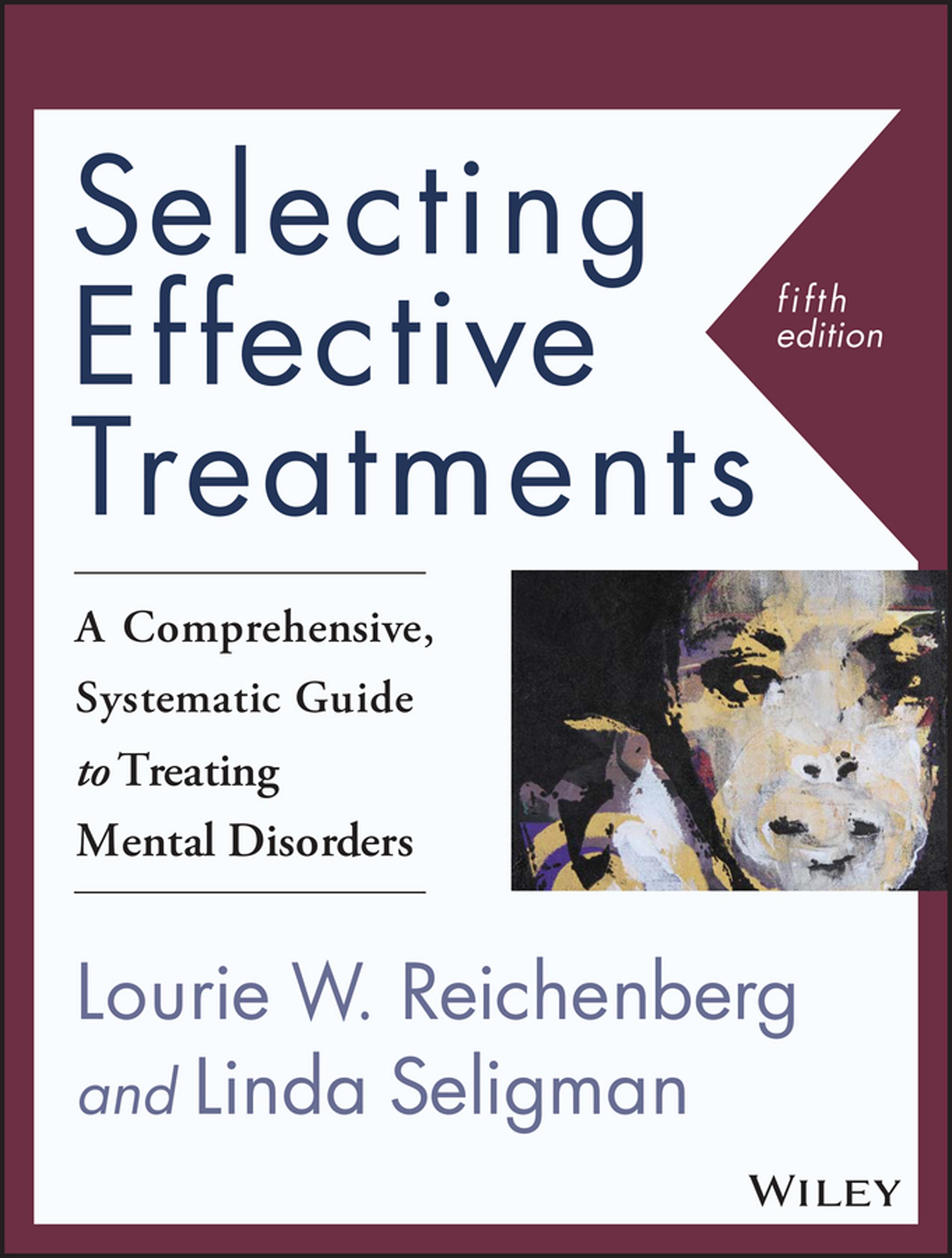
1 IntroductiontoEffectiveTreatment Planning
WHYISDIAGNOSIS ANDASSESSMENTIMPORTANT?
Ihaveheardstudents,colleagues,interns,and licensedprofessionalsalikereacttothediagnosis ofmentaldisordersasaformof“labeling” clients,andinsistthat“Diagnosisisonlyforthe insurancecompanies.”Forsomereason,these commentsseemtohaveincreasedsincethe
CaseStudy1.1
publicationof DSM-5, perhapsasresistanceto oravoidanceoflearningaboutnewandsometimesnuanced,diagnosticchanges.Diagnosis cancertainlybeachallenge,butwithoutan accuratediagnosis,howcouldwepossiblyknow whattreatmentstorecommend?
Considerforamomentthefollowing scenarios:
JackA.,a64-year-oldman,beginscouplescounselingwithhiswifebecausehehasbecomeirritableand difficulttobearound.After35yearsofmarriagehehasbeguntoshoutathiswifeandbecomesparticularly hostileattheendoftheday.Sheisconsideringleavinghim.Theyattendweeklycouplescounselingbut ratherthangettingbetter,thesituationseemstobegettingworse.
CaseStudy1.2
Jillianisa14-year-oldgirlwhoisbeingtreatedbyapsychiatristwithSSRIsforhersymptomsofOCD.Sheis fearfulofeatingfoodthathasbeentouchedorpreparedbyothers,andnowweighslessthan100pounds. Thepsychiatristrefersthegirlforindividualtherapy,buthernewcounselordecidedshewouldfitperfectly intoaweeklysupportgroupsherunsforadolescentgirlswithanorexia.Insteadofgettingbetter,however, Jillianlostanother5poundsinthefirstmonth.
CaseStudy1.3
A37-year-oldmarriedmotherofthreeactiveboyshasbeendiagnosedwithfibromyalgiaandrheumatoid arthritis.Sheisexhaustedallthetime,inpain,andrecentlyresignedfromherjobsoshecoulddevoteallof hertimetotakingcareofherselfandherfamily.Attherecommendationofherdoctor,shebeginstoattend weeklytherapysessions.UsingtheGestaltempty-chairtechnique,hertherapistencourageshertogiveher illnessanameandexpressherangertothechair.
Inaccurate(orno)diagnosis,inappropriate treatment,andpoorclinicalunderstandingon thepartofthetherapistcontributedtothesituationsjustdescribed.
Monthslater,thefirstmanwenttothe doctorforanannualphysicalexamination.His wifementionedhisincreasingirritabilitytothe doctor,whorecognizedtheend-of-dayirritabilityas“sundowner’s,”apotentialsymptom ofAlzheimer’sdisease.Thepatientwasreferred toaneurologistwherehereceivedanaccurate diagnosis.
TheyounggirlwithOCDwasreferred byherpsychiatristforindividualcounseling, whichcouldhavebeenanappropriatecompaniontherapytomedicationmanagement,if shehadreceivedindividualsessionsofCBTto helpreduceherobsessionsandcompulsions. Unfortunately,puttingherinagroupwith othergirlswithanorexiaprovidedheranopportunitytolearnnewobsessiveandcompulsive eatingbehaviorsthatshehadneverthought ofbefore.Italsobroughtouthercompetitive nature.Withinamonth,herweightbecame dangerouslylowandshewashospitalized.
Theyoungmotherhadapainfulmedical disorderthatwasexacerbatedbystress.Shewas eventuallyreferredtoamindfulness-basedstress reductiongroupwhereshelearnedmindfulness meditation,acceptance,andrelaxationtechniques.Sheisnowabletomanageherpain withoutmedicationandhaslearnedhowto treatherselfwithcompassion.
Asthesestoriesillustrate,theprimarygoalof diagnosisandtreatmentplanningistobeableto makesoundtherapeuticdecisionsthatwillhelp clientsfeelbetteraboutthemselvesandtheir lives,returntobetterfunctioning,andachieve theirgoals.Justlikeothermedicalandmentalhealthprofessionals,doctors,psychiatrists, psychologists,counselors,socialworkers,and addictionsspecialistsmustfirstdonoharm.
Butinordertofollowthatedict,wemust beknowledgeableaboutwhathelpsandwhat hasthepotentialforcausingourclientstoget worse.
Forsomewell-researcheddisorders,suchas generalizedanxietydisorder,majordepressive disorder,andsomeoftheeatingdisorders,researchhasfoundspecificevidence-basedtreatmentsthataremoreeffectivethanplacebo conditionsornotreatmentatall.Whenthese interventionsareusedforspecificdisordersthey resultinimprovementoverrelativelyshortperiodsoftime,andtheimprovementsareoftenofa dose-by-dosenature.Moreimportantly,treatmentgainsaremaintainedaftercounselinghas ended.
