THE ESNEFT TRAINING PROSPECTUS









Welcome to East Suffolk and North Essex foundation trust (ESNEFT). ESNEFT provide services from Colchester and Ipswich hospitals, Aldeburgh, Clacton, Halstead, Harwich and Felixstowe community hospitals and Bluebird Lodge near Ipswich. It serves a population of close to one million people in a diverse range of settings from large inner city communities to rural and coastal settings. It is the largest healthcare employer in the East of England and is focussed on provided high quality care in as timely a fashion as possible.
The trust values the education and training of all its staff highly and this is overseen by a multiprofessional faculty of education. We provide undergraduate medical education, working in partnership with medical schools in Cambridge, Anglia Ruskin University, University of East Anglia and Queen Mary University of London. We are part of the East of England foundation school and postgraduate rotations and have approximately 500 post graduate medical trainees across our sites in a variety of medical and surgical specialities as well as foundation dentists.
Your education will be supported by a vibrant training team with an active programme of robotic and laprascopic surgery training based in the ICENI centre in Colchester and the East Anglian simulation centre in Ipswich.
Access to state-of-the-art simulation and virtual reality training equipment supplements an extensive library service on both sites.
At ESNEFT you will be welcomed into a multiprofessional team . Although our workforce is large, ESNEFT prides itself on being a welcoming and supportive place to work and our experienced team in medical education will do all they can to support you to achieve your aims.
I hope this prospectus will encourage you to explore potential careers in ESNEFT and I look forward to welcoming and supporting your learning in the future.
Dr Peter Bishop FRCA FFICM Consultant Intensive care and Anaesthetics Director of Medical Education
Hello and Welcome to East Suffolk and North Essex Foundation Trust.
The Medical Education Team look after over 1500 Undergraduate Medical Students, Physician Associate Students, Dental Trainees and Postgraduate Doctors in Training. We have dedicated admin teams on both of our main sites, Ipswich and Colchester. We can be found in the Postgraduate Medical Education Centre, Villa 8, Colchester and in the Postgraduate Medical Education Centre in the main hospital building at Ipswich Hospital.
We are here to support you, and to ensure you have the best training experience during your time at ESNEFT.
We actively encourage your feedback and we appoint trainee representatives from our training programmes each year. We take your wellbeing seriously. We operate an open door policy and encourage our students and Doctors in training to talk to us if they have any issues or concerns.
We have excellent Junior Doctors’ Mess facilities on both sites and a very active programme of events including annual balls, sports teams (football, netball and badminton) and social events.
In Colchester, there is a healthy mix of bars, cinemas, restaurants, theatres and night clubs and Ipswich has a very vibrant and eclectic mix of restaurants, entertainment and the area around the Marina is a popular place for our Doctors in Training. We are also surrounded by beautiful countryside, rivers and east coast fishing villages and resorts.
We look forward to you joining us at ESNEFT’
Nora Tester, Head of Medical Education
The East Suffolk and North Essex NHS Foundation Trust comprises of two acute teaching hospitals: Ipswich Hospital and Colchester Hospital. Previously two separate trusts, formed together on 1st July 2018. We are the largest NHS organisation in East Anglia and several of our clinical services are among the largest in England: acute children’s services, oncology, trauma and orthopaedics, general surgery, urology and ophthalmology.
Both hospitals provide many of the same acute services for their local communities, providing healthcare to almost 1 million people. Most specialities have their own separate teams at each hospital, with ENT and Vascular providing a shared service across both sites. In addition to our acute hospitals, we also provide care from Aldeburgh, Clacton, Halstead, Harwich and Felixstowe community hospitals and Bluebird Lodge.

Ipswich Hospital is a large district general hospital providing acute hospital services to nearly 400 000 people who live and work in Ipswich and East Suffolk. The hospital has just over 550 beds.

There is an excellent Post-Graduate medical centre, housed in a purposebuilt unit at the hospital, with a wellstocked medical library and simulation suite.
Ipswich Hospital is part of the Comprehensive Local Research Network for Norfolk and Suffolk with a particular strength in research on Cancer, Diabetes and Rheumatology.
Colchester Hospital is a large district general hospital providing hospital services to a surrounding population of nearly 370 000 people. The hospital has just over 760 beds.
There is an onsite state of the art surgical simulation center (the ICENI center) which is widely recognized by healthcare professionals across the country and internationally.
Colchester Hospital has a number of large developments taking place, including the building of a dedicated orthopedic center.

Ipswich is the county-town of Suffolk and is one England’s oldest towns. It benefits from being a vibrant town with easy access to beaches and countryside.


Colchester has become one of the fastest growing places in eastern England and in 2022, regained city status as part of the Platinum Jubilee celebrations. With its museums, art galleries, theatres and restaurants, the city offers opportunities to explore the locale’s rich historic cultural and culinary influences. Both places have brilliant train links to London; only 1 hour from Ipswich and only 45 minutes from Colchester.
Ipswich and Colchester Hospitals have active and sociable Doctor’s Mess. Ipswich Hospital has one of the biggest Doctor’s Mess in the country with sky TV, pool table and table tennis. Colchester Hospital has a recently renovated modern Doctor’s Mess. They both have very busy social calendars and organise frequent events with highly anticipated annual balls. Both hospitals have weekly sports groups including football, badminton and netball.
There are cliffs, heaths, forests and estuaries to explore: Orford, Rendlesham Forest, Lavenham, Dedham Vale. Places to eat


Award winning gastropubs: The Unruly Pig (rated top UK gastropub 2022)
Famous Aldeburgh fish and chips.
It is a rapidly developing City centre with regional acclaim for its shopping and dining, ‘The Arts Centre’ is a renowned music and comedy venue.
11th century Norman castle in Colchester city centre built on the foundations of the largest Roman Temple on Britain; Flatford Mill made famous by artist John Constable; Sutton Hoo featured on the Netflix film
‘The Dig’; Framlingham ‘the castle on the hill’ sung about by Ed Sheeran.
Ipswich waterfront A popular place for doctors to live due to its views over the marina and its acclaimed bars and restaurants.
There are 400 miles of beautiful coastline to explore across Suffolk and Essex: Southwold, Aldeburgh, Walberswick, Frinton, Waltonon-the-Naze.


ESNEFT prides itself on being a supportive workplace that cares about the wellbeing of its staff. Below are just some of the ways that we offer support to staff:
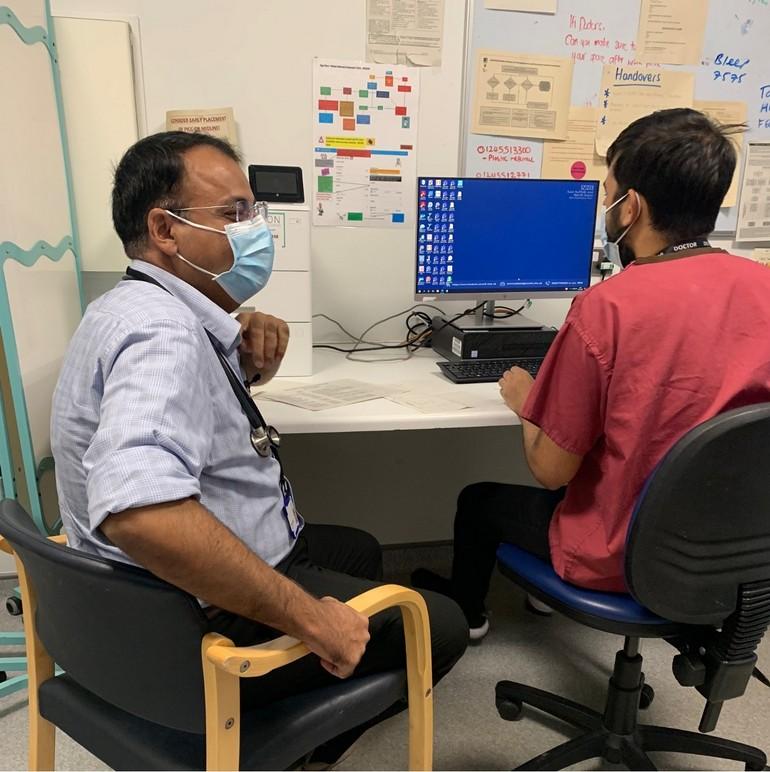
Every doctor in the hospital will be allocated an educational and clinical supervisor. Your clinical supervisor is a consultant based within the specialty that you are working in and is there to help with matters related to the workplace. Your educational supervisor is a consultant who will support you with career planning and completing logbooks/portfolios. Both are sources of support that you can go to at anytime to discuss issues that may be arising.
The guardian of safe working ensures that issues of compliance with safe working hours are addressed by the doctor and the employer (ESNEFT) as appropriate. If you feel that you are continually working unsafe hours, then this is the person to approach.
There are many staff at ESNEFT who are trained mental health first aiders, including the postgraduate medical education team. This means they have a formal qualification in supporting people with mental health concerns in the workplace.

Colchester Hospital has a confidential service available called ‘Talk to Sophie’. It provides doctors of any grade with an opportunity to meet with a friendly colleague to talk things through. Our ‘listener’ doctors have all been nominated by junior doctors as trusted and empathic. Doctors can access this service between 9am and 6pm Monday to Friday by calling switch board and letting them know you would like to access the Talk to Sophie service. This service will soon be accessible at Ipswich Hospital.
Health Education England (HEE) in the East of England (EoE) are committed to supporting doctors through their training. It provides a wellbeing service which offers specialist support for trainees who may require it. There are regular wellbeing events and workshops that can be accessed through their website. There is also additional support available through referral to their team (either self-referral or referral from an educator).
Our chaplains are available to visit wards and departments to offer a listening ear. They are here for people of all faiths and beliefs, including people who do not think of themselves as religious. They are onsite Monday to Friday (8am-4pm) and available 24/7 via switchboard. The chapel is also available 24/7 for staff who would like a quiet place to sit.
Important contacts:
wellbeing@esneft.nhs.uk
chaplaincy@esneft.nhs.uk
At ESNEFT, trainees have access to high quality Library services to help you practice evidence-based decision making, contribute to research and quality improvement projects, write and publish journal papers, and support your career development.
There is a physical library space at both Colchester and Ipswich Hospital, both accessible 24/7 with access to networked PCs, generous study space and books. You will also find printing, scanning and binding facilities. You can borrow books any time of day or night using the self-service kiosks.

If we don’t have the book you need we can get it for you from another library.
Colchester library.services@esneft.nhs.uk Ipswich hospital.library@esneft.nhs.uk
A wealth of online resources is provided, including access to ClinicalKey, Oxford Handbooks Online, e-books and e-journals. The Library and Knowledge Hub provides quick access to nationally and locally purchased resources.
It is easy to stay updated with the latest developments and evidence in your subject area by joining KnowledgeShare. This current awareness service provides you with alerts tailored to your specific interests.
If you need the best evidence to inform your research, audit or quality improvement, our experienced librarians can perform in-depth searches of healthcare databases and email you a list of relevant research papers. If you prefer to search yourself, we can offer advice on search strategies and resources,.





