www.delamed.org | www.djph.org Oral Health Volume 9 | Issue 1 April 2023 A publication of the Delaware Academy of Medicine / Delaware Public Health Association Public Health Delaware Journal of
Delaware Academy of Medicine OFFICERS
S. John Swanson, M.D. President Killingsworth
Lynn Jones, FACHE President-Elect
Professor Rita Landgraf (Co-Chair) Vice President
Jeffrey M. Cole, D.D.S., M.B.A. Treasurer
Stephen C. Eppes, M.D. Secretary
Omar A. Khan, M.D., M.H.S. (Co-Chair)
Immediate Past President
Timothy E. Gibbs, M.P.H. Executive Director, Ex-officio DIRECTORS
David M. Bercaw, M.D.
Lee P. Dresser, M.D.
Eric T. Johnson, M.D.
Erin M. Kavanaugh, M.D.
Joseph Kelly, D.D.S.
Joseph F. Kestner, Jr., M.D.
Brian W. Little, M.D., Ph.D.
Arun V. Malhotra, M.D.
Daniel J. Meara, M.D., D.M.D.
Ann Painter, M.S.N., R.N.
John P. Piper, M.D.
Charmaine Wright, M.D., M.S.H.P. EMERITUS
Robert B. Flinn, M.D.
Barry S. Kayne, D.D.S.
Delaware Public Health Association
Advisory Council:
Omar Khan, M.D., M.H.S. Chair
Timothy E. Gibbs, M.P.H. Executive Director
Louis E. Bartoshesky, M.D., M.P.H.
Gerard Gallucci, M.D., M.H.S.
Melissa K. Melby, Ph.D.
Mia A. Papas, Ph.D.
Karyl T. Rattay, M.D., M.S.
William J. Swiatek, M.A., A.I.C.P.
Delaware Journal of Public Health
Timothy E. Gibbs, M.P.H. Publisher
Omar Khan, M.D., M.H.S. Editor-in-Chief
Jeffrey M. Cole, D.D.S., M.B.A., F.A.G.D.,
Daniel J. Meara, M.S., M.D., D.M.D., M.H.C.D.S., F.A.C.S.
Guest Editors
Liz Healy, M.P.H.

Managing Editor
Kate Smith, M.D., M.P.H.
Copy Editor
Suzanne Fields
Image Director
Public
A publication of the Delaware Academy of Medicine / Delaware Public Health Association
3 | In This Issue
Omar A. Khan, M.D., M.H.S.
Timothy E. Gibbs, M.P.H.
4 | Guest Editor
Jeffrey M. Cole, D.D.S., M.B.A., F.A.G.D.
Daniel J. Meara, M.S., M.D., D.M.D., M.H.C.D.S., F.A.C.S.
6 | Toward Optimal Health for All: The American Dental Association Takes on Sugar and its Impact on Oral Health
George R. Shepley, D.D.S.
8 | A Public Health Update: The Oral Health of Delaware’s Kindergarten and Third Grade Children in 2022

Nicholas R. Conte Jr., D.M.D., M.B.A.
16 | Odontogenic Infections and a Pound of Prevention
Daniel J. Meara, M.S., M.D., D.M.D., M.H.C.D.S., F.A.C.S.
18 | More Premiums Spent on Patient Care? A Great Idea That Should Apply to Dental Insurance
Mark A. Vitale, D.M.D.
20 | The National Healthy People Initiative: History, Significance, and Embracing the 2030 Oral Health Objectives
Timothy L. Ricks, D.M.D., M.P.H., F.I.C.D., F.A.C.D., F.P.F.A.
26 | Human Papilloma Virus (HPV) and the Current State of Oropharyngeal Cancer Prevention and Treatment
Jacob P. Gribb, D.M.D
John H. Wheelock, D.D.S.
Etern S. Park, M.D., D.D.S.
30 | Global Health Matters January/February 2023
Fogarty International Center
42 | Update on Medication Related Osteonecrosis of the Jaws
Barry C. Boyd, D.M.D., M.D., F.A.C.S.
44 | Reconsidering Autonomy: Ethical Reflections from the Frontlines of IDD Dental Care
Andrew Swiatowicz, D.D.S., D.A.B.D.S.M., F.A.G.D.
Brandon Ambrosino, M.T.S.
50 | The Mouth is the Mirror to the Body: Oral-Systemic Health
Roopali Kulkarni, D.M.D., M.P.H.
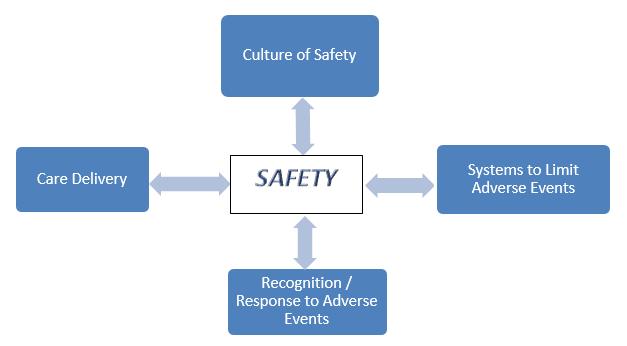
52 | Safety in the Dental Office
Louis K. Rafetto, D.M.D., M.Ed.
56 | Career and Technical Education: The Future of Delaware’s Healthcare Workforce
Jonathan S. Lee, B.A.
58 | Patient Safety at Forefront of OMS Anesthesia Delivery
Paul J. Schwartz, D.M.D.
60 | ORAL HEALTH LEXICON
62 | ORAL HEALTH RESOURCES
64 | Index of Advertisers
66 | Public Health Delaware Journal of Public Health Submission Guidelines
The Delaware Journal of Public Health (DJPH), first published in 2015, is the official journal of the Delaware Academy of Medicine / Delaware Public Health Association (Academy/DPHA).

Submissions: Contributions of original unpublished research, social science analysis, scholarly essays, critical commentaries, departments, and letters to the editor are welcome. Questions? Write ehealy@delamed.org or call Liz Healy at 302-733-3989
Advertising: Please write to ehealy@delamed.org or call 302-733-3989 for other advertising opportunities. Ask about special exhibit packages and sponsorships. Acceptance of advertising by the Journal does not imply endorsement of products.
Copyright © 2023 by the Delaware Academy of Medicine / Delaware Public Health Association. Opinions expressed by authors of articles summarized, quoted, or published in full in this journal represent only the opinions of the authors and do not necessarily reflect the official policy of the Delaware Public Health Association or the institution with which the author(s) is (are) affiliated, unless so specified.
Any report, article, or paper prepared by employees of the U.S. government as part of their official duties is, under Copyright Act, a “work of United States Government” for which copyright protection under Title 17 of the U.S. Code is not available. However, the journal format is copyrighted and pages June not be photocopied, except in limited quantities, or posted online, without permission of the Academy/DPHA. Copying done for other than personal or internal reference use-such as copying for general distribution, for advertising or promotional purposes, for creating new collective works, or for resale- without the expressed permission of the Academy/DPHA is prohibited. Requests for special permission should be sent to ehealy@delamed.org
ISSN 2639-6378
Health Delaware Journal of
April 2023 Volume 9 | Issue 1
Oral health is a critical component of overall health and well-being, and it is also an essential aspect of public health. The condition of a person’s oral health can—at minimum—affect their ability to speak, eat, and socialize comfortably. Oral health problems can also lead to pain, infection, and other serious health issues, such as cardiovascular disease, respiratory infections, and diabetes, through a variety of mechanisms still being elucidated. April is Oral Cancer Awareness Month, highlighting the importance of early detection and prevention of this deadly disease. Oral cancer can occur in any part of the mouth, including the tongue, gums, lips, and tonsils. It is essential to maintain good oral hygiene habits and receive regular dental check-ups to detect any signs of oral cancer early. Sugar is one of the leading causes of tooth decay, which is the most common chronic disease among children and adults. When sugar is consumed, it interacts with the bacteria in the mouth to produce acid, which can erode the enamel on the teeth and cause cavities. It is crucial to limit the intake of sugary foods and drinks to maintain good oral health.
In addition to cavities, odontogenic infections can also occur due to poor oral hygiene. These infections are caused by bacteria that enter the tooth or gum tissue, causing swelling, pain, and other symptoms. In severe cases, they can lead to systemic infections, which can be life-threatening. In a national effort to improve the health and well-being of All Americans, the Healthy People 2030 initiative includes goals to improve oral health by promoting good oral hygiene habits, increasing access to dental care, and reducing the incidence of oral diseases.
One oral health issue that has gained attention in recent years is Medication-Related Osteonecrosis of the Jaw (MRONJ). This condition can occur in individuals taking certain medications, such as bisphosphonates, which are commonly used to treat osteoporosis and other bone diseases. MRONJ can cause severe pain, swelling, and other complications, making it essential for individuals taking these medications to inform their dental care providers.
Individuals with Intellectual and Developmental Disabilities (IDD) also require specialized dental care. These individuals may have difficulty communicating or may have unique oral health needs due to their disabilities. It is essential to provide IDD individuals with the necessary dental care to maintain their oral health and overall well-being.
Safety in the dental office is critical for both patients and dental professionals. Dental offices must adhere to strict infection control protocols to prevent the spread of infectious diseases, and dental professionals must follow proper safety procedures when handling equipment and administering anesthesia. This is particularly relevant in the time of COVID-19 and related respiratory/droplet/airborne infections.
In this issue of the Delaware Journal of Public Health, guest editors Daniel J. Meara, MD, DMD, and Jeffrey Cole, DDS, MBA have brought together a diverse set of articles about these and other oral health, treatment, and workforce issues.

As always, we have included a resources section as well as a lexicon of terms. We welcome your feedback and thoughts!

IN THIS ISSUE
Timothy E. Gibbs, M.P.H Publisher, Delaware Journal of Public Health
Doi: 10.32481/djph.2023.04.001
Omar A. Khan, M.D., M.H.S. Editor-in-Chief, Delaware Journal of Public Health
3
Oral Health
Jeffrey M. Cole, D.D.S., M.B.A., F.A.G.D. Program Director, General Practice Dentistry Residency Program, ChristianaCare
Daniel J. Meara, M.S., M.D., D.M.D., M.H.C.D.S., F.A.C.S. Chair, Department of Oral and Maxillofacial Surgery & Hospital Dentistry, ChristianaCare
During the planning for this oral health edition of the Delaware Journal of Public Health, Dr. Cole recalled a story that was shared by a professor while he was a student at Georgetown University School of Dentistry. The oral surgeon spoke about his first day of deployment to a field hospital during the Vietnam War. His commanding officer, a physician and surgeon told him, “Put your thumb in your mouth and stretch out the rest of your fingers. If you can touch it, it’s yours. The rest is mine. Now get to work!” While this encounter showed a unique approach to defining scope of practice, it also illustrated the disintegration that often existed between medicine and dentistry; mutual coexistence instead of collaboration in the treatment of patients. Integration of medicine and dentistry stresses the importance of oral health as an essential part of overall health. For decades, oral health has been defined by national and international groups in dentistry and medicine as the absence of disease and associated symptoms of the oral cavity and oropharynx. The FDI World Dental Federation has developed a definition for oral health that is designed to bridge the gaps that sometimes exist between oral healthcare and overall health of the body. The FDI defines oral health in this way:
“Oral health is multifaceted and includes the ability to speak, smile, smell, taste, touch, chew, swallow, and convey an array of emotions through facial expressions with confidence and without pain, discomfort and disease of the craniofacial complex.”
They further identify attributes of oral health.
“Oral health is a fundamental component of health and physical and mental well-being. It exists along a continuum influenced by the values and attitudes of individuals and communities. Oral health reflects the physiological, social and psychological attributes that are essential to the quality of life. Oral health is influenced by an individual’s changing experiences, perceptions, expectations, and ability to adapt to circumstances.”
When strategically addressing the promotion of oral health, there is a lot of discussion around access to care, but less attention to two essential components of success in this area: utilization of services and oral health literacy. It is with this background that we hope this edition of the Delaware Journal of Public Health will inspire the multidisciplinary team of healthcare providers and advocates to continue to add to their comprehensive understanding of oral health, the challenges we face, and the opportunities we have in working together. You cannot have systemic health without oral health.
Doi: 10.32481/djph.2023.04.002
4 Delaware Journal of Public Health - April 2023
April 2023
The Nation’s Health headlines
Online-only news from The Nation’s Health newspaper

Stories of note include:
Child vaccination rates falter as misinformation, skepticism grow
Teddi Nicolaus
Local abortion supporters help patients navigate access as laws shift
Kim Krisberg
End to COVID-19 emergency policies could set back health
Mark Barna
Wastewater surveillance warrants further investment, development
Kim Krisberg
Q&A: New CDC office could help make inroads on work to combat disparities in US rural health

Maaisha Osman
Belt, buckle & boost: Keep your kids safe in the car
Teddi Nicolaus
Vaccine uptake gets a boost when people know others are on board
Maaisha Osman
https://www.thenationshealth.org/
HIGHLIGHTS FROM The NATION’S HEALTH A PUBLICATION OF THE AMERICAN PUBLIC HEALTH ASSOCIATION 5
Toward Optimal Health for All: The American Dental Association Takes on Sugar and its Impact on Oral Health
George R. Shepley, D.D.S.
President, American Dental Association; General Dentist, Private Practice
For 164 years, the American Dental Association (ADA) has been leading the national discourse on oral health. From advocating for critical legislation to improve health equity to driving the evidence-based insights that advance the profession, the ADA’s endeavors are propelled by a fundamental commitment to making people healthy.
This commitment bears that, as a community of essential healthcare providers, the ADA has an imperative to be champions for overall wellbeing and to take a stand on issues that could impede the improvement of public health. It’s an imperative we’ve lived up to.
Consider, for example, the stand the Association has taken on smoking and tobacco products, whose deleterious oral and systemic health effects are well known. Among many actions in recent years, the ADA has supported the regulation of e-cigarettes and synthetic nicotine products.
The Association also continues to guide clinicians in offering smoking cessation advice to their patients. A 2022 study in the Journal of the American Dental Association found that dentists’ chairside counsel can be influential—smoking cessation advice from a dental team member is associated with an 18 percent increase in the number of times a patient tries to quit smoking.1
The study is a nod to the great potential for dentistry (both as a professional community and as individuals) to be active partners, alongside medical colleagues, in helping patients achieve whole-body health. Oral health is integral to overall health— research reflects the relationship between oral disease such as periodontal disease and systemic conditions that include type 2 diabetes2 and cardiovascular disease.3
Dental-medical integration in primary care is gaining prominence, and increasingly more dental students are being trained to have an innate sense of their contributions to a patient’s overall wellbeing. In addition to seeing the importance of interdisciplinary collaboration, emerging professionals are understanding their role in not solely treating disease, but in actively promoting health, too.
Although dentistry is our area of expertise, the concern of whole-body health remains a key area of focus for the ADA as we meet our constitutional objective to encourage public health.
In 2023, the Association has a renewed opportunity to address a public health issue whose impact dentists see directly in their work—from caries to periodontitis, to the systemic conditions that have oral manifestations, like inflammation and diabetes. A common denominator the Association wants to address is the overconsumption of sugar.
The effect of sugar on a person’s oral health is hardly a new frontier in dentistry. For many children, early lessons on caring for their teeth include brushing, flossing, and avoiding candy to avoid cavities. Yet, in patients of all ages, the overconsumption of sugar is continually associated with diseases that go well beyond the mouth. But the mouth is often where it starts, with the excessive intake of sugary beverages, sweet snacks, and processed foods.
In a 2012 article for Nature, authors Robert H. Lustig, Laura A. Schmidt, and Claire D. Brindis write, “Evolutionarily, sugar was available to our ancestors as fruit for only a few months a year (at harvest time), or as honey, which was guarded by bees. But in recent years, sugar has been added to nearly all processed foods, limiting consumer choice. Nature made sugar hard to get; man made it easy.”4
Excessive sugar intake can also be tied to foods that are specifically marketed to consumers as good for them. Some yogurts, for example, can have as many as 32 grams of sugar per serving. For perspective, there are 39 grams of added sugar in a 12-ounce can of Coke.
In turn, the American Heart Association (AHA) reports that the average American consumes 77 grams of sugar a day5—well beyond the U.S. Food and Drug Administration’s recommendation that people over age three have no more than 50 grams of added sugars a day.6 The AHA’s recommendation is more conservative, suggesting that the daily intake of added sugars should be limited to 36 grams for men and 25 grams for women.
With its policies on diet and nutrition, the ADA, too, acknowledges the benefit of healthy diets that avoid added sugars as a step toward optimal oral health. We also recognize the value of professional education, public awareness, patient information, and continued research on nutrition’s role in oral and overall health.
This year, the ADA is taking its work on diet and nutrition further with the establishment of the Presidential Task Force on Sugar, Nutrition, and Diet. Current members represent the ADA Board of Trustees, Council on Advocacy for Access and Prevention, Council on Governmental Affairs, Council on Scientific Affairs, along with general ADA membership. The group also includes experts on dietetics and endocrinology.
The Task Force was formed to review existing ADA policies on sugar, nutrition, and diet, and propose changes to expand the ADA’s involvement with other healthcare stakeholders and facilitate dental-medical collaboration on the topic.
Doi: 10.32481/djph.2023.04.003
6 Delaware Journal of Public Health - April 2023
Last fall, the Biden-Harris administration hosted the White House Conference on Hunger, Nutrition, and Health—the first meeting of its kind in 50 years. As outlined during the conference, key actions of the national strategy include investing in creative research approaches regarding the relationship between nutrition, disease, and comprehensive health; advancing research on the prevention and treatment of diet-related diseases; and strengthening and diversifying the nutrition workforce.
The ADA Task Force’s review of the White House strategy will help shape its recommended revisions to current ADA policy with the goal of further driving oral health, nutrition, and improved health outcomes.
Efforts like these are positioning the ADA to not only spearhead the national discourse on oral health, but to become a respected leader in shaping healthcare at large.
Just as vital as our collective efforts are the thousands of clinicians who have the individual power to help their communities—one visit and one patient at a time. This, too, is where we improve population health— by arming our patients with the knowledge that enables them to make informed choices.
We should remember the old adage: knowledge is power. Both knowledge and power can create a sense of agency and self-advocacy for patients. And a sense that—along with their dentist, physician, and other healthcare providers—they are a member of their own healthcare team. And that their decisions, whether to try to quit smoking or to be more aware of their sugar intake, can bring them one step closer to being their healthiest selves.
Together, with the large-scale work of the ADA and other organizations, each step brings all of us closer to healthier communities, a healthier nation, and a healthier world.
The very publication of the Delaware Journal of Public Health helps to make this vision possible, with the platform it provides to inform its diverse readership on public health research, policy, practice, and education per its mission.
I’d like to thank the following individuals for providing this venue to highlight oral health’s vital role in public health:
• Guest Editor Dr. Jeffrey Cole, who is a former ADA president and currently the program director of the General Practice Dentistry Residency Program at Christiana Hospital in Wilmington.
• Guest Editor Dr. Daniel Meara, current chair of the Commission for Continuing Education Provider Education and chair of Christiana Hospital’s Department of Oral and Maxillofacial Surgery and Hospital Dentistry.
• Dr. Brian McAllister, current chair of the National Commission on Recognition of Dental Specialties and Certifying Boards and attending staff for the General Practice Dentistry Residency Program at Christiana Hospital.
Thank you for being among the Delaware dentists who are driving public health forward as clinicians, educators, and leaders.
Dr. Shepley may be contacted at shepleyg@ada.org
REFERENCES
1. Yadav, S., Lee, M., & Hong, Y.-R. (2022, January). Smokingcessation advice from dental care professionals and its association with smoking status: Analysis of National Health and Nutrition Examination Survey 2015-2018. J Am Dental Assoc, 153(1), 15–22.
https://doi.org/10.1016/j.adaj.2021.07.009
2 Wu, C. Z., Yuan, Y. H., Liu, H. H., Li, S. S., Zhang, B. W., Chen, W., . . . Li, L. J. (2020, July 11). Epidemiologic relationship between periodontitis and type 2 diabetes mellitus. BMC Oral Health, 20(1), 204.
https://doi.org/10.1186/s12903-020-01180-w
3. Zardawi, F., Gul, S., Abdulkareem, A., Sha, A., & Yates, J. (2021, January 15). Association between periodontal disease and atherosclerotic cardiovascular diseases: Revisited. Frontiers in Cardiovascular Medicine, 7, 625579
https://doi.org/10.3389/fcvm.2020.625579
4 Lustig, R. H., Schmidt, L. A., & Brindis, C. D. (2012, February 1). Public health: The toxic truth about sugar. Nature, 482(7383), 27–29.
https://doi.org/10.1038/482027a
5. American Heart Association. (2022, Jun). How much sugar is too much?
https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/sugar/ how-much-sugar-is-too-much
6. U.S. Food and Drug Administration. (2022, Feb). Added sugars on the new nutrition facts label.
https://www.fda.gov/food/new-nutrition-facts-label/added-sugars-newnutrition-facts-label
7
A Public Health Update: The Oral Health of Delaware’s Kindergarten and Third Grade Children in 2022
Nicholas R. Conte Jr., D.M.D., M.B.A.
Dental Director, Bureau of Oral Health and Dental Services, Division of Public Health, Delaware Department of Health and Social Services; Prosthodontist, Private Practice.
INTRODUCTION
Good oral health means more than healthy teeth and gums. Oral diseases, such as tooth decay and gum disease, are multifactorial in causation and affect general health status. Oral health problems usually involve significant social and cultural factors that require many resources and partners to implement prevention and treatment services.1 Social determinants of health include income, education, occupation, geographic implications, and cultural beliefs.2 Access to oral health care is affected by similar social, cultural, economic, geographic, and structural factors, but more so by the separation of the oral health from the health care system. People and communities with inadequate access to oral health care experience notable social and economic burdens.3 Tooth decay is a serious public health problem that can affect a child’s overall health and well-being. It can lead to pain and disfigurement, low self-esteem, nutritional problems, and lost school days. Children with oral health problems are three times more likely to miss school due to dental pain, and absences caused by pain are associated with poorer school performance.4
The National Oral Health Surveillance System (NOHSS) is a collaborative effort between the Centers for Disease Control and Prevention (CDC), Division of Oral Health and the Association of State and Territorial Dental Directors (ASTDD). NOHSS monitors the burden of oral disease, use of the oral health care delivery system, and the status of community water fluoridation on national and state levels. NOHSS captures oral health surveillance indicators based on data sources and surveillance capacity available to most states.
The Council of State and Territorial Epidemiologists (CSTE) and the National Association of Chronic Disease Directors (NACDD) developed a framework for chronic disease surveillance indicators, including oral health indicators for adult and child populations.
Children’s oral health data from NOHSS include indicators for caries experience, untreated tooth decay, and dental sealants. More specifically, these indicators measure the percentage of third grade students with caries experience, the percentage of third grade students with untreated tooth decay, and the percentage of third grade students with dental sealants on at least one permanent molar tooth.5
Recognizing the need for community level oral health status and dental care access data, ASTDD developed the Basic Screening Survey (BSS). The primary purpose of the BSS is to provide a framework to collect oral health data efficiently and inexpensively in a consistent manner. By collecting data in a standardized manner, communities and states can compare their data with data collected by other organizations or agencies using the same methodology; and/or data from previous surveys.
The BSS model has two basic components: direct observation of a child’s oral cavity and questions asked of, or about, the child being screened.6
To assess the current oral health status of Delaware’s elementary school children, the Bureau of Oral Health and Dental Services (BOHDS) within the Delaware Department of Health and Social Services, Division of Public Health coordinated an inaugural statewide oral health survey of kindergarten and third grade children attending Delaware’s public schools. The survey was conducted during the 2021-2022 school year among kindergarten and third grade children receiving a BOHDS dental screening at 40 schools. BOHDS received 4,236 oral health surveys and performed in-person screenings on 1,601 kindergarten and 1,517 third grade children. The kindergarten screening survey had not been completed previously in Delaware and the previous third grade BSS was completed in 2012. These two cohorts were selected because third grade oral health is a national comparison point used to assess the health of school age children, as there is a good mixture of primary and permanent dentition present. The kindergarten group allows for baseline assessment of oral health upon entry into the school system.
DATA SOURCE AND METHODS
BOHDS employees and Delaware state employees conducted the survey, screening children in kindergarten and third grade from a representative sample of Delaware’s non-virtual public schools. The preliminary planning phase for the basic screening survey started more than six months prior to the in-school screenings taking place by collaborating with the Delaware Department of Education (DOE) to gain approval for the survey and to determine the procedure for distribution of the forms throughout the state, as well as obtaining individual consent to participate from the families of the students. To determine the schools included in the BSS, technical assistance was provided by an ASTDD consultant. Assuring the sampling scheme is correct is essential to submit the data for inclusion into the U.S. Oral Health Surveillance System, NOHSS.
To assure representation by geographic region and socioeconomic status, the sampling frame was ordered by county, then by the percentage of students in each school identified by DOE as being low-income and eligible for Temporary Assistance for Needy Families or the Supplemental Nutrition Assistance Program (SNAP). If a school with only third grade was selected, the appropriate kindergarten feeder school7 within the district was added to the sample. A systematic probability proportional to size sampling scheme was used to select a sample of 25 third grade schools. As four of the selected third grade schools did not have kindergarten students, the appropriate kindergarten feeder schools were added to
Doi: 10.32481/djph.2023.04.004
8 Delaware Journal of Public Health - April 2023
the sample for a total of 28 schools representing 25 sampling intervals. Fifteen additional schools volunteered to participate, and their data were included in the results.
After developing data collection forms and the survey letters, the schools were contacted and arrangements were made for an in-person screening date, allowing ample time for the forms to be distributed and returned to BOHDS.
All the screeners were trained and calibrated by a representative from ASTDD and are actively licensed as either a dentist or a dental hygienist in the State of Delaware. The following definitions were used by the screeners to consistently categorize observations:
Decay experience refers to a child having tooth decay in the primary (baby) and/or permanent (adult) teeth in his or her lifetime. Decay experience can be past (fillings, crowns, or teeth that have been extracted because of decay) or present (untreated tooth decay or cavities) and refers to having untreated decay or a dental filling, crown, or other type of restorative dental material present at the time of the screening.
If left untreated, tooth decay can have serious consequences, including needless pain and suffering, difficulty chewing (which compromises children’s nutrition and can slow their development), difficulty speaking, and lost days in school. Untreated decay is used to describe dental caries or tooth decay that have not received appropriate treatment.
Dental sealants are plastic-like coatings applied to the chewing surfaces of back teeth. The applied sealant resin bonds into the grooves of teeth to form a protective physical barrier. Most tooth decay in children occurs on these surfaces. Sealants protect the chewing surfaces from tooth decay by keeping germs and food particles out of these grooves. Screeners utilized visual inspection to identify the presence of a dental sealant.
Each child who completed an in school, in-person screening received an oral health kit that included a toothbrush and toothpaste, age-appropriate dental education, oral health literature, and a dental resource guide. A copy of the screening result was sent home for the student’s parent or guardian to review. For students where an urgent need was identified, BOHDS conducted case management and connected the family to a provider to address their oral health needs.
The information was collected using both the returned paper and electronic survey forms and the in-person screening. It included: grade, age, race/ethnicity, presence of untreated decay, presence of treated decay, presence of dental sealants on the permanent first molar teeth, and urgency of need for dental care. BOHDS used the BSS clinical indicator definitions and data collection protocols authored by ASTDD, titled Basic screening surveys: An approach to monitoring community oral health. 6 The forms included an optional parent questionnaire which collected information on dental insurance, time since last dental visit, whether the child had a toothache or other dental problems in
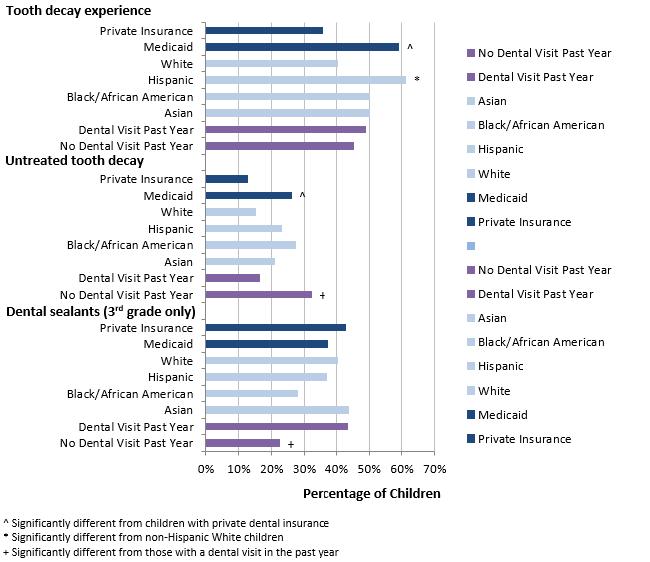
Figure 1. Prevalence of Tooth Decay Experience and Untreated Tooth Decay, and Dental Sealants Among Kindergarten and Third Grade Children by Type of Dental Insurance, Race/Ethnicity, and Dental Visit in the Past Year, Delaware, 2021-2022
9
Table 1. Prevalence of Tooth Decay Experience and Untreated Tooth Decay in the Primary and Permanent Teeth Among Kindergarten and Third Grade Children Combined by Selected Characteristics, Delaware, 2021-2022
Lower CL = Lower 95% confidence limit, Upper CL = Upper 95% confidence limit
* Significantly different than reference (p<0.05)
the last year, and whether the child needed dental care during the last year but was unable to obtain the needed care. All statistical analyses were performed using the complex survey procedures within SAS (Version 9.4; SAS Institute Inc., Cary, NC). Sample weights were used to produce population estimates based on selection probabilities.9
RESULTS
There were 8,847 kindergarten and 3rd grade children enrolled in the participating schools for the 2020-2021 academic year. Three thousand one hundred and eighteen received a dental screening for a response rate of 35%. The following is a summary of the results of the 3,118 in-person screenings completed (figure 1, table 1). Forty-five percent of Delaware’s kindergarten children have at least one tooth with decay experience. Twenty-two percent of Delaware’s kindergarten children have untreated tooth decay. Since permanent molars generally appear in the mouth at six years of age, information on protective dental sealants in kindergarten was not included.
Regarding third graders, 53% of Delaware’s third grade children have at least one tooth with decay experience and 19% of Delaware’s third grade children have untreated tooth decay. Only 38% of Delaware’s third grade children were found to have protective dental sealants in present (table 2).
Delaware children with Medicaid have a significantly higher prevalence of decay experience and untreated tooth decay than those with private dental insurance. Over 60% of surveyed Hispanic/Latinx children had tooth decay experience compared to over 40% of surveyed non-Hispanic White children. Non-Hispanic Black and non-Hispanic Asian children had over 50% tooth decay experience compared to 40% for non-Hispanic White children. The prevalence of untreated tooth decay is significantly higher among children without a dental visit in the past year (over 30%) compared to those with a dental visit (over 20%). Among third grade children, those without a dental visit in the past year are significantly less likely to have protective dental sealants.9
Characteristic Decay Experience Untreated Decay Survey Total Percent Yes Lower CL Upper CL # With Data Percent Yes Lower CL Upper CL ALL CHILDREN 3,118 48.3 41.4 55.2 3,118 20.4 13.8 27.0 Race/Ethnicity Asian 175 50.2 39.8 60.7 175 20.8 8.1 33.6 Black/African American 603 50.0 38.5 61.6 603 27.3 16.8 37.8 Hispanic/Latinx 632 61.2* 56.4 65.9 632 23.1 17.6 28.7 White (reference) 1,450 40.4 34.1 46.7 1,450 15.0 10.5 19.5 County Kent 763 47.8 42.3 53.3 763 19.6 14.6 24.6 New Castle 1,392 47.8 36.0 59.5 1,392 20.6 9.1 32.0 Sussex 963 50.7 43.5 57.9 963 21.0 17.2 24.9 Dental Insurance Private Insurance (reference) 1,475 35.5 27.8 43.2 1,475 12.8 8.6 16.9 Medicaid 1,221 59.1* 52.2 65.9 1,221 26.0* 17.3 34.7 Dental Visit in Last Year No 673 45.2 40.0 50.5 673 32.2* 25.6 38.8 Yes (reference) 2,402 49.0 41.2 56.7 2,402 16.4 10.1 22.8 Toothache/Cavities in Last Year No (reference) 2,397 38.0 32.7 43.3 2,397 12.9 9.1 16.7 Yes 608 79.8* 71.4 88.1 608 40.1* 29.3 50.9 Needed Care but Couldn’t Obtain No (reference) 2,715 45.9 38.9 52.8 2,715 16.6 10.7 22.6 Yes 300 64.6* 58.3 70.9 300 43.3* 36.3 50.2
10 Delaware Journal of Public Health - April 2023
Lower CL = Lower 95% confidence limit, Upper CL = Upper 95% confidence limit
* Significantly different than reference (p<0.05)
DISCUSSION
The results of this BSS demonstrate that Delaware’s third graders have experienced less decay than the national average yet are comparable to the national average for untreated decay. Fifty-three percent of Delaware’s third grade children have at least one tooth with decay experience, which is lower than the national average of 60%. It was found that 19% of Delaware’s third grade children have untreated tooth decay, similar to the national average of 20%; and only 38% of Delaware’s third grade children have protective dental sealants, lower than the national average of 42%.
The decay experience and untreated decay rates for kindergarteners are higher than national averages. Forty-five percent of Delaware’s kindergarten children have at least one tooth with decay experience, higher than the national average of 42%. Twenty-two percent of Delaware’s kindergarten children have untreated tooth decay, higher than the national average of 15%.
More importantly, the results indicate that significant oral health inequities exist in Delaware, with tooth decay being more common in children from low-income households and among Hispanic children
LIMITATIONS
It is important to understand the intent and limitations of a screening survey. A dental screening is not a thorough clinical examination and does not involve making a clinical diagnosis resulting in a treatment plan. A screening is intended to identify definitive dental or oral lesions and is conducted by dentists, dental hygienists, or other appropriate health care workers, in accordance with applicable state law. The information gathered through a screening survey is at a level consistent with monitoring the national health objectives found in Healthy People 2030, the United States Public Health Service’s 10-year agenda for improving the nation’s health.11 Surveys are cross sectional (looking at a population at a point in time) and descriptive (intended for determining estimates of oral health status for a defined population).6
It should be noted that the Delaware survey was conducted during the Coronavirus 2019 (COVID-19) pandemic and the lower prevalence of dental sealants may be partially due to limited access to preventive dental services at that time.
Characteristic Dental Sealants on Permanent Molars Survey Total Percent Yes Lower CL Upper CL ALL THIRD GRADE CHILDREN 1,508 37.5 26.2 48.8 Race/Ethnicity Asian 88 43.7 22.9 64.6 Black/African American 289 27.8 13.3 42.2 Hispanic/Latinx 307 37.1 26.1 48.2 White (reference) 702 40.5 27.5 53.4 County Kent 344 28.4 14.9 41.9 New Castle 703 47.0 28.3 65.6 Sussex 461 22.0 7.8 36.2 Dental Insurance Private Insurance (reference) 757 42.8 27.9 57.6 Medicaid 534 37.3 26.8 47.8 Dental Visit in Last Year No 300 22.5* 11.4 33.6 Yes (reference) 1,179 43.5 32.2 54.7 Toothache/Cavities in Last Year No (reference) 1,167 39.7 28.3 51.1 Yes 285 39.6 27.7 51.4 Needed Care but Couldn’t Obtain No (reference) 1,310 41.0 30.0 52.1 Yes 143 32.0 18.0 46.0
11
Table 2. Prevalence of Dental Sealants on Permanent Molar Teeth Among Third Grade Children by Selected Characteristics, Delaware, 2021-2022
DENTAL CARE IN DELAWARE
More than two hundred families responded to the questionnaire that they had no dental insurance or were unsure of having any benefit. This information is important to consider as many individuals need assistance with navigating through healthcare benefits, understanding eligibility and determining potential of out-of-pocket costs before obtaining care.
Dental case management is one method that BOHDS has utilized in this effort to address these inequities and improve the overall oral health of these and other high-risk populations. Increasing access to care by the removal of barriers to care delivery ultimately results in connecting families to providers who match their preferences, thus establishing a dental home.13
To facilitate accessibility of a dental home, it is necessary to develop trust. Understanding a family’s preferences, cultural beliefs, and ability to navigate the health care system is as critical as delivering care. For families to follow through with oral and dental health care, providers must educate them on the importance of preventive practices. Improving health literacy is needed to understand the connection between oral and systemic health. Offering appointment assistance regarding potential transportation options, provider schedules, and after care proves valuable to establishing a meaningful connection. Lastly, families can make well-informed decisions and be comfortable in their selection of an oral health provider when they receive administrative assistance to help determine benefit eligibility, comply with referrals, and pay responsibly.
To further address care needs, BOHDS developed the First Smile Delaware Dental Resource Guide in 2020. The resource guide is distributed during all community outreach events and public engagement and is available both electronically and in print.14 It is designed to assist the public with finding a dentist that is right for them individually. The guide helps patients understand which dental benefits are covered, how to apply for dental insurance, and how to access oral health services in Delaware. BOHDS continually monitors the effectiveness of the resource guide and its content through consumer and dental provider feedback and updates the document annually. BOHDS plans to conduct a phone survey in the fourth quarter of 2023 with providers that have accepted referrals to assess their overall experiences, garner feedback on what has been working well and identify opportunities for improvement.
NEXT STEPS
BOHDS expects the next BSS to be conducted for kindergarteners and third graders during the 2026-2027 academic year. While the BSS kindergarten and third grade screening surveys have a periodicity schedule of every five years, BOHDS’ daily activity is similar in nature. BOHDS engages in community outreach activities and an in-school screening program throughout the year. The Delaware Smile Check Program is a school-based screening program that provides dental education and preventive services within the school, and includes dental case management for any family that identifies that they are without a dental home. If an urgent or emergent situation is identified during a screening visit that requires treatment, a BOHDS staff member will reach out to the parent or guardian and try to connect the child to a provider within 48 hours. Similar to the BSS, any child who is seen as part of the Delaware Smile Check Program receives customized dental education and oral health instruction in addition to a toothbrush, toothpaste, and a dental resource guide. A copy of the screening result is sent home with the child
for the guardian’s review and the school nurse receives a copy for the student’s school health record. BOHDS will look to evaluate the effectiveness of the case management activities at the end of 2023 to determine what percentage of families were connected to a dental provider and if this has had impact on the burden of oral disease in the state. Since its inception in 2016, the Delaware Smile Check Program has provided services to more than 15,000 children throughout the state.
PUBLIC HEALTH IMPLICATIONS
Tooth decay is preventable. Connecting children to a permanent dental home will work towards lowering the incidence of dental caries and the prevalence of untreated decay. To help lower the burden of childhood oral disease, BOHDS will continue to coordinate with Federally Qualified Health Centers and private dental providers across the state to link families in need of a provider to a dental home. When Delaware reaches the public health goal of lowering the burden of oral disease, our residents will experience an improved quality of life.
Dr. Conte may be contacted at Nicholas.conte@delaware.gov
REFERENCES
1. Centers for Disease Control and Prevention. (2021, Feb). Disparities in oral health. https://www.cdc.gov/oralhealth/oral_health_disparities/index.htm
2. Fédération Dentaire Internationale World Dental Federation. (2015). The challenge of oral disease – A call for global action. The Oral Health Atlas. 2nd ed. Geneva.
3. Tiwari, T. & Franstve-Hawley, J. (2021, Sep 30). Addressing oral health of low-income populations—A call to action. Journal of the American Medical Association Network Open, 4(9), e2125263. Doi: 10.1001.jamanetworkopen.2021.25263
4. Jackson, S.L., Vann, W.F., Kotch, J.B., Pahel, B.T., & Lee, J.Y. (2011, Oct). Impact of poor oral health on children’s school attendance and performance. Am J Public Health, 101(10), 1900-1906. Doi: 10.2105/AJPH.2010.200915
5. Centers for Disease Control and Prevention. (2019, May). Oral health data. Child indicators. https://www.cdc.gov/oralhealthdata/overview/childindicators/index.html
6. Association of State and Territorial Dental Directors. (2017, Jul). Basic screening surveys: An approach to monitoring community oral health head start and school children. July 2017. https://www.astdd.org/docs/bss-childrens-manual-july-2017.pdf
7. Law Insider. (2023). Feeder pattern. Law Insider Inc. https://www.lawinsider.com/dictionary/feeder-pattern
9. Delaware Bureau of Oral Health and Dental Services. (2022, Feb). Delaware oral health and dental services data brief - the oral health of Delaware’s kindergarten and third grade children 2022. https://www.dhss.delaware.gov/dhss/dph/hsm/ohphome.html
11. States Department of Health and Human Services. (n.d.). Healthy People 2030. https://health.gov/healthypeople
13. Greenberg, B.J., Kumar, J.V., & Stevenson, H. (2008, Aug). Dental case management increasing access to oral health care for families and children with low incomes. Journal of the American Dental Association, 139(8), 1114-1121. Doi: 10.14219/jada.archive.2008.0314
14. Delaware Department of Health and Social Services. (n.d.). Dental resource guide. https://www.dhss.delaware.gov/dhss/dph/hsm/files/dentalresourceguide.pdf
12 Delaware Journal of Public Health - April 2023
Financial Aid
2023 Workforce Initiative
Application open until funds are depleted
Eligibility:
• U.S. Citizen or permanent resident (I-151 or I-551 card)
• One year of residency in the State of Delaware
• Enrolled in an approved degree-granting program or certificate in Nursing, Medical Assistant, Dental Assistant, Physician Assistant, Behavioral Health or Allied Health

