Message From The Dean

Dear Alumni, Friends, and Colleagues, As we start the 2025–26 academic year, it will not only be a new beginning for our entering students, but also a new role for me, as I began serving as dean ad interim while the search for a permanent dean continues.
We also welcome a new chair of the department of medicine, Vicki Jackson, MD, MPH. Please read more about her on page 24.
This issue of BU Medicine has many articles of interest. Our cover story shines a light on student wellness and the many programs we offer to help medical and graduate students build resilience and community, including our Alumni Medical Library’s Little Free Library, which offers access to leisure reading and has been a great success on campus.
We celebrate our graduating classes of 2025; the annual faculty and staff award winners; the outstanding GMS student achievement awardees; the 40th anniversary of the Master’s in Medical Sciences program; the selection of our own Darrell Kotton, MD, as BU’s Innovator of the Year; the grant renewal for the landmark Framingham Heart Study; and the opening of the Rod Hochman Family Clinical Skills & Simulation Center.
We also feature the annual anatomy donors memorial service, which unites students and families as they pay tribute to these donors and thank them for their dedication to science and learning, and discuss the important roles of basic and clinical science in developing new trials and treatments.
We’ve highlighted what has been a long-term goal for the Medical Campus, a fitness center for our students. Thanks to a $1 million donation by Dean’s Advisory Board member Richard Catrambone, DMD, MD’92, and his wife Sophia Catrambone, the center is close to becoming a reality. We could use your help! To donate, please contact Associate Dean of Development Suzanne Maselli.
Our Giving section features the women’s health webinar, as well as stories on research supported by the Brain & Behavior Research Foundation and March of Dimes.
Boston University Medicine
Boston University Medicine is published by the Chobanian & Avedisian School of Medicine Communications Office.
Maria Ober
Associate Dean, Communications
design & production
Boston University Creative Services
contributing writers
Lisa Brown, Gina DiGravio, Doug Fraser, Sarah Rowan
photography
Doug Hyde Photography, Jake Mackey
Please direct any questions or comments to:
Maria Ober Communications Office
Boston University Medical Campus
85 East Newton Street, M810H Boston, MA 02118
P 617-358-7869 | E mpober@bu.edu 0825
Our Alumni section celebrates Rod Hochman, MD’79, CAS’79, who received the prestigious AHA Distinguished Service Award. It also announces our Alumni Award recipients. Stephanie Feldman, MA’10, MD’14, will receive the Emerging Leader Alumni Award. Larry Nichter, MD’78, CGS’71, CAS’73, will receive the Humanitarian Award. Ziv J. Haskal, MD’86, CAS’86, will receive the Distinguished Alumni Award, and Vladimir Kefalov, PhD’99, will receive the GMS Distinguished Alumni Award. Recipients will be recognized at a ceremony and luncheon on September 26 as part of our Alumni Weekend festivities.
Thank you to our donors and friends for your continued commitment to our school and your generous support of our outstanding students, faculty, and staff on the front lines of medicine and science.
Please enjoy this issue of BU Medicine. Best Regards,
Hee-Young Park, PhD
Dean Ad Interim, Chobanian & Avedisian School of Medicine Associate Dean of Faculty Affairs
Carolann S. Najarian Professor and Chair, Medical Sciences & Education Professor of Dermatology

MD, PhD, Master’s Graduates
Celebrate at Convocations
Ceremonies mark milestone leading to careers in healthcare

Vaibhav Gupta, MD’25, gives a thumbs-up as he takes his seat at the MD/PhD convocation ceremony May 15 at BU’s Track & Tennis Center.


In her welcoming remarks at the MD and PhD convocation on May 15 at BU’s Track & Tennis Center, Karen Antman, MD, BUMC provost and dean of the Chobanian & Avedisian School of Medicine, described the ceremony as one of the most joyous events in academic life.
“Our graduates gather together today with faculty, families, and friends to publicly recognize the credentials that they have earned and to celebrate their major life transition to the doctorate,” Antman said.
The afternoon MD and PhD convocation awarded 21 PhDs, 159 MDs, five MD/PhDs, one MD/MBA, one MD/JD, one MD/MPH, and two MD/OMFS (Oral Maxillofacial Surgery) degrees. Seventeen students graduated cum laude, five magna cum laude, and three—Keith Gagnon, Noelle Wojciechowski, and Melani Zuckerman— graduated with summa cum laude honors.
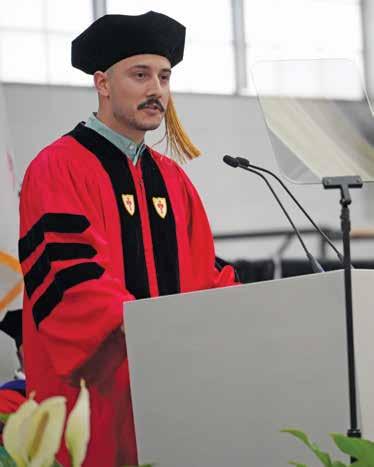
The PhD student speaker Jhonatan Henao Vasquez said that new graduates face political and societal uncertainties that will define the future of science and their place in it.
Grace Gibson (left) and Nyah Huntley toast their new status as MAMS graduates following the GMS convocation May 15.
Jake Mackey
Pulitzer Prize–winning journalist and physician Sheri Fink delivers the keynote address during the MD/PhD convocation. Fink is the author of the best-selling nonfiction book Five Days at Memorial
“In facing these challenges, we will do what we have always done. We will adapt. We will push forward. We will advocate for one another,” said Vasquez, who immigrated with his parents to the US from Colombia at two years old and is the first in his family to attend college.
“Our journey has taught us that uncertainty is not a roadblock; it is a call to action. It is an opportunity to innovate, to challenge the status quo, and to forge new paths.”
Richard Wu, chosen student speaker by his MD classmates, is the child of parents who immigrated to the US from China. As an undergraduate, Wu worked with AmeriCorps teaching underserved preschoolers. In medical school, he led teaching and mentorship student organizations and served as an advocate for students and patients.
“This is a class with a deep-rooted passion for justice in all domains of life,”
Wu told his classmates. “We must take our charge as the future of medicine seriously and not remain silent in the face of changing political tides, but dive into the uncomfortable truths…for the sake of our patients, our profession, and our world.”
Student-selected convocation speaker Sheri Fink, MD, PhD, is a best-selling author and the recipient of the 2010 Pulitzer Prize for her investigative reporting on deaths at New Orleans Memorial Medical Center during Hurricane Katrina.
“Never let go of the humility you have now as a student,” Fink advised graduates. “Maintaining humility will help you stay accountable to those you have the honor of serving. It’ll also give you the chance to keep growing and learning throughout your life.”
Earlier that morning, Graduate Medical Sciences (GMS) held its convocation at the
Newly minted MDs recite the Hippocratic Oath during the convocation ceremony.
same venue, bestowing 35 MA, 322 MS, and five combined degrees.
“Your hard work here has prepared you, and we are confident that you have the will, the courage, and the tools necessary to make a difference to all of our futures,” said C. James McKnight, PhD, associate provost and dean of GMS.
“We’ve grown into people who know how to show up, especially when it’s hard; who can make the leap, even when the outcome isn’t certain; who trust ourselves and believe in our ability to make it happen,” said Joshua Kidwell, one of three peer-chosen student speakers. A Master’s in Medical Sciences (MAMS) program graduate, Kidwell is heading to Creighton University School of Medicine to pursue his MD.
Born in Baghdad, Iraq, speaker Yousuf Al Naseri said his parents immigrated to the US to secure a better life for their children.

Raised in Maryland, Al Naseri graduated from the University of North Carolina Chapel Hill with a BS in biology, received his MS in oral health sciences at the GMS ceremony, and will matriculate into BU’s Henry M. Goldman School of Dental Medicine.
“Everything in life is a privilege. It is a privilege to study, to be able to invest in yourself, and it is a privilege that a school like Boston University takes a risk on you and opens its doors for you to succeed,” Naseri said. “During the difficult moments of your future studies, careers, or research endeavors, I urge everyone to shift their perspective from viewing tasks as obligations, to recognizing them as privileges.
“Shifting your mindset from ‘I have to’ to ‘I get to’ will transform your duties into opportunities.”
An immigrant from Guatemala, Cynthia Ordonez Salguero recalled being cautious of others and pretending everything was okay. “I developed all kinds of strategies to keep my family and me safe,” she said.
Graduating with an MA in mental health counseling, Salguero noted that her role as a therapist meant letting go of that mindset and embracing the world, her community, and the support available to her.
“I believe the future will mirror the life you’ve already known; beautiful and brutal, marked by soaring highs and crushing lows, sudden losses that shake you, and moments of joy that remind you why you keep going,” she said. “Your community will be your anchor, your strength, and your lifeline. As the old African proverb goes, ‘If you want to go fast, go alone. If you want to go far, go together.’” ●
“Our journey has taught us that uncertainty is not a roadblock; it is a call to action. It is an opportunity to innovate, to challenge the status quo, and to forge new paths.”
PHD
STUDENT SPEAKER JHONATAN HENAO
VASQUEZ
Jhonatan Henao Vasquez, PhD’25, speaks at the MD/PhD convocation.

Jake Mackey
GMS student speaker Yousuf Al Naseri, MS’25.

20th Annual McCahan Medical Campus Education Conference Focuses on Tradition, Transformation
BU Medical Campus Provost and Chobanian & Avedisian School of Medicine Dean
Karen Antman, MD, noted the passage of time in her opening remarks to both in-person and online attendees at the 20th annual McCahan Medical Campus Education Conference on May 21 at Hiebert Lounge.
“We started this conference 20 years ago and it seems like yesterday,” said Antman, who founded the event in her first year as dean of the medical school to honor John McCahan, MD, who served as the medical school’s associate dean of academic affairs for 30 years and was retiring after two years as interim medical school dean.
“It was so important to have a day to celebrate education, pedagogy, and research in education highlighted once a year, that we continued the tradition,” Antman said. “Our trainees pursuing PhDs and professional degrees are expected to assimilate vast amounts of information, and therefore we owe it to them to make it as easy as possible to do so.”
“It is one of the events that gets faculty from different disciplines together in the same room. It’s a wonderful, wonderful concept,” McCahan said.
Focused on Tradition & Transformation, this year’s conference included in-person and online workshops, roundtable discussions, educator awards, a research poster session,
and awards for research abstracts by faculty, staff, residents, fellows, and students.
Antman, who aims for BU to become even more widely recognized as a leader in healthcare education research, spoke about more training for students, staff, and faculty in leadership, communication, and conflict management skills.
“You need to be forming educational teams. Nobody in the research labs writes single-author papers,” she said.
“I think it’s really incredible to have the opportunity to present medical education research,” said third-year medical student Rachel Kim, MS’23, standing near her research poster with third-year medical student Samuel Roytburd. Kim noted how rewarding it was to pursue projects that may improve the experience of other medical students. Her research focused on evaluating medical student participation in a group educating heart failure patients on managing their condition to reduce hospital readmission.
“A lot of work is being done in silos, and this is a good way to break that down and
During McCahan Day, members of the BUMC community celebrate Karen Antman’s 20-year tenure as Medical Campus provost and medical school dean.
be able to see what others are doing and get feedback on your own research,” said Omar Siddiqi, MD, assistant professor of medicine in cardiovascular medicine and director of the Cardiovascular Medicine Fellowship Program.
Following the conference, Antman was honored by approximately 150 well-wishers, including 50 online, in the Instructional Building’s L4 Team-Based Learning Lab.
During Antman’s tenure, a transformative $100 million gift from Edward and Pamela Avedisian named the school the Chobanian & Avedisian School of Medicine and provided $50 million for medical student scholarships, $25 million for endowed professorships, and $25 million to the Avedisian Fund for Excellence, supporting research and teaching.
In addition, every floor of the Instructional Building was substantially renovated, a new medical student residence was built along with new research cores and centers, and the recently completed clinical skills
and simulation center was realized with a $10 million donation from Rod Hochman, MD, CAS’79, CAMED’79, and his wife Nancy Hochman, Sargent’77,’83.
Antman thanked donors, current and former chairs, deans, and financial and facilities leadership. “Looking at everyone here today, I can’t think of a group more dedicated to the school in so many ways,” she said.
University President Melissa Gilliam, MD, MPH, told Antman, “My favorite thing that I’ve observed about you is your tireless advocacy for students. The skills lab, the cost of education, the fitness center, the dorms—no matter what the topic, you are a student-first person. You bring wit, humor, kindness, and smarts to everything that you do. You and your enduring vision and your tireless efforts ensure that the future of this institution is very, very bright.” ●

JOHN MCCAHAN EDUCATOR AWARD WINNERS
Graduate Medical Sciences Faculty
Recognition Award
Elizabeth Duffy, MA, assistant professor of pathology & laboratory medicine
Henry M. Goldman Faculty Appreciation Award, Predoctoral Category
Jason Zeim, DMD, clinical instructor of general dentistry; director, predoctoral endodontics
Henry M. Goldman Faculty Appreciation Award, Postdoctoral Category
Robert McDonough, MA, instructor of health policy & health services research
Crest Oral-B P&G Professional
Oral Health Excellence in Teaching the Basic Sciences Award
Elizabeth Whitney, PhD, clinical associate professor
SPH Innovation Award, Educational
Marcia Pescador Jimenez, PhD, assistant professor of epidemiology
Chobanian & Avedisian SOM Affiliate Teaching Award
Olga Kuznetsova, MD, lecturer
Kaiser Permanente Silicon Valley Affiliate Teaching Award
Latasha Williams, MD
Best Student Abstract
“Enhancing Teaching Assistant Preparedness in Dental Education: Development and Delivery of a Feedback Training Module,” Mary Catherine Carroll, BA1, Marianne Jurasic, DMD, MPH1,2, Robert McDonough, MA1,2, Matthew Mara, DMD, EdD1,3
1Goldman School of Dental Medicine, 2Health Policy & Health Services Research, 3Global & Population Health
Best Resident Abstract
“Cross-cultural Adaptation of the Flipped Classroom Pedagogy in Dental Education,” Kevin Ma, DDS, Goldman School of Dental Medicine, Orthodontics and Dentofacial Orthopedics
Best Faculty/Staff Abstract
“The Thrive Liaison Initiative: Outreach to New Students to Increase Belongingness and Connection to Support Staff and Campus Resources,” *Mary Murphy-Phillips, MS1, *Julia Lanham, MPH2, *Carol Dolan, PhD3
*Co-First Authors 1School of Public Health, Graduate Student Life, 2Career & Practicum Office, 3Community Health Sciences
Karen Antman presents John McCahan with a prism in honor of his contributions to the BUMC community.
Mackey
Match Day Envelopes Reveal What the Future Holds for MD Students
On Friday, March 21, fourthyear medical students gathered for Match Day at George Sherman Union’s Metcalf Hall to learn which residency program they would join for the next three to seven years, training in their chosen specialties under the supervision of experienced physicians. At exactly noon, students opened their envelopes—and relief, happiness, and nervous anticipation all bubbled up into cries of excitement as students embraced family and friends in celebration.
“The days are long, but the years are short,” Medical Campus Provost and Dean Karen Antman, MD, told students.
“Not only do our faculty think that you are going to make outstanding physicians, but the programs that have chosen you think so as well,” she said.
Organized by the Student Affairs Office and the Student Match Day Committee, Match Day is an annual ritual repeated at all medical schools across the country on the third Friday in March as graduating medical students open white envelopes simultaneously. Since the 1950s, Match Day has relied upon an algorithm overseen by the National Resident Matching Program to match students to residency programs according to preference lists developed by the student and the programs.
“You have participated in research that will contribute to science across disciplines; you have spent hours in service to our Boston community, and you have done all of this while successfully completing your own requirements and coursework, taking board exams and managing life that continues to happen. You are more than ready for residency,” said Priya Garg, MD, associate dean of medical education.

