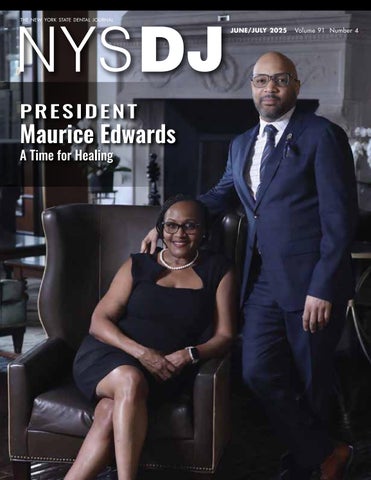
PRESIDENT Maurice Edwards
A Time for Healing

16 To Thine Own Self be True
Periodontist Allison Rascon reflects on celebration of Pride Month and her journey to embracing her personal identity.
18 Turning the Page on the Past
Maurice L. Edwards, D.M.D., NYSDA’s 144th President, is committed to making a fresh start for the Association and its members.
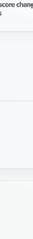
26 Practicing Dentistry in the Age of Periodontal Risk
Roger N. Warren, D.D.S.; Liana Umbrio, D.D.S.; Leena Palomo, D.D.S., M.S.D.
Dental professionals are equipped with evidence-based risk factors to predict and prevent progression of periodontal disease. Implementing chairside risk assessment allows for prevention and early intervention, potentially reducing healthcare costs and promoting simpler solutions in unpredictable economy.
33 Orofacial Manifestations of Highly Active Antiretroviral Therapy (HAART) and Pre-Exposure Prophylaxis (PrEP)
Alec Donelian; Yuedi Yu; Ezzard Rolle, D.D.S.; Alison Newgard, D.D.S.
Improved treatments for HIV have enhanced lives and life expectancy of patients, but have also produced a range of orofacial side effects. Authors provide clinical recommendations for dental professionals treating patients on either HAART or PrEP and their associated risk factors.
40 Assessment of
Cristina Osorio, D.D.S.;
Study undertaken to evaluate patient understanding of scope of prosthodontic treatments revealed gap in patient awareness of full range of prosthodontic services.
B.D.S.;
Hannah Jeong; Thomas S. Giugliano, D.D.S.
Cover: NYSDA President Maurice L. Edwards and wife, Michelle. Striving for a life worth living.
Photo by Carlo Messina, F/X Video
Good Faith Estimates and the No Surprises Act
Federal law requires dentists to be up front with self-pay patients about the cost of their treatment. Surprises may lead to penalties.
The No Surprises Act (NSA) went into effect on Jan. 1, 2022. This is a federal law that applies to all health-care providers, including dentists. The law gives certain rights to patients to help protect them from receiving surprise medical bills. These surprises usually occur when a person has no control over who treats them, such as during an emergency or when they are treated unknowingly by an out-of-network provider.[1]
Within the NSA there are provisions for health-care providers to furnish patients with a good faith estimate (GFE). Any dental patient who doesn’t have dental insurance or doesn’t want to file a claim must be provided with a GFE before treatment can be rendered. NYSDA Legal Counsel Lance Plunkett explained in a memo to members: “If you bill an insurer at all, then the good faith estimate does not apply. It doesn’t matter if the insurer refuses to pay or if the patient pays first. If you send a claim to the insurer, then the good faith estimate does not apply.”
There are times when a patient doesn’t want to wait for the preauthorization to come back and they pay in advance. These patients are not self-pay, because they have insurance, in what is described as only a case of delayed insurance billing.
Mr. Plunkett also said it doesn’t matter if you’re a participating provider with the plan or not. So long as the patient has dental insurance and you are billing it out for them, there is no need to provide a GFE (Medicaid being the exception). Mr. Plunkett stressed, “However, if there is no coverage at all for a service, the patient selfpays, no claim is filed with the insurer, and the dentist is not bound by any non-covered service discounts and charges—then that is a self-pay scenario requiring a good faith estimate.”
There are also dental plans that necessitate non-covered services (which are not insured services) to be paid at a discounted rate (that is, discount plans), and since those discounts are part of the patient’s insurance plan, dentists are not required to provide a good faith estimate. Though vetoed twice by the governor, NYSDA is again seeking legislation to terminate discounted rate plans in New York State, which would then require GFEs.
And there is a scheduled time frame within which the GFE must be provided, as well as requirements for structuring the GFE.[2,3,4] I have outlined these below as they should be presented to your patients. Note that the deadline for providing a GFE is triggered either when the patient asks for an estimate or schedules an appointment.
What Your Patients Need to Know Time frame for a Good Faith Estimate
“You should get a good faith estimate if you schedule an appointment at least 3 business days in advance. You can ask your provider directly for an estimate if they don’t give one to you.
• When you schedule care 0-2 business days in advance, you aren’t entitled to get a good faith estimate.
• When you schedule care 3-9 business days in advance, you’ll get the estimate within 1 business day.
• When you schedule care 10 or more business days in advance, you’ll get the estimate within 3 business days. You can ask your provider for an estimate before you schedule care. They must give it to you within 3 business days.”[3]
The GFE should include the name and birthdate of the patient, when the primary service is to be performed, the dental codes/medical codes for the work being done, the practice/provider’s name, tax ID, NPI, the address where treatment will be rendered and a list of possible treatments that will be needed afterward.[5,6] These must be given “in a way that’s accessible to you (the patient), like in large print, Braille, audio files, or other forms of communication. Providers and facilities must also explain the good faith estimate to you over the phone or in person if you ask, then follow up with a written (paper or electronic) estimate, per your preferred form of communication.”[7]
Good Faith Estimate Inclusions
• “A description of the service you will be getting;
• A list of other services that are reasonably expected to be provided with the service you are getting;
• The diagnosis and expected service codes;
• The expected charges for the services;”[2]
• A disclaimer.
Charts can also be utilized in preparing the GFE,[5] and there are some very good examples online.[8,9] I am happy to share with you the forms I use in my office when providing patients with a good faith estimate. Email me at eperio@aol.com and I will send them to you.
Putting the Law into Practice
According to my office manager, our earliest and perhaps biggest challenge was generating a GFE that fits our practice and reflects our services and costs in a way that is accurate without being overwhelming to patients, while meeting the GFE compliance standards.
For us, this meant creating different versions of the GFE: one for new patients outlining consultation costs; one for surgical patients; and one for recall hygiene patients. Our office
EDITOR
Stuart L. Segelnick, D.D.S., M.S.
MANAGING EDITOR
Mary Grates Stoll
ADVERTISING/SPONSORSHIP MANAGER
Jeanne DeGuire
ART DIRECTOR
Ed Stevens
EDITORIAL REVIEW BOARD
Frank C. Barnashuk, DDS. Past Clinical Assistant Professor, Department of Restorative Dentistry, University at Buffalo School of Dental Medicine, Buffalo, NY.
David A. Behrman, DMD. Chief, Division Dentistry/OMS, Associate Professor of Surgery, New York-Presbyterian Hospital, Weill Cornell Medicine, New York, NY.
Michael R. Breault, DDS. Periodontic/Implantology. Private Practice. Schenectady, NY.
David Croglio, DDS. Clinical Assistant Professor, University at Buffalo School of Dental Medicine, Buffalo, NY. Private Practice (retired), Amherst, NY.
Jennifer Frustino, DDS, PhD. Director, Oral Cancer Screening and Diagnostics, Division Oral Oncology and Maxillofacial Prosthetics, Department of Dentistry, Erie County Medical Center, Buffalo, NY.
Michael F. Gengo, DDS. Board-certified Endodontist, Clinical Assistant Professor, Department of Endodontics, University at Buffalo School of Dental Medicine, Buffalo, NY. Private Practice, Hamburg, NY.
G. Kirk Gleason, DDS. General Dental Practice (retired), Clifton Park, NY.
Kevin Hanley, DDS. Orthodontic Private Practice, Buffalo, NY.
Stanley M. Kerpel, DDS. Diplomate, American Board Oral and Maxillofacial Pathology, Associate Director, Oral Pathology Laboratory, Inc. Attending, Section of Oral Pathology, New York-Presbyterian, Queens, NY.
Robert M. Peskin, DDS. Dental Anesthesiology Private Practice, Garden City, NY.
Mohini Ratakonda, DDS, Clinical Assistant Professor, University at Buffalo School of Dental Medicine, Buffalo, NY. Endodontics.
Joseph Rumfola, DDS. Clinical Assistant Professor, AEGD Program Director, University at Buffalo School of Dental Medicine, Buffalo, NY. Private Practice, Springville, NY.
Jay Skolnick, DMD. Board-certified Pediatric Dentist. Attending dentist, Rochester General Hospital. Private Practice, Webster, NY.
Lisa Marie Yerke, DDS, MS. Diplomate, American Board Peiodontology, Clinical Associate Professor, Director Advanced Education Program in Periodontics, University at Buffalo School of Dental Medicine Department Periodontics & Endodontics, Buffalo, NY. Private Practice, East Amherst, NY.
PRINTER
Fort Orange Press, Albany

NYSDJ (ISSN 0028-7571) appears two times a year in print: January and June/July. The March, April, August/September and November issues are available online only at www.nysdental.org. The Journal is a publication of the New York State Dental Association, 20 Corporate Woods Boulevard, Suite 602, Albany, NY 12211. In February, May, October and December, members have online access to the NYSDA News. Subscription rates for nonmembers: $75 per year or $12 per issue, U.S. and Canada; $135 per year foreign or $22 per issue. Editorial and advertising offices are at Suite 602, 20 Corporate Woods Boulevard, Albany, NY 12211. Telephone (518) 465-0044. Email info@nysdental.org. Website www.nysdental.org.
then prepares and sends out the GFEs immediately following the scheduling of the appointment via email. We find this to be the best practice to ensure compliance.
Some patients may not have access to email or may struggle to open encrypted files. Patients can insist on a written estimate instead of ones sent electronically. In these instances, postal mail will be sent. Patient information, including the patient’s full mailing address, will need to be collected. Some new patients may be hesitant to provide this information prior to their first office visit.
We also took time to prepare versions of the GFE in Spanish and Russian, including disclaimers. Other practices may need to do the same, depending on their patient demographic, to ensure accessibility of the GFE.
A good time to provide the GFE is when the patient is in the office scheduling their next appointment. Remember, same-day emergency care, or scheduling appointments within two days, does not initiate the GFE process and, therefore, a GFE does not need to be given.
The No Surprises Act stipulates that the patient has a right to dispute their bill only if the GFE differs by $400 dollars or more from what was charged. This is separate from their right to receive the GFE. Penalties range from having
lation. According to Mr. Plunkett, the Office of Professional Discipline (OPD) might take action against a dentist’s license for willful violation of the law; therefore, it is always best to comply with the law and avoid the possible surprising penalties of noncompliance.

REFERENCES
1. https://www.mayoclinic.org/billing-insurance/no-surprises-act#:~:text=Under%20the%20 law%2C%20healthcare%20providers,items%20or%20services%20are%20provided (Accessed 8/11/2024)
2. https://www.dfs.ny.gov/consumers/health_insurance/protections_federal_no_surprises_act (Accessed 8/11/2024)
3. https://www.cms.gov/medical-bill-rights/help/guides/good-faith-estimate (Accessed 8/11/2024)
4. https://www.ecfr.gov/current/title-45/subtitle-A/subchapter-B/part-149#p-149.610(c)
5. https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/GuidanceGood-Faith-Estimate-Patient-Provider-Dispute-Resolution-Process-for-Providers-FacilitiesCMS-9908-IFC.pdf
6. https://www.cms.gov/files/document/gfe-and-ppdr-requirements-slides.pdf
7. h ttps://www.cms.gov/files/document/nosurpriseactfactsheet-whats-good-faith-estimate508c.pdf
8. https://www.cms.gov/files/document/good-faith-estimate-example.pdf
9. https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fwww.michigandental. org %2Fwp-content%2Fuploads%2F2022%2F02%2FSample-Good-Faith-Estimate-for-


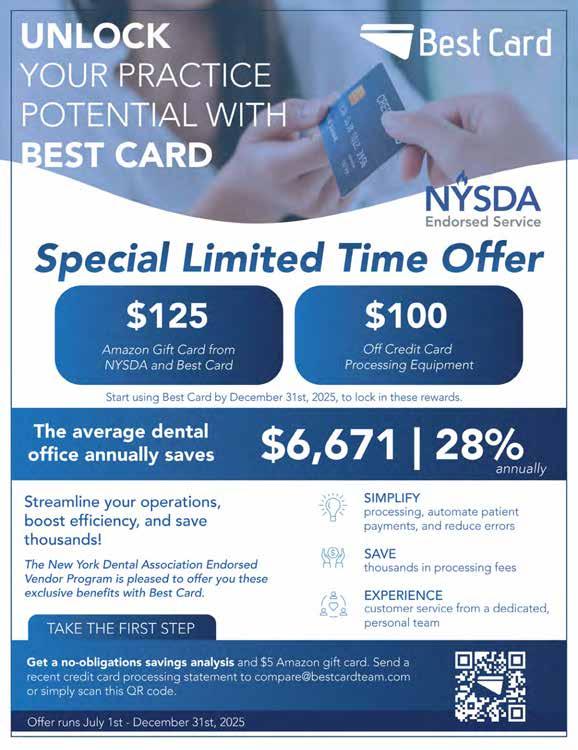
New York Dentists: Unlock Savings with NYSDA-endorsed Best
Card Promotion!
In a continued effort to look out for its members, the New York State Dental Association is proud to offer a valuable benefit: an exclusive partnership with Best Card, the industry leader in credit card processing for dental practices.
Why This Partnership Matters for NYSDA Members
By partnering with Best Card, NYSDA ensures that dentists can access one of the most trusted and costeffective payment processors in the industry. Dentists who switch to Best Card save an average of $6,671 per year, reducing their payment processing costs by about 28%. These savings go directly to your bottom line-- money that can be better spent improving your practice or patient care.
Best Card’s tailored services include standalone terminals, mobile processing, online payment options, and seamless integration with popular dental software, all designed with your practice in mind.
Limited-Time Offer: Get $125 Amazon Gift Card!
NYSDA and Best Card are offering a limited-time promotion for our members. Sign up between July 1 and December 31, 2025, and you’ll receive a $125 Amazon gift card from Best Card. It’s a simple, nostrings-attached way of thanking you for making a smart decision for your practice.
How to Get Started
To see how much you can save, email a recent credit card statement to compare@bestcardteam.com or call 877-739-3952 for a personalized savings analysis. Best Card’s team will show you exactly where you can cut costs—and they’re always available to answer your questions.
Don’t Miss Out - Sign Up Today!
This exclusive promotion is a limited-time opportunity to enjoy both upfront rewards and long-term savings for your practice. If you’re ready to take control of your payment processing costs, contact Best Card today to get started. Join the thousands of dentists already benefiting from Best Card’s unmatched service and savings - and earn a $125 gift card!
Learn more here: https://bestcardteam.com/NYSDA



