TheProject




Marc Buoniconti President
Dr. Allan D. Levi
Clinical Director, Professor and Chair of the Department of Neurological Surgery
Suzanne M. Sayfie Director Major Gifts Buoniconti Fund
Jeanette Bajo Center Administrator
Robert Camarena Senior Graphic Designer
David McMillan, Ph.D. Director, Education and Outreach
Management
Dr. Barth A. Green
Chairman, Professor of Neurological Surgery
Dr. Mark Nash
Associate Research Director
Teresa De Jesus Arcay
Assistant to Marc Buoniconti
Diana Berning Senior Manager, Business Operations
Cynthia Jones Manager, Facilities and Operations
Randy L. Medenwald
Senior Director, Advocacy and Donor Relations
Erika M. Suazo
Executive Assistant to Dr. W. Dalton Dietrich
Editor & Contributor, David McMillan, Ph.D.
Managing Editor, Scott Roy
Graphic Editor, Robert Camarena
Cover image by Dr. Pantelis
Dr. W. Dalton Dietrich Scientific Director, Professor of Neurological Surgery
Stephanie Sayfie Aagaard Executive Director
Betsy Arias Senior Manager, Research Grants
Teri I. Bendell Director, Web Services, Auction, and Database
Jacqueline Manzano Manager, Marketing
Scott P. Roy Director, Public Relations and Communications
Taimy Trujillo
Assistant to Dr. Barth A. Green
Rebecca Avshalom
Ashley Beckwith Javier Burgos
Maria Chagoyen
Danielle Cilien
Frank Diaz
Gigi Giobio


Evelyn Gomez
Alejandro Labrada
Carole Robbins
Stephanie Lacayo Rodriguez
Paul Sanchez
Sean Sadler Scientific Staff & Trainees
Dr. Alexander Marcillo
Post-doctoral Fellows
Graduate Students
Medical/Residents/Observorships
Undergraduate Students Volunteers
Other Students Research Staff
Dr. Jennifer C. Munoz Pareja’s Visionary Journey
Through meticulous research and collaboration with esteemed colleagues like Dr. Juan Pablo de Rivero Vaccari, Dr. Munoz Pareja is unraveling the mysteries of pediatric TBI one biomarker at a time
Jennifer C. Munoz Pareja, M.D., Associate Professor Division of Pediatric Critical Care and Associate Program Director of the Pediatric Critical Care fellowship program at Holtz Children’s Hospital, joins The Miami Project to Cure Paralysis to further develop proven neuroscientific excellence onto the topic of pediatric critical care. Her demonstrable experience and expertise with biomarkers for neurological conditions in the pediatric intensive care setting now unites with The Miami Project’s expertise in neurologically relevant biomarkers to shape a vision for the future of pediatric critical care.
Born and raised in Colombia, Dr. Munoz Pareja’s early fascination with aerospace medicine propelled her towards a career dedicated to healing and discovery. After completing her medical training in her home country, the William J. Harrington Internal Medicine Residency Training Program enabled a residency at Nicholas Children’s Hospital linking training to the University of Miami Leonard M. Miller School of Medicine and Jackson Health Systems. Her subsequent fellowship at Harvard Medical School / Massachusetts General Hospital with Dr. Ann-Christine “Tina” Duhaime, M.D., Chief of Pediatric Neurosurgery, solidified her interest in a neurological specialization. Soon after, in her appointment at University of Florida College of Medicine, she refined her neurological interests under the training of Kevin K. Wang, Ph.D., well known for their biomarker research as a site of the NINDS-funded, multicenter Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI). Dr. Munoz Pareja now moves to the Miller School to conduct research through The Miami Project to Cure Paralysis with an eye for biomarkers in the post-traumatic and hemodynamic pediatric intensive care setting. She does so while maintaining a practice of excellence in pediatric critical medicine and contributing to the training of the next generation of physicians in her specialization.
With her vision informed by this rich experience, Dr. Munoz Pareja now unites her clinical acumen with The Miami Project’s scientific affordances. Her trajectory demonstrates she has realized the potential of fluid biomarkers in the pediatric clinical care setting, and tapping into The Miami Project will unlock a deeper understanding of pediatric TBI and revolutionizing the diagnosis and treatment of brain trauma in children.
Her groundbreaking work, highlighted in a recent paper published in Journal of Neurotrauma, titled “Prognostic and Diagnostic Utility of Serum Biomarkers in Pediatric Traumatic Brain Injury”, showcases the potential of this union. The study analyzed biomarkers like GFAP, tau, S100B, and p-tau181 in blood to predict TBI severity and long-term neurological outcomes. The results of the study suggest that a specific panel of biomarkers blood, a bodily fluid already readily and routinely accessed in this situation, at key points after TBI can aid in earlier diagnosis and more granular prognosis compared to current standards. This study epitomizes the power of uniting Dr. Munoz Pareja’s visionary mindset with The Miami Project neuroscientific expertise, notably the fluid biomarkers expertise of Dr. Juan Pablo de Rivero Vaccari, to understand pediatric TBI and inform subsequent critical care. This study not only informs clinical decisionmaking now, but the approach also holds the promise of identifying novel therapeutic targets for TBI and other critical conditions. This multidisciplinary approach to pediatric medical research, leveraging advanced technologies like the Simoa HD-X empowered biomarkers core that she helped advocate for, epitomizes the potential afforded by Dr. Munoz Pareja bringing pediatric medical research to The Miami Project. The future will include the deep dive into TBI and include nontraumatic brain injury, especially those from hemodynamic dysfunction since these causes of brain emergencies are not readily diagnosed radiologically, thus warranting fluid biomarker efforts. Already she has launched a project with

congenital heart disease in children that leads to reduced brain blood delivery with neurological impacts, and she plans also to continue previous collaborations to study another nontraumatic neurological condition in the form of childhood delirium.
In addition to her research endeavors, Dr. Munoz Pareja is an active leader in her field and, while also still in many ways at an early phase of her career, already passionate about training the next generation in a truly global context. For the Neurocritical Care Society pediatric research group global health division she is involved in an approved simulation curriculum, funded by an AHA-linked area-nine company partner that commercializes medical simulation technology that enables training in areas such as Africa and Latin America. Locally, she is the Associate Program Director of the Pediatric Critical Care fellowship program at Jackson Health System’s Holtz Children’s Hospital, where she shapes the next generation of pediatric critical care physicians. Her Florida ties also keep her linked to the state’s consortium for pediatric clinical care.
So it is that Dr. Jennifer C. Munoz Pareja’s visionary approach to academic medicine unites with The Miami Project’s neuroscientific expertise to bring pediatric critical care to new heights.


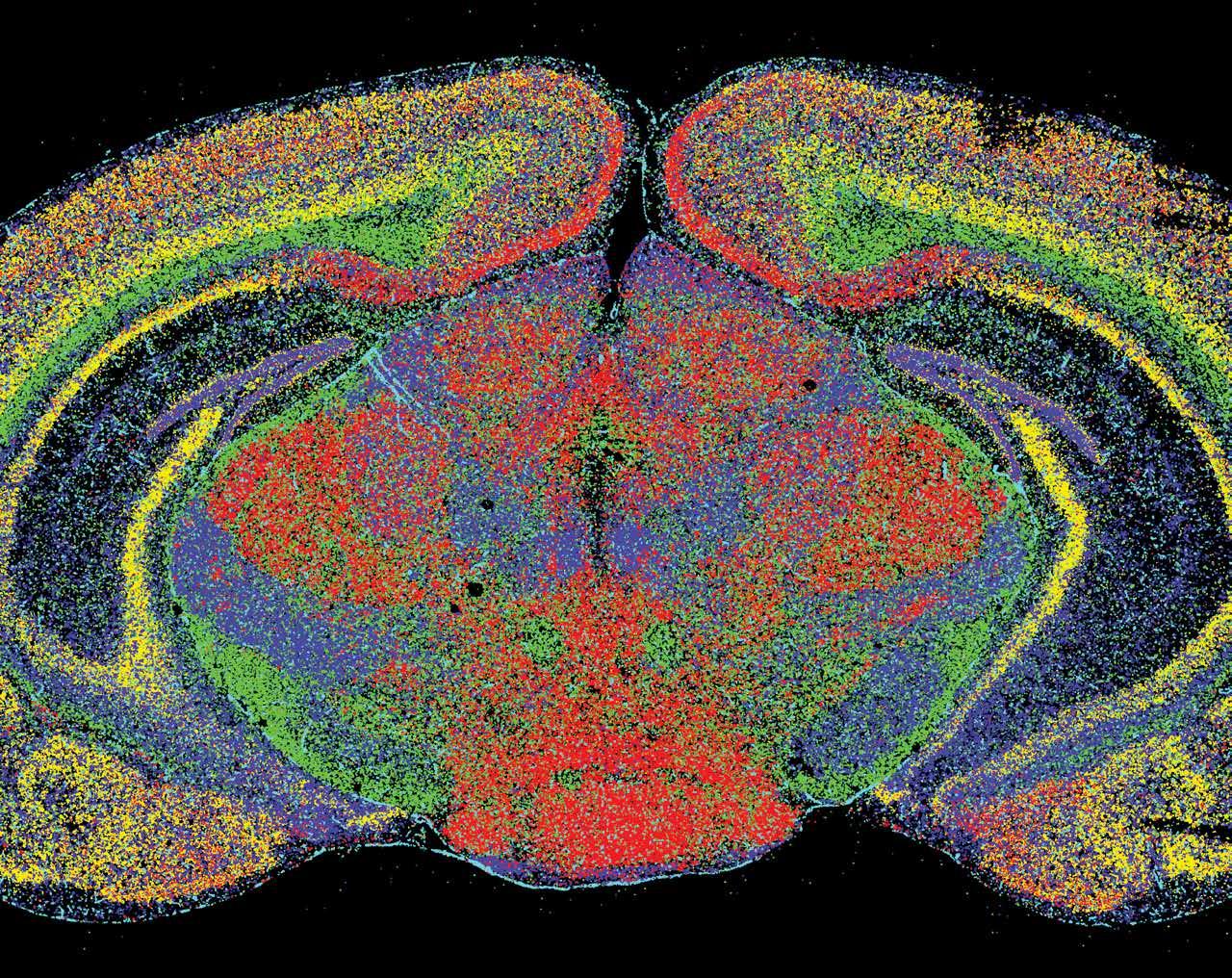
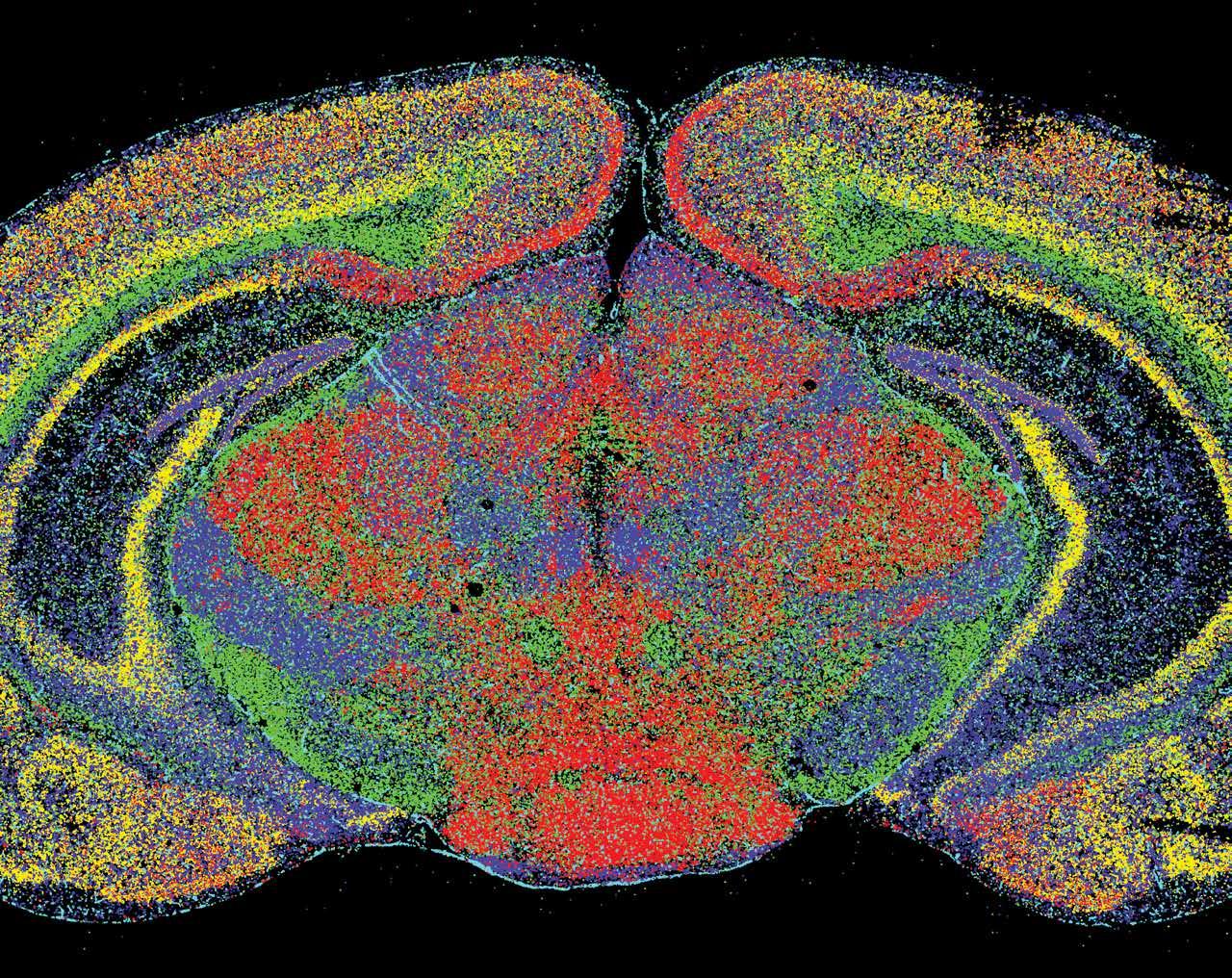
The Miami Project’s Dr. Pantelis Tsoulfas, Associate Professor of Neurological Surgery and Cell Biology, continues a long line of collaborative work with Dr. Murray Blackmore, Professor of Biomedical Sciences at Marquette University. Equipped with a new federal award, this accomplished pair continues to employ their established and proven neuroanatomical approach while venturing into new territory mapping the entirety of the supraspinal, or brain, connections between the central nervous system (CNS) and functional recovery after spinal cord injury (SCI).
At first glance it might not be obvious why the brain changes after SCI, since trauma occurred to the spinal cord and it is in the cord that the glia and fibrotic scar forms. Considering the old adage “use it or lose it”—which is formalized in neuroscience as activity-based plasticity—it becomes clear that the reduction in sensory input from the body, no longer transmitted to the brain, leads to a
reduction in brain regions that would typically process that input. Known as cortical remapping, these changes also occur not only in brain regions that receive information but also in outgoing regions that no longer routinely activate due to the futility of their no longer transmitted message to the body. Neuroscientists have long since studied the connection between select brain regions after SCI. Drs. Tsoulfas and Blackmore have been diligently pursuing their goal of charting the entire network of brain connections, termed the “supraspinal connectome”, rather than focusing on just one or two, to establish a neuroscientific framework for understanding the variations in functional outcomes after SCI. Their new award integrates previously proven but separate approaches in a pivotal and thorough investigation, demonstrating the power of the model they have developed.
Drs. Tsoulfas and Blackmore’s supraspinal connectome journey began in 2018, when Dr. Blackmore was a postdoctoral fellow at The Miami Project. Blackmore, and
Tsoulfas embarked on implementing a novel viral technique in SCI that had been developed for labeling neurons projecting their fibers to various targets throughout the central nervous system. The strength of this viral method lies in its capacity to label all intact brain connections with just a single application of the tracer in the spinal cord. The difficulty in leveraging this capability lies in the requirement to image an entire, undamaged brain rather than just a subregion as conventional technologies allow for. Thus, the realization the supraspinal connectome paradigm is made possible by a significant advancement in microscopy known as light-sheet microscopy. Traditional microscopy requires the sectioning, or slicing, of thin waferlike sections of a sample so that light can penetrate and thus illuminate the tissue and the scientist’s chosen labels. In light-sheet microscopy, the sample is not sectioned but instead cleared, using a chemical process making the tissue transparent. A sheet of light is then passed through the entire sample, in this case the whole brain, to illuminate
and reconstruct in 3D the intact tissue without the need to section. Combining the viral tracer with light-sheet makes good sense given the ability to label the entire CNS and then image the neurons with their processes without disturbing anything in the environment.
Their latest project goes beyond simply capturing images of the CNS post-SCI; it also aims to understand how changes in the connectome relate to functional outcomes. By adopting a connectome approach, Tsoulfas, Blackmore, and their team aim to link changes in brain regions above the injury site with the restoration of motor function, aiming to understand the relationship between the connectome and behavior. The variability in recovery post-SCI, how it is that some smaller injuries lead to profound deficits while larger SCIs result in relatively minor impairments, remains an important and unanswered question.
Incorporating an element of causation into their groundbreaking study, the team plans to deactivate certain brain regions implicated through imaging as being involved recovery after SCI. If silencing leads to the loss of a previously regained function, it will provide strong evidence of that region’s causal involvement in the function being studied.
This federally funded sustaining collaboration, which adopts a systems-based approach to develop a neuroscience paradigm specific to SCI, exemplifies The Miami Project’s ethos and Tsoulfas’s career-long dedication to understanding and eventually curing SCI. “Science thrives on reciprocity and collaboration of different teams,” Tsoulfas emphasizes, “and the value of long-term professional relationships cannot be overstated.”
Upon completion of their project, Tsoulfas, Blackmore, and their team will have developed a comprehensive CNS labeling and imaging approach that intergrates the supraspinal connectome with functional recovery after SCI, this paradigm will also shed light into the complex relationship between the supraspinal connectome and functional outcomes post-SCI. This approach will be incorporated into future analyses of interventions and treatments, attributing effects to specific nuclei regardless of the of intervention type, whether involves devices, pharmaceuticals, or biologic treatments.

