





As I reflect on the past year at Swiss TPH, I feel immense pride and gratitude for all that we have achieved – my sincere thanks go to all the staff and partner organisations who have contributed to this success. In the years to come, we will need all our strength. Since the turn of the millennium, global health has made extraordinary strides: new vaccines, medicines, and diagnostics, stronger health systems and better-trained health professionals have improved lives worldwide. Yet today, this progress is at risk. Political instability, misinformation, and funding cuts threaten to undermine scientific advancements and weaken our ability to respond to emerging health threats.
Now more than ever, we need institutions like Swiss TPH that pursue evidence-based research through trusted partnerships. A powerful example of this is Swiss TPH’s leadership in shaping the research agenda for noma, a devastating disease primarily affecting children in extreme poverty. By bringing together experts from across sectors, including noma survivors themselves, Swiss TPH advances research, raises awareness, and drives action to combat this disease. This work exemplifies what Swiss TPH does best: bridging research and implementation to create lasting impact.
Swiss TPH also plays a critical role in uniting stakeholders to address global health challenges. In February last year, I had the pleasure of opening a symposium on improving access to healthcare in low- and middle-income countries, which brought together over 300 experts from the public and private sectors, product development partnerships, academia, and NGOs. These discussions are more than just conversations –they foster partnerships across sectors to develop tangible solutions for those who need them most.
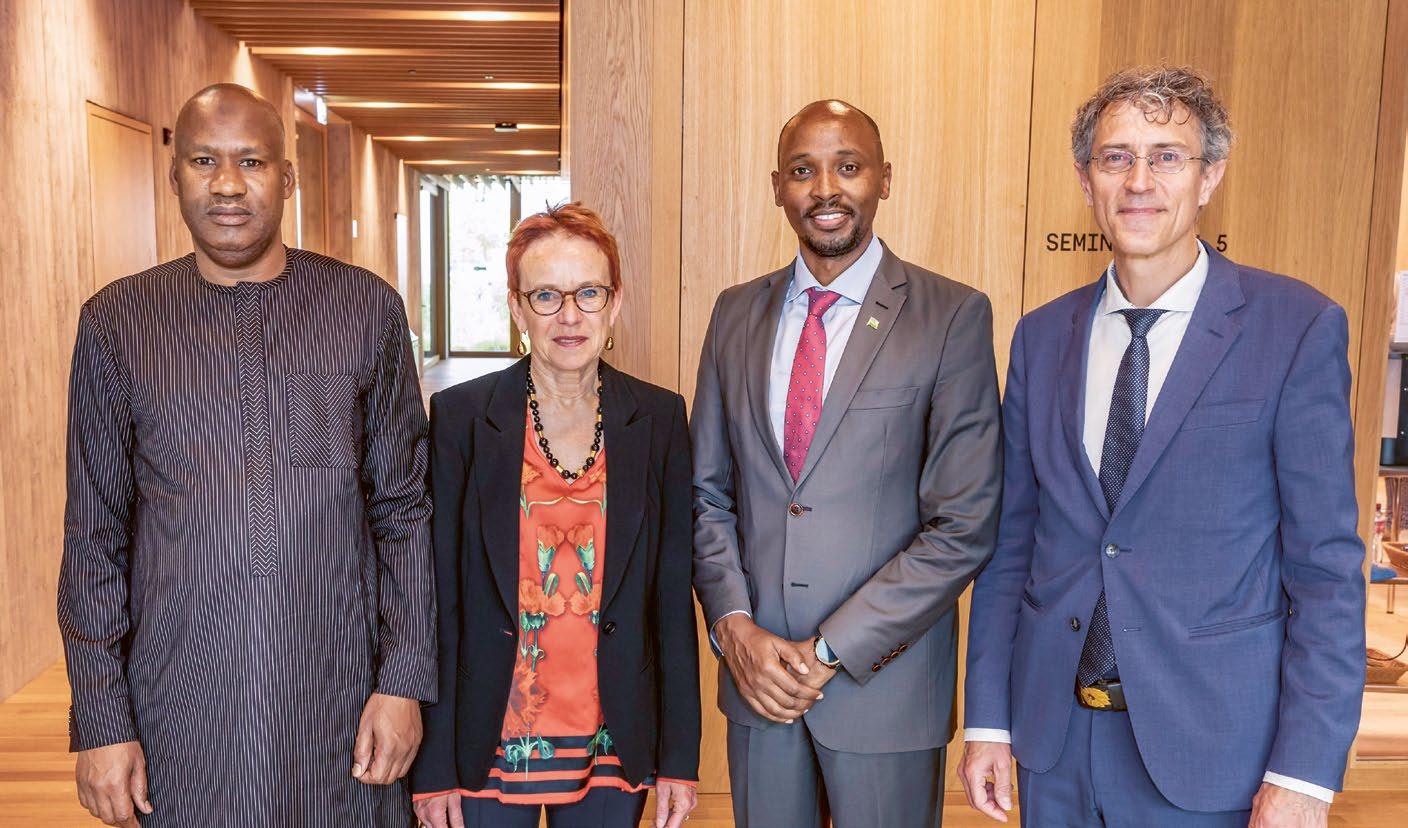
Swiss TPH’s impact is also visible through its commitment to empowering the next generation of global health leaders. Around the world, our alumni are at the forefront of research and innovation, health promotion, and systems strengthening, influencing policy at the highest levels. An example of this was the visit of Rwanda’s and Senegal’s Ministers of Health, Sabin Nsanzimana and Ibrahima Sy – both Swiss TPH alumni. Their leadership in shaping national health strategies today is a testament to Swiss TPH’s long-standing commitment to capacity strengthening and knowledge circulation.
Today, we are facing major challenges. Swiss TPH has always been a force for progress, and its role is more critical than ever. By driving innovation, fostering collaboration, and equipping the next generation of leaders, we are making a lasting impact on global health. As Chair of the Board of Governors, I am committed to ensuring that Swiss TPH remains a leading force in shaping a healthier, more equitable future for all.

Dr. Eva Herzog President of the Swiss TPH Board of Governors
“Our mission is more relevant than ever”

This past year reaffirmed the essence of Swiss TPH: an institute anchored in scientific excellence, enriched by diverse perspectives, and united by a shared mission – to improve health worldwide.
Across countries and communities, our teams have made a difference. In 2024, Swiss TPH was involved in more than 400 projects spanning 126 countries. These achievements were made possible by the dedication of nearly 1,000 staff and students from 96 nations. These numbers speak to more than our global reach – they reflect the trust placed in us by our partners, governments and funders, and the power of collaboration that fuels everything we do.
Public health has always played a vital role in enabling societies to thrive. At Swiss TPH, we contribute through cutting-edge research, comprehensive education and training and the provision of quality health services – made possible by our unique network of partnerships around the world.
As we entered the new year, we experienced a global health landscape shaped by uncertainty, shifting priorities and increasing pressure on resources. Yet, our mission is more relevant than ever. Over the past year, we made important scientific advances: revealing a key malaria invasion mechanism, advancing our understanding of multidrug-resistant tuberculosis, and pushing forward the clinical development of promising new drugs against parasitic worm infections. Simultaneously, we strengthened health service
delivery in fragile settings – such as in Somalia, where our digital health initiative ALMANACH is enhancing care for children.
We also celebrated notable milestones and outcomes across our projects. The 20-year anniversary of the Chronic Diseases Clinic of Ifakara stands as a powerful testament to the impact of long-term partnership. In Switzerland, our study showed the long-term impact of the Youth+Sports programme and illustrated how sustained investment in prevention fosters lasting public health benefits. Our modelling work on climate-sensitive disease risks, such as the projected rise in malaria burden in Kenya, is contributing critical insights to guide public health preparedness and tailored responses.
Swiss TPH also continued to serve as a platform for meaningful dialogue and action. Our symposia on noma, women and gender in global health, and access to healthcare in low- and middle-income countries brought together voices from across science and society – sparking conversations that aim not just to highlight challenges, but to shape real, implementable and impactful solutions.
The success of Swiss TPH lies in the strength of its people. To our staff, students and partners: thank you for your dedication, your expertise and your unwavering commitment to advancing global health. Together, we are well positioned to meet the challenges ahead – with resilience, with scientific rigour, and with a steadfast focus on improving health so that nobody is left behind.

Prof. Dr. Jürg Utzinger Director, Swiss TPH

→ The success of Swiss TPH lies in the strength of its people – staff, students and partners. Together, they face the challenges ahead to continue improving people’s health.
Disinformation as a global risk, growing international pressure on science, financial challenges – State Secretary Martina Hirayama discusses the importance of education, research and innovation for Switzerland, the role of international partnerships, and the contribution of institutes such as Swiss TPH.
Three years ago, you gave the opening speech at the new Swiss TPH headquarters in Allschwil. What was your impression at the time – and how do you see Swiss TPH today?
Martina Hirayama: “It was impressive to enter the new building – modern, open, full of energy. The infrastructure is a perfect match for the cutting-edge research taking place inside. Today, Swiss TPH is an important pillar in Switzerland’s education, research and innovation system and is indispensable nationally in the field of public health. What is also impressive is its international presence – Swiss TPH is active and well-connected worldwide.”
You took part in the World Economic Forum (WEF) in January 2025. Disinformation was ranked as the greatest global risk over the next two years, ahead of extreme weather events and armed conflicts. How can stakeholders in Switzerland’s education, research and innovation sectors address this risk?
Martina Hirayama: “There are three key elements: First, education – it empowers people to think critically and navigate the media landscape. Only then can we properly assess information. Second, science – it must be transparent, including about its limitations. Research is a process, and answers aren’t always immediate. And third, the development of technological tools to detect disinformation – here, research is just as essential as the responsible use of these technologies.”
Switzerland has topped the UN Global Innovation Index for the 14th year in a row. Could recent government austerity plans jeopardise this position?
Martina Hirayama: “Our innovation capacity is built on a wide range of factors: a strong vocational education and training system, excellent universities, high-quality basic research, and effective knowledge and technology transfer. Collaboration with industry also plays an important role. In Switzerland, around two-thirds of research and innovation funding comes from the private sector. This requires an appropriate framework, for large companies as well as for SMEs and start-ups. International cooperation is also vital, for example through European programmes or bilateral agreements that enable joint research and mobility in education. Other factors include quality of life, political stability, and a reliable legal system. It’s true that the financial situation is tight, and setting political priorities will be crucial. But education, research and innovation enjoy broad political and public support in Switzerland. There is a strong awareness of the need to invest in these areas.”
Science is also under pressure internationally –for example in climate research, biomedicine, and global health. Should Switzerland take a stronger position here?
Martina Hirayama: “One thing that sets our education, research and innovation policy apart from many other countries is its strong bottom-up ap -