A range of training workshops are offered. You can learn how to critically appraise research papers, how to effectively communicate with patients and carers through our health literacy training, how to reflect for CPD, and how to write for publication.
If you are studying for Royal College exams, we can support you with a range of exam preparation books and online tools.
Our website

Extensive information about our services, links to all online resources and helpful guides can be found on our website:

The East Anglian Simulation and Training Centre, based at Ipswich Hospital, has a suite of simulation rooms providing multidisciplinary healthcare education using high fidelity patient manikins is a state-ofthe-art simulation room. The simulation centre is run by 4 expert colleagues who lead and facilitate the training. The team has the ability to run concurrent sessions in the simulation area as well as in clinical areas within the hospital.

The simulation suite is constantly developing to provide the most up to date training facilities for all trainees. A new manikin has been purchased which has capabilities including sweating, fitting, light activated pupil reactions and enhanced sound production during auscultation. This new manikin will also facilitate trauma scan practice. In addition, there will shortly be a new manikin that can facilitate female simulations including birthing simulations.
The simulation suite facilitates learning for undergraduate and postgraduate doctors and nurses in medicine, surgery, A&E and paediatrics. Some examples of training includes foundation doctor simulation days, 5th year medical students ‘bleep week’ and weekly training in the emergency department resus. There are also skills trainers for ultrasound including FAST scanner, Chest drain insertion, TruPICC and Central line insertion.
The Virtual Reality (VR) training is offered to medical and nursing trainees to provide an immersive, and engaging learning environment. It allows trainees to work through clinical scenarios with a facilitator to focus on decision making in a safe environment without compromising patient safety. The VR training is delivered through Oxford Medical Simulation (OMS) software which is an award-winning evidencebased learning platform.

The ICENI Centre is a purpose-built medical education and training centre based at Colchester Hospital. The centre delivers training on-site and remotely using state of the art augmented and virtual reality simulation equipment in robotic surgery, laparoscopy, hysteroscopy, endovascular, ophthalmology and endoscopy. The quality of the courses available is widely recognised by healthcare professionals across the globe who travel to share their expertise and/or learn from our expert faculty to advance their practical skills, away from the pressures of a clinical environment.

The ICENI centre is equipped with cutting edge technology including the Intuitive Da Vinci XI simulation console; Inovus laparoscopy and hysteroscopy simulators; Mentice 7 endovascular VR equipment; EyeSi VR stack and; the Endosim endoscopy trainer. Through attending courses, trainees can track their performance through objective data that measures the level of skill set attained and practice complex technical surgical interventions. Trainees benefit from being able to access facilities in their own time either at home (using the Inovus box trainer) or at the ICENI centre.

Some of the courses available include:
• Colorectal
• Core surgical skills
• ENT
• Obstetrics and Gynaecology
• Ophthalmology
• Robotics
• Stroke emergency medicine & thrombolysis
• Radiology
• European Paediatric Advanced
Click here for more information about ICENI
Ipswich Hospital teaches 1st to 6th year medical students from Cambridge University and the University of East Anglia (UEA). It has an onsite medical education center which is home to the undergraduate medical education team. There are 3 clinical education fellows that provide the majority of undergraduate teaching. They are a great source of knowledge and expertise as they have recent experience of the Foundation Programme.
The medical education center has a state-of-the-art simulation suite, teaching classrooms, lecture hall and clinical skills labs (click on this link to find out more about these facilities). Medical students will have a variety of teaching sessions on their placement including ward-based
teaching, simulation experience, clinical skills sessions, small group tutorials, case-based discussions and lectures.

The undergraduate team receives very good feedback from medical students who have completed their placements and medical electives here. There are a number of departments that are keen to have medical students on their electives, in particular the paediatric department. These can be arranged by contacting the department lead directly.
The medical education team at Ipswich hospital friendly and welcoming team that provide high quality teaching for 1st to 6th year medical students.
Teaching undergraduate students is a rewarding job and we use a variety of teaching methods including bed-side teaching, simulation, lectures and small group tutorials. As clinical fellows, we have the opportunity to complete a PGCERT which is either part, or fully funded. There are also opportunities to undertake projects which help with applications to specialty training.
Sandeep Singh, Clinical Teaching Fellow Dr
Dr
Colchester Hospital teaches medical students from Barts University London and Anglia Ruskin University. It has an onsite medical education team who can be found in Villa 8.
There is a dedicated team of medical education fellows; 3 junior fellows and 1 lead, senior fellow. The education fellows work 4 days a week within the education department and 1 day a week clinically in their chosen specialty. The fellows also have an opportunity for funding towards a PGCert qualification in medical education.

Medical students on placement at Colchester will receive a wide variety of teaching including ward-based, clinical skills, cased-based discussion and online teaching. Simulation based teaching is also provided using the onsite surgical simulation center, ICENI, which contains lecture theatres, simulation suites and clinical skills labs (click on this link to find out more about these facilities).
It is a pleasure to work in the Colchester medical education team –everyone is friendly, diligent, and passionate about providing the best possible experience for our medical students. We work closely together and support each other with teaching commitments, training opportunities, and research projects. Creative socials are also a highlight and feature activities such as medical escape rooms!
Dr Izem Onadim, Senior FellowThe undergraduate medical education team receive excellent feedback from medical students emphasizing high quality, engaging teaching and supportive teaching fellows. Many students choose to return to Colchester for subsequent placements, electives and foundation training.

The UK foundation programme is the 2-year training programme leading from undergraduate medical school training to further speciality training. The purpose of the foundation programme is to ensure newly qualified doctors develop core clinical and professional skills. This is mainly through experience within the clinical setting and is supported with simulation teaching and virtual reality training. Ipswich and Colchester Hospital are both part of the East Anglia Foundation School
ESNEFT foundation trainees rotate through 3 specialities in their first year followed by another 3 specialities in their second year. Rotations at ESNEFT cover a range of specialities including acute medicine, anaesthetics/ITU, cardiology, endocrinology and diabetes, cardiology, gastroenterology, respiratory, renal, emergency medicine, care of the elderly, psychiatry, general surgery, urology, haematology and oncology, obstetrics and gynaecology, ENT, paediatrics, trauma and orthopaedics.
We host a number of specialist foundation programmes including the academic foundation programme (AFP) and the foundation priority programme (FPP). The AFP programme based at Ipswich Hospital has a focus on medical education with the ability to complete a post-graduate certificate of education (PGCERT). The FPP programmes offer further teaching and training experience for individuals with a specific interest in these certain specialities such as psychiatry and paediatrics.
There is weekly mandatory teaching for foundation years covering a wide range of topics. This is an excellent opportunity to keep up to date with clinical practice. Most departments also provide weekly teaching in their speciality. Taster weeks are offered to trainees so that they can explore a speciality of interest. The taster can be taken once throughout the foundation training, usually towards the end of FY1. Taster weeks can also be taken in specialities that do not normally have foundation trainees, specifically palliative care.
At both hospitals, foundation trainees are paired up with a ‘buddy’ to help support them through their first year. At Ipswich Hospital, trainees are paired with a doctor in foundation year 2. At Colchester Hospital, trainees are paired with a senior nurse. The ‘buddy’ system adds a level of informal support, alongside the more formal element of support offered by clinical and educational supervisors.
I applied for the educational Academic Foundation Programme at Ipswich as it allows you to complete a PGCert in medical education, develop educational projects and teach medical students alongside the teaching fellows whist training as a foundation doctor. 60% of your time is spent working clinically and 40% is spent working towards your academic projects. The PGCert is based at UEA in Norwich where we have faceto-face teaching sessions on the theory and application of medical education. I would thoroughly recommend this foundation programme to anyone who enjoys variety in their work and wants to maintain academic interests.

Foundation year 1 (FY1)
The first year of foundation training focuses on developing the clinical skills and medical understanding gained in undergraduate training. The learning objectives for this year are set out by the General Medical Council (GMC) and Health Education England (HEE). Trainees will be expected to keep a record of all clinical skills, competencies and feedback via the online e-portfolio system Horus. At the end of the year, FY1 trainees will need to demonstrate they have met the standards of competence in order to progress to FY2.
Foundation year 2 (FY2)



The second year of foundation training builds on the first, with a particular focus on assessing and managing the acutely ill patient. For some specialities, including T&O, general surgery, ENT and paediatrics, you will have the opportunity to hold a referral bleep. Trainees will also need to keep their portfolio up to date in order to demonstrate they have met all the standards of competence for completing foundation training. They will be awarded a certificate of completion following a successful ARCP outcome.
 Dr Sophie Goddard, FY2 AFP
Dr Sophie Goddard, FY2 AFP
Core surgical training (CST) is the 2-year general training programme leading from the Foundation Programme to specialist surgical training. It comprises of training periods in different surgical specialities to gain skills and competencies to prepare doctors for ST3, registrar selection.
Core surgical training is currently available at the Colchester Hospital site within ESNEFT. At Colchester Hospital core surgical training includes trauma and orthopaedics, general surgery (UGI and colorectal), vascular, otorhinolaryngology and urology.
GMC training survey data has shown that Trainees at Colchester feel wellsupervised with overall satisfaction in Trauma and Orthopaedics being above national average.
During core surgical training there are core competencies that should be acquired that are common to all surgical specialities (defined as common competencies). There are also a limited range of competencies to be acquired that are relevant to the trainee’s chosen surgical speciality.

Core surgical trainees are also expected to complete the MRCS examinations part A and B before taking an ST3 post. The East of England Deanery runs a plethora of courses including MRCS preparation courses to help with passing these exams.


There are a wealth of training opportunities available. The ICENI Centre, an onsite state-of-the-art education and training suite, is available for simulation and surgical skills sessions.
In the clinical setting, there are excellent registrars and consultants on-hand to train in theatre, clinic and the wards. In particular, the trauma and orthopaedic surgeons have won awards for their roles in training junior doctors.

