Bearing witness to a pandemic
Delivering unconditional care

2020 International Year of the Nurse and the Midwife
Bearing witness to a pandemic
Delivering unconditional care
Index
Bupa Chile S. A.
Legal representative: carlos jaureguizar CEO Bupa Global, India & UK Former General Manager Bupa Chile
Management: Cerro Colorado 5240, Las Condes, Santiago – Chile www.bupa.cl Bearing witness to a pandemic
A Bupa initiative in the International Year of the Nurse and the Midwife. © Bupa Chile © NegroEditores isbn: 978-956-402-907-8
Firstirst edition: March 2021 1,500 copies Santiago de Chile Printing: ograma impresores
Original idea carla alarcón
Editorial team ana maría q uezada josé soto ignacio vidaurrázaga
Editorial committee carla alarcón laura alvargonzalez gianina espinoza coral novo raquel pérez ana maría q uezada donna ritchie luis rojas josé soto ignacio vidaurrázaga
General coordination josé soto
Spanish coordination donna ritchie
Research and interviews ignacio vidaurrázaga
Report editing ignacio vidaurrázaga sandra bustos
Art direction patricio arellano Design Negro.cl
Illustrations manuela montero
Photography cristóbal marambio / Santiago christián jammet / Arica matías quilodrán / Antofagasta rodolfo muñoz / Reñaca Archives Bupa Chile
Prologues
Florence Nightingale
Tales
23 I kept my promise anonymous
24 Being surrounded by death makes you value life more Sofía Gaete
28 All he wanted was a hug giannina allende
30 The hardest winter in Madrid daniel millán
32 Your mother was never alone marta rodríguez
36 Things you never forget silvia jiménez
38 We transform our capability to help others mª ester smith
42 Unprecedented tsunami sergio castaño
44 We are not heroes, we are committed professionals donna ritchie
46 Today we value our team and apreciate life more mª gloria marinas
51 Patients did not die alone lidia gómez
52 We just hoped for a miracle natalia castañeda
56 We care for each patient, as if they were the only one adolfo vásquez
A traumatic night shift mª eugenia fernández
I take my hat off to my team yolanda huerta
When you are caring for people you don’t feel any fear natalia sáez
People were anxious when they called alejandra llorente
I was lucky to be a nurse laura alvargonzalez
Mama, when is this going to end?
Facing the crisis as a team
I enjoyed learning a new role during the pandemic
My small part in the fight against the pandemic gianina espinoza
When you are the patient you feel vulnerable claudia escobar
remember how lonely the patients felt claudia collao
never lost my strength violeta carrión
wouldn’t change what I went through constanza núñez
volunteered to help my colleagues
support
what I do I always wanted to be a
Educating, guiding and accompanying our patients angélica rodríguez
A time of fast learning and great camaraderie maría gonzález
Closer to our patients with cancer sonia guerrero
Nothing prepares you for this tamara casado
The loneliness pandemic andrea espiñeira
When the patients went home, we celebrated with music and clapping covadonga medrano
No time to think clara gonzález
United as a team hilda vargas
Love is what keeps us going judith aguilera
Empathy prevention and care juan pablo vásquez
Communication with the family made all the difference sarvia mardones
We’ll get through this together alejandro lleixa
I am stronger than I think mª jesús puyol
Learning raquel pérez
Always a nurse, with or without a pandemic mª francisca castillo
Each customer and individual evelyn jara
Introduction
Editorial committee December 2020Bearing Witness to a Pandemic was born out of Bupa Chile’s interest in documenting the experiences of the nurses and midwives of Chile and Spain, how the organisation was put to the test and the solutions that were found in the fight against the Covid pandemic in 2020.
We carried out in-depth interviews with our people working in Bupa-Sanitas in order to provide important historical evidence of the key role that health professionals played in this unprecedented world health crisis.
These reports are the result of over 80 interviews and over 70 hours of recorded material, gathered over a period of three months. The recorded material has been transcribed, whilst carefully ensuring that the emotional and individual content of each story is not lost.
The resulting stories give us not just an institutional perspective on the impact of this pandemic, but also, behind each story, an insight into the human experience of the patients and their families.
Usually for such projects, a book is written after the stories it tells have happened. But in this case the stories are being told in real-time. Interviews were carried out between shifts, from home offices, when interviewees went home after work or even in their breaks. We were moved by the willingness of each participant to take part in this project.
Given the difficult circumstances, with quarantine and strict protocol, taking photographs was particularly difficult. Images were taken by photographers in Santiago, Reñaca, Antofagasta and Arica. There are also photographs taken by the interviewees themselves. We are grateful to all of them for sharing their own personal photographs.
We are delighted with the result and thankful for the confidence placed in the editorial team. We are proud to have had the opportunity to take part in the creation of a book written at the same time as these facts are being played out on the world stage.
Prologues
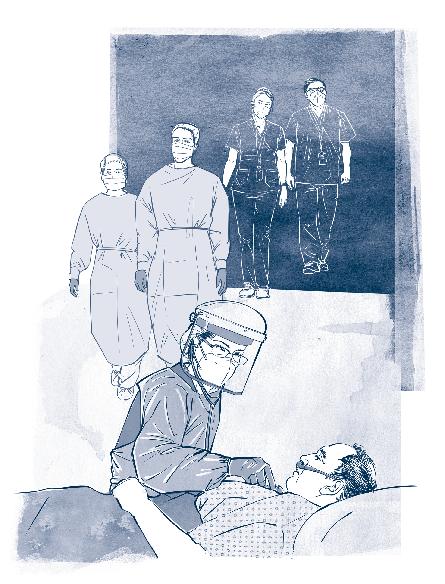
carlos jaureguizar CEO Bupa Global, India & UK Former General Manager Bupa ChileIt is significant that such an unprecedented world crisis, which has demanded from people, companies, systems and countries our very best efforts in caring for and supporting each other, has coincided with the International Year of the Nurse and the Midwife. Those who work in these professions are dedicated to their work, empathetic and resilient. They are the ones who are at the patients’ side at all times, holding their hands and speaking words of comfort in times of doubt and fear.
In a year that history will not forget, we will also never forget the commitment, effort and love shown by millions of nurses and midwives to their work and to those they care for.
This book, in which it is an honour to participate, seeks to reflect the personal stories and experiences of our network of professionals in Chile and Spain, paying homage to all those who fought valiantly throughout this pandemic.
I am immensely proud of each person who took part, as well as those who did not. May they continue to give their utmost every day. Thank you so much for your dedication and passion. �
josé francisco tomás Director General Sanitas Hospitals, ppp and New ServicesNobody working in health can think about providing quality patient healthcare without counting on a group of professionals working on the front line of health management and administration. These workers are dedicated to their work and use their knowledge to provide the best care for patients. These are the nurses and midwives for the recognition of whom the who has particularly set apart the year of 2020, when we celebrate 200 years since the birth of Florence Nightingale, who created the first school of nursing in the world, at St Thomas’ Hospital, London.
In a year marked by a huge world pandemic caused by the SarsCoV2 virus, I believe it is time not just to highlight the work of nurses all over the world in fighting the virus and its impact, but also to remember another great woman who pioneered something that we are all pinning our hopes on at this time vaccination campaigns. That woman is Isabel Zendal, a Spanish woman born in a small village in the province of La Coruña in 1771 and who took part in the Royal Philanthropic Vaccine Expedition led by Francisco Javier de Balmis. On 30 November 1803 they set sail from La Coruña to carry out the biggest vaccination campaign the world had seen at that time. They were planning to vaccinate all the children in the overseas provinces against smallpox. Isabel took 22 children with her who had not had the smallpox. She infected each child using pus from the sores. These children were live vaccine carriers. After arriving in Puerto Rico at the beginning of 1804, the expedition travelled to New Spain (today’s Mexico) and the vice royalties of New Granada, Peru and Chile. The expedition then went on to the Philippines, returning to Acapulco in 1809. It is estimated that they vaccinated 250,000 people, thus contributing to the immunity of those communities.
So, when we now place our hope in vaccines, we should remember that it was a Spanish nurse who was recognised by the who as the first nurse in the history of international mission and the first to take vaccines to Chile and other countries. She is an example of hope and recognition to all our nurses and midwives. �
This book is being published in a special year, in which we have experienced many different emotions. Firstly, the worry and grief caused by the pandemic and the pain people have had to go through. Then, on the other hand, the pride and hope found in seeing, yet again, the commitment, skill and excellence in healthcare shown by all our employees, health professionals, technical, administrative and managerial teams in rising to this challenge.
The pandemic has put our skills and knowledge, working procedures and relationships with our patients and their families to the test. It has challenged us both as professionals and as people, as well as, quite naturally, filling us at times with fear and uncertainty.
The country has faced this challenge with a united front. The public and private sector have worked together, as have the different levels in our own company, with the support of Bupa and the advantage of foreknowledge learnt from countries where the pandemic hit some months before it hit Chile. The joint work with Sanitas in all areas and in matters such as organisation, remote working, new systems and care flows, scientific evidence, practical experience, taking care of our employees and shared experiences are all evidence of the advantages of being a global company.
As a company, whilst we took all the necessary measures to protect our clinical and non-clinical employees, we also enlarged and adapted our capacity, structure and equipment to help those who needed it, whether Covid-19 patients or not. We quickly and efficiently brought in new care strategies like video appointments, home care, exams and procedures, a safe maternity programme, remote prescriptions, triage and telephone and web support, amongst others. Parallel to this, we brought in new support and guidance services and special cover for our isapre (private insurance) and health-plan costumers. Our clinical laboratory pioneered in the country a faster technique for the pcr test, which allowed them to increase capacity to meet the huge demand. We are also part of the integrated public and private network for Covid-19 patient care, contributing to the national strategy for fighting the pandemic.
How did this book “Bearing Witness to a Pandemic ” come about? There is no doubt that at the end of 2019, when the who proposed, backed up by Bupa all over the world, that 2020 be celebrated as the “International Year of the Nurse and the Midwife”, we did not expect what has hit us. We were busy preparing to celebrate with our various nursing and midwifery teams, planning professional training and development, extension activities for patients and costumers, environmental projects for recycling
clinical material, events to recognise all our teams and a special prize for outstanding nurses and midwives. Then the pandemic hit and everything changed. We had to change our focus completely.
Yet in some way, as is the way of life, this change and the huge challenge it brought with it opened another door and another perspective to us and focussed our attention on the key role of nursing and midwifery, which looks after people at all stages of life.
This year, more than ever, we value, thank and admire the work of those who look after our patients and their families, treating and curing all those affected by this pandemic, looking after those we cannot save and ushering in the new lives that are being born and that are bringing hope in our moments of pain.
We are proud of the work of the teams at our clinical and medical centres, who have allowed Bupa Chile to continue with our role and our mission, at a time when we are learning new lessons every day and where there are no certainties.
As an institution and as a healthcare team, we have responded to this challenge by innovating and growing in many different areas, learning new ways every day of caring for Covid-19 patients and using preventive measures to protect relatives, other patients and the team themselves. We have acquired, in record time, new skills to meet new demands. We have seen general care nurses learn to care for intensive care patients, paediatric nurses learn to care for adult patients, midwives supporting with nursing tasks and developing safe birthing skills, students carrying out basic nursing tasks, the redesigning of employee work flows and patient care procedures in outpatient facilities and new roles created in telephone services. We have also pioneered sample taking for the diagnosis of Covid-19. All of this shows us, more than ever, what a huge pool of human and professional resources we have in our nursing and midwifery teams.
At the same time, we have developed new healthcare procedures that allow us to continue to provide the quality, personal care we have always promised, even at a time of restrictions, preventive measures and patient isolation. Our nursing and midwifery teams have been key too, demonstrating yet again their excellent training and practical vocation, where rigorous scientific training goes hand in hand with quality and relationships. Many of the stories in this book show not just how the personal touch was always there, but also how it was reinvented and reinforced during the pandemic.
That is why when Carla Alarcón, Director of Nursing at Bupa Chile Hospitals, came up with this initiative, we had no doubt that we should
run with it and showcase, recognise and thank our nurses and midwives for their dedication and their huge contribution during the pandemic even more so in this particular year dedicated to them. These are their own stories, allowing us a glimpse into their contribution and their experiences.
As the management team of Bupa Chile, we are delighted to add to this project and know that the editorial team, made up of representatives from many different areas, took it on board right from the start. The Sanitas nursing team also wanted to be represented in this book, adding to the experiences of our network of hospitals and health centres and showing through their own stories that we are all one big team with one purpose and common values.
Going forward, we would like to add two final thoughts: on the one hand, we need to keep up the effort and learn from our experiences so that we can continue the fight against this pandemic. The pandemic is not over yet the second wave is raging in Spain and we have no idea whether there will be second or further waves in Chile, and how big these might be. We also need to consolidate and grow the new developments the pandemic has given rise to, ensuring that they are here to stay and that they help us give even better care and support to our patients and costumers.
I invite you now to read and to enter into the stories in this book, getting to know those we have deservedly called “Bearing witness to a pandemic delivering unconditional care.” �
barbara stilwell Executive Director Nursing Now Global CampaignIt is an honour to write a foreword to this book which shows the reality of nurses’ lives during the Covid-19 pandemic. 2020 was the International Year of the Nurse and the Midwife, and celebrated the bicentenary of Florence Nightingale’s birth; we had much planned at Nursing Now to celebrate the year and the crucial contribution of nurses to global health, but much of it had to be postponed, cancelled or take place virtually. Ironically, despite all of our campaign challenges, it was a year like no other for the spotlight it shone on the critical importance of the work of nurses globally.
I doubt that there has ever been a more critical moment for governments everywhere to invest in nursing, and I hope that your stories in this book will be part of the wake up call. Action is needed NOW because the world needs not only to rebuild its health systems that have been so severely damaged, but also to deliver universal health coverage – health for everyone, everywhere. Without nurses this simply cannot happen.
Your stories have to be valued for the skilled care they describe. Nurses around the world raise their voices with you in pride. Thank you for all you have done and for sharing your story. �
The who declared 2020 the International Year of the Nurse and the Midwife, coinciding with the bicentenary of the birth of Florence Nightingale. Nurses had many plans to showcase nursing and the extraordinary role of their profession and to celebrate nursing. However, Covid-19 has changed everything. It has changed our world. It has changed our way of life, the way we socialise, work, interact with each other and the way nurses provide care.
The Covid-19 pandemic has raised the visibility of nursing like never before, as well as showing us how indispensable they are to healthcare and how they make up the backbone of all healthcare services.
Nurses have faced the pandemic and all its implications for healthcare with compassion, care, resilience, creativity and great leadership skills, as we will see in the reports and stories told in this book. Many lives have been saved, whilst at the same time we are sad to say that many of our colleagues have died whilst carrying out their duty of care. We must keep building on the visibility we have achieved during this year of the pandemic. We owe that to the nurses who have given their lives and to society itself. We must be partners in healthcare and be involved in each policy making decision, playing a central part in strategic planning and working groups. We must get alongside those who are making the decisions in order to build a better future, a better society and a better world in healthcare.
The huge commitment and value shown by nurses in 2020 makes me optimistic about the future. I would like to encourage them to make the most of the opportunity to get their voices heard, in spite of the huge challenges ahead.
This book of reports from nurses on the front line of the pandemic in Spain and Chile marks the International Year of the Nurse in a real and personal way. Their stories will touch you and move you. They show the compassion, dedication, knowledge, skills and professionalism of nurses in what has been an incredibly difficult year. These professionals have always
represented the human, caring, holistic side of healthcare. This year, more than any other, they have shown the world why we must do more than just clap for nurses if we want to give nursing the value it deserves and invest in its future.
We will always have problems, but we can overcome them. We can work together to build a better future for our nurses and our patients. I have seen the value of our younger colleagues and have been impressed. Nursing is in good hands. We must not just wait for opportunities to arise, we must create them and make the most of them. We cannot just dream, or wish, we must do and we can do. Each of us can make a bit of difference, but together, twenty-seven million nurses can change the world and can start straight away, in 2021. The future is in our hands.
This book shows the real human side of nursing and should be read by everyone, not just by nurses and healthcare professionals. �
annette kennedy President of the International Council of Nurses icn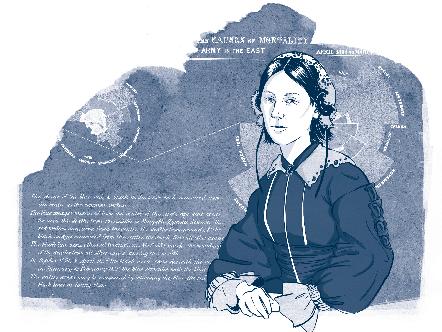
More contemporary than ever
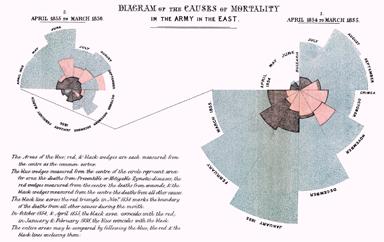
Florence was an expert at presenting data in a visual way to get across her message and secure funding. Such was her contribution to statistics that she was recognised by the bestowal of membership of the Royal Statistical Society - the first woman to gain this honour.
Florence Nightingale is considered to be the mother of modern nursing, as creator of the first conceptual model of nursing with an intersectorial, interdisciplinary and global vision. Florence was born on 12 May 1820 to English parents.
2020, the bicentenary of her birth, was declared by the World Health Organisation (who) to be the International Year of the Nurse and the Midwife. In the same year of such recognition, the world has seen and suffered the worst pandemic in the last few decades.
In this time of crisis, the strength and capacity for action of nurses, pioneered by Florence Nightingale, has been put to the test at a global level. Nurses all over the world have had to find solutions to daily problems. Their observation, organisation, forward-thinking, personal and data analysis skills have been crucial in the fight against Covid.
Florence Nightingale, who was from an aristocratic English family, believed that knowledge and statistical methods and instruments were key to developing concrete solutions to problems. From a young age, she showed an interest in maths, but her mother encouraged her to develop skills in the home and her father asked her to study subjects that were “more appropriate for a woman.” But Florence was persistent, and her parents ended up allowing her to study arithmetic, geometry and algebra.
Florence was an expert at presenting data in a visual way to get across her message and secure funding. Such was her contribution to statistics that she was recognised by the bestowal of membership of the Royal Statistical Society the first woman to gain this honour. She was even made an Honorary Member of the American Statistical Association
As someone with very modern ideas for the time she lived in, Nightingale had to fight against prejudice to work as a nurse, administrator, researcher, writer and teacher. She visited hospitals in many countries, such as: France, Greece, Switzerland and Egypt. These trips were her formative years. What she learnt and experienced is recorded in her travel journals and other writings.
To achieve her dream of caring for the sick, she had to come up against her family, who were opposed to their daughter, a member of the aristocracy, carrying out such a “menial” task as nursing. They saw her future as getting married and bringing up a family. Surprisingly however, her life took another twist when her maternal grandmother and a doctor friend of the family gave her financial support to start her studies.
This change in her personal history was to be crucial to Great Britain and the future of healthcare. Then, from October 1853 to February 1856, war broke out between the Russian Empire and the allies, France, the United Kingdom, the Ottoman Empire and the Kingdom of Piamonte - Cerdeña (The Crimean Wars). Although the allies beat the Russians on the battlefield, sickness ate away at the British army. There were not enough doctors, medicine or nurses. Sidney Herbert, Great Britain’s War Secretary and an acquaintance of the Nightingale family, asked Florence for help.