As Dr. Dumont’s pioneering work continues to unravel the mysteries of polymeric nanoparticles, the prospects for engineering stepwise systems therapeutics aimed at neurological outcomes has never been more promising.
Courtney Dumont, Ph.D., Assistant Professor Department of Biomedical Engineering and The Miami Project, leads the Neural Stem and Tissue Engineered Microenvironments (NeuSTEM) group conducting ground-breaking research at The Miami Project to Cure Paralysis. Her rising career is now furthered via the National Science Foundation (NSF) prestigious Faculty Early Career Development Program (CAREER) award. The NSF CAREER award focuses on a specific nanoparticle project, and more broadly allows Dr. Dumont to build upon her work at the interface of neural, vascular, and immune engineering to overcome barriers that arise after injury to the nervous system.
Central to Dr. Dumont’s research is the engineering of modular biomaterial systems for gene, drug, and stem cell delivery to promote repair of the central nervous system. The NSF CAREER award focuses on a specific tactic in this broader strategy, focusing on the utilization of nanoparticles (NPs) of polymeric origins. Unlike conventional drug carriers, polymeric NPs are not preloaded with therapeutic cargo but instead are meticulously engineered to target and sequester specific molecules within the body. In the case of Dr. Dumont’s CAREER project, the NPs will have two phases, engineered first to hunt specific cytokine targets, and after sequestering cytokines to then be identified and ingested by specific immune cells known as macrophages. This design approach starts with anti-inflammation that then transitions to immune modulation.
Along with the unique bi-phasic action engineered into these molecules, the polymeric NPs are comprised of simple components that degrade into biocompatible constituents, such as sugars. Dr. Dumont’s project takes advantage of glycosaminoglycans (GAGs), a class of

sugars, to tune the NP properties. In particular, the potent negative charge of GAGs facilitates precise targeting and interaction with target molecules, particularly cytokines, key mediators of inflammation. Due to the natural presence in the body of the materials the NPs are made of, Dr. Dumont’s polymeric NPs ought not be viewed as conventional drugs.
Action on multiple targets, engineerability of target specificity, and controlled degradation highlight why polymeric NPs offer unparalleled versatility and biocompatibility. Dr. Dumont and her NeuSTEM team now carry out their NSF CAREER award project using polymeric NPs. Their ability to seamlessly integrate into biological systems and undergo controlled degradation ensures minimal toxicity and maximal therapeutic efficacy.
The clinical implications of Dr. Dumont’s research are far-reaching, with acute emergency management emerging as a primary use case. The rich history of neurotrauma at The Miami Project underscores the pivotal role of inflammatory processes in conditions such as paralysis following brain and spinal cord injuries, clearly implicating application of polymeric NPs in neurotraumatic cases. As Dr. Dumont’s pioneering work continues to unravel the mysteries of polymeric nanoparticles, the prospects for engineering stepwise systems therapeutics aimed at neurological outcomes has never been more promising. Stay tuned as Dr. Dumont leverages her NSF CAREER award to set her professional trajectory on a fast track to engineering world-class neurotherapeutics.


The Miami Project to Cure Paralysis carries on a historied tradition of developing technologies that tap into the central nervous system with recent developments in detecting and interpreting electrical signals produced by the brain. Known in the industry as brain-computer interface (BCI), this technology that turns thoughts into digital commands includes recent updates from The Miami Project’s Dr. Matija Milosevic and Dr. Abhishek Prasad—each employing distinct approaches.
Dr. Matija Milosevic, recently appointed assistant professor of Neurological Surgery and Biomedical Engineering, brings to The Miami Project his laboratory of NeuroModulation, Engineering, and Therapeutics (NeuroMET Lab). Core to the laboratory is the use of brain signals from BCI to trigger stimulation that modulate neurological activity. Now at The Miami Projectm, Dr. Milosevic expands from a recent focus on therapeutics that modulate the upperextremities (e.g., arm and hand) that famously human brains are wired to have more direct control over. He turns his laboratory’s focus now on lower-extremity function (e.g., standing and walking) that are more so driven by neurological activity at the level of the spinal cord. The underlying principle of intention-driven Hebbian plasticity remains the same, but different neural circuits are modulated with different functional outcomes. The importance of BCI is realized at two levels of the underlying principle. First, BCI interprets the specific intent to move in the form of electrical brain activity, allowing for closed-loop control of neuromodulatory simulators to be driven by user intent. Concurrently, BCI engages the user in an active attempt to produce movement (i.e., intent) which sends signals toward the desired-yet-interrupted target circuits in the cord. This more nuanced component is key to the Hebbian component of plasticity. Hebbian plasticity, a type of learning at the cellular level, is famously summarized as “neurons that fire together wire together.” With motor intent from the brain as the descending signals and movement from neuromodulation as the ascending signal, the precise pairing of these two modalities is the key to tapping into Hebbian plasticity. In engineering therapeutics that take advantage of this phenomenon, Dr. Milosevic’s pioneering work seeks not to replace function but to restore it, a key distinguishing feature between his neural therapeutics and other neural prosthetics.

Concurrently Dr. Abhishek Prasad, established Miami Project scientist and associate professor of Biomedical Engineering, takes an invasive route in BCI innovation. The lab’s long line of neural interface research is now furthered by a recent NIH award of $2.79 million to investigate the impact of iron accumulation from microelectrodes placed into brain tissue. When engineering the architecture of implanted BCI detecting electrodes, the question of “on or in” the brain must be considered. For BCI sensors that sit on the surface of the brain, the presence of molecular iron from bleeding is not so much a problem. But when engineered to penetrate neurological tissue, BCI electrodes are miniaturized to cause as little damage as possible, but still face the problem of iron accumulation from the inevitable disruption of the miniscule and ubiquitous microvasculature required to supply every neuron with blood. The project will explore ways to chelate, or dissolve, the iron that accumulates around implanted BCI microelectrodes.
Despite differences in invasiveness, the BCI-enabled research programs of Drs. Milosevic and Prasad seek a similar aim—to engineer mechanisms of restoring communication and control in people living with paralysis. This neural engineering vision was recently exemplified in the doctoral dissertation project of now-Dr. Kevin Davis, an MD/

Ph.D. student in the Miller School’s federally funded MSTP program. Dr. Davis’s dissertation, recently successfully defended, was conducted under the primary supervision of Dr. Prasad with collaborative research carried out in the laboratory of Dr. Milosevic. Integrating the imperative to use BCI to restore independence via a pairing with meaningful movement from neuromodulation, his dissertation included both invasive and non-invasive BCI. In a case study, Dr. Davis shepherd the research arm of a man with tetraplegia who volunteered to have neurosurgeon Dr. Jonathan Jagid implant a BCI in the form of surface electrode over the area of his brain responsible for hand movement. At the same time a group of participants had noninvasive BCI technology detect their intended hand movement to trigger neuromodulation that stimulated grasping rehabilitation. In integrating these parallel lines of BCI research Dr. Davis’s dissertation demonstrates the potential of uniting various experts under a common mission of concurrently caring for and curing paralysis.
Interested in contributing to our BCI research? With these and other projects in the works, stay tuned and reach out to our Office of Education and Outreach with any questions, or to inquire about participation, via email at mpinfo@miami.edu or phone 305-243-7108.