Butmanytimes,littleornoresearchisavailableonadisorder,ordespiteawealthofresearch, notonespecifictreatmentmodalitystands outasthemosteffective.Inothercases,aswith conductdisorder,bipolardisorder,andborderlinepersonalitydisorder,treatmentwilldepend onthestageofthedisorder,themosttroublesomesymptomsatthattime,andalong-term approach.
Manyofthediagnosesin DSM-5 donot haveevidence-basedtreatments.Somearetoo newtohaveanadequateresearchbase,and somedisordersaretooraretohavegarnered enoughinterestandfundingforresearch.In thosesituations,casestudiescanoftenbefound intheliteraturethatcanbeculledfrom,and approachesthatprovidesymptomreliefcanbe recommended.
Inthesecasesinparticular,ithelpsto rememberthatpsychotherapy is effective.So effectivethatnearly40yearsagoSmith,Glass,& Miller(1980)conductedameta-analyticreview ontheeffectivenessofpsychotherapy.They concluded,“Theaveragepersonwhoreceived therapyisbetteroffattheendofitthan80%of thosewhodonot”(p.87).
ANINTEGRATEDMODEL FORTREATMENTPLANNING
Treatmentplanninggenerallymovesfrom recognitionofthesymptomsofthedisorderinto considerationoftheclient’scharacteristicsand ontothetreatmentapproach.Thatsequence willbefollowedthroughoutmostofthisbook withthehelpofanintegratedtreatmentmodel calledtheClientMap.
Alltheelementsnecessaryforeffective treatmentplanning—diagnosis,objectivesof treatment,andtypesofinterventions—willbe discussedhereintermsoftheDOACLIENT MAPmneumonic.Readerswhoarefamiliar withtheClientMapmethodofdiagnosisand assessmentalreadyknowhowthissimpleacronymhelpstomaketheprocessmorethorough andeffectivebycoveringallthemajorelements ofthetreatmentplanningprocess.Forthose learningthesystemforthefirsttime,eachof the12lettersintheDOACLIENTMAP mneumonichelpstofacilitaterecallforeach ofthe12partsoftheassessmentandtreatment planningprocess:
◾ Diagnosis
◾ Objectivesoftreatment
◾ Assessment—toolstohelpclarifyassessmentmayincludestructuredclinical interviews,inventories,scales,neurologicaltests,ormaybeassimpleas symptomchecklistsandself-reports
◾ Cliniciancharacteristics
◾ Locationoftreatment
◾ Interventionstobeused
◾ Emphasisoftreatment—forexample levelofsupportneeded,levelofdirectivenessbythetherapist,whetherfocus iscognitive,behavioral,emotional,ora combinationofthethree
◾ Numbers—whoshouldparticipate intreatment?Isthemosteffective treatmentindividualtherapy?Family therapy?Group?
◾ Timing—frequency,pace,andduration oftreatment
◾ Medicationsneeded,ifany
◾ Adjunctservices—communityservices, supportgroups,alternativetreatments
◾ Prognosis
TheclinicianwhogathersclientinformationforeachoftheitemsintheClientMap willhavecompletedtheassessmentandhavethe informationnecessaryforastructuredtreatment planthatinformshisorherworkwiththat client.Theacronymisusedthroughoutthis booktoillustratesamplecasestudiesrelevantto thediagnosesineachchapter.
Theformatpresentedherefordiagnosis andtreatmenthasbeenusedsuccessfullyby students,interns,therapistsandothermental healthprofessionalsforatleasttwodecades.Itis comprehensive,providesasolidfoundationon whichevidence-basedpracticecanbebuilt,and haswithstoodthetestoftime.Now,withthe eliminationofthemulti-axialsystemin DSM-5, thesimpleClientMapacronymprovidesstudentsandexperiencedtherapistsalikewithan easy-to-usediagnosticframeworkfortheirwork withclients,iftheychoosetouseit.Let’sget started.
DIAGNOSIS
(DOACLIENTMAP)
Effectivetreatmentplanningbeginswiththe conceptualizationofadiagnosis.Severaldifferentclassificationsystemsareavailablethatreflect ourcurrentlevelofknowledgeandtheresearch
available.Althoughthebestthatwehave availableatthistime,theseclassificationsystems mustbeconsideredtobefluiddocuments thatevolvewithnewscientificknowledge. Theymustbeupdatedandrevisedperiodicallytoremainrelevantwithcurrentmedical knowledgeandchangingconceptsofillness (Moriyama,Loy,&Robb-Smith,2011).
The DiagnosticandStatisticalManualofMentalDisorders,5thedition(DSM-5;American PsychiatricAssociation[APA],2013)isthe classificationsystemusedmostfrequentlyinthe UnitedStates.
The InternationalClassificationofDiseasesand RelatedHealthProblems(ICD) wasdevelopedby theWorldHealthOrganization(WHO)and isusedby117countriesaroundtheworldto reportnationalmorbidityandmortalitystatistics. Itisupdatedperiodicallyandiscurrentlyinits tenthversion,althoughan11theditionisbeing developed.Asofthiswriting,theUnitedStates isusing ICD-10-CM (ClinicalModification) asthebasisformedicalcodingandreporting. IntheUnitedStates,theNationalCenterfor HealthStatisticsoverseesthisprocess.Asof October,1,2015,allU.S.healthcareproviders coveredundertheHealthInsurancePortability andAccountabilityAct(HIPAA)wererequired tousethe ICD-10-CM diagnosticcodesfor medicalandmentalhealthprocedures.Bothsets ofcodes(for ICD9 and ICD10)arecreated bytheWorldHealthOrganization.Thecodes areavailableforusefreeofchargefromthe WHOwebsite(www.who.int/classifications/ icd/en)andarealsoprintedin DSM-5 andin DSM-5Essentials:TheSavvyClinician’sGuideto theChangesinCriteria (Reichenberg,2014).
Boththe DSM andthe ICD areupdated periodicallyinkeepingwiththerealityofnew research,newstatisticsonprevalencerates,and newinsightsintotheetiologyandnosologyof mentaldisorders.Bothclassificationsystemsare
primarilydiagnostic,anddonotventureintothe areaoftreatmentinterventions.
Also,bytheirverynature,bothsystemsare imprecise.Ratherthanbeingthefinalwordon diagnosis,itismorehelpfultoconsider DSM-5 and ICD-10 tobethebestinformationthatwe haveatthecurrenttime,withtheunderstanding thatclassificationswillchangeasourknowledge basechanges.Mentalhealthprofessionalsmust stayinformedandkeeppacewiththechanges inourprofession.
Other,largerphilosophicalquestionsabout thejudgmentsthatmustbemadetodetermine theboundariesofnormalcyversusadisorder; thestandardsagreedtoforguidingresearch;even questionsrelatedtocausation,culturaldifferences,andwhatconstitutesamedicalillness versusamentaldisorderareallfascinatingtopics fordiscussion,buttheyhaveallbeencovered elsewhereandarebeyondthescopeofthisbook. Certainlycareshouldbetakentodistinguish betweenatruementaldisorderandanormal reactiontostressfullifeevents.Morethan70%of disordersin DSM-IV includedclinicallysignificantdistressorimpairmentasarequiredcriterion fordiagnosis. DSM-5 providesanewdefinition ofamentaldisorderthatisslightlydifferent:
Amentaldisorderisasyndrome characterizedbyclinicallysignificantdisturbanceinanindividual’s cognition,emotionregulation,or behaviorthatreflectsadysfunction inthepsychological,biological,or developmentalprocessesunderlying mentalfunctioning.Mentaldisorders areusuallyassociatedwithsignificant distressordisabilityinsocial,occupational,orotherimportantactivities. (APA,2013,p.20)
Untilwereachapointwhenallmental disorderscanbemeasuredandtheunderlying
causativefactorsidentified,clinicaljudgment willstillbenecessarytodeterminewhena behaviororsequelaeofbehaviorshasbecome dysfunctionalorisassociatedwithsignificant distress.Untilthen, DSM-5 and ICD reflectthe bestcurrentlyavailableinformationwehavefor thediagnosisofmentaldisorders.
Anotherdiagnosticchallengeisthepresence ofco-occurringorcomorbiddisorders.The DSM-5 allowsformultiplediagnosestobe givenatthesametime,aslongasthediagnostic criteriaaremet.Greatercomorbiditymeans diagnosiswillbemoredifficult,andtreatment willbemorecomplicatedasissuesofpersonality, behavior,substanceuse,andotherinfluences willneedtobefactoredintothetreatmentplan.
