

Message From The Dean
Dear Alumni, Friends, and Colleagues,
We are already midway through our academic year. Our campus is full and energized essentially, normal postpandemic.
I hope you enjoy this content-rich edition of BU Medicine celebrating Mr. Edward Avedisian’s historic, transformational $100 million gift that has renamed the School of Medicine the Boston University Aram V. Chobanian & Edward Avedisian School of Medicine. Dr. Chobanian and Mr. Avedisian both have deep ties to BU. Sadly, Mr. Avedisian—who was able to attend and enjoy the September 29, 2022, public announcement event and many of the subsequent stories about his gift and career—passed away on December 7, 2022.
Mr Avedisian’s gift, which will arrive over the next five years, includes scholarships, professorships, and funding for excellence in education and research programs that will transform our school now and for centuries to come. Those of you who were unable to join us for the festivities can read about the news in our cover story.
Our Emerging Leaders Program for early-career faculty resumed postpandemic with a robust class of 52 faculty representing the three Medical Campus schools and, for the first time, faculty affiliated with St. Elizabeth’s Medical Center.
We feature a story on a new collaboration between the MD program offices of medical education, student affairs, and research to streamline and coordinate the available medical student research opportunities and match students and their particular fields of interest with faculty doing peer-reviewed research in those fields. The program is partially supported by the new Dr Judith Vaitakaitis Medical Student Research Endowment as well as by generous alumni.
Some of our student achievements are celebrated with profiles on MD candidates Lindsey Claus, Rebecca Wolinsky, and Bita Naimi as well as PhD student Jhonatan Henao Vasquez.
Boston University Medicine
Boston University Medicine is published by the Chobanian & Avedisian School of Medicine Communications Office.
Maria Ober
Associate Dean, Communications
design & production
Boston University Creative Services
contributing writers
Joel Brown, Lisa Brown, Gina DiGravio, Doug Fraser, Alaina Mencinger
photography
David Keough, Chris McIntosh, Dana J. Quigley Photography, Jackie Ricciardi
Please direct any questions or comments to:
Maria Ober
Communications Office
Boston University Medical Campus
85 East Newton Street, M810H
Boston, MA 02118
P 617-358-7869 | E mpober@bu.edu
0323
We introduce you to our two newest chairs, Tony Hollenberg, MD, chair of the Department of Medicine, and Venetia Zachariou, PhD, chair of Pharmacology, Physiology & Biophysics, and pay tribute to trailblazer Marcelle Willock, MD, our beloved professor and chair emerita of anesthesiology, who passed away in October We will miss her dearly
Our giving section and donor report (page 27) highlight significant investments and renovations supported by your generous gifts. We describe the legacy of endowed professorships by our former Professor and Chair of Medicine David Coleman, MD, and feature stories on the Mac Parkman Foundation support for Ann McKee, MD; a Chan Zuckerburg grant to Joshua Campbell, PhD; Alex’s Lemonade Stand for Hui Feng, PhD; and the American Heart Association grant to Katya Ravid, DSc.
Our alumni section (page 32) profiles Drs. Mary Jane England (’64), Thomas Insel (’74), Robert Jackler (’79) and Louis W. Sullivan (’58), and offers a recap of our Alumni Weekend festivities.
As always, special thanks to our donors and friends for your continued commitment to our school and your generous support for our outstanding students, faculty, and staff on the front lines of science and medicine.
Best Regards,
Karen Antman, MD Provost, Medical Campus Dean, Chobanian & Avedisian School of Medicine

campus news
52 Faculty Participate in Emerging Leaders Program
Resuming after a three-year delay due to the pandemic, the BUMC Emerging Leaders Program returned with a robust class of 52 representing Medical Campus schools and, for the first time, faculty affiliated with St. Elizabeth’s Medical Center (SEMC). Initiated in 2007, the program has been offered seven times and served 237 participants.
Held on the Charles River Campus, the two-day intensive workshop hosted a cohort of later-career assistant professors and earlycareer associate professors who learned about the characteristics and key leadership skills of effective leaders. They then participated in discussions and panels, practicing and discussing those skills with a network of peers.
“I thought this was the right meeting for my current position in my academic career. I loved having an opportunity to focus on leadership qualities, examining communication and negotiation skills that are so applicable in interactions with colleagues, trainees, and patients, thinking about financial considerations that academic institutions face, and networking with other BU faculty,” says Alena Goldman, MD, assistant professor of medicine and associate program director of the Cardiovascular Fellowship Training Program, Division of Clinical Cardiac Electrophysiology, SEMC.
“The Emerging Leaders Program was a great experience. It was a unique opportunity to meet Medical Campus colleagues and receive training in soft skills such as team communication, negotiation, and conflict resolution. I especially appreciated learning about formal leadership and administration at the university level as well as how I can improve my interpersonal communication and organization on a daily
basis,” says Prasad Patil, PhD, assistant professor of biostatistics.
“The Emerging Leaders Program was a two-day opportunity to learn many high-yield pearls of leadership wisdom from fantastic speakers from across Boston University, as well as a chance to get to know tomorrow’s leaders on the Medical Campus,” says Kevin J. Chang, MD, an associate professor of radiology and section chief of abdominal imaging and director of MRI at Boston Medical Center.
Showing their commitment to developing emerging leaders, Medical Campus Provost Karen Antman, MD, and Deans Sandro Galea, MD, and Cataldo Leone, DMD, attended the workshop and made themselves available for informal networking. Presenters shared their expertise in dental medicine, public health, medicine,
healthcare, research, finance, academic legal issues, and communication.
Participants who showed promise as leaders—as evidenced by their effectiveness, innovation, reliability, and capacity to energize and motivate others—were nominated by their department chairs, division chiefs, associate deans, and center directors.
“Faculty are key to our teaching, research, and community outreach mission on the Medical Campus. This program is one way we help develop early-career faculty into future leaders on the Medical Campus,” says Hee-Young Park, associate dean for faculty affairs and professor and chair of medical sciences & education. Program graduates now serve as department chairs, section chiefs, associate deans, assistant deans, and program directors. ●

Two-day program aims to help develop early-career faculty into Medical Campus leaders
New, Enhanced Program and Website Help Medical Students Find Research Opportunities
Ayear into his newly created position of assistant dean for research, Matthew Layne, PhD, associate professor of biochemistry, sees himself as a matchmaker connecting medical students to the large research community on the BU Medical Campus (BUMC). Layne’s new position is central to BUMC Provost and Chobanian & Avedisian School of Medicine Dean Karen Antman’s goal of incorporating more research opportunities into the MD program.
“These are highly qualified, capable students, and many of them are passionate about research. They have questions, and they just need to learn about the research opportunities and how to connect with faculty so that they can join a research project,” says Layne.
With input from the offices of Medical Education, Enrichment, and Student Affairs, Layne worked with Eliana Bolanos, executive assistant to Associate Dean for Research Andrew Taylor, PhD, to create a new website that collects all of the medical school’s student research opportunities—previously spread across personal, lab, and departmental websites—and provides information and contacts all in one place. It’s part of a multiprong approach to student research that includes extending summer research into the academic year and across the four years of medical school, assessing the quantity and quality of student research, and incorporating research and an optional dedicated research year into the curriculum.
In part, the school is responding to requests from students with concerns about increased competition for residency programs, particularly in medical specialties that tend to require or favor applicants with research experience and published papers, says Taylor.
But that’s not the only reason.
Third-year medical student Lindsey Claus just started clinical rotations. Her
presentation of a team research project on ultrasound education swept student award categories at the International Association of Medical Science Educators in June 2022. She says research gives her a measure of hope, particularly when caring for a patient experiencing a difficult and complicated prognosis.
“You kind of struggle thinking about longterm answers and structural problems, and research provides a really helpful way of figuring out what those might be,” she says.
Some students make their own research arrangements and go uncounted, according to Layne. That’s something he’d like to change.
“We are working to enhance the research and mentoring experiences of all medical students,” he says.
“Part of this includes developing strategies to better understand where the students are performing research and tracking the outcomes of their work, including publications,” he says.

By providing strategies to find mentors and projects, basic information on how to do both long- and short-term research, contacts, links to applications and scholarships, and a section highlighting student research experiences and achievements on a single website, Layne is hoping to attract medical students to work through his office.
Many medical students are introduced to research at BU through the seven-to-tenweek Medical Student Summer Research Program (MSSRP)—occurring between the first and second years of medical school— with 40–50 students participating annually.
“We’re looking at [the MSSRP] as the launch point,” says Taylor, where the student researcher finds a project of interest; connects with faculty; learns research ethics, enhanced research techniques, and science; and gets accustomed to the research schedule.
The school’s policy already allows students to pursue research on their own, part-time in the first two years, during a four-week research block in the third year, and for up to 12 weeks in the final year. Students can add an optional research year.
Now, students can apply to do longitudinal research, working with faculty mentors, at the beginning of their second year, with an option of taking a research year between the second and third years or third and fourth years as part of the academic program. They can continue research through their final two years, supported by an advisor and advisory committee with an annual report and presentations at an annual research symposium required.
Layne sees increased participation by medical students also benefitting the school’s research community.
“[Medical students] are a fantastic resource for us to recruit into our labs because they have knowledge and motivation and passion, and the faculty can, in turn, mentor them and help them develop into physician-scientists,” he says. ●
In part, the school is responding to requests from students with concerns about increased competition for residency programs.
DEIA Statements Added to BU Profiles
When launched in 2012, BU Profiles served as an online dossier for biomedical researchers engaged in research networking and collaboration by employing software that automatically updated user profile categories like publication, citations, grant funding, honors, coauthor research networks, and publication timelines. Over time, BU Profiles has evolved to provide researchers with metrics that monitor and assess their research productivity, impact on science and policy, and influence on the public through social media and news stories.
Now, the platform has been further enhanced to give the nearly 5,000 biomedical faculty, researchers, and staff users the option of adding a personalized Diversity, Equity, Inclusion, and Accessibility (DEIA) statement to their profile.
“A DEIA statement is really about the importance overall of diversity in our organization, in society, and a recognition that higher education has to be a leader,” says Christopher Dorney, director of BUMC IT’s application services. The site has 4,662 profile users and 16,000 unique visitors monthly.
Advocates hope DEIA statements will resonate within the academic community by inspiring and sustaining the collective multicultural growth of students, staff, and faculty.
Part of a translational research networking initiative supported by BU’s Clinical & Translational Science Institute, “BU Profiles now enables our community to convey a unified public message on how they see their research, mentoring, teaching, clinical practice, and service contributing to a campus culture that values diversity and inclusion and accessibility,” says Deborah Fournier, PhD, former assistant provost for institutional research & evaluation.
“We’re asking profile users to reflect on the meaning of [DEIA] in their professional lives and to join us in a collective response in documenting our commitment to enhance our culture of inclusive excellence that enables students, staff, and faculty to learn and work on a campus where they feel valued, seen, and heard,” says Fournier, who oversees BU Profiles with Dorney and Christopher Shanahan, MD, associate professor of general internal medicine, director of the Community Medicine Unit, and BUMC faculty lead for research networking.
Recent personnel decisions may help gain widespread adoption. The medical school’s executive committee approved including DEIA statements as part of new job applications and they are now an optional question in annual reviews for basic science and clinical faculty.
BU Profiles users completely control what gets displayed on their profile and can remove or edit their DEIA statement at any time. A statement can be a personal essay of how past experiences have contributed to one’s personal and professional growth, for example, or a description of academic pursuits and accomplishments.
In her profile, Assistant Professor of Medicine Mara Murray Horwitz, MD, MPH, included a few brief paragraphs to filter her work as a clinician, researcher, and teacher through the lens of “improving healthcare outcomes and equity and helping build a more diverse workforce in medicine.”
Befitting her background and new role as associate dean for diversity & inclusion, the DEIA statement of Angelique Harris, PhD, details her work on issues of diversity and inclusion, listing her awards, involvement on BU and national committees, courses taught, publications, and speaking engagements.
“I am deeply familiar with the benefits, challenges, and opportunities that come with promoting inclusive excellence,” Harris wrote.
Faculty have varying levels of experience and fluency in the language of diversity and inclusion and may have concerns about staking out a public position on what has become a politically divisive topic—or may simply want help in thinking through their experiences and ideas. Online faculty seminars were held on how to write diversity statements and incorporate DEIA work into CVs and BU Profiles. ●
“A DEIA statement is really about the importance overall of diversity in our organization, in society, and a recognition that higher education has to be a leader.”
CHRISTOPHER DORNEY
“We’re asking profile users to reflect on the meaning of [DEIA] in their professional lives and to join us in a collective response in documenting our commitment to enhance our culture of inclusive excellence.”
DEBORAH FOURNIER, P h D
Gross Anatomy Lab Renovations Looking Good
In the process of becoming a doctor, anatomy class is one of the steps involved.
“If we taught you how to ride a bicycle the way we’ve traditionally taught anatomy, you’d have to learn every part of the bicycle before you actually got on it,” says Jonathan Wisco, PhD (’03), associate professor of anatomy & neurobiology.
Thanks to an anonymous, significant gift, a $1 million overhaul of the Gross Anatomy Lab began in 2020 and is nearly complete. According to Wisco, the anatomy lab upgrade reflects multiple pathways to learning and is in step with new curriculum changes implemented this year for the Class of 2026 that incorporate self-directed learning and early exposure to clinical concepts.
“We’re providing students the exposure to the 3D donor—plus the technology—before they dissect,” says Wisco. “The more that students know what they are looking for, the better dissectors they are.”
Located on the 10th floor, the lab features new windows that flood the area with sunlight, including the section where dozens of donor bodies lie in bright-blue body bags on portable dissection tables.
“The natural sunlight coming in puts your mind at ease,” says Anatomy Laboratory Director and Anatomical Gift Director Robert Bouchie. “It shouldn’t be macabre; it should be something that you’re embracing.”
As many as 45 donor bodies are used every year for between 309 and 370 students, with as many as 180 medical students and 130 dental students participating. The lab is noisy when in session, says Bouchie, but it’s the good sound of students learning how they can help future patients.
“I want there to always be this subliminal feeling of life,” he says.
The upgrades include improved communications for instructors with an enhanced sound system and monitors linked to iPads, as well as updated lighting, heating, air conditioning, and ventilation. New technology includes ultrasound units and an Anatomage virtual dissection table. Communications upgrades allow images from the Virtual
Human (VH) Dissector—displaying 3D and cross-sectional views of more than 2,000 anatomical structures—to be displayed on monitors across the lab.
Wisco encourages students to use both traditional teaching aids (such as anatomy books and photos) and new technologies to prepare for dissection on donor bodies and to work backward from dissection, through the
Third-year medical student Jessica Landau-Taylor uses a new ultrasound machine on second-year medical student Nimish Saxena in the newly renovated Gross Anatomy Lab. Students use the ultrasound to see how organs and other bodily systems look and work in a living person.

Gross Anatomy Lab research assistant and second-year anatomy & neurobiology graduate student Tyler Capen demonstrates the new Virtual Human (VH) Dissector that displays 3D and cross-sectional views of more than 2,000 anatomical structures.

technology to the textbooks, to better understand what they encounter.
“That way, they are contextualizing more and more sophisticated information that they imprint in their minds,” he explains.
With new technologies that can duplicate dissection, third-year medical student Jessica Landau-Taylor was initially skeptical about the need for real donor bodies until she found
the new technology in the lab worked well with dissection, improving the process by providing context and the opportunity for self-directed learning.
“There’s nothing quite like actually being able to see the structure—tissues, organs— in an actual human being, in color, with your eyes, the same way you see everything else,” says Landau-Taylor. “It’s also good to see it in a way that’s been formatted to help you learn.”
“[The Anatomage table] is a great way to visualize anatomy, especially anatomy that may be difficult to see on a cadaver,” says postgraduate teaching assistant Sydney Mosaheb, MS, who also is a research assistant in the BU CTE Center. The technology makes it easy for students to investigate on their own or double-check their work on the human donor.
“Trial and error, at least for me, is helpful for learning and medical students have to learn so many things that being able to just memorize it in a way that makes sense to them is very helpful,” says teaching assistant Paola Castro, MS, who also is a research technician in the Cellular Neurobiology Lab.
The new technologies also lend color and a realistic look to organs and other structures that can be relatively colorless and physically flattened in donor bodies due to the embalming process. The ultrasound, VH Dissector, and Anatomage also help students interpret scanned images from similar instruments like Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) that students will see in their clinical rotations and as physicians.
STaRS Shine during 10-Week Program
The Summer Training as Research Scholars (STaRS) Program concluded its 10-week experience with an oral presentation symposium held August 9–11. The scholars also participated in the GMS summer research poster symposium on August 11.
Overseen by Graduate Medical Sciences, the STaRS Program is funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health. It has trained over 180 scholars and received more than 3,500 applications since its inception.
In the STaRS program, scholars realize independent cutting-edge biomedical research projects under the guidance of their research mentors—faculty, students, postdoctoral associates, fellows, and residents.
Scholars also present their research, significantly increase their network, build powerful and lasting relationships, and attend career development seminars aimed at preparing them for school applications and research paths.
After an opening welcome from Isabel Dominguez, PhD, assistant professor of medicine and director of the STaRS Program, the symposium began by acknowl-
edging the faculty mentors, professionals, student mentors and panelists, and administrators who contributed to the success of the program. This included the STaRS mentors—Carolyn Wilson (MD student), Hunter Kelley (MAMS student), and Felix Litvak (MD student)—who advised and helped scholars before, after, and during the program.
The scholars showcased their oral presentations and posters, and discussed their work on a variety of topics, including inflammatory biomarkers, mouse lung fibroblasts, aortic disease, lung cancer, podocyte injury, cerebral microbleeds, connective tissue diseases, prostate cancer, animal model behavior, extracellular matrix in kidney disease, amyloidosis, mitochondrial disfunction, ECM extraction methods, fibroblast differentiation, arteriovenous access, enterotoxigenic bacteria, and sleep apnea. They received certificates to mark the completion of the program.
This year’s class included 16 undergraduates from across the country and one current Chobanian & Avedisian School of Medicine student. The 2022 scholars were Arjun Kumar Batra, Yariann Del Mar Camacho Rosario, Carlos Noel Centeno
“I had no radiology experience, and this [VH Dissector] made it click for me when I first saw an MRI,” says teaching assistant and second-year anatomy & neurobiology graduate student Tyler Capen. “An MRI is a lot of black and white, but if you know what the structures look like, what shapes they are, and where they’re supposed to be, you can correlate that.”
Second-year medical student Nimish Saxena found the technology helped inject excitement into the daily routine of lectures and rote memorization, and employing technology that resembles what they will use as clinicians made the anatomy courses more relevant to students.
“It’s really good for melding that clinical relevance with the coursework we’re studying,” says Saxena. ●
Velez, Coralys Ivette Cuevas Hornedo, Sophia Karise Ellis, Eli River Engledow, Nusrat Islam, Alexis Kidiani Kiyanda, Christine Le, Zoe Nicole Matacchiera, Alejandra Sofia Medina, Nubaira Zaheen Milki, Karlianie Rivera Rodriguez, Muriel Louise Ruppert, Eduardo David Salazar, Emily Katherine Stein, and Carolyn Wilson. Faculty mentors included Esther Bullit, PhD; Isabel Dominguez, PhD; Hui Feng, MD, PhD; Chris Heaphy, PhD; Matt Layne, PhD; Jessica Levi, MD; Weining Lu, MD; Sarah Mazilli, PhD; Joseph P. Mizgerd, ScD; Gareth Morgan, PhD; Rafael Romero, MD; JeanPierre Roussarie, PhD; Karin Schon, PhD; Francesca Seta, PhD; Manveen K. Sethi, PhD; Joseph Zaia, PhD; and Jeffrey Siracuse, MD.
The summer poster symposium also hosted three summer Undergraduate Research Opportunities students: Sanjana Prudhvi, Lydia Bischoff, and Eric Ibarra.
“It is rewarding to watch the STaRS enhance their communication and research competencies, and to take on leadership roles in the program,” says Dominguez.
“I am very impressed with the scholars’ research accomplishments under the guidance of our faculty and team mentors. It is very gratifying to see the scholars empowered to follow their path to graduate school and to be future researchers.” ●
Physicians Stress the Importance of the Physical Exam at 5th Annual Lorraine Stanfield Lecture
Speaking to first-year medical students at the 5th Annual Lorraine Stanfield, MD, Memorial Doctoring Lecture, keynote speaker Robert Lowe, MD, associate professor of gastroenterology, contemplated a future in which technology eclipsed the need for the