The Miami Project clinical researchers currently have several clinical trials and clinical studies available for people who have had a spinal cord injury; some are for acute injuries and some are for chronic injuries. The clinical trials are testing the safety and efficacy of different neuroprotective, reparative, or modulatory interventions. The clinical studies are investigating questions regarding exercise science, nutrition, rehabilitation training, pain, male fertility, aging, and brain-machine interface technology.
If you would like to be considered for these, or future Miami Project trials or studies, please see our Register for a Research Program section of our website, send us a message, or call The Miami Project Education Office at 305-243-7108.
BODY COMPOSITION, POSTPRADNIAL FAT METABOLISM, AND PAIN IN SPINAL CORD INJURY
Purpose: To study relationships between body composition (e.g., percent body fat), chronic pain, and measures of inflammation in blood in individuals with chronic spinal cord injury (SCI).
Qualification summary: Age 18-65 years; SCI occurring at least 2 years prior to study entry; neurological level of injury (LOI) between C4 and L2; American Spinal Injury Association Impairment Scale (AIS) A-D. (contact for more information)
Status: Enrolling Principal Investigator: Elizabeth Felix, Ph.D.
Contact: Lais Vidotto | phone: 305-243-3860 | email: lxv429@miami.edu
NERVE TRANSFER FOR RESTORING UPPER EXTREMITY MOTOR FUNCTION AFTER TETRAPLEGIA
Purpose: The purpose of the study is to investigate the effectiveness of nerve transfer surgery in improving hand function for spinal cord injury patients. The study will assess hand strength, range of motion, and other factors to determine if the surgery offers functional benefits.
Qualification summary: This study is for people 18-65 with chronic tetraplegia who haven’t improved in 3 months and meet specific muscle function criteria. It excludes people with active infections, ongoing recovery, certain medical conditions, and other specifics. (contact for more information)
Status: Enrolling Principal Investigator: S. Shelby Burks, MD
Contact: George Jimsheleishvili, MD | phone: 305-243-4781| email: gxj150@med.miami.edu
CUNEIFORM NUCLEUS DEEP BRAIN STIMULATION FOR GAIT FACILITATION FOLLOWING SCI
Purpose: This study aims to investigate the effectiveness of deep brain stimulation (DBS) of the cuneiform nucleus in improving walking ability and other functions for people with incomplete spinal cord injury. Researchers will implant electrodes in 6 participants and assess changes in gait speed, endurance, and quality of life.
Qualification summary: This study is for people with incomplete spinal cord injury (walking difficulties but some leg movement) who are at least 1-year post-injury, mentally sound, and able to commit to a 6-month training program. It excludes people with severe depression, cognitive impairment, substance abuse, certain medical conditions, or pregnancy. (contact for more information)
Status: Approved, not yet recruiting Principal Investigators: Brian R. Noga, Ph.D. and Jonathan R. Jagid, MD Contact: Letitia Fisher | phone: 305-243-3056 | email: lfisher@med. miami.edu
SELF-REPORT ACCURACY OF THE ASIA CLASSIFICATION EXAM IN SCI
Purpose: This study aims to compare how people with spinal cord injuries perceive their own level of function compared to how doctors assess it through a standardized exam. Researchers will ask participants about their injury and then conduct a detailed physical examination to measure nerve damage.
Qualification summary: Adults with a spinal cord injury or disease from any cause. (contact for more information)
Status: Enrolling Principal Investigator: W. Dalton Dietrich, Ph.D. Contact: Nilanjana Datta, MD | phone: 305-243-7108 email: nxd693@ med.miami.edu
EQUITY AND QUALITY IN ASSISTIVE TECHNOLOGY (EQUATE)
Purpose: To study the assistive technology used by individuals with spinal cord injury (SCI) and those with diagnoses that affect the spinal cord.
Qualification summary: This study is for adults (18+) with a spinal cord injury (affecting movement or sensation) from at least a year ago, who can understand English and have internet access to participate. (contact for more information)
Status: Enrolling Principal Investigator: Elizabeth R. Felix, Ph.D. Contact: Matthew DeVlieger | phone: 786-496-0448 | email: mxd4401@ med.miami.edu
ASSOCIATION OF SCI PHYSICAL ACTIVITY GUIDELINES AND HEALTH OUTCOMES
Purpose: To understand whether meeting the spinal cord injury physical activity guidelines is associated with positive health-related outcomes.
Qualification summary: Adults with chronic spinal cord injury. (contact for more information)
Status: Enrolling Principal Investigator: Elizabeth R. Felix, Ph.D.
Contact: Katherine Martinez | phone: (786)-540-4104 | email: kxm940@ miami.edu
SPINAL CORD INJURY EXERCISE AND NUTRITION CONCEPTUAL ENGAGEMENT (SCIENCE)
Purpose: The goal of this study is to assess the impact of home-based functional electrical stimulation leg cycle ergometry plus diet versus diet alone on body composition, insulin sensitivity, glucose effectiveness, and basal metabolic rate, as well as lower extremity bone mineral density, lipid profiles, and inflammatory markers in people with SCI. Participants will be randomized to either diet only or diet and exercise.
Qualification summary: This study seeks adults (18-65 years old) with complete motor loss (AIS A, B, C) due to a C4-T4 spinal cord injury that occurred at least one year ago. (contact for more information)
Status: Concluding recruitment
Principal Investigator: Gary J. Farkas, Ph.D.
Contact: Dinorah Rodriguez | phone: 305-243-2797 | email: dinorah@ med.miami.edu
DIET AND RMR
Purpose: The purpose of this study is to determine the relationship between nutritional needs, metabolic health, and body composition of individuals with and without spinal cord injury. Participants will maintain a diet log at home, interview with a registered dietician, complete a body composition analysis, and participate in fasting blood draw and medical screening.
Qualification summary: This study is for adults (18-65 years old) with complete motor loss (AIS A, B, C) in their spine (C4-L2 region) from an injury at least one year ago. (contact for more information)
Status: Enrolling
Principal Investigator: Dr. Gary Farkas, Ph.D.
Contact: Gary J. Farkas, PhD | phone: 305-243-4581 | email: gjf50@med. miami.edu
ALTERED BODY REPRESENTATION IN PEOPLE WITH SPINAL CORD INJURY AND ITS ASSOCIATION WITH PAIN SENSATION
Purpose: To define changes in body ownership underlying compromised multisensory integration in spinal cord injury (SCI) individuals by using
the rubber hand illusion procedure (RHI); ii) to determine the relation between compromised multisensory integration after SCI and its impact on pain.
Qualification summary: This study is recruiting three groups of adults (18-50 years old) for a pain research visit: people with incomplete spinal cord injury and chronic pain, people with incomplete spinal cord injury but no pain, and healthy volunteers with no history of injury. (contact for more information)
Status: Enrolling Principal Investigator: Eva Widerstrom-Noga, Ph.D. Contact: Linda Robayo Riofrio, Ph.D. | phone: 305-243-0233 | email: linda.e.robayo@miami.edu
EFFECTS OF BODILY ILLUSION AND TDCS ON SCIRELATED NEUROPATHIC PAIN
Purpose: To determine to what extent neuropathic pain following spinal cord injury (SCI) is reduced after a non-pharmacological treatment involving bodily illusion (BI) and transcranial Direct Current Stimulation (tDCS).
Qualification summary: This study seeks men and women aged 18-70 with incomplete spinal cord injuries in the neck (cervical) region and chronic pain lasting at least 3 months (moderate or worse, rated 4 or higher on a 0-10 scale). (contact for more information)
Status: Enrolling Principal Investigator: Eva Widerstrom-Noga, Ph.D. Contact: Roberta Vastano, Ph.D | phone: 305-243-0233 | email: rxv331@ med.miami.edu
PHYSIOLOGICAL AND BEHAVIORAL REGULATION OF FEEDING AFTER SPINAL CORD INJURY
Purpose: The goal of this study is to determine the effects of spinal cord injury on appetite and gut metabolism following 2 meals in adults with and without SCI.
Qualification summary: Adult men and women with complete and incomplete C3-L3 chronic (at least 1-year post-injury) spinal cord injury (AIS A, B, and C). (contact for more information)
Status: Concluding recruitment
Principal Investigator: Gary J. Farkas, Ph.D. Contact: Gary J. Farkas, PhD | phone: 305-243-4581 | email: gjf50@med. miami.edu
MALE FERTILITY EVALUATION
Purpose: To determine the cause of low sperm motility in men with SCI. Qualification summary: Adult men with spinal cord injury. (contact for more information)
Status: Enrolling Principal Investigator: Emad Ibrahim, MD Contact: Orrey Padilla | phone: 305-243-1491 | email: oxp210@med. miami.edu
STAKEHOLDER PERCEPTIONS AND CLINICAL ASSESSMENT OF CARDIOMETABOLIC DISEASE/ SYNDROME AFTER SPINAL CORD INJURY
Purpose: This study investigates whether individuals with spinal cord injury (SCI) are aware of their risk for heart disease, diabetes, and other health problems, and how these risks change over two years post-injury. Researchers will compare participants’ self-reported awareness with actual measurements of their risk factors.
Qualification summary: Motor complete or incomplete, C5-L1, traumatic spinal injury; 18 – 70 years old; within 2 months of discharge from initial rehabilitation post-injury. (contact for more information)
Status: Enrolling Principal Investigator: Mark S. Nash, Ph.D.
Contact: Katherine Martinez | phone: (786)-540-4104 | email: kxm940@ miami.edu
SPINAL CORD INJURY REGISTRY (NORTH AMERICAN CLINICAL TRIALS NETWORK)
Summary: The NACTN Spinal Cord Injury Registry aims to understand the natural course of recovery and complications in newly injured patients by collecting one-year follow-up data. This information will help design future clinical trials by identifying high-risk periods and expected recovery patterns.
Qualification summary: This study is for men or women 18 or older with a new traumatic spinal cord injury causing paralysis, weakness, or numbness, who haven’t received prior medical care for this injury at a specific type of hospital and can consent to participate. (contact for more information)
Status: Enrolling Principal Investigator: James D. Guest, MD, Ph.D.
Contact: George Jimsheleishvili, MD | phone: 305-243-4781| email: gxj150@med.miami.edu
SAFETY AND EFFICACY OF AUTOLOGOUS HUMAN SCHWANN CELL (AHSC) AUGMENTATION OF NERVE AUTOGRAFTS AFTER SEVERE PERIPHERAL NERVE INJURY
- This is open only to people with severe injury to a peripheral nerve (in leg or arm) and is NOT open to people with a spinal cord injury.
Purpose: To evaluate the safety of injecting one’s own Schwann cells along with nerve autograft (e.g. sural nerve – the sural nerve is a sensory nerve in the leg) after a severe injury to a major nerve has occurred. The secondary purpose of this research project is to evaluate whether transplanted Schwann cells can enhance recovery of sensory and motor function.
Qualification summary: This study is for people aged 18-65 with a severe recent nerve injury in their arm, leg, or sciatic nerve, but excludes people with certain medical conditions, pregnancy, or substance abuse. (contact for more information)
Status: Enrolling Principal Investigator: Allan D. Levi, M.D., Ph.D.
Contact: George Jimsheleishvili, MD | phone: 305-243-4781| email: gxj150@med.miami.edu
SYSTEMIC HYPOTHERMIA IN ACUTE CERVICAL SPINAL CORD INJURY
Purpose: This clinical trial investigates the use of intravascular hypothermia to improve neurological outcomes in acute cervical spinal cord injury patients. By potentially reducing dependence on caretakers and increasing patient productivity, this approach could benefit both patients and society. Qualification summary: This study is for adults 18-70 with a moderate or severe spinal cord injury (AIS A-C) from a non-penetrating blow, who can receive cooling treatment within 24 hours. It excludes people with very severe injuries, pre-existing health conditions, or who are pregnant. (contact for more information)
Status: Enrolling Principal Investigator: Allan D. Levi, MD, PhD Contact: George Jimsheleishvili, MD | phone: +1-305-243-4781| email: gxj150@med.miami.edu
COMPARING CLINICALLY VALIDATED UPPER-EXTREMITY ASSESSMENTS IN SCI
Purpose: This study aims to compare four common assessments used to measure upper limb function in adults with chronic tetraplegia. Researchers will assess participants using the GRASSP, CUE-T, ARAT, and Wolf Motor tests and compare their effectiveness in evaluating hand and arm function.
Qualification summary: This study is for adults (over 18) with chronic spinal cord injury in the neck (C2-C7) for over a year, regardless of injury severity (ASIA A-D), but excludes people with severe upper arm spasticity, fractures/contractures, or who cannot consent. (contact for more information)
Status: Enrolling Principal Investigator: David W. McMillan, Ph.D. Contact: Nilanjana Datta, MD | phone: 305-243-7108 | email: nxd693@ med.miami.edu
TRANSFORMATIVE POTENTIAL OF ADAPTED OCEAN ACTIVITIES
Purpose: This study aims to investigate the impact of open water activities (sailing, paddling, etc.) on health and wellbeing in disabled adults. Researchers will use surveys to assess self-reported changes in quality of life, self-efficacy, and other health domains following participation in these activities.
Qualification summary: Adults with disability who have participated at least one time in one of the adapted ocean activities being studied. (contact for more information)Status: Enrolling Principal Investigator: David W. McMillan, Ph.D.Contact: David W. McMillan, Ph.D. | phone: 305-243-5569 | email: dmcmillan@med.miami. edu
ACCURACY OF SELF-REPORT WEIGHT AND HEIGHT IN PEOPLE WITH SCI
Purpose: This study investigates the accuracy of self-reported weight and height in people with spinal cord injury. Researchers will compare selfreported measures with direct measurements and analyze how factors like time since last measurement and injury severity influence the accuracy of self-reporting.
Qualification summary: Adults with spinal cord injury or disease from any cause. (contact for more information)
Status: Enrolling Principal Investigator: David W. McMillan, Ph.D. Contact: Nilanjana Datta, MD | phone: 305-243-7108 | email: nxd693@ med.miami.edu
DEVELOPING A MULTI-CHANNEL QUANTATIVE
AUTONOMIC DIAGNOSTIC TO ASSESS THE SYMPATHETIC LEVEL OF INJURY Purpose: The study seeks to adapt the sympathetic skin response (SSR) test to determine the sympathetic level of injury (SLOI) in individuals with and without spinal cord injury (SCI), aiming to understand the correlation between sympathetic and somatic levels of injury. This investigation addresses the need for a clinically useful method to quantify sympathetic LOI, potentially enhancing practitioners’ understanding of changes in involuntary bodily functions following SCI. Qualification summary: Adults with and without spinal cord injury. (contact for more information)
Status: Approved, not yet recruiting
Principal Investigator: David W. McMillan, Ph.D.
Contact: David W. McMillan, Ph.D. | phone: 305-243-5569 | email: dmcmillan@med.miami.edu
URSOLIC ACID FOR MUSCLE STRENGTH AND GLYCEMIC CONTROL IN SCI
Purpose: The purpose of this pilot study is to assess the potential of Ursolic Acid (UA) in mitigating muscle wasting and insulin resistance in individuals with chronic spinal cord injury (SCI). By investigating UA’s effects on muscle mass, strength, and metabolic parameters, the study aims to provide insights into potential therapeutic strategies for improving health outcomes in the SCI population.
Qualification summary: This study is for men and women aged 18-65 with chronic (over 1 year) spinal cord injury, either complete or incomplete (AIS A/B/C), in either the thoracic (T2-T8) or cervical (C4-C7) spine. It excludes pregnant or breastfeeding women. (contact for more information)
Status: Concluding recruitment
Principal Investigator: Mark S. Nash, Ph.D.
Contact: Patricia Grahm | phone: 305-243-5119 | email: pgraham1@med. miami.edu
EXPLORING EFFECT OF MINDFULNESS ON QUALITY OF LIFE IN SCI
Purpose: The purpose of the study is to explore the impact of a one-month mindfulness intervention on physiological stress markers and quality of life in individuals with spinal cord injury (SCI). By measuring changes in heart rate, blood pressure, metabolism, and quality of life scores before and after the intervention, the study aims to provide insights into the potential benefits of mindfulness practices for SCI patients.
Qualification summary: This study is for adults (18-70) with spinal cord injury (C5-T10, any severity), who are healthy and able to consent, but excludes pregnant women and those on certain medications. (contact for more information)
Status: Approved, not yet recruiting
Principal Investigator: Mark S. Nash, Ph.D.
Contact: Patricia Grahm | phone: 305-243-5119 | email: pgraham1@med. miami.edu
BRAIN-CONTROLLED SPINAL SIMULATION THERAPY FOR RESTORATION OF WALKING AFTER INCOMPLETE SCI
Purpose: The purpose of this pilot clinical trial is to investigate the therapeutic effects of non-invasive Brain-Computer Interface (BCI)Transcutaneous Spinal Cord Stimulation (TSCS) therapy for improving neuromotor recovery in individuals with incomplete spinal cord injury (SCI). Through exploring effective therapy methods and optimizing brain decoding algorithms, the study aims to establish the feasibility and efficacy of long-term BCI-TSCS locomotor therapy, potentially offering a novel approach to enhance walking function in this population.
Qualification summary: This study is for adults (21-70 years old) with incomplete spinal cord injury (more than 6 months old) who have some leg movement and can commit to a 6-month training program. It excludes people with other neurological problems, severe spasticity, certain medical conditions, or metal implants. (contact for more information)
Status: Enrolling Principal Investigator: Matija Milosevic, Ph.D. Contact: Patricia Grahm | phone: 305-243-5119 | email: pgraham1@med. miami.edu
RELATION BETWEEN RESPIRATORY PERFORMANCE AND SEATED BALANCE IN SCI
Purpose: This study aims to investigate the relationship between breathing and balance in individuals with chronic spinal cord injury (SCI), focusing on how these functions impact quality of life and daily activities. Despite the known connection between breathing and balance, this link is not wellunderstood, especially in chronic SCI patients.Qualification summary: Adults with spinal cord injury. (contact for more details)
Status: Re-opening for enrollment
Principal Investigator: Mark S. Nash, Ph.D.
Contact: David W. McMillan, Ph.D. | phone: 305-243-5569 | email: dmcmillan@med.miami.edu
SPINAL CORD NEUROMOULATOR BY SPINEX AND SCONE TO TREAT NEUROGENIC BLADDER
Purpose: The purpose of the SCONE “CONTINENCE” CLINICAL STUDY is to evaluate the efficacy and safety of the SpineX Spinal Cord Neuromodulation (SCONE) Device in treating Neurogenic Lower Urinary Tract Dysfunction (NLUTD) resulting from spinal cord injury, multiple sclerosis, or stroke. This prospective, multicenter, single-blind, randomized sham-controlled study aims to assess the comparative effectiveness of SCONE neuromodulation therapy versus inactive sham control in improving symptoms of NLUTD over a 12-week period. Qualification summary: This study is for men and women aged 18-75 with lower urinary tract dysfunction due to spinal cord injury, stroke, or multiple sclerosis. They must be able to self-catheterize or have urgency/frequency urination. It excludes people with certain medical conditions, catheters, or implants, and those who are pregnant, breastfeeding, or have significant social/psychological problems. (contact for more information)Status:
Recruitment concluding
Principal Investigator: Raveen Syan, MD Contact: Zoe Szczotka | email: zxs537@miami.edu
THE MICROBIOME AFTER SCI: GASTROINTENSTINAL DYSFUNCTION MECHANSISMS AND MARKERS OF GI STATUS
Purpose: The purpose of this study is to investigate the impact of spinal cord injury on the intestinal microbiome and epithelium, aiming to uncover mechanisms underlying gastrointestinal dysfunction and identify potential biomarkers. By examining alterations in gut microbiome composition and intestinal tissue function, the study seeks to inform the development of personalized therapeutic interventions for individuals with spinal cord injury.
Qualification summary: This study is for people aged 18-65 with spinal cord injury (tetraplegia or paraplegia) and constipation or bowel problems, or for healthy people of the same age range. It excludes people with certain medical conditions, implants, or recent surgery, and those who are pregnant or breastfeeding. (contact for more information)
Status: Enrolling
Principal Investigator: Sylvia Daunert, PharmD, Ph.D. Contact: Gregory O’Connor, Ph.D. | phone: 305-243-6282 | email: goconnor@miami.edu
NUTRITION EDUCATION PROGRAM IN SCI (NEURONUTRITION CLINIC)
Purpose: This study aims to assess whether a year-long nutrition education program improves dietary knowledge and related health markers in individuals with spinal cord injury. Researchers will compare bloodwork, body measurements, and nutrition knowledge tests before and after the program.
Qualification summary: This study is for consenting adults (18+) with spinal cord injury (paraplegia or tetraplegia), but excludes pregnant women, children, and prisoners. (contact for more information)
Status: Enrolling Principal Investigator: Elizabeth Felix, Ph.D. Contact: Alicia Sneij, PhD, RD | phone: 305-978-4079 | email: a.sneij@ umiami.edu
If you would like to be considered for these, or future Miami Project trials or studies, please see our Register for a Research Program section of our website, send us a message, or call The Miami Project Education Office at 305-243-7108.
The Miami Project believes in working with our local community to develop and implement strategies that can potentially treat paralysis.
The Miami Project’s Office of Education and Outreach, directed by David W. McMillan, Ph.D., links a variety of non-scientific stakeholders to The Miami Project’s dizzying diversity of cutting-edge science and technical expertise. Doing so requires the liaising of a single mission across a wide variety of audiences and settings that are not obviously related, from climatologists framing climate justice through the lens of spinal cord injury to architectural students on a sailboat contemplating the accessibility of floating structures.
The Office’s outreach to Shake-A-Leg Miami (SALM), a local not-for-profit with a regional mission to provide ocean access for all, exemplifies the multi-modal education and outreach approach. Harry Horgan founded SALM after a sit-ski experience transformed his life post-SCI, but the organization did not have a Miami mission until the invitation of Dr. Barth Green brought Harry and his efforts to the Tropical Atlantic to harness the healing powers of the sea. The Miami Project’s outreach strategy to SALM includes linking all three University of Miami campuses—the Medical Campus housing the Miller School, the Marine Campus housing the Rosenstiel School, and the Gables Campus housing the remaining majority of academic units. This complex outreach strategy has begun to bear fruit, with collaborators across various disciplines now integrating The Miami Project’s mission into their seemingly unrelated efforts. The Climate Resilience Academy (CRA) course, a flagship academic effort, aligned with Miami’s current and coming need for climate adaptation. Via collaboration with professor Katherine “Katie” Mach, Ph.D., the course now includes a module on Climate Justice where spinal cord injury is used as a teaching case of disproportionate vulnerability to climate hazards, complete with Miami Project research participants giving guest lectures from their wheelchairs from the perspective of lived-experience. Via collaboration with School of Architecture (SoA) professor Veruska Vasconez and instructor Sophie Juneau a design studio, titled “The Aquatic Dis_Ordinary”, was conducted where architecture students dove into the realm of inclusive design in the maritime environment, focusing on the accessibility of floating structures

designed so people with paralysis can participate in coastal society. The students visited SALM’s facilities to interact with current accessibility solutions in this context, and received a lecture from the deck of a wooden cat-ketch sailboat. Via collaboration with College of Engineering’s (CoE) professor Derin Ural, Ph.D. and instructor Nina Mariea Jean-Louis Amador, the novel Innovation, Technology, and Design (ITD) program now includes a Miami Project aligned effort in their unique multi-semester student-lead “design challenge” project. One of the ITD design challenge groups is employing the design thinking process to find solutions to boat and water ingress and egress challenges, focusing on the historic Freedom 20 keelboats designed by none other than Harry himself. Finally, via collaboration with School of Communication (SoC) professor Trevor Green, journalism students learning about documentary filmmaking are showcasing the stories of paralyzed stakeholders overlapping with The Miami Project community, from adapted scuba diving to mixedabilities dancing via a profile of the Karen Peterson Dancers who have performed at a Miami Project event.