proach. We count on researchers to take initiative and define priorities, rather than imposing political directives on what should be explored. While there are specific thematic focuses, such as national research programmes or strategic areas, we fundamentally believe that the driving force lies in research itself, and that scientists are best placed to identify the most relevant questions for the future. Take nanotechnology, for example, which was recognised as important by scientists long before it appeared on the political radar. The same applies to global health: research institutions like Swiss TPH define their priorities based on their scientific expertise.”
How can Switzerland remain innovative and competitive, and what role do research institutions of national importance like Swiss TPH play?
Martina Hirayama: “Swiss TPH is rightly recognised as a research institution of national importance. It works closely with universities such as the University of Basel and brings valuable international perspectives. The Basel region has developed into a strong ecosystem for life sciences and global health. Fondation Botnar’s investment
in the region is largely due to excellent institutions like Swiss TPH. Internationally – especially in Africa – Swiss TPH is a visible and valued partner. That also enhances Switzerland’s reputation as a trustworthy research hub.”
The Swiss Science Council notes in its evaluation that Swiss TPH will become even more important in the future due to the health risks associated with climate change. What is your view?
Martina Hirayama: “Unfortunately, I think that’s the case. We’re already seeing diseases emerge in regions where they were previously uncommon. For example, mosquitoes that can transmit such diseases are finding new habitats due to climate change. With its long-standing experience in combating tropical diseases, Swiss TPH can also make an important contribution in Switzerland – for instance, in early detection and prevention. Its close ties with countries in tropical regions also make it an ideal partner in tackling new challenges in these diseases – for example, by developing new control strategies or treatments in collaboration with local partners.”
Swiss TPH works along the entire value chain –from basic research to the testing and application of research findings. How important is the practical application of science, and how should it be supported?
Martina Hirayama: “Basic research remains crucial – it generates new knowledge. At the same time, it’s important to find ways to translate this knowledge into real-world solutions. This means researchers need to be aware of the practical potential of their work, and we need the appropriate policy framework and funding instruments, such as Innosuisse, which help SMEs access this knowledge and develop applications. Collaboration between research and practice is essential – and ultimately a prerequisite for our ability to continue investing in basic research.”
You recently visited Tanzania and Kenya to strengthen bilateral relations in education, research and innovation. What impressions did you take away?
Martina Hirayama: “It was inspiring to see the dedication of local researchers – for example, at the Ifakara Health Institute (IHI), which works closely with Swiss TPH. This collaboration, which has existed since 1956, shows what can be achieved through long-term strategic partnerships. Today, IHI is a research institute with an international reputation, attracting funding thanks to its scientific excellence and strong track record as a research partner.”
Martina Hirayama has been Head of the State Secretariat for Education, Research and Innovation (SERI) since 2019. She studied chemistry at the University of Fribourg, ETH Zurich, and Imperial College London, and completed a postgraduate degree in business economics. After completing her PhD, she worked in the ETH Zurich’s Department of Materials, becoming head of the Polymer Chemistry Group. She was also co-founder and CEO of a start-up in new coating technologies.
From 2003, she was a professor of industrial chemistry at the Zurich University of Applied Sciences (ZHAW) in Winterthur, where she developed the field of polymer materials and the Institute of Materials and Process Engineering. From 2011 to 2018, she was Director of the ZHAW School of Engineering.
Martina Hirayama has held numerous national and international roles, including president of the board of the Federal Institute of Metrology, vice president of the Innovation Promotion Agency Innosuisse board and member of the Swiss National Science Foundation board.

“I work with an international team on an open-source database that enables rapid viral classification, tracking, and vaccine development, covering viruses like Ebola and Mpox. At a time when misinformation is rife, it is more important than ever to uphold open science and accessible data.”
Together with our partners, we currently work on 437 projects in 126 countries.
995
Employees at Swiss TPH
184
Employees based abroad
Universidad Peruana Cayetano Heredia, Peru
Long-term Partnerships
Swiss TPH has a long-standing collaboration with research institutes in Tanzania, Côte d’Ivoire, Chad, Lao PDR, Papua New Guinea and Peru, all of which have played an integral role in the history and strategic development of Swiss TPH.
≥ 10 projects
≥ 5 projects
≥ 1 project
Swiss TPH offices
437
Projects to improve people’s health and well-being
Centre Suisse de Recherches Scientifiques en d’Ivoire (CSRS)
Centre Suisse de Recherches Scientifiques en Côte d’Ivoire (CSRS)
Employees based in Allschwil/Basel
Centre de Support en Santé Internationale (CSSI), Chad Ifakara Health Institute (IHI), Tanzania
Countries in which we work
Nations represented at Swiss TPH
Lao Tropical and Public Health Institute (Lao TPHI), Laos
Papua New Guinea Institute of Medical Research (PNGIMR), Papua New Guinea
Swiss TPH is a world-leading institute in global health, with a particular focus on low- and middle-income countries. By uniquely combining research, education and services, we aim to improve the health and well-being of people through a better understanding of disease and health systems and by acting on this knowledge.
Application
Discover novel diagnostics, drugs and vaccines and develop new approaches and tools
Generate evidence in countries we work under real-world conditions
Integrate new treatments and approaches into policy and health systems
Swiss TPH works across a value-chain, from innovation and validation to application. Innovations such as new diagnostics, drugs and vaccines or approaches and tools are rigorously validated in real-world settings and applied and integrated into health systems and policies.
The five departments at Swiss TPH work across three fields – research, education and services – to improve health globally.
Medical Parasitology and Infection Biology (MPI)
MPI studies diseases of poverty and develops diagnostics, drugs and vaccines to combat them
Epidemiology and Public Health (EPH)
EPH studies health and diseases in relation to their social, ecological and genetic determinants
Medicine (MED)
MED provides clinical and diagnostic services and conducts clinical research in low-resource settings
Swiss Centre for International Health (SCIH)
SCIH provides policy advice, project design and management in the area of national and global health
Education and Training (ET)
ET offers local, national and international training programmes and courses at graduate and postgraduate levels
Scientific and policy advice
Our employees are members of various expert bodies and provide advice to boards and committees. For example, we advise Swiss federal commissions and international organisations such as the WHO on evidence-based health policy.
More information about our memberships can be found on our website: → www.swisstph.ch/en/about/memberships
Scientific output: 499 peer-reviewed publications spanning topics such as infectious diseases and public, environmental and occupational health, to immunology and microbiology.
Public, Environmental & Occupational Health
Infectious Diseases
Tropical Medicine
Parasitology
Environmental Sciences & Ecology
General & Internal Medicine
Science & Technology
Microbiology
Pharmacology & Pharmacy
Healthcare Sciences & Services
Immunology
Research & Experimental Medicine
Other Topics
Distribution of “research areas” of Swiss TPH publications in 2024 according to Web of Science (accessed: April 2025)
The 2030 Agenda for Sustainable Development with the 17 Sustainable Development Goals (SDGs) provides a compass to tackle the global challenges we face, including those related to poverty, inequality, climate and health.
Swiss TPH is committed to the achievement of the SDGs, placing particular emphasis on SDG 3 “Ensure healthy lives and promote well-being for all at all ages” and Universal Health Coverage (UHC). With our research projects and service mandates, we contribute to 15 of the 17 SDGs.


Symposium on Improving Access to Healthcare in Low- and Middle-Income Countries (LMICs) Access to drugs, diagnostics and vaccines remains a challenge in many LMICs. Swiss TPH hosted a symposium bringing together 350 experts and key players from academia, the pharmaceutical industry, politics and product development partnerships to assess current strategies and foster synergies in research, drug development and medicines’ implementation.

Centre for Tropical and Travel Medicine Now in the “Turmhaus” at Aeschenplatz For 80 years, doctors have been advising, vaccinating and treating travellers at Swiss TPH’s Centre for Tropical and Travel Medicine. It is the largest centre of expertise for tropical and travel medicine in Switzerland and advises around 15,000 clients from Northwestern Switzerland every year. In January, the Centre moved to its new location in the heart of the city.

Strategic Interventions for Inclusive and Quality Healthcare in Albania The Health for All Project (HAP) aims to improve primary healthcare services for the Albanian population, particularly for vulnerable groups. Now in its third phase, the project funded by the Swiss Agency for Development and Cooperation (SDC) can look back on eight years of high-impact implementation, including strengthening health management capacity, new models of home-based care services, infrastructure improvements and continuing medical education.

→ Data from 21 villages showed that 27% of the rural population presented with steatotic liver disease.
New Discovery Unravels Malaria Invasion Mechanism A recent breakthrough sheds light on how the malaria parasite, Plasmodium falciparum, invades human red blood cells. The study, led by Swiss TPH and Griffith University’s Institute for Glycomics, reveals the role of a sugar called sialic acid in this invasion process. The findings, published in Cell Reports, have major implications for malaria vaccine and drug development.

→ Children under 10 are now 40% more likely to survive to their next birthday than before the introduction of EPI in 1974.
Heat as a Health Risk: Need for Action to Raise Public Awareness On behalf of the federal government, Swiss TPH conducted Switzerland’s first national survey about heat and its effects on health. The results show that while the population is generally aware of heat protection, many helpful measures are either unknown or not actively implemented, leading to avoidable health consequences.
Parasitic Worms and Liver Disease in Rural Laos Research by Swiss TPH and partners in Lao PDR has found high rates of steatotic liver disease in a rural region where liver fluke infections and diabetes are common. Surprisingly, in some cases, the parasitic worms appeared to have a protective effect against steatotic liver disease. Published in Annals of Medicine, the study highlights the interplay between infectious and non-communicable diseases.

→ The findings offer hope for urgently needed new antimalarial drugs.
154 Million Deaths Averted: Contribution of Vaccination over the Past 50 Years In 1974, the World Health Organization (WHO) launched its Expanded Programme on Immunization (EPI). 50 years later, a study shows that an estimated 154 million deaths have been averted thanks to vaccination. The study, published in The Lancet, was led by Swiss TPH in collaboration with WHO and numerous research organisations.


→
Launch of Swiss TPH Alumni Network Since its founding in 1943, education and training have been a cornerstone of Swiss TPH. Over the past 25 years, around 3,000 students from more than 80 countries graduated from Swiss TPH. Many of them now hold prominent positions in multilateral organisations, government, NGOs, research and the private sector. They shape policy and implement health system change as leaders at global, national and local levels. To further strengthen the connection with alumni, the Swiss TPH AlumNet was launched.

→ Chronic pain is widespread among Somali pastoralists in Ethiopia, especially among women and the elderly.
Not Just a Sneeze: Pollen Increases Blood Pressure Pollen allergies affect an estimated fifth of the world’s population. Researchers from Swiss TPH found that high pollen concentrations on average increase blood pressure in allergic people. This effect highlights a significant public health concern as pollen seasons lengthen and intensify due to climate change.

→ Swiss TPH offers training programmes and courses at graduate and postgraduate levels.
Chronic Pain and Pastoralists in Ethiopia Chronic pain is a global health concern and access to pain control is a basic human right. While the burden of chronic pain is well described in high-income countries, there is limited data in low- and middle-income countries, in particular in marginalised communities such as pastoralists. A study by Swiss TPH and partners found a high prevalence of chronic pain among Somali pastoralists in Ethiopia.

Strengthening Swiss-Ivorian Research Partnership Swiss TPH and the Centre Suisse de Recherches Scientifiques en Côte d’Ivoire (CSRS) have a long-standing partnership. Starting with a small field laboratory in 1951, the CSRS has grown into a full-fledged centre of excellence in research, education and sustainable development, recognised for its contributions to scientific knowledge in West Africa. To support the research activities, new infrastructure projects are required, including the construction of a new laboratory.