stethoscope, the utilitarian symbol of doctoring since its invention in 1816 by the French physician, René Laennec.
“I can guarantee you that you will walk out with these tools, and someone will say to you, ‘Ugh, a stethoscope? Those will be obsolete in about five minutes,’” said Lowe. The annual event also included distribution of the classic medical tools, purchased by alumni donors, to the students.
Despite the proliferation of technological tools that can probe the human body beyond vision and touch, Lowe explained that the role of the physical exam—how a patient looks, behaves, what they say, how their body responds to touch, and what the relatively unsophisticated instruments like the stethoscope, a patella hammer for checking reflexes, the ophthalmoscope to peer into eyes, and the otoscope for looking into the ear canal tell the physician—still plays a vital role in making a diagnosis and deciding what steps to take.
“You are the main diagnostic tool,” Lowe told his audience. “Your history-taking skills combined with your eyes, your ears, your senses, what you feel, how you examine people—that’s how you are going to start the process and it will lead you to the technology.”
Even a relatively simple tool like the stethoscope is more effective in the hands of
someone who is attuned to the patient and what their senses detect.
“I’ll tell you a story about a man who comes into our emergency room,” Lowe said. “He’s a 52-year-old man with a history of high cholesterol, high blood pressure; he’s got a pain right here and you have to make sure he’s not having a heart attack.”
A lab test shows no enzymes indicative of heart issues, the EKG is normal, a chest x-ray also reveals no injury, Lowe continued. But the next morning, the man has a rash spread across the right upper torso.
“It was shingles, which your grandmother could diagnose when she sees the rash,” said Lowe. “There’s no other way to diagnose this but to look at it.”
Lorraine Stanfield was an assistant professor of medicine who taught at the medical school for more than 20 years and worked at Dorchester House, a community health center affiliated with Boston Medical Center, for 25 years. She succumbed to breast cancer at age 56, in 2017. Two years prior, in 2015, she received the Stanley L. Robbins Award for Excellence in Teaching, the school’s highest teaching honor.
“During my time at the (Dorchester House) clinic, I constantly heard her name mentioned in conversation,” second-year medical student and Lorraine Stanfield Scholar
told the students.
Even a relatively simple tool like the stethoscope is more effective in the hands of someone who is attuned to the patient and what their senses detect.
Continued from previous page
“Sometimes while reviewing a note, I would come across one signed by Dr. Lorraine Stanfield. Even now, she continues to guide us all.”
“She never lost her wonder that we can make a diagnosis and learn so much from a physical exam,” added Kathryn Harris, MD, who worked alongside Stanfield at Dorchester House for 25 years.
Lowe said that even those who didn’t know, or who had never met, Stanfield were the beneficiaries of the knowledge passed down to her from her mentors—knowledge that she, in turn, imparted to colleagues and students, who, in turn, taught others.
First-year student Avenelle Onaif paused from unboxing the new stethoscope she’d picked up following the lecture. Lowe had urged students to find a mentor and Onaif felt the alumni gift of medical instruments was emblematic of the supportive structure buoying new entrants.



“The beautiful thing about medicine is the passing down of tradition and the passing down of information,” she said. ●
Lindsey Claus Sweeps Awards at IAMSE Meeting
Third-year medical student Lindsey Claus swept the student awards at the International Association of Medical Science Educators (IAMSE) annual meeting, receiving a Student Educational Scholarship Grant, a Travel Grant, and an Outstanding Student Oral Presentation Award. It is the first time a BU student has won all three awards in the same year.
Claus received the Student Grant award for her research project, “Building Self-Directed Dyadic Learning Experiences Through Preclinical Ultrasound Education,” which will provide the first comparative study of portable and nonportable ultrasound probes’ effectiveness in helping students with cognitive load and self-directed learning.
As part of the Travel Award, IAMSE will cover Claus’ conference registration to attend the next annual meeting, to be held in Cancún, Mexico.
The Outstanding Presentation Awards recognize the most outstanding medical education peer-reviewed oral or poster presentations at the meeting. Claus received this honor for her presentation, “Preclinical Ultrasound Education Using a Near-Peer Educational Model.”
Born and raised in Mansfield, Mass., Claus concentrated in mathematics at Harvard College before turning to medicine. Her research interests include medical education, ultrasound, clinical reasoning, and the application of machine learning to medical decision-making.
Also contributing to Claus’ work were fellow medical students Jessica Landau-Taylor, Brett Cassidy, and Minali Prasad, along with Jonathan J. Wisco, PhD, associate professor of anatomy & neurobiology.
IAMSE is a nonprofit professional development society, organized and directed by health profession educators with the goal
of promoting excellence and innovation in teaching, student assessment, program evaluation, instructional technology, human simulation, and learner-centered education. ●
Rebecca Wolinsky Named 2022 Pisacano Scholar
Rebecca Wolinsky, a fourth-year medical student, has been named a 2022 Pisacano Scholar, one of ten awardees selected by the board of directors of the Pisacano Leadership Foundation (PLF), Inc.
Recipients of the award are outstanding medical students who have committed to the specialty of family medicine. They possess demonstrable leadership skills, superior academic achievement, strong communication skills, identifiable character and integrity, and a noteworthy level of community service engagement. The scholarship, valued at approximately $28,000 for each recipient, provides educational programs, leadership training, and funding for fourth-year medical students identified as future leaders in family medicine.
Originally from Houston, Wolinsky earned her BA in Africana studies and community health from Brown University, where she received the Department of Africana Studies
Ida B. Wells Award for Community Activism and Undergraduate Scholarship.
While at Brown, driven by health equity and racial justice principles, Wolinsky worked to address structural determinants of health through Health Leads Providence, including work in the Providence refugee community and completion of an Africana studies honors thesis analyzing impacts of racism in medicine on US refugee healthcare.
Wolinsky then completed Bryn Mawr College’s postbaccalaureate premedical program and worked at Beth Israel Deaconess Medical Center as a medical practice assistant in a gynecology clinic that specializes in transgender health. Subsequently, she matriculated at Chobanian & Avedisian School of Medicine and, already committed to a career in family medicine, was selected as a National Health Service Corps scholarship recipient for all four years.
At Chobanian & Avedisian SOM, Wolinsky cofounded Creating Leadership and Education to Address Racism, a now-annual enrichment series featuring experts in the field, and also
cofounded the school’s Racism in Medicine Vertical Integration Group, which performed a detailed review of the MD program curriculum and developed recommendations for addressing racism in medicine. Committed to reproductive justice, she organized workshops to expand abortion access, led the largest delegation of medical students at the ROE Act Hearing, and was the sole medical
Bita Naimi Receives Physicians of Tomorrow Award

Fourth-year medical student Bita Naimi received a $10,000 Physicians of Tomorrow scholarship from the American Medical Association (AMA) Foundation. Scholarships are based on academic excellence and financial need.
Naimi is an Iranian American originally from Northern California. She is completing a research year in Philadelphia in the department of otolaryngology at Thomas Jefferson University. Her research focuses on rhinology (nose and sinus) and skull base surgery and she is working on a phase 2 clinical trial treating smell loss after COVID-19.
student to testify. She is a member of the Gold Humanism Honor Society and the Shapiro Academic Honors Society for clinical professionalism and humanism.
Wolinsky is thrilled to pursue a career in full-spectrum family medicine that combines her commitments to community health, reproductive justice, and addressing racism in medicine.

Since 1993, the PLF has selected 176 outstanding medical students. Approximately 3,000 applicants representing close to 200 medical schools competed for these scholarships. ●
Enrolled in the Seven-Year Liberal Arts/Medical Education BA/MD Program, Naimi is passionate about addressing healthcare disparities in minority and underserved populations and participates in several initiatives that address this issue.
The AMA Foundation has a long-standing tradition of supporting medical students. Since 1950, they have awarded more than $61 million in scholarships. With 12 scholarship categories and a variety of focus areas, including serving those underrepresented in medicine, the AMA Foundation works to recognize a diverse cohort of medical students each year. ●
Wolinsky is thrilled to pursue a career in full-spectrum family medicine that combines her commitments to community health, reproductive justice, and addressing racism in medicine.
PhD Student Spotlight: Jhonatan Henao Vasquez
Jhonatan Henao Vasquez is a fourth-year PhD candidate in the graduate program in Molecular & Translational Medicine (MTM).
Henao Vasquez entered Graduate Medical Sciences (GMS) through the Program in Biomedical Sciences (PiBS). He currently works in the Pulmonary Center, researching MIWI2-positive multiciliated cells.
Henao Vasquez is keeping his options open, but he knows that he sees himself returning to industry work.
Originally from Colombia, Henao Vasquez and his family immigrated to New Hampshire when he was two years old. After earning a chemistry degree from College of the Holy Cross, Henao Vasquez was on the fence about heading straight to graduate or medical school.
First, he decided to work at several area biotechnology companies, starting with positions at Lonza Biologics and Vertex Pharmaceuticals before moving to Moderna.
“Industry is something I’ve had the goal in mind to do,” Henao Vasquez says. “I want to learn what’s new in science and how to gain
those critical thinking skills that you get from a PhD education, but then incorporate that into a business aspect as well.”
That’s what led Henao Vasquez to enroll in PiBS.
He liked that the program’s first year was rotational, letting him explore varied interests in virology and infectious diseases. Ultimately, he chose to specialize in molecular and translational medicine, landing in the Pulmonary Center under Associate Professor of Medicine Matthew Jones, PhD, and Professor of Medicine Alan Fine, MD.
His research studies a subpopulation of multiciliated cells in the lung airway that— according to initial findings—exacerbate influenza. These cells express the MIWI2 gene, and Henao Vasquez’s specific project examines how this gene could contribute to viral pathogenesis and disease.
This research earned him the Ruth L. Kirschstein Predoctoral Individual National Research Service Award, an F31 grant awarded through the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Despite the challenges that come with completing his rigorous program, Henao Vasquez has found support both in and out of the lab within his cohort and lab members. Those friendships have been key during his time in the program, whether through hiking in the White Mountains, exploring Boston’s breweries, or playing video games.
“That’s been one of my favorite memories, getting to know the people and knowing that you’re not in it alone,” Henao Vasquez says. “Everyone is together; I like that camaraderie.” ●

Despite the challenges that come with completing his rigorous program, Henao Vasquez has found support both in and out of the lab within his cohort and lab members.
Lesotho-Boston Health Alliance Receives UN, WHO Primary Health Care Award

An innovative program between the department of family medicine and the Lesotho Ministry of Health recently was honored by the United Nations (UN) at the annual meeting of the Friends of the UN Interagency Task Force on the Prevention and Control of Noncommunicable Diseases.
Aimed at improving the physician-patient ratio for Lesotho and training leaders for public health infrastructure, the LesothoBoston Health Alliance (LeBoHA) allows students from Lesotho who have completed medical school abroad to return to their home country, in Southern Africa, to complete their residency—and remain there.

The 2022 UN Interagency Task Force and the World Health Organization (WHO) Special Programme on Primary Health Care Award recognizes LeBoHA’s achievements in strengthening Lesotho’s healthcare system by providing context-specific primary healthcare training for providers at the community level.
The award highlights LeBoHA’s role in providing an exemplary platform for primary healthcare professionals to collaborate and
jointly strengthen action across Europe, including advocating for ever-stronger, fairer, and more equitable primary care. This year, the task force joined forces with the WHO Special Programme on Primary Health Care and expanded the award to recognize work in primary care for the prevention and control of noncommunicable diseases.
“I am humbled by this honor,” says Brian Jack, MD, professor of family medicine and LeBoHA director. “I would like to thank all of our members who made this award possible and who continue to work to make our pro-
gram an example for healthcare delivery in low-income countries.”
Started in 2003, the partnership between the department of family medicine and the Lesotho Ministry of Health has developed an innovative family medicine residency program in Lesotho, which is now fully accredited, self-sustaining, and directed by a program graduate. All program graduates have remained in Lesotho to practice, which has improved the country’s physician-patient ratio, trained leaders, and strengthened the public health infrastructure. ●
The award highlights LeBoHA’s role in providing an exemplary platform for primary healthcare professionals to collaborate and jointly strengthen action across Europe.
CityLab Receives NIH Award to Increase Diversity in Biomedical Sciences Workforce & STEM

Boston University CityLab, a biotechnology learning laboratory for middle and high school teachers and their students, has received a five-year, $1.3 million Science Education Partnership Award (SEPA) from the National Institute of General Medical Sciences of the National Institutes of Health (NIH), the only new SEPA award made to a Massachusetts institution in 2022.
This will allow CityLab to develop, implement, and evaluate a new curriculum for high school students that explores genome editing and builds awareness of diversity, equity, inclusion, and social justice in STEM, as well as emphasize their importance to the biomedical sciences.
A partnership between Boston University’s Chobanian & Avedisian School of Medicine and Wheelock College of Education & Human Development, CityLab was first funded by the NIH SEPA program in 1991 and is one of just a few programs continuously operating since. The new grant project, “Mystery of the Crooked Cell 2.0: CityLab’s Next Generation Socioscientific Approach to Gene Editing,” addresses the need for NIH’s pre-college activities to focus on biomedical workforce preparedness, especially for underrepresented minorities.
This project will expand CityLab’s “Mystery of the Crooked Cell” hands-on, inquiry-based curriculum supplement that focuses on the molecular basis of sickle cell disease by incorporating state-of-the-art gene editing content immersed with socioscientific reasoning (SSR). “This project will reach close to 600 local URM [Underrepresented Minority] students and, through planned web-based dissemination of the finished curriculum, will reach thousands of students,” explains coprincipal investigator Carl Franzblau, PhD, professor of biochemistry and CityLab founder.
According to coprincipal investigator Donald DeRosa, EdD, clinical associate professor and science education program director at Wheelock College of Education & Human Development, the “SSR approach places science content in a meaningful social context and motivates students to take ownership of their learning.” SSR skills include realizing the complexity of the content and context of an issue, analyzing an issue from multiple perspectives, seeking out sources of bias in data, and considering if and how scientific investigations can advance understanding of an issue.
“Genome editing is becoming part of the physician’s toolkit, so teaching young people about this important and rapidly advancing field will prepare them to be informed patients and, we hope, will position them to enter careers in the biomedical sciences or health professions,” says coprincipal investigator Carla Romney, ScD, CityLab director of research. ●
A partnership between Boston University’s Chobanian & Avedisian School of Medicine and Wheelock College of Education & Human Development, CityLab was first funded by the NIH SEPA program in 1991 and is one of just a few programs continuously operating since.
faculty news
Appointments, Honors & Awards
Anthony “Tony” Hollenberg, MD, has been named John Wade Professor and chair of the Department of Medicine (DOM) at the Chobanian & Avedisian School of Medicine, and physician-in-chief at Boston Medical Center (BMC).

Hollenberg previously served as chair of the Joan and Sanford I. Weill Department of Medicine at Weill Cornell Medicine and physician-in-chief at New York-Presbyterian/ Weill Cornell Medical Center in New York City. He also served as chief of the Division of Endocrinology, Diabetes and Metabolism and vice chair for mentoring at Beth Israel Deaconess Medical Center and professor of medicine at Harvard Medical School.
lism, including body weight. His laboratory also explores the underpinnings of thyroid gland development. He has published more than 98 original studies in journals and contributed 31 book chapters and reviews. Hollenberg’s extensive research expertise will enhance preclinical, translational, and clinical research across the department.
Venetia Zachariou, PhD, Appointed Chair, Pharmacology, Physiology & Biophysics

Venetia (Vanna) Zachariou, PhD, was named chair of pharmacology, physiology & biophysics, effective December 1, 2022. Zachariou is replacing David Farb, PhD, who announced his intention to step down last year, and William Lehman, PhD, who was appointed ad interim chair upon David Atkinson’s announcement, also last year. The name of the combined department will be chosen after discussions with the faculty, students, and other stakeholders.
conditions and pain/addiction comorbidities. Her team has identified several intracellular pathways that control the perception and maintenance of chronic pain states. They also have developed novel interventions in epigenetic pathways that allow transitioning to nonopioid analgesics while preventing the development of physical dependence.
Zachariou received her BSc in pharmacy from the University of Patras, Greece, and her PhD in pharmacology from the Medical College of Georgia. Following a postdoctoral fellowship in the department of psychiatry at Yale University and a junior faculty position at UT Southwestern Medical Center in Dallas, she established her laboratory at the University of Crete School of Medicine. In 2012, she joined the departments of neuroscience and pharmacological sciences at the Icahn School of Medicine at Mount Sinai in New York as an associate professor (with tenure since 2016), and as full professor since 2018.
Hollenberg’s extensive research expertise will enhance preclinical, translational, and clinical research across the department.
A native of Toronto, Hollenberg received his bachelor’s degree from Harvard College and his medical degree from the University of Calgary. He completed his residency in internal medicine at Beth Israel Deaconess Medical Center followed by a clinical and research fellowship at Massachusetts General Hospital.
A leading physician-scientist specializing in endocrinology, Hollenberg’s work focuses on thyroid disorders and investigating the physiological and molecular mechanisms by which thyroid hormones regulate metabo-
Zachariou previously served as professor of neuroscience and pharmacological sciences at the Icahn School of Medicine at Mount Sinai. She studies signal transduction and epigenetic mechanisms of neurological disorders and their treatment using genetic mouse models, genomic assays, and brain biochemistry. Current projects investigate transcriptional and epigenetic mechanisms of chronic pain with emphasis on the identification and validation of novel treatments for the management of peripheral neuropathy and other chronic pain conditions. Another line of research in her laboratory investigates the role of G protein signal transduction complexes in drug addiction, opioid analgesia, and physical dependence. By understanding intracellular adaptations to peripheral nerve injury and/or prolonged opioid exposure, she aims to develop novel therapeutics for chronic pain
Current
projects investigate transcriptional and epigenetic mechanisms of chronic pain with emphasis on the identification and validation of novel treatments for the management of peripheral neuropathy and other chronic pain conditions. Another line of research in her laboratory investigates the role of G protein signal transduction complexes in drug addiction, opioid analgesia, and physical dependence.
Zachariou is a member of the editorial boards of Biological Psychiatry, Molecular Pain, Science Signaling, and Neurobiology of Pain, section editor for European Journal of Neuroscience, and a member of the NIH Molecular and Cellular Neuropharmacology study section. She is a fellow in the American College of Neuropsychopharmacology and chairelect for the ASPET Neuropharmacology Division.
Appointments, Honors & Awards
David M. Greer, MD,Appointed Secretary of Neurocritical Care Society
Chair of Neurology David M. Greer, MD, MA, was appointed secretary of the Neurocritical Care Society (NCS), effective October 2022.
The NCS is the only professional society representing multidisciplinary teams of neurocritical care providers around the world whose mission is to improve outcomes for patients with life-threatening neurological illnesses. Comprising physicians, nurses, pharmacists, advanced practice providers, researchers, and scientists, the neurocritical care team serves patients with life-threatening brain and spinal cord emergencies and injuries, using training in areas like advanced brain and nervous system monitoring and pharmacotherapy, with one goal—to bring their collective knowledge to drive the best possible outcomes.
Greer, who also serves as chief of neurology at Boston Medical Center, has research interests that include predicting recovery from coma after cardiac arrest, brain death, targeted temperature management for acute brain injuries, and multiple stroke-related topics including acute stroke treatment and stroke prevention. He is a leader in the Neurocritical Care Society, the Society of Critical Care Medicine, and the American Academy of Neurology.
He received his BA in English Literature from Williams College, an MA in English Literature and MD from the University of Florida, and an MA privatim from Yale University. He completed his internship in internal medicine and residency in neurology at Massachusetts General Hospital (MGH), followed by fellowship training in vascular neurology and neurocritical care, also at MGH.
Greer is the editor-in-chief of Seminars in Neurology and a fellow of the Society of Critical Care Medicine, American Academy of Neurology, American Heart Association, American Neurological Association, and Neurocritical Care Society. He has authored more than 350 peer-reviewed manuscripts, reviews, chapters, guidelines, and books.
Aram Kaligian, MD, MPH, Named Director, BU-Armenia Medical Partnership