Numerous research opportunities are on offer at Colchester to Trainees, with many Supervisors holding research interests. Thus each Department offers opportunities to engage and develop skills in original research, audit and quality improvement.
Trainees benefit from regular departmental teaching within their specialty as well as focused CST teaching each month with the College Tutor. Additionally, Trainees also benefit from the centralised CST teaching which runs remotely for Trainees nationwide.
Trainees are also given the opportunity to develop as clinical teachers, with opportunities to teach medical students and foundation trainees.
Acute Care Common Stem (ACCS) is a three-year programme which covers the acute specialties of anaesthesia, acute medicine, emergency medicine and intensive care medicine. The ACCS programme is an alternative route into anaesthetia instead of core anaesthetic training, and an alternative route into acute medicine instead of internal medical training. It is the only route to enter training in emergency medicine. The purpose of the ACCS curriculum is to equip trainees with the skills and competencies required to recognize and undertake initial management of the acutely unwell patient.
The first two years of training are part of the ACCS generic curriculum. Trainees rotate around 4 x 6-month placements in anesthesia, emergency medicine, internal medicine and intensive care medicine. The anaesthesia training in ACCS is identical to the first six months of core anaesthesia training. In the final year of ACCS, trainees work in their chosen specialty to meet the entry requirements detailed for higher specialty training.
There is weekly teaching for ACCS trainees which complements learning in a clinical environment. Teaching is also provided in a number of different ways including simulation, virtual reality and labbased clinical skills. The simulation center runs several ultrasound skills courses including FAST scanner, Chest drain insertion, TruPICC and Central line insertion. There is also weekly simulation teaching run in the emergency department in the resuscitation room.
Progression through the ACCS curriculum is determined by the ARCP process. The successful completion of ACCS will be dependent on achieving the expected level in all learning outcomes. These include staying up to date with work-based assessments and keeping an eportfolio.





Internal medical training (IMT) has replaced core medical training since August 2019. It is a training programme that forms the first years of post-foundation training for the majority of medical specialities. The programme is designed to prepare doctors with the skills and competencies required to become a medical registrar. At ESNEFT there is the opportunity to complete rotations within a wide range of medical specialities. There are 2 rotations that are compulsory within IMT training; care of the elderly and intensive care medicine. All rotations (apart from intensive care medicine) include participation in the on-call medical rota which involves clerking the acute medical take and out of hours ward cover.
It is a requirement of IMT doctors to meet capabilities in practice set out by the Joint Royal College of Physicians Training Board.
Trainees will have an opportunity to help manage the acute take towards the end of year 2 with the view to managing the acute take with indirect supervision in year 3.
There is a further requirement by the end of IMT year 3 to complete the MRCP(UK) diploma examination in order to progress into registrar training (ST4). There is generous study leave funding to attend extra-curricular courses including simulation, procedural skills and dedicated PACES teaching.
ESNEFT offers support for IMT doctors completing the MRCP (UK) diploma. This includes funding for a PACES examination course and examination resources such as free access to BMJ examination.


The majority of training opportunities will occur in the clinical setting. These include consultant-led teaching ward rounds, practising procedures on the ward, managing acutely unwell patients and the acute medical take. However, there are a number of training opportunities in the simulated setting including simulation days, virtual reality training and clinical skills courses. We run an IMT clinical skills course which will provide an opportunity to practise core procedures.
Part of the internal medical training curriculum requires trainees to have experience in the outpatient setting. At Ipswich hospital, this experience is allocated into your rota as a 1month block where you are able to attend as many clinics as you would like. This 1-month block is during your intensive care placement. At Colchester hospital, you will have dedicated clinic time (clinic weeks) built into your rota throughout the three years.
I have thoroughly enjoyed my time spent working in Ipswich and the broad range of specialties and training opportunities offered here. Notably, there is generous study leave funding to attend extracurricular courses including simulation, procedural skills and dedicated PACES teaching. The introduction of a self-directed 'clinic month' also allows you to attend an array of speciality clinics and facilitates mandatory practical skills. This is not only useful in terms of achieving ePortfolio targets but helps to broaden your experiences.
Working at a large general district hospital affords a great many development
opportunities, which can be more difficult to attain in busier tertiary centres. However it is the close knit community here at Ipswich which I have found to be particularly special. The hospital has an excellent reputation for offering high quality medical training in a friendly and supportive environment. The doctors’ mess is also renowned as being one of the best in the country.
With excellent training prospects on offer, I would highly recommend choosing Ipswich if you are considering a place to start internal medicine training.
 Dr Michelle Richardson, IMT1, Ipswich Hospital
Dr Michelle Richardson, IMT1, Ipswich Hospital

GP training currently involves 3 years of training (ST1-3). From August 2022 the training programme involves one year of hospital posts (ST1), a year of community posts (ST2) and a final year of GP practice (ST3). The year of hospital posts in ST1 is split in 3 x 4-month placements. Hospital posts are available in a wide range of medical and surgical specialities. Community posts that are available include: palliative care, paediatrics, rehabilitation medicine and ophthalmology. There is also now the opportunity to undertake Integrated Training Programmes (ITP) from ST2 which means you split your time each week between a hospital placement and general practice.

There is a compulsory education programme (Vocational Training Scheme teaching) that runs on Wednesday afternoons. It runs for 30 weeks of the year, split across three terms. The teaching programme is based on the GP curriculum developed by the Royal College of General Practitioners.
This is the same curriculum that forms the bases of the MRCGP (the assessment procedure for all GP trainees introduced from August 2007). By the end of the three years, trainees will have to meet all the requirements of the MRCGP in order to obtain your certificate of completion of training (CCT).
In addition, there are optional training opportunities that trainees with a particular interest in a specialty may wish to undertake. These include the diploma of the royal college of obstetricians and gynaecologists, diploma of child heath, diploma of family planning and sexual health, diploma in geriatric medicine and certificate in palliative care.
Ipswich has around 20 GP practices that are linked to the GP training programme. Each practice has 1 or more GP trainers. Trainees will be allocated a programme director as their mentor when they join the scheme in addition to an educational supervisor. Your educational supervisor is a useful source of support during hospital posts and to help keep in touch with primary care, whilst your mentor is there to help with any problems you might have through your training.
Colchester has around 10 GP practises that are linked to the GP training programme. Each practice has 1 or more GP trainers. As in Ipswich, trainees will be allocated an educational supervisor who will offer support with career planning throughout training. They will also help you to keep in touch with primary care whilst you are on hospital placement.


I joined the GP training scheme in Colchester due to its proximity to where I live and luckily ended up in a lovely program.
Initially, we were introduced to the Training Programme Directors (TPDs) and were informed about what it is like to be a GP and the opportunities the training program offered us. From then on, we were exposed to a wide range of specialties from ST1, not only in the hospital but also in the community. The introduction of the Integrated training Posts (ITP) program also benefited us as GP trainees, giving us a good knowledge base and ideas of the opportunities available to GPs.
We are encouraged to give feedback at our weekly Vocational Training Scheme (VTS) teaching sessions.
This feedback is discussed regularly and is acted on to keep it trainee centred. Being a Trainee representative, I can see the enthusiasm from the TPDs to constantly keep improving our overall experience in GP training with the focus not only on the exams but the knowledge we would need in our future careers
The scheme covers a wide area and includes people from all walks of life and socioeconomic standing, which as a GP, would be ideal. I would be so bold as to say there is something here for everyone making it a lovely area to live in and a training program I would happily recommend.
 Dr Abishek Gregory Britto, GP trainee Colchester
Dr Abishek Gregory Britto, GP trainee Colchester
Dental Foundation Training is a oneyear vocational training programme after Dental school. It’s purpose is to “enhance clinical and administrative competence and promote high standards through relevant postgraduate training and meet the needs of general dental practice in the NHS”.
Foundation Dentists spend a year in approved practices undertaking training. It introduces gradate dentists to general dental practice under the supervision of an
experienced dentist ‘educational supervisor’ . In some practices, two dentists share this role. The ESs provide supervision, help where needed, and deliver tutorials.
The two groups attend a number of courses online, at Cambridge and at Ipswich. Ipswich provides the hands on teaching courses, covering topics such as Oral surgery and Prosthetics. This helps them if they want to select a specialty and reinforce practical skills that they may not have covered since their degree course.

“Explanations were excellent and detailed. Tasks were well demonstrated and explained. Feedback and evaluations of tasks were invaluable. All staff extremely were approachable, friendly and knowledgeable. I liked the fact that the course was very hands-on, with valuable feedback being given, along with demonstrations.”

“The hands-on portion of removing bone, raising flaps and sectioning teeth was extremely relevant and useful as I had not done any surgical extractions at university.”
“The lecturers are really useful and it was amazing to also look into some of the real life cases that they carried out on their own patients.”


The acute medicine departments at Ipswich and Colchester hospital provide a high-quality, rapid medical assessment service to a population of over 800,000. The acute medical team work closely with General Practitioners (GPs) and the Emergency Department to review and manage patients who present with a wide range of medical conditions.

The acute medicine team comprises of a large multidisciplinary team of consultants, junior doctors, advanced nurse and care practitioners, senior nurses and therapy teams. There are 7 consultants and 4 registrars. There is also a large team of foundation, ACCS, GP trainees and IMT doctors.
The department at Ipswich hospital comprises of an emergency assessment unit (EAU), and an ambulatory same-day emergency care unit (AMSDEC). There are also 6 acute medicine wards with 28beds each. The acute medicine team provides a consultant-led service from 8am-8pm, 7 days a week. This includes daily consultantled ward rounds.
The acute medicine team at Colchester hospital is made up of several trust grade registrars and IMT 3 doctors. Alongside them is a large team of consultants, ACCS, GP trainees, IMT1/2 and foundation doctors.
The acute medicine department is responsible for the care of all patients in the emergency assessment unit (EAU) and the ambulatory same-day emergency care unit (AMSDEC). This includes all patients on the acute-take who have been referred by the emergency department or by the GP.
A typical day for a registrar involves reviewing patients on EAU who have already been seen on a post-take ward round. Typically, this is around 20-25 patients a day. Other days, responsibilities include clerking patients, accepting referrals and managing the acute medical take.

The acute medical take has a high turnover of patients with varied pathology. Trainees have the opportunity to manage the acute take either with direct or indirect supervision. Higher specialty trainees will also hold the medical referral bleep from the emergency department and out-of-hours GPs.


At Ipswich, there is weekly departmental teaching where trainees take it in turns to teach on a topic of interest and present complex cases. Colchester, provides the majority of their teaching at the bedside and prioritises learning in this way. There is also the opportunity to teach medical students that attend the department on placement.
AMSDEC offers important training opportunities for managing patients in a clinic/outpatient setting.


There are daily consultantled ward rounds which enable opportunities for bedside teaching and work based assessments, including case-based discussions and acute care assessment tools (ACAT).
On the acute medical wards there is always a high volume of clinical procedures including lumbar puncture, abdominal paracentesis and chest drains. Consultants and senior registrars are readily available to support with these.