Improved HIV Treatment for Children and Adolescents Globally, around 2.6 million children and adolescents are living with HIV, with the majority of them residing in sub-Saharan Africa. These young people are more likely to experience treatment failure compared to adults. While experts have long assumed that testing for viral drug resistance could improve treatment in cases of failure, research led by the University of Basel, Swiss TPH and partners shows that supporting patients in taking their medication regularly is far more important.

Dogs for Hunting Tigers Swiss TPH investigated whether trained dogs could detect tiger mosquito larvae to support control efforts. In lab tests, dogs identified larvae with 80 – 90% accuracy. Field training proved more challenging, requiring extensive repetition. Further research is needed to optimise training methods and explore synthetic odours for practical application in mosquito surveillance.
The Nutrition in City Ecosystems (NICE) project is transforming lives by improving nutrition and promoting healthier diets through locally-led action. Across six secondary cities in Rwanda, Kenya and Bangladesh, NICE works closely with local communities to connect consumers with farmers who produce food sustainably. A video, telling the story of Aline and her son shows how the project successfully combats malnutrition.
→ Watch the video here

Study Shows Effectiveness of Organised Youth Sports in Switzerland Maintaining physical activity throughout life is crucial for health and well-being. However, the age-related decline in average physical activity is a challenge. The study, published in Swiss Medical Weekly, found that organised sports, supported by the Swiss Youth+Sports (Y+S) programme, plays an important role in counteracting this trend. Children who participate in this programme are much more likely to maintain an active lifestyle as they get older.

Symposium on Defining the Noma Research Agenda The symposium brought together around 100 scientists, public health experts, politicians, health advocates as well as noma survivors. The aim of the symposium was to join forces against noma – a severe and rapidly progressing condition primarily affecting children living in extreme poverty – and define a common research agenda. The key outcomes of the symposium were published in PLoS Neglected Tropical Diseases


→ Non-communicable diseases are a growing burden in rural areas and CDCI plays an important role in tackling them.
Increase in Northern Kenya A study by researchers from Swiss TPH and the Kenya Medical Research Institute (KEMRI) revealed how climate change, socio-economic changes such as urbanisation and malaria control efforts are influencing the spread of malaria in Kenya. Using advanced geostatistical modelling, the study found that despite a decline in malaria overall, there was a significant rise in malaria risk in some regions. The findings highlight the need for adaptable public health strategies amid climate change.

New Swiss TPH Diversity, Equity and Inclusion (DEI) Policy Swiss TPH introduced a DEI Policy to strengthen inclusion, accountability and fairness. It reinforces the zero-tolerance stance on discrimination and integrates DEI into research, education and services. The policy applies to leadership as well as our partnerships to actively cultivate DEI.
20 Years of Pioneering HIV
ease
in Rural Tanzania The Chronic Diseases Clinic of Ifakara (CDCI) celebrated its 20th anniversary, marking two decades of providing healthcare, health training and clinical research in rural Tanzania. Established through a collaboration between Swiss and Tanzanian institutions to support individuals living with HIV/ AIDS, CDCI has evolved into a leading model for HIV care in rural Africa and a major training platform.

Towards a Post-Donation Era in Parasitic Worm
Control Over the past 25 years, huge progress has been made in the prevention, control and elimination of parasitic worm infections, which affect more than a billion people worldwide. Mass drug administration mainly targeting school-aged children, facilitated by public-private partnerships and donations of billions of deworming drugs by pharmaceutical companies, played a key role. However, with declining infection rates and pharmaceutical companies considering an end to the large-scale drug donations, it is time to reflect on a “post-donation era”.

Children Will Experience Four Times More Extreme Events Due to Climate Change Swiss TPH researchers and partners published a report that shows that children born in Europe in 2020 will experience four times more extreme events, especially heatwaves, due to climate change compared to children born in the 1960s. The systematic review, conducted on behalf of the European Environment Agency, underscores the urgent need for child-focused health measures.

→ Mothers with young children in Zambia often have little access to mental health support due to staff shortages and lack of resources.
R. Geigy Award 2024: Cutting-Edge Research to Control Communicable and Non-Communicable Diseases in Côte d’Ivoire The 13th R. Geigy Award, endowed with CHF 20,000, went to scientists from the CSRS. Siaka Koné is being recognised for his work on long-term cohorts and demographic and health surveillance systems in rural Côte d’Ivoire. Julien Zahouli, Emmanuelle Lisro, Laurence Yao and Marc Adou were rewarded for their work on the validation of the effect of insecticides on disease vectors.


Nearly half of schools in European cities are in urban heat islands, where temperatures are at least 2 °C higher than regional averages.
New Intervention Significantly Improved Mental Health Well-Being for Zambian Mothers A study by Swiss TPH and partners has shown that a new, locally adapted mental health intervention for women with young children in Zambia led to a 50% reduction in symptoms. The intervention also empowered the women, resulting in a positive impact on the relationship with their children and their economic situation. Published in The Lancet Psychiatry, the findings highlight an important step towards improving maternal mental health in sub-Saharan Africa.

award
Symposium on Women and Gender in Global Health The symposium brought together around 160 experts from academia, public administration, international organisations and the private sector. The aim of the symposium was to share insights and develop innovative solutions to improve the health and well-being of women and girls around the globe.

→ Financial support increases the chance of mothers continuing breastfeeding.
A Tropical Disease in Switzerland: Call for Coordinated Action on Chagas Disease In collaboration with WHO and other partners, Swiss TPH researchers conducted a comprehensive review of Chagas disease in Switzerland. Although typically found in Latin America, Chagas disease affects between 2,000 and 4,000 people in Switzerland. The review, published in Swiss Medical Weekly, underscores the need for improved screening and healthcare strategies to eliminate Chagas disease in Switzerland.
Financial Support Significantly Improves Breastfeeding Success in Lao PDR A Swiss TPH study published in JAMA Pediatrics found that financial support significantly increases exclusive breastfeeding rates amongst new mothers in Lao PDR. These findings highlight the potential of cash transfers to improve maternal and child health by promoting WHO’s recommendations for exclusive breastfeeding for the first six months of an infant’s life.

→ Integrating Chagas screening into antenatal and paediatric care for early detection and prevention of mother-to-child transmission is a priority.

“I measure exposure to 5G and electromagnetic fields (EMF) on the Swiss TPH rooftop and by hiking to various places across Switzerland – from city centres to nature areas. My research helps to better understand this complex and sometimes controversial exposure and to inform the population about their typical EMF exposure.”
Timely and accurate diagnosis of childhood illnesses can mean the difference between life and death. Yet in many low-resource settings, frontline health workers struggle with overwhelming patient loads, limited training and inadequate infrastructure. As a result, millions of preventable child deaths occur each year. To tackle this issue, Swiss TPH is developing practical digital tools to support primary care and improve child health.
In 2022 alone, 4.9 million children under the age of five died according to the World Health Organization (WHO), mainly from treatable conditions such as pneumonia, diarrhoea, and malaria. Over 80% of these deaths occurred in sub-Saharan Africa and South Asia, where access to quality healthcare remains limited. The challenge is not so much the availability of treatments but ensuring they reach those who need them most. To achieve this, healthcare professionals must be able to make accurate diagnoses and competent treatment decisions. Inadequate diagnosis can lead to serious illness or death, while over-diagnosis contributes to antibiotic overuse and antimicrobial resistance.
This is where clinical decision support systems (CDSS) come in. CDSS are digital tools that support medical staff in diagnosing and treating children according to evidence-based guidelines. By integrating patient data with medical protocols, CDSS improve diagnostic accuracy, optimise treatment, reduce unnecessary antibiotic use, and generate valuable data for health system planning. Designed for primary care, CDSS enhance – rather than replace – clinical judgement, keeping healthcare providers central to decision making while improving the overall care quality.
Digital tools for smarter care
Swiss TPH is a pioneer in CDSS development, driving key initiatives to improve child health. As a co-founder of the CDSS Community of Practice, we develop open source solutions, support WHO’s SMART guidelines (standardised, machine-readable clinical protocols) and provide training in digital health and CDSS use.
One of our key projects is ALMANACH (ALgorithm for the MANagement of CHildhood Illness), developed by Swiss TPH over 15 years ago to guide health workers step-by-step through the WHO guidelines for Integrated Management of Childhood Illness (IMCI) in primary healthcare. Continuously updated and enhanced, ALMANACH integrates new recommendations and can be adapted to country-specific needs. In collaboration with the International Committee of the Red Cross (ICRC) and local health authorities, it has been piloted in Afghanistan and implemented in Nigeria, Somalia, and most recently Libya
The results are promising: in Somalia, a study showed that antibiotic prescribing fell from 58.1% to just 16%, with a 30-fold reduction for upper respiratory tract infections, while adherence to IMCI guidelines increased significantly.

Effectiveness evaluation in Nigeria showed that children seeking care in ALMANACH-facilities had a significantly higher rate of (caregiver-reported) recovery within a week of treatment and profited from improved quality of care, such as more accurate antibiotic prescription or better communication. In Libya, the tool is now being scaled up and handed over to the Ministry of Health, where it can once again demonstrate its impact and deliver its contribution to universal health coverage.
Another impactful project working on transforming paediatric care is the Tools for Integrated Management of Childhood Illness (TIMCI) project, led by PATH. It’s aim is to improve the detection a nd treatment of severe illness by integrating pulse oximetry and digital clinical decision support algorithms into primary healthcare. Pulse oximetry is a low-cost, non-invasive method for detecting hypoxaemia (low oxygen levels in the blood). The condition is strongly linked to child morbidity and mortality but often
goes undetected in low-resource settings due to a lack of diagnostic tools. TIMCI worked in Kenya, Senegal, Tanzania and India, equipping health workers with pulse oximeters to enable more accurate diagnoses and timely referrals. Swiss TPH is leading a large-scale impact study to evaluate the project’s effectiveness, cost-effectiveness and scalability. The results will help shape policy for integrating these life-saving tools into health systems worldwide.
Another major initiative is the DYNAMIC study, a digital health project led by Unisanté and Swiss TPH, focused on improving child healthcare and promoting responsible antibiotic use in Tanzania and Rwanda. It combines ePOCT+, a smart clinical decision support algorithm, with rapid diagnostic tests to help health workers make accurate diagnoses and follow treatment guidelines. Studies in health facilities using ePOCT+ have shown a major drop in antibiotic prescriptions – from 70.1% to 23.2% in Tanzania and from 70.5% to 24.5% in Rwanda – without affecting