Aram Kaligian, MD, MPH, assistant professor of family medicine, has been named director of the BU-Armenia Medical Partnership, succeeding Richard Babayan, MD, professor and chairman emeritus of urology.
The partnership was formed in 1991 by then-Dean (now President Emeritus) Aram Chobanian, MD, to help improve medical care and education in the Republic of Armenia. The primary activities include facilitating medical school faculty exchanges and a fourth-year medical student elective rotation in Armenia and helping develop medical school curricula in Armenia.
Formerly director of the Family Medicine Inpatient Service at Boston Medical Center, Kaligian has a primary care practice at South Boston Community Health Center. His activities in Armenia have included retraining physicians in primary care as part of a USAID program and conducting a public health study in Nagorno-Karabagh. He received his bachelor’s degree in biochemistry and English from the University of Massachusetts Amherst and his MD and MPH from Tufts University School of Medicine.
Toby C. Chai, MD, Elected Trustee of American Board of Urology

Toby C. Chai, MD, chair of urology, was elected a trustee of the American Board of Urology (ABU) to a six-year term starting February
23, 2023. Chai was nominated to the ABU by the American Urological Association (AUA).
Chai, also chief of urology at Boston Medical Center, has been actively involved in urologic research to seek improvements in urologic care. He received career development awards from the American Foundation for Urologic Diseases and a K08 grant from the National Institutes of Health (NIH) prior to receiving independently funded, investigator-initiated research awards from the NIH as principal investigator including R01, U01, and P20 grant mechanisms.
He has been recognized for his academic accomplishments including the Society of Basic Urologic Research Young Investigator Award; the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction Zimskind Award and Distinguished Service Award; the AUA Victor A. Politano Award for outstanding work in treatment of urinary incontinence and innovations in bladder research, and the Distinguished Service Award for work on urologic research advocacy. He has also received the Continence Champion Award from the advocacy group National Association for Continence.
Chai serves as an associate editor for Journal of Urology and on the editorial board for American Journal of Physiology—Renal Physiology. He has served as both a charter and ad hoc member of numerous NIH grant review committees and was a charter member for the US Food and Drug Administration Bone, Reproductive, and Urologic Drug Advisory Committee.
Founded in 1935, the American Board of Urology acts for the benefit of the public by establishing and maintaining standards of certification for urologists, working with certified urologists to achieve lifelong learning to ensure the delivery of high-quality, safe, and ethical urologic care. Six urologic societies nominate to the ABU and sponsor its activities, including the American Urological Association, the American Association of Genitourinary Surgeons, the American Association of Clinical Urologists, the American College of Surgeons, the Society of Academic Urologists, and the Societies for Pediatric Urology. ●
The primary activities include facilitating medical school faculty exchanges and a fourth-year medical student elective rotation in Armenia and helping develop medical school curricula in Armenia.
Marcelle W. Willock, MD
MARCELLE W. WILLOCK, MD , professor emerita of anesthesiology and from 1982 to 1998 chair of the department, passed away October 12, 2022, from complications after emergency surgery while visiting relatives in Toronto, Canada. She was 84.
Willock remained vibrant and engaged within the department after retirement, attending lectures and interacting with residents and faculty. She was among the first women of color to lead an academic and clinical department in the United States and the first Black woman to achieve emerita status at the school.

Her many noteworthy accomplishments while serving in the former Boston University Medical Center Hospital and Boston City Hospital (now Boston Medical Center) included accrediting the anesthesia residency program and modernizing the administration of anesthetics from both professional and technological standpoints. She was responsible for standardizing guidelines related to patient safety and for the introduction of pulse oximetry, capnography and transesophageal echocardiography, among other innovations, into operating rooms. In the early 1980s, there still were dentists providing anesthesia care at Boston City Hospital. One of her most remarkable actions was to end this practice and assure that only qualified physician anesthesiologists could provide anesthesia care following the care team model promulgated by the American Society of Anesthesiologists.
She was on multiple Medical Campus committees, served as president of the Massachusetts Society of Anesthesiologists and the Society of Academic Chairs, and held a variety of leadership positions
with the American Society of Anesthesiologists. She also served as president of the Louis and Martha Deveaux Foundation, a charitable organization in the Republic of Panama.
Willock was a consultant for the Federal Bureau of Investigation, a member of the
board of directors for the Boston Police Athletic League, worked in the Office of the Chief Medical Examiner in New York City, and served as a trustee for the College of New Rochelle. After leaving BU, Willock became the first female dean of Charles Drew University College of Medicine and Science in Los Angeles, where she retired in 2005. An advocate for civil rights and diversity, she collaborated with many programs addressing healthcare disparities and the fair treatment of minorities.
She generously supported two important funds at BUMC, the Violeta Martinez and Rafael Ortega Anesthesiology Research Fund, and the Marcelle W. Willock, MD, Faculty Development & Diversity Program, a longitudinal leadership and career development program for BUMC faculty from underrepresented racial and ethnic groups.
Willock is survived by her niece and nephews Jason, Yvette, Dominic, and George. ●
An advocate for civil rights and diversity, she collaborated with many programs addressing healthcare disparities and the fair treatment of minorities.





behind astonishing $100 million gift to BU’s School of Medicine
The Lifelong Friendship end
Alumni clarinetist’s philanthropy and humility result in the Boston University
Aram V. Chobanian & Edward Avedisian School of Medicine
BY JOEL BROWNEditor’s Note: This story originally appeared September 29, 2022, in BU Today. Sadly, Mr. Avedisian passed away December 7, 2022. He was 85.
TWO ARMENIAN FAMILIES FINDING FREEDOM IN AMERICA.
Two boys growing up poor a few doors apart in hardscrabble Pawtucket, Rhode Island.
Two successful men—one a renowned cardiologist and former president of Boston University, the other a celebrated clarinetist for the Boston Pops—changing the course of Boston University history.
Lifelong friends Aram V. Chobanian, MD (Hon.’06) and Edward Avedisian (CFA’59,’61, Hon.’22) will now be connected forever as the namesakes of BU’s medical school. Thanks to a $100 million gift from Avedisian that will support scholarships, endowed faculty chairs, and cutting-edge research and teaching, the school is being renamed the Boston University Aram V. Chobanian & Edward Avedisian School of Medicine.
University President Robert A. Brown called it “one of the most remarkable grants in the history of higher education” at a private signing ceremony at his residence in late August to accept the gift and formalize the school’s name change.
The gift was announced to the public in September at the school, before invited guests under a tent on Talbot Green, where both men shared the podium with Brown; Ahmass Fakahany (Questrom’79), BU Board of Trustees chair; and Karen Antman, MD, dean of the medical school and provost of the Medical Campus. Avedisian received a standing ovation and cheers before the sign with the new name was unveiled.
“This is a historic day for the medical school and for Boston University,” Brown said. The gift “gives an extra tailwind and boost to our aspirations that will benefit so many,” Fakahany said.
Avedisian and Chobanian donned ballcaps and white medical coats emblazoned with the new name. “With this white coat, I’m ready to see patients,” Chobanian said to laughter.
Avedisian is retired after nearly four decades of playing the clarinet with the Boston Pops and the Boston Ballet Orchestra. But it was the stunning success of his personal investments that afforded him the opportunity to give back to others. He has never forgotten his parents’ hard work and sacrifice, or the emphasis they placed on education, and he became a generous philanthropist to both the United States and Armenia in his later years. “I felt very fortunate, for BU and others that helped along the way,” he says.
Even still, in all of his donations to colleges, hospitals, and schools, Avedisian never wanted anything named after himself, and he didn’t want his gift to BU to be any different. But when he proposed that his donation instead honor his childhood friend Chobanian, president emeritus of BU and dean emeritus of the School of Medicine and provost of the Medical Campus, as well as a nationally renowned cardiologist, the plan hit a bump. Chobanian, showing the same humility as Avedisian, firmly declined the honor when first asked—and a few more times after. Neither man, it seemed, wanted his own name up in lights.
“Both men are very, very, humble,” Brown says. “Really oldschool.”
Brown persisted with the pair, until finally they agreed as long as both their names were included. Brown calls it “the grand compromise.”
“How could I obstruct a gift of $100 million to the medical school that I spent my life at?” Chobanian says. “That was obviously a big factor, but I still felt it should be named after him, and my name didn’t have to go on there.”
“I didn’t want anything named after me,” Avedisian says. “But he said, ‘I’ll only do this if your name is attached.’ So, we’re attached.”
STUDENTS, SCHOLARSHIPS, AND RESEARCH ALL BENEFIT
The gift “will transform the medical school,” says Antman. The Aram V. Chobanian & Edward Avedisian School of Medicine
Endowed Fund will provide:
• $50 million to support scholarships for medical students
• $25 million to support endowed professorships
• $25 million to the Avedisian Fund for Excellence to keep the school at the forefront of research and teaching
“I am glad that much of the gift will support scholarships,” Antman says. “Medical school debt is a problem across the United States.” A study on the Class of 2021 by the Association of American Medical Colleges found the average medical school debt among students attending a public school was $194,280. That contributes to the growing shortage of primary care doctors in the United States, since the much higher salaries for specialists make it possible for them to pay off student loans more rapidly. Some aspiring pediatricians and primary care doctors simply may not be able to afford to do so.
The cost also affects who can choose medical school, Antman says. “If you are first-generation American or firstgeneration in college, the idea that you are going to graduate
Lifelong friends, Dr. Chobanian and Mr. Avedisian will be connected forever as the namesakes of BU’s medical school.
with $200,000plus in debt is unconscionable. They are afraid to take on that much debt.”
Avedisian’s gift, she says, “will approximately double the endowed scholarship aid we can offer.” The funds will come in over a period of at least five years.
One of the endowed professorships from the fund will be created in the name of Richard K. Babayan, professor and chair emeritus of urology and former chief of urology at Boston Medical Center, BU’s primary teaching hospital and Boston’s safety net hospital. A friend of the Avedisians, Babayan is the former director of the medical school’s Armenia Medical Partnership Program, a post now held by Aram Kaligian, an assistant professor of family medicine.
Another endowed chair will support the director of the National Emerging Infectious Diseases Laboratories (NEIDL), who will be a professor at the medical school.
“The endowed chairs will help us recruit the best and the brightest faculty,” Antman says, “which also helps attract the best students. The best students really resonate with the best faculty. The two together are synergistic—and then getting better equipment for both of them.”
Expensive equipment such as a cryogenic electronic microscope or a research MRI suite can cost millions. Granting agencies that support such purchases, such as the National Institutes of Health, often like to see matching dollars, Antman says.
“Then they’re more likely to give us the grant, so again we can attract the best faculty and students doing the most exciting cuttingedge research,” she says. “With these funds, we can renovate labs and attract students who might have gone elsewhere.”
THE STORIES BEHIND THE NAME
Both men’s ties to BU date back more than half a century.

Chobanian joined the BU School of Medicine faculty in 1962 and made an impact as a professor, dean, and Medical Campus provost, taking a lead role when Boston City Hospital and Boston University Medical Center Hospital merged to create Boston Medical Center in 1996. He then stepped in during a tumultuous time as BU president ad interim after John Silber stepped down as president for good in 2003; the trustees removed the “ad interim” from his title in 2005.
“At a time of turmoil,” says Brown, who succeeded Chobanian as president in 2005, “his calming influence held the University together and advanced it.”

Two successful men —one a renowned cardiologist and former president of Boston University, the other a celebrated clarinetist for the Boston Pops— changing the course of Boston University history.
Avedisian, in addition to being an alum, has made a number of previous donations to BU, including to scholarship funds in Chobanian’s name. The gift to the medical school also enabled the endowment of two scholarships at BU’s College of Fine Arts named in honor of Avedisian’s wife and Chobanian’s wife (see sidebar). His other BU connections include his niece and nephew: Laurie Onanian, who worked in BU’s development office for nine years, and Craig Avedisian (LAW’93), a commercial litigator. Both were deeply involved in arranging the gift.

But long before their BU days, Avedisian’s and Chobanian’s friendship was forged on the streets of Pawtucket.
“I first met Ed when he was a little squirt,” Chobanian says with a grin.
Both families suffered tragic losses in the Armenian genocide, in which it’s estimated that as many as 1.5 million people died. Both men’s parents met and married after immigrating to the United States, and settled down to raise their children in Pawtucket, where there were plenty of jobs in the textile mills. The Chobanians lived at 549 Broadway, the Avedisians a few doors down, at 575.
With eight years between them (Chobanian was born in 1929, Avedisian in 1937), the boys weren’t that close—Chobanian knew Avedisian’s older brother, Paramaz, better, as they were only two years apart. “Ed was very small, but a very active individual,” Chobanian says. “He hung around, and we didn’t know what to do with him.”
But Avedisian says Chobanian was indirectly responsible for his eventual distinguished career in music.
“Aram was the pace car. Whatever Aram did, my brother did,” Avedisian says. “Aram studied clarinet, my brother studied clarinet. Then they both gave it up, and there was a clarinet in the house, and I said, ‘OK, I’ll take that on.’”
Soon Chobanian went off to college and medical school. Avedisian found his calling in the woodwind instrument.
He chose BU after becoming entranced with the clarinetist on a recording of the Boston Symphony Orchestra he heard on the radio. “Who is this guy?” the teenage Avedisian asked himself. “I want to study with him.” The musician was Manuel Valerio, a professor at CFA.
At BU, Avedisian earned bachelor’s and master’s degrees in music—with a $350 scholarship his first year, he says, and more
$1 Million for CFA
IN ADDITION TO CREATING the Chobanian & Avedisian School of Medicine, the gift also enabled the endowment of two scholarships in music and visual arts at the College of Fine Arts: the Jasmine Chobanian Endowed Fellowship Fund for Visual Arts and the Pamela Avedisian Endowed Fellowship Fund for Performance Music.
The late Jasmine Chobanian was regarded as the “First Lady” of Boston University during her husband’s tenure as BU’s leader. They knew each other casually growing up in Pawtucket, Rhode Island, but didn’t become a couple until both were studying at Brown University. She was a patron of the arts who served on the board of the Boston Ballet and a talented painter who studied at what is now the School of the Museum of Fine Arts. She shared her husband’s Armenian heritage. They were married for 59 years, until she died after a brief illness in 2014.

Pamela Avedisian (Hon.’22) is a talented pianist who spent a year as a piano major at Stetson University School of Music in Florida, but transferred to Endicott College after deciding not to make music her career. She became a legal secretary and worked for 20 years for the head of the litigation department at a top Boston law firm. She had met Avedisian when he was directing a chorus at Endicott and she asked if he needed a pianist. They started dating a few years later and married in 1994. She has learned to read, write, and speak Armenian.
Both of the women’s husbands are also immersed in the arts, says Harvey Young, dean of CFA, noting Avedisian’s orchestra career alongside his investing.
“Dr. Chobanian, although he led the medical school, he is a person who is highly invested in the arts personally,” says Young. “In his retirement, he has moved into composition, working with members of the CFA music faculty. That love for medicine and love for the performing arts is distinctive about him.
“Too often we create a false divide between the sciences and the arts, as if people come from totally different worlds or inhabit different planets,” Young says, “and what these two individuals demonstrate is that those are essentially one and the same.” ●
Chobanian, showing the same humility as Avedisian, firmly declined the honor when first asked—and a few more times after. Neither man, it seemed, wanted his own name up in lights.
later. He went on to play for decades with both the Pops and the Boston Ballet Orchestra, appearing with the Boston Symphony Orchestra and the Metropolitan Opera, among many others, and backing greats like Luciano Pavarotti and Leontyne Price.
GOOD FORTUNE LEADS TO ANOTHER PATH
As his music career was thriving, it was Avedisian’s “sideline” as an investor, beginning in the 1970s, that ultimately made his generous philanthropy possible. He was self-taught, an avid reader of books on the topic as well as of Investor’s Business Daily, and eventually became a regular viewer of CNBC and Bloomberg on cable.
“You think about the deep discipline that’s required to be a high-level professional musician, the years of self-study and attention to detail—he applied that same skill set to become a masterful investor,” says Harvey Young, PhD, dean of CFA.
From previous gifts that he’d made, many people knew Avedisian had done well—but hardly anyone knew just how well until the magnitude of this year’s gift was revealed. A clarinetist donating $100 million?