Provisionaldiagnosesmayalsobegiven,if thereisastrongindicationthatthefullcriteria willultimatelybemet.Theprovisionalspecifier isaddedfollowingthediagnosisifnotenough informationisavailable.Aprovisionaldiagnosis canalsobegivenifthedurationcriterionfora disorderhasnotbeenmet.
Alsoimportanttodiagnosisisanunderstandingoftheclient’sdevelopmentalstage, andprocessessuchasattachment,socialization,genderidentity,andmoralandemotional development.Understandingtheclient’sstage ofdevelopmentisparticularlyimportantwhen treatingchildren,adolescents,families,andolder adults(Levant,2005).Ofequalimportanceis thedevelopmentalbackgroundofadisorder, whensymptomsfirstbegan,andhowitmay haveimpactedthechilddevelopmentally.Some peoplewithlongstandingdisordersmayhave failedtoreachimportantdevelopmentalmilestones,especiallyintheareasofself-direction andsocialization.
DSM-5 incorporatesyearsofresearchduringwhichthousandsofexpertsparticipatedin morethan160taskforcesandworkgroupsover a12-yearperiodtoconductresearchfieldtrials ofdiagnosticcriteriaformentaldisorders.Atthe
endoftheprocess,theBoardofTrusteesofthe AmericanPsychiatricAssociationapprovedthe finalchangesthatnowconstitute DSM-5. AccordingtotheAPA,allthechangeswere intendedtomoreaccuratelyandclearlydefine thecriteriaformentaldisorderstoensure diagnosticaccuracyandconsistencyfromone cliniciantoanother(APA,2013).
Followingaresomeofthemostsignificant changesin DSM-5. Readerscanfindacomplete listofchangesmadefrom DSM-IV to DSM-5 in DSM-5Essentials:TheSavvyClinician’sGuideto theChangesinCriteria (Reichenberg,2014).
1.Movementtoanonaxialdiagnostic system(similartoWHO’s International ClassificationofDiseases)whichcombinesalldiagnosestogetherandlistsas manydiagnosesasnecessarytoprovide theclinicalpicture.
2.Betterclarificationofthenototherwise-specified(NOS)diagnostic categoriesfrom DSM-IV. Insteadof thecatchallNOScategory,clinicians maynowidentifypresentationsthat areclinicallysignificantbutdonot meetthefullcriteriaforadisorderand explainwhythecriteriahavenotbeen met.Or,asinemergency-roompresentations,cliniciansmayreportthat insufficientinformationisavailable, andan“unspecified”diagnosiswould begiven.Thesetwooptionsarenow availableforalldisordersin DSM-5.
3.Reclassificationofdisordersintoa dimensionalapproachratherthanthe categoricalapproachusedin DSM-IV. Forexample,OCDisanewclassificationandislocatednexttoanxiety disorders. DSM-5 providesdimensionalandcross-cuttingmeasuresto helpclarifydiagnosisandincreasethe clinicalutilityofthemanual.
4.Somecategorieshavetakenona“spectrum”approach(asinschizophrenia spectrumandotherpsychoticdisorders),andmaybeconsideredone disorderwitharangeofpresentations.
5.Theseparationofsomedisorders,such asagoraphobiaandpanic,fromeach other.Toprovidefurtherdiagnostic clarification,panicattackisnowalso consideredtobeaspecifierthatcanbe appliedtootherdisordersaswell.
DSM-5 alsoadoptsadevelopmentaland lifespanapproachandincorporatesdisorders thatusuallyfirstbegininchildhoodintothe chapterswithadultdiagnoses.Forexample, informationonanxietydisordersinchildren andadolescentsisnowincludedwiththeanxietydisordersforadults.Thebookalsobegins withneurodevelopmentaldisorders,whichfrequentlybegininchildhood,andworksthrough disordersastheyoccuracrossthelifespanup totheneurocognitivedisordersthatgenerally occurinolderadults.
Manychangeshavebeenmadeinspecific disordersin DSM-5 asaresultoftheseandother advancesinourknowledgeaboutmentaldisorders.Adimensionalapproachtodiagnosisof substanceuse,forexample,eliminatesthecategoriesofabuseanddependencewhichwereused in DSM-IV, andnowdeterminesdiagnosisbased onseveritylevels.Adjustmentdisorders,some ofthemostfrequentlydiagnoseddisordersin DSM-IV,arenowconsideredtobeasevere reactiontoastressfullifeeventandhavebeen recategorizedasatrauma-orstressor-relateddisorderalongwithPTSDandreactiveattachment disorder.These,andotherchanges,willbe discussedthroughoutthistextaswefollow thenew DSM-5 developmentalandlifespan approach.
Forsimplicity,andeaseofuse, SelectingEffectiveTreatments,5thed.(SET-5)willbeconsistent
withtheformatof DSM-5 andcanbedivided intothreeparts:
SectionI Thissectionprovidesbasicintroductorymaterial,howtousethisbook, andintroducestheClientMapsystem ofdiagnosisandtreatmentplanning.
SectionII Thissectionprovidesthe20classificationsofdisordersinthesameorder as DSM-5.
SectionIII Thissectionincludesanappendix ofmaterialfromthefourtheditionof thistexttohelpclinicianswithsuicide assessment.Extensiveauthorandsubjectindexesarealsoincluded.
OBJECTIVESOFTREATMENT
(DO ACLIENTMAP)
Generally,determinationoftreatment objectivesandgoalsshouldbeacollaborative processbetweenthetherapistandclient.Many variablesmustbetakenintoaccountincludingcostconsiderations,andindividualclient variablessuchasreadinessforchange,client motivation,andexpectationsfortreatment. Otherclientqualitiescanstrengthenorweaken treatmentoutcomesandshouldbetakeninto accountwhendeterminingtreatmentgoalsand objectives,sincetheyarelikelytohaveaneffect ontreatmentoutcome.Theyincludedegreeof participationintreatment,severityofthedisorder,willingnessandabilitytotakeaction, andpersonalitycharacteristicsoftheclient (Muran&Barber,2010;Prochaska,Norcross, &DiClemente,2013).
Clientswithverylowlevelsofreadinessto changeneedtherapistswhocanfocusonconsciousnessraising,dramaticrelief,andenvironmentalevaluation.
Resistancetochangeisnotdirectlyconfrontedbythetherapist;rather,itisreframedas
ambivalenceandthetherapistuseshisorher skillsatcreatingtheRogerianconditionsfor change(empathy,congruence,andunconditionalpositiveregard),settinguptheconditions inwhichtheclientcanexplorebothsidesof thedynamic(Seligman&Reichenberg,2013).
CarlRogersnoted,“significantpositivepersonalitychangedoesnotoccurexceptina relationship”(Rogers,1967,p.73).Supportinga client’sreadinessforchangeisthegoalofmotivationalinterviewing,aperson-centeredapproach originallycreatedbyMillerandRollnick(2013).
Motivationalinterviewinghelpsthetherapisttoestablishtheconditionsinwhich theclientcanchoosetochangeandisoften usedatthebeginningoftreatmentforconditionsthatmaybetreatmentrefractorysuch asduallydiagnoseddisorders,eatingdisorders,substanceuse,andgambling.Therapists whoincorporatemotivationalinterviewing intotheirtreatmentinterventionsaremore likelytoachievesuccesswithambivalent clientsthanthosewhodonot(Stasiewicz, Herrman,Nochajski,&Dermen,2006).
It’sawell-knownfactthatsomepeople improvesimplyasaresultofhavingspecial attentionpaidtothem(Prochaska&Norcross, 2010).Thisso-calledHawthorneeffectcan improveself-esteem,reduceanxiety,andpromoteimprovement.
Theclient’sreadinesstochangeunfolds overfivedistinctstages:(1)precontemplation, (2)contemplation,(3)preparation,(4)action, and(5)maintenance(Prochaska&Norcross, 2010).Eachstagerepresentsaperiodoftime duringwhichcertainattitudes,behaviors,and languageoccur.Aggregatedataacrossstudies andpopulationsfoundthattheclient’sreadiness tochangehasasignificantimpactonwhether theytakeaction,basedonthefollowing:
Precontemplation Peopleinthisstagehaveno plantochangetheirbehaviors,although
theymaythinkaboutitorwishthey could.Tomovebeyondthisstagethey mustrecognizeandadmittheyhavea problem.Coaching,onthepartofthe therapistcanhelp,androughly40%to 45%ofpeoplewillmoveontothenext stage.