Taking with her thirty-eight volunteer nurses she had personally trained up, Florence left in October 1854 for the British operations base in Scutari, on the Crimean Peninsula. On arrival, a scene of desolation met her: an overworked medical team and wounded soldiers receiving totally inadequate treatment. The hygiene was deplorable. The medical care was just not sufficient to care for the sheer number of sick people. Neither was there enough food or appropriate equipment to cook food for the patients. Ten times more soldiers were dying of diseases such as typhoid fever, cholera and dysentery than from battle wounds.
«Observation will show us the patient’s condition, reflection will show us what we must do, and practical skills will show us how we must do it. Training and experience are necessary to knowing how to observe and what to observe, how to think and what to think».
Just as the hospitals have done during this world health crisis, under Florence’s direction, the hospitals in Crimea underwent a change in procedures, skills, equipment and space. Florence ordered that contaminated waste be cleaned up, created new patient care procedures and improved ventilation in the hospitals in order to bring down the mortality rate. She succeeded so well at this task that she was received as a heroine in her own country at the end of the war.
After the war, Florence promoted revolutionary ideas in patient care and public health in Great Britain and all over the world. During a long period of sickness, she passed the time writing letters to politicians and statisticians and publishing scientific articles putting forward proposals for the strengthening of military nursing training.
Later, she modernised patient care training, creating a new teaching model. 1859 saw the publication of her “Notes on Nursing: What it is and What it is Not”, which was used as the basis of the study programme in the Nightingale School and other nursing schools. Florence never married: she gave her whole life to the service of others and those most in need.
Her studies led her to define sickness as nature’s way of freeing us from the effects and conditions that have interfered in our health. She believed that in order to have good health you needed a healthy environment (pure air, potable water, sewage treatment, clean quarters and light). She also put great value on feeding the human spirit, an attitude that continues to be just as important in our times.
The lessons of this pandemic are still to be seen, but without a doubt Florence’s thoughts about acting in spite of fear, about facing challenges head on and trusting in hard data and, above all, her words about heroism are still important: “I am of certain convinced that the greatest heroes are those who do their duty in the daily grind of domestic affairs whilst the world whirls as a maddening dreidel”. �
florence nightingale, Notes on Hospitals, 1863. ↑ Diagram showing the causes of death of the army in the East, by Florence Nightingale.Tales
When you can heal, heal
When you can’t heal, alleviate suffering
When you can’t alleviate suffering, provide comfort When you can’t provide comfort, just be there.

I kept my promise
«I worked my normal shift, and up until then nothing out of the ordinary happened. We started the rounds and at that point, one of my patients started to deteriorate. We have seen how Covid can be like that - sometimes it advances very quickly. The doctor saw her and we started to prepare her for intubation and transfer to the intensive care unit; the doctor was talking to her and she seemed calm in spite of it all. When everyone had gone, she looked at me and said: When my time comes, please pray the Lord’s Prayer over me. I can’t deny that although I saw such scenes on a daily basis, I felt a lump rise in my throat as I told her: Don’t worry, I am sure you are going to be fine. She answered me: I am not afraid of dying, I am right with God, all I ask is that you pray over me when my time comes. I promised her that. If it wasn’t me, it would be one of my colleagues… I finished my shift, all the time wondering what would happen to her and how it would be. It’s strange, but I felt a huge burden of duty and could hardly speak. On my next shift, she was really unwell. When I could, I asked how she was and was told that she was unlikely to make it through the night. Her family had already been informed. They all had Covid too and couldn’t even come and see her through the screen. I finished my shift and went to see her. She was dying. I went in, touched her hand and prayed for her. I felt so much peace - I had kept my promise. I felt privileged to be on the front line».

Being surrounded by death makes you value life more
sofía gaete Nurse Bupa Santiago Hospital
I have been a nurse for ten years and I work in the intensive care unit at the Bupa Santiago Hospital. I have always looked after my patients as if they were my family, caring for their needs and treating them like I would my own family. At the clinic, there are spaces where the whole family is involved. Patients often tell me, Miss, I don’t want to disturb you, you need to get on with your work, but that is my work, being with them, helping them feel better and just being there.
The pandemic is something we never expected to live through. From the start of this year, we began to prepare for what was coming, training up extra staff and looking at how the pandemic would behave in Chile at its peak and how we would deal with that. It ended up being even worse than we expected. June and July were the worst, when many people didn’t even make it to the intensive care unit, and others couldn’t be saved despite our very best efforts.
Patients would come in urgently needing a ventilator. They were awake when they arrived and I would discuss with them what was going to happen. They were between the ages of 35 and 80 years old. For many of them, these were their last conversations. They have stuck in my memory. When I talked to them before intubating and sedating them, they weren’t thinking about their last wishes, simply asking us to look after them and tell their family they loved them lots and were hoping to see them again.

One patient I particularly remember. He was 75 years old and didn’t want to be intubated. His daughter called us in desperation, asking us: please convince papa this is his last chance. I talked with him and explained that if he chose not to go on a ventilator he would have to be removed from the intensive care unit, because there were seven or eight people waiting for ventilators. It was all very dramatic. I finally convinced him to talk to his daughter on the phone and she persuaded him to do it. All three of us cried at that point.
Then, Raúl said: I accept, connect me up and do everything that is needed to get me better. Before he was connected up to the ventilator, he asked for pencil and paper to write a letter to his family. He wrote a beautiful message about how he would be fine, how he loved them lots and was looking forward to them coming and getting him soon. Sadly, he died.
The family couldn’t come and get him, and I thought the letter might be lost, as a deceased person’s effects are stored away in a bag. So I asked my boss to take a picture of it and send it to the family by e-mail. His daughter sent me a thank you message saying: Sofía, I can’t thank you enough. This makes me feel close to papa. I know you would have talked to him the way I would myself if I had been at his side, and I want to thank you from the bottom of my heart.
Our profession is like no other. Sometimes, no matter how much you give the very best of care, things happen, situations that are out of our control. There were not only the difficult times, but there were the successes too. I had one patient whose face I remember more than their name. He was 33 years old. He came in during my night shift and was very unwell. He told me he had kept on working because he wanted to buy an apartment, but ended up catching Covid. He deteriorated quickly. He was young but had underlying risk factors. After nearly a month and a half, he began to come round and I told him: don’t worry, I am here to look after you. He was embarrassed because I had to bathe him. People feel it takes away their dignity, but we always make them feel better. He began, little by little, to recover. One day, he gestured through the screen with his hand and said to me: Thank you Sofía. I couldn’t stop crying.
Through all of this, I have learnt that we need to take stock of what we are going through, what we are learning, how we are going to look at life from now on and, of course, how fragile we humans are. �
Through all of this, I have learnt that we need to take stock of what we are going through, what we are learning, how we are going to look at life from now on and, of course, how fragile we humans are.
All he wanted was a hug
giannina allende Nurse San José de Arica HospitalWe have a reputation for being an intensive care unit with the human touch in the First Region in the north of Chile. We are known for the way we bring the family into our patient care and treatment.
Nevertheless, during the pandemic we had to restrict contact with both Covid patients and non-Covid patients with serious illnesses.
It was very difficult for us to see the families unable to accompany people in the toughest of times.
For me, the most moving case was that of Juvenal, 50 years old, who came to us with a very serious abdominal trauma. He was on non-invasive mechanical ventilation. One day he said to me: Please Miss Giannina, can I hug you? I knew he felt alone. Together with my colleague Mónica, We hugged him. He took my hand, I prayed with him and said: Don’t worry, don’t be afraid, we’re looking after you.
That day when I finished my 24-hour shift I was really worried. An hour later my colleague Darío told me: Juvenal is very unwell and we can’t do any more for him, he is going to die shortly. That really touched me, because all he had asked for was a hug. Sadly he died.
I have also seen many miracles at our intensive care unit. People have come in very unwell, at risk of dying, and we have fought with all we have to save them. My sister and I decided to cut ourselves off because of the risk of Covid, as she works with patients in an intensive care unit (icu). Our grandparents are isolating with a younger sister and the two of us send food once a month, which we disinfect beforehand. �

The hardest winter in Madrid
daniel millán Nurse Sanitas Hospital La Moraleja«I would finish my shift at ten or twelve at night and travel home on a deserted road. It was March and winter in Madrid, very dark and depressing. I would have a good cry in the car. This was unbelievable, it couldn’t be happening, there was no one around.
Some days were really frustrating. Patients would come into the emergency unit walking and after a couple of hours, or the next day, they had died. You felt powerless, because you couldn’t do anything, the demand was too high and the resources too few. People were dying and their family couldn’t even be with them».
Your mother was never alone
marta rodríguez Nurse Las Rozas Care Home

There are times when people want answers but all you can do is listen. Words are not enough. The best thing you can do is to be there at someone’s side so they don’t feel alone.
This is the residents’ home. As well as our rooms, there are big common areas with gardens, trees, grass and flowers, as well as a vegetable garden. We have residents from the age of 73 upwards. I even had a patient of 101 years old. Less than half of them are totally independent. At the moment, in August, we have 109 residents. All this peace and quiet was broken in March when Covid broke in on our lives.
Eva, our director, had to make tough decisions. And she had to make them quickly and safely. We had to move many patients from their rooms to make an isolation zone. We had to tell them why we were doing this and help them understand.
All the residents were tested and the results took us completely by surprise. Many of our residents had Covid and we had the break the news to the team and the residents’ families.
I don’t want to revisit that grief, it was horrible to think how we wouldn’t be able to look after our residents like before and how we would have to say goodbye to some. That, for me, was the hardest thing of all. I remember I went down to my office and burst into tears. The director sent me home: Go home, you’re not doing so well. I said: I am fine. I just need to have a good cry. Could I just have a cry? I didn’t want to worry her and let her see my suffering, but I really needed to do that to help me get through.
MADRID — SPAINIt must be said, Sanitas quickly set up a system where you could speak to a psychologist on the phone if you needed to.*

I am 42 years old and have been with Sanitas since I was 16. I think nursing gets top marks for its support and care of people, and we have adapted to a very different environment, which has really changed us (drips for intravenous care, individual protection equipment (ppe), deserted rooms, everything happening behind closed doors, hallways buzzing, but not with residents…).
Despite the chaos, we had some beautiful moments. Like the time one of our residents’ wives was hospitalised and we couldn’t get in touch with her. I tried finally with my own mobile and managed to get through. I said to her: We are calling you so you can speak to your husband, as he is not very well, shall I pass the phone to him? She said: Yes, yes, put him on… I want to talk to him. Our resident couldn’t hold the phone so I had to put it on speaker.
Wow! Those two really loved each other! Their conversation was so moving and emotional. Sadly, it was their last conversation, as he died some hours later.
At some point in a team meeting our director suggested that we authorise one family member to accompany residents who were dying. The family were very glad to be able to come. Being there at the deathbed meant a lot to them, even if they couldn’t hug or kiss their loved one and they were wrapped up in ppe.
Last July, we were able to hold a funeral with families for deceased residents. A tree was planted in the grounds of the home as a symbol of resilience. I think that was a special moment for all of us, both families and staff.
I love my work and it is a part of me. Some people have made us out to be super-heroes. No, we are not super-heroes, we are nurses, and that word in itself means everything to me.
I remember the daughter of one resident saying to me: the only thing I ask for is that if my mother has to die, she should not be alone. I answered her: I have seen her about ten times today and she isn’t talking much. When I go in it’s just to change the drip or give her intravenous antibiotics… But each time I have taken her hand and spoken to her. I want you to know that your mother has someone nearby at all times.
Last July, we were able to hold a remembrance service with families for deceased residents. A tree was planted in the grounds of the home as a symbol of resilience. I think that was a special moment for all of us, both families and staff.
I am married and have two children a girl of 8 years old and a boy of 6. For months, we have been isolating at home. I even slept in a separate room at the beginning. The children were very good about me going to work.

One day is etched on my memory, when I was in the shower and the little one came in with his favourite teddy … He came in to use the toilet and left his teddy next to my clean clothes. I could see him from the shower and saw how his little fingers were stroking my clothes at the same time as his teddy. He was stroking mummy’s clothes!
My husband, my rock, never told me of his fear, but I could see it on his face. All the employess were tested and when I got the result, I told him: It’s negative. We had to make a decision together on where to go from there. Two days later I told the children: You can go outside and play now, and I think we can go back to a bit of normality in the house...
These have been very difficult times, but I am happy to be strong and proud of where I am today. I love my work and it is a part of me. Some people have made us out to be super-heroes. No, we are not superheroes, we are nurses, and that word in itself means everything to me. Nursing doesn’t only heal, it cares. �
Things you never forget
silvia jiménez Nurse Bupa Antofagasta HospitalAt the beginning of all this, they would talk about how many intensive care unit spaces or ventilators we had in the country. But it’s important to remember that a ventilator on its own doesn't save a person. You need a 24/7 multidisciplinary team to care for each patient.
The workload and emotional load in particular have been heavy. We have had to isolate from our families, and some even from their partners, in order to look after our patients. I have stayed with my family: my husband and three children, as well as my mother-in-law, but I have had to stay away from my own parents - I would have never forgiven myself if they had got sick because of me. My mum has been very worried. She always cries when we say goodbye on video calls. That is really hard for me.
One of the most difficult moments in the last few months was when one of my work colleagues was transferred from the La Portada clinic on my shift. It was really tough to go through what we went through - you never think
someone you know is going to be a victim. When he came he was very upset and afraid, and I wanted to go and cry with him. But I couldn’t do that because I was more than a colleague, I was his nurse, and we should never cry in front of our patients - we always need to be strong for them. I am happy now though, as he recovered and is moving on.
Last week, a woman of 38 years old came from the wards very unwell. I remember we had to let her husband come in to say goodbye to her, and they were from a different community of Antofagasta, Mejillones. I let him in. He was a big, bulky fellow. We wrapped him up in the PPE and left him in the room with a paramedic and the head doctor. He asked his wife Why are you leaving me alone, what will I tell the children? Then he came back and asked us Why do so many of the best people die?
At times like that, your heart bleeds for these people. And that will stay with me forever. �

We transform our capability to help others
Nurse Bupa Santiago HospitalI have two roles: paediatric care of straightforward cases and pediatric critical care unit, where the more complex cases are, as well as intermediate and intensive care cases. The usual paediatric patients were not coming in because they were shut up at home and weren’t going to their normal childcare facilities. The odd appendicitis case or child with fever would come in, or one who had fallen and had a brain injury, or other such cases.
On 19 May, I was asked to set up twelve adult beds on the paediatric floor, which then became eighteen beds and by the end of the week was thirty beds. We did everything we could at the clinic to adapt to the needs of the patients during the pandemic. We needed to make ourselves useful. We were specialists in paediatric nursing, but our profession is one of service to others.
We started refreshing our training so that we could look after adult Covid patients. In paediatrics, we are used to looking after patients in isolation all year round. In winter, for example, it’s the respiratory viruses. We were somewhat used to wearing aprons and gloves to protect other patients from viruses.

CHILE
We have always helped each other at this hospital. And that was what we did, help other human beings who might have been our relatives, our grandparents, our parents, a cousin, in their time of need. Our care is something practical and solid, such as the need to retrain for adult care. With Paola Vallarino, the training nurse, the whole intensive care paediatric team took a course in adult care and we designated nurses from the clinic to go and learn anything we still needed to know.
At the same time, those of us in intensive paediatric care were sent to train in adult care. All of that happened at the beginning of April, and by mid-April 100% of our more experienced nurses and nursing technicians in the icu had been trained in the theory of caring for adult Covid patients.
Basically, we all retrained. At first, the aim was to train at least 80% of the employees, but we managed to train 100%. Then we set to finding out what equipment and medicines we would need for adult patients. We found we would need larger endotracheal tubes, catheters and so on.
The adult team was almost 100% external and we worked really well together. At the beginning, nobody knew each other and we invented a code, coto: C stood for comprehensive patient care, O for organisation, T for teamwork and O for order. We did that to get the team working together, because we were all from different worlds and different clinics and we needed a common identity.
We managed to really get a dynamic, united team going. We worked with strangers who were looking for an opportunity to work. And we went from less to more.
My team would say: We are their family right now, which is why we like calls and video calls so much. We use the SAP system for electronic filing and we managed to include care therapy as a nursing plan of action. And we wrote it down to motivate people: Today Pedro spoke to his daughter.
I am in leadership, but I also work alongside people a lot. We get together and talk: How are you? How are you feeling? And when I am really tired I tell them I am, because we are all in this together. Less than a month ago, quality management started a pilot scheme called Safety Pause, which is four safety questions asked of staff. One key question is: How are you at the start of this shift? Every day, in less than ten minutes, each one is asked to tell us how they feel at the start of their shift.
How has this been for me? Well, my mother died in February. It wasn’t Covid. She deteriorated very quickly, was brought to the clinic and died in adult intensive care at the age of 88. That was very difficult. I live with my husband and my two children, Emilio, aged 13, and Josefa, aged 12. Our house has two floors, and they set up home on the top, whilst I lived on the first floor. My husband was laid off in March, in the middle of all of this. That was both a bad and a good thing. He helped a lot with the children and the house, and also retrained. He started cooking and selling beautiful things and is doing really well now.
My children have seen how their mother is helping and are really proud of me. As my work is mainly planning, I didn’t feel at first that I was on the front line, but there came a time when I did. �
And that was what we did, help other human beings who might have been our relatives, our grandparents, our parents, a cousin, in their time of need.
Unprecedented tsunami
sergio castaño Nurse Sanitas Hospital La Moraleja
Sanitas Hospital La Moraleja
«I haven’t had any rest. I couldn’t, because we had to look after others and forget about ourselves. We doubled up shifts and were at the hospital all day. You had to be really aware of what was going on, because it was all new, and there was new protocol the whole time. Once things were brought under control it was all different, but at the beginning we had no idea what was going on. It hit us like a tsunami - we had no idea of what had hit us. From the first moment we would say: We are not heroes, or martyrs, not at all. I didn’t study nursing to be in a war, but to be in a hospital, helping people».
We are not heroes, we are committed professionals
 donna ritchie Lead Manager Sanitas Healthcare Funding
donna ritchie Lead Manager Sanitas Healthcare Funding
The different sectors of Sanitas work together really well, and that has helped us give the very best care during the pandemic, as we have been able to take advantage of the organisation’s excellent infrastructure. I, along with many colleagues have been released from our usual functions to provide support where it was most needed, which is normally in hospitals or care homes. We have four hospitals, three in Madrid and one in Barcelona, as well as forty-seven care homes throughout Spain.
I think we have been through three very different periods. The first was at the start of March, which was the period of incredulity. Then, in April, when Spain experienced the peak, we were doing everything we could to cope with it. And the third was when the cases started to fall and the pressure eased off a bit.
The care homes are full of older people who often have underlying illnesses, which unfortunately makes them more susceptible to getting seriously ill with Covid. When cases of the virus increased in Spain, the decision was made to close the care homes to visitors. The residents were isolated in their rooms and were tested. I had the opportunity to
lend a hand at one of our homes. In spite of such a difficult situation, my experience at the home was a positive one. There was a great atmosphere, the residents were very well cared for and we had a lot of fun.
In Sanitas, there has been a focus on digitalization for a long time now. When the pandemic came and people had to quarantine we were prepared with a video consultation platform and so we were able to to provide online appointments with over three thousand doctors. Our patients have been able to attend medical consultations from their own homes. As part of our service, Sanitas has an urgent care phone support system. Due to the pandemic, the demand for this service has increased significantly and my colleagues and I have been supporting the team. I attended customers with many different health problems, all affected by the pandemic in one way or another, and some of them in very difficult situations. I am privileged to have had that experience, and the opportunity to help.
The pandemic has brought us many challenges and in order to help us cope, Sanitas offers a psychological support service to its healthcare staff, who are the “indirect victims” of this pandemic. We are not heroes, we are committed professionals, trained for this. One of Bupa’s core values is courage, and there has been plenty of this. We have been able to support each other, but above all we have been able to give the best possible service to our customers, patients and residents who are, at the end of the day, our reason for being. �
Today we value our team and apreciate life more
I have been a nurse at La Zarzuela Hospital for twenty years. Our focus at the beginning was to treat the largest number of patients possible, and to do that we increased our number of ICU beds by almost threefold. We even set up a field hospital so we would have the extra space if we needed it. We also worked with the public health service to treat more patients. I think we have done a really good job both in terms of the hospital itself and its employees.
Patients would come in with underlying conditions and a very poor prognosis. Health recommendations were that we should not allow any visitors, in order to avoid community transmission. It was an ethical dilemma, because a dying person is normally surrounded by their loved ones.
 mª gloria marinas Nurse Sanitas Hospital La Zarzuela
mª gloria marinas Nurse Sanitas Hospital La Zarzuela
All of it made us very tired. There were days I would get home and it would make me cry to speak with someone who could actually hear me properly. I think I needed to offload all that anxiety and pain I had been through.
The emergency room was the place where patients had to say their goodbyes, face the fact they knew they would not make it and would probably not see their families again. I remember when I had to look after someone who was at the end, because they had a serious underlying illness. He was pretty young, in his fifties. His wife could only have a few moments to say goodbye from behind a screen, because visitors were not allowed in the rooms at any time. It was sad to think that this was the last time this couple would see each other. I tried to lighten the situation a bit for the few moments I was there. Then I had to just get on with things.