“Ed has done just phenomenally as an investor,” Brown says with a smile. “And as in most cases for investors, unless they’re dot-com founders, so you can see their founder stock, you really don’t know. You just do not know. He’s done phenomenally well, and when you think about the generosity of giving $100 million and the other gifts he’s given, he’s just an incredibly generous human being.”
The friendship of the two, Chobanian and Avedisian, blossomed slowly in recent years. As adults, they saw each other occasionally—a wave or a friendly word when Chobanian attended a Boston Ballet performance, for example. They began to talk more in the 1990s, after Avedisian sent a donation for the Armenia Medical Partnership Program, along with a note to Chobanian.
Chobanian says that when he retired from the BU presidency in 2005, they grew closer.
“I had more time and we started to socialize, and we became very good friends, and our wives became friends, as well,” he says. “He’s done unbelievable amounts in his lifetime. It’s amazing how he’s such a fine musician of the highest caliber, but still is able to become a philanthropist—I don’t think there are many musicians who can say that.”
The admiration goes both ways.
He “can’t do enough for people, and does it all with great ease and graciousness, really exemplary,” Avedisian says of Chobanian. “His personality has never changed—that’s just the way he is.”
Both men have been particularly determined to help their families’ homeland.
Chobanian joined the board of directors of the Fund for Armenian Relief. He also focused on improving medical education and care through a variety of programs, including training physicians, nurses, and other health professionals in emergency medicine and healthcare management, and the development of medical residency and postgraduate educational programs in Armenia.
For his part, Avedisian became a trustee of the American University of Armenia, supported construction of its Paramaz Avedisian Building, named for his brother, and the new Khoren and Shooshanig Avedisian School and Community Center, named for his parents. Recipient of an honorary doctorate from the University of Rhode Island in 2019, he is also a trustee for the Armenian Missionary Association of America and the National Association for Armenian Studies and Research.
SHOULDER TO SHOULDER
At the late afternoon signing event in August, Chobanian and Avedisian arrived separately and greeted BU officials and others cheerfully. But they both lit up simultaneously when they saw each other, grinning as they bantered, lifelong friends making a difference in the world—together.
A few days later, after Chobanian had time to reflect on the naming gift, he said that he was beginning to appreciate the significance of it: “I think it’s wonderful for the medical school and the University. It’s still uncomfortable for me, but very satisfying at the same time, very beautiful.”
One last note about that new name for the medical school: that’s a lot of syllables to stitch onto the traditional spot on all those white coats that medical graduates receive. “We were trying to figure out how to fit it on the pocket,” Antman says with a smile. “It would have to be very tiny print.” The solution? Two lines on the left breast.
Richard Reidy (Questrom’82), vice chair of the BU Board of Trustees, who attended the signing event, told the small gathering that Avedisian’s gift is “a spectacular milestone in the history of Boston University.”
“There is an Armenian aphorism that says, ‘Once we give shoulder to shoulder we can turn mountains,’” Reidy said. “The members of the BU medical community are going to wake up every morning and turn mountains to reach the underserved, to innovate new treatments and breakthrough cures, and to never stop learning.” ●
Students, AdministratorsFaculty, Cheer Historic Name Change, Major Donation
UP UNTIL THE BIG REVEAL, attention had been focused on the two men onstage. Edward Avedisian and Aram Chobanian, MD, were childhood friends whose parents had fled genocide in Turkish Armenia in the 1910s. They lived four doors away from one another in Pawtucket, Rhode Island, and both achieved remarkable success—Avedisian as a clarinetist with the Boston Pops and Boston Ballet Orchestra and as an extremely savvy investor who quietly accumulated a fortune, and Chobanian, who had a long career at Boston University as a pioneering cardiologist, dean of the medical school, medical campus provost, and University president.
The two were onstage on Talbot Green in the afternoon of Thursday, September 29, to announce Avedisian’s donation of $100 million and the renaming of the medical school as the Aram V. Chobanian & Edward Avedisian School of Medicine. Under the big white tent, they were joined by invited guests, faculty, medical and graduate students, and other curious passersby who had gathered on the lawn to witness the new name revealed on the entrance to the Instructional building.
Reactions from the audience varied depending on their connection to Avedisian and Chobanian and how the $100 million—with $50 million going to student scholarships, $25 million to endowed professorships, and another $25 million to research and teaching—will affect them.
All were drawn to the story of a lifelong friendship.
MELISSA
HWANG
“It was so heartwarming to see the both of them talk about the challenges they had to overcome and the people they helped along the way,” said Melissa Hwang, a second-year medical student from Taiwan who had volunteered to work the event.
ANGELA JACKSON, MD


Angela Jackson, MD, associate dean for student affairs and associate professor of medicine/GIM, thought the additional scholarship money would make a huge difference to students. But she also felt the message being conveyed by the gift was an affirmation of the students and the medical school’s mission.

EVA GAUFBERG
“I think it’s incredible. I feel everything helps,” said second-year medical student Eva Gaufberg, from Winchester, Massachusetts, who also volunteered to help out at the ceremony. Gaufberg found it extremely thoughtful that Avedisian decided to give the largest portion of the gift to relieve student debt.
“Being able to make things even just a little bit more affordable is important and something I think a lot of students think about when choosing a school,” said Gaufberg.

“Most important is that there is an individual who cares so much about the future of medical students as individuals, and also about the future of medicine…that they are willing to provide this huge gift to the medical school,” said Jackson. “I think it speaks volumes to the recognition that we’re doing good work…”
FREDRIC MAJNOUN
As a fellow Armenian, Fredric Majnoun, associate dean for research administration, was proud to see Avedisian and Chobanian’s names on the medical school. Chobanian hired him 22 years ago. The $50 million split between endowed professorships and teaching and research will help recruit and retain high-quality faculty, he said.

“Recruiting faculty is expensive, and these kinds of donations will help us compete with other universities,” said Majnoun. “It gives the freedom to choose what kind of research [faculty] want to do, who they want to recruit, what kind of equipment they want to purchase, and what renovations need to be done,” he said.
ANGELIQUE HARRIS, PHD

“It really highlights and emphasizes the role and the influence the institution has because [Avedisian] could have given this money to a number of different institutions,” said Angelique Harris, PhD, associate dean of diversity & inclusion. “I was very excited about the prospect of faculty who are doing this really innovative, incredible research being able to be retained here.”
BENJAMIN WOLOZIN, MD, PHD
Chobanian also hired Benjamin Wolozin, MD, PhD, professor of pharmacology & experimental therapeutics, who stood on the sidewalk watching the ceremony.
JACK RUSKE
“I can say that debt is on the minds of all medical students,” said Jack Ruske, a third-year MD student. “Students will be able to come and train at BU and BMC [teaching affiliate Boston Medical Center] and do that because they want to help underserved populations rather than going somewhere else that is less expensive.”

“I just have a really warm place in my heart for him,” said Wolozin. “He’s such an amazing guy and the idea of a name change that reflects on two people so intimately connected to BU, I think it’s wonderful. And that the money fits in with the mission of BU.”
Wolozin said he was surprised at the size of the donation.
“BU needs those kinds of donations to really achieve greatness,” he said.
research
● BU Participates in the New England Pathogen Genomics Center of Excellence

Boston University Chobanian & Avedisian School of Medicine will partner with the Massachusetts Department of Public Health (DPH) and six other institutions to participate in the Pathogen Genomics Center of Excellence (PGCoE) network, to help foster and improve innovation and technical capacity to better prevent and respond to infectious disease outbreaks.
Twenty-five million dollars in funding over five years will establish DPH as a regional focus for developing state public health laboratory genomics capability and epidemiologic application of genomics to public health.
Connor and his team are studying how rapid sequencing of viral genomes can be paired with contact tracing data to understand how and where disease gets spread.
• educate and train health departments on the use of genomics; and
• prepare for and respond to infectious disease threats.
“The Massachusetts COVID-19 response has relied on our many colleague laboratories, institutions, and organizations, including universities and partners in the medical, public health, and scientific community,” says DPH Assistant Commissioner Kevin Cranston, director of the Bureau of Infectious Disease and Laboratory Sciences. “We believe this Center of Excellence will spur new innovation and inform how we address future public health threats.”
Nationally, a total of $1.7 billion in funding from the American Rescue Plan is helping to support current and future genomic surveillance. These funds include $400 million for innovation, approximately $90 million of which will support the PGCoE network over the next five years.
● Study Finds Full-Occupancy, In-Person Teaching Did Not Lead to SARS-CoV-2 In-Class Transmission at BU
One of five national recipients selected to establish a center by the Centers for Disease Control and Prevention (CDC), the DPH also chose MIT’s Broad Institute, Harvard University, Yale University, Fathom Information Design, Massachusetts General Hospital, and Theiagen Genomics to partner in their initiative.
Leading the research is John H. Connor, PhD, associate professor of microbiology and a researcher at the National Emerging Infectious Diseases Laboratories. Connor and his team are studying how rapid sequencing of viral genomes can be paired with contact tracing data to understand how and where disease gets spread. “We need a greater understanding of where transmission happens and what practices can keep people safe,” he says.
The four other regional centers designated by the CDC include the Georgia Department of Public Health, Minnesota Department of Health, Virginia Division of Consolidated Laboratory Services, and Washington State Department of Health. Combined, these Centers of Excellence will serve as a network to:
• perform a landscape analysis of gaps, needs, and opportunities for genomics in the US public health system;
• pilot and implement genomics technologies and applications for public health;
SARS-CoV-2 has displayed personto-person transmission in a variety of indoor situations. This potential for robust transmission posed significant challenges to colleges and universities, where indoor learning is a focus.
Is there evidence of in-class transmission of SARS-CoV-2 on a university campus that has mandated vaccination and masking? The answer is no, according to a study in JAMA Network Open
“Going back to full-occupancy, in-person teaching at BU did not lead to SARS-CoV-2 transmission in class,” says John H. Connor, PhD, associate professor of microbiology, one of the study’s corresponding authors.

SARS-CoV-2 has displayed person-to-person transmission in a variety of indoor situations. This potential for robust transmission posed significant challenges to colleges and universities, where indoor learning is a focus.
To determine whether in-class instruction, without any physical distancing but with other public health mitigation strategies (masking, surveillance testing, enhanced air filtration, vaccinations), is a risk for driving transmission, the researchers used a blend of surveillance testing,
epidemiology, and viral genomics to analyze incidences of likely transmission in more than 140,000 class meetings. Only nine instances of potential in-class transmission were even identified.
“Our reasoning was that if there was in-class transmission, then each person in that potential transmission event would have the same genome,” says Connor. “It turned out that none of the nine potential in-class transmission events was real.”
● Plus-Sized Models Rising in Presence on Social Media
With the changing societal body image in America, plus-sized models have gained in popularity and positively impacted a body-inclusive model of beauty.

“While the American standard of beauty appears to idolize extreme thinness as seen in Victoria Secret models and their diminishing body sizes, we sought to explore the impact of plus-sized models by reviewing their body size metrics and social media presence to better understand their emerging role in the current standards of beauty,” explains corresponding author Neelam Vashi, MD, associate professor of dermatology.
A total of 169 models were included in this study (159 plus-sized models and 10 mainstream models). Data pertaining to social media presence was collected for each model using Social Blade (http://socialblade.com).
Collectively, 144 plus-sized models had 51 million followers, while the top 10 highest paid mainstream models averaged 38 million followers.
● Many Pain Medications Can Be Used for Spine-Related Pain in Older Adults
Spine-related pain is increasingly common in older adults. While medications play an important role in pain management, their use has limitations in geriatric patients due to reduced liver and kidney function, comorbid medical problems, and polypharmacy.

A new study finds acetaminophen is safe in older adults, but nonsteroidal anti-inflammatories (ibuprofen) may be more effective for spine-related pain. Nonsteroidal anti-inflammatories should be used
Collectively, 144 plussized models had 51 million followers, while the top 10 highest paid mainstream models averaged 38 million followers.
short-term in lower dose courses with gastrointestinal precaution while corticosteroids show the least evidence for treating nonspecific back pain.
Additionally, nerve pain medications (gabapentin and pregabalin) can be used in older persons, with caution to dose and kidney function. Newer antidepressants (duloxetine) more so than older ones (nortriptyline) can help with spine-related pain, with attention to possible sedation and dizziness. Some muscle relaxants (baclofen and tizanidine) can be used in older persons, again accounting for kidney and liver function. Opioids have limited use in common spine-related pain but can be used with caution in cases that don’t respond to treatment.
The mechanisms responsible for the underlying risk in human brain cell types have been unclear until now.
“Our findings provide a helpful medication guide for physicians to use for spine pain in an older population that can have a complex medical history,” explains study corresponding author Michael D. Perloff, MD, PhD, assistant professor of neurology.
● BU Researchers Untangle the APOE4 Gene, the Most Significant Genetic Risk Factor for Alzheimer’s Disease
Alzheimer’s disease is a progressive neurodegenerative disorder and the most common cause of dementia, affecting more than 5.8 million individuals in the US. Scientists have discovered some genetic variants, such as the APOE4 allele, increase the risk for developing Alzheimer’s; however, the mechanisms responsible for the underlying risk in human brain cell types have been unclear until now.
Researchers from the Chobanian & Avedisian School of Medicine have discovered two important novel aspects of the gene: 1) human genetic background inherited with APOE4 is unique to APOE4 patients, and 2) the mechanistic defects due to APOE4 are unique to human cells.
“Our study demonstrated what the APOE4 gene does and which brain cells get affected the most in humans by comparing human and mouse models. These are
important findings as we can find therapeutics if we understand how and where this risk gene is destroying our brain,” says study corresponding author Julia TCW, PhD, assistant professor of pharmacology & experimental therapeutics.
● Novel Gene for Alzheimer’s Disease in Women Identified
In a study published in Alzheimer’s Disease & Dementia: The Journal of the Alzheimer’s Association , researchers at the University of Chicago and Chobanian & Avedisian School of Medicine have identified a new gene called MGMT that increases the risk of Alzheimer’s in women.
The researchers conducted a genome-wide association study for Alzheimer’s in two independent datasets using different methods. One approach focused on dementia in a large extended family of
The researchers conducted a genome-wide association study for Alzheimer’s in two independent datasets using different methods.
Hutterites, a founder population of central European ancestry who settled in the Midwest region of the US. Hutterites are often studied for genetic determinants of disease because they have a relatively small gene pool due to their isolated, insular culture. In this study, the individuals with Alzheimer’s were all women. The second approach, predicated on evidence suggesting a link between Alzheimer’s and breast cancer, analyzed genetic data from a national group of 10,340 women who lacked APOE4 . In both datasets, MGMT was significantly associated with developing Alzheimer’s.
“This is one of a few and perhaps the strongest associations of a genetic risk factor for Alzheimer’s that is specific to women,” says Lindsay Farrer, PhD, chief of biomedical genetics and the study’s co–senior author.

They found that in the majority of young, healthy, and vaccinated adults, the infectious period for SARS-CoV-2 is limited, with only 17 percent remaining positive beyond five days.
● BU Researchers Examine the Infectious Periods in Vaccinated Individuals with SARSCoV-2 Omicron and Delta Variants
In January 2022, the US shifted its guidelines to recommend isolation of five days from COVID-19 symptom onset, followed by an additional five days of mask wearing.

To examine the infectious periods in vaccinated individuals with the SARS-CoV-2 Omicron and Delta variants, researchers from Chobanian & Avedisian School of Medicine collected daily anterior nasal swabs for at least 10 days from a group of college students and staff for reverse transcription-polymerase chain reaction (RT-PCR) test and culture and with antigen rapid diagnostic testing (RDT) on a subset of individuals.
They found that in the majority of young, healthy, and vaccinated adults, the infectious period for SARS-CoV-2 is limited, with only 17 percent remaining positive beyond five days.
“As isolation can have a significant impact on both the economy of a country and the mental health of its citizens, it is imperative to make efforts to reduce isolation periods while simultaneously preventing infectious individuals from spreading the disease,” explains study corresponding author Tara Bouton, MD, MPH, assistant professor of medicine. ●
giving
Scan for a complete list of BUSM’s FY22 donors.