→ Clinical decision support systems guide health personnel step-by-step through a consultation on a tablet.
cure rates. Originally developed for countries in the Global South, the solution is now being adopted in the Swiss canton of Vaud through a reverse innovation approach. Swiss TPH is also working to extend the software’s functionality and build an open source community by coordinating multiple contributing organi sations.
Three approaches, one goal
ALMANACH, TIMCI and DYNAMIC all enhance child healthcare through digital clinical decision support. A key benefit of these projects is their ability to generate real-time data, enhancing clinical decision-making and enabling continuous refinement of the tools. This constant flow of information supports healthcare providers in delivering timely and accurate care while simultaneously driving continuous improvements of the tools making the CDSS smarter over time and further improving healthcare delivery.
Despite their transformative potential, CDSS are not a one-size-fits-all solution. Infrastructure limitations, maintenance costs, and the need for continuous workforce training pose challenges. Ensuring interoperability with existing health systems and user acceptance is crucial for long-term adoption. While CDSS assist in decision-making, they do not replace clinical judgement – health personnel must have the skills and confidence to interpret data and make informed choices. Strong partnerships, training
and support, as well as sustained investment can help overcome these barriers, ensuring broader impact and ultimately contribute to improving survival rates for millions of children worldwide.
Swiss TPH is driving digital innovation to improve health outcomes around the world. From openIMIS – an open-source platform advancing social health protection – to SysRef, which enhanced refugee health management in Chad through digital clinical decision support, our projects are transforming health systems through smart, practical technologies. IMCI-PLUS uses AI-powered ultrasound to support paediatric respiratory care, TB Triage+ combines AI and pointof-care diagnostics to improve tuberculosis screening in remote communities, and DigitalECD evaluates virtual tools to promote early childhood development in Peru.
Malaria remains a major health problem, especially in sub-Saharan Africa. In 2023, the WHO reported 263 million cases and 597,000 deaths in 83 countries, mostly among young children. Swiss TPH conducts research, tests treatments and supports countries in applying and monitoring malaria control measures to improve prevention, treatment and efforts to eliminate malaria. Join us in looking back at some milestones we achieved with our partners in 2024.
Understanding how the parasite that causes malaria works, is an important piece of the puzzle in tackling the disease. There are five Plasmodium parasite species that cause malaria in humans. P. falciparum is the deadliest malaria parasite and the most prevalent on the African continent. All clinical symptoms of malaria are caused by the multiplication of malaria parasites in the red blood cells. The most common early symptoms of malaria are fever, headache and chills, while symptoms of severe malaria include fatigue, confusion, seizures, and difficulty breathing.
Key component found for malaria invasion
P. falciparum invades human red blood cells, but the precise details of the targets that the parasite binds to has not been known until recently. Although we knew that the malaria protein cysteinrich protective antigen (Pf CyRPA) is essential for the invasion of red blood cells, its precise role in this process was not understood.
Findings by a multidisciplinary, collaborative research team from six institutions, led by Swiss TPH and the Institute for Glycomics in Australia, have provided new insights into how P. falciparum invades red blood cells. Published in Cell Reports, the study revealed that the parasite protein PfCyRPA binds specifically to a glycan structure containing sialic acid on the red blood cell surface – a key step in the invasion process. This
discovery not only improves understanding of host-pathogen interactions but also supports the continued development of Pf CyRPA as a potential blood-stage malaria vaccine component and as target for novel antimalarial drugs. As the emergence of drug resistance in malaria parasites is a threat to malaria control programmes, new antimalarial drugs are urgently needed.
Closing treatment gaps for the most vulnerable
Early diagnosis and treatment of malaria reduces disease, prevents deaths and contributes to reducing transmission. Malaria is a serious infection and always requires treatment with medicine. Several antimalarial treatments exist and doctors chose the appropriate therapy based on the type of malaria, drug resistance, weight or age of the patient and whether a person is pregnant. Artemisinin-based combination therapy medicines are the most effective treatment for P. falciparum malaria.
However, current antimalarials have not been developed specifically for infants weighing under 5 kg. There is no approved treatment available for them, and they are treated with tablets meant for children above 5 kg adjusted by weight. Yet, these tiny patients handle drugs differently due to the immaturity of their metabolising organs, which can lead to overdose and toxicity. To

help fill this gap, Swiss TPH supported the CALINA study, which is led by Novartis with support from Medicines for Malaria Venture (MMV). The study evaluated a new formulation of Coartem® (artemether-lumefantrine) designed for babies weighing less than 5 kg in a clinical trial in several African countries. Swiss TPH was in charge of carrying out the study in the Democratic Republic of the Congo. Setting up study sites in challenging environments in low- and middle-income countries to test drugs for poverty-related diseases is something Swiss TPH has been doing for over 20 years in partnership with different organisations and countries.
The new formulation provides optimised dosing specifically tailored to the needs of these vulnerable patients. The results showed good efficacy and safety, with pharmacokinetic profiles suitable for this age and weight group. If approved, the treatment will close a significant treatment gap.
These two examples show how Swiss TPH is working along the entire value chain - from basic research on malaria parasites to the validation of new drugs in clinical research. We also work with partners to put new knowledge and tools into practice. For example, large-scale implementation studies in endemic countries provide critical evidence to support decision-makers worldwide in the fight against malaria.
In total, more than 200 researchers work on malaria at Swiss TPH. They are involved in the development of new diagnostics, treatments and vaccines as well as vector control strategies. As a WHO Collaborating Centre and a member of the Swiss Malaria Group, Swiss TPH plays a vital role in advancing innovative strategies for malaria elimination.

Climate change is no longer a future threat – it’s a present-day health crisis. Rising temperatures, shifting weather patterns, and increasing air pollution are already affecting how and where people live, work, and stay healthy. While no one is immune, vulnerable populations – especially those with limited access to healthcare and fewer resources to adapt – are most at risk. By 2050, an estimated six billion people will be at risk of climate-related diseases such as malaria and schistosomiasis.
At Swiss TPH, the connection between environment and health has long been part of our work. But with the growing urgency of climate-related health risks, we’ve made it a strategic priority for the years ahead.
Our researchers are asking urgent questions – and answering them with science, data, and collaboration. How do extreme temperatures impact healthcare systems? How can we track pesticide exposure in farming communities? What role can urban green spaces play in preventing disease? How are climate patterns shifting disease risks across regions?
The answers lie not only in the evidence – but in the people behind it.
Across departments and disciplines, Swiss TPH researchers are working to understand and tackle the complex links between a warming planet and human health. From environmental epidemiologists and mathematical modellers to experts in vectorborne diseases, urban planning and pesticide exposure, they are translating science into action.
Their work is grounded in collaboration – across sectors, borders and communities – because the solutions we need are as interconnected as the challenges we face. By generating policy-relevant evidence, co-developing interventions with partners, and empowering the next generation of scientists, they are not only responding to today’s crisis, but helping shape a healthier, more just and climate-resilient tomorrow.

What motivates you to work on climate change and health?
“
From a professional standpoint, working in urban public health offers many opportunities to engage in interdisciplinary and cross-sector collaborations, driving science into real-world impact, which is something I am passionate about. On a personal level, I am fully aware that those of us living in wealthy countries bear the greatest responsibility for the climate crisis. This awareness drives me to actively contribute to urgent solutions that protect and promote health and well-being in the face of global climate change. ”
Mirko Winkler is Head of the Urban Public Health unit at Swiss TPH. His research focuses on the interaction between environmental change, social change, sustainable development and public health.
Why is it important that we research climate change and health?
“ My research focuses on environmental exposures like air pollution, pollen, and urban green spaces – factors that are all interconnected. Trees and green areas are important to cool our cities and provide shade, but smart planning is essential so that we get to enjoy co-benefits like increased biodiversity, lower air pollution and more opportunities for physical activity, while avoiding highly allergenic pollen. Investing in climate-resilient public spaces and making it easier for people to walk, cycle, or use public transport are great forms of health prevention. If we do it right, the health benefits are bigger and more equitable than any treatment you can get at a doctor’s office. ”

What motivates you to work on climate change and health?
“ I really enjoy the scientific challenge and working with “big data”, but I’m also driven by my ethical concerns about the future we’re building for the next generations. Framing climate change through the lens of human health makes it more relatable for people and politicians – and the co-benefits of climate action have a huge potential to cascade into sustainability and nature protection. As societies increasingly experience the effects of climate change and start to understand the risks, this awareness can shape political priorities, scientific research and technological development – which I find very motivating. ”

Marloes Eeftens leads the Sensoring and Environmental Epidemiology group at Swiss TPH. Her research explores how environmental exposures affect human health.
Alonso Bussalleu is a PhD student in the Environmental Exposures and Health unit at Swiss TPH. His research focuses on modelling high-resolution daily temperature across Europe.
What is the biggest challenge in addressing climaterelated health risks today?
“ As a public health institute, we have to ask ourselves: how can climate and health research lead to real change? I strongly believe our greatest impact is through policy-relevant data, such as informing urban planners on how to design healthier cities. With the evidence we produce, coupled with strong science communication, we can support people shifting towards more sustainable life styles. Working closely with study participants through cohort studies brings us closer to this goal – and gives me hope for a healthier, more sustainable future. ”

Nicole Probst-Hensch is Head of the Department of Epidemiology and Public Health at Swiss TPH. Her research focuses on chronic diseases, with expertise in environmental and molecular epidemiology, cohort studies, and exposome science.

What gives you hope for the future?
“ There is growing awareness of the health risks posed by extreme heat and the urgent need for action. Initiatives are emerging to address these risks, but the pace of implementing adaptation and mitigation measures is still too slow. Rather than relying on hope alone, I believe we must find a way to drive change by working across disciplines and with stakeholders to build shared understanding, shape common visions, and co-develop solutions that protect health, reduce inequalities, and respond to one of the most pressing challenges of our time. ”

Martina Ragettli is project leader in the Environmental Exposures and Health unit. Her current research focuses on the health impacts of climate-related environmental exposures such as heat, air pollution or green space and policy-relevant ways to minimise them.

What is your research about, and how does it relate to climate change and health?
“ Rising temperatures may increase pest infestations and lead to greater pesticide use, increasing exposure risks for farm workers, their children, and nearby communities. My research focuses specifically on how pesticide exposure factors including both behavioural and environmental affect the reproductive health of children. By understanding the pathways and impacts of the pesticide exposure, we can better address environmental health risks that are indirectly fuelled by climate change. ”
Regina Molomo is a PhD student in the Chronic Disease Epidemiology unit. Her research focuses on pesticide exposure among children and adolescents in South Africa.
What gives you hope for the future?
“ Despite the challenges – like misinformation, siloed efforts, and declining funding – there is hope. Communities are becoming more aware of the health impacts posed by climate change, and governments are increasingly introducing climaterelated policies. When we combine indigenous knowledge with government actions, we can create climate-resilient health systems. The growing number of young researchers, greater public engagement, and a shift in global conversations highlighting climate change as a health issue give me confidence that together, we’re moving in the right direction. ”
Bryan Nyawanda is a post-doctoral scientific collaborator in the Biostatistics unit at Swiss TPH. His interests are in Bayesian and frequentist statistics, machine learning, epidemiology and disease modelling.
What gives you hope for the future?
“ Climate change is shifting mosquito habitats and expanding the risk of disease to new regions – but what gives me hope is the steady progress in research, innovation, and collaboration. Advances in mosquito control strategies, such as genetic modification, improved insecticides, and biological control methods, are providing new tools to combat vector-borne diseases more effectively. Many mosquitoborne diseases are preventable, and with ongoing scientific advancements and continued global commitment, I believe we can reduce their burden and improve global health. ”

Tobias Suter leads the Arthropod Testing Facility at Swiss TPH. His research focuses on evaluating tools and strategies to control disease-transmitting mosquitoes.