Dr. Paul Leary
“I have been an active participant with Best Card since its initial recommendation as an ADA/NYSDA-sponsored credit card processor. Their customer service made our transition to their service flawless. Their rates have saved me thousands of dollars in credit card processing fees and their attention to PCI compliance makes the entire relationship one I rely on to handle all this in one stop. Our experience with them has been great.”
TRevised Law Impacts Conduct of Business in Office and at Home
The ease of automatic renewals is countered by strict new requirements in General Business Law attached to their use.
Lance Plunkett, J.D., LL.M.
he 2025-2026 New York State Budget contains few new laws related to dentistry. Note that the 2025 legislative session may have finished with the State Budget but is continuing in June with respect to other stand-alone bills.
The final budget did not include amendments to the Material Transactions Law that was covered extensively in the April Journal. Many people had expected that law to be expanded, but Gov. Hochul’s ideas on that were not adopted by the Legislature. However, the New York State Department of Health issued its promised model reporting form and instructions, which can be accessed at the following link: https://survey. alchemer.com/s3/8019921/Material-Transaction-Notice.
While the Material Transactions Law applies to dental practices, the $25-million gross revenue threshold seriously limits which dental practice transactions will need to be reported to the Department of Health. Of more interest in the State Budget are sweeping revisions to sections 527 and 527-a of the New York State General Busi-
ness Law (GBL) concerning automatic renewals of subscriptions, memberships and other similar arrangements. The changes to the law follow an increasing trend in New York to enhance consumer protections. The new laws will mostly affect NYSDA but could also affect dental practices that offer patients in-house payment plan arrangements if they auto-renew, and dentists’ personal rights concerning their own subscriptions and memberships. The new laws take effect on Nov. 5, so there is time to come into compliance with them in advance.
Make it Clear and Conspicuous
GBL Section 527(1) defines an automatic renewal as “a plan or arrangement in which a paid subscription or purchasing agreement is automatically renewed at the end of a definite term for a subsequent term.” GBL Section 527-a(1)(a) makes it unlawful for any business making an automatic renewal or continuous service offer to a consumer to fail to present to the consumer, in a clear and conspicuous manner, the material
terms of any automatic renewal offer or continuous service offer, including but not limited to:
1. A description of the product or service subject to renewal.
2. The amount of the costs that will be charged. 3. The frequency of charges.
4. The deadline by date or frequency by which the consumer must act to prevent or stop further charges.
5. The cancellation mechanisms described in the new law.
These items must be provided before consent to the offer or billing information has been requested and in visual proximity, or in the case of an offer conveyed by voice, in temporal proximity, to the request for consent to the offer.
If the offer also includes a free gift or trial, or the price is temporary, the offer shall include a clear and conspicuous explanation of how and when the price will change and the price or prices that will subsequently be charged to the consumer. “Clear and conspicuous” is defined in GBL Section 527(2) to mean in larger type than the surrounding text, or in contrasting type, font or color to the surrounding text of the same size, or set off from the surrounding text of the same size by symbols or other marks, in a manner that clearly calls attention to the language.
In the case of an audio disclosure, “clear and conspicuous” means in a volume and cadence sufficient to be readily audible and understandable.
The cancellation mechanisms in the new law are described in GBL sections 527-a(1)(d) and 527-a(1) (d-1). Section 527-a(d)(1) makes it unlawful to fail to provide the consumer with the option to cancel at any time using a simple cancellation mechanism that is as easy to use as the mechanism that the consumer used to provide consent and that is through the same medium that the consumer used to provide consent.
GBL Section 527-a(1)(d-1) also makes it illegal to fail to provide the consumer with the option to cancel at any time through all mediums by which the business allows a consumer to provide affirmative consent to the automatic renewal, continuous service offer or any price increase.
Where consent was obtained in person, in addition to offering cancellation, where practical via an in-person method similar to what the user used to consent, the business shall at least offer cancellation through an online mechanism or over a telephone number.
Note that price increases cannot be easily hidden under the new law. Special provisions cover situations
NYSDA Directory
OFFICERS
Maurice Edwards, President 30 East 60th St., #1401, New York, NY 10022
Amarilis Jacobo, President-Elect 824 East 181st St., Bronx, NY 10460
Lynn Stacy, Vice President 7504 East State St., Lowville, NY 13367
Paul Leary, Secretary-Treasurer 80 Maple Ave., Ste 206, Smithtown, NY 11787
William Karp, Speaker of the House 4500 Pewter Ln., Bldg 6, Manlius, NY 13104
BOARD OF TRUSTEES
Prabha Krishnan, Immediate Past President 11045 Queens Blvd., Ste 108, Forest Hills, NY 11375
Brendan Dowd, ADA Trustee 3435 Main St., Squire Hall, Room 235G, Buffalo, NY 14214
NY – James E. Jacobs 30 Central Park South, Room 2A, New York, NY 10019
2 – John P. Demas 8814 Fort Hamilton Pkwy, Brooklyn, NY 11209
3 – Geoffrey Gamache 24 Eastview Rd., Averill Park, NY 12018
4 – Adrienne L. Korkosz 1309 Union St., Schenectady, NY 12308
5 – Steven Stacey 6702 Buckley Rd., Ste 120, Syracuse, NY 13212
6 – Louis Giordano 864 Hooper Rd., Endwell, NY 13760
7 – David Ramjattansingh 71 King Arthurs Ct., Rochester, NY 14626
8 – Raymond G. Miller 122 Covington Rd., Buffalo, NY 14216
9 – Gary M. Scharof f 1255 North Ave., Ste A1H, New Rochelle, NY 10804
N – Donald R. Hills 136 Woodbur y Rd., Ste L3, Woodbury, NY 11797
Q – Mitchell S. Greenberg 11966 80th Rd., #1A, Kew Gardens, NY 11415
S – Martin Dominger 5225 Nesconset Hwy., Suite 57, Port Jefferson Station, NY 117776
B – Jacqueline J. Samuels 120 Alcott Place, Bronx, NY 10475
COUNCIL CHAIRPERSONS
Dental Benefit Programs
Dental Education
Joseph A. Craddock 3325 East Main St., Attica, NY 14011
Robert M. Peskin 601 Frankline Ave. #225, Garden City, NY 11530
Dental Health Planning Maria Maranga 8 Rolling Meadow Ln., Northport, NY 11768
Dental Practice Mina Kim 2 West 46th Street, #501, Br yant Park Dental Assoc., New York, NY 10036
Ethics
Governmental Affairs
Membership & Communications
Nominations
Peer Review
OFFICE
Julie A. Connolly 115 East 61st Street, Fl. 8, New York, NY 10065
Radha Sachdeva-Munk 203 Smithtown Blvd., Nesconset, NY 11767
Christopher W. Calnon 3220 Chili Ave., Rochester, NY 14624
Prabha Krishnan 11045 Queens Blvd., Ste 108, Forest Hills, NY 11375
Lawrence J. Lehman 7303 197th St., Fresh Meadows, NY 11366
Suite 602, 20 Corporate Woods Blvd., Albany, NY 12211 (518) 465-0044 | (800) 255-2100
Michael Herrmann Executive Director
Lance R. Plunkett General Counsel
Mary Grates Stoll Managing Editor
Jenna Bell Director Meeting Planning
Briana McNamee Director Governmental Affairs
Jacquie Donnelly Director Dental Practice Support
Heather Relation Director Outreach Membership & Engagement
Stacy McIlduff Executive Director NYS Dental Foundation
where any increase in price is involved. Section 527-a(1)(b) makes it illegal to charge the consumer or the consumer’s account with a third party (like a credit card or bank account) for the initial term of an automatic renewal or continuous service offer without first obtaining the consumer’s affirmative consent to the agreement containing the terms of automatic renewal or continuous service offer, including the terms of an automatic renewal or continuous service offer that is made at a promotional or discounted price for a limited period of time.
In addition, GBL Section 527-a(1)(b-1) makes it illegal to charge the consumer or the consumer’s account with a third party following an increase in price, or a price higher than what was disclosed pursuant to the original required disclosures, relating to an automatic renewal or continuous service offer to which the consumer previously consented, without either: 1) first obtaining the consumer’s affirmative consent to such increased price; or 2) allowing the consumer to cancel such automatic renewal or continuous service anytime within, at least, fourteen days after such charge and refund the consumer in the amount equivalent to the price of the remaining term of the service, at the time of such cancellation, on a pro rata basis.
However, a business is not required to obtain affirmative consent from the consumer regarding a price increase, or a price increase not disclosed in the original automatic renewal or continuous service offer, more than once prior to charging the consumer the increased price.
Give Prompt Notice
GBL Section 527-a(1)(c) also makes it illegal to fail to provide notice promptly following obtaining affirmative consent in a manner that is capable of being retained by the consumer. Such notice must include:
1. The terms of the automatic renewal or continuous service agreement.
2. The amount of costs that will be charged.
3. The frequency of charges.
4. The deadline by date or frequency by which the consumer must act to prevent or stop further charges.
5. The cancellation mechanisms required under the new law.
This notice is separate from the notice described above in GBL Section 527-a(1)(a).
GBL Section 527-a(1)(e) makes it illegal to impose unreasonable or unlawful conditions upon, refuse to acknowledge, obstruct or unreasonably delay cancellation requested or attempts to request cancellation by a consumer. In addition, the law defines unreasonable or unlawful conditions to include, without limitation, hanging up on
consumers who call to cancel, providing false information about how to cancel, misrepresenting the consequences or costs of cancellation, or misrepresenting the reasons for delays in processing consumers’ cancellation requests.
If a consumer conveys a request to cancel, the business may present the consumer with a discounted offer, retention benefit or information regarding the effect of cancellation but may not impose unreasonable or unlawful conditions upon the consumer’s ability to cancel, or refuse to acknowledge, obstruct or unreasonably delay the cancellation requested.
The new law also limits the ability to impose any extra charge for renewals. GBL Section 527-a(1)(f) makes it illegal to fail to notify a consumer of an automatic renewal or continuous service charge for an automatic renewal or continuous service offer with an initial paid term of one year or longer, provided that such automatic renewal or continuous service renews for a paid term of six months or longer, at least fifteen days before, but not more than forty-five days before, the cancellation deadline for such automatic renewal in the manner selected by the consumer, including text, email, app notification, or any other notification channel offered by the business. Such notice must include instructions on how to cancel the renewal charge.
Similarly, Section 527-a(1)(g) makes it illegal to fail to provide a consumer who has accepted an automatic renewal or continuous service offer with a clear and conspicuous notice of any material change to the terms of the automatic renewal or continuous service offer, including any price increases, at least five business days prior, but no more than thirty days prior, to the date of the change, in the same manner as required for notice of renewal charges.
Similarly, GBL Section 527-a(1)(h) makes it illegal to fail to notify a consumer of an automatic renewal or continuous service charge for an automatic renewal or continuous service offer if the automatic renewal or continuous service offer includes a free gift or trial for a period of more than a month, followed by an upcoming automatic renewal or continuous service charge, at least three days before but not more than twenty-one days before the cancellation deadline for the first chargeable period in the manner selected by the consumer, including text, email, app notification or any other notification channel offered by the business. Such notice shall include instructions on how to cancel the renewal charge.
Finally, GBL Section 527-a(2) provides that in any case in which a business sends goods, wares, merchandise or products to a consumer, under a continuous service agreement or automatic renewal of a purchase, without first obtaining the consumer’s affirmative consent, the goods,
wares, merchandise or products shall for all purposes be deemed an unconditional gift to the consumer, who may use or dispose of the same in any manner such consumer sees fit without any obligation whatsoever on the consumer’s part to the business, including, but not limited to, bearing the cost of, or responsibility for, shipping any goods, wares, merchandise or products to the business.
The New York State Attorney General may seek injunctive relief to stop any business from violating the new law. In addition, a court may impose a civil penalty of not more than $100 for a single violation and not more than $500 for multiple violations resulting from a single act or incident. A knowing violation of the law is punishable by a civil penalty of not more than $500 for a single violation and not more than $1,000 for multiple violations resulting from a single act or incident. However, no business is deemed to have violated the provisions of the law if the business shows, by a preponderance of evidence, that the violation was not intentional and resulted from a bona fide error made notwithstanding the maintenance of procedures reasonably adopted to avoid such error.
Laws Favor Consumers
New York State is increasingly enacting stronger consumer protection laws that impose burdens on all businesses. When dentists are consumers, they may find the new laws helpful. When dentists offer certain deals through their professional practices, they may find the new laws cumbersome.
New York is not alone in having concerns with people getting trapped in automatic renewal arrangements from which they find it difficult to extricate themselves, especially when they include price increases. The federal government and other states have been moving in a similar direction. This is an issue where self-interest plays a big role. Anyone who has felt he or she is a victim of an autorenewal scheme agrees with the consumer-friendly direction the new law takes.p



Making Our Voices Heard
ADVOCATING FOR THE PROFESSION is one of the most important services the ADA provides for its members. This benefit was in full force Mar. 30 to April 1 when the American Dental Political Action Committee (ADPAC) appeared in Washington, DC, for its annual Dentist and Student Lobby Day. Among the over 1,100 assembled from around the country, was a delegation of 63 from New York State that included 24 member dentists, 36 students from all five dental schools in the state and 3 NYSDA staff. It was led by the Second District’s ADPAC Board Representative Dr. Michael Shreck. He was assisted by Dr. Vera Tang, American Academy of Periodontics Board Representative.
While in Washington, ADPAC hosted a very successful fundraiser at the ADA townhouse on the House side of Congress for GOP Representative Dr. Brian Babin of Texas, one of three ADA members in Congress and a sponsor of the bipartisan Resident Education Deferred Interest Act.
During their stay in the nation’s capital, members of the New York delegation visited with their state’s senators and almost every New York Representative in Congress. They were advocating for three measures that directly affect practicing dentists, dental students and the public. They include the following.
• The Dental and Optometric Care (DOC) Act. Would prevent dental and vision plans from requiring providers to accept fees for non-covered services. Would also prevent insurance plans from classifying non-covered services as “covered,” allow contract extensions beyond two years only with the provider permission and prohibit restricting providers’ choice of labs or suppliers.
• The Resident Education Deferred Interest (REDI) Act. Would ensure medical and dental residents qualify for an interest-free deferment on payment for their government student loans until after residency is completed.
• Community Water Fluoridation: The Importance of Rigorous Research. An appropriations measure asking the National Institutes of Health to conduct a study regarding low levels of fluoride exposure and IQ. Aimed at combatting the flawed 2024 National Toxicology Program report that has created many false and misleading claims about fluoride.
In Washington, DC, to speak to concerns of dental profession are New York representatives, from left, Second District Trustee Brendan Dowd, NYCDS President Vera Tang, ADPAC Board representative Michael Shreck, NYSDA President and President-Elect Prabha Krishnan and Maurice Edwards, NYSDA Executive Director Michael Herrmann.
Dr. Shreck with Dr. Brian Babin of Texas, one of three dentists serving in House of Representatives.
Association Activities


Team NYSDA
In what has become an annual tradition, NYSDA fielded a group of runners/walkers in the CDPHP Workplace Team Challenge on May 15 in downtown Albany. The 3.5-mile challenge, now in its 45th year, attracts more than 8,000 participants, making it the largest running event in the Capital Region. Proceeds go to support the philanthropic and community projects of the Hudson-Mohawk Road Runners Club. Assembled at the starting point are, from left, Peter Lacijan, Lauren Heisinger, Kasey Bennett, Katie Rothas, Heather Relation, Stacy McIlduff, Patty Marcucia. Amanda Armao, at far right, participated virtually.
State Board Appointments Announced
TWO NYSDA MEMBERS are among those tapped by the New York State Board of Regents to serve on state professional boards. Dr. Patricia Haberman of the Eighth District was appointed to a five-year term as an extended member of the New York State Board for Dentistry, and Dr. Richard Goliber of the Third District was reappointed to a five-year term on the Professional Assistance Program (PAP).
Dr. Haberman of Williamsville is on the faculty of the University at Buffalo School of Dental Medicine. As an extended member of the Board for Dentistry, she will serve on licensure disciplinary and/or licensure restoration and moral character panels. Dr. Goliber is retired and lives in Albany.
ETHICS COUNCIL ISSUES RULINGS
ON APRIL 8, 2025, the NYSDA Council on Ethics issued an order to suspend Dr. Peter Salvatore Felpo (License No. 034250) from membership for two (2) years; execution of said suspension be stayed; and respondent be placed on a two (2) year probation to include continuing education.
After a full hearing on March 21, 2025, the Council on Ethics found that Dr. Felpo had been disciplined for professional misconduct by the New York State Education Department Board of Regents and, as such, was in violation of Paragraph B of Section 20 Chapter X of the NYSDA Bylaws. Dr. Felpo did not appeal the Council’s decision within the requisite 30-day timeframe to the American Dental Association (ADA). The decision of the NYSDA Council on Ethics thereby became final and effective as of May 8, 2025.
ON APRIL 8, 2025, the NYSDA Council on Ethics issued an order to suspend Dr. Marshall Steven Skopp (License No. 045275) from membership for two (2) years; execution of said suspension be stayed; and respondent be placed on a two (2) year probation.
After a full hearing on March 21, 2025, the Council on Ethics found that Dr. Skopp had been disciplined for professional misconduct by the New York State Education Department Board of Regents and, as such, was in violation of Paragraph B of Section 20 Chapter X of the NYSDA Bylaws. Dr. Skopp did not appeal the Council’s decision within the requisite 30-day timeframe to the American Dental Association (ADA). The decision of the NYSDA Council on Ethics thereby became final and effective as of May 8, 2025.
Association Activities
House of Delegates Annual Session
May 30-31





NYSDA’s 2025-2026 leaders following installation at HOD Annual Meeting. From left, Secretary-Treasurer Paul Leary, Vice President Lynn Stacy, President-Elect Amarilis Jacobo, President Maurice Edwards, Immediate Past President Prabha Krishnan, Speaker of House William Karp.
Bernard Hackett, due to retire at end of year as Second District Dental Society Executive Director, is proud new honorary member of ADA.
Taking seat on Board are three new trustees, sworn in at Annual Meeting. They are, from left: James Jacobs, New York County; David Ramjattansingh, Seventh District; Martin Dominger, Suffolk County. They are joined by Dr. Krishnan.
Recognized for service on NYSDA Board are retiring trustees, from left, Past President Anthony Cuomo, Thresea Casper-Klock, Guenter Jonke. They are joined by Dr. Krishnan. Dr. Jonke was further honored as recipient of 2025 Mark J. Feldman Distinguished Service Award.
Maria Maranga congratulates Payam Goudarzi, Sixth District, elected to serve as next Second District Trustee to ADA.
In Memoriam
SECOND DISTRICT
Stephen Cohen
Temple University ‘72
75 Riverside Dr., Apt 5F
New York, NY 10024
May 2, 2025
FIFTH DISTRICT
Howard Berg
University of Pennsylvania ‘63
1660 Gaton Dr., Apt SQ25
San Jose, CA 95125
October 18, 2024
SIXTH DISTRICT
James Farrell
University of Pennsylvania ‘59 2423 Donlon Rd
Wilmington, DE 19803
May 2, 2025
EIGHTH DISTRICT
William Maher
University at Buffalo ‘63 5238 Lake Shore Rd. Hamburg, NY 14075
May 23, 2025
Legal ProtectionPlan Protection Plan
NINTH DISTRICT
Stephen Oustatcher
New York University ‘70 21 Dads Ln.
Stamford, CT 06903
May 16, 2025

Sales tax audits
OPD investigations
Insurance company disputes
HIPAA and OSHA complaints and compliance
Workers’ Compensation challenges and investigations
Defending claims involving identity theft issues
Investigation/proceedings before IPRO and Office of Civil Rights
Responding to claim reimbursement by NYS or federal regulatory agencies including Medicaid and Medicare


Endorsed Vendor Updates Endorsed Vendors, Exclusive Discounts: Explore the Latest Deals and Save Big with NYSDA’s Trusted Endorsed Vendors.
Real Feedback. Trusted Vendors. Smart Choices.
When it comes to making financial decisions for your dental practice, a trusted recommendation can make all the difference. In this month’s NYSDJ, we’re spotlighting the voices that matter most—yours. Our members have shared their experiences working with the vendors we’ve recommended, offering honest insights into the value, service, and results they received. These testimonials highlight the power of peer-to-peer connections and reinforce our commitment to providing resources that truly deliver.
Read on to learn what your fellow members have to say—and discover why these vendor partnerships are paying off.
I couldn’t be happier with my experience in working with Bank of America for my startup business loan. They were my North Star during the storm that is the build-out period, and helped me find my way to creating the practice of my dreams. Highly recommend!
Jacqueline Dikansky, Manhattan

I worked with Bank of America to get a loan for my dental startup. I was happy to choose Bank of America as they are always involved in events held by NYSDA and my local chapter, the Second District Dental Society. I felt well cared for along the way, and all my questions were answered. I am so happy to be a member of the ADA, NYSDA, and Second District Dental Society—it helps make me feel confident in my decision to go with Bank of America when making such an important decision for my future and business.
Stephanie Sager, Brooklyn

Being a Prosites customer for over twelve years, I am convinced there is no better website services provider for dental practices of all types out there. Site design options are abundant, content is great, customization is easy and their services are so affordable. But the clincher is customer service—the best!
Larry Volland, Buffalo




I have been an active participant with Best Card since its initial recommendation as an ADA/NYSDA-sponsored credit card processor. Their customer service made our transition to their service flawless. Their rates have saved me thousands of dollars in credit card processing fees and their attention to PCI compliance makes the entire relationship one I rely on to handle all my needs in one stop. The reliance of many patients making credit card payments make this a great company to partner with and our experience with them has been great.
Paul Leary, Smithtown
Endorsed Vendor Updates

For 50 years and counting, MLMIC has proudly stood as a dedicated partner to New York’s dental community, providing exceptional dental professional liability protection, invaluable resources, and service like no other. We understand the unique challenges and evolving landscape dentists face, which is why we’ve cultivated a comprehensive suite of support tools. Our commitment extends beyond coverage, offering specialized guidance through MLMIC Dental Liability Insights, practical Risk Management Tips, innovative Publications, and an array of Dental Malpractice FAQs, all readily available on our website. Looking for more insights? Our YouTube channel offers a non-CME webinar on “Managing Patient Expectations”—a crucial topic for any practice. Check it out today! We are here to empower dentists with the knowledge and security needed to focus on what they do best: delivering outstanding patient care. Visit us online at: www.mlmic.com/dentists/resources.





