“I love New York. It’s where my family is; it’s where I’m from. I’m so happy,” said Nisha Mathur, who celebrated her acceptance into an internal medicine residency at New York University Grossman School of Medicine with her extended family, including her grandmother, a physician who traveled from India for Match Day.
Mathur served as director of the Stop Shackling Patients Coalition, a BU medical and public health students and faculty-led collaborative effort to end universal shackling of prisoners while they receive medical treatment. She was inspired to enter medical school by her grandfather in India and her mother who immigrated to the US, both physicians caring for the underserved. As a child, she often spent summers in India with her grandparents.
“He was a pediatrician, and he had his clinic in the basement of his house. He used to have patients lined up down the street, and he would see them until very late,” Mathur said, adding that her grandfather sometimes wouldn’t join the family until the last patient left at midnight.
“That was my first exposure to medicine, and I think it really inspired me,” said Mathur, who also was influenced by the long-term relationships and the trust that her mother, a primary care doctor in the Bronx, had with her patients.
“I think both of those experiences combined to inspire me from a young age to know that this is what I want to do.”
It took Rachel Ingraham, who matched into the University of California, San Francisco-East Bay in general surgery, a little longer than most of her classmates to arrive at Match Day. Before entering medical school in 2019, the Minnesota native had spent four years as a research assistant at Brigham and Women’s Hospital, followed by four years at Boston Medical Center, first as a patient experience coordinator and then as one of three patient advocates at the hospital.
Her healthcare experiences convinced Ingraham that as a physician, she wanted to care for the most vulnerable patients, while also being a healthcare leader focused on medical ethics. Ingraham received a combined MD/MBA from BU along with an MS in bioethics from Harvard. Working toward her master’s degrees and taking a year off to care for her ailing grandfather lengthened her time in medical school. Ingraham envisions a future in academia and a practice as a general surgeon focused on shaping healthcare policy and ethics.
“It’s a beautiful city,” Ingraham said of San Francisco, but it was the Oakland-area community that drew her to the program.
“The culture there is so unique, and the patient population definitely aligns with my values and who I am. I look forward to being very well trained there. I know that they are top-notch, and I am confident I will come out as
Ana Paula Gushken, ENG’20, MD’25 (right), shares her joy at matching to a pediatric residency at New York’s Montefiore Medical Center with her sister Fernanda (left). Fernanda traveled from her medical school in Brazil to open an email with the news that she’d matched in a psychiatry residency at the University of Miami.
a really great surgeon,” Ingraham said.
“Hold on to your values and remember that MD that you earned will make people listen to you, so use that microphone wisely,” said Angela Jackson, MD, associate dean of student affairs. “You are ready because of all the hard work that you put in, and wherever that envelope takes you, your patients will be lucky to have you.”
I’m so excited for what lies ahead,” said Nicholas King, who matched into the University of Massachusetts Chan Medical School general surgery residency program. From Cambridge, Massachusetts, King also had some gap years before entering medical school. Following graduation from Yale University, where he majored in cell biology with a computational focus, he worked for three years as a respite case manager at Healthcare for the Homeless, where he was responsible for planning discharges for patients from the medical respite facility to a substance use program or transitional housing.
“It was very challenging work, and I have a ton of respect for the people who do it,” he said. “I learned a lot about barriers to care, things like people not having physical time to get to their appointments, or having other obli-
gations, like work or childcare, or other things going on in their lives,” said King.
“You all have been enormously resilient, passionate about helping others, and deeply committed to your goals. I am really grateful to have known all of you,” Kristen Hanssen, MD, associate dean of admissions, told the students before they opened their envelopes.
“I’m looking forward to continuing to learn more and treating patients. I’m really happy,” said Ana Paula Gushken, who is from Sao Paulo, Brazil, and comes from an extended family of physicians. She matched into a pediatric residency at Montefiore Medical Center in the Bronx, New York.
Gushken’s sister Fernanda, a medical student in Brazil, joined her sister at BU to open their Match Day announcements together, hugging each other and joining the choruses of screams and shouts around them as Fernanda matched into the University of Miami in psychiatry.
The medical profession runs in their family— their mother is a pediatrician, their father an OB/GYN, and aunts and uncles on both sides of the family are doctors.
“From my experience, I think it’s hard to grow up and not see how amazing medicine is—that you can really make a difference and take care

Students Matching in Primary Care
INTERNAL MEDICINE 50 students
29.9%
PEDIATRICS
21 students
12.6%
FAMILY MEDICINE
5 students 3%
of people in the most vulnerable moments in their lives,” said Ana Paula, who earned a BS in biomedical engineering and early acceptance into medical school through BU’s Modular Medical/Dental Integrated Curriculum program.
“I was really excited to be able to continue here at BU, because I think what’s unique is the focus on advocacy and serving underserved populations,” she said.
“Medicine will challenge you; it will shape you, and it will sometimes exhaust you. But the passion and values that brought you to this school of medicine will sustain you. Hold on to them and take the time to care for yourself. Continue to live by the words ‘I can do it,’ because you can,” said Heather Miselis, MAMS’00, MPH’00, MD’04, associate dean for alumni affairs.
Following graduation in May, 39 medical students plan to stay in Massachusetts, including 14 at BMC; New York (34), California (26), and Pennsylvania (12) were the next most popular states. The class matched in a range of programs. The top specialties were internal medicine (50), pediatrics (21), emergency medicine and surgery (14 each), and anesthesiology (10). ●
Michael Batista, MD’25, who was accepted into the psychiatric residency program at Mount Sinai Hospital, celebrates with Lillian Vo, MD’25, who placed in pediatrics at Yale School of Medicine. Jake Mackey
Ribbon Cutting Officially Opens New Rod Hochman Family Clinical Skills & Simulation Center
New technology & design will prepare students for the realities of patient diagnoses and care

The hallways of the new Rod Hochman Family Clinical Skills & Simulation Center were freshly painted, with bright overhead lighting reflecting off polished floors. Cutting-edge equipment and advanced technology awaited students in every room, but Madison Ellin, MD’25, was most impressed that the new facility looked like any other hospital or clinic.
“When you’re going into your third year, to urgent care or outpatient settings, this hallway reflects what it feels like to be in a
clinic—and you really get that feeling that you can do it,” said Ellin, who is headed to a pediatric residency at Columbia University.
The original simulation center, located in the basement of the L-building, was crowded, occasionally experienced flooding, and had older equipment and an inefficient design. Dean’s Advisory Board (DAB) member Rod Hochman, MD, CAMED’79, CAS’79, and his wife Nancy Hochman, Sargent’77,’83, donated $10 million to build and operate the larger, more technologically advanced new facility. Dedicated to preparing MD, physician
assistant, mental health, and genetic counseling students for the realities of patient diagnosis and care using a team-based approach, the new center opened for the start of the 2025 academic year
During a long and distinguished career, Rod Hochman has held senior executive healthcare positions, including 18 years as president and chief executive officer of the Providence healthcare system. Nancy Hochman has served in the healthcare profession as a physical therapist for 30 years.
Speaking at the May 8 ribbon cutting,
Nancy Hochman, daughter Lindsey, and the Hochmans’ grandson are shown a clinical simulator manikin during a tour of the new clinical skills & simulation center.
Jake Mackey
Hochman praised Karen Antman, MD, dean of the medical school and Medical Campus provost, for her vision and persuasiveness.
“When the dean asked me what I thought about a [new] clinical skills and simulation center…I said, ‘Okay, you got it,’” he recalled. “This is a real gift, to be able to give the students what they need. To see this happen is so near and dear to my heart.”
The center is part of the school’s plan to reframe medical student training—also represented in the recent curriculum redesign—to integrate learning theory and make learning more active.
“One of the most important things to us is that we create safety in the transition of students from a classroom to the clinical environment. We do this by providing a space where they can practice and understand the real-world issues that come up when they’re in the clinical environment,” said Associate Dean of Medical Education Priya Garg, MD. “It made natural sense to have more simulation and standardized patient experiences. Our future patients, when they see our graduates, need to know that our doctors were well-trained in the skills that we value the most, which are developing rapport with our patients, communicating in a way so that [patients] feel they are heard, and having the diagnostic and clinical reasoning skills that make them excellent diagnosticians.”
Garg said that the school had been discussing clinical care education with Hochman for years, tapping his experience as a CEO; the new center was a natural extension of those ongoing conversations.
Three times larger than the original, the new center has rooms that are grouped around teaching clinical skills, including the physical examination, hospital care, and skills instruction. It features 13 clinical skills classrooms, 13 examination rooms for standardized patient (trained actors who grade the students) experiences, and four simulated emergency/hospital rooms.
New and upgraded technology includes ultrasound, intercoms, and all the equipment found in a standard examination room, while
a web-based instructional system allows faculty to observe students remotely, with two cameras in each room providing full room coverage.
The four hospital rooms mimic a typical inpatient or emergency room with hospital
Students on the DAB tour were impressed by the design and the technology of the new facility.
Neil Singh Bedi, MD’26, recalled the “deer in the headlights” feeling of seeing his first real patient.
“One of the most important things to us is that we create safety in the transition of students from a classroom to the clinical environment. We do this by providing a space where they can practice and understand the real-world issues that come up when they’re in the clinical environment.”
ASSOCIATE DEAN OF MEDICAL EDUCATION PRIYA GARG, MD
beds, high-fidelity manikins (lifelike patient simulators used in medical training), wall screens showing simulated patient vital signs and x-rays, and handheld ultrasound machines. In an adjacent room behind one-way mirrors, faculty members answer student questions addressed to the manikin in the voice of the high-fidelity patient, observing the students so they can facilitate a debrief following the simulation session.
During the May 8 facility tour, a baby’s cry interrupted Molly Cohen-Osher’s presentation to DAB members. Cohen-Osher, MD, MMedEd, assistant dean of medical education for curriculum and instructional design as well as the family medicine director of medical student education, instinctively moved to the source of the crying, a realistic manikin of a baby on a hospital bed hooked up to a monitor displaying its vital signs.
The baby manikin can be programmed to display symptoms and respond to treatment. It can run a fever and sweat, take medication and fluids, be intubated, undergo a needle decompression or a tracheotomy, take chest tubes, and have seizures. The baby’s internal electronics analyze student hand placement, compression, and air flow during CPR.
“Practicing in an environment like this, that feels like the real thing, gives you that sense of competence and confidence you need,” he said. “Then, when you go onto the real wards, you feel like you’re just doing it all over again. It’s familiar.”
Speaking at the ribbon cutting, Boston University President Melissa Gilliam, MD, MPH, stressed that the new center reflects the need to be technologically current as well as the importance of giving students the best skills training possible. “If we do that at this institution, then we can also attract the best students,” she said.
“Your generosity is helping us stay at the forefront of medicine,” Gilliam told the Hochmans. “The students are our future… what we do here, combining an incredible mission with the best possible training, will really change the world.” ●
Celebrating the 2025 GMS Outstanding Student Achievement Award Winners
Graduate Medical Sciences (GMS) presented three high-achieving Class of 2025 graduates with Outstanding Student Achievement Awards for Community Service and Outstanding Research

Todd W. Dowrey
PhD in Molecular & Translational Medicine, Program in Biomedical Sciences
Outstanding Student Achievement Award: PhD Research Category
Dowrey matriculated into the PhD Program in Biomedical Sciences (PiBS) in 2020 before transferring to the department of Molecular and Translational Medicine (MTM). He completed his research with Associate Professor of Medicine George Murphy, PhD, who cofounded the BU and BMC Center for Regenerative Medicine (CReM).
Dowrey’s research centers on understanding healthy aging by studying centenarians, individuals who live over 100 years, by developing a human stem cell–based model of resiliency. He studies how cells produced from centenarian subjects respond to stress and insult, and how these responses may be different and more effective than cells produced from a typical ager.
“We believe centenarians provide the blueprint to living longer, healthier lives due to not only their extended lifespan, but their extended health span, or years of life lived without disability, age-related disease, or cognitive decline,” Dowrey says.
This research works to address the limited amount of access and biomaterial available for collection and characterization from exceptional agers. During the pandemic, for example, accessing this older population was significantly more challenging out of concern for their safety.
Using a stem cell–based approach has allowed Dowrey and his lab mates to generate a renewable source of biomaterial to use for a variety of current and future projects.
Dowrey, who was a pioneer student for the Murphy Lab’s projects on aging, has successfully defended his dissertation, “Induced Pluripotent Stem Cell–Based Modeling of Resiliency: Understanding the Molecular Mechanisms of Exceptional Longevity.”
Looking ahead, Dowrey hopes to continue his research on regenerative medicine and healthy aging as he finishes his PhD and explores industry science positions in the field.
“Stem cell–based models are an area of high interest for their potential in regenerative medicine and the modeling of aging-related disease,” Dowrey says. “I plan to remain in these fields and work toward advancing our understanding of aging-related disease, and hopefully develop therapies aimed at combating these diseases and improving our resiliency.”

Gloria Urrutia
Master of Science in Medical Sciences (MAMS) Program
Outstanding Student Achievement Award: Master’s Research Category
Urrutia matriculated into the MAMS program in 2023, graduating in May 2025. For her thesis, Urrutia worked on projects addressing educational and healthcare barriers that disproportionately affect underrepresented communities.
For her thesis working with Assistant Professor of Pharmacology, Physiology & Biophysics Marisol Lopez, PhD, Urrutia investigated how technical flaws in physiology multiple-choice question (MCQ) assessments impact graduate and professional student performance.
The mixed-methods approach found that flawed MCQs may favor students who have knowledge of test-taking strategies and can navigate misleading question and answer choices. The research highlights the importance of effective MCQ construction
in ensuring equitable assessments for students.
Urrutia also worked on two clinical research projects focused on improving healthcare communication and education among Latinx and Caribbean communities. In the first project, she worked with Assistant Professor of Medicine Shana A.B. Burrowes, PhD, CPH, to explore patient-provider communication around antibiotic prescribing for respiratory tract infections.
In the second project, she worked with Assistant Professor of Medicine Katherine Rizzolo, MD, to conduct Spanish-language interviews with Latinx patients to better understand their experiences with kidney disease education.
“[These projects] have given me the opportunity to uplift the voices of underrepresented communities and contribute to change through research,” Urrutia says.
This work is deeply meaningful for Urrutia. A first-generation Latina student, she was inspired to join these projects after participating in Lopez’s study investigating perceptions of minority students in physiology.
“Hearing the stories of students like me, as well as patients who resemble my own family members, motivates me to continue finding ways to help patients access the care and resources they need,” she says. “Whether through clinical or educational research, I’ve found that meaningful solutions come from listening to those we aim to serve, and that is what continues to guide my work.”
This year, Urrutia presented her research at the American Physiological Society Summit and the International Association of Medical Science Educators Conference.
“These research experiences have deepened my commitment to supporting underrepresented populations,” she says. “I look forward to continuing this work and integrating it into my future career in healthcare and research.”

Marine Chido Nimblette Master of Science in Medical Sciences (MAMS) Program Outstanding Student Achievement Award: Master’s Community Service
Nimblette, a member of the MAMS Class of 2025, served on the 2024–2025 mayorappointed SPARK team, a volunteer leadership and civic engagement council for Boston residents ages 20 to 35. As part of SPARK, she advised Boston Mayor Michelle Wu on programs and policies that affect young adults across the city.
Nimblette represented the Fenway/Kenmore area, where she helped set policy priorities, address city issues, plan for Boston’s future, and increase civic engagement.
In February 2025, Nimblette designed a Black History Month campaign encouraging Bostonians to shop at Black-owned businesses across the city.
The campaign urged residents to have conversations about supporting Blackowned businesses and to celebrate culture in a tangible way. It culminated in a celebration at The Mix, a Black-owned restaurant in Dorchester, where Nimblette and her fellow SPARK members honored campaign participants.
“I plan to continue using both my personal time and my role on SPARK Boston to uplift local communities, especially by advocating for civic participation and highlighting Black entrepreneurs.”
The daughter of immigrant parents from Grenada and Zimbabwe who run their own family business, Nimblette credits her parents for teaching her to value and participate in community service.
“Growing up within a small, family-owned business gave me a deep understanding of the unique challenges that Black business owners face every day,” Nimblette says. “No matter where I am, I make it a priority to dedicate my personal time to support and uplift Black entrepreneurs and help ease some of those everyday stressors.”
Nimblette also worked on several events encouraging Gen-Z Bostonians to register to vote during the 2024 presidential election campaign, including voter registration events at the Museum of Fine Arts and several community roundtables with SPARK members.
“I enjoyed seeing firsthand how accessible and joyful civic engagement can be when young people are invited into the process in creative ways. I plan to continue using both my personal time and my role on SPARK Boston to uplift local communities, especially by advocating for civic participation and highlighting Black entrepreneurs,” she says. “I’m particularly passionate about initiatives that blend health education, policy, and entrepreneurship.” ●
Annual Memorial Service Honors Anatomy Donors
Anatomical gift donors are the silent heroes of science
Katie Gorman did not expect to cry at the ceremony, but when first-year medical student
Gabrielle Ruban sang “Moon River,” the tears came.
Her mother, Mary Gorman, was one of 31 anatomical gift donors honored by medical and dental students at the annual memorial service for anatomy donors held on May 5 in Hiebert Lounge. As Gorman looked at the nearly 90 family members representing 20 of the donors, she thought of them being united in loss—but also in noble sacrifice.
The musical performances and heartfelt speeches by students touched her.
“They talked about the bodies of the donors so respectfully, and everybody said, ‘Thank you, thank you,’” said Gorman, who was among nearly 200 attendees. Gorman was accompanied by family members including her sister, Anne Richards. After the
ceremony, she met three first-year dental students who directly benefited from her mother’s sacrifice.
“It really is your first exposure to the human body, to working on a person, and the entire time you are so grateful for what they [the donors] are providing to us. It really increases your empathy and your respect for them,” said first-year dental student Nicole Kenda. Through donors, students learn how the body reflects physical stress, dietary habits, diseases, and injuries.
At the memorial service, students view photos of the donors and meet family members who can further elaborate on their loved one’s personal and family history. The event unites families and students as they all pay tribute to the donors.
“It was really very rewarding and emotional, too, because we know different aspects of the person,” said first-year dental
student Purnima Sainani, who spoke with donor families following her performance playing three short piano compositions.
“We’re all here for the same reason. It’s really beautiful.”
First-year medical student Sydni Britton was initially intimidated by the Gross Anatomy Lab and the donor bodies, but her interest in learning prevailed.
“When you understand what you’re doing, what you are there to do, it is more humbling than scary,” said Britton, who spoke with donor families after the service. “I told them that there’s nothing that can replace what we learn from an actual person, and that their family member meant a lot to us.”
Britton spoke with members of the McCormack family, there to honor Henry McCormack, Jr., a graphic artist with a dry sense of humor, according to his niece Charlotte McCormack.