It was also very stressful changing into full protective equipment each time I went into a different cubicle. This change in working practices made it very hard for us. As well as the technical challenge, being dressed in an overall, mask and screen and then to have to take them all off just as quickly made us anxious. It is hard knowing you are at risk the whole time.
All of it made us very tired. There were days I would get home and it would make me cry to speak with someone who could actually hear me properly. I think I needed to offload all that anxiety and pain I had been through.
You have a lot of pent-up tension, especially because you are worried about your own family. I myself have two children, a girl of 14 and a boy of 11. The first days of the pandemic I would get home really frightened of infecting them. Thank God, that did not happen. My children have really helped me through this. They would say: Mama, don’t worry, if you can get through this, we all can. Give us kisses and hugs They needed those, because their routine and their way of life had also changed radically from one day to another. I know it’s been hard for my son not being able to see his friends like he used to when he went to school, as he relied on his friends for a lot of things. My daughter, being that bit older, has managed her frustration better. We are all having a hard time and we need to stick together.
MADRID — SPAIN
I think this disease has come to stay. It’s really difficult to stop it completely, but I know they are working on a vaccine, which is key for the most vulnerable people. We have managed to slow the spread of the pandemic by using masks and washing our hands. I think with winter coming it’s going to get difficult again, because October and November are the months when respiratory diseases usually spread. Respiratory problems will increase and there will be more fevers, and we will have to work out whether it’s Covid or the cold virus.
Of course, we are worried about the situation getting really bad again, but we know so much more now and we are stronger. Now we value our team and appreciate life. �
Patients did not die alone
 lidia gómez Nurse
lidia gómez Nurse
Sanitas Hospital La Zarzuela
«We were very concerned about the last moments, the care and affection that people need. At our centres, patients did not die alone. We would hate the families to feel that people died alone. So we decided to write a little letter along with the personal belongings handed over to the family. A small note, telling them how our team had been there with their loved one at the end».
We just hoped for a miracle
natalia castañeda Nurse Bupa Santiago HospitalLooking after Covid patients was initially a professional challenge and a learning curve for me. Over time, I also realised that it was also an emotional challenge, because of the fact that patients were alone. Worse than being sick was the anguish of not being able to see their loved ones or have anyone with them. That is such an important factor in patient recovery.
At the start of the pandemic, some of my colleagues passed the virus to their families. The teams began to diminish in numbers and we had to take on new people. It was like an earthquake. It was all very draining.
I had stopped seeing my grandparents when I started working with Covid patients, because I didn’t want to expose them to the virus. At the beginning I thought about even moving out of my home, as I live with my elderly mother and my young nieces. I was so worried about passing the disease to them and would be so careful when I got back from a shift. I remember in May my grandmother and my mother were a bit sad that they wouldn’t be able to spend Mother’s Day together, but that was the way it was.
I knew what was likely to happen next in technical terms, but I was his granddaughter and I didn’t want him to die. Inside me, I was hoping for a miracle.
One day my grandfather, Osvaldo, who is 88 years old, started to have sleeping problems and didn’t feel well. He had a chronic lung problem, and a medical team came to see him at his home. The diagnosis was pneumonia. Because of the pandemic and his symptoms, the whole family had to have a pcr test. The next day we got the news: the test was positive for Covid. He had been out to collect his pension a few days earlier. The trip out was only about half an hour, but it was enough to infect everyone.
The week of 20 May, my grandfather Osvaldo was very ill and my family knew they had to do something, because he was too unwell to stay at home. I decided to take him to the clinic where I worked and where I have colleagues. Where would he get the best care?

It was a really difficult week for the country because there weren’t enough beds and we were at the peak of the infections, and they were setting up ICU beds in the emergency unit. I had never seen people sitting on seats outside a hospital before. We had to find more spaces for
more patients, because we had to move them from the emergency unit. At first, my grandfather had to wait at the hospital, where he had been taken urgently, for an intensive care bed.
CHILE
SANTIAGO
He was always very aware and never got confused. He knew very well where he was and what worried him the most was that he might not be allowed home. He said to me: Take me home, I don’t want to be here. I told him: Tata, I can’t take you home - I would if I could.
I knew what was likely to happen next in technical terms, but I was his granddaughter and I didn’t want him to die. I was hoping for a miracle. It was very sad because normally, as a nurse, I would be giving hope to the families, but this time I was both a nurse and a family member.
I talked to the medical team about treatment options, which I then passed on to my family my mother and her brothers who had always trusted me.

Things started to get worse, and he needed oxygen and became distressed. That was the second last day I saw him. One of the doctors told me that there was the chance to move him to the intensive care unit to put him on mechanical, non-invasive ventilation, which would help him to breathe but wasn’t like intubation. There was nothing else for it, because he had severe pneumonia and an underlying lung disease that was hardly letting him breathe. He died the next day.
My grandfather, Osvaldo, was like a father to me. He and my grandmother, Edelmira (even though everyone calls her Rosa) brought me up for 20 years.
So his death was very painful to me. I am consoled by the thought that I really made the most of them both.
My grandmother, who had Alzheimer’s, was always asking me: You took Osvaldo away, when are you bringing him back? She must have felt like a part of her had gone with him. They had 70 years together and I know they were very happy.
I am happy I had the chance to say goodbye to him, and he was happy to have someone he knew by his side. He was not alone. I wanted to be a paediatric nurse, but life brought me adult patients. If that hadn’t happened, I probably wouldn’t have been able to be at my grandfather’s side. I feel I was able to bring dignity into his last days. I am happy he could slip away peacefully with his hand in mine.
Then I got sick myself. But that’s another story. �
We care for each patient, as if they were the only one
 adolfo vásquez Nurse Bupa Reñaca Hospital
adolfo vásquez Nurse Bupa Reñaca Hospital
I started working at the hospital last year, before the pandemic started. I was asked to cover the medical and surgery wards, where we care for patients who have been hospitalised and are Covid positive. They had no symptoms, no serious respiratory problems and were stable. By our ratings, they were medium level of difficulty.
The patients were totally isolated. The only chance they had to see us was when they talked to someone from the clinical team, which was usually the nurse who went in to do exams or give medicine. Many patients felt like having conversation and talked to us about their lives; they had not seen their families for one or two weeks. You would grow close to them and those were special times on our shifts.
What was not so good was when you would arrive, for example, at room 405, where a patient that you had been caring for all week had been , and they were no longer there. You would ask: Oh, what happened to that patient? They had been transferred to intermediate because they had got worse. Then you would ask intermediate and they had gone to icu and next thing you knew they had passed away.
At those times, we would think of our patients who had passed away and had children. I am from Villa Alemana and
— CHILE
I have two children. When I got home, I would act as if I had the virus, which was a good thing in terms of being careful, but at the same time I really just wanted to get home, rest and hug my children.
I think I chose a good profession and I think healthcare workers really have a generous spirit. Everyone who works in health - because you get cleaning people, service assistants, paramedics, nurses and doctors, all working with Covid patients. They are all really professional and caring, looking after each person as an individual. If the person is in pain, they are there, if they deteriorate, they quickly check up on them.
Even though there are lots of patients, each one is treated as if they were the only one. Each time one of them is discharged we are happy and it lifts our spirits - we know we have done well and saved a life. �
A traumatic night shift
mª eugenia fernández Healthcare Supervisor Sanitas Healthcare Funding«I work in management and when the Covid crisis got worse I saw that they didn’t have enough staff in the hospitals and I volunteered to cover shifts where it was needed. I was at the Virgen del Mar hospital. Now I just need to rest, be with my family, read a book or just sleep. I feel such pain because
— SPAIN
I have seen terror on people’s faces, like in a war. I won’t forget them, and I have my memories in a journal, because each one had their own story and they touched my heart. I remember a woman who was widowed. She hung around days after she had been discharged. She was afraid to go home because her husband wouldn’t be there».
I take my hat off to my team
yolanda huerta Nurse Bupa Antofagasta HospitalOur work was to calm and reassure cancer patients, who were concerned that because of the pandemic or the lockdown their treatment would be stopped.

The first thing we did was call our cancer patients, remind them of the prevention guidelines to help protect themselves from the virus, inform them of how their appointments would be dealt with, encourage them to only leave their homes when absolutely necessary. Finally, we provided them with our mobile number so they could ring us if they had any questions. It was a mammoth task.
Our patients are aged between 26 and 90 years old and they are immunocompromised and therefore very vulnerable to Covid.
If anyone was ill and had to come to the emergency unit, we would work together with the emergency manager so that the patient didn’t have to wait and could come in quickly. Our objective was to protect them from any unnecessary risk.
It is sad to see how people haven’t really taken it on board and are just walking around the streets freely. It is so different to how it has been for us here in the firing line, leaving our families, changing our way of life and working double or triple shifts.
For most of our cancer patients, the centre is like their second home. We are very close to them. They tell us: You cheer us up every day, you sort things out for us, you are always smiling. That’s why a patient’s death is not easy for us and not easy to tell the family. You suffer, because you have grown to love them too, but you have to be happy and positive. At times like that, a hug means so much, and we can’t give one.
The doctors have been very protective of us, trying to keep us from getting Covid or from infecting the patients. That’s why we would have 14-day shifts.
As coordinator of the oncology centre, I am so proud of my team. It’s been hard over these past months but they have been amazing. We have looked after each other and thank God, nobody has caught it. The team’s families have also been well. I take my hat off to them. �
When you are caring for people you don’t feel any fear
natalia sáez Nurse Sanitas Hospital La MoralejaThe operating room stopped functioning and within a week we had converted it into an intensive care unit and from then on we had intensive care nurses. The work was completely different. We had to change the way we worked and learn to move about in all that protective clothing that slowed us down.
At the beginning, they said it was older people who were more affected, but then patients of my age started to come in and that made us really worried. We felt really sorry for them, because young people were coming in who had children, and they were really unwell.
We were used to seeing patients for one or two hours at a time. We were spending eight hours a day with these patients. It was strange how aggressive the virus was. It would come in quietly and within a few days the person was really ill and didn’t seem to recover. They would be ill for weeks and not get better. We had never seen that before. I told my family that although I had never been in a war, I could imagine that this was a bit like nursing in a war zone.
When you left your house you would get to the hospital and think: My God, I am scared to go in! But once you went in you would forget your fear. When you are looking after people you are not afraid, you are just giving your best. Then you would come out of there and start to think again about how you could pass it to those who were waiting for you at home.
Recently, in April, we started to get some control of the situation. From then, we started to see people getting better. I think it was a short time before Easter, around 7 or 8 April, when we managed to get the tubes off the first patient we had in the icu, which was a really great moment, seeing people getting better, leaving, gave the whole team a lot of hope.
I usually worked the morning shift, but then there were no set times, you could work morning, night or afternoon, depending on what was needed. Sometimes we worked back to back shifts.
Now, the hospital is no longer overwhelmed. Now we are doing more pcr tests and we find there are people who are infected who we wouldn’t have tested before. It’s not like it was in March. Now the people coming in are not so critically ill. But it could happen that within a month we end up like we were at the end of March, which would be awful.
I remember a patient only a couple of years older than me who
MADRID — SPAIN
had to have a tracheotomy. When he woke up he couldn’t speak. He was upset with everyone and we couldn’t understand him and tried to tell him: Don’t worry, you’re awake, everything’s fine. We couldn’t understand why he was so upset, and we gave him a board and he wrote on it for us. He was upset because he didn’t know anything about his family and thought his wife and children had died of Covid. That was the most touching moment for me. It still gives me goosebumps. He knew his telephone number by heart and wrote it down and we rang his wife and his children, aged 15 and 16 years old. They all cried. He asked them about his parents and they were well too. He was the only one in the family who got really sick. Later, when he recovered, he sent us a lovely card and some sweets.

Personally, the best thing was the teamwork and the support from colleagues. Sometimes you get on better with one or another, but now we are all so united that we have worked together really well. This was a very different time, one that we will never experience again. We all go back to our own lives and routines and forget the moment.
I don’t know how we did it, I really don’t. I hope they develop a vaccine and are able to vaccinate the majority of the population, but I don’t think that’s the whole answer. I imagine this will go on for a while, perhaps one or two years.
Now I am worried about the children going back to school in a fortnight, perhaps not so much for the younger ones, but for the older ones. I think the measures they are putting in are good and I think the children need to be with their peers again. My daughter of 10 years old wants to go back, but the little one, who is 5, likes being at home with us.
My husband has been remote working and has looked after everything the house, the children, everything. The hospital gave us the chance to stay for free in apartments that they rented for us. But my husband preferred me to be with them, and I felt the same. We have taken a small break, in a little village in Ávila, where my parents are from, very close to Madrid. I have been a nurse for twenty-two years and I think I am going to go back to it with more enthusiasm than ever. �
We managed to take the tubes off the first patient we had in icu, and that was a great moment.
People were anxious when they called
alejandra llorente Projects and Innovation Sanitas Healthcare FundingMADRID — SPAIN
At the beginning, it was very difficult, because in the 24 hour telephone support service we usually took a maximum of a thousand calls a day, but now we were taking up to about 4,500. We all had to answer them, no matter what our role, because it was important not to let our health centre collapse.
In the middle of the pandemic we were able to help people by phone thanks to our digital health programmes. We have been working with these systems for ten years. We also have video calls too and soon we hope to offer our health programmes digitally, through an app .

In the health promotion service we give support using an online platform with a team of health professionals made up of doctors, nurses, nutritionists and psychologists. We all use phone, video and chat to talk to our customers. We also have a 24-hour service to manage potential emergencies, sending ambulances or staff to peoples’ homes - doctors, nurses and even oxygen therapists.
The huge increase in the number of calls was due to peoples’ fears. It was difficult for us to answer them quickly and sometimes they had to wait quite a while or we called them back thinking: My God! What am I going to say to this person? And then, at the other end of the phone was a person who was so grateful, because they just wanted to be reassured that they were doing the right thing.
Now, in the month of August, we are seeing another surge in cases. There are a lot of surges in Spain and we are very worried about how it will be in September. Now that they are finding a lot of asymptomatic people, people are more uncertain about what is going to happen. That is one of the most common reasons customers call, because that is what we are going through as a country.
I live with my husband and my two children. We have had to adapt. It is hard, especially as the children are so young. But hey, if they appear in a meeting or someone sees them, it’s not that bad. Everyone understands that you are at home and things are different.
I think we have worked really well and now we need to keep going forward, always giving our best. �
I was lucky to be a nurse
laura alvargonzalez Director of Nursing Hospital Sanitas La MoralejaThe nursing supervisors and I need to be seen to be strong, the ones with the answers, even when we are just as worried as everyone else. The attitude and dedication of the staff is indescribable. I can’t begin to express how proud I have been of our staff, how they have surprised me time and time again in a positive way, and the knowledge we have built up between us in this crisis.
Covid hit our hospital suddenly with our first case, on a Friday. The next week we had reached 50 cases and it carried on like that for the first weeks. On 11 March a state of emergency was declared in Spain and on 18 March the hospital was full, all of them Covid patients. We were forced to cancel every other scheduled appointment, except emergencies. We had to create new circuits and procedures, making almost a whole new organisation. We opened extra units and had to double the number of beds in the hospital and in the intensive care unit and also reinforce our emergency department.
Madrid was one of Spain’s worst-affected areas. There weren’t enough staff they had all been called up by the public health service. We had more and more patients to treat, and management were asking more and more of us. Sometimes I would get cross with my boss, as if the pandemic was his fault. We had to change. We were used to having one patient per room and we had to double them up. It wasn’t just the extra workload, it was the psychological burden.
MADRID — SPAINWe would get to work at seven in the morning and go home at midnight or 1 a.m. the next day. We worked like that for six weeks, without one single day off, because we couldn’t stay at home. We weren’t the only ones nearly all the staff had that attitude, with very few exceptions. They worked double shifts, which was physically and mentally exhausting, and didn’t complain. It wasn’t the work itself that was too much for us, but the helplessness we felt as everything was out of our hands, out of our control and beyond our knowledge.
We have evolved since then in our knowledge of Covid and as a result we work differently now. At the beginning, we were applying treatments that didn’t work with poor results. Little by little, we started to change our procedures, to understand what we were fighting, and this was a great boost for our morale.
One of our successes was the recovery of Juan Antonio, a 53 year old man, our first patient in the new ICU, which was actually the operating room, converted for the purpose. That happened on 29 March. His recovery was an injection of strength for us all. It was also a great and well-deserved reward for the professionals who experienced it. It was the operating room nurses who managed to save a great guy. They were amazing!
I am so lucky to work for this company! We had so many people supporting us. All you had to do was pick up the phone and say: I need masks, more beds, people to look after the children, and our people would come to work willingly, even renting hotel rooms so they didn’t infect their families.
Another key thing was that Sanitas has been working with video appointments for a long time. Our director has insisted on the implementation of digital technology. To be honest, health professionals are very reluctant in some ways, because we like to be able to see and touch things, and because of that, it took over a year to introduce the digital platforms. Then suddenly, Covid forced us to do in one week what would have taken us ten years. Perhaps we will never fully appreciate how far we have come and how much it has meant to be able to hold remote consultations. We must not forget that our non-Covid patients needed and deserved our attention.
In the first weeks the world shut down and patients came in alone, without anyone accompanying them, because we couldn’t control what they touched or whether they were well-protected, and we had to be careful not to spread the disease.
We had to abandon our customary personal touch with patients. Where we knew the person wasn’t going to recover and was going to die soon, we would call the family in to say goodbye, but it was all very cold. We only let them have twenty minutes, and didn’t let them get too close.
But we tried to make up for that with the miracle of technology. We used everything constantly: phones and tablets that the company provided. A lot of farewells were said that way and you felt like you were invading what ought to have been a very private time.
I remember the good moments, of which there were many. We watched lots of patients recover, people who went out stronger and who helped us keep going ourselves.
My family were hugely supportive. I am married, with three children aged 17, 15 and 13 years old. My husband is asthmatic and I was really afraid of passing it to him. I can’t thank him enough for how easy he made it all for me. The first weeks, he worked from home, which helped me be able to be very flexible, and he didn’t let me lift a finger at home. I would open my front door and go straight to my room. The next day, I would have a shower and go back. That was my family relationships for the first two or three weeks non-existent, basically. My husband would say: Forget the house - I will deal with that, you deal with the hospital.
That helped me to be with my team, who were very overworked. I tried to lighten their load and doing analyses and dealing with the deceased so that they didn’t have to deal with the corpse of someone they had got close to.

We were more afraid of the future than the present. There were times when we couldn’t see any light at the end of the tunnel, but after four weeks of lockdown in Spain we started to see a small shaft of light. Where there had been 100 Covid patients waiting to be admitted, it was down to twenty.


