

ACCELERATING RESEARCH MEANINGFUL IMPACT

ABOUT US
Our mission is to accelerate arthroplasty research and to promote and support innovation, research, and education. Our work is driven by our passion to make a meaningful impact on the lives of those affected by joint diseases.
The Concordia Arthroplasty Research team is deeply committed to advancing patient experiences and access to research. Our focus on scientific discovery aims to improve the health and quality of life for all individuals affected by joint pain and mobility challenges.
We understand the increasing impact of joint diseases on people’s lives, and we are dedicated to being prepared to offer our support.
Orthopedic research at Concordia is rooted in empathy and compassion, continuously seeking to push the boundaries of medical advancements to alleviate the suffering experienced by individuals with joint pain, poor joint function, and limited mobility.
Our research not only addresses the growing needs of our patients but also seeks to uplift and strengthen the local community and contribute to the advancement of orthopedic care on a global scale. We recognize the rising demand for arthroplasty research and are committed to extending our efforts beyond our current scope.
As joint replacement volumes increase and patients strive to lead longer, more active lives, we empathize with the challenges they face. We are prepared to meet these challenges head-on, utilizing science to develop data and evidence that inform our best practices and enhance care at Concordia.
Dr. Thomas Turgeon, MD, BSc., MPH, FRCSC, FAAOS
Orthopedic Surgeon and Director of Arthroplasty Research
Anupam Kothari, Chair, Arthroplasty Research Committee, Concordia Foundation





OUR 3-YEAR STRATEGY
4
STREAMS
- 3 YEARS
Stream 1 – Innovation and Legacy Planning
A. Robot-Assisted Surgical Innovation
B. New Implant Research and Development
C. Training the Next Generation of Surgeons and Scientists
Stream 2 – Medical Imaging
A. Next Generation Implant Stability
B. Assessment of Bone Implant Integration
C. Computer Vision of Patient X-rays/ CT Scan
Stream 3 – Clinical Trials
A. Implant Safety Analysis Hub Using CT-Migration
B. Pre-Operative Weight Loss to Improve Patient Outcomes
C. Evaluation of New Surgical Techniques
Stream 4 – Big Data
A. Concordia Research Database
B. Linkage of Manitoba Administrative Databases
C. Analysis Hub for National Administrative Data





STREAM 1 Innovation and Legacy Planning

Robot-Assisted Surgical Innovation
Problem Identified: Robotic-assisted surgery is a hot topic, but does it improve arthroplasty? How does it improve arthroplasty?
Our Goals:
1. Evaluate, procure and implementation of robotic-assisted surgical technologies
2. Assess patient outcomes, operating room efficiency and surgical accuracy improvements.
3. Optimize robotic technology usage to deliver improved patient care.


New Implant Research and Development
Problem Identified: What contributions can we make to new treatments and technologies in arthroplasty?
Our Goals:
1. Research, evaluate and co-develop subsequent generation tissueengineered orthopaedic implants and methods of pre-clinical assessment.
2. Design, refine and produce next-generation metal 3-D printing technologies for patient-matched orthopaedic implants.
3. Continue research, development and advancement of 3D printed resorbable, antibiotic implant materials toward clinical application.
Training the Next Generation of Surgeons and Scientists
Problem Identified: How do we leave a lasting legacy of excellence? How do we attract the best and brightest to Concordia to care for all Manitobans?
Our Goals:
1. Training of surgical residents and fellows focusing on a structured approach to clinical research.
2. Enhance the learning experience for young surgeons and engineers with the latest technologies, providing opportunities for self-directed research, learning, and enhanced clinical integration.
3. Encourage and empower the next generation of young researchers.