A group of University of
students
demonstrations of aquatic accessible solutions alongside a number of people with disability who are the end users of these technologies

Expanding its reach beyond UM, the Office is excited to be collaborating with Dr. Suan Solman, D.P.M., R.Ph., a tetraplegic professor of medicine at Florida International University (FIU) Herbert Wertheim College of Medicine. Dr. Solman is spearheading a much needed initiative to increase the accessibility of healthcare. Launched by an award from the Christopher and Dana Reeve Foundation titled “Educating Medical Students on Examining and Caring for People Living with Paralysis,” lectures and hands-on workshops on safe transfers and primary care are now integrated into medical and physician assistant program coursework. Dr. Solman pays people living with paralysis from SCI to participate in the workshop as real models, showcasing the power of realistic simulation training in instilling inclusive care in medical education. Dr. McMillan infuses the educational effort with The Miami Project expertise by partnering with Dr. Solman and delivering lectures on transfer techniques as well as inclusivity in the primary care setting, emphasizing the difference between cure and care. They continue to collaborate on the project, with plans to scale the workshops to other campuses to increase accessibility in the medical education setting.

Alongside these recent advancements, the Office’s engagement continues to nurture the next generation of neuroscience enthusiasts. The BrainBee, a neuroscience competition for teens, congratulates the 2024 Miami BrainBee winner Davud Skenderi and wishes him luck in the national competition. As part of the prize, Davud and his peers embarked on a tour of TMP’s facilities, brining into reality the neuroscience concepts and techniques they learned about in theory. The BrainFair was once again a success at the Miami Dade County Public School (MDC-PS) Science, Technology, Engineering, Art and Mathematics (STEAM) Expo. This primary education neuroscience education and outreach event involves collaboration with Florida International University (FIU), St. Thomas University, and Barry University. Dr. McMillan and new outreach coordinator Alejandro Labrada also joined The Miami Project faculty member Gillian Hotz in her KiDZ Neuroscience Center pedestrian safety education and outreach efforts. At local primary schools, the WalkSafe and BikeSafe events emphasize the unique pedestrian safety concerns faced by many wheelchair users and discuss some of the similarities and differences between bicycle and wheelchair infrastructure solutions.

Each year, scientists at The Miami Project seek funding for their research by submitting proposals to the National Institutes of Health, the Department of Defense, and other funding agencies and foundations.
Their scientific peers rate the merits of the proposed experiments in a highly competitive process, and only the best projects are funded. The agencies and organizations listed here supported research at The Miami Project during 2023.
Grants & Contracts
Restricted Gifts
Endowment
IDC Allocation
Other Income & Credit
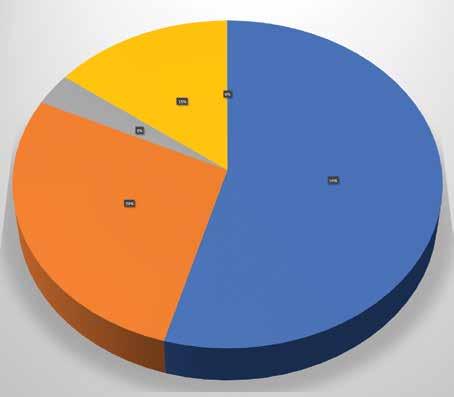
Income Expenses
Research Programs
Fund Raising
General Administration


National Institutes of Health (NIH)
Dietrich D (PI) Human Schwann Cell-Derived Exosome Treatment for Traumatic Brain Injury
Lee J (PI) Regeneration-permissive glia after spinal cord injury
Tsoulfas P (PI) Combinatorial Manipulation of Transcription Factors to Promote CNS Regeneration
Prasad A (PI) Effects of Iron Accumulation in Intracortical Implants and Protection by Iron Chelation
Levi A (PI) University of Miami Neurosurgery eDucation Strategy (UMINDS)
Levi (Co-I) Schwann cell delivery via enhanced collagen-glycosaminoglycan tubes to improve outcome from critical length nerve gap repairs
Liebl D (PI) Stabilizing the tripartite synaptic complex following TBI
Al-Ali H (PI) Developing a kinase inhibitor drug to treat spinal cord injury
Lee J (PI) Targeting cell-type specific disease phenotypes to promote CNS repair
Lee J (PI) Targeting lipid clearance pathways to promote repair after SCI
Ganzer P (PI) Enhancing Sympathetic Outflow Control Following Spinal Cord Injury Using Targeted Plasticity Therapy
Starke R (PI) Endothelial cell dysfunction in cerebral aneurysm pathogenesis
Lemmon V (PI) Targeting multiple kinases to treat experimental spinal cord Injury
Lemmon V (PI) Pan-Neurotrauma Data Commons
Dietrich D (PI) and de Rivero Vacari JP (Co-I) The Importance of Abnormal Inflammasome Activation as a Risk Factor between Traumatic Brain Injury and Alzheimer’s Disease
de Rivero Vaccari JP (Co-PI) Keane (Co-PI) Role of ASC in TBIMediated Systemic Inflammation
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
Brambilla R (PI) Role of astrocytic TNF receptor 2 in synaptic stability and cognitive function after traumatic brain injury
Ibrahim E (Sub-I) Disease Modifying Treatment Using Combined Shockwave Therapy and Platelet Rich Plasma In Microvascular Erectile Dysfunction
National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR)
Nash M (Co Project Director) South Florida Spinal Cord Injury Model Systems
Department of Defense (DOD) and United States Army Medical Research Acquisition Activity (USAMRAA)
Levi A (PI) Systemic Hypothermia in Acute Cervical Spinal Cord Injury – A Prospective Case Controlled Study
Levi A (PI) Safety and Efficacy of Autologous Human Schwann Cell (ahSC) Augmentation in Severe Peripheral Nerve Injury (PNI)
Noga B (PI) DBS Orientation Selective Pathway Activation for Gait
Ignition Following SCI
Pearse D (PI) targeting the arginylation pathway Neuroprotection After SCI
Pearse D (PI) Functionalized Peptide Gels and Schwann Cells for Repair of the Injured Spinal Cord
Ibrahim E (PI) A Novel Therapy to Improve Reproductive Potential in Men with Spinal Cord Injury (SCI)
Widerström-Noga E (PI) Consumer perspectives on a multimodal approach to make neuropathic pain manageable after SCI
Widerström-Noga E (PI) Mechanisms and Utility of Multisensory BodyRepresentation in SCI and SCIRelated Neuropathic Pain
Sagen J (PI) Innovative treatment for


neuropathic pain after spinal cord injury
Sagen J (Co-I) Testing RNA Aptamers as Analgesic Candidates in a Rat Model of SCI pain
Sagen J (PI) Alleviation of chronic SCI neuropathic pain using novel engineered human iPSC-derived chromaffin cell grafts
Sagen J (PI) Developing Gene Therapies Targeting Cannabinoid Receptors for Treatment of Chronic SCI Pain
Lee J (PI) Macrophage-Specific Drug Targets for Treating SCI
Dietrich D (PI) Preclinical Evaluation of FDS Approved Human Neural Stem Cell
Burks S (Site PI) Nerve transfers to improve upper extremity function and quality of life in tetraplegic patients
Veterans Affairs Medical Center (VAMC) & U.S. Department of Veteran Affairs (VA)
Kerr N (Co-I) IPA Therapeutic interventions for post-stroke rehabilitation
Dietrich D (Co-I) Therapeutic interventions for post-stroke rehabilitation
Bramlett H (PI) Novel Pharmacological and NonPharmacological Interventions for Bone Loss in SCI
Atkins C (PI) Chronic memory Risk Factors for Chronic Memory Problems after Traumatic Brain Injury
Atkins C (PI) The Interaction of Stress and Mild Traumatic Brain Injury
Sagen J (PI) Evaluation 6SHG/EM1 as a treatment for spinal cord injuryinduced neuropathic pain in a pig model
Ghosh M (Co-I) Exosomal vesicles for neuroprotection and repair after SCI
Lemmon V (Co-I) Shuanglin Hao The molecular mechanisms of astrocytes-neurons interaction in the morphine use disorder
Florida Department of Transportation (FDOT)
Hotz G (PI) BikeSafe Middle School Clubs in Miami-Dade County
Hotz G (PI) BikeSafe Elementary School Program in Miami-Dade County
Hotz G (PI) Sustainability and Expansion of the WalkSafe and BikeSafe Programs for K-8 Grades in Miami-Dade County
Florida Department of Health (FDOH)
Bramlett H (PI) Post-stroke combination of therapeutic hypothermia (TH) and whole bodyvibration (WBV) improves cognition in nicotine- exposed rats
Starke R (PI) Cigarette smoke induces endothelial dysfunction leading to cerebral aneurysm pathogenesis
Shah A (CO-I) Levi A (CO-I) Pilot Award RFA Florida Center for Brain Tumor Research
Dietrich D (PI) The Administrative Core
Brambilla, R (PI) Restoring cholesterol homeostasis for neuroprotection and neurorepair in spinal cord injury
Jergova S (PI) Analgesic potential of transplanted recombinant human iPSCs and their exosomes in a model of spinal cord injury induced pain
Kerr N (PI) The role of extracellularvesicle mediated inflammasome signaling in disruption of the bidirectional brain-gut axis after Traumatic Brain Injury
Lemmon V (PI) Spatial Omics of Human Spinal Cord Injury
Guest J (PI) Determination of effects of Transcutaneous Spinal Cord Stimulation on cortical, brainstem, and local segmental outputs to improve function and reduce spasticity
State of Florida (MMJ Outcomes)
Widerström-Noga (PI) Effects of cannaboidiol on resting state EEG and neuropathic pain severity in people with spinal cord injury
Craig H. Neilsen Foundation (CNF)
Sagen J (PI) Human iPSC-derived chromaffin cell transplants for alleviation of chronic neuropathic SCI pain
Lemmon V (PI) Bixby J (Co-PI)
Al-Ali H (Co-PI) Novel and potent compounds that promote axon growth
Nash M (Co-PI) Intermittent Hypoxia, Respiratory Performance, and Motor Plasticity after Spinal Cord Injury
Vastano R (Co-P.I.), WiderströmNoga E (Co-P.I.) EEG correlates of multisensory integration in spinal cord injury: sensory and pain mechanisms.
Widerström-Noga E (PI) Development of pain education for improving pain health literacy and quality of life after spinal cord Injury
Christopher & Dana Reeve Foundation (CRF)
Widerström-Noga E (PI) The impact of spinal cord injury and neuropathic pain on multisensory bodyrepresentation
Guest J (Center P.I. and Co-chair) North American Clinical Trials Network for the Treatment of SCI
Florida Brest Cancer Foundation
de Rivero Vaccari JP (PI) Inflammatory Responses in Radiosensitivity and Breast Cancer Prognosis Disparity
Bryon Riesch Paralysis Foundation
Ghosh M (PI) Targeting innate immune response to promote histopathological & locomotor function after spinal cord injury repair
Alzheimer’s Association
Kerr N (PI) Pyroptosis-induced gut-brain disruption after stroke in Alzheimer’s disease
Fondazione Italiana Sclerosi Multipa (FISM)
Brambilla R (PI) Cognitive dysfunction in multiple sclerosis: role of astroglial TNFR2 signaling
League of American Bicyclists
Hotz G (PI) popup protection safe cycling for all
NeuroTrauma Sciences
Atkins C (PI) Re-Calibration of the Fluid Percussion Device to Model Moderate-to-Severe TBI in the Sprague Dawley Rat
BrainQ Tech
Dietrich D (PI) The safety and efficacy of a BCI-based electromagnetic field treatment in chronic SCI - A Pilot Study
BioResponse, LLC
Atkins C (PI) Evaluation of Parenteral Diindolylmethane (BR4044) for

Miami Project graduate students pointing out features of an image produced by the High Content Screening Core
Treatment of Fluid Percussion induced Traumatic Brain Injury (TBI) in Rats
Neurosurgery Research & Education Foundation (NREF)
Shah A (PI) Epigenetic potentiation of immune checkpoint inhibition through endogenous retroviral immune responses
Ed and Ethel Moore Alzheimer’s Disease Research Program
Atkins C (PI) Cyclic Nucleotide Regulation in Alzheimer’s
Dietrich D (PI) The Importance of the Innate Immune Response as a Mechanistic Link between TBI and AD
Elsa U. Pardee Foundation
Shah A (PI) Targeting Epigenetic Regulators of Endogenous Retroviruses to potentiate Immunotherapy for Glioblastoma
Paralyzed Veterans of America
Ibrahim E (PI) How to manage reproductive and sexual dysfunction in men with spinal cord injury? A provider workshop
Rails to Trails Conservancy
Hotz G (PI) Rails to Trails Conservancy Grant
Society of NeuroInterventional Surgery Foundation (SNIS)
Starke R (PI) Optical coherence
tomography to evaluate in-stent endothelial growth following endovascular treatment of cerebral aneurysms
National Football League
Hotz G (PI) Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI Longitudinal Study)
Else Kroner-Fresenius-Stiftung
Lee J (CO-I) Role of the bloodderived coagulation factor Fibrinogen on Fibrotic Scaring In CNS disease
NASA Headquarters
de Rivero Vaccari J (PI) Inflammation
The faculty of The Miami Project are a talented multidisciplinary team. In the following Profiles, each faculty member describes their specific research focus and highlights of recent progress.

W. DALTON DIETRICH, PH.D.
Scientific
Director
Kinetic Concepts Distinguished Chair in Neurosurgery
Senior Associate Dean for Discovery Science
Professor, Departments of Neurological Surgery, Neurology, and Cell Biology
Neuroprotection and Improved Recovery of Function following CNS Trauma
My laboratory is focused on clarifying the pathophysiology of brain and SCI with the goal of developing new therapies to protect and enhance functional recovery. My colleagues and I have studied the cellular and molecular injury mechanisms underlying various neurological disorders including stroke, TBI, SCI, and neurodegenerative diseases. We have advanced our pre-clinical therapeutic hypothermia findings into the clinic where we are conducting clinical trials in patients with SCI. Recently, we have also investigated the importance of abnormal inflammasome activation in the brain and SCI and identified a novel therapeutic target for neuroprotection. We are using novel cellular and drug treatments to promote reparative processes and functional recovery. My laboratory is funded by the NIH and DoD and I also train the next generation of scientists and clinicians in neurotrauma research.

ALLAN D. LEVI, M.D.,
PH.D., F.A.C.S.
Robert Buck Distinguished Chair in Neurological Surgery
Professor, Departments of Neurological Surgery, Orthopedics, and Physical Medicine & Rehabilitation
Chairman, Department of Neurological Surgery
Chief of Neurosurgery, Jackson Memorial Hospital
Cellular Transplantation Strategies after SCI/Systemic Hypothermia after Acute SCI
My clinical research interests currently focus on developing cellular transplantation strategies to repair injuries within both the human central and peripheral nervous system. I am currently Co-PI on our clinical trials involving the transplantation of autologous human Schwann cells (SCs), which represent first-in-man studies of autologous human SCs for patients with sub-acute and chronic SCI. We are also conducting a phase I trial evaluating SCs for peripheral nerve injuries with long segmental defects, which follows up on our previous two single patient experiences. Hypothermia continues to show promise in a variety of acute central nervous system injuries. There are various factors that need to be considered with systemic cooling of the SCI patient, including methods of cooling, window from injury to initiation, duration and depth of hypothermia, rate of re-warming, etc. While profound levels of hypothermia (<32°C) can be difficult to administer and are subject to increased complication rates, mild (modest) levels of hypothermia (32-34°C) have been shown to provide significant protection against traumatic and ischemic neuronal cell death. I am currently the PI of our institutional protocol as well as a multi-center Department of Defense funded randomized trial studying systemic hypothermia induced via an intravascular catheter and continued for 48 hours after acute cervical SCI.