Requirements:
• Completed online application
• Online self-certification form
• Copy of most recent signed Delaware tax return (personal and/or parents, if dependent)
• Proof of Delaware residency (driver’s license, vehicle registration, voter’s registration card)

• Letter of Acceptance
• Promissory Note and Loan Agreement
Funding:
• Funded by the Delaware American Rescue Plan Act (ARPA) for shortages in the healthcare field due to the COVID-19 pandemic
• Loan amount averages between $2,500 to $15,000 annually
Repayment:
• Interest-free while enrolled in an approved degree program
• Repayment begins 6 months after graduation depending on the length of the degree program
• Repayment plan options will depend on the degree type
- Certification programs: 1 to 3-year plans
- Associates, Bachelors, or Masters Degree programs: 5 to 7-year plans
- Doctoral (Ph.D.) programs: 7 to 11-year plans
Note: Terms of repayment of loans are covered through the promissory note and loan agreement
To apply, visit: https://delamed.org/student-financial-aid/
Contact: Giselle Bermudez, MS, Student Financial Aid Coordinator
email: gbermudez@delamed.org
phone: 302-733-1122
This program is supported by State and Local Fiscal Recovery Funds thru the Department of Treasury and State of Delaware [SLFRP0139].
13
All concussions are brain injuries
A concussion is caused by a bump, blow, or jolt to the head or body that causes the head and brain to move quickly back and forth. During Brain Injury Awareness Month, the Delaware Coalition for Injury Prevention’s Brain and Spinal Cord Injury Team wants Delawareans to know that all concussions are brain injuries.
According to the Centers for Disease Control and Prevention (CDC), concussion symptoms are headache or “pressure” in the head; nausea or vomiting; and dizziness or balance problems. The injured individual may have blurred or double vision, light or noise sensitivity, ringing in ears, confusion, and difficulty concentrating or remembering The person may feel slowed down, tired, sad, irritable, and be more emotional or not feel right. Toddlers and infants will not stop crying, cannot be consoled, and will not nurse or eat.



Someone with a concussion may appear dazed or lose consciousness, though that does not always occur. The injured person may have slurred speech, move clumsily, appear off balance, and be slow to answer questions. They could exhibit a change in behavior, mood, or personality, including irritability or aggressiveness; and be more tired than usual. A change in sleep pattern could occur.
If you have a concussion, stop your activity immediately and get evaluated by a medical provider. Do not try to judge the severity yourself. Delaware law says all children must be evaluated prior to returning to any sporting activity.
For more information and training, visit the CDC’s Headsup website: https://www.cdc.gov/headsup/ Another resource is the State Council for Persons with Disability (https://scpd.delaware.gov/); access the Brain Injury Fund Assistance.
Brain Injury Association of Delaware announces virtual conference series


The Brain Injury Association of Delaware (BIADE) is hosting its 2023 Annual Conference in March through a virtual webinar series. The series will be held every Thursday in March from 6:00 p.m. to 7:30 p.m. and are free to survivors and caregivers.
BIADE says the sessions share information on new advancements in care, service, and program options for survivors, and teach attendees how to advocate for traumatic brain injury survivors.
The webinar schedule is:
Session I: March 2, 2023, 6:00 p.m.
Following the Data of Brain Injury in Delaware
Dr. Gurpreet Kaur, MD, MBA, Delaware Health Information Network (DHIN) and Dee Rivard, State Council for Persons with Disabilities
Session II: March 9, 2023, 6:00 p.m.
Cognitive-Communication Disorders Following Traumatic Brain Injury. Maggie Kalinec, Defy Therapy Service
Session III: March 16, 2023, 6:00 p.m.
Gaps in Service for Brain Injury Survivors Dr. Terry Harrison-Goldman, Nemours Children’s Health
Session IV: March 23, 2023, 6:00 p.m.
Brain Injury and Seizures - What We Know And What We Don’t Dr. John Cheng, Christiana Care Health System
Session V: March 30, 2023, 6:00 p.m.
Traumatic Brain Injury: Not Just One Moment in Time - Long-Term Health Effects after TBI

Dr. Dawn R. Tartaglione, DO, Bayhealth Neurosurgery.
Register at www.biade.org
Watching all five webinars can earn 5.0 CEU credits for Speech Language Pathologist, Occupational Therapy, and Physical Therapy, plus Nurse Practitioners and Nursing (pending application).
For more information, contact BIADE at 302-3462083.
14 Delaware Journal of Public Health - April 2023
of Public Health March 202
From the Delaware Division
Learn about chronic kidney disease during National Kidney Month
Chronic kidney disease (CKD), also called Chronic Renal failure, is a condition where the kidneys gradually lose function over time, eventually leading to complete kidney failure. CKD is caused by a variety of factors, including high blood pressure, diabetes, and certain inherited disorders. Symptoms of CKD may not appear until the disease has progressed significantly, and may include fatigue, swelling, and changes in urination patterns. CKD can be managed with lifestyle changes and medical treatment, but in advanced stages, a kidney transplant or dialysis may be necessary.
Prevent CKD with these tips from the Centers for Disease Control and Prevention (CDC):
• Prevent high blood pressure by self-monitoring and following your treatment plan.
• Schedule regular check-ups with your health care provider to monitor kidney function and detect diseases early when they are more treatable. This is important for individuals with diabetes, who are at a higher risk for developing CKD.

• Follow a healthy diet that is low in salt, sugar, and unhealthy fats.
• Get regular physical activity.
• Avoid harmful substances such as tobacco, excessive alcohol, and certain medications.
• Manage other health conditions such as heart disease and liver disease
Call a doctor immediately if you have chest pain or shortness of breath. See a provider for changes in urination patterns, including increased frequency, decreased volume, or the appearance of blood in the urine. Other symptoms of impaired kidney function are swelling in the face, legs, or feet; anemia; nausea or vomiting; and itchy skin
The Division of Public Health (DPH) offers free sixweek self-management workshops to adults who have or care for someone living with a chronic condition. For more information, visit Healthy Delaware or call 302-208-9097.
Delaware residents diagnosed with End Stage Renal Disease can apply to the Chronic Renal Disease Program for financial assistance. Reach the Division of Medicaid & Medical Assistance online, call the Delaware Help Line at 211, or call 302-424-7180.
Seven public libraries offer kiosks for telehealth appointments and more Delawareans can access telehealth, legal support, and employment assistance for free at seven public libraries. Private, soundproof kiosks are available at the Woodlawn, Route 9, Georgetown, Laurel, Lewes, Milton, and Milford public libraries through a Delaware Libraries pilot program.
Each kiosk offers high-speed Internet, an iPad, and a hand sanitizer station. With the tablets, Delawareans can Zoom, Skype, and use other videoconferencing software to hold virtual appointments with health care providers, connect with social service specialists about Medicaid, and apply for food, housing, and other essential benefits. The kiosks can also be used for interviews, job training, legal appointments, and education.
The kiosks fit up to three people, are wheelchair accessible, and offer hand sanitizer stations. Reserve a kiosk at https://delawarelibraries.libcal.com/appointments/. This is a grant-funded project from several local and national nonprofits and the federal government. More kiosks are planned at additional libraries. Chromebooks, Wi-Fi hotspots, and blood pressure cuffs can also be borrowed from public libraries throughout the state.
In Delaware:
• Telehealth appointments can occur through video as well as audio-only technologies.

• Patients can access telehealth services if there is an established physician-patient relationship.
• Informed consent is required and must comply with current HIPAA requirements.
• Prescriptions may be prescribed through a telehealth visit once the physician-provider relationship is established.
• Medicaid, Medicare, and private insurance carriers reimburse for telehealth services if those in-person services are covered.
For more information, visit GetConnected.DelawareLibraries.org and https://www.matrc.org/ Visit the 2022 National Telehealth Conference Summary B and Telehealth.HHS.gov to learn how to use telehealth and prepare for a virtual visit.
15 The DPH Bulletin – March 2023 Page 2 of 2
A urine test and a blood test can check for kidney disease. niddk.nih.gov
Division of Libraries
Odontogenic Infections and a Pound of Prevention
Daniel J. Meara, M.S., M.D., D.M.D., M.H.C.D.S., F.A.C.S. Chair, Department of Oral and Maxillofacial Surgery & Hospital Dentistry, ChristianaCare
THE PROBLEM
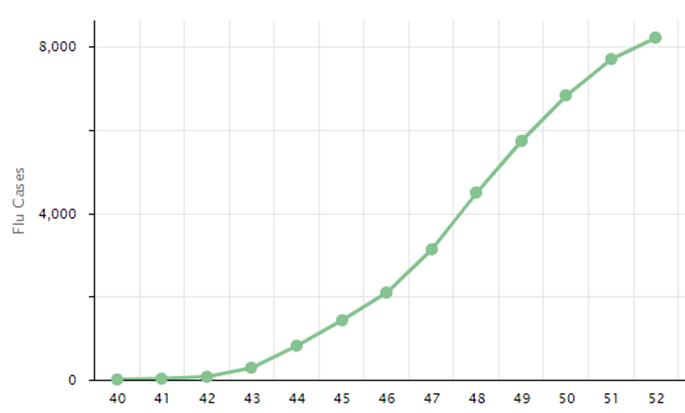
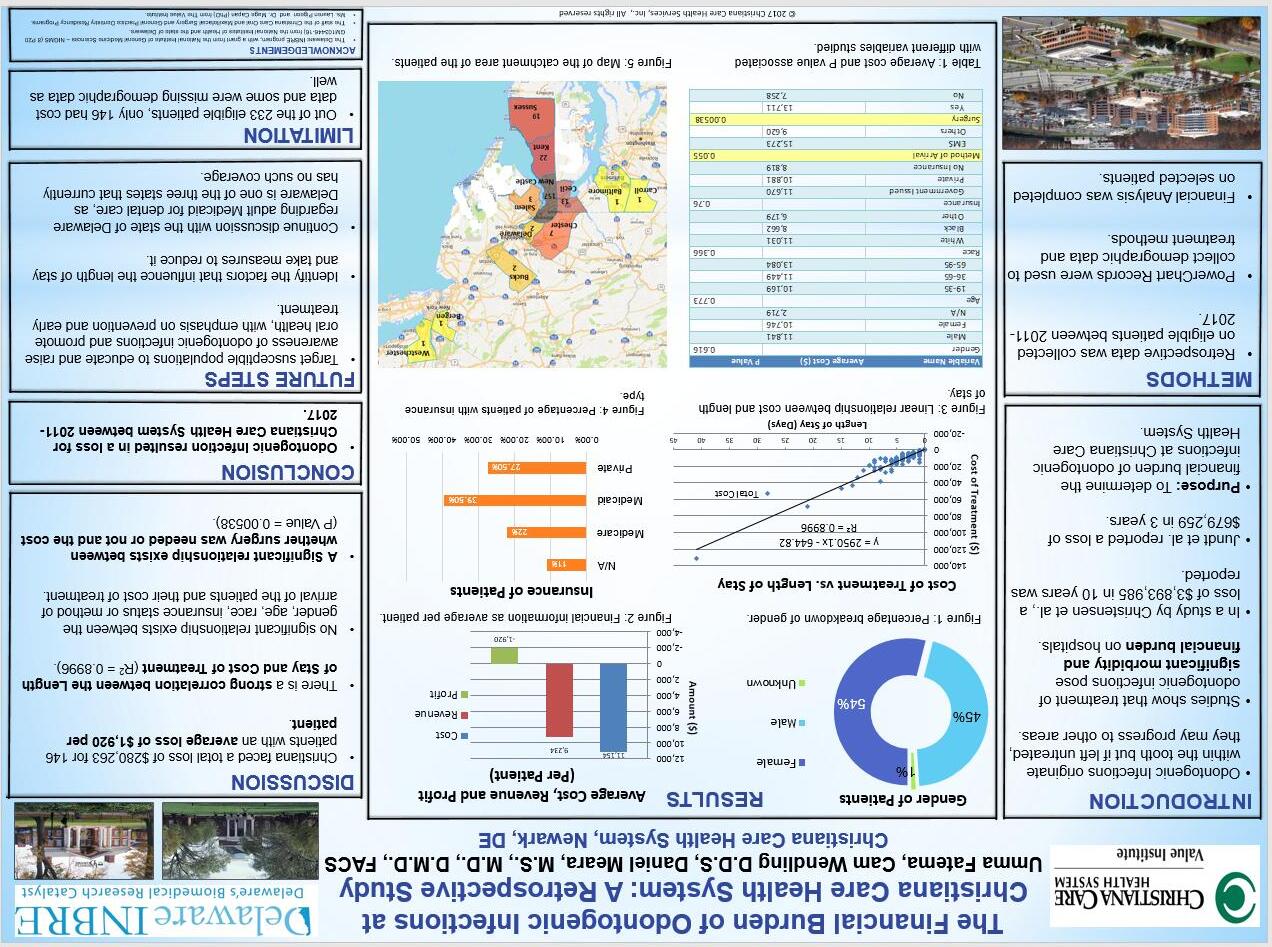
Oral health is essential for systemic health and overall well-being. However, odontogenic infections plaque the healthcare system, with estimates that the cost is over $200 million dollars annually in the United States.1 Further, almost all of these odontogenic infections are preventable when individuals have proper access and engagement in dental services. A 2018 Delaware IDeA Network of Biomedical Research Excellence (INBRE) study out of the Department of Oral and Maxillofacial Surgery and Hospital Dentistry, at Christiana Care Health System, noted that from 2011-2017 a total of 146 patients, with complete cost data, were treated for odontogenic infections, resulting in a total cost of care of over $1.62 million dollars (Figure 1). Christiana Care Health System, with the state’s only oral/ maxillofacial surgery unit and as a tertiary referral center, treats about 33 cases per year at an average cost of over $11,000 per patient.
This problem stems from the fact that approximately 25% of the US population (approximately 82 million Americans) have no dental insurance.2 Moreover, vulnerable populations such as Medicaid eligible patients have limited state-based dental benefits. In Delaware, adults with Medicaid dental benefits have access to $1000 per year, though another $1500 can be available for ‘emergency’ care. Once the benefit limits have been reached, any future costs are out of pocket for the patient until the next benefit reset.
THE RESULT
The result is a disconnect between oral and system health, which impacts the health of the individual as well as the health of the population. Simply, one cannot have true health without oral health being optimized.
OPPORTUNITIES
Integration of oral health metrics and outcomes assessment into risk-based contracts will be an essential lever to drive change, make oral health a priority, and provide the financial structure for sustained and longterm success. Further, coordination of care, primary care in the dental office or dental care in the primary care office, and expanded team care with dental specialists embedded on teams dedicated to diabetic and cardiac patients much like is already done for cleft and oral cancer patients is needed.
In addition, social determinants of health greatly impact health, especially oral health. Limited transportation options, healthy food deserts, smoking and vaping shops on neighborhood street corners, and lack of oral health education are significant challenges for individuals and communities.
PREVENTION
The focus must be on moving away from access to care only when an acute issue arises, such as an odontogenic infection, to a system of care that prioritizes prevention of disease, maintenance of health and care based on what is best for the patient and not just on what is feasible from a financial standpoint.
ACHIEVING CHANGE
As was detailed in my 2018 DJPH article on oral health and achieving population health, we all must think differently to realize meaningful change. Ultimately, to drive change and for access and quality of oral healthcare to improve, silos must be removed, outcomes must be measured, incentives must align, innovation must be fostered, successes must be highlighted and insurance must be affordable. Health and the future of America depends on it!
Dr. Meara may be contacted at dmeara@christianacare.org
REFERENCES
1. Meara, D. J. (2018). Oral health is essential to achieving population health: Thinking differently to achieve meaningful change. Delaware Journal of Public Health, 4(1), 50–51. 10.32481/ djph.2018.01.011
2. U.S. Department of Health and Human Services. (2000). Oral health in America: A report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health.
Doi: 10.32481/djph.2023.04.005
16 Delaware Journal of Public Health - April 2023
17
Figure 1. The Financial Burden of Odontogenic Infections at Christiana Care Health System.
More Premiums Spent on Patient Care? A Great Idea That Should Apply to Dental Insurance
Mark A. Vitale, D.M.D. Chair, New Jersey Dental Political Action Committee, New Jersey Dental Association; President, Dental Lifeline Network, New Jersey
On November 8, 2022, 72% of Massachusetts voters said ‘yes’ to a ballot measure known as Question 2, setting the stage for changing how dental insurance operates in the United States. So, what is Question 2?
Question 2 establishes a minimum Medical Loss Ratio (MLR) requirement for dental insurers and enacts a number of reporting and oversight laws in Massachusetts. MLR is the percentage of premium revenue insurers take in, compared to how much they spend on actual health care services. MLR has been an insurance measuring method for decades, but it gained real traction when the Affordable Care Act (ACA) became law. It requires health plans to calculate their MLR to ensure they spend no less than 80-85% of premium revenue on health care services, but dental insurers are not included in this law. Massachusetts’ Question 2 mirrors what the ACA accomplished by requiring dental insurance companies to spend at least 83% of premium revenue on dental services as opposed to executive salaries or other administrative costs. Like the ACA, dental insurers spending less than 83% must refund the difference to patients.
MLR puts patients at the forefront of the health care system, where they should be. For patients enrolled in dental plans, MLR ensures the investment of their premium dollars is maximized in the form of actual dental care services. It is designed not only to show insurers’ investment in actual care, it also incentivizes insurers to “be better” because they must refund the difference in premium if they don’t meet the 83% MLR. And that is why a large majority of voters in Massachusetts asked for this accountability and value.
The potential benefits of this public policy become even more important when we consider how dental insurance is designed. Unlike health insurance, dental plans are similar to gift cards with an annual maximum the plans pay on behalf of patients; once the annual benefit maximum in the plans is reached, the insurer is done paying for care. Because of this, insurers are motivated to dissuade patients from seeking dental care since unused dental benefit premiums revert back to the insurer as profit. MLR flips that incentive on its head. Under minimum MLR requirement model, insurers will seek ways to encourage patient care so that they can avoid having to issue rebates for not spending enough on actual dental care. MLR laws give patients an assurance that their investment in dental insurance has real value.
In the wake of the landslide decision in Massachusetts, at least eleven states are pursuing MLR legislation for dental plans. Legislators in many states are taking note of the bipartisan and overwhelming voter support in Massachusetts. It is clear that voters are ready to have their insurance companies held accountable. While opponents to MLR try to question the importance of MLR, their testimony so far has shown they are only interested in protecting the status quo. In particular, they want to maintain the incentive structure where premiums not paid out in care mean a better bottom line for insurers. It’s rather simple; patients having more spent on their care will improve their oral health and overall health. The MLR requirement for major medical plans enacted in 2010 has a proven track record of helping health insurance customers. It is about time dental insurance companies provide this consumer protection and be incentivized to spend a greater percentage of the premium dollars they collect on actual patient care.
Dr. Vitale may be contacted at mvitale590@aol.com
Doi: 10.32481/djph.2023.04.006
18 Delaware Journal of Public Health - April 2023
If you have chronic pain, chronic illness, or diabetes, or are a cancer survivor, there are FREE workshops that can help you live better. You’ll meet others like you, learn skills to manage your illness, and start to redefine your life and your health.