I think Covid gave me back the chance to be on the front line with my patients.
Before that, I sometimes wondered why I had studied nursing if I was going to end up in administration. I should have studied business administration, as all I did was project planning, human relations, but no nursing. But after all we have been through I can only say: How lucky I am to have studied nursing!
The most difficult part is behind us and is actually the most gratifying part of my ten years as nursing director. It is really special when your staff tell you that they have felt supported and that they knew they were not alone in the crisis. �
I am so lucky to work for this company! We had so many people supporting us. All you had to do was pick up the phone and say: I need masks, more beds, people to look after the children, and our people would come to work willingly.
Mama, when is this going to end?
«In the paediatric intensive care unit we have had the challenge of looking after adult patients. Even now, we have a smaller number of children, and we still work as a high dependancy unit for adults. I am a mother to twins of 4 years old. As well as the extra shifts due to the pandemic over the past few months, the schools have been closed and I had the added stress of being a teacher to my children. It has been really hard for them. Their friends are in the flat below and they haven’t been able to play with them. They ask me: When is this going to end? When is the coronavirus going away? I sometimes worry that I’ll run out of ideas to entertain them. Until we get the vaccine, we will keep on living this half-life».
REÑACA — CHILE

Facing the crisis as a team
betsy moraga Nurse Clinical ServiceOne thing we have really done well is teamwork. If it wasn’t for the commitment and effort from all the nurses, technicians, paramedics and the management team, we could never have risen to the challenge.

The pandemic has been a difficult situation for us. Everything is different in peoples’ homes. A nurse goes to a patient at home and they are often chronically ill and surrounded by their family. Our service has to go into a home where there are no hospital facilities and we have to give them medical care in that context. If there are any problems, you have to use your initiative, because you don’t have a doctor beside you who you can ask what to do.
Our service is different from others. We care for people in their homes. We have all types of patients some are very sick, others less so. We have built a national network, though the biggest area is in Santiago. We go to Antofagasta, La Serena, Viña del Mar, Puerto Montt, Concepción and Temuco, all with the same working model.
One of the most difficult things has been having resources to meet the demand. We received around 8 to 10 patients per day to free up hospital beds and to care for them in their homes.
I know that the commitment of the team has kept us going and helped us work well and be cheerful and enthusiastic. We have formed a really good loyal network and and we are stronger because of it. �
I enjoyed learning a new role during the pandemic
paulina roa Midwife Bupa Santiago HospitalBefore this, I worked as an emergency midwife in the same clinic. In June, I was asked to take on a new position to help with the pandemic. I was just coming to the end of my maternity leave at home. My baby girl is 8 months and I have another girl of 4 years old. I had the right to continue with my leave, but when I received the call asking to take the helm and to be a resident midwife, I said: Yes, let’s do this, I accept the challenge. It is a challenge, mainly because being a lead midwife can be more difficult, and because there were some new procedures. But it was a really rewarding role, and I was able to rub shoulders with different leaders in different services. It was a great atmosphere, in spite of the situation we were going through.
My work was to manage the beds across the clinic, as well as staffing, and you get an overall perspective and do a bit of everything in the clinic. You are in charge. It is hard work, because you are in charge of planning and you have to help deal with any problems as they arise in any of the areas. What we do as residents is receive all the teams, go through each service looking at staffing, beds, whether there are going to be any potential problems and such. You become like a mother in the company.
One of the most difficult things I had to contend with was that when a patient died of Covid, the resident had to be an eye-witness. You had to console the families, many of whom had not seen the person before they died. It was the last chance to do your bit for them at such a difficult time.

Nobody teaches you how to console families, especially in a situation like this, so you have to improvise. Sometimes their situations are so sad and you really feel for them. I would think to myself: If I was that person, what would I want someone to say, or what would I need? Sometimes I would just listen, because words were not enough, and they just needed to feel like someone was there for them, which made them feel better. Feeling listened to and understood helped them more than words. Yet you had to console them whilst social distancing, and that is difficult. I would hug you if I could, but I can’t. But I am here.
For seven months I didn’t see my parents, because both are at-risk, as they have cancer. I preferred not to see them because I love them. It was hard.
Nobody prepares you for such a time, for such a huge health crisis. Your emotions are complicated. Sometimes you say to yourself: Marcela in room 540 could be my mother and she is going through this. It is really shocking. You cry afterwards because you don’t want to make things worse you are there to help. But it’s difficult, and it gets to us all.
Even though it is hard, I have enjoyed this role, although there are things I didn’t know, but the experience has helped me develop. Midwives have some autonomy and this prepares you for decision making, which you have to do constantly in this crisis.

On a personal note, it was quite difficult to leave my daughters 24-hours a day. I did all my work at the hospital and during my breaks, I had to express milk, because my little one was allergic to milk protein, so I couldn’t stop giving her breast milk.
My husband was massively supportive. He told me he would look after the girls. He is a dentist and at the beginning he couldn’t open his surgery. He was with them for the first month. Then he was able to go back to work and my cleaner helped with the girls. She and my husband were a tremendous help.
My 4 year old daughter found it difficult not having mama there at night. I usually lie down with them and read them a story. The littlest one cried a lot before going to sleep, but my husband was able to give her lots of comfort. When I got home, I had been awake for 24-hours, but I would take a shower and start the day playing with my daughters. At the end of such a long period of time awake, I was very tired.
For seven months I didn’t see my parents, because both are at-risk, as they have cancer. I preferred not to see them because I love them. It was hard not to have them there for me, and my daughters didn’t really understand why they couldn’t see their grandparents.
It was tough, but it was a good opportunity, because it has helped
— CHILE
me get where I am today, a supervising midwife with shifts that suit me much better and no more night shifts.
At the clinic we are getting ready for the second wave. Someone said, we are going back into this really difficult situation, perhaps with a different perspective but also perhaps more tired, because we all had such a big shock. The biggest impact it has had on healthcare workers is stress. We are exhausted. Some people still can’t see their family, and that is very stressful, because family are often your support circle, and the people you would normally count on.
I am grateful for the experience of working with really good teams who gave 200% of themselves to help us through this crisis. I confirmed that midwifery is what I love, especially as I got to work in management. I think I was able to make a contribution. �
My small part in the fight against the pandemic
Territorial Quality Coordinator
Bupa Chile
«Currently, I don’t work in a hospital, but in the healthcare management field. I have worked in front-line nursing all my professional life and that is why I was very happy during this crisis to have been able to be there with the teams and make my own little contribution to the fight against the pandemic. I have had the benefit of a different perspective, looking from the outside in, but still part of it, knowing the protocols and able to suggest improvements and innovation in real-time. I have worked hand-in-hand with the hospitals and medical centres where, for example, we have created a system of control points to minimise the spread».

When you are the patient you feel vulnerable
Nurse Bupa Santiago HospitalCHILE
A week before I had obvious symptoms I had backache, but I thought it was because I had been moving patients around. However, that evening the doctor checked me over and found a noise on my lungs.
When you are the patient you feel vulnerable. I was one of the first people to be tested. The scan showed nothing and the pcr test was negative. A week later I felt terrible, shivering and with a headache. I took my temperature in the afternoon and I had a fever. I was taken off the shift immediately. I felt bad abandoning the team, because it meant they would have to work harder.
They took me to the medical centre, but the doctor checked me over and sent me back to emergency for an x-ray because my pulse was very high. I had to be admitted by my own team as a patient.
Once I had been assessed, I went home. I live with my parents. I shut myself in my room and waited for the results of the pcr test. I was one of the first people to become ill, and I chose to stay at home. The second pcr test was also negative, but I still had a fever. I had a fever for eleven days. I felt really ill and my parents decided to take me to the emergency department again. That day I got up to have a shower and couldn’t even manage that. I was breathless and found it hard to breathe. I felt like an old person even though I didn’t smoke and didn’t have any other illnesses.
My colleague Bartolomé admitted me. That day Doctor Vargas saw me. She took me for a scan herself, which showed that my lungs were badly affected. I heard them outside the cubicle saying: Oh my, Claudia is really ill. They put me on oxygen and I was in hospital for a week. I lost five kilos because I had no appetite. I was off work for a month. My family were really worried. My mother looked after me. Thankfully, none of them got sick, not even my brother.
SANTIAGO
I went back ready to fight the pandemic and empathise with the patients, give them everything they needed, especially someone by their side and someone to talk to. Because the person in that cubicle is completely lost, lost in time and space. The disease means you have to be alone. I lived through it. �
I remember how lonely the patients felt
Bupa Santiago HospitalBefore the pandemic, I had always worked in clinical risk, which was mainly about adverse events in healthcare and preventing and monitoring the occurrence of these.
I have been a nurse since 2001 and have worked in a lot of healthcare settings, various intensive care units and lots of different hospitals. I am passionate about working directly with patients.

Working in quality, on the other hand, is about looking in from above, watching what is going on. That is why I wanted to go back to shift work so I could work more closely in health in the pandemic.
It was Carla, the nursing director, who realised I wanted to have a more active role and gave me the opportunity to take on a new position that was available at the clinic, that of resident nurse, just when we had entered the peak of the pandemic. I talked about it with my family, who didn’t like it much. My husband said: You will be more exposed to the disease, but if it’s what you want, you should do it.
claudia collao NurseAs the resident nurse, I had to visit the whole clinic. I felt like crying, especially in the emergency unit. I feel like crying when I think about those days, because we were stretched to the limits.
Four of us got together and took on this new role. As more and more people got the disease, things heated up. We could see that everyone was giving their utmost on every shift. Sometimes it seemed really chaotic. It was very stressful for everyone the patients, the healthcare teams and the administrative teams who, although they were “invisible” were supporting everyone with standards and procedures.
At the same time, my boss took on my usual functions so I could get right into the new role. A lot was asked of all of us. For example, there was a time when we had to set up a pre-emergency section, where we set up some chairs for people to sit on before they got through to the old emergency section, because there weren’t enough spaces.
The nurses were doing 24-hour shifts and often got no rest at all, because it was relentless. At five or six in the morning we were moving patients. Everyone was worn out and exhausted. People just kept coming and coming and we had to hospitalise them temporarily in the emergency department.
It was really hard having to wear the mask all day. You felt you couldn’t get enough air, and it was worse for colleagues working 24-hour
shifts. You would find people without their masks on and they would say: I am just having a breather, I feel like I am drowning. When we were at a distance from others we could be a little bit more relaxed, taking down the mask for a few moments. A lot of colleagues had sores on the end of their noses, even when they sewed on patches to protect them.
As the resident nurse, I had to visit the whole clinic. You felt like crying, especially in the emergency unit. I feel emotional when I think about those days, because we were stretched to the limits, anxious and often felt like everything was completely out of control. I remember the will people had to live. I remember the loneliness of the patients in the emergency rooms with the lights off so they could rest and you would open the door a crack and there was a person all curled up and just about breathing.
We went through so much anguish and grief, but there were also unexpected and even magical moments. Comforting situations where you could really be there for people. I remember another colleague who was also a resident. She said to me on my shift, Claudia, I am here, can I help you? She had finished her shift and was also tired, but we took a break and had coffee together. Such gestures were very precious to me.
As for triumphs, there were little victories on each shift just finishing a shift was a victory. Being able to say in the morning: these patients are well enough to be moved, but this other patient has deteriorated and we transferred them; there weren’t enough staff. At times like that you value the small, daily steps.
Of course, it’s a team effort. There was a period of change and then we got into a new working routine. That was our triumph: being able to get a work flow going in the emergency unit, meaning we had got a handle on the pandemic. Now, the hospital is getting back to normal and in mid-August we are assessing and making the necessary changes.

I don’t want people to see me as a hero this is my vocation and my profession. I studied to look after patients, not to get a statue made of me. When I decided to go to university, why did I choose nursing? Because my mother is a nursing auxiliary and she encouraged me. Then I realised that since a child this was what I had been doing when I cared for my mother by putting wet flannels on her when she had a fever. It was what I wanted to study and what I wanted to do.
I am happy to have been in the line of fire, and I will never forget it. �
I never lost my strength
violeta carrión Nurse Sanitas Jardines de Sabatini MADRID — SPAINOne morning on my shift, at the end of March, I was taking temperatures and one of our older residents had a temperature of 38.3 °C. In that moment, I got a fright and thought the thermometer must be wrong. I tried with another, but it still came out at 38 °C. Literally seconds later, he started to cough and seemed really ill. He destabilised in moments and his oxygen saturation levels were very low. I remember what a chaotic morning that was. I was lucky that a doctor came straight away, assessed him and sent him to hospital. When he went on that stretcher, nearly all the staff gathered round to say goodbye. We could see how unwell he was.
We soon found out he was Covid positive and he died a few days later. From that moment, when we had our first positive case, cases started increasing at the home.

I am 28 years old and I live alone. Obviously, I didn’t want to visit my parents or relatives. In April, at the peak, I found it very difficult and was very stressed. To add to it, my sister told me my parents had Covid symptoms. That was when I said, If anything happens to my family, I can’t go on. I lost seven kilos and had no appetite for eating or for anything else.
My parents did actually turn out to be positive, but thankfully they weren’t severly ill. When I realised what a state I was in, I talked to people, particularly my sister, and decided to change my chip. I tried to spend my spare time doing something I enjoyed. Then the infection rates started to go down a bit and I started to feel better.
I never gave up and I always remembered: These patients are all we have and we can’t let them down. We need to give them all we have.
The families called us because they needed us to comfort and calm the residents for them. Sometimes you don’t have that peace yourself, so it is hard to give it to others.
Now that family members can visit their elderly relatives and can see how well we have looked after them, I am really encouraged. �
I wouldn’t change what I went through
On 10 June I woke up with no sense of taste or smell, which we call anosmia and ageusia. I couldn’t taste anything. I called my boss, Carol, and said: I don’t have any taste or smell, I am scared. She said: come to the hospital straight away and we will do the pcr test. Then I went into quarantine. My first pcr test was negative but a second one, fifteen days later, was positive.

I was infected by a patient who had Covid and had an anxiety disorder that was not well-controlled. I was coming off my break and he was having a crisis in the corridor and I had to put cold compresses on him. He came in walking and an hour later he was confused, aggressive and needed a ventilator. He was 58 years old and had no underlying illnesses. This happens with hypoxia: the lack of oxygen in the brain makes them confused and overwhelmed.
It was really difficult to keep a distance from my family. I knew I had Covid, even though the first PCR test was negative, because the symptoms were obvious. I am the oldest daughter. I have a sister of 21 years old and my parents are still young, so we have a great relationship. Telling my parents I was ill and they couldn’t come over but not to worry was hard. They left me food at the door. I would just put the rubbish out.
constanza núñez Nurse Bupa Reñaca Hospital BearingIt took me a month to get over it that was the longest month ever. I felt that I wouldn’t die of Covid. I think I was most afraid of getting a blood clot, so I tried to do exercises lying down, as I spent all the time lying down. I couldn’t get up. I didn’t have enough breath to get up. Just going to the bathroom was awful. I would shower sat on the tub. The steam suffocated me. Everything was horrible. I lost six kilos, but I kept going.
As I had a high fever, I didn’t even really know what was going on. If the world had ended I would have ended with it. I wasn’t fully aware of anything.
On 30 June I started to be able to smell a few things again. I remember crying when I could smell coffee again.
I went back to work on 13 July. I knew I would have to get used to using a mask again, so two days before going back, I spent the day wearing it to get me used to full-time mask wearing.
I am one of the lucky ones because once I recovered, my scans came out clean. I don’t have any after effects except a bit of a cough which might last a long time.
As a hospital, in the Region of Valparaíso we had just one emergency department until March, and everything was dealt with there. From one week to another we divided up the work flow and the emergencies and that was when we started using surgical masks and full gear.
If the world had ended I would have ended with it. I wasn’t fully aware of anything.
During the first few weeks of April the virus was getting out of hand and we started to see changes in symptoms: at first it was just fever and respiratory symptoms, then in the first weeks of May gastrointestinal symptoms and then people with diarrhoea and vomiting were also suspected of having Covid. In April, we saw the first respiratory problems: someone who came into the hospital with normal saturation levels and after less than an hour their levels went down and they needed urgent mechanical ventilation. In July, patients were coming in in a worse state, because people were afraid of coming in and waited until the last minute at home. So they would come into the emergency department, already gravely ill.
Covid is airborne, so although nebulisers are useful we can’t use them, because the virus is transmitted that way.
The other thing that made it difficult during the pandemic was the way we dealt with Covid patients. As soon as they were being treated, accompanying people and visitors were restricted, so people preferred not to come to hospital if possible.

Personally, I think alongside the vaccine, health education is what will change things. They will be small changes, but they are needed and we will need to live with them. For example, hand-washing, which people weren’t very aware of before, but is now an essential part of our habits.
We are social beings and have found it difficult to keep our distance from each other. I think there will be consequences to this difficulty to get close to people. Going back to work, for example, I found out that a paramedic on our team had been diagnosed with terminal cancer. We are supporting each other and taking it a day at a time. We have aromatherapy, background music and group activities, but I think after the pandemic we will need to get more personal, closer to people.
I have been an emergency nurse at the clinic for five years. I am 28 years old and have never doubted that this is what I am here for. Nursing is my life and breath. I love it. I wouldn’t change from nursing, or change what I went through. I am thankful for the opportunity to develop professionally and I wouldn’t change my job for the world. �
I volunteered to help my colleagues
In the past, our phone calls would be emergency calls and would last three or four minutes. Now they last from ten to fifteen minutes because we are dealing with patients’ worries.

On 8 January I became the father of twins, Mateo and Bruno, who are now six and a half months old. My partner’s name is Natalia. She is a nutritionist. We are both on maternity and paternity leave at the moment. I was due back at work on 12 May. Once I had agreed that with my partner, I volunteered to do telephone triage. I couldn’t stay at home watching the news on TV, and decided to support my colleagues because I was afraid my unit was falling apart. We were used to getting between 800 to 900 calls a day and around 20 to 30 emergency video appointments. Now we have around 6,500 calls a day and do over 200 video appointments.
I went to the office to get the computer equipment and set up the new office in the children’s bedroom. As they are twins and still small, we cleared out their room and had them in cribs on each side of our own bed. Then I started doing triage.
At first, I just did calls, as there were a lot of people waiting. We were used to three or four minute calls, which is normal in the emergency unit, responding to all types of emergencies, from patients with headaches to people who were unconscious. But we were now spending ten or fifteen minutes on calls and many of our patients were very worried.
We couldn’t meet the demand of the volume of calls we were receiving, so we recruited new team members and even asked for volunteers from other Sanitas departments. Together with my boss, we decided that I would provide training on the IT systems. Before that, healthcare staff were used to seeing people face to face, not virtually, and this was a big change.
In my case, being a father, I couldn’t stick to exact work hours. I would fit the work around other duties in the day. You think your first experience as a father will be all lovely and in a bubble, although obviously you are worried about your children being born and growing up healthy. My experience is different to that, very unique in all sorts of ways. �
SPAIN
óscar cruz
Sanitas 24 hours Coordinator
Sanitas Healthcare Funding
I got Covid
rosa larios Nurse Hospital Virgen del MarI have managed to get the fatigue under control. I do my breathing exercises and all that, but I still have muscle aches, particularly in my legs.
When we started the year we saw on tv about the virus in China, but never imagined it would affect us so profoundly. It crept up on us suddenly. First there were two or three patients, then it suddenly grew. All the beds filled up and people came in very unwell, with fever and problems with oxygen saturation levels. We didn’t know what to do. You would come out of a room and find another person had died.
I have lived in Spain for twelve years and worked at this clinic for ten of them. I am single and my whole family, who live in Peru, have been very worried. I have no family here, only friends. I had been hoping to visit my family in October, but I couldn’t.
At the end of March I was on a night shift and started to feel the symptoms coming on. I did the pcr test at the same hospital and it was positive. When I went home I felt I was going to be fine and I would be able to control it, but that’s not how it went. I ended up having to go to hospital and all in all I was in hospital for a month and four days.
My colleagues were so kind to me. I know it was very strange for them to now have me as a patient. I didn’t have to be intubated, just given oxygen. What kept me in hospital longer was the fever. Then I got better and was able to come home.
MADRID — SPAIN
I was really unwell in April. I could hardly walk, my legs were sore and I was very tired. I set myself exercises for the morning and afternoon and gradually improved.
I went back to work at the end of June. I really wanted to go back but I must say I am a bit afraid.
I wasn’t the only one who got Covid. One colleague was intubated and another in hospital for seven days, but has already managed to go back to work. Another colleague has recovered but isn’t back at work yet. It seems they have neurological problems. This virus has many after effectssometimes it’s fatigue. In my case, it’s pains in my legs.
My colleagues were my nurses and I was the patient. �
I love what I do -
I always wanted to be a nurse
grace vera Nurse IntegraMédica Outpatients ClinicsI am 33 years old. Until 2014 I was an auxiliary, and then I studied nursing. I have been working since the beginning of the pandemic, when my baby was only five and a half months old. My family has criticised me a lot, even my mother. She says I should ask for time off and shouldn’t be exposing my baby at such a young age.
My little one is called Dante and he was born on 27 July last year, 2019. I finished my maternity leave and went straight back to work, so I had to stop breastfeeding at that point. He stayed at my home in my house in Buin, looked after by Carolina, his nanny.
People in my family would say I was a bad mother, but I would say: I will take all the precautions as a professional, using all the equipment, and I won’t get it. I studied for this and I need to get involved, as it’s what I wanted. I can’t get away from what I do, and I do it with love.

