Dedication
Thisfourtheditionisdedicatedwithloveandgratitudeto:
My husband Jim “Bear” Baranoski For the support, encouragement, and devotion you have given me for half century. I couldn’t love you more.
The Baranoski offspring and their significant others Jim Jr.; Deborah and Mark Prosise; Jeffrey and Kari Baranoski; and JR (John Robert) and Carissa Baranoski, thank you for your love and laughter and for bringing joy and craziness to my life. I am so blessed to have wonderful children. Love you all, Mom.
The Baranoski grandchildren Maddie Gombosi, Morgan Prosise, Lexi, and Lanie Baranoski; Brek and Brooklyn Baranoski; Alia and Tyler (TJ) Baranoski; and any future ones to come. I love you all from the deepest part of my heart. You brighten my life and certainly make me laugh and very proud. I love you much, Gramma.
To all the nurses, physicians, healthcare practitioners, and healers who have honestly acknowledged how much we don’t know and how much we have to learn. Never stop wanting more.
“Familyiseverything.”
That’s whatmyparents,Phyllis andTony,andbrothers,BobandRon,taught me.
So thank you to my families biological and professional friends, and patients who have shared their experiences, supported, and nurtured me through this educational journey. There are too many of you to mention individually;itwould take more thanwhatcould be contained onthis page.
Hopefully I have done a good job of expressing my appreciation and gratitudetoyoueachandeveryday.
To:
Katie,whotaughtmethepsychosocial meaningofhealing
Sarah,whotaughtmethetruemeaningofhealing
Wendy, who taught me the meaning of hope for healing and the promise of tomorrow
A. Scott, who taught me to never stop learning and who brings the art to balance my science. Thank you for being there, so I can dance like nobody iswatching
Contributors
ElizabethA.Ayello,PhD,RN,ACNS-BC,CWON,MAPWCA,FAAN Faculty
Excelsior College Schoolof Nursing
Albany, New York
ClinicalAssociate Editor
Advances in Skin & Wound Care
Executive Editor Emerita
Journalof the World Councilof EnterostomalTherapists (WCET)
Senior Adviser
The John A Hartford Institute for Geriatric Nursing President
Ayello, Harris & Associates, Inc.
New York, New York
SharonBaranoski,MSN,RN,CWCN,APN-CCRN,MAPWCA,FAAN
President
Wound Care Dynamics, Inc.
Nurse Consultant Services
Shorewood, Illinois
Symposium Director
ClinicalSymposium on Advances in Skin & Wound Care
EditorialAdvisory Board
Advances in Skin & Wound Care
NursingAdvisory Board
Rasmussen College
Romeoville/Joliet, Illinois
Councilof Regents & NursingAdvisory Board
Lewis University
Romeoville, Illinois
DanR.Berlowitz,MD,MPH
Co-Director
Center for Healthcare Organization and Implementation
Bedford Virginia Research Hospital
Bedford, Massachusetts
JonathanS.Black,MD Fellow Physician
Department of Plastic Surgery
MedicalCollege of Wisconsin
Milwaukee, Wisconsin
Joyce M.Black,PhD,RN,CWCN,FAAN
Associate Professor
College of Nursing
University of Nebraska MedicalCenter Omaha, Nebraska
BarbaraBraden,PhD,RN,FAAN
Dean Emerita
Graduate Schooland University College
Creighton University Omaha, Nebraska
DavidM.Brienza,PhD
Professor
Department of Rehabilitation Science and Technology
University of Pittsburgh Pittsburgh, Pennsylvania
GregoryBrown,RN,ET
Case Manager
Dallas Veterans MedicalCenter
Dallas, Texas
Janet E.Cuddigan,PhD,RN,CWCN,FAAN
Associate Professor
College of Nursing, Omaha Division
University of Nebraska MedicalCenter Omaha, Nebraska
LindaE.Dallam,MSN,RN-BC,GNP-BC,CWCN-AP
ClinicalDocumentation Specialist/Care Management Coordinator
CMO, Utilization Management Montefiore MedicalCenter Bronx, New York
BeckyDorner,RD,LD,FAND
President
Becky Dorner & Associates, Inc
Nutrition ConsultingServices, Inc. Naples, Florida
PaulaErwinToth,MSN,RN,CWOCN,CNS
Director Emerita, WOC NursingEducation
Cleveland Clinic
Cleveland, Ohio
Caroline E.Fife,MD,UHM,CWS
MedicalDirector
St. Luke’s Wound Clinic
Chief MedicalOfficer
Intellicure
The Woodlands, Texas
Professor of Geriatrics
Baylor College of Medicine
Houston, Texas
SusanGallagher,PhD,MSN,MA,RN
Senior ClinicalAdvisor
Celebration Institute, Inc.