STREAM 2 Medical Imaging
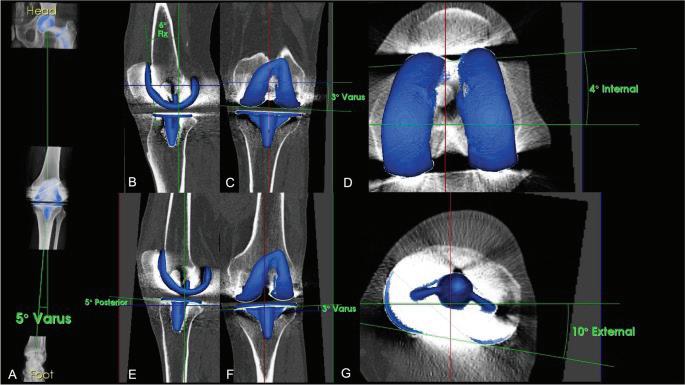
Next Generation Implant Stability
Problem Identified: Not all innovations are improvements – we need both RSA and CT imaging to ensure the implants we use are safe, durable, and perform as they should as part of our rigorous improvement process.
Medical imaging rapidly evolves, and staying updated with the latest technology is critical in research.
Our Goals:
1. Evolve Current RSA research regulation into the next generation of measuring joint replacement stability and longevity using CT imaging. RSA, or ‘radiostereometric analysis,’ is a specialized method of reading X-rays with high accuracy to detect minimal movements between an implant and the bone. Consider measuring a faint crack in a bridge to forecast collapse—the traditional method is a yardstick, and RSA is a micrometre. These ‘cracks’ or the movement of implants within bone help us predict the failure (or success) of new implant technologies and surgical techniques. RSA allows us to do this better and, faster.
2. Validate and implement the CT imaging methodology at Concordia. RSA traditionally requires tiny beads or markers that are implanted into the bone during surgery, which requires a specialized x-ray system. Next generation technology uses CT imagining and other techniques to eliminate the need for the beads or specialized x-rays making the technology more accessible and applicable.
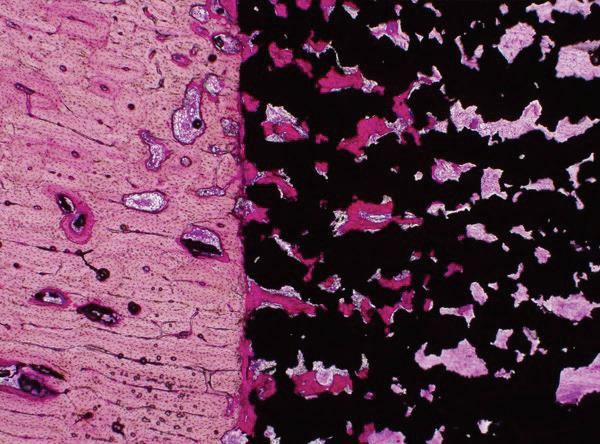

Assessment of Bone Implant Integration
Problem Identified: The junction between an implant and bone is critical to the success of arthroplasty. However, it is never guaranteed and can vary significantly between implant technologies and bone qualities.
Our Goals:
1. Feasibility of measuring bone in-growth / on-growth of orthopedic implants shortly after surgery to assess the quality of fixation and stability.
2. Concordia is first in the market. No other technology exists.
Computer Vision of Patient X-rays/ CT Scan
Problem Identified: Trends and patterns of failure in arthroplasty are difficult for the human eye (and brain) to catch.
Our Goals:
1. Develop a machine learning algorithm for automatic analysis of routine clinical X-rays for signs of implant or bone issues
2. We aim to use AI to analyze our many thousands of standard-of-care X-rays to look for patterns across our entire patient database. We can collect large amounts of data from our 20-year patient database’s X-rays using AI.
3. Analyze this data for trends and patterns to help us identify bone or implant problems that would otherwise go unnoticed. This technology complements our CT-imaging program.
STREAM 3 Clinical Trials
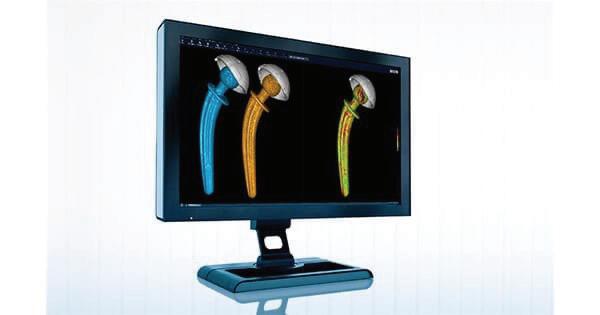