The anaesthetic departments at Ipswich and Colchester hospital provide a comprehensive 24/7 anaesthetic service for upper/lower GI, urology, ENT, obstetrics, gynaeoncology, orthopaedics, vascular and spinal surgery. There are also elective theatre lists which include experience in paediatrics.
The anaesthetics team at Ipswich Hospital currently have 32 generalist anaesthetic consultants, 9 critical care anaesthetic consultants, 7 speciality doctors and up to 30 junior doctors (anaesthetic core trainees, speciality trainees, ICM, ACCS, DREEM IMT and FY1 doctors).
There are 19 operating theatres at Ipswich Hospital and a 14-bed critical care unit that has easily accessible extension area to cohort Covid-19 patients. There is a dedicated 4 theatre day surgery unit with an excellent paediatric area.
Ipswich is a regional tertiary referral centre for spinal surgery and gynaeoncology which presents many training opportunities for managing complex cases.
The anaesthetics team at Colchester hospital is made up of a dedicated team of consultants, SAS doctors, higher speciality and core trainees.
The anaesthetics team provide a service for all medical and surgical specialities within the hospital including emergency and elective obstetrics and an acute pain service.
A typical day for a trainee starts at 07:30 with pre-assessment of patients for theatre. There is also a morning MDT meeting with the theatre team. Trainees report excellent opportunities in intraoperative patient management and post-operative pain management.
The anaesthetic department is friendly and extremely supportive. There is a lot of hands-on teaching and learning, both in and out of the theatre environment.

Dr Ruth Warne, ST1 AACS
There are excellent training opportunities for upper/lower GI, urology, ENT, gynae-oncology, obstetrics, orthopaedics, complex spinal surgery, trauma and regional anaesthesia. There is also an excellent acute pain service.
Orthopaedics, trauma and spines:

Ipswich is a regional tertiary referral centre for spinal surgery, with 2 lists per day and a wide variety of interesting spinal operating including posterior cervical surgery, ALIF/XLIF and scoliosis surgery.
ENT, oral surgery:
There are plenty of training opportunities for difficult airway management in oral surgery. Techniques used include jet ventilation, videolaryngoscopes and fibre-optic airway management.
Lower GI & Urology: Ipswich and Colchester perform major lower GI surgery and nephrectomies as well as adrenalectomy procedures. We have recently started using robotics for lower GI and gynaeoncology surgery.
Regional anaesthesia and acute pain service:

The anaesthetics team are keen on using regional anaesthesia offering plenty of upper and lower limb block opportunities. The acute pain team site erector spinae catheters for patients with rib fractures. Recuts sheath catheters are used for the majority of laparotomy patients.


Obstetrics & Gynae-oncology: Ipswich is the tertiary referral centre for gynae-oncology which presents many opportunities for managing complex patients and major haemorrhage. They also have approximately 4000 deliveries per year with a 23% LSCS rate.



Day Surgery:
Ipswich treat approximately 5,000 adult and paediatric patients per year, undergoing surgical and investigative procedures requiring local, regional and general anaesthesia. There are a large number of paediatric patients (approx. 1200 per year) between the ages of 1 year and 16 years operated on in this area.
The cardiology departments at Ipswich and Colchester Hospital work to diagnose and treat a wide variety of cardiac pathology. Both sites have dedicated cardiac catheter laboratories where they provide a wide range of invasive and non-invasive diagnostic and therapeutic procedures.
The cardiology team is made up of 8 consultants, 3 deanery higher specialty registrar trainees with national training numbers and 1 IMT3 doctor. There are also several foundation doctors and GP trainees.
The department comprises of a 24 bedded inpatient ward with 10 coronary care unit beds. There is a dedicated cardiac catheter laboratory where a wide range of invasive diagnostic and therapeutic procedures are conducted. A limited number of primary percutaneous coronary interventions (PCI) are conducted within normal working hours. Out of hours primary PCI is sent to Papworth hospital, Cambridge.
The cardiology team at Colchester hospital is made up of 8 full-time consultants, 1 associate specialist doctor, 2 deanery higher speciality registrar trainees with national training numbers, 1 cardiology fellow and 8 IMT, GP trainees and foundation doctors.
The department comprises of a 29 bedded inpatient ward with 18 coronary care unit beds. There is a newly built cardiac catheter laboratory where a wide range of invasive diagnostic and therapeutic procedures are provided. The imaging department also offers a wide range of non-invasive cardiac investigations.


The cardiac catheter laboratory undertakes a high volume of procedures including diagnostic coronary angiograms, implantation of pacemakers, pericardial drainage, and DC cardioversions. The imaging department is equally busy offering a wide range of noninvasive cardiac investigations including transthoracic and transoesophageal echocardiogram, CT coronary angiogram, bubble contrast study and Dobutamine Stress echocardiogram. Ipswich also has a cardiac MRI unit which runs twice a week.
Although there is no cardiothoracic surgery on site, trainees are encouraged to attend the weekly specialist MDT meeting with the cardiothoracic surgeons. This enables discussion of complex cases. There is also a monthly regional clinical governance meeting with regular presentations on emerging research projects. This gives trainees opportunities to present and be involved with research projects.

Higher speciality trainees have regularly scheduled protected time to attend the cardiac catheter laboratory, cardiology clinics and imaging investigations including echocardiography and myocardial perfusion imaging. Trainees report that this is a particular strength of the department and helps with achieving competencies in a wide range of skills.

There are 4 care of elderly inpatient wards at Ipswich hospital, each with 28 beds. Out of these wards, 2 are complex elderly wards, 1 is a short stay ward, and 1 is a stroke ward. In addition to these wards, there is 1 orthogeriatric ward (staffed with orthopaedic junior doctors).
The care of elderly teams at Ipswich and Colchester hospital are some of the largest departments in the hospital. During a patient’s stay, there is great emphasis on prompt diagnosis and multidisciplinary rehabilitation. Maintaining dignity and individual privacy is extremely important and experienced therapy staff work closely with the medical staff to achieve this.
The care of the elderly team at Ipswich Hospital is made up of 10 consultants (including 1 orthogeriatrics consultant and 3 stroke consultants). There are 2 permanent speciality doctors and 6 speciality nurses (frailty and Parkinson’s disease). There are also 3 higher speciality trainees and 14 junior doctors (GP trainees, IMT doctors and foundation doctors).
There are 3 community rehabilitation hospitals (Aldeburgh, Felixstowe and Bluebird Lodge). Higher Speciality trainees have a rotation based in these community hospitals.

The care of the elderly team at Colchester Hospital is made up of a large multidisciplinary team. Comprehensive geriatric assessment and care is provided by consultants and junior doctors supported by a team of dedicated and experienced specialist nurses and therapists, with input from borough-based social care practitioners.
There are 4 care of the elderly wards (28 to 36 beds on each ward). A typical day consists of a morning board round with the multidisciplinary team, to enable early discharge planning and rehabilitation plans. This is then followed by a ward round. New or unwell patients are reviewed by a consultant and the remaining patients are reviewed by junior doctors. Higher speciality trainees will usually review the care of the elderly outliers and any new referrals.
Care of the elderly medicine benefits from a wide variety of pathology which allows trainees to gain experience in managing a broad range of conditions. These include frailty, multimorbidity, polypharmacy, falls, dementia, delirium and end of life care. Care of the elderly is not only about prescribing medications and treating illnesses, but it is also about assessing patient’s needs, making them comfortable and keeping their relatives up to date.
Alongside the inpatient setting, there are a large variety of outpatient clinics that trainees are encouraged to attend. These include Parkinson’s disease, memory clinic, movement disorders. Higher speciality trainees will have clinics scheduled into their rota with the expectation to lead clinics. Internal medical trainees (IMT) will also have scheduled clinic time in their rota. They will have the opportunity to review patients with the support of consultants.
There is a daily rapid assessment TIA clinic which provides opportunities for trainees to review and manage patients who have been referred by the emergency department and GPs. There is also a frailty assessment base clinic which enables trainees to review and manage acute pathology with the aim to prevent admissions, where possible.

There is weekly lunchtime care of the elderly teaching, Each trainee takes it in turns to present at these teaching sessions. This departmental teaching covers the important topics relating to care of the elderly.

There are monthly M&Ms to ensure patient safety is at the center of the department. Quality improvement projects are also encouraged. Trainees are encouraged to support the teaching of medical students working in the department, predominantly those in 3rd to 5th year of training.

The emergency departments at Ipswich and Colchester Hospitals serve a combined catchment population of around 800,000 people. They provide comprehensive 24/7 services and offer a wealth of training opportunities for their trainees.

The Emergency Department at Ipswich Hospital is made up of a large multidisciplinary team of doctors, nurses and advanced care practitioners (ACPs). There are 14 consultants, 9 registrars, 9 CT1 doctors (3 ACCS) and 6 FY2 doctors. In addition, there are 11 ACPs, 5 regular senior locum doctors and 10 ENPs.
Ipswich has a catchment population of around 400,000 and sees around 80,000 patients a year (15% of these are paediatrics). The emergency department is made up of a dedicated resus area and a major and minor treatment area. There are 6 resus beds and 13 major cubicles. There are also 4 dedicated paediatric cubicles and a paediatric resus bay. There are x-ray facilities within the department.
Additionally, there is a purposebuilt urgent treatment center which sees minor injuries and fractures. This is predominantly staffed by ENPs. There is instant access to x-ray facilities and orthopaedic technicians for fracture casting.
The Emergency Department at Colchester Hospital is made up of a large multidisciplinary team. There are 7 registrars, 2 core trainees and 8 foundation doctors (FY2). In addition, there are several trust grade doctors.
Colchester has a catchment population of around 370,000 and sees around 14,000 patients a month. The emergency department is made up of a resus area and a major and minor treatment area. There is also a dedicated paediatric emergency department.
Each shift in the emergency department provides a broad range of training opportunities, particularly on shifts in resus. Procedures include chest drains, fracture manipulation, external pacing and lumbar puncture. There are also 2 ultrasound machines available in the department. There are consultants and senior registrars readily available to support with these.


The department has its own dedicated resus team which responds to crash calls, trauma calls and leads cardiac arrests. The department runs courses in Advanced Trauma Life Support (ATLS), Advanced Life Support (ALS) and Advance Paediatric Life Support Courses (APLS). In addition, there are courses available in ultrasound including FAST scanner, Chest drain insertion, TruPICC and Central line insertion.
There is weekly simulation-based training, with a focus on acute management of common conditions. Simulation teaching covers both adults and paediatrics. Supporting professional activities (SPA) days are available to attend fracture clinics, urgent treatment centre, eye clinics, paediatric ED and theatres to improve airway skills.
Ipswich has weekly departmental teaching on a Wednesday. This is tailored to each level of training with separate teaching for junior and senior trainees. In addition, there are weekly clinical based discussion slots that are facilitated by consultants to allow review of complex cases.


Colchester hospital has a longstanding involvement in high quality research including: the SHED study and TERNACS next year.