Houston, Texas
SusanL.Garber,MA,OTR,FAOTA,FACM
Professor
Department of PhysicalMedicine and Rehabilitation
Baylor College of Medicine
Houston, Texas
MaryJoGeyer,PT,PhD,CPed,FCCWS,CLT
Program Director
Indian River State College
Fort Pierce, Florida
KeithHarding,MB,ChB,FRCGP,FRCP,FRCS
Dean of ClinicalInnovation
Head of Wound HealingResearch Unit
Schoolof Medicine
Cardiff University
Cardiff, Wales, United Kingdom
WendyS.Harris,BSHS,BSN,RN
Hollis Hills, New York
SamanthaHolloway,MSc,PGCE,FHEA,RN
Senior Lecturer
Wound HealingResearch Unit
Schoolof Medicine
Cardiff University
Cardiff, Wales, United Kingdom
CarolinaJimenez
Research Assistant
Queen’s University, Schoolof Nursing
Kingston, Ontario
PaulKim,DPM,MS,FACFAS
Associate Professor
Director of Research
Division of Wound Healing
Department of Plastic Surgery
Georgetown University Hospital Washington, District of Columbia
Robert S.Kirsner,MD,PhD
Professor, Vice Chairman, and StiefelLaboratories Chair
Chief of Dermatology
University of MiamiHospital
University of MiamiMiller Schoolof Medicine
Miami, Florida
CarlA.Kirton,DNP,RN,MBA
Chief Nurse Executive
Lincoln Hospital& MentalHealth Center New York, New York
RonaldA.Kline,MD,FACS
Chief Division of Vascular and Endovascular Surgery
MedicalDirector of Wound Care
Carondelet St. Joseph Hospitaland Tucson Kindred Hospital Tucson, Arizona
StevenP.Knowlton,JD,RN
Partner
Locks Law Firm, PLLC New York, New York
JavierLaFontaine,DPM,MS
Associate Professor Department of Plastic Surgery UT Southwestern MedicalCenter
Dallas, Texas
Diane K.Langemo,PhD,RN,FAAN
Consultant, Langemo & Associates
Adjunct/Emeritus Professor
University of North Dakota College of Nursing
Grand Forks, North Dakota
Lawrence A.Lavery,DPM,MPH
Professor
Department of Plastic Surgery
University of Texas Southwestern MedicalCenter Dallas, Texas
KimberlyLeBlanc,MN,RN,CETN(C),PhDStudent
Advanced Practice Nurse KDS ProfessionalConsulting Ottawa, Ontario, Canada
JeffreyM.Levine,MD,AGSF,CMD,CWS-P
AttendingPhysician
Center for Advanced Wound Care
Mount SinaiBeth Israel
New York, New York
AndreaMcIntosh,RN,BSN,CWOCN,APN/CCNS Manager
Wound Center and WOCN Department
Silver Cross Hospital
New Lenox, Illinois
LindaMontoya,BSN,RN,CWOCN,APN
Corporate Wound Consultant Symphony Post Acute Network Lincolnwood, Illinois
JeffreyA.Niezgoda,MD,FACHM,MAPWCA,CHWS President and CMO WebCME Milwaukee, Wisconsin
MarciaNusgart,RPh Executive Director
Alliance of Wound Care Stakeholders
Bethesda, Maryland
MaryEllenPosthauer,RDN,LD,CD,FAND
President
MEP Healthcare Dietary Services, Inc.