EMPOWERED.
or
to
or
more. Chronic Disease | Diabetes | Chronic Pain | Cancer Feeling better starts
feeling 19
Call 302-990-0522
visit HealthyDelaware.org/SelfManagement
register
learn
with
The National Healthy People Initiative: History, Significance, and Embracing the 2030 Oral Health Objectives
Timothy L. Ricks, D.M.D., M.P.H., F.I.C.D., F.A.C.D., F.P.F.A. Indian Health Service, Department of Health and Human Services
ABSTRACT
Since 1979, the U.S. Department of Health and Human Services has worked with multiple subject matter experts and the public to develop and issue a set of ambitious, measurable objectives known as “Healthy People.” These objectives are aimed at improving the health of the nation issued at the start of each decade, and feature specific targets to be achieved at the end of the decade. The fifth iteration, Healthy People 2030, consists 358 measurable public health objectives associated with evidence-based interventions. Oral health is represented by 11 specific objectives aimed at reducing dental caries in children and adolescents, reducing untreated decay and periodontal disease in adults, and promoting evidence-based prevention strategies, including community water fluoridation, dental sealants, oral cancer screenings, and, most importantly, increasing access to dental services. In fact, access to the oral health care system for children, adolescents, and adults is identified as a Healthy People 2030 Leading Health Indicator – a high-priority Healthy People 2030 objective selected to drive action toward improving health and well-being – for the second straight decade. With the continued promotion of multidirectional integration of oral health and overall health across multiple disciplines, many – including policymakers, oral health professionals, other healthcare professionals, dental and public health organizations, and community advocates – have a role in affecting the outcome of the Healthy People 2030 oral health objectives.
INTRODUCTION
In 1979, Surgeon General Dr. Julius Richmond issued a landmark report entitled Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention 1 This report established the framework for “Healthy People,” a collection of science-based, measurable national objectives released each decade that are aimed at improving the health of the nation. Healthy People 2030 marks the fifth decade of these national health priorities, and oral health has had multiple objectives in each of these iterations. Informed by the most current science and breakthroughs, Healthy People 2030 includes measurable oral health objectives with targets, features a set of Leading Health Indicators, and highlights five key social determinants of health: economic stability; education access and quality; social and community context; health care access and quality; and the neighborhood and built environment. As the recent Oral Health in America: Advances and Challenges report demonstrates, all five of these social determinants of health, when favorable, “contribute to better oral health and facilitate favorable oral health trajectories during the life course.”2
LAYING THE FOUNDATION: HEALTHY PEOPLE 1990
Healthy People 1990 focused on health across the life span with overarching goals to decrease mortality in infants and adults and to increase independence among older adults. Objectives were organized into three areas: preventive services, health protection, and health promotion. In that first iteration of Healthy People, oral health objectives were classified under the health protection area, and included 12 very ambitious objectives:3
i. By 1990, the proportion of nine-year-old children who have experienced dental caries in their permanent teeth should be decreased to 60 percent (baseline was 71 percent).
ii. By 1990, the prevalence of gingivitis in children six to 17 years old should be decreased to 18 percent (baseline was 23 percent).
iii. By 1990, in adults the prevalence of gingivitis and destructive periodontal disease should be decreased to 20 percent and 21 percent, respectively (baselines were 25 percent and 23 percent, respectively).
iv. By 1990, no public elementary or secondary school (and no medical facility), should offer highly cariogenic foods or snacks in vending machines or in school breakfast or lunch programs (no baseline data).
v. By 1990, virtually all students in secondary schools and colleges who participate in organized contact sports should routinely wear proper mouth guards (no baseline data).
vi. By 1990, at least 95 percent of school children and their parents should be able to identify the principal risk factors related to dental diseases and be aware of the importance of fluoridation and other measures in controlling these diseases (no baseline data).
vii. By 1990, at least 75 percent of adults should be aware of the necessity for both thorough personal oral hygiene and regular professional care in the prevention and control of periodontal disease (baseline was 52 percent).
Doi: 10.32481/djph.2023.04.007
20 Delaware Journal of Public Health - April 2023
viii. By 1990, at least 95 percent of the population on community water systems should be receiving the benefits of fluoridated drinking water (baseline was 60 percent).
ix. By 1990, at least 50 percent of school children living in fluoride-deficient areas that do not have community water systems should be served by an optimally fluoridated school water supply (baseline was six percent).
x. By 1990, at least 65 percent of school children should be proficient in personal oral hygiene practices and should be receiving other needed preventive dental services in addition to fluoridation (no baseline data).
xi. By 1990, a comprehensive and integrated system should be in place for periodic determination of the oral health status, dental treatment needs, and utilization of dental services of the U.S. population (no baseline data).
xii. By 1985, systems should be in place for determining coverage of all major dental public health preventive measures and activities to reduce consumption of highly cariogenic foods (no baseline data).
ORAL HEALTH AS A LEADING HEALTH INDICATOR
By the time Healthy People 2020 was published, Healthy People had significantly expanded to almost 1,300 objectives (1,111 measurable objectives), including 33 oral health objectives,4 in 42 topic areas. One of the most significant aspects of Healthy People 2020 was the development of Leading Health Indicators, a small subset of objectives selected to spotlight high-priority health issues and actions that can be taken to drive progress toward the Healthy People goals and targets and address morbidity and mortality. In recognition of its role in overall health, oral health was selected as one of the 12 topics. More specifically, Healthy People 2020 Oral Health Objective OH-7, which had a stated goal to “increase the proportion of children, adolescents, and adults who used the oral health care system in the past year” and called for a 10 percent improvement over a baseline access rate of 44.5 percent at the beginning of the decade, was selected as a Leading Health Indicator for oral health and one of 26 Leading Health Indicators overall. Unfortunately, despite the increased attention to oral health access, there was very little change, and the final access rate at the end of the decade was 43.3 percent accessing dental care in the past year, far from the goal of 49.0 percent.5
STREAMLINED APPROACH: HEALTHY PEOPLE 2030
Launched in 2020 and streamlined to promote foci on a reduced number of objectives, Healthy People 2030 includes 358 specific and measurable public health objectives with targets and that are associated with evidence-based interventions. The vision for this fifth iteration of Healthy People is “a society in which all people can achieve their full potential for health and well-being across the lifespan.”6 The overarching goals for Healthy People 2030
not only build on previous iterations, but also place additional emphasis on advancing health equity, health literacy and social determinants of health:
• Attain healthy, thriving lives and well-being free of preventable disease, disability, injury, and premature death.
• Eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all.
• Create social, physical, and economic environments that promote attaining the full potential for health and wellbeing for all.
• Promote healthy development, healthy behaviors, and wellbeing across all life stages.
• Engage leadership, key constituents, and the public across multiple sectors to take action and design policies that improve the health and well-being of all.
The Healthy People 2030 oral health goal is to “improve oral health by increasing access to oral health care, including preventive services.” As part of the overall streamlining of Healthy People objectives, oral health (OH) objectives have been reduced from 33 in Healthy People 2020 to 11 in Healthy People 2030:7
• OH-01: Reduce the proportion of children and adolescents with lifetime tooth decay (baseline is 48.4 percent and the target is 42.9 percent by 2030).
• OH-02: Reduce the proportion of children and adolescents with active and untreated tooth decay (baseline is 13.4 percent and the target is 10.2 percent).
• OH-03: Reduce the proportion of adults with active or untreated tooth decay (baseline is 22.8 percent and the target is 17.3 percent).
• OH-04: Reduce the proportion of older adults with untreated root surface decay (baseline is 29.1 percent and the target is 20.1 percent).
• OH-05: Reduce the proportion of adults aged 45 years and over who have lost all their teeth (baseline is 7.9 percent and the target is 5.4 percent).
• OH-06: Reduce the proportion of adults aged 45 years and over with moderate and severe periodontitis (baseline is 44.5 percent and the target is 39.3 percent).
• OH-07: Increase the proportion of oral and pharyngeal cancers detected at the earliest stage (baseline is 29.5 percent and the target is 34.2 percent).
• OH-08: Increase use of the oral health system (baseline is 46.2 percent and the target is 45.0 percent).
• OH-09: Increase the proportion of low-income youth who have a preventive visit (baseline is 75.8 percent and the target is 79.9 percent).
• OH-10: Increase the proportion of children and adolescents who have dental sealants on one or more molars (baseline is 37.0 percent and the target is 42.5 percent).
• OH-11: Increase the proportion of people whose water systems have the recommended amount of fluoride (baseline is 72.8 percent and the target is 77.1 percent).
21
As with Healthy People 2020, Healthy People 2030 has prioritized specific objectives as Leading Health Indicators, naming 23 specific objectives that “impact major causes of death and disease in the United States.”8 Oral Health objective (OH-8) “increase use of the oral health care system” is one of the Healthy People 2030 Leading Health Indicators.
WHAT IS YOUR ROLE IN HEALTHY PEOPLE 2030?
One of Healthy People 2030’s overarching goals is to engage leadership, key constituents, and the public across multiple sectors. This overarching goal recognizes the imperative of enlisting and engaging diverse users across sectors to achieve the Healthy People 2030 targets. With the continued multidirectional integration of oral health and overall health across multiple disciplines, many professionals affect the outcome of the Healthy People 2030 oral health objectives. Healthcare professionals and others can advocate for policies that enhance access to dental care, especially for underserved and vulnerable populations. Public health professionals can promote evidence-based prevention strategies, such as early access to dental care, improving oral health literacy of patients and the public, dental sealants, topical fluorides, and community water fluoridation. Private practitioners can do their part by becoming knowledgeable about the oral health objectives and adopting evidencebased policies and practices to promote access to care for those at high risk for dental caries or periodontal disease, including historically marginalized communities, people living in poverty, and people living in geographically isolated areas (i.e., dental health professional shortage areas). Finally, medical providers and community partners can promote oral health through education and referral to oral health professionals.
The Healthy People 2030 Federal Oral Health Workgroup – comprised of representatives from the Centers for Disease Control and Prevention (CDC), Health Resources and Services Administration (HRSA), National Institute of Dental and Craniofacial Research, and the Indian Health Service – has developed several specific strategies that oral health professionals can adopt to help the nation reach its 2030 targets on the oral health objectives. These strategies include:
1. Promote and use evidence-based prevention practices;
2. Improve skills and comfort of oral health professionals to provide care to children as soon as the first tooth erupts or by age 1;
3. Embrace oral health workforce delivery models that improve access to care for underserved and vulnerable populations;
4. Use an integrated approach to improve access to care, working collaboratively with medical and community partners; and
5. Work with state and local agencies and other advocates to educate decision makers about the benefits of community water fluoridation.
Healthy People offers an array of evidence-based resources related to oral conditions listed in the oral health objectives. These can be found at https://health.gov/healthypeople/objectives-and-data/ browse-objectives/oral-conditions/evidence-based-resources and include:
• Treatment of periodontitis for glycemic control in people with diabetes mellitus
• Pit and fissure sealants versus fluoride varnishes for preventing dental decay in the permanent teeth of children and adolescents
• Fluoride varnishes for preventing dental caries in children and adolescents
• Oral Health in America: Advances and Challenges
• Pit and Fissure Sealants for Preventing Dental Decay in Permanent Teeth
• Micro-Invasive Interventions for Managing Proximal Dental Decay in Primary and Permanent Teeth
• Fluoride Toothpastes of Different Concentrations for Preventing Dental Caries
• Interventions with Pregnant Women, New Mothers and Other Primary Caregivers for Preventing Early Childhood Caries
• Fluoride Mouth Rinses for Preventing Dental Caries in Children and Adolescents
• Fluoride Gels for Preventing Dental Caries in Children and Adolescents
• Community Water Fluoridation
• Implementation of Evidence-Based Preventive Interventions
• Preventing Tooth Decay
• Dental Caries (Cavities): Community Water Fluoridation
• Dental Caries (Cavities): School-Based Dental Sealant Delivery Programs
• Prevention of Dental Caries in Children Younger Than 5 Years: Screening and Interventions
Healthy People 2030 is our opportunity to collectively improve the oral health of the nation. Each of us – oral health professionals, other healthcare professionals, communities, dental and public health organizations, government agencies, etc. – can do our part by learning about the eleven oral health objectives and using or promoting evidence-based strategies to address them.
Dr. Ricks may be contacted at tim.ricks@ihs.gov
REFERENCES
1. U.S. Department of Health, Education, and Welfare. (1979). Healthy people: The surgeon general’s report on health promotion and disease prevention. https://files.eric.ed.gov/fulltext/ED186357.pdf
2. Institutes of Health. (2021). Oral Health in America: Advances and challenges. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Institute of Dental and Craniofacial Research, 1, 5-6. https://www.nidcr.nih.gov/research/oralhealthinamerica
22 Delaware Journal of Public Health - April 2023
3. Public Health Service (DHHS). (n.d.). The 1990 health objectives for the nation: A midcourse review. Public Health Service (DHHS), Rockville, MD. Office of Disease Prevention and Health Promotion. https://eric.ed.gov/?id=ED296989
4. HealthyPeople.gov. (n.d.). Healthy people 2020, topics & objectives. Office of Disease Prevention and Health Promotion, Department of Health and Human Services, Washington, D.C. https://wayback.archive-it.org/5774/20220413162703/ https://www.healthypeople.gov/2020/topics-objectives
5. Office of the Assistant Secretary for Health. (n.d.). Healthy people 2020: an end of decade snapshot. Office of Disease Prevention and Health Promotion, Department of Health and Human Services, Washington, D.C. https://health.gov/sites/default/files/2021-03/21%20 HP2020EndofDecadeSnapshot2.pdf
6. Office of Disease Prevention and Health Promotion. (n.d.). Healthy people 2030 framework. Department of Health and Human Services, Washington, D.C. https://health.gov/healthypeople/about/healthy-people-2030-framework
7. Office of Disease Prevention and Health Promotion. (n.d.). Oral conditions. Department of Health and Human Services, Washington, D.C.
https://health.gov/healthypeople/objectives-and-data/browse-objectives/ oral-conditions
8. Office of Disease Prevention and Health Promotion. (n.d.). Leading health indicators. Department of Health and Human Services, Washington, D.C. https://health.gov/healthypeople/objectives-and-data/leading-health-indicators
Delaware Journal of Upcoming Issues
Public Health
Each year, the Delaware Journal of Public Health publishes five different theme issues. Article submissions are accepted on a rolling basis, and the editorial board considers all submissions, both those connected directly to a theme issue, and non-thematic submissions. The editorial board reserves the right to include non-thematic submissions in each issue.
The working publishing calendar and thematic issues for 2023 are as follows:
If you have questions about submissions, ideas for an article, or suggestions for a future theme issue, please email Liz Healy: ehealy@delamed.org
All submissions can be submitted via the online submission portal: https://www.surveymonkey.com/r/2DSQN98
Submissions guidelines can be found at: https://djph.org
23
Issue Submission Publication Oral Health March 2023 April 2023 Homelessness April 2023 May 2023 Neurological Impairment/Stroke July 2023 September 2023 Bio Tech/Research September 2023 October 2023 Health Policy/Ethics November 2023 December 2023
Take good care of your heart
February is American Heart Month, an appropriate time to think about your heart’s health Heart disease – including coronary artery disease, heart failure, and stroke –is the leading cause of death globally. Many cases of heart disease can be prevented by adopting healthy behaviors such as eating a healthy diet, getting regular physical activity, not smoking, and managing stress. While there is no cure, heart disease can be treated and managed through lifestyle changes, medications, and by selfmonitoring blood pressure.
The Centers for Disease Control and Prevention advises taking these steps to prevent heart disease:

• Get regular check-ups and cardiovascular screenings to identify issues early.

• Eat a healthy diet that is low in salt, saturated and trans fats, and added sugars.
• Get regular physical activity. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week.
• Maintain a healthy weight. If you are overweight or obese, work to lose weight through diet and physical activity.
• Quit smoking and avoid secondhand smoke.
• Limit your alcohol intake.
• Get enough sleep
• Manage stress.
People with diabetes are at an increased risk of developing heart disease and other cardiovascular conditions High blood sugar levels can damage the blood vessels and nerves that supply the heart, leading to an increased risk of heart attack and stroke. It is also common for people with diabetes to have high blood pressure, high levels of LDL ("bad") cholesterol and low levels of HDL ("good") cholesterol, and to be obese – all which increase the risk of heart disease.
If you are at risk for heart disease or have high blood pressure, learn about the Healthy Heart Ambassador-Blood Pressure Self Monitoring Program by calling 302-208-9097 or visiting healthydelaware.org

Learn how to recognize a stroke
Stroke is a time-sensitive disease that can cause long-lasting movement, speech, and thinking issues. Some stroke victims need to re-learn how to walk or hold a spoon. Others are unable to work and require long-term care.

A stroke can also be fatal. Cerebrovascular Disease, which includes stroke, is the fourth leading cause of death in the state, according to the 2019 Delaware Vital Statistics Annual Report. Treatments for strokes are time dependent. Some therapies must be started within two to four hours of the onset of symptoms. Missing this window can have a significant effect on the patient’s outcome. Call 911 immediately if you notice stroke symptoms. Act FAST!


F: Face Drooping
A: Arm Weakness
S: Speech Difficulty
T: Time to call 911
Calling 911 for Emergency Medical Services (EMS) is the quickest and safest way to get the patient to a Stroke Center. EMS can initiate care and make sure that the patient is transported urgently to the appropriate level Stroke Center All Delaware hospitals are Joint Commission and Delaware designated Stroke Centers. EMS calls ahead so the hospital’s Stroke Team can prepare equipment and medications None of these time-sensitive interventions can occur if the patient is taken to the hospital in a private vehicle
In 2021, Delaware’s EMS agencies responded to 2,944 possible stroke patients. According to Delaware’s Stroke Registry Data (American Heart Association’s Get With the Guidelines®) for 2021, Delaware Stroke Centers treated 3,225 confirmed strokes. Among those patients, the three highest risk factors were hypertension (71 percent), high cholesterol (52 percent), and diabetes (32 percent).
To learn more about preventing and responding to stroke, visit the American Stroke Association at www.stroke.org
From the Delaware Division of Public Health February 202
24 Delaware Journal of Public Health - April 2023
Delaware’s four Systems of Care provide quality and equal care
A System of Care provides timely access to optimal, equitable, and accessible care, beginning when a patient enters the system throughout their treatment, rehabilitation, and recovery.

Delaware has four Systems of Care to reduce morbidity and mortality and to preserve lives and livelihoods The Trauma System of Care was legislatively mandated in 1996, becoming the state’s first State legislators established the Delaware Pediatric System of Care in 1997, the Delaware Stroke System of Care in 2016, and the Delaware Overdose System of Care in 2018 Wherever an injury, stroke, or overdose occurs, patients enter a System of Care that follows the same guidelines, regulations, and standards statewide.
The Division of Public Health’s Office of Emergency Medical Services (OEMS) oversees and manages the Systems of Care through agreements with hospitals and other facilities, EMS, first responders, rehabilitation services, and state agencies. Oversight committees review policies, data, and health outcomes.
“We direct the right patient to the facility with the right resources for their condition, at the right time,” said OEMS Systems of Care Coordinator Paul Westlake. Systems of Care continuously resolve any differences in patient care and outcomes. For example, the Delaware Stroke System of Care addresses disparate mortality rates. According to the 2019 Delaware Vital Statistics Annual Report, in 2015-2019, the non-Hispanic Black stroke mortality rate of 55.9 deaths per 100,000 population was 39 percent higher than the non-Hispanic White rate of 40.3 deaths
For more information about Systems of Care, visit https://www.dhss.delaware.gov/dph/ems/ems.html or call 302-223-2700.
COVID-19 Call Center closes
Due to a low volume of calls, the Division of Public Health (DPH) closed its COVID-19 Call Center on January 31.
For COVID-19 information, visit de.gov/coronavirus General questions can be submitted via a contact form at coronavirus.delaware.gov/contact or by emailing DPHCall@delaware.gov Send vaccinespecific questions to Vaccine@delaware.gov Individuals can also call 2-1-1 and those who are deaf or hard of hearing can text their ZIP Code to 898-211, or email delaware211@uwde.org Monday through Friday between 8:00 a.m. and 9:00 p.m. and Saturday from 9:00 a.m. to 9:00 p.m.
DPH launched the COVID-19 Call Center on March 4, 2020, to handle the tremendous number of calls about the novel coronavirus. At the time, Delaware had no reported cases. The call center provided critical information to schools, medical providers, state agencies and community organizations.
DELPH program selects DPH’s Mathew
Michelle Mathew of the Division of Public Health (DPH) was selected to participate in the Diverse Executives Leading in Public Health (DELPH) program. DELPH is a joint venture between the Association of State and Territorial Health Officials and the Satcher Health Leadership Institute at the Morehouse School of Medicine.
The 10-month program, funded by the Centers for Disease Control and Prevention, provides opportunities to explore individual leadership identity and actions to positively influence the work and culture of organizations through communication, leadership, and goal setting. Mathew attended an inperson kick-off in Atlanta and engages in live-virtual webinars, collaborates with public health leaders on projects and assignments, and reads related literature recommended by leaders from all over the country.
Mathew, a Public Health Administrator I, oversees the Bureau of Adolescent and Reproductive Heath within the Family Health Systems Section. She began working at DPH as a Health Program Coordinator in 2003.
 Michelle Mathew
Michelle Mathew
The DPH Bulletin – February 2023 Page 2 of 4
25
Human Papilloma Virus (HPV) and the Current State of Oropharyngeal Cancer Prevention and Treatment
Jacob P. Gribb, D.M.D.
Resident Physician, Oral and Maxillofacial Surgery, ChristianaCare Health System
John H. Wheelock, D.D.S.
Resident Physician, Oral and Maxillofacial Surgery, CristianaCare Health System
Etern S. Park, M.D., D.D.S.
Attending Surgeon, Oral and Maxillofacial Surgery, ChristianaCare Health System
INTRODUCTION
Head and neck cancers now account for almost 3% of all new cancer cases nationwide, with 47,813 new cases and 10,492 deaths per year.1 Malignancies of the head and neck most commonly originate from epithelial origin, namely squamous cell carcinoma (SCCa). Oropharyngeal cancer has been rising yearly by an average of 0.6% per year, with the average five-year relative survival rate at an estimated 68%.2 Human papillomavirus (HPV) is, historically, most associated with cervical cancer in women. However, HPV-related head and neck malignancies are becoming more prevalent in the United States, with a higher predilection for the male population. HPV-related oropharyngeal SCCa has now surpassed cervical cancer as the most common HPV-related cancer in the US, representing 19,775 yearly cases, compared with 12,143 yearly cases of cervical cancer.3 Current projections estimate a current upward trend for the next decade, with predictions greater than 30,000 annual cases by year 2029.3 HPVassociated malignancies are 2.7 times more frequently diagnosed in men, and has a mortality 2.8 times that of women according to the latest data.4
RISK FACTORS
The main risk factors for oropharyngeal SCCa have been multi-factorial, including tobacco and alcohol use. Recent data has shown an increasing trend with HPV-associated tumors, specifically, HPV-16 which has accounted for more than 90% of cases. Approximately 80% of oropharyngeal cancers in the US are associated with HPV.5 These specific tumor types have been the main reason for increasing incidences, especially in the younger population.
HPV-16 and HPV-33 have been recognized as the main etiologic factors for the increase of cancers in the cervix, vulva, vagina, penis, and anus, as well as the oropharynx, which contrasts with traditional tobacco- and alcohol-related HPV-negative cancers. The HPV-associated disease is molecularly and clinically unique compared to the traditional HPV-negative oropharyngeal cancers. The etiology is from the double stranded DNA viruses E6 and E7 oncogenes that inactivate the p53 tumor suppressor gene and the retinoblastoma protein which leads to release of transcription factors causing cell cycle progression.3
Currently, HPV is the most common and widespread sexually transmitted disease worldwide, and is the main cause of cancer in anogenital and oropharyngeal regions. Even though there has been a decrease in HPV-negative oropharyngeal cancers, there continues to be an increase in the HPV-related oropharyngeal SCCa. The main accepted hypothesis is that oral sexual behaviors
have become more common and frequent in the last 50 years, particularly in younger age groups. Individuals with more than ten lifetime oral sex partners have a greater than four-fold increased risk of HPV-positive oropharyngeal SCCa.3
DIAGNOSIS
Patients with HPV-related SCCa have a better prognosis and are usually younger and non-smokers compared to HPV-negative SCCa patients (figure 1). The HPV-related SCCa usually demonstrates a nonkeratinizing epithelium which is distinct from tobacco and alcohol related oral diseases, which are usually keratinizing SCCa.6 Due to the improved survival rate of HPVassociated oropharyngeal SCCa, the American Joint Committee on Cancer has made important changes to its staging system. In 2018, the American Society of Clinical Oncology, National Comprehensive Cancer Network, and College of American Pathologists developed guidelines that all specimens should be tested for HPV-tumor status using immunohistochemical staining against p16 with at least 70% nuclear and cytoplasmic expression as an indicator (figure 2). The other gold standard is the HPV E6/ E7 mRNA and HPV DNA detection by polymerase chain reaction and in situ hybridization. In 2017, the eighth edition classified oral and oropharyngeal cancers by the p16 marker, downstaging the p16 positive oropharyngeal cancers from previous editions.6
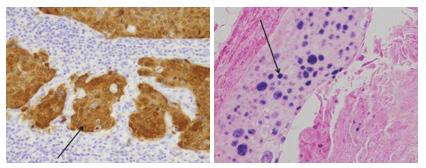
Doi: 10.32481/djph.2023.04.008
Figure 1. HPV-Negative Squamous Cell Carcinoma
Figure 2. Immunohistochemistry Staining of p16 in HPV-Positive Oropharyngeal Squamous Cell Carcinoma Tumor.
26 Delaware Journal of Public Health - April 2023
The arrows indicate a cluster of tumor cells staining positive for p16.7
VACCINATION
The best diagnostic strategy for HPV-related oropharyngeal SCCa continues to be early diagnosis as well as vaccination against HPV-infection. The FDA currently has four preventive cancer vaccines, with three of the vaccines, Cervarix, Gardasil, and Gardasil-9, approved to prevent the infection of HPV and one preventive Hepatitis B (HBV) vaccine (HEPLISAV-B) that protects against the Hepatitis B virus which prevents development of HBV-related liver cancer. Since 2016, Gardasil-9 has been the only HPV vaccine available in the US and protects against the subtypes of HPV-6, 11, 16, 18, 31, 33, 45, 52, 58. HPV vaccines were initially developed to prevent anogenital tract cancers, but since the 2-dose scheduled vaccine protects against the other high-risk variants of HPV that can cause oropharyngeal cancers, the vaccine can be used to prevent oropharyngeal diseases.8 The CDC and American Academy of Pediatrics highly recommend administering the first dose of the HPV vaccine to children as early as 9-years old, but definitely by ages 11-12 years. Doses are given 6 to 12 months apart. Children who start the HPV vaccine series on or after their 15th birthday need three doses, given over 6 months. Everyone through age 26 years should get the HPV vaccine, and if over the age of 26 should consult with their doctor.9
In 2018, the American Dental Association and the American Academy of Pediatric Dentistry developed guidelines for dentists to participate in the prevention of oral and oropharyngeal cancer through education and endorsing the HPV vaccination. In 2019, Oregon passed legislation to allow dental healthcare providers to prescribe and administer any vaccine as part of Public Health Modernization Implementation.5 In 2018, Oregon’s HPV initiation dose was 67% and HPV completion doses were 46%, which has increased by 6% and 7%, respectively, in 2022. In 2019, 71.5% of adolescents aged 13-17 years had received one dose of HPV, and 54.2% had completed the HPV vaccination.10 Each year, 88.9% of eligible adolescents obtain the first dose, however only 53.7% follow up for the second dose indicating that continued efforts are needed to improve for follow up.11
TREATMENT
Patients diagnosed with oral and oropharyngeal SCCa require a multidisciplinary work up and treatment. The new staging algorithm for HPV-positive oropharyngeal SCCa is different from staging for HPV-negative oropharyngeal SCCa, which is based off the biomarker p16 (figure 3). Staging for p16-positive does not include T4b diseases and defines clinical nodal stages by size and laterality and defines pathological nodal stage by number of lymph nodes. Pathologic and clinical nodal staging for p16-positive diseases also omits consideration of extra nodal extension.12 Based on the most recent TNM staging, most patients with early-stage disease of the soft palate/oropharynx/tonsils/base of tongue are treated with definitive surgical resection even with evidence of isolated nodal disease.13
Patients with HPV-related oropharyngeal SCCa presented with higher two-year survival rates than those patients with HPV-unrelated oropharyngeal SCCa. Due to better response to surgical resection and chemoradiotherapy, there has been a de-intensification of HPV-related oropharyngeal SCCa therapies. Different nonsurgical approaches have included reducing radiotherapy or chemotherapy doses. The radiotherapy usually includes 44-72 Gy depending on tumor infiltration.13 The customary approach was previously radiation doses above 50 Grays, which caused patients to experience significant side effects (e.g.: dry mouth, limited mouth opening, loss of taste). Lowering the radiation doses as low as 44 Grays has been shown to be both safe and effective, and has resulted in patients experiencing fewer side effects.13 Optimal treatment options continue to be unclear, however the advancements of de-intensification treatments along with the better prognosis and higher five-year survival rates are improving the long-term quality of life for the patient with HPVpositive oropharyngeal cancer.14
It is important to note that in HPV-positive OPSCC, pathological staging criteria differ from clinical staging criteria. Early-stage disease is generally managed with single-modality treatment, whereas advanced-stage disease requires chemoradiotherapy with or without neck dissection or surgical resection with reconstruction and postoperative chemoradiotherapy.13
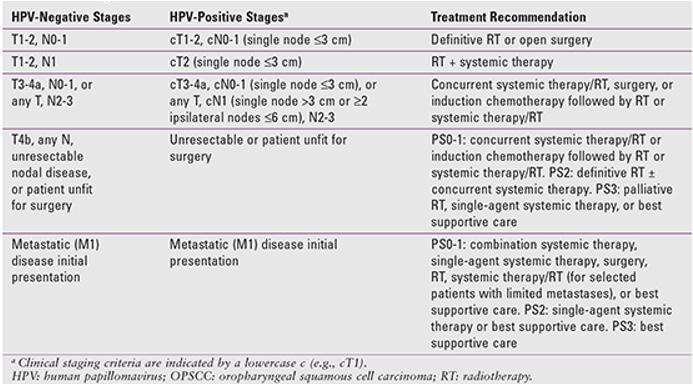
27
Figure 3. NCCN Recommendations for Managing the Different Clinical Stages of HPV-Positive and HPV-Negative Tumors
CONCLUSION
HPV-related SCCa continues to cause an increased incidence of oropharyngeal cancer in the US. HPV-related oropharyngeal cancer has distinct risk factors with unique epidemiology, staging, and prognosis. Within the head and neck cancer community and dental community, early diagnosis and treatment are the most important primary factors. HPV-positive oropharyngeal SCCa has great prognosis and multiple trials continue to take place to de-intensify treatment with the goal to decrease treatment related morbidities.15 Continual promotion and education of the HPV vaccination has the potential to bring more of a positive impact on public, with vaccination likely preventing oral HPV infection and the potential of living longer and better quality lives.
Dr. Park may be contacted at etern.s.park@christianacare.org.
REFERENCES
1. U.S. Cancer Statistics Working Group. (2022). U.S. cancer statistics data visualizations tool. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute.
https://www.cdc.gov/cancer/dataviz
2 National Cancer Institute. (n.d.). Cancer stat facts: oral cavity and pharynx cancer.
https://seer.cancer.gov/statfacts/html/oralcav.html
3 Rettig, E. M., & Sethi, R. K. V. (2021, October). Cancer of the oropharynx and the association with human papillomavirus. Hematology/Oncology Clinics of North America, 35(5), 913–931. 10.1016/j.hoc.2021.05.004
4. Siegel, R. L., Miller, K. D., & Jemal, A. (2017, January). Cancer statistics. CA: a Cancer Journal for Clinicians, 67(1), 7–30. 10.3322/caac.21387
5. Louredo, B. V. R., Prado-Ribeiro, A. C., Brandão, T. B., Epstein, J. B., Migliorati, C. A., Piña, A. R., SantosSilva, A. R. (2022, August). State-of-the-science concepts of HPV-related oropharyngeal squamous cell carcinoma: A comprehensive review. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 134(2), 190–205. 10.1016/j. oooo.2022.03.016
6. Sabu, A., Mouli, N. V. R., Tejaswini, N., Rohit, V., Nishitha, G., & Uppala, D. (2019). Human papillomavirus detection in oropharyngeal squamous cell carcinoma using p16 immunohistochemistry. International Journal of Applied & Basic Medical Research, 9(4), 212–216 10.4103/ijabmr. IJABMR_221_18
7 Compton, A. M., Moore-Medlin, T., Herman-Ferdinandez, L., Clark, C., Caldito, G. C., Wang, X. I., Nathan, C. O. (2011, July). Human papillomavirus in metastatic lymph nodes from unknown primary head and neck squamous cell carcinoma. Otolaryngology - Head and Neck Surgery, 145(1), 51–57. 10.1177/0194599811400385
8. Dunn, G. P. (2023). Cancer Vaccines: Preventive, therapeutic, personalized. Cancer Research Institute.
https://www.cancerresearch.org/treatment-types/cancer-vaccines
9 Centers for Disease Control and Prevention. (n.d.). National center for HIV/AIDS, viral hepatitis, STD, and TB prevention. https://www.cdc.gov/nchhstp/default.htm
10 Oregon Immunization Program. (n.d.). ALERT Immunization Information System.
https://www.oregon.gov/oha/PH/PREVENTIONWELLNESS/ VACCINESIMMUNIZATION/ALERT/Pages/index.aspx
11 Elam-Evans, L. D., Yankey, D., Singelton, J. A., Sterrett, N., Markowitz, L. E., Williams, C. L., . . . Stokley, S. (2020, August). National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years— United States, 2019. MMWR. Morbidity and Mortality Weekly Report, 69(33), 1109–1116 10.15585/mmwr.mm6933a1
12 Flavill, E., Fang, Y. V., Miles, B., Truelson, J., & Perkins, S. (2014, May). Induction chemotherapy followed by concurrent chemoradiotherapy for advanced stage oropharyngeal squamous cell carcinoma with HPV and P16 testing. The Annals of Otology, Rhinology, and Laryngology, 123(5), 365–373.
13. National Comprehensive Cancer Network. (2023, Jan). Cancer of the oropharynx.
https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1437
14. Silver, J. A., Turkdogan, S., Roy, C. F., Subramaniam, T., Henry, M., & Sadeghi, N. (2022, May). De-escalation strategies for human papillomavirus-associated oropharyngeal squamous cell carcinoma-Where are we now? Current Oncology (Toronto, Ont.), 29(5), 3668–3697 10.3390/curroncol29050295
15 Vermorken, J. B., Psyrri, A., Mesía, R., Peyrade, F., Beier, F., de Blas, B., Licitra, L. (2013, May). OP041: Impact of human papillomavirus (HPV) and p16 status on survival and response with cisplatin plus 5-FU and cetuximab in recurrent and/or metastatic squamous cell carcinoma of the head and neck (R/M SCCHN): Analysis of the phase III extreme trial. Oral Oncology, 49(suppl 1), S19–S20 10.1016/j. oraloncology.2013.03.049
28 Delaware Journal of Public Health - April 2023