The diabetes and endocrine team is a busy department that offers extensive experience in a supportive MDT. Inpatient work is predominantly general internal medicine with some specialist work, especially related to the diabetic foot and endocrine emergencies. In the outpatient setting, there is extensive opportunity to experience a wide range of endocrine conditions and become experienced in diabetic management
There are 5 consultants, 2 higher specialty trainees with training numbers and an IMT3 doctor. There are also several foundation doctors and GP trainees that rotate through the specialty.
There is currently one 28-bed inpatient diabetes and endocrine ward. There are some specialist diabetes and endocrinology inpatients with the remaining patients being general medicine. The department runs a ‘a consultant of the week’ model with one consultant covering the ward with registrar support, offering daily ward rounds and excellent support to the team.
As endocrinology and diabetes is a predominantly an outpatient specialty, there are extensive outpatient clinics to attend including general diabetes and endocrinology clinics, as well as more specialist ones (insulin pump, diabetic foot and diabetic antenatal clinics).
Education is fundamental to the diabetes and endocrinology team. Trainees are released to attend the teaching opportunities offered within the trust. Additionally, within the department, there are multidisciplinary team meetings with educational content. There is also a pituitary MDT based at Addenbrooke’s Hospital.
There are plenty of opportunities to work with members of the multidisciplinary team including endocrine nurses, inpatient and outpatient diabetes specialist nurses, dietitians and podiatrists. The team also works very closely with the vascular surgical team and there is an MDT meeting with the interventional radiologists.



The department has a strong track record in both original and industry led research especially in diabetes. Dr Sharma leads this research program. Trainees are welcome to be involved if they have a particular interest in this area.

The gastroenterology departments at Ipswich and Colchester Hospital provide a variety of services for the management of gastrointestinal disorders including inflammatory bowel disease, oesophageal diseases, hepato-pancreatic diseases, small bowel disorders and nutrition management. They also provide bowel cancer screening and health promotion programs.
The gastroenterology department at Ipswich hospital has an inpatient 28-bed ward that is shared with general surgery. There is also a JAG accredited, dedicated endoscopy unit for inpatient and outpatient, diagnostic and therapeutic procedures.
A major benefit of working in gastroenterology is that it allows collaborations with the multidisciplinary team (MDT) such radiologists, pathologists,

GI surgeons, liver transplant teams, clinical nurse specialists, dieticians, pharmacists and psychologists. The department liaises closely with tertiary units within the East of England and beyond for outreach cancer clinics, liver and intestinal transplantation.
The gastroenterology team at Colchester Hospital is made up of 5 consultants, 2 specialty registrars with training numbers and up to 8 junior doctors (IMT, FY2 and FY1 doctors).
There is a 28-bed inpatient ward that is shared with the renal team. In addition, there is a dedicated endoscopy suite which undertakes flexible sigmoidoscopy, gastroscopy, ERCP, endoscopic ultrasound and colonoscopy.
A typical day for a higher specialty trainee starts with a morning board round, followed by a ward round. The afternoon consists of seeing ward referrals, endoscopy or clinics. Trainees have 2 clinics and 2 endoscopy lists scheduled each week with the opportunity to attend more.
ST4 (first year) trainees at Ipswich and Colchester hospitals will receive intensive endoscopy training. This enables trainees to complete their competence in endoscopy by the end of their first year. At Colchester, there is also an onsite simulation suite (ICENI) which provides courses in endoscopy. These simulation facilities can be accessed out of hours for practice.
There are opportunities to take part in national, regional and local audits with excellent guidance. Junior doctors are encouraged and supported to participate in different leadership roles. Our consultants are recognised external examiners and readily give teaching to help prepare trainees for examinations.


The dedicated endoscopy units provide services for diagnostic and therapeutic procedures for both upper gastrointestinal (stents, dilatation, PEG, NJ, push enteroscopy),and lower gastrointestinal (ERCP, endoscopic ultrasound, bowel cancer screening service, capsule endoscopy). This provides a wide range of opportunities with guaranteed weekly training lists. Training lists can also be tailored towards an area of interest that a trainee may have, for example ERCP.
Trainees have the opportunity to participate in weekly gastroenterology radiology meetings and the upper GI and hepatobiliary MDTs. There is also the monthly gastroenterology journal club and the clinical governance/M&M meetings. Trainees are encouraged to present at these.

The opportunities available to trainees are limitless. We are supported academically, and clinically with bedside teaching, case-based discussions and taking part in national, regional and local audits with excellent guidance. We are also supported with bedside


hands-on procedures such as paracentesis. Junior doctors are encouraged and supported in participation in different leadership roles. Our consultants are recognised external examiners and readily provide teaching to give trainees an edge to ace their examinations.
Dr Obinna Kevin Onwuteaka, ST4 Ipswich HospitalThe oncology team at Ipswich hospital comprises of 3 higher specialty trainees with training numbers.
There is one inpatient ward with 32 beds which is shared with haematology. There is also a day unit onsite which provides chemotherapy and radiotherapy.

A typical day for an oncology registrar includes half a day of clinic and half a day of radiation therapy planning. One day a week trainees will be expected to cover the day unit and see the acute oncology service referrals.
There is weekly Tuesday morning teaching in which the oncology team take it in turns to teach. Trainees are also encouraged to participate in the multidisciplinary team meetings, the governance and audit meetings. The oncology department receive particularly good feedback for their support in teaching for FRCR exams.
Ipswich hospital benefits from having a new state-of-the-art breast care centre. The new centre has transformed the experience patients have when they come to hospital by bringing all elements of breast care under one roof – the clinic, the imaging department and hospital breast screening.

Colchester hospital has an onsite wellbeing centre which offers support and a peaceful space for those affected by cancer. It is a beautiful space with a serene interior and garden space. The Wellbeing Centre was funded entirely by donations to Colchester & Ipswich Hospitals Charity.


The dedicated critical care units (CCU) at Ipswich and Colchester Hospitals provide care for critically ill medical and surgical patients. The departments also provide higher level post-operative care for high-risk elective patients. Both units have the facilities to offer level 2-3 support for up to 14 patients at a time.
The CCU team is made up of 9 consultants and a large team of approximately 30 trainees (anaesthetic core trainees, speciality trainees, ICM, ACCS, DREEM, IMT and FY1 doctors). There are also 2 ACCPs who are a consistent presence in the department. They provide support to trainees in terms of process and policy as well as education.
There is a large nursing team providing expert and specialist care such as haemofiltration, inotropes and care of intubated patients.

The CCU is a 14-bed level 2 (single organ support) and level 3 (multiple organ support) unit that has easily accessible extension area to cohort Covid-19 patients.
In addition, the team provides support to the paediatricians to stabilise unwell children prior to retrieval by regional transfer teams. They also provide mutual aid to other critical care units in the East of England.
The CCU team is made up of 10 consultants and a large team of trainees including specialist registrars, core trainees, foundation doctors. Alongside this, there are critical care practitioners. The critical care unit is staffed daily by 7 junior doctors and 1 on-call consultant.
The CCU is a 14-bed level 2 and level 3 unit. A typical day on the critical care unit consists of a morning handover and ward round with plenty of training opportunities throughout the day. Both Ipswich and Colchester departments have the same computerized records system, Metavision. This allows for easy communication between the two hospitals. The front-end terminals allow easy access to images, ICE and TOXBASE and multidisciplinary department guidelines.
Intensive care medicine training requires trainees to become proficient in a wide range of procedures. Ipswich and Colchester sites offer plenty of opportunities and support to become competent in these procedures including central venous catheter insertion, arterial lines, intubation and extubation, and tracheostomy. Consultants are readily available to assist with these.

There are daily consultant-led ward rounds which enables regular bedside teaching and work-based assessments. Trainees are also expected to review patients independently and present their findings to consultants. As a result, trainees report they are able to achieve a large number of workbased assessments whilst working on the unit.
The consultants place an emphasis on good quality teaching. As a result, there is weekly departmental teaching which covers a wide range of topics including management of the acutely unwell patient, airway management and imaging techniques. In addition, trainees can volunteer to present in these teaching sessions.
Discussion about the most complex patients is held at the specialist multidisciplinary team meetings. Trainees are encouraged to attend these in order that they understand the complexities of decision making and ethical scenarios.



The CCU research team has an excellent track record of conducting, presenting and publishing clinical research in intensive care related topics. Colchester hospital participates in a number of important studies including the UK-ROX and SIGNET study.
Ipswich also has an active research programme mostly focused on the NIHR portfolio projects. They have a lead for research and are well supported by the Trust’s Research Nurses. They are keen for trainees to get involved in projects.

The neurology departments at Ipswich and Colchester Hospital offer comprehensive services for patients with disorders of the brain and nervous system. The team is complemented by an on-site neurophysiology team. They also have close links with the neurosurgical teams at Addenbrooke’s (Ipswich) and Queen’s Hospital (Colchester).
Neurology at Colchester hospital is predominantly an outpatient specialty with a wide range of clinics available to attend. There are also inpatient opportunities through seeing ward referrals alongside the consultant on-call.
The neurology team at Ipswich hospital is made up of 5 consultants, 1 higher speciality trainee, and 2 IMT doctors (who are shared with rheumatology).
The neurology department at Ipswich hospital benefits from having inpatient beds on a shared ward with general medicine. In addition, there is a wide range of outpatient clinics where the majority of neurology patients are managed.
Speaking from experience, Neurology registrar training at Ipswich is great! It has been my favourite DGH neurology rotation in the East of England region. The department is small, friendly and supportive, from our five consultants to our specialist nurses, secretaries and allied healthcare professionals. As a trainee, you really feel that you are part of a committed and caring multidisciplinary team full of colleagues who strive to do their best for patients and each other. The educational supervisors are very good and take registrar development seriously. If you are just starting your neurology training, you will find yourself very well supported.

Consultants are readily available to offer supervision, guidance and teaching, including on the daily consultant ward round and with each of the registrar clinics. Equally if you are more senior, the rotation provides an excellent opportunity to practice with increasing independence and explore some subspecialty interests. There is lots of scope and support if you wish to pursue a particular project. Overall, Ipswich is a great place to get stuck in to typical DGH neurology and I would highly recommend the rotation.


Ipswich hospital benefits from having both inpatient beds and outpatient clinics. This gives trainees exposure to a wide range of both acute and chronic neurological conditions. There is a daily consultant ward round for inpatients which is an excellent opportunity for teaching-based ward rounds and work-based assessments. Whilst Colchester hospital does not have allocated inpatient beds, there are plenty of opportunities to review neurology inpatients through ward referrals.
Registrars split their time between inpatient ward rounds and referrals, general neurology clinics and specialty clinics. One day a week is spent in Addenbrooke’s hospital, Cambridge, attending specialty clinics and the regional neurology academic meeting. Registrars are encouraged to shape their timetable based on their training needs. The day a week spent at Addenbrooke’s is largely selfdirected, and can prove invaluable in helping trainees tick off the more specialised areas of the curriculum (for example, attending clinics in neuropsychiatry, neurogenetics, syncope, sleep, and pain)
There is a wide range of subspeciality experiences on offer at Ipswich include an MDT muscle clinic, MDT motor neurone disease clinic, multiple sclerosis clinic, neurophysiology clinics, spasticity and dystonia clinics, and opportunities to visit the specialist neurological care and rehabilitation centre (Sue Ryder at The Chantry). Higher speciality trainees are expected to lead at least 2 clinics a week with the support of consultants.
In addition, at Ipswich hospital, there are specific teaching clinics for internal medicine trainees (IMT). Every Wednesday, there is a teaching clinic where IMT doctors are expected to see two new patients with the support of consultants. In addition, there is a lumbar puncture clinic which is an excellent opportunity to become proficient in lumbar puncture; a core part of the IMT curriculum.
Trainees within the neurology department report that there are generally low volumes of inpatients in neurology which allows a generous amount of time to take advantage of the wide range of training opportunities available. It also allows time for other career-developing activities.