Evansville, Indiana
SandyQuigley,RN,MSN,CWOCN,CPNP-PC
ClinicalSpecialist in Wound, Ostomy, and Continence Department of Nursing
Boston Children’s Hospital Boston, Massachusetts
KarenRavitz,Esq.
Nusgart Consulting, LLC
Silver Spring, Maryland
PamelaScarborough,PT,DPT,CDE,CWS,CEEAA
Pamela Scarborough Doctor of PhysicalTherapy
Certified Diabetes Educator
Certified Wound Specialist
Certified Exercise Expert for AgingAdults
Director of Public Policy and Education
American MedicalTechnologies Irvine, California
GregorySchultz,PhD
Professor of Obstetrics & Gynecology Institute for Wound Research University of Florida Gainesville, Florida
R.GarySibbald,BSc,MD,FRCPC(Med,Derm),MACP,FAAD,M.Ed, MAPWCA,D.Sc.(Hons)
Professor of Medicine and Public Health University of Toronto
ClinicalEditor, Advances in Skin & Wound Care
Course Director IIWCC & Masters of Science, Community Health (Prevention & Wound Care)
Past President World Union of Wound HealingSocieties Mississauga, Ontario, Canada
MaryY.Sieggreen,APRN,CNS,NP,CVN
Nurse Practitioner, Vascular Surgery
Harper University Hospital, Detroit MedicalCenter
Detroit, Michigan
StephenSprigle,PhD,PT
Professor
Applied Physiology, Bioengineeringand IndustrialDesign
Georgia Institute of Technology
Atlanta, Georgia
Joyce K.Stechmiller,PhD,ACNP-BC,FAAN
Associate Professor and Chair
Adult and Elderly Nursing
University of Florida College of Nursing
Gainesville, Florida
NancyA.Stotts,RN,EdD,FAAN
Professor Emeritus
University of California
San Francisco, California
LindaJ.Stricker,MSN,RN,CWOCN
Program Director
R.B. Turnbull, Jr, MD Schoolof Wound Ostomy Continence NursingEducation
Cleveland Clinic Digestive Disease Institute
Cleveland, Ohio
MarjanaTomic-Canic,PhD
Professor of Dermatology Director
Wound Healingand Regenerative Medicine Research Program
Department of Dermatology and Cutaneous Surgery
University of MiamiMiller Schoolof Medicine
Miami, Florida
TerryTreadwell,MD,FACS
MedicalDirector
Institute for Advanced Wound Care
Montgomery, Alabama
Suzanne vanAsten,MD,MSc
Department of Plastic Surgery
University of Texas Southwestern MedicalCenter
Dallas, Texas
Department of InternalMedicine
VU University MedicalCenter
Amsterdam, the Netherlands
ElizabethVanDenKerkhof,RN,DrPH
Professor
Department of Anesthesiology and Perioperative Medicine
Schoolof Nursing
Queen’s University Kingston, Ontario, Canada
FreyaVanDriessche,MS
Wound Research Fellow
Department of Dermatology and Cutaneous Surgery
University of MiamiSchoolof Medicine
Miami, Florida
Gregory RalphWeir, MBChB (UP), MMed(Chir)(UP), Cert Vasc Surg (SA),IIWCC(ZA)
MedicalDirector
Vascular and Hyperbaric Unit
Eugene Marais Hospital
Pretoria, South Africa
KevinY.Woo,PhD,RN,FAPWCA
Assistant Professor
Schoolof Nursing
Faculty of Health Sciences
Queen’s University Kingston, Ontario, Canada
KarenZulkowski,DNS,RN
Associate Professor
Montana State University College of Nursing
Billings, Montana
Foreword
Itis mypleasure to write the foreword for the fourtheditionof Wound Care Essentials: Practice Principles,editedbytwoofthemostrespectedpeople in the field of wound care, Dr. Elizabeth Ayello and Sharon Baranoski. As always, these editors have done a superb job of makingimprovements to a text that is already outstanding. The changes they have made are relevant and timely, and they have brought together an inimitable teamof experts to write each chapter. Over half of the chapters in this edition have either entirely new authors or additional experts added to a team of authors to assurethemostup-to-date,accurate,andpertinentcontent.