Call the Delaware Quitline and free yourself from tobacco. Free counseling, cessation aids, and medications are available to help you get on the path to living tobacco-free. Stop getting pulled back in. Let us help you quit for good. QuitSupport.com TRAPPED BY TOBACCO? WE HAVE A WAY OUT. 29
GLOBAL HEALTH MATTERS
GLOBAL HEALTH MATTERS
Cultivating oral health research in Thailand…p. 5
Cultivating oral health research in Thailand…p. 5
Cultivating oral health research in Thailand…p. 5
Cultivating oral health research in Thailand…p. 5




Kilmarx steps in as Acting Fogarty Director
Kilmarx steps in as Acting Fogarty Director
Kilmarx steps in as Acting Fogarty Director
Kilmarx steps in as Acting Fogarty Director




Peter Kilmarx, M.D., has stepped in as Acting Director of the Fogarty International Center and Acting Associate Director, Global Health Research, National Institutes of Health, after the departure of Roger I. Glass, M.D., Ph.D. An expert on infectious disease research and HIV/AIDS prevention, Dr. Kilmarx was named Deputy Director of the Fogarty International Center in 2015.
Peter Kilmarx, M.D., has stepped in as Acting Director of the Fogarty International Center and Acting Associate Director, Global Health Research, National Institutes of Health, after the departure of Roger I. Glass, M.D., Ph.D. An expert on infectious disease research and HIV/AIDS prevention, Dr. Kilmarx was named Deputy Director of the Fogarty International Center in 2015.
Peter Kilmarx, M.D., has stepped in as Acting Director of the Fogarty International Center and Acting Associate Director, Global Health Research, National Institutes of Health, after the departure of Roger I. Glass, M.D., Ph.D. An expert on infectious disease research and HIV/AIDS prevention, Dr. Kilmarx was named Deputy Director of the Fogarty International Center in 2015.
During his tenure at Fogarty he has led the analysis of NIH global health activities, built coalitions within NIH and with external stakeholders, and represented Fogarty and NIH in forums around the globe. He co-led an initiative to transform African health professional education and research, resulting in the formation of the African Association for Health Professions Education and Research (AFREHealth), as well as the African Postdoctoral Training Initiative (APTI), which brings African postdoctoral fellows to NIH. He has also focused on efforts to increase equity in global health research and building global capacity for pandemic preparedness.
During his tenure at Fogarty he has led the analysis of NIH global health activities, built coalitions within NIH and with external stakeholders, and represented Fogarty and NIH in forums around the globe. He co-led an initiative to transform African health professional education and research, resulting in the formation of the African Association for Health Professions Education and Research (AFREHealth), as well as the African Postdoctoral Training Initiative (APTI), which brings African postdoctoral fellows to NIH. He has also focused on efforts to increase equity in global health research and building global capacity for pandemic preparedness.
Peter Kilmarx, M.D., has stepped in as Acting Director of the Fogarty International Center and Acting Associate Director, Global Health Research, National Institutes of Health, after the departure of Roger I. Glass, M.D., Ph.D. An expert on infectious disease research and HIV/AIDS prevention, Dr. Kilmarx was named Deputy Director of the Fogarty International Center in 2015. During his tenure at Fogarty he has led the analysis of NIH global health activities, built coalitions within NIH and with external stakeholders, and represented Fogarty and NIH in forums around the globe. He co-led an initiative to transform African health professional education and research, resulting in the formation of the African Association for Health Professions Education and Research (AFREHealth), as well as the African Postdoctoral Training Initiative (APTI), which brings African postdoctoral fellows to NIH. He has also focused on efforts to increase equity in global health research and building global capacity for pandemic preparedness.
During his tenure at Fogarty he has led the analysis of NIH global health activities, built coalitions within NIH and with external stakeholders, and represented Fogarty and NIH in forums around the globe. He co-led an initiative to transform African health professional education and research, resulting in the formation of the African Association for Health Professions Education and Research (AFREHealth), as well as the African Postdoctoral Training Initiative (APTI), which brings African postdoctoral fellows to NIH. He has also focused on efforts to increase equity in global health research and building global capacity for pandemic preparedness.




“I’m grateful for the leadership and mentoring of Dr. Roger Glass," said Dr. Kilmarx. “I’m excited about this opportunity to serve Fogarty and our partners, strengthening global research capacity and partnerships to address the critical global health challenges of our time.” Dr. Kilmarx will over-
“I’m grateful for the leadership and mentoring of Dr. Roger Glass," said Dr. Kilmarx. “I’m excited about this opportunity to serve Fogarty and our partners, strengthening global research capacity and partnerships to address the critical global health challenges of our time.” Dr. Kilmarx will over-
“I’m grateful for the leadership and mentoring of Dr. Roger Glass," said Dr. Kilmarx. “I’m excited about this opportunity to serve Fogarty and our partners, strengthening global research capacity and partnerships to address the critical global health challenges of our time.” Dr. Kilmarx will over-
see an annual budget of more than $95 million and a portfolio of nearly 600 active grants. Meanwhile, Fogarty will continue its mission of supporting and facilitating global health research conducted by U.S. and international investigators, building partnerships between health research institutions in the U.S. and abroad, and training the next generation of scientists to address global health needs.
see an annual budget of more than $95 million and a portfolio of nearly 600 active grants. Meanwhile, Fogarty will continue its mission of supporting and facilitating global health research conducted by U.S. and international investigators, building partnerships between health research institutions in the U.S. and abroad, and training the next generation of scientists to address global health needs.
see an annual budget of more than $95 million and a portfolio of nearly 600 active grants. Meanwhile, Fogarty will continue its mission of supporting and facilitating global health research conducted by U.S. and international investigators, building partnerships between health research institutions in the U.S. and abroad, and training the next generation of scientists to address global health needs.
see an annual budget of more than $95 million and a portfolio of nearly 600 active grants. Meanwhile, Fogarty will continue its mission of supporting and facilitating global health research conducted by U.S. and international investigators, building partnerships between health research institutions in the U.S. and abroad, and training the next generation of scientists to address global health needs.
Dr. Kilmarx previously served as the Center for Disease Control and Prevention’s Country Director in Zimbabwe, providing oversight for 30 CDC staff who managed implementation of the U.S. efforts to reduce HIV/AIDS, tuberculosis and malaria, and rose to the rank of Rear Admiral and Assistant Surgeon General in the U.S. Public Health Service.
Dr. Kilmarx previously served as the Center for Disease Control and Prevention’s Country Director in Zimbabwe, providing oversight for 30 CDC staff who managed implementation of the U.S. efforts to reduce HIV/AIDS, tuberculosis and malaria, and rose to the rank of Rear Admiral and Assistant Surgeon General in the U.S. Public Health Service.
Dr. Kilmarx previously served as the Center for Disease Control and Prevention’s Country Director in Zimbabwe, providing oversight for 30 CDC staff who managed implementation of the U.S. efforts to reduce HIV/AIDS, tuberculosis and malaria, and rose to the rank of Rear Admiral and Assistant Surgeon General in the U.S. Public Health Service.
Dr. Kilmarx previously served as the Center for Disease Control and Prevention’s Country Director in Zimbabwe, providing oversight for 30 CDC staff who managed implementation of the U.S. efforts to reduce HIV/AIDS, tuberculosis and malaria, and rose to the rank of Rear Admiral and Assistant Surgeon General in the U.S. Public Health Service.
Rachel Sturke, Ph.D., M.P.H., M.I.A., Deputy Director and Senior Scientist for the Fogarty Center for Global Health Studies, will step in as Acting Deputy Director for the Center. Dr. Sturke joined Fogarty in 2006 and oversees a portfolio of global projects that include a focus on building research capacity in implementation science in low- and middleincome countries (LMICs) and using innovative platforms to bring implementation science practitioners together with decision-makers and program implementers from LMICs. “We’re very pleased that Dr. Rachel Sturke is taking on the role of Acting Deputy Director,” said Dr. Kilmarx. “She is an exceptionally qualified global expert on implementation science and, having been with Fogarty since 2006, brings a wealth of institutional knowledge to the role.”
Rachel Sturke, Ph.D., M.P.H., M.I.A., Deputy Director and Senior Scientist for the Fogarty Center for Global Health Studies, will step in as Acting Deputy Director for the Center. Dr. Sturke joined Fogarty in 2006 and oversees a portfolio of global projects that include a focus on building research capacity in implementation science in low- and middleincome countries (LMICs) and using innovative platforms to bring implementation science practitioners together with decision-makers and program implementers from LMICs. “We’re very pleased that Dr. Rachel Sturke is taking on the role of Acting Deputy Director,” said Dr. Kilmarx. “She is an exceptionally qualified global expert on implementation science and, having been with Fogarty since 2006, brings a wealth of institutional knowledge to the role.”
Rachel Sturke, Ph.D., M.P.H., M.I.A., Deputy Director and Senior Scientist for the Fogarty Center for Global Health Studies, will step in as Acting Deputy Director for the Center. Dr. Sturke joined Fogarty in 2006 and oversees a portfolio of global projects that include a focus on building research capacity in implementation science in low- and middleincome countries (LMICs) and using innovative platforms to bring implementation science practitioners together with decision-makers and program implementers from LMICs. “We’re very pleased that Dr. Rachel Sturke is taking on the role of Acting Deputy Director,” said Dr. Kilmarx. “She is an exceptionally qualified global expert on implementation science and, having been with Fogarty since 2006, brings a wealth of institutional knowledge to the role.”
Celebrate with us: Fellows & Scholars at 20
“I’m grateful for the leadership and mentoring of Dr. Roger Glass," said Dr. Kilmarx. “I’m excited about this opportunity to serve Fogarty and our partners, strengthening global research capacity and partnerships to address the critical global health challenges of our time.” Dr. Kilmarx will over-
Celebrate with us: Fellows & Scholars at 20
Rachel Sturke, Ph.D., M.P.H., M.I.A., Deputy Director and Senior Scientist for the Fogarty Center for Global Health Studies, will step in as Acting Deputy Director for the Center. Dr. Sturke joined Fogarty in 2006 and oversees a portfolio of global projects that include a focus on building research capacity in implementation science in low- and middleincome countries (LMICs) and using innovative platforms to bring implementation science practitioners together with decision-makers and program implementers from LMICs. “We’re very pleased that Dr. Rachel Sturke is taking on the role of Acting Deputy Director,” said Dr. Kilmarx. “She is an exceptionally qualified global expert on implementation science and, having been with Fogarty since 2006, brings a wealth of institutional knowledge to the role.”
Celebrate with us: Fellows & Scholars at 20
Celebrate with us: Fellows & Scholars at 20
Fogarty’s flagship Global Health Fellows and Scholars program, now known as LAUNCH (Launching Future Leaders in Global Health Research Training Program), will celebrate its 20th Anniversary in 2023. To mark the occasion, Fogarty invites current and former fellows, scholars, principal investigators, and mentors, as well as Fogarty and NIH staff to join us for a commemorative event on the main NIH campus on April 13, 2023. Contact FICEvents@nih.gov for more information.
Fogarty’s flagship Global Health Fellows and Scholars program, now known as LAUNCH (Launching Future Leaders in Global Health Research Training Program), will celebrate its 20th Anniversary in 2023. To mark the occasion, Fogarty invites current and former fellows, scholars, principal investigators, and mentors, as well as Fogarty and NIH staff to join us for a commemorative event on the main NIH campus on April 13, 2023. Contact FICEvents@nih.gov for more information.
Fogarty’s flagship Global Health Fellows and Scholars program, now known as LAUNCH (Launching Future Leaders in Global Health Research Training Program), will celebrate its 20th Anniversary in 2023. To mark the occasion, Fogarty invites current and former fellows, scholars, principal investigators, and mentors, as well as Fogarty and NIH staff to join us for a commemorative event on the main NIH campus on April 13, 2023. Contact FICEvents@nih.gov for more information.
Fogarty’s flagship Global Health Fellows and Scholars program, now known as LAUNCH (Launching Future Leaders in Global Health Research Training Program), will celebrate its 20th Anniversary in 2023. To mark the occasion, Fogarty invites current and former fellows, scholars, principal investigators, and mentors, as well as Fogarty and NIH staff to join us for a commemorative event on the main NIH campus on April 13, 2023. Contact FICEvents@nih.gov for more information.
Celebrating former director, Dr. Roger I. Glass
Celebrating former director, Dr. Roger I. Glass
• An extraordinary career
FOCUS
• Goodbye as director, hello as emeritus
• An extraordinary career
Celebrating former director, Dr. Roger I. Glass
• Tributes
• Goodbye as director, hello as emeritus
• An extraordinary career
• Tributes
• Goodbye as director, hello as emeritus
• Tributes
Read More on pages 35-37
Read more on pages 6 – 9
Read more on pages 6 – 9
Read more on pages 6 – 9
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue FOCUS JAN/FEB 2023 Celebrating former director, Dr. Roger I. Glass • An extraordinary career • Goodbye as director, hello as emeritus • Tributes Read more on pages 6 – 9
Dr. Peter Kilmarx
www.fic.nih.gov
Inside this issue
FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES
2023
FOCUS JAN/FEB
GLOBAL
HEALTH MATTERS
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue
JAN/FEB 2023
GLOBAL
HEALTH MATTERS
Dr. Peter Kilmarx
www.fic.nih.gov FOGARTY INTERNATIONAL CENTER • NATIONAL INSTITUTES OF HEALTH • DEPARTMENT OF HEALTH AND HUMAN SERVICES Inside this issue
JAN/FEB 2023
FOCUS
Dr. Peter Kilmarx
34
30 Delaware Journal of Public Health - April 2023
Haiti combats cholera amid turbulence
Health workers in Haiti, facing a resurgence of cholera throughout the country, are making headway against the disease by scaling-up treatment centers, implementing oral rehydration points in high-risk communities, and conducting vaccination campaigns in the regions hit hardest.
Cholera, a diarrheal infection caused by eating food or drinking water contaminated with the Vibrio cholerae bacterium, is commonly treated with oral rehydration solution. Three WHO pre-qualified vaccines can prevent the disease.

“The big picture is that we are in a better place than we were at the beginning of the outbreak and, while things are still very difficult and very complicated, I think we've made progress,” said Dr. Vanessa Rouzier, Director of Research at GHESKIO, a Haitian-led non-profit. She and her co-author and colleague, Dr. Karine Severe, provided an update to their article, “Resurgence of Cholera in Haiti amidst Humanitarian Crises,” published in the New England Journal of Medicine (NEJM) in December 2022.
Political chaos, catastrophic shortages
On October 1, 2022, the Haitian Ministry of Health reported a surge in cholera patients in Port-au-Prince. This is more than a decade after the devastating 2010 cholera epidemic which caused more than 10,000 deaths, explained Rouzier, Severe, and co-author Dr. Nadalette Alcenat. The current outbreak coincides with recent political chaos, gang violence, and a blockade of Port-au-Prince’s main port, leading to a “catastrophic shortage of food, potable water, and fuel,” they wrote.




“Today, the political chaos and the gang violence does remain, unfortunately, so we continue to work in a very challenging environment,” Rouzier told Fogarty. “The major difference being that fuel is available, even if it's with some amount of difficulty. It’s available, at least, in the capital city of Port au Prince.”
One negative change in the past few weeks is transmission of the disease has continued. At the time of the NEJM publication, eight out of the total 10 Departments (top level government administrative regions equivalent to states) had been affected, now all 10 Departments and the majority of the island nation’s population are
affected, said Severe. A total of 25,182 cases and 496 deaths had been reported as of January 19, 2023.
Despite challenges and setbacks, progress has been made. With greater access to fuel (at least in the capital), it has been easier to increase the number of cholera treatment centers, which provide care for those who are sick, noted Rouzier. GHESKIO has also begun to implement oral rehydration points, a highly successful intervention from the previous epidemic. “It’s within communities and staffed by people from the community. Because its within walking distance, you don't have to leave your area, which is often a challenge for security reasons, so you can start treatment early,” said Rouzier. Oral rehydration points are also a platform from which health professionals can conduct door-to-door sensitization, provide oral rehydration packages (salts) and hygiene kits (with chlorine tablets to decontaminate water) and offer counseling, explained Severe, adding, “It’s important for us to remain very alert to avoid another peak and further spread of this outbreak.”
Vaccines help to stop spread
The vaccination campaign started in December. Despite other cholera outbreaks ongoing in the world, Haiti was able to procure 1.7 million oral vaccines from the International Coordinating Group (ICG) that manages the global stockpile. So far, 1.1 million have been received and are being deployed in the West Department, encompassing Port-au-Prince, and the Center Department.
Finally, GHESKIO plans to partner with Agence Française de Développement, which has offered support at cholera epicenters requiring sanitation measures. This project is looking to collaborate with local mayoral offices on trash removal, cleaning of sewage systems in canals, and mobilizing the community to help decrease contamination and create access to safe water.
JANUARY/FEBRUARY 2023 2
Photo courtesy USAID 31
The petri dish on the left indicates a positive result for the Vibrio cholerae bacteria at the National Laboratory in Port-au-Prince, Haiti.
Delegates address health challenges at US-Africa summit
HHS hosted a roundtable on health equity and health systems strengthening with delegates from 12 African countries plus the African Union as part of the 2022 U.S.Africa Leaders Summit which took place in Washington, DC, in mid-December. Fogarty Acting Director Dr. Peter Kilmarx represented NIH and focused on the importance of health research as a key contributor to health infrastructure and the broader medical workforce. “The delegates were particularly energized around the research discussion and spoke favorably about research to address health challenges and develop evidence-based policies,” noted Kilmarx. Dr. Jennifer Troyer of the National Human Genome Research Institute (NHGRI), Dr. Francis Collins, former NIH Director now at NHGRI, and representatives from the National Cancer Institute (NCI) and the National Institute of Mental Health (NIMH) also attended. Delegates agreed on “the need for local capacity, new government commitment and investment in research as retention factors for top national talent,” Kilmarx added.

Building on the first summit, which took place in 2014, the second U.S.-Africa Leaders Summit covered topics from economic engagement and climate change to food security and health cooperation over three days. Among the several side events that took place was a roundtable on global partnerships for sickle cell disease (SCD) held at the Embassy of the Republic of Tanzania. Kilmarx and Collins, along with Dr. George Mensah from the National Heart, Lung, and Blood Institute (NHLBI), participated. Mensah gave an overview of the Sickle Pan-African Research Consortium (SPARCO), which was launched via an NHLBI grant in 2017. He also addressed how local partners and governments need to think about the sustainability of programs like SPARCO, after initial funding runs out. Dr. Julie Makani, principal investigator (PI) on SPARCO, emphasized how basic science research goes hand in hand with implementation science.
“Mechanisms of disease cannot be answered by shipping samples outside of Africa,” she said while adding that doing research into things like the genomics of SCD must hold equal importance as providing access to curative therapies.
Dr. Collins echoed this sentiment, “We have to do both— address current patient needs and conduct bold research.” An outpatient procedure to treat SCD not requiring an advanced degree to perform and done without expensive equipment is “the dream,” Collins said. However, a
reframing from “donorship” to “ownership” is required with African institutions and governments ensuring the sustainability of such initiatives. Collins referred to the Human Heredity and Health in Africa (H3Africa) and Harnessing Data Science for Health Discovery and Innovation in Africa (DS-I Africa) programs—in which grants went directly to African organizations resulting in new research networks, South-South collaboration, and diminished brain drain—as a model. At both the SCD event and the Ministerial Roundtable, Collins championed a concept developed by African scientists and H3Africa PIs Drs. Christian Happi, Ambroise Wonkam, and Nicola Mulder for African genomics centers of excellence throughout the continent, each focused on their particular interest whether it be pandemic preparedness, infectious diseases, or noncommunicable diseases like SCD. There are economic arguments in addition to ones for public health for such a venture, Collins said.
On the main agenda for the Summit was the “Partnering for Sustainable Health Cooperation” forum, hosted by Loyce Pace, Assistant Secretary for Global Affairs at HHS which included remarks by HHS Secretary Xavier Becerra, President Yoweri Museveni of Uganda, President Mokgweetsi Masisi of Botswana—who called out former Fogarty Fellow Dr. Sikhulile Moyo’s discovery of the omicron variant of COVID-19—and CDC Director Dr. Rachel Walensky. The forum also included two panels which addressed investment in public health initiatives and the expansion and strengthening of Africa’s health care workforce, including the Biden-Harris Administration’s Global Health Worker Initiative and USAID’s partnerships to accelerate primary health care in African nations.
3 JANUARY/FEBRUARY 2023
Photo: Fogarty International Center
Francis Collins (left) of NHGRI spoke about the importance of addressing current patient needs and conducting bold research at a roundtable held at the Tanzanian embassy.
32 Delaware Journal of Public Health - April 2023
PROFILE
Haitian TB researcher shifts focus to cholera outbreak
Haitian TB researcher shifts focus to cholera outbreak
“It has been extremely challenging for us,” is how Dr. Yvetot Joseph described the situation in Haiti in December 2022.
“It has been extremely challenging for us,” is how Dr. Yvetot Joseph described the situation in Haiti in December 2022.
Haiti is currently suffering a resurgence of cholera, an acute diarrheal illness often spread through contaminated water. The ongoing humanitarian crisis, political conflict, lack of fuel, and suffering economy in Haiti have exacerbated the current outbreak. The Haitian Ministry of Public Health has reported over 13,000 cases and over 280 deaths as of mid-December.
Haiti is currently suffering a resurgence of cholera, an acute diarrheal illness often spread through contaminated water. The ongoing humanitarian crisis, political conflict, lack of fuel, and suffering economy in Haiti have exacerbated the current outbreak. The Haitian Ministry of Public Health has reported over 13,000 cases and over 280 deaths as of mid-December.
Dr. Joseph joined the GHESKIO Clinical Trials Unit research team in 2015 as a research physician focusing on tuberculosis (TB) treatment for people living with HIV (PLWH). GHESKIO operates medical treatment and research centers in Port-au-Prince and other clinics around Haiti, and boasts the largest research center for HIV/AIDS and TB in the Caribbean. He completed his medical degree at the Université Notre Dame d’Haïti (UNDH) and postgraduate training in infectious disease and HIV/AIDS through a UNDH partnership with the University of Maryland, Baltimore.
Dr. Joseph joined the GHESKIO Clinical Trials Unit research team in 2015 as a research physician focusing on tuberculosis (TB) treatment for people living with HIV (PLWH). GHESKIO operates medical treatment and research centers in Port-au-Prince and other clinics around Haiti, and boasts the largest research center for HIV/AIDS and TB in the Caribbean. He completed his medical degree at the Université Notre Dame d’Haïti (UNDH) and postgraduate training in infectious disease and HIV/AIDS through a UNDH partnership with the University of Maryland, Baltimore.
As a research physician and coordinator at GHESKIO, Joseph has had to adapt to ensure trials are still completed despite the unforeseen challenges in Haiti over the last two years.
As a research physician and coordinator at GHESKIO, Joseph has had to adapt to ensure trials are still completed despite the unforeseen challenges in Haiti over the last two years.
In 2018 Joseph was accepted as a Fogarty Global Health Fellow in the Consortium of Vanderbilt, Emory, Cornell, and Duke (VECD), studying the association between successful TB treatment and the long-term mortality of those living with HIV. His mentors included Drs. Jean Pape, Karine Severe, and Dan Fitzgerald at the GHESKIO Centers in Portau-Prince. He says, “the mentorship and training I received while working on my Fogarty project taught me skills that have been extremely helpful in today’s climate.”
In 2018 Joseph was accepted as a Fogarty Global Health Fellow in the Consortium of Vanderbilt, Emory, Cornell, and Duke (VECD), studying the association between successful TB treatment and the long-term mortality of those living with HIV. His mentors included Drs. Jean Pape, Karine Severe, and Dan Fitzgerald at the GHESKIO Centers in Portau-Prince. He says, “the mentorship and training I received while working on my Fogarty project taught me skills that have been extremely helpful in today’s climate.”
From an early age, Joseph knew he would study HIV/ AIDS as he noticed the extreme stigma around the disease. During one of his first clinical rounds, a person living with HIV was abandoned at the hospital by his parents and the head nurse asked for help cleaning the patient’s bed sores. Though Joseph did not hesitate to care for the patient, his
From an early age, Joseph knew he would study HIV/ AIDS as he noticed the extreme stigma around the disease. During one of his first clinical rounds, a person living with HIV was abandoned at the hospital by his parents and the head nurse asked for help cleaning the patient’s bed sores. Though Joseph did not hesitate to care for the patient, his


Yvetot Joseph, M.D.
Yvetot Joseph, M.D.
Fogarty Fellow: 2018–2019
Fogarty Fellow: 2018–2019

U.S. institution: Weill Cornell Center for Global Health
U.S. institution: Weill Cornell Center for Global Health Foreign institution: GHESKIO Centers, Port-au-Prince, Haiti Research topic: Immune factors associated with recurrent tuberculosis in HIV-infected patients
Foreign institution: GHESKIO Centers, Port-au-Prince, Haiti Research topic: Immune factors associated with recurrent tuberculosis in HIV-infected patients
colleagues felt apprehensive about taking on the task. “I understood from that moment that I wanted to help improve these patients’ quality of life. I just remember their gratitude.”
colleagues felt apprehensive about taking on the task. “I understood from that moment that I wanted to help improve these patients’ quality of life. I just remember their gratitude.”
With little data available on the long‐term mortality after successful TB treatment in PLWH, approximately 816 patients were enrolled to participate in a 14-year longitudinal study (CIPRA HT-001) between 2005 and 2018. It was known that, with medication and prevention strategies, PLWH in Haiti were living longer, and while TB is preventable and curable, it has remained one of the leading causes of death among this population, accounting for about one‐third of all reported HIV‐related deaths. When analyzing the data from this cohort, they found that those successfully treated for TB had a better chance for a longer life span compared to those who were never diagnosed. While there is still much to learn about the underlying mechanisms associated with TB, the immediate recommendation based on this study is to implement aggressive measures for health promotion and disease prevention for people living with HIV.
With little data available on the long‐term mortality after successful TB treatment in PLWH, approximately 816 patients were enrolled to participate in a 14-year longitudinal study (CIPRA HT-001) between 2005 and 2018. It was known that, with medication and prevention strategies, PLWH in Haiti were living longer, and while TB is preventable and curable, it has remained one of the leading causes of death among this population, accounting for about one‐third of all reported HIV‐related deaths. When analyzing the data from this cohort, they found that those successfully treated for TB had a better chance for a longer life span compared to those who were never diagnosed. While there is still much to learn about the underlying mechanisms associated with TB, the immediate recommendation based on this study is to implement aggressive measures for health promotion and disease prevention for people living with HIV.
While Joseph hopes to continue this research, efforts at GHESKIO have shifted to focus on the current situation. As Haiti welcomes the first batch of cholera vaccines in the country, Joseph says that in the meantime, their strategy has been focused on educating the public on the signs of cholera and encouraging them to seek help.
While Joseph hopes to continue this research, efforts at GHESKIO have shifted to focus on the current situation. As Haiti welcomes the first batch of cholera vaccines in the country, Joseph says that in the meantime, their strategy has been focused on educating the public on the signs of cholera and encouraging them to seek help.
Joseph will soon graduate from Cornell with a Master of Science in Clinical Research and plans to pursue his Ph.D. in the very near future. He says, “I am grateful for the mentors I have met through my Fogarty project and the opportunities it has opened for me.”
Joseph will soon graduate from Cornell with a Master of Science in Clinical Research and plans to pursue his Ph.D. in the very near future. He says, “I am grateful for the mentors I have met through my Fogarty project and the opportunities it has opened for me.”
4
PROFILE
4
33
WARANUCH PITIPHAT, DDS, MPHM
Waranuch Pitiphat, Dean and Associate Professor at Khon Kaen University in Thailand, also serves on the Board of Directors of the DeRouen Center for Global Oral Health at the University of Washington in Seattle. She earned her DDS from Chulalongkorn University, MPHM from Mahidol University, followed by a MSc and ScD in Epidemiology from Harvard University. Dr. Pitiphat is a former president of the Thai Society of Public Health Dentistry and the Asian Academy of Preventive Dentistry and executive member of Thailand’s Royal College of Dental Surgeons. She has authored more than 80 papers published in peer-reviewed journals and serves as editorial board member for several reputable journals.