The team at Colchester Hospital is made up of 12 consultants, 2 associate specialists, 7 higher specialist trainees, 4 advanced paediatric/neonatal nurse practitioners and 7 SHOs.
The pediatric and neonatal team at Ipswich Hospital comprises of 10 consultants, 2 associate specialist doctors, 4 advanced paediatric/neonatal nurse practitioners, 7 higher specialty registrars and 4 senior house officers (SHOs). There are also a number of foundation doctors and GP trainees who rotate through the specialty.
The paediatric department has one inpatient ward with 4 x level 1 HDU beds, a paediatric assessment unit (PAU) and a paediatric investigation unit (PIU). The team works closely with the paediatric emergency department and attends peadiatric resus calls in the dedicated resus bay.
The neonatal department includes a level 2 NICU, the delivery and postnatal wards. It is a busy and active service with up to 500 admissions a year.
Ipswich Hospital is in the process of a £7 million update of the paediatric ward and outpatients department, so that all children and families in the area can benefit from the new and improved space.

The paediatric department has one inpatient emergency ward, one elective ward and a children’s assessment unit (CAU). The CAU operates a 24-hour service and the elective ward is used for elective surgical admissions and paediatric investigations. The team works with the emergency department, attending resus calls in the dedicated paediatric resus area. The team will also see any children under the age of 1 year as direct referrals to paediatrics.
The neonatal department includes a level 2 NICU, delivery and postnatal wards.
Ipswich Hospital was rated “outstanding” by the CQC. They also have excellent 2021/22 GMC survey results with ratings above average in a number of domains.
The consultants at Ipswich and Colchester hospitals have a wide variety of specialist interests and have clinics that trainees are encouraged to join including endocrine, epilepsy, oncology, cardiology, allergy, cystic fibrosis and neonatal medicine. Trainees have protected clinic time allocated on their rota.

Simulations are organised for both paediatric and neonatal experience, making use of the dedicated high-tech simulation suite at Ipswich Hospital. Specialist courses such as ePALs are also run in the ICENI center.
A regular Child Health Programme is published every month giving details of meetings and teaching scheduled. There are twice weekly departmental teaching, monthly x-ray meetings, governance and audit meetings. Trainees are encouraged to present at these.
Ipswich hospital strongly welcomes medical students on their paediatric rotation, elective placements from local universities, and junior doctors looking for exposure to paediatrics as a speciality on taster weeks. The department can be contacted directly to make inquiries.
I have been working at Ipswich Hospital for the last eight years, which should give you an idea that it is really a great place to work. Last year, I spent 6 months working as trust grade doctor in paediatrics. I enjoyed this so much that I decided to enter paediatric specialty training at Ipswich.
The department has been a great place to start my training. One advantage of working in a district general hospital is the close knit team, it doesn’t take long to get to know everyone you work with.
Getting to know my seniors has meant they are able to recognise my abilities
and limitations, allowing them to tailor the support and training they give me. I’ve been encouraged to undertake practical procedures, given autonomy to assess and make plans for patients, and the support to feel confident to do so safely.

Another advantage of working in a small community is that you quickly get to know many of the patients in the region. Building relationships with patients and their families like this is one of my favourite aspects of paediatrics.
Dr Robert Mooney, ST1 Ipswich HospitalAll new radiology trainees (ST1) receive training at the East of England Imaging Academy for the first rotation (4 months). This is a dedicated training facility which gives an introduction to radiology training. It teaches on important topics such as anatomy and physics. ST1 trainees will then start training in the hospital setting from the 2nd rotation (December).
The radiology departments at Ipswich and Colchester hospital provide a comprehensive reporting and vetting service for a wide range of imaging modalities including ultrasound, x-ray, CT and MRI. Both sites also have active interventional radiology departments.
The radiology teams at both hospitals comprise of a large multidisciplinary team of consultants, higher specialty trainees, radiographers, imaging assistants and nurses. At Ipswich hospital, there are 4 radiology higher specialty registrars with training numbers. At Colchester Hospital, there are 3 higher specialty trainees with training numbers. Trainees report feeling well supported by the consultants within the departments.
Once trainees return to the hospital, the majority of their time is spent within the radiology department. A typical day for a trainee involves reporting a variety of scans including x-rays, CT scans, MRI and nuclear medicine studies.
It also includes performing and reporting a range of ultrasound scans which enable them to gain confidence with this imaging modality. During duty sessions, the trainee will also be involved in vetting and approving scans. All reports are checked by consultants before verification which creates a supportive environment to learn in

There is weekly teaching for trainees. The main focus of these teaching sessions is to review and discuss interesting cases, different pathologies and management plans. Trainees will also have the opportunity to present during these sessions. In addition, the radiology team participates in MDT discussions for a number of specialties
. There are plenty of training opportunities available within the interventional radiology department which conducts a high volume of procedures including ultrasound or CT guided biopsies, drain insertions and ablations.

I am very fortunate to be a part of such an amazing team in Radiology department at Ipswich Hospital.
I have learnt a lot from all members of the team during my training and I have been developing skills in a range of different modalities such as plain films, ultrasound, CT and MRI by interpreting and discussing challenging cases with consultants and experienced members of the team.
Every day I have the opportunity to learn different pathologies through a variety of imaging modalities in
1-2-1 and small group sessions and regular well-balanced teaching.


The most enjoyable part of the job is to contribute to the correct diagnosis for a patient, which is the main reason why I chose this field in the first place.
We also have a great opportunities to work on different audit and quality improvement projects to improve the performance of the department.
 Dr Simin Arfa, ST2 Ipswich Hospital
Dr Simin Arfa, ST2 Ipswich Hospital

The renal medicine departments at Ipswich and Colchester Hospital provide a comprehensive service for a wide range of renal pathology including chronic kidney disease, nephrotic syndromes and renal failure. Both hospitals have onsite facilities for dialysis.
The renal medicine team at Ipswich Hospital is made up of 5 consultants, 4 renal specialist nurses, 2 higher speciality trainees with training numbers and 4 IMT, GP trainees and foundation doctors.
There is one 28-bed inpatient ward shared with the diabetes and endocrinology team. There is also a specialised renal unit on site where both the haemodialysis and home therapy teams operate from.
The home therapy team manages both home haemodialysis and peritoneal dialysis. The haemodialysis team (renal specialist nurses) manage the dialysis unit which runs 3 shifts a day; morning, afternoon and twilight. There is also another small unit at Aldeburgh hospital.
The renal medicine team at Colchester Hospital is made up of 4 consultants, 1 trust grade registrar and 4 IMT, GP trainees and foundation doctors.
There is one 29-bed inpatient ward shared with the gastroenterology team. There is also a 3-bed dialysis unit on the ward that is available for use of inpatients. The renal specialist nurses mange this unit.

There are a wide range of training opportunities available for trainees in the inpatient and outpatient settings. A typical day for trainees involves a consultant-led ward round in the morning which allows for bed-side teaching and workbased assessments.
Trainees are encouraged to attend outpatient procedure lists. There are a number of procedures that are carried out including: renal biopsy, haemodialysis lines (temporary Vascath and permanent tunnelled catheters), and peritoneal dialysis catheters.




In the afternoon, trainees have the opportunity to see ward referrals or attend clinics. There are plenty of outpatient clinics to attend led by both consultants and renal nurse specialists. These include, transplant and transplant assessment clinics, general nephrology and CKD clinic. At Ipswich hospital, there are also weekly teaching clinics specifically for IMTs and higher speciality trainees. These enable trainees to review and assess patients in the clinic setting with the support of consultants.
The renal medicine team place an emphasis on high-quality teaching for trainees. Higher specialty trainees have weekly joint teaching across both hospitals which is broadcast online from Colchester Hospital. There is also a weekly renal MDT attended by the renal consultants, junior doctors, renal dieticians and representatives from each of the renal units (haemodialysis and home therapies). In addition, there is a monthly biopsy meeting where histology and patient management plans are discussed.
The Departments of Respiratory Medicine at Ipswich Hospital and Colchester Hospital work to diagnose and treat a wide range of lung conditions including cystic fibrosis, chronic obstructive lung disease, asthma, interstitial lung disease, lung cancer and sleeping disorders.

The respiratory medicine team is made up of 7 consultants, 2 higher specialty trainees, 3 internal medicine trainees and 4 foundation doctors. There are also 2 trust grade doctors, 1 physician associate and 3 respiratory nurses.
The department has one medical ward with 35 beds. The acute respiratory care unit (ARCU) is located here. A typical day on the ward starts with a multi-disciplinary board round, followed by ward rounds. Areas of specialist interest within the department include experience with non-invasive ventilation (NIV) on ARCU and exposure to pleural procedures (ultrasound, pleural taps and chest drains).
The respiratory medicine team compromises of 5 full time consultants and 2 higher specialist trainees with national training numbers. Alongside this there are 3 internal medical trainees, 1 general practice trainee, 2 foundation year trainees, and 1 trust grade doctor. There is also an advanced clinical practitioner.
The department comprises of a 25 bedded medical ward with respiratory expertise and a separate respiratory high dependency unit. This high dependency unit has 8 dedicated side rooms with frequent air changes, equipped with monitors to Intensive Care Unit (ICU) standard. Each of the rooms has the capacity to provide CPAP or NIV and there are also 8 Optiflow devices. The unit is staffed to HDU levels, and the highly qualified respiratory nurses initiate noninvasive ventilation, CPAP, Opitflow as well as care for patients with tracheostomy tubes.
The department is a positive outlier for clinical supervision (98%) and educational governance (78%). As well as achieving positive feedback in other areas: overall satisfaction (85%), supportive environment (80%).
Trainees are encouraged to attend outpatient clinics. These are in the chest clinic which provides immediate access to lung function, chest radiography and cardiology. There is also a well-established sleep and home NIV service, and a specialist asthma and interstitial lung disease clinic. In addition, at Colchester, there is a a training clinic covering acute respiratory outpatient presentations called the ‘HOT’ clinic which provides excellent training opportunities for IMT and SpR trainees.
Bronchoscopy is another training opportunity. Lists are carried out twice a week with both video and fibreoptic bronchoscopes. The Endobronchial Ultrasound (EBUS) service has been running since 2012. Linear EBUS is currently used and there is the hope to expand the physician led cancer diagnostics with the introduction of ultrasound guided biopsy, radial EBUS and medical thoracoscopy.
There is a weekly clinic for the outpatient management of pleural effusions. Trainees can attend these for teaching and to develop procedural skills which is a core part of the IMT and higher speciality curriculum.