Contemplation Duringthisstageofchange, thepersonreadilyadmitstheyhave aproblemandwouldliketochange. Fortunately35%to40%ofthemwill takeactiontowardsignificantbehavioral changes.TherapistswhouseSocratic questioningarelikelytoencourage furtheraction—evenasmallfirststep— towardbehavioralchange.
Preparation Duringthisstage,behaviorand intentionsarealignedand20%ofpeople arepreparedtotakeaction.
Action Duringtheactionstage,people begintomodifytheirbehaviors.This stagemaylastfrom1dayto6months, duringwhichthepersonisacquiring skillsandstrategiestopreventrelapse. Thetherapistsintheactionandmaintenancestagesprovideexpertadvice andsupportwhenneeded(Prochaska etal.,2013).
Maintenance Maintainingbehavioralchange forlongerthan6monthsisthehallmark ofthemaintenancestage.
ThenextstepintheClientMapprocessisan overviewofassessment.
ASSESSMENT
(DO A CLIENTMAP)
Muchhasbeenwritteninthepast20years abouttheimportanceofconductingacomprehensive,measurable,clinicalassessmentasa necessaryfirststepinevidence-basedpractice.
Overtheyears,clinicianshavecometorely lessonprojectivetests(e.g.,TAT,Rohrschach), andbecomeincreasinglyreliantonassessment teststhatarebothpsychometricallysound andclinicallyuseful.Inotherwords,theyrely onteststhatarestandardized,reliable,have concurrentandpredictivevalidity,andare eithernormedorhavespecificcriterion-related cutoffscoresthatmakethemeasiertousein individualsettings(Hunsley,Lee,Wood,& Taylor,2015).Thedevelopmentinrecent yearsofbrief,focusedassessmentinstruments forspecificsymptomsanddiagnoseshasbeen helpful.
Ultimately,thegoalofanassessmentisthe developmentofacomprehensivediagnosisand correspondingtreatmentplanthatisspecific totheclient’sneeds,thatisconsistentwith evidence-basedpractice,andthatwillbeeffectiveinthetreatmentofthatparticulardiagnosis. Forthattooccur,thetherapistmustfirstbegin withathoroughunderstandingoftheperson. Theimportanceoftheabilitytotrulylistento theclientandtobegenuine,supportive,and flexiblecannotbeoverlyemphasized.Many ofthesecliniciantraitshavebeenfoundtobe positivelyassociatedwiththedevelopmentof astrongallianceandsuccessfultreatmentoutcomes.Onestudyfoundthatevenduringthe assessmentprocess,apatient-andtherapist-rated alliancedevelopedandwasstrongerforthose usingacollaborativetherapeuticmodelthan forthosereceivingpsychologicaltestingas usual(Hilsenroth,Peters,&Ackerman,2004).
Therapistsshouldkeepthisinmindduringall stagesoftreatment,butespeciallyduringthe initialassessmentprocess.
Importantaspectsoftheinitialintakeassessmentwiththeclientwillincludedataonthe followingdimensions:
◾ Descriptionofthepresentingproblem
◾ Demographiccharacteristicsandculturalbackgroundoftheclient
◾ Assessmentofmentalstatus
◾ Physicalandmedicalconditionofthe client
◾ Therapist’simpressionofcognitive functioning,behavior,affect,andmood
◾ Intelligenceandexecutivefunctioning (e.g.,goalsetting,planning,organizationalability)
◾ Familybackgroundandsupport
◾ Otherrelevanthistoryandexperiences
◾ Dailyfunctioningandqualityoflife (assessedthroughdirectobservationand self-report)
◾ Historyofrelationships,anyinterpersonalproblems
◾ Lifestyle
◾ Educationalandoccupationalhistory
◾ Familyhistoryofpsychiatricillness
◾ Historyofpriorviolentorsuicidal behavior
◾ Anyotherrelevantinformation(Seligman,2004;Strub&Black,2000).
Clinicianswillwanttogatherandreview anyrelevantrecords,previousassessments(i.e., psychologicaltests,medicalevaluations),and arrangetoobtainreleasessotheycancontact currentmedicalpractitionersaspartofcontinuityofcare.
Increasingly,mentalhealthprofessionals aremakinguseofsemi-structureddiagnostic interviews,psychologicalinventories,andrating scalesinthepreliminaryassessmentofclient functioning.Nosingleinstrumentfitsallsituations,andcliniciansmustdeterminewhatbest suitstheirneeds,alwaysleavingroom,of course,tocustomizequestionstothespecific scenario,andleavingacertainamountofflexibilitytoaccommodatetheclient.Therapists areremindedthatfosteringapositivetherapeuticallianceisfarmoreimportanttothe developmentofafacilitativerelationshipwith theclientthanthegatheringofspecificdetails. Thisisnevermoretruethanintheinitial
sessionswhenaclientmaybenervous,fearful ofbeingjudged,oruncertainofwhattoexpect intherapy.
Structureddiagnosticinterviewsinclude:
◾ StructuredClinicalInterviewforthe DSM-5(SCID-5;First,Williams,Karg, &Spitzer;2015)
◾ InternationalPersonalityDisorder Examination(Loranger,Janca,& Sartorius,1997)andtheSCID-5-PD (First,Williams,Benjamin,&Spitzer) forpersonalitydisorders(InPress)
◾ SymptomChecklist-90Revised(Derogatis,1994)—a90-itemchecklistcovering9symptomclusters
◾ BriefSymptomInventory(BSI;Derogatis&Melisaratos,1983)—a53item self-reportbasedontheSCL-90-R;easilyadministeredinlessthan10minutes)
◾ ScheduleforAffectiveDisordersand Schizophrenia(SADS;Endicott& Spitzer,1978)
Generalpersonalityinventoriesinclude:
◾ MillonClinicalMultiaxialInventory-III (Millon,Millon,Davis,&Grossman, 2009)
◾ MinnesotaMultiphasicPersonality Inventory-2(MMPI-2;Hathaway& McKinley,1989)
Scalestoassesssuicidalideation:
◾ ScaleforSuicidalIdeation(SSI;Beck, Steer,&Ranieri,1988)—a21-item ratingscalethatassessessuicidality.
◾ BeckScaleforSuicideIdeation(BSI; Beck&Steer,1991)—a21-itemselfreport.
Disorder-specificinventoriesareoftenused fordiagnosistodeterminetheseverityandfrequencyofsymptoms,andasabaselineforfuture
measurement.Assessmentsspecifictoeachdiagnosisarelistedintheappropriatechapters.Some ofthemostcommonlyusedinclude:
◾ BeckDepressionInventory(Beck, Steer,&Brown,1996)
◾ BeckAnxietyInventory(Beck&Steer, 1990)
◾ MichiganAlcoholismScreeningTest (Selzer,1971)
◾ Conners3rded.(Conners3;Conners, 2015)
◾ BehavioralAssessmentSystemfor Children–2(BASC-2;Reynolds& Kamphaus,2002)
◾ EatingDisorderExamination,16thed. (EDE;Fairburn,2008)
◾ DrugAbuseScreeningTest(Skinner, 1982)
Somemeasuresandscalesareincludedin DSM-5 tohelpwiththeinformation-gathering process.EmergingmeasuresfoundinSection IIIof DSM-5 (APA,2013)canhelptoprovidecross-cuttingsymptommeasurestoaidin diagnosis;disorder-specificseveritymeasuresto assessseverity,frequency,intensity,anddurationofsymptomsforspecificdisorders(e.g.,for depression,PTSD);ratingsofhomebackground andearlychildhooddevelopment;andcultural formulationinterviews.Thesecross-cutting toolsdonothaveenoughscientificevidence forsupportbutaredesignedtostimulatefuture research.ClinicianscanlinkintotheeHRS (electronichealthrecords)formorecomplex assessmentsofsymptoms(APA,2013,p.745).
TheWorldHealthOrganizationDisabilityAssessmentSchedule2.0(WHODAS 2.0)(Üstün,Kostanjsek,Chatterji,&Rehm, 2010)isa36-itemself-reportthatprovidesa usefulassessmentscalethatcanbehelpfulin trackingtreatmentprogress.Otherinventories andscalesarealsousefultoassessdifferentaspectsoftheperson,includingintelligence,
aptitude,achievement,interests,values,and careeraspirations.
Assessmentisanimportantcomponent oftreatmentplanningandshouldbeundertakenwithcare.Effectivetreatmentplanningis unlikelyunlesstheclinicianhasmadeanaccurateandcomprehensivediagnosisandhasa goodgraspoftheclient’sneedsandstrengths. Thiscanonlybeacquiredbytakingthetime toconductathorough,carefuldiagnostic assessment.