“I manage and monitor health projects funded by the Global Fund in Senegal and São Tomé and Príncipe, with a focus on building efficient and equitable health systems. I appreciate being part of such an international environment and contributing to countries’ efforts to achieve their goals.”
For more than 80 years, Swiss TPH has been developing and implementing its activities through a strong network of partnerships around the world. Guided by our three strategic goals – excellence in science, taking science to impact, and mutual learning for sustainable development – we remain committed to improving health and well-being through a unique combination of research, education and services.

We generate knowledge on diseases and health systems and develop novel diagnostics, drugs and vaccines as well as new approaches and tools.

We integrate new treatments and approaches into policy and health systems to improve care and public health locally, nationally and globally.
Our vision is to make the world a healthier place. We achieve this by continuously assessing the impact of our work, reporting on progress within our strategic goals and topics, and demonstrating our contribution to the Sustainable Development Goals (SDGs).
In our new strategy 2025 – 2028, we have streamlined our strategic topics from eight to five, re -

We share knowledge and practical expertise with partners, students, professionals, beneficiaries, organisations and society.
flecting our commitment to excellence and impact. By sharpening our focus, we strengthen interdisciplinary collaboration, enhance synergies and ensure that our research and partnerships drive meaningful change. This refined approach allows us to align even more closely with key emerging issues in global health and development cooperation priorities, maximising the reach and relevance of our work.
Global health is at a crossroads, and our new strategic topics (STOs) reflect the challenges of today and tomorrow. Climate change is reshaping disease patterns and threatening health worldwide. Infectious diseases – both old and emerging – demand renewed attention in the face of impending pandemics and antimicrobial resistance. According to the World Health Organization, non-communicable diseases (NCDs) now account for 74% of global deaths, requiring ur-
gent prevention and control measures, particularly in the context of a growing double burden of disease. At the same time, increasing health inequities call for stronger engagement with societal and cultural factors to achieve universal health coverage. To drive sustainable impact, we focus on strengthening health systems and promoting evidence-informed policies that translate science into real-world solutions.
We excel in transdisciplinary and action-oriented research at the nexus of climate change, environment and health to address increasing global health challenges.
We tackle infectious diseases through innovative research, sustainable solutions and global collaboration, addressing challenges such as antimicrobial resistance, emerging pathogens and diseases.
We improve the prevention and control of NCDs through innovative, affordable, sustainable and efficient approaches that are adapted to local contexts and promote social equity.
We foster health equity by engaging communities, civil society and citizens in research and implementation, addressing social determinants and developing inclusive, contextspecific health solutions.
We strengthen health systems and promote health by engaging communities, health workers and policy-makers to ensure inclusive, evidencebased and sustainable health interventions for all.


“Diagnostics play a crucial role in health systems –they guide how we diagnose, treat and prevent diseases. Having worked at Swiss TPH for nearly 20 years, I’ve seen how vital fast and accurate diagnostics are, especially for infectious diseases like malaria. In a world facing a rise in infectious diseases, our work has never been more important.”
Directorate
Directorate
Prof. Dr. Jürg Utzinger Director
Prof. Dr. Kaspar Wyss Deputy Director (until 28 February 2025)
Mathias Kronig Administrative Director
Additional Members of the Managing Board
Prof. Dr. Julia Bohlius
Prof. Dr. Sébastien Gagneux
Prof. Dr. Daniel Paris
Prof. Dr. Nicole ProbstHensch
Dr. Helen Prytherch (a.i. from 1 March to 15 June 2025)
Dr. Alexander Schulze (as of 16 June 2025)
Dr. Eva Herzog
President of the Board of Governors, Member of the Swiss Council of States
Dr. Rolf Borner Director, Infrastructure and Operations, University of Basel
Dr. Ariane Bürgin
Head of Higher Education, Cantonal Department of Education, Basel
Prof. Dr. François Chappuis
Head of Tropical and Humanitarian Medicine Division, Geneva University Hospitals
Prof. Dr. Sabina De Geest
Institute of Nursing Science, University of Basel
Prof. Dr. Jacques Fellay (as of 1 January 2025) Head of Research Laboratory “Human Genomics of Infection and Immunity”, EPFL, Lausanne
Dr. Alban Frei
Head of Higher Education, Directorate of Education, Culture and Sport, Canton of Basel-Landschaft
Dr. Lutz Hegemann
President, Global Health and Swiss Country Affairs, Novartis
Dr. Olivier Küttel (until 31 December 2024) Former Head, International Affairs, EPFL, Lausanne
Dr. Cornelia Staehelin (until 31 December 2024) Senior Physician, University Hospital Bern
Dr. Barbara Wieland (as of 1 January 2025) Director, Federal Institute of Virology and Immunology, Bern
Dr. Deborah Studer (as of 1 January 2025) Observer, Scientific Advisor, National Research, State Secretariat for Education, Research and Innovation, Bern
Dr. Luca Tratschin (until 31 December 2024) Observer, Deputy Head, National Research, State Secretariat for Education, Research and Innovation, Bern
Prof. Dr. Jürg Utzinger Director, Swiss TPH (ex officio)
Mathias Kronig Administrative Director, Swiss TPH (ex officio)
R. Geigy Foundation: Foundation Board and Administration
Prof. Dr. Jürg Utzinger President of Foundation Board, Director, Swiss TPH
Prof. Dr. Christoph B. Bühler
Vice-President of Foundation Board, Lawyer, LL.M., Honorary Professor, University of Zurich
Beat Berger Foundation Board Member, Managing Director, Berger Liegenschaften
Stefan Mörgeli Foundation Board Member, Administrative Director emeritus, Swiss TPH
Prof. Dr. Nicole ProbstHensch Foundation Board Member, Head Department of Epidemiology and Public Health, Swiss TPH
Daniel O.A. Rüedi Foundation Board Member, CEO Baumann & Cie., Banquiers, Basel
Jürg Toffol
Foundation Board Member, Senior Associate Partner Itten+Brechbühl AG
Dr. Lukas Meier
Managing Director
Prof. Dr. Marcel Tanner Honorary President, Director emeritus, Swiss TPH
The Department of Medical Parasitology and Infection Biology (MPI) investigates the biology and transmission of pathogens and the host immune responses to infection. Findings from this research inform the development of new diagnostics, treatments and vaccines against infectious diseases that affect the world’s most vulnerable populations.

Sébastien Gagneux, Head of MPI

MPI is comprised of 11 research groups focusing on various parasitic, bacterial, and viral diseases, including malaria, tuberculosis (TB) and neglected tropical diseases (NTDs) such as schistosomiasis and Chagas and emerging viral diseases such as COVID-19. The aim of our work is to better understand the biology, host-pathogen interaction and transmission of these diseases, as well as how the human immune system responds to infections by these diverse pathogens. We use this information to develop new methods to prevent, diagnose and treat these diseases. We are also studying why and how these different pathogens develop resistance to old and new antimicrobials. This knowledge will help extend the lifetime of existing drugs and support the development of new ones. All this work is done in close collaboration with our long-term partner institutions based in areas where these infectious diseases remain a major public health concern.
Highlights for 2024 include the discovery by Pascal Mäser’s group of the bacterial metabolite venturicidin A as a highly selective agent
against Leishmania and Trypanosoma parasites. They showed how this compound attacks the single mitochondrion of these parasites in a manner consistent with inhibition of the ATP synthase (published in Antimicrobial Agents & Chemotherapy). In another exciting development related to clinical drug development, Jennifer Keiser’s team confirmed the efficacy and safety of emodepside for the treatment of Trichuris trichiura and hookworm infections in a clinical trial conducted on Pemba Island, Tanzania (published in The Lancet).
In the context of developing new malaria vaccines, Claudia Daubenberger’s group, together with our long-term partner, the Ifakara Health Institute (IHI), was able to show that co-infection with HIV does not impair the human immune response to PfSPZ, one of the leading malaria vaccine candidates (published in EBioMedicine). Sébastien Gagneux’s group, in collaboration with IHI and Tanja Stadler’s group at ETH Zurich, found that TB patients co-infected with HIV were less likely to transmit their TB bacteria than HIV-uninfected TB patients (published in PLoS Pathogens). Further work on TB in Damien Portevin’s group showed that the response of human
macrophages to TB infection differs depending on the bacterial strain infecting these macrophages (published in Scientific Report).
The year ended with Emma Hodcroft, who leads the Epidemiology and Viral Evolution group at MPI and co-founded Pathoplexus, being named in Nature ’s prestigious “Who to Watch in 2025” list, which highlights scientists who are making a significant impact in their fields. This recognition underlines the importance of creating open, communitydriven solutions for virus sequence sharing and outbreak monitoring. The feature has helped raise the profile of open data, open science and Pathoplexus.
Daniela Brites received her venia docendi from the University of Basel. She works as a senior bioinformatician and project leader in the TB Ecology and Evolution unit.
Jennifer Keiser has been appointed Full Professor at the Faculty of Science at the University of Basel as of 1 February 2025.
The Department of Epidemiology and Public Health (EPH) investigates distribution and causes of infections and non-communicable diseases. To understand and promote the well-being of people in different cultural, environmental, and political contexts, EPH applies various methods ranging from anthropology and social science to biostatistics and mathematical modelling as well as observational cohorts with biobanks and intervention studies.
In 2024, EPH had a total of 196 projects. With 178 employees and 124 PhD students, EPH is the largest Department at Swiss TPH with 10 units.
Projects and research highlights in 2024
The MEZA project, funded by the Gates Foundation, supports malaria elimination in Zanzibar through targeted, evidence-based interventions. Additionally, a five-year Swiss Government grant ensures continued malaria programme support in Tanzania and Zan zibar, fostering synergies with other initiatives. A key milestone was the December 2024 dissemination meeting in Dar es Salaam, where findings from a Tanga Region larviciding operation were shared. This government-led effort provided valuable insights into feasibility, cost, and impact, though effectiveness varied by transmission intensity.
Traffic noise and air pollution are closely linked environmental risk factors that contribute significantly to the development of diseases such as diabetes, hypertension and atherosclerosis. MARKOPOLO, a new EU project, seeks to provide new insights into the effects of environmental factors on the human body, improving risk assessment and evaluating the effectiveness of preventive strategies. By exploring societal and political contexts, the researchers aim to deepen understanding of the complex interplay between noise, air pollution and human well-being. The findings are expected to support the development of new guidelines.
The SAPALDIA cohort study, which has been running for over 30 years, and the biobank infrastructure of Swiss TPH have received the NORMA certification label from the Swiss Biobanking Platform. This confirms the decades of experience in setting up and running long-term studies at Swiss TPH. The SAPALDIA cohort and biobank have been contributing to our understanding of the health effects of a wide range of environmental factors – the exposome – for decades, thereby informing environmental policy and urban plan ning. In
the context of the Horizon 2020 exposome project EXPANSE, SAPALDIA contributes with blood from diabetes and chronic obstructive pulmonary disease (COPD) case-control samples and stored for over 20 years in its biobank to understand the biological mechanisms by which exposure mixtures consisting of air pollution, greenspace, ambient temperature or transportation noise affect cardio-metabolic and respiratory diseases.
From science to policy
Human, animal and environmental health are closely linked in what is known as the “One Health” approach. Swiss TPH scientists have substantially contributed to an evidence review report, requested by the European Commission. The report provides evidence-based options for policy on the operationalisation of “One Health” in the European Union.
Local and global partnerships
Dengue is on the rise globally. In Abidjan, Côte d’Ivoire, Swiss TPH in collaboration with the Centre Suisse de Recherches Scientifiques en Côte d’Ivoire (CSRS) has completed a cluster-randomised trial to evaluate the efficacy of larval source management strategies that were co-developed with the local communities alongside mass trapping to reduce the risk of dengue transmission. While the risk for autochthonous dengue transmission is still low in Switzerland, Swiss TPH is

Nicole ProbstHensch, Head of EPH
working together with federal and cantonal administrations to develop action plans for mitigating the risk of dengue in Switzerland, including the surveillance and control of the Asian tiger mosquito.
Swiss TPH established a new collaboration with the International Center for Theoretical Physics (ICTP) in Trieste to advance malaria modelling. By combining ICTP’s climate-focused VECTRI model with Swiss TPH’s intervention-focused OpenMalaria model, the aim is to integrate epidemiological and climate science expertise to enhance malaria prediction and control strategies.
Organisational changes and promotions
Sonja Merten, Head of the Society, Gender and Health unit was appointed Adjunct Professor for social and preventive medicine at the Faculty of Medicine of the University of Basel. Sarah Moore, Head of the New Vector Control Interventions group was appointed Adjunct Professor for epidemiology at the Faculty of Science of the University of Basel. Rea Tschopp received her venia docendi from the University of Basel. Nakul Chitnis was appointed Head of the Disease Modelling unit.