This edition follows rapidly on the heels of the recent release of the 2014 NPUAP/EPUAP/PPPIA clinical practice guidelines and systematicallyincorporates these into all appropriate chapters. Readers can be assured that clinical recommendations incorporated fromthe guidelines have been subjected to structured and deliberate scientific scrutiny to evaluate the strength of the evidence. In addition, clinicians can depend on the expertise of the authors to deliver the best in clinical decision making whenevidenceislackingbutactionisnecessary.
High-resolution color photos, so important to understanding the nature of various types of wounds and treatments, are no longer confined to the center pages ofthe bookbutare integrated throughoutthe textand placed in proximity to the content that is germane to the type of wound or type of treatment under discussion. In addition, Chapter 24 has a wound photo galleryof39differenttypes ofwounds withquestions for readers toanswer andconsider.
Several topics have expanded coverage in this edition. There is an entirelynew chapter onQualityofLife issues for patients withwounds that lays a sound foundation of theoretical issues before moving on to clinical concerns related to quality of life. Skin tears have been more thoroughly addressed, and the update includes the work of International Skin Tear AdvisoryPanel (ISTAP).Also,inthisnew andimprovededition,thereader will find the chapter onwound bioburdenhas beenrewrittenand expanded and fistula management has been added to the chapter on tubes and drains. These are but a few examples, but because of the many chapters that have new authors or coauthors, many other changes will be evident to those
familiar withthethirdedition.
As in the previous edition, a general emphasis on knowledge management remains. Knowledge management involves gatheringdata from a variety of sources, organizing it so that patterns become apparent, providing context that is relevant to understanding the principles related to action(inthis case, professional practice) and deliveringall ofthese things to the end user in timely fashion and in a format that expedites rapid assimilation.Thesearethe“bones”aroundwhichthethirdeditionof Wound Care Essentials: Practice Principles was built and the fourth edition retains this structure. New authors, new content, and new sources of evidence have been added. Context is provided with patient scenarios and case discussions as well as anexpanded use ofcolor photos withinthe text. Questions are provided atthe end ofeachchapter as a self-assessmentwith answers provided at the end of the book. All are in a format that supports rapidassimilationofcontent.
Congratulations to the editors and the authors on producing a book that will help clinicians, whether novices or experts, to manage the complex knowledgesurroundingwoundcareinatrulysubstantiveway
BarbaraBraden,PhD,RN,FAAN Dean Emerita, Graduate School and University College
Creighton University Omaha, Nebraska
Preface
“May there never develop in me the notion that my education is complete, but give me the strength and leisure and zeal continually to enlarge my knowledge”
We agree with the above statement by Maimonides. That’s one of the reasons that we have decided to update and expand this fourth edition of Wound Care Essentials: Practice Principles. Over the years, you, our colleagues, have told us the role our book has played in your continuing professional education. Whether it was for studying for certification, updating policies and procedures, or serving as a concise compendium of evidence for informed practice. Your feedbackis valuable to us; youspoke and we have listened! You asked for some new features and we have delivered. The first obvious change is we have increased the number of color photos, and they are now within each chapter rather than just in one color section. Eachchapter has beenreviewed, revised, and updated. Your enthusiastic support of the “Show what youknow” feature of our bookwill remain at the end of each chapter. As you requested, we have moved the answers to the back of the book so you don’t immediately see the answer below each question. No peeking now! You told us that you wanted to be challenged with more pictures to strengthen your ability to assess and identify wounds. New to this edition of Wound Care Essentials is the Wound Gallery. This chapter will give youthe opportunityto applyand test your knowledge gained fromthe fourth edition. See how well you do with this new photo quizfeature ofour book. Ofcourse, we have retained all the other components of our book that you love including the patient scenarios attheendofeachchapter.
Thank you to all who have come up to us at clinical symposiums and congressestoshow usyour well usedcopy!Wearethrilledtoknow thatour book hasn’t sat on a shelf unused. Essential to our book has been the interprofessional approach to both the content and authorship of the chapters. We are delighted that so many of our previous authors could continue to share their expertise with you as well as to welcome new authors to this fourth edition. Thank you to all of our authors for your contributions. We are deeply grateful to Barbara Braden for once again writingtheforewordtothisour fourthedition.