Throughoutthisbookassessmentmeasures willbediscussedforeachdisorder,whensuch measuresareavailable.
CLINICIANCHARACTERISTICS
(DOA CLIENTMAP)
Thetherapeuticalliance—thequalityof thebondbetweentheclientandtherapistand howwelltheyareabletoworktogetherto bringabouttherapeuticchange—isthebest predictoroftreatmentoutcome(Horvath& Symonds,1991).Individualdifferencesbetween therapistsarestronglypredictiveofthealliance quality(Laska,Smith,Wislocki,Minami,& Wampold,2013).
Ameta-analysisthatlookedattheroleof thetherapeuticalliancefoundthatitaccounted for8%ofthevarianceintreatmentoutcomes (Horvath,DelRe,Flückiger,&Symonds, 2011).Anothermeta-analysisofnearly70 studiesconfirmstheeffectofthetherapiston theallianceisasignificantpredictoroftreatmentoutcome(DelRe,Flückiger,Horvath, Symonds,&Wampold,2012)andthiscorrelationmaybeunderestimatedintheliterature(Crits-Christoph,ConnollyGibbons, Hamiltonetal.,2011).Theestablishment ofacollaborativerelationshipbetweenthe therapistandclientrefersnotonlytothe bondbetweenthembutalsototheirabilityto
establishandagreeonthegoalsoftreatment (Hatcher,Barends,Hansell,&Gutfreund,1995; Hatcher&Barends,1996,2006;Horvath& Bedi,2002).
Morethan50yearsofresearchhasprovided agooddealofevidenceonthecharacteristics, attitudes,andapproachesonthepartofthe therapistthatarecorrelatedwithtreatment outcomes.Wehavealsolearnedwhichones arenotimportant.Gender,age,andcultural background,forinstance,havelittleinfluence ontreatmentsuccess.Therapistswhorate higherontheRogerianconditionsofempathy,congruence,andunconditionalpositive regardtendtodevelopbettertherapeutic alliancesandhavemoresuccessfuloutcomes thanthosewhoranklower.Thisistrueregardlessofthetherapist’stheoreticalorientation (Zuroff,Kelly,Leybman,Blatt,&Wampold, 2010).
Thestabilityoftheallianceisalsoimportant;thereforeanyrupturesthatoccurmustbe recognizedandrepairedbythetherapistbefore theybecomebreaks.Rupturesmayincludemisunderstandingsbetweenthetherapistandclient oranyfeelingsonthepartoftheclientofbeing criticized,patronized,orunsupported;basically anyfeelingthatraisesconcernsintheclient’s mindaboutthetrustworthiness,sensitivity,or empathyonthepartofthetherapistcanbeconsideredtobeapotentialrupture.Thetherapist addressessuchconcernsastheyariseandmakesa concertedefforttoreassuretheclientandrestore thetherapeuticalliance.
Ofcourse,clientswillvaryintheirability toformatherapeuticalliance.Thosewithmore severementaldisorders(e.g.,schizophrenia spectrum,bipolar,severepersonalitydisorders), thosewhocannottrust,andthosewithmore severechildhoodattachmentwoundsmayneed additionalsupportivetherapyinordertobe abletodevelopapositivealliancewiththe therapist.Ineithercase—whetherarupture
occursorwhenaclienthasdifficultyestablishingatrustingrelationship—thetherapist mustslowthepaceoftherapy,respondwith empathy,addresswhatisgoingonintheroom withgenuineconcernandunconditionalpositiveregard—thefoundationonwhichtherapy isbuilt.
Itisonlybyactivelyworkingtomaintain thetherapeuticalliancethatpeoplewithsevere disordersorsubstanceabuseproblemswillstay intreatmentandgetthehelptheyneedtoovercometheirproblems.
Othertherapistvariablesalsoaffectoutcomes.Therapistswhoareemotionallyhealthy themselvesandwhoareactive,hopeful,optimistic,nonjudgmental,straightforwardandyet encouragingofresponsibilityonthepartofthe clientarethemostlikelytoachieveapositive outcome.Followingaresomeoftheresearch findingsrelatedtotherapistattributesthathelp tocreateandmaintainapositivetherapeutic alliance:
◾ Communicatingempathyandunderstanding
◾ Maintaininghighethicalstandards
◾ Havingstronginterpersonalskills;communicatingsupport,warmth,caring respect,acceptance
◾ Areassuringandprotectingattitude
◾ Affirmingratherthanblamingclients
◾ Beingabletohelptheclientaccessand tolerateemotion
◾ Empoweringclientsandsupporting theirautonomy
◾ Beingopen-mindedandflexible
◾ Beingnonjudgmentalandtolerantof ambiguityandcomplexity
◾ Modelingmentallyhealthyqualitiesof self-actualization,self-fulfillment,selfdevelopment,andbeingabletocope withtheirownstress
◾ Beingauthentic,genuine,credible
◾ Expressingoptimismandhope
◾ Beingculturallycompetent
◾ Beingactivelyengagedwithandreceptivetoclients
◾ Givingsomestructureandfocustothe treatmentprocess,butnotbeingoverly directive
◾ Beingauthoritativebutnotauthoritarian,andfreeingratherthancontrolling ofclients
◾ Beingnondefensive;beingawareof theirownlimitations,havingacapacity forself-criticism,alwayslookingforthe bestwaytohelpclients
◾ Focusingonpeopleandprocesses,not rules
◾ Andmostimportantly,establishinga positivetherapeuticallianceearlyon, andthenattendingtotheallianceat everystageoftreatment;addressing rupturesastheyoccur;andmanaging negativeprocesseseffectively(Bowman, Scogin,Floyd,&McKendree-Smith, 2001;Greenberg,Watson,Elliott,& Bohart,2001;Lambert&Barley,2001; Lambert&Cattani-Thompson,1996; Meyeretal.,2002;Muran&Barber, 2010;Orlinsky,Grawe,&Parks,1994; Rimondinietal.,2010)
Itshouldgowithoutsayingthattherelationshipbetweentherapistandclientisaprofessional one.Boundariesaresetthatarenottobebroken.Clientscometotherapyvulnerableandin needofsupport,andtherapistsareresponsible formaintaininghighethicalstandards.
Severalmeta-analysesconfirmthataquality allianceismorepredictiveofpositiveoutcomesthanthetypeofinterventionused (Karver,Handelsman,Fields,&Bickman,2006; Martin,Garske,&Davis,2000;Shirk&Karver, 2003).Therapistscanlearntoimprovetheir alliance-buildingbehaviorsthroughtraining,
supervision,andbyincreasingtheirresponsivenesswiththeirclients(Anderson,Lunnen,& Ogles,2010;Stiles,2009).
Carefulhandlingofalliancerupturesalso providestheclientwiththechancetolearnin thehere-and-nowofthetherapysessionhow torelatetoothersandaddressconcernsina productivemanner.Thiscanbeusedoutsideof therapyintheirrelationshipswithothers(Stiles etal.,2004).
Littleresearchisavailableontherelationshipbetweentherapistexperienceandtreatment outcome.Whatresearchisavailableisinconclusive.Someresearchindicatesthathavingmore experiencedoesnotguaranteeabetterworking alliance(Hersoug,Hoglend,Monsen,&Havlik, 2001),andtwostudiesfoundexpertisetobe moreimportantthantheoreticalorientation (Eells,Lombart,Kendjelic,Turner,&Lucas, 2005).Todate,othertherapistvariables,such astheamountofthetherapist’straining,the amountofprofessionalexpertise,orthetherapist’sprofessionaldiscipline(e.g.,psychologist, counselor,socialworker)havenotbeenfound toberelatedtotreatmentoutcomes.Oneearly study(Berman&Norton,1985)foundthat professionalsandparaprofessionalswereequally effective.
Therapistdemographicvariablessuchas gender,race,andreligion,andclinicalexpertise havenotbeenfoundtoberelatedtotherapeutic outcome(Bowmanetal.,2001;Wampold& Brown,2005).Ameta-analyticreviewofmore than60studiesontherapistgendershowed thatgenderhadnoeffectontreatmentoutcomes(Bowmanetal.,2001),ordrop-outrates (Cottone,Drucker,&Javier,2003).However,it shouldbenotedthatthegenderofthetherapist maybeimportanttosomeclients.Evenifgendermatchingdoesnotleadtoimprovedoutcomes,itmayenhancethetherapeuticalliance
tohonorsuchrequestsandmaybeworth considering.