I have always been keen to come and work, because of everything that is happening. I have a good relationship with my team at work, and I feel I have helped them keep the stress levels down. I am lucky that my partner understands me and has been really supportive.
Until March, I worked on the endoscopy ward as normal, but when the pandemic arrived we had to stop the endoscopy because of the risks, and then I started doing the pcr tests to check for Covid.
I stand by my decision to keep working, because I have always wanted to be a nurse, since I was a child. I never dreamt of doing anything else.

We used to work with basic safety equipment, but that has all changed. We started using the face shield and special masks, as well as being very careful when putting on and taking off the protective clothes. There were new procedures every day, which was stressful for the team. The hardest time was when my two colleagues got infected and I had to work on my own.
Buin was one of the communities that was put under lockdown and that affected public transport. I had to start driving. I did have a licence but didn’t drive because I was afraid of the motorway. I would only go as far as the supermarket in Buin. But going on the metro would have exposed me more, all of a sudden I had to start driving on the motorway. At first, I drove really slowly in the slow lane, but I soon got used to driving to and from work. I did all that to protect my son more.
We were lucky that my husband’s working day was shortened and he was able to spend more time with our son. Then there was Carolina, who I trust completely. My son doesn’t even cry when I leave for work, so that means all is well. We communicate during the day. She also trusts me and knows I take all the necessary precautions.
To start with, the demand for tests was crazy. Between March and April it was very high, because everyone needed to be tested. At one point we had 100 a day. Later it got more selective, because we would do a more detailed triage and look at the symptoms more closely.
At first, we would do the pcr with a swab or a cotton bud, then we started doing tests by using a syringe to collect secretions. And of course, always using the protective equipment. Now it’s August and it has gone down a lot. For the last three weeks floor 7, the Covid floor, has been quiet. We only do about five tests a day.
Nowadays you can get a pcr test result in 48 hours. It is pretty effective, though of course the results are not always correct. The doctors tell us there is a certain percentage of false negatives. I know of three cases of a negative PCR and the person had all the symptoms fever, cough, etc.

As far as mental health goes, I spend a lot of time talking to God, but sometimes I explode and some days I cry a lot. I think my working environment is a very good one. On some of my worst days, I have been supported by colleagues and we have had a laugh together and felt better. At times, when I have had a meltdown, I have had to shut myself in the bathroom and pray and ask God to
SANTIAGO —help me calm down before I went back on my shift.
In the midst of this pandemic, we have built a really good atmosphere of trust. There was one point where I had to stand in for my boss, because she got Covid. I have always been quiet and worked behind the scenes. Two weeks ago I was invited to apply for a management post in the medical centre. I felt really honoured to be invited and to grow skills that I didn’t know I had, in decision making and leadership. Amongst all the stress of the pandemic, this has been a high point for me.
I stand by my decision to keep working, because I have always wanted to be a nurse, since I was a child. I never dreamt of doing anything else. Since fourth grade, I knew this was what I wanted to do. I did actually start off studying as a nursing auxiliary, for financial reasons, but I really wanted to be a nurse. �
Educating, guiding and accompanying our patients
 Outpatients
Outpatients
I am part of a specialised call team set up to triage positive patients and follow them up.
The main problem is older adults, who are more likely to get seriously ill. They also get very scared, and we need to help and calm them on the phone. We do a complete health assessment so we can pinpoint the problem. We have a set of questions designed to get the most information possible in the shortest period of time. If the person has respiratory symptoms and difficulty breathing, we make them an urgent appointment to come in.
When we have told a positive patient to isolate, most of them understand. But sometimes I would call a patient and they would be out and about when they answered. Then I would say to them: Even though you feel fine, it doesn’t mean you might not pass it on to others.
I am also responsible for managing home visits, video appointments or support with sick leave paperwork. On top of the illness, many of the people who needed sick leave were worried about losing their jobs.
I only graduated a year ago, so having to work in the pandemic has been a real challenge, because people are
really suffering. June was the toughest month, emotionally. I would call some of my follow-up patients and find out they had died. I imagined us getting to the point of piling up bodies and not being able to give people proper funerals. I would have hated that. But thankfully it didn’t come to that.
Nurses are very close to patients. In our call team we have a complete protocol, a kind of Covid guide, written in very accessible language so people can understand it.
I think that nurses have been very important at this time, not just in primary care but also in our roles as educators and in health promotion. �
A time of fast learning and great camaraderie
I am a theatre nurse and during the pandemic our hospital was a hospital of reference for covid. That meant we took patients from both the public and the private sector. Our hospital has six floors. It isn’t very big. But we do a lot of surgery. We have ten operating rooms and around 87 beds. We had to turn these operating rooms into intensive care units, especially the recuperation areas and another part that was more for patient induction. We put intubated patients there. We even had to turn anaesthetic machines into respirators.
When I got ill at the end of January/ beginning of February I was very ill, but Covid was still quite uncommon. I personally had symptoms: I felt breathless, I was very tired and I had a temperature of 38.5 °C. I spent some days in bed. I hardly ever get that sick. I spent two days sweating, feeling awful and had a dry cough.
 maría gonzález Nurse Hospital cima Sanitas
Bearing
maría gonzález Nurse Hospital cima Sanitas
Bearing
We were very scared at the beginning. You could see it on everyone’s faces. But we were all really supportive of each other and learnt from each other. What one didn’t know, the other taught them.
I started to take a load of things, including natural plant medicines and my usual medication. When I recovered, I had no sense of smell or taste, at a time when we didn’t know about Covid yet. When the state of emergency was declared, we were tested and I had antibodies.
We were very scared at the beginning. You could see it on everyone’s faces. But we were all really supportive of each other and learnt from each other. What one didn’t know, the other taught them. You have to remember that at the beginning we were not intensive care unit or anaesthesia nurses, but we learnt really quickly and we had respirators and medical pumps. We would change them from their backs to their fronts and in that position, we provided all the care that a critical patient needs. We learnt all this from scratch basically.

I remember once in the icu there was a young man we were giving a procedure to and a psychologist came in with a mobile phone. They would record the families and let the patients hear their voices. They used an iPad so they could see the families and it helped them recover more quickly. This was done whether the patients were awake or asleep, but usually they were all asleep. We would put the phone next to them and their grandchildren, children, wives and other loved ones would talk to them. Once I had to leave a patient’s room and go to the bathroom for a really good cry after hearing a four year old girl saying to her father: Papa, please get better, we want you home.
Patients have recovered and walked out of here without any obvious after effects, though they are obviously quite weak. Some of them come back to see us and bring us sweets and thank you cards to cheer us up.
Thank God, I have a very strong partner at home who has supported me a lot. He also works in healthcare and has good mental health. We would talk about it every day at home. I did a lot of sport and meditated a bit. A while ago I tried to do a very hard climb, almost a 7.5, which was a tough one for me. I fell off the rope but I am fine.
I have pictures from the lockdown in Barcelona at the start of the pandemic, and the


BARCELONA — SPAIN
streets are deserted. I would drive to work and the police would stop me and ask for my travel documents. At the supermarket you had to queue. Once the state of emergency was lifted, we could go back to a bit more normality.
I am Spanish, from the Canary Islands, now I am in El Hierro on holiday, which was originally declared to be Covid free. My family live here and it’s very different from the life we live in Barcelona. We even go to the beach. We wear masks now, but for the first twenty days of August we lived an almost normal life. It’s almost the end of August now and I think there’s going to be another surge, but not as bad as the last one.
Finally, I would like to say that we have a team of colleagues up there who are great. Without the team we wouldn’t have made it. They are all great. They give their all every day! And there is a great team atmosphere. I never worked anywhere as good as this and I have worked in Holland, Belgium, Spain, in Madrid, and the Canary Islands. �
Closer to our patients with cancer
 sonia guerrero Nurse Bupa Santiago Hospital
sonia guerrero Nurse Bupa Santiago Hospital
Some cancer patients are with us for one or two years. There are all ages, from a young person of 17 years old to more elderly people. Other people at risk that we treat are the immunosuppressed with HIV who also have cancer. All of them need special care because of the risk of Covid.
Our patients have had to quarantine since the start of their illness and they know about not getting visitors. In some cases, one family member has been allowed to visit, with a lot of restrictions (masks, robes, distancing) but in other cases that hasn’t been possible because of the high risk, due to their low levels of immunity. They are very responsible people who take great care with all the safety measures and look after themselves and their families.
SANTIAGO — CHILEThe people we look after have highs and lows and can deteriorate very quickly. Cancer patients often get a fever and have to be treated with antibiotics. On the other hand, the patients are constantly hearing messages on the TV, in the media and elsewhere that remind them how vulnerable they are. To support them in this, we have worked together with psycho-oncology and psychiatry.
In our department, the nurses get very close to the patients because we don’t have lots of patients and they tend to stay a long time. This means we can work well with them and give them really comprehensive care.
Thankfully, none of our patients have been infected and I think that is because we have been careful and have worked together as an oncology team and with patients and families. �
Nothing prepares you for this
I am a nurse and the supervisor at Almenara Care Home. Before Covid, it was very peaceful here. It was a well-organised home but then we are in a small village, perhaps a bit cut off and with not many visitors coming in and out. We were preparing for the arrival of the virus, and worried about what would happen.
At the beginning of March we had 106 residents. Everything changed at the end of the month of March, around 21 March a couple of patients developed coughs, though they didn’t have a fever. We immediately quarantined them, partly because we didn’t know much about the symptoms of Covid. On 25 March I could see things were getting difficult and decided to take my son, Martin, to stay with my parents. Then it was just me and my partner.
At the end of March, almost 80% of the residents were sick and we had to take on new staff because a lot of the staff were off sick. At the beginning, nobody wanted to come and work at the home because of Covid. Around 28 March, almost as if by magic, a whole load of young people from El Salvador in Central America turned up, (I call them my angels), who hadn’t lived in Spain long.
— SPAIN
When these young people came along we trained them up in care: how to bathe the residents, feed them and look after them. They were quick learners, which was helpful, because we needed all hands on deck to look after the patients so that we could deal with the medical side.

We have zones in the home a Covid zone and a non-Covid zone, even though when we first tested everyone they had in fact all had contact with infected people, except for five people out of the 106 residents. Everything was sectioned off. Staff were not allowed to mix, not even for a break, never.
The hardest day was in April, when seven residents died. I especially remember one of them, because he was such a warm person and spent a long time with us, and one morning he told us he had had a bad night and at five past eight in the morning when I looked in on him he was very unwell. I remember how helpless I felt and how I started to cry and asked myself: When will all this end?
Residents deteriorated so quickly one minute they were fine and the next they had gone. People between the ages of 71 and 95 or 96 years old. Yet we have residents of 100 years old who have survived. What is the difference? We still don’t know the answer to that.
For a whole, tough month I couldn’t see my son Martin. During that time he had his first birthday and started walking, all without me there. These things are hard, but that is how it is. Once during that time I went to my parents’ house just to leave them some provisions. I kept my distance and didn’t go in or anything, and he saw me and cried and stretched out his little hands to me.
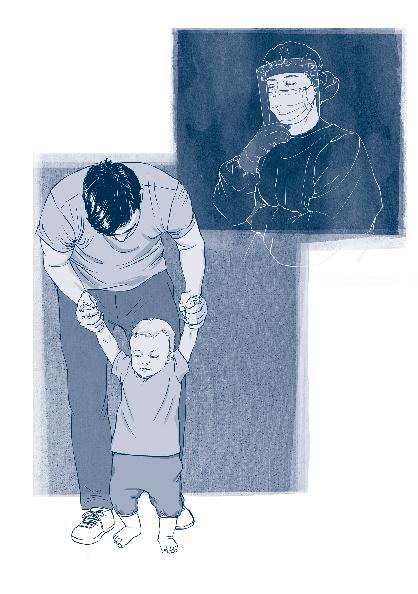
I have had lessons on tropical medicine, where they were talking about major diseases on other continents. But nobody prepares you, either professionally or psychologically, for what we had to go through. It’s not just about healthcare but about what nurses have to suffer when they stand by helpless and watch twenty people die in front of them. The emotional strain is very hard.
It is months since I have slept eight hours on the trot. That’s an obvious repercussion, but at the moment I don’t even really have time to think about it.
As far as mental health goes, Sanitas has provided us with guidance. We also have sessions with a psychologist, but until it all passes and we go back to normality I don’t think we can really take stock of what each of us needs, in psychological terms. We are still going through it.
It is months since I have slept eight hours on the trot. That’s an obvious repercussion, but at the moment I don’t even really have time to think about it.
I don’t know how it is in other countries, but in Spain you either suffer or you move on, that’s how it is. Not everyone knows what it’s like to look at rooms full of corpses! It’s the same with the news, they report as if we weren’t doing anything in the care homes. That really hurts. I love the Sanitas homes and I love my work and I have to say, they don’t know what they’re talking about! I haven’t seen my son for over a month. I have missed a whole load of important milestones in his life, yet I get no recognition for it and still have to hear such rubbish on the news!
To get back to normal, I think we have to recognise what we have been through in this Covid crisis and I hope that one day they will truly recognise our work, not just in the hospitals but in all the care homes too. �
The loneliness pandemic
andrea espiñeira Healthcare Manager Sanitas Healthcare FundingWhen the pandemic started our colleagues in the 24-hour telephone service were overwhelmed with calls, so we started to work together to provide support. My Regional Director asked if I was interested in helping and I never thought twice about it.

GIJÓN — SPAIN
I have always loved being a nurse and working in insurance, I continue to do that, just from a different angle. I started to work for the 24-hour service, gathering information about how the whole system worked. To start with, we knew it was a virus that showed itself in flu-like symptoms, then there were more and more protocols, which I would put up on my kitchen wall near my computer.
I have a daughter of 10 years old and live in Avilés, Asturias. My ex-husband lives really nearby and she has been able to live alternate weeks with each of us. That has been good for us all.
One of the calls that touched me was from a young married couple. The wife was really afraid and anxious. She put her husband on and he told me he had to work a night shift and she would be alone in the house. I told him we were a 24-hour service and your wife can call us at any time of the night and we will look after her. That calmed her down and her husband thanked us for being there.
Another patient asked me if we could do some sort of test so that she could go back to her family in Madrid. She was grieving for her father, she hadn’t been able to be with him and was alone during the lock-down. She was quarantining alone. They were all sad stories. Without a doubt, one of the biggest tragedies of this lockdown and this pandemic is the loneliness and isolation felt by those who get infected and by their families.
There were particularly stressful moments, but we were lucky because the company gave us internet gym courses and psychological support via video call. They also did a series of conferences by a psychologist. Those were fantastic.
I have felt fully supported from the start. I have never felt worried about not having a job and I am very grateful for the opportunity to work with the Sanitas 24-hour service. �
When the patients went home, we celebrated with music and clapping
I have worked for ten years in the Intensive Care Unit. I love this work and I think it’s the best. I have never found it hard to work under the pressure of it. There came a point where I wanted a bit of a change of direction and I changed to x-ray. Now I work in outpatient consultations. As well as working in the hospital, I also work at a care home.

I was really afraid of catching coronavirus. I would go in with my masks and gear until one day they said: Cova! You need to move from outpatient consultations to work in intensive care, because that’s what you know best and your colleagues need you. I remember that day really well, because it all happened at lightning speed, my God! People were dying…
I had worked before as a nurse in intensive care, and there had been people who went into cardiac arrest, strokes, hard stuff, but it wasn’t an everyday occurance. In ten years, I had never seen anything like those worst days. Every day there were people whose hearts stopped, intubations and watching people die. I think that was the hardest thing I ever went through.
covadonga medrano Nurse Virgen del Mar Hospital BearingI hadn’t cried in a long time, I think since my mother died, and this whole time has been so bad, so much fear, so much uncertainty, fear of getting home and wondering: Have I passed it on to my daughters? I have always been strong in the face of fear, and I have been through a lot of times in life when I was afraid, but this made me realise that the most important things are your health and your family. Without those, you are nothing.
When I was in the icu, many colleagues didn’t agree with us using tablets for video calls and phone calls from families. They said it affected the patients too much. Personally, I have seen people respond really well to it, and seeing them lift even a finger or seeing a change in their heartbeat is really important to me. Every day I have worked in icu I have tried to put patients in contact with their families. My colleague and I firmly believe that this works and really helps the patients.

Every time a patient is moved out of intensive care, we have celebrated as if it’s Christmas, with music and applause. Many patients with poor prognosis recovered, who previously looked as though they weren’t going to make it. There are a lot of bright spots like the time when a patient came back the month after they had been discharged, just to thank us. Or there was my colleague Victor, an auxiliary nurse who got really sick, and who sent me a message just to say: Thank you! And how, because I am one of the few who has family, my colleagues would change shifts with me so I could have more days off.

I think I had Covid without symptoms. I am not sure when it was, but there was a time when I felt quite bad, very tired, but it passed. And there were weeks on end where I just worked the whole time, and at two jobs. As well as my home. I would think: Is this normal?
Sometimes I needed to relax, I just wanted to help out at home, and I would say to my husband: let me at least wash up. My husband’s name is Alberto and my daughters are Covadonga, 7 years old, and Carlota, 5 years old, and then there’s Bruno, our dog. The name Covadonga is Asturian and it comes from the name of a battle. The person who has felt it the most is my older daughter. She is very sensitive and was always saying to me:
— SPAIN
mama, please don’t get infected, please don’t do anything at home, why didn’t you choose a different profession? Mama, please help as much as you can, but don’t catch the bug.
I think if I died and came back, I would still choose to be a nurse 100 times over, and I say that to my daughters, my friends and anyone who asks. The song, Resistiré (I will make it through) became our anthem. I have many regrets. The main one is the deaths. Each death feels like a failure. At the same time, I think about how much we fought and I believe we are all winners in this tough situation.
I had a carpal tunnel operation on my hands recently, but I am better now. On 10 September I will probably go back to work, because I still have stitches. I spoke to my supervisor and they told me things are quite bad again. Now, instead of Covid patients occupying one floor like before, they have two. I hope that if things get bad again I can go back and help. �
Every discharge from icu we have treated like Christmas, with music and applause.
No time to think
gonzálezI think the company has looked after the health of its customers right from day one. They tell us to make sure every sick person has everything they need, and that we do all we can to meet every need.
I am a nurse and I have worked in health management for seventeen years. That day in March when they said we were going into lockdown I took home the bare minimum. Just my laptop - that’s about it. I remember it was a Thursday. I thought I would be at home for fifteen days but I didn’t go back to the office until 22 June.
Our colleagues in the call centre in Madrid couldn’t manage all the calls they were receiving and they asked our team for volunteers to help with the call centre and with video calls. The rest of us took on the work of those who were moved to help with the crisis.
Then the hospitals started to collapse and there weren’t enough beds. We had to move people from one centre to another. The Sanitas Hospital in Barcelona became a Covid specialist centre. We tripled the capacity of this hospital. It was really hard, especially the first days and weeks, until the numbers started to go down.
We had to change the patient list every day. I remember once when a patient wasn’t listed on entries or discharges. It was a patient of my own age who had been in ICU for almost a month. I knew him, he was a widower with a son of the

same age as my daughter: 17 years old. The worst thing was to think that boy might lose his other parent. Thankfully, that didn’t happen and the man got better.
At the beginning, families found it hard to all be at home 24-hours a day. But I think we have learnt that our lives were really too busy and we didn’t have any time for reflection.
I also found my teenage daughter difficult at the beginning. She was very stressed, but she became calmer, more thoughtful and helpful, which helped our relationship a lot. My husband spent some time furloughed (unemployed but with a right to part of his salary), but thankfully soon went back to work.
Although it has had its good side, I wouldn’t want to go back to lockdown. �
United as a team
hilda vargas Head of Nursing San José de Arica Hospital«Our profession is very well organised, we work with standards and protocols that must be followed strictly. We have very strict guidelines, and the word “uncertainty” is in itself very stressful for healthcare workers. That is why it has been very important to keep the team united, giving them all the chance to express themselves and make their voice heard».