Why did you become a dentist and a researcher?
Dentistry is one of the professions that helps people. We do good deeds every day we work. I started at Khon Kaen University in the Community Dentistry Department, where we conducted research in the field, and this included providing dental treatment to villagers. As I became more aware of dental public health, I wanted to learn more about epidemiology and biostatistics. Epidemiology is very exciting. I felt like a detective trying to find the causes of disease. Conducting clinical and epidemiological research, I combine my wish to help people with my love for biostatistics and epidemiology.
What are you working on now?
My current project continues the work of Dr. Timothy DeRouen of the University of Washington in Seattle, who began to build capacity for oral health research in Thailand in 2006. Over the years, he partnered with me at Khon Kaen University and others to provide research training for dentists first in Thailand and then other Southeast Asian countries. Over 15 years and three Fogarty grants, we have educated almost 300 trainees.
Today I am principal investigator (PI) for the same program (funded mainly by NIDCR). To sustain research within the region, we are building and utilizing a network of our own and have created a training program with five levels. The first level is an annual five-day workshop on clinical research methods conducted in the Southeast Asian region. It’s similar to what we’ve done in the past, but we’ve added e-modules of background material for the trainees and the courses are taught mainly by lecturers from our own region, with some help from the U.S. The second level takes place at the University of Washington and consists of their long-standing Summer Institute in Clinical Research Methods. Due to COVID-19, we’ve been conducting this online for the past couple of years, but this March we’ll send participants to gain
additional experience in Seattle. The third level is a fourmonth training program in research methodology and biostatistics offered annually at Khon Kaen University in Thailand. The fourth level provides each dentisttrainee with an opportunity to do non-degree research in their own country. Each has one local mentor, one mentor in Thailand and one mentor in the U.S., which gives them a chance to work internationally and improve their knowledge of research… and English! The final level supports dentists from Southeast Asia to pursue a doctorate in Oral Sciences in Thailand.
Why is regional oral health research important?


Oral health research is very young in Southeast Asia. With a population of over 650 million, our region is very large and very diverse, with different ethnicities, cultures and religions—including Islam, Christianity and Buddhism—among and within countries. We need region-relevant and country-specific research so that we can provide appropriate public health programs and plan prevention and treatment strategies for our populations.
Are you planning any other projects?
We are working on several oral health problems and trying to work with other countries in the region. In Thailand, we conducted a cohort study in infants to investigate the association of prolonged breastfeeding and early childhood caries (tooth decay). In the Philippines, we are conducting a study on caries risk assessment and evaluation of the risk factors for early childhood caries. We’ll be starting some work in Cambodia soon. We also have projects in Thailand and Vietnam focused on cleft lips and cleft palates. We’re also conducting clinical trials addressing various issues including the treatment of orofacial (oral and facial) pain. Geriatric patients are increasing in Southeast Asia and orofacial pain affects that population.
A&Q 5 34 Delaware Journal of Public Health - April 2023
FOCUS FOCUS
FOCUS FOCUS
The extraordinary career of Dr. Roger I. Glass
The extraordinary career of Dr. Roger I. Glass
On January 14, 2023, Dr. Roger I. Glass transitioned to senior scientist emeritus from his position as the longest-serving director of Fogarty International Center and associate director for international research at the National Institutes of Health. During his tenure, global health at NIH and on university campuses throughout the world has changed in visible and measurable ways. Fogarty was part of this change. Global health in the 20th century was grounded in infectious diseases and tropical medicine with smaller investments in maternal, neonatal and child health (MNCH), cancer, and other chronic diseases. Until the funding for HIV/AIDS grew, few of NIH’s 27 institutes and centers (ICs) had substantial interest or investments in the diseases and health problems effecting people in lowand middle-income countries (LMICs).
On January 14, 2023, Dr. Roger I. Glass transitioned to senior scientist emeritus from his position as the longest-serving director of Fogarty International Center and associate director for international research at the National Institutes of Health. During his tenure, global health at NIH and on university campuses throughout the world has changed in visible and measurable ways. Fogarty was part of this change. Global health in the 20th century was grounded in infectious diseases and tropical medicine with smaller investments in maternal, neonatal and child health (MNCH), cancer, and other chronic diseases. Until the funding for HIV/AIDS grew, few of NIH’s 27 institutes and centers (ICs) had substantial interest or investments in the diseases and health problems effecting people in lowand middle-income countries (LMICs).


In the U.S., interest in global health practice and research grew out of the PEPFAR program (the United States President’s Emergency Plan for AIDS Relief), the U.S. government’s largest investment to date in global health with funds provided to support treatment and prevention of HIV/AIDS.
In the U.S., interest in global health practice and research grew out of the PEPFAR program (the United States President’s Emergency Plan for AIDS Relief), the U.S. government’s largest investment to date in global health with funds provided to support treatment and prevention of HIV/AIDS.


Fogarty seized this opportunity, using the platform of PEPFAR to expand training of physicians and health personnel in LMICs to areas beyond HIV/AIDS. Fogarty engaged all 27 institutes and centers of NIH in its programs; today just under 90% of its grants receive co-funding from another IC. Furthermore, over the past 20 years, the Fogarty Global Health Fellows and Scholars Program, renamed LAUNCH, has provided research training for more than 1,400 students and fellows in the health sciences, both U.S. and foreign, in a wide variety of topics to start them on a pathway that might lead to productive careers in
Fogarty seized this opportunity, using the platform of PEPFAR to expand training of physicians and health personnel in LMICs to areas beyond HIV/AIDS. Fogarty engaged all 27 institutes and centers of NIH in its programs; today just under 90% of its grants receive co-funding from another IC. Furthermore, over the past 20 years, the Fogarty Global Health Fellows and Scholars Program, renamed LAUNCH, has provided research training for more than 1,400 students and fellows in the health sciences, both U.S. and foreign, in a wide variety of topics to start them on a pathway that might lead to productive careers in


global health research. The AIDS International Training and Research Program (AITRP) trained more than 5,000 foreign scientists experiential training in clinical research and trials.
global health research. The AIDS International Training and Research Program (AITRP) trained more than 5,000 foreign scientists experiential training in clinical research and trials.


Dr. Glass explained: “I spoke with directors of each NIH institute about diseases in their portfolios that might be best studied in LMIC populations, areas where the population experienced unusual exposures to infections, environmental pollution, or genetic background or where their conditions could be better studied due to issues in the delivery of care. I was suggesting to them that they ‘take their science to where the diseases were,’ the easiest way being to invest in a fellow in their field who was passionate about research and could benefit from mentors both at home and in the LMICs.”
Dr. Glass explained: “I spoke with directors of each NIH institute about diseases in their portfolios that might be best studied in LMIC populations, areas where the population experienced unusual exposures to infections, environmental pollution, or genetic background or where their conditions could be better studied due to issues in the delivery of care. I was suggesting to them that they ‘take their science to where the diseases were,’ the easiest way being to invest in a fellow in their field who was passionate about research and could benefit from mentors both at home and in the LMICs.”
Dr. Glass’ career as an epidemiologist began when he joined the Epidemic Intelligence Service (EIS) at the CDC (U.S. Centers for Disease Control and Prevention). “I did 12 epidemic investigations—snowstorm deaths; Native American railroad employees dying in the heat of Texas; fishermen dying in the hulls of their ships; low sperm counts among Chicano pesticide workers. They were all fascinating, all sparked my curiosity, and all were published.” Wanting to travel, Dr. Glass accepted an appointment to the International Center for Diarrhoeal Disease Research in Bangladesh (icddr,b) in 1979. “By serendipity, Jan Holmgren, who made the oral vaccine for cholera, lodged in the same guest house and for three and a half years, we worked together closely on cholera and rotavirus. He said the work
Dr. Glass’ career as an epidemiologist began when he joined the Epidemic Intelligence Service (EIS) at the CDC (U.S. Centers for Disease Control and Prevention). “I did 12 epidemic investigations—snowstorm deaths; Native American railroad employees dying in the heat of Texas; fishermen dying in the hulls of their ships; low sperm counts among Chicano pesticide workers. They were all fascinating, all sparked my curiosity, and all were published.” Wanting to travel, Dr. Glass accepted an appointment to the International Center for Diarrhoeal Disease Research in Bangladesh (icddr,b) in 1979. “By serendipity, Jan Holmgren, who made the oral vaccine for cholera, lodged in the same guest house and for three and a half years, we worked together closely on cholera and rotavirus. He said the work
Left to right: In 2009, Dr. Glass and Dr. Francis Collins (middle), attended the inaugural meeting of the Consortium of Universities for Global Health (CUGH). Also in attendance was Dr. Patricia Garcia (right). Middle: In 2014, Dr. Glass attended the graduation ceremony at the University of Global Health Equity (UGHE) in Kigali, Rwanda, with Drs. Agnes Binagwaho (left) and Paul Farmer (right). Right: Dr. Glass holds a Rwandan Ministry of Health document listing the health measures taken to prevent an Ebola outbreak.
35
Left to right: In 2009, Dr. Glass and Dr. Francis Collins (middle), attended the inaugural meeting of the Consortium of Universities for Global Health (CUGH). Also in attendance was Dr. Patricia Garcia (right). Middle: In 2014, Dr. Glass attended the graduation ceremony at the University of Global Health Equity (UGHE) in Kigali, Rwanda, with Drs. Agnes Binagwaho (left) and Paul Farmer (right). Right: Dr. Glass holds a Rwandan Ministry of Health document listing the health measures taken to prevent an Ebola outbreak.
I’d done on cholera would be suitable for a Ph.D. in Sweden, so I went to the University of Gothenburg and, over a period of nine months, I wrote up eight papers on the epidemiology of cholera and defended my thesis.”
Next, Dr. Glass joined the NIH’s laboratory of infectious diseases. “I spent three years focusing on the molecular biology of rotavirus with Dr. Al Kapikian, who made the first rotavirus vaccine.” Needing to grow, Dr. Glass returned to CDC as chief of the viral gastroenteritis unit at the National Center for Infectious Diseases. “I stayed for 20 years and trained EIS officers and laboratory scientists from around the world to work with rotavirus and other enteric viruses.”
“My years in Bangladesh underscored the devastating impact diarrhea had on children under 5,” observed Dr. Glass. In 2013 alone rotaviruses caused about 215,000 childhood deaths according to the WHO, predominantly in developing countries. Over three decades, Dr. Glass conducted field studies in India, Bangladesh, Brazil, Mexico, Israel, Russia, Vietnam, and China, documenting the epidemiology and enormous global burden of rotavirus. He also helped develop vaccines (and the protocols for their use) to prevent disease.
His exhaustive efforts paid substantial public health dividends. Today, more than 120 national immunization programs include rotavirus vaccines, significantly reducing diarrheal hospitalizations and deaths and improving the health of millions of children worldwide.
Dr. Glass joined Fogarty as director on March 31, 2006. During his 17-year tenure, he steered the center toward building partnerships between U.S. and lower resource country institutions, while supporting the career development of global health researchers and leaders at home and abroad. Researchers trained by Fogarty have enhanced global security through their involvement and leadership in response to the epidemics of HIV, Ebola, Zika and COVID-19.
As NIH’s associate director for international research, Dr. Glass established a productive collaboration with Dr. Francis Collins, then director of NIH. Together they partnered with PEPFAR to develop the Medical Education Partnership Initiative in Africa, helped launch the Consortium of Universities for Global Health, assisted NIH in joining the Global Alliance for Chronic Diseases, and, through the NIH Common Fund, supported both the Human Heredity and Health in Africa and the Harnessing Data Science for Health Discovery and Innovation in Africa programs. Dr. Glass helped bring Bill Gates to campus to deliver the David E. Barmes Global Health Lecture, which led to annual partnership activities between the philanthropist’s own organization and NIH.

Over the course of his career, Dr. Glass also worked at Mount Sinai Health System in New York City, Oxford University in England, the Sysin Institute in Moscow, and the WHO in Geneva. He has co-authored more than 600 papers and chapters. Along the way, he became fluent in French, Spanish, Portuguese, and Russian. Among his many honors, Dr. Glass received the 2015 Albert B. Sabin Gold Medal Award from the Sabin Vaccine Institute, and was inducted into the National Academy of Medicine. As an emeritus scientist, he hopes to expand engagement in global health, bolster equity and diversity in Fogarty programs, and support existing partnerships. He also plans to spend more time with his wife, Dr. Barbara Stoll, and his three children: Nina, Michael and Andy Glass.
“Being the director of Fogarty was an absolute joy; it is surely one of the best positions to support the training of future researchers and leaders in global health research. I sometimes feel that in my years at NIH and CDC, I never worked a day in my life.”
FOCUS ON COVID AWARDS 7 FOCUS ON AN AMERICAN SCIENTIST, ROGER I.GLASS
Left: Dr Glass speaks informally with Bill Gates (right), founder of Microsoft and the Gates Foundation. Right: In 2022, Dr Glass attended the second DS-I Africa meeting in Cape Town, South Africa. He met with Dr. Lulu Nair (left) of the South African Medical Research Council and Dr. Keymanthri Moodley (center) of Stellenbosch University. (Courtesy of Keymanthri Moodley)
36 Delaware Journal of Public Health - April 2023
Goodbye as director, hello as emeritus
Goodbye as director, hello as emeritus
Goodbye as director, hello as emeritus


 By Dr. Roger I. Glass
By Dr. Roger I. Glass
By Dr. Roger I. Glass
By Dr. Roger I. Glass
By Dr. Roger I. Glass
By Dr. Roger I. Glass
This position for the past 17 years has been a love affair: A love affair with the science, a love affair with the mission, a love affair with the people on this team and with our trainees in the field. When I was first asked to take on this role, I was hesitant and, for the first three months, I wasn’t sure whether I was suited for the position and whether I was going to stay. Very quickly I became enthusiastic about the mission and the center’s potential impact.
This position for the past 17 years has been a love affair: A love affair with the science, a love affair with the mission, a love affair with the people on this team and with our trainees in the field. When I was first asked to take on this role, I was hesitant and, for the first three months, I wasn’t sure whether I was suited for the position and whether I was going to stay. Very quickly I became enthusiastic about the mission and the center’s potential impact.
This position for the past 17 years has been a love affair: A love affair with the science, a love affair with the mission, a love affair with the people on this team and with our trainees in the field. When I was first asked to take on this role, I was hesitant and, for the first three months, I wasn’t sure whether I was suited for the position and whether I was going to stay. Very quickly I became enthusiastic about the mission and the center’s potential impact.
The foundation for all I’ve done here at Fogarty was laid at CDC, where I understood that I needed to build people. You have to engage people’s intellect in the science with a mission that is important. If you train people, the return on investment is a career. Fogarty has launched nearly 1,500 fellows and scholars into global health research careers. Many have already done amazing things and all of them will have another 20 or 30 years to grow. To me the greatest joy is to go to an international meeting and have people come up to me, and say, “I was a Fogarty trainee, and I did this.” The footprint of the thousands of people we have trained is our contribution to global health.
The foundation for all I’ve done here at Fogarty was laid at CDC, where I understood that I needed to build people. You have to engage people’s intellect in the science with a mission that is important. If you train people, the return on investment is a career. Fogarty has launched nearly 1,500 fellows and scholars into global health research careers. Many have already done amazing things and all of them will have another 20 or 30 years to grow. To me the greatest joy is to go to an international meeting and have people come up to me, and say, “I was a Fogarty trainee, and I did this.” The footprint of the thousands of people we have trained is our contribution to global health.
The foundation for all I’ve done here at Fogarty was laid at CDC, where I understood that I needed to build people. You have to engage people’s intellect in the science with a mission that is important. If you train people, the return on investment is a career. Fogarty has launched nearly 1,500 fellows and scholars into global health research careers. Many have already done amazing things and all of them will have another 20 or 30 years to grow. To me the greatest joy is to go to an international meeting and have people come up to me, and say, “I was a Fogarty trainee, and I did this.” The footprint of the thousands of people we have trained is our contribution to global health.
Terms I’ve always thought are wonderful for Fogarty are “nimble” and “small but mighty,” because we are the smallest institute at NIH, yet we punch above our weight. We do this by working with our friends. We can’t do what we do alone, so we’ve changed the paradigm, we’ve changed the panorama and now all the different institute directors see our dynamic, our community spirit, and they want to contribute. My vision for the world is that, in a decade or so, scientists will be more fluid in how they conduct research, and we will all
Terms I’ve always thought are wonderful for Fogarty are “nimble” and “small but mighty,” because we are the smallest institute at NIH, yet we punch above our weight. We do this by working with our friends. We can’t do what we do alone, so we’ve changed the paradigm, we’ve changed the panorama and now all the different institute directors see our dynamic, our community spirit, and they want to contribute. My vision for the world is that, in a decade or so, scientists will be more fluid in how they conduct research, and we will all
Terms I’ve always thought are wonderful for Fogarty are “nimble” and “small but mighty,” because we are the smallest institute at NIH, yet we punch above our weight. We do this by working with our friends. We can’t do what we do alone, so we’ve changed the paradigm, we’ve changed the panorama and now all the different institute directors see our dynamic, our community spirit, and they want to contribute. My vision for the world is that, in a decade or so, scientists will be more fluid in how they conduct research, and we will all
work together to solve the world’s problems. We have no monopoly on good brains.
work together to solve the world’s problems. We have no monopoly on good brains.
work together to solve the world’s problems. We have no monopoly on good brains.
I look forward to remaining here at Fogarty as senior scientist emeritus on a regular-irregular basis. I plan to contribute as a mentor and by helping others, while addressing diversity and equity, expanding engagement in global health, and reinforcing our existing partnerships. I also want to work on challenges that remain in my own rotavirus projects. Seventeen years after we have new vaccines, only half the children in the world are vaccinated. We've done better with COVID-19 than with rotavirus, which is still the number one killer of children.
I look forward to remaining here at Fogarty as senior scientist emeritus on a regular-irregular basis. I plan to contribute as a mentor and by helping others, while addressing diversity and equity, expanding engagement in global health, and reinforcing our existing partnerships. I also want to work on challenges that remain in my own rotavirus projects. Seventeen years after we have new vaccines, only half the children in the world are vaccinated. We've done better with COVID-19 than with rotavirus, which is still the number one killer of children.
I look forward to remaining here at Fogarty as senior scientist emeritus on a regular-irregular basis. I plan to contribute as a mentor and by helping others, while addressing diversity and equity, expanding engagement in global health, and reinforcing our existing partnerships. I also want to work on challenges that remain in my own rotavirus projects. Seventeen years after we have new vaccines, only half the children in the world are vaccinated. We've done better with COVID-19 than with rotavirus, which is still the number one killer of children.


I've begun traveling again and, in these past eight months, I’ve had the chance to think about all we’ve done. We are better off than we’ve ever been. We have strength, we have friends, we have a rising budget—and we have a wonderful staff. Now is the best time to turn over the reins to Peter Kilmarx, who has brought so much seniority and wisdom to the institute. It’s the right moment to leave the center in his capable hands.
I've begun traveling again and, in these past eight months, I’ve had the chance to think about all we’ve done. We are better off than we’ve ever been. We have strength, we have friends, we have a rising budget—and we have a wonderful staff. Now is the best time to turn over the reins to Peter Kilmarx, who has brought so much seniority and wisdom to the institute. It’s the right moment to leave the center in his capable hands.
I've begun traveling again and, in these past eight months, I’ve had the chance to think about all we’ve done. We are better off than we’ve ever been. We have strength, we have friends, we have a rising budget—and we have a wonderful staff. Now is the best time to turn over the reins to Peter Kilmarx, who has brought so much seniority and wisdom to the institute. It’s the right moment to leave the center in his capable hands.
FOCUS ON AN AMERICAN SCIENTIST, ROGER GLASS
Left: Dr. Tikki Pang (left), WHO's Director of Research Policy at the time, and Dr. Glass. Right: Dr. Roger Glass addresses the annual meeting of the Consortium of Universities for Global Health, established in 2008.
“
To me the greatest joy is to go to an international meeting and have people come up to me, and say, “I was a Fogarty trainee, and I did this . ” The footprint of the thousands of people we have trained is our contribution to global health.
”
FOCUS ON AN AMERICAN SCIENTIST, ROGER GLASS
Left: Dr. Tikki Pang (left), WHO's Director of Research Policy at the time, and Dr. Glass. Right: Dr. Roger Glass addresses the annual meeting of the Consortium of Universities for Global Health, established in 2008.
“
To me the greatest joy is to go to an international meeting and have people come up to me, and say, “I was a Fogarty trainee, and I did this . ” The footprint of the thousands of people we have trained is our contribution to global health.
”
FOCUS ON AN AMERICAN SCIENTIST, ROGER GLASS
Left: Dr. Tikki Pang (left), WHO's Director of Research Policy at the time, and Dr. Glass. Right: Dr. Roger Glass addresses the annual meeting of the Consortium of Universities for Global Health, established in 2008.
“
To me the greatest joy is to go to an international meeting and have people come up to me, and say, “I was a Fogarty trainee, and I did this . ” The footprint of the thousands of people we have trained is our contribution to global health.
”
37
“Dr. Roger Glass’ commitment and leadership have enhanced and elevated Fogarty International Center nationally and internationally. His contributions to world health and his trailblazing are unparalleled. How proud my Dad would be of his exceptional stewardship of Fogarty.”
Mary McAndrew, daughter of Congressman John E. Fogarty, namesake of Fogarty International Center, and Chair, John E. Fogarty Foundation for Persons with Intellectual and Developmental Disabilities
His persistence and evidence-based approach to advocacy has built partnerships across the globe, the public health sector, and within NIH to launch new initiatives of highest priority.”
“Roger’s passion for promoting Fogarty has wisely extended beyond the traditional NIH circles to the broader community of societies and related organizations.”
Karen Goraleski CEO, American Society of Tropical Medicine and Hygiene
“Roger Glass is not only the longest serving Fogarty director but the most effective. His efforts to form new and impactful partnerships with both the public and private sectors are unparalleled.”
Gail Cassell, MD, Vice President, TB Drug Development, Infectious Disease Research Institute
“Roger Glass has been a real force and a beacon of hope for those of us working in developing countries. He has always been attentive to our needs and the multiple challenges we face.”
Jean William (“Bill”) Pape, MD Executive Director and founder, GHESKIO Centers
“What I have come to appreciate most about Roger is his passion and commitment for his work and the compassion he demonstrates towards the people he works with.”
Vikas Kapil, MD, Chief Medical Officer & Associate Director for Science, Center for Global Health, Centers for Disease Control and Prevention
“Roger is an exemplary American physician of whom the country is proud. His tenure as director of Fogarty has capitalized on his remarkable good humor, scientific rigor, and remarkable acceptance in countries around the world.”
J on Rohde, MD, former senior advisor, UNICEF and BRAC (Bangladesh Rural Advancement Committee); visiting scholar, Harvard T.H. Chan School of Public Health
“Roger has exhibited deep humility and constant optimism in the pursuit of advancing health equity. His commitment to equitable partnership, equity of opportunity, and to global scientific workforce and ecosystem development is to be applauded and has been the bedrock for his tenure at Fogarty.”
Trevor Mundel, MD, PhD, President Global Health, Gates Foundation
“Roger Glass has added an entirely new dimension to the ability of the NIH to interact at the global level in so many ways. One of the most important has been Fogarty’s highly successful training of international scientists who directly and indirectly have become true collaborators with NIH and even part of the NIH family.”
Anthony Fauci, MD, former director of NIAID
“Roger has been not only the director of Fogarty but so much more: a MENTOR; a VISIONARY LEADER; an ARCHITECT OF THE FUTURE OF GLOBAL HEALTH; and a GREAT ADVOCATOR of the importance of training people globally and investing in capacity building FOR A MORE INCLUSIVE AND EQUITABLE WORLD.”
Patty Garcia, MD, MPH, Dean, School of Public Health, Cayetano Heredia University, Peru; Former Minister of Health, Peru
“He is highly regarded across the globe for his deep commitment to those less fortunate – a commitment he turned into Fogarty Center training programs for African scientists and health care providers that have changed the face of the HIV response on the continent.”
Salim & Quarraisha Abdool Karim, PhDs, Directors, Center for the AIDS Program of Research in South Arcaro (CAPRISA); Vice-Chancellors, University of KwaZulu-Natal, South Africa
“It’s impossible to overstate the profoundly important contributions that Roger Glass has made to global health research. He has left a permanent and powerful imprint on NIH’s global health contributions.”
Francis Collins
MD, PhD, Science Advisor to the President; former Director, NIH
“Roger Glass helped to build capacity in the Global South, promoting research and elevating the academic standards of science everywhere. His actions will be remembered.”
Paulo Buss, MD MPH, PhD, Professor Emeritus, Oswaldo Cruz Foundation, Brazil
“The world has been made that much safer during Roger’s tenure as Director. The many individuals trained by Fogarty have become leaders who will continue to work to assure a healthier world in the years ahead.”
Mary Woolley, President, Research! America
TRIBUTES
Sten H. Vermund, MD, PhD, Dean and Anna M.R. Lauder Professor of Public Health, Yale School of Public Health
38 Delaware Journal of Public Health - April 2023
OPINION
By Dr. Peter Kilmarx, Acting Director, Fogarty International Center
Fogarty continues core programs and values
I was honored to be asked to serve as acting director of the Fogarty International Center and acting NIH associate director for International research while the search for a permanent director is ongoing. I’ve served as the deputy director for more than seven years and am very grateful to former Director Dr. Roger Glass for his leadership and mentoring in that time. I look forward to ongoing interactions with him in his new role as a senior scientist emeritus. I’m also very pleased that Dr. Rachel Sturke has agreed to serve as acting deputy director during this period of transition. She is a recognized global expert on implementation science and, having been with Fogarty since 2006, is exceptionally qualified to help keep us moving full speed ahead.
I know well the critical role played by Fogarty in advancing global health research and I am also well-acquainted with the extraordinary abilities and commitment of the Fogarty team. This is an exciting time with substantial challenges in global health but also major opportunities for global health research, partnership building, and capacity strengthening. Pandemic preparedness is a global imperative, with research training as a key component. We’ve seen firsthand how scientists who were trained with support from Fogarty contributed to and in some cases led the global response to COVID-19. Today, there remain significant unfinished research agendas for COVID-19 and also for longer-standing infectious disease scourges, including HIV/AIDS, malaria, and tuberculosis. We also plan to continue our support of the One Health concept, which takes a transdisciplinary approach to address zoonotic and vector-borne diseases, antimicrobial resistance, and other threats.
While I serve as acting director, we will also emphasize planetary health, which focuses on the already large and growing health impacts of human disruptions to earth’s systems, especially climate change, but also declining biodiversity, increasing pollution, and shortages of natural resources. I’m excited to represent Fogarty on the Executive Committee of the NIH Climate Change and Health Initiative, together with NIEHS and several other Institutes and Centers (ICs), developing NIH-wide initiatives to address this existential threat.
Another area I will continue to highlight is noncommunicable diseases. The impacts of chronic diseases, which include cardiovascular diseases (such as heart attacks and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma) and diabetes, have increased substantially in recent years, especially in low- and middle-income countries. They remain a priority area for Fogarty in collaboration with other NIH ICs, the Global Alliance for Chronic Diseases, and other partners. Many of these illnesses have overlapping risk factors, such as hypertension, high body mass index, high plasma glucose, and ambient air pollution, which are also increasing and so suggest important areas for research and intervention.
We will also press forward with critical cross-cutting areas. Implementation research—promoting the uptake of evidence-based policies and interventions— is needed for all fields to address persistent gaps between the promise of proven effective innovations and their successful implementation. We’re also seeing the promise of data science, digital health, and related technologies to address multiple health problems. Fogarty staff helped lead the NIH Common Fundsupported the Harnessing Data Science for Health Discovery and Innovation in Africa (DS-I Africa) and Mobile Health: Technology and Outcomes in Low- and Middle-Income Countries (mHealth) programs, both of which have significant interest from the scientific community and engagement with other NIH ICs.
Finally, I’m especially interested in the distinct but related issues of promoting equity in our global health research partnerships as well as linking efforts to address health disparities and engaging underrepresented populations in global health research in the United States and abroad.
Overall, we see strengthening research capacity in resource-poor settings as the most effective way to improve global health in the long run. Embracing diversity, equity, and inclusion as core values will help ensure our success in both the short and long term. I welcome your input during this pivotal time. Please get in touch at: ficinfo@fic.nih.gov.
10
39
UGHE names Jim Yong Kim chancellor

Dr. Jim Yong Kim, a Partners in Health (PIH) co-founder, was named chancellor of the University of Global Health Equity in Rwanda, a role previously held by the late Dr. Paul Farmer. Kim previously served as President of the World Bank Group, the President of Dartmouth College, and Director of the WHO HIV/ AIDS department.
WHO welcomes new chief scientist, nursing officer
Current Wellcome Trust Director Dr. Jeremy Farrar has been named chief scientist at WHO. Farrar, a clinical scientist, previously served as director of the Clinical Research Unit at the Hospital for Tropical Diseases in Vietnam prior to his role at Wellcome, where he has expanded the organization's global health outlook.
Dr. Amelia Latu Afuhaamango Tuipulotu has been named WHO’s chief nursing officer. Tuipulotu was the Kingdom of Tonga's first female Minister for Health and the first Tongan to receive a Ph.D. in nursing. In her new role, she will champion nurses and midwives to ensure their experience is utilized in strengthening global health systems.