First-year dental student Simon Fidlin plays a solo at the memorial service.


“The students I spoke with were very open about how they worked with the donors, how important it was for them to actually see things they’d only actually seen in textbooks, and that the value it brought them as students was tangible,” Charlotte McCormack said. “They were very gracious and extremely appreciative of the families and the donors.”
According to his wife Susan Weegar, donor Charles Brent Harold was a radical. “He was willing to speak up and say what he thought,” she said. A former English professor, newspaper columnist, and author, Harold was always learning how to do something new, like playing the banjo, building a house, and sailing. Weegar noted that Robert Bouchie, anatomy lab manager and director of the anatomical gift program, and other program staff ensured that donors, like patients, were treated with dignity, respect, and care at all times.
“It’s a good feeling for you as a survivor to know that,” Weegar said.
Joyce Kelleher attended the ceremony with her extended family to honor their father John. Her mother Marjorie, who passed away last year, also donated her body.
“My mother talked about doing it for 34 years,” Kelleher recalled. The program and service inspired her brother to donate his body, and Kelleher has started paperwork to do the same.
“I think this [anatomy] program is incredibly well run,” said first-year medical student Stuart Sommers. “Throughout the program, there were many reminders that the donors are human beings with life stories, and of how much more they were beyond their body.”
He recalled talking to one family who said their family member had run away to Las Vegas at age 14, taking his grandfather’s name.
“I was very impressed by the courage that it took to do that. It was such an interesting back story,” said Sommers, who volunteered to be master of ceremonies. Nearly 50 students signed up for the memorial service committee.
“Each donor has provided us with an incredible gift, one that allowed us to learn, grow, and further develop as healthcare professionals and scientists,” said student speaker Ashley Fair, who is pursuing a Master of Science in anatomy & neurobiology. “Donors are the silent heroes of science.” ●
First-year medical student Sydni Britton talks with donor family members Charlotte McCormack (center) and Gretchen Van Ness (right).
Jake Mackey
First-year medical student and master of ceremonies Stuart Sommers addresses a full house at the event.

MAMS Turns 40!
Officially launched in 1985, MAMS was one of the first SMPs in the country. Since its foundation, MAMS has helped over 4,000 students gain admission to medical schools across the United States.
First conceived in the early 1980s over a faculty lunch table, BU’s MS in Medical Sciences (MAMS) program has grown to become a renowned Special Master’s Program (SMP) and one of the most successful in the country.
In the early 1980s, faculty from the Boston University School of Medicine Department of Microbiology gathered around a lunch table to discuss a groundbreaking new program, and one that would soon become the school’s Master of Science in Medical Sciences, or MAMS.
According to Glen Zamansky, PhD, the idea was the brainchild of the late Selwyn Broitman, PhD, a professor of microbiology, pathology, and laboratory medicine and later, an assistant dean of the school’s Graduate Medical Sciences (GMS).
Zamansky, who retired in 2020, is the former College of Arts & Sciences assistant
dean for premedical studies, director of the Seven-Year Liberal Arts/Medical Education (SMED) Program, and associate professor of microbiology.
“Sel brought these big ideas of a real second chance for students to prepare for, apply to, and go to medical school,” says Zamansky. “[We] gave him a run for his money, but Sel was determined, and it became a feasible program.”
The group envisioned the program with a twofold purpose: to help students reach goals that had previously been out of their reach by providing them with the foundation to do so, and to create a program that would foster growth in the medical school itself.
Officially launched in 1985, MAMS was one of the first SMPs in the country. Since its foundation, MAMS has helped over 4,000 students gain admission to medical schools across the United States.
Jake Mackey
Class of 2024 MAMS graduates.
MAMS Grows by Leaps and Bounds
Originally enrolling around 10 students, MAMS expanded quickly. By the early 2000s, enrollment in the program had increased to an average class size of about 150, with some years admitting even more.
As the program grew, its curriculum took on new elements to bolster student success. MAMS, now a Master of Science degree, introduced an advising program for students and the requirement of a final thesis project. The curriculum also evolved to include small group discussions, giving students the same experiences they would eventually encounter in medical school.
MAMS students primarily graduated with the intention of pursuing an MD or DO medical degree, with some pursuing additional education in physician assistant and dental medicine programs.
MAMS was followed by the creation of new and focused programs for GMS students, such as the Master of Science in Oral Health Sciences (OHS)—which began as a track within MAMS for predental students and eventually became its own degree—and the Physician Assistant program.
Associate Professor of Medicine Gwynneth Offner, PhD, has served as program director since 2010, during which time MAMS has continued to grow and adapt to the changing needs of 21st-century medicine.
“Working with so many bright and talented students has been one of the highlights of my career at Boston University,” Offner says. “They continue to inspire me with their commitment to making a difference in the lives of their future patients, and I am immensely proud of all of their accomplishments.”
A Rigorous Curriculum Meets Evolving Student Needs
According to Karen Symes, PhD, MAMS is a rigorous degree that instills confidence in students that they can one day manage the coursework of a medical or other professional school.
Symes, an assistant dean of MD student affairs who serves as a core instructor and advisor to students enrolled in the MAMS program, says, “The students get to see that they can do it. The volume of information is massive and they’re not just memorizing, they have to apply information. They
develop a really good skill set and lots of discipline.”
Current students are required to complete a minimum of 32 graduate credit hours consisting of at least 24 course credits and up to eight credits of research toward a thesis. All students complete the foundational coursework in the first two semesters, with many using the optional second year to gain research and clinical experience.
The program has evolved to further align with the MD program, incorporating different pedagogies and more opportunities for problem- and team-based learning.
The curriculum now includes MCAT preparation, courses in topics such as pharmacology and immunology, and increased exposure to public health, advocacy, and social justice. Students also have more opportunities to gain valuable clinical experience and to work as medical scribes in several Boston Medical Center departments.
“I chose the MAMS program because of its rigorous science curriculum, its research thesis in the second year, and its extensive track record of good outcomes for its graduates, from medical school acceptance to career growth in industry,” says Javi Sanchez, MS, a 2021 MAMS graduate.
Currently a second-year MD student at Yale School of Medicine, Sanchez credits the MAMS program with instilling a “growth mindset” in him along with the ability to “learn for a career and not an exam,” both lessons that he has continued to heed during his medical school career.
“When our students go on to the next step, they have a really strong basic science foundation,” Symes says. “It enables them to fully engage in classes as it gives them time to think about and apply the material effectively.”
Supporting Students Now and into the Future
Support and mentorship are central to MAMS. The program boasts a successful advising system that pairs faculty members with small groups of students, which is especially helpful during the first year of the curriculum and as students apply to medical school.
Maryann MacNeil, MA, a clinical associate professor of anatomy & neurobiology
and BU alumna, served as a MAMS advisor for close to a decade, supporting between 11 to 14 students per academic year.
“I knew my advisees inside and out,” MacNeil says. “It was a nice relationship. One of the strengths of the program is the support that students feel, in advising and overall, from faculty.”
Throughout her time at BU and as a MAMS advisor, MacNeil has gained a tremendous respect for students in the program, the majority of whom have entered to better prepare for the challenges of medical school.
“What it always shows me is that these students are resilient, hardworking, and goal-oriented,” MacNeil says.
As MAMS continues to welcome new cohorts of students, the support offered by faculty and staff and the long-lasting camaraderie built between classmates will remain a core part of the program.
Lee Jamison, MD, a 2008 MAMS graduate, noted that while the program was academically the hardest challenge he’d ever faced, it put him in a significantly stronger position to apply to medical school and build a successful career in medicine.
Jamison, who enrolled in MAMS as a nontraditional student, is currently a hematologist-oncologist at Rex Hematology Oncology Associates in Raleigh, North Carolina.
“Everything I have been able to accomplish in my life professionally, from medical school to residency, to a successful career in the United States Army, to my current position as a community oncologist, was built upon the foundation that started with the MAMS program,” Jamison says. “I cannot thank the individuals enough who were responsible for encouraging me and mentoring me along the way.” ●
Landmark Framingham Heart Study Renewed

The National Heart, Lung, and Blood Institute (NHLBI) has renewed the contract for the iconic Framingham Heart Study (FHS), the source of many landmark discoveries on heart disease and stroke that have led to lifestyle changes and medications directly responsible for extending the human lifespan. The six-year contract covers operation and research—extending its 77 years of research to date and its legacy as the longest continuous cohort study in the United States.
“The Framingham Heart Study has allowed us to help people avoid heart attacks and devastating strokes, because we now understand the root causes,” says FHS Director and cardiologist Donald Lloyd-Jones, MD, ScM. “It is absolutely true to say that measurable changes in lifespan can be directly ascribed to the study and its discoveries. And even more importantly, I think there are measurable changes to the health span, which is not just your lifespan, but how long you live healthy, which is what we really are trying to maximize.”
Boston University partnered with the NHLBI in 1971.
Today, many participants are generational descendants of the original 5,209 Framingham residents who were recruited in 1948 to help researchers uncover the causes and consequences of heart disease and stroke. More than 15,000 volunteers have participated
“What FHS has really evolved into is a premier study of aging in organ systems beyond the heart. The focus has really shifted from disease to health and trying to understand how people can maintain optimal health for as long as possible into their lifespan.”
in regular examinations since then, driving the study.
Lloyd-Jones credits the funding renewal to the dedication of these volunteers. “They’re amazing people. They truly have changed the world because of the understanding we’ve gained about healthy aging and about what causes diseases,” he says.
Two cohorts of Hispanic, Asian, and Black participants were recruited in the 1990s and early 2000s to better reflect the shifting demographics of Framingham and the nation.
In addition to funding the core examination of participants who return to the research center in Framingham every two to three years for a detailed medical history, physical examination, and laboratory tests, the NHLBI also supports the collecting and archiving of blood and tissue samples, monitoring of participants, and data analysis. FHS-affiliated researchers must seek separate competitive grant funding to pay for ancillary studies.
In 1948, heart disease and stroke were considered an inevitable consequence of aging. FHS research has been responsible for medications and recommended lifestyle changes that made those conditions manageable—and even avoidable. Much of what we now take for granted when it comes to heart disease and stroke originated with the study, which identified the fundamental risk factors for heart disease such as smoking, diabetes, and obesity; the height-
Donald Lloyd-Jones, MD, ScM, director of the Framingham Heart Study.
Jake Mackey
ened stroke risk from high blood pressure; the benefit of physical activity; and the central role of cholesterol.
The last of the original participants passed away in 2023 at the remarkable age of 105, but the foresight of recruiting within families has paid off, as advancements in the science of genetics promise new solutions in fighting and preventing disease.
“Having generations of related individuals was a perfect study design to allow for the power of genetics to come through,” says Lloyd-Jones. “Three generations of related individuals have taught us immense amounts about the origins of heart disease, stroke, brain-aging, the life course of our weight, and trajectories of our endocrinologic, bone, liver, and kidney health.”
The renewed contract will allow FHS to continue to follow the three generations of participants and the most recent cohorts over at least two new examination cycles.
“It’s a very broad base to look at the life course of health and disease,” says Lloyd-Jones.
Of course, many of the descendants of the original participants have not remained in Framingham. The renewed funding allows
FHS to collect data in new ways, including wearable devices like watches, electronic questionnaires, and traveling to the homes of participants.
As a federally funded study, FHS also serves as a resource for other scientists. Framingham investigators have collaborated on projects studying stroke and dementia, lung diseases, osteoporosis and arthritis, nutrition, diabetes, eye diseases, hearing disorders, and genetic patterns of common diseases.
According to Lloyd-Jones, FHS has taken advantage of huge advances in genetic research since the last contract renewal in 2019.
“Over the last six years, we’ve been able to generate that full sequence of pathway data to understand a lot more about the molecular processes of aging, health, and disease. And that will be a major focus going forward with the new funding,” he says.
“What FHS has really evolved into is a premier study of aging in organ systems beyond the heart. The focus has really shifted from disease to health and trying to understand how people can maintain optimal health for as long as possible into their lifespan.” ●
Alumni Medical Library’s Little Free Library
Offers Access to Leisure
The cutting-edge Alumni Medical Library includes extensive electronic collections comprising 3,600+ current journals, 20,000+ e-books, hundreds of databases, and 50+ quality-filtered subject guides. Library users can also access the University Libraries collections of more than 2.4 million physical volumes, over 45,000 current unique serials titles, and 77,000 media titles.
“As a health sciences library, most of our books and journals are electronic,” says Director of Library Services Kate Flewelling, MLIS, AHIP. “They’re not something you would necessarily read for pleasure, and so we’ve wanted the library to promote access to leisure reading.”
After flooding shuttered the South End branch of the Boston Public Library (BPL), closing it indefinitely, the Alumni Library partnered with BPL to do signups for digital library cards. The library also collaborated with the BPL, the Massachusetts Department of Transportation, and the Massachusetts Library System to place stickers at nearby transit stops, allowing students and other commuters to scan them and
Reading
gain access to digital audiobooks, e-books, newspapers, and magazines through a BPL program called “Browse, Borrow, Board.”
Believing that students needed even more immediate access to leisure reading, Flewelling applied for and received a $1,000 Inclusion Catalyst Grant from BU Diversity & Inclusion to open the Little Free Library. The grants support “collaborative and creative programs and initiatives that generate learning and stimulate efforts that foster inclusive and equitable communities at Boston University.”
Based in St. Paul, Minnesota, the Little Free Library is a nonprofit with nearly 200,000 library boxes distributed across the country—their response to a literacy crisis in the United States.
Most days, the bright-red, glass-fronted cabinet stuffed with books is located at the Alumni Medical Library, but it also travels around the Medical Campus on a cart featuring a beverage station. Anyone can borrow a book, leave a book behind in exchange if they choose to, and return a book when they’re finished reading it. Or, they can hold on to it.
Library staff have donated books, and students can also suggest titles to be purchased. The library has committed to buying books for the Little Free Library from More Than Words—which employs youth ages 16–24 who are in foster care, homeless, out of school, or in the court system, and teaches them to run an online retail bookstore while receiving both personal and career support— and two Black-owned bookstores. ●
The Little Free Library display case can hold up to two dozen books that are free to borrow or keep. You can also leave a book for others to read.
Pulmonologist Darrell Kotton Is BU’s Innovator of the Year
Boston University pulmonologist
Darrell Kotton, MD, and his team imagine a future where they can use a patient’s own cells to fix lung damage caused by disease—reprogramming cells in a laboratory dish and transplanting them back into the patient. The new lung cells would replicate, like regular cells do, replacing the damaged and diseased areas of the lung. By refining their work using sophisticated stem cell technology, Kotton and his team are inching closer and closer to realizing that vision.
For this cutting-edge work, which could eventually help cure diseases like cystic fibrosis—a disease caused by a genetic mutation—and pulmonary fibrosis, and reverse lung damage from conditions like emphysema, Kotton has been named BU’s Innovator of the Year.
“This is an unexpected honor,” says Kotton, the David C. Seldin Professor of Medicine. “I’m grateful to our team that helped innovate, and for an environment like BU, where I have complete support from colleagues and leadership.”
An attending physician and scientist, Kotton is a founding director of the Center for Regenerative Medicine (CReM) of Boston University and Boston Medical Center, BU’s primary teaching hospital. The type of cellular engineering taking place in Kotton’s lab is at the forefront of regenerative medicine and research.
“Darrell has identified gaps in diagnostics and treatments for pulmonary diseases and creative ways to use tissue stem cells to define how diseases develop, plus find targets for treatment,” says Karen Antman, dean of BU’s medical school and provost of the Medical Campus. “He has been equally creative in assembling a team of investigators in this cutting-edge
Cydney Scott
science, getting them funded and creating a space conducive to efficient, collaborative research. He has been innovative both in science and management—a really effective combination.”
At the start of Kotton’s career, reprogramming stem cells—undifferentiated cells of the human body that transform into specialized cells and have the ability to replicate indefinitely—to cure disease was considered “extremely esoteric,” he says, adding that he and his team pushed forward anyway. “We loved the mission and the questions so much that even if nothing worked, it was still fascinating and enough for us.”
cells. Those engineered cells, called induced pluripotent stem (iPS) cells, won Yamanaka the Nobel Prize in 2012, and opened the door to an entire new field of genetic engineering— and, according to Kotton, propelled his own research from esoteric to mainstream.
“That discovery meant that the same recipes and protocols we had been developing were suddenly applicable to the new engineered iPS cells, and we were extremely well positioned to apply a lot of our hard work and new knowledge immediately to this new type of cell,” he says. Now, instead of making lung cells out of embryonic stem cells, they could create them from a person of any age with their
“The advances of CReM will allow for novel therapies previously not obtainable. This exemplifies why Dr. Kotton is an ideal choice of Innovator of the Year and why his leadership allows BMC and BU to remain at the leading edge of scientific discovery.”
TONY HOLLENBERG, BMC PRESIDENT AND PROFESSOR OF MEDICINE
At the time, Kotton and his team focused on basic science questions, studying how pluripotent stem cells, which are only found in embryos, grow and transform to become specialized cells in the body. Then, in 2006, Japanese scientist Shinya Yamanaka figured out how to revert adult skin or blood cells back into an embryonic stem cell–like state, meaning that adult cells could be turned into any cell type in the body, including lung
own cells, making it more likely that new implanted cells would be accepted.
“Like many of the world’s leading scientific innovators, Dr. Kotton is driven by an altruistic ambition to discover cures for currently incurable diseases,” says Thomas Bifano, BU vice president, associate provost ad interim for research, and a previous Innovator of the Year winner. “His pioneering work using induced pluripotent stem cells
as building blocks to regenerate lung tissue has significantly advanced research into debilitating conditions such as cystic fibrosis. Beyond his groundbreaking contributions to lung regeneration, Dr. Kotton is widely recognized for his unwavering commitment to open-source biology—freely sharing ideas, databases, cell lines, protocols, and expertise to accelerate scientific innovation and discovery.”
In 2023, two studies published in Cell Stem Cell detailed how Kotton and his colleagues engineered lung stem cells and successfully transplanted them into injured lungs of mice. Two lines of cells targeted two different parts of the lung: the airways, including the trachea and bronchial tubes, and the alveoli, the delicate air sacs that deliver oxygen to the bloodstream. The findings could eventually lead to new ways for treating severe cases of COVID-19, emphysema, pulmonary fibrosis, and cystic fibrosis.
The Innovator of the Year award was announced at a special event that highlighted how BU faculty work with industry experts to address challenges associated with developing treatments for lung disease. For example, Kotton’s team recently began collaborating with United Kingdom–based biopharma giant GSK to use CReMdeveloped lung cells to better understand pulmonary fibrosis and identify new drug targets to halt or slow the progression of the currently incurable disease. Kotton is CReM’s second Innovator of the Year winner; codirector Gustavo Mostoslavsky, PhD, a professor of gastroenterology, earned the award in 2017.
“The work by Dr. Kotton and his colleagues meets unmet medical needs by harnessing innovative technology to develop cellular therapies for human diseases,” says Tony Hollenberg, president of BMC and a BU professor of medicine. “The advances of CReM will allow for novel therapies previously not obtainable. This exemplifies why Dr. Kotton is an ideal choice of Innovator of the Year and why his leadership allows BMC and BU to remain at the leading edge of scientific discovery.” ●
GMS Research on Display at Inaugural Research Symposium
More than 150 students, faculty, and staff attended the inaugural Graduate Medical Sciences (GMS) Research Symposium on April 10 in Hiebert Lounge. Speakers included PhD and MD/PhD students who were selected for Research Talk Awards, as well as postdoctoral fellows. The symposium also featured 79 poster presentations highlighting the wide range of work being done by postdoctoral researchers, MD/PhD, PhD, and master’s students.
Participants said the symposium helped them experience the broad scope of GMS research and presented an opportunity to sharpen their science communication skills, essential for success in academia and in their careers.
“Doing presentations is a fundamental part of being a scientist, or being a graduate student or a postdoc,” said Nicholas Skvir, PhD, MS’14. “It’s how you sell yourself and your research, how you get recognition, and that’s very necessary.”
Originally from Westwood, Massachusetts, Skvir is a postdoctoral researcher in aging and gerontology. He was presenting research he’d done with others in the Murphy Laboratory at the Center for Regenerative Medicine (CReM) investigating the role of megakaryocytes—cells typically found in the bone marrow and responsible for producing blood platelets that also are found in lung tissue.
Skvir noted that lab director George Murphy, PhD, associate professor of medicine, generously provided participants with opportunities to present research.
“He’s given me lots of chances to get out there, become more experienced at speaking, and go to lots of conferences,” Skvir said.
Gillian Fennell, PhD, a first-year postdoctoral quantitative researcher working under an NIH National Research Service Award fel-