To Thine Own Self be True
THE NYSDA DIVERSITY and Inclusion Task Force, charged with acknowledging and promoting the disparate components of the Association’s membership, joins in the national observance of June as Pride Month.
Designated in 1999, Pride Month commemorates the contributions to life and culture made by lesbian, gay, bisexual, transgender and queer people. Among those celebrating and being celebrated this month is NYSDA member Allison Rascon, D.D.S., M.S.
Dr. Rascon, a board-certified periodontist and implant specialist at MicroPerio in New York City, is a native of Miami, FL. She holds a Bachelor of Science Degree in Biomedical and Health Sciences from the University of Central Florida and DDS Degree from NYU. Dr. Rascon received her certificate in periodontics and Master of Science Degree in Oral Biology from the University of Pennsylvania.
The Task Force asked Dr. Rascon to share her thoughts about her chosen profession and the special role she plays within it as a member of the LGBTQ+ community.
Q. Please share a brief overview of your journey to becoming a periodontist and what inspired you to pursue this path? Were there any pivotal moments that shaped your decision?
Dr. R. I always knew I wanted to work in health care. It was a natural calling for me, driven by a desire to help others and a fascination with how the body works. That eventually led to a curiosity as to why the mouth always seemed to be considered “separate” from the body, always a division between medicine and dentistry—or so I thought. As I progressed through dental school, I explored various specialties,
but it wasn’t until my rotation in the periodontics department that everything truly clicked. I was genuinely taken aback by the range and complexity of surgical procedures that periodontists perform, from regenerative therapies and hard/softtissue augmentations to implant placements and surgical interventions for advanced periodontal disease. It was eyeopening to see how surgical skill, medical knowledge and patient care came together in this field.
That experience was a turning point. I realized periodontics wasn’t about treating periodontal disease; it was a specialty that offered the opportunity to make a real, lasting impact on patients’ health and quality of life. Since then, I’ve been dedicated to pursuing this path, continuously inspired by the blend of precision, challenge and meaningful care that defines this specialty.
Q. What does Pride Month mean to you—not only as a dental professional, but as a person?
Dr. R. Pride Month holds deep personal significance for me, not only as a dental professional, but as a member of the LGBTQ+ community. It’s a time to celebrate how far we’ve come, to honor those who have fought for our rights and to reflect on the work that still lies ahead. It reminds me that visibility and representation matter, especially in health care, where trust and comfort are essential to delivering quality care.
I’m acutely aware of the barriers that LGBTQ+ individuals can face when seeking dental and medical care—whether it’s fear of discrimination, financial obstacles, or simply not feeling they are being seen or understood by their providers.
Dr. Allison Rascon believes authenticity in her personal identity is key to her professional success.
Periodontist Allison Rascon describes herself as being passionate about her research in periodontal and peri-implant regeneration.
That’s why I’ve always made it a priority to volunteer with organizations and clinics that serve our community. Giving back through service is one way I try to bridge that gap and make care more accessible to those who need it most. As a periodontist, I believe that creating an inclusive and affirming space is just as important as clinical expertise. Pride Month reinforces my commitment to ensuring that every patient, regardless of identity, feels safe, respected and supported when they walk through the door.
Q. How has your experience as a member of the LGBTQ+ community shaped your path in dentistry—from dental school to residency to where you are now?
Dr. R. My experience as a member of the LGBTQ+ community has had a profound impact on my journey in dentistry. From the very beginning in dental school, I was aware that I carried an identity that isn’t always openly represented in professional spaces. At times, that meant navigating subtle biases or feeling the pressure to “blend in” rather than bring my full self to the table. But it also gave me a deeper empathy for others who feel like they don’t quite fit the mold. That perspective shaped how I approached patient care, how I built relationships with mentors and peers, and, ultimately, how I defined success for myself.
During residency, I became even more com mitted to showing up authentically, not just for myself, but for others who might be looking for representation in our field. It’s one thing to learn clinical skills but learning how to lead with empathy and advocate for equity is just as essential. Where I am now, I feel a strong sense of responsibility and pride. Being out and visible in this profession matters. It sends a message to both patients and colleagues that the dental field is evolving, that there’s space for everyone and that our differences are a strength, not a limitation. My identity has not only shaped my path; it’s become one of the most meaningful parts of the work I do.
Within professional organizations, LGBTQ+ representation fosters a more inclusive culture, where diverse voices help shape policies, education and patient care standards. It signals to both students and colleagues that this profession values authenticity and equity, not just clinical excellence. While organizations like the ADA have made commendable strides in promoting inclusivity and visibility, there is still significant room for growth in others. For instance, the American Academy of Periodontology (AAP) currently lacks dedicated programs or discussions focused on the LGBTQ+ community, which can sometimes contribute to feelings of isolation among members. I hope to contribute to helping the AAP expand its efforts and include more LGBTQ+ friendly initiatives in the future.

Personally, I’ve seen firsthand how meaningful visibility can be. Patients have shared how relieved they felt knowing they were in the hands of someone who understands them without judgment. And within the professional sphere, I’ve had younger students and residents approach me just to say,
“Thank you for being out, it makes a difference.” Those moments reinforce why showing up authentically matters. When we expand who is visible, we expand what’s possible, for our patients, our peers and the future of dentistry itself.
Q. What words of advice or encouragement would you give to LGBTQ+ dental students or early-career professionals who are finding their voice in the profession?
Dr. R. To LGBTQ+ dental students and early-career professionals, know that there is strength in being your true self, even when it feels uncertain. Finding your voice in this profession doesn’t happen overnight, and that’s okay; it’s a process, not a race. There may be moments when you feel like you are the only one in the room, but you’re not alone. Your presence, perspective and resilience matter more than you realize.
Q. Why do you think LGBTQ+ visibility matters in dentistry, both for patients and within professional organizations? Have you seen the impact of that representation firsthand?
Dr. R. LGBTQ+ visibility in dentistry is vital, not just as a matter of representation, but as a catalyst for trust, equity and better health outcomes. For patients, seeing themselves reflected in their providers can mean the difference between avoiding care out of fear and finally feeling safe enough to seek it. When people feel judged or misunderstood, they’re less likely to access regular dental care, which can lead to preventable health issues. Visibility helps break that cycle.
One thing I’ve always believed and often say is that closets are for clothes! Our profession needs more people who are willing to show up as their whole selves, not just for visibility, but to help shape a more inclusive future in dentistry. When you lead with authenticity, you give others permission to do the same. Build your network, find mentors you can trust, and don’t be afraid to advocate for yourself and your community. Your identity is not a limitation, it’s an asset. It brings empathy, strength and a deeper understanding to everything you do. And trust me, the more you lean into who you are, the more rewarding this journey becomes. p

Turning the Page on the Past
Maurice Edwards sees his presidency as an opportunity to look forward and begin again.
The New York State Dental Association welcomes Maurice L. Edwards, D.M.D., its 144th President.
BY THE TIME he stood to address the NYSDA House as its newly installed president, Dr. Maurice Edwards had already decided what he wanted his legacy to be. Having come into office as the Association was being roiled by differences of opinion that threatened the fabric of the organization, Dr. Edwards offered himself up as a healer.
Calling the moment “a turning point,” Dr. Edwards urged his colleagues “…not to look back in frustration, but to look forward with intention. Not to dwell on what went wrong, but to focus on what we can make right.” To that end, he promised to steer the Association toward healing, rebuilding, recommitting, leading and, importantly, toward remembering “we are not each other’s opponents; we are teammates.”
Maurice Luther Edwards, D.M.D., NYSDA’s 144th President, and the first person of color to hold the top elected post, admits to being an optimistic person, which should
serve him well as he fulfills his self-described mission to remake the Association “stronger, smarter and more united than ever.”
An oral and maxillofacial surgeon, Dr. Edwards lives in the Nassau County community of Lynbrook. He grew up in the nearby village of Freeport. His practice, Maurice L. Edwards, D.M.D., P.C., is located in the heart of Manhattan, on East 60th Street. He did his undergraduate work at the University of Rochester, received his D.D.S. Degree from the University of Pennsylvania School of Dental Medicine and completed a residency in oral and maxillofacial surgery at Bellevue Hospital Center/NYU Medical Center.
In addition to his private practice, Dr. Edwards is an associate clinical professor at New York University College of Dentistry, Department of Oral and Maxillofacial Surgery; an attending physician at Mount Sinai Hospital, Depart-
Edwards family enjoys stroll down 60th Street in Manhattan. From left: daughter Brianna; grandson Kyrie; Dr. Maurice Edwards; grandson Kaleed; daughter Keanna; wife, Michelle; son, Christian.
Photos by Carlo Messina, F/X Video

ment of Otolaryngology/Division of Oral and Maxillofacial Surgery; and at Mount Sinai West/St. Luke’s Department of Otolaryngology/Division of Oral and Maxillofacial Surgery. Two years ago, following a rigorous review process, he was appointed a police surgeon by the New York Police Department, placing him on call for emergency and nonemergency consultations for procedures for NYPD officers hurt in the line of duty and for their families. He performs similar duties as a state trooper surgeon for the New York State Police Troopers.
It Started with a Broken Tooth
Dr. Edwards likes to recount the story of how he got started in dentistry. It was when he was playing football in high school, he relates. He broke his front tooth right before a scheduled vacation.
“I was embarrassed,” he recalls, and “didn’t want to go. My mother took me to our family dentist, who in less than an hour fixed my broken tooth and as far as I was concerned, saved both me and my family vacation. The pride he had in his work and the feeling of completeness he gave back to me by restoring my smile were probably the biggest draws into dentistry for me.”
It was that one positive experience, he says, that put the medical profession on his radar. It may have triggered something else in the young man that remains with him to-
day and that is a desire to better himself by helping others. It’s why there are few hours in his day that aren’t devoted to the work of organized dentistry, in service to its members; or ministering to the needs of the community, especially those who are less served; or pitching in in emergency situations—the oral and maxillofacial surgeon is also a volunteer firefighter with the Lynbrook Fire Department.
The Particulars
Dr. Edwards’s ascendency to the presidency of NYSDA is the culmination of many years of contributions made to organized dentistry. Highlights of his service include past president of the New York County Dental Society, former chair of the NYSDA Council on Communications and Membership, NYSDA Trustee and ADA Delegate, Washington Leadership Conference—New York State Action Team Leader, and Greater New York Dental Meeting Organizing Committee member.
He is a graduate of the ADA Institute for Diversity and Leadership, has participated in New York County Give Kids A Smile programs numerous times, NYCDS’s annual Charity Golf Outing, and has volunteered for community oral and cancer screening programs. His altruism is further reflected in his membership in Alpha Phi Alpha Inc., which has led him to participate in efforts to feed and clothe residents of homeless shelters in Brooklyn.
Sunday in the park, Central Park. From left, Keanna, Brianna, Dr. Edwards, Michelle, Christian. Grandsons Kaleed and Kyrie in front.
Photos by Carlo Messina, F/X Video

A Conversation with NYSDA President Maurice Edwards
Who are the members of your immediate family?
My wife, Michelle; children Keanna, Brianna and Christian; grandkids Kyrie and Kaleed; mother, Diann; father, Edward; brother, Mark, and his wife, Wendy; mother-in-law, Lola; and sister-in-law, Desiree.
What are your goals for the coming year?
To bring harmony to a turbulent Board by letting go of the past and moving forward to complete the business of the Association. I also want to help our governmental affairs team work on changing the scope-of-practice definition for dentistry. That as well as finding concrete solutions for the workforce shortage that is plaguing our state.
What are the greatest challenges facing dentistry and how should we respond?
One of the greatest challenges facing dentistry is the amount of educational debt that new dentists carry as they attempt to start their careers. This burden is forcing many graduates to forego specialty training out of fear of accruing more debt during their time in training.
The second biggest challenge is the constant downward trend of membership in organized dentistry. If we are unable to convince younger dentists of the positive impact the tripartite has on advocacy and the practice of dentistry, all three levels of the association will become powerless to effect change and then politicians and other specialty lobbying groups will be the ones who define how dentists practice their profession.
On top of declining membership, there are questions about the financial health of the ADA. We aren’t approaching a critical time at the ADA; that time is now. And leadership needs to find a solution that makes membership worth every dollar spent on dues. If not, within a very short time, we will find our market share to be less than 50% and our ability to influence legislators will be lost.

You are involved in a lot of organized groups, but being a member, especially a contributing member of a specialty organization, does not seem to be so important today. How do you propose making organized dentistry more relevant and attractive to young dentists in particular? I agree that organizations are having a difficult time getting and retaining members. This is a result of both financial constraints and, possibly, the loss of perceived value. I think organized dentistry needs to rethink what members want from their association.
The ADA is trying to use artificial intelligence to gather information on what individual member’s interests are and then tailor benefits to that member. The hope is that if a member is more interested in, say, continuing education or dental technology or buying or selling a practice, his or her benefits would be tailored to offering discounts towards CE credit or on services from groups that help purchase or sell practices, or directed towards a group of retailers who offer dentists great deals on their purchase of dental technology.
The idea is to tailor the information coming from organized dentistry toward each individual dentist. It will require an enormous amount of thinking power on the part of the association to give each member what it is they need at the time they need it, at the price they want and as quickly as they want.
Is there a chance organized dentistry will cease to exist if it doesn’t change? Has it become too expensive?
I believe organized dentistry will always exist because most professionals enjoy having contact with their colleagues, to
compare notes and learn of possible solutions to common problems and experiences. I’m not sure if membership has become too expensive or if newer dentists are drowning under educational debt and tend to be more careful about what they spend their money on. So, organized dentistry needs to prove its value to new dentists to make membership more desirable.
The problem dentistry is having is not specific to our profession. It’s seen across all member-based organizations. The fact that it’s easy for individuals to find the things that organizations offer online and at less cost has left a lot of membership-based organizations struggling to identify what it is they can do and offer their members that members can’t easily find on their own.
In dentistry in particular, the practice model has slowly changed so that new dentists are more interested in join-

Dr. Edwards is assisted in his office by brother, Mark, and wife, Michelle.
Dr. Edwards stands with NYSDA delegation in State Capitol in Albany prepared to lobby for legislation favorable to dentistry.


ing DSOs, which provide them with continuing education, malpractice insurance and opportunities to meet up with colleagues to exchange ideas. Organized dentistry at the national, state and local level is dealing with these declining trends, trying to find ways to make itself a more valuable proposition for these new dentists.
The strongest thing organized dentistry provides is its advocacy; however, as we lose more and more of the market share of practicing dentists, as older dentists retire and aren’t replaced by newer dentists, organized dentistry will find it more difficult to secure a seat at the table with legislators.
Are you an optimistic person? Do you have a guiding philosophy that keeps you going?
I definitely believe I’m an optimistic person. I have several philosophies that I live by. One is “You can sleep when you’re dead.” Another is “If you are not at the dinner table, you were on the menu.” And lastly, “I am my brother’s keeper.” These are the principles that allow me to get up every day and function as a productive member of whatever organization or group or event that I plan to give my time to.
I truly believe we were all put on this earth to do the best we can to make this world a better place. It is my goal to do everything I can to provide for my family while doing as much good for this planet as I can. I joined the fire department believing that if I can use my spare time to save just one life, I’ll feel I’ve done a little more good while on this earth. And I understood during my residency at NYU and Bellevue Hospital that I had the opportunity to save several lives and restore faces to provide those patients with a better quality of life. I sit with my fraternity brothers and plan charitable events and other community programs to give back to those who are less fortunate than I am. I joined the Knights of Columbus after the passing of my father-in-law as a tribute to him and as a way to continue the good work he did while he was alive. He was a veteran and someone I looked up to. I became involved with many of the other organizations I belong to for the same reasons more or less— because I believe we can touch more people as a collective than as individuals.
Lastly, my parents didn’t raise me to be lazy or useless. While I have the energy and the ability, I will strive to do things that make the world just a little bit better, so that when it’s my time to finally sleep, I can rest peacefully.
Any thoughts on being the first person of color to hold the top elected post of NYSDA?
I would be lying if I did not say that I feel the immense weight and honor that goes with being the first person of color to
An oral and maxillofacial surgeon, Dr. Edwards sees patients at his practice on East 60th Street in Manhattan.
Firefighting is family affair. Dr. Edwards with wife, Michelle; son, Christian; daughter Brianna.
serve as president of the New York State Dental Association. It causes a little self-induced pressure only because I understand that those from my ethnic group or other ethnic groups will be watching me either hoping I have a successful year or to see if I perform as well as my predecessors did. It is my goal with every task I undertake to leave the situation better than I found it. It’s no different with NYSDA. I sincerely hope that when I’m done, people will look back on all the work I did with the volunteers and Board of Trustees and say, he did a really good job. Then I’ll be happy.
My goals are simple: to instill trust and enable the Board to work productively with me, with each other and with staff. We will continue to push our legislative priorities. Chief among these is our scope-of-practice bill, medical loss ratio and I hope something that addresses the workforce shortage.
I want my legacy to be when people look back at my presidency they simply say, he did his best and he was a good guy. We have already had our first Board meeting, and every member cooperated to give us a great start to this administration. With everyone working hard to move forward, everything else will be icing on the cake.
Tell us about your career as a volunteer firefighter. Do you actually fight fires?
My career is in its infancy. I only recently graduated from one level of firefighter academy, where I learned the essentials. I’ll return to learn primaries, which will allow me to be an interior firefighter. Until I finish that course, most of my firefighting will be limited to the external portions of buildings and vehicle fires. For the most part, I am with the medical company of the Lynbrook Fire Department, where we are on call once a week but may be asked to be available daily by page to respond to medical emergencies, car accidents or fires. Eventually I expect to be asked to respond to interior structural fires, vehicle fires and wildfires if necessary.
Some people have asked why an oral and maxillofacial surgeon would join the volunteer firefighting company? My answer is simple. I have the energy, the desire to help and I do not like to be bored. Plus, my daughter and my son joined the department, and my wife is a member of the auxiliary firefighter company, so it’s a family affair.
What drives you to do all the different things you do?
My family. I’ve always been an ambitious person, and I try to impart that to my kids. I firmly believe you show your true self through your actions. Every time I had an interest or desire or wish I wanted to come true, I focused on making it


happen without fear of failure. I am fortunate both my parents are alive to share in my success. I was the second one in our family to complete college, following in my brother’s footsteps. Both he and I made it our mission to make sure all our children finish college, which they did, and several of them went even further to get their master’s degrees.
Michelle and I are doing everything we can to have a successful business with the hope that one of our children will eventually enter dentistry and take over the practice. Michelle runs the office, she answers the phones, schedules patients, orders supplies, collects payments, communicates with referring doctors, sends prescriptions and verifies insurances, among her many responsibilities. I think it’s safe to say that everything that we do is with the hope that we provide our kids with a better life than we had. And that they will do the same for their children and their children’s children and so on.
Overall, Michelle and I consider ourselves extremely fortunate to have lived the lives we have. We couldn’t be prouder of our children and the rest of our family and hope we’ve passed on a little bit of our luck to all of them. If just a small part of what we wish for them becomes reality, then we can say we lived a life worth living. p
Maurice and Michelle Edwards tour island of Aruba on motorcycle.
Dr. Edwards with Alpha Phi Alpha Fraternity brothers, from left, Bryce Tarrant, Terrance Martin, Romane Paul.

ProSites Reviews

Save
Time and
Acquire New Patients with Seamless Review Management
ProSites Reviews is a review management platform to help dental practices manage patient reviews across all review sites easily and instantly. ProSites Reviews connects to your practice management system to save time and acquire new patients to increase revenue and reach practice goals. Unlike other solutions, our platform’s user-friendly interface and our superior customer support make review management a seamless process.
Key Benefits for Practice Owners: 88% of people trust online reviews as much as a personal recommendation. This shows exactly how important it is for your practice to have a strong online reputation. ProSites Reviews makes it easy to get and keep a positive online reputation and helps you acquire new patients, increase revenue, and reach your practice goals.
Having a positive online reputation is also critical when hiring, as 86% of employees and job seekers research company reviews and ratings before deciding to apply for a job. Utilizing ProSites Reviews doesn’t just help you attract new patients, it also helps you attract top talent!
Key Benefits for Practice Staff: Online review management is time-consuming. Keeping track of reviews across different review sites, responding to both positive and negative reviews, and asking happy patients to leave positive reviews takes a lot of effort and time. ProSites makes this entire process simple, reducing both your workload and stress.

Reviews Dashboard: Our easy-to-use reviews dashboard collects all your reviews from the different review sites your patients visit, making it easy to see feedback from your patients. This dashboard also includes analytics to help you understand exactly how your practice is doing.











Make Review Management Easy and Reach Your Practice Goals!

Review Invites: ProSites Reviews connects to your practice management system and includes all your contacts. Using these contacts, you can easily send personalized texts to happy patients asking them to leave a 5-star review.
Automated Review Notification: ProSites Reviews sends email alerts any time a patient leaves a review, so you will never miss a review again, and can respond in a timely manner.
Response Tool: You can respond to both positive and negative reviews from any review site directly from the ProSites Reviews Dashboard. No more logging into multiple review sites and remembering multiple passwords, making responding to online patient reviews seamless.