FY22 Gifts from the Dean’s Advisory Board, Alumni, Faculty and Staff, Parents, and Friends
It is with appreciation that Boston University Chobanian & Avedisian School of Medicine recognizes our donors for their contributions this past year. Their generosity has supported the study and practice of medicine and research. We thank our donors and value the impact they have made on our school, our students, and our research.
DONOR REPORT Thank you, donors.
GIVING LEVELS:
$50,000–$99,999
Mercury members
• Invitation to the spring Chester S. Keefer, MD Society Dinner
• Honorary plaque
$100,000–$249,999
Bronze members
• All of the previously listed benefits
• Invitation to and preferred seating, when available, at select University and school events throughout the year
$250,000–$499,999
Silver members
• All of the previously listed benefits
• Personalized tour of research/ clinical area of your choice at BU Medical Campus
$500,000–$999,999
Gold members
• All of the previously listed benefits
• Direct communication with the recipients of your generosity (students, faculty, researchers)
$1,000,000+
Platinum members
• All of the previously listed benefits
• Private lunch with the Dean and other leadership of the School of Medicine
■ 2022 Donor
■ Deceased
■ New Keefer Member
This year, the FY22 (July 1, 2021, to June 30, 2022) Chobanian & Avedisian School of Medicine donor rosters are available online. In this issue, only the Dean’s Advisory Board and the Chester S. Keefer, MD Society are listed below. For a complete list of the FY22 donors, including all individual and foundation giving, please scan the QR code above or visit our website at bumc.bu.edu/busm/giving/who-gives.
The Chester S. Keefer, MD Society • The Chester S. Keefer, MD Society recognizes individuals whose personal philanthropy has helped advance the school by supporting the research and educational mission of Chobanian & Avedisian School of Medicine. The society is named in honor of Dr. Chester S. Keefer, a distinguished physician scientist who served as chairman of the Department of Medicine, dean of Boston University Chobanian & Avedisian School of Medicine, and director of the Medical Center. Dr. Keefer was responsible for laying the foundation for the center and, as the dean of the school, he established a tradition of cutting-edge research that continues to this day. In memory of Dr. Keefer, we honor the outstanding generosity of donors whose lifetime contributions to Chobanian & Avedisian School of Medicine have reached $50,000 or more.
PLATINUM
Joel J. Alpert ■ and Barbara W. Alpert (SPH’79)
Edward Avedisian (CFA’59,’61, Hon.’22) ■ and Pamela A. Avedisian (Hon.’22) ■
Merwyn Bagan (’62, SPH’95) and Carol J. Bagan
Nancy L. Bucher ■
Howard D. Buzzee ■
Shamim A. Dahod (CGS’76, CAS’78, CAMED’87) and Ashraf M. Dahod ■
Richard H. Egdahl ■ and Cynthia Taft (GRS’77) ■
Alan Gerry and Sandra Gerry
Jonathan P. Gertler (Questrom’99) and Jane R. Clark ■
Albert M. Ghassemian ■
Audrey & Martin Gruss Foundation
Lewis Heafitz and Ina B. Heafitz ■
Stephen R. Karp (CAS’63) and Jill E. Karp ■
Sarkis J. Kechejian (’63) ■
Stanley H. Konefal (’47) ■ and Catherine M. Konefal ■
Sherry M. Leventhal and Alan M. Leventhal (Hon.’09) ■
Inez Lopez ■
Frank J. Miselis (’45) ■ and Theodora T. Miselis ■
Carl A. Olsson (’63) and Mary D. Olsson
Peter T. Paul (Questrom’71) ■ ■
Jerome S. Serchuck and Joan S. Serchuck ■
Richard C. Shipley (Questrom’68,’72, Hon.’22)
Wesley R. Skinner ■ and Charlotte A. Skinner ■
Jack N. Spivack ■
Christine E. Stiefel ■
Helen L. Tarlow ■ and Sherwood J. Tarlow ■
Diane Tauber and Laszlo N. Tauber ■
GOLD
Norman W. Alpert and Jane D. Alpert
Karen H. Antman and Elliott Antman ■
Nancy Baler
Anita B. Barkan (CAS’46) ■ and Donald B. Barkan (’45) ■
George A. Finley III and Phyllis A. Finley
John L. Hall II (CAS’65) and Ann T. Hall
Rod F. Hochman (’79, CAS’79) and Nancy J. Hochman (Sargent’77,’83) ■
Paul F. Nace, Jr.
Joelyn L. Rohman and Michael Rohman (’50) ■ ■
Albert Rosenthaler and Debbie Rosenthaler ■
Paul Rothbaum and Jean Rothbaum ■
Elayne Russek
Thomas J. Ryan ■ and Nancy T. Ryan
Robert E. Schiesske (MET’78, Questrom’82) ■
Andrew Yee and Mirta Yee ■
SILVER
Erika Ebbel Angle (’12) and Colin Angle ■ William Y. Au (CAS’51, CAMED’55) and Beverly N. Au ■ ■
Donna R. Barnard (’65) and Douglas E. Barnard (’65) ■
Gerald Besson (’50) ■ and Eleanore S. Besson ■
Mary Ann Blount and James A. Blount, Jr.
Paul C. Burke and Gloria J. Burke ■
Helen L. Burr ■ and George Burr ■
David J. Caron and Susan M. Caron ■
Lin Castre and Abraham D. Gosman ■
Richard J. Cavell (’61) and Bonnie Cavell ■
Ann C. Cea (’67) and Anthony Tedeschi ■
Aram V. Chobanian (Hon.’06) and Jasmine Chobanian ■ ■
Andrew B. Crummy, Jr. (’55) and Elsa E. Crummy ■ ■
Elizabeth C. Dooling (’65) ■
Idea S. Fiering ■
Robert C. Green and Sally E. McNagny
Hideo H. Itabashi (CAS’49, CAMED’54) ■ and Yoko O. Itabashi ■
Donald M. Kaplan (’73) and Edna E. Kaplan (COM’88) ■
Reshma Kewalramani (’98, CAS’98) and Abhijit R. Kulkarni (ENG’93,’97) ■
Joseph J. Konefal (’77) and Karen G. Konefal ■
Lenore Larkin and Harold S. Larkin ■
Susan E. Leeman
Henry T. Lew (’62) and Winifred Lew ■ ■
Douglas N. MacInnis (’46) ■
Barry M. Manuel (CAS’54, CAMED’58) and Patricia D. Manuel (SON’78, Wheelock’86) ■
Rita Z. Mehos ■
Steven A. Miller (’70, CAS’70) and Jacqueline H. Miller (CAS’70)
Joseph B. Mizgerd and Ann F. Mizgerd ■ ■
John H. Nichols, Jr. ■
Simon C. Parisier (’61) and Elaine S. Parisier ■
Peter E. Pochi (’55) ■
Jeffrey D. Tripp and M. Douglass Poirier (CAS’73, CAMED’76)
Ronald L. Ragland (’82) ■
Alexander M. Rodger ■
Richard D. Scott and Mary Scott ■
DEAN’S ADVISORY BOARD
Erika Natalie Ebbel Angle, PhD (’12,’12) ■
Amin Ashrafzadeh, MD (CAS’93, CAMED’97) ■
Gabriella J. Avellino, MD (’09,’13)
John T. Avellino ■
Steven L. Berk, MD (’75) ■
H. Kim Bottomly, PhD ■
Elizabeth R. Brown, MD ■
Richard J. Catrambone, MD, DMD (’92) ■
Ann Christine Cea, MD (’67) ■
Harold N. Chefitz (CGS’53, COM’55) ■
Jane R. Clark, MD ■
Illaria Conti, MD, PhD
Suzanne Cutler, PhD (Questrom’61) ■
Shamim A. Dahod, MD (CGS’76, CAS’78, CAMED’87) ■
David R. Edelstein, MD (‘80) ■
Mary Jane R. England, MD (’64, Hon.’98) ■
Joseph S. Fastow, MD (’70) ■
Maurice R. Ferre, MD ( CGS’81, CAMED’92, SPH’92) ■
Dan R. Fishbein, MD (’85, CAS’85) ■
Jonathan P. Gertler, MD (Questrom’99) ■
Shahram S. Gholami, MD (’96) ■
Burton P. Golub, MD (’65) ■
Lewis Heafitz ■
Rod F. Hochman, MD (‘79, CAS‘79) ■
Christine Spitaels Hunter, MD (’80, CAS’80) ■
Jeffrey Robert Jay, MD (’83, CAS’83) ■
Donald Martin Kaplan, MD (’73) ■
Sarkis J. Kechejian, MD (’63) ■
Reshma Kewalramani, MD (‘98, CAS‘98) ■
Sherry M. Leventhal ■
Douglas M. Macdonald, PhD (GRS’92, CAMED’98) ■
J. Kenneth Menges, Jr., Esq (Questrom’79) ■
Simon C. Parisier, MD (’61) ■
Peter T. Paul (Questrom’71) ■
Terry R. Peel ■
Albert Rosenthaler ■
Pedram Salimpour, MD (’96,’00) ■
Robert William Schulze, MD (CAS’86, GRS’88, CAMED’92, Questrom’17) ■
Jerome S. Serchuck ■
Leslie Karen Serchuck, MD (’90) ■
Emily M. Wise Shanahan, MD (’09) ■
Richard C. Shipley (QUESTROM’68,’72)
Lee Bryan Silver, MD (’82, CAS’82) ■
Rachelle L. Silver ■
Louis Wade Sullivan, MD (’58, Hon.’90) ■
Patricia J. Williams, MD (CAS’84, CAMED’89)
■ FY22 Donor
New DAB Members in Italics
Lee B. Silver (’82, CAS’82) and Rachelle L. Silver ■ Sumner Stone (’58) and Martha Skinner ■
Louis W. Sullivan (’58, Hon.’90) and E. Ginger Sullivan ■
Mary U. Taylor ■
A. Raymond Tye (Questrom’47) ■
Martin L. Vogel (’53) and Phyllis M. Vogel ■
Arthur B. Wein (’39) ■
Madeline Wikler and Joseph M. Wikler ■
Deborah W. Wilson (GRS’72) and John Wilson ■
Amber Wong
Arnold Wong, Jr.
Jeremiah O. Young (’62) and Beverly A. Young ■
BRONZE
Anonymous (4) ■
Carmela R. Abraham and Menachem E. Abraham
Winston D. Alt (’80) and Deborah A. Gribbon ■
Rahul S. Anand (CAS’97, CAMED’01) and Meredith Anand ■ ■
Gerhard R. Andlinger ■ and Jeanne D. Andlinger
Michael L. Apuzzo (’65) ■
John T. Avellino and R. Ellen Avellino ■
Ruth M. Batson (Wheelock’76) ■
Robert M. Beazley ■
Melvin R. Berlin ■ and Randy L. Berlin
Jag Bhawan and Pratibha G. Bhawan ■
David G. Bradley and Katherine B. Bradley
Yvonne K. Brockman and Stanley K. Brockman (’55) ■ ■
Alan J. Brody ■
Elizabeth R. Brown ■
Richard J. Catrambone (’92) and Sophia Catrambone ■
Robert D. Champion and Marjorie Champion
Harold N. Chefitz (CGS’53, COM’55) and Charlotte M. Chefitz ■
Hsi-Pin Chen (CAS’89, SPH’91, CAMED’96,’96) and Kenneth E. Hancock (ENG’92,’01) ■
Yi-Chuan Ching (’58) and Helen Yu-Ching ■ ■
Michael J. Critelli and Joyce M. Critelli
Suzanne Cutler (Questrom’61) ■
Clare L. Dana (’69) ■ ■
Paul R. Dooling ■ and Sandra A. Danussi
E. Elaine Erbey (Wheelock’72)
Joseph S. Fastow (’70) and Ellen K. Fastow ■
Maurice R. Ferré (CGS’81, CAMED’92, SPH’92) and Maria D. Ferré ■
Joseph T. Ferrucci and Brenda Ferrucci
Samuel Finkielsztein and Gala Finkielsztein ■
Frederick L. Fox (’68) and Gail P. Fox ■
Charles N. Freed ■ and Marlene Freed
Patricia L. Freysinger (SON’82) ■
Ralph G. Ganick (’67, CAS’67) and Lois B. Ganick ■
Shahram S. Gholami (’96) and Neda Gholami ■
Godley Family Foundation
Burton P. Golub (’65) and Lee H. Golub ■
Malcolm Gordon (’48) ■ and Nan Miller ■
Donald J. Grande (’73) and Elena M. Grande ■
David T. Greenleaf (’65) and Katherine O. Greenleaf
Jack C. Guden ■
Haynes Family Foundation ■
Lea Highet and Ian Highet
Michael F. Holick and Sally A. Holick
Thomas R. Insel (CAS’72, CAMED’74, Hon.’20) and Deborah J. Insel (Wheelock’71) ■ ■
Jeffrey R. Jay (’83, CAS’83) and Mary Ellen A. Jay ■
Denise S. Katsaros (Wheelock’69) and Arthur T. Katsaros
Earl G. Kendrick, Jr. and Randy Kendrick
The Kessler Family
Nasir A. Khan ■
Elaine B. Kirshenbaum (CAS’71, Wheelock’72, SPH’79) ■ and Howard D. Kirshenbaum ■
Shirley P. Klein (’68, CAS’68) ■
Rose Ann Kornfeld and Lewis F. Kornfeld, Jr. ■
Lawrence E. Langsam (Questrom’57) and Hannah S. Langsam
Estella I. Leach ■
Patricia M. Leavitt (CAS’54,’58)
Richard S. Leghorn
Ruth R. Levine ■ and Martin J. Levine ■
Jodi Dome Linger and Nicholas T. Linger ■
Rita E. Loos ■
James H. Lowell II and Susan W. Lowell
The Estate of Lillian A. Luksis
Jules N. Manger (CGS’66) ■ and Janis G. Manger ■
Rocco S. Marino (’42) ■
Allan P. Markin and Patricia Markin
JoAnn McGrath
Robert B. Melikian (CGS’60, CAS’62) ■
Ruth A. Moorman (CAS’88, Wheelock’89,’09) and Sheldon N. Simon
Charles Mosesian ■
Peter J. Mozden (’53) ■
Carolann S. Najarian (’80) and K. George Najarian ■
John Noble ■ and Ewa Kuligowska
Wilson Nolen and Eliot Nolen
Zein E. Obagi and Samar A. Obagi
Paul I. Ossen (’43) ■
William Patty and Eliot Patty
Louise E. Penta and P. A. Penta (’51) ■
Carol C. Pohl (’67) and Alan L. Pohl ■
Theodore Polos (’47) and Jean Polos
Allen Questrom (Questrom’64, Hon.’15) and Kelli Questrom (Hon.’15)
Martin S. Rifkin (Questrom’82) and Judy A. Rifkin ■
Elihu Rose and Susan W. Rose
Doris M. Russell and Robert F. Russell (’46) ■ ■
David J. Salant and Anne Salant ■ ■
Paulette Samowitz ■
The Schulze Family ■
Charles L. Schwager (Questrom’66) and Evelyn C. Schwager (Questrom’66)
Richard Seeborg
Florence Seldin ■ and Ira L. Seldin ■
Leslie K. Serchuck (’90) ■
Muriel Shapiro and Arnold Shapiro ■
Stuart E. Siegel (’67, CAS’67) ■
John Silber (Hon.’95) ■ and
Kathryn U. Silber (Hon.’01) ■
Charles W. Smith and Hazel Smith ■
Gordon L. Snider ■
Edward Spindell (’53) ■ and Judith K. Spindell
Eliot B. Stewart and John M. Stewart ■
Elliott H. Sweetser (’43) ■ and Aileen B. Sweetser ■
Nevart Talanian
Gloria P. Talis ■ and George J. Talis (’50) ■
Alfred I. Tauber and Paula Fredriksen
Gerald Treece and Patricia Treece
Yolande Tsampalieros and Gabriel Tsampalieros ■
Burton White (’61) and June S. White ■
Marcelle M. Willock (Questrom’89) ■ ■
Henry R. Wolfe (’45) ■ and Grace A. Wolfe ■
Herbert H. Wotiz ■
Sam S. Wu (CAS’87, GRS’90, CAMED’92, SPH’92) and Patricia C. Tsang (’92, CAS’92, GRS’92)
Lawrence A. Yannuzzi (’64) and Julie Yannuzzi ■
Larry C. Young and Sue Young ■
Lily M. Young (’65) and John G. Johansson ■
The Family of Alan Ziskind ■
MERCURY
Anonymous (3) ■ ■
Lawrence D. Ackman and Ronnie Ackman
Noubar B. Afeyan and Anna Afeyan
Gerald Ajemian and Lucille Ajemian
Dwight M. Akers (’53) ■ and Beverly R. Akers ■
Max M. April (CAS’81, CAMED’85) and Pamela T. April (Questrom’83)
Steven Baker ■ and Shirley Baker ■
Elizabeth D. Barnett (’85) and Suleiman N. Mustafa-Kutana ■
Paul C. Barsam (STH’52) and Joyce L. Barsam
Howard C. Beane (’57) ■ and Shirley T. Beane
John H. Bechtel (’50) ■ and Shirley F. Bechtel
Franklyn D. Berry (’41) ■
David W. Bishop (’46) ■
Elsa C. Bodon (’41) ■
James F. Bopp, Jr. ■
S. Arthur Boruchoff (’51) ■ and Anna Silverman-Boruchoff (’49) ■
Robert A. Cameron ■
Robert J. Carey (’54) ■ and Mary E. Carey (Wheelock’55)
Russell K. Carney and Geraldine Carney ■
Lisa B. Caruso (SPH’99) ■ ■
Edmond E. Charrette (’62) and Maria T. Charrette ■
Jeremy Chess (’70, CAS’70)
David J. Chronley (’74) and Marianne K. Chronley
Frank Citrone, Jr. and Carol Citrone
John P. Cloherty (’62) ■
John F. Cogan, Jr. ■ and Mary L. Cornille (GRS’87)
Alan S. Cohen (’52) ■ and Joan P. Cohen
Patricia A. Connolly (’84) ■
Marian M. Cook
Ronald B. Corley and Janice Corley ■
Sidney Covich ■
Brit D’Arbeloff and Alexander V. D’Arbeloff ■
R. Gordon Darby ■
David P. DiChiara (CAS’80, CAMED’84) and Maria J. DiChiara ■ ■
Paul E. Dixon, Jr. and Rebecca K. Dixon ■
Thomas J. Dowling, Jr. (’81, CAS’81) and Rosemary Dowling
Hilda R. Dressler (’34) ■
Carol A. Dyer and Gene Gordon (’46) ■
Alan M. Edelstein (Questrom’47, LAW’49) ■ and Sybil Edelstein
David R. Edelstein (’80) and Eve L. Edelstein ■
Alvin N. Eden (’52) and Elaine R. Eden ■ ■
Mary Jane R. England (’64, Hon.’98) ■
Michael J. Esposito (’49) ■
Geraldine L. Feldman (’69, CAS’69) ■
Judith N. Feldman
I. Howard Fine (’66) and Victoria Fine ■ ■
Bertha Offenbach Fineberg (’36) ■ and Nathan L. Fineberg (’30) ■
Nicholas J. Fiumara (’39) ■
Daphne H. Foster (CAS’79, Questrom’82) and Lawrence Foster
Beverly R. Franklin (CAS’44) ■ and William E. Franklin (’46) ■
Myrna Franzblau (Wheelock’73) and Carl Franzblau
Monte Friedkin and Skeets Friedkin
Ronald S. Gabriel (’63) and Pamela Hobbs ■ ■
Ray A. Garver ■ and Donna L. Garver ■
Marion L. Gendron (PAL’26) ■
George E. Ghareeb (’62) ■ and Nancy B. Ghareeb
Arnold Goldenberg (’54) and Gloria Goldenberg ■
Dorothy A. Gottlieb (CAS’76) and Leonard S. Gottlieb ■
Doris Grabosky and Jack Grabosky
Ellen R. Grass ■
Robert E. Griffin and Cathleen Griffin
Morton S. Grossman (MET’42) ■ and Sylvia Grossman ■
Kenneth M. Grundfast and Ruthanne Grundfast
Fritz Grunebaum (Hon.’79) ■
Robert W. Healy (’67) and Bonnie M. Healy ■
Juan D. Hernandez Batista ■ and Maria A. Tavarez-De Hernandez
Arnold S. Hiatt
George L. Hines (’69, CAS’69) and Helene A. Hines (Sargent’69) ■
Ann S. Hintlian ■ and Deran Hintlian
Michael G. Hirsh (’63) ■ and Carol N. Hirsh
Marvin J. Hoffman (’47) ■ ■
Betsy E. Horen ■
Arline Housman ■ and Herbert E. Houseman ■
Charles Housman
Edward L. Housman (Questrom’42) ■ and Charlotte Housman ■
James B. Howell (’65) and Marlene A. Howell
Bernard L. Huang (CAS’57, CAMED’62) ■ and Ann M. Huang
Richard E. Hunter (’44) ■ and Minta L. Hunter ■
David Ingall (CAS’52, GRS’53, CAMED’57) and Carol Ingall
Patricia K. Issarescu (’61) ■
Joseph A. Izzi, Sr. and Barbara A. Izzi
Peter F. Jeffries (’60) ■ and Jeanne F. Arnold (’61) ■
Clinton W. Josey, Jr. and Betty Josey ■
Lori A. Jurado and Xavier Jurado ■ ■
Esther B. Kahn (Wheelock’55, Hon.’86) ■
Charlotte A. Kaitz ■ and Louis L. Kaitz ■
Damon J. Keith ■
The Kibrick Family
Burton I. Korelitz (’51) ■ and Ann Z. Korelitz
Conan Kornetsky ■
Bernard E. Kreger ■ ■
Edward E. Krukonis (’63) and Priscilla J. Krukonis ■
Saul Kurlat ■
Cecelia Lance ■
Charna C. Larkin and Alan B. Larkin ■
Robert E. Leach and Laurine Leach
Brian Levine and Beth Levine
Brigette Lonner and Joseph J. Lonner ■
Thomas A. MacLean (’64) and Colleen K. MacLean ■
William I. Malamud (’54) ■ and Camille C. Malamud ■
William M. Manger and Lynn S. Manger
Richard C. Marcus
Stella C. Martin and Clive R. Martin
Ronald P. McCaffrey and Maureen McCaffrey
John F. McCahan and Kathleen B. McCahan ■ ■
Edward J. McDonald, Jr. and Catherine A. McDonald
Hubert W. McDonald and Ann S. McDonald ■ ■
Jean E. McPhail ■
Robert F. Meenan (’72, Questrom’89) ■
Mark S. Michelman (’67) and Susan F. Michelman ■ ■
Daniel E. Moalli (’61) and Glenna M. Moalli ■
Jordan Monocandilos
Rodney A. Montag and Sally A. Montag
Sanford R. Montag and Nancy L. Montag
Thomas J. Moore and Mary C. Moore ■
Sunit Mukherjee (’89, CAS’89) and Sumeeta Mukherjee
Michael F. Mullarkey (’70) and Dawn Mullarkey (CAS’68)
G. Vijaya Naidu
Sonya Nersessian (LAW’85) and Richard K. Babayan ■
Newton Family Fund
Merel G. Nissenberg
Dawn B. Norcia and David J. Norcia
N. Stephen Ober (CAS’82, CAMED’86)
John F. O’Brien (’59) ■ ■
Anne W. O’Connor and John F. O’Connor (’57) ■
Hytho H. Pantazelos (’63) and Peter G. Pantazelos ■ ■
Dianne M. Parrotte (’79, CAS’79)
Edward F. Parsons (’65) ■
Jordan C. Paul and Valerie J. Paul ■
Lita Perkins ■ and John S. Perkins ■
Jona A. Perlmutter and Donna Perlmutter
Astrid O. Peterson (CAS’74, CAMED’77)
N. Neal Pike (LAW’37) ■
John I. Polk (’74, Wheelock’13) and Mary C. Nugent Polk (SON’76,’77) ■
Helen S. Ratner ■ and Frank Ratner (’47) ■
Iver S. Ravin (’40) ■
Nancy E. Rice (’65) and Millard J. Hyland ■
Joel A. Roffman (CAS’72, CAMED’75) and Nancy C. Roffman ■
Gerald L. Ross ■
Melanie Rothbaum and David Rothbaum (’82) ■
Richard A. Rudders ■
Stephen W. Russell (’55) and Gail D. Russell
Ralph L. Sacco (’83) and Scott Dutcher ■
Pedram Salimpour (’96,’00) and Stacy Weiss ■ ■
Hannah E. Sandson and John I. Sandson ■ Francis P. Saunders (’58) and Lydia M. Saunders
Frank J. Schaberg, Jr. (’68, CAS’68) and Monica J. Schaberg (’68, CAS’68) ■
Alan L. Schechter (’78) and Genevieve Schechter
Harold S. Schell (’70) and Antoinette M. Schell ■
Rocco Schelzi ■
Herman Selinsky (’24) ■
Richard J. Shemin (CAS’72, CAMED’74) and Susan H. Shemin
Norton L. Sherman ■ and Claire M. Sherman
William F. Shields (GRS’90, CAMED’94) ■
The Shooshan Family ■
Barry E. Sieger (’68) and Margarete Sieger ■
Richard L. Simmons (’59) ■
Simon L. Strong (ENG’79, Questrom’91) and Sarah A. Strong
Lois N. Talis (PAL’49) ■
Tony Y. Tannoury and Viviane Tannoury
Stephen M. Tringale (CAS’80, GRS’86, CAMED’90) ■
Sanford W. Udis (’44) ■
Marian A. Vita ■
Franz Waldeck ■
Carl W. Walter ■ and Margaret H. Walter ■
Murray Weinstock (’65) and Gloria Weinstock
Sue Rosenwasser Weiss and Seymour Rosenwasser ■
Anthony Weldon
Judith F. Wellington and Peter S. Wellington ■
Jerrold Wexler and Joan Wexler
Robert H. Wexler ■ and Joanna B. Wexler ■
Alan Winters and Hope Winters
Robert A. Witzburg (’77) and Lorraine G. Witzburg (Wheelock’06) ■
Peak Woo (’78, CAS’78) ■
Earle G. Woodman (’58) ■
Moshe Yanai and Rachel Yanai
Charles R. Young ■ and Marion L. Young ■
Frances W. Young ■
Barry S. Zuckerman and Pamela A. Zuckerman
HONORARY
Dorothy C. Keefer (PAL’46,’48) ■
Ishebel K. Lyle ■ and Carl Lyle ■
David Coleman’s Legacy of Endowed Professorships
$26 MILLION IN ENDOWMENTS KEY TO ATTRACTING, RETAINING TOP FACULTY
Retiring from Boston University after 16 years as chair of the department of medicine at the Chobanian & Avedisian School of Medicine and physician-in-chief at Boston Medical Center, David Coleman, MD, leaves a legacy of nine endowed professorships—supported by more than $26 million— created during his tenure.