The Swiss Centre for International Health (SCIH) provides consultancy, project design and conception, as well as project and grant management services. With multidisciplinary teams in Switzerland and around the world, SCIH offers a broad range of expertise including strategic reviews, project implementation, policy advice and implementation research.

SCIH strengthens health systems and improves access to health services in low- and middle-income countries in Africa, the Balkans and Eastern Europe, as well as in Switzerland. Special attention is given to gender, equity and inclusion of marginalised and vulnerable groups. SCIH has expertise in a broad range of topics along the interface of infectious and non-communicable diseases (NCDs), including primary healthcare development, health workforce strengthening, health financing, health information systems, programme performance monitoring, supply chain management and digital health.
Several long-term projects have strengthened primary and secondary healthcare systems and improved the quality and accessibility of services: The Healthy Life project in Moldova, for instance, showed strong results at the nexus between development cooperation and humanitarian assistance and was able to improve capacities of family doctors and nurses in NCD control and reinforce primary care provision to vulnerable communities. This led to the extension of the project for another four years and will allow to further fostering of NCD prevention and quality of care. In Kosovo, the Accessible Quality Healthcare project has continued to assist the Ministry of Health and municipalities in rolling out quality improvement in primary care across the country, for example through the use of clinical guidelines and protocols. In Chad, the “Programme d’Appui au Développement Sanitaire”, funded by the Swiss Agency for Development and Cooperation (SDC), has allowed for the building up of the health infrastructure and has contributed to the conception and implementation of the Universal Health Coverage (UHC)
scheme, as well as to quality of care improvements in two regions.
Led by Pact, Swiss TPH continued to assist the Ukrainian government in developing surveillance, response, and other critical public health capacities. Simultaneously, we continue the Swiss Medical Education Development project, which improves undergraduate, postgraduate, and ongoing professional education while strengthening the skills of primary care workers.
A significant number of people and families across various countries, including Cameroon, Chad, Rwanda, Somalia, Albania, Kosovo and Moldova, experienced enhanced healthcare services, expanded access to medical care, and greater community involvement. These improvements were realised through diverse approaches, such as capacity strengthening measures for health workforce development, reinforcing health literacy among target groups, advancing health insurance programmes, and implementing digital insurance solutions like openIMIS. openIMIS is an opensource health insurance management system that enhances efficiency, transparency and accessibility in healthcare financing. Additionally, Swiss TPH facilitates the integration of electronic clinical decision support systems that support healthcare professionals in making informed, evidence-based decisions in patient assessment and treatment. Throughout our efforts, we remain dedicated to supporting the realisation of the Sustainable Development Goals and advancing progress toward UHC.
Implementation science is used to integrate research findings into real-world practice, im-

Kaspar Wyss, Head of SCIH
(until 28 February 2025)
proving healthcare policies, programmes, and interventions for greater effectiveness, sustainability and impact. Together with the Basel Centre for Health Economics, we initiated the formative and outcome evaluation of a large integrated health service model, the “Réseau de l’Arc” in the Jura region of Switzerland.
The Pediatric Praziquantel Consortium achieved the inclusion of the new praziquantel formulation for the treatment of schistosomiasis among children aged three months to six years in the World Health Organization list of prequalified medicines. SCIH is currently assisting with the introduction of the drug into control programmes in several African countries. New projects to demonstrate the feasibility of accelerated leprosy transmission interruption in Tanzania and to achieve Schistosoma mekongi transmission interruption in Cambodia and Lao PDR have also been initiated.
Services to Global Fund and Gavi
SCIH remains actively engaged as a Local Fund Agent for the Global Fund, overseeing the execution of programmes aimed at combating HIV/AIDS, tuberculosis and malaria, while also supporting the strengthening of health systems. With 13 portfolios spanning 16 countries – primarily across Africa, as well as the Middle East –, SCIH plays a key role in ensuring effective programme delivery. Additionally, as a quality assurance service provider, SCIH has carried out health facility assessments, evaluations of care quality and independent data accuracy and quality assessments in both Burkina Faso and Chad.
Gavi, the Vaccine Alliance, entrusted SCIH with an evidence review on the diphtheria, tetanus and pertussis booster vaccination. Similarly, a literature review on the integrated bite case management implementation and post-exposure prophylaxis of rabies was successfully completed to inform policy. This has resulted in a new assignment researching community engagement strategies that demonstrate positive impact on rabies post-exposure prophylaxis as well as implementation strategies for its integration into routine vaccination programmes.
The Department of Medicine (MED) conducts clinical research on drugs, diagnostics and vaccines with a focus on tropical and poverty-related diseases. Major pillars are the National Diagnostic Reference Centre and a growing platform for clinical translational research involving projects in academia and industry.

Strengthening collaborations with the pharmaceutical industry
The Clinical Operations unit and the Genotyping group support industry trials like the Novartis-MMV-EDCTP CALINA study in DRC, the first high-impact antimalarial for neonates under 5 kg, and the Novartis KALUMA study, managing trials in DRC and analysing samples. The Genotyping group serves as a central laboratory for over ten African countries.
The Medicine Development unit has started a new partnership with Merck, involving genotyping samples from an ongoing phase II malaria study.
After successful phase II trials of emodepside against Trichuris trichiura and hookworm, Swiss TPH and Bayer partnered to advance the drug for approval. An interdisciplinary Swiss TPH team is now setting up two pivotal regulatory phase III trials in the Philippines and Tanzania, with Swiss TPH as sponsor.
Research highlights in 2024
The Clinical Research unit coordinated transnational tuberculosis (TB) projects; namely DRTB-HDT and TB TRIAGE+. TB TRIAGE+ recruited over 20,000 participants for the main active case-finding trial and published several scientific articles, including an evaluation of C-reactive protein and AI-assisted chest X-ray for TB triage in Southern Africa.
The Medicines Development unit is developing a malaria mRNA vaccine candidate based on the highly conserved Plasmodium falcipar-
um blood-stage antigen CyRPA as a lipid nanoparticle formulation, and a Buruli ulcer toxoid vaccine candidate with substantial toxin-neutralising activity. Both have shown promising results in mouse infection models and are now approaching clinical development.
The Genotyping group secured major grants and presented their research at the Multilateral Initiative on Malaria (MIM) conference in Rwanda, the Genomic Epidemiology of Malaria conference in the UK and the annual meeting of the American Society of Tropical Medicine and Hygiene in the US, with findings published in the Lancet Microbe and Scientific Reports. Malaria genomic surveillance activities are ongoing in Tanzania, Ghana and Rwanda.
The Ifakara Clinic Platform in Tanzania has advanced use and training of medical imaging diagnostics for non-communicable diseases (NCDs). Key publications cover point-ofcare sonography in rural areas, antiretroviral drug resistance in youth living with HIV and hypertension management.
highlights 2024
The Swiss TPH Diagnostic Centre was re-accredited in 2024 and performed over 60,000 analyses for tropical and travel-associated infections. The team supported malaria clinical trials in DRC and Kenya, and evaluated the performance of several rapid diagnostic tests for malaria and Strongyloides stercoralis

Daniel Paris, Head of MED
The pioneering Bacoba phase I trial of an innovative topical treatment for leishmaniasis was successfully completed. This first-ever biotech-academic product development collaboration, funded by Innosuisse, marked an important step in clinical translational research.
To meet the training needs resulting from important changes in global and national clinical research regulations, MED added a good clinical practice refresher course to its training portfolio.
Partnership highlights
In Tanzania, we celebrated 20 years of the Chronic Diseases Clinic of Ifakara and ten years of the One Stop Clinic at the St. Francis Regional Referral Hospital in Ifakara. The Emergency Department and new Intermediate Care Unit served more than 90,000 patients, while the Heart and Lung Clinic started community-based NCD screening and offered echocardiography and point-of-care ultrasound courses.
The integrated diagnosis and sequencing platform (IDSP) joined major multinational consortia in TB and malaria, and is building expertise in bioinformatics and sustainable sequencing services for Tanzanian institutions.
A multidisciplinary sickle cell disease management initiative was launched with Novartis and the Centre Suisse de Recherches Scientifiques en Côte d’Ivoire (CSRS). Our local office in DRC successfully supported multiple pivotal and regulatory clinical trials in drug development for TB, malaria and helminth infections with local and national stakeholders.
In Rwanda, MED provided courses on malaria diagnostics, drugs and vaccines through the Malaria Modelling for Africa programme and is supporting five PhD projects at the Rwanda Biomedical Centre. A delegation met with the National TB Programme in Kyrgyzstan to establish collaboration with the TB programmes in Kyrgyzstan and Uzbekistan.
Daniel Paris has co-edited the reference book “Migrations- und Flüchtlingsmedizin”, a practical guide for primary and basic health care.
The Department of Education and Training (ET) develops and coordinates courses and programmes at Swiss TPH, the University of Basel, and partner institutions worldwide. With extensive experience in education, training and capacity strengthening, ET offers state-of-the-art learning facilities at the Swiss TPH headquarters in Allschwil.