Practicing Dentistry in the Age of Periodontal Risk Management
Roger N. Warren, D.D.S.; Liana Umbrio, D.D.S.; Leena Palomo, D.D.S., M.S.D.
ABSTRACT
Purpose of review. To provide clinicians with knowledge of periodontal risk assessment that can be applied chairside effortlessly.
Recent findings. Detecting periodontal risk factors early may reduce the morbidity of oral and systemic diseases, as oral and systemic health can have a bidirectional relationship.
Summary. Dental professionals are equipped with evidence-based risk factors to predict and prevent the progression of periodontal disease. Implementing chairside risk assessment allows for prevention and early intervention, potentially reducing healthcare costs and promoting simpler solutions in an unpredictable economy.
The cultural, economic and historic backdrop of current times leaves the dentist to navigate and balance prevention with diagnosis and treatment. This mandates that the dentist behave as an actuary, responsible for predicting disease and intervening strategically as patients demand better, faster, cheaper care. The stakes have never been higher. Be it periodontitis, tooth loss or peri-implantitis, we live in the age of periodontal risk management. Luckily, there are simple tools to approach the challenge.
Periodontal risk assessment is defined by the American Academy of Periodontology as the process by which quali-
tative or quantitative assessments are made of the likelihood for adverse events to occur as a result of exposure to specified health hazards or by the absence of beneficial influences.[3]
Almost every disease that has been identified has certain “risk factors” that contribute to or modify the course of a disease process. Newman and Carranza’s text states that risk factors are “environmental, behavioral, or biologic factors that, when present, increase the likelihood that an individual will develop the disease. Risk factors are identified through longitudinal studies of patients with the disease of interest.”[4]
Thus, risk factors do not cause the disease, since causality is any factor without which the disease would not have occurred. Rather, risk factors are conditions that the disease experience would not have been the same without.
After Loe[5] demonstrated that the etiology of gingival inflammation was essentially bacteriologic, most of the other observations, both systemically and locally, regarding periodontal disease have been influencers or modifiers of periodontal disease or risk factors. Some are systemic; many are local factors. Some are modifiable; and many are not.
We will attempt to list the many risk factors observed to be related to periodontal disease and briefly comment on what the literature has found to be their effect on periodontal disease. The primary goal of this article is to present a review of evidence to provide clinicians with assessment and management options that translate from the research realm to chairside application seamlessly. The secondary goal is to create teamwork between the medical and dental community to provide clinicians with a pathway to improve overall quality of life.
Modifiable Factors
Differentiating modifiable from non-modifiable factors empowers the clinician to strategically affect patients’ periodontal health. Ideal care and attention to detail can enable the patient to experience optimal dental health and fulfill the challenge of dentistry expressed by Prichard that nature intended the teeth to last a lifetime. With proper home and professional care from early childhood, there are few people who cannot realize this expectation.[2]
Smoking Tobacco
Although tobacco smoking has been declining in the United States, a considerable number of smokers, about 30 million Americans, still exist. Tobacco smokers have more periodontal disease than nonsmokers, and they have a more rapid progression of periodontal disease. Smokers have a diminished response to periodontal therapy. Many surgical procedures are affected, as tobacco smoking alters the healing process. Implant failures are twice those of nonsmokers.[6] Smoking impairs vascular factors and inflammatory mediator production, antibody production, fibroblast activity and neutrophil function. However, the good news is that those who have quit smoking have a response similar to nonsmokers to both periodontal and implant procedures.[7]
Recommendation: Smoking cessation has a positive effect on the occurrence and healing of periodontal disease.[8] The U.S. Department of Health and Human Services provides strategies for smoking cessation.[9] Two European workshops on the prevention and cessation of tobacco use reported the importance of tobacco smoking cessation by dental professionals.[10,11]
Cannabis
Now that recreational marijuana smoking is becoming more commonplace, accepted and legal, the prevalence of periodontal disease has increased, and altered healing is a factor in treatment planning. Besides greater attachment loss among frequent cannabis users, there are more complications following intraoral surgeries.[12] Cannabis has a profound influence on the oral microbiome and may compromise the immune response to plaque, resulting in greater attachment loss from periodontal disease.[13]
Recommendation: Smoking cessation, as regular, long-term use of cannabis is a risk factor manifesting as clinical attachment loss, deep pockets, gingival recession and enlargement.[14]
E-cigarettes
A combination of a carrier (propylene glycol or glycerin),
nicotine and flavorings can increase the risks for cardiovascular and lung health and may affect the oral microbiome, making e-cigarettes a poor alternative to tobacco smoking. [12] There is an increase in Fusobacterium and Bacteroides subgingivally in people using e-cigarettes[15] and a higher amount of inflammation.[16]
Recommendation: Smoking cessation, as it is suggested that e-cigarettes increase destruction of the periodontium by the development of periodontitis.[17]
Systemic Factors
Diabetes
Epidemiologic data demonstrates that the prevalence and severity of periodontal disease is more significant in patients with Type 1 and Type 2 diabetes than those without diabetes, and that the level of diabetic control is a crucial variable in this link. There are more than 30 million diabetics in the United States, and many have yet to be diagnosed. It is estimated that one in four adults over the age of 65 is affected by diabetes. The dentist should keep apprised of the HbA1c level of their patient and communicate with the physician regarding the patient’s glycemic control. It may be necessary to modify therapy, depending on the patient’s assumed ability to heal satisfactorily. The dental profession must prevent and treat periodontal disease not only to preserve the dentition, but also to reduce the effect of periodontitis on diabetes and its complications.[18]
Recommendation: Diabetes-control interventions, such as dietary changes, exercise and oral health education.[19,20]
Cardiovascular Disease (CVD)
Periodontal disease contributes to the total infectious and inflammation burden and may contribute to cardiovascular events, such as stroke, in high-risk patients. The lipopolysaccharide and monocyte-related responses suggest a link between these two diseases.[21] There are risks and complications in patients undergoing periodontal therapy who are on anti-thrombotic therapy.[22]
Recommendation: Patient education on increased risk of CVD complications, and on how to control CVD risk factors.[23] Dental professionals should monitor patient blood pressure at appointments, use local hemostatic measures and consult the patient’s physician prior to invasive procedures.[22]
Obesity
Obesity increases the risk for periodontal disease, and there is an increase in periodontal disease prevalence in obese and overweight individuals. Over 35% of Americans suffer from obesity. There is an altered immune response, microbial dysbiosis, genetic polymorphisms and increased stress
in these individuals. Adipose tissue can be considered an inflammatory organ. The oral microbiome is altered in obese individuals—for example, Tannerella forsythia are present in greater proportions. Periodontal treatment can improve this situation.[24]
Recommendation: Dietary changes[19] and physical activity as potential tools for reducing the occurrence of periodontal disease.[20]
Stress
Stress makes it more difficult for the body to fight against infections, including periodontal disease. Stress markers have been found in the blood of people experiencing psychological stress. The composition of the biofilm is changed. Also, changes in lifestyle, such as ignoring oral hygiene, smoking, consuming more fat and sugars, plus an increase in IL-6, all play a role in increased susceptibility to periodontal disease. The hope is to develop a saliva test to identify people experiencing stress and then devise appropriate treatment.[25]
Recommendation: Stress decreases saliva flow and increases plaque formation. Also, cortisol is increased in the gingival crevicular fluid so that stressed individuals need a careful watch for periodontal disease.[26] Poor healing is also associated with stress,[27] suggesting close monitoring as well.[28]
Osteoporosis
Osteoporosis is usually asymptomatic until a fracture occurs. It is present in both men and women; however, onethird of women aged 60 to 70 have osteoporosis, defined as 2.5 standard deviations below the norm. Both osteoporosis and periodontal disease are bone-resorptive diseases; and they appear to be correlated. Osteoporotic individuals have increased severity of periodontal disease and experience greater tooth loss. Altered trabeculation on dental radiographs can be an indicator of skeletal bone mineral density. Therefore, some reports of reduced bone mass make one more susceptible to periodontal disease.[29]
Recommendation: Hormone replacement therapy with estrogen as treatment for postmenopausal osteoporosis suggests some evidence of reduction in bleeding on probing (BOP) and pocket depth, but has a minimal effect on radiographic bone loss and tooth loss.[30]
Pregnancy
Hormonal changes during pregnancy can result in gingival hyperplasia and an exaggerated response to plaque bacteria. Both the innate and adaptive immunity are affected, resulting in possible magnified degree of periodontal dis-
ease. Pregnant women have increased BOP, deeper pocket depths and greater inflammation. It is hypothesized that hormonal changes lead to a reduced resistance to bacterial inflammation and the ability to repair.[31] Low birth weight babies and premature births were also cited due to a direct pathway through dental bacteremia.[32]
Recommendation: Treatment of gingivitis and periodontitis during pregnancy is associated with decreased risk of adverse pregnancy outcomes.[33]
Hormonal Influence
Circulating corticosteroids, androgens, estrogens and progesterone cause increased bone resorption, stimulate fibroblast synthesis, immune suppression and increased fluid exudation. Also, oral contraceptives and the second trimester of pregnancy cause an increase in Porphyromonas [Bacteroides] intermedius. The result is increased probing depths, which leads to a change in attachment levels and bone loss.[34]
Recommendation: Strict oral hygiene measures for patients using oral contraceptives to prevent or decrease severity of periodontitis.[35]
Respiratory Diseases
According to several researchers, periodontal disease can have an influence on chronic obstructive pulmonary disease (COPD), asthma, pneumonia, obstructive sleep apnea and COVID-19. This may be due to the aspiration of oral pathogens and/or the systemic effect of pro-inflammatory mediators produced in the periodontal tissues. The effect may be bidirectional. Porphyromonas gingivalis and Treponema denticola appear to be the main etiologic agents. Asthma and pneumonia present the weakest connection to periodontal disease.[36]
Recommendation: For COPD, smoking cessation is critical because smoking is a risk factor for periodontitis and COPD. Reinforcing oral hygiene is imperative because insufficient oral hygiene has been shown to be associated with exacerbations of COPD.[23]
Kidney Disease
Periodontitis has been established as an independent risk factor for chronic kidney disease (CKD).[37] The hypothesis that an increased inflammatory response in kidney disease destroys endothelial vasculature may be related to periodontal inflammation and the development and progression of kidney disease is suggested. Screening for periodontal disease may help prevent the progression of kidney disease.[38]
Recommendation: There is a bidirectional relationship between CKD and periodontal disease; therefore,
managing periodontal disease is important in treating CKD.[39] Periodontal treatment can have a positive effect on the estimated glomerular filtration rate, a measure of kidney disease.[40]
Alzheimer’s Disease
Alzheimer’s disease is considered a neuroinflammatory disease and because periodontitis results in increased proinflammatory mediators, it may exacerbate this condition.[41]
Recommendation: Multidisciplinary treatment plan with physician, caregiver, family and patient. Establish oral hygiene routine and manage dietary habits. Encourage autonomy of patient for as long as possible.[42]
Age
Older people have higher rates of periodontal disease. Severity and prevalence increase with age. About two-thirds of patients over the age of 65 have periodontal disease, whereas, overall, there is about a 47% prevalence of periodontal disease. Advanced age may modify periodontal disease by increased exposure to plaque, a different composition of plaque, greater susceptibility to periodontal disease and/or slower wound healing.[43]
Recommendation: Early and individualized treatment of most pathologic conditions usually leads to a more favorable outcome.[44]
Socioeconomic Status
Decreased dental awareness or lack of regular care can increase the risk of periodontal disease, but low socioeconomic status alone will not cause periodontal disease. The prevalence of periodontal disease is lower with a healthy lifestyle compared to an unhealthy lifestyle.[45] Income inequity relates to oral health in that lower individual/household income is associated with increased occurrences of dental caries, periodontal disease, traumatic dental injuries and oral cancer.[46]
Recommendation: Implement outreach programs in areas of socioeconomic at-risk populations to increase access to care.[47,48]
Sex
Men have a greater risk for destructive periodontal disease, but studies have yet to show that they are at higher risk for more rapid periodontal destruction than women. Poorer oral hygiene and irregular care, in addition to a genetic difference, may account for this disparity. Sex steroids influence inflammatory cytokines, especially IL-1β and TNF-α, to magnify injury and infection in men.[49]
Recommendation: Since men are more likely to ignore their oral health, it is critical to develop education and treatment strategies to improve their oral health.[50]
Education
There seems to be a correlation between less education and income with periodontal disease prevalence and severity. [51]
Recommendation: Implement oral health education programs and endorse educational attainment.[47]
Genetics
Some people have a genetic predisposition to periodontal disease despite regular care and good oral hygiene. If detected early, aggressive intervention is indicated. IL-1α is a cytokine associated with a susceptibility to periodontal disease. Control of the inflammatory process and the proresolution process result in a degree of periodontal destruction. Currently, 65 genes have been associated with periodontal disease, so the problem is quite complex.[52]
Recommendation: Epigenetics is a reversible change to how the body reads a DNA sequence.[52] Epigenetics, altering gene expression resulting in a modification of the structure of DNA rather than changes in the genetic code as in mutations, is a possible route towards a perio-systemic health link.[28] DNA methylation or histone modifications can selectively activate or deactivate genes, resulting in the outcome of many inflammatory diseases, including periodontitis.[53]
Medications
Several medications, such as calcium channel blockers, phenytoin and cyclosporine, can cause gingival hyperplasia and promote periodontal disease. Unregulated fibroblasts produce increased amounts of collagen and/or extracellular connective tissue matrix. Anti-inflammatory drugs such as corticosteroids and NSAIDs affect the balance between pro-inflammatory cytokines and the anti-inflammatory cytokines (IL-4, IL-10) but have no effect on the severity of periodontal disease. Immunosuppressive medications for rheumatoid arthritis result in increased inflammation and periodontal disease. Oral contraceptives can exaggerate the body’s response to plaque bacteria. Bisphosphonates are anti-resorptive osteoclastic inhibitors that when taken intravenously can cause osteonecrosis of the jaw. Minimizing infection and improving plaque control prior to taking bisphosphonates is beneficial. Anti-platelet drugs are beneficial in minimizing inflammation in animal studies. Statins lower cholesterol and are anti-inflammatory. Anticancer treatments result in transient neutropenia, which can exacerbate periodontal disease.[54]
Recommendation: Discontinue or change the offending medication if appropriate and after consulting with the patient’s physician, in conjunction with surgical and nonsurgical treatments.[55]
Conclusion
Available evidence provides the clinician with a number of potential risk factors for the progression of infection and inflammatory diseases, such as periodontal and periimplant diseases. Risk assessment empowers dentists and hygienists to identify potential problems early on and pro-
vide focused, proactive interventions for cases that are susceptible to disease or disease progression[56] (Figure 1). Preliminary data show that this approach can reduce shortand long-term health-care costs. As the economy continues on its unpredictable path, we are optimistic that such strategic, early interventions will reduce the need for more costly, and often more traumatic, complex treatments and promote simpler, more highly predictable and, likely, more durable solutions to dental disease. p
Queries about this article can be directed to Dr. Warren at rw845@nyu.edu.
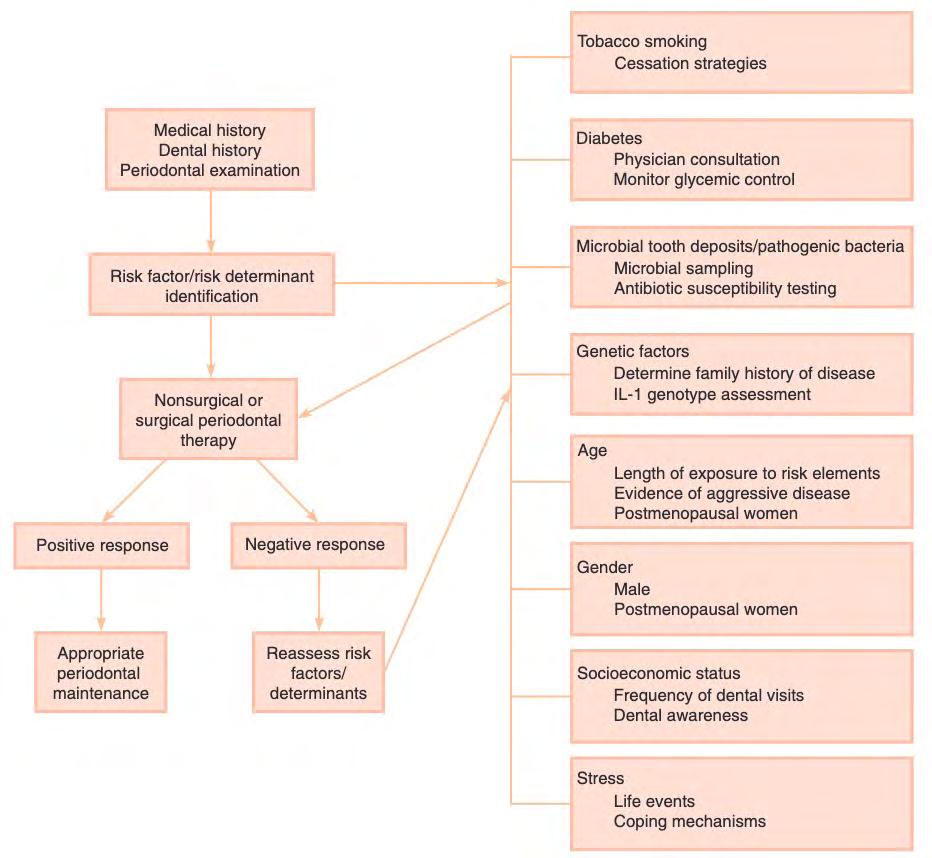
Figure 1. Assessing risk factors for periodontal treatment. Risk assessment is critical in both diagnosis and treatment of periodontal disease. Figure demonstrates initial assessment of risk factors before starting therapy and reassessment of risk factors following negative response to treatment. (Retrieved from Newman and Carranza’s Clinical Periodontology 13th Ed (p. 412e) by Newman MG, Takei HH, Klokkevold PR, Carranza FA, 2019, Saunders.)[4]