Love is what keeps us going
I am the head nurse in the critical patient unit. I have worked as a nurse for twenty-five years, all of them in intensive care at the Bupa Antofagasta Hospital. My unit is made up of three sub-units that were basically one ICU and two high dependancy units, but with Covid they were made into three intensive care units plus one high dependancy unit, and we increased our beds by 100%.
We made the change beetween March and part of April, and the healthcare team were always very willing to cooperate in everything they could in terms of the pandemic. A lot of them actually helped with the changes right from the start.
Although not many have got sick in the Covid team, we had to take on more people because of the changes and because of other health problems people started getting as a result of the heavy workload:
 judith aguilera Head of Nursing Intensive Care Unit Bupa Antofagasta Hospital
judith aguilera Head of Nursing Intensive Care Unit Bupa Antofagasta Hospital
As a nurse, I have to put others before myself, because our profession is about caring for people, whether it’s to cure them or be there when they die.

aches and pains, backache and shoulder-ache (rotator cuff), because of moving patients, especially sedated patients, who are very heavy. We had to organise training, induction and specialised emotional support for our new colleagues. That involved the older ones too, people who had been working 30 or 35 years in intensive care, who had to be retrained and find the right balance.
On the whole, we hadn’t had many deaths, but now they have gone up and that worries us. The toughest moment was at the peak of the pandemic. That actually came quite late for us. We had expected it in June and July, but it came in July and August. During those months, the healthcare teams were tired, not just physically but also emotionally, because everything feels worse when someone close to you gets sick, which was what happened to a colleague of ours who was about 47 or 48 years old. It was not easy to care for him when he was so ill. I think it was the toughest moment for all of us. He is an auxiliary nurse in icu and has been at the clinic for twenty-five years, the same as me. In fact, we started at almost the same time. He was very unwell, lying face down on mechanical ventilation and on a lot of medication. Our teams did everything to help him. Recently, at the beginning of August, we were able to extubate him.
When we finally discharged him, it was a moment of great happiness and hope for us all.
It is very important to see each person in our team as an individual, with their own world, their own family, their own concerns and needs. Sometimes all you need is someone to come up to you and tap you on the shoulder and ask you: How are you?
98% of us here are women, young adults mainly, with children aged between two and five years old. You can’t help but feel sorry for many of them. Many of them have decided to leave their children in other towns with family and live on their own. Others have left their partners in charge of the children. The families are very supportive.
I am the mother of two children, Gabriel aged 9 and Tomás, the oldest, who is 14 years old. I get home about eight at night every day and go through a whole disinfection procedure, and it is only after this that we hug and talk. That’s when we share our days. By ten at night I am exhausted. I think it’s my family’s love that has kept me going. Without my husband’s support I couldn’t have done it with the children. At this point, we both work the same amount. My husband doesn’t work in healthcare, but he met me some years ago when he was working as an intensive care nurse and thankfully understands my work. His name is Patricio. He had Covid and pneumonia at the start of the pandemic and I
—
have to say, the physical consequences are terrible a person is never the same afterwards. He is 42 years old, really sporty, has played rugby his whole life, but his fitness has changed. He is more tired, less energetic, wants to sleep more and is even more irritable. He was at home with us the whole time. They found he had the virus because he started with renal colic. We will never know who infected who. The children and I were asymptomatic. The emotional side is the worst. We were just talking about that last night. I asked him how he was and he said he was fine. You don’t look fine, I said, you look different. He paused for a moment, looked at me and said: In September I will go back to training.
As a nurse, I have to put others before myself, because our profession is about caring for people, whether it’s to cure them or be there when they die. Although I have worked for twenty-five years, I still feel it when someone dies. I think you have to be calm and remember you have done your best. People are more than just a body, they are a soul too and the legacy they leave is more important than their body. �
Empathy prevention and care
juan pablo vásquez Nurse Clinical ServiceThe strange thing about going into a home where there are patients recovering from Covid is that usually you are looking after the medical side, but here it is all about education.
When we take on a patient, we fill in a form, making sure there is always a family member responsible, or a guardian, but that the whole family is present. We tell them how home hospital works and we inform them all together so that they know what to do: What are the alarm signals?
When should we notify? When to go to a&e, etc. For each entry we take the name of the family member responsible and we give them a mobile number that is active 24-hours a day.
Covid mainly affects patients’ respiratory system. The second, I would say, is motor-related. They lose a lot of their movement, especially older adults. The third is a difficulty
CHILE
in swallowing, which happens to patients who spent a long time on a mechanical ventilator. They can’t feed themselves and have to use a tube for a long time, some even using a gastrostomy tube. Those are people who will have to do rehabilitation with specialists.
I remember one patient on a ventilator who was transferred to hospital at home. When we got to her home in the ambulance, the family didn’t want to take her in. They begged me to take her back to the hospital, even though we had told them we were coming. They had got a room ready, but they were really afraid. Finally, after talking to them for a long time, they felt comfortable enough for her to be cared for at home. Those are things you don’t expect to happen.
At my house, we have always been really worried, especially about my partner. I also got Covid and spent a couple of weeks in quarantine, but luckily I didn’t get too ill.
As healthcare professionals, we have had to learn to live with the rules and safety measures in order to protect those closest to us. We have got used to it. I think the best way to protect yourself is always information and prevention. We all need to respect the rules and precautions and show respect and empathy for others. �

Communication with the family made all the difference
José de Arica Hospital
— CHILE
«One of the situations that has impacted me the most is the way that this pandemic has hit our communication with the families, and how our relationships have been disrupted due to isolation. By the same token, I am filled with joy and satisfaction when, after taking the necessary precautions, we have facilitated the communication of patients with their families thanks to the technology available. I went through this experience when my brother Gedeón was admitted to hospital with coronavirus in Santiago, and a fellow nurse helped us get through to him.
It definitely made the difference for our family; everything was better after we had news from our brother. Her presence there was not something whimsical or esoteric, instead, it was Our Lord helping us through this difficult time».
We’ll get through this together
alejandro lleixa Healthcare Supervisor Sanitas Healthcare FundingI work in a healthcare funding department in Barcelona, but for a long time, I worked in the health promotion service in Madrid, which is an online service that includes the 24-hour service for urgent phone calls and video consultations for Sanitas patients. At the start of the pandemic, we were sent home to work. We didn’t really know how things were going to pan out. My old boss asked me for help. She said: You should work on the 24-hour service because you know it well.
I helped out by attending calls when the lines were saturated, but my main role was to help to organise, coordinate and support my colleagues from the funding management departments who had volunteered to help out. On a normal day there would be 600 to 700 calls or, when there was a lot of flu around, it would go up to 1200, but now we were getting five or six thousand calls a day at its peak. 90% of the calls are related to Covid.
BARCELONA — SPAIN
At the beginning, there were lots of different questions, but they got more complicated over time. They would ring and ask: What do I have and what should I do? What are the risks? Is this curable, do I have it mildly? And other such questions.
Our role was largely to inform and guide. When family members started ringing it got difficult. I remember a young man who was quarantining in his room at home, and nobody wanted to touch anything belonging to him. The young man was really worried about his family: I am almost imprisoned here. We would also get calls from older people with underlying diseases. They were very worried.
As coordinator, we started each day with a report of the situation of each hospital; where we could send patients to and where not. For people who were not so bad, we would start by recommending paracetamol, isolation at home and rest. But those who needed hospital we would deal with as quickly as we could.
From March to April everything got worse. At the end of April, more or less, that was the worst, really. After the first week of May I was able to go back to my usual work. We weren’t getting any more Covid admissions, but in the last week I worked we started getting new admissions again.
At the moment, at the beginning of August, I am on holiday and we are planning to visit my partner’s parents. I believe things are quite quiet. I am from Barcelona and we have another variant that seems to be more difficult to control. I feel like we have tried but we haven’t learned to live with it. We don’t seem to be able to take the necessary precautions and live more or less a normal life at the same time.
I think that the last one had to do with education and age range. People over 25 years old are very aware and know how to follow the guidelines, but teenagers are a bit of a problem because a lot of them are carrying the virus but are asymptomatic.
I have been in nursing twenty years, but nobody prepares you for this. I believe they are going to start vaccinating in Russia this week or next. Meanwhile, the who is talking about 2022. I think it’s more likely to be 2022 than the first quarter of 2021. All of it has a certain amount of trial and error to it. Vaccines can work on some people and not others.


I haven’t worried about passing it to my immediate circle, because we have been working from home, but in the end, when you have said the same thing to 50, 60 or 70 people, you get really worried when you see that the virus is still raging. No system is prepared. Sanitas acted well and quickly, but the whole health system has been badly affected.
I think the whole system and the whole of society need to be aware of the gravity and serious nature of the situation and of how individual behaviour is important, so that we can beat this together. If we can’t stop the spread, I don’t think it is likely we will be able to go back to a life like we had before. �
I think the whole system and the whole of society need to be aware of the gravity and serious nature of the situation and of how individual behaviour is important, so that we can beat this together.
I am stronger than I think
MADRID — SPAIN
You know your job, but not how to deal with a pandemic: How do you care for a Covid patient? How do you tell the family certain things? These are some of the things we have had to learn in recent months.
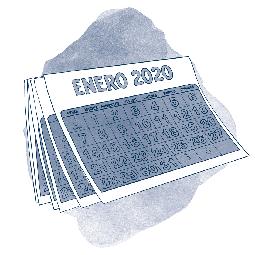
When the first case of Covid in Madrid was confirmed, we had 68 residents. We look after Alzheimer’s patients and people who are recovering from fractured hips. Some people came to take their family members home before the care home was closed to visitors. So we were down to forty-eight residents, whose families couldn’t visit them. We have tried to communicate as much as possible so the families are not worried, but it’s sometimes not good news and it’s hard to say to a daughter: Your father doesn’t have long left.
I remember one of the advanced Alzheimer’s patients at the centre who had some really bad days. I thought she would die, that she wouldn’t make it. But she was really strong and survived. Of course, she lost weight and lost a lot of mobility after what she went through. Now when I see her I say: Look at her, there she is.
I knew there would be difficult times in my job, but now I can’t even imagine what I might face tomorrow… That daily worry doesn’t let you relax.
We have been through really tough times, because Covid is a bit capricious. You think your patient is well and then four or five days later they suddenly get worse. I couldn’t have imagined having to work this way. You know your job, but not how to deal with a pandemic: How do you care for a Covid patient? How do you tell the family certain things? These are some of the things we have had to learn in recent months.
There is also the worry about my own family. I am not from Madrid, I am from Granada. I live here with only my partner. Some days I take selfies in the mirror after I have done everything and send it to my mum so she can see I am all protected in the ppe and she says: I don’t recognise you under all that stuff.
I don’t think this is over yet, I think this is just a lull. I think we will get more, because people are really tired of masks and don’t see why they have to follow certain rules. Many don’t follow them. We have to stay alert. �
Learning
raquel pérez Depute Manager Patient Safety Bupa Chile«I think we have proved, yet again, that teamwork is really efficient, both for those who work in front-line and for those who work in administration and give remote support. We have learnt a lot of lessons from this about being prepared for the unexpected, on the one hand, and to keep insisting that everyone, wherever we are, can do our bit to make things better».

Always a nurse, with or without a pandemic
 mª francisca c astillo Nurse IntegraMédica Outpatients Clinics
mª francisca c astillo Nurse IntegraMédica Outpatients Clinics
I am 32 years old and have been a nurse for eight years. Our centre is the biggest of all of them and I don’t think we were prepared for this pandemic. What we had to do, most of all, was to make sure the patients got quality, safe care.
In February, we started talking about how we could prepare for this. In the third or fourth week the first Covid cases started coming in. In March it became an avalanche and one suspected case became fifteen to twenty a day.
March was a really bad month. I was on the verge of tears on many occasions. That month was a mixture of people coming in for pcr tests and appointments for patients with chronic illnesses high blood pressure, diabetics, etc.
In March and April, we started to receive protocols from the Ministry of Health with guidelines on how to deal with the pandemic within the different procedures and areas of the medical centre. In April we started to get it all organised. Over time, we were able to fine-tune it.
One of the most difficult things was notifying the seremi (Ministry of Health) correctly and making sure we didn’t contribute to under-reporting of national numbers. I think between March and April people started to realise how serious the pandemic was and would only the visit the centre if it was really necessary.
In the first two weeks of June there were lots of cases and lots of tests. Everything fell apart. There were lots each day and most of them were positive.
It was really important to stop the spread, because so many people were dying every day. In May it was 50 a day and in the first two weeks of June between 100 and 200. It started to calm down in July and patients came less to the medical centre and the number of people testing with pcr tests went down.

Generally, nobody can say for sure if people can get coronavirus again or whether they are immune, but now we have the igg and igm tests which can show how much immunity a patient has built up.
I haven’t had a cold in ten years and I have never had bronchitis in my life. I am a vegetarian and am really careful about what I eat. I was sure I wouldn’t get ill, but my family was worried. My mother, instead of encouraging me, would get me worried, asking all the time: What if you get Covid? What will you do? What if you are infected?
Generally, nobody can say for sure if people can get coronavirus again or whether they are immune, but now we have the IgG and IgM tests which can show how much immunity a patient has built up.
Nurses are always educating, including about how to wash your hands properly.
Until coronavirus, some people still didn’t know how to sneeze properly. When I talk to people, I tell them: Did you know that in order to pick up a virus you have to inhale droplets from someone who left them on a surface? They would say: How disgusting! And I would say, how do you think we pick things up?
Strictly speaking, I think face shields are better than masks, because people often don’t use masks properly. Some people wear them under their noses or to the side and they end up being more of a virus transmitter than a protector. The same is true of gloves: they should only be used for medical uses, because they collect micro-organisms and become transmitters.
— CHILE
When we came out of lockdown last week I started cycling. I still need to get back to my hobbies I do pilates and yoga, and I haven’t been able to do them for months.
On the emotional side of things, the hardest thing has been the distance from my family, my home and my husband. As well as my two little dogs.
If anyone asks me if the pandemic has made me want to stop nursing, I tell them no way, I would do it a thousand and one times, pandemic or not. �

Each customer and individual
Isapre Cruz Blanca Health Insurance«I see medical reports and I think about how behind every report, behind the statistics and the details, there is the family of a sick person. But more than a customer, the person is always going to be a patient, because we know their story, we see them go through it and watch as to whether they will recover or not. I get involved in every case I see. They are not just numbers, statistics and resources. I have found it comforting to see how, in spite of all the families’ suffering, isapre has always been committed to supporting them».

Professionalism and love, that’s our job
I was born in the town of Iquique and have been a nurse for twelve years and worked in the company for ten years. I have been Assistant Manager of Nursing since October 2019. 2020 had started with a lot of problems because of the social crisis in Chile, and when we were just getting used to that, the pandemic hit. At the beginning, we just heard news that made us really unsure, and couldn’t really work out what was happening, and the Covid arrived to the clinic later than the rest of Chile, so the demand on us was very high. In mid-March our first patient arrived, then a second, and suddenly we had twenty. That was when we quickly extended our critical care units.
In April we were mid-pandemic, the emergency rooms were full and we could see that at any moment our system was going to collapse. We adapted critical care beds and split the hospital into Covid and nonCovid areas. A lot of people were off because of the risk and because of stress, in some cases, and we started to work with the team leaders to help them look after their teams. The team responded amazingly, even though nobody was prepared for this. We were sure of one thing, that we had to pull together to get through this.
During this time I have really seen what it means to be professional and love your job, even when you are overwhelmed, tired, frustrated. Everyone has just wanted to give their best. I must say, I am proud of the team. Amongst the measures that we have taken to protect ourselves and avoid spreading the virus was to use safety equipment and social distancing, but the most effective thing has been reinforcing and insisting on these until you see the cultural shift.
Around the end of April, beginning of May, we went through the most difficult time. The hospital in Calama asked us to take some of their patients but we didn’t have the capacity, and couldn’t make it happen in such a short time, because patient recovery is slow. It normally takes about two weeks.
The critical patients are normally adults older adults, but there are exceptions, like the first one we had a young athlete who nobody understood why he needed to be intubated. He had no underlying
 ximena báez Deputy Director of Nursing Bupa Antofagasta Hospital
ximena báez Deputy Director of Nursing Bupa Antofagasta Hospital
illnesses, he wasn’t a smoker and his quality of life was good. That made us think that “nobody escapes from this”, or perhaps he just came to the hospital a bit late. So, when that patient was discharged, we had a real party, with applause, crying and all. It was very emotional, a precious moment, because he was the first critical patient who recovered. A newspaper photographer even came. It was a victory. Many patients who have recovered send us thank you messages, which is lovely.
With everything we are going through, I couldn’t lower the intensity at work, and had to be at the hospital every day. Even at weekends. My husband is a doctor and we have a son of 4 years old, Andrés Emilio. The apple of my eye. While I was at the hospital, my son and my husband stayed at home, as my husband was able to have flexibility with his hours. Our nanny was also very supportive. She is like family to us. We had to be really careful at home because we knew that my husband or I could get sick at any moment and pass it to the other. I was ultra careful with everything, because I knew that whenever I came back from the hospital I could well be carrying the virus. I was careful and methodical when coming in, when staying and when going out, with lots of procedures in place.
ANTOFAGASTA — CHILE

I live near the clinic and walk to work through a park. At the start, there weren’t many people around, but then people started coming out again. It worried me to see people not distancing as they should, or little ones running around without masks. I would ask myself: What do we have to do to make people take this seriously? This has to stop soon. Soon we will be able to get together again, to celebrate all the missed birthdays and share again, but we can’t stop yet.
All of this reminds me of when I was a student in university. I remember clearly that a professor of epidemiology told us about pandemics and the importance of the role of nurses as organisers and team leaders. He also talked about Florence Nightingale, who was in the Crimean War in the mid xix century and brought in organisation of areas, dirty here and clean there. She insisted on the importance of something as basic as washing your hands. She said: “Humanity is going to be 100 years late in giving value to nursing.”*