lowship in rheumatology, stood ready beside her poster to explain her research on the prevalence and burden of chronic pain.
“I’m the first in my family to take this academic path,” said Fennell, who went to Cornell as an undergraduate and received her PhD from the University of Southern California. “I’m excited to come and work in my cubicle every day, figure out problems, and come up with creative, more accurate interpretations of data.”
As a postdoc with relatively few people in her program, Fennell said she often felt isolated by the daily routine, and the social aspect of the GMS symposium was a plus.
“It’s nice to get the opportunity to meet
your same-age peers,” she said.
“Most everyone, faculty and students, in their day-to-day work become very focused on what they’re doing and what they’re knowledgeable about, even though there’s a lot of research that’s occurring across campus,” said poster contest judge Adam Hall, PhD, assistant professor of anatomy & neurobiology.
He noted that the GMS symposium format is a useful introduction to the presentation process, which is integral to a researcher’s career. Scientific conferences, applying for grants, and even defending graduate theses all require effective presentation skills.
“For some of the younger students who
During the symposium’s poster contest session, fifth-year MD/PhD student Rose Zhao explains her research to judge Adam Hall, PhD, assistant professor of anatomy & neurobiology.
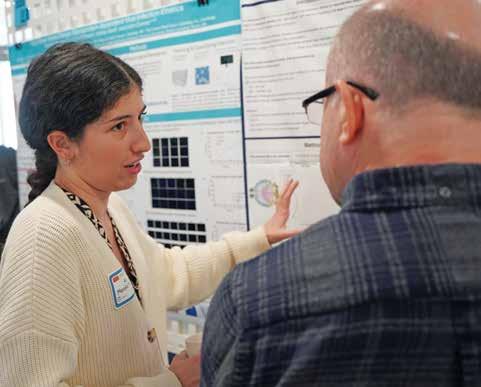
may not have presented yet at a conference, this is an easier format—it’s a smaller venue, they don’t have to travel, and it still gives them the same type of experience,” Hall said.
“I think it’s important for me to understand what my colleagues are doing, and this helps broaden my horizons,” said Guanghao Yu, a second-year student in the MS in Medical Sciences (MAMS) program, the largest GMS program. Most MAMS graduates continue on to medical school.
Yu was presenting research from the Majmundar Lab at Boston Children’s Hospital on a novel mechanism in a rare kidney disease.
“I think research is an integral part of being a well-rounded physician/scientist.
My mentors have had their patients in clinic inform their research and vice versa. To be a great physician, it’s important to be part of the scientific discovery aspect to better take care of our patients,” Yu said.
Rose Zhao, an MD/PhD student in her fifth PhD year, is nearing the end of the research portion of her medical education. Her poster outlined her work with the Ganem Lab studying how specific types of errors in cell division give rise to specific tumor cells.
“These symposiums are great. They’re internal, so everyone is very supportive. No one’s here to challenge you; they’re just trying to understand what you’re doing,” said Zhao.
A postdoctoral research fellow working in the Hagedorn Lab, Gwen Beacham, PhD, was one of six presenters selected from an applicant pool of 33 PhD and MD/PhD students and postdoctoral researchers to receive the GMS Research Symposium Talk Award. Beacham was drawn to BU by Elliott Hagedorn, PhD, assistant professor of medicine, and his work exploring how blood and cancer cells migrate into and out of distinct tissues and organs.
“Everyone is supportive of each other, and it’s really a special environment here,” said Beacham, who also noted the advantages of working near Boston Medical Center and collaborating with clinicians.
Other GMS Research Talk Award winners included third-year PhD students Isabel Orbe and Dilnar Mahmut; fifth-year MD/ PhD student Linzheng Shi; fifth-year PhD candidate Chelsey Skeete; and postdoctoral researcher Jose Andres Alepuz Guillen, PhD.
Out of the 79 posters presented, judges selected nine student winners. ●
Master’s Programs:
Samuel Camilli and Kai Blumen
Early Career PhD or MD/PhD Programs:
Third-year PhD students Andre Krunic and Thomas Murphy
PhD or MD/PhD Programs:
Fourth-year PhD students Angela Capriglione and Ivy Hughes, and fifth-year PhD student Todd Dowrey, who has since successfully defended his thesis and now is a postdoctoral researcher
Postdoctoral Fellows:
Ioanna Yiannakou, PhD, MS, and Madeline Nowak, PhD
Ana Morello Megias, a PhD candidate in anatomy & neurobiology, explains her research during the inaugural GMS Research Symposium.
Jake Mackey
Hee-Young Park, PhD, Appointed Dean Ad Interim

Last spring, Karen Antman, MD, announced her intention to step down as provost of the Medical Campus and dean of the Chobanian & Avedisian School of Medicine. As the search for a permanent successor continues, Hee-Young Park, PhD, assumed the role of interim dean of the medical school, effective July 1, and will report to the University provost along with all other academic deans.
The Carolann S. Najarian, MD, Professor, chair of medical sciences & education, professor of dermatology, and associate dean of faculty affairs, Park has established herself as a trusted, collaborative leader with deep insight into the academic and clinical priorities of the Medical Campus for more than
three decades. She has played a central role in faculty advancement, educational leadership, and institutional governance, earning the respect and confidence of her colleagues on the Medical Campus and across the University.
A highly regarded scientist and educator, Park focuses her research on the molecular and cellular pathways involved in human pigmentation and wound healing. She is a dedicated mentor to students and trainees at all levels and has received numerous honors for her teaching and research. She also is an active contributor to campus life, serving on the Faculty Council, University Council, and University Council Committee on Faculty Policies, as well as the Committee on Faculty Affairs at the medical school. ●
Vicki Jackson, MD, MPH, Named Chair of Medicine

Vicki Jackson, MD, MPH, has been named chief and chair of the department of medicine as of September 2, 2025. Dr. Jackson joins our community from Massachusetts General Hospital, where she has served with distinction for more than two decades, most recently as the Blum Family Endowed Chair in Palliative Care and the chief of the division of palliative care and geriatric medicine. Jackson also was a professor of medicine at Harvard Medical School, codirector of the Harvard Medical School Center for Palliative Care, and founding director for the Harvard Palliative Medicine Fellowship.
A nationally recognized leader in palliative care, Jackson received Harvard Medical School’s prestigious A. Clifford Barger mentoring award in 2019. She is a coinvestigator and mentor on numerous studies funded through the National Institutes of Health, the National Cancer Institute, and
the Patient-Centered Outcomes Research Institute investigating the effect of early, integrated palliative care for patients with advanced cancer. She also coauthored the books Living with Cancer: A Step-by-Step Guide for Coping Medically and Emotionally with a Serious Diagnosis and What’s in the Syringe? Principles of Early Integrated Palliative Care . Jackson fulfilled her residency and chief residency in internal medicine at Cambridge Hospital and received training in research methods through the Harvard general medicine fellowship. She earned a master’s in public health at Harvard T.H. Chan School of Public Health and completed training in palliative care at Dana-Farber Cancer Institute and Brigham and Women’s Hospital.
The school is grateful to Sushrut Waikar, MD, for leading the department as interim chief and chair while continuing in his role as section chief of nephrology. ●
Meet the 2025 Annual Faculty and Staff Award Recipients
At the end of each academic year, the school recognizes faculty and staff for their excellence in mentoring, teaching, and service through faculty and staff awards. The school community submits nominations, from which recipients are decided upon by the school’s Awards Committee.
Stanley L. Robbins Award for Excellence in Teaching
Christine
Phillips, MD

An assistant professor of medicine and primary care physician at Boston Medical Center (BMC), Phillips specializes in general internal medicine with a focus on student and resident education and clinical skills development. She serves as a co-director for the courses Doctoring 1 and 2 and as director of the Clinical Skills and Simulation Clinic, in which she helped to redesign the preclinical curriculum with emphasis on physical diagnosis, clinical reasoning, and communication skills. To ensure medical students receive early and continuous training in these areas, she has incorporated simulation-based learning and hybrid clinical scenarios, and uses skills trainers who demonstrate a more hands-on approach to mastering physical diagnosis.
Described by a colleague as an exceptional scholar, educator, and innovator in medical
education, Phillips has made a lasting impact through innovative curriculum development, scholarly dissemination, and exceptional teaching. “Dr. Phillips’ invaluable leadership in curriculum development and thoughtful mentorship of students and other educators demonstrate the significant impact she has had on medical student education at our institution,” said the colleague.
Leonard Tow Humanism in Medicine
David Harrison, MD

An assistant professor of obstetrics & gynecology (OB/GYN), Harrison has been an attending OB/GYN at BMC since 1988. According to a colleague, Harrison best exemplifies The Gold Foundation’s ideals of integrity, excellence, collaboration and compassion, altruism, respect and resilience, empathy, and service as shown by his outstanding compassion in the delivery of care and respect for patients, their families, and healthcare colleagues. He serves as a role model for students and other trainees and consistently demonstrates the highest standards of clinical excellence.
“Dr. Harrison is one of the most dedicated providers, repeatedly showing up for his patients when they need him, patiently guiding learners and new providers as they explore clinical decision-making, and leaving an impression on learners, providers, and patients that is memorable and positive,” said the colleague.
Educator of the Year Awards
Preclerkship
Aaron W. Young, PhD
An assistant professor of pharmacology, physiology & biophysics, Young serves as

assistant director of the MS in the Oral Health Sciences program. Prior to joining BU, he completed his undergraduate (HBMSc) and graduate (PhD) training in Canada, both in physiology & pharmacology. Working with athletes and chronic lung disease patients, he did previous research centered on respiratory, cardiovascular, and exercise physiology in a clinical setting.
A colleague says that both Young’s passion for teaching and his extremely student-centric approach are unwavering and impressive, and he goes above and beyond what is required to ensure his students understand a topic or mechanism. According to the colleague, “His ability to use feedback to create better courses is amazing and admirable.”
Clinical
Christine Crawford, MD, MPH
An assistant professor of psychiatry and an adult, child, and adolescent psychiatrist who sees patients in the BMC Child & Adolescent Outpatient Psychiatry Clinic, Crawford serves as vice chair of education in the department of psychiatry and as the department’s director of medical student education. She completed her adult psychiatry residency as well as child and adolescent psychiatry fellowship training at Massachusetts General Hospital/McLean Hospital. Crawford receives consistent feedback from students regarding her infectious energy and engagement, with many saying that she inspired them to pursue psychiatry as a career. “She often challenges students to think about patients holistically, including by pushing them to incorporate social, economic, and cultural factors into their assessments of patients,” said her nominator.