REFERENCES
1. Lim G, Janu U, Chiou LL, Gandhi KK, Palomo L, John V. Periodontal health and systemic conditions. Dent J (Basel) 2020 Nov 19;8(4):130.
2. Prichard J. Philosophy of practice. Periodontics 1965;3(1):32-37.
3. American Academy of Periodontology statement on risk assessment. J Periodontology 2008;79(2):202.
4. Newman MG, Takei HH, Klokkevold PR, Carranza FA. Newman and Carranza’s Clinical Periodontology 13thed. Philadelphia, PA:Saunders. 2019. p.410-412.
5. Loe H, Theilade E, Jensen SB. Experimental gingivitis in man. J Periodontol (1930) 1965;MayJun;36:177-87.
6. Johnson GK, Hill M. Cigarette smoking and the periodontal patient. J Periodontol 2004 Feb;75(2):196-209.
7. Johnson GK, Guthmiller JM. The impact of cigarette smoking on periodontal disease and treatment. Periodontol 2000 2007;44:178-94.
8. Fiorini T, Musskopf ML, Oppermann RV, Susin C. Is there a positive effect of smoking cessation on periodontal health? A systematic review. J Periodontol 2014 Jan;85(1):83-91.
9. Tobacco Use and Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update. Rockville (MD): US Department of Health and Human Services; 2008 May. 3, Clinical Interventions for Tobacco Use and Dependence.
10. Ramseier CA, Suvan JE. Behaviour change counselling for tobacco use cessation and promotion of healthy lifestyles: a systematic review. J Clin Periodontol 2015; 42 (Suppl. 16): S47–S58.
11. Ramseier CA, Woelber JP, Kitzmann J, Detzen L, Carra MC, Bouchard P. Impact of risk factor control interventions for smoking cessation and promotion of healthy lifestyles in patients with periodontitis: a systematic review. J Clin Periodontol 2020 Jul;47 Suppl 22:90-106.
12. Chaffee BW, Couch ET, Vora MV, Holliday RS. Oral and periodontal implications of tobacco and nicotine products. Periodontol 2000 2021 Oct;87(1):241-253.
13. Scott DA, Dukka H, Saxena D. Potential mechanisms underlying marijuana-associated periodontal tissue destruction. J Dent Res 2022 Feb;101(2):133-142.
14. Quaranta A, D’Isidoro O, Piatelli A, Hui WL, Perrotti V. Illegal drugs and periodontal conditions. Periodontology 2000 2022 Oct:90(1):62-87.
15. Thomas SC, Xu F, et al. Electronic cigarette use promotes a unique periodontal microbiome. mBio.2022 Feb22;13(1):e0007522.
16. Wasfi RA, Bang F, et al. Chronic health effects associated with electronic cigarette use: a systematic review. Front Public Health 2022 Oct 6;10:959622.
17. Figueredo CA, Abdelhay N, Figueredo CM, Catunda R, Gibson MP. The impact of vaping on periodontitis: a systematic review. Clin Exp Dent Res 2021 Jun;7(3):376-384.
18. Genco RJ, Graziani F, Hasturk H. Effects of periodontal disease on glycemic control, complications, and incidence of diabetes mellitus. Periodontol 2000 2020 Jun;83(1):59-65.
19. Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, Hooks B, Isaacs D, Mandel ED, Maryniuk MD, Norton A, Rinker J, Siminerio LM, Uelmen S. Diabetes Selfmanagement Education and Support in Adults With Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care 2020 Jul;43(7):1636–1649.
20. Ferreira RO, Corrêa MG, Magno MB, Almeida APCPSC, Fagundes NCF, Rosing CK, Maia LC, Lima RR. Physical activity reduces the prevalence of periodontal disease: systematic review and meta-analysis. Front Physiol 2019 Mar 21;10:234.
21. Kinane D, Bouchard P. Group E of European Workshop on Periodontology. Periodontal diseases and health: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol 2008 Sep;35(8 Suppl):333-7.
22. Sanz M, Marco Del Castillo A, Jepsen S, Gonzalez-Juanatey JR, D’Aiuto F, Bouchard P, Chapple I, Dietrich T, Gotsman I, Graziani F, Herrera D, Loos B, Madianos P, Michel JB, Perel P, Pieske B, Shapira L, Shechter M, Tonetti M, Vlachopoulos C, Wimmer G. Periodontitis and cardiovascular diseases: Consensus report. J Clin Periodontol 2020 Mar;47(3):268-288.
23. Herrera D, Sanz M, Shapira L, Brotons C, Chapple I, Frese T, Graziani F, Hobbs FDR, Huck O, Hummers E, Jepsen S, Kravtchenko O, Madianos P, Molina A, Ungan M, Vilaseca J, Windak A, Vinker S. Association between periodontal diseases and cardiovascular diseases, diabetes and respiratory diseases: Consensus report of the Joint Workshop by the European Federation of Periodontology (EFP) and the European arm of the World Organization of Family Doctors (WONCA Europe). J Clin Periodontol 2023 Jun;50(6):819-841.
24. Pamuk F, Kantarci A. Inflammation as a link between periodontal disease and obesity. Periodontol 2000 2022 Oct;90(1):186-196.
25. Akcali A, Huck O, Tenenbaum H, Davideau JL, Buduneli N. Periodontal diseases and stress: a brief review. J Oral Rehabil 2013 Jan;40(1):60-8.
26. Reners M, Brecx M. Stress and periodontal disease. Int J Dent Hygiene 2007;5:199-204.
27. Ball J, Darby I. Mental health and periodontal and peri-implant diseases. Periodontol 2000 2022 Oct;90(1):106-124.
28. Vishakha G, Kapoor A, Malhotra R, Sachdeva S. Epigenetics and periodontal disease: hope to tame the untameable. Curr Gene Ther 2014;14(6):473-81.
29. Geurs NC. Osteoporosis and periodontal disease. Periodontol 2000 2007;44:29-43.
30. Chaves JDP, Figueredo TFM, Warnavin SVSC, Pannuti CM, Steffens JP. Sex hormone replacement therapy in periodontology: a systematic review. Oral Dis 2020 Mar;26(2):270-284.
31. Chen P, Hong F, Yu X. Prevalence of periodontal disease in pregnancy: a systematic review and meta-analysis. Journal of Dentistry 2022;(125):104253–104253.
32. Figuero E, Han YW, Furuichi Y. Periodontal diseases and adverse pregnancy outcomes: mechanisms. Periodontol 2000 2020 Jun;83(1):175-188.
33. Le QA, Eslick GD, Coulton KM, Akhter R, Condous G, Eberhard J, Nanan R. Does treatment of gingivitis during pregnancy improve pregnancy outcomes? A systematic review and meta-analysis. Oral Health Prev Dent 2021 Jan 7;19(1):565-572.
34. Sooriyamoorthy M, Gower DB. Hormonal influences on gingival tissue: relationship to periodontal disease. J Clin Periodontol 1989 Apr;16(4):201-8.
35. Ali I, Patthi B, Singla A, Gupta R, Dhama K, Niraj LK, Kumar JK, Prasad M. Oral health and oral contraceptive - Is it a shadow behind broad daylight? A systematic review. J Clin Diagn Res 2016 Nov;10(11):ZE01-ZE06.
36. Molina A, Huck O, Herrera D, Montero E. The association between respiratory diseases and periodontitis: a systematic review and meta-analysis. J Clin Periodontol 2023;50:842-887.
37. Lertpimonchai A, Rattanasiri S, Tamsailom S, et al. Periodontitis as the risk factor of chronic kidney disease: mediation analysis. J Clin Periodontol 2019;46:631-639.
38. Priyamvara A, Dey A, Maddi A, Teich S. The relationship between periodontal and kidney disease: a critical review. Quintessence Int 2022;53:744-751.
39. He I, Poirier B, et al. Demystifying the connection between periodontal disease and chronic kidney disease- an umbrella review. J Periodontal Res 2023 Oct;58(5):874-892.
40. Chambrone L, Foz AM, Guglielmetti MR, Pannuti CM, Artese HP, Feres M, Romito GA. Periodontitis and chronic kidney disease: a systematic review of the association of diseases and the effect of periodontal treatment on estimated glomerular filtration rate. J Clin Periodontol 2013 May;40(5):443-56.
41. Sansores-Espana D, Carrillo-Avila A, Melgar-Rodriguez Diaz-Zuniga J, Martinez-Aguilar V. Periodontitis and Alzheimer’s disease. Med Oral Patol Oral Cir Bucal 2021 Jan 1;26(1):43-48.
42. Marchini L, Ettinger R, Caprio T, Jucan A. Oral health care for patients with Alzheimer’s disease: an update. Spec Care Dentist 2019 May;39(3):262-273.
43. Van der Velden U. Effect of age on the periodontium. J Clin Periodontol 1984 May;11(5):281-94.
44. Curtis DA, Lin GH, Rajendran Y, Gessese T, Suryadevara J, Kapila YL. Treatment planning considerations in the older adult with periodontal disease. Periodontol 2000 2021 Oct;87(1):157-165.
45. Gundala R, Chava VK. Effect of lifestyle, education and socioeconomic status on periodontal health. Contemp Clin Dent 2010 Jan;1(1):23-6.
46. Singh A, Peres MA, Watt RG. The relationship between income and oral health: a critical review. J Dent Res 2019 Jul;98(8):853-860.
47. Boillot A, El Halabi B, Batty GD, Rangé H, Czernichow S, Bouchard P. Education as a predictor of chronic periodontitis: a systematic review with meta-analysis population-based studies. PLoS One 2011;6(7):e21508.
48. Nguyen TM, Tonmukayakul U, Le LK, Calache H, Mihalopoulos C. Economic evaluations of preventive interventions for dental caries and periodontitis: a systematic review. Appl Health Econ Health Policy 2023 Jan;21(1):53-70.
49. Shiau HJ, Reynolds MA. Sex differences in destructive periodontal disease: a systematic review. J Periodontol 2010 Oct;81(10):1379-89.
50. Lipsky MS, Su S, Crespo CJ, Hung M. Men and oral health: a review of sex and gender differences. Am J Mens Health 2021 May-Jun;15(3):15579883211016361.
51. Sabbah W, Tsakos G, Sheiham A, Watt RG. The effects of income and education on ethnic differences in oral health: a study in US adults. J Epidemiol Community Health 2009 Jul;63(7):516-20.
52. Loos BG, Van Dyke TE. The role of inflammation and genetics in periodontal disease. Periodontol 2000 2020 Jun;83(1):26-39.
53. Shaddoz LM, Morford LA, Nibali L. Periodontal health and disease: the contribution of genetics. Periodontol 2000 2021;85:161-181.
54. Heasman PA, Hughes FJ. Drugs, medications and periodontal disease. Br Dent J 2014 Oct;217(8):411-9.
55. Mawardi H, Alsubhi A, Salem N, Alhadlaq E, Dakhil S, Zahran M, Elbadawi L. Management of medication-induced gingival hyperplasia: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol 2021 Jan;131(1):62-72.
56. Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodontol 2000 2013 Jun;62(1):59-94.



Roger N. Warren, D.D.S., is an assistant professor, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, NY.
Liana Umbrio, D.D.S., is a graduate of New York University College of Dentistry, New York, NY, and an incoming first-year resident at the Eastman Institute for Oral Health, University of Rochester School of Medicine and Dentistry, periodontology program, Rochester, NY.
Leena Palomo, D.D.S., M.S.D., is professor and chair, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, NY.
Dr. WarrenDr. UmbrioDr. Palomo
Orofacial Manifestations of Highly Active Antiretroviral Therapy (HAART) and Pre-Exposure Prophylaxis (PrEP)
Implications for Dental Care and Guidelines for Management
Alec Donelian; Yuedi Yu; Ezzard Rolle, D.D.S.; Alison Newgard, D.D.S.
ABSTRACT
HAART and PrEP have demonstrated reduction of HIV-related mortality and HIV infection, respectively. A range of orofacial side effects has been associated with both HAART and PrEP. As PrEP usage has increased, there has also been an increase in sexually transmitted infections that have orofacial symptoms. As oral health-care providers, it is important that we recognize these orofacial side effects and symptoms. Further, we offer clinical recommendations for dental professionals treating patients who are on either HAART or PrEP and their associated risk factors.
Human immunodeficiency virus (HIV) is a viral pathogen that attacks the body’s immune system, weakening it over time and making it increasingly susceptible to a range of infections and diseases. If left untreated, HIV can progress to acquired immunodeficiency syndrome (AIDS), a severe and often life-threatening condition. Although there is no definitive cure for HIV, the disease can be managed effectively with highly active antiretroviral
therapy (HAART). Comprising a combination of at least three antiretroviral drugs, HAART aims to suppress the viral load, thereby improving the quality of life and minimizing the risk of HIV transmission.[1] Table 1 summarizes different classes of HAART medications and their mechanisms of action.
Beyond the management of people living with HIV, the prevention of HIV transmission plays a crucial role in the comprehensive approach to tackling this health challenge. Pre-exposure prophylaxis (PrEP) has revolutionized HIV prevention since its FDA approval. These drug regimens are now commonly prescribed to high-risk patients, making it a standard aspect of preventive health care. Its widespread use and accessibility through health-care providers means it’s not just a specialized treatment but a broadly applicable preventive measure.
Major PrEP medications include Truvada®, Descovy®, and Apretude®. Table 2 summarizes available PrEP medications, their components and their respective routes of administration. Like HAART, these medications function by inhibiting essential enzymes involved in the life cycle of HIV.
Both HAART and PrEP have demonstrated reduction of HIV-related mortality and HIV infection, respectively. However, like many medical interventions, these therapies are not without their drawbacks.[2,3] Specifically, a range of oro-
facial side effects has been associated with both HAART and PrEP medications.[4,5] Certain medications, such as Truvada® and Descovy®, are used in both HAART and PrEP regimens. Specifically, the components emtricitabine, tenofovir and tenofovir alafenamide found in these medications could induce similar orofacial side effects in both HAART and PrEP.
This brief aims to discuss the oral manifestations associated with the use of HAART and PrEP medications. Further, we offer recommendations for dental professionals treating patients who are on either HAART or PrEP and their associated orofacial risk factors.
Orofacial Side Effects of HAART and PrEP
The adverse systemic and orofacial effects associated with antiretroviral drugs impact the quality of life of patients and significantly contribute to noncompliance. Because these medications are administered long-term, typically dosed daily, and require a high level of adherence to be effective, understanding and managing their side effects are essential to successful treatment.
In addition to the established systemic effects of antiretroviral drugs, such as gastrointestinal disturbances, reduced bone mineral density, and altered kidney and liver function, a subset of associated orofacial manifestations has been documented. HAART regimens are associated with a variety of adverse orofacial effects, including xerostomia, taste disturbances, ulcers, erythema multiforme,
toxic epidermal necrolysis, facial lipoatrophy, perioral paresthesia, exfoliative cheilitis, oral mucosal hyperpigmentation and oral warts.[4]
NRTIs, NNRTIs and PIs commonly used in HAART also cause changes in the growth and differentiation of gingival epithelium, including loss of tissue integrity, increased tissue proliferation, impaired healing ability and cell cycle dysregulation. These cytologic alterations may present clinically as fragile gingival tissue, ulcers and blisters. This may also increase patients’ susceptibility to viral tumors and opportunistic infections.[6]
HAART-associated oral conditions include xerostomia, which results in increased caries risk and vulnerability of mucosa to mechanical injury. While most HAART-related adverse oral effects are not exclusive to a specific class of antiretroviral agent, it has been suggested that erythema multiforme is common in NNRTIs.[4] Ulcers, xerostomia and lipodystrophy are common in NRTIs.[4] Taste disturbances, paresthesia and xerostomia are common in PIs.[4] Several dentofacial complications specific to HIV-infected children on HAART have also been reported. They include molar-incisor hypomineralization, delayed dental eruption and lipodystrophy.[7] Table 3 summarizes common HAART-related oral complications and their respective clinical presentations. Though the literature surrounding the adverse effects of PrEP, specifically Truvada® and Descovy®, is limited, several studies have started to identify oral complications in HIV-un-

infected populations taking these preventative medications. The prolonged use of PrEP is associated with xerostomia, increased thirst and taste disturbances.[5] Given that PrEP and HAART regimens share common antiretroviral agents, specifically the NRTI tenofovir, preliminary data has suggested that PrEP may also exert a pro-inflammatory effect on the oral mucosa similar to the adverse cytologic alterations to gingival epithelium reported in HAART patients.[8]
No studies to date have specifically explored the orofacial effects of Apretude®, the newest PrEP formulation. However, allergic reactions to Apretude® can result in swelling of the mouth, face, lips or tongue. This medication’s route of administration as a long-acting bimonthly injection poses a promising solution to the compliance issues surrounding oral PrEP formulations.
One recent study investigating antibiotic resistance in men who have sex with men (MSM) taking PrEP determined that the oropharynx of MSM on PrEP was significantly enriched with higher levels of bacteria that contain genes which confer resistance to fluoroquinolones, macrolides, tetracyclines and multidrug efflux pumps when compared to the general population.[9] This finding emphasizes the importance of minimizing unnecessary prescription of antimicrobial agents to dental patients in this population.[9]
Increased STIs in HAART and PrEP Users
The implementation of pre-exposure prophylaxis (PrEP) as a preventive measure against HIV transmission among men who have sex with men (MSM) has garnered attention for its effectiveness. However, a growing body of research highlights a concerning trend of increased STIs following PrEP initiation. Numerous studies indicate a significant rise in STI rates among individuals starting PrEP.[10] Some studies suggest an escalation in STIs, such as syphilis, especially among MSM, whether people living with HIV or on PrEP.[11]
There have also been reports of increases in chlamydia, as well as HPV in PrEP users.[12,13] These findings underscore
the need for comprehensive STI prevention and care strategies in conjunction with PrEP implementation. PrEP users reported an increase in high-risk behaviors, including a decrease in consistent condom use. In those recent reports, approximately 50% of participants were diagnosed with an STI within 12 months of follow-up, highlighting potential challenges in maintaining vigilance against STIs.[14]
This data is important because many of the STIs mentioned have oral manifestations necessitating the importance of recognizing these lesions as an effort for early detection and treatment. They include the following:
• Syphilis is a bacterial infection caused by the spirochete bacterium Treponema pallidum. In the mouth, syphilis can present as mucous patches or white lesions on the tongue, lips or inside the cheeks.
• Herpes Simplex Virus (HSV-2) is a common viral infection that can affect the mouth and oral mucosa, causing cold sores or oral herpes. These cold sores typically appear as small, fluid-filled blisters on or around the lips or inside the mouth. While oral herpes is generally not as severe as genital herpes, it can still cause discomfort and pain during outbreaks.
• Human Papilloma Virus (HPV) is a group of viruses known to cause various types of warts, including genital warts. In the context of STIs, high-risk HPV strains are associated with the development of certain cancers, including cervical, anal and oral cancers. HPVrelated oral lesions can appear as warts or raised growths in the mouth, including the oral cavity and back of the throat.
• Gonorrhea is a bacterial infection that primarily affects the genital and urinary tracts. Although gonorrhea can cause symptoms, such as painful urination and discharge, it is not a common cause of oral manifestations. However, in rare cases, gonorrhea can be transmitted through oral sex, leading to throat infections (pharyngeal gonorrhea), characterized by sore throat, swollen lymph nodes and discomfort while swallowing.
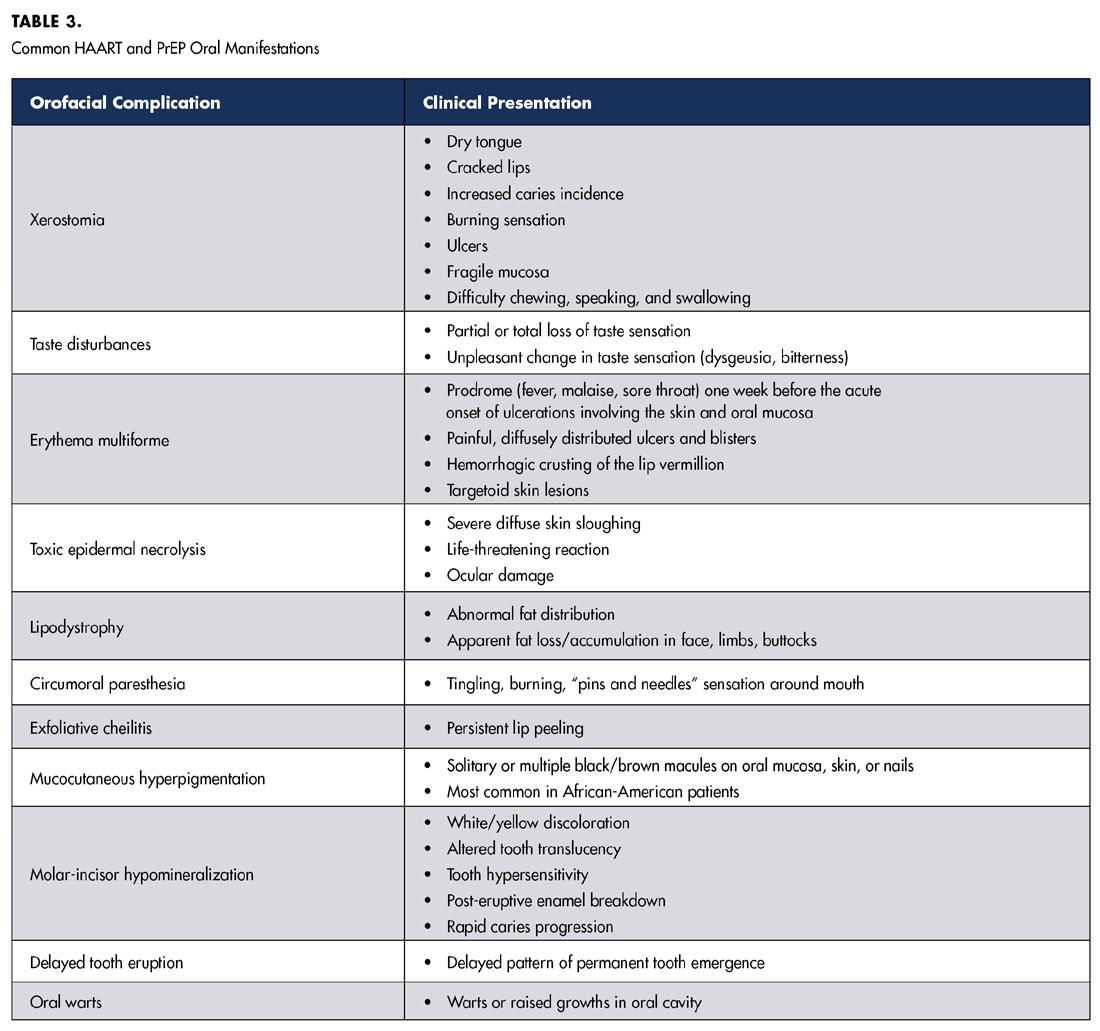
• Chlamydia is a bacterial infection commonly transmitted through sexual contact. While it primarily affects the genital and urinary tracts, most chlamydia infections in the throat have no symptoms. When symptoms are present, they can include a sore throat. It’s important to note that STIs can vary widely in their presentation and impact on different individuals. Regular STI testing, practicing safe sex and maintaining good oral hygiene are crucial steps in preventing and addressing these infections, both in the genital and oral areas (Centers for Disease Control).
Consequently, the integration of STI prevention and care with PrEP programs is gaining significance as a strategic approach to addressing this emerging concern. A recent regimen, doxycycline prophylaxis/post-exposure prophylaxis (DoxyPrEP/PEP), developed to mitigate the rise in bacterial STIs, has been gaining traction in the medical community and may be observed being used in patients, especially those taking PrEP. Research in this area is promising. Although further robust data are required to better understand its efficacy, target population suitability, community acceptability and potential impact on behavioral risk compensation.
While PrEP remains an essential tool in HIV prevention, it’s crucial to consider the broader implications on STI transmission and adopt measures that ensure the holistic well-being of those utilizing PrEP services.
Clinical Recommendations for Providers
It is important to equip dental health-care providers with essential knowledge to better treat patients taking HAART or PrEP. The following are recommendations for best treating this population.
1. Patient Assessment: Perform a thorough dental and medical history review, including the patient’s HIV status and current medications (including HAART or PrEP).
2. Infection-Control Measures: Adhere strictly to infection-control protocols to minimize the risk of cross-contamination and transmission of infections.
3. Oral Hygiene Instruction: Provide oral health education to patients on HAART or PrEP, emphasizing the importance of maintaining good oral hygiene practices.
4. Regular Oral Examinations: Schedule regular oral examinations, at least every six months, for patients on
HAART or PrEP to monitor for any oral manifestations or side effects.
5. Preventative Care: Emphasize the importance of preventative dental care, such as regular cleanings and prophylactic treatments, to minimize the risk of oral complications.
6. Counsel on Medication-Related Oral Side Effects: Educate patients about potential oral side effects of HAART or PrEP. Encourage patients to report any unusual oral symptoms promptly.
7. Collaborative Care:
a. Maintain open communication with patient’s HIV care team to ensure coordinated care and management of oral manifestations.
b. If you have any doubts, consider referring patient to specialty clinics, like oral pathology or oralfacial pain, for final diagnosis and management.
8. Management of Xerostomia (Dry Mouth): Recommend sugar-free gum or lozenges to stimulate saliva production. Prescribe artificial saliva substitutes if needed. During routine dental check-ups, dentists can engage in open, confidential and non-judgmental conversations with
Your dental practice is more than a business—it’s your legacy. At Henry Schein Dental Practice Transitions, we specialize in helping practice owners with seamless, stress-free transitions tailored to personal, professional, and financial goals.
Why Choose Us for Your Practice Transition?
• Unlock your practice’s true value with expert, data-driven valuations to unlock your practice’s true value
• Gain access to 36,000+ purchasers
• Full-service support from your first consultation to final closing
• Unmatched expertise backed by local insights and deep industry connections
• Over 500 closings with over $400MM in sales price since 2023
Start your journey to a rewarding retirement today. Contact us or scan the QR code to schedule a complimentary consultation.
800-988-5674
DPT@henryschein.com