Fiocruz director helms Brazil's health ministry
Dr. Nisia Trindade-Lima, former director of the Oswaldo Cruz Foundation (Fiocruz), is now the first woman to lead the Health Ministry in Brazilian history. During her tenure as director at Fiocruz, Trindade-Lima managed the construction of a hospital center for COVID-19 treatment and research and the development of tests to identify coronavirus variants.

Fogarty grantee joins JID editorial board

Dr. Igho Ofotokun of Emory University School of Medicine has been added to the Journal of Infectious Disease (JID) editorial board. Ofotokun currently serves as principal investigator on the Fogarty-funded Emory-Nigeria HIV Research Training Program. JID is the official journal of the Infectious Diseases Society of America.

Ugandan research physician receives Hakim award
Dr. Angel Nanteza, of Uganda’s Butabika Mental Health Hospital, is the 2023 recipient of the James G. Hakim Global Health Award for submitting the highest-ranked abstract to the Consortium of Universities for Global Health (CUGH) annual meeting. The award—established by Fogarty, CUGH, and AFREhealth in 2021—will provide travel support to CUGH meetings.
Nature launches open access for LMIC authors
Springer Nature announced that primary research from authors from World Bank-classified low- and middle-income countries (LMICs) accepted for publication in either Nature or one of the Nature research journals can now be published open access at no cost.
State to open health security bureau

U.S. Secretary of State Anthony Blinken announced his intent to establish the Bureau of Global Health Security and Diplomacy which will bring together several existing offices, including PEPFAR. He will ask current U.S. Global AIDS Coordinator, Ambassador Dr. John Nkengasong, to be the first head of the new bureau.
WHO releases health equity report
The Global report on health equity for persons with disabilities makes evidence-based recommendations for country-level actions to address gaps in health care and standards, including 40 targeted and comprehensive actions that countries can take to strengthen their health systems and reduce health inequities for persons with disabilities
Meharry announces Global Health Equity Institute
The Global Health Institute at Meharry Medical College will serve as the foundation for the first school dedicated to global public health at a historical Black college or university. Daniel E. Dawes, J.D., a health policy expert, researcher, and attorney, will lead the Institute. The school is set to open in 2026.
Lancet Global Health seeks guest editors
Lancet Global Health is looking for guest editors who are currently working in a global health field, preferably early-career to mid-career stage, and are based in an LMIC. This is one of various initiatives announced by the journal to honor their commitment to making global health research, publishing, and practice a more equitable and effective space.
HEALTH Briefs Global PEOPLE 11
40 Delaware Journal of Public Health - April 2023
Funding Opportunity Announcement Deadline Details
International Research Scientist Development Award (IRSDA)
K01 Independent Clinical Trial Required
K01 Independent Clinical Trial Not Allowed
Implementation Research on Noncommunicable Disease Risk Factors among Low- and Middle-Income Country and Tribal Populations Living in City Environments
R01 - Clinical Trial Optional
R61/R33 - Clinical Trial Required
International Bioethics Training
D43 Clinical Trial Optional
R25 Clinical Trial Not Allowed
For more information, visit www.fic.nih.gov/funding
Global Health Matters

January/February 2023
Volume 22, No. 1 ISSN: 1938-5935
Fogarty International Center National Institutes of Health Department of Health and Human Services
Managing editor: Judy Coan-Stevens Judith.Coan-Stevens@nih.gov
Writer/editor: Mariah Felipe Mariah.Felipe@nih.gov
Writer/editor: Susan Scutti Susan.Scutti@nih.gov
Digital analyst: Merrijoy Vicente Merrijoy.Vicente@nih.gov
Designer: Carla Conway
All text produced in Global Health Matters is in the public domain and may be reprinted. Please credit Fogarty International Center. Images must be cleared for use with the individual source, as indicated.
Scan and read this issue online

SUBSCRIBE: www.fic.nih.gov/subscribe
Mar 8, 2023
http://bit.ly/IRSDAK01
Mar 9, 2023
https://bit.ly/GACD_funding
Jun 6, 2023
http://bit.ly/BioethicsTraining
Partnership to publish cardiovascular disease dashboard annually
Cardiovascular diseases consistently top the list of leading causes of death worldwide. These diseases—heart disease, stroke, brain bleeds, aortic valve calcification (hardening), heart failure due to alcoholism, aneurysm (a ballooning in the wall of a blood vessel) and endocarditis (inflammation of the heart lining), among others—also contribute to loss of health and excess health system costs.
How do public health researchers keep abreast of changing regional trends in prevalence and impact? The Global Burden of Cardiovascular Diseases Collaboration, an alliance between the Institute for Health Metrics and Evaluation, the National Heart, Lung, and Blood Institute, and the Journal of the American College of Cardiology (JACC), provides answers.
Launched in 2020, this partnership has delivered a five-part region-specific series highlighting the distinct epidemiology of disease for East Asia, North America, South America, sub-Saharan Africa, and Western Europe. Yet in December, the cardiovascular disease collaboration announced a small, though significant change.
“Knowing that the global cardiovascular clinical and research communities desire these data with more frequency, it is our intent to publish results annually,” wrote Dr. Muthiah Vaduganathan and his co-authors in “The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health.” Going forward, annual estimates can be used to guide allocation and prioritization of resources for research, health care, and public health, suggested the authors.
JANUARY/FEBRUARY 2023
Photo courtesy of Vaduganathan M, et al., Journal of the American College of Cardiology
41
A map representing the global burden of cardiovascular diseases using Age-Standardized DALYs (disability adjusted life years).
Update on Medication Related Osteonecrosis of the Jaws
Barry C. Boyd, D.M.D., M.D., F.A.C.S.
Department of Oral and Maxillofacial Surgery and Hospital Dentistry, ChristianaCare
INTRODUCTION
Osteonecrosis of the jaws (ONJ) has emerged as a clinical condition with case reports appearing at least 20 years ago. Early cases were discovered in patients receiving treatment for primary and metastatic bone neoplasia as well as in those being treated for non-neoplastic conditions including osteoporosis and metabolic bone disease processes. Many of the reported cases involved patients treated with bisphosphonates and the term Bisphosphonate Related Osteonecrosis of the Jaws (BRONJ). Other terms later evolved including Antiresorptive agent Related Osteonecrosis of the Jaws (ARONJ) and more recently Medication Related Osteonecrosis of the Jaws (MRONJ). Patients in need of these medications receive much needed, highly effective treatment of primary and metastatic bone malignancies and osteoporosis, including improvement in survival as well as immeasurable improvements in quality of life. However rare, osteonecrosis—depending upon the severity—may have negative impacts upon quality of life for some.
CLINICAL FEATURES AND STAGES
Osteonecrosis of the jaws was first documented in case reports in the scientific literature dating back to 2003 and 2004. Since then the clinical entity has been studied extensively, but there remains much to be learned about the pathophysiology, and evidencebased treatment is still to be determined. At best, the etiology of the process is thought to be multifactorial. There are several hypotheses regarding the etiology of MRONJ, including bone remodeling inhibition, inflammation and infection, angiogenesis inhibition and soft tissue toxicity.1 Although much study has been devoted to role of antiresorptive agents in development of MRONJ, steroids, chemotherapy agents and compromises of the immune system are also associated with the process.2,3
The American Association of Oral and Maxillofacial Surgeons has convened panels of experts in the specialty that developed a position paper in 2007, with revisions in 2009, 2014 and most recently in 2020. The definition of MRONJ has remained constant since the first position paper and requires the following three criteria based on history and clinical examination:
1. Current or past treatment with antiresorptive therapy alone or in combination with immune modulators or antiangiogenic medications;
2. Exposed bone or bone that can be probed through an intraoral or extraoral fistula(e) in the maxillofacial region that has persisted for more than eight weeks; and
3. No history of radiation therapy to the jaws or metastatic disease of the jaws.
To aid diagnosis and prioritization of treatment, the AAOMS panelists developed a staging system (1 through 3) described in the 2009 position paper. In the 2014 position paper, a stage 0 was added (analogous to stage 0 of femoral head avascular necrosis
described in the orthopedic surgery literature). The stage 0 classification includes several non-specific symptoms without clinically evident bone exposure. Stages 1 through 3 remain unchanged in the most recent position paper.2
Stage 0 (Non-exposed bone)
• Odontalgia in absence of pulpal pathology
• Dull bone pain
• Sinus pain with possible antral mucosal or bone changes
• Trigeminal neurosensory alterations
• Intraoral or extraoral swelling
• Loosening of teeth in absence of periodontal pathology
• Alveolar bone resorption in absence of chronic periodontal disease
• Sclerotic trabecular changes or lack of new bone in extraction sites
• Osteosclerosis of alveolar bone and/or basilar bone
• Thickened lamina dura, sclerosis, obscuring of periodontal ligament space
Stage 1
Exposed necrotic bone or fistula that probes in asymptomatic patient with no evidence of inflammation or infection. May also have alveolar resorption, sclerotic trabecular patterns paucity of new bone in extraction sites and periodontal ligament space reductions
Stage 2
Exposed, necrotic bone or fistula that probes to bone with inflammation and or infection with symptoms. May also have radiographic signs described above.
Stage 3
Exposed, necrotic bone or fistula that probes to the bone with one or more of the following:
• Exposed, necrotic bone extending beyond alveolus to inferior border of mandible, antrum and zygoma (maxilla);
• Pathologic fracture;
• Extraoral fistulae;
• Oral antral/oral nasal communication; and/or
• Osteolysis to inferior border of mandible or maxillary sinus floor.
The bisphosphonates include orally administered alendronate risedronate and parenteral agents zoledronic acid and ibandronate. These agents directly inhibit osteoclast activity through several different mechanisms. They remain within bone for many years and have half-lives approaching ten years. The Receptor activator of nuclear factor Kappa-B ligand (RANK-L) denosumab is an antibody against RANK ligand which inhibits
Doi: 10.32481/djph.2023.04.009
42 Delaware Journal of Public Health - April 2023
bone resorption through osteoclast inhibition.1 In contrast to the bisphosphonates, RANK-L inhibitors do not bind to bone and inhibition of bone remodeling declines significantly after six months of withdrawal of therapy.2,3
PREVENTION
A multidisciplinary approach to prevention of ONJ is recommended by the AAOMS panel, including dental providers and medical providers who direct therapy with any of the associated agents. Optimization of overall health with special emphasis on dental health optimization is critical. Patient education must take place at all levels of care, including education on the risks of medication therapy and risks imposed by compromised oral health. Management of active periapical and periodontal inflammation prior to initiation of therapy with antiresorptive agents is preferred to minimize the need for extractions or other bone trauma after initiation of therapy.2 For patients requiring dentoalveolar surgery after initiation of antiresorptive therapy, several strategies have been employed including minimal access surgery, perioperative antibiotics, antimicrobial rinses and primary closure of extraction sites. The level of evidence to support the drug holiday concept is low and as such the panel has not been able to reach a consensus. The use of bone turnover markers to determine optimal timing of dentoalveolar surgery for patients on antiresorptive agents has not been validated.2 Patients receiving antiresorptive agents for nonmalignant conditions may proceed with dentoalveolar surgery with consideration of preventive strategies. Patients receiving antiresorptive agent for malignant conditions should avoid dentoalveolar surgery if at all possible. Consideration for root retention strategies should receive priority given the greater risks of MRONJ in this population.
TREATMENT
Treatment of MRONJ is based on clinical history, exam, stage of disease, and on overall patient health and risks imposed by the signs symptoms, as well as the risks and morbidity of the treatment. The most recent AAOMS Position Paper provides algorithms to guide decision making in care of the MRONJ patient. The guidelines emphasize shared decision making between providers, patients, and patient families to guide selection from non-operative versus operative management for stages 1 through 3. Non-operative approaches have merit in stable or resolving disease at all stages. For stages 2 and 3, risk/ benefit analysis with consideration of patient co-morbidity and surgical risk, as well as quality of life considerations must be weighed. Conversely, operative management at all stages has been recognized as a viable option to reduce progression of MRONJ and enhance patient benefit.
CURRENT AND FUTURE RESEARCH
The use of adjunctive agents in the management of MRONJ is the subject of current studies including the use of vitamin E and pentoxifylline. Teriparatide, recombinant parathyroid hormone has been evaluated in small randomized controlled studies of ONJ patients with clinical improvement seen in enrolled subjects reaching clinical significance.2,4 The use of dose reducing schedules, drug holidays and biomarkers in preventive strategies warrant future research efforts.
Dr. Boyd may be contacted at barry.c.boyd@christianacare.org.
REFERENCES
1. Aghaloo, T., Hazboun, R., & Tetradis, S. (2015, November). Pathophysiology of osteonecrosis of the jaws. Oral and Maxillofacial Surgery Clinics of North America, 27(4), 489–496. https://doi.org/10.1016/j.coms.2015.06.001
2. Ruggiero, S. L., Dodson, T. B., Aghaloo, T., Carlson, E. R., Ward, B. B., & Kademani, D. (2022, May). American Association of Oral and Maxillofacial Surgeons position paper on medicationrelated osteonecrosis of the jaws-2022 update. J Oral Maxillofac Surg, 80(5), 920–943 https://doi.org/10.1016/j.joms.2022.02.008
3 Fleisher, K. E., Janal, M. N., Albstein, N., Young, J., Bikhazi, V., Schwalb, S., Glickman, R. S. (2019, February). Comorbid conditions are a risk for osteonecrosis of the jaw unrelated to antiresorptive therapy. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 127(2), 140–150. https://doi.org/10.1016/j.oooo.2018.09.012
4. Sim, I. W., Borromeo, G. L., Tsao, C., Hardiman, R., Hofman, M. S., Papatziamos Hjelle, C., . . . Ebeling, P. R. (2020, September 10). Teriparatide promotes bone healing in medication-related osteonecrosis of the jaw: A placebocontrolled, randomized trial. J Clin Oncol, 38(26), 2971–2980 https://doi.org/10.1200/JCO.19.02192
43
Reconsidering Autonomy: Ethical Reflections from the Frontlines of IDD Dental Care
Andrew Swiatowicz, D.D.S., D.A.B.D.S.M., F.A.G.D. ChristianaCare; Swiatowicz Dental Associates
Brandon Ambrosino, M.T.S. Doctoral Candidate, Theology & Ethics, Villanova University
ABSTRACT
Ever since the first publication of Beauchamp and Childress’s landmark bioethics textbook, US healthcare has championed patient autonomy as the guiding principle of doctor/patient encounters. Although US bioethics seems to regard autonomy as sacrosanct and beyond questioning, we wonder whether dominant ways of understanding patient autonomy fail to consider the lived experiences of large swaths of disabled people who routinely interact with healthcare providers. Reflecting on our experiences treating and working with patients with intellectual and developmental disabilities (IDD), we interrogate and ultimately challenge the bioethical principle of autonomy by critically engaging with the philosophical ideas undergirding it, namely personhood, consent, and desire.
BACKGROUND
A few months ago, we had a 12-year-old patient visit our office for a cleaning. Like many of our patients, Billy (not his real name) is intellectually disabled. For the past decade, a major focus of our practice has been treating people with intellectual and developmental disabilities (IDD). This particular patient came to the office with his father, although many, especially adults, are brought to their appointments by other caregivers, such as guardians or employees at their group homes.
At the end of the cleaning, Dr. Andy asked Billy which flavor toothpaste he wanted applied to his teeth. “We have piña colada, chocolate, strawberry, or bubble gum.”
“Bubble gum!” Billy answered. As Dr. Andy started to open the toothpaste, Billy’s dad cut in.
“If you give him a list of choices, he’s just going to pick the last option.”
Billy’s Dad has always seemed to be a supportive and caring parent, and so we don’t want to criticize him. The comment did, however, feel dismissive. Billy was asked what he wanted and he answered. There was no reason to doubt that he was expressing his choice: perhaps it is usually the case that what he wants just happens to be the last option presented to him. That doesn’t make those choices any less “real.” But even if the father’s suggestion is correct that Billy is not really voicing his desire so much as parroting the last thing he hears, it is not the place of a healthcare provider to join Billy’s father in this judgment. People with disabilities are often not encouraged to speak up, to voice their needs and wants, to take up space. Doctors and dentists have a unique opportunity to care for IDD patients simply by choosing to engage them in friendly conversations, even about “trivial” issues. Perhaps Dr. Andy was the only person that day to ask Billy to speak up for himself. By asking Billy to participate in his care, Dr. Andy was not only empowering Billy to take ownership of his dental health — he was, for the onlooking father, modeling one way of interacting with Billy, one that takes as its point of departure a real interest in Billy’s desires.
Over the past few months, we’ve thought a lot about Billy, his simple request for a toothpaste flavor, and his father’s dismissive commentary on Billy’s choice. We’ve allowed this scene to provoke us into thinking about important questions about personhood, desire, consent, and authority. Although these concepts have been undertheorized, they all nevertheless converge in discussions of bioethics, even when they are not explicitly named. For instance, was Billy’s choice of toothpaste flavor truly reflective of his desire? Should his choice be ignored because “he’s just going to pick the last option?” Or should his choice be ignored because he’s a minor? Should Dr. Andy believe the father and give Billy a flavor other than bubblegum, since Billy didn’t really want bubblegum in the first place? Say the choice offered was weightier: a big filling or a crown? Should Dr. Andy even offer Billy those choices, or should he simply consult the father? The father, of course, is the agent authorized to offer consent on Billy’s behalf for his dental and medical treatments. But the father has just given Dr. Andy good reason to believe that he is not very interested in figuring out what his son wants. It is in the end the son who is Dr. Andy’s patient. And yet it is the son’s father who has authority to enact and withhold consent on his son’s behalf.
These ethical reflections are not simply abstract exercises for philosophers but are in fact practical concerns for doctors who treat IDD patients. The law and, to a lesser extent, bioethics have tried to offer a straightforward way out of this bind: patient autonomy is signified via informed consent, whether it is contractually enacted by the patient’s own signature or by the signature of someone authorized to offer it on the patient’s behalf. This, we have often been told, is the very foundation of the doctor/patient relationship.
Although Western bioethics seems to regard autonomy as sacrosanct and beyond questioning, we wonder if the dominant ways of understanding patient autonomy fail to consider the lived experiences of large swaths of disabled people who routinely interact with healthcare providers. What we offer in this essay are reflections on the limits of theories of patient autonomy, informed by encounters that Dr. Andy has had with IDD patients. This essay is exploratory and creative: we are imagining new ways-ofbeing with our most vulnerable patients, and we are inviting other healthcare experts to join us in these imaginings.
Doi: 10.32481/djph.2023.04.010
44 Delaware Journal of Public Health - April 2023
It should be noted that we are not arguing that bioethics ought to adopt two different definitions of autonomy, one for the disabled and non-disabled. Instead, we suggest that autonomy, precisely because it fails to attend to the full realities of persons with disabilities, is therefore not a good foundation for bioethics.
RETHINKING AUTONOMY
The American Dental Association Code of Ethics is based upon five principles: patient autonomy, nonmaleficence, beneficence, justice and veracity. Noting that these principles “can overlap each other as well as compete with each other for priority,” the ADA nevertheless insists that dentistry ought to be based upon these “fundamental principles,” which it claims is “the profession’s firm guideposts.”1 The first four of these principles form the foundation of contemporary medical ethics, particularly following Beauchamp and Childress’s classic 1979 text.2 Each principle is given its own chapter, beginning with autonomy. While the authors caution that all four principles must be carefully balanced, its first-place position in the discussion may give the impression that autonomy is the most important principle for healthcare workers to safeguard. As philosopher Rachel Haliburton points out, many bioethicists see autonomy as the “central value they need to defend,” and interpret and apply the other three principles in light of the first (p. 39).3 All roads lead back to patient autonomy.
But over-prioritizing patient autonomy in healthcare settings is problematic precisely because the concept of autonomy that many bioethicists and providers work with is often “narrow and undertheorized,” argues philosopher Susan Dodds (p. 216).4 Based on modern philosophical and legal understandings of personhood,
“the conception of autonomy used in bioethics is rationalistic, atomistic, and individualistic. It assumes something like an atomistic individual, making a choice wholly for herself or himself. It assumes that, paradigmatically, individuals are equally rational and able to reflect on complicated choices once given adequate information. It ignores the social circumstances and power relations that affect choice contexts.”4
Any talk about self-determination must take for granted some idea of self: who is it that is doing the determining? In healthcare settings, a self-determining person is assumed to be a rational individual who knowingly pursues her own good (even though we have scores of research clearly demonstrating that humans do not tend to act rationally). This assumption is reflected in the pride of place afforded to informed consent contracts: the individual whose name appears on the form has reached her own decision without undue interference by her healthcare provider.
And yet, this conception of personhood overlooks the myriad ways that every single one of us is always already inextricably bound up with other people. Just as there is no self-determination apart from self, there is no self apart from others. We become who we are only in relationship with other people. These relationships are not “add-ons” to an already formed self, but they are in fact constitutive of that very self.
Buddhist monk Thich Nhat Hanh offers the following example to explain what he calls “interbeing:”
“Looking into a flower, we can see that it is full of life. It contains soil, rain, and sunshine. It is also full of clouds, oceans, and minerals. It is even full of space and time. In fact, the whole cosmos is present in this one little flower. If we took out just one of these “non- flower” elements, the flower would not be there. Without the soil’s nutrients, the flower could not grow. Without rain and sunshine, the flower would die. And if we removed all the non-flower elements, there would be nothing substantive left that we could call a “flower.” So our observation tells us that the flower is full of the whole cosmos, while at the same time it is empty of a separate self-existence. The flower cannot exist by itself alone.”5
In fact, claims Hanh, this is the case with everything that exists: “everything relies on everything else in the cosmos in order to manifest— whether a star, a cloud, a flower, a tree, or you and me” (p. 14).5 We exist only in interrelationship. “To be is to interbe,” he concludes. Or as Simone Weil puts it, “To say ‘I’ is to lie” (p. 132).6
We believe the concept of interbeing undermines the very foundation of patient autonomy. The idea that an individual, independent substance which calls itself “I” shows up to a doctor’s office ready to make a decision completely unencumbered by any “outside influence,” so to speak, is not based on an accurate account of personhood. Patients and doctors inter-are. If bioethics is going to continue to take “autonomy” as its first principle, then the concept at the very least ought to be revised to reflect a thicker conception of persons — not as independent but interdependent, always already existing in relationship. If a person is constituted by her relationships, then any theorization of autonomy should have relationship at its heart.
Some ethicists, following the lead of feminist philosophers, have tried to reframe the concept of autonomy in the wake of metaphysical critiques of the human. They believe that while traditional bioethical notions of autonomy fall victim to modernist myths about personhood, there are nevertheless important features of autonomy that should be retained. Rather than throwing the baby out with the bathwater, so to speak, these ethicists propose that we think about autonomy in explicitly relational terms.
According to philosophers Carolyn McLeod and Susan Sherwin, relational autonomy involves “explicit recognition of the fact that autonomy is both defined and pursued in a social context and that social context significantly influences an agent has to develop or express autonomy skills” (p. 259-260). Autonomy is not “pre-loaded” into persons; it must be developed, rehearsed, and performed in the context of relationships. Rather than seeing autonomy as “an achievement of individuals,” relational autonomy makes “visible the ways in which autonomy is affected by social forces, especially oppression (p. 260).”7
Think about Billy selecting a toothpaste flavor. Had his father not invalidated his decision by dismissing it as a non-decision, Billy would have been given an opportunity to construct his own autonomy in a safe environment. As McLeod and Sherwin rightly note, “autonomy is based on self-trust,” without which “any agent would have little motivation to deliberate on alternative courses of action (p. 263).”7 Even though Billy’s father didn’t realize it, he — like Dr. Andy and the dental assistants in the room — was
45
participating in Billy’s autonomy. Instead of talking to Dr. Andy about Billy’s choice, the father could have talked to Billy about his own choice, maybe asking him why he chose the way he did, or telling him that he made a good choice, or reminding his son that he too likes bubblegum! All of these options would have assisted in Billy’s construction of self-trust, which is a minimum condition for any meaningful version of autonomy to be present. Instead, Billy was sent the message that his desires ought not be voiced, presumably because of assumptions about his intellectual state.
RELATIONAL AUTONOMY
Even though we believe that allowing Billy to voice his desires is important, we realize the stakes in the toothpaste flavor story are not very high. Often with our IDD patients, the stakes are much higher. As one of the only general dentists credentialed to treat IDD patients in the operating room, Dr. Andy regularly brings patients into surgicenters to provide them with dental care. Many of these patients require a great deal of support. It is often the case that Dr. Andy cannot perform routine exams until the patients are under general anesthesia. At that point, treatment needs must be assessed on the fly. If the patient requires extensive work, Dr. Andy will speak with the parents or caregivers before undertaking treatment.
Because these procedures take place in hospital settings, where priority is often given to the inflexible demands of bureaucrats and lawyers, healthcare providers tend to find themselves advocating on behalf of IDD patients to no avail. Hospital policies are often created by those who believe that “informed consent” is the only way a patient’s full agency can be respected. These misguided policies often put healthcare providers who work with IDD folks in very tough binds. Rather than serving our patients, we are made to feel that our primary responsibility is to obey hospital policies.
Here’s an example: Dr. Andy recently scheduled time to examine and treat an intellectually disabled patient who requires a great deal of daily support. On the morning of her procedure, Linda (not her real name) showed up to the hospital escorted by two caregivers who work with her every day in her group home. When the hospital asked if the state-appointed guardian was present to sign an informed consent form, the caretakers explained that Linda had been on a waiting list for a stateappointed guardian ever since her mother abandoned her when she reached 18 years old.
“So then this patient cannot consent to treatment,” a hospital representative said, sending the patient away. There was no reasoning with the hospital. There was no explaining to them what relational autonomy looked like. There was no explaining to them that the two women who spend daily time with the patient were well-positioned to help us interpret what Linda wanted. For that matter, there was no explaining to the hospital that human beings often express ourselves non-verbally, and that doing so does not mean that we are unable to communicate our desires, nor does it mean that we are unworthy of care.
In an essay reimagining autonomy in relational contexts, Catriona MacKenzie and Natalie Stoljar suggest we ought to think of autonomy “as a characteristic of agents who are emotional, embodied, desiring, creative, and feeling, as well as rational, creatures” (p. 21).8 Their conception of autonomy does not
foreground rationality — instead, rationality is included as a kind of afterthought. “Humans are so many things … and oh yeah, we’re sometimes rational.” A working conception of autonomy in IDD patients, especially nonverbal ones, doesn’t pretend that an informed consent signature is the only way to figure out what a patient wants. IDD people experience and communicate joy, displeasure, fear, and physical pain. It is up to providers and caregivers who are working with these populations to find new ways to attend to these experiences. This can only be done with time, by not rushing through appointments, by paying attention to nonverbal cues, by listening to the advice of caregivers who spend time with the patients. It’s also up to us to assume, unless we are given compelling evidence to the contrary, that our IDD patients want what most of our other non-disabled patients want: to live free of disease and pain.
We are aware that what we are suggesting could be criticized with accusations of paternalism — the idea that healthcare workers will always act in the patients’ “best interests” and therefore ought to be able to make unilateral decisions on behalf of their patients. But we’re not arguing that final healthcare decisions for IDD patients should be left up to one single person who has legal say over them; that is the hospital’s position. What we are suggesting is that because autonomy is relationally developed, enacted, and at times obstructed, autonomous healthcare decisions should be understood to be arrived at in the context of relationships between patients, caregivers, families, hospital staff, and yes, the treating physicians. While paternalism in healthcare contexts is a concern, it is less likely to occur when patients and the providers who treat them have ongoing relationships of care.
We cannot definitively say what Linda wants from Dr. Andy. She is nonverbal and has an autism diagnosis. What we do feel comfortable suggesting, though, is that whatever Linda wants will not suddenly change when the state appoints her a guardian. Whether or not she has a guardian to authorize her treatment, Linda will likely want the same thing we all want from dentists: help with our oral health. In equating informed consent with autonomy, the hospital has unfortunately confused authority with competence. A state-appointed guardian will have the authority to speak for Linda. It does not follow, however, that the guardian will have the competence to do so. It may well be the case that those who are most competent to advocate for and with Linda are those whose very voices the hospital chooses to ignore.
BEYOND AUTONOMY
So far in this essay, we’ve been reworking the concept of autonomy, perhaps realizing that US healthcare ethics and law are not going to rid themselves of principlism anytime soon. But we’d be remiss if we concluded without raising the question: Does patient autonomy add something important to healthcare? Put differently: Can healthcare be ethical without an explicit acknowledgment of patient autonomy?
For all of their flaws, many misguided bioethical accounts of autonomy seem to want to safeguard the belief that persons are not interchangeable, that they have unique desires which are fitting to their unique situations-in-life, and that these desires help them achieve their own flourishing. These ideas are worth preserving, especially in healthcare settings, but it’s possible to champion them without flattening them down to
46 Delaware Journal of Public Health - April 2023
a hospital-approved notion of “autonomy.” In fact, we already have a good concept to help us out: love.
What would it look like if the foundation of bioethics weren’t autonomy, but were instead a commitment to work for the good of our patients because we and they are mutually bound together in this world in love? Admittedly, love does not often feature in bioethical discussions. But that does not mean that love does not come to bear on doctor/patient encounters; it may just mean that healthcare and ethical professionals are simply not comfortable talking out loud about love. And why not? We are helping our patients lead happy, healthy, flourishing lives; we are caring for them and nurturing them; we are sharing in their joys and pains. Love, it seems to us, is a perfectly fitting word to describe these relationships of mutuality, compassion, and care.
According to Catholic ethicist Edward Vacek, “love is an emotional, affirming participation in the dynamic tendency of an object to realize its fullness” (p. 44).9 When dentists and healthcare workers participate in a patient’s movement toward their own flourishing, and when we do so with an awareness that we are emotionally involved with them, we love them. What is important to note about this definition is that it is serious about what “autonomy” tries (but often fails) to safeguard; namely, the belief that a person has unique desires, that these desires help “internally nudge” a person to his or her own flourishing, and that our responsibility is to help our patients continue along their way. Patients arrive to us already in motion; to love them is to help them continue that motion, and to be emotionally involved in their journey.
It is love, and not some universal concept of autonomy, that helps us navigate both Billy’s and Linda’s respective situations. It is love that attends to Billy’s toothpaste flavor option, that attends to the voice that announces itself in this choice, that encourages that voice to keep speaking up for itself. It is love that attends to Linda’s desire to be free of pain-inducing oral disease, that attends to the many ways she expresses her desires beyond words, that advocates alongside her as she makes her way through a healthcare system that does not always affirm her full personhood. And it is love, in the end, that shares Linda’s disappointment that she will not receive dental treatment because a panel of bioethicists somewhere decided what “autonomy” should always look like. Perhaps some will criticize us for suggesting that the bioethics guiding healthcare providers ought to be based in a difficultto-explain concept like “love.” But as we have tried to show, autonomy is a much more nebulous concept. It is much easier to determine whether a doctor has acted lovingly toward a patient than to figure out whether the consent form the doctor has collected truly reflects her patient’s desires.
CONCLUSION
In conclusion, we are not suggesting that the principle of autonomy in bioethics be replaced by love. What we are suggesting is that when healthcare providers allow love to guide their encounters with patients, the “heavy lifting,” so to speak, that autonomy pretends to be doing is no longer necessary. Nor are we suggesting that love should be a guiding principle only in healthcare providers’ encounters with disabled patients. What we are suggesting is that because some IDD patients require a lot of support, much of it visible, from families, friends, and
other caregivers, the love involved in these situations is more readily apparent to folks who are not accustomed to looking for it in healthcare settings. It is our hope that by calling attention to the love already inherent in many relationships between IDD patients and those who support them, we might encourage doctors and dentists to begin to think through important bioethical issues in ways that push beyond limited and limiting notions of autonomy and consent.
Dr. Swiatowicz may be contacted at delawaretoothdoctor@gmail.com
REFERENCES
1. American Dental Association. (2023). Principles of ethics and code of professional conduct.
https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/ about/ada_code_of_ethics.pdf
2. Beauchamp, T. L., & Childress, J. F. (1979). Principles of biomedical ethics. Oxford University Press.
3. Haliburton, R. F. C. (2014). Autonomy and the situated self: A challenge to bioethics. Lexington Books.
4. Dodds, S. (1999). Choice and control in feminist bioethics. In C. Mackenzie & N. Stoljar (Eds.). Relational autonomy: Feminist perspectives on autonomy, agency, and the social self. Oxford University Press.
5. Hanh, T. N. (2003). No death, no fear. Riverhead Books.
6. Weil, S. (1970). First and last notebooks, translated by Richard Rees. Oxford University Press.
7. McLeod, C., & Sherwin, S. (1999). Relational autonomy, selftrust, and health care for patients who are oppressed. In C. Mackenzie & N. Stoljar (Eds.) Relational autonomy: Feminist perspectives on autonomy, agency, and the social self. Oxford University Press
8. MacKenzie, C., & Stoljar, N. (1999). Autonomy refigured. In C. Mackenzie & N. Stoljar (Eds.). Relational autonomy: Feminist perspectives on autonomy, agency, and the social self. Oxford University Press.
9. Vacek, E. C. (1994). Love, human and divine: The heart of Christian ethics. Georgetown University Press.
47
Source: https://myhealthycommunity.dhss.delaware.gov/portals/flu/