BARTH A. GREEN, M.D.,
F.A.C.S.
Professor of Neurological Surgery, Neurology, Orthopedics, and Rehabilitation
Co-Founder and Chairman, The Miami Project to Cure Paralysis
Executive Dean for Global Health and Community Service
Translational Interventions
Over the recent years my research efforts have mainly involved taking the cutting edge basic neuroscience work product and data created by our Miami Project team from the bench to our UM affiliated clinics and hospitals. A good example of such translational research efforts has included the use of modest hypothermia for neuroprotection both in cases of acute spinal cord injury and for use in the operating room for patients undergoing high risk spinal cord surgery. I am also privileged to be able to collaborate with The Miami Project cellular transplantation programs and have been working on projects involving adult mesenchymal stem cells, as well as being part of the major effort transforming our successful Schwann cell laboratory model into clinical trials. Other areas of research and clinical interest include the diagnosis and treatment of tethered cord syndrome, spinal cord cysts and Chiari I malformation.
HASSAN A ALI, PH.D.
Associate Professor, Department of Neurological Surgery and Medicine
Drug Discovery for CNS Repair
As a chemical and computational biologist, my lab focuses on identifying pharmacological targets that can induce robust axon regeneration in the injured central nervous system. To accomplish this, my lab developed a unique drug discovery platform that combines phenotypic screening, target-based profiling, and sophisticated machine learning algorithms. The approach identified a promising drug candidate that is now in preclinical development. We continue to develop these methodologies to advance drug discovery in spinal cord injury, as well as in other therapeutic areas including cancer and kidney disease.

COLEEN ATKINS, PH.D.
Associate Professor, Department of Neurological Surgery

Developing Novel Therapies for Traumatic Brain Injury and Spinal Cord Injury
The research in my laboratory focuses on developing novel therapeutic interventions for traumatic brain injury (TBI) and spinal cord injury (SCI). The research goal of my laboratory is to enhance rehabilitation and recovery by manipulating synaptic plasticity at specific levels of the neuroaxis following TBI and SCI. We have found that specific synaptic plasticity signaling pathways are altered after TBI, and we are currently using pharmacotherapies to target those pathways to improve behavioral recovery after TBI.

JOHN BIXBY, PH.D.
Professor, Departments of Molecular & Cellular Pharmacology and Neurological Surgery, Center for Computational Science, Hussmann Institute for Human Genomics, Sylvester Cancer Center Vice Provost for Research
VANCE LEMMON, PH.D.
Walter G. Ross Distinguished Chair in Developmental Neuroscience
Professor, Department of Neurological Surgery, Center for Computational Science, Hussmann Institute for Human Genomics, Sylvester Cancer Center High Content Screening and Functional Genomics of the Nervous System

Our laboratory has developed methods to test thousands of genes or chemicals in hundreds of thousands of neurons each week to obtain quantitative information about cell morphology and gene expression. This “high throughput” capability allows us to tackle questions about axon growth and regeneration using systems biology approaches, and to query the results in animal models of injury. The Lemmon-Bixby lab has several ongoing projects related to axon regeneration. One project is to test the roles of known signaling proteins called protein kinases. In this screen we have tested >1600 kinase inhibitors, dozens of which strongly promote neurite growth in vitro. Using bioinformatics, biochemistry, and machine learning we can identify key kinases and their signaling networks as well as potential lead therapeutic compounds, one of which has proven active in two different models of spinal cord injury. A second project is based on the observation that injured peripheral sensory neurons initiate a genetic program appropriate for axonal regeneration. Our laboratory has combined next-generation sequencing with cell-based phenotypic screening to identify genes, especially transcription factors, that appear to mediate this genetic program, and is testing them in vitro and in vivo. The last project is to test several hit compounds identified in a screen testing 440 million different small molecules to see if the hits promote axon regeneration.

ROBERTA BRAMBILLA, PH.D.
Associate Professor, Department of Neurological Surgery
Modulation of the Neuro-Immune Response in Neurologic Disease
The main focus of my research is to understand the role of neuroinflammation in the pathophysiology of neurodegenerative disorders (e.g., multiple sclerosis, spinal cord injury and stroke), with a specific interest in the contribution of glial cells. We study astrocytes and microglia for their involvement in the neuro-inflammatory response to injury, and oligodendrocytes and oligodendrocyte precursor cells for their role in axon myelination, metabolic support of neurons and myelin repair. Currently, our primary lines of research in the area of neuroimmunology are centered on: (1) investigating the role of tumor necrosis factor and its receptors in the processes of neuroinflammation, demyelination and remyelination, and (2) understanding how mitochondrial dysfunction in oligodendrocytes may be involved in the etiopathology of multiple sclerosis.
HELEN M. BRAMLETT, PH.D.
Professor, Departments of Neurological Surgery and Psychology, Undergraduate Neuroscience Program Director, and Health Scientist Veterans Affairs
The Pathophysiology and Treatment of CNS Injury
The focus of my neurotrauma laboratory is to investigate both acute and long-term consequences of brain and spinal cord trauma. My current research interests are on the pathophysiology of traumatic brain and spinal cord injury with an emphasis on the pathogenesis of progressive white matter damage as well as the benefits of therapeutic hypothermia. My laboratory is also investigating mechanistic events leading to the development of posttraumatic epilepsy. Additionally, our current work is also focusing on complex traumatic brain injury models that mimic polytrauma as this type of injury has become more prevalent in combat areas.

JUAN PABLO DE RIVERO VACCARI, PH.D., M.S.B.A.
Associate Professor, Department of Neurological Surgery
Underlying Mechanisms of the Immune Response and Contributions to Various CNS Diseases
My research focuses on understanding early inflammatory events in central nervous system (CNS) injury and disease, as well as aging. Currently, my laboratory studies how natural-aging produces inflammation in the brain, a phenomenon known as brain inflammaging, which potentially precedes the onset of age-related neurodegenerative diseases. In addition, we are studying the mechanism by which brain injury causes systemic inflammation such as acute lung injury. Moreover, we also study the prognostic and diagnostic potential of inflammasome proteins as biomarkers of CNS injury and disease, including brain and spinal cord injury, stroke, multiple sclerosis, mild cognitive impairment and depression.
COURTNEY M. DUMONT, PH.D.
Assistant Professor, Department of Biomedical Engineering
Biomaterial Approaches for Spinal Cord Injury Repair
We are currently exploring the integration of nanoscale biomaterials with our scaffolds to improve on-demand pharmacological agent localization within the injury site as well as cytokine scavenging capabilities to reduce inflammation. Together, these strategies will help to move the field of neural tissue engineering forward, while also providing essential information about the underlying cellular biology and injury pathophysiology.


PATRICK D. GANZER, PH.D.
Assistant Professor, Department of Biomedical Engineering Neural Engineering, Brain-Computer Interfaces, Bioelectronic Medicines and Machine Learning
Broadly we are focused on the role that bioelectronic medicines will play in the understanding and treatment of neurological conditions, with a special focus placed on the importance of timing of stimulation with biologically relevant events. I come to The Miami Project from a background of research focused on enhancing neuroplasticity after sensorimotor injury using targeted vagus nerve stimulation, notably as a Principal for Battelle Memorial Institute’s Bioelectronic Medicine program and the N3 program funded by DARPA. I carry on my work with vagus nerve stimulation, and expand my lab via The Miami Project to understand and steer the somatic and autonomic nervous system after spinal cord injury (SCI).

MOUSUMI GHOSH, PH.D.
Research Associate Professor, Department of Neurological Surgery
Altering Host Glial Responses following CNS Injury and Disease to Promote Repair
My research interests are focused on altering the hostile environment of the injured or diseased CNS to one that is conducive to repair through altering inflammation. Specifically, our work focuses on delineating the intrinsic and extrinsic signals present after injury that antagonize the conversion of activated microglia and macrophages to a reparative phenotype in experimental models of CNS injury and disease. We are also interested in understanding how altering the immunophenotypical profile of macrophages and microglia can modulate spinal cord injury induced central neuropathic pain, affect host glial responses, including glial scar formation, as well as influence the ability of transplanted cells, such as Schwann cells and stem cells, to mediate neurorepair.


JAMES D. GUEST, M.D., PH.D., F.A.C.S.
Clinical Professor, Department of Neurological Surgery
The Preclinical to Clinical Spectrum in Spinal Cord Injury Therapeutics. The Path to Clinical Testing and Establishing Clinical Evidence
Our SCI research spans preclinical proof-of-concept studies of therapeutics into early Phase, and pivotal clinical trials of SCI. We are translational scientists using a variety of clinicallyrelevant tools within the complex process of determining which potential human therapeutics have a probability of success in clinical trial testing. We use our experience and expertise to test combinations of cellular, molecular, tissue engineering and neuromodulatory therapeutics in large animal models. We have expertise in tissue physiologic monitoring, neurophysiology and kinematic analysis of gait. In addition, we have experience in device development and testing. The lab group has members and colleagues ranging from senior medical faculty to postdoctoral students, medical students, neurosurgery residents, and undergraduate students. This is a good setting for those trainees who aim for careers in neurologic therapeutics both in academia and industry and with an interest in how medical evidence is developed. We are simultaneously involved with animal and human studies across the translational spectrum including Phase 1-3 studies.
GILLIAN A. HOTZ, PH.D.
Research Professor, Department of Neurological Surgery Director, KiDZ Neuroscience Center; Director, Concussion, WalkSafeTM & BikeSafeTM Programs
Injury Prevention and Concussion Management

As a behavioral neuroscientist my clinical interests have always been investigating the neurocognitive deficits of those individuals that have sustained a traumatic and acquired brain injury. I have co-authored two neurocognitive tests, The Brief Test of Head Injury for adults and the Pediatric Test of Brain Injury for children. My research has focused on developing evidence based injury prevention programs in order to prevent brain and spinal cord injuries in children. In 2003, our team developed the WalkSafe program, which has been shown to decrease the number of elementary school age children that get hit by cars, and in 2009 we developed the BikeSafe program which educated middle school age children on bicycle safety skills. As the Director of the Concussion Program, we have spent many years developing and implementing a comprehensive countywide high school sports concussion care program, which includes neurologic evaluation, neuroimaging, neuropharmacological management, neuropsychological testing, and baseline test with ImPACT, a computerized neurocognitive screening measure. We also have developed a Concussion Injury Surveillance system. Our program is multidisciplinary and assesses and treats athletes from all levels of play. I am also the PI on many local and federal grants: Safe Routes to School initiatives, Transportation Alternative Programs, GE/NFL MRI Phase 2 study, Brainscope EEG study, one of the TRACK TBI sites, and a new project that will study the Effects of Cannabinoids on Mild TBI.

EMAD IBRAHIM, M.D., HCLD
Assistant Clinical Profesor, Departments of Urology and Neurological Surgery
Male Fertility Following Spinal Cord Injury
The research is focused on understanding and improving the impairments to male fertility which occur following spinal cord injury (SCI). Following SCI, most men, but not women, experience impaired fertility. Specifically, most men with SCI are anejaculatory, and some experience erectile dysfunction. Although their semen may be obtained by medically-assisted ejaculation procedures, in most cases, semen quality is impaired, specifically, sperm motility and viability are abnormally low, although sperm numbers tend to be normal.

JONATHAN R. JAGID, M.D., BS ME
Clinical Professor, Department of Neurological Surgery, Neurology, Orthopedics, Rehabilitation Medicine
Interventions in SCI and TBI
My research includes projects investigating the use of Deep Brain Stimulation for spinal cord injury, novel brain machine interfaces to improve quality of life in spinal cord injury, as well as hypothermia for traumatic brain injury. Presently, we are looking at the use of a novel Deep Bain Stimulation device modified to act as a brain machine interface in an effort to bypass spinal cord injury and restore cortically controlled limb movement.
STANISLAVA JERGOVA, PH.D.
Research Assistant Professor, Department of Neurological Surgery
Advancing Chronic Pain Relief: Recombinant Human Cells and Gene Strategies
Our lab’s research goals involve investigating potential cell and gene therapies for chronic pain induced by spinal cord injuries (SCI) and other injuries of the central nervous system. We aim to better understand the mechanisms of chronic pain and develop new treatment options that can provide long-lasting relief for patients. As chronic pain is a multifactorial condition with several pathways involved, simultaneous targeting of different pathways with precise localization is essential. Recombinant cells and designed analgesic genes provide a great tool to achieve our goal. We explore different biomaterials as delivery vehicles to develop safe and potent approach to combat chronic pain.


ROBERT W. KEANE, PH.D.
Professor, Departments of Physiology & Biophysics, Neurological Surgery, and Microbiology and Immunology
Regulation of Innate Immunity after CNS Trauma
Innate immunity is the first line of defense against pathogens and host-derived signals of cellular stress. My research focuses on investigating mechanisms that direct normal innate immunity and its dysregulation in central nervous system injury and disease, including (1) agonists and activation mechanisms of inflammasomes, (2) regulatory mechanisms that potentiate or limit inflammasome activation after injury, and (3) emerging data linking inflammasome proteins as biomarkers for CNS injury.
NADINE A. KERR, PH.D.
Research Assistant Professor, Department of Neurological Surgery
Mechanisms of Systemic Organ Dysfunction after Central Nervous System Injury
The focus of our research is to examine the pathomechanisms of the systemic inflammatory response and non-neurological organ dysfunction following Central Nervous System (CNS) injury, particularly traumatic brain injury (TBI) and stroke. After CNS injury and damage to the blood-brain barrier (BBB), inflammatory mediators are released into the circulation and contribute to systemic organ damage. This can then lead to further neurological damage resulting in bidirectional communication between the brain and systemic organs. The two main organ systems that we are currently investigating are the respiratory and gastrointestinal systems.


DANIEL
JAE K. LEE, PH.D.
Professor, Department of Neurological Surgery
Promoting Proper CNS Wound Healing Response to Enhance Regeneration
The long-term research goal in my laboratory is to elucidate the mechanisms of cellular interactions in the injured CNS that create an environment inhibitory to cellular regeneration. Similar to other tissue, injury to the CNS triggers a wound healing response characterized by inflammation, cellular proliferation, and matrix remodeling. Sometimes this wound healing response is incomplete and leads to tissue cavitation, while other times it is excessive and leads to scar formation (both gliotic and fibrotic). A better understanding of this scarring process will help identify novel therapeutic targets that can promote a more permissive environment for CNS regeneration.
J. LIEBL, PH.D.
Professor, Department of Neurological Surgery
Molecular Mechanisms that Regulate Cellular Dysfunction and Death Following CNS Injury, and Mechanisms to Promote Regeneration and Recovery
The goal of my laboratory is to identify the mechanisms that lead to CNS pathophysiology and its regenerative potential. We focus on growth and guidance molecules, which play important roles in the developing, regenerating, and injured nervous systems. Specifically, we are currently interested in areas of adult neurogenesis, neuroprotection, apoptotic cell death, synaptic plasticity, angiogenesis, regeneration, and therapeutic strategies. Overall, our approach is to develop novel strategies to minimize CNS damage and maximize regeneration/tissue repair, which can be best achieved through a comprehensive mechanistic approach.


ALBERTO MARTINEZ-ARIZALA, M.D., F.A.A.N.
Clinical Professor, Departments of Neurology, Neurological Surgery, and Physical Medicine & Rehabilitation
Pathophysiology and Treatment of Secondary Complications in Spinal Cord Injury
My research interests focus on common complications that are seen following spinal cord injury: pain, spasticity, syringomyelia, and tethered cord syndrome. My interests include investigating the basis for the development of the different spasticity and pain profiles in the spinal cord injured population and to study potential novel treatments for those conditions.
DAVID W. MCMILLAN, PH.D.
Director of Education and Outreach, The Miami Project
Research Assistant Professor, Department of Neurological Surgery
Understanding and Treatment of Secondary Complications of SCI; Community Partnership
My dissertation pertained to the role of the autonomic nervous system in the absorption, trafficking, and fates of dietary fat. I am now refocusing my efforts to align with local opportunities seen from my Outreach role—aiming at the disproportionate risks and rewards posed by the Tropical Atlantic on people living with SCI (PwSCI). Regarding risks, I study the vulnerabilities of PwSCI to climate hazards in the form of flooding, heat, and hurricanes. Regarding rewards, I study the transformative potential that adapted ocean activities—such as sailing, scuba diving, swimming, and others—carries for adults with physical disability.


MATIJA MILOSEVIC, PH.D.
Director of Neuromotor Rehabilitation, The Miami Project
Assistant Professor, Departments of Neurological Surgery and Biomedical Engineering
Neuromotor Rehabilitation
My research is focused on developing neuromodulation technologies and therapeutic approaches to restore and improve motor function of individuals living with spinal cord injuries. My research program applies a transdisciplinary approach, spanning the fields of neural engineering, neuroscience, and clinical translation to develop and test techniques and approaches for neuromotor recovery. My research team is developing approaches for therapeutic application of electrical stimulation to activate and elicit neuroplastic changes to spinal and corticospinal neural circuits.
JENNIFER C. MUNOZ PAREJA, M.D.
Associate Professor Pediatric Critical Care & Associate Program Director, Pediatric Critical Care, University of Miami Biomarkers in Acute Brain Injury
The overarching goal of my laboratory is to gain a comprehensive understanding of the diverse pathomechanisms contributing to adverse outcomes in pediatric acute brain injury. We strive to identify specific biomarkers that can be employed as objective measures for assessing the severity of pediatric acute brain injury, as well as predicting patient outcomes. Moreover, recognizing neuroinflammation as a central pathophysiological aspect of acute brain injury and acknowledging that a limited understanding of the intricate cellular and molecular sequelae has hindered previous translational efforts, my current focus centers around studying the role of the inflammasome in the innate immune response following injury. By accomplishing this, we aim to enhance our ability to evaluate injury severity and provide valuable prognostic and therapeutic information to this vulnerable population.

MARK S. NASH, PH.D., F.A.C.S.M.

Associate Scientific Director for Research, The Miami Project to Cure Paralysis
Vice-Chair for Research, Department of Physical Medicine & Rehabilitation Professor, Departments of Neurological Surgery, Physical Medicine & Rehabilitation, and Physical Therapy Co-Director, DHHS-NIDILRR South Florida SCI Model System
Physiological Assessment of Secondary Complications following SCI: Electrical Stimulation, Cardiometabolic and Vascular Physiology, Cardioendocrine Pathology and Intervention, and Exercise and Nutritional Biochemistry
One of the enduring goals of The Miami Project has been to test and then translate strategies that optimize health of persons with SCI. A significant target for this strategy has focused on physical activity to lessen secondary risks of SCI associated with physical deconditioning. We also examine complementary themes to optimize exercise prescription after SCI, identify optimal nutritional intake, and use prescription and non-prescription agents that reduce hazards of fasting and postprandial lipid disorders, dysglycemia, and vascular inflammatory stress.
BRIAN R. NOGA, PH.D.
Research Professor, Department of Neurological Surgery
Brain and Spinal Mechanisms Controlling Walking
Neuromodulation technologies are increasingly looked at as potential treatment options for paralysis associated with spinal cord injury (SCI). Deep brain stimulation is one such method that so far has had little or no application in persons with SCI even though most new and chronic injuries are incomplete. Recent work in our laboratory has pointed to a brain target for controlling walking. We are currently investigating the usefulness of stimulating this site to enhance walking in a translational large animal model of SCI.


KEVIN K. PARK, PH.D.
Associate Professor, Department of Neurological Surgery
Promoting Neural Regeneration and Survival
My lab is interested in understanding mechanisms that account for axon growth, guidance and circuit formation in the central nervous system (CNS). Previously, I and others have identified several key proteins that regulate axon regeneration, which are present in mature CNS neurons. In my current research, I seek to better understand the cellular and molecular mechanisms governing axon growth and connectivity during development and in adults after injury, and to explore the potential of developing therapeutic strategies for spinal cord injury and other neurodegenerative conditions.
DAMIEN D. PEARSE, PH.D.
John M. and Jocelyn H.K. Watkins Distinguished Chair in Cell Therapies Professor, Department of Neurological Surgery, Health Scientist Veterans Affairs
Exploration and Translation of Therapeutic Strategies to Repair the Injured Spinal Cord and Brain
My laboratory focuses on several key aspects of CNS injury repair, including (1) the utility and clinical translation of exogenous and endogenously harnessed cell therapeutics (particularly when used in combinatory approaches), (2) understanding the role of, and developing therapies for, altered cyclic AMP (adenylyl cyclase, phosphodiesterases, and PKA) and MAPK signaling in neurons and glia after CNS injury, (3) the use of nanotherapeutics for multifunctional and sitedirected gene/drug targeting to the injured CNS, and (4) the application of methodologies for improved imaging of axonal regeneration and cell integration within the injured CNS such as 3D ultramicroscopy and diffusion tensor imaging.


SUHRUD
ABHISHEK PRASAD, PH.D.
Associate Professor of Biomedical Engineering
Our lab is investigating better and alternate materials for electrodes and insulation that will minimize the corrosion and delamination problem. To mitigate the foreign body response due to implanted materials, we are using therapeutic and pharmacological approaches to reduce the neuroinflammation and oxidative stress that occurs after an electrode implant.
M. RAJGURU, PH.D.
Co-Director, Institute for Neural Engineering
Professor, Departments of Biomedical Engineering and Otalaryngology
Assistant Director, University of Miami CTSI Team Science
My laboratory and collaborators (W. Dalton Dietrich and Michael Hoffer) at the University of Miami have been at the forefront of using therapeutic hypothermia applied locally to the inner ear to benefit patients undergoing cochlear implantation. Now we have expanded its application using a custom-designed device and a unique non-invasive approach to noise-induced hearing loss. Our work on therapeutic hypothermia has been published in multiple peer-reviewed studies and presented at national and international conferences.


JACQUELINE SAGEN, PH.D., M.B.A.
Professor, Department of Neurological Surgery
Cellular Implants and Gene Therapy for the Alleviation of Chronic Pain and CNS Injury
Our laboratory is exploring novel and more effective strategies in the therapeutic management of chronic debilitating pain. Our recent research is focused on (1) identification of more effective analgesic agents and combinations for alleviating pain using SCI and peripheral neuropathic pain models and (2) development of emerging therapeutic interventions, including cell transplantation and gene therapy, which have the potential to provide long-term alleviation in people with intractable pain, overcoming the need for repeated pharmacologic administration.
PANTELIS TSOULFAS, M.D.
Associate Professor, Departments of Neurological Surgery and Cell Biology & Anatomy
Neurotrophins: Specificity of Action
My laboratory is interested in two areas of neurobiology that are significant for developing new strategies for spinal cord injury repair. Over the past years, we have worked to modify neurotrophins that are better suited for use in SCI. We are also interested in understanding the processes involved in maintaining and differentiating neural stem cells.


MICHAEL Y. WANG, M.D., F.A.C.S.
Professor, Departments of Neurological Surgery and Physical Medicine & Rehabilitation Director of Neurosurgery, University of Miami Hospital
Spinal Cord Injury Outcomes
My primary research has been in the investigation of SCI Outcomes. I work with Miami Project researchers Drs. Allan Levi and Barth Green in studying the clinical effects of Hypothermia. Currently, a multi-center randomized, prospective study on the effects of hypothermia in SCI is underway. In addition, I am studying the clinical application of SCI biomarkers to predict the effects of both injuries as well as therapeutic interventions with Drs. Dalton Dietrich and Ross Bullock.
EVA WIDERSTRÖM-NOGA, D.D.S., PH.D.
Research Professor, The Miami Project to Cure Paralysis, the Departments of Neurological Surgery and Physical Medicine & Rehabilitation
Interdisciplinary Research Approaches to Improve Neuropathic Pain Management after Neurotrauma

My research program is interdisciplinary and includes the identification of clinical correlates of underlying mechanisms of neuropathic pain associated with neurological trauma as a way to facilitate the translation of basic research findings to treatments tailored to specific mechanisms. A recent line of research in my program aims to better understand cortical mechanisms of multisensory integration and how to manipulate these mechanisms by visual illusion and transcranial electrical stimulation to reduce pain. In addition, we have examined SCI stakeholders (people with SCI and neuropathic pain, their significant others and SCI healthcare providers) perspectives on barriers and facilitators to optimal management of neuropathic pain. Based on this work we have developed a preliminary pain education tool that is now further refined based on structured stakeholder feedback. My research program is highly collaborative and includes extensive interdisciplinary protocols for a multimodal evaluation of self-reported pain symptoms and its psychosocial impact, quantitative assessment of neurological function, and biomarkers including non-invasive brain imaging and electrophysiology.

Published studies that have passed the test of peer review are the benchmark of scientific progress. Listed here are research publications by Miami Project scientists and colleagues.
Aarabi B, Neal CJ, Hersh DS, Harrop JS, Fehlings MG, Toups EG, Guest JD, Ugiliweneza B, Akhtar-Danesh N, Kurpad SN, Grossman RG. Mortality in ASIA Impairment Scale grade A to D Patients With Odontoid Fracture and Magnetic Resonance Imaging Evidence of Spinal Cord Injury. Neurotrauma reports. 2023;4(1):375-83.
Abrams SK, Rabinovitch BS, Zafar R, Aziz AS, Cherup NP, McMillan DW, Nielson JL, Lewis EC. Persons With Spinal Cord Injury Report Peripherally Dominant Serotonin-Like Syndrome After Use of Serotonergic Psychedelics. Neurotrauma reports. 2023 Aug 1;4(1):543-50.
Adebiyi E, Pareja JC, Alba-Sandoval M, Almodovar M. Impact of congenital heart disease on mortality and other associated outcomes in children hospitalised for acute asthma exacerbation. Cardiology in the Young. 2023:1-7.
Ambati VS, Macki M, Chan AK, Michalopoulos GD, Le VP, Jamieson AB, Chou D, Shaffrey CI, Gottfried ON, Bisson EF, Asher AL. Three-level ACDF versus 3-level laminectomy and fusion: are there differences in outcomes? An analysis of the Quality Outcomes Database cervical spondylotic myelopathy cohort. Neurosurgical focus. 2023;55(3):E2.
Ayling OG, Wang MY. The MIS PSO. Neurosurgery Clinics of North America. 2023;34(4):653-8.
Barrett JN, Barrett EF, Rajguru SM. Mitochondrial responses to intracellular Ca2+ release following infrared stimulation. Journal of neurophysiology. 2023;129(3):700-16.
Bechara A, Nawabi H, Moret F, Yaron A, Weaver E, Bozon M, Abouzid K, Guan JL, Tessier‐Lavigne M, Lemmon V, Castellani V. FAK–MAPK‐dependent adhesion disassembly downstream of L1 contributes to semaphorin3A‐induced collapse. The EMBO journal. 2008 Jun 4;27(11):1549-62.
Bisson EF, Mummaneni PV, Michalopoulos GD, El Sammak S, Chan AK, Agarwal N, Wang MY, Knightly JJ, Sherrod BA, Gottfried ON, Than KD. Sleep Disturbances in Cervical Spondylotic Myelopathy: Prevalence and Postoperative Outcomes—an Analysis From the Quality Outcomes Database. Clinical spine surgery. 2023;36(3):112-9.
Bloom O, Guest J. Update on current topics in spinal cord injury, trauma and rehabilitation. Current opinion in neurology. 2023;36(6):505-6.
hyperoxia-induced hippocampal brain injury in neonatal mice. Journal of Neuroinflammation. 2023;20(1):205.
Chan AK, Bydon M, Bisson EF, Glassman SD, Foley KT, Shaffrey CI, Potts EA, Shaffrey ME, Coric D, Knightly JJ, Park P. Minimally invasive versus open transforaminal lumbar interbody fusion for grade I lumbar spondylolisthesis: 5-year follow-up from the prospective multicenter Quality Outcomes Database registry. Neurosurgical focus. 2023;54(1):E2.
Chu KY, Khodamoradi K, BlachmanBraun R, Dullea A, Bidhan J, Campbell K, Zizzo J, Israeli J, Kim M, Petrella F, Ibrahim E. Effect of Radiofrequency Electromagnetic Radiation Emitted by Modern Cellphones on Sperm Motility and Viability: An In Vitro Study. European urology focus. 2023 Jan 1;9(1):69-74.
Anand N, Mummaneni PV, Uribe JS, Turner J, Than KD, Chou D, Nunley PD, Wang MY, Fessler RG, Le V, Robinson J. Spinal Deformity Complexity Checklist for Minimally Invasive Surgery: Expert Consensus from the Minimally Invasive International Spine Study Group. World Neurosurgery. 2023;173:e472-7.
Andreu M, Matti N, Bramlett HM, Shi Y, Gajavelli S, Dietrich WD. Dosedependent modulation of microglia activation in rats after penetrating traumatic brain injury (pTBI) by transplanted human neural stem cells. Plos one. 2023;18(5):e0285633.
Asher AL, Haid RW, Stroink AR, Michalopoulos GD, Alexander AY, Zeitouni D, Chan AK, Virk MS, Glassman SD, Foley KT, Slotkin JR. Research using the Quality Outcomes Database: accomplishments and future steps toward higher-quality real-world evidence. Journal of neurosurgery. 2023;139(6):1757-75.
Astorino TA, Robson T, McMillan DW. Classifying Intensity Domains From Arm Cycle Ergometry Differs Versus Leg Cycling Ergometry. The Journal of Strength & Conditioning Research. 2023 Nov 1;37(11):2192-9.
Ayling O, Rodgers RB, Levi AD. Spinal cerebrospinal fluid leaks. Journal of Neurosurgery: Spine. 2023;39(2):298-9.
Bergin SM, Michalopoulos GD, Shaffrey CI, Gottfried ON, Johnson E, Bisson EF, Wang MY, Knightly JJ, Virk MS, Tumialán LM, Turner JD. Characteristics of patients who return to work after undergoing surgery for cervical spondylotic myelopathy: a Quality Outcomes Database study. Journal of Neurosurgery: Spine. 2023;38(5):530-9.
Berry KM, Govindarajan V, Berger C, Maddy K, Roman RJ, Luther EM, Levi AD. Effects of Obesity on Cervical Disc Arthroplasty Complications. Neurospine. 2023;20(4):1399.
Bianchi A, De Castro Silva I, Deshpande NU, Singh S, Mehra S, Garrido VT, Guo X, Nivelo LA, Kolonias DS, Saigh SJ, Wieder E. Cell-autonomous Cxcl1 sustains tolerogenic circuitries and stromal inflammation via neutrophil-derived TNF in pancreatic cancer. Cancer discovery. 2023;13(6):1428-53.
Bigford GE, Betancourt LF, Charlifue S, Nash MS. Therapeutic Lifestyle Intervention Targeting Enhanced Cardiometabolic Health and Function for Persons with Chronic Spinal Cord Injury in Caregiver/Care-Receiver Co-Treatment: A Study Protocol of a Multisite Randomized Controlled Trial. International journal of environmental research and public health. 2023;20(19):6819.
Bigford GE, Szeto A, Darr AJ, Illiano P, Zambrano R, Mendez AJ, Nash MS. Characterization of Gastrointestinal Hormone Dysfunction and Metabolic Pathophysiology in Experimental Spinal Cord Injury. Journal of neurotrauma. 2023;40(9-10):981-98.
Boutzoukas AE, Olson R, Sellers MA, Fischer G, Hornik CD, Alibrahim O, Iheagwara K, Abulebda K, Bass AL, Irby K, Subbaswamy A. Mechanisms to expedite pediatric clinical trial site activation: The DOSE trial experience. Contemporary Clinical Trials. 2023;125:107067.
Bydon M, Sardar ZM, Michalopoulos GD, El Sammak S, Chan AK, Carreon LY, Norheim E, Park P, Ratliff JK, Tumialán L, Pugely AJ. Representativeness of the American Spine Registry: a comparison of patient characteristics with the National Inpatient Sample. Journal of Neurosurgery: Spine. 2023;1(aop):1-0.
Cabrera Ranaldi ED, Nuytemans K, Martinez A, Luca CC, Keane RW, de Rivero Vaccari JP. Proof-of-principle study of inflammasome signaling proteins as diagnostic biomarkers of the inflammatory response in Parkinson’s disease. Pharmaceuticals. 2023;16(6):883.
Cajigas I, Davis KC, Prins NW, Gallo S, Naeem JA, Fisher L, Ivan ME, Prasad A, Jagid JR. Brain-Computer interface control of stepping from invasive electrocorticography upper-limb motor imagery in a patient with quadriplegia. Frontiers in human neuroscience. 2023;16:1077416.
Campbell K, Arbelaez MC, Ghomeshi A, Ibrahim E, Roy S, Singh P, Khodamoradi K, Miller A, Lundy SD, Ramasamy R. Next-generation sequencing analysis of semen microbiome taxonomy in men with nonobstructive azoospermia vs. fertile controls: A pilot study. F&S Science. 2023 Aug 1;4(3):257-64.
Challa NV, Chen S, Yuan H, Duncan MR, Moreno WJ, Bramlett H, Dietrich WD, Benny M, Schmidt AF, Young K, Wu S. GSDMD gene knockout alleviates
Chan AK, Shaffrey CI, Park C, Gottfried ON, Than KD, Bisson EF, Bydon M, Asher AL, Coric D, Potts EA, Foley KT. Do comorbid self-reported depression and anxiety influence outcomes following surgery for cervical spondylotic myelopathy?. Journal of Neurosurgery: Spine. 2023;1(aop):1-7.
Chauhan D, Ahmad HS, Subtirelu R, Mannam S, Turlip R, Bryan K, Bathula S, Ghenbot Y, Yang AI, Wang MY, Basil G. Defining the minimal clinically important difference in smartphone-based mobility after spine surgery: correlation of survey questionnaire to mobility data: Presented at the 2023 AANS/CNS Joint Section on Disorders of the Spine and Peripheral Nerves. Journal of Neurosurgery: Spine. 2023;1(aop):1-1.
Chédotal H, Narayanan D, Povlsen K, Gotfredsen CH, Brambilla R, Gajhede M, Bach A, Clausen MH. Smallmolecule modulators of tumor necrosis factor signaling. Drug Discovery Today. 2023:103575.
Cherup NP, Robayo LE, Vastano R, Fleming L, Levin BE, WiderströmNoga E. Neuropsychological Function in Traumatic Brain Injury and the Influence of Chronic Pain. Perceptual and Motor Skills. 2023 May 23:00315125231174082.
Chow DS, Nguyen A, Park J, Wu L, Toups EG, Harrop JS, Guest J, Schmitt KM, Aarabi B, Fehlings MG, Boakye M. The RISCIS-PK substudy: An analysis of pharmacokinetics, pharmacodynamics, and impact on axonal degradation of riluzole in patients with traumatic cervical spinal cord injury enrolled in the RISCIS Phase III Randomized Controlled Trial. Journal of neurotrauma. 2023;40(17-18):18891906.
Cordeiro JG, de Monaco BA, Benveniste R, Alkhachroum A, Krueger EM, O’Phelan K, Jagid JR. Chronic subdural hematoma drainage using anti-thrombotic catheter technique. World neurosurgery. 2023;19:100215.
Costello MC, Errante EL, Maddy K, Tigre JY, Levi AD, Burks SS. Repair of complete median nerve transection from shoulder arthroscopy following rotator cuff injury. Interdisciplinary Neurosurgery. 2023;32:101743.
Costello MC, Errante EL, Smartz T, Ray WZ, Levi A, Burks SS. Clinical Applications of Electrical Stimulation for Peripheral Nerve Injury: A Systematic Review. Frontiers in Neuroscience. 2023;17:1162851.
Davies B, Brannigan J, Mowforth OD, Khan D, McNair AG, Tetreault L, Sadler I, Sarewitz E, Aarabi B, Kwon B, Gronlund T. Secondary analysis of a James Lind Alliance priority setting partnership to facilitate knowledge translation in degenerative cervical myelopathy (DCM): insights from AO Spine RECODEDCM. BMJ open. 2023;13(7):e064296.
Eeswara A, Pacheco-Spiewak A, Jergova S, Sagen J. Combined non-psychoactive Cannabis components cannabidiol and β-caryophyllene reduce chronic pain via CB1 interaction in a rat spinal cord injury model. PloS one. 2023;18(3):e0282920.
Fadli RA, Yamanouchi Y, Jovanovic LI, Popovic MR, Marquez-Chin C, Nomura T, Milosevic M. Effectiveness of motor and prefrontal cortical areas for braincontrolled functional electrical stimulation neuromodulation. Journal of Neural Engineering. 2023;20(5):056022.
Farkas GJ, Caldera LJ, Nash MS. Assessing the efficacy of duration and intensity prescription for physical activity in mitigating cardiometabolic risk after spinal cord injury. Current opinion in neurology. 2023;36(6):531-40.
Farkas GJ, Gater D, Sneij A, Felix ER, Nash MS. Honoring the Life and Legacy of David R. Gater, Jr, MD, PhD, MS: Pioneering Physician-Scientist, Visionary Leader, and Staunch Advocate. Archives of Physical Medicine and Rehabilitation. 2023;104(7):1158-60.
Fehlings MG, Moghaddamjou A, Harrop JS, Stanford R, Ball J, Aarabi B, Freeman BJ, Arnold PM, Guest JD, Kurpad SN, Schuster JM. Safety and Efficacy of Riluzole in Acute Spinal Cord Injury Study (RISCIS): a multi-center, randomized, placebo-controlled, doubleblinded trial. Journal of neurotrauma. 2023;40(17-18):1878-88.
Fehlings MG, Neal CJ, Hejrati N, Harrop JS, Toups EG, Guest JD. An Introduction to the North American Clinical Trials Network for Spinal Cord Injury Special Edition: Reflections on Accomplishments and a Look to the Future. Journal of neurotrauma. 2023;40(17-18):1811-6.
Franklin ME, Bennett C, Arboite M, Alvarez-Ciara A, Corrales N, Verdelus J, Dietrich WD, Keane RW, de Rivero Vaccari JP, Prasad A. Activation of inflammasomes and their effects on neuroinflammation at the microelectrodetissue interface in intracortical implants. Biomaterials. 2023;297:122102.
Futch BG, Kouam RW, Ugiliweneza B, Harrop J, Kurpad S, Foster N, Than K, Crutcher C, Goodwin CR, Tator C, Shaffrey CI. Demographics, Mechanism of Injury, and Outcomes for Acute Upper and Lower Cervical Spinal Cord Injuries: An Analysis of 470 Patients in the Prospective, Multi-Center, North American Clinical Trials Network Registry. Journal of neurotrauma. 2023;40(17-18):1918-27.
Gao H, Di J, Clausen BH, Wang N, Zhu X, Zhao T, Chang Y, Pang M, Yang Y, He R, Wang Y. Distinct myeloid population phenotypes dependent on TREM2 expression levels shape the pathology of traumatic versus demyelinating CNS disorders. Cell Reports. 2023;42(6).
Ge M, Molina J, Kim JJ, Mallela SK, Ahmad A, Santos JV, Al-Ali H, Mitrofanova A, Sharma K, Fontanesi F, Merscher S. Empagliflozin reduces podocyte lipotoxicity in experimental Alport syndrome. Elife. 2023 May 2;12:e83353.
Ghosh M, Pearse DD. Schwann CellDerived Exosomal Vesicles: A Promising Therapy for the Injured Spinal Cord. International Journal of Molecular Sciences. 2023;24(24):17317.
Govindarajan V, Shah AH, Morell AA, Borowy V, Ingle SM, Valdez MJ, Rivas S, Eichberg DG, Luther E, Lu V, Heiss J. Predicting Academic Career Placement via Development of Novel Intraresidency Metrics. World Neurosurgery. 2023;174:e35-43.
Guest JD, Kelly-Hedrick M, Williamson T, Park C, Ali DM, Sivaganesan A, Neal CJ, Tator CH, Fehlings MG. Development of a Systems Medicine Approach to Spinal Cord Injury. Journal of neurotrauma. 2023;40(17-18):1849-77.
Guest JD, Luo Z, Liu Y, Gao H, Wang D, Xu XM, Zhu H. Acute penetrating injury of the spinal cord by a wooden spike with delayed surgery: a case report. Neural regeneration research. 2023;18(12):2781-4.
Gurumani M, Mallela SK, Varona J, Merscher S, Fornoni A, Al-Ali H. A Robust Phenotypic Screening Assay Utilizing Human Podocytes to Identify Agents that Modulate Lipid Droplets. InLipidomics: Methods and Protocols 2023 Jan 19 (pp. 163-174). New York, NY: Springer US.
Hassanzadeh H, Baber J, Begier E, Noriega DC, Konishi H, Yato Y, Wang MY, Le Huec JC, Patel V, Varga P, Liljenqvist U. Efficacy of a 4-Antigen Staphylococcus aureus Vaccine in Spinal Surgery: The STaphylococcus aureus suRgical Inpatient Vaccine Efficacy (STRIVE) Randomized Clinical Trial. Clinical Infectious Diseases. 2023;77(2):312-20..
Hejrati N, Aarabi B, Neal CJ, Ugiliweneza B, Kurpad SN, Shaffrey CI, Guest JD, Toups EG, Harrop JS, Fehlings MG. Trends in the Use of Corticosteroids in the Management of Acute Spinal Cord Injury in North American Clinical Trials Network Sites. Journal of neurotrauma. 2023;40(17-18):1938-47.
Jamshidi AM, Soldozy S, Levi AD. Percutaneous Direct Pars Repair in Young Athletes. Neurosurgery. 2023;92(2):26370.
Javeed S, Greenberg JK, Zhang JK, Plog B, Dibble CF, Benedict B, Botterbush K,
Khalifeh JM, Wen H, Chen Y, Park Y. Association of upper-limb neurological recovery with functional outcomes in high cervical spinal cord injury. Journal of Neurosurgery: Spine. 2023;1(aop):1-8.
Jergova S, Dugan EA, Sagen J. Attenuation of SCI-Induced Hypersensitivity by Intensive Locomotor Training and Recombinant GABAergic Cells. Bioengineering. 2023;10(1):84.
Johnson NH, de Rivero Vaccari JP, Bramlett HM, Keane RW, Dietrich WD. Inflammasome activation in traumatic brain injury and Alzheimer’s disease. Translational Research. 2023;254:1-2.
Johnson NH, Kerr NA, de Rivero Vaccari JP, Bramlett HM, Keane RW, Dietrich WD. Genetic predisposition to Alzheimer’s disease alters inflammasome activity after traumatic brain injury. Translational Research. 2023;257:66-77.
Johnson NH, Kerr NA, Vaccari JP, Bramlett HM, Keane RW, Dietrich III WD. Inflammasome Activation after Traumatic Brain Injury as a Risk Factor for Alzheimer’s Disease. Alzheimer’s & dementia. 2023;19:e062441.
Kantar RS, Esenlik E, Al Abyad OS, Melhem A, Younan RA, Haddad M, Keith K, Kassam S, Annan B, Vijayakumar C, Picard A. The first hybrid international educational comprehensive cleft care workshop. The Cleft Palate Craniofacial Journal. 2023;60(10):1189-98.
Kattan D, Barsa C, Mekhijian S, Shakkour Z, Jammoul M, Doumit M, Zabala MC, Darwiche N, Eid AH, Mechref Y, Wang KK. Inflammasomes as biomarkers and therapeutic targets in traumatic brain injury and related-neurodegenerative diseases: A comprehensive overview. Neuroscience & Biobehavioral Reviews. 2023;144:104969.
Kelly-Hedrick M, Ugiliweneza B, Toups EG, Jimsheleishvili G, Kurpad SN, Aarabi B, Harrop JS, Foster N, Goodwin RC, Shaffrey CI, Fehlings MG. Interhospital Transfer delays care for spinal cord injury patients: A Report from the North American Clinical Trials Network for Spinal Cord Injury. Journal of neurotrauma. 2023;40(17-18):1928-37.
Kinnunen K, Robayo LE, Cherup NP, Frank SI, Widerström-Noga E. A preliminary study evaluating self-reported
effects of cannabis and cannabinoids on neuropathic pain and pain medication use in people with spinal cord injury. Frontiers in Pain Research. 2023;4:1297223.
Klein BR, Sowah MN, Levi AD. The role of limited access to students from more diverse nonfeeder medical schools in creating diversity inequities in neurosurgical residency. Neurosurgical Focus. 2023;55(5):E13.
Koester SW, Bishay AE, Lyons AT, Lu VM, Naik A, Graffeo CS, Levi AD, Komotar RJ. The Neurosurgery Match: COVID Comparison and Bibliometric Analysis. World Neurosurgery. 2023;178:e13-23.
Kressler J, Mendez A, Betancourt L, Nash M. Salsalate Improves Postprandial Glycemic and Some Lipid Responses in Persons With Tetraplegia: A Randomized Clinical Pilot Trial With Crossover Design. Topics in Spinal Cord Injury Rehabilitation. 2023;29(3):1-3.
Krueger EM, Benveniste RJ, Lu VM, Taylor RR, Kumar R, Cordeiro JG, Jagid JR. Simple wound closure compared with surgery for civilian cranial gunshot wounds. Journal of neurosurgery. 2022 Jun 24;138(2):437-45.
Krueger EM, Benveniste RJ, Taylor RR, Shah S, Moll J, Figueroa JM, Jagid JR. Neurologic Outcomes for Octogenarians Undergoing Emergent Surgery for Traumatic Acute Subdural Hematoma. World Neurosurgery. 2023;171:e404-11.
Kuhn JE, Zabala MC, Chavez MM, Almodóvar M, Mulinari LA, Sainathan S, de Rivero Vaccari JP, Wang KK, Pareja JC. Utility of Brain Injury Biomarkers in Children With Congenital Heart Disease Undergoing Cardiac Surgery. Pediatric neurology. 2023;148:44-53.
Lagu T, Schroth SL, Haywood C, Heinemann A, Kessler A, Morse L, Khan SS, Kershaw KN, Nash MS. Diagnosis and Management of Cardiovascular Risk in Individuals With Spinal Cord Injury: A Narrative Review. Circulation. 2023;148(3):268-77.
Lasham DJ, Arta RK, Hadi AF, Egawa J, Lemmon VP, Takasugi T, Igarashi M, Someya T. Effects of MAP4K inhibition on neurite outgrowth. Molecular brain. 2023;16(1):79.
Levi DJ, Brusko GD, Levi AD, Wang MY. Does hinge sidedness influence laterality of C5 palsy after expansile opendoor cervical laminoplasty?. Neurosurgical Focus. 2023;55(3):E6.
Lu VM, Brusko GD, Levi DJ, Borowsky P, Wang MY. Associations with daily opioid use during hospitalization following lumbar fusion: A contemporary cohort study. Clinical Neurology and Neurosurgery. 2023;224:107555.
Lu VM, Cordeiro JG, Urakov T, Benveniste RJ, Levi AD, Komotar RJ. Integration of Veterans Affairs Medical Centers Into Neurosurgical Residency Programs. Neurosurgery. 2023;92(6):e1356.
Lu VM, Levi AD, Basil GW. Endoscopicassisted fusion for lumbar pars fracture repair in an adolescent patient. Clinical neurology and neurosurgery. 2023;233:107920.
Lund MC, Clausen BH, Brambilla R, Lambertsen KL. The role of tumor necrosis factor following spinal cord injury: A systematic review. Cellular and molecular neurobiology. 2023;43(3):92550.
Lund MC, Ellman DG, Nielsen PV, Raffaele S, Fumagalli M, Guzman R, Degn M, Brambilla R, Meyer M, Clausen BH, Lambertsen KL. Selective Inhibition of Soluble Tumor Necrosis Factor Alters the Neuroinflammatory Response following Moderate Spinal Cord Injury in Mice. Biology. 2023;12(6):845.
Maddy KS, Tigre JY, Lu VM, Costello MC, Errante EL, Levi AD, Burks SS. Influence of instrumentation type on outcomes after surgical management of spondylodiscitis: a systematic review and meta-analysis. European Spine Journal. 2023:1-6.
Mansoor Ali D, Sivaganesan A, Neal CJ, Thalheimer S, Ugiliweneza B, Toups EG, Abd-El-Barr M, Jimsheleishvili G, Kurpad SN, Aarabi B, Shaffrey CI. Bulbocavernosus Reflex Has No Prognostic Features During the Acute Evaluation of Spinal Cord Injuries. Journal of neurotrauma. 2023;40(17-18):1970-5.
Masterson TA, Atuluru P, Zucker I, Molina M, Ibrahim E, Nackeeran S, Kava B, Ramasamy R. Collagenase Clostridium histolyticum treatment improves degree
of curvature in Peyronie’s disease with calcified plaques. European urology focus. 2023 Jan 1;9(1):55-9.
Masterson TA, Molina M, Ledesma B, Zucker I, Saltzman R, Ibrahim E, Han S, Reis IM, Ramasamy R. Platelet-rich Plasma for the Treatment of Erectile Dysfunction: A Prospective, Randomized, Double-blind, Placebo-controlled Clinical Trial. The Journal of Urology. 2023 Apr 30:10-97.
McMillan DW, Bigford GE, Farkas GJ. The Physiology of Neurogenic Obesity: Lessons from Spinal Cord Injury Research. Obesity Facts. 2023 May 22.
Millet B, Snapp HA, Rajguru SM, Schaefer Solle N. Prevalence of Hearing Loss and Perceptions of Hearing Health and Protection among Florida Firefighters. International journal of environmental research and public health. 2023;20(5):3826.
Mowforth OD, Burn L, Khan DZ, Yang X, Stacpoole SR, Gronlund T, Tetreault L, Kalsi-Ryan S, Starkey ML, Sadler I, Sarewitz E. Lived experience-centred word clouds may improve research uncertainty gathering in priority setting partnerships. BMC medical research methodology. 2023;23(1):100.
Mylavarapu RV, Kanumuri VV, de Rivero Vaccari JP, Misra A, McMillan DW, Ganzer PD. Importance of timing optimization for closed-loop applications of vagus nerve stimulation. Bioelectronic medicine. 2023;9(1):1-8.
Nash MS, Boddu JV, Green BA. Methylprednisolone following acute traumatic spinal cord injury. Journal of Neurosurgery: Spine. 2023;39(6):851-2.
Neal CJ, Ugiliweneza B, Toups EG, AbdEl-Barr M, Jimsheleishvili G, Kurpad SN, Aarabi B, Harrop JS, Shaffrey CI, Fehlings MG, Tator CH. Variability in early surgery for acute cervical spinal cord injury patients: an opportunity for enhanced care delivery. Journal of neurotrauma. 2023;40(17-18):1907-17.
Neuman BJ, Wang KY, Harris AB, Raad M, Hostin RA, Protopsaltis TS, Ames CP, Passias PG, Gupta MC, Klineberg EO, Hart R. Return to work after adult spinal deformity surgery. Spine deformity. 2023;11(1):197-204.
Palermo AE, Cahalin LP, Nash MS. A Secondary Analysis of Short-and Long-Term Variability of Inspiratory Muscle Performance in People Living With SCI. Topics in Spinal Cord Injury Rehabilitation. 2023;29(2):97-106.
Park C, Mummaneni PV, Gottfried ON, Shaffrey CI, Tang AJ, Bisson EF, Asher AL, Coric D, Potts EA, Foley KT, Wang MY. Which supervised machine learning algorithm can best predict achievement of minimum clinically important difference in neck pain after surgery in patients with cervical myelopathy? A QOD study. Neurosurgical focus. 2023;54(6):E5.
Passias PG, Tretiakov PS, Nunley PD, Wang MY, Park P, Kanter AS, Okonkwo DO, Eastlack RK, Mundis GM, Chou D, Agarwal N. Incremental benefits of circumferential minimally invasive surgery for increasingly frail patients with adult spinal deformity. Journal of Neurosurgery: Spine. 2023;1(aop):1-7.
Patel A, Kondapavulur S, Umbach G, Chan AK, Le VP, Bisson EF, Bydon M, Chou D, Glassman SD, Foley KT, Shaffrey CI. Greater improvement in Neck Disability Index scores in women after surgery for cervical myelopathy: an analysis of the Quality Outcomes Database. Neurosurgical focus. 2023;55(5):E7.
Perez-Roman RJ, Boddu JV, Bashti M, Bryant JP, Amadasu E, Gyedu JS, Wang MY. The Use of Carbon Fiber-Reinforced Instrumentation in patients with Spinal Oncologic Tumors: A Systematic Review of Literature and Future Directions. World Neurosurgery. 2023;173:13-22.
Piedade GS, de Monaco BA, Guest JD, Cordeiro JG. Review of spinal cord stimulation for disorders of consciousness. Current opinion in neurology. 2023;36(6):507-15.
Pradhyumnan H, Reddy V, Bassett ZQ, Patel SH, Zhao W, Dave KR, PerezPinzon MA, Bramlett HM, Raval AP. Post-stroke periodic estrogen receptorbeta agonist improves cognition in aged female rats. Neurochemistry international. 2023;165:105521.
Raciti FM, Morales Y, Snapp HA, Rajguru SM. A reliable and reproducible protocol for sound-evoked vestibular
myogenic potentials in rattus norvegicus. Frontiers in integrative neuroscience. 2023;17.
Radabaugh HL, Ferguson AR, Bramlett HM, Dietrich WD. Increasing rigor of preclinical research to maximize opportunities for translation. Neurotherapeutics. 2023;20(6):1433-45.
Rajjoub R, Ghaith AK, El-Hajj VG, RiosZermano J, De Biase G, Atallah E, Tfaily A, Saad H, Akinduro OO, Elmi-Terander A, Abode-Iyamah K. Comparative outcomes of awake spine surgery under spinal versus general anesthesia: a comprehensive systematic review and meta-analysis. European Spine Journal. 2023;33:985–1000.
Robayo LE, Govind V, Salan T, Cherup NP, Sheriff S, Maudsley AA, Widerström-Noga E. Neurometabolite alterations in traumatic brain injury and associations with chronic pain. Frontiers in neuroscience. 2023;17:1125128.
Rujeedawa T, Mowforth OD, Davies BM, Yang C, Nouri A, Francis JJ, Aarabi B, Kwon BK, Harrop J, Wilson JR, Martin AR. Degenerative Thoracic Myelopathy: A Scoping Review of Epidemiology, Genetics, and Pathogenesis. Global spine journal. 2023:21925682231224768.
Saltzman RG, Molina ML, Ledesma BR, Ibrahim E, Masterson TA, Ramasamy R. Rationale and design for the COCKTAIL trial: a single-center, randomized, doubleblind, sham-controlled study combining shockwave therapy and platelet-rich plasma for erectile dysfunction. European urology focus. 2023 Jan;9(1):8.
Sanchez-Molano J, Blaya MO, Padgett KR, Moreno WJ, Zhao W, Dietrich WD, Bramlett HM. Multimodal magnetic resonance imaging after experimental moderate and severe traumatic brain injury: A longitudinal correlative assessment of structural and cerebral blood flow changes. PloS one. 2023 Aug 7;18(8):e0289786.
Sangaletti R, Tamames I, Yahn SL, Choi JS, Lee JK, King C, Rajguru SM. Mild therapeutic hypothermia protects against inflammatory and proapoptotic processes in the rat model of cochlear implant trauma. Hearing research. 2023;428:108680.
Sasaki A, Cao N, Yuasa A, Popovic MR, Nakazawa K, Milosevic M. Effects of trunk neuromuscular electrical stimulation on the motor circuits of able-bodied individuals. Experimental Brain Research. 2023;241(4):979-90.
Sasaki A, Kato T, Kaneko N, Masugi Y, Milosevic M, Nakazawa K. Distinct contribution of interneuronal circuits in the human motor cortex during interlimb interactions: A transcranial magnetic stimulation study. Brain Stimulation: Basic, Translational, and Clinical Research in Neuromodulation. 2023;16(1):246-7.
Schoen N, Matichak D, Armstrong V, Sedighim S, Lew E, Jagid J, Bullock MR, Richardson A. The Cost of Gunshot Wounds to the Head: An Unevenly Distributed Burden. World neurosurgery. 2023;172:e201-11.
Shahrestani S, Chan AK, Bisson EF, Bydon M, Glassman SD, Foley KT, Shaffrey CI, Potts EA, Shaffrey ME, Coric D, Knightly JJ. Developing nonlinear k-nearest neighbors classification algorithms to identify patients at high risk of increased length of hospital stay following spine surgery. Neurosurgical focus. 2023;54(6):E7.
Shakil H, Santaguida C, Wilson JR, Farhadi HF, Levi AD, Wilcox JT. Pathophysiology and surgical decisionmaking in central cord syndrome and degenerative cervical myelopathy: correcting the somatotopic fallacy. Frontiers in Neurology. 2023;14:1276399.
Shpiner DS, Peabody TK, Luca CC, Jagid J, Moore H. Deep Brain Stimulation for an Unusual Presentation of Myoclonus Dystonia Associated with RussellSilver Syndrome. Tremor and Other Hyperkinetic Movements. 2023;13.
Snapp HA, Coto J, Solle NS, Khan U, Millet B, Rajguru SM. Risk-taking propensity as a risk factor for noiseinduced hearing loss in the general population. International journal of audiology. 2023;62(12):1166-75.
Snapp HA, Millet B, Schaefer-Solle N, Rajguru SM, Ausili SA. The effects of hearing protection devices on spatial awareness in complex listening environments. PloS one. 2023;18(1):e0280240.
Snapp HA, Vanlooy L, Kuzbyt B, Kolberg C, Laffitte-Lopez D, Rajguru S. Peripheral vestibular loss in noise-exposed firefighters. Frontiers in integrative neuroscience. 2023;17.
Soldozy S, Warner T, Tigre JA, Marquez B, Burks SS, Levi AD. Surgical Management of Lumbosacral Plexus Tumors. World neurosurgery. 2023;173:e452-61.
Sowah MN, Fuller AT, Chen SH, Green BA, Ivan ME, Ford HR, Zipfel GJ, Pennicooke B, Theodore N, Levi AD. Promoting diversity in neurosurgery: a multi-institutional scholarship-based approach. Journal of Neurosurgery. 2023;138(6):1773-80.
Spurlock M, An W, Reshetnikova G, Wen R, Wang H, Braha M, Solis G, Kurtenbach S, Galindez OJ, de Rivero Vaccari JP, Chou TH. The InflammasomeDependent Dysfunction and Death of Retinal Ganglion Cells after Repetitive Intraocular Pressure Spikes. Cells. 2023;12(22):2626.
Tejeda G, Ciciriello AJ, Dumont CM. Biomaterial strategies to bolster neural stem cell-mediated repair of the central nervous system. Cells Tissues Organs. 2023;211(6):655-69.
Thougaard E, Carney B, Wlodarczyk A, Brambilla R, Lambertsen KL. Peripherally-derived myeloid cells induce disease-dependent phenotypic changes in microglia. Frontiers in cellular neuroscience. 2023;17:1295840.
Thougaard E, Nielsen PV, Forsberg A, Phuong V, Velasco AM, Wlodarczyk A, Wajant H, Lang I, Mikkelsen JD, Clausen BH, Brambilla R. Systemic treatment with a selective TNFR2 agonist alters the central and peripheral immune responses and transiently improves functional outcome after experimental ischemic stroke. Journal of neuroimmunology. 2023;385:578246.
Tigre JY, Kloehn AJ, Scemama A, Boddu J, Costello MC, Levi AD, Burks SS. Resection of a lumbar intradural tumor. Surgical Neurology International. 2023;14:377.
Tigre JY, Puerto A, Russo JP, Kloehn AJ, Abdullah N, Burks SS, Levi AD. Intraoperative embolectomy of a left illiac
artery thrombus during an anterior lumbar interbody fusion. Surgical neurology international. 2023;14:374.
Toups EG, Ugiliweneza B, Howley SP, Neal CJ, Harrop JS, Guest JD, Grossman RG, Fehlings MG. North American clinical trials network for spinal cord injury registry: methodology and analysis. Journal of neurotrauma. 2023;40(1718):1817-22.
Vastano R, Widerstrom-Noga E. Eventrelated potentials during mental rotation of body-related stimuli in spinal cord injury population. Neuropsychologia. 2023 Jan 28;179:108447.
Vontell RT, de Rivero Vaccari JP, Sun X, Gultekin SH, Bramlett HM, Dietrich WD, Keane RW. Identification of inflammasome signaling proteins in neurons and microglia in early and intermediate stages of Alzheimer’s disease. Brain Pathology. 2023;33(4):e13142.
Widerström-Noga E, Anderson KD, Robayo LE, Perez S, Cherup NP, Fernandez GE. Development of a pain education resource for people with spinal cord injury. Frontiers in public health. 2023;11:1197944.
Widerström-Noga E, Biering-Sørensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, Richards JS, Rosner J, Taylor J. The international spinal cord injury pain basic data set (version 3.0). Spinal cord. 2023;61(10):536-40.
Widerström-Noga E. Neuropathic Pain and Spinal Cord Injury: Management, Phenotypes, and Biomarkers. Drugs. 2023 Jun 16:1-25.
Williams EC, Ma Y, Loo DM, Schaefer Solle N, Millet B, Harris K, Snapp HA, Rajguru SM. Monitoring Occupational Noise Exposure in Firefighters Using the Apple Watch. International journal of environmental research and public health. 2023;20(3):2315.
Yamaguchi A, Sasaki A, Popovic MR, Milosevic M, Nakazawa K. Low-level voluntary input enhances corticospinal excitability during ankle dorsiflexion neuromuscular electrical stimulation in healthy young adults. Plos one. 2023;18(3):e0282671.
Yang E, Mummaneni PV, Chou D, Bydon M, Bisson EF, Shaffrey CI, Gottfried ON, Asher AL, Coric D, Potts EA, Foley KT. Cervical laminoplasty versus laminectomy and posterior cervical fusion for cervical myelopathy: propensity-matched analysis of 24-month outcomes from the Quality Outcomes Database: Presented at the 2023 AANS/CNS Joint Section on Disorders of the Spine and Peripheral Nerves. Journal of Neurosurgery: Spine. 2023;39(5):671-81.
Yang Z, Apiliogullari S, Fu Y, Istanbouli A, Kaur S, Jabbal IS, Moghieb A, Irfan Z, Patterson RL, Kurup M, Morrow L. Association between Cerebrospinal Fluid and Serum Biomarker Levels and Diagnosis, Injury Severity, and Short-Term Outcomes in Patients with Acute Traumatic Spinal Cord Injury. Diagnostics. 2023;13(10):1814.
Yousuf MS, Sahn JJ, Yang H, David ET, Shiers S, Mancilla Moreno M, Iketem J, Royer DM, Garcia CD, Zhang J, Hong VM. Highly specific σ2R/TMEM97 ligand FEM-1689 alleviates neuropathic pain and inhibits the integrated stress response. Proceedings of the National Academy of Sciences. 2023 Dec 26;120(52):e2306090120.
Yunga Tigre J, Levy A, Wu EM, Boddu J, Kumar V, Levi AD, Burks SS. Surgical resection of an intradural extramedullary spinal tumor. Neurosurgical Focus: Video. 2023;9(2):V9.
Zaki MM, Joshi RS, Ibrahim S, Michalopoulos GD, Linzey JR, Saadeh YS, Upadhyaya C, Coric D, Potts EA, Bisson EF, Turner JD. How closely are outcome questionnaires correlated to patient satisfaction after cervical spine surgery for myelopathy?. Journal of Neurosurgery: Spine. 2023;1(aop):1-9.
Zhang E, Abdel-Mottaleb M, Liang P, Navarrete B, Yildirim YA, Campos MA, Smith IT, Wang P, Yildirim B, Yang L, Chen S. Magnetic-field-synchronized wireless modulation of neural activity by magnetoelectric nanoparticles. Brain stimulation. 2022;15(6):1451-62.

The Miami Project to Cure Paralysis was established in 1985 to develop new therapies to improve function in paralyzed individuals. We are very enthusiastic about our current accomplishments and multi-disciplinary research programs. In addition, we are most eager about the future as we continue to move new treatments forward to treat paralysis.