their patients emphasizing the interconnectedness of oral and general health. Dentists can facilitate referrals to appropriate physicians. This proactive approach not only enhances patients’ awareness but also emphasizes the commitment of dentists to their patients’ overall health and well-being. Ultimately, the dental chair can serve as a platform for comprehensive health discussions, contributing to an interdisciplinary approach to health care. p
Queries about this article can be sent to Dr. Newgard at an2621@cumc.columbia.edu.
REFERENCES
1. Eggleton JS, Nagalli S. Highly Active Antiretroviral Therapy (HAART). 2023. StatPearls. StatPearls Publishing.
2. Panos G, et al. Mortality and morbidity of HIV infected patients receiving HAART: a cohort study. Current HIV Research 2008. 6(3):257–260.
3. Fonner VA, et al. Effectiveness and Safety of Oral HIV Pre-exposure Prophylaxis for All Populations. AIDS (London, England), 2016. 30(12):1973–83.
4. Diz Dios P, Scully C. Antiretroviral therapy: effects on orofacial health and health care. Oral Diseases 2014;20(2):136–45.
5. Macedo N, et al. Oral conditions and salivary analysis in HIV-uninfected subjects using preexposure prophylaxis. Medicina Oral Patología Oral y Cirugia Bucal 2022;27(3):e265–73.
6. Mitchell D, et al. HIV nucleoside reverse transcriptase inhibitors efavirenz and tenofovir change the growth and differentiation of primary gingival epithelium. HIV Medicine 2014;15(4):196–202.
7. Madam et al. A review of basic knowledge of HIV infection for orthodontic management of HIV patients. 2023. Cureus. https://doi.org/10.7759/cureus.37770.
8. Baggio G, et al. Inflammatory cytologic alterations in the oral epithelium associated with HIV Pre-exposure prophylaxis: a preliminary study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology 2021;131(5):534–39.
9. Van Dijck C, et al. The oropharynx of men using HIV Pre-exposure prophylaxis is enriched with antibiotic resistance genes: a cross-sectional observational metagenomic study. Journal of Infection 2023;86(4):329–37.
10. Azarnoosh M, Somuncu JI, Martin-Iguacel, R. Incidence of sexually transmitted infections after initiating HIV Pre-exposure prophylaxis among MSM in Southern Denmark. American Journal Men’s Health 2021;15(3). 15579883211018917.
11. Lemmet T, et al. High syphilis prevalence and incidence in people living with HIV and Preexposure prophylaxis users: a retrospective review in the French Dat’AIDS cohort. PLOS ONE 2022;17(5), p: e0268670.
12. Traeger M, et al. Association of HIV Pre-exposure prophylaxis with incidence of sexually transmitted infections among individuals at high risk of HIV infection. Journal American Medical Association 2019;321(14):1380-90.
13. Cotte et al. Prevalence and incidence of human papillomavirus infection in men having sex with men enrolled in a Pre-exposure prophylaxis study: a sub-study of the Agence Nationale de Recherches sur le SIDA et les Hépatites Virales “Intervention Préventive de l’Exposition aux Risques avec et pour les hommes Gays” trial. Clinical Infectious Disease 2021;72(1): p.4 1-9.
14. Scott H, Klausner J. Sexually transmitted infections and Pre-exposure prophylaxis: challenges and opportunities among men who have sex with men in the US. AIDS Research and Therapy 2016;13(1):5.
Alec Donelian is a dental student, Columbia University College of Dental Medicine, New York, NY.
Yuedi Yu is a dental student, Columbia University College of Dental Medicine, New York, NY.
Ezzard Rolle, D.D.S., is assistant professor, Columbia University College of Dental Medicine, Section of Cariology and Restorative Sciences, Division of Operative Dentistry, New York, NY,
Alison Newgard, D.D.S., is assistant professor, Columbia University College of Dental Medicine, Section of Cariology and Restorative Sciences, Division of Operative Dentistry, New York, NY.


Learn how to defend your practice from the latest cyber threats.
Register for this timely discussion between your NYSDA Technology Chair and the CEO of Black Talon.

A 2-Part Fireside Chat
Webinar Series
with Dr. Mitchell Rubinstein and Gary Salman
Ransomware, Reputation, and Regulation: What NY Dentists Need to Know Now
Thursday, August 14 @ noon ET

If You Can’t See It, You Can’t Stop It: The X-Ray Mindset for Cybersecurity
Thursday, September 25 @ noon ET



Register today @ blacktalon.co/nysda
A Black Talon Security webinar series offered exclusively for NYSDA members.
Gary Salman CEO Black Talon Security
Mitchell Rubinstein, DMD Information Technology Chair NYSDA
Assessment of Patient Knowledge and Awareness of Prosthodontics for Student and Patient Education and Communication
Mijin Choi, D.D.S., M.S., M.B.A.; Tejal Gohil, B.D.S.; Cristina Osorio, D.D.S.; Hannah Jeong; Thomas S. Giugliano, D.D.S.
ABSTRACT
This study evaluates patient understanding of the scope of prosthodontic treatments. Utilizing an 11-question survey, 149 patients at a postgraduate prosthodontic clinic were queried. Data analysis included frequency summaries, cross-tabulations and Pearson Chi-square tests. Results showed 68.4% of respondents knew about the role of prosthodontists. Their main concerns were improving chewing (43.9%) and smile (42.6%), varying by age. While many recognized prosthodontists’ scope, cosmetic and complex dental treatments were less well known as prosthodontic specialties. This highlights a gap in patient awareness regarding the full range of prosthodontic services.
The purpose of this research study was to understand patients’ level of awareness about prosthodontics via survey. The specialty has struggled with raising public awareness since prosthodontics was recognized by the American Dental Association as a specialty in 1947.[1] The American College of Prosthodontists (ACP) is helping to change public awareness through National Prosthodontics Awareness Week, via local and national proactive public relations tools, and training.
In the last five years, there have been efforts to increase the media presence of the prosthodontics specialty by the ACP. The ACP 2017 Public Relations Activities Summary reports there were 70,265 mentions of the terms prosthodontist and prosthodontics in social media and 13,119 in traditional media in 2017,[2] whereas in 2011, there were 864 traditional media mentions of these terms.[3] Presence in social and traditional media has become crucial in the overall effort to increase knowledge of the specialty. During Dr. John Agar’s ACP presidency in 2013-2014, the word “prosthodontist” was added to Microsoft’s spell check for the first time.[4] This illustrates how long the specialty has struggled to establish broader recognition in the minds of the public.
The Glossary of Prosthodontic Terms 10th edition (GPT-10) defines prosthodontics as “the dental specialty pertaining to the diagnosis, treatment planning, rehabilitation, and maintenance of the oral function, comfort, appearance, and health of patients with clinical conditions associated with missing or deficient teeth and/or maxillofacial tissues by using biocompatible substitutes.”[5] This definition has not been helpful to the general public’s understanding of the complex restorative and reconstructive scope of dental care that only trained prosthodontists are educationally qualified to provide.
The belief that all general practitioners and prosthodontists possess an equal level of training is normally due to a lack of knowledge about the specialty. Determining if patients are aware of prosthodontic specialty services is a
question of whether sufficient and effective marketing and patient education have been provided to the public.
According to a survey of 500 people, the criteria which are most important to people when finding a new dentist are, in order of importance, convenience in terms of distance and appointments, and online reviews.[6] Whereas in the past, before the use of social media as a referral tool, the public relied on word-of-mouth to satisfy their personal requirements for deciding on a dentist.[7,8] Oddly, the wordof-mouth recommendation is still the most powerful tool in marketing.
Prosthodontics as a specialty is just as mysterious to dental students as it is to the general public. In a 2020 survey of senior dental students, the students were asked about their confidence levels in various clinical skills and abilities. Eighty-one percent of seniors felt they received an adequate level of restorative clinical experience, while only 57% felt the same about the restoration of implants.[9] In the survey, prosthodontics (complex restorative dental care) was not part of the questions. However, the survey also indicated an upward trend of students seeking advanced education, from 35% in 2015 to 40% in 2020.
While these data do not address the need for further training in prosthodontics (complex restorative treatments), the recent trend reflects students’ desire to pursue advanced restorative education that includes implant restorative dentistry. The irony is that these same students, for the most part, feel they received adequate education (34.8% highly confident and 48.9% moderately confident) to carry out dental treatments for replacement of teeth, including fixed, removable and dental implant prosthodontics.
The survey presented here attempted to investigate the public’s knowledge of prosthodontics and prosthodontists. The hypothesis was that older age groups would have different preferred ways to learn about prosthodontists and different treatment concerns than younger age groups.
Materials and Methods
Eleven questions were designed for the study, and 149 survey responses were analyzed. The full survey questions are shown in tables 1a and 1b. An Institutional Review Board (IRB) approval was received before beginning the survey (NYU Langone IRB S17-00318). The patients who presented in the postgraduate prosthodontic clinic were approached, and individuals who consented and were able to complete the survey in English were enrolled. The completed surveys were stored in a secure location in the principal investigator’s office. Data from the study was saved on a networked and password-protected computer.
Data Analysis and Data Monitoring
Data was entered into an Excel spreadsheet and exported to IBM SPSS (v28, IBM Corp., Armonk, NY) for analysis. Data were summarized as the number and percentage responding to each question. The age groups were collapsed into two groups—18 to 65 and over 65—so that there were a similar number of participants in each group. Associations between responses to certain pairs of questions were analyzed using the Chi-square test. Statistical significance level was set at 0.05.
Results
The survey questions and frequency analysis are shown in tables 1a and 1b. The makeup of the groups was 54.4% of participants were between the ages of 18 to 65, and 45.6% were above 65 years of age. On the question “How did you hear about NYUCD?” 46.2% indicated that family and friends were the most frequent source. TV/radio or internet advertisements only accounted for 7.5%. Also, 54.8% of the participants were referred by undergraduate and postgraduate clinics combined; 45.2% were referred by outside dentists or self-referred (Table 1a). Therefore, the majority of referrals were internal, from the New York University College of Dentistry. Finally, 80.8% of participants were existing patients in the prosthodontic clinic (Table 1a).
Regarding participants’ ongoing treatment experiences in the prosthodontic clinic, implant (48.3%), complete dentures (33.6%) and crowns (20.8%) were the most common responses (Table 1a).
The number one treatment concern was improving chewing ability (43.9%), followed by improving smile (42.6%) and replacing missing teeth (31.1%) (Table 1a). Other concerns listed were overall health, dental health, facial esthetics, finances, replacement of teeth, replacement restorations or prostheses, pain relief and treatments for failed restorations.
Participants’ past treatment experiences were mostly provided by prosthodontists and general dentists (Table 1b). General dentists (48.3%) were the most frequently visited previous dentists.
Regarding the question on how the participants learned about what a prosthodontist does (Question 9), 67.0% answered that they learned from previous students, general dentists or other specialists, while the remainder listed friends and family, news and advertisements (Table 1b).
On the question “Do you know what a prosthodontist is?” 68.4% answered “Yes” (Table 1b). When asked about the treatments prosthodontists provide (Question 10), most participants answered crowns (56.4%), bridges (55.0%),
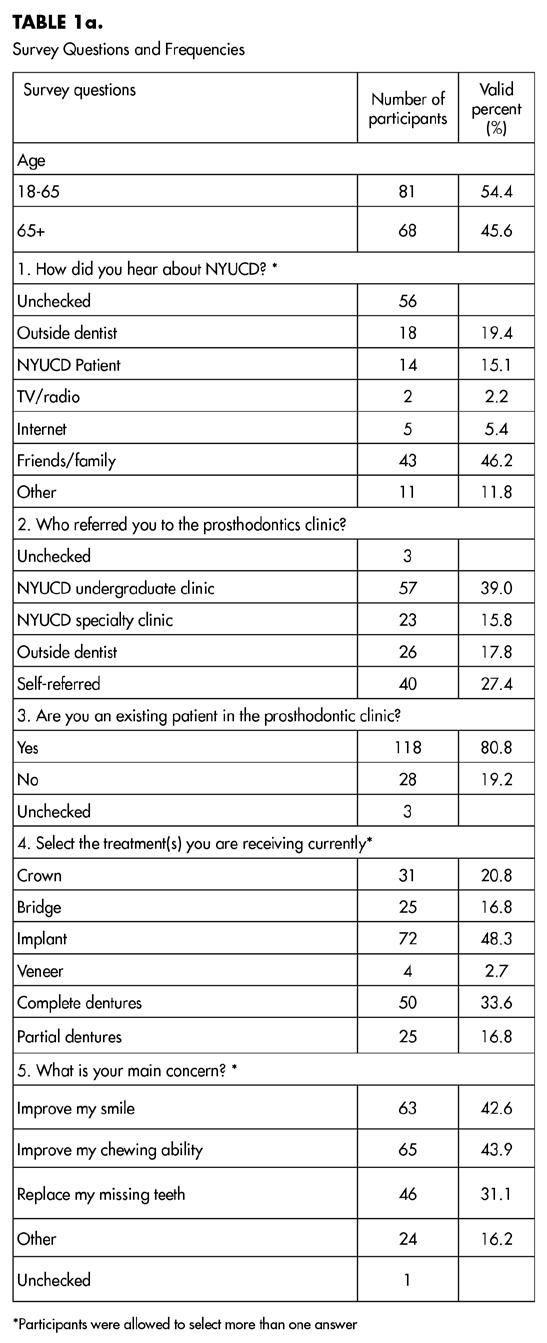
implants (60.4%), complete dentures (56.4%) and partial dentures (53.0%). Fewer listed “complicated treatments” (34.9%) and veneer (cosmetic) restorations (39.6%), and fewer yet thought prosthodontists provide braces and root canals (Table 1b).
Question 11 (Table 1b) asked about the preferred ways to learn about prosthodontists. The top two responses were “education by general dentists” (52.1%) and “Google search” (44.5%). Social media (7.6%) was their least preferred way. In the cross-tabulation analysis between age groups and social media as a way of learning about prosthodontists, both respondents 18 to 65 years old (87.5%) and 65 and above (98.2%) also chose social media as the least preferred way to learn about prosthodontists (Table 2, P = 0.028).
The participants’ responses on whether they previously received prosthodontic treatments (Question 7) were crosstabulated with the responses regarding the scope of care in the specialty of prosthodontics (Question 10). Participants who previously received treatment by prosthodontists were more likely to say that prosthodontists specialize in crowns (67.7%, P = 0.014), bridges (66.2%, P = 0.016), implants (70.8%, P = 0.023) and complete dentures (69.2%, P = 0.005). Although there was no statistical significance, it is important to mention that the many participants with past prosthodontic treatment experience did not recognize partial dentures (40.0%), complex treatments (60.0%) and cosmetic dentistry (58.5%) as scopes of treatments in prosthodontics (Table 3).
The participants’ main treatment concerns (Question 6) were related to age (Question 1). The 18-to-65 age group was more likely to be concerned with improving their smile (55.6%, P < 0.001) and had multiple concerns relative to the other participating age group. The over-65-age group was more concerned with improving chewing ability (55.2%, P = 0.012) than the 18-to-65 age group (Table 4).
Discussion
Demographics of Dental Specialties
According to the 2022 American Dental Association (ADA) Health Policy Institute Analysis, prosthodontists comprised less than 2% of all dental specialties, including general practice, making prosthodontics the sixth specialty in number among the 12 dental specialties recognized by the National Commission on Recognition of Dental Specialties and Certifying Boards (NCRDSCB). The growth of the number of prosthodontists from 2001 to 2022 was 13.7%. More than three-quarters (78.5%) of all practitioners are general dentists. The second-highest percentage of dental practitioners are orthodontists (5.4%), followed by pediatric den-

