MA/MS Programs
Elizabeth Duffy, MA

An assistant professor of pathology & laboratory medicine, Duffy is director of the MS in Pathology Laboratory Sciences program and director of the Laboratory and Biorepository Research Services Core at BMC.
A colleague who has worked closely with Duffy has witnessed her excellent teaching style, professionalism, and connection with the students. “She is thoughtful, generous with her time, engaging, and stimulates discussion and welcomes the students to speak up and participate. Professor Duffy always gives constructive feedback, which her students clearly enjoy.”
PhD Programs
Barbara Schreiber, PhD

An associate professor of biochemistry & cell biology and assistant dean of alumni affairs in Graduate Medical Sciences (GMS), Schreiber directs graduate studies in the department of biochemistry & cell biology and is past director of the PhD Program in Biomedical Sciences (PiBS). She is course director for a professional skills course taught to first-year PiBS students and also directs the biochemistry class taught to first-year Goldman School of Dental Medicine DMD and GMS Oral Health Sciences students.
“Schreiber has worked tirelessly in GMS education for years teaching classes, serving as the biochemistry program director and director of the Program in Biomedical Sciences. She is more than worthy of this award,” said a nominator.
Resident Educator
Isa Jacoba, MD
A fourth-year resident in pathology & laboratory medicine at BMC, Jacoba has served for the past three years as the principal liaison for third- and fourth-year medical students studying pathology and laboratory medicine for their clerkships.
Described as friendly, kind, effective, efficient, and a clear communicator, Jacoba is a role model of professionalism. According to her nominator, “Dr. Jacoba teaches by example as well as in formal settings, at the microscope, in the surgical pathology dissection laboratory, in formal didactics, and lectures in the classroom. Her teaching skills shine with her knowledge and engaging manner, encouraging students to participate in a safe space, ask questions, and seek out answers.”
Excellence in Research Mentorship, GMS
Neil J. Ganem, PhD

An associate professor of pharmacology, physiology & biophysics, Ganem received his PhD in biochemistry from the Geisel School of Medicine at Dartmouth, where he studied mechanisms of mitotic spindle assembly and chromosome movement in the lab of Duane Compton, PhD. His laboratory uses a combination of high-resolution microscopy, genome-wide RNAi screening, cell biology, and bioinformatics to study the causes and consequences of genome instability in human cancer.
A student nominator describes Ganem as a brilliant scientist and leader in the field of genomic instability and cancer biology, with remarkable qualities as a mentor, particularly in his ability to connect with trainees and
offer personalized guidance to help students achieve their goals. “Dr. Ganem has established a highly collaborative and welcoming lab environment where students of all levels can learn and conduct research. He routinely encourages us to take ownership of our projects, think creatively, and ask important questions, while also providing guidance in carrying out rigorous and thoughtful scientific research.”
Excellence in Research Mentorship, MD Program
Charlene Ong, MD, MPHS

An assistant professor of neurology & neurosurgery and a clinical neuro-intensivist at BMC, Ong does research that focuses on the development and validation of data-driven tools to support clinical decision-making in patients with catastrophic neurologic injury, including ischemic and hemorrhagic stroke, traumatic brain injury, and anoxic brain injury. Ong received her undergraduate degree from the University of Pennsylvania, MD from Columbia University, and Master of Population Health Sciences from Washington University School of Medicine. According to a student nominator, Ong is an exceptional mentor who makes an enormous effort to guide, support, and inspire her mentees. “Her dedication to mentorship, commitment to fostering future physician-scientists, and ability to inspire curiosity and critical thinking make her truly deserving of this recognition,” said the nominator.
Excellence in Faculty Mentorship, Early Career Faculty
Heather Hsu, MD, MPH
An assistant professor of pediatrics and a pediatric hospitalist at BMC, Hsu also serves as the scientific director of BMC’s Clinical

Data Warehouse for Research. Within the department of pediatrics and the Boston Combined Residency Program, Hsu is a founder and lead faculty mentor for Health Equity Rounds, a solutions-oriented, resident-led, case-based conference series focused on illuminating and eliminating the impact of racism, bias, and other intersectional forms of systemic oppression on health and healthcare.
According to Hsu’s nominator, her mentorship has been invaluable for her students’ career growth. “As a research project mentor to me, Heather fostered space for my creativity, was incredibly responsive, and made herself available for regular meetings to provide very helpful feedback. She also continues to serve as a peer mentor to me, giving me advice on navigating academia and the challenges of conducting research.”
Excellence in Faculty Mentorship, Senior Faculty
Craig Noronha, MD

A clinical associate professor of medicine and associate chief for education for the section of general internal medicine at BMC, Noronha also is associate program director of the Internal Medicine Residency program and has held key leadership positions in residency education, including director of ambulatory education, director of quality improvement and patient safety education, and director of professional development. He currently coleads a department of medicine initiative aimed at improving feedback across all departmental members.
According to his nominator, Noronha has sought to use his experience and the challenges he has faced in his career to help empower both junior faculty members and his peers, actively seeking out opportunities to work with colleagues to help them define and achieve their professional goals.
Community Service & Engagement
Kaku So-Armah, PhD

An associate professor of medicine, So-Armah is an epidemiologist with expertise in cross-sectional and longitudinal analyses of cohort studies and the use of electronic health record data for research. His lab employs molecular biology coupled with data on health behaviors, risk factors, and disease diagnoses to identify and explain novel epidemiological associations and identify novel intervention targets.
He engages with patient populations who live in resource-limited settings and have been historically excluded from informed participation in biomedical research. So-Armah’s long-term goal is to translate the growing understanding of the mechanisms of excess HIV and substance use-related comorbid disease risk into effective, sustainable interventions.
So-Armah has worked to increase pathways for underrepresented trainees to enter the field of HIV research through both mentorship and formal programs. “Dr. So-Armah advocates for the recruitment of underrepresented students and ensures the course content is representative of our diverse clinical faculty. He also takes every opportunity to provide mentorship to underrepresented faculty and students,” said his nominator.
Above and Beyond Staff Award
Laura Anastasi
Anastasi joined the geriatrics section in the department of medicine in 1986 and has held various roles including administrative manager, financial manager, and section administrator before assuming her current role of administrative director in 2015.

In 2013, she received the inaugural George Rosenthal Award for Service Excellence within the Geriatrics Section. In 2014, she received the department of medicine’s Administration Award for Outstanding Achievement, and in 2023 she won the STARDoM Award for recognition of service, thoughtfulness, extraordinary dedication, and overall excellence within the department of medicine.
According to her nominator, Anastasi’s excellence, passion, and dedication to the geriatrics section—as well as to the department and University—have been apparent year in and year out. “She has an exemplary work ethic and customer service expertise. I consider her a role model in this respect and am proud to have her as a colleague,” said the nominator.
Above and Beyond Staff Award
Nicholas J. DiPersio

The executive director of finance, administration & operations for the Framingham Heart Study (FHS), DiPersio oversees all aspects of financial planning and analysis for the FHS Center’s portfolio of sponsored programs and institutional accounts. He also oversees administration—including human resources— and operations for an organization of approximately 75 employees.
His role centers on strategic decisionmaking, ensuring the organization remains properly staffed, financially sound, and operationally efficient. He collaborates closely with FHS leadership to drive key initiatives, enhance organizational effectiveness, and align resources with long-term objectives and urgent priorities. While he provides direct leadership to the administrative and financial teams, he also maintains broad oversight of the entire organization through structured reporting lines.
According to his nominator, DiPersio “exemplifies all of the criteria described in this award, consistently exceeds expectations, and innovates to the benefit of the entire school and BU community.” ●
Bottom left corner, fourth-year MD/PhD candidate Kristen Segars, wearing a shawl and hat she knitted herself. Bottom center, third-year medical students Nick Whitcomb and Kyle Quan Bui out on a run.
WORK LIFE
From 5Ks to knitting, wellness programs help medical and graduate students build


AS AN UNDERGRAD AT WILLIAMS
COLLEGE, third-year medical student Nick Whitcomb was a competitive intercollegiate swimmer.
“It took up 20-plus hours of my week, but it was very therapeutic for me,” he says.
The workouts and competition schedule helped get him through a rigorous premed curriculum, but medical school has been even more demanding of his time, with little opportunity for workouts—a challenging situation for someone who’d been a competitive swimmer since the age of six.
“For the first month or so, I felt like there was a big part of me missing,” says Whitcomb. “I was very wound up and didn’t have that outlet to exercise and be social.”
He tried to take advantage of FitRec’s competition pool on the Charles River Campus with the goal of training for an Olympic tryout, but the added commute time and the official pool hours didn’t fit his schedule.
That’s when Whitcomb discovered the Medical Student Wellbeing program managed by the Student Affairs office. Embracing the opportunities the program offered, he participated in its annual 5K road race and joined the Medical Campus Run Club’s weekly group run.
“I started going to all the wellness events, and it was really nice to have that social outlet. Arguably, that was the more important part for me, because I’ve met all my closest friends through Run Club,” says Whitcomb. He now serves as the club’s coleader and as the physical wellness steering leader for the Wellness Initiative, which is run by medical students working directly with Student Affairs to promote student wellness, resource development and sharing, and wellness-centered events.
Wellness programs help medical students navigate the stresses of medical school and prepare them for life as physicians by building resiliency and self-awareness. They offer support and resources for students facing personal and academic challenges and foster recognition of the concept that professional excellence is linked to self-care.


“The focus is on helping medical students to understand that their wellness, their wellbeing, is their responsibility. We can help by providing different opportunities,” says Angela Jackson, MD, associate dean of student affairs and associate professor of medicine. “We can provide support to help students actively engage in developing the skills to meet their individual needs and to be able to manage and secure their wellbeing moving forward as physicians.”
The importance of self-care also is at the core of wellness programming offered by Graduate Medical Sciences (GMS) for master’s and PhD students.
“If you don’t decide early on that you’re going to have some sort of balance between personal wellbeing, academics, and professional development, you are not going to survive a sixyear PhD program, or a one- or two-year master’s program that may be a stepping stone to medical or dental school,” says Theresa Davies-Heerema, PhD, assistant dean for GMS master’s programs and clinical associate professor of medical sciences & education. “You need to learn how to
balance academics and taking care of yourself. Have some time for yourself and your friends.”
Earning the MD/PhD is a marathon of learning and research taking between seven and 10 years to complete. According to Kristen Segars, a fourth-year MD/PhD candidate, students are constantly being compared to each other.

“The good thing about wellness clubs, in general, is that they encourage students to feel good about something that’s just for them,” says Segars, who joined the wellness program’s knitting club in her second year of medical school and has since produced hundreds of knitted items.
“You’re not just a doctor, you’re not just a scientist, you’re not just a student. You’re a whole person. Part of that is doing things for fun, doing things that make you happy and that you’re passionate about.”
BU’s History of Concern for Student Wellbeing
In 2019, the Wellbeing Project launched as a University-wide initiative. BU created the
Student Wellbeing office in 2021, the same year the medical school started its Medical Student Wellbeing program and GMS unveiled the Community Catalyst Center (C3) to support its more than 1,000 graduate students.
Graduate and medical schools have a critical window of opportunity to address issues around work-life balance, mental health, financial health, and other topics before students begin their postgraduate careers.
In response to concerns about medical student wellbeing and the link to physician burnout, the Liaison Committee on Medical Education now includes medical student wellness as one of their medical school accreditation standards, requiring schools to provide “an effective system that promotes wellbeing and facilitates adjustment to the physical and emotional demands of medical education.”
Across the University, the wellbeing template includes an emphasis on physical, emotional, intellectual, financial, community, and ethical wellness. Programming incorporates social activities as well as professional and personal development.

Members of the Run Club gather for a group photo.
The Run Club on a weekly run with Nick Whitcomb (left).


Wellness Programming Addresses Academic Stress Points
Jackson explains that programming for MD students focuses on the four stress points in academic life: arrival at the medical school; preparation for the Step 1 test; the transition to clinical rotations in the third year; and matching to resident training programs in the fourth year.
The Medical Student Wellbeing program includes individual resources and a variety of events including a wellness fair, a fall mixer, a 5K run, and more. The program also offers book clubs, cooking classes, career planning and professional events, yoga, and access to mental health and nutrition resources. Most of these ideas—and many others—are in response to MD student feedback represented by the Wellness Committee, composed of Wellness Initiative student members, medical student wellness representatives from the Student Committee on Medical School Affairs (SCOMSA), the Student Affairs office wellness program coordinator, and the dean.
In 2022, the Medical Student Wellbeing program was officially integrated into the advising curriculum. Faculty from the Academy of Medical Educators serve as core advisors for
students for 30-minute, one-on-one sessions for the entirety of their medical school studies, with sessions occurring during the 9–5 class day.
“These advisors have a unique relationship with the student because they are teaching doctoring,” says Tiffany Wong, MA, program coordinator, Student Wellbeing & Advising.
“We always give students freedom to talk about something that’s pressing, that they really want to share in this dedicated, intentional time with their core advisor.”
Through the Student Affairs office, the Medical Student Wellbeing program also offers a voluntary 15-minute individualized wellness check-in, a one-on-one session with Wong during which students identify areas of improvement concerning their wellbeing, decide on an action plan, and secure resources to help implement it.
Commitment at the Highest Levels
In 2023, Medical School Dean and Medical Campus Provost Karen Antman, MD, created a Dean’s Advisory Board (DAB) Wellness Task Force to gather student input and make recommendations.
Second-year medical students Aryan Wadhwa (second from left) and Giulio Cataldo (third from left) showcase budgetfriendly recipes for their classmates in the Student Wellbeing program’s student-led cooking classes.
Last year, the Dean’s Advisory Board established the Student Wellness Fund to provide resources for student wellness initiatives.


“We were asked how we make life better for medical students,” recalls Elizabeth Brown, MD, associate professor of pediatrics at the school from 1987 to 2016, DAB member and cochair of the Wellness Task Force. Topping the student wish list was the request for a fitness center, also a popular request from GMS students.
The task force identified unused space in the basement of the main Instructional Building. A $1 million donation by Dean’s Advisory Board member Richard J. Catrambone, DMD, MD’92, and his wife Sophia Catrambone is a big step towards making the $2 million facility a reality.
(See sidebar, page 34.)
Last year, the Dean’s Advisory Board established the Student Wellness Fund to provide resources for student wellness initiatives.
“As students, back in 1989, we were focused on academics and managing our student debt,” says Patricia Williams, MD’89, former vice president of Worldwide Safety, Surveillance, and Risk Management for the global pharmaceutical company Pfizer. “Students today worry about academics and debt, but they also prioritize worklife balance, as does the Chobanian & Avedisian School of Medicine, which is a positive change to medical education.”
Fourth-year medical student and SCOMSA Wellness Liaison Christina Jefferson said she entered medical school a happy, social person, but the demands of medical education on personal and family time eroded some of her joy. Participating in the Student Wellness Initiative has made her more cognizant of her personal needs.
“I feel like it’s a constant conversation with yourself,” Jefferson says. “I know that I will not be that person who just does their job every day— and their job becomes their life. I would like a good work-life balance, and I feel like prioritizing my happiness and my wellness now, hopefully, can be the foundation for my future wellness.”
Graduate Student Pressures Take a Toll
Among other factors, long hours, the pressure to publish, increased competition for grants, higher data requirements for publication, the rising cost of living expenses, mentor/mentee relationships, and funding and employment uncertainties have increased the stress on graduate students.
(continued on page 35)
Fourth-year MD/PhD candidate Kristen Segars in her lab.
New Medical Campus Fitness Center Gets Big Boost with $1M Alumni Gift
Fitness Center Topped the Medical Student Wish List


Thanks to a $1 million donation by Chobanian & Avedisian School of Medicine
Dean’s Advisory Board member Richard J. Catrambone, DMD, MD’92, and his wife Sophia Catrambone, a new Medical Campus fitness center is close to becoming a reality.
“Physical fitness is important to Sophia and me, and to both of our children. When this proposal came along, it really resonated with me,” said Catrambone, adding that starting a fitness program and healthy eating habits as a student can help a physician attain a better work-life balance, be more resilient, and prevent burnout.
“When this proposal came before the advisory board, with so many students expressing the need for such a facility, I felt it was important for Sophia and me to support students in achieving that healthy balance as they navigate the stress of graduate and medical school.”
After graduating with honors from Assumption College and Tufts University School of Dental Medicine, Richard Catrambone completed a four-year residency in oral and maxillofacial surgery at Tufts, followed by a one-year fellowship in anesthesiology at Boston City Hospital. He went on to graduate with honors from Boston University Chobanian & Avedisian
School of Medicine, after which he completed a PGY-2 year of general surgery training at Boston’s Beth Israel Hospital.
Catrambone has served as president of the medical school’s alumni association and as a vice president on the association’s alumni board. He currently practices oral and maxillofacial surgery in Brockton, Massachusetts, with his daughter, Karina E. Catrambone, DMD, CAS’12, and son-in-law Brandon J. Saxe, DMD. His son Christopher J. Catrambone, JD, is an estate law planner.
In preliminary drawings, the 2,450-squarefoot Catrambone Fitness Center includes 1,800 square feet of workout space with various machines, treadmills, free weights, and a yoga area, along with 640 square feet of men’s and women’s locker rooms with bathroom facilities and showers. With a total cost estimated at $2 million, the center will be built in existing unused space on the ground floor of the Instructional Building across from Chequers.
“It’s so exciting. It will make a huge difference for students,” said Associate Dean of Student Affairs Angela Jackson, MD. “They have finite disposable time and money, and to spend any of it commuting to FitRec (the University’s fitness and recreation center on the Charles River Campus) or paying to join a
private gym doesn’t work.”
A fitness center has consistently been a top student request—as communicated through informal discussions, the Student Committee on Medical School Affairs, and on campus wellness surveys—and a longterm goal of Student Affairs and Dean Karen Antman, MD.
According to Jackson, key meetings with the Dean’s Advisory Board task force on student wellness helped promote the proposal.
“The dean had always been 100 percent on board. She had the plan of where it would be located. But funding was needed. We don’t have endless resources. We have to be thoughtful about what gets pushed forward, and the fitness center’s time has come,” she said.
A fundraising campaign has been initiated to raise the remaining $1 million. Richard and Sophia Catrambone encourage alumni, parents, and friends to also donate generously to realize the goal of making the Catrambone Fitness Center a reality for Medical Campus students.
To donate or for more information, please contact Suzanne Maselli, associate dean of development, at smaselli@bu.edu or at 617-358-9530.
Richard Catrambone, DMD, MD’92, and his wife Sophia Catrambone.

