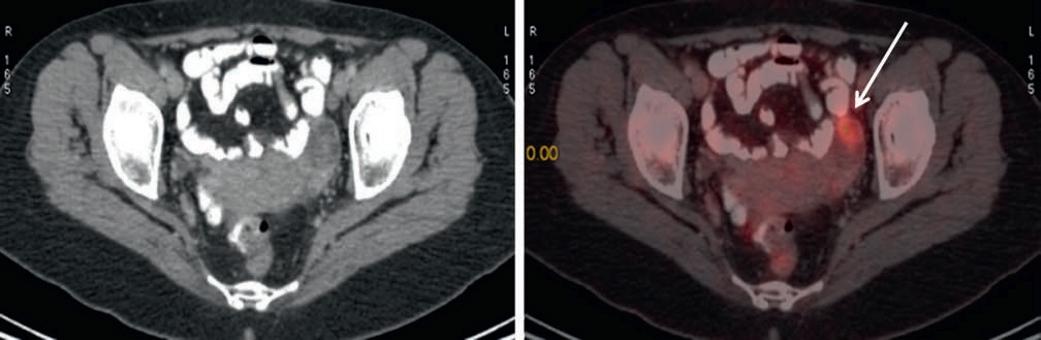
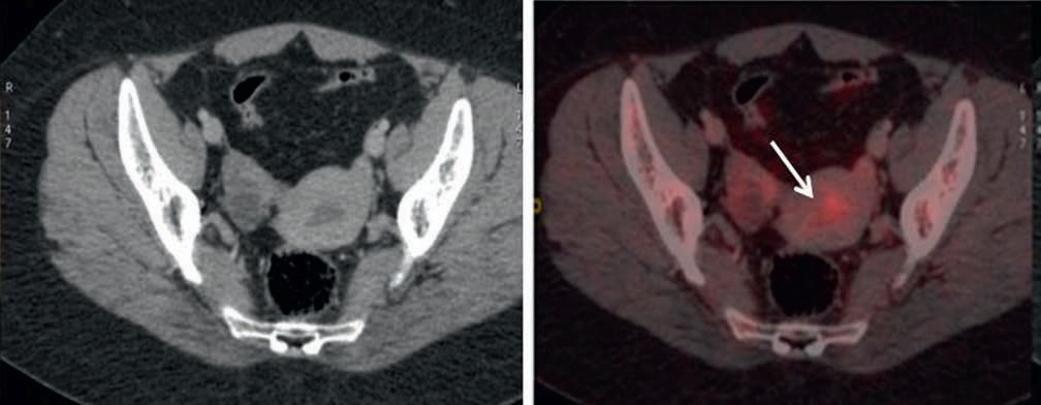
Figure 1.8 FDG PET-CT of a 27-year-old female. (a) Transaxial CT of pelvic region and (b) fused PET-CT image of pelvic region revealing FDG uptake in fluid in the endometrial cavity (arrow) corresponding to menstruation.
Figure 1.10 (a) In a carcinoma larynx patient, the MIP image of FDG PET-CT reveals a hypermetabolic lesion in the neck corresponding to the site of primary malignancy (black arrow). (b) Fused PET-CT image shows increased FDG uptake in the intercostal muscles and diaphragmatic crura (white arrows). (c) Transaxial CT of the same region. The augmented FDG uptake in these muscles of respiration was the result of labored breathing due to narrowing of the airway caused by the laryngeal malignancy.

(i.e. greater signal-to-noise and contrast to noise ratios) and hence facilitate detection of abnormality. Hence, contrast imaging agents are often used for better visualization of the tissue of interest by CT [21, 22].
Today, a wide range of ionic and nonionic contrast agents is available and effective diagnostic dose of a contrast agent
for CT imaging is in the molar concentration range. Since use of intravenous contrast is known to be associated with adverse effects in susceptible population and allergies, caution needs to be exercised during their use. When diagnostic contrast-enhanced CT with intravenous contrast media is to be performed (after the PET/CT examination), indications, contraindications, and restrictions have to be assessed by a qualified physician/radiologist. Medication that interacts with intravenous contrast (e.g. metformin for the treatment of diabetes) and relevant medical history, especially compromised renal function, have to be taken into consideration [23].
Gastrointestinal Contrast Agent
Depending on the ROI, gastrointestinal luminal contrast agent may be administered to improve the visualization of the gastrointestinal tract in CT (unless it is not necessary for the clinical indication or it is medically contraindicated). This is more commonly done via oral administration and less commonly by the rectal enema route for evaluation of colonic pathologies.
It should be noted that the contrast agents alter the attenuation caused by tissues and hence result in overestimation of SUV values used in PET quantification (more so with IV contrast as compared to gastrointestinal) [24].