«I beat ‘covis.19’ with your help Thank you »
I am really thankful to the whole team.
All life’s emotions condensed into a few months
isabel rico Nurse Mas Camarena Care HomeIt’s been like taking all the emotions you might feel all your life and compressing them into a few months. That’s how intense it has been.
I think as an organization we have made radical changes. We were an open centre where families were part of our daily routine. They were an integral part of caring for the older people in our care, and even did training with us.
But now, since the centre has been sealed, we have had to learn to work in a different way. We used to work with groups, but now we work more with individuals, because people can’t mix with each other. So far, we have had no cases of Covid, neither staff nor residents.
When the pandemic arrived there were 71 people in the team: auxiliaries, maintenance, managers, nurses and doctors. There were 119 residents and all of them were very vulnerable, either because they are older and we also have
 — SPAIN
— SPAIN
highly dependent, younger people who live with mechanical ventilation. They are really dependent. So if the virus got in it would be fatal.
Communication has formed the base of our teamwork. There is nothing I have gone through that the team hasn’t been a part of. I am talking about the whole team: cleaners, kitchen staff, auxiliaries, etc. Our residents have been informed of all the decisions we have made that affect them directly, such as the zoning off. I remember a lady of over 100 years old who is still quite independent. We told her and her comment was: Yes, it’s a really bad flu. Like the one 100 years ago.
In Sanitas Mayores we have an app that we use to keep in touch with our resident’s families. This is a very new project, about a year and a half or two years old. They can download it on their phones and use it to message any employee of the centre at any moment.
I have been here for fifteen years and haven’t had a break in working since 1999, so I have been a nurse for twenty-one years. Over the past few months, I have also been shielding my daughter and my son and my husband. I have been the only one going out.�
At times, it all seemed like a maze
I work attending urgent phone calls. The pandemic hasn’t been the same for me as for those who work directly with patients. We have offered a service for families who can’t go into the hospitals or patients being managed at home because the hospitals have been full. Everyone in our service was sent to work from home and we were provided with laptops and we continued to provide our 24-hour urgent telephone service.
It was usually more about fear than symptoms: I travelled, or I was in contact with someone who travelled; I went to Italy … We would advise our patients that unless they had serious symptoms such as breathlessness or fever, that they should stay at home. We also asked them to quarantine as much as possible.
The worst thing was when healthcare staff got Covid. It got more complicated then. There weren’t the medical teams to look after patients, and nowhere to refer them to. Field hospitals were even set up, because the current hospitals weren’t coping. Soon, new teams were set up to support people who had coronavirus at home.
 maría casas Nurse Sanitas 24 hours Sanitas Healthcare Funding
maría casas Nurse Sanitas 24 hours Sanitas Healthcare Funding
I think my mood changed. To start with, I didn’t even have time to think. There were so many calls, and I spent so many hours at the computer there wasn’t time for thinking.
At times, it all seemed like a maze. So, for example, a family had to send an older couple in an ambulance and couldn’t go with them. To start with, we and the family would know which hospital they were going to, but sometimes we lost track of them. We didn’t even know if there would be a bed for them when the ambulance got to the hospital. The family would ask: Please, write down our phone number and call us when you know what is happening. The families knew that once their sick relatives had been taken away in the ambulance, they might not see them again.
There was a lot of uncertainty. The ambulance driver might say: I am taking your father to such and such a hospital. But you wouldn’t know how long the person might be there for or how it would be, or whether they would be put on a ventilator, or taken to another hospital. At the beginning, that was happening to hundreds and thousands of people. It was really difficult.
The families had so many questions about their relative: Will they be on their own? Will they need anything? Will they suffer? Will everything be taken care of? Will someone look after their needs? And all of this was being done by phone call. Little by little, things got more organised, and they started centralising coronavirus admissions, which made it quicker and easier to locate people. To be honest, it was a feeling of complete helplessness, being on the computer at home, knowing that there were never enough staff. And it took longer to support people and help them by phone.
We were getting a total of eight or ten thousand calls a day. Mostly, people were really understanding, just scared, but there were some people who were really angry. At the end of the day, it was a really unprecedented situation.

I think my mood changed. To start with, I didn’t even have time to think. There were so many calls, and I spent so many hours at the computer there wasn’t time for thinking. I had to quarantine at my parents’ house recently and then I had some more time.
Then we had a month and a half or two months when the volume of work was more or less normal, for that time of year, then at the start of July it was increasing, and got worse again. The fear came back, there were more cases again, but they were milder and less people needed to go to hospital, but there were still sick people. Now, in mid-August, cases and calls are rising again. More people are getting symptoms. Since life has gone back to “normal” cases are on the increase and that shows in the volume of work.
I still need the help of my elderly parents. If my daughter picks it up at nursery, it would probably not be serious for her, but it would be for my parents. So I am worried too. Because children share everything. They pick things up and put them in their mouths. It is difficult to keep them apart. How can you make sure they don’t swap dummies, which is something so simple?
As a nurse, I have worked for many years in hospitals and A&E and you will see someone coming through the door and pick up how they are. That’s the experience we have. I feel my work has been important because I have contributed to our emergency hospital services not collapsing.�
Cooperation at all times
marta quelle Nurse La Coruña Care HomeWe were all afraid. When I was afraid I would lean on my director, and she would do the same with me. That’s how we worked. Nobody was exempt from being afraid, but all together we were strong.
I have been a nurse for thirteen years. Now I work in an a care home for elderly people. Our work is very varied. We are nurses, assistants, therapists and even do maintenance. I think the biggest thing I have learnt through all of this is that it’s not about your job or other peoples’ jobs but about all pulling together to look after the residents.
We are certainly, as Latin people, very physical and sociable. Here in Galicia we have a lot of festivals, but they may not happen this year.
Personally, I was able to have a holiday. I couldn’t actually go away, because my family live 70 kilometres away, but I was able to spend time at home. Who needs a holiday more than healthcare staff, who have been on the front line in this crisis and been far from our families and following strict guidelines?

I have learnt a lot of things over the past few months. Cooperation between teams has a certain structure to it, normally, but during this time it has had to be about
spontaneous reactions at times. We had to make new isolation zones and didn’t even have furniture for them. It was all very temporary. It was all done by teamwork, even the maintenance assistant who made a piece of furniture for us to store the ppe.
I have never doubted I am in the right job. Actually, when I finished my studies I thought I might go into Medicine, but I have always wanted to be a nurse. I chose the career I am in, and even love the administrative work, although sometimes it feels like our work is taken for granted.
I think we will reach a time when everything is under control and then all or most of us will start to feel down, which will be the next problem to be dealt with and conquered. �
The nurses behind the management
 daniela figueroa Nurse Bupa Reñaca Hospital
daniela figueroa Nurse Bupa Reñaca Hospital
I have been a nurse for fourteen years. Now I have an administrative role. All the clinics have people in such a role. Although we are not on the front line of Covid, dealing directly with sick people, we make sure the patients are well cared for.
I am in charge of the department ges /cae. ges is a law in Chile that brings together 85 diseases that have certain special characteristics and cae is an insurance that ISAPREs have to cover catastrophic diseases which are high cost.
In March, before Covid started, there were lots of meetings of doctors about what was happening in China and how it could come to Chile. On 14 March it was my birthday and I travelled to Santiago to celebrate with my family. We had to come back on 15 March when the state of emergency was declared in Chile.
In April the chaos started, the last half of April and into May, but even worse in June. Around the end of May, a message came out from the Ministry of Health which asked the isapres to give cae funds to all patients who were Covid positive, because it was obviously going to be a high cost disease, spending twenty days in an icu could cost millions of pesos. So these patients would have financial protection. From that moment, we had to review all cases, even closed cases.
My work was to call about administrative issues, which could be really cold. You would have to say to the family: We are going to bring your dad in in an ambulance, so I need you to give me an address to send you the documents to sign. Though that sounds cold, you can say it in a kind way that shows you understand the anguish and fear the family are feeling.
I worked 24/7 on that. I would be called at ten at night for a transfer and I would be there until two or three in the morning coordinating everything until the patient arrived at the hospital. It was all very difficult. Sometimes the family didn’t want to accept that their father be sent to another town.
I often gave out my private number to families, and they would call and say: the icu doctor hasn’t called me for two days now. Or I would call them and they would say: we call but nobody answers , and I would check and find that they had the number wrong and that’s why the family hadn’t heard anything.
What you often don’t realise is that there is a chain of administration events that have to happen so that this patient can get quality care and recover. That’s our invisible contribution.
I am lucky that I practise and know about some alternative therapies. I practise yoga a lot and my teacher agreed to continue via video call. This has helped me a lot. We noticed at work that the clinical staff were very anxious and exhausted. The head nurse came to me because she knows I am an “esoteric medium” as she calls it. So we brought yoga into the hospital and that has been great. Also, three weeks ago we started aromatherapy sessions in the icu and in the emergency department. All with the support of the staff.
I remember how I was shocked to learn that in Santiago, the icus started to be 99% full. The isapres would ask us to take patients into our icus, because some of the regions were going to collapse if we didn’t help out. I think we had the advantage of being almost a month behind the peak in Santiago, and also having hospitals the size of the Gustavo Fricke which were newly opened, so we could put in a lot of intensive care beds. We were able to contain Covid with the resources we had in the Region. When you looked at the statistics, we never went higher than 82 or 83% occupation of the ICU network, and although that is high, fortunately we never reached the number of 90 or 98% that happened in Santiago.

Since I studied nursing, I have never worked much in hospitals, always in management. I think nurses are well prepared for working in management and administration. It is important that the administrative work we have undertaken during the pandemic is made visible as it has been very difficult and intense during the pandemic.�

They would call me at ten at night for a transfer and I would be there until two or three in the morning coordinating everything until the patient arrived at the clinic.
Video consultations are here to stay
patricia gajardo Deputy Manager Outpatient Services Isapre Cruz Blanca Health InsuranceWhy would you travel to a face-to face appointment? It doesn’t really make sense for less serious health issues that can be dealt with remotely.

We have looked after our beneficiaries by making sure they don’t need to go out for appointments, to stop the spread of the pandemic. Also by supporting healthcare systems, which are on the brink of collapse.
We have brought in video consultations, which is a service that has been around for a while, but the public in general hadn’t made the most of it. Perhaps because they didn’t really know how to use it, or didn’t trust it. I think the feedback has been amazing, considering that everyone in the organisation is working from home remotely.
I think this way of working has come to stay. It’s a great way of people not wasting time or risking infection when they go to A&E for something minor.
You have to remember that healthcare teams are exhausted right now. I have a daughter who is a nurse and works on the front line, and I can see she has lost weight and is very anxious. But that is not my only worry. My mother
SANTIAGO —is 85 years old and has a complex cancer. She lives at home with a nephew. Not being able to visit her at all has been very stressful.
I think the company could easily have said: We will do what we are obliged to and nothing more. But the truth is that the company and I have always given more than we have had to, because we know this is an unprecedented situation and we need to be there for people. That has been really special.
I am a very positive person, and I think that through all this I have been able to react well and give our beneficiaries the answers they have needed. Our objective, during this time, has been to provide and maintain our services as much as possible. �
Non-Covid patients also need us
 teresa fernández Nurse San José de Arica Hospital
teresa fernández Nurse San José de Arica Hospital
«I am in charge of the intensive care unit here at the hospital. In March, we were preparing for Covid, but time went by and then they told us we were going to be a “clean” hospital, because another hospital would take the Covid patients. They even asked us for our ventilators. Personally, I think I could have done even more. I would have liked to have done my part in the pandemic, using my experience, because I worked for many years in the hospital in the intensive care unit. But I know we are doing our part, because the nonCovid patients need us and always will».
No statistics can show what people have been through
cristina satóstegui Nurse Hospital Sanitas La ZarzuelaI would come home from the hospital and take all the necessary precautions, because my husband is very vulnerable. We have three children. The two boys live with us and our older daughter is studying in the usa. We had to get her back to Spain and that was not easy. The borders were closed. We had a lot of problems, but we managed it in the end. Now I worry about my grandparents who don’t live with us but we do their shopping and they try not to go out.
Thanks to my family and their support, I was able to dedicate myself totally to my work. On 9 March, our first Covid patient arrived. He was the only one in icu, where we have twelve beds and two isolation cubicles. I gave all my time to that patient and looked after him every day until he died. He was the first one to die of Covid in the whole hospital.
Then it started to fill up. That’s how we ended up with four icu units with different functions. For example, I was transferred from the adult icu to post-surgical icu, and instead of having intensive care assistants we had anaesthetists. There were new doctors, new areas and surgical ventilators. Little by little, we managed to get all that we needed.
The patients coming into the icu at that time came in to be intubated. Their oxygen saturation levels were very low. A lot of them had fever and some had diarrhoea. The patients couldn’t tell us if they had pain anywhere, because they were unconscious.

The treatment was very aggressive and caused alterations to the liver. At first, we cared for them face down, but later on that changed. Putting the patient in that position needs a lot of staff and a lot of strength, which we didn’t have towards the end. We started to get used to all the clothes and the heat. You start to feel in control and that cheers you up.
We would have patients from aged 40 years old. There weren’t so many women. About 80% men and 20% women. A lot of them didn’t have underlying illnesses, but others did. Things like obesity and high blood pressure, mainly. We have had people of all ages at this hospital. There are no limits. Some people have been up to 85 years old.
I think our death levels have been low, from what I’ve heard from colleagues from other hospitals. But of course, statistics are cold when it comes to talking about what we have been through.
As far as consequences for people who have survived, I would say muscular problems are the most common. We set up a physiotherapy
service from the beginning, and patients get it as soon as they stabilise.
Instead of one session a day, they get two. There is a morning and an afternoon team. I think this speeds recovery. We had a case where we had to amputate a patient’s leg, but they already had problems with that leg, and they ended up dying. We have had a lot of cases of blockages in the trachea and we have had to ask the pneumologist to come in to treat them and unblock it.
All the heads of intensive care in Madrid are working together, both public and private. Whatever a large hospital tried and that worked would be passed on to all the hospitals. So if someone finds a successful treatment, all the procedures change everywhere. Every day was a new world.

All the heads of intensive care in Madrid are working together, both public and private. Whatever a large hospital tried and that worked would be passed on to all the hospitals.
I think Madrid is expected to reach its peak in mid-September, before the winter. How people have reacted or behaved has depended on different areas. I think young people and a lot of adults too are afraid when someone we don’t know sits beside us on the metro. We protect ourselves with masks. But if we are with a friend, we seem not to worry, and get confident and throw caution to the wind because we are with someone we know. But it shouldn’t be like that. I think it’s very hard for young people to understand.
So what I would do was that when I finished at the icu on the surgical floor I would go up and sit with my colleagues and tell them about my morning. The hospital also provided us with a psychologist and we have had group therapy every week. I find out then how my colleagues are. Some are very affected, others are better. We are a very stable team and have been together a long time. We always talk to each other so that hasn’t been hard.
I am very thankful at how lucky I have been, firstly because I have never caught Covid. My whole family is well and I have been able to give myself totally to my work, knowing everything else is under control. Except for my daughter’s return, my husband has dealt with everything else at home.�
VALENCIA — SPAIN
Valuing the simple things
begoña inchaurraga Nurse El Mirador Care Home
— SPAIN
«With Covid, you couldn’t do a lot really. For those who believed in God you would pray the Lord’s Prayer. For those who aren’t so religious, you would tell them: Look, your wife is there, your parents… waiting for you. You needed to transmit to them the peace they needed to keep going. Today, my life revolves round work and home because of the Covid restrictions. At the end of July, I felt overwhelmed. Work had never affected my lifestyle before. My relaxation these days is to go up into the hills with my son. That’s all».
Make the most of every moment
laura visansay Nurse Santa Provença Care HomeBARCELONA —
In the first days, perhaps the first fifteen or twenty, I slept in another room. I live with my husband and a daughter of 5 years old. I started to isolate when I saw how bad it was.
To begin with, it felt like we were making sure the bug didn’t get into our care home and we were happy. Then one case arose and then we had an outbreak. We couldn’t understand how it could have got in when we had been preparing for a week but of course just the weekend before we had had families over and they had been in contact with the residents and auxillaries. A week earlier, we weren’t using ppe equipment and of course, that was when the infections started.
What the press were saying about the Care Homes was hard to accept, because from the inside, we knew all the effort and the dedication of all the staff. Once I remember saying: I don’t watch the news any more, or read the newspapers, because it just gets me down.
Now, in August, after months of it, everything is more complicated. I’ve had holidays, but I found that I didn’t want to come back, because I didn’t know if I was ready to go through it all again. But then you think about the residents again and know you have to be strong and keep going, and then you do, so that you can be on top of things.
I think everything we have been through makes you value life and make the most of every moment. All of us have tended to live very rushed lives.
After this, I think we will have to put in certain protection and hygiene measures. We know the nature of the beast now, and there may be others, so we need to protect life.�
The next challenge
ana maría quezada Coordinator of Professional Development Bupa Chile
«I think nursing has thought a lot during this crisis, and the next challenge will be to deal with all the illnesses that have been delayed because of the pandemic. We need to start caring for our patients again».

Welcoming new lives
Everything has had to be different during this time, because in normal times our patients have their partners or another close family member with them throughout their labour, who are there to support them. At times of pain such as this, which is of course a natural part of childbirth, they have psychological and emotional support. During the birth, having their loved ones nearby is really important. Then, when they leave the birthing suite, when you are with all the emotions of the birth of your child, it is important to be able to share that with your closest loved ones.
Now it’s all different and you can’t see your family and tell them: I went through such and such last night, I felt or feel such and such. And especially when they are breastfeeding they are worried the baby isn’t feeding properly and have lots of little questions and worries that they need advice on and need listening to. Now, the partners come onto the ward only at the moment of birth, and that is the only time they are physically present.
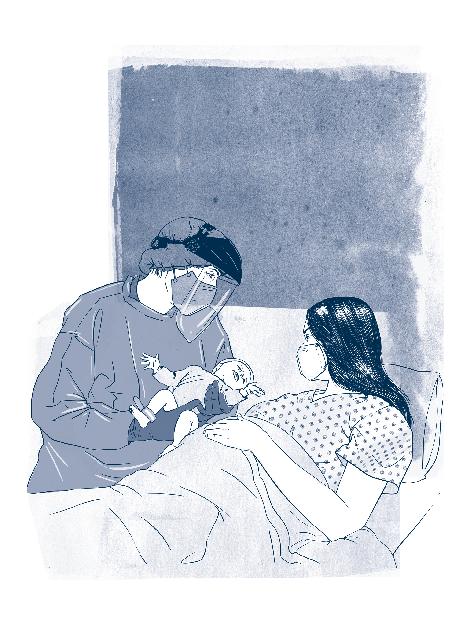 zaira villagra
Midwife San José de Arica Hospital
zaira villagra
Midwife San José de Arica Hospital
We work with patients in the emergency unit too, and they go through exactly the same feelings, because we care for them wearing ppe. It is rather shocking for them to see someone totally geared up and who can’t get near to them. I have been through the same with my little daughter. Even though she knows well that mama works at a hospital and knows that when I get home I have to clean up and go through the process of desinfection and that I can’t touch her.
To be honest, we have just done everything we can so that births happen in a normal atmosphere, so that the mothers are happy to have been here.
To be honest, we have just done everything we can so that births happen in a normal atmosphere, so that the mothers are happy to have been here. Our objective has been, with each one of them, that such a natural physiological process can be a good experience for them. Covid is out there, and it obviously has an impact, but we have done our best to be there for each of them and make these births special, because new lives are coming into the world.
The patients need comforting, because they can’t have visitors. Because they haven’t been able to have visitors or anyone to talk to we, the midwives, have needed to be much closer and more attentive.

In maternity, the shift midwife is in charge of emergencies, new births, post-op, incoming gynaecological and obstetrics patients and the same patients when they leave the hospital. So there is a vast range of duties. You want to look after everything well, give your best, not let anything go wrong, no adverse events, and you have a lot to deal with, but you are still content, because you see all of it, all the good things that happen on the shifts. It is very satisfying.
In this situation, some mothers were very eager to be discharged because they wanted to get home to be with their families. For us, it is clear that some mothers wish to go home as soon as possible after the birth.
But at the same time, many of them were really grateful, because they have had to become mothers in a pandemic, and they are very grateful for all the time we spent with them. Sometimes, at 3 a.m. they ring the bell because they are stressed, they can’t feed the baby, they are in pain. So you go and help them so that the babies can calm down and stop crying. That gives the mothers a rest. It means a lot to them that someone who is not a family member is helping them.
We have had to learn how to support them yet at a distance, in a certain way. We can’t hug them or massage them when they are giving birth or take their hand or stroke their forehead. We have had to show our empathy in a more psychological and supportive way than ever before. Knowing how to comfort someone without touching them has been both a personal and professional learning curve.�
Thinking of future generations
paula feres Nurse Isapre Cruz Blanca Health Insurance«After it’s all over we will have to adapt and change the switch. I think it will bring about a progressive cultural change. Washing our hands, carrying hand sanitiser in our bags or rucksacks to use when we get out of a public transport or touch railings, will have to become habits. Another thing we will need to do is make handling a pandemic one of the curricular items on healthcare courses. We need to raise awareness in future generations».