“I think BU has a pretty good culture of wellness. Most people are aware that the Wellness Committee exists and that there is programming that reaches out to varied groups of people and their different interests.”
THIRD-YEAR MEDICAL STUDENT KYLE QUAN BUI
Known as C3, the GMS Community Catalyst Center opened its doors in August 2021 with the aim of creating communities for more than 1,000 graduate students across 30 degree programs to help them adjust to Boston and the Medical Campus. Eight affinity centers now welcome students of similar backgrounds including international students, nontraditional and first-generation students, military veterans, and LGBTQIA+ students. C3 provides resources and hosts events and workshops to support students throughout their time in graduate school.
While the Medical Student Wellbeing program serves a smaller, more homogenous MD student body, GMS wellness programs face challenges in the number of students and programs as well as the range of timeframes leading to degrees. Programs vary from a year in Oral Health Sciences, a pre-dental program, to five or more years for students pursuing a doctorate.
“C3 is a community resource center for GMS students,” says Community Relations Specialist and C3 Manager Sarah Rowan. “It aims to foster holistic success across the GMS community in various buckets like academic growth, social learning, professional development, and community building.”
President of the Biomedical PhD Student Organization—which was founded to build and strengthen community among students in PhD programs, especially those in biomedical science—third-year PhD student Kaitlyn Alimenti says that C3 offers a central location on campus to easily find information, or to meet others.
“The affinity groups have been very helpful for PhD students on the Medical Campus. It
gives students from marginalized backgrounds the opportunity to talk to people about issues that labmates might not necessarily talk about,” Alimenti says. “It’s less about creating a distinctive group of people who are going to hang out over and over again, and more about having friendly faces and meeting people who have similar backgrounds or struggles.”
The Role Student Input Plays
Generated through student interactions with staff and faculty, surveys, and student wellness advisory groups, student input is critical to the success of wellness programs. Alimenti points to student feedback resulting in the creation of a private space where students can go to receive telehealth mental health counseling.
Student input also inspired MD Student Affairs to successfully advocate for changes to the academic calendar. Exams for first-, second-, and third-year students are now scheduled for Fridays, giving students the weekend to decompress. Students Affairs also helped incorporate three personal days per semester—available to be used for any reason— into third-year student rotations.
“If we only focus on school all the time, it can be really difficult and draining,” says third-year medical student Kyle Quan Bui, who serves as Class of 2027 SCOMSA vice chair and as a liaison to the Student Wellness Committee. “I think BU has a pretty good culture of wellness. Most people are aware that the Wellness Committee exists and that there is programming that reaches out to varied groups of people and their different interests.” ●
● Study Explores Race, Ethnicity Dynamics, and Survival in the US
Though African Americans have higher death rates before their 80s, after about age 85, their age-specific death rate falls below that of the white population, a phenomenon known as the Black-White mortality crossover. New research published in the Journal of Internal Medicine reveals that this lower mortality among African Americans persists to age 100+ years.
The study relied on data adjusted for potential misreporting of age, race, and ethnicity from the US National Center for Health Statistics—as well as other life table variables—to obtain life expectancy at birth and at ages 70, 85, and 100 years according to year, sex, race, and ethnicity.
When Asian population data became available in 2019, African Americans had the second-lowest life expectancies at birth in the US (74 years for women and 68 for men). However, after age 86 for women and age 88 for men, African Americans had lower death rates compared with whites. Death rates for Black and Hispanic populations became similar to the Asian population’s death rate around age 98, while the white population’s higher death rate persisted at these oldest ages.
The researchers hypothesize that African Americans who live beyond about age 85 are a select survivor group, with resilience due to psychosocial and biological factors that allow them to withstand socioeconomic disadvantages and other causes of higher mortality risk, which enables them to have lower death rates after age 85 and up to age 100 compared with whites.
“This study reinforces that people with different racial or ethnic backgrounds may vary in what characteristics determine how well and how long they live,” explains corresponding author Thomas Perls, MD, MPH, professor of medicine and geriatrics, and director of the New England Centenarian Study. ●
To investigate the relationships between duration of ice hockey play and CTE diagnosis and severity, the researchers studied male brain donors who had been amateur and professional ice hockey players.
● Study of CTE in Male Ice Hockey Players Finds Odds Increase with Each Year Played
In the largest study of its kind to date of chronic traumatic encephalopathy (CTE), the Boston University CTE Center studied 77 deceased male ice hockey players and found that the odds of having (CTE) increased by 34% each year played, and that 18 of 19 National Hockey League players studied had CTE.
A neurodegenerative disease caused by repeated traumatic brain injuries and most frequently found in former contact sport athletes exposed to repetitive head impacts (RHI), CTE is often perceived as a risk limited to hockey enforcers. This study makes it clear that all male ice hockey players are at risk.
“Ice hockey players with longer careers not only were more likely to have CTE, but they also had more severe disease,” says corresponding author Jesse Mez, MD, MS, codirector of clinical research at the CTE Center and associate professor of neurology.
To investigate the relationships between duration of ice hockey play and CTE diagnosis and severity, the researchers studied male brain donors who had been amateur and professional ice hockey players. They found 96% (27 of 28) of professional players had CTE pathology (18 of 19 NHL and 9 of 9 non-NHL professionals); as well as 46% of college, juniors, and semi-professional players (13 of 28); and 10% (2 of 21) youth and high school players.
Researchers stress that the frequencies of CTE reported in this study should not be construed as the prevalence of CTE in the target population, since families whose loved ones are symptomatic are more likely to donate their brains. ●

● Scientists Uncover Structure of Critical Component in Deadly Nipah Virus
Researchers at Boston University Chobanian & Avedisian School of Medicine and Harvard Medical School have mapped a critical component of the Nipah virus, a highly lethal bat-borne pathogen that has caused outbreaks in humans almost every year since it was identified in 1999.
The advance, described in Cell, brings scientists a step closer to developing much-needed medicines. Currently, there are no vaccines to prevent or mitigate infection and no effective treatments for the Nipah virus other than supportive care.
The researchers homed in on a part of the viral machinery called the viral polymerase complex, a group of proteins the virus uses to copy its genetic material, spread, and infect cells. The work provides a detailed three-dimensional picture of the virus’s polymerase and its key features. Understanding the structure and behavior of this critical piece of the viral machinery illuminates how the pathogen multiplies inside its hosts.
Researchers conducted the experiments in two different ways. First, they purified the polymerase and determined its structure using cryo-electron microscopy, a technique that allows scientists to visualize the structure of biologic samples at the scale of individual molecules. Second, they induced mutations in the polymerase and then observed how the mutated polymerase behaved in cells to understand how these mutations affected its function.
“Identifying how the polymerase is regulated to switch on and switch off the different enzymatic activities that are required for viral replication would be game-changing, and this study represents a key step towards that goal,” says study co-corresponding author Rachel Fearns, PhD, chair and Ernest Barsamian Professor of Virology, Immunology & Microbiology.
Until now, the structure and function of the Nipah virus polymerase was poorly understood, researchers say, cautioning that further research would be needed to fully understand how the polymerase makes the different types of genetic materials that enable the virus to multiply. ●
The advance, described in Cell, brings scientists a step closer to developing much-needed medicines.
● Study Finds Consumer Devices Can Be Used to Assess Brain Health
Technology is changing how physicians think about assessing patients and, in turn, how patients expect to be able to measure their own health. Apps designed for smartphones and wearable devices can provide unique insights into a user’s brain health.
A study in Nature Medicine found widely used consumer-grade digital devices, such as the iPhone and Apple Watch, can be effective in assessing an individual’s cognitive health without requiring in-person visits or supervision. This is the largest cognition study of its kind to demonstrate that self-administered cognitive assessments can be leveraged to accurately assess cognitive health over time.
“In the long term, we may be able to track digital health metrics and identify those reflecting cognitive changes that are on a trajectory of decline and warrant follow-up with a medical professional to determine if an early intervention treatment plan is needed to either slow or prevent progression,” says coauthor Rhoda Au, PhD, professor of anatomy & neurobiology.
The study enrolled more than 23,000 adults from across the US who used an iPhone. Broad enrollment included individuals who consented to sharing their data and were 21–86 years of age. Both cognitively healthy individuals as well as those who were diagnosed with mild cognitive impairment participated.
Of the participants enrolled, over 90% were able to adhere to the study protocol for at least one year, which included using an iPhone and wearing an Apple Watch on a daily basis, as well as taking cognitive assessments on their own and completing questionnaires at monthly and quarterly intervals.
The ability to accurately measure cognitive health remotely could be the first step in providing individuals with the information they need to actively improve their

Collaboration Between BU Clinicians, Basic Scientists, and Engineers Can Lead to New Disease-Fighting Drugs
Recent studies illustrate that together, basic science and clinical research can lead to new trials, treatments
New drugs and therapeutic solutions don’t suddenly appear—they are rooted in collaboration between basic and clinical science research. In two examples, BU researchers have seen their basic science research of devastating diseases, for which therapy remains limited, advance to the clinical phase.
“Understanding basic mechanisms that lead to diseases can identify targets for the further development of therapeutics and new diagnostic tools,” said Katya Ravid, DSc, Barbara E. Corkey Professor of Medicine and founding director of the Evans Center for Interdisciplinary Biomedical Research, of which novel Affinity Research Collaboratives (ARCs) are building blocks.
With central support from the Department of Medicine, along with the BU Clinical and Translational Science Institute, BU Associate Provost for Research Office, BUMC Provost’s Office, and recently, Boston Medical Center (BMC), ARCs use interdisciplinary, convergence science approaches—integrating the physical and biological sciences—to address complex medical problems. According to Ravid, studies aiming to identify mechanisms behind the pathophysiology of disease are, importantly, largely funded by the National Institutes of Health.
Basic science research can make the leap to clinical studies and new drugs and/or treatments through two main routes, one of which is for biotech companies to learn about advancements through published research and opt to develop them into possible clinical applications. The other route involves investigators pursuing their own findings with the support of the school’s technology development office, and the help of additional funding sources.


Ravid’s lab studies mutations in blood stem cells that are generally associated with aging and cause primary myelofibrosis (PMF), a disease that manifests as uncontrolled proliferation of blood cells and the appearance of a very dense, nearly clogged fibrotic bone marrow hindering the ability to produce a normal balance of different blood cells. Symptoms also include abnormal blood cell counts, an enlarged spleen, and damage to veins carrying blood from the spleen to the liver. In some cases, PMF can lead to myeloid leukemia.
“This is a harsh disease for which current therapies are still only partially effective,” said Ravid. While studying cellular reprogramming in the mutated cells, her lab found that lysyl oxidase (LOX) was highly expressed in mutated blood cells of the platelet lineage. Ravid and her lab mentees found that inhibiting this enzyme in experimental models reduced bone marrow clogging and other hallmarks of the disease, and identified cellular mechanisms that lead to this favorable outcome.
The published studies from this research attracted the attention of the biotech company Pharmaxis (renamed Syntara in 2023), which provided the Ravid Lab with more specific pharmacologic inhibitors of LOX for further testing. Successful results obtained and published by Ravid’s lab prompted a clinical trial with favorable results in human cohorts, which was published in April 2025 in the journal Haematologica
That study concluded that preliminary indications of clinical efficacy were evident, including a reduction in bone marrow clogging collagen, and that continued investigation was warranted for the LOX inhibitor PXS-5505 as a possible remedy for PMF.
Led by Vipul Chitalia, MD, PhD, professor of medicine & pathology, and Jean Francis, MD, associate professor of medicine and medical director of BMC’s Kidney Transplant Program, another study investigating the role of the protein interleukin-6 (IL-6) in the disease calciphylaxis also resulted in clinical trials. Chitalia and Francis are coleaders of the Thrombosis and Hemostasis ARC.
Calciphylaxis is a rare disease characterized by dermal microvessel thrombosis, the
blockage of small blood vessels in the skin that results in skin tissue death. Occurring mostly in those with end-stage kidney disease, calciphylaxis, afflicts patients with debilitating pain, recurrent hospitalizations, limited mobility, depression, poor quality of life, and brings with it a high (45–80%) annual mortality. The molecular events driving calciphylaxis are largely unknown, which has significantly impeded the development of a disease marker and targeted therapies.
“To date, there is no approved therapy for calciphylaxis and we have only off-label therapies that are ineffective and not well tolerated,” said Chitalia.
Along with collaborators, Chitalia and Francis examined skin and blood samples from calciphylaxis patients and investigated a highly potent and prevalent blood-clotting pathway that was triggered by IL-6, an inflammatory protein. Researchers found that excess IL-6 initiated thrombosis resulting in rapidly expanding skin necrosis.
Published in April 2025 in the journal Science Translational Medicine, the study concluded that results supported exploring IL-6 clot-forming as a marker and possible target for therapeutic medicines, which attracted the interest of pharmaceutical companies that had approved anti-IL-6 antibodies.
“This body of work paved the way to treat calciphylaxis with anti-IL-6 therapeutics. We have initiated a pilot study at BMC, where our first patient showed encouraging results,” said Francis.
Ravid said the calciphylaxis research is an example of how ARCs work.
“This study is a manifestation of the creativity of our faculty, aided by the strong interdisciplinary research and platforms that we have developed here at the medical school through ARCs that can really bring such research to fruition; first through the basic discovery and publication, and then taking it beyond,” Ravid said. “[With ARCs] we see fruits of collaboration between clinicians, basic scientists, and engineers across all BU campuses, in line with our long-standing mission of promoting multidisciplinary, convergence science.” ●
From left, Jean Francis, MD, Vipul Chitalia, MD, PhD, and Katya Ravid, DSc.
Venetia Zachariou, PhD, Receives Distinguished Investigator Award to Study Novel Therapeutics Targets for Chronic Pain Conditions giving

Venetia Zachariou, PhD, Edward Avedisian Professor and chair of pharmacology, physiology & biophysics, has received a Distinguished Investigator award from the Brain & Behavior Research Foundation (BBRF). The one-year, $100,000 grant will fund her research, “Targeting G Protein Pathways in the Periaqueductal Gray to Optimize the Actions of Opioids.”
Morphine, oxycodone, and other opioids possess strong analgesic properties, but their long-term use can result in developing tolerance, dependence, and transitioning to addiction. Identification of intracellular pathways and circuits that promote the analgesic efficacy of opioids without increasing the risk of addiction may represent opportunities for therapeutic avenues.
The award will support Zachariou’s research on understudied G protein signal-
ing complexes that regulate transcriptional activity within brain regions involved in pain perception and analgesia; these signaling complexes also affect the activity of neuronal projections that mediate the rewarding effects of opioids. By targeting these multiprotein complexes, Zachariou aims to block the addiction-related effects of opioids while enhancing their analgesic properties.
“Opioid use disorders are rising in the general population, as well as among chronic pain patients. Research efforts are needed to decipher the intracellular pathways mediating the actions of opioids,” Zachariou explains.
Zachariou studies signal transduction and epigenetic mechanisms of neurological disorders and their treatment using genetic experimental models, genomic assays, and brain biochemistry. Her projects have investigated transcriptional and epigenetic mechanisms of chronic pain with emphasis on the identification and validation of novel treatments for the management of peripheral neuropathy and other chronic pain conditions. Her team has identified several intracellular pathways that control the perception and the maintenance of chronic pain states and has also developed novel interventions in epigenetic pathways that allow transitioning to nonopioid analgesics while preventing the development of physical dependence.
Zachariou received her BSc in pharmacy from the University of Patras, Greece, and her PhD in pharmacology from the Medical College of Georgia. Following a
postdoctoral fellowship in the department of psychiatry at Yale University and a junior faculty position at UT Southwestern Medical Center in Dallas, she established her laboratory at the University of Crete School of Medicine. In 2012, she joined the departments of neuroscience and pharmacological sciences at the Icahn School of Medicine at Mount Sinai in New York as an associate and full professor before joining BU in 2023.
Zachariou is a member of the editorial boards of Biological Psychiatry, Science Signaling, Neurobiology of Pain, British Journal of Pharmacology, and Molecular Pharmacology She is a fellow in the American College of Neuropsychopharmacology and chair of the ASPET Neuropharmacology Division.
BBRF Distinguished Investigator Grants fund talented, established scientists with a record of outstanding research accomplishments. These research projects are intended to provide new approaches to understanding or treating severe mental illness. If successful, the grants could result in later funding from other sources. These grants are among the most competitive in mental health research and demonstrate the power of investigator-initiated research to produce new and creative ideas ●
Wendy Kuohung, MD, Awarded March of Dimes Grant to Uncover Therapeutic Agents for Preeclampsia