Therapistage,whenlinkedtotherapist’s interpersonalskills,hadasignificanteffecton treatmentoutcomesinonestudybyAnderson andcolleagues(2009).Clientsseemtoprefera therapistwhoisoldenoughtounderstandthe client’sage-relatedanddevelopmentalissues, andwhoismatureenoughtohavesufficient experience,butnotsooldastohaveoutmoded ideasorbeliefsabouttreatment.
Therapistsmustalsobeawareofhowtheir ownworldviewsandthoseoftheirclients shapetheirexperiencesandassumptions.Every person,therapistandclientalike,willhavea varietyofdimensionsinwhichtheyidentify themselves(e.g.,age,gender,race).Therapists mustbeculturallycompetentintheirworkwith clients,recognizingthateveryoneisuniqueand willhaveexperiencesandbackgroundsthat differfromtheirowninoneormoreways.The mnemonicADDRESSINGcanbeagoodway torememberthewiderangeofsocial“locations”thatweallcomefrom.ADDRESSING standsforAge,Disability(acquired),Disability(developmental),Religionandspirituality, Ethnicity,Socioeconomicstatus,Sexualorientation,Indigenousheritage,Nationalorigin, Gender/sex(Hays,2001,2008).Understandingaperson’sculturecanbeasimportantas knowingtheirfamilybackgroundandcanmake treatmentmoreeffective(Hays,2009;Schnyder, 2009).
Therapistsshouldalsobeawareofanypersonaltraits,suchasbeingtoocriticalordemanding,thatmightdetractfromthedevelopmentof asolidworkingalliance.Defensiveness,excessive useoftechniques,andover-orunderstructuring sessionscanallinterferewiththedevelopment ofatherapeuticalliance(Sharpless,Muran,& Barber,2010).
LOCATIONOFTREATMENT
(DOACLIENTMAP)
In2012,34.1millionadultsintheUnited States(14.5%ofthepopulation)reportedhavingusedsometypeofmentalhealthtreatment orcounselingintheprevious12months.Of thosepeople,12.4%usedprescriptionmedications,6.6%soughtcounselingorotheroutpatientmentalhealthservices,and0.8%usedinpatienthospitalization(SAMHSA,2013).
Thesettinginwhichmentalhealthtreatmentisprovidedvariesbetweeninpatientand outpatientprograms.Ingeneral,thetreatment locationwillbedeterminedbythefollowing considerations:
1.Thedangerthattheclientposestoself orothers
2.Diagnosis,andnatureandseverityof symptoms
3.Goalsandobjectivesoftreatment
4.Costoftreatmentandconsideration ofinsurancecoverageandtheclient’s financialresources
5.Client’scurrentlivingsituationand supportsystems
6.Natureandeffectivenessofpriortreatment
7.Clientpreferences(Seligman,2004)
Theleastrestrictivesettingthatprovides optimalcarefortheperson’sneedsandthe disorderisoftenthebestchoice.Ifthesetting lacksresourcesthepersonneedsorisoverly restrictive,itmaynotbetherapeutic.Managed caremayalsorequiretheuseofthemostcosteffectivetreatment,forexample,requiringthat outpatienttreatmentforsubstanceabuseis consideredbeforeinpatienttreatmentwillbe considered.
Determiningthebesttreatmentplacement foranadult,adolescent,orachildrequires weighingavarietyofcomplicatedandinterrelatedfactors.Oftenthedecisionismadebased oninsurancecoverageandotherfinancialconsiderations.Optionstypicallyincluderesidential treatment,inpatienthospitalization,partial hospitalizationprogram(PHP),oroutpatient treatment.Theresearchliteratureprovideslittle guidance,sodecisionsmustbemadebasedon soundclinicaljudgment.Abriefdescriptionof eachfollows.
ResidentialTreatment
Residentialtreatmentprogramsareoftenconsideredforthosewithsevereeatingdisorders (e.g.,anorexia),chronicsubstanceusedisordersthathavenotrespondedtooutpatient treatments,andthosewhorequireadditional intensivetreatmentfollowinginpatientpsychiatriccare.Childrenandadolescentswith seriousemotionalandbehaviorproblemsmay beplacedinresidentialtreatmentsotheycan receive24-hoursupervisionandmonitoringby trainedstaff.Often,educationalrequirements willbemaintained.Placementinaresidential treatmentprogramisusuallyforanextended periodoftime.
InpatientHospitalization
Hospitalizationfortreatmentofmentalhealth issuesisusuallyrequiredincrisissituations, whenclientsneedtobecloselymonitored andwhenhelpingtoadjustorstabilize theclient’smedications.Inpatienthospitalizationissignificantlyshorterthanresidential treatmentandmayrangefromovernighttoless thanafewweeksinmostcases.Theaverage
lengthofaninpatienthospitalizationformental disorderswas7.2days(CentersforDisease Control,2010).Inpatienthospitalizationmay beappropriateforpeoplewhoareadangerto themselvesorothers,aswhensuicidalorhomicidalideationispresent.Treatmentprograms areusuallyhighlystructured.Patientsarelikely tobedischargedfromthehospitaltoaless restrictivesettingsuchasaPHPoroutpatient treatmentassoonaspracticable.
PartialHospitalizationPrograms(PHPs)
PHPsandday-treatmentprogramsarehighly structuredprogramsfocusedonthespecific needsoftheclient(e.g.,substanceuse,depression,dualdiagnosis,eatingdisorders).These programsallowpeopletoliveathomewhile attendingtreatmentduringtheday.PHPsoften serveastransitionaltreatmentfromresidential orhospitalizationprograms.Daytreatmentcan beaneffectiveandlesscostlyoptionforpeople whodonotneed24-hourcare.“Steppeddown”half-dayprograms,orweeklygroup meetingsthathelptomaintaintreatmentgains usuallyfollowPHPprograms.Limitedresearch showsthatdaytreatmentisbeneficialfor thetreatmentofpsychosis,mooddisorders, anxietydisorders,andborderlinepersonality disorder(Lariviere,Desrosiers,Tousignant,& Boyer,2010).Preliminaryresearchspecificto adolescentswithamooddisorderfoundthe PHPprogramdecreasedsymptomseverityand wasconsideredbytheadolescentstobean acceptableformoftreatment(Lenz,DelConte, Lancasteretal.,2013).PHPtreatmentalso reducescoststothird-partyandprivatepayers (Garfieldetal.,2010).
OutpatientTreatment
Themajorityoftreatmentformentalhealth disorderstakesplaceinoutpatientsettingsthat
includeprivatepractice,communitymental healthcenters,andagenciesthatfocusonspecificpopulationsorproblems(e.g.,domestic violence,children,multicultural,suicideprevention).Accordingto2012statistics,ofthosewho soughtoutpatienttreatmentforamajordepressiveepisode,themajorityofpeople(58.5%)did soattheirphysician’soffice.Morethan34%saw apsychiatristorpsychotherapist;24.6%went toacounselor’soffice;24.3%sawapsychologist,19%soughtreligiousorspiritualadvice; 11.6%sawanothermedicaldoctor,11.4%went toasocialworker,and7%sawanothermental healthprofessional(SAMHSA,2013).
INTERVENTIONS
(DOACLIENTMAP)
Thegrowingnumberofpsychosocial optionsforthetreatmentofmentalhealth disorderscreatenewpossibilitiesformillionsof people.Currently,morethan400differentnonmedication-relatedtreatmentinterventionsare knowntoexist,andmanymoreareevolving. Newtechnology-assistedtreatmentdelivery methodsaremakingitpossibleformorepeople thaneverbeforetoreceivetreatment,eventhose whocannotleavetheirownhomes.
Newmindfulness-andacceptance-based approachesarehelpingpeopletocontrolrumination,anxiety,anddepression,andmany therapistsaremovingtowardtransdiagnostic treatmentapproachesthatfocusonrelated symptomsratherthantheoreticalorientation.
Eachofthesenewmodesoftreatment providesadditionaloptionsformorespecializedtreatmentgearedexclusivelytotheclient experiencingaspecificdisorder.
Moreandmorefrequently,therapistsare saying“IwastrainedinX,Y,orZapproach,but nowIhaveexpandedintoCBT,mindfulness, existential,orinterpersonaltherapy.”Many
prefertoworktogetherwiththeclienttoestablishasolidworkingrelationshipinwhichthey cancollaborativelydeterminewhatapproach willworkbest.