Delaware reports 8,529 total flu cases
Delaware had 8,529 total flu cases from October 2, 2022 through January 7, 2023, according to the Division of Public Health (DPH). Additionally, there have been 64 flu-related hospitalizations for the season, and three flu-related deaths.
New weekly flu cases declined from 790 during the week of December 18 to 516 between Christmas and New Year’s Eve, and to 282 during the week of January 1.
DPH advises Delawareans 6 months of age and older to get their annual flu vaccine for protection against flu illness, hospitalization, and death. Visit flu.delaware.gov to find flu vaccine. For flu data, visit My Healthy Community
Pediatric invasive Group A streptococcal infections rose in fall of 2022
The Centers for Disease Control and Prevention issued a Health Advisory to notify clinicians and public health authorities that pediatric invasive Group A streptococcal infections (iGAS) increased between September to November, above what was seen in 2020 and 2021.
Seek immediate treatment for GAS illnesses including: pharyngitis (strep throat), rheumatic fever, streptococcal toxic shock syndrome, necrotizing fasciitis, and skin and soft tissue infections (including cellulitis).
New XBB.1.5 variant causes 70% of new COVID-19 cases in the Northeast
The Centers for Disease Control and Prevention (CDC) is closely watching the new XBB.1.5 variant that comprises greater than 70% of COVID-19 viruses in the Northeast. The first cases of XBB.1.5, which is believed to have originated in the U.S., were seen in Delaware in December

XBB.1.5 is thought to be more transmissible but not more virulent and it is not causing more severe illness. The CDC says getting the bivalent booster is important as variants continue to circulate. It should provide some protection against transmission, but mostly against more serious illness and outcomes. Delawareans ages 5+ who received the primary COVID-19 vaccine series are eligible for the bivalent booster if they are fully vaccinated and have not had a booster since August. Visit de.gov/boosters.


As of January 11, 2023, 643,835 Delawareans are fully vaccinated against COVID-19, 94,958 are partially vaccinated, and 173,916 received their bivalent booster doses, according to the Division of Public Health (DPH). For more data, visit the My Healthy Community data portal, which is now updated every Wednesday to be consistent with the CDC’s updated reporting structure. If there is a significant surge in cases, DPH will make more realtime data available.
December marked two years since the first patient in the United States received a COVID-19 vaccine. A recently published Commonwealth Fund study estimates that from December 2020 through November 2022, the U.S. COVID-19 vaccination program prevented more than 3.2 million additional deaths and 18.5 million additional hospitalizations. The modeling indicates that there would have been nearly 120 million more COVID-19 infections over that period and the vaccination program saved over $1.15 trillion in medical costs that would have been incurred otherwise in the United States alone.
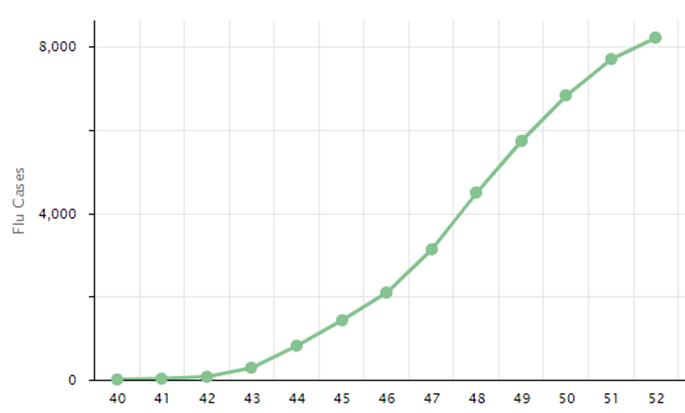
From the Delaware Division of Public Health January 202
48 Delaware Journal of Public Health - April 2023
Total Flu Cases, 2022-2023 Flu Season, Delaware, Weeks 40-51 (October 2, 2022-December 31, 2022)
U.S. adolescent overdose deaths rise 109%
The potency of drugs was a major contributing factor in the 109% increase in the median monthly drug overdose deaths among U.S. youth ages 10 to 19 years (adolescents) between July to December 2019 and July to December 2021, according to the Centers for Disease Control and Prevention (CDC). The CDC article, "Drug Overdose Deaths Among Persons Aged 10-19 Years - United States, July 2019-December 2021," was published in the December 16, 2022 Morbidity and Mortality Weekly Report.
The median monthly overdose deaths among U.S. adolescents involving illicitly manufactured fentanyl increased 182% from July to December 2019 to July to December 2021 During the same period, approximately 90% of U.S. adolescent overdose deaths involved opioids and 83.9% involved illicit manufactured fentanyl. According to the CDC, most youth who overdosed had no prior opioid use history. About 25% of the deaths included evidence of counterfeit pills. Approximately 41% of the youths who overdosed had a history of mental health treatment, diagnosed depression, or suicidal or selfharm behaviors.
The CDC urges parents to monitor adolescent behavior. DPH’s Office of Health Crisis Response, and the Division of Substance Abuse and Mental Health developed the toolkit, Talk2Kids About Drugs, which is available on HelpIsHereDE.com The site also offers treatment and recovery resources for youth struggling with a mental health or substance use disorder. Crisis intervention services for children under 18 are available 24/7 for parents and caregivers at 800-969-4357 or by texting DE to 741741.
All ages can call the Delaware Hope Line at 1-8339-HOPEDE for free 24/7 counseling, coaching, and support, plus links to mental health, addiction, and crisis services. To learn the warning signs of drug use and how to respond quickly to an overdose, register for a Narcan administration training at https://www.helpisherede.com/overdose-prevention

Prepare for winter power outages
Those who prepare for winter power outages should be able to cope better. Follow this advice from the Centers for Disease Control and Prevention:
• Make an emergency plan that includes a disaster supply kit of water, dried and canned food, and emergency supplies to last at least three days.
• Use battery-operated lanterns instead of candles to reduce the chance of a fire.
• Install a battery-operated or battery back-up carbon monoxide (CO) detector and smoke detector in your home. Make sure the batteries are working. CO is a colorless, odorless gas that can kill you. To prevent CO poisoning, only use generators, grills, and portable gas camp stoves outdoors. When generators are in use, they should be at least 20 feet away from the home. Never heat a home with a gas range or oven.
• Keep appliance thermometers in your refrigerator and freezer. The refrigerator should be at 40°F or below. The freezer should be at 0°F or below.

• During an outage, keep refrigerators and freezers closed. If the power has been out for four hours, put refrigerated perishable foods (meat, fish, cut fruits and vegetables, eggs, milk, and leftovers) in a cooler with ice, frozen gel packs, or dry ice and keep it at 40°F or below You can safely refreeze or cook thawed frozen food that still contains ice crystals or is at 40°F or below. Discard refrigerated perishable foods after four hours without power with no added cold source and if the temperature in the refrigerator or cooler falls below 40°F. If the freezer doors stay closed, food will stay safe for up to 48 hours in a full freezer or 24 hours in a half-full freezer.
• Throw away refrigerated medication when the power is out for a day or more, unless the drug label says otherwise or if a life depends on it
• Check with local authorities to be sure your water is safe. Bottled, boiled, or treated water is safe for drinking, cooking, and personal hygiene.
• Wear layers of clothing to keep in body heat and keep extra blankets on hand to prevent hypothermia, an abnormally low body temperature that is a medical emergency. Babies and older adults should not sleep in cold bedrooms.
The DPH Bulletin – January 2023 Page 2 of 2
CDC 49
The Mouth is the Mirror to the Body: Oral-Systemic Health
Roopali Kulkarni, D.M.D., M.P.H. Assistant Professor of Oral Medicine, School of Dental Medicine, Assistant Director of Postdoctoral Oral Medicine Program, University of Pennsylvania; Section Chief of Oral Medicine, ChristianaCare Hospital
Teeth do not just float about like objects in space. They are in fact attached to a person: a person with a unique background, experiences, and story. Although a clear division between dentistry and medicine has been created, the social determinants of health argue otherwise. Oral health and systemic health are intertwined, and all the various parts that make us who we are contribute to our health. Let’s discuss this, keeping in mind two of the most important dental instruments: the mirror and the explorer, with a reflection of our past and an excitement to venture into the future. The mouth is the mirror to the body and can reveal signs of underlying health issues. Thus, a teambased approach to care is needed to optimize patient health as we move into the next era.
This concept is not a new one. For over a century, healthcare has explored the relationship between periodontal disease and cardiovascular health, diabetes, among other conditions. Fast forward: in recent times, the Surgeon General’s report in 2000 called for more extensive research exploring the connection between oral health and systemic diseases and emphasized the importance of oral health. And now, as we collectively work towards Healthy People 2030, there are several goals surrounding oral conditions, with the understanding that a healthy mouth contributes to a healthy body. Nowadays, there are unique threats to maintaining a healthy body. People are living longer, and with our “aging” population, we have challenges we never faced before. Through the years, we have noticed a stark rise in chronic diseases, everything from dental caries to heart disease to cancer. Chronic diseases pose significant social, economic, and political burdens on society. Just as the mouth is the mirror to the body, healthcare is the mirror of society. How healthy a community is reflects closely on how that community is functioning. As the focus of public health is protecting and improving the health of communities, oral healthcare professionals focus on prevention to protect and improve the oral health of people. Although in existence for decades, oral medicine is now one of the newly recognized American Dental Association specialties. The field specifically focuses on chronic disease management, the diagnosis and management of medically related diseases affecting the oral and maxillofacial region, and dentistry for medically complex patients. Every day, we encounter the connection between oral and systemic health, seeing its effects on the patients we treat.
Many times, the mouth is the first sign of a systemic condition or even the only manifestation. In a traditional sense, we see systemic conditions that manifest orally, such as ulcerations in Crohn’s disease, dry mouth in Sjogren’s syndrome, or tissue inflammation in systemic lupus erythematosus. But we also see how oral and systemic health are connected through other parts of health, such as sleep, nutrition, and mental health. Oral healthcare professionals can help treat patients with sleep-related breathing disorders, such as obstructive sleep apnea. They may act on interdisciplinary teams to provide patients the ability to chew, swallow, and obtain adequate nutrition. They also work to create healthy smiles, which can correlate to reduction in mental illness.
Healthy mouths can also be negatively impacted by other conditions. Viruses, like human papillomavirus and COVID-19, can manifest orally. With the advent of vaccinations, we can work to lower the risk of certain cancers related to human papillomavirus, including oropharyngeal cancers, and lower the risk of mortality associated with COVID-19. Oral healthcare professionals are moving to the forefront of educating patients and increasing awareness of the importance of vaccination.
As we use our mirror to reflect, it is even more important to use our explorer to ask the question, how can we move forward? I believe in the power of integration, innovation, and interdisciplinary care. Integration of medicine and dentistry is key, with more open dialogue on patient care. Innovation comes in all forms, from research to the creation of clinical practice guidelines to technological advancements. Interdisciplinary approaches to care allow all expertise to be included. Collaboration, creativity, and community will push patient-centered care to the forefront. These tenants will also allow us to better explore how the health of the mouth and the health of the body are truly connected.
Dr. Kulkarni may be contacted at roopalik@upenn.edu.
Doi: 10.32481/djph.2023.04.011
50 Delaware Journal of Public Health - April 2023



LIVE proudly and confidently. Find out when you should get screened. DELAWARE HEALTH AND SOCIAL SERVICES Division of Public Health Bureau of Chronic Diseases Visit HealthyDelaware.org/ LGBTC ancer or call 2-1-1 for more information. Take control of your health. Get peace of mind from a cancer screening. The LGBTQIA+ community lives with a higher risk of cancer, but screenings can detect cancer early — when it’s most treatable.* Call your health care provider to schedule a cancer screening today. If you don’t have one, a nurse navigator can offer support and help schedule a cancer screening — even if you don’t have insurance. * Top Health Issues for LGBT Populations Information & Resource Kit, Substance Abuse and Mental Health Services Administration, 2012, https://store.samhsa.gov/sites/default/files/d7/priv/sma12-4684.pdf 51
Safety in the Dental Office
Louis K. Rafetto, D.M.D., M.Ed. Chairman, Oral and Maxillofacial Surgery Section, ChristianaCare Health System
INTRODUCTION
When patients attend an appointment in their dentist’s office, they assume that care will be performed in a safe and effective manner. This article will consider matters related to safety in dentistry, including how safe is the dental office, what are some of the causes of adverse events, and what can be done to allow limit the incidence and impact of adverse events in the dental office?
BACKGROUND
Attention began to focus on the issue of safety in healthcare in 1999 when the Institute of Medicine reported that between 44,000 to 98,000 deaths per year were due to “adverse events”.1 Despite efforts to identify ways to improve on this record, medical errors continue to be described as a leading cause of death in the U. S., emphasizing the serious nature and complexity of the problem. Most experts now recognize that adverse events and bad outcomes are generally not just the result of personal errors or “bad apples.” Rather, it seems that in many—if not most—cases, factors conspire in a manner that makes errors more likely to occur. This can be appreciated graphically by the “swiss cheese” model proposed by psychologist James Reason. Professor Reason also pointed out,
“Almost every day we choose whether or not to cut corners in order to meet operational demands. For the most part, such shortcomings bring no bad effects and so become a habitual part of routine work practices. It’s easy to forget to fear things that rarely happen. Unfortunately, this gradual reduction in systems safety margins exposes it to increasingly vulnerable accident-causing factors.”2
This statement emphasizes the need for constant vigilance on the part of all healthcare providers including the dental team.
HOW SAFE IS THE DELIVERY OF CARE IN THE DENTAL OFFICE?
The incidence of adverse events in the dental office is difficult to estimate, in large part because they generally have a limited impact on outcomes. Examples of common adverse events include operating on the wrong tooth; prescribing the wrong dose of a medication; or an inadvertent laceration of the tongue, lip, or buccal mucosa during an operative procedure. Studies attempting to quantify such adverse events differ in the method used for counting and often rely on self-reporting. Further complicating this matter is that there are no uniform requirements for reporting adverse events to state or other agencies, and that most events were managed without noticeable injury to the patient. For our purposes, it is safe to say that the incidence of adverse events in the dental office is not zero.
The area in which the most serious adverse events occur in dentistry is in the administration of anesthesia beyond that of local anesthesia. The California and Texas Dental Boards conducted five-year retrospective reviews of deaths or permanent
injuries associated with the administration of in the care of dental patients. The California Board’s review considered pediatric (21 years & under) anesthesia related deaths from 1/1/2010 –12/31/2015. It could not identify a reliable estimate of the number of patients treated (n) during this time interval. They were able to identify nine documented deaths. Of the nine cases, one occurred in an oral surgery office, and the rest in the offices of general dentists, pediatric dentists and itinerant dentist anesthesiologists. Three occurred in a hospital or surgical center and three were associated with local anesthesia overdose.
The Texas panel reviewed “major adverse events” (mortality or permanent morbidity) and “mishaps” (no permanent morbidity) investigated by the state dental board between 2011-16. Six cases were identified including five deaths and one brain injury. Two patients were adults, both of whom were medically compromised, and four were children, of which three were healthy and one had pre-existing cardiac disease. Four of the six cases involved secondary anesthesia providers including physician anesthesiologists and dentist anesthesiologists.
These two studies and others attempting to quantify serious events likely capture a fraction of the overall morbidity and mortality related to dental anesthesia, and suffer from the absence of a database that could provide a better estimate of incidence and prevalence.
Better data comes from the specialty of oral and maxillofacial surgery. For example, at the American Association of Oral and Maxillofacial Surgeons (AAOMS) Clinical Science Innovations in Oral and Maxillofacial Surgery meeting in April 2017,3 Thomas B. Dodson reviewed relevant outcomes studies in an effort to arrive at estimated death and adverse outcome rates. Together these studies suggest an estimated death rate of 1.5 per 1,000,000 anesthetics for the office-based team model in oral and maxillofacial surgery, although this seems unrealistically optimistic because of the method of collecting data in some of the surveys utilized.
WHAT ARE THE SOURCES OF ERRORS?
There are many potential sources of errors in the dental office. One way to consider sources of error in general comes from the work of Drs. Gorovitz and MacIntyre, who explored the nature of fallibility and proposed three major factors that play a role in leading to errors4:
1. Ignorance. Despite ongoing efforts, science affords a limited understanding of how complex things behave, making it difficult to predict when something adverse may happen.
2. Ineptitude. Even when knowledge / understanding is available, individuals / teams may fail to apply what they know or understand correctly.
3. Necessary Fallibility. Some things in the world of science and technology will never be fully understood, which they categorized as the problem of omniscience.
Doi: 10.32481/djph.2023.04.012
52 Delaware Journal of Public Health - April 2023
The first and second proposed reasons seem to be surmountable, and it is there that we must focus our attention as that is where we have some degree of control.
ELEMENTS THAT PREVENT OR MINIMIZE ADVERSE EVENTS
Since prevention of adverse events is critical, it is worth considering the value of four elements that have been demonstrated to limit the incidence and severity of adverse events in healthcare. These elements are:
1. A “culture of safety”,
2. Systems / routines that encourage safety,
3. The knowledge, skills and equipment necessary to provide safe care, and
4. Team preparation to effectively recognize and respond in the event of an adverse event (figure 1).
consultation with other experts. It is also important to recognize the limits of the office venue and equipment as well as the capabilities of the dental team before engaging in patient care.
Delivery of Care
The ability for any team to deliver care depends on having knowledgeable and well-trained individuals who function as team. Ongoing education should be a priority and targeted to grow and reinforce the knowledge and skills necessary to deliver safe and effective care. These educational activities should lead to the development of good clinical judgment. There are diverse forms of continuing education available, ranging from webinars and other forms of distance learning, to in-person lectures and workshops, to experiential offerings that encourage feedback and give and take with participants. The same level of priority should also apply to having the necessary instruments, equipment, and protocols in place to support care delivery. The team must function in a manner that supports one another, recognizing the value of each person in the quest for the whole to be greater than the sum of its parts. Training must include all members of the clinical and clerical staff.
Preparation: Recognition and Response to Adverse Events
The dental team should be on the alert for the possibility of an adverse event occurring and all members empowered to speak up when then identify such. Because adverse events cannot be completely eliminated, the team must be trained and current in recognition and management of crisis events. In that effort, regular and realistic mock drills should be conducted, targeted to address a wide variety of potential adverse events.
THE ROLE OF KNOWLEDGE AND PERFORMANCE
Culture of Safety
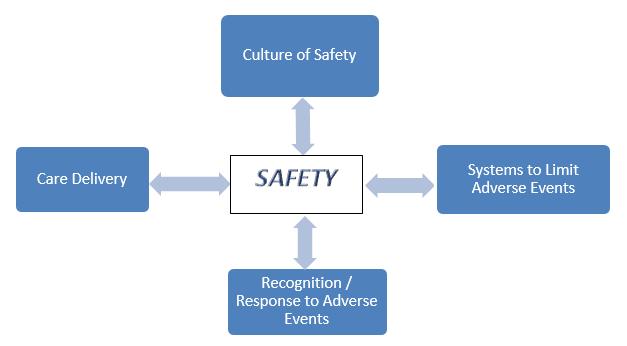
It is fundamental to support an environment that values and emphasizes the importance of working together as a team in the effort to ensure safety of patients and fellow team members. The words of W. Timothy Gallwey reflect the importance of embracing a mindset that prioritizes matters like safety when adopting an office identity:
“Take a moment to reflect on what you pursue in the name of ‘success.’ Clarity about your purpose informs all the other decisions in your life. Without clarity, nothing keeps you from pursuing ends not aligned with your core desire and lose yourself in the process.”5
Systems to Limit Adverse Events
Every office should have systems or routines in place that make it hard to do the wrong thing and easy to do the right thing. One such routine to identify potential risks is the time-honored “time out,” intended to be performed before beginning any procedure to confirm core elements such as the patient’s name, the planned procedure, the site of the procedure, changes in medical history, etc.6 While some adverse events are associated with performance of a procedure, such as aspiration of an instrument or crown, attention should also be paid to identifying in advance potential medical and physical constraints that may impact the safe delivery of care. Doing so might indicate the need for
It is important to recognize that both knowledge and skills decline over time. For example, in Resuscitation (2008), Smith, Gilcrest and Pierce reported that Advanced Cardiac Life Support (ACLS) skills degrade faster than Basic Life Support (BLS) skills.7 They considered 133 subjects trained in ACLS and BLS and found that only a percentage could pass the course three or twelve months later (table 1).
While there are numerous courses, books, and other resources available to help in the effort to obtain and update this base of knowledge, another excellent reference to grow knowledge are guidelines issued by related organizations in an effort to improve and standardize patient care. An example is the AAOMS Parameters of Care, Clinical Practice Guidelines for Oral and Maxillofacial Surgery 8 After obtaining the necessary knowledge base, teams should establish a written plan (protocol) that concisely summarize keys to the recognize and manage adverse events.
The ability to deliver care in a safe manner requires not only knowing what to do (knowledge), but also the ability to put acquired knowledge and skills to work (performance).
Figure 1. Four Elements that Limit Adverse Events in Health Care
Passed BLS Skills Training Passed ACLS Skills Training 3 Months 12 Months 3 Months 12 Months 63% 58% 30% 14%
Table 1. Skill Declination
53
Making decisions and performing under pressure is never a simple undertaking, particularly given the emotions and complexity inherent in crisis situations. Pressure occurs when a person is attempting to do something they are not sure they are capable of. The further they are from the familiar, the further away they are from being comfortable and confident. This applies to everything we do in life. A multi-year study of the top 10% of 12,000 athletes and business leaders using 360-degree multiple rater assessments revealed that:
1. Pressure adversely impacts cognitive success,
2. Pressure downgrades behavioral skills,
3. Pressure makes people perform below their capacity, and
4. Pressure is often camouflaged.9
Given the above, it is important that the team adopt a productive mindset. Such a mindset is often referred to as being in the zone. One way to encourage entering the zone of performance is to use tools commonly employed by sports psychologists (mental skills) to enhance performance. An example of mental skill training is to use imagery, a form of rehearsing in advance in a manner that encourages people to visualize / live through a potential adverse event in advance. Mock drills are a form such practice / rehearsal.
Mock Drills
Once an adverse incident is triggered, the best chance of a successful outcome occurs when there are well-trained people and systems in place to recognize and respond effectively. While simulators provide the best method for conducting mock crisis experiences, they are not yet readily available and/or affordable for most. The next best approach is mock drills.
Properly conducted, mock drills allow team to practice in advance of the real thing, so that if and when a crisis occurs, members of the team are more capable in their role in the response process. The familiarity and confidence that can result from having practiced for such events equips them to embrace the challenge when it presents itself, rather than allowing the challenge to control the moment. Mock drills should be realistic, immersive learning experiences that support:
1. Identification of shortcomings
• Were communications clear?
• Were roles and responsibilities understood?
• Were the appropriate resources available?
• What errors were made?
• What went well?
2. Implementation of strategies to solve them.
• Use the “1-2-3 approach”:
1) Tell, 2) Show, and 3) Do.
3. Revision of protocols to improve team performance.
Tips for Effective Crisis Management
Important strategies to practice during mock drills and to employ during an adverse event include:
1. Call for help early,
2. Mobilize resources,
3. Allocate attention wisely,
4. Use all available information,
5. Communicate effectively, and
6. Act as a team.
Failure to speak up because of fear of being wrong or intimidated, failure to confirm communication (not closing the loop), and neglecting to include key facts are common errors in communication. Clear, unambiguous language is preferable during all adverse events, avoiding implied or and inferred communication.
Another approach to consider in the management of adverse events is to follow the acronym “STOPAR:”
S - Stop (control anxiety and fear),
T - Think (get organized),
O - Observe (identify key factors / avoid denial),
P – Plan,
A - Act (deliberate and decisive actions), and
R - Revise / Reassess
CONCLUSIONS
Perhaps the most important single thing to limit adverse events and enhance safety in the dental office is to foster a culture of safety. In addition, every office should employ an ongoing process to monitor and evaluate clinical performance, patient outcomes, and adverse events in the effort to support continuous performance improvement and ensure the best opportunity for favorable outcomes. Further, having productive systems/ routines in place give the dental team the best chance to do the right thing and avoid doing the wrong thing. Finally, given that unanticipated adverse events do occur, the team should be properly prepared to recognize and respond in a timely and effective manner. This is best accomplished by conducting regular, realistic mock drills that can help to identify areas needing improvement as well as equip the team to respond in an effective manner should such an event take place.
One final note: going forward, it will be important for the dental community to make a concerted effort to improve their safety data base and work to standardize reporting requirements of adverse or “near miss” events.
Dr. Rafetto may be contacted at lkrafetto@gmail.com
REFERENCES
1. Donaldson, M. S., Corrigan, J. M., & Kohn, L. T. (Eds.). (2000). To err is human: building a safer health system. Washington, DC: National Academies Press.
2. Gawande, A. (2001). Complications, a surgeon’s notes on an imperfect science. http://picadorusa.com
54 Delaware Journal of Public Health - April 2023
3. Bouloux, G. F., Aghaloo, T., Campbell, J. A., Chou, J., Edwards, S. P., Kademani, D., . . . Peacock, Z. (2020, Mar). Proceedings from the clinical and scientific innovations in oral and maxillofacial surgery conference 2019. J Oral Maxillofacial Surg, 78(3), 327-334.
https://doi.org/10.1016/j.joms.2019.11.006
4. Gorovitz, S., & MacIntyre, A. (1975, December). Toward a theory of medical fallibility. The Hastings Center Report, 5(6), 13–23. Retrieved from https://philarchive.org/archive/GORTAT-11
https://doi.org/10.2307/3560992
5 Gallwey, W. T. (2001). The inner game of work: Focus, learning, pleasure, and mobility in the workplace. New York: Random House
6 Haynes, A. B., Weiser, T. G., Berry, W. R., Lipsitz, S. R., Breizat, A. H. S., Dellinger, E. P., Gawande, A. A., & the Safe Surgery Saves Lives Study Group. (2009, January 29). A surgical safety checklist to reduce morbidity and mortality in a global population. The New England Journal of Medicine, 360(5), 491–499
https://doi.org/10.1056/NEJMsa0810119
7 Smith, K. K., Gilcreast, D., & Pierce, K. (2008, July). Evaluation of staff’s retention of ACLS and BLS skills. Resuscitation, 78(1), 59–65.
https://doi.org/10.1016/j.resuscitation.2008.02.007
8. American Association of Oral and Maxillofacial Surgeons. (2021). Parameters of care: clinical practice guidelines for oral and maxillofacial surgery.
9. Weisinger, H. (2015). Performing under pressure: the science of doing your best when it matters most. New York: Crown Business.
LOWERING YOUR HIGH BLOOD PRESSURE IS EASIER THAN YOU THINK. There are FREE classes to help you get healthier and stay that way. HealthyDelaware.org/HealthyHeart 302-208-9097 55
Career and Technical Education: The Future of Delaware’s Healthcare Workforce
Jonathan S. Lee, B.A. Undergraduate Student, Johns Hopkins University
INTRODUCTION
As populations age, greater utilization of medical, dental, and behavioral health services place significant strain on healthcare systems. With the proportion of Delawareans aged 65 and older projected to grow 48.6% by 2050, state-led initiatives such as DIMER, DIDER, and the Delaware Health Care Provider Loan Repayment Program aim to train and retain Delawarean physicians and healthcare professionals.1,2 In recent years, initiatives have also focused on the development of career and technical education (CTE) for middle and high school students. CTE programs currently exist in 41 of Delaware’s 45 public high schools with the goal of providing meaningful work experience prior to entering the workforce or higher education.3 In 2020-2021, 15,781 CTE students were enrolled, of which 14.1% were studying careers in health science.4
CURRICULUM
Health science programs across Delaware prepare students for careers as dental assistants, medical assistants, physical therapy health aides, certified nursing assistants, and patient care assistants. At schools such as Sussex Tech High School, first-year students rotate through six technical areas before deciding what area to pursue. Between sophomore year and graduation, students attend their technical area every day, learning alongside the same group of classmates for the next three years.5
Dental assisting students, for example, spend their first year learning about dental anatomy, head and neck anatomy, and various oral diseases. Students practice taking dental impressions, pouring and trimming models, and creating whitening trays. In junior year, students prepare for the Dental Assisting National Board (DANB) Radiation Health and Safety (RHS) exam. Upon passing, students earn a state certificate as a Dental Radiation Technician. As seniors, students can substitute their last class period with workbased learning – a program that allows students to gain “hands-on training in job-related situations.” Sussex Tech has partnerships with dental practices throughout southern Delaware, and many of these practices offer paid positions during the school year that can lead to full-time employment during the summer.5
FROM A STUDENT’S PERSPECTIVE
As a graduate of Sussex Tech’s Dental Services and Technologies program, the quality of education I received was exceptional. The classroom offered three fully-functional operatories, panoramic and periapical x-ray machines, a lab with four model trimmers, an autoclave, an ultrasonic, and various dental instruments. After listening to lectures and taking notes on textbook readings, students hone their
clinical skills by practicing with one another. I remember when my classmates and I were learning how to take impressions sophomore year, I had to start over three times. While I felt incredibly awkward, I felt worse for my partner who, as the person I was practicing on, took the brunt of my learning curve. Fortunately, I didn’t feel as bad in the end because when it was my partner’s turn, they had to restart a similar amount of times. This was one of my favorite aspects of being in a CTE program. Providing students with an interactive curriculum and classmates they’ve known since sophomore year allows students to learn in an environment where they aren’t afraid to make mistakes and provide feedback to their peers.
After passing the RHS exam, students are prepared to begin seeking work experience as a dental assistant. Going into the summer of my senior year, I was determined to find a summer job where I could continue developing the skills I had learned over the past 2 two years. After a few weeks of applying to dental offices, I was offered a position as an oral surgery assistant. On the first day, the oral surgeon sat me down and expressed his expectations for me. I had to be willing to challenge myself, listen to my fellow assistants, and learn from each new experience. To this day, the culmination of everything I learned made that summer the most impactful experience of my life. I assisted with surgeries, provided pre/post-op instructions, and interacted with patients from around southern Delaware. As a sixteenyear old, the maturity and confidence I gained through serving patients prepared me for college and my various endeavors since then. While in college, I continued working as an oral surgery assistant for two more summers along with serving as a COVID-19 contact tracer for Delaware throughout the pandemic.
Gaining these experiences at a young age piqued my interest in public health. Through oral surgery, I was given the opportunity to work with patients from anywhere between two weeks to 98 years old. My understanding of how health inequities affect different patient populations greatly evolved, and through speaking with patients, I began learning about how a lack of transportation, familial support, and food insecurity can serve as barriers towards improved health. I also learned that while a healthcare professional needs to be able to treat a disease, they similarly need to understand how social determinants of health impact their patient’s health. The importance of understanding the unique challenges that patients in certain communities face became especially evident throughout the pandemic. Developing a healthcare workforce consisting of individuals born and raised in Delaware not only improves employee retention but also ensures that our providers have a holistic understanding of the needs of the communities they serve.
Doi: 10.32481/djph.2023.04.013
STUDENT SPOTLIGHT 56 Delaware Journal of Public Health - April 2023
PLANNING AHEAD
Studies have found that CTE provides various benefits ranging from reduced dropout rates to increased rates of postsecondary enrollment.6 From personal experience, many of my classmates began healthcare careers following graduation while others with aspirations of becoming dentists, physicians, pharmacists, physician assistants, nurses, physical therapists, and occupational therapists, pursued higher education. In recent years, the number of CTE programs across Delaware have grown significantly; however, in order to provide students with tangible work experience that can shape their understanding of public health in their local communities, we need to continue developing programs that provide students with opportunities to gain direct exposure caring for patients.
Currently, initiatives such as Apollo: Youth in Medicine, a shadowing program that connects high school students primarily around northern Delaware with physician mentors, do exist, yet more can be done to create similar programs for other healthcare fields throughout the state.7 For students who are able to acquire certifications through their CTE programs, Delaware can potentially partner with established healthcare practices to offer paid summer internships for students going into the summer before their senior year of high school or first year of college. This program can be state subsidized to incentivize healthcare professionals to hire students from their local community. Developing these types of opportunities will provide students with opportunities beyond the typical seasonal employment that consists of working in retail or at the beach. Instead, they can gain meaningful experience working in healthcare and learning about public health in Delaware.
Mr. Lee may be contacted at jonathanlee7026@gmail.com
REFERENCES
1. Delaware Health and Social Services & Delaware Healthcare Commission. (2022, May). 2021 Delaware nursing home utilization statistical report.
https://dhss.delaware.gov/dhcc/hrb/files/nursinghomeutilization2021.pdf
2. Delaware Health and Social Services. (n.d.). The Delaware Institute of Medical Information and Research (DIMER).
https://dhss.delaware.gov/dhcc/dimer.html
3. University of Delaware College of Education & Human Development (2022, June). UD researchers partner with Delaware Department of Education to examine equity and access in career and technical education.
https://www.cehd.udel.edu/delaware-career-and-technical-education/
4. U.S. Department of Education, National Perkins Reporting System. (2022). Delaware Career Cluster Enrollment.
https://cte.ed.gov/profiles/delaware