“If you told me 10 years ago that our department would create nine new endowed professorships using departmental funds and donations . . . I would have been very, very surprised,” says Coleman.
Endowed professorships are the highest academic award bestowed on a faculty member and a key tool in attracting and retaining top-flight faculty, offering both prestige and a steady source of additional funding to be used for salaries, research programs, or both, depending on how the use of the money is structured.
“Most of the people who have endowed professorships are individuals who are active researchers,” says Coleman. “There are a relatively small number of truly outstanding investigators . . . and recruiting and retaining them is extremely competitive and very challenging.
“We had, what was for me, a very large deficit in the number of endowed professorships when I arrived in 2006,” he says. “So, our strategic goal was to change that.”
Coleman says the department had sufficient reserves to support an aggressive investment strategy. A very favorable stock market over the past decade resulted in $22.5 million for endowed professorships. Private donations accounted for $3.5 million of the $26 million funding the nine positions.
Endowed professorships are managed so that the principal remains largely intact, and funding can continue in perpetuity.
Each year, the University determines what percentage of the endowment to distribute to recipients. Coleman says that amount has been around four percent of the corpus of the endowment, or approximately $100,000 on a $2.5 million professorship.
“The real benefit is that, over the long term, this department will always be able to bestow these professorships in addition to the endowed professorships that were created through other philanthropic sources,” Coleman says. “Endowed professorships are a very important source of stability and excellence for the department, and ultimately for the school and University.”
The school has honored Coleman by establishing the David Coleman, MD, Junior Faculty Prize to recognize junior faculty
members in the department who exemplify excellence in research and good citizenship through volunteer leadership, educational initiatives, and commitment to diversity. Thus far, there have been more than $53,000 in donations toward a $100,000 goal.
“The award is very meaningful and flattering and is very congruent with my own values—namely, recognizing and rewarding individuals with important accomplishments and great promise for the future,” he says. ●
G. Levinsky, MD, Professorship in Nephrology
Franz J. Ingelfinger, MD, Professorship in Gastroenterology
John Noble, MD, Professorship in General Internal Medicine
Joseph A. Vita, MD, Professorship in Cardiovascular Medicine
Barbara E. Corkey, PhD, Professorship in Medicine
Jerome S. Brody, MD, Professorship in Pulmonary Medicine
Louis W. Sullivan, MD, Professorship in Medicine
David J. Salant, MD, Professorship in Nephrology
Sushrut Walker, MD* 2016
Currently Vacant** 2017
Jeffery H. Samet, MD, MA, MPH 2017
Naomi M. Hamburg, MD, MS, FACC 2018
Katya Ravid, DSc 2021
Joseph P. Mizgerd, ScD 2021
Sabrina Assoumou, MD, MPH 2021
Laurence H. Beck, MD, PhD 2022
Total Endowment $26 million***
Sources: Chobanian & Avedisian School of Medicine Development and David L. Coleman, MD
*Inaugural chair was David Salant, MD
**Previously held by Hemant K. Roy, MD
***Each endowment is $2.5 million
Two additional professorships were created during Coleman’s tenure as department chair: the Alan S. Cohen Professor of Rheumatology (with $2.5 million from an existing endowed professorship, currently held by Tuhina Neogi, MD, PhD); and the Gitta and Saul Kurlat Chair in Hematology/Oncology (with a $2.5 million donation from the Kurlat estate; recipient to be named in 2023).
Endowed professorships are managed so that the principal remains largely intact, and funding can continue in perpetuity.
● Mac Parkman Foundation Funds Brain Injury Research in Young Athletes
The Mac Parkman Foundation has committed $258,000 to William Fairfield Warren Distinguished Professor and Professor of Neurology and Pathology Ann McKee, MD, to study changes in the brains and neuropsychiatry of young contact sport athletes.
In collaboration with John Crary, MD, PhD, at the Icahn School of Medicine at Mount Sinai, the research team will investigate white matter degeneration and corresponding disturbances—such as behavioral changes, depression, and suicidality—in the brains of 150 deceased contact sports athletes between ages 17 and 45.
Through this project, the McKee/ Crary team will apply a novel machinelearning computational approach to digital pathology images from young athletes who experienced repetitive head impacts (RHI) and compare findings to those of young individuals not exposed to RHI. “This work,” says McKee, “aims to help explain how white matter changes arising from repetitive head impacts lead to serious morbidity, including death. It has the potential to dramatically alter the way American football is played and neuropsychiatric illness is diagnosed.”
The Mac Parkman Foundation was established by the family of Mac Parkman, a football player and wrestler who died by suicide at age 17 in 2020. After his death, his family donated his brain for study by McKee, who confirmed brain pathology consistent with her findings in older athletes. Mac’s father, Bruce Parkman, wants other parents to know the risks their children face by participating in sports that involve repetitive hits to the head. “Our family didn’t know that these sports were literally killing Mac,” says Parkman. “We’re supporting this research so others don’t need to suffer the way he did— and so other families have information about the risks of certain sports. We truly believe this research will save lives.”
● Chan Zuckerburg Funds Initiative to Improve SingleCell Genomic Data
Joshua Campbell, PhD, assistant professor of computational biomedicine, has been
awarded a $200,000 grant from the Chan Zuckerberg Initiative. With this support, he will develop methods and software to improve the quality of single-cell genomic data.
Single-cell technologies can generate intricate data on complex biological systems. Although they have many advantages, the insights gained from this data can be hindered by different types of noise, such as contamination that comes from dead or dying cells. With support from this grant, Campbell will develop novel statistical approaches for estimating and removing contamination from single-cell data modalities, such as RNA-seq, ATAC-seq, and CITE-seq. He also will extend software that allows for benchmarking and comparisons between different decontamination tools.
Campbell plans to make these algorithms and tools available online, enabling noncomputational users to easily run and evaluate decontamination tools on their own data. “This work will enhance the ability of researchers to gain meaningful insights from their single-cell data, even in cases where higher levels of contamination are present,” he says.
● Alex’s Lemonade Stand Foundation Funds Cancer Research in Pediatric Neuroblastoma
Hui Feng, MD, PhD, associate professor of pharmacology & experimental therapeutics, has been awarded a $250,000 Innovation Grant from Alex’s Lemonade Stand Foundation (ALSF).
ALSF’s Innovation Grant program supports research likely to have a significant and sustained impact on the childhood cancer research field. With this support, Feng will investigate why MYCN-driven cancers are aggressive and treatmentresistant in the context of neuroblastoma.
Children with high-risk neuroblastoma often have extra copies of MYCN, which can result in increased disease aggression and a less-than-50-percent survival rate. Combining analysis of human patient samples and in-vitro cell culture systems with an innovative zebrafish model, Feng has found that T regulatory cells are enriched into the tumor microenvironment
to suppress anti-tumor immune responses and promote tumor aggression in MYCNdriven neuroblastoma. In this project, Feng will shed light on the underlying mechanisms and evaluate available drugs for improved treatment.
“This study could uncover effective drugs for treating high-risk neuroblastoma and perhaps other types of MYCN-driven pediatric cancers,” says Feng. “These treatments could be much less toxic than chemotherapy and radiation for children.”
● American Heart Association Supports Continued Research on Racial Disparities
Katya Ravid, DSc, Barbara E. Corkey Professor of Medicine, received a grant from the American Heart Association to study cardiovascular complications, as influenced by health inequities, in breast and prostate cancer survivors.
Cardiovascular disease is the leading cause of death in cancer survivors who haven’t experienced recurrence, and Black survivors of breast and prostate cancers appear to be at disproportionately higher risk for heart damage.
Ravid and her research team hypothesize that this disparity is at least partially due to “allostatic load”—broadly defined as the biological burden of chronic stress attributed to socioeconomic conditions and other stressors and associated with worse health outcomes.
Using a large dataset, Ravid and her collaborators, who include researchers from VA Boston Healthcare and Boston Medical Center (including Chobanian & Avedisian School of Medicine Associate Professor Vipul Chitalia, MD, PhD), will investigate impacts of well-defined parameters of allostatic load on various manifestations of cardiovascular disease in breast and prostate cancer survivors across racial groups. They also will compare intensity of allostatic load with biological response to cancer treatment. “This study,” says Ravid, “will help us understand why some populations of cancer survivors disproportionately endure cardiovascular complications—and how we may be able to prevent or lessen disease.” ●
alumni news
Greetings,
LAST FALL, WE EXPERIENCED A HISTORICAL PHILANTHROPIC COMMITMENT from the Avedisian family to the school, a momentous gift born from a lifelong friendship and decades of connection to Boston University. Their extraordinary generosity will have a long-lasting impact for which we are eternally grateful.
The naming event in September kicked off the return of in-person class reunions, during which we welcomed alumni home for the first time in two years. It was wonderful for current students to hear the Class of 1972 and others reflect on their days as students, and for students to provide glimpses of med school today.
As we continue to move forward, we are learning how best to support alumni, student engagement, and meaningful on-campus activities. We are exploring ways that work for YOU. What medical school affinity resonates with you—Pathway?
Class year? Professional affinity? Please take a moment to share your thoughts by simply scanning the QR code below for our survey. Your feedback will help direct how the Alumni Association reconnects you with classmates, other graduates, and current students.

We are well into celebrating our 175th Anniversary! On the following pages you will read the stories of four alumni who have a few things in common, including receiving the Chobanian & Avedisian School of Medicine Distinguished Alumni Award. We learn that what brought them to BU—a passion for medicine and public service—has never wavered, and that the word “retirement” may be defined differently than some may imagine.
Whose story would you like to feature as part of our 175th anniversary celebration? We seek the rising star who is actively championing to improve health and medicine, the one who opted for a nontraditional pathway, and the seasoned professional who left their mark in the world of science and medicine decades ago—and left us all better for it. Each of us has a story. You have a story. Please share!
As always, we greatly appreciate your insights and your steady connection.
Sincerely,
Alumni
Weekend Features Reunions, Dining, Reflection
Alumni Weekend opened on Thursday, September 29, with the surprise announcement of the transformational $100 million gift to the medical school and its formal renaming as the Aram V. Chobanian & Edward Avedisian School of Medicine.
The backstory is especially heartwarming, with Avedisian (CFA’59,’61, Hon.’22), a longtime clarinetist with the Boston Pops and Boston Ballet orchestra and a savvy investor, making the donation to honor his longtime childhood friend Chobanian (Hon.’06), a noted cardiologist, former medical school dean, and University president emeritus.
Friday featured an insightful panel discussion and the Distinguished Alumni Awards luncheon, honoring this year’s recipients Drew Weissman, MD, PhD (’87, GRS’87), Roberts Family Professor of Vaccine Research at the University of Pennsylvania’s Perelman School of Medicine; Gail D’Onofrio, MD, MS (’87), Albert E. Kent Professor of Emergency Medicine at Yale School of Medicine; and Daniel Rotrosen, MD (’78), director of the division of allergy, immunology and transplantation at the National Institute of Allergy and Infectious Diseases (NIAID).
Heather Miselis, MD, MPH (’00,’04, SPH’00)
 Assistant Dean for Alumni Affairs
Assistant Dean for Alumni Affairs
Held in Keefer Auditorium and also livestreamed, the morning panel discussion with the three award recipients was co-moderated by Assistant Dean for Alumni Affairs Heather Miselis, MD, MPH (’00,’04, SPH’00) and Alumni Association President Amin Ashrafzadeh, MD (CAS’93,
CAMED’97). With two immunologists on the panel, the conversation naturally gravitated toward COVID-19. Weissman was optimistic about the applications of nucleoside-modified messenger RNA platforms.
“It’s going to be applied to a huge number of vaccines,” he said. It was already employed for vaccines headed to human clinical trials for HIV, influenza, and genital herpes, and to develop vaccines targeting noroviruses and malaria.
But it’s also being used for gene therapy, especially in connection with sickle cell anemia.
“What we’re developing will be a single injection that will target the bone marrow and cure the disease,” he told the audience.
Rotrosen said COVID made his agency pivot from mouse to human immunological trials wherever possible. “That set us up for this explosion of research and important findings . . . on how the human immune system works,” he said.
D’Onofrio’s work targets the opioid crisis’ impact on emergency rooms.
“There isn’t any other disease that causes so much death in the emergency room. Probably having a huge heart attack is the only thing that comes close,” D’Onofrio said. Her goals include changing national policies on opioids and introducing new interventions.
“The pandemic has really made all substance abuse disorders go out of control,” she said. “More people are using more drugs and more people are vulnerable than ever before.”
COVID-19 worsened an already escalating opioid crisis. One of the big questions for D’Onofrio is why so many people forgo treatment following a non-fatal overdose, despite statistics showing that five percent of overdose survivors die within a year and would have a much higher survival rate with treatment.
COVID-19 also exposed weaknesses in healthcare, exacerbating existing inequities in treatment and accessibility for marginalized populations. These inequities were something all three panelists witnessed during their medical school training and clinical rotations at the school’s primary teaching affiliate Boston Medical Center (then known as Boston City Hospital, or BCH).
“Equity has always been important and a driving force in my career,” said Weissman.
D’Onofrio said her exposure to urban healthcare through her medical school training and clinical work at BCH was the foundation of her life work addressing addiction and substance use as underlying causes for the emergency room caseload.

“You couldn’t have had better training than we had,” she said.
“I learned so much from the patients,” said Rotrosen, who appreciated that the medical
school and hospital encouraged students to participate in patient care. His medical school experience of traveling with physicians to see geriatric patients in their homes moved him, he said.
That experience stuck with him through his career at NIAID, which has an asthma program where physicians do home visits.
“Children, women, in urban areas suffer disproportionately from asthma and we’ve made major advances in our understanding, not just of the biology but of the socioeconomic demographic factors,” Rotrosen said.
The luncheon celebrated the many accomplishments of the award recipients. Each was introduced by Alumni Association President Ashrafzadeh and presented with a crystal pyramid engraved with their name.

At the luncheon’s conclusion, Heidi Abdelhady, MD (’98), was introduced as the incoming alumni association president.
“I’m grateful for this opportunity,” Abdelhady said. “I’m humbled by this community as I look at the alumni in this room. I can’t say it enough that my mind is absolutely blown by the three people (D’Onofrio, Weissman, Rotrosen) getting awards today. They not only contributed to science but they actually changed our lives for the better.
“I’m excited for the year ahead.”
Other special alumni events included reunion dinners, including the Class of 1972 50th Reunion Dinner, and tours of campus landmarks, like the new Instructional building team-based Learning Center on L4 and the newly renovated Gross Anatomy Lab. ●
ALUMNI STORIES
Mary Jane England (’64, Hon.’98)
Medicine runs in Mary Jane England’s blood. Her mother was a nurse, and England graduated from Boston University with her MD in 1964. Her son Thomas graduated from her alma mater in 2014 and her daughter Alexandra graduated from the School of Public Health in 2010.
England’s mother pushed her to become a doctor rather than a nurse. “My mother felt that if I was really interested in medicine, I should become a physician,” England says. “She felt that physicians had more authority and training and because of that, could effect more change.”
Always interested in using her medical training to help women, whom she believed were mistreated by healthcare providers, England—originally a psychiatrist—planned to go into gynecology. Then, “The more I looked into the issues women were grappling with, I found they were mental health issues,” she recalls. “When the mother is depressed, it’s not just impacting her, it’s impacting the whole family. That’s been the theme of my life—really looking at kids and families, and how we can improve services for them.”
In 2009, England chaired the Institute of Medicine’s committee on parental depression.
During her time at the school, England focused on the role of women, who made up less than 10 percent of students enrolled. She valued the support of female mentors, especially in psychiatry, and became involved with the American Medical Women’s Association (AMWA) during medical school. In 2004, the association awarded her the Elizabeth Blackwell medal, which celebrates female physicians who make outstanding contributions to the cause of women in the field. The following year, she was elected president of the AMWA.