tists (4.4%). New York State has the third-highest number of dentists in the U.S., behind California and Texas.[10]
The first recognition of prosthodontics as a specialty by the ADA House of Delegates was in 1947. According to PubMed and Google Scholar search, using keywords “awareness AND prosthodontists,” “knowledge AND prosthodontists,” there were no articles published in the United States on the awareness or knowledge level of the general population regarding prosthodontists. Also, there was no research on how patients learned about prosthodontists and their preferred source of information regarding prosthodontists.
Patients’ Preferences for Learning about Prosthodontics
The participants in this study preferred to acquire information about prosthodontists first from their own general dentists, second via self-directed research through Google search, or third through friends and family members’ recommendations (Table 1b). These results showed that the credibility and trust of the source of information are most important. Their own dentists are professionals patients trust, and word-ofmouth (WOM) referrals by other people appeared to provide more confidence when selecting their new prosthodontist.
The power of direct personal communication, aka WOM marketing, has been working since the Stone Age. The story of traditional marketing is that one caveman found a good hunting area and spread the word to his friends. Before long, the place became the most popular hunting area because of WOM “marketing.”[11]
In the modern era, WOM marketing includes Instagram, Twitter, Facebook, Google and Yelp reviews. With such an abundance of information, people must determine if the reviews are authentic and understand if self-perceived dental treatments should be provided by a prosthodontist. Moreover, the public must know what prosthodontists specialize in. Therefore, people are now looking for curated information by established organizations or by credible professionals.
One study conducted in Norway in 2000 looked at the public’s awareness of oral implant therapy. The study concluded that news media (newspapers and TV/radio) was rated as the most prevalent source of information. However, direct personal communication showed a more positive impact, indicating that personal communication with positive validation was regarded as a more reliable source of information.[12] This study also showed the same result, social media being the least preferred way of learning about prosthodontists or prosthodontics (Table 2).
These findings indicate that patient education would be more effective after gaining trust through credible marketing. Effective marketing should include
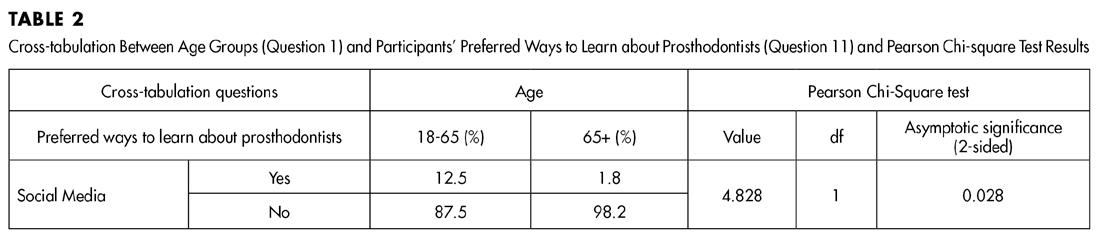
both simple patient education and content that includes the positive experiences of other people, as well as endorsements by well-known people with trusted credibility. People’s interests are sparked when positive experiences are shared by others who have had similar problems. Collecting testimonials from patients and sharing experiences on web-based platforms are important pieces in closing the gap between patient education and gaining trust.
Patients’ Perception
Participants with prosthodontic treatment experience gave implants the highest level of recognition as a treatment modality provided by prosthodontists, followed by complete dentures, then crowns and bridges. However, complex dental treatments (listed as complicated treatments in the survey) were not recognized as the scope of care provided by prosthodontists in 60.0% to 69.1% of the responses regardless of prosthodontic treatment experience (Table 3).

As the definition of prosthodontics by the GPT-10 does not include specific dental treatment modalities, educating patients and dental students on what a prosthodontist does has been a challenge. The difficulties in defining the scope of care in prosthodontics further complicated the perceptions of the public and dentists on when a referral should be made for complex oral and esthetic rehabilitative or reconstructive dental treatments. Defining the scope of prosthodontic care that includes dental treatment modalities will ultimately help to improve understanding of prosthodontics by patients, dental students and other dental professionals.
Patients’ Treatment Concerns
For statistical analyses, participants were divided into two age groups: 18 to 65 and older than 65. In the younger group, smile improvement was the main oral health concern, followed by chewing ability. Improving chewing ability was the main concern in the older group (Table 4). These findings are not surprising because as people age, function may become a higher priority than esthetics for the majority of people.
Recognition of Prosthodontic Treatments
The first definition for prosthodontics under the Google search states, “the branch of dentistry concerned with the design, manufacture, and fitting of artificial replacement for teeth and other parts of the mouth.” How can we de-
The
first definition for prosthodontics under the Google search states, “the branch of dentistry concerned with the design, manufacture, and fitting of artificial replacement for teeth and other parts of the mouth.”
scribe what a prosthodontist does in short sentences for the general public’s understanding? Surely we have been challenged with this since the beginning. Do the explanations of our specialty include treatment modalities that other specialties or dental school education do not provide? We are educationally qualified to perform complex oral rehabilitative and reconstructive dental treatments. For the general public, not as a full definition for the GPT-10, we propose the following statement:
“Prosthodontists specialize in complex dental treatments that may involve high-level esthetic restorations with implants, crowns, bridge, and dentures for missing and defective teeth and jaw structures.”


Study Limitations
A limitation of this study is that the number of participants was relatively small for a strong qualitative survey study. All study participants received information about prosthodontics because the participants were referred for prosthodontic consultation and treatment. Therefore, the findings were used to analyze the effectiveness of the information provided about prosthodontists.
A larger sample size with dental patients who may or may not have prior experience with prosthodontists would have yielded improved insight into the public’s knowledge about the prosthodontic specialty. Furthermore, a multicenter study that includes a broader spectrum of patients would reduce convenience bias.
Conclusion
Despite continued efforts to educate the public and students, describing the specialty of prosthodontics remains a challenge. This study showed that, on average, 57% of participants recognized the common services provided by prosthodontists, such as crowns, bridges, implants and complete dentures. And, on average, only 37% of participants recognized cosmetic dentistry and complex treatments as being within the prosthodontic scope of care. These findings showed that efforts to increase awareness about prosthodontists among the general public should include more emphasis on educating patients with a simple and clear description about prosthodontics. Providing a better description about the scope of prosthodontic treatments may enable more effective and efficient communication between patients and dentists. p
The authors deny any conflicts of interest related to this study. Queries about this article can be sent to Dr. Choi at mc185@nyu.edu.
REFERENCES
1. Transactions of the American Dental Association 1947:80-1.
2. Barth C. Summary Report: 2017 ACP Public Relations Activities, 2017. www.prosthodontics. org/acp-publications/annual-reports/ [Accessed 11 December 2023].
3. Barth C. Summary Report: 2015 ACP Public Relations Activities, 2015. www.prosthodontics. org/acp-publications/annual-reports/ [Accessed 11 December 2023].
4. ACP press release dated November 21, 2014. https://www.prosthodontics.org/assets/1/7/ Agar_Past_President-_na_cb_jra_approved_11-21-14.docx.pdf [Accessed 7 September 2020].
5. Layton DM (Ed.), Morgano SM, Muller F, Kelly JA, Nguyen CT, Scherrer SS, et al. Glossary of Prosthodontic Terms 2023: 10th edition. J Prosthet Dent 2023;130(4S1):e1-e126. PII: S002-3913(23)X0002-X.
6. DentalIQ.com: 2013. https://www.dentistryiq.com/practice-management/article/16354970/ convenience-honesty-and-online-reviews-some-of-the-things-your-dental-patients-want/ [Accessed 1 September 2020].
7. Garry JF. How (and why) patients choose a dentist and stay with him. Orange Cty Dent Soc Bull 1972:5.
8. Book DS, Stockton HJ. Why patients choose a particular dentist. J Can Dent Assoc 1986;52:123-6.
9. Istrate EC, Slapar FJ, Mallarapu M, Stewart DCL, West KP. Dentists of tomorrow: an analysis of the results of the 2020 ADEA Survey of US dental school seniors. J Dent Educ 2021;85:427-40.
10. Supply of Dentists in the U.S.: 2001-2022. https://www.ada.org/en/resources/research/ health-policy-institute/dentist-workforce [Accessed 11 December 2023].
11. Whitler K. Forbes.com. https://www.forbes.com/sites/kimberlywhitler/2014/07/17/why-word-ofmouth-marketing-is-the-most-important-social-media/#7c444f1454a8 [Accessed 2 July 2020].
12. Berge TI. Public awareness, information sources and evaluation of oral implant treatment in Norway. Clin Oral Impl Res 2000;11:401-8. doi: 10.1034/j.1600-0501.2000.011005401.x



Dr. Choi Dr. Gohil Dr. Giugliano
Mijin Choi, D.D.S., M.S., M.B.A., FACP, is clinical professor, Department of Prosthodontics, New York University College of Dentistry, New York, NY.
Tejal Gohil, B.D.S., is clinical assistant professor, Department of Comprehensive Dentistry, University of Texas Health San Antonio School of Dentistry, San Antonio, TX.
Cristina Osorio, D.D.S., is in private practice in Miami, FL
Hannah Jeong, is a fourth-year predoctoral dental student, New York University College of Dentistry, New York, NY
Thomas S. Giugliano, D.D.S., is clinical assistant professor, Department of Prosthodontics, New York University College of Dentistry, New York, NY.

Second District cont. Component
SECOND DISTRICT SDDS Awards
Academic Excellence
Second District’s Awards Committee
had a very busy month, once again providing two $250 awards to two graduating students from the Tottenville High School dental assisting program, two $500 awards to two hygiene students graduating from the CUNY College of Technology Dental Hygiene Program and four $500 awards to four students from the CUNY College of Technology Restorative Dentistry Program.
From Tottenville, the awards went to seniors Tristan Ryan and Nicholas Ho, both for clinical and academic excellence in dental assisting.
From the Restorative Dentistry Program at CUNY—NYCCT, the awards went to: Melissa Lee, graduating stu-
dent, for academic excellence; Genesis Rosario Lara, graduating student, for technical proficiency; Shani Yanowitz, for academic excellence for first-year student; and Dorothy Wong, for technical proficiency for first-year student.
From the Hygiene Program at CUNY—NYCCT, the awards went to: Cassy May, graduating student, for academic excellence, and Le Van La, graduating student, for professionalism.
Loan Forgiveness Program
Second District came through in a big way for its younger members with its Loan Forgiveness Program. Members, up to five years out of dental school, are invited to apply for a grant from the Loan Forgiveness fund to help relieve the astro-

SECOND DISTRICT



SECOND DISTRICT
Marc Meiselman, at right, presents achievement awards to Tottenville dental assisting graduates Tristan Ryan, left, and Nicholas Ho. Teacher Gail Battista is also pictured.
Weather was lousy but golfers had fun at Richmond County outing. They included Drs. Louis Desantis and Bryan Pieroni.
Richmond County President Bryan Pieroni is on giving end of awards presented to day’s outstanding golfers.
Executive Director Bernie Hackett proudly accepts honorary membership in ADA, presented by ADA President Brett Kessler.
Cassy May, CUNY-NYCCT hygiene graduate, accepts award for academic excellence from SDDS President Paul Teplitsky.
nomical dental school debt they have. In the eight years of its existence, the program has awarded 134 recipients with over $1.3 million in grants. The grants are sent to the banking institution holding the recipient’s note, to be applied to the loan principle. This year, 18 new recipients received $10,000 each.
Each year, the Awards Committee examines its available funds and determines the number and size of the grants it can award. The committee is chaired by past SDDS and NYSDA President Dr. Craig Ratner. He is assisted by Drs. Emma Guzman, Christopher Bowers, Tricia Quartey-Sagaille and Kirstin Wolfe, and staff coordinator Christine Terrio.
ED Named Honorary Member
Congratulations to Executive Director Bernie Hackett, who was awarded Honorary Membership in the American Dental Association. It was presented to him by ADA President Dr. Brett Kessler at the Annual Meeting of the NYSDA House of Delegates in May in Uniondale, Long Island. Mr. Hackett has been ED since 1991. He is retiring at the end of this year.
A Rainy Affair
The annual Richmond County Dental Society Golf Outing was held on a very wet May 22 at the Richmond County Country Club. Thirty golfers braved the inclement weather and soggy course but, as they say, a bad day on the golf course is always better than a good day at work.
Congratulations to Mike D’Anna, Ron Leader, Brian Perrone and Terry Craven, who walked away with 1st Place gross honors, and the team of Bryan Pieroni, Grant Bried, Chris Zissler and Jerry Zagury, who earned 1st Place net honors. The long-drive winner was Ron Leader. Closest to the pin went to Grant Bried.
Many thanks to outing sponsors Align Tech, Zimvie, Tru Abutment, Smile IT and DLG.

BRONX COUNTY
BRONX COUNTY
Amarilis Jacobo Installed to NYSDA Office
Don Safferstein, D.D.S.
Bronx County Denal Society congratulates all NYSDA’s new officers, installed at the Annual Meeting of the Association’s House of Delegates in May in Uniondale. Kudos to our own Dr. Amarilis Jacobo, now president-elect of the Association.
CE Courses Set for Fall
You’ll want to mark your calendars for the following upcoming CE courses.
BCDS will offer CPR training on Tuesday, Sept. 16. The class will meet at 6 p.m. at Maestro’s Caterers.
And on Tuesday, Oct. 28, we will host Dr. Joshua Gindea for a presentation entitled “2005 and Beyond.”
SUFFOLK COUNTY
Signing Day
Devin J. Klein, D.D.S., M.S.
Our annual Signing Day on April 16 was another great success, as 100% of the Stony Brook Class of 2025 (47 members) signed up to become ADA members. A big shout-out and thank you to Drs. Devin Klein, Claudia Mahon Vazquez, Ivan Vazquez, Patrick Lloyd, Guenter
Jonke, Patricia Swanson, Jeff Seiver and Joseph Graskemper, who were there to lend their support.
We must also thank Daniella Zajac, Carol Deerwester and 2026 DDS candidate Lasya Anantuni, who arranged the event with support from the New York State Dental Association, which sponsored the luncheon.
The ADA joiners all received a chairside instruction manual, an overview of organized dentistry and some fun questions/answers with giveaways.
Give Kids A Smile
Our April 26th Give Kids A Smile event at the LI Aquarium saw 130 volunteers deliver donated dental care to more than 200 underserved children. A very big thank you to our Ultimate Diamond Sponsor Healthfirst and our Diamond Sponsor Henry Schein without whom this event would not be possible.
A big shout-out to our other sponsors, including the NYS Dental Foundation, Lions Club (Mattituck), Catholic Health Services (St. Charles Hospital) and the American Dental Association. And huge thanks to our member volunteers and supporters, including Stony Brook School of Dental Medicine, Hygiene Care Center at Farmingdale College, Eastern Suffolk BOCES, Long Island Head Start, Bixhorn Technical Center and the Sunrise Hi Railers.
Bronx County delegates to NYSDA House include, from left, Don Safferstein, Executive Director Stephen Harrison, Jerica Cook, Amarilis Jacobo, Richard Herman. Dr. Jacobo was installed NYSDA President-Elect at the meeting.
Component
Suffolk County cont.
Greater Long Island Dental Meeting
The Greater Long Island Dental Meeting (GLIDM) on April 27 was by all accounts a wonderful event, attracting more than 150 people. The feedback from attendees and exhibitors was positive. The educational offerings were top-notch, the food and overall experience outstanding.
Nassau and Suffolk County Dental societies, sponsors of the meeting, thank all the attendees, as well as the exhibitors, who help make the meeting possible: They include Adin Implants, Altfest, Augma Biomaterials, Brasseler USA, Carestream Dental, Dexis, Doral Refining, Garfield Refining, General Refining Corp., Hiossen, Inventory Sight, Jim O’Brien Architecture & Interiors, Law Office of Alan Stein, MLMIC, Neoss, NSK Dental, Orascoptic, Orion Dental Solutions (Creodent), Philips, Precision Dental, Reads, Pulpdent, Rivkin-Radler, LLC, The Smilist, Total Dollar Insurance, TruAbutment and US Dental Practices.
We are already hard at work planning the 2026 meeting, which we expect will return to its original two-day format. Stay tuned for more information.
SCDS Demonstrates What is Possible! Want to know what we did to buck the national and state active licensed dentist market-share trend? Email us at Contact@SuffolkDental.Org or call us at (631) 232-1400. (Note: the 2024 yearend datapoints are unavailable owing to a Salesforce/Fonteva issue.)
Don’t Miss a Thing
We continue to make a significant push to better communicate and connect with our members in methods that more easily integrate with their life-


SUFFOLK COUNTY

April Give Kids A Smile event at Long Island Aquarium drew large cohort of volunteers, who delivered much-needed dental care to more than 200 underserved children.
style. You can find us on Facebook, X, Instagram, LinkedIn and, even, Spotify, in addition to our traditional www. SuffolkDental.Org presence.
SEVENTH DISTRICT Dentists Impacting Communities around the Globe
Becky Herman, Executive Director
Dr. Rosemeire Santos-Teachout Brings Compassion and Care to Guatemala.
In a powerful testament to the life-changing work dental professionals can do beyond the office, Dr. Rosemeire Santos-Teachout recently led a transformative mission to Guatemala, delivering critical dental care to underserved communities.
Joining forces with Women Physicians & Dentists in Christ (WPDC) and the Christian Medical & Dental Associations (CMDA), Dr. Santos-Teachout’s team partnered with Advancing the Ministries of the Gospel (AMG) to serve the villages of Cubulco and Chirramos. Despite the rugged journey, including a heart-pounding 90-minute ride clinging to the back of a truck loaded with supplies, their commitment never wavered.
Dr. Santos-Teachout led the dental team, joined by one hygienist and one dental student. Together, they provided compassionate, hands-on care to 30 patients, many of whom needed two to five extractions each. In addition to oral surgery, they provided vital hygiene education and services.
“This was the most impactful mission I’ve ever experienced,” said Dr. Santos-Teachout. “We didn’t just bring care, we brought hope. If sharing our journey inspires other professionals or encourages donations, I would be truly grateful.”
Dr. Sean McLaren Provides Much Needed
Care in Honduras
For the fifth straight year, Dr. Sean McLaren, provided much needed dental care to children in remote villages of Honduras. His mission entailed treating 30 patients a day with no power, X-
rays or handpieces. Dr. McLaren joined students from Duke University on this trip, making a global impact through compassionate care.
At the Seventh District Dental Society, we are proud to celebrate our members’ dedication and leadership. Drs. Santos-Teachout and McLaren exemplify the spirit of our Smile Bright, Community Right campaign, proving that when dental professionals come together, we can change lives, one smile at a time.
New Fellow
Dr. Matthew Valerio, president of the Seventh District Dental Society, chair of its Ethics Committee and delegate
to the NYSDA House, was inducted as a fellow into the Pierre Fauchard Academy during the NYSDA HOD meeting in May in Uniondale.
The Academy is an international dental honor organization that recognizes current and future leaders of the profession.
District Members Attend NYSDA HOD
Seventh District members generously shared their time and insights at the 2025 NYSDA House of Delegates meeting in May in Uniondale. They joined fellow delegates and colleagues from across the state to address important issues, help shape policy and elect future leaders.