Trainees are encouraged to participate in MDT meetings. There is a weekly MDT lung cancer/general radiology meeting with a thoracic surgeon, oncologist, pathologist, radiologist and lung cancer specialist nurses. Thoracic Surgery is provided elsewhere, however at Ipswich, there are thoracic surgery outpatient clinics for both new and follow up patients


“A very friendly and supportive department where you will learn a lot about general and respiratory medicine. We receive excellent feedback from trainees, and several have returned as registrars and consultants. The department has a great reputation for publishing case reports, audits, QIP projects and research studies. There are currently 2 research studies on going.“
The Ear, Nose and Throat (ENT) team works across Ipswich and Colchester hospitals, providing a shared service for a population of over 800,000 patients. The hospitals operate a ‘hot’ and ‘cold’ week system where each hospital takes it in turns to be on-call.
The ENT team at Ipswich Hospital comprises of 5 consultants, 3 higher specialty trainees, 2 SAS doctors, 2 GP trainees and 1 FY2 doctor. In addition, there are 5 advanced nurse practitioners who work closely with the junior doctors. The team works alongside allied health professionals such as the speech and language therapist and dieticians.
Junior doctors will receive an induction course at the start of their rotation. This introduces them to the day-to-day cases they would encounter and the minor procedures they would be expected to carry out during the rotation.
The department sees a wide variety of patients with varied pathology from pediatrics to adults. In particular, the department has a specialist interest in head and neck surgery. Trainees will see many patients with head and neck cancer who have had major surgery such as laryngectomy.
The ENT team at Colchester hospital is made up of 5 consultants, 5 SAS doctors, 2 higher specialty trainees with training numbers, 2 core surgical trainees and 6 foundation doctors and GP trainees.
Foundation doctors and core trainees at Colchester hospital benefit from participating in general surgery oncalls which allows for experience in a wide-range of surgical pathologies.
The ENT departments at Ipswich and Colchester are predominantly outpatient based. However, there is capacity for ENT patients on the surgical wards. There is a high volume of patients that attend for day cases. At Ipswich hospital, day cases are performed at the Rushmere Day Unit. At Colchester hospital, these are performed at the Elmstead Day Unit.

Ipswich and Colchester hospitals operate a ‘hot’ and ‘cold’ week system where each hospital takes it in turns to be on-call. As a result, the training opportunities differ each week. During ‘hot weeks’ (oncall weeks), the volume of patients seen is typically higher than on ‘cold weeks’.
During ‘hot weeks’ trainees will take referrals from GPs and the hospital that is on ‘cold week’. This allows for a lot of independence with appropriate support from senior doctors. The on-call SHO will take referrals, reviews patients and make initial management plans.
There are plenty of opportunities for trainees to practice clinical procedures. These include microsuction, popewick insertion/ removal, flexible nasendoscopy (FNE), nasal packing, nasal cautery, foreign body removal, quinsy aspiration and abscess incision and drainage. Foundation doctors and core trainees who are new to the department will receive an induction at the beginning of their placement which includes training in some of these procedures.
During ‘cold weeks’ the volume of inpatients is typically lower than on ‘hot weeks’. As a result, there are extra opportunities for career and portfolio development including attending theatre lists, clinics, audits and quality improvement projects.
Trainees have regular scheduled time to attend and lead clinics with the support of consultants. There are core trainee and registrar clinics scheduled for almost every afternoon.
“The ENT team are the kindest and most understanding team, they are always happy to help and teach. There is an excellent work-life balance with enough time for career development opportunities. ” Dr Rana Batir
 Trainee Feedback
Trainee Feedback
The general surgery departments at Ipswich and Colchester hospital provide high-quality surgical care for a wide range of surgical conditions of the upper GI tract, lower GI tract and hepatobiliary system. In order to gain CCT in general surgery, all trainees will acquire the knowledge, clinical and technical skills to obtain the competency levels defined for ST8.
There are 3 main surgical wards at Ipswich Hospital - 2 for emergency care and 1 for elective care. There is a new purpose-built surgical assessment unit where new admissions to the surgical department are reviewed.
The Ipswich surgical unit has subspeciality interest in inflammatory bowel disease/pouch surgery, pelvic floor surgery and colorectal cancer surgery including laparoscopic complete mesocolic resections and laparoscopic TME surgery for rectal cancers.
There are 3 higher specialty trainees with national training numbers at Colchester Hospital. There are also ICENI surgical fellows who are involved in surgical simulation training and clinical care (click here for more information).

The Colchester surgical department is a national training unit, undertaking around 200 laparoscopic colorectal resections per year. This work has been facilitated by the installation of 2 elective main theatres and one emergency state of the art, high definition, 3D ready laparoscopic theatre.
There are 3 main surgical wards with outliers and surgical inpatient referrals. In a typical week registrars usually cover ward rounds, theatres and clinics (minimum 4 sessions of theatre per week).
Higher specialty trainees report an excellent amount of time in theatre with a minimum of 4 theatre sessions per week. The Ipswich surgical unit has subspeciality interest in inflammatory bowel disease/pouch surgery, pelvic floor surgery and colorectal cancer surgery. There are also opportunities to be involved with cytoreductive surgery with gynae-oncology colleagues in complex gynaecology pelvic malignancies.
The Colchester surgical department is a national training unit, undertaking around 200 laparoscopic colorectal resections per year. This offers extensive opportunities to undergo dedicated laparoscopic modular training including CME, TME, TaTME and TAMIS, with the aim to perform independent resections at the end of training. There is also the opportunity to perform advanced laparoscopic procedures including bile duct exploration, splenectomy, TAPP, TEPP and incisional hernia repair.
Colchester Hospital has an onsite state-of-the-art surgical simulation center, the ICENI center. It is a globally recognised on-site training unit with simulation training including Intuitive Da Vinci XI simulation console and Inovus laparoscopy simulators. These training facilities are always accessible (including out of hours). More information about the ICENI center and the fellowships offered can be found by scanning the below QR code.
There is access to dedicated colonoscopy training lists recognized under the JAG training programme. Trainees report that the consultants are very keen to teach and provide excellent support with developing clinical and technical skills. There are also weekly surgical multi-disciplinary team meetings to attend.



The department of Obstetrics and Gynaecology (O&G) offers comprehensive services at both Ipswich and Colchester sites providing emergency 24/7 treatment for pregnant and nonpregnant women. This also includes a comprehensive elective service managing antenatal, gynae-oncology and fertility.

Ipswich O&G department facilities learning for a large number of trainees. There are currently 10 specialty registrars and nine core trainees. In addition, there are several foundation doctors and GP trainees. Ipswich is a busy District General Hospital (DGH) with around 4000 deliveries per annum. There is a large dedicated obstetrics and gynecology building with 3 theatres, 1 labour ward, 1 gynaecology ward and 1 post-natal ward. There is also a same-day gynae-assessment unit.
There are extensive training opportunities in open, laparoscopic and robotic surgery techniques. The department offers specialist services in minimal access surgery, gynaeoncology and urogynaecology. In addition, Ipswich hospital is one of the few hospitals in the East of England that has a very busy gynae-oncology center.
The state of art ICENI centre allows for training in laparoscopic hysterectomy and laparoscopic myomectomy, ovarian cystectomy excision of endometriosis and salpingotomy which is reinforced by live theatre sessions.
The department has invested heavily in high fidelity dry and wet lab hysteroscopic models and instruments. It also has augmented reality laparoscopic trainers with metrics for feedback regarding progress and learning.
There are training opportunities in fetal anomaly scanning, first trimester scanning, management fetal growth disorders and maternal and fetal doppler. Including exposure to invasive techniques in fetal medicine, advanced fetal imaging and fetal echocardiography.
There are a wide variety of outpatient clinics available including antenatal, gynaeoncology, fertility, termination of pregnancy, post-menopausal bleeding, colposcopy and menopause.
Ipswich Hospital runs a several national research projects which trainees are encouraged to participate in. Every trainee is also assigned a quality improvement project for which supervision is provided.

There is weekly department teaching that includes journal club once a month. In addition, there are perinatal M&M and aduit meetings monthly. Ipswich hospital also runs 3-4 regional teaching days and workshops. They also run RCOG recognized regional courses.



The ophthalmology departments at Ipswich and Colchester Hospital offer a comprehensive service for a wide range of ophthalmic conditions including glaucoma, age-related macular degeneration and cataracts. Ophthalmic surgery is performed at both sites.
There are 4 higher speciality trainees at Colchester Hospital. It is a wellsupported environment with consultants readily available to offer guidance many of whom trained in the East of England. There are also several fellows and Medical Training Initiative doctors.
There are 4 higher specialty trainees at Ipswich Hospital. Trainees are supported by 8 consultants and 2 associated specialist doctors. The team comprises of a large MDT including optometrists, orthoptists and nurses.
Ophthalmology is predominantly an outpatient specialty with most of the patients being seen in the main eye clinic. It is a large and busy department with clinics running most mornings and afternoons. Subspecialities include glaucoma, cornea, vitroretinal, medical retina, oculoplastics and paediatrics/oculomotility.
There are 2 ophthalmic theatres at the Ophthalmic Day Care Unit. This where most operations are performed including cataract surgery. The Clive Edelsten Retinal Suite is where macula clinics are held and where intravitreal injections are performed in a purposebuilt treatment room.
Most clinics and surgeries occur at the Primary Care Centre attached to Colchester Hospital. A small number of clinics also take place at Clacton Hospital a short 30-minute drive. Trainees are expected to undertake clinics with the supervision and support of consultants. Each room has dimmable lights, a full complement of lenses, a modern LED slit lamp and dual monitor computers. Imaging techniques readily available include Optos, OCT, visual fields and B-Scan.
There are 2 theatres at the Primary Care Centre which is where all local anaesthetic cases are performed. General anaesthetic cases take place at the Elmstead Day Unit at Colchester Hospital. Femto laser machines are frequently used and there are plenty of training opportunities to become proficient in using them.
As part of ophthalmology training in the East of England (EoE), new ST1 trainees benefit from a week-long induction course held at Norwich which is a great way to learn core clinical skills and knowledge. It helps prepare trainees before they start working and running clinics. It is also a great way to meet and socialise with other EoE trainees.
The ophthalmology departments take pride in offering high quality teaching. There is weekly departmental teaching in which trainees take turns in presenting a topic of interest and discuss complex cases.