Wendy Kuohung, MD, associate professor of obstetrics & gynecology, has received a two-year Discovery Research Grant from March of Dimes. The $200,000 award will fund her research, “APOL1 variant-overexpressing cell lines in compound screening for preeclampsia (PE) drug discovery.”
Preeclampsia is a pregnancy complication characterized by high blood pressure (hypertension), swelling (edema), and protein in the urine (proteinuria) that typically occurs after 20 weeks of gestation. While the exact cause is unknown, PE is believed to be related to an abnormal interaction between the placenta and the mother’s blood vessels. Therapies for this disorder have not advanced in more than a century.
Kuohung will develop an assay to identify drugs that could treat PE in women who have genetic mutations that increase
their risk. These genetic mutations—called APOL1 gene variants—are thought to be particularly important in the development of PE in Black women, who are 60% more likely to have the condition compared to white women. Kuohung’s assay will involve adding hundreds of different drug compounds to placental cells expressing APOL1 gene variants; compounds that decrease cellular stress markers in her assay may be good candidates for novel drug therapies to
light on the pathophysiological mechanisms underlying this cryptic obstetrical disorder,” says Kuohung, who also is director of the division of reproductive endocrinology at Boston Medical Center (BMC).
Kuohung is an expert in treating infertility, fertility preservation, in vitro fertilization, menstrual disorders, fibroids, endometriosis, Müllerian anomalies, and in conducting minimally invasive and robotic gynecologic surgery. Her research interests lie in disparities in reproductive care, placental development, and the microbiome of the reproductive tract.
Kuohung received her MD from the Yale University School of Medicine, completed her residency in obstetrics & gynecology at BMC, and conducted fellowship training in reproductive endocrinology and infertility at Brigham and Women’s Hospital/Harvard Medical School.
“Our research to screen libraries of novel and existing drugs for safe and effective preeclampsia therapeutics will advance the field of women’s health and may help to mitigate the Black maternal health crisis in the US.”
treat PE. In addition, she will conduct original, first-of-its-kind research into how PE develops using the placental cells carrying APOL1 variants.
“Our research to screen libraries of novel and existing drugs for safe and effective preeclampsia therapeutics will advance the field of women’s health and may help to mitigate the Black maternal health crisis in the US. Identification of lead compounds effective against PE may also finally shed
March of Dimes is a nonprofit organization committed to ending preventable maternal health risks and death, ending preventable preterm birth and infant death, and closing the health equity gap for all families. March of Dimes Discovery Research Grants are annual awards for established scientists with a long history of published work in maternal fetal health and related fields. ●
Researchers Discuss Their Work During Women’s Health Webinar

In her introduction to the webinar, “Women’s Health: Research Between Bench and Bedside” organized by BU Development, then-Medical Campus Provost and Dean of Chobanian & Avedisian School of Medicine Karen Antman, MD, noted that historically, women have been underrepresented in health studies, including animal studies that only used males and studies that excluded women of childbearing age.
“Research has not focused on sex- and gender-based differences,” Antman told the audience of 120 in attendance.
Antman cited Boston University’s ongo-
ing important women’s health research at the Framingham Heart Study and the Black Women’s Health Study, plus studies on women military veterans and gender differences in PTSD, intimate partner violence and military sexual trauma, and numerous other research projects.
Emelia Benjamin, MD, ScM, associate provost for faculty development, introduced the webinar’s four speakers: Associate Professor of Medicine Kimberly Bertrand, ScD; Professor of Biomedical Engineering Catherine Klapperich, PhD; Professor of Pediatrics Elisha Wachman, MD’06; and Professor of Epidemiology Lauren Wise, MSc, ScD.
The Klapperich Laboratory is focused on lab- and organ-on-a-chip technologies, particularly as they apply to female reproductive tissues. Lab-on-a-chip is a miniature device that can perform lab functions like blood screens, while organ-on-a-chip is a small, handheld device that mimics human physiology using microchips. The Klapperich Lab grows tissues, cells, or organs on these small microfluidic chips.
Klapperich discussed her research on placental malaria, uterine fibroid organoids, and the role of extravillous trophoblasts in preeclampsia. Her remarks focused on human papillomavirus (HPV), a sexually transmitted
disease that can cause cervical cancer. HPV has been dramatically reduced in the US through an HPV vaccine, but kills upwards of 240,000 women a year worldwide, mostly in developing countries with limited screening technologies.
Klapperich’s lab is working on technology, similar in design to an at-home pregnancy test, that could detect HPV quickly, avoiding the long trips to a clinic and extended wait times for lab test results.
“Cost-benefit analyses that have been done in rural settings have shown that HPV testing, even once in a lifetime, can make a measurable difference in the survivability of cervical cancers in those settings,” said Klapperich.
“A lot of it is focused on nonpharmacologic measures like ‘rooming in’ at the hospital, where the mother and baby are cared for in the same room, promoting breastfeeding and [other] models that have been shown to dramatically improve outcomes,” Wachman said.
Wise is principal investigator of Pregnancy Study Online (PRESTO), an internet-based examination of more than 22,000 North American couples that has been funded by the National Institutes of Health since 2013. She cited statistics showing that since 2007, US fertility rates have been consistently below replacement levels. In 2023, that rate fell to the lowest in recorded history. Similar
“ We here at BU have been innovators in the treatment of opioid use disorder in pregnancy and at the forefront of developing what is now becoming the standard of care for these pregnant people and infants.”
PROFESSOR OF PEDIATRICS ELISHA WACHMAN, MD
Wachman completed her pediatric residency in the Boston Combined Program, and now is a neonatologist at Boston Medical Center. Most of her work has centered around infants exposed to opioids who develop neonatal opioid withdrawal syndrome.
“We here at BU have been innovators in the treatment of opioid use disorder in pregnancy and at the forefront of developing what is now becoming the standard of care for these pregnant people and infants,” Wachman said. Her research looks at ways to optimize treatment of these infants, but also how to make this experience more family centered.
declines have been observed in semen quality worldwide, and it is unclear what factors are driving these trends. Over the past two decades, the use of fertility treatments has increased substantially in the US, but these treatments are expensive and inaccessible to most Americans, and there are large racial and socioeconomic disparities in treatment success rates.
“Thus, identifying modifiable determinants of infertility is an important public health goal,” Wise said.
PRESTO participants complete periodic online questionnaires during the preconception, pregnancy, and postpartum periods. PRESTO research has shown that
preconception exposure to stress, depressive symptoms, poor diet, and certain endocrine-disrupting chemicals may reduce fertility.
For example, a Mediterranean diet involving higher consumption of vegetables, fruits, whole grains, olive oil, and fish was associated with higher fertility, while higher consumption of processed foods, red meat, and foods that increase inflammation in the body was associated with reduced fertility.
In addition, preliminary PRESTO data shows that exposure to selected per- and polyfluoroalkyl substances (PFAS), the so-called “forever chemicals,” was associated with reduced fertility, consistent with previous literature.
Bertrand, a multiple principal investigator on the Black Women’s Health Study, is working to identify novel risk factors for breast and other cancers among Black women. The study began in 1995 with the recruitment of 59,000 Black women from across the United States.
Even though statistics show that, collectively, Black people have the highest death rate and the shortest survival rates of any racial and ethnic group in the US for most cancer types, and that Black women are 40% more likely to die of their breast cancer compared to non-Hispanic white women, widely used breast cancer risk prediction models are based primarily on data gathered from white women.
“It turns out that [the models] don’t perform quite as well in Black women, who are more likely to be diagnosed at younger ages and with more aggressive forms of disease,” Bertrand said, adding that by using data exclusively from Black women, the study was able to improve upon existing models and could be particularly useful for younger Black women to help guide decisions about when to start screening.
“We are uniquely positioned to study the experiences of racism as a risk factor for disease,” Bertrand said. ●
Greetings, Alumni and Friends,

THIS ISSUE OF BU MEDICINE HIGHLIGHTS THE IMPORTANCE OF WELLNESS as new and ongoing efforts by faculty, staff, and students continue to ensure the mental and physical wellbeing of the next generation of physicians, scientists, and other health professionals.
As a faculty member of the Academy of Medical Educators (AME) program, I have had the unique opportunity to build longitudinal relationships with medical students, supporting their personal and professional development while regularly checking in on their wellbeing through the Medical Student Wellbeing program. As AME advisors, we help students identify and work toward their individual wellness goals, fostering reflection, balance, and self-directed growth as they progress through their training. These efforts are complemented by the newly launched Chobanian & Avedisian School of Medicine Student Wellness Fund. Backed by students and supported
by alumni, these funds help provide resources that support student wellbeing, including financial literacy workshops, fitness programs, and assistance for those facing food insecurity. By building a culture of wellness, the school aims to identify concerns and create initiatives that assist in developing resilience and long-term skills to maintain wellness beyond medical school training.
This past academic year our Alumni Association team has continued to offer ways for alumni to engage with students and classmates both virtually and in person. We hosted four Alumni Pathways seminars for students to learn about and discuss career and lifestyle choices, two alumni neighborhood events, and four alumni tours highlighting the continued growth of our institution. We invite you to join us in hosting your own alumni gathering or to come home, meet with students, and take a guided campus tour. We look forward to deepening your connection with the school and encouraging ongoing engagement with alumni and students.
Thank you for your generous participation on Giving Day, which successfully raised $68,669. Your support has been integral to helping us enhance our institution and expand opportunities for the next generation of health professionals. We thank Alumni Board President Daniel Oates, MD’00, MSc, for dedicating his time, effort, and philanthropic support as the 2025 CAMED Giving Day Ambassador.
This spring we celebrated both endings and beginnings with great pride. We bid farewell to the Class of 2025 at their graduation ceremony, celebrating their accomplishments and wishing them well as they start on the next phase of their journey as residents and new alumni. At
the same time, we celebrated our new Rod Hochman Family Clinical Skills & Simulation Center, a state-of-the-art facility designed to enhance hands-on learning and prepare our students for the realities of clinical practice in a low-risk environment. Our sincerest gratitude to the Hochman family for their generous support.
Congratulations to our 2025 Alumni Award recipients: Stephanie Feldman, MD (CAMED’10,’14), received the Emerging Leader Alumni Award; Larry Nichter, MD (CAMED’78, CGS’71, CAS’73), the Humanitarian Award; Ziv Haskal, MD (CAMED’86, CAS’86), the Distinguished Alumni Award; and Vladimir Kefalov (CAMED’99), the GMS Distinguished Alumni Award. Their dedication and achievements are truly inspiring! The Alumni Association continues to develop new ways of engaging and celebrating our alumni community. Through our expanded social media initiatives, we offer opportunities to spotlight alumni each month by aligning the work they do with health holidays. To participate in these spotlight posts, we encourage you to reach out to our office so we can create important content together.
Thank you for your continued support. I look forward to seeing you soon and encourage you to remain connected.
Sincerely,
Heather Miselis, MAMS’00, MPH’00, MD’04 Associate Dean for Alumni Affairs

Rod Hochman Receives AHA Distinguished Service Award
Rod Hochman, MD’79, CAS’79, has received the 2025 American Hospital Association (AHA) Distinguished Service Award.
Hochman, the former president and CEO of Providence Health & Services based in Renton, Washington, received the award on May 5 during a ceremony at the AHA Annual Membership Meeting in Washington, D.C.
Hochman retired at the close of 2024 as president and CEO of Providence Health & Services after 45 years in healthcare, including 17 with the Providence family of organizations. At Providence, he worked hard to expand access to care, especially to those most in need, create innovations in care delivery and patient experience, and increase quality of care. Hochman also diligently invested in mental health and wellbeing for staff and community members alike. Today, Providence is a family of 120,000 healthcare professionals serving in 51 hospitals, more than 1,000 clinics, and hundreds of programs and services across seven states.
“A servant leader who always puts patients and caregivers first, Rod has dedicated his life and career to improving access to care for the most vulnerable and making healthcare better for all,” said AHA President and CEO Rick Pollack. “In addition to helping lead our field as AHA chair through the early days of the COVID pandemic, Rod has a unique ability to look into the future and stay ahead of the curve. To state it simply, Rod’s work has improved the lives of millions of Americans and has set a new standard for the hospital field.”
As AHA board chair in 2021, Hochman led through the depths of the pandemic, his training as an immunologist proving invaluable as he served as the voice of hospitals and health systems nationwide. A visionary known for outside-the-box thinking, he fostered collaboration among hospitals and health systems in search of new innovations to enhance care and the patient experience. Actively engaged with the AHA since 2008, Hochman chaired the Executive Committee, the Committee on Nominations, the Center for Health Innovation Leadership Council, and Regional Policy Board 9. He has also served on the Healthcare Advisory Council, the Health Systems Committee, the Coalition to Strengthen America’s Healthcare Board, and numerous other committees and task forces Hochman is a member of the Chobanian & Avedisian School of Medicine Dean’s Advisory Board. He and his wife Nancy (Sargent’77,’83) have established the Rod Hochman Family Clinical Skills & Simulation Center with a $10M gift. ●
1966
Peter Schwartz of Port Saint Lucie, Florida, writes, “Who says lightning doesn’t strike twice? On January 7, 2025, while riding my bicycle on a designated pedestrian crossing, I was struck by a car, resulting in an ambulance ride to a trauma center where I was diagnosed with a fracture of my right wrist/ thumb. Unfortunately, the right, so I was unable to hold a fork or spoon, pencil or pen, or type on a keyboard. Very limiting. Now three months later and still cannot do any of those functions. What’s truly remarkable is that on January 3, 2022, I was struck in the same pedestrian walkway and landed about four feet before my present landing. Result then was not as limiting.
Still working, just finishing a 13-month contract as a consultant and coach for a department chair. Also still on the Board of Frontier Nursing University, which graduates about 30% of the country’s nurse midwifery graduates annually, and still going to Ethiopia almost annually to teach medical ethics as part of my responsibility as a member of the Ethiopian Society of Obstetricians and Gynecologists. I also sit on the board of the medical humanities curriculum at Tower Health, an attempt to modify the dehumanization of the patient-physician interaction resulting from the corporatization of healthcare.
I regret the lack of interaction with my classmates and believe that after the 50th reunion we should explore the opportunity of electronic reunions at the midpoint between the five-year reunions.”
1967

Stuart Siegel of Pacific Palisades, California, writes, “I received the inaugural Ronald McDonald House Charities (RMHC) Global Legacy Award at the 50th anniversary gala in Chicago, Illinois, on November 16, 2024. I currently serve on the RMHC Board as chair of the Program Committee. I am also serving as chair of the Board of the Health Care Foundation of Ventura County, and chair of the board of DNA-SEQ, Inc., a biotech company that is developing new anticancer drugs using AI technology. The company recently was named the AI drug development company of the year for 2024 by Life Sciences Review magazine.”

1974
Robert Gilman of Ann Arbor, Michigan, writes, “After 32 years in practice in Wellesley, Massachusetts, and serving as a clinical instructor in the Harvard Plastic Surgery residency program, I was invited to join the full-time faculty in plastic surgery at the University of Michigan. After 11 years here, I am now a clinical associate professor and director of aesthetic surgery. I will be entering phased retirement this July, continuing to operate and teach on a halftime schedule. In early 2026 I will become president of the Rhinoplasty Society, a national multidisciplinary organization furthering advancement in the subspecialty of rhinoplasty and rhinology.”
1977
Jeffrey Allard of Wilbraham, Massachusetts, writes, “I just opened a museum office building from which I conduct my consulting business.”