Julia Bohlius, Head of ET

ET provides education at all academic levels, from bachelor’s to postgraduate training. In 2024, more than 100 facilitators supervised around 210 PhD students, 80 MSc Epidemiology and Infection Biology students, and 480 postgraduate learners. ET’s programmes attract diverse students from around the world, some supported by Alcea Foundation, R. Geigy Foundation and private donors, supporting equal access to quality education.
ET’s commitment to excellence is reflected in student evaluations, particularly in the MSc programmes, where many courses scored 5.5 or higher out of possible 6. The graduation was celebrated with partner institutes from the University of Basel’s biology programme.
A major milestone was the approval of the interfaculty Graduate School of Medical and Health Sciences (GSMHS), which will enrol PhD students from autumn 2025. Current health PhD programmes at the Medical and Science faculties of the University of Basel will join the GSMHS, fostering interdisciplinary exchange.
At the postgraduate level, ET ran 34 courses, including the “CAS Internationale Zusammenarbeit und Globale Gesundheit” (CAS IZGG), which celebrated its 80th anniversary. Launched in 1944 as the first general tropical course, the CAS IZGG continues to be updated to meet today’s health issues.
To support leadership in an interconnected world, ET published a competency framework outlining ten key skills for public health leaders. This tool helps educators align curricula with local needs, strengthen workforce connections, and better equip future leaders for complex global health challenges.
As a consultancy, we worked with SCIH to develop an online training programme on monitoring and evaluation of health system strengthening projects. The training, tailored to train participants around the globe, combined self-study with interactive classroom teaching.
In 2024, ET launched the Swiss TPH AlumNet, an official alumni network designed to strength-
en connections with graduates from the Msc, PhD and postgraduate programmes.
Adapting to emerging trends, ET placed a strong focus on AI and digitalisation. We introduced a new course on Digital Health Management, and explored the perceptions and use of Generative AI (GenAI) among students and facilitators, funded by the “Freie Akademische Gesellschaft” (FAG). Both groups shared similar views: GenAI was widely used and generally viewed as beneficial, yet concerns remained, underscoring the need for further training, clear guidance, and policy development. Another project, in collaboration with the University of Basel’s Medical Faculty, explored the use of GenAI in medical education to mitigate implicit bias in clinical consultations.
ET also strengthened its expertise in systematic reviews, now offering dedicated support to researchers and students across Swiss TPH.
→ swisstph.ch/en/study-with-us
The Department of Administration (ADMIN) is the backbone of Swiss TPH. Its Finances and Controlling, Human Resources, Informatics and Infrastructure teams provide support in the areas of research, education and services. Around 60 people work in ADMIN at Swiss TPH.

Last year, the Department of Administration successfully concluded the strategy period 2021 – 2024. A particular highlight was the feedback from the 2024 Employee Engagement Survey: with an engagement score of 86%, staff and students once again demonstrated high levels of motivation and pride in being part of Swiss TPH.
As part of the new Swiss TPH Strategy 2025 –2028, a strategic framework is being developed for the underlying “Success Factors”: People and Culture, Partnerships and Networks, Digital Transformation, Infrastructure, Good Governance, and Sustainability. The framework aims to define cross-institutional objectives that go beyond Administration and include areas such as communication and projects and grants.
The digital transformation continued to progress last year, with the goal of simplifying collaboration across departments. The E-Collaboration project was successfully launched, the IT organisation was repositioned, and
the IT support team was strengthened with the addition of student supporters. Initial efforts to better align IT and business processes were launched, and, in close collaboration with Research IT, the first digital solutions were successfully implemented for research units.
Together with the Department Education and Training, an internal “Leadership Academy” was established to strengthen leadership skills across the management team. The internal research career path was revised and rolled out. The employee sports programme was expanded, and the “Fit4Future” lunchtime seminar series continued. The mentoring programme for staff and students saw a particularly high level of participation in 2024. The Code of Conduct was completely revised to reflect the new strategy and updated values and rolled out at the start of 2025. The Employee Engagement Survey was completed successfully, and concrete improvement measures are now being developed together with a Sounding Board.
A series of workshops on work culture took place to help cultivate a positive working en-

Mathias Kronig, Administrative Director
vironment rooted in the values and culture of Swiss TPH. Our values – courage, integrity, passion and respect – were at the heart of the discussions. To further encourage informal exchange, foster connections among colleagues, and spark new ideas, five “Get Together Apéros” were held throughout the year
In 2024, the ADMIN team managed around 600 project and service cost centres. The rooftop solar panel installation was expanded, and the building’s ventilation systems were optimised, leading to reduced energy consumption. January 2024 marked the successful opening of the new Centre for Tropical and Travel Medicine in the “Turmhaus” at Aeschenplatz in Basel, in close proximity to the main train station.
To provide attractive and affordable accommodation options for Swiss TPH researchers, students and guests, construction of the Swiss TPH Guest House will begin at the HOPE building on the BaseLink site, with the groundbreaking scheduled towards the end of 2025.
Jeroen Aarden joined Swiss TPH in August 2024 as the new Head of the Informatics unit. Brigitta Bildstein took over as Head of the Controlling group within the Finance and Controlling unit.
Board of Governors
Members from the cantons of Basel-Stadt and Basel-Landschaft, Swiss universities and the private sector
Eva Herzog, President
Rolf Borner, Ariane Bürgin, François Chappuis, Sabina De Geest, Jacques Fellay, Alban Frei, Lutz Hegemann, Barbara Wieland, Deborah Studer (observer)
www.swisstph.ch/en/about/ board-of-governors
Administration Departments
Administration
Mathias Kronig
Deputy: Iris Haueter and Deniz Gör
Finances
Deniz Gör
Human Resources
Iris Haueter
Informatics
Jeroen Aarden
Infrastructure
Florian Frenzel
Directorate
Director
Jürg Utzinger
Administrative Director
Mathias Kronig
Department Heads
Mathias Kronig, Nicole Probst-Hensch, Sébastien Gagneux, Helen Prytherch a.i., Daniel Paris, Julia Bohlius
Epidemiology and Public Health
Nicole Probst-Hensch
Deputy: Jakob Zinsstag
Biostatistics
Penelope Vounatsou
Chronic Disease Epidemiology
Nicole Probst-Hensch
Disease Modelling
Nakul Chitnis
Environmental Exposures and Health
Martin Röösli
Health Interventions
Manuel Hetzel
Household Economics and Health
Systems Research
Günther Fink
Human and Animal Health
Jakob Zinsstag
Society, Gender and Health
Sonja Merten
Urban Public Health
Mirko Winkler
Vector Biology
Pie Müller
Medical Parasitology and Infection Biology
Sébastien Gagneux
Deputy: Till Voss
Clinical Immunology
Claudia Daubenberger
Helminth Drug Development
Jennifer Keiser
Malaria Gene Regulation
Till Voss
Malaria Host Interactions
Nicolas Brancucci
Parasite Chemotherapy
Pascal Mäser
Tuberculosis Research and Evolution
Sébastien Gagneux
Communications, Sabina Beatrice-Matter
Internal Audit, Vincent Bodenez
Medical Services, Esther Künzli, Andreas Neumayr and Sandra Brandenberger
Project & Grant, Michael Käser
Security, Safety & Health, Marco Tamborrini
Swiss Centre for International Health
Helen Prytherch a.i.
Digital Health
Fenella Beynon
Diseases and Programmes
Peter Steinmann
Systems Performance and Monitoring
Odile Pham-Tan
Systems Strengthening and Health Promotion
Helen Prytherch
Medicine
Daniel Paris
Deputy: Christian Burri
Clinical Operations
Elisabeth Reus
Clinical Research
Klaus Reither
Diagnostics
Beatrice Nickel
Medicines Development
Daniel Paris
Medicines Implementation
Research
Christian Burri
Education and Training
Julia Bohlius
Bachelor-Master-Doctorate
Peter Odermatt
Library and Documentation
Giovanni Casagrande
Professional Postgraduate Training
Karin Gross
Teaching Technology and Didactics
Christoph Pimmer
Organigram valid April 2025
All Swiss TPH staff: www.swisstph.ch/en/staff