England met her husband, Robert England (’64), while in medical school. By her third year of studies, she had her first child and upon completing her residency, she and
her husband, also a medical student, had two more. “It was a juggling act,” England remembers. Despite having to balance her course load and hospital responsibilities with raising three young children, England was certain that she was “in the right place and doing the right thing.”
learned was the importance of the whole person.”
Her father was a Boston police officer; her daughter Kara is a Massachusetts State Police captain. Her commitment to public service is a key factor in England’s career and has always guided her professionally. In 1979, she became the first commissioner of the Massachusetts Department of Social Services. “Starting a brand-new agency is tough,” she admits. She strived to provide families with the tools to stay together. “I felt we needed to support the families with social services, housing, and daycare.” She also brought in a fellow psychiatrist to work in the department, combining social services with mental health support.
Decreasing stigma around mental illness is another priority. She was a member of a steering committee for Advancing Care Together, a four-year program designed to bring mental health services to rural Colorado, and also worked on former first lady Rosalynn Carter’s mental health task force. “We have trouble recognizing that we might have a mental illness,” England says. “It’s easier to say I have a condition, or migraines, or something else, but to say and recognize that we might have a mental illness is just hard.”
From 2001 to 2011, England served as president of Regis College, her alma mater, building graduate programs with a focus on nursing and health sciences.
Medical school taught her to look at patients holistically. “It was more than just medicine,” she says, recalling going to housing projects in Roxbury to deliver healthcare, where she ended up cooking oatmeal and changing diapers for a mother. “In those days, we didn’t have disposable diapers. We had to wash them by hand. So, I kind of showed the patient how to be a mom. I think one of the things we
England’s connection to BU remains strong. She received an honorary degree from BU in 1998 and returned as a professor at the School of Public Health, where she conducted a review of mental health services on the Medical Campus. She is also a member of the Chobanian & Avedisian Dean’s Advisory Board. “Dean Antman is a role model for so many women—and men, too,” she says.
England tells young women in medicine to take up space in the medical field. “Never say no to the opportunity to get involved in things,” she advises. “Your view of the world is very important.” ●
England’s connection to BU remains strong. She received an honorary degree from BU in 1998 and returned as a professor at the School of Public Health, where she conducted a review of mental health services on the Medical Campus.
ALUMNI STORIES
Thomas Insel (’74, Hon.’20)
Thomas Insel, MD, says that over his lifetime he’s had five different careers—and the self-described mental health entrepreneur, father, and grandfather has no intention of retiring. “I don’t even know what that means at this point,” he jokes.

His father, an ophthalmologist, believed medical school was a “basic education that everybody needed to do,” Insel says. But the future neuroscientist wasn’t sure he wanted to pursue medicine until, at 18 years old, he traveled to work in the clinics and hospitals of South Asia.
His experiences convinced him that medicine was worthwhile. “Being on the front lines, having babies die in my arms with tetanus, or seeing young people die from snakebites—looking back, it’s incredible to think about these sorts of problems for an 18-yearold,” Insel reflects. “But I came out of it feeling like this was something I wanted to be a part of. This was something really important.”
Insel originally planned to pursue tropical medicine, which he practiced during his travels. But he was drawn to mental health and neuroscience at the school. “I wanted to help people where the suffering was the greatest,” he explains. “It originally seemed to me that was in the parts of the world that were the most impoverished. Then, in medical school, I discovered the profound suffering in the world of mental illness.”
Insel’s research, conducted at the National Institute of Mental Health (NIMH), focused on the neuropeptides oxytocin and vasopressin and their role in social behavior. After 15 years at NIMH, Insel left the institute for Emory University, where he founded the Center for Behavioral Neuroscience. Ansel and his Emory team founded a new field of neuroscience, social neuroscience, that investigates how brain chemistry and systems affect social behavior. The Center for Behavioral Neuroscience brought together students and faculty from several universities
in the area, including Georgia Tech, Georgia State, Morehouse, Spelman, and Morehouse School of Medicine, to conduct research. “That was a blast,” Insel recalls. “We had some really great faculty from all these different institutions who came together, and
Insel left the NIH to start working in Silicon Valley at Alphabet’s health company, Verily (originally Google Life Sciences). “I left the NIH partly because I thought there was so much going on in the technology industry to change the way that goods and services were getting delivered,” he says. “It felt like we needed to do something disruptive in mental health care.”
After a year, Insel left Verily to join the mental health tech startup Mindstrong as president and cofounder, and would later cofound Humanest, an online mental health community and resource for college students. Tech, Insel says, has the potential to bring objective diagnostics into the often-subjective world of therapy. “We tend to base our diagnostics and treatments on measurements. We measure blood pressure. We measure blood sugar. We measure a whole range of factors that let us know whether someone’s getting better or not.
“But in mental health care, there’s nothing objective. I kept wondering whether we could use objective measures because we have all these new technologies that are so good at capturing how we think, feel, and behave. Sometimes they know more about us than we know about ourselves.”
we had students going back and forth. Our paths never would have crossed if not for this shared interest.”
After eight years in research at Emory, Insel turned to mental health policy. He returned to the National Institutes of Health (NIH)—but this time as director of the NIMH. He notes that mental health had often been ignored in public policy settings, and that raising awareness was key: “Mental illness is often grossly misunderstood, and either neglected, or worse than neglected, people with mental illness are actually inappropriately channeled into the criminal justice system or into homelessness and poverty. So, it’s really important for people to understand mental illness.”
Humanest, which is tailored to digitally savvy 20-somethings, has seen improved engagement with mental health resources, and was preferred to traditional one-onone care.
Insel’s newest career is journalism. Last year, he co-founded MindSite News, an online news organization dedicated to mental health coverage. He is also a book author and has published Healing: Our Path from Mental Illness to Mental Health, which investigates solutions to mental health infrastructure around the world. “I’ve always been so excited about science,” he says. “Now I’m excited about issues of service and how we can do better for people with mental illness.” ●
He notes that mental health had often been ignored in public policy settings, and that raising awareness was key.
Robert Jackler (’79) ALUMNI STORIES
“There’s a difference, in personal relationships, between falling in love and being in love,” says Robert
Jackler,MD, the Sewall
Professor of Otolaryngology—Head &Neck Surgery and Neurosurgery at Stanford University. “The first being easier than the second.”
He’s not talking about people but reminiscing about his decades-long relationship with the field of otolaryngology. When the surgeon was deciding on an area of study, he wanted to pick a specialty that other surgeons not only fell in love with, but also stayed in love with.
Decades later, he’s still in love with the field.
“I got really very fascinated by the fact that otolaryngology had to do with human communication—hearing and voice,” Jackler explains. “And, when you think about it, what is more essential to the nature of being human?”
Jackler received his medical degree from Boston University in 1979. However, his experience in medicine goes back to childhood, when he would accompany his cardiologist father on hospital rounds. A World War II veteran and Chobanian & Avedisian graduate, Jackler’s father brought him to various hospitals in his hometown of Waterville, Maine. “The nurses would absolutely dote on me,” Jackler recalls.
His father died in his 30s, when the future surgeon was only 9 years old. Despite the financial and personal struggles his family endured after this tragic loss, Jackler says that his father’s legacy was a guiding light in his career. “It was an inspiration, in a way, where his life and career were cut so short that I always felt sort of motivated to complete what he was never able to do,” he says.
In his fourth year of medical school, the New England native spent a month in San Francisco, which ultimately led him to rank
the University of California, San Francisco as his first choice for residency.
Jackler has remained in California ever since, specializing in complex ear diseases including tumors of the lateral and posterior cranial base. He compares the technical
also initiated the Stanford Initiative to Cure Hearing Loss, an interdisciplinary research program seeking to overcome hearing loss through regenerative means. Jackler says there has been significant progress towards the program’s goal of “making the currently untreatable cochlear hearing loss—the most prevalent form of hearing loss—curable.”
His research extends outside the field of otolaryngology; in 2006, he and his wife Laurie founded the Stanford Research into the Impact of Tobacco Advertising research group. He became interested in tobacco advertising after his mother, a lifelong smoker, developed lung cancer. Jackler says that as a child he would steal her cigarettes— not to use them, but to throw them away.

“I became curious how the cultural acceptance of shredded leaf wrapped in paper became…associated with all aspects of life, work and play,” he says. “I was intrigued by the genius of tobacco marketers in making cigarettes hugely popular.” When he started investigating tobacco advertising, he was surprised to find little previous scholarship on the topic.
difficulty of auditory surgery—with its small, delicate tools and complex procedures—to watchmaking. His technical innovations, which he illustrated in a series of microsurgical atlases, have focused on creating means of accessing difficult-to-reach intracranial tumors.
Jackler relishes the long-term relationships he has built with patients through otolaryngology. “I enjoy taking care of patients who I’ve known for a long time,” he says. “I’ve had patients who I operated on when they were infants, and I now take care of them and their children decades later.”
For 18 years, Jackler chaired Stanford’s Otolaryngology department, growing the program from just six faculty members to 55. He
Since 2006, Jackler has amassed a research collection of more than 60,000 tobacco advertisements, which are now housed at the Smithsonian National Museum of American History in Washington, D.C., and viewable through his Stanford research website.
His group’s current research focus is on emerging nicotine products such as e-cigarette brands like JUUL, with the goal of informing policymakers on ways to educate the youth targeted by these brands.
“I am often asked why an ear surgeon would choose to become an expert in tobacco advertising. What motivated me was that there is only one leading preventable cause of disease and death—tobacco use— and I felt if I could help reign in the tobacco industry’s promotion of its deadly products, it could make a real difference.” ●
Jackler has amassed a research collection of more than 60,000 tobacco advertisements, which are now housed at the Smithsonian.
Louis W. Sullivan (’58, Hon.’90) ALUMNI STORIES

By the age of five, Louis W. Sullivan was telling everyone that he wanted to be a doctor. His mother said that he would make a fine one, and Sullivan says that “there was never a doubt in my mind that I was going to be a doctor when I grew up.”
Sullivan and his family relocated from Atlanta to Blakely, Georgia when he was a child. In rural Blakely, there were two physicians, both white, with segregated waiting rooms. So, many Black residents of Blakely chose to travel more than 40 miles to see Joseph Griffin, the only Black physician practicing in the area.
Sullivan’s father, who provided ambulance services for Griffin, would often let his son ride along to the office, and the physician became a role model for Sullivan. “Dr. Griffin really was a magician. He had skills no other people had—he could cure people of illness and injuries,” Sullivan says.
When he started studying medicine, Sullivan intended on returning to Georgia to become a general practitioner like Griffin. However, the doctor’s career would ultimately reach further than his home state and he would devote much of it to increasing diversity and representation in the medical field.
Sullivan graduated from Morehouse College magna cum laude in 1954, the same year the Supreme Court decided Brown v. Board of Education. Morehouse advisors encouraged their graduates to apply to predominantly African American medical schools like Meharry and Howard and to other schools around the country.
Sullivan was accepted into every medical school to which he applied; Boston University was the first to extend an offer. When he moved from Georgia to Massachusetts, it was his first time living in a nonsegregated environment.
Seven years after earning his medical degree, cum laude, the alum returned to the
school, this time as a professor rather than a student, remaining for almost a decade.
In 1975, the doctor returned to his first alma mater, Morehouse College. He established a two-year medical education program at the college. “There was a shortage of Black
notable alumni like Regina Benjamin, who served as the US Surgeon General from 2009 to 2013, and Wayne J. Riley, MD, president of SUNY Downstate Health Sciences University.
In 1989, Sullivan left the MSM presidency to become the US Secretary of Health and Human Services (HHS) for the George H.W. Bush (Hon.’89) administration; he was just the second African American appointed to the position. He subsequently returned to MSM and served as the school’s president until 2002, when he retired and was appointed president emeritus.
As secretary of HHS, Sullivan appointed Bernadine Healey as the first woman director of the National Institutes of Health (NIH); Antonia Novello as the first woman of color as Surgeon General; and Gwendolyn King as the first Black commissioner of the Social Security Administration. Under Sullivan’s leadership, William Toby served as the first Black administrator of the Health Care Financing Administration, now the Center for Medicaid and Medicare. Sullivan also established the NIH Office of Research on Minority Health, and inaugurated the NIH Women’s Health Research Program.
physicians in the country,” he says. “The need was quite obvious.”
Georgia only had two medical schools, so many prospective doctors left the state for medical school and never returned to practice there. Morehouse College was unique because it helped boost the number of Black physicians in both Georgia and the entire medical field. “Of [the] 47 new medical schools that came into existence during the second half of the 20th century, one was predominantly African American. That is the Morehouse School of Medicine (MSM),” he says. Sullivan served as the founding dean and president of MSM until 1989.
Sullivan considers founding MSM as one of his proudest achievements, and highlights
It was Sullivan’s first experience in government service, and he made collaboration and communication indispensable.
When Sullivan began his tenure as Secretary of HHS, he invited staff members to join him and his wife of more than 60 years, attorney E. Ginger Sullivan, on their walks to converse about the country’s health, and when he traveled, he would invite other government officials to walk with him. The walks were incredibly popular. “I would have anywhere between 25 and 100 people show up and walk with me,” he says.
The daily walks evolved into an annual fundraiser for the local hospital on Martha’s Vineyard, where Sullivan and his wife summer. They’ve held the walk for more than 30 years and raised over $800,000 for the Martha’s Vineyard Hospital. ●
The doctor’s career would ultimately reach further than his home state and he would devote much of it to increasing diversity and representation in the medical field.
1965
William Christmas of Taos, New Mexico, writes, “After two years of COVID-19 selfimposed quarantine at home in Taos, Polly and I recently resumed visiting our families and friends on both coasts. In September 2022, we did a grand tour of New England by auto. A highlight of the trip was a visit with David and Kathy Greenleaf in Norway, Maine. They are enjoying David’s retirement. One of David’s favorite activities is helping to maintain a network of trails in a local wilderness area.”
1966
Paul Gitman of New Hyde Park, New York, writes, “Finally resumed travel but with much trepidation. Spent 35 days in Antarctica, South Georgia, and the Falklands in December and then Greenland and the Northwest Passage in July. Fortunately, we are well as are the children and grandchildren. Three grandchildren in college but alas, none seem to be inclined toward medicine. Still trying to improve my photography but it has been a challenge. Retirement has given me time to follow my passion. Next trips to Galapagos (with grandchildren), Sea of Cortez, and then Indonesia and Bali. Health, as always, will be a limiting factor. Visit gitman.shutterfly.com to see photos.”

1969
Marc Hirsch of Bowling Green, Kentucky, writes, “I am very grateful for the time I spent at BU. The things I’ve done, babies I delivered as a GP in the early 1970s, C-sections, multiple vehicle high-speed car crashes I attended to the aftermath of, police and fire fighters I took

care of. I picked up so much bedside manner from those impressionable years in Boston as a med student. My advice to medical students and residents has always been nonmedical: ‘Live cheap so you never resent practicing medicine to pay the bills.’ I’ve met doctors I helped train who laugh when they see me and say that was the best thing I ever taught them. What about fluids and electrolytes?
Who knew that within months of the 50-year anniversary of graduating there would be a pandemic. With the money we saved on the travel we didn’t do, I started a marketing company for my 1950s historical detective fiction, the Alice White Investigator series. My books—The Case; Hard Case; The Con Case; and The Case of the Butcher, the Bank Robber, and the Blonde—are on Amazon and Audible plus my own online store in e-book, paperback, and audiobook. I’m currently writing book number five. I’m online at marchirsch.com.”
Michael Salcman of Baltimore, Maryland, writes, “After 50 years of practice I closed my medical office in September of 2019. Just a few months before, I gave both an invited lecture on the construction of my anthology, Poetry in Medicine, and a poetry reading at Newcastle University in the UK. I didn’t know that normal life for me would end on Jan. 23, 2020, when I gave a lecture in New York, available on YouTube, “The Brain as a Metaphor Making Machine,” and I have not been free to travel since the pandemic began. My fourth collection of poems came out about the same time. Shades & Graces: New Poems (Spuyten Duyvil, 2020) was the inaugural winner of the Daniel Hoffman Legacy Book Prize and got a glowing review in the spring 2021 issue of The Hudson Review. Hoffman served as US poet laureate in 1973. Self-quarantine proved to be congenial for my literary productivity but not for the diagnosis of any medical problems. It turned out that I had a “low-grade cancer” of my prostate and underwent robot-directed surgery in January 2022. Fortunately, my PSA dropped to zero, but I am still recovering from side effects. My fifth collection of poems came out only five days after the operation. I have terrible timing; once more I couldn’t give any in-person readings. However, Necessary Speech: New & Selected Poems (Spuyten Duyvil, 2022) has also gotten a nice reception. In May 2022 I almost made it to New York but the night before my COVID self-test turned positive, and I had to cancel the trip even though it was a mild case. I wonder how many folks like me have been lucky enough to survive both childhood polio 70 years ago as well as COVID in the present day! In any case, Ilene (CAS’70) and I have been happily married for more than 50 years and are definitely going to make a Thanksgiving visit to our children and grandchildren in California. With best wishes to all the other alumni.”

1972
James Brasic of Baltimore, Maryland, writes, “I am grateful to BU for providing the foundation for a rewarding career. Since I was not allowed to conduct meetings in person due to the pandemic, I began conducting research and teaching online at home in Baltimore. I am learning how to conduct sessions online despite disconnections and
other interruptions. An enormous advantage of virtual meetings is the capability to include participants around the world. I have the good fortune to have an international team of colleagues and students to develop investigations of motor assessment, autism spectrum disorder, and other situations. I welcome the participation of students and alumni and love teaching outstanding students throughout the globe. I benefited from the feedback from colleagues for my presentations in person at the International Congress of Parkinson’s Disease and Movement Disorders in September 2022 in Madrid, Spain. While walking on the street in Madrid, Sasha, a Russian living in Portugal, photographed me for his collection of images of strangers on Instagram. He said that I had an amazing appearance!
I welcome opportunities for collaboration with students and alumni throughout the world.”

1974
Alice Rothchild of Seattle, Washington, writes, “For almost four decades, I worked as an ob-gyn and during the last decade, I turned my attention to health and human rights issues in Israel/Palestine, publishing three books and contributing to a number of anthologies. Over the last six years I have focused my attention on writing children’s books that either take place in Israel/Palestine or include stories about that region. My first of three books, Finding Melody Sullivan, a young adult novel, was published in Janu-

ary 2023. I am negotiating a book reading in the Boston area, probably at Brookline Booksmith. My new website is alicerothchildbooks.com.”
1976
Mark Goulston of Los Angeles, California, writes, “I was honored to receive the 2022 Shine the Light Media Award from the Los Angeles County Medical Association’s Patient Care Foundation for positively impacting the lives of LA County residents and improving healthcare in local communities. I was also thrilled to have my book, Just Listen, ranked number four among the top 15 communication skills books of all time by Most Recommended Books.”
1977
Gary Stanton of Cambridge, Massachusetts, writes, “I am still in the full-time practice of neurology and sleep medicine in Concord, which I greatly enjoy. Studying for board recertifications (again!) I’ve also become more active in the world of acupuncture (member of the board of directors of the American Academy of Medical Acupuncture, and of the Scientific Board of the 2023 11th International Auriculotherapy Symposium (Copenhagen). Personal interests include languages (French, Hebrew, and Japanese) and piano.”
1981
Melody McCloud, of Atlanta, Georgia, writes: “I recently authored Black Women’s Wellness: Your “I’ve Got This!” Guide to Health, Sex & Phenomenal Living (Sounds True/Macmillan, 2023). The book addresses the unique physical and psychosocial challenges Black women face, and has received notable reviews. Actress Pauletta Washington (Denzel’s wife) states, ‘Whether it’s fibroids, heart disease, diabetes, cancers, maternal mortality, mental health, or life lessons, this book gives a blueprint to help us ensure total health.’