Trainees will attend at least 2 theatre sessions a week with the opportunity for more. At Colchester hospital there is an onsite surgery simulation called EyeSi for cataract and vitreoretinal surgery. These facilities are accessible out of hours which enables trainees to practise surgical techniques at a time that is convenient for them.
Colchester has a particular subspeciality interest with a strong portfolio in minimally invasive, as well as advanced, glaucoma surgery, ophthalmic lasers and cataract surgery.
Ipswich Hospital has a particular focus in medical and surgical retina.
Research projects at Colchester are readily available especially in the sub-specialities vitreo-retinal and glaucoma. Colchester is the first in the country to pioneer a minimally invasive glaucoma surgery implant MINIject. The outcomes are currently being collated for analysis and publication.

Trauma and orthopedics (T&O) at Ipswich and Colchester Hospitals are busy and active departments that see a wide range of trauma and elective cases. There is also a spinal team that operates across both sites. Ipswich is a regional tertiary referral centre for spinal surgery.

The T&O team at Ipswich Hospital is comprised of 7 consultants and 6 higher speciality trainee registrars. There are also 4 advanced nurse practitioners (ANPs), 2 trust grade SHOs and several foundation doctors.
There are two 28-bed trauma wards, one of which is an orthogeriatrics ward. There are trauma theatre lists running every day.
The T&O team at Colchester Hospital is comprised of 14 consultants (3 knee, 4 hip, 3 upper limb, 3 foot and ankle and 1 spine), 2 associated specialists, 6 higher speciality trainee registrars and 1 core trainee. There are also 3 staff grade senior registrars and 6 trust grade SHOs.
There are two 32-bed trauma wards and one 32-bed elective ward. There are a large number of trauma and elective theatre cases every day. A dedicated Orthopaedic Centre is currently being built on site and will provide a specialist service with 6 theatres and 2 wards. This will provide an even higher volume of trauma and elective cases for trainees.
Colchester was awarded Training Hospital of the Year in the East of England Orthopaedic Training Survey two years in a row (2021 and 2022).
Trainer of the Year (Mr Loeffler) with 3 consultants as runners up for this award.
Trauma and orthopaedics is a busy department with a wide variety of trauma experience. The departments pride themselves on ensuring trainees have protected theatre time. Trainees report excellent opportunities in theatres which enable them to achieve exemplary logbook numbers. There are particular opportunities for arthroplasty including NAVIO/CORI Smith and Nephew robotic navigated total knee replacements.
There is regular departmental teaching including daily trauma meetings and weekly SHO teaching. There are opportunities for higher speciality trainees to teach at these weekly sessions. Trainees are also encouraged to attend specialist MDT meetings, these include hips, knees, foot and ankle, upper limb, and a specialist knee infection MDT.

Alongside theatre experience, at Colchester hospital there is an onsite simulation centre, ICENI, which runs numerous orthopaedic courses including soft tissue knee course, arthroscopy and compartment syndrome.

Trainees are encouraged to take part in audits and quality improvement projects with plenty of ideas and support available for these. There are monthly audit meetings where these can be presented.



The urology departments at Ipswich and Colchester Hospital provide surgical care for a wide range of urological conditions, across all age groups, including cancer diagnostics, kidney stones, incontinence and infective conditions.
The team is comprised of 15 consultants and 14 registrars. There are 2 core trainees/trust grade doctors and several foundation doctors.
There are 3 surgical wards at Colchester Hospital with up to 30 urology inpatients. In addition, registrars will see ward referrals for the rest of the hospital, including medical patients.

The urology departments at Ipswich and Colchester ensure there is plenty of dedicated time for developing surgical skills. There are training opportunities in using robots, laser and shockwave machines. Colchester trainees benefit from onsite simulation-based training in the ICENI center which includes a VR robot simulator. The department has particular strengths in upper tract laparoscopy, stones and reconstruction.
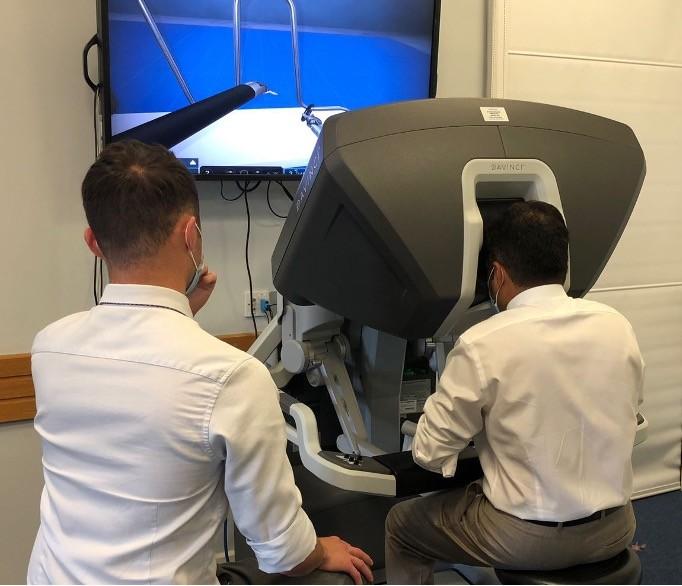
Training opportunities include experience in flexi-cystoscopy and difficult catheterization. There is also a wide variety of outpatient clinics to attend. Registrars will have the opportunity to lead clinics with the support of consultants.
The department encourages trainees to be involved in teaching. At Colchester, there is weekly departmental teaching where trainees are encouraged to present complex cases and interesting topics. There are also opportunities to teach the medical students that rotate through the department.


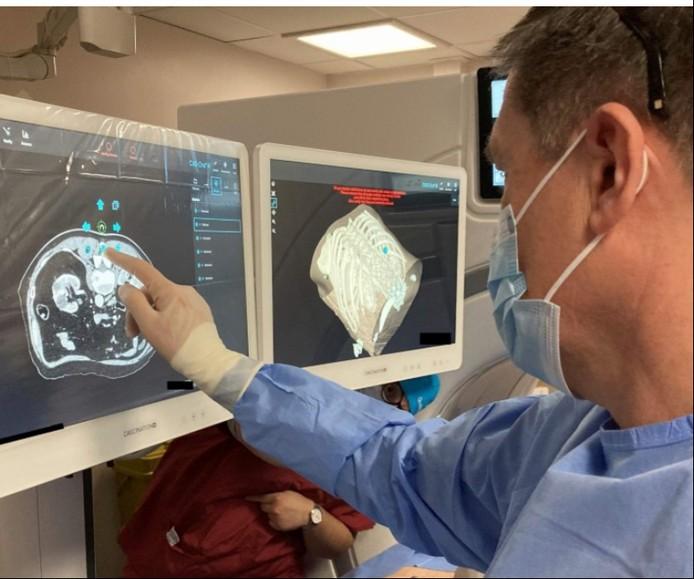
The Five Rivers Vascular Network operates across Colchester and Ipswich Hospital sites. Consultants and registrars work across both sites to provide high-quality care across the region. The team is made up of 7 consultants, 2 higher speciality trainees and 6 vascular specialist nurses. Colchester Hospital is the main centre and is responsible for managing complex cases. There are also occasional clinics at Clacton Community Hospital.
Colchester Hospital has an on-call consultant and registrar who manage the inpatients on the vascular ward and acute referrals for the week. There is a 24-hour vascular service here. Colchester Hospital also offers elective aortic surgery, day case surgery, interventional radiology, clinics and vascular studies.
Ipswich hospital has vascular services that run within normal working hours (08:00-17:00 Monday to Friday). Anything urgent outside of these hours is referred to the on call vascular registrar at Colchester Hospital. There is a designated consultant and registrar each day as well as a vascular nurse specialist. Ipswich hospital also benefits from having day case surgery, interventional radiology, vascular studies, and clinics.
There are plenty of opportunities to attend theatres and clinics at Colchester Hospital, and a list of these can be found on Medirota. Higher speciality trainees have dedicated time for these opportunities. Junior doctors are also encouraged to attend these if the ward jobs are completed. There are both emergency theatre lists and day case surgery including elective aortic surgery.
There are daily consultant led ward rounds and an additional weekly diabetic foot round. This enables opportunity for teachingbased ward rounds and wardbased assessments. Teaching and presenting opportunities are available at the monthly vascular clinical governance and M&M meetings (alternate months).


There is a weekly vascular MDT meeting across both Colchester and Ipswich sites involving the vascular surgeons, interventional radiologists and anaesthetists. This allows for discussionof the more complex cases.

I have been working at ESNEFT for the last 3 years. I completed my foundation training at Ipswich Hospital and worked as a clinical teaching fellow at Colchester Hospital. I have loved my time working in the trust and will be starting IMT here in August. ESNEFT is a friendly working environment with excellent learning opportunities. Suffolk is also a beautiful place to live and explore. There aren’t many places where you can get to the beach in 20 minutes and London in 1 hour. I look forward to working with you in the future!
With thanks to
Dr Julius Obilahi, Dr Siobhan King, Dr Benedict Scoones, Dr Stephen Cole, Dr Ruth Warne, Dr Paul Mallett, Dr Ginevra Bolino, Dr Kersten Morgan Bates, Dr Sohail Choksy, Dr Zafar Ullah, Dr Mark Scoote, Dr Tomi Ataiyero, Dr Alexandra Newman, Dr Sudharsan Nagendran, Dr Daniel Stanciu, Dr Craig Parkinson, Dr Duncan Fowler, Dr Louise Scovell, Dr Obinna Onwuteaka, Dr Georgios Chatzithanasis, Dr Thashi Thakshyanee, Dr Edward Riddell, Dr Pooja Pooja, Dr Clare Galton, Dr Deepti Marchment, Miss Haroona Khalil, Mr Deepak Vayalambrone, Dr Peta Lowin, Dr Omar Burgan, Mr Timothy Parratt, Dr Alexandra MacMillan, Dr Prathiba Pai, Dr Lauren Filby, Dr Duy Tu Nguyen, Dr James Hathorn, Dr Simin Arfa, Dr Jonathan Douse, Dr Rekha Badiger, Mr Andreas Hilgear, Mr Billy Wong, Dr Sophie Goddard, Dr Sandeep Singh, Dr Amar Odedra, Dr Pete Bishop, Dr Jonathan Campbell, Dr Izem Onadim, Dr Michelle Richardson, Dr Abishek Gregory Britto, Dr Robert Mooney, Dr Rana Batir, Mr Sam Datta, Miss Sunita Saha,Dr Yvette Adjei-Gyamfi, Dr Mehdi Syed, Dr Mohammed Osman, Deborah Lepley, Jo Wesley, Sally Foster, Nora Tester, Chris Brammar, Allys Walker

Trust Website
https://www.esneft.nhs.uk/
Health Education England
https://www.hee.nhs.uk/
ICENI centre

https://icenicentre.org/
Library services
https://esneft.libguides.com/homepage
Ipswich
https://allaboutipswich.com/#/ Colchester
https://www.visitcolchester.com/