Our dream of a book that contained the essentials of wound care was inspired by our mentor and dear late friend, Roberta Abruzzese. We hope we have lived up to her words “keep the words succinct, and clear so to help the clinician by compiling the latest and best information they need in practice.”
Bringing a book to publication is no easy task, but we have been supported by a phenomenal team from Wolters Kluwer. Thank you to Shannon Magee, Maria McAvey, Emilie Moyer, Karen Doyle, Tom Conville,andall thosewhoworkedtoproduceour book.
To our readers, we hope the knowledge youacquire fromour bookwill positivelyimpact, and change outcomes for your patients and perhaps even the care delivery systems within your work place. For we believe what NelsonMandela said “Education is the most powerful weapon which you can use to change the world. ”
SharonandElizabeth
Quality of Life and Person-Centered Concerns
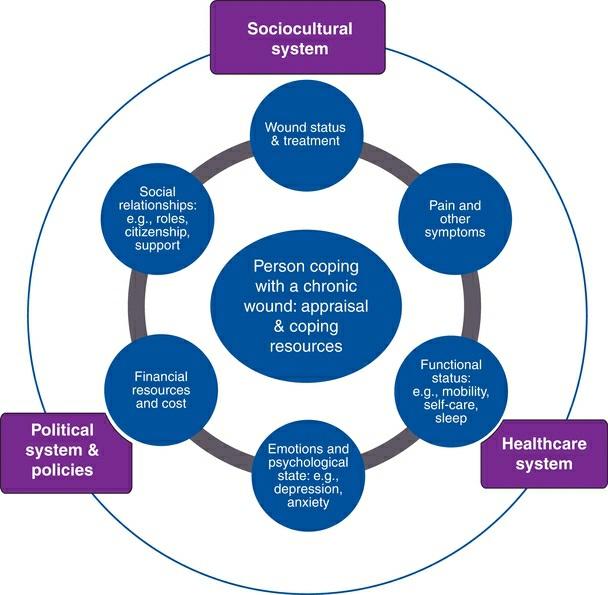
What is quality of life (QoL)? Generally, QoL is defined as a general perception of well-being by an individual. It is a subjective but dynamic construct that is influenced by emotions, beliefs and values, social context, and interpersonal relationships, which together account for its variability.3 Health-relatedqualityoflife (HRQoL) refers tothe sense ofwell-beingthat is specificallyaffected byhealthand illness alongwithother related efforts to promote health, manage disease, and prevent recurrence 4 According to the model proposed by Wilson and Cleary,5 multiple overlapping dimensions (e.g., biological and physiological factors, symptoms, functioning,general healthperceptions,andoverall QoL) areascribedtothe underlying structure of HRQoL. Each component may carry more
importanceatagiventimebasedonthecontextofhealthandillness.Among people with chronic wounds, there is very little dispute that their QoL is severelydiminished.6,7
QualityofLifeInstruments
There are a number of validated instruments to measure QoL. The generic instruments most commonly used are the Medical Outcomes Study Short Form 36 (SF-36) and adaptations, Research and Development 36-item Form, Sickness Impact Profile, Quality of Life Ladder, Barthel Index, the Nottingham Health Profile, and EuroQol EQ-5D Specific instruments that are used to evaluate HRQoLfor patients with diabetic foot ulcers include Cardiff Wound Impact Schedule Diabetes 39, Norfolk Quality of Life in Diabetes Peripheral Neuropathy Questionnaire, Neuro-QoL, the Manchester-Oxford FootQuestionnaire, and Diabetic FootUlcer Scale. For the leg ulcer patient population, the Hyland Leg and Foot Ulcer Questionnaire, Charing Cross Venous Leg Ulcer Questionnaire, and SheffieldPreference-basedVenousLegUlcer 5Dcouldbeconsidered.8,9
QualityofLifeand ChronicWounds
The three major chronic wound types are PrUs, diabetic foot ulcers, and venous leg ulcers. A PrU is an area of skin breakdown due to prolonged exposure to pressure, shear, and frictionleadingto tissue ischemia and cell death. PrUs remaina significantproblemacross the continuumofhealthcare services; prevalence estimates range from3.7% to over 27% dependingon the setting of care.10,11 PrUs are linked to a number of adverse patient outcomes includingprolonged hospital stay, decline inphysical functioning, and death. Infact, patients witha PrUhave beenreported to have a 3.6-fold increased riskofdyingwithin21 months, as compared withthose withouta PrU.12 Gorecki and colleagues12 reviewed and summarized 31 studies (10 qualitative studies and 21 quantitative studies) that examined issues related to QoL in people with PrUs. Common concerns and salient issues were synthesizedandcategorizedintothefollowingthemes:
1. Physical restrictions resulting in lifestyle changes and the need for environmental adaptations