Inthe1980s,muchwasrevealedaboutthe importanceofthetherapeuticallianceinthecreationofevidence-basedtreatments.Thencame researchoncommonfactorsthatarefoundinall successfultherapies,regardlessofthediagnosis, suchasthetherapeuticalliance,clientmotivation,therapistskill,andtheeffectofthecollaborativerelationshipontreatmentsuccess.It isbecomingmoreandmoredifficulttoadvocateforonetheoreticalorientationortreatment modality,astheresearchbeginstomakeclear thatmosttreatmentsareeffective,ifcertainconditionsaremet.Oneofthemostwidelystudied commonfactorsisthetherapeuticalliance.That thestrengthoftheallianceisrelatedtotreatmentoutcomehasbeenverifiedovertheyears innumerousstudiesandmeta-analyses(DelRe etal.,2012;Gaudiano,Dalrymple,Weinstock,& Lohr,2015;Martinetal.,2000).
Today,theexperiencedtherapist,knowledgeableinevidence-basedpractice,knowsthe followingtruths:
◾ Theallianceisresponsibleforalarge partofthesuccessoftherapy.
◾ Theallianceconsistsofthetherapist andtheclient,andtherelationshipthat developsbetweenthem.
◾ Sometreatmentsareevidence-basedfor usewithcertaindisorders(e.g.exposure therapyforspecificphobias;dialectical behaviortherapy[DBT]forborderline personalitydisorder).
Withcaseformulationprovidingthefoundation,treatmentrecommendationsshouldfirst considerevidence-basedtreatmentsthatare available(Chorpita,Daleiden,&Weisz,2005). Awealthoftreatmentinterventionoptionsare
available,andsettinggoalsandobjectivesfor treatmentshouldbeacollaborativeexercise withthetherapistprovidingtheexpertiseabout treatmentrecommendations,whilebeingflexibleenoughtotweaktherecommendationsto theneedsoftheclient.Insomecases,comorbiddisorderswillneedtobeaddressedbefore treatmentcanbegininearnest.Forothers, relationshipissues,emotionaldysregulation,or symptomsofpersonalitydisordersmayneedto beaddressed.
EmpiricallySupportedTreatments
TheAmericanPsychologicalAssociationbegan trackingempiricallysupportedtreatments (ESTs)in1993throughitsDivisionofClinical Psychology.In1995,thefirstlistofESTswas createdthatmetthecriteriafordifferentlevelsof support.“Well-establishedtreatment”requires eitherofthefollowing:(1)tworandomized trialsthatdemonstratedefficacycomparedwith aplacebooranotherestablishedtreatmentor(2) alargeseriesofsingle-casedesignexperiments. “Probablyefficacioustreatment”hasfewer restrictions.
AmericanPsychologicalAssociation’sPresidentialTaskForceonEvidence-BasedPractice (2006)establishedawebsitelistingthebest availableresearchevidencewhich,whencombinedwithclinicalexpertiseofthetherapist, andclientcharacteristicsandvalues,provides thebestevidence-basedpracticesavailable.The listcanbesortedbydisorderorby75treatments thathavemetthecriteriaforempiricallysupportedtreatment.WhentheDivision12Task ForcepublisheditsfirstlistofESTsin1995, only18treatmentswereidentifiedashaving empiricalsupport;todaythereareover75,many ofthemwithwell-establishedresearchsupport.
Manyoftheresearch-supportedpsychologicaltreatments(e.g.,socialskillstraining forschizophreniaandstressinoculation
training),havebecomestandardsinmost therapist’srepertoire.OtherESTsaretreatments recentlyadded,suchasacceptanceandcommitmenttherapyforchronicpain,CBTforsocial anxiety,andprolongedexposureforPTSD. SomeoftheotherESTsarelistedhere.The completelistisavailableonlineatwww.div12 .org,alongwithinformationonclinicaltrials, bonusmaterial,andlinkstotrainingmanuals andinteractivecontent.
◾ Acceptanceandcommitmenttherapy forchronicpain,depression,mixed anxiety,psychosis,andOCD
◾ Cognitivebehavioraltherapyfor ADHD,eatingdisorders,generalized anxietydisorder(GAD),specificphobias,socialanxiety,panic-disorder, schizophrenia,andPTSD
◾ Behavioralcouplestherapyforalcohol usedisordersanddepression
◾ Dialecticalbehaviortherapyforborderlinepersonalitydisorder
◾ Eyemovementdesensitizationandreprocessing(EMDR)forPTSD
◾ Emotion-focusedtherapyfordepression
◾ Family-focusedtherapyforbipolar disorder
◾ Family-basedtreatmentsforanorexia andbulimianervosa
◾ Interpersonaltherapyforbinge-eating disorder,bulimianervosa,anddepression
◾ Exposureandresponseprevention (E/RP)forOCD
◾ Exposuretherapiesforspecificphobias
◾ Schema-focusedtherapyforborderline personalitydisorder
◾ Sociallearning/tokeneconomyprogramsforschizophrenia
◾ Socialskillstrainingforschizophrenia
◾ Supportedemploymentforschizophrenia
TheAmericanPsychologicalAssociation’sDivision53maintainsalistof evidence-supportedtreatmentsforchildren andadolescents.Themostwellestablishedare:
◾ CBTandinterpersonalpsychotherapy (IPT)fordepression
◾ BehaviortherapyforADHDandautism spectrumdisorders
◾ Familytherapyforeatingdisorders
◾ Trauma-focusedCBTforanxiety
◾ Parentmanagementtrainingforoppositionaldefiantdisorderandconductdisorder
Thewebsite(effectivechildtherapy.org) containsotherpromisingtreatmentsandisupdatedonaregularbasisasacommunityservice tothepublic.
Otherresourcesforevidence-basedtreatmentsincludetheNationalInstituteforHealth andClinicalExcellence(NICE)andthe NationalRegistryofEvidence-BasedPrograms andPractices(NREPP).Eachoftheseorganizationsislistedintheresourcessectionatthe endofthischapter.
AlthoughESTshavebeenidentifiedfor manydisorders,acomprehensivelistofeffective treatmentsforeverydisorderdoesnotexist. Insomecases,severaldifferenttreatmentshave beenfoundtobeeffective(asisthecasewith anxietyandmooddisorders,schizophrenia,and borderlinepersonalitydisorder).Inothercases, notreatmentapproacheshavereceivedstrong researchsupport.Inthistext,thefocusisprimarilyonwhattreatmentinterventionsare efficaciousandofferthebesttreatmentoptions forclients.Whenthatresearchisnotavailable, casereportsintheliteraturecanhelptoprovide someguidance,ascanrelatedtreatmentsfrom similardisordersbeusedtoextrapolatepotential outcomes.Theinterventionssectionforeach
disorderwilldescribeevidence-basedtreatments iftheyareavailableforthatdisorderoritcan provideothertreatmentrecommendationsthat havesomeresearchsupport.
A“research–practicegap”seemstoseparatethetimewhenatreatmentintervention isdeterminedtobeefficaciousandwhenthe interventionbecomescommonpractice.One studyfoundthatmosttherapistsarenottrained inevidence-basedtreatments(Schnyder,2009). However,mostclientsdonotlookforatherapistbasedontheirtheoreticalorientation. ManyESTsaremanual-based,andsomeclients feelputoffbytreatmentmanuals.Whether manual-basedornot,alaterstudybySchnyder foundthat20%ofclientsdroppedoutof empiricallysupportedtherapies.
Clearlytherearesomemodesoftherapy thatareharmfulandshouldnotbeused.Some mayhaveambiguousresearchresultsorthe researchstudyitselfmaybeflawed.Clinicians areresponsibleforchoosingthetreatment methodologiesusedintherapyandhaveaprofessionalresponsibilityaspartofthebroader medicalcommunitytoabidebytheHippocratic oathto“First,donoharm.”Theuseoftreatmentsthatarenotevidence-basedshouldbe donewithcaution.Treatmentsknowntocause harmortoresultindecrementsincareshould notbeusedatall.
Agrayareaexists,however,intreatments thathavenotbeenwellresearchedbutarebeing usedextensivelybytherapists.Thishasbeenthe subjectofmuchcontroversyintheprofessional literature,anditmustbenotedthatsomeofthe so-calledcontroversialtreatmentsofadecade agohavebecomethenewerevidence-based treatmentsoftoday.Readersareencouraged toconductduediligencebeforeimplementing novelandunsupportedtherapies,especially whenthereislittleornounderlyingtheoretical basis(Pignotti&Thyer,2015).Acompelling
andcomprehensivelookattheoverarching controversiesinpsychologicaltreatmentcanbe foundinLilienfeld,Lynn,andLohr(2015). Experiencedtherapistsalsoknowthatthere aremanydifferentwaystofostersuccessin clientoutcomes.Beginningwiththeveryfirst telephonecallfromaclient,theyworktoward thecreationofacollaborative,professional,and therapeuticrelationship.Itisthisrelationshipon whichmosttherapeuticchangeisgrounded.