Implant Safety Analysis Hub Using CT-Migration
Problem Identified: How can Concordia collaborate with centres across Canada to promote and expand new CT imaging research in arthroplasty? Sharing this information benefits us all.
Our Goals:
1. Expand Concordia’s national leadership role as a hub for CT imaging clinical trials.
2. Contribute to early clinical investigation of new and novel joint replacement technologies with high-precision imaging and data.
Pre-Operative Weight Loss to Improve Patient Outcomes
Problem Identified: New medications are now available that may improve arthroplasty for overweight patients, but more evidence is needed.
Our Goals:
1. Partner with a manufacturer of GLP-1 antagonist medication to initiate a clinical trial for patients with a BMI over 40.
2. Assess whether pre-operative weight loss reduces complications and improves patient outcomes following surgery.
Evaluation of New Surgical Techniques
Problem Identified: Surgical innovation is constantly occurring, but many innovations are not broadly adopted because there is no robust, unbiased evidence. Can Concordia lead large, multi-center, multi-surgeon clinical trials to generate this evidence?
Our Goals:
1. Understand the relationship between patient outcomes and limb alignment after knee replacement.
2. This is one of those big projects we propose. Should your knee be in ‘straight’ alignment with your hip and ankle, or should it be as close as possible to what it was before arthritis hit? Or should we match it to your other knee? What’s the best alignment theory that provides the best-performing knee for each patient?
Seek a definitive answer as to the benefit of patella resurfacing vs non-resurfacing. In a knee replacement, we ‘resurface’ the bones with metal and plastic to replace the damaged cartilage. But the knee joint also has a kneecap—the patella. Some surgeons ‘resurface’ the patella at the same time as the knee joint, while some don’t, and some do it selectively. It is challenging to know the best option for any patient.
Evaluate other novel surgical techniques. How do novel surgical techniques these compare to patient outcomes? Do any reduce surgical time, lower infection risk, or avoid complications or other postsurgery issues?

STREAM 4
Big Data



Concordia Research Database
Problem Identified: Extensive datasets offer the best foundation for answering crucial questions, but skill is necessary to extract this information accurately. Although our local database contains high-quality data, it has not been fully utilized yet.
Our Goals:
1. Complete the current project portfolio, which includes seven studies.
2. Utilize a 20-year database to develop pilot data as a springboard for launching new large-scale projects that are surgeon-driven, industrysupported, and collaborative in Manitoba
3. New machine learning projects.
Linkage of Manitoba Administrative Databases



Problem Identified: Manitoba has some of the best medical data records in North America, but they have yet to be used for arthroplasty research due to complex linkages that need to happen.
Our Goals:
1. Combine rich data within Manitoba together with the local registry
2. The Manitoba administrative databases are so rich that we can ask and answer some of the big questions about arthroplasty care, including medication usage, mental health, speed and accessibility of care, and contributors to the success or failure of surgery.
Analysis Hub for National Administrative Data

Problem Identified: Canada’s high-quality arthroplasty databank is underutilized, lagging behind similar databanks in other nations with well-established research teams.
Our Goals:
1. Be recognized as the Canadian Hub to analyze the underutilized Canadian Joint Replacement Registry.
2. Create a local scientific research program and collaborate with other Canadian surgeons.
3. Develop a structure for industry-funded research studies.
Indigenous access to care project
Problem Identified: Are indigenous people receiving equal and equitable care? Numerous factors generally hamper the speed at which indigenous people receive the care they need, such as rural living, geographical distance to medical services, lack of internet or phone connectivity, social and cultural differences, language barriers, prejudices, and financial resources.
Our Goal:
1. We aim not just to identify problems but to propose and implement solutions.
01 COLLABORATION
We recognize the importance of collaboration in our work as scientists and medical professionals. We are committed to continuing our partnerships with esteemed institutions such as the University of Manitoba, Queen’s University, Western University, Mount Sinai Hospital, the University of Toronto, the University of Nebraska Medical Center, and Leiden University Medical Center. Collaboration is a key factor in realizing the groundbreaking breakthroughs we aim for.
03
05 COORDINATION FUNDING
It’s crucial to coordinate and manage all moving parts, stay ahead of the curve, pivot when necessary, and be resilient. We are fortunate to have exceptional leadership and expert staff members, some of the best in the field.
WHAT WILL IT TAKE TO ACHIEVE THESE GOALS?
02 COLLEAGUES & STAFF
Our team is comprised of highly skilled professionals who are dedicated to their work and have been with us for many years. The diverse mix of age groups, professional designations, and life experiences has contributed to our success. Over the next three years, we will expand our team to complement the current group and increase our staff capacity.
04
CRITICAL THINKING & ANALYSIS
Critical thinking is is a key pillar of research that demands a level of expertise that can be relied on to achieve results for the team and to meet these goals.
06
FUNDING GOALS
Capital Needs 2024-2027: $3.5 Million
To meet the ambitious program’s capital and operating costs, the plan incorporates a multifaceted approach that will enable us to have a sustainable funding program to meet the future. Donors, grants and endowment funds are part of our strategy.
Operating Needs 2024-2026: The Concordia Foundation Endowment Fund for Arthroplasty Research and other private funders have pledged $1 million over three years. An additional $810,000 will be raised to operate these streamed programs.