2. Social isolationandrestrictedsocial life
3. Negative emotions and psychological responses to changes in body
imageandself-concept,andlossofindependence
4. PrUsymptoms: managementofpain,odor,andwoundexudate
5. HealthdeteriorationcausedbyPrU
6. Burdenonothers
7. Financial hardship
8. Wounddressings,treatment,andother interventions
9. Interactionwithhealthcareproviders
10. PerceptionofthecauseofPrU
11. Needfor educationaboutPrUdevelopment,treatment,andprevention
Diabetes is one of the leading chronic diseases worldwide.13 Persons with diabetes have a 25% lifetime risk of developing foot ulcers that precede over 80% of lower extremity amputations in this patient population.14,15 The 5-year mortalityrates have beenreportedtobe as high as 55% and 74% for new-onset diabetic foot ulcers and after amputation, respectively; the number of deaths surpasses that associated with prostate cancer, breast cancer, or Hodgkin’s disease.15 Individuals with unhealed diabetic foot ulcers share some unique challenges. Due to problems using the foot and ankle, patients with foot ulcers suffer from poor mobility limiting their ability to participate in physical activities.16 Mobility issues may also interfere with their performance at work resulting in loss of employment and financial hardship. Increased dependence can lead to caregiver stress and unresolved family tension. High levels of anxiety, depression, and psychological maladjustment may affect patients’ abilities toparticipateinself-managementandfootcare.16,17
It is estimated that approximately 1.5 to 3.0 per 1,000 adults in North America have active leg ulcers, and the prevalence continues to increase due to anagingpopulation, sedentarylifestyle, and the growingprevalence of obesity.18 Chronic leg ulcers involve an array of pathologies: 60% to 70% of all cases are related to venous disease, 10% due to arterial insufficiency, and 20% to 30% due to a combination of both.19 Although venous leg ulcers are more common in the elderly, 22% of individuals develop their first ulcer by age 40 and 13% before age 30, hindering their ability to work and participate in social activities.20,21 To understand the experience of living with leg ulceration, Briggs et al.22 reviewed findings from 12 qualitative studies. Results were synthesized into five categories, similar tothoseidentifiedaboveinindividualswithPrUs:
1. Physical effectsincludingpain,odor,itch,leakage,andinfection
2. Understandingandlearningtoprovidecarefor legulcers
3. Thebenefitsanddisappointmentinapatient–professional relationship
4. Social,physical,andfinancial costofalegulcer
5. Psychological impactanddifficultemotions(fear,anger,anxiety)
Intwoother reviews examiningthe impactofwounds onQoL,a total of 2223 and 24 studies24 were identified. Both qualitative and quantitative studies were included in the reviews. Pain was identified as the most common and disabling symptom leading to problems with mobility, sleep disorders, and loss of employment. Other symptoms associated with leg ulcers, including pruritus, swelling, discharge, and odor, are equally distressing but often overlooked by caregivers. In the studies, patients discussed the impact of leg ulcerations on their ability to work, carry out housework, performpersonal hygiene, and participate insocial/recreational activities Patients feel depressed, powerless, beingcontrolled bythe ulcer, and ashamed of their body. Efforts were taken to conceal the bandages/dressings with clothing or shoes; however, the latter were often considered less attractive thanwhatwould normallybe worn. Bothreviews identified the need to address patient engagement and patient knowledge deficitstopromotetreatmentadherence.23,24