Financial statements established in accordance with Swiss GAAP FER

“My studies equipped me with the skills to tackle public health challenges, engage stakeholders and drive evidence-based policy. These have been essential in scaling up our deworming programme to include pre-school children in 2024. In total, the programme has reached 40 million children since 2019.”
Core Funding
Canton Basel-Landschaft, CH
Canton Basel-Stadt, CH
State Secretariat for Education, Research and Innovation (SERI), CH University of Basel, CH
Research Funding
Basel Research Centre for Child Health (BRCCH), CH EU research grants (e.g. ERC, Horizon, EDCTP), EU Federal Commission for Scholarships for Foreign Students (ESKAS), CH
National Institutes of Health (NIH), US Swiss National Science Foundation (SNSF), CH Swiss Network for International Studies (SNIS), CH University of Basel, CH
Foundations
Aeras Global TB Vaccine Foundation, US Albert-Heim-Stiftung, CH
Anesvad, ES
Baylor College of Medicine Children’s Foundation Lesotho (BCMCFL), LS
Bill & Melinda Gates Foundation (BMGF), US Biovision Foundation, CH
Boehringer Ingelheim Fonds, DE CDC Foundation, US
Cesti Fondatione Onlus, IT
Clinton Health Access Initiative (CHAI), US Computer Simulation & Advanced Research Technologies (CSART), AU Eckenstein-Geigy-Stiftung, CH Elrha, UK
Else Kröner-Fresenius-Stiftung (EKFS), DE Fondation Alcea, CH
Fondation Botnar, CH
Fondazione Adiuvare, CH Fondazione lstituto Nazionale di Genetica Molecolare (INGM), IT Forlen Stiftung, CH
Freiwillige Akademische Gesellschaft (FAG), CH Global Health Innovative Technology Fund (GHIT), JP Health Information Traceability Foundation (HIT), CH Health Promotion Switzerland, CH kENUP foundation, EU Krebsforschung Schweiz, CH
Moritz Straus-Stiftung, CH Novartis Foundation, CH
Public Health Charity Foundation, CH R. Geigy Foundation, CH Sight and Life (SAL), CH Sint Antonius Foundation, NL Skat Foundation, CH
Stanley Thomas Johnson Foundation, CH Syngenta Foundation for Sustainable Agriculture (SFSA), CH Walter Fischli Stiftung, CH Wellcome Trust, UK
Public Clients Switzerland
Amt für Ausbildungsbeiträge Basel-Stadt, CH Amt für Umwelt und Energie Basel-Stadt, CH Bundesamt für Raumentwicklung (ARE), CH Commission for Research Partnerships with Developing Countries (KFPE), CH Entwicklungszusammenarbeit des Kantons Basel-Stadt, CH Federal Department of Defence, Civil Protection and Sport (DDPS), CH Federal Department of Economic Affairs, Education and Research (EAER), CH
Federal Food Safety and Veterinary Office (FSV), CH Federal Office for Agriculture (FOAG), CH Federal Office of Public Health (FOPH), CH Federal Office of Sport (FOSPO), CH Federal Office of the Environment (FOEN), CH Federal Statistic Office (BFS), CH Innosuisse – Swiss Innovation Agency, CH Kantonsspital Basel-Landschaft, CH MeteoSchweiz, CH Nationales Referenzzentrum für Legionellen (NRZL), CH Swiss Agency for Development and Cooperation (SDC), CH Swiss Federal Institute of Aquatic Science and Technology (Eawag), CH Swiss Federal Laboratories for Materials Science and Technology (EMPA), CH Swiss Pathogen Surveillance Platform (SPSP), CH Swiss Personalized Health Network (SPHN), CH University Hospital Basel, CH
Public and Public-Private Clients International Adamawa State Primary Health Care Development Agency (ADSPHCDA), NG African Population and Health Research Center (APHRC), KE African Society for Laboratory Medicine (ASLM), ET Agence Française de Développement (AFD), FR Agence nationale de sécurité sanitaire de l’alimentation, de l’environnement et du travail (ANSES), FR Asian Development Bank (ADB), PH Association of Churchbased Development NGOs (ACDEP), GH Bundesamt für Auswärtige Angelegenheiten (BfAA), CH Canadian Association for Global Health (CAGH), CA Centers for Disease Control and Prevention (CDC), US Centre de Support en Santé Internationale (CSSI), TD Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ), DE Direction des Services Vétérinaires (DSV), FR Drugs for Neglected Diseases initiative (DNDi), CH Elgo Dimitra – Ellinikos Georgikos Organismos, GR Epicentre, FR European Institute of Public Health Policy (EIPHP), UA European Space Agency, EU Federal Ministry for Economic Cooperation and Development (BMZ), DE Food and Drug Administration (FDA), US Foundation for Innovative New Diagnostics (FIND), CH Gavi, the Vaccine Alliance, CH German Institute for Medical Mission (DIFAM), DE Grand Challenges Canada, CA Health and Environment Alliance (HEAL), BE Helse Nord Tuberculosis Initiative Malawi (HNTI), NO Human Sciences Research Council (HSRC), ZA Innovations for Poverty Action (IPA), US Institut de Recherche pour le Développement (IRD), FR Institut de Recherches en Elevage pour le Développement (IRED), TD Institut National d’Hygiène Publique (INHP), CI Institut national de l’environnement industriel et des risques (Ineris), FR Instituto Nacional de Saúde (INS), MZ International SOS (Africa Holdings) Ltd, UK International Committee of the Red Cross (ICRC), CH ISGlobal, ES Kreditanstalt für Wiederaufbau (KfW), DE L’Organisation de Coordination pour la lutte contre les Endémies en Afrique Centrale (OCEAC), CM Medical Care Development International (MCDI), US Medicines for Malaria Venture (MMV), CH Muséum national d’Histoire naturelle, FR
National Center of Tuberculosis and Lung Diseases (NCTLD), GE National Public Health Center (Nemzeti Népegészségügyi Központ), HU Norwegian Agency of Development Cooperation (Norad), NO Nutrition International, CA Right to Care Zambia (RTCZ), ZM Swiss Red Cross (SRC), CH The Global Fund, CH
The International Society for Research in Human Milk and Lactation (ISRHML), US
The Task Force for Global Health, US tropEd Network for Education in International Health, DE Unitaid, CH
United Kingdom Department for International Development (DFID), UK United Nations Children Fund International (Unicef), US United Nations Development Programme (UNDP), US United Nations Population Fund (UNFPA), US
United States Agency for International Development (USAID), US Unlimit Health, UK
West African Health Organisation (WAHO), BF World Bank, US
World Health Organization (WHO), CH World Organisation for Animal Health (WOAH), FR
Private Clients and Non-Profit Organisations Abwenzi Pa Za Umoyo (APZU), MW AEDES, BE
Anglo American Services (UK) Ltd., UK Astellas Pharma AG, CH Bacoba AG, CH BASF SE, DE Bayer AG, CH
BioInitials, CH Bionorica SE, DE Bristol Myers Squibb, US Cardno Emerging Markets East Africa Ltd. (CEM), KE Conseil Santé, FR Deutsche Lepra- und Tuberkulosehilfe e. V. (DAHW), DE Effectum Medical AG, CH Fields at Work GmbH, CH Game Solutions Lab, NL GFA Consulting Group GmbH, DE Grolimund + Partner AG, CH Health Effects Institute (HEI), US Hemex AG, BS Ideas for Change, ES Insuco Burkina Faso, BF Insuco, UK
International Association for Maternal and Neonatal Health (IAMANEH), CH Life4me+, CH Lygature, NL
Martin Systems GmbH, DE Médecins Sans Frontières (MSF), CH Merck, DE MSD Merck Sharp & Dohme AG, CH NED-TECH AG, CH Novartis Pharma AG, CH OmicScouts, DE OptiMedis AG, DE Oryx Expertise, FR Oxfam Novib, NL Pact, US
PATH, US Privatklinik Meiringen, CH RANAS Ltd., CH Rotarians Against Malaria (RAM), PG Science for Change, ES Seboche Mission Hospital, LS SKAN, CH SolDevelo, PL SolidarMed, CH Specs Compound Handling B.V., NL Swiss Excellence Forum, CH Syngenta, CH TB Alliance, SA Terre des hommes, CH VisibleSolutions AG, CH Wits Health Consortium (Pty) Limited (WHC), ZA
Academic Partners
Academic Medical Center (Academisch Medisch Centrum), NL Addis Ababa University (AAU), ET African Society for Laboratory Medicine (ASLM), ET Agricultural University of Athens, GR Armauer Hansen Research Institute (AHRI), ET Berner Fachhochschule (BFH), CH Bernhard-Nocht-Institut für Tropenmedizin, DE Boston University, US Brown University, US Centre hospitalier régional et universitaire de Besançon (CHRU), FR Centre national de la recherche scientifique (CNRS), FR Centre Suisse d’Electronique et de Microtechnique (CSEM), CH Centre Suisse de Recherches Scientifiques en Côte d’Ivoire (CSRS), CI Centre universitaire de médecine générale et santé publique, Lausanne (unisanté), CH
Charité – Universitätsmedizin Berlin, DE College of Art and Sciences, Xavier University, Cincinnati, US Consiglio Nazionale delle Ricerche, IT Cyprus University of Technology, CY École Polytechnique Fédérale de Lausanne (EPFL), CH
Eindhoven University of Technology, NL
Eucor – The European Campus, CH, DE, FR Forschungszentrum Borstel, Leibniz Lungenzentrum (FZB), DE Geneva University Hospitals (HUG), CH Ghent University, BE Harvard T.H. Chan School of Public Health, US Helmholtz Centre for Infection Research, DE Hes-so Leading House (MENA), CH Ifakara Health Institute (IHI), TZ Imperial College London, UK Innovative Vector Control Consortium (IVCC), UK Inselspital Bern, CH Institut Mines-Télécom (IMT), FR Institut Pasteur, FR Institute of Social and Preventive Medicine (ISPM), Bern, CH Institute of Tropical Medicine Antwerp (ITM), BE Instituto de Higiene e Medicina Tropical Universidade Nova de Lisboa (IHMT), PT Instituto Nacional de Saúde (INS), MZ
Institutul de Ftiziopneumologie “Chiril Draganiuc”, MD Institutul de Pneumoftiziologie “Marius Nasta” (IPMN), RO James Cook University (JCU), AU KEMRI – Wellcome Trust Research Programme, KE Kenya Medical Research Institute (KEMRI), KE
Lao Tropical and Public Health Institute (Lao TPH), LA Lausanne University Hospital (CHUV), CH
Liverpool School of Tropical Medicine (LSTM), UK
London School of Hygiene & Tropical Medicine (LSHTM), UK
Lucerne University of Applied Sciences and Arts (HSLU), CH
Ludwig Maximilian University of Munich (LMU), DE Makerere University, UG
Manhiça Health Research Centre (CISM), MZ
Massachusetts General Hospital, US Moi University, KE
MRC/Wits Agincourt Field Office, ZA
National Institute for Medical Research (NIMR), TZ
National Institute for Research in Tuberculosis (ICMR), IN Nofer Institute of Occupational Medicine, PL Norwegian University of Life Sciences (NMBU), NO Obafemi Awolowo University, NG
Ospedale San Raffaele (SRL), IT
Palestine Polytechnic University, PS
Papua New Guinea Institute of Medical Research (PNG IMR), PG
Paul Scherrer Institute (PSI), CH
Penta Child Health Research, IT
PNG National Research Institute, PG
Public Health Laboratory Ivo de Carneri (PHL-IdC), TZ
Qom University of Medical Sciences, IR Radboud University Nijmegen, NL
Robert Koch-Institut (RKI), DE Rwanda Biomedical Centre (RBC)
Sapienza University of Rome, IT School of Social Work Fribourg (HETS-FR), CH Somali Research & Development Institute (SORDI), SO South African Medical Research Council, ZA Swiss Association for Quality (SAQ), CH Swiss Federal Institute of Technology in Zurich (ETHZ), CH Swiss Institute of Bioinformatics (SIB), CH Swiss School of Public Health (SSPH+), CH swissuniversities Development and Cooperation Network (SUDAC), CH Technische Universität München (TUM), DE Temple University, US The Aurum Institute, ZA
The George Institute for Global Health India, IN Umeå University, SE Unisanté, CH
Universidad Peruana Cayetano Heredia (UPCH), PE Universität St. Gallen, CH
Universitäts-Kinderspital beider Basel (UKBB), CH Universitätsklinikum Bonn (UKB), DE Université de Genève, CH Université de Lausanne, CH Université de Neuchâtel, CH Université des Sciences, des Techniques et des Technologies de Bamako (USTTB), ML Université Félix Houphouët-Boigny (UFHB), CI University of Antwerp, BE
University of Applied Sciences and Arts Northwest Switzerland (FHNW), CH University of Applied Sciences and Arts of Southern Switzerland (SUPSI), CH University of Applied Sciences and Arts Western Switzerland (HES-SO), CH University of Basel, CH University of Bergen (UiB), NO University of Bern, CH University of Bologna, IT
University of Buea, CM University of Calabar, NG University of California San Francisco (UCSF), US University of Cambridge, UK University of Cape Town, ZA University of Dundee, UK University of Ghana, GH University of Ghent, BE University of Gothenburg, SE University of Groningen (RUG), NL University of Health and Allied Sciences (UHAS), GH University of Heidelberg, DE University of Ibadan (UI), NG University of KwaZulu-Natal, ZA University of Lugano, CH University of Luzern, CH University of Maiduguri, NG University of Malawi, MW University of Maryland, US University of Montpellier, FR University of Nairobi, KE University of Nebraska, US University of Oxford, UK University of Pécs, HU University of Sao Paulo (USP), BR University of Strasbourg, FR University of the Witwatersrand, ZA University of Turin, IT University of Utrecht, NL University of Vienna, AU University of Warwick, UK University of Washington (UW), US University of Zurich, CH Weizmann Institute of Science, IL Yale University, US
*The list reflects all Swiss TPH partners and funders that are within our staff-managed project database.

Concept and edits: Layla Hasler
Additional contributions: Sabina Beatrice-Matter, Myrta Brunner, Valérie Busson, Danielle Powell, Ella Walch, Eva Herzog, Jürg Utzinger, Department Heads and Swiss TPH staff members
Layout and design: Neeser Müller Görner, Basel
Pictures: Adobe stock photos, Muna Ally, BBC StoryWorks Commercial Productions, Olivier Brandenberg, Valérie Busson, Centre Suisse de Recherches Scientifiques en Côte d’Ivoire, Salomon Djekorgee Dainyoo/Swiss TPH/ Fairpicture, Eva Flury, Health for All Project, Christian Heuss, ICRC Somalia, Alice Kayibanda/ Swiss TPH/Fairpicture, Kenneth Nars, Joachim Pelikan, Danielle Powell, Magali Rochat, RTI International/Muhammad Fadli, Thomas Schuppisser, Tobias Suter, University of Basel/ Christian Flierl, Ella Walch and Swiss TPH staff
Cover photo: Joachim Pelikan
Printing: Gremper AG
Copyright: Swiss TPH, 2025