1979
Gary Stanton of Cambridge, Massachusetts, writes, “Now I’m a grandfather. Here is my sweet grandson, Rex. A different type of milestone. I’m still in the full-time practice of neurology, very much enjoying it.”
John Herzenberg of Boulder, Colorado, writes, “Merrill and I both retired in 2023 in order to be full-time grandparents. We have grandchildren in Boulder, Colorado, and Miami, Florida, so we go back and forth reg-

Herzenberg, MD’79, volunteering in Nepal.
ularly. I am emeritus faculty at Sinai Hospital of Baltimore, and clinical professor at University of Maryland. I continue to be involved in research, publishing, teaching, and international pediatric orthopedic service missions. Since retiring, I have volunteered and operated in Liberia, Nepal (photo), Honduras, Israel (x3), and Ukraine. Also, invited teaching gigs at Washington U, Vanderbilt, Dubai, and Japan. No rest for the weary!”
1983
Alan Ettinger of Dix Hills, New York, writes, “Based in part upon my grant-supported research on music and health, our musical group, Synaptic Groove Band, performs at concerts and lectures for the lay public on
John
Robert Gilman, MD’74
Stuart Siegel, MD’67
Rex, grandson of Gary Stanton, MD’77

the health benefits of music. We have also performed for the Long Island Music & Entertainment Hall of Fame, medical staff societies, and assorted disease-related organizations.”
1985
Alan Multz of Woodbury, New York, writes, “I am the associate medical director for quality, White Plains Hospital, Montefiore Health System, and a United Health Fund Award recipient for being a 2025 Quality Improvement Champion. I was given this award for my leadership monitoring quality metrics and risk adjustments for each discharged patient, reviewing and addressing clinical care issues, and cochairing a readmissions task force to drive quality improvement for readmission rates.”
1986
Steve Ober of Yarmouth Port, Massachusetts, writes, “During my orthopedic surgery residency, I sustained a pathologic fracture of my left femur while assisting on an AAA (Abdominal Aortic Aneurysm) repair. I completed the case, but left the OR on a gurney, following the gurney of the patient on whom I had just operated. After much soul-searching, I left clinical medicine and entered the business side of healthcare. I graduated with an MBA from the Harvard Business School in 1991 and immediately started my first company in the clinical analytics space. After selling it, I started my second company in biotechnology. These
were followed by several years of consulting to large and small companies throughout the US in all aspects of healthcare. I loved it. Unfortunately, my left leg was amputated above the knee in 2014 due to complications of a rare bone disease I have had since birth. This was followed by diagnoses of non-Hodgkin’s lymphoma and Guillain-Barre syndrome (GBS) in 2018. While both were successfully managed, my GBS recurred in early 2024. I have been wheelchair bound for the past 15 months with no chance of ambulating with crutches or other walking aids. A local church installed a beautiful aluminum ramp to my front door so I can leave the house without a problem.

I have been married for 8 years to the most amazing woman. Despite not being from the healthcare field, she has learned more about my conditions than many physicians I know! She has taken amazing care of me despite fighting her own battle against breast cancer. I am a very lucky man to have found her. Despite the adversities I have faced, I am an extremely happy guy! My advice to folks undergoing adversity? FORGET ABOUT IT! Do as I have done—follow the philosophy of Bing Crosby. That crooner released a song in 1937 called ‘Accentuate the Positive, Eliminate the Negative.’ Using this philosophy, find new activities, careers, and people to push your adversities to the back of your head—or out of your head entirely. It really can work. I tell people that when I leave this fine world, it will take the funeral director a week to get the smile off my face! When people ask me how I am doing, I give
them my candid, honest answer: ‘Life? She’s sweet!’ Finally, remember the 1988 song by Bobby McFerrin, ‘Don’t Worry, Be Happy’! Go get ‘em, folks!”
1988
Doreen Parkhurst of Boynton Beach, Florida, writes, “Having retired from a career in emergency medicine, I am now engaged in patient advocacy.”
Carl Rosen of Anchorage, Alaska, writes, “I now work half-time as an oculoplastic surgeon at Ophthalmic Associates in Anchorage, Alaska. I recently ran into Mike Singer (MD’86), a retina specialist in Hawaii, who was gracious enough to join me on my YouTube channel, Einstein’s Eyes. On it, I talk about ophthalmology, innovation, tech, policy, and related medical topics. I invite all to take a look. Alaska is a great place to visit in the summer.”
Lancelot Williams of Long Beach, California, writes, “I moved to California after completing medical school for an emergency medicine (EM) residency at LAC-USC Medical Center. After two years, realizing that EM was not for me, I returned to Boston to complete residency training at Beth Israel Deaconess-Harvard Medical School in anesthesiology. The beautiful California weather lured me back to the West Coast, and I’ve now been here in southern California for
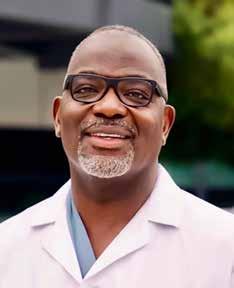
Alan Multz, MD’85
Steve Ober, MD’86, with wife Reese.
Lancelot Williams, MD’88
thirty-plus years. I’m staring retirement in the face—hopefully within the next year. It’s been a good life and a wonderful career in anesthesiology!”
1990
Edward Gosselin of Bridgewater, New Jersey, writes, “I’ve been practicing emergency medicine these past 35 years, the last 10 traveling as a locum tenens provider. I continue with my Emergency Medicine Expert

Witness business. My wife Geri and I have welcomed our first grandson, Kane, into our family. Although still in New Jersey, we try to visit Boston any chance that we get.”
1992
Elliott Leitman of West Chester, Pennsylvania, writes, “It is hard to believe that I am on the back end of my rewarding career in orthopedic surgery. In addition to practicing orthopedic sports medicine in Delaware for the past 26 years, I have had the honor of serving our military as a surgeon in the US Army Reserve and Air National Guard. Proudly, I have two wonderful children working in medical-related fields. When not working, my wife and I enjoy travel, kiteboarding, and pickleball. I have found time to maintain my interest in aviation, along with biking, skiing, and various other outdoor activities.”

1994
Brinda (Trivedi) Gupta of Lexington, Massachusetts, writes, “I am a primary care pediatrician in Newton, Massachusetts. I LOVE my job! My MMEDIC buddy, Cristina (Deluca) Holt (MD’94), is an internist in Medford, Massachusetts. Our families remain friends, and she and I make pizzellis from her grandmother’s recipe every Christmas!”
1999
Rubeen Israni of Newark, Delaware, writes, “Recently I took the position of senior director in clinical development at Novartis pharma and was part of the team that obtained the first approval of a drug for a rare kidney disease called C3G. After a successful career in private practice, I switched to working in industry in 2018. My current work in rare kidney diseases is especially gratifying.”
Scott Lisson of Cary, North Carolina, writes, “I am currently the medical director for the Department of Urology at WakeMed Health & Hospitals in Raleigh, North Carolina. Our department consists of 14 attending surgeons and 17 advanced practice providers across three hospital campuses. My wife, Dr. Gail L. Lisson, continues to practice clinical psychology as a solo private practitioner. My daughter, Paige, is a sophomore nursing student at the University of Miami, and my son, Jonas, is a graduating high school senior headed to Boston College in the fall.”
Patricia Takach of Philadelphia, Pennsylvania, writes, “Wrapping up my work at the University of Pennsylvania. So fortunate to care for many patients, work with brilliant colleagues, and be supported by caring staff during this time. I will miss all of them!”
2001
James Nassiri of Los Angeles, California, writes, “Recently, I participated in a medical mission in the City of Hue, Vietnam, organized by a nonprofit organization, the Arpan Global Group. I collaborated with residents and faculty within the department of anesthesiology, which did not have a pain management division. In the unique setting of a foreign country with limited resources, I shared my knowledge and experience in pain management. I taught eager young faculty and senior residents basic interventional techniques so that their patients have nonsurgical treatment for debilitating spinal conditions.”

Ramin Tabaddor of East Greenwich, Rhode Island, writes, “This has been a fruitful year professionally. I recently was awarded the Kent Hospital Specialty Surgeon of the Year Award, the hospital where I serve as chief of orthopedics. I was recognized as a Rhode Island “Top Doc” for orthopedics and was also appointed fellowship director for the Brown Orthopedic Sports Medicine Program.
Brinda (Trivedi) Gupta, MD’94, with friend Cristina (Deluca) Holt, MD’94.
James Nassiri, MD’01
Edward Gosselin, MD’90
I am completing my 16th year as head team physician for University of Rhode Island Athletics. I am grateful and humbled by these acknowledgements.”
2006
Fouad Abuzeid of Stuart, Florida, writes, “Neurosurgical critical intensivist at the Cleveland Clinic, just got an additional faculty appointment at the Florida State University College of Medicine.”
2007
David Scott of Hilton Head Island, South Carolina, writes, “Recently founded my own healthcare consulting firm, Scott-Health Consulting. We help medical groups and hospitals with strategy, expansion, mergers & acquisitions, innovation implementation, and overall clinic and business operations.”
2009

Jules Manger of Tucson, Arizona, writes, “I was recognized by Newsweek in its first ranking of America’s best prostate cancer surgeons. The list recognizes the 150 best prostate cancer surgeons in America based on outcomes data and peer review. I currently live in Arizona with my wife Linda and three sons.”
2014
Kristine Karkoska of Cincinnati, Ohio, writes, “My husband, David Robinson (MD’14), and I completed our family with the birth of Emma Suzanne Robinson on March 9, 2025.


She joins big sister Maura (age 4) and Owen (age 2).”
2016
Michele DeBiasse of Maynard, Massachusetts, writes, “With colleagues in Canada, I published a chapter, ‘Diversity, equity, and inclusion in the dietetics profession: Past, present, and ways forward,’ in the recently published textbook, Equity, Diversity and Inclusion in Healthcare Professions: From Knowledge to Practice.”
Oscar Gonzalez of Ayer, Massachusetts, writes, “Lawrence Wong (Questrom’20) and I, partners at Sigma Lab Consulting, are excited to share that our abstract was accepted for a featured talk at the 2025 EP3M Summit this September in Cambridge, Massachusetts. The session will focus on practical strategies for advancing operational excellence across the drug development lifecycle, drawing from more than 15 completed projects over the last two and a half years.
Sigma Lab specializes in helping biopharma organizations—from early-stage to enterprise—improve cross-functional delivery, streamline decision-making, and scale what works. As part of this mission, the firm has developed a suite of targeted assessments that help research & development, clinical, and facilities teams benchmark performance, identify friction points, and drive measurable improvement.
I am also preparing to publish my first book this fall, which introduces a practical framework for operational excellence in biopharma. The book distills real-world insights
from my professional career and Sigma Lab’s work and is designed to help leaders simplify complexity, align teams, and make data-informed decisions across their portfolios.
Rooted in the values and interdisciplinary mindset originally cultivated at BU, Lawrence and I continue to build a firm that blends systems thinking, lean principles, and life sciences expertise to deliver clarity, alignment, and meaningful change.”
Jonathan Silva of Norwell, Massachusetts, writes, “I am working in the alternative investments space leveraging incident management skills acquired during my time at Boston University!”

Kristine Karkoska, MD’14, is busy with children Emma (newborn), Maura (age 4), and Owen (age 2).
Oscar Gonzalez, MSc’16
Jonathan Silva, MSc’16
Jules Manger, MD’09
alumni news | class notes
2021
Alawi Habara of Al-Qatif, Saudi Arabia, writes, “I earned my PhD in molecular and translational medicine in January 2021. It was a long journey with plenty of ups and downs, but it was definitely worth it! Getting my degree from Boston University turned out to be one of the best decisions I’ve made in my academic life. After graduating, I returned home to Saudi Arabia, where I’m now an assistant professor in the clinical biochemistry department at the College of Medicine. I also serve as chairperson for the College of Medicine laboratory committee.
My current research focuses on genetics and molecular pathways in hemoglobinopathies. I truly enjoy teaching medical students and students from other medical disciplines, and always aim to create a collaborative and interactive classroom. Expect plenty of engaging discussions and practical activities throughout our time together!
Outside of academia, spending quality time with my family, who are the most important part of my life, is what I cherish

most. I also enjoy traveling, exploring new places, and experiencing different cultures, which helps me recharge and brings fresh perspectives into my teaching and research.”
2023
Benjamin Martin of Jersey City, New Jersey, writes, “I’ve been working as an emergency management specialist with the Federal Emergency Management Agency (FEMA) in New York, supporting the mission of helping people before, during, and after a disaster. During my deployment to support the Hurri-


canes Helene and Milton recovery, I was recognized for my dedication to the FEMA core values of compassion and fairness.”
Erika Minetti of Allston, Massachusetts, writes, “This year I’m celebrating 10 years at Boston University! In 2019 I got my BA in biochemistry and molecular biology with a minor in music performance. Then I did a couple of years of research in the Whitaker Cardiovascular Institute at the School of Medicine before returning as a student in the Master’s in Medical Sciences (MAMS) program. I graduated from MAMS in 2023, where I got to deliver the commencement speech—definitely a highlight of my time at BU! Currently I’m working in Dr. Naomi Hamburg’s lab, where I study vascular endothelial health. In November 2024 I gave my first moderated poster presentation on electronic cigarettes at the American Heart Association Scientific Sessions conference. I’m also a proud member of the MA Chapter of the Association for Women in Science (AWIS) where I serve as the communications committee co-chair, and I’ve written several articles on topics such as women’s health for the AWIS magazine. Aside from all things science and medicine, I’m concertmaster of the Student Center Orchestra at Harvard, and I also enjoy jogging and cycling in Boston. Now, I’m looking forward to spending some time back home in Milan this summer before starting medical school at BU in August and becoming a Triple Terrier!”
2024
Victoria Monetti of Snyder, New York, writes, “I’m now working for the New York State Police crime laboratory system as a forensic scientist at the New York State Police Southern Tier Satellite Crime Laboratory. There, I am an analyst in the seized drugs unit.”

Valentina Moreno Escobar of Boston, Massachusetts, writes, “After graduating with a master’s in oral health science, I went on to work at BU’s Henry M. Goldman School of Dental Medicine as a dental assistant for the global and public health department while applying to dental school. Now, as a first-year dental student at Tufts University, I want to thank all the staff, students, and faculty for the opportunities BU offers; without their support, I wouldn’t be the ‘Jumbo’ I am today.” ●
Benjamin Martin, MSc’23
Alawi Habara, PhD’21
Erika Minetti, MSc’23
Valentina Moreno Escobar, MSc’24
Congratulations!
The Chobanian & Avedisian School of Medicine Alumni Association announces the 2025 Alumni Award recipients




Emerging Leader Alumni Award
Stephanie Feldman, MD (CAMED'10,'14)
In recognition of remarkable promise, leadership, and commitment to advancing healthcare, research, education, or advocacy in the early stages of their professional career.
Humanitarian Award
Larry Nichter, MD (CAMED'78, CGS'71, CAS'73)
In recognition of exemplifying the highest ideals of compassion, service, and dedication to improving health and enhancing the lives of others, making a meaningful and lasting impact on our world.
Distinguished Alumni Award
Ziv J. Haskal, MD (CAMED'86, CAS'86)
In recognition of extraordinary dedication, visionary leadership, and transformative contributions to the advancement of clinical care and biomedical research.
GMS Distinguished Alumni Award
Vladimir Kefalov, PhD (CAMED’99)
In recognition of many contributions in research, mentoring, and leadership.
Alumni Award recipients will be recognized at an in-person ceremony and luncheon on Friday, September 26, as part of our Alumni Weekend events.


Robert Kelley of Wellesley, Massachusetts, passed away November 9, 2024.


Gerald Hazard of Barnstable, Massachusetts, passed away January 3, 2025.


Cyril Kim of Manchester, Connecticut, passed away January 3, 2025.

Mark Michelman of Quincy, Massachusetts, passed away October 26, 2024.
Harold “Hackie” Reitman of Weston, Florida, passed away March 4, 2025.

I. Howard Fine of Eugene, Oregon, passed away August 29, 2024.
Frank Toppo of St. Petersburg, Florida, passed away August 10, 2024. ●

Act today for better tomorrows
Act today for better tomorrows
With one simple move, you can change the lives of BU students for generations to come—and save money for your loved ones, too.
With one simple move, you can change the lives of BU students for generations to come—and save money for your loved ones, too.
Your unused retirement assets—an IRA, 401(k), 403(b), or other tax-deferred plan—could be a substantial legacy. But leaving them to your family may trigger substantial income taxes. Instead, you could provide for your loved ones with other assets and consider naming BU as a beneficiary of your retirement accounts.
Your unused retirement assets—an IRA, 401(k), 403(b), or other tax-deferred plan—could be a substantial legacy. But leaving them to your family may trigger substantial income taxes. Instead, you could provide for your loved ones with other assets and consider naming BU as a beneficiary of your retirement accounts.
It’s easy to do, and we’ll be happy to help. To learn more, please contact Boston University Planned Giving at 800-645-2347 or opg@bu.edu, or visit bu.edu/plannedgiving.
It’s easy to do, and we’ll be happy to help. To learn more, please contact Boston University Planned Giving at 800-645-2347 or opg@bu.edu, or visit bu.edu/plannedgiving.
Download a complimentary copy of our Estate Planning Guide at bu.edu/estateguide.
Download a complimentary copy of our Estate Planning Guide at bu.edu/estateguide.