A special feature of the book is my firstof-its-kind Societal Stress & Black Women’s Health: The ‘Rejection Connection’ flowchart
that demonstrates how prevailing psychosocial stressors—including microaggressions— adversely affect Black women’s physical health, often resulting in increased morbidity and mortality.
Relatable, yet well-researched with comparative data for Black, White, Hispanic, Asian, and Native American women, there’s information about head-to-toe medical conditions, sexology, psychology, relation-
ship concerns, and sage strategies to be an empowered patient and improve healthcare outcomes. Knowledge is power, and it’s time to change the history of Black women’s health. It can be done. Changing the health of Black women changes that of her family and future generations.
The triumphant spirit of historical and modern-day Black women is also included with references to Dr. Rebecca Lee Crumpler, the first Black female physician in the United States (who graduated in 1864, from what became the Chobanian & Avedisian School of Medicine); to Dr. Kizzmekia Corbett, who worked with the NIH in developing lifesaving COVID-19 vaccines.
Ob-gyn Dr. Jennifer Ashton, chief medical correspondent to ABC News and Good Morning America, states, ‘Black women are known to have specific risk factors . . . this book could not be more relevant. Black Women’s Wellness will improve women’s lives.’ I am available for television, radio, print, and podcast interviews, and the book is available in all formats wherever books are sold.”
1988
Jamel Patterson of Pomona, New York, writes, “I am president of a nonprofit organization called Ageno Foundation International, Inc. and we serve Eastern Africa and the Caribbean, providing access to clean water, education, economic empowerment, healthcare, and nutrition. We work in DR Congo, Kenya, Malawi, Uganda, Haiti, and Jamaica, and drill boreholes in these areas for clean water. Presently, we are drilling in Tinga, Kenya, on Maasai Land, which is the first time they would have had running clean water. To see what we are doing, you can visit our website at agenofoundation.org or contact us at agenofoundation.org.”
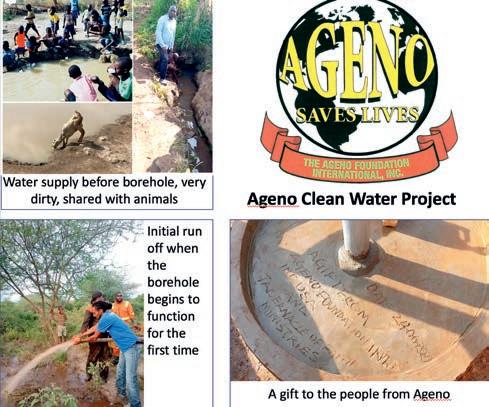
1992
David Shein of Wayland, Massachusetts, writes, “I am very happy to announce my marriage to Meredith Ainbinder (Brown’99, BC LAW’04) in June 2022 at the Hyatt Regency, Cambridge (with a view of BU across the river). The bridal party included several BU alumni, including the mother of the groom Elaine Manuel Shein (CAS’61); the mother of the bride Annette Kahalas Ainbinder (CAS’63, Wheelock’67); brothers of the groom Warren Shein (CAS’96) and Jeremy Shein (COM’01). I am an internist and medical director of a private practice in Wellesley and teach at Harvard Medical School and the New England College of Optometry. Meredith is chief of


staff and senior advisor to the president of Brandeis University.”
1993
1990
George Chaux of Los Angeles, California, writes, “Hi all, I’m still going strong at Cedars-Sinai Medical Center, currently holding the position of medical director of Interventional Pulmonology and have been promoted to professor of medicine at UCLA/Cedars. It’s been a long and very rewarding road. I’m enjoying life with my fiancée Mojan, who has traveled with me to all corners of the world. Looking forward to doing a lot more of that in the future.”
Jeffrey Johnson of New Albany, Ohio, writes, “I recently moved back to Columbus, Ohio, and am now division director for Maternal-Fetal Medicine (MFM) for a healthcare system in the city. I oversee the MFM program for three hospitals with over 8,000 deliveries per year and have a research project that is being presented orally at the Society for Maternal-Fetal Medicine annual meeting in San Francisco in 2023. Had several publications over the past few years, including a research project through the NIH during the pandemic. Back to my roots in Ohio, and so nice to be close to my extended family again. We are now empty nesters and able to take more time to travel and explore.”
Vyvyane Loh of Newton, Massachusetts, writes, “Was on STEM-Talk discussing obesity and how it impacts brain health.” The interview can be found at Apple Podcasts, STEM-Talk, episode 142.

education, economic empowerment, healthcare, and nutrition to people in Eastern Africa andthe Caribbean.
I also gave a presentation at the Institute for Human and Machine Cognition, ‘The Magical Mystery Macrophage Tour,’ which is on YouTube. My podcast, vlmd rounds, launched last September and focuses on medical science and tools to optimize health to reverse/prevent chronic diseases. You can find out more on my website, vyvyanelohmd.com, or check out my YouTube channel, vlmd rounds.”
Keyvan Nouri of Miami Beach, Florida, writes, “Published a textbook, Skin Cancer: A Comprehensive Guide, with McGraw Hill Publishing company. Was awarded inaugural Mentorship Award by Association of Academic Cosmetic Dermatology.”

1997
Darin Olson of Edwards, Colorado, writes, “Left Emory and the Atlanta VA after 24 years for private practice in the mountains of Colorado at Colorado Mountain Medical and Vail Health.”

2002
Amy Fogelman of Needham, Massachusetts, writes, “I recently had dinner with Fred Goldman, Burr Loew, Ken McDonald, and their lovely wives. It was fun to reminisce about our medical school days. I see patients in urgent care. I also continue to run my medical-legal consulting business and have started offering education to medical professionals on how to succeed as a Medical Expert Witness.”
2003
Shawn Smith of Chicago, Illinois, writes, “Was awarded the John X. Thomas, Jr. Best Teachers of Northwestern Feinberg School of Medicine Award in recognition of my work in curriculum development and/or innovation in teaching and assessment. Nominations were from curricular leadership in the MD, PA, and PT programs and are a wonderful opportunity to recognize the creative and innovative work that faculty are doing. I colead the Health
Equity and Advocacy Thread for the medical school. Winners were announced on Medical Education Day in September.” ●

1948
Malcolm Gordon of Norwalk, Connecticut, on July 2, at the age of 96. Malcolm was born in Boston to Barnett David Gordon and Ruth Myers Gordon. A 1943 graduate of Phillips Exeter Academy, Malcolm attended MIT for one year—where he was one of the top students in his class—before enrolling at Boston University, where he received his MD in 1948. He then joined his father’s textile business, MKM Knitting Mill, and moved to Puerto Rico in 1955 to establish and manage a manufacturing plant in Cayey. He re-entered medicine at age 50, practicing geriatric psychiatry in nursing homes throughout Connecticut and finally in diverse private practice. Malcolm lived life to its fullest, fearlessly pursuing adventure and accumulating lifelong friendships. Amateur aviator, explorer, skier, accomplished musician, lifelong learner, tinkerer, and, most of all, sailor, he was also a man of deep ethical convictions and a generous, compassionate heart, who sponsored refugees of international conflict and exchange students seeking a better education. Malcolm is survived by his wife, Nan Miller; sons, Andrew, Michael (Ellen), and Richard Gordon (Min Xiao); Jethro Miller (Renata); eight grandchildren; and one great-grandson.
1955
Donald Perlman of Swampscott, Massachusetts, on July 20, from ALS. Following medical school at Boston University, Donald trained at Case Western Reserve University Hospital in Cleveland and began his surgical career as a captain in the United States Army, stationed at Fort Jay in New York and Fort Devens in Massachusetts. A clinical instructor in surgery at Harvard University School of Medicine, he was on the staff of Massachusetts General Hospital and trained a generation of surgical residents there from 1962 to 1987. Donald truly loved medicine and practiced surgery faithfully on the North Shore at the hospitals in Lynn, Union, Saugus, and Salem for more than 50 years, until he retired at the age of 84. His patients were first and foremost with him, and he was tireless in his quest to heal them. He loved his office staff— with whom he worked for the greater part of his career—and collaborated with and respected his fellow doctors, nurses, and hospital staff, and looked forward to working with them every day. However, he delighted most in his family, with whom he spent his happiest moments in life.
He is survived by his wife, Cynthia; daughters Lisa (Alan) and Victoria; son Timothy (Amy); and three grandchildren. He was predeceased by his eldest son, Michael.
1955
Hilbert Ziskin of Amsterdam, New York, on May 5. Born in New Haven, Connecticut, on January 23, 1930, Hilbert was the son of Benjamin and Lena Ziskin. A 1951 graduate of Yale University, he received his medical degree from Boston Uni versity in 1955, served his internship and residency at Albany Medical Center from 1955 to 1960, and completed his tenure there as chief surgical resident. He became a diplomate of the American Board of Surgery in 1961 and was inducted as a fellow into the American College of Surgeons in 1964. Hilbert served in the United States Air Force from 1960 to 1962, rising to the rank of captain. In 1962, he moved to Amsterdam, where he made his home for 60 years.


Hilbert was a licensed airplane pilot and an avid skier. In addition, he was a passionate sports fan and had an encyclopedic knowledge of classical music. In 1951, he met and fell in love with Elizabeth Wham, his medical school classmate and lab partner. They were married on May 27, 1954. Together, they raised eight children and were happily married for 52 years, until her death in 2006. He is survived by his children, Charles W. Ziskin (Kazumi Kuriyama), Benjamin W. Ziskin (Lynnette), Joseph W. Ziskin (Paula), James W. Ziskin (Lakshmi), David W. Ziskin (Constance), Mary Beth Ziskin (Suzanne Mudge), and Nancy Ellen Deneen (Peter); 12 grandchildren; and six great-grandchildren.
1959
N. Chester Reynolds of New London, New Hampshire, on May 14 at his home, following a long illness. Born in Boston on February 18, 1934, Chet was the beloved son of Florence Ash Reynolds and Nicholas Chester Reynolds, Sr., of Revere, Massachusetts. He graduated from Harvard University in 1955 and earned his MD from Boston University in 1959. He met Carolyn “Candie” Jourdan Nichols in 1956 and they married in 1958. They had one son and two daughters and lived in Boston and Providence while he was a surgical resident at Massachusetts Memorial Hospital and Providence VA Hospital. In 1965, Chet joined a surgical practice in Tampa, but was drafted to serve in a MASH unit in Vietnam in 1966. In 1967, he served at the US Army Hospital Fort George G. Meade in Maryland. In 1968, the Reynolds family returned to New England, where Chet started a surgical practice in Andover, Massachusetts, practicing vascular and general surgery and covering ER shifts at Lawrence General Hospital and Bon Secours Hospital in Methuen. Chet and two colleagues formed Andover Surgical Associates.
In 1986, Chet and Candie “retired” to New London. Soon thereafter, Chet joined a surgical group at Dartmouth Hitchcock Concord, where he practiced surgery and taught medical residents at Concord Hospital until 2000. He was a fellow of the Society of Laparoscopic Surgeons and the International Society of Endovascular Surgeons. He was an active member of the New London Rotary Club and was passionate about addressing the world’s environmental crises and international affairs. Chet and Candie founded the Kearsarge Ecumenical Refugee Sponsor Group, which sponsored families from Bosnia and Algeria, and they enjoyed housing Colby Sawyer College international students from Cote D’Ivoire, Afghanistan, and Nepal in their home near campus. Chet and Candie delighted in travel and visited many countries throughout Europe and Asia. Chet was always building something—whether in Andover or New London, or on Diamond Island in Lake Winnipesaukee. He relished time there constructing stone walls. He enjoyed gardening, golf, tennis, and classical music. Chet is survived by his wife Candie; son Joshua Robert Reynolds (Katharine); daughters Carolyn Reynolds Peach (William) and Rebecca Reynolds Moore (Gerald); and nine grandchildren.

1963
Nina Kivelson Auerbach of San Francisco, California, on July 11, after a short illness. Nina was born in New York City on February 22, 1935. She lived a full life, starting at the Brearley School in Manhattan and graduating from Vassar College in 1956. She obtained an MA in French literature at Columbia University. Never daunted by a new challenge, Nina then decided she wanted to pursue a career in medicine. She received her MD from Boston University in 1963, completed a neurology residency at Stanford University, and followed that with a second residency in psychiatry at Mt. Zion Hospital in San Francisco. Once in California, she never left. Psychiatry became her primary occupation, and she maintained a private practice until the time of her death. A lifelong lover of learning and a voracious reader, she continued to study and expand her horizons, obtaining a law degree from USF and delighting in a string of continuing education courses at Stanford University.
A colorful and lively personality, Nina was always immaculately “put together.” Her hair and nails were perfect; her outfits coordinated with glasses, shoes, and jewelry. She knew everyone in each shop she frequented. She was always on the lookout for new and stimulating experiences. Nina particularly loved the theater and travel. She frequently went to London and New York City to check out the latest theater productions. She also enjoyed local theater and the opera. She was an adventurous traveler and often went on trips with good friends or with her
sister-in-law, Margaret Kivelson. Maintaining a lovely house that was always full of relatives and friends, Nina ran a full-service “bed and breakfast.” She took great joy in entertaining countless relatives, friends she had made on airplanes, friends of friends, and the fascinating collection of people she gathered in her circle. She was much beloved by her nieces, nephews, grandnieces and grandnephews, and countless others whom she adopted as family. She encouraged many of them in their careers and enjoyed offering wise counsel. Nina was predeceased by her brothers, Arnold Kivelson and Daniel Kivelson.
1965
M. David Kelleher of Boston, on September 7. Son of the late Kathryn Gray Kelleher and Charles Porter Kelleher, Jr., David grew up in Winchester and Haverhill. He earned scholarships to Phillips Andover Academy and Harvard University. He worked full time while attending Harvard and met his wife of 53 years, Elizabeth (Betty) Frances Callahan while working at Massachusetts General Hospital.
David received his MD from Boston University in 1965, with an internship and residency at University Hospital (now Boston Medical Center). With colleagues, he opened a private internal medicine practice in Chestnut Hill. He was a physician for the occupational medicine department at the Gillette headquarters in South Boston and at their executive offices in the Prudential Center, and he worked for the Commonwealth Medical Group, before retiring in 1996.
David loved renovating the old farmhouse he and Betty bought in Norwell and tending his wildflower and perennial gardens. He enjoyed woodworking and pottery in a barn/art studio he had built on the property. He and Betty had a lifetime of love and devotion, and he became her primary caregiver with her ALS diagnosis in 2007 until her death seven-and-a-half years later. A few years after she passed, he was diagnosed with Alzheimer’s disease and was cared for at home, then for over two-and-a-half years at Allen House in the Springhouse Senior Living community in Boston. He continued to love walks outside, gardening, painting, puzzling, dancing, singing, and telling stories about his life, his beloved wife, and the children and grandchildren of whom he was so proud.
David is survived by his twin sister, Sandra Kelleher Walker; four daughters, Siobhan Kelleher (Robert Torres), Judy Davis (Joe), Heather Izanec (Peter), and Lisa Kelleher (David); son, Mark Kelleher; and four grandchildren.
1993
Robert K. McIntyre of Westwood, Massachusetts, on March 17, in a diving accident in Florida. Bob was known for his compassion, intelligence, kindness, and sense of humor. A 1986 graduate of St. Michael’s College, he received his MD from BU in 1992 and served as a captain in the Medical Corps of the Massachusetts Army National Guard. He was an extraordinarily gifted physician who cared deeply about his patients and colleagues and was a mentor and educator to many. He was a primary care physician at Waltham Hospital, St. Elizabeth’s Medical Center, Beth Israel Deaconess, and Newton Wellesley Primary Care. He was a hospitalist at Cape Cod Hospital and then became chief of internal medicine for South Shore Hospital. He also served as medical director for many years at the Campion Center. He loved traveling, reading, hockey, tennis, and golf, and had a passion for exploring the ocean.

Bob is survived by his wife, Susan; children Connor, Luke, Brennan, and Graham; mother Marguerite L. (Millette) McIntyre; and siblings Kathleen Golden (Timothy), Helen Golden (Peter), Stephen McIntyre (Gina), James McIntyre (Maria), David McIntyre (Kerry), Carolyn Mayen (Gustavo), Mary Garrett (John), and Christopher McIntyre (Jenn).
1997
Rosita Gameros Vega of Beaufort, South Carolina, on September 13, from glioblastoma multiforme. Rosie completed her undergraduate degree at the University of the Incarnate Word, her medical degree at Boston University, and her pediatrics residency at the Baystate Medical Center. In service to her country, she came to South Carolina as a navy lieutenant commander stationed to serve the dependents at the Naval Hospital Beaufort. She was a well-loved pediatrician who served Beaufort, Hampton, and Colleton counties for many years. She loved and considered her patients her “children.” Rosie was a wonderful wife of 26 years. Most of all, she was a wonderful and devoted mom. She is survived by her husband, Luis R. Vega, MD; sons Louie and Isaac; daughters Isabel and Sofie; father Manuel Gameros; sister Julie Woodley; and brothers Oscar, Carlos, and Tony.

2000
Suraj Kurup of Orlando, Florida, on October 29. Suraj earned both his undergraduate and medical degrees at Boston University. He was a dedicated physician who loved cardiology. He was the most humble, generous, and loyal friend. He was a mentor, colleague, husband, and father. He had a love for reading, books, history, art, and poetry. He enjoyed traveling and especially enjoyed a good wagyu steak. He was always ready with a joke and a story for everyone’s amusement, including his own. Suraj is survived by his wife, Parvathi (Micky) Kurup, and daughter, Devika.

2004
Robb D. Kociol of Milton, Massachusetts, on June 2. A graduate of the University of California at San Diego, he received his MD from Boston University summa cum laude in 2004 and was class valedictorian. He went on to do his internship and residency at Brigham and Women’s Hospital in Boston, where he met his wife, Kristin. Shortly after they were married, they moved to Durham, North Carolina, where Robb started his cardiology fellowship at Duke University. He returned to Boston to complete an advanced heart failure and transplantation fellowship at Tufts Medical Center. Robb’s proudest achievement, other than his family, was starting the Advanced Heart Failure Program at Beth Israel Deaconess Medical Center. His hard work and dedication changed the lives of many patients and physicians. His family is proud of the legacy he left on this program and that it continues to flourish. Robb had transitioned to working in the pharmaceutical industry for Boehringer Ingelheim and, most recently, Cytokinetics. Robb enjoyed traveling, concerts, and spending time with his family, who were truly the cornerstone of his life.
Robb is survived by his wife, Kristin (Gannon) Kociol; children Sophia and Olivia; father Stephen Kociol; brother Brett Kociol (Daneen); brother-in-law Mark Gannon and his partner Melissa Miele; and Colleen Donovan and her husband Adam. ●
Here are some ways you can turn tax dollars into charitable dollars and support the cause at BU that matters to you.


Qualifie d Charitable Distribution (QCD)




Persons aged 70 1/2 or older can direct up to $100,000 from an IRA directly to a qualified charity like BU. This may lower your income and your taxes.

Outright gift of an asset

By making a gift of stock, real estate, or other appreciated assets, you may avoid paying capital-gains tax on the transfer and receive a tax-saving charitable deduction
Charitable gift annuity
No matter what happens with the economy, your payments are secure and fixed at a rate that will never change. You will receive a tax-saving charitable deduction, and a portion of your payments could be tax-free.