We celebrated the recovery of each patient
beatriz estéfani Nurse Sanitas Hospital La ZarzuelaMADRID — SPAIN
I was off for a few days and when I came back I found the intensive care unit practically 100% full, with all the patients lying face down and gravely ill.
The first day, I literally thought I was going to die. What shall we do? I doubted, I wondered what to do in such a mess. I didn’t study nursing to be in a war like this. It seemed much like biological warfare, after all. Sometimes I wondered if my colleagues had gone mad. How could they be so calm and smiling, talking about other things. But that was just on the first day. I felt a bit better on the second. Then I realised that if you used the protection, nothing was going to happen to you.
After a while, I started to think that if you got sick it was because you weren’t protecting yourself properly and that I wasn’t going to get sick. I didn’t, but I don’t know if that was coincidence.
It was hard to see patients under the age of 50 years old, with no underlying illnesses and with a poor prognosis. I especially remember two of them. One survived, the other didn’t. Sometimes they left letters in the cubicles. If you read them you would feel really sad. You were sad because their families didn’t even get to see them or keep their personal objects, because everything taken to the crematorium.
So, when we had patients who came out of intensive care, we would put their favourite songs on high volume. Some of them chose something from Nirvana, Metallica, and nearly all of them were a bit into heavy rock. We would clap for them, record them and send it to their family. Because every patient that recovered was a victory for us.
I know that now the pandemic is back to the same level as it was in March. There are new cases every day. I look forward to working hard again with the team, but the most difficult thing will be the isolation. Some people at least had chalets, older children, and could sort something out. But I live in an apartment with a little boy aged 3 years old. The isolation is what really gets me, more than working with Covid patients.�


The role of nurses in the pandemic

At the beginning, everything was really uncertain, although we knew what had happened in other countries. But going through it yourself is different, because at the start we didn’t have all the Covid guidelines. We had to sort out our own procedures for informing patients and training staff. It was all new. As a nursing team, we drew up many protocols, which contributed to knowledge, gave us confidence and a platform from which to work safely. We were constantly drawing up new standards and care procedures, bringing in continual improvements from our own learning and from evidence coming from other countries.
The nursing team were the first to have pcr tests for Sars-CoV2, which was an important role in the operation of medical centres because the auxiliary staff weren’t familiar with the technique and were unsure how to handle the exam or how to make sure they didn’t get infected. At that point, our role was to educate and deal with their fears. It was hard, but we managed, and were able to make the staff feel secure and confident, because we knew there was going to be a surge in infections and we would need more technical support to handle the number of patients, which we were able to prepare for together with the auxiliary teams.
Nursing team IntegraMédica Outpatients ClinicsIn human terms, it has been difficult to handle our personal situations and support all the people who need us. It is a real challenge to be a flexible leader. But we chose this job and looking after patients is our life, and this strengthens us and helps us to grow as professionals.
Another challenge we have faced is having enough staff to cope with the demand. We had to train a lot of new people as well as informing and reassuring our employees and patients on our care measures. We are still on a journey, and that means insisting daily on the preventive measures, because patients get relaxed. We are still training and raising awareness of the rest of the staff. Every day we learn new ways of looking after patients well and being safe and giving quality care.
Another important thing during the pandemic has been resources, especially ppe. The key is estimating and managing efficiently. The clinical protocols are important, defining the types of PPE for each different function. In the first stages, everyone wanted to use all the protective gear, even more than the evidence and the guidelines suggested, and that was something we had to deal with.
Our aim was to involve the whole medical centre team, so that they understood and adhered to the changes and the new care model for Covid times. The first thing was dealing with appointments, samples and imaging, then safe procedures for clinical processes. We had to sort out the journeys for Covid and non-Covid patients in each network medical centre, with the peculiarities of each. We set up triage in the entrance zones so that we could direct patients in accordance with their needs and clinical condition. We also put up signs in all the areas giving information about the protective measures and the care flows, to deal with the growing number of patients. Then, gradually, we started to bring things back to normal, with demand challenging us to open new provisions and procedures under new standards.
Our role as lead nurses in medical centres is to be proactive in taking on board and making the different procedures, standards and checks work. There were more and more as the pandemic went on. We also had to make sure all the safety procedures were implemented as soon as they were brought in, make the changes, make sure they were followed all the time, and that nobody broke the rules, because that would put our patients and/or staff at risk. That meant a lot more work every day. To do all that, we needed to work together with different units in the centre, both administrative and clinical.
It was important that we made good decisions that ensured continuity and a good level of care and excellent quality.
Managing, directing work teams in a dynamic and changing
Our aim was to involve the whole medical centre team, so that they understood and adhered to the changes and the new care model for Covid times.
context, the product of a pandemic like no other the world had ever known, required comprehensive leadership. It was a challenge to our resilience and capacity to adapt to constant change.
The role of lead nurses in medical centres, put in charge of epidemiology, has contributed to the traceability of cases and the correct handling of tracing contacts. This new role made our daily administration tasks more difficult, whilst we juggled this epidemiological function with the multiple nursing tasks we were handling and in which we must maintain the highest levels of quality and safety.
Thanks to our teamwork, we have been able to maintain quality and continuity of care during the pandemic and make an important contribution nationally, becoming an indispensable organization because of the large number of people we attend to and who put their confidence in us.�
We have transformed ourselves to take better care of and save more people
carla alarcón Director of Nursing at Bupa Chile HospitalsWe want to make our teams’ stories heard, put them in the spotlight, make sure they become a legacy. This book is a way of recognising the work and dedication of nursing and midwifery teams, which can’t really be fully measured.
We started planning 2020 as the International Year of the Nurse and the Midwife, as declared by the WHO. However, like the rest of the world, we had to adapt quickly to the new context the pandemic had created, which has meant our profession has been more in the spotlight than ever.
Working with Spain
In March, the first news started to break. We had to quickly change our focus and plan how to fight the pandemic. We got a lot of information from Spain, because the pandemic hit there before it did here. Working committees were set up between the two countries, at which each Sanitas hospital would report on their situation. They would share strategies and success stories. The idea was to learn from the experiences of their teams and copy good practice and procedure, bringing that into line with the standards dictated by the Ministry of Health in Chile. From that foundation, we would draw up our own protocol.
Personally, I had a lot of contact with Laura Alvargonzalez, Director of Nursing at La Moraleja, one of the Sanitas hospitals in Madrid. I remember something she told me: buy ppe equipment (personal protection equipment such as masks, gloves, disposable boots, etc.) to stop the spread, because it will never be too much. Looking after your staff is the key to success.
Being part of a multinational organisation and the time it took for the pandemic to hit Chile, later than Spain, helped us prepare to fight it better. We saw how nowhere in the world was prepared for such a crisis, but I think Bupa Chile was able to plan quickly and well.
Ensuring we had staff and equipment
Because of the scale of the crisis, we had to have a joint vision that then moved into specific strategies, to deal with different situations. I think that is illustrated when we think about the planned purchase of PPE, because we needed to make sure we had enough stock to meet the projected increase in the number of beds, with occupation projected at around 100% and over 80% of that likely to be Covid patients.
Another important factor was having enough staff, because we would have people off sick with the disease or in quarantine because of contact they had had with infected people. We estimated an increase in staff based on two variables: standard care ratios and back up teams to cover sickness because of infection or quarantine, so we estimated a rise in 30% in the number of care staff. With that information in hand, the challenge was to recruit staff in a context where all healthcare providers were in the same boat and the market didn’t have enough trained professionals. So, we had to find ways to be more competitive and attractive for recruitment.
Emergency training
As there were not enough nurses with experience in intensive care unit, we brought in training in caring for patients in critical units and training in specific Covid protocol.
We created a training programme with five modules: General care of Critical Patients, Haemodynamics, Respiratory Pathology, Pharmacology and other systems focused on the main objectives in caring for critical patients, using the existing Bupa Chile platform which all our clinics have access to across the country. We also set up assessment and built a network of delegates from all the clinics to incorporate, with our contracting teams, all the people coming in from whichever modality. It was a success, and we hired and trained over 1000 people in these specific capacities.
The platform allowed us to have a system of control and followup of all the clinics and we were able to get feedback on advances or partial results, so that we could strengthen and encourage learning. That way we prepared our teams in advance, from the simplest to the most complex units.
Safety for all our patients
We prepared well, from a technical point of view, but it was not enough, if you take into account the many aspects, such as ensuring safety for all those people who needed emergency medical attention or had pressing needs other than Covid. So, plan in hand, and working together with operations, customer care, marketing, hai (Healthcare acquired infections), Quality and others, we drew up care flows to section off emergency areas. It was hard work, but we did it together.
We created two emergency zones: one for respiratory patients and the other for general consultations. We also sectioned the outpatients area with circulation flows, corridors and lifts. We put up signs for each type of care, had lines on all the floors, messages on our digital platforms and training for our teams so that they could guide patients. The sectioning off of flows and areas also took into account the hospital floors in respiratory areas and “clean” areas, as well as including a ward for surgical emergencies for positive patients or suspected Covid patients with exclusive anaesthesia machines with a double filter, amongst other measures.
The experience of clinical management

The pandemic gave us the opportunity to put to the test and show our profession’s values and the people working in healthcare. That, as well as expert knowledge, allowed us to show how versatile nursing and midwifery is, as a career. It clearly has multiple roles: care, or primary care for patients with complex needs, which needs specialised technical and professional knowledge, administration and control of resources to ensure availability and appropriate use of critical resources, the role of education for patients, families and employees, and the need to train people with the necessary knowledge and skills to meet the demand for healthcare.
We should also point out the role of clinical management, because during the pandemic we had to set up 24/7 shifts of nurses and resident midwives, to manage the beds, giving the internal and external requirements. That is because the Ministry of Health decree meant we were part of a national integrated network of care providers.
We had to report our capacity and the availability of ventilators on a daily basis, so that they could send patients from other places, and that required a lot of fine-tuning.
BearingIt has been shown that communication can be effective in many ways, that technology should be our main support, that digital transformation could get faster than it has been because of emergencies such as this one. We can only react appropriately when we unite and work together for a common objective.
Medical safety
A lot of the ward team (nurses, technicians and anaesthetists), trained up and we were able to put together mixed teams: experts with newly trained staff, to balance things out. Also, we set up a very successful position of technical visitor for nursing, made up of senior nurses in intensive care unit. They would make daily visits to new areas of the icu and talk to the nurses, making sure that all clinical safety measures were in place. We drew up a checklist, including key aspects that we called “the non-negotiables”.
We also made courtesy calls. We would go through the clinic with our lawyer and if we saw someone not using their ppe correctly we would teach them. Some got annoyed, but it was part of the strategy, and we used the situation to raise awareness and remind people that it was a standard and it had to be followed. At the same time, we made a WhatsApp video on how to use the ppe. At one point we even put up mirrors to help people use ppe correctly.
Dealing with the emotional impact
I think at the beginning we didn’t realise the extent of the emotional impact on our teams. We were of course concentrating on what our patients were going through, who were mainly elderly adults, having to die far from their families. They weren’t allowed anyone with them due to the preventive measures or because they were brought in by ambulance from other health centres and their families arrived too late.
In these situations, our teams were the ones who accompanied them on the journey from life to death. They got very emotionally involved, but they had to go on, because the situation wasn’t letting up. I can remember many such moments, and it always makes me emotional.
After that, we came up with a plan for someone from the family to be there when the prognosis was not good, and we trained them in the correct use of the ppe. So we managed to balance prevention with having someone there for the patients. That was a very important measure and I think it helped ease the emotional burden on our teams.
We have also brought in various initiatives to support the clinical teams. Every weekend people from the leadership teams go in pairs to visit the units, talk to the staff, make suggestions, provide snacks in addition to the normal meals and to thank them for their dedication and efforts.
We have also provided psychologists to support our teams, to help them and be there for them when they need us. We also have a support line, which they can call whenever they need us. Another initiative that has gone really well, in emergency, is that each day we start with a safety pause when the shifts change. Teams can tell us if they are feeling low on energy and in talking about it everyone else is put on the alert.
The psychological support is also available for patients and families. The care teams are grateful for that, because it means they can focus on the technical jobs, knowing that the families and patients can be comforted by experts.
As healthcare professionals, we are prepared to support and focussed on saving lives. We love to help our patients improve, get better and be healthy again. But now, a lot of the time, we have had to understand that this is not possible, and our role has been to be there for them and give them a good death ie, without pain, calm, knowing that we did all we could. Many times, the people who were by their side prayed or were simply there for them to help them pass from life to death our auxiliaries, nurses, doctors, therapists.
As well as having to deal with more patient deaths than usual, there was the fear of getting infected. In most cases, it wasn’t just about them, but about how they might pass it on to their families and their families get sick. Statistically, they knew that if they got sick, the potential for it being serious was low, because most of them are young people at low risk, but there was always the risk of passing it to their families.
Team absences
We had people of sick with the disease and people quarantining, and that was difficult to deal with at the beginning. Once we got the flows working better, we had more control and we were able to watch for surges in different units and intervene quickly. For those tasks, we got together working teams who, due to company policy, were sent home to protect themselves because they were at risk or vulnerable: pregnant women or people with diseases of the immune system.
We covered these absences with our part time staff or with agency staff. We had people available, we just needed to qualify and train them. I remember an auxiliary who worked part time with us: I can’t begin to say how impressed I was with the way they worked, the atmosphere, and I had never seen such dedication at such a young age. I have worked for over twenty-three years and had never seen that. It was as if all the patients were their father or mother, even worrying about whether there was a wrinkle in the sheet that could hurt the patient. That made me feel that we were meeting our objectives, looking after the patients and helping our teams do their work as well as possible.
Our families, unconditional support
I must also talk about how the families of all our teams have played a fundamental part in all of this. They may not be seen, but they give their time so that mama, papa, brother or children can look after those who are alone, during the day, the night and the weekend.
My husband is a doctor. He has been through what I have. But he was able to organise his time to be at home more and give more time to our daughters, helping them with the new home school routines. It was difficult to start with, but they soon got used to it. I talk to my daughters a lot, telling them stories, telling them what is going on. I want them to know what their mama does every day and why I have to spend so many hours at the hospital. At the beginning of July, I got infected with Covid, along with everyone at home. Thankfully, none of us were seriously ill.
Creative solutions
Creativity has helped us deal with problems that have arisen from the extra restrictions of the pandemic. Problems such as: keeping vigilant and keeping down entry into the rooms in order to avoid the spread of the virus. We have put in extensions and pumps and ventilation equipment outside the rooms, which has helped us reduce the exposure of our staff.
Another example of creativity which we set up together with the customer experience department was to encourage patients’ families to send them messages printed in big letters, which we stick
on the windows of their rooms so they can see them. That was really important for the people in hospital, and helped them feel less alone. Another idea our teams had, to deal with the damage caused to peoples’ skin because of using masks all the time, was to make caps with buttons they could fix onto.
Overall, it has been a time of creativity, lots of different ideas of how to deal with big problems and challenges faced every day. That was when we realised it was important and necessary to give visibility and recognition to our professionals. To tell the world what nurses, midwives and all healthcare teams do, but also to show them all the skills that are not always recognised and that are part of their deep commitment to the wellbeing and care of others. Without this commitment and passion they put into their work, we wouldn’t have been so successful.
Bupa Chile has set up a working group to prepare for the celebration of the International Year of the Nurse and the Midwife, led by the Medical Management and coordinated together with Sanitas, which had to modify its initial programme because of the pandemic. In this context, a book of recognition is a new way of commemorating such a special year.
The idea of this book of stories snowballed. Everyone we shared the idea with supported us and brought in more ideas. We started enthusing others, we shared the ideas with nurses in Spain and they loved it! The manager of the clinical sector encouraged us and gave us the opportunity to present the book project to the Bupa Chile board, and we did that. We have a really united committee. They were really excited about the ideas and proposals and brought in new ideas too. Soon we had everyone in agreement with the project.
To tell the world what nurses, midwives and all healthcare teams do, but also to show them all the skills that are not always recognised and that are part of their deep commitment to the wellbeing and care of others.

Telling our stories
This has been an amazing experience and we should pass it on to those who will carry the torch into the future, helping them do things right. If they can act based on evidence, they can act more quickly and confidently.
During the pandemic, we took part in and organised various webinars about the pandemic and its different aspects. It was always really useful and enriching to hear and learn about others’ experiences and see the evidence that science has made available to the world and use it in our own protocols and guidelines.
This has been an amazing experience and we should pass it on to those who will carry the torch into the future, helping them do things right. If they can act based on evidence, they can act more quickly and confidently.
There are certainly a lot of things we will do differently in the future. For example, we have action plans for emerging diseases and segmentation measures to prevent infection.
It has been shown that communication can be effective in many ways, that technology should be our main support, that digital transformation could get faster than it has been because of emergencies such as this one. We can only react appropriately when we unite and work together for a common objective.�

judith aguilera carla alarcón giannina allende laura alvargonzalez constanza avendaño ximena báez rossana bravo carolina burgos mª elena bustamante violeta carrión tamara casado mª victoria casas natalia castañeda sergio castaño mª francisca castillo claudia collao óscar cruz geidy cuza alicia díaz claudia escobar gianina espinoza andrea espiñeira beatriz estéfani paula feres mª eugenia fernández teresa fernández
daniela figueroa paulina roa sofía gaete patricia gajardo marta garcía patricia godoy lidia gómez maría gonzález clara gonzález sonia guerrero estefanía hernández yolanda huerta begoña inchaurraga evelyn jara silvia jiménez susana jorquera rosa larios alejandro lleixa alejandra llorente purificación loeb sarvia mardones mª gloria marinas covadonga medrano daniel millán betsy moraga constanza núñez
valeria pardo raquel pérez lucrecia pinillos mª jesús puyol marta quelle isabel rico nuria ríos donna ritchie angélica rodríguez marta rodríguez melanie rodríguez natalia sáez cristina satóstegui elizabeth silva mª ester smith darío tapia susana toro esther ulloa hilda vargas adolfo vásquez juan pablo vásquez grace vera zaira villagra laura visansay *
We are grateful to everyone who has generously shared their experiences of the pandemic, because without their valuable contributions, this book would not have been possible. We would also like to thank all the healthcare staff whose work and commitment have inspired this book.

This book is dedicated to all the healthcare and support teams, whose work and committment has inspired the whole world, and to all our colleagues who have lost their lives in this pandemic and whose stories will never be told.
In this book, Bupa Chile pays tribute to the women and men whose dedication has been a credit to their profession in the worst pandemic of the last 100 years.
In the International Year of the Nurse and the Midwife, these professionals have been put to the test at the toughest of times and have displayed the utmost skill and ability in the managing, serving, healing, relieving or simply being there for people.
Based on 80 interviews carried out in Chile and Spain, these real-time reports show how this crisis has affected people deeply and helps us understand the huge task undertaken by those on the front line, leaving a legacy for future generations.
«Your stories have to be valued for the skilled care they describe. Nurses around the world raise their voices with you in pride. Thank you for all you have done and for sharing your story».
«These nurses have faced the challenges of the pandemic and other healthcare problems with compassion, care, resilience, creativity and great leadership skills, as we will see from the reports and stories in this book».
President of the International Council of Nurses, icn
annette kennedy barbara stilwell Executive Director of Nursing Now Global Campaign