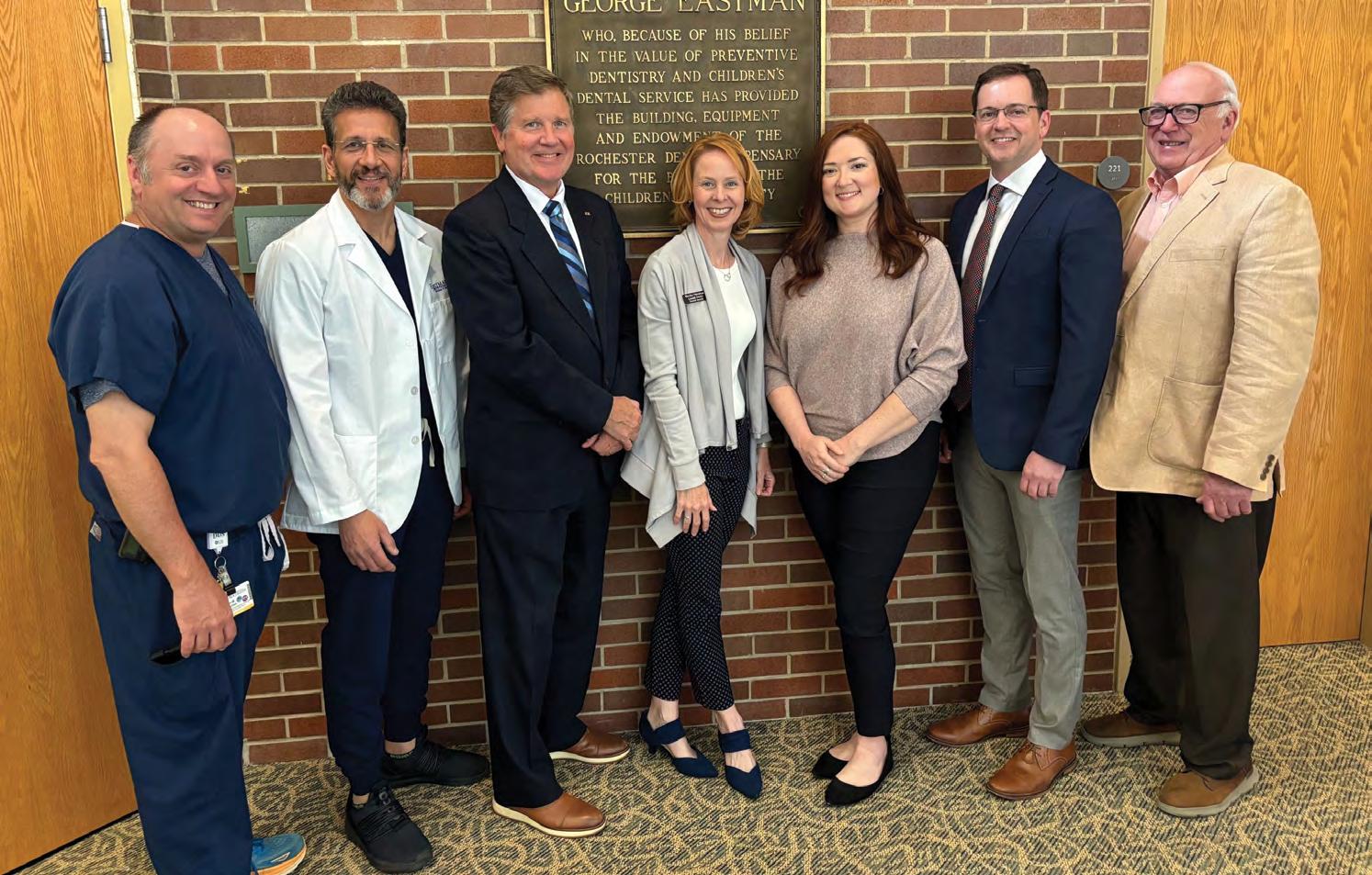
SEVENTH DISTRICT
Program presenters at Eastman Institute for Oral Health include, from left, 7th District Past President and EIOH Medical Director Sean McLaren, District President-Elect and EIOH Director Advanced Education in General Dentistry Alexis Ghanem, ADA Trustee Brendan Dowd. District Executive Director Becky Herman, NYSDA Director Membership Outreach Heather Relation, NYSDA Membership and Communications Chair Christopher Calnon, ADA, NYSDA and District Past President William Calnon.
Seventh District delegates and alternate delegates were prominent presence at Annual Meeting of NYSDA House in May.
Component
Seventh District cont.
Among those recognized at the meeting was Dr. Theresa Casper-Klock, who received a plaque marking her dedicated service as a NYSDA Trustee for the last four years. Dr. David Ramjattansingh was elected to serve as trustee for the next four years.
MCDS Presents Awards to Graduates Dr. Taylor Squires, Monroe County Dental Society President, and Ms. Andrea Hughes, Seventh District Dental Society Communication/Event Manager, participated in the Monroe Community College (MCC) Dental Studies Program Pinning Ceremony. They presented the Dental Hygienist Award to Skylar Lyon, for her hard work, academic excellence and leadership and a Dental Assistant Award to Dominique Fulton, for excellence in patient care. Each received a certificate and monetary award.
Dr. Jay Skolnick, Seventh District Dental Society and MCDS past president and a current MCC Dental Studies Program faculty member, presented the Stevenson Award on behalf of the New York State Dental Foundation.
Tripartite Event for Residents and Residency Program Faculty
Representatives from the American Dental Association, the New York State Dental Association and the Seventh District Dental Society came together to host a special event at the Eastman Institute for Oral Health (EIOH). The nearly 90 people in attendance included residents and residency program faculty, along with EIOH Director and Vice Dean for Oral Health in the School of Medicine and Dentistry Dr. Eli Eliav. They shared ideas, concerns and brainstormed opportunities for
engagement and collaboration in organized dentistry. Tripartite representatives emphasized the importance of organized dentistry and the many benefits of membership.
All enjoyed a catered dinner in the EIOH lobby following presentations and discussion.
Social and Leadership Development Program Planned
Join us Aug. 18 from 6-9:30 p.m. when we launch our new “Spark Connections” Mentorship & Leadership Development Program, designed to bring together new dentists and residents with seasoned dentists to foster the growth of future leaders by providing them with guidance, support and knowledge from our more experienced professionals.
The program will be followed by an all-member social—an evening of great food and drinks, conversation and networking to celebrate summer in Rochester.
Thank you to our sponsors: Bryan Gray, CPA; Empire Dental Administrators; Genesee Regional Bank; Henry Schein; Morganstern DeVoesick; Patterson Dental; RTG Lab; Straumann; Vision Financial Group; and Walsh Duffield.
Register today at https://www.7dds. org/resources-faq-pages/events/allmember-resident-summer-social.
County Hosts Oral Pathology Lecture
The Monroe County Dental Society hosted a dynamic, insightful and humorous lecture, “Lumps & Bumps in the Mouth: Mastering the Fundamentals,” presented by Dr. Samson Ng on May 2 at Comedy at the Carlson. Attendees left with a deeper understanding of oral pathology and what to look for in their patients’ mouths.
Thank you to our generous sponsors: DDSmatch, Empire Dental Administrators, Genesee Regional Bank, Jim Casper & Associates, RTG Lab and Walsh Duffield.




SEVENTH DISTRICT
Dr. Rosemeire Santos-Teachout delivering care on “impactful” mission to Guatemala.
Theresa Casper-Klock, whose term on the NYSDA Board came to close at May meeting, welcomes her successor from 7th District, David Ramjattansingh.



Foundation Spotlights HPV Prevention at Annual Brunch
On Saturday, May 31, Foundation friends and supporters gathered for the Annual Brunch during the NYSDA House of Delegates meeting.
This year’s event spotlighted the dental provider’s role in the prevention of HPV-related cancers. Foundation Trustee Dr. Liz Kapral spoke about some of the work being done to raise awareness about the importance of HPV vaccination in New York State, including the Foundation’s “9 to Thrive” HPV prevention campaign, featuring continuing education for the dental community and an HPV-prevention toolkit.
Oral cancer survivor Mandy Hughes delivered a moving and courageous keynote address that left a lasting impression on everyone in attendance, reminding attendees that behind every statistic is a person, a family and a future worth protecting.
A highlight of the morning was a special surprise tribute to Dr. Maria Maranga, who was honored for her 12 years of dedicated service to the Foundation’s Board of Trustees. In recognition of her leadership and unwavering commitment to veterans’ initiatives both statewide and nationally as chair of the ADA Foundation’s Give Vets a Smile program, Dr. Maranga was presented with an American flag that had been flown over the U.S. Capitol in her honor.
Thanks to the generosity of sponsors, dedicated trustees and supporters, the event raised over $40,000 in vital funds to support the Foundation’s oral health initiatives.
The Foundation will bring the 9 to Thrive: HPV Vaccination for Cancer Prevention course to the Greater New York Dental Meeting on Sunday, November 30, and to Rochester on Friday, February 27, 2026.

BANKING
Bank of America
800-932-2775
800-497-6076
US Bank
888-327-2265

FINANCIAL SERVICES
CareCredit
800-300-3046 (#5)
Altfest Personal Wealth Management
888-525-8337
Best Card
877-739-3952
Laurel Road
855-245-0989
INSURANCE SERVICES
MLMIC
800-683-7769
888-263-2729
888-744-6729
Arthur Gallagher
888-869-3535
Long-term Care
844-355-2596
OTHER
Henry Schein
800-734-5561
Prosites
888-932-3644
www.prosites.com/nysda
Mercedes
866-628-7232
Lands’ End
800-490-6402
UPS
800-636-2377
iCoreExchange
888-810-7706
The Dentists Supply Company
888-253-1223
Volvo
800-550-5658 ada.org/volvo
OnDiem
hub.ondiem.com
Practice Mojo
888-932-3644 practicemojo.com


















FOURTH DISTRICT Congress Features Presentations and Award
The Fourth District hosted its annual Saratoga Dental Congress in early May. We were pleased to have NYSDA President Dr. Maurice Edwards attend our Business Meeting to kick off the event.
Honored at this year’s meeting with the Robert A. Smith Award was Dr. Loren Baim, for her impactful and continuous work in our district and her dedication to the New York State Dental Foundation. Congratulations, Loren. We admire your service and commitment to the dental profession and are honored to count you as a member of the Fourth District.


FOURTH DISTRICT
President Kluth and President-Elect Edmund Wun with Saratoga Dental Congress presenter Dr. Tracey Nguyen.
President Jennifer Kluth, right, congratulates Dr. Loren Baim, this year’s recipient of Robert A. Smith Award.
Saratoga Dental Congress speakers Dr. Tracey Nguyen (“Airway Management”) and Dr. Susan McMahon (“Cosmetic Dentistry”) presented to large audiences. Also well-attended was the Cancer Prevention Summit at the City Center, sponsored by the New York State Dental Foundation.
In Service to the House
Thank you to this year’s 4th District delegates and alternate delegates to the Annual Meeting of the NYSDA House in Uniondale for their time and commitment. They include Drs. Adrienne Korkosz, Fred Wetzel, Michael Breault, John Milza, Jennifer Kluth, Rachel Hargraves, Christina Cocozzo and Edmund Wun.
Hygiene Award
Each year, the Fourth District honors a hygiene student attending Hudson Valley Community College with its Dr. Mark Bauman Scholarship for their leadership, high professional standards and demonstration of patient compassion and care. Congratulations to Audra Arnold, the 2025 scholarship winner.
Golf and Learn
The Fourth District’s annual Golf Tourney and CE is set for Friday, Sept. 19, at Hiland Park Golf Club. A risk management program will be offered in the morning. Call (518) 371-1114 to register.
NEW YORK COUNTY
New Dentists Celebrate Ocho de Mayo
Egidio Farone, D.M.D.
Bank of America held a special event for new dentists May 8 at NYCDS Headquarters. Recognizing the financial challenges faced by dentists early in their careers, Bank of America met with young professionals to provide them with valuable guidance and resources.
Robert Malandruccolo and Jarrett Mathews from Bank of America led an insightful presentation focused on essential banking and financial services tailored specifically to new dentists. Attendees left equipped with practical tools and the confidence to make informed decisions and build a strong foundation for their professional futures.
To add a festive touch, expert mixologist Kevin Falatko crafted a signature cocktail, “Garden Glow,” inspired by Ocho de Mayo (Eighth of May). After the presentation, participants enjoyed a hands-on experience creating their own versions of the drink, wrapping up the evening on a lively and engaging note.
Dental Communities celebrate Asian American and Pacific Islander Heritage Month
Members of the New York County Dental Society, New York State Dental Association, Asian American Dental Society and Ivoclar gathered May 19 to

FOURTH DISTRICT
celebrate Asian American and Pacific Islander Heritage Month. The evening brought together dental professionals eager to connect and enjoy excellent food while honoring the Asian American dental community.
NYCDS President Dr. Vera W.L. Tang delivered an impactful address, in which she highlighted the unique oral health disparities within the Asian American community, especially among older adults. Her remarks inspired thoughtful discussion among attendees. Later, hygienist Carly Zenobi delivered her presentation, “Varnishes for Caries Prevention and Biofilm Focused Care,” explaining how targeted biofilm management can improve both oral and overall health.
The night was filled with camaraderie, learning, and a shared commitment to support one another and advance oral health within the community.
NYCDS President Hosts Advocacy Event
NYCDS President Dr. Vera Tang inspired a group of enthusiastic NYU and Columbia students at the “Classroom to Capitol” advocacy awareness event. The students shared firsthand experiences from recent ADA and NYSDA lobby days, bringing their stories of advocacy and impact to life.
Joining the conversation were Dr. Michael Shreck, District 2 Representative on the ADPAC Committee, and Dr. Tang, who represents the American Academy of Periodontology on the ADPAC Committee. Together, they described the critical role organized dentistry plays in shaping legislation and advancing the future of the profession. The event sparked inspiration and highlighted the power of collective voices in driving meaningful change.
Special Olympics Long Island Region Games
On May 3, volunteers brought healthy smiles to the Special Olympics Long Island Region Games. Athletes received screenings, fluoride varnish and oral hygiene tips. These services are espe-
Fourth District delegates and alternate delegates to Annual Meeting of NYSDA House take break from proceedings for group photo. They are, from left, Drs. Adrienne Korkosz, Fred Wetzel, Michael Breault, John Milza, Jennifer Kluth, Rachel Hargraves, Christina Cocozzo, Edmund Wun.
New York County cont.
cially important because people with intellectual and developmental disabilities (IDD) often have extra challenges maintaining oral health. For many, limited motor skills, sensitivities and certain medical conditions make daily care harder and raise cavity risk. Regular fluoride use through toothpaste, water or professional treatments is especially important for them.
With misinformation about fluoride spreading, confusion is growing. Some caretakers refused fluoride for their athletes, worried about possible side effects. Past President Mina Kim notes, “It’s important to educate patients about fluoride’s benefits, since reducing access will cause the most harm to children, low-income families and people with disabilities.”
2025 House of Delegates
NYCDS past president Maurice Edwards was installed as president of the New York State Dental Association during the Annual Meeting of the NYSDA House of Delegates in May in Uniondale. His election to the post speaks to his longstanding dedication to organized dentistry and his continued leadership within the profession.
Following his installation, Dr. Edwards delivered a powerful speech that reinforced his commitment to the mission of the Association and genuine belief in the strength of its members. Dr. Edwards’s vision for NYSDA and NYCDS centers on renewed collaboration and shared purpose. He believes that by learning from our challenges, we can become stronger and more connected than ever before.
We look forward to witnessing the positive impact of his leadership and can’t wait to witness his accomplishments in the year ahead.



NEW YORK COUNTY
Newly installed NYSDA President Maurice Edwards (front row, center) with members of NYCDS delegation at House of Delegates Annual Meeting in May.
Asian American Dental Society President Janet Youn and NYCDS Past President Mina Kim, at left, with hygienist Carly Zenobi and NYCDS President Vera W.L. Tang, presenters at event marking Asian American and Pacific Islander Heritage Month.
Bank of America representatives Jarrett Mathews and Robert Malandruccolo, at left, with new dentists, from left, Jacqueline Katz, Jessie Reisig, Yassmin Parsaei, Lauren Lubowitz following May 8th financial presentation.

Meeting Dates:
November 28th – December 3rd
Exhibit Dates:
November 30th – December 3rd
JACOB K. JAVITS CONVENTION CENTER 11th Ave Between 34th & 39th Street
The only major dental meeting with no preregistration fee returns this year. The Greater New York Dental Meeting (GNYDM) has big plans in store, featuring some of the most highly regarded educators in the field of dentistry. Choose from full-day seminars, halfday seminars and hands-on workshops. But that’s not all. In 2025, GNYDM will also offer attendees access to the World Implant Expo, Annual Global Orthodontic Conference, 3D Printing Conference, Oral Health Symposium, Pediatric Summit, Women’s Program, Public Health Program, Special Needs Programs, and Dental Laboratory Education. Attend the GNYDM with no registration fee!
Upcoming Continuing Education Schedule
• 7/23 9:30 AM – 1:30 PM Risk Management Course, by MLMIC (InPerson)
• 8/05 9:30 AM – 1:30 PM Basic Life Support/CPR Certification Course (In-Person)
• 9/11 4:00 PM – 7:00 PM The Next Dimension: Cosmetics, Digital Dentistry, CBCT, 3D Printers and More. How Dentists Thrive Today, with Dr. Susan McMahon (In-Person)
• 9/12 9:30 AM – 4:30 PM Veneer Planning and Preparation: Setting up for Successful Cosmetic Enhancement. Workshop with Dr. Susan McMahon (In-Person)
• 9/17 9:30 AM – 4:30 PM Intuitive Endodontics. Workshop with Dr. Anne Koch (In-Person)
• 9/25 6:00 PM – 8:00 PM The Good, the Bad & Compliance: Ignorance of HIPAA Can Mean Massive Penalties, with Dr. Lorne Lavine (Zoom)
• 10/08 9:30 AM – 1:30 PM Infection Control for the Dental Practice, with Dr. Peter Mychajliw (In-Person)
• 10/10 9:30 AM – 4:30 PM Minimally Invasive Posterior Restorations. Workshop with Dr. Amelia Orta (InPerson)
• 10/17 9:30 AM – 12:30 PM Modern Approach to Integrating OAT for Sleep Apnea into Dental Practice, by Dr. Maria Sokolina (In-Person)
• 10/20 9:30 AM – 1:30 PM Basic Life Support/CPR Certification Course (In-Person)
• 10/22 7:00 PM – 9:00 PM OSHAMandated Update for Dentists and Staff; What You Need to Know to Comply with the Law, with Dr. Peter Mychajliw (ZOOM) New courses are added regularly so be sure to visit https://www.nycdentalsociety.org/ for the latest course schedule.
NINTH DISTRICT Revamped Schedule
Now that we are at the end of our spring CE course presentations, we’ve switched gears and incorporated some fun and beneficial events into the schedule. On June 4, the 9th hosted its annual


NEW YORK COUNTY
Advocacy awareness was theme of “Classroom to Capitol” event held to introduce NYU and Columbia dental students to power of the collective voice in driving