WhentoRecommendNoTreatment
Research-basedpracticelooksatalloptionsfor treatment,andtheoptionofnointerventionat allmustbeconsidered.Thefactis,asmanyas5% to10%ofpeoplewhoreceivetreatmentdeteriorateduringtheprocess(Lambert&Ogles,2004). Althoughlittleresearchisavailableonthenegativeeffectsofpsychotherapy,itappearsthatno treatmentatallmightbethebestrecommendationinthefollowingspecificsituations:
◾ Clientswithanestablishedhistoryof multiple-treatmentfailures.
◾ Clientswhoareintheprocessoflitigation(e.g.,divorce,childcustodydispute,court-orderedtreatment).These clientsmayhaveanulteriormotive forseekingtreatmentandmight,therefore,obfuscateorotherwiseconfound treatment.
◾ Newclientswhoattendtherapyforthe expressedpurposeoffilingadisability claimandmayhaveaninvestmentin failingtomakeprogress.
◾ Peoplewithmalingeringorfactitious disorderswhoreceivesecondarygain fromattendingtherapysessionsbuthave nomotivationorintentiontochange.
◾ Peoplewhoareatincreasedriskof havinganegativeresponsetotreatment,
includingthosewithingrainedpersonalitydisorders(e.g.,narcissistic,borderline,obsessivecompulsive,antisocial), thosewithoppositionaloraggressive personalitypatterns,orpeoplewhoare destructivetoselforothers.
Othercausesoftreatmentdeteriorationincludeamismatchbetweentherapistandclient ongoals.Suchlackofcongruenceoftenresults inclientsdroppingoutoftreatment(Antony& Barlow,2011).Assessingreadinessforchange, asdiscussedearlier,canoftenreducesuch treatmentfailures.Therecommendationofno treatmentisdesignedtoprotectclientsfrom harm,preventnegativetherapyexperiences, anddelaytreatmentuntiltheclientismore receptive.Insomecases,peoplemaycometo therapymerelyoutofcuriosityandtoseewhat itisallabout.Intheabsenceofanidentifiable disorderorcondition,theyshouldbeinformed thattheywouldmostlikelynotbenefitfrom therapy.Althoughtherecommendationofno therapymaybethebestchoice,discouraging peoplefrombeginningtherapywhenitisdifficulttoknowiftheyactuallymightbenefitmay becounterintuitive,andmanytherapistsmaybe unwillingtousethisoption.
EMPHASIS
(DOACLIENTMAP)
Clinicianstendtoadaptmodelsofpsychotherapytofittheirownpersonalstylesand tofittheindividualizedneedsofparticular clients.Evenwithinthesametreatmentmodality,differenttherapistswillapplythemethod differently.Clientswillalsohavetheirown effectontreatment.Itcanevenbesaidthatthe applicationofanapproachtopsychotherapy differsfromonetherapeuticrelationshipto
another.Thedimensionsoftherapydiscussedin thissectionreflectsomeofthewaysinwhich treatmentisadaptedtotheindividualthrough variousareasofemphasis.
DirectiveVersusEvocative
Therapeuticapproachescanbedirective,evocative,ormixed.Thedirectiveapproachhasbeen correlatedwithafocusongoalattainmentand lower-than-averagelevelsoftherapeuticalliance (Hersoug,Hoglend,Havik,vonderLippe,& Monsen,2009;Malik,Beutler,Alimohamed, Gallagher-Thompson,&Thompson,2003; Muran&Barber,2010).Evocativeapproaches emphasizeprocessessuchascatharsisandabreaction;genuineness,empathy,andreflection offeeling;support;andunconditionalpositive regard.Evencriticismorconfrontationissupportive.Sometimestherapistsmixapproaches; initiallybeingmoreevocativeandsupportive inassessmentorsymptomfocus,andmore directiveintreatmentincognitiveandbehavioralgoals.
Directiveapproachesgenerallyseekto changebehaviororcognitions.Thetherapist isincharge,determinestreatment,andtargets specificsymptomsorgoals.Anyofthetechniquesinthecognitivebehavioralspectrum willbedrawnontohelptheclientexperience realbehavioralchange.Systematicdesensitization,flooding,positivereinforcement,token economies,Socraticdialogue,bibliotherapy, andothertechniqueswithinthesession,reinforcedbetweensessionswithassignments, journaling,bibliotherapy,andbehaviorcharts toreinforcelearning.AlbertEllis,founderof rationalemotivebehaviortherapy,encouraged clientstoformulateexperimentstheycould conductbetweensessionsanddiscusstheresults ingreaterdepthatthenextsession.Inall directiveapproaches,thetherapistassumesan
authoritativestance,definestargetconcerns, andoverseesaspecificprogramdesignedto changeovertandcovertsymptoms.
Alternatively,anevocativeapproachseems morelikelytobesuccessfulwithpeoplewho areself-directedandmoreabletoparticipatein asoundalliancebetweenclientandtherapist (Maliketal.,2003;Sharplessetal.,2010). Approachesthatareprocess-experiential,psychodynamic,andhumanistic(e.g.,Gestalt, person-centered,emotion-focused)modelsare generallylowondirectionandhighonevocativeness,trustingtheclienttodeterminethe focusofthesessionbasedontheirownsenseof priority.Evocativetherapiesaremoreprocessexperientialandviewthepersonastheexpert onhisorherownlifeand,therefore,theone bestabletosolvetheproblem.
ExplorationVersusSupport
Anotherdimensionthathasbeenthesubject oflittlefocusintheliteraturebutisanimportantaspectoftreatmentisthedimensionof explorationversussupport.Thosethatfocuson explorationaretypicallyanalytical,probing,and interpretive.Recognitionofpastinfluencesand patternsofbehaviorarestressedinaneffortto promoteinsight.Bycontrast,approachesthat emphasizesupporttendtofocusonthepresent withagoalofsymptomreliefandbehavioral change.
However,researchhasconcludedthat insightisnotalwaysnecessaryforchangeto occur(Wallerstein,1986).In45%ofcases, changesseemedtogobeyondthelevelofinsight thatwasattained,whereasinsightsurpasseddiscernedchangeinonly7%ofthecases.Overall, Wallersteinconcludedthatsupportivetherapy wasmoreeffectiveinthesecasesthanhadbeen expected,anditdidnotseemtobelesseffective thanexploratorytherapy.Indeed,Schnyder
(2009)statesthat70%oftherapyissupportive therapywithorwithoutmedication,despite thelackofempiricalsupportforthistreatment modality.
Supportivepsychotherapyprovidesempathy,encouragement,andreassuranceandhelps toenhancetheclient’sself-esteematatime whenheorsheisincrisis,isrecoveringfroma diagnosisofaseriousmentalillness(i.e.,bipolar, schizophrenia,dementia),orhasdecompensated tothepointwhereunconditionalacceptance, activelistening,andempathyprovidedina safeenvironmentisnecessarytoprovidecontainment,tobuildatherapeuticalliance,and toinstillhope,sothat,eventually,psychoeducation,cognitiverestructuring,problemsolving, orenvironmentalchangecantakeplace.
Supportivetherapyhasbeendefinedasan interventiondesignedtostrengthenegofunctioning,realitytesting,andclarityofthought sothatthepersoncanresume,orcontinueon withtheskillsofdailyliving.Rockland(2003) outlinedanapproachtosupportivetherapythat providesbothsupportiveandexploratoryinterventions.Byfindingtherightmixofsupport andexploration,thetherapistcantailorthe interventionstobestfittheclient’sneedsina particularsituation.
OtherAspectsofEmphasis
Howmuchthetreatmentfocusesonthepast,the present,orthefutureisalsoanimportantdimensionoftreatmentthatwillbeinfluencedby theclient’sneedsinconjunctionwiththetherapist’spredilections,amongotherconsiderations. Adaptingatreatmentapproachtoaspecificperson,aswellasknowingwhentofocusonaspects ofonetheoreticalorientationoveranother areoftendeterminedbytherapeuticinstincts. Mosttherapistsintuitivelydetermine whethertheirclientsneedhighorlowlevels