5. Sussex County Vocational Technical School District. (n.d.). Dental Services and Technology.
https://www.sussexvt.org/hs/home/technical-courses/dental-services/
6. CTE Policy Watch. (2021, May). Analyzing CTE’s Impact on Postsecondary Outcomes.
https://ctepolicywatch.acteonline.org/2021/05/analyzing-ctes-impacton-postsecondary-outcomes.html
7. Apollo: Youth in Medicine. (n.d.). Program Info. https://www.apolloprogram.org/
57
Patient Safety at Forefront of OMS Anesthesia Delivery
Paul J. Schwartz, D.M.D.
President, American Association of Oral and Maxillofacial Surgeons; Assistant Professor, Departments of Oral and Maxillofacial Surgery/Anesthesiology, School of Dental Medicine, University of Pittsburgh
Patient safety is of upmost importance to oral and maxillofacial surgeons who treat thousands of patients every day, particularly in the realm of sedation and anesthesia. While anesthesia provides many patient benefits, it also presents risks to patient safety if providers are not properly trained, regulated, and monitored.
Oral and maxillofacial surgeons are uniquely qualified to comment on dental anesthesia delivery due to the sheer volume of anesthetics performed by the profession. During calendar years 2018-2021, office-based dental anesthesia services were delivered to 24,194,239 individuals insured by private dental insurance in the United States. Of all the moderate and deep sedation/general anesthesia cases performed in 2018-2021, oral and maxillofacial surgeons performed 6,929,439 – or 78% - of the total case load (8,894,182). In children ages 8-12 requiring deep sedation/general anesthesia, OMSs provided 80% of these procedures. For children ages 1-7 requiring sedation services, OMSs provided 41% of these anesthesia services.1
The availability for patients to receive OMS- provided anesthesia care is clearly critical to providing compassionate dental care. These statistics were extrapolated by the AAOMS using data from the U.S. Census Bureau and information provided by FAIR Health based on its privately insured dental claims data for calendar years 2018-2021.
As President of the American Association of Oral and Maxillofacial Surgeons (AAOMS), I am immensely proud of my specialty’s record and commitment to patient safety as exemplified in our white paper, Office-based Anesthesia Provided by the Oral and Maxillofacial Surgeon. As stated in the publication, oral and maxillofacial surgeons:
• Are highly trained professionals with dedicated hospital-based rotations in sedation/anesthesia who also engage in ongoing continuing education efforts.
• Utilize the OMS anesthesia delivery model that engages the entire care team in patient treatment.
• Possess an advanced grasp of anesthetic techniques, risks and complications.
• Hold a unique in-depth knowledge of the importance of patient evaluation and monitoring.
• Recognize the need for required office anesthesia evaluations and the potential perils of mobile anesthesia delivery models.
• Are committed to patient safety as exemplified by their ongoing engagement in lifelong learning from multiple sources and conducting required emergency preparedness drills for both the staff and provider.
• Have created a state-of-the-art simulation-based learning experience intended to provide every OMS and their staff training in Office-Based Emergency Airway Management (OBEAM) and Office-Based Crisis Management (OBCM).
The AAOMS has consistently prioritized anesthesia safety throughout its existence, which is evident by our low rate of adverse events. Ongoing quality assessment and lifelong learning are signature elements in the delivery of high-quality state-ofthe-art patient care and optimized patient safety and emergency response. Given that oral and maxillofacial surgery spans both medicine and dentistry, ongoing quality assessment has been an integral part of the specialty as we collectively strive to cultivate a culture of safety. The results should be continually monitored using objective measures.
The AAOMS and the American Board of Oral and Maxillofacial Surgery fully support this process.
Dr. Schwartz can be contacted at pschwartz@aaoms.org.
REFERENCES
1. American Association of Oral and Maxillofacial Surgeons. (2022). White paper: Office-based anesthesia provided by the oral and maxillofacial surgeon. Retrieved from: https://www.aaoms.org/docs/govt_affairs/advocacy_white_papers/ office_based_anesthesia_whitepaper_whitepaper_1.pdf
Doi: 10.32481/djph.2023.04.014
58 Delaware Journal of Public Health - April 2023
What is the LT. Governor’s challenge?

The mission of the Lt. Governor’s Challenge is to improve the quality of life of all Delawareans. The program honors the individuals, organizations, and institutions that inspire others by making healthy choices the easiest choices for their communities, ultimately helping elevate the well-being, productivity, and prosperity of our state.
NOMINATION MUST INCLUDE THE FOLLOWING:
• Who or what team or organization is responsible for the achievement?
• What PSE changes did they make, and what did these changes accomplish?
important dates
For more detailed information, visit LtGovernorsChallenge.org.
Nominations Open Mar. 30 2023 Winners Selected Sum mer 2023 Wellness Leadership Awards nov. 2023 Nominations Close May 12 2023 Nominee’s Area of Focus Emotional Well-being Healthy Living Mother and Child Health Chronic Disease Management and Prevention Who is eligible? Individual Workplace School Community with a Shared Interest Town, City, or Neighborhood Submit Your Nomination
a nomination at
Submit
LtGovernorsChallenge.com
59
ORAL HEALTH LEXICON
Alveolar Bone
e thick ridge of bone which contains the tooth sockets. Located on both jaw bones.
Angiogenesis
e development of new blood vessels.
Anogenital
Relating to the anus and genitals.
Antiresorptive
Slowing or blocking the resorption of bone.
Antral Mucosa
Mucus-secreting protective covering that lines the inside of the stomach.
Autonomy
e right or condition of self-government
Basilar Bone
e bone of the jaw bones that does not contain tooth sockets.
Beneficence
e concept in research ethics that states researchers should have the welfare of the research participant as a goal of any clinical trial or other research study.
Bisphosphonates
A group of drugs used to limit the loss of bone density in conditions such as osteoporosis and bone cancer.
Caries
Decay and crumbling of a tooth or bone.
Cariogenic
Causing tooth decay.
Chemoradiotherapy
Treatment that combines chemotherapy with radiation therapy. Also called chemoradiation.
Cytoplasmic Expression
Presence within the cytoplasm of a cell.
Dentoalveolar
Of, relating to, or involving the teeth and their sockets.
Dietetics
e branch of knowledge concerned with the diet and its e ects on health, especially with the practical application of a scienti c understanding of nutrition.
Endocrinology
e branch of physiology and medicine concerned with the endocrine glands and hormones.
Epithelial
Relating to or denoting the thin tissue forming the outer layer of a body’s surface and lining of the gut.
Etiology
e cause or set of causes of a disease or condition.
Extraoral
Situated or occurring outside the mouth.
Fistula
An abnormal or surgically made passage between a hollow or tubular organ and the body surface, or between two hollow or tubular organs; an abnormal connection between two body parts.
Immunohistochemical Staining
A laboratory method that uses antibodies to check for certain antigens or markers in a sample of tissue. e antibodies are usually linked to an enzyme or a uorescent dye.
In Situ Hybridization
A laboratory technique used to determine the location of a sequence of DNA or RNA in a biological sample.
Keratinizing
e acquisition of a horn-like character by the epithelial tissue in many parts of the body.
Lamina Dura
A mark seen on X-rays, the presence of which is an indication of the health of teeth.
Maleficence
e act of committing harm or evil.
Malignancy
e tendency of a medical condition to become progressively worse.
Mandible
e lower jaw bone.
60 Delaware Journal of Public Health - April 2023
Maxilla
ORAL HEALTH LEXICON
e upper jaw bone, which also forms part of the nose and eye socket.
Medical Loss Ratio
e percentage of insurance premium revenue insurers take in, compared to how much they spend on actual health care services
Morbidity
e condition of su ering from a disease or medical condition.
Necrosis
e death of most or all of the cells in an organ or tissue due to disease, injury, or failure of the blood supply.
Neoplasia
e formation or presence of a new, abnormal growth of tissue.
Nuclear Expression
Presence within the nucleus of a cell.
Odontalgia
Pain or in ammation in or around the tooth, o en caused by tooth decay or infection.
Oncogenes
A gene which, in certain circumstances, can transform a cell into a tumor cell.
Oropharyngeal
Relating to the part of the membrane-lined cavity behind the nose and mouth and connecting them to the esophagus, that lies between the so palate and the hyoid bone.
Osteoclast
A large bone cell which absorbs bone tissue during growth and healing.
Osteolysis
e progressive destruction of bony tissue.
Osteonecrosis
e death of bone tissue due to a lack of blood supply.
Osteoporosis
A medical condition in which the bones become brittle and fragile from loss of tissue, typically as a result of hormonal changes, or de ciency of calcium or vitamin D.
Paternalism
e interference of a state or an individual with another person, against their will, and defended or motivated by a claim that the interference is “for their own good.” e behavior can also express an attitude of superiority.
Paucity
e presence of something only in small or insu cient quantities or amounts.
Periapical
Encompassing or surrounding the tip of the root of a tooth.
Periodontal
Relating to or a ecting the structures surrounding and supporting the teeth.
Periodontitis/Periodontal Disease
In ammation of the tissue around the teeth, o en causing shrinkage of the gums and loosening of the teeth, and can destroy the jaw bone.
Polymerase Chain Reaction
A method of making multiple copies of a DNA sequence, involving repeated reactions with a polymerase (enzyme).
Prinicplism
An applied ethics approach to the examination of moral dilemmas that is based upon the application of certain ethical principles
Probability Proportional to Size Sampling Scheme
A survey method where each element of the population has some chance to be selected to the sample when performing a single draw.
Retrospective
Looking back on or dealing with past events or situations.
Sclerotic Trabecular Changes
A thickening of spongy bone as a result of bone-remodeling abnormalities.
Single-Modality
A situation in which only one treatment type is chosen from among several options available.
Trigeminal
Of, or relating to, the main sensory nerve of the head and face, and the motor nerve of the muscles used in chewing.
Veracity
Conformity to facts; accuracy.
61
ORAL HEALTH RESOURCES
Campaign for Dental Health
Oral Health Prevention Primer
https://ilikemyteeth.org/oral-health-prevention-primer/
Delaware Department of Health and Social Services
Delaware Burden of Oral Disease Report (2020)
https://www.dhss.delaware.gov/dhss/dph/hsm/files/burden_of_oral_disease.pdf
Bureau of Oral Health and Dental Services
https://www.dhss.delaware.gov/dhss/dph/hsm/ohphome.html
First Smile Delaware:
Campaign
https://www.dhss.delaware.gov/dhss/dph/hsm/ohpfirstsmilede.html
Dental Resource Guide
https://www.dhss.delaware.gov/dhss/dph/hsm/files/dentalresourceguide.pdf
Delaware Oral Health Surveillance Plan, 2020-2025
https://www.dhss.delaware.gov/dhss/dph/hsm/files/oralhealthsurveillanceplan.pdf
Oral Health Toolkit
https://www.dhss.delaware.gov/dhss/dph/hsm/tkhome.html
Delaware Health Force
Workforce Report
https://dehealthforce.org/
Delaware Thrives
Healthy Smiles
https://dethrives.com/programs/healthy-smiles
National Institute of Dental and Craniofacial Research
https://www.nidcr.nih.gov/
62 Delaware Journal of Public Health - April 2023
ORAL HEALTH RESOURCES
Free and Low-Cost Dental Centers
ChristianaCare Hospital Dentistry Clinic – Wilmington Hospital. TEL: 302-320-4850
Reduced fees, and accepting un- and under-insured individuals. Treatment is performed by dental residents of ChristianaCare, and supervised by community dentists and faculty.
DSAMH Dental Clinic – New Castle. Referral Required. TEL: 302-255-4484
Offers basic oral health services to underserved adult clients not covered by private dental insurance or participate in Delaware Medicaid. Services include oral exam, x-rays, hygiene and oral health education.
DTCC Dental Health Center – Wilmington. TEL: 302-571-5364
An educational clinical facility supporting the Dental Hygiene program at Delaware Technical Community College. Provides quality dental care for the community while enabling students to meet the educational requirements of the Dental Hygiene program.
https://www.dtcc.edu/our-campuses/wilmington/dental-health-center
Financial Assistance Program
https://www.dtcc.edu/our-campuses/wilmington/dental-health-center/program-eligibility
Delmarva Rural Ministries, Inc. – Dover. TEL: 302-678-3652
Offer high-quality, low cost dental care to the low income, un- and under-insured communities in Kent County.
Henrietta Johnson Medical Center – Southbridge – Wilmington. TEL: 302-655-6187
Various health and dental care is offered on a sliding scale or lower cost, including cleanings. Hygienists and dentists on location.
Kent Community Health Center – Dover. TEL: 302-678-2000
Low cost dental care, sliding fee scale, government and private insurance accepted. Services include general dentistry, basic oral surgery, and cleanings.
La Red Health Center, Inc. – Georgetown. TEL: 302-855-1233
Westside Family Healthcare, Inc. – Wilmington. TEL: 302-655-5822
63




Index
Advertisers The Nation's Health . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5 American Public Health Association The DPH Bulletin - March 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14 Delaware Division of Public Health The DPH Bulletin - February 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24 Delaware Division of Public Health The DPH Bulletin - January 2023 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 48 Delaware Division of Public Health Submission Guidelines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 66 Delaware Journal of Public Health 64 Delaware Journal of Public Health - April 2023
of
n Works best if taken within five days of symptoms starting.
n Helps reduce symptoms.
n Especially important for those age 50+ or unvaccinated.
Talk to your health care provider or learn more at de.gov/covidtreatments.
GOT COVID-19? GET TREATMENT.
If you test positive, treatment is available.
65
Public Health Delaware Journal of Submission Guidelines
updated April, 2020
About the Journal
Established in 2015, The Delaware Journal of Public Health is a bi-monthly, peer-reviewed electronic publication, created by the Delaware Academy of Medicine/Delaware Public Health Association. The publication acts as a repository of news for the medical, dental, and public health communities, and is comprised of upcoming event announcements, past conference synopses, local resources, peer-reviewed content ranging from manuscripts and research papers to opinion editorials and personal interest pieces, relating to the public health sector. Each issue is largely devoted to an overarching theme or current issue in public health.
The content in the Journal is informed by the interest of our readers and contributors. If you have an event coming up, would like to contribute an Op-Ed, would like to share a job posting, or have a topic in public health you would like to see covered in an upcoming issue, please let us know.
If you are interested in submitting an article to the Delaware Journal of Public Health, or have any additional inquiries regarding the publication, please contact DJPH Deputy Editor Elizabeth Healy at ehealy@delamed.org, or the Executive Director of The Delaware Academy of Medicine and Delaware Public Health Association, Timothy Gibbs, at tgibbs@delamed.org
Information for Authors
Submission Requirements
e DJPH accepts a wide variety of submission formats including brief essays, opinion editorials pieces, research articles and findings, analytic essays, news pieces, historical pieces, images, advertisements pertaining to relevant, upcoming public health events, and presentation reviews. If there is an additional type of submission not previously mentioned that you would like to submit, please contact a staff member.
The initial submission should be clean and complete, without edits or markups, and contain both the title and author(s) fulls name(s). Submissions should be 1.5 or double spaced with a font size of 12. Initial submissions must also contain a cover letter with concise text (maximum 150 words). Once completed, articles should be submitted via email to Elizabeth Healy at ehealy@delamed.org as an attachment. Graphics, images, info-graphics, tables, and charts, are welcome and encouraged to be included in articles. Please ensure that all pieces are in their final format, and all edits and track changes have been implemented prior to submission.
Cover Letters must address the following four article requirements:
1. A description of what the paper adds to current knowledge, in particular with respect to material previously published in DJPH, and if systematic reviews exist on the topic.
2. The public health importance of the paper.
3. One sentence summarizing the main message(s) of the paper, which may be used to disseminate the paper on social media.
4. For individual or group randomized trials, provide the date of trial registration and the NCT number from www.Clinicaltrials.gov or other approved registry. In the cover letter only, not in the paper. Do NOT include the trial registration or NCT number in the abstract or the body of the manuscript during the initial submission.
All manuscripts must be submitted via email to Elizabeth Healy at ehealy@delamed.org.
66 Delaware Journal of Public Health - April 2023
To view additional information for online submission requirements, please refer to the website for the Delaware Journal of Public Health: https://djph.org/sample-page/submit-an-article/

Submission Length
While there is no prescribed word length, full articles will generally be in the 2500-4000-word range, and editorials or brief reports will be in the 1500-2500-word range. If you have any questions regarding the length of a submission, or APA guidelines, please contact a staff member.
Copyright
Opinions expressed by contributors and authors do not necessarily reflect the opinions of the DJPH or affiliated institutions of authors. Copying for uses other than personal reference or interest without the consent of the DJPH is prohibited. All material submitted alongside written work, including graphics, charts, tables, diagrams, etc., must be referenced properly in accordance with APA formatting.
Conflicts of Interest
Any conflicts of interest, including political, financial, personal, or academic conflicts, must be declared prior to the submission of the article, or in conjunction with a submission. Conflicts of interest are any competing interests that may leave readers feeling misled or deceived, and/or alter their perception of subject matter. Declared conflicts of interest may be published alongside articles in the final electronic publication.
Nondiscriminatory Language
Use of nondiscriminatory language is required in all DJPH submissions. The DJPH reserves the right to reject any submission found to be using sexist, racist, or heterosexist language, as well as unethical or defamatory statements.
Additional Documents and Information for Authors
Please Note: All authors and contributors are asked to submit a brief personal biography (3 sentences maximum) and a headshot along submissions. These will be published alongside final submissions in the final electronic publication. For pieces with multiple authors, these additional documents are requested for all contributors.
Abstracts
Authors must submit a structured or unstructured abstract along with their article.
The word limit is 200 words, including headings. A title page should be submitted with this abstract as well.
Structured abstracts should employ 4-5 headings: Objectives (begins with “To…”)
Methods Results
Conclusions
A fifth heading, Policy Implications, may be used if relevant to the article.
Trial Registration information is required for clinical trials and must be included in the final version abstract
All abstracts should provide the dates(s) and location(s) of the study is applicable.
Note: There is no Background heading.
67
Delaware Academy of Medici ne / DPHA
P.O. Box 89 Historic New Castle, DE 19720 ISSN
www.dela med.org | www.djph.org
e Del aware Academy of Medicine is a private , nonprofit organization founded in 1930. O ur mission is to enhance the well being of our communit y through medical education an d the promotion of public health. O ur educational initiatives span the spect rum f rom consumer health education tocontinuing medical education conferences and symposia e Del aware Public Health A ssociation wa s officially rebor n at the 141 st Annual Meeting of the American Public He alth A ssociation (AHPA) hel d in B oston, M A in November, 2013. At this meeting, af filiation of t he DPH A wa s t ransferred to the Del aware Academy of Medicine officially on November 5, 2013 by action of the A PH A Governing Council . e Del aware Academy of Me dicine, who’s mission statement is “ to promote the well-being of o ur communit y through education and the promotion of public health,” is honored to take on t his responsibility in the First State
Follow Us: 2639-6378









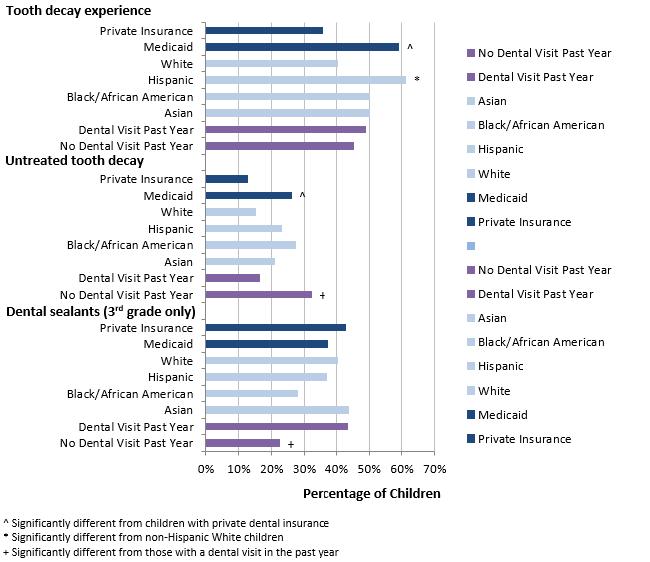










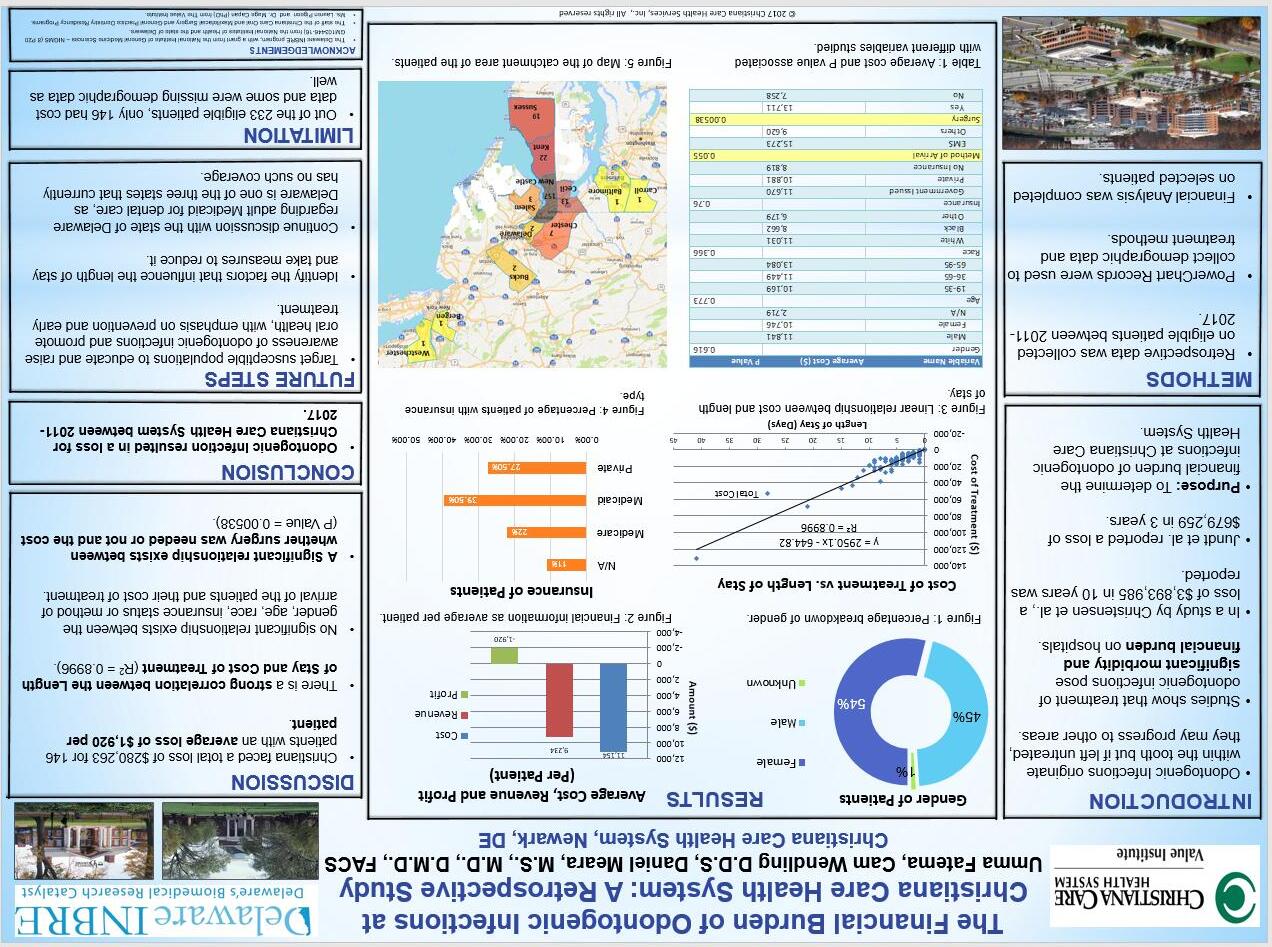








 Michelle Mathew
Michelle Mathew