





Robert Freedman Endowed Chair and Professor
C. Neill Epperson, MD, is the Robert Freedman Endowed Professor and Chair of the Department of Psychiatry in the School of Medicine at the University of Colorado Anschutz Medical Campus where she is also the Executive Director of the Helen and Arthur E. Johnson Depression Center and Colorado Women’s Behavioral Health and Wellness. Dr. Epperson is internationally known for her unique lifespan approach to reproductive psychiatry and mental illness in women with respect to clinical, training, research, and advocacy mission areas. Her work has been funded by the National Cancer Institute, National Institute on Aging, National Institute of Mental Health, the Office of Research on Women's Health, and/or the National Institute on Drug Abuse for 3 decades.
Her body of work has led to a greater appreciation of the impact of childhood adversity on physiologic responses during times of hormonal fluctuation as well as gonadal steroid effects on brain and behavior.

Dr. Epperson has mentored more than 57 students, residents, and fellows and is an independent investigator with more than 400 peer-reviewed publications and presentations. Before being recruited to CU Anschutz, Dr. Epperson served as the founder and director of both the Penn Center for Women's Behavioral Wellness and Penn PROMOTES, Research on Sex and Gender in Health at the Perelman School of Medicine at the University of Pennsylvania where she was a tenured Professor of Psychiatry and Obstetrics and Gynecology until 2018. Dr. Epperson received her medical degree at The University of North Carolina at Chapel Hill and completed her residency and research training in psychiatry at Yale University School of Medicine, where she remained on faculty until 2009. Dr. Epperson’s career mission has been to promote the centrality of the brain with respect to all areas of health Dr. Epperson is honored to lead the Department of Psychiatry at the University of Colorado Anschutz Medical Campus where she and the entire Department emphasize the importance of brain health to all health through clinical care, research, training, and collaboration.

With 437 paid faculty and 800 total employees, the CU Department of Psychiatry is one of the largest academic departments of psychiatry in the nation. Faculty and staff work at the CU Anschutz Medical Campus and its hospitals, the Department of Corrections, Colorado State Hospitals in Pueblo and Fort Logan, residential programs in Fort Collins, the Metropolitan State University Auraria Campus, and four outpatient medication assisted treatment programs across the Denver Metro region. Additional affiliate faculty work at Denver Health and Hospital Authority and the VA Medical Center. The Department also boasts 150 volunteer faculty who participate in the training of its psychiatry residents and fellows and more than 200 trainees in multiple-disciplines. The Department is comprised of five specialty area divisions with more than 70 clinical, research, and training programs and 2 CU-designated Centers
The CU Department of Psychiatry sets the standard for education and training of leaders in psychiatry and mental health care, conducts ground-breaking research that aims to eradicate suffering due to psychiatric and substance use disorders, provides ready access to state of-the-art mental health preventions and interventions across the continuum of care, and collaborates with the community and other key stakeholders to promote well-being among all Coloradans. We accomplish this vision in a manner that respects, values and advocates for the dignity and worth of each individual and family. The department is dedicated to serving a community in which we value all people and have a continued commitment to diversity and inclusion in our clinical, research, treatment and educational activities. We strive to always uphold our anchoring belief - brain health for all, for life.

Brain & Behavior
Innovation Center (BBICen)
Brain
Imaging Center (BIC)
Division of Adult Psychiatry
Helen and Arthur E. Johnson
Depression Center (JDC)
Division of Child & Adolescent Mental Health
Division of Interdisciplinary Neuroscience
Division of Addiction Sciences, Prevention, & Treatment
Office of Psychological
Science and Practice (OPSP)
Division of Community, Population, and Public Mental Health
Office of the CO Mental Health
Access Programs (CO-MAP)

Since FY19, the Department of Psychiatry has aimed to quantify the number of “Lives Touched” by departmental services, including direct clinical care, doc-todoc consultations, trainings, and other educational offerings. Lives touched are reported by mission area. A “life touched” is defined as anyone who has received a service or gained in some way by interacting with the department. Number of lives touched has grown year over year since the inception of this project, increasing from 17,534 in FY19 to 90,731 in FY25.
“Reach,” is also tracked and refers to anyone who has accessed materials via the website, social media, research studies, scholarly papers and other offerings.
Our reach for FY24 was over 1.1 million lives touched.

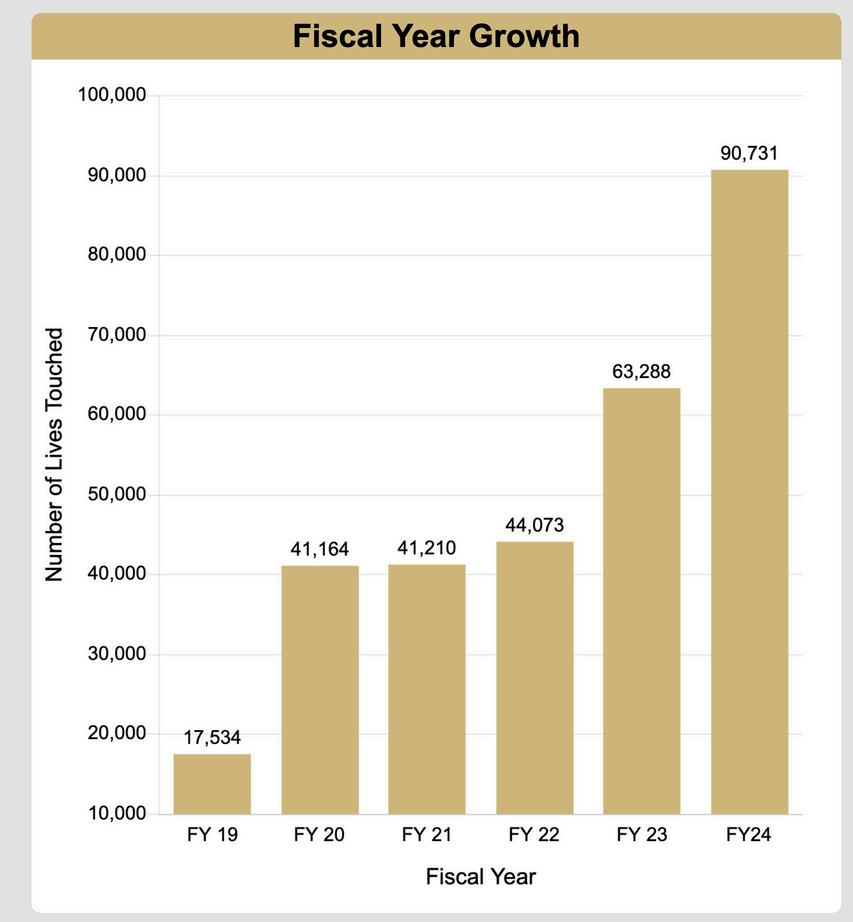
Please note the sharp increase in FY24 is mainly related to an increase in our clinical care services and community & advocacy programs.


Neill Epperson, MD
Robert Freedman Endowed
Chair and Professor

Melissa Sinclair, CPC, MA
Director and Vice Chair of Finance and Administration


Amanda J. Law, PhD
Vice Chair of Research

Robert D. Davies, MD
Vice Chair of Education

Rachel A. Davis, MD
Vice Chair of Clinical Affairs and Strategy

Sarah Nagle-Yang, MD
Vice Chair of Quality
Bruno Anthony, PhD
Vice Chair of Psychology in Psychiatry


K. Ron-Li Liaw, MD
Vice Chair of Diversity, Equity & Inclusion


The CU Department of Psychiatry sets the standard for education and training of leaders in psychiatry and mental health care by conducting groundbreaking research that aims to eradicate suffering due to psychiatric and substance use disorders. The DOPsych provides ready-access to state of-the-art mental health preventions and interventions across the continuum of care, and collaborate with the community and other key stakeholders to promote well-being among all Coloradans.
To best serve this mission in meaningful and specialized ways, the department is comprised of five divisions. All divisions have dual- pair faculty and staff leadership to ensure the progression and growth of all team members Additionally, all divisions have the support of departmental programs and administrative cores which were established to advance the academic success of faculty members in the Department of Psychiatry by providing research-related administrative, operational, and educational support. Structure, divisions, and leadership are pictured on the right.
Dr. Neill Epperson
Department of Psychiatry Chair
Adult Psychiatry
Director: Dr. Christopher Schneck
Administrator: Anthony Pfaff
Child & Adolescent Mental Health
Director: Dr. Ron-Li Liaw
Administrator: Stacey L'hommedieu
Interdisciplinary Neuroscience
Director: Dr. Amanda Law
Administrator: Stephanie Vetter
Addiction Sciences, Prevention, & Treatment
Directors: Drs. Tyler Coyle & Joseph Schacht
Administrator: Elisa Upwood
Community, Population, and Public Mental Health
Director: Dr. Scott Simpson
Administrator: Viki Manley
Outpatient Clinics
Encompass
Executive Functioning
Faculty/Staff Mental Health
Immigrant and Refugee
Johnson Depression Center
Interventional Psychiatry
OCD Clinic
Outpatient Psychiatry Clinic
PEACS- Early Psychosis
Student/Resident
START Clinic
Women’s Behavioral Health
Intensive Outpatient
UCH Affiliated Services
Hospital: CL, CDU2,
Inpatient, ECT
Outpatient Integrated Care
services: Transplant, Burn unit, Neurology, NICU, HIV Clinic, NES Clinic, Family Medicine, Internal Medicine, PROMISE
Research
Stress, Hormone, and Health Research Group
Epperson (Lead)
Novick
Phimphasone-Brady
Olsavski
Demers
Metcalf
Vargas
Research: embedded in multiple clinics
Education: Residents, Fellows, other trainees (Psychology, social work, medical students, NP students)
Child & Adolescent
Mental Health
Inpatient services
CHCO Partial Hospitalization
CHCO Eating Disorders Unit
CHCO Neuropsychiatric Special Care Services
CHCO Medical Day
Treatment Program
CHCO Outpatient services at 3 sites
CHCO ED Coverage
CHCO CL Services
Integrated services within but not limited to,
Pediatric Primary Care, Transplant, CF clinic, Sie Center for Down
Syndrome, GI, Neurology, Special Care
Healthy Expectations Program
Harris Infant Mental Health
JFK Program, including school based services
CO Springs Outpatient, Partial Hospitalization, ED and Integrated Services
Traverse Academy (School-based integrated IOP Program)
Crisis Services
Partners in Children’s Mental Health
Outpatient Specialty Programming (Mood, Early Childhood)
Multiple Research Labs and Programming
Neuroscience
Research: Neurodevelopmental and Neuropsychiatric Genetics Program: Law Lab Laboratories of Translational Psychiatry: Bale Lab Thompson Lab
Developmental
Research: Hunter/Freedman/ Hoffman Lab
Colorado Neuroscience of Behavioral Health and Wellness Research Group: Tregellas Lab Legget Lab Behavioral Immunology and Endocrinology
Bradley Lab
Training: Developmental Psychobiology Research Group (DPRG): T32 Program
Service Center
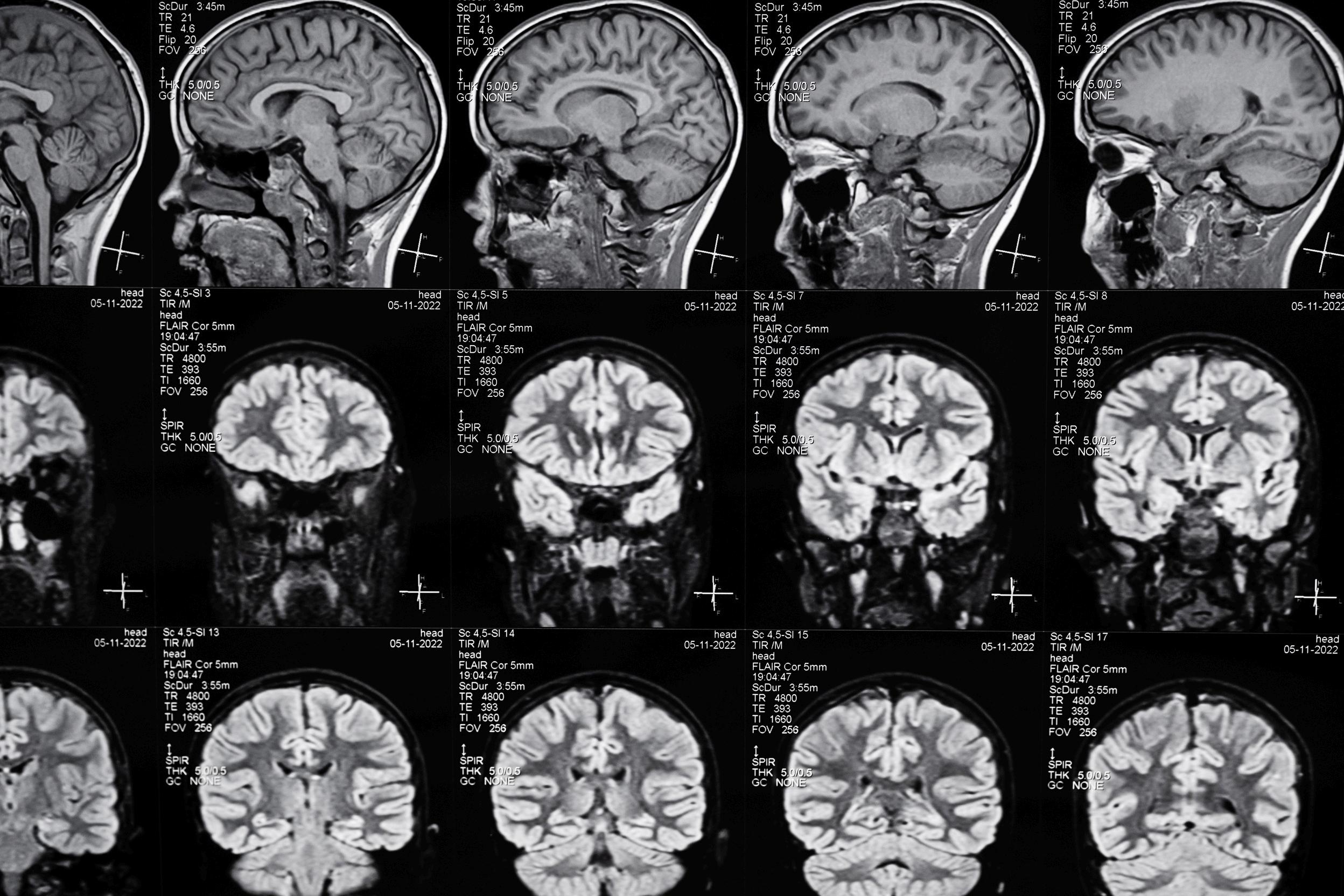
Brain Imaging Center –Research dedicated facility: Siemens 3T wide bore scanner
GE SIGNA Premier 3T wide bore scanner (coming soon)
Research Programs:
Rocky Mountain
Cannabis Research Center (NIDA P50)
Cannabis, Health, and
Addiction Over the Lifespan Lab (Hutchison)
Colorado
Neuromodulation Lab (Sakai)
Translational
Addiction Imaging Lab (Schacht)
Addiction Biology Lab (Schacht)
Addiction Education Lab (Coyle)
Ellingson Lab
Hopfer Lab
Riggs Lab
Clinical Programs –
Addiction Research & Treatment Services
Adult Outpatient + Mobile Unit
Reflections for Women (Women’s Residential)
Inspiration for Men (Men’s Residential)
Synergy (Adolescent Outpatient)
Encompass (Integrated Mental Health + Substance
Use Treatment for Adolescents & Young Adults)
Community, Population, & Public Mental Health
Behavioral Health and Wellness Program
Colorado Mental Health Hospitals at Pueblo and Fort Logan
Colorado
Department of Corrections
Mental Health
Transitional Living Program
Forensic Services
Forensic Psychiatry Fellowship
Health Center at Auraria Student
Mental Health Learning Management System
Medical-Legal Consultation Program
Native Health Programs
Public health training, consultation, and evaluation

Christopher Schneck, MD
Adult Psychiatry

Tyler Coyle, MD
Addiction Sciences, Prevention, & Treatment

K. Ron-Li Liaw, MD
Child & Adolescent Mental Health

Joseph Schact, PhD
Addiction Sciences, Prevention, & Treatment


Amanda J. Law, PhD Interdisciplinary Neuroscience
Scott Simpson, MD
Community, Population, and Public Mental Health


The Adult Division comprises 145 faculty from a diverse array of disciplines and backgrounds: 34% physicians, 29% psychologists, 17% social workers, 10% APPs, and the remainder licensed professional counselors and other therapists. The clinics, programs, and services span the UCH and CU Medicine systems, with affiliations to Denver Health and the VA system. The division operates 15 outpatient clinics that provide care for a variety of specific patient populations, along with an array of integrated behavioral health services embedded in medical clinics across the campus
Throughout the system, trainees of all disciplines, including psychiatry residents, fellows, medical students, nursing students, social work students, psychology interns, externs, post-docs, and addiction trainees, are integrated. Research is also integrated into a number of clinical services, with the aim of producing new knowledge to benefit patients and their families.
The Adult Division has undergone dramatic growth and expansion of services in the last six years, growing from 63 faculty in 2018 to 145 faculty in 2024 (a 130% increase). The faculty span a broad array of disciplines, including psychiatrists, psychologists, nurse practitioners, physician assistants, social workers, licensed professional counselors, and marital and family therapists.
The clinical services have expanded in both general and specialty psychiatric and integrated care settings. Specialty focus areas include mood disorders, OCD, refugee mental health, neuromodulation/interventional psychiatry, trauma and disaster-related care, women's behavioral health and wellness/reproductive psychiatry, executive functioning, and early psychosis. Psychologists or licensed prepared therapists are integrated into family medicine, internal medicine, OB, neurology, PM&R, bariatrics, transplant, and burn. The Division houses clinical services for the Anschutz campus, including faculty/staff (and their families) mental health, student/resident mental health, and additional UCH services (consult-liaison psychiatry, inpatient psychiatry, emergency psychiatry, addiction psychiatry).
Services have been provided to Coloradans in 466 out of 513 (90%) Colorado ZIP codes in the last 5 years and clinical care has been provided to people from all 50 states. The Division is also strategically partnering with CU Innovations to seed innovations in mental health care.
Each year, 55 psychiatry residents (PGY1-4) are trained, along with a number of forensic, child, consult liaison, and addiction fellows, as well as a host of social work interns/externs, NP students, and psychology trainees. BY THE NUMBERS
$25 Million In annual patient services revenue
300,000+ Completed patient visits since 2018
$6.3 Million Received across 22 active grants
The vision for CAMH is to advance a youth and family-centered, coordinated system of mental health care with collaborative partners, ensuring equitable access to high-quality, evidencebased care and prevention. CAMH is dedicated to making a positive impact in the lives of children and adolescents across the state of Colorado through cutting-edge research, evidencebased clinical care, strategic community partnerships, and a robust education program to train the next generation of mental health clinicians and researchers.
175
Total faculty & staff members
46,859 Annual screenings for suicide risk BY THE NUMBERS
$60+ Million philanthropic dollars raised


Traverse Academy opened its doors in 2023 in collaboration with the C&A Division and Cherry Creek School District to establish a first of its kind IOP imbedded program within a brick-and-mortar school-based setting.
Crisis program services opened doors in 2024 to provide patients and families with timely, effective care during a mental health crisis. This is a new level of care for patients not yet safe to go home and would benefit from a family-centered, acute crisis intervention.
Through philanthropic support, PMHI is in process of developing a learning health system aimed to:
Integrate rapid, pragmatic research into clinical programs to identify best practices, Engage and support the spectrum of care team members, patients, family and community members as collaborators in research and part of routine clinical care
Collect and use inclusive data and quality metrics to guide and iteratively improve equitable reach, implementation, impact and sustainment of care delivery and patient outcomes.

The Division of Interdisciplinary Neuroscience is a team of researchers who focus on interdisciplinary approaches to understanding brain development and function in health and disease with a focus on neurobiological mechanisms. Research in the division spans basic and clinical neuroscience and studies across the lifespan in the context of mental health and mental health disorders. The faculty support and train undergraduate, graduate, post-graduate, and resident trainees across several graduate school programs and departments in the School of Medicine. The Division is led by Director Amanda J. Law, PhD, Tenured Professor of Psychiatry and the Nancy Gary Endowed Chair in Children’s Mental Health Research.
40 Percent of DEI Subcommittees co-chaired by Division of Neuroscience leadership BY THE NUMBERS
$9+ Million Research dollars obtained in FY24 85% Increase in faculty, staff, students, and trainees since 06/30/22 (25 new hires)
Dr. Jason Tregellas, Professor of Psychiatry and Director of the Brain Imaging Center (BIC), received a NIH $2 million High End Instrumentation grant to purchase a new MR scanner. This will be housed and operated in the BIC.
The Division has a research portfolio spanning NIMH, NICHD, NIDDK, NIDA, NCI, AHA, VA, and ICMD. The research team leads 8 R01’s, an R37, an F31, an S10, a T32, a Diversity Supplement, 2 VA Merit awards, and a VA Research Career Scientist Award. The Division’s awards exceeded $9 million in FY24.
Research conducted by Drs. Sharon Hunter, Camille Hoffman, Amanda J. Law, Randy Ross, and Robert Freedman has produced evidence of choline’s effectiveness to support human brain development in-utero, when included as a prenatal supplement. As a result, in June 2024, Governor Polis signed into Colorado Law, “Measures to Improve Perinatal Health Outcomes”. Included in the law, is a mandate that Medicaid cover the addition of choline supplements to prenatal vitamins already covered.
First Lady Jill Biden, visited the Anschutz Medical Campus on April 20, 2024. Dr. Tracy Bale, Tenured Professor, Psychiatry, met with the First Lady to discuss women’s health and sex differences research. Dr. Bale holds the Anschutz Foundation Endowed Chair in Women's Integrated Mental and Physical Health Research at the Ludeman Center, which leads the country in women’s health and sex differences research.


The Division of Addiction Science, Prevention, & Treatment is comprised of three strong and inter-related arms: Research, Clinical, and Education. Current Division addiction research programs and expertise include genetics, epidemiology, biomarkers of addiction and treatment response, medication development, human laboratory studies, clinical trials, deep brain stimulation, and health & neurocognitive effects of cannabis use across the lifespan. The Division's clinical arm, Addiction Research & Treatment Services (ARTS), provides residential and outpatient addiction care for adults, as well as outpatient care for adolescents. The Division is home to the Rocky Mountain Cannabis Research Center (RM-CRC) offering mentored research training and pilot research funding opportunities for medical students, graduate students, post-doctoral fellows, and junior faculty interested in cannabis research. The RM-CRC places special emphasis on recruitment and outreach to trainees and junior faculty from groups underrepresented in medicine.
The Division recently received funding for the Rocky Mountain Cannabis Research Center, a NIDA-funded P50 Center of Excellence for research on the health effects of cannabinoids. The grant will be funded from 2023 to 2028 and provides $15M in total costs.
The Division boasts multiple University-wide awardees for clinical excellence and teaching, including:
Joe Sakai MD (UCH Clinician of the Year, 2024)
Michelle LaLinde FNP-BC (CUSOM Distinguished APP Clinician of the Year, 2024)
Tyler Coyle MD (CUSOM Chancellor's Teaching Award, 2023)
The Division launched the Mobile Methadone Unit in the summer of 2024. We are one of only two mobile methadone units in Colorado

7.6 Million NIH direct cost dollars granted across 22 faculty
$1,000,000+ Philanthropic support in FY24
800+ Patients receiving treatment daily at ARTS
The CPP Division advances an equitable, excellent, and evidence-based behavioral health system in Colorado through clinical, public health, and educational partnerships. The Division’s faculty care for the most vulnerable Coloradans through their work in state mental health hospitals, correctional care facilities, forensic programs, and national telehealth programs. The Division's educational programs include an accredited Forensic Psychiatry Fellowship, public health training initiatives, and a new statewide behavioral health training system for the public.
BY THE NUMBERS
$15,000,000 External funding for public health training, consulting, and eval work since 2019

100% Psychiatrist staffing in the Colorado Department of Corrections, serving more than 15,000 patients per year
632 State mental health hospital patients served by 66 CPP faculty

CPP works with the Colorado Department of Human Services to launch the state's new Mental Health Transitional Living Program and support individuals with severe and persistent mental illness towards communitybased recovery.
For 20 years, the Behavioral Health and Wellness Program has secured more than $1 million annually in external funding for its training, consulting, and evaluation work.
CPP faculty care for more than 600 inpatients in state mental health hospitals at Pueblo and Fort Logan and 15,000 inmates in the Colorado Department of Corrections
CPP faculty care for a community of 38,000 students on the Auraria campus.
The BHA Learning Management System has enrolled over 1000 learners, published 32 Crisis Professional Curriculum courses, 22 Behavioral Health courses published, and has 42 additional courses under development to be published in the next few months. Additionally, a Behavioral Health Care Navigator Credential Foundations course published per legislative mandate (C.R.S 27-60-204).


In addition to supporting its clinical, research, education, and community missions through its divisions, the DOPsych boasts two Centers housed within the department, as well as multiple programs working to promote growth not only within the department but across the school, campus, and university.
These Centers serve as hubs for innovating research, fostering collaboration among faculty, students, and external partners. The programs are designed to address the evolving needs of the community, ensuring that the department remains at the forefront of advancements in mental health care. This comprehensive approach not only enhances the well-being of those served but also contributes to the broader academic and healthcare landscape.


Jay Shore, MD
Brain and Behavior
Innovation Center (BBICen)

Neill Epperson, MD
Helen and Arthur E. Johnson Depression Center (JDC)

Sandra Fritsch, MD
Office of the Colorado Mental Health Access Programs (CO-MAP)

Bruno Anthony, PhD

Jason Tregellas, PhD
Brain Imaging Center (BIC)

Matt Mishkind, PhD
Office of Psychological Science and Practice (OPSP)

Community Engagement Services (CES)

The Brain and Behavior Innovation Center (BBICen) at the University of Colorado Anschutz Medical Campus was created on October 16th, 2023, made possible with generous support and leadership from the Chancellor's office, including initial five years of seed funding for its establishment and development. BBICen fosters innovation in mental and behavioral health treatment and care delivery, aiming for "Brain Health for all, for life" to enhance the well-being of patients, their families, and communities in the greater Rocky Mountain region and beyond. This mission is achieved by advancing innovations in mental and behavioral health through its three pillars of Technology, Novel Therapeutics, and Care Redesign within the Department of Psychiatry and across the CU Anschutz campus. BBICen fosters internal and external collaborations across academia, government, industry, and the community.
34 Current projects in the Center Portfolio
18 Projects ongoing or completed in the Technology
$8,000,000
Health Rhythms is a remote patient monitoring system checklists/screeners with AI passive monitoring of beh detect worsening of symptoms and enhance care deliv
BBICen is engaging in cycles of iterative refinement to
BBICen leaders are in the final stages of establishing a Israel Deaconess Medical Center to launch a new prog integrate mindLAMP, a mental health application index Digital Health Atlas, into a telehealth treatment progra this initiative is to enhance patient monitoring and imp enabled care.
The use of psychedelic compounds to treat a wide rang conditions heralds a potential revolution in the ability to symptoms. While there is great excitement about prom much that remains uncertain and unknown. Faculty in t important contributions to advance understanding of h compounds and assess their efficacy.

The mission of the Helen and Arthur E. Johnson Depression Center (JDC) is to improve the lives of people with depression, bipolar disorder, anxiety, and related disorders through clinical excellence, innovative care models, community engagement, research, and workforce development. Founded in 2008 as an original member of the National Network of Depression Centers, the JDC leads efforts and collaborates with other leading academic medical centers and programs to ensure the delivery of best-in-class clinical care and educational programs to Coloradans. The JDC's Board of Advisors plays a key role in its success and has been instrumental in many initiatives, including hosting an annual luncheon with over 500 community participants

59,000+ Completed Patient Visits Since 2018
47,000+ Community Members Trained since 2016 $3,000,000+ Raised During Annual Luncheon since 2016

JDC clinicians form a multidisciplinary team of psychiatrists, psychologists, advanced practice providers, social workers, and licensed counselors delivering care to patients across the lifespan and family system. The center has deep expertise in providing services to individuals with mood and related disorders, developing and implementing integrated care models both inperson and virtually, and integrating other technology-based solutions with traditional care models.
Research is conducted for the purpose of improving the identification and treatment of mental health concerns. One example is the Child Bipolar Network (CBN), a consortium of five universities across the country (CU, UCLA, University of Pittsburgh, University of Cincinnati, and Virginia Commonwealth University) investigating the best ways to treat children or adolescents who are showing the first signs of bipolar disorder.
The center's community programs are designed to extend its reach across the state and nationally through diverse educational offerings aimed at increasing understanding of depression, bipolar disorder, anxiety, and related disorders, reducing stigma, preventing suicide, and enhancing access to quality mental health care. These educational programs are delivered to communities, schools, businesses, and professional groups.
In 2020, the JDC received an $8 million addition to its endowment, which now totals $24 million to support clinical services and education and training of the next generation of providers.

The Brain Imaging Center (BIC) at the University of Colorado Anschutz Medical Campus (CU AMC) is part of the Department of Psychiatry, Division of Neuroscience. It is a research-dedicated facility that houses a Siemens Skyra 3.0 Tesla wide-bore MRI scanner. The imaging center offers resources for stimulus delivery, response recording, and subject monitoring, including an MR-compatible goggle system with eye-tracking, MR-compatible headphones, four- and two-button response boxes, a highspeed eye-tracking system, and an MR-compatible pulse oximeter. Additionally, the BIC features an MR-compatible 64-channel EEG system. The center is led by Jason Tregellas, PhD, Professor of Psychiatry, serving as Director of the Brain Imaging Center, and Kristina Legget, PhD, Associate Professor, as the Assistant Director.
$1,000,000 Scan revenue in FY24
100 Active protocols utilizing our services
In 2024, Dr. Tregellas received an NIH $2 million High End Instrumentation grant to purchase a new MR scanner. This will be an additional machine housed and operated in the Brain Imaging Center. Dr. Tregellas had previously received the same award in 2015, which allowed for the purchase of the scanner currently in use.
The Brain Imaging Center is currently expanding its hours to accommodate substantially increased use over the last several years. Soon, it will be open 7 days per week, 12 hours per day.
The Brain Imaging Center has been the most productive research-dedicated imaging resource at the Anschutz Medical Campus for two decades. Currently, it supports dozens of NIH-funded research studies, including those requiring body imaging.

The Office of Psychological Science and Practice (OPSP) reflects the foundational contributions of psychology and psychologists to the clinical, research, educational, and service missions of the Department. With over 200 full-time and voluntary faculty, OPSP represents one of the largest and most accomplished groups of psychologists in a Department of Psychiatry within an academic medical center and its affiliate institutions (Children’s Hospital, University of Colorado Hospital, Denver Health, and the VA Eastern Colorado Health Care System) These psychology faculty are leaders in their field and specialties, demonstrated by their track record of grants, publications, awards, and roles in professional organizations and government-sponsored boards and committees. The Office supports the career development of doctoral-level psychologists, identifies, encourages, and supports opportunities for interdisciplinary research and innovative evidence-based clinical practice and policy, and standardizes, integrates, and promotes training for learners at various levels and across disciplines
200 Full time and volunteer faculty
50 Child- and adult-focused predoctoral, doctoral and post-doctoral students
6,000 Patients seen in the past year
Since its inception in 2021, OPSP has ra roles. It has established a robust resear Intervention and Implementation Resea multidisciplinary, multi-institutional grou graduate students, and community part individuals with behavioral health or neu
Psychologists within OPSP lead a variety of philanthropic, federal, and statefunded initiatives focused on service development and implementation science across various areas, including suicide prevention, executive functioning, family support, and women’s health. Through strong individual and group mentorship within CIIRG, junior faculty psychologists have recently received four career development awards (CHCO RISA Awards, NIMH K awards). Leveraging their training in evidence-based practice, psychologists provide clinical leadership across the Department and its clinical partners.
At CHCO, psychologists serve as clinical directors, overseeing treatment programs in the large Integrated, Ambulatory, and Colorado Springs Divisions, as well as the adult outpatient clinic. Nationally, psychologists are leaders in the expanding field of integrated behavioral health, where physicians and behavioral health clinicians collaborate with patients and families to deliver coordinated, systematic, and cost-effective patient care. OPSP leadership actively supports the development of integrated care across partner clinical entities


The Department has a history of robust community-academic partnerships. These community-based programs promote strategies for increasing mental health awareness, reducing stigma, identifying and eliminating health disparities, and addressing discrimination and harassment within our community. Through these partnerships, the Department of Psychiatry fulfills its educational, research, and community missions.
Community Engagement Services (CES) was established in early 2022 to serve as the core support service for the Department's various programs that collaborate with local communities. Key responsibilities of CES include supporting departmental programs in promoting strategies for increasing mental health awareness, addressing systemic health disparities, and advocating for systemic change.
Beyond its internal role, CES aims to be a voice that influences how communities and workplaces advocate for change, collaborate with existing systems, and understand, discuss, and prevent mental health challenges through evidence-based, accessible, and sustainable education and training programs.
CES recently partnered with Communications and Events to establish a core structure aimed at better serving the needs of all Department faculty and staff. This initiative seeks to promote community and donor engagement, as well as further the development of community-academic partnerships.
The first Community Programming Environmental Scan and Assessment of Needs was conducted by CES in 2022 to create the Department's inaugural Community Engagement Report.
CES serves as a continuing education office providing American Psychological Association continuing education credits.
An assessment of VitalCog: Suicide Prevention in Construction found that for every $1 spent on VitalCog training, $8.70 of social value was returned.
130,000+ Lives touched directly by Partnership programs
80
Percent of programs specific to the needs of Colorado 70% Department programs were developed in response to a request from a community group

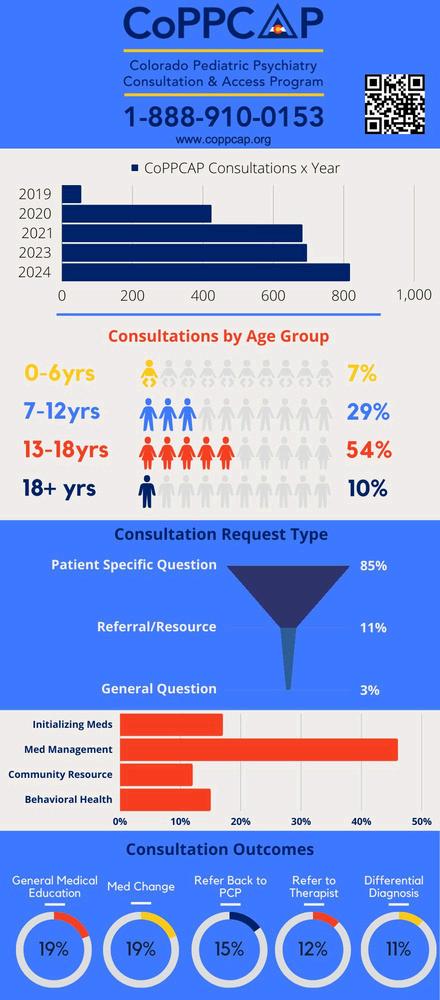
AP, the Office of the Colorado Mental Health Access Programs, is a newly formed y dedicated to supporting primary care access and treatment of mental health ncerns across the lifespan. Currently, the Office oversees one fully functioning am, CoPPCAP (Colorado Pediatric Psychiatry Consultation and Access Program), with two developing programs: EASY and PROSPER. These programs aim to assist ary care and perinatal providers through peer-to-peer consultations, identifying ment resources, providing patient consultations to guide treatment in primary care settings, and offering education.
CAP was developed following funding availability for Pediatric Mental Health Care Access (PMHCA) programs under the 21st Century Cures Act. EASY receives nthropic support from the El Pomar Foundation, while PROSPER secured 5-year unding from the Health Resources and Services Administration Maternal Mental h and Substance Use Disorder (MMHSUD) program in October 2023. CoPPCAP enrolled its first practice in September 2019.
AP is led by Sandra Fritsch, MD, who serves as the Medical Director and Project ector of CoPPCAP. The Office receives administrative support from Alexandra drews, MA, who also provides project management assistance for EASY and ER Thida Thant, MD, acts as the Medical Director for EASY, and Celeste St JohnLarkin, MD, serves as the Medical and Project Director for PROSPER
CoPPCAP enrolled its first practice in September 2019. Since then, CoPPCAP has enrolled 92 practices (including 3 that have subsequently closed), totaling approximately 980 pediatric primary care providers across Colorado, caring for approximately 635,000 youth. The program has facilitated over 3,060 peer-to-peer consultations and conducted 27 different ECHO series for providers in the CoPPCAP Network.
CoPPCAP has received support from AAP-CO (American Academy of Pediatrics-Colorado Branch) and CAFP (Colorado Academy of Family Physicians) to promote the program among their practice members. Additionally, CoPPCAP has presented at the Colorado Rural Health Association summits, the Colorado Youth Healthcare Alliance (Colorado School-Based Health Care Association) annual meetings, as well as AAP-CO and CAFP annual meetings to provide further educational offerings. When state ARPA funds became available, additional funding for CoPPCAP was included in SB22-147, signed by the governor in May 2022, securing $4.6 million in funding.


Kimberly Kelsay, MD
Interim Program Director, Psychiatry Residency Training

Sara Schwenk, NP
Co-Training Director of PMHNP Training
DOP/School of Nursing

Amy Lopez, PhD, LCSW Director, Colorado
Educator Support Program, Director of Social Work



Austin Butterfield, MD Director of Medical Student Education
Laurie Ivey, PsyD, MA Director of Psychology Education and Postdoctoral Training
The Office of Education and Training (OET) oversees the Department of Psychiatry's commitment to preparing healthcare professionals at all levels and disciplines to deliver the highest quality mental health care, conduct innovative research, and become the next generation of mental health educators. The training programs administered by OET encompass a full spectrum of educational levels and disciplines, including undergraduates, medical students, psychiatry residents and fellows, social work interns and fellows, nurse practitioner fellows, psychology externs and interns, and clinical and research post-doctoral fellows. OET emphasizes interdisciplinary collaboration and ensures that its training programs offer state-of-the-art and innovative education.
programs

The general psychiatry program has expanded to 15 residents per year and has developed three distinct tracks - the Pathways Resident Research Track (supported by R25 MH125758), the Adult/Child Combined Track, and the Community and Public Psychiatry Track. In addition, the program provides concentrations in psychotherapy and reproductive psychiatry
This year, the DOPsych and CU Medicine worked with Medicaid and several of the major insurance companies to allow for billing for services by trainees. This will increase access for patients, generate further revenue for the department, and allow for a wider range of learning opportunities for behavioral health trainees
The OET's trainee travel fund has supported 73 trainees in attending and presenting research at national meetings over the past 3 years







The Department of Psychiatry is dedicated to fostering a collaborative and inclusive workplace culture that prioritizes the well-being of its team members. The department maintains a robust and active Diversity, Equity, and Inclusion (DEI) committee, along with multiple sub-committees, focused on embedding these values throughout all aspects of its operations. The DEI group convenes regular committee and subcommittee meetings, offering department-wide opportunities such as training sessions and workshops to enhance cultural competency, actively recruit diverse faculty and staff, and establish support networks for underrepresented groups.
In addition to DEI efforts, the department places a high priority on workplace wellness through various programs led by Wellness Champions. These initiatives include access to counseling services, wellness workshops, and flexible work arrangements aimed at promoting work-life balance.
The department believes that cultivating a healthy and inclusive workplace environment leads to improved outcomes for both staff members and the communities they serve. By advocating for DEI and wellness initiatives, the department strives to create a supportive atmosphere where all individuals can thrive, make meaningful contributions, and reach their full potential. This commitment underscores the department's overarching mission to advance brain health for all, throughout life.



The DEI Committee within the Department comprises senior faculty, staff, administration, PRAs, and trainees This diverse group includes individuals of various racial/ethnic backgrounds and sexual orientations/identities across all levels, all dedicated to fostering diversity within the department and celebrating differences in all their forms.

AMC attendees at the 2024 National Conference On Race and Ethnicity (NCORE)
DOPsych DEI recently initiated a new department benefit for all faculty and staff called LEADER Time (Learning, Engagement, Advancement, Diversity, Experience, Relationships). LEADER time is 16 hours per fiscal year (prorated based on FTE).
With the time, individuals are encouraged to participate in activities across the department and campus wide, related to learning, and engaging with departmental committees or campus events, that advance diversity, enrich professional relationships, and/or professional development which helps to increase a sense of belonging, and promotes retention.
81 Active DEI members in the DOPsych
Provided consultation to the Children’s Hospital Colorado Diversity Health Equity and Inclusion team to launch the training series "Destination Equity," a multi-part training designed to provide clinical and non-clinical team members with knowledge and skills to address disparities and improve outcomes in healthcare.
67% Completed DEI training within the last year
In collaboration with CU SOM IT and Department of Family Medicine DEI partners, developed and is piloting implementation of a comprehensive diversity HR dashboard, which tracks key metrics across recruitment, retention, equity, and dimensions of diversity of staff, faculty, and trainee workforce.
96%
Faculty who cited specific examples of DEI in their PRISM reports
The Department's inaugural Faculty Wellness Officer, Dr. Liz Chamberlain, leads wellness initiatives in collaboration with Dr. Dyrbye's Office for the Faculty Experience. Additionally, the department provides funding for Staff Wellness Officers, currently held by Shanna Trott and Dana Kennedy. Guided by the Surgeon General's Workplace Wellbeing model, the Stanford Model, and departmental PWAC data, efforts are focused on enhancing professional fulfillment, addressing systemic drivers of burnout, and fostering community and connection among the dedicated teams within the Department of Psychiatry.
79% Of staff feel recognized for a job well done (increased from 67% in 2023)
54 Team Connection Event participants

54% Of psychiatrists report High Professional Fulfillment (compared with 41% nationally)

In 2024, physicians and APPs within the Department demonstrate significantly lower burnout rates compared to national benchmarks, while psychologists report significantly higher rates of professional fulfillment than national benchmarks (PWAC, 2024).
Adapted the Stanford PFI survey to create a benchmark for both Faculty and Staff in 2023, conducted 18 focus groups across diverse divisions to better understand drivers of burnout and fulfillment at the local level. 66% of DOPsych Staff find their work meaningful (completely/very true)
Awarded Growth and Development Funds in FY 2023 which allowed the wellness group to: Develop Team Connection Events, deliver trainings in Mindful SelfCompassion, Mindful Team Communication, Email Burden Reduction, DISC trainings.
Developed and currently implementing Email Burden Reduction program modules for both faculty and staff in the DOPsych and will share with other SOM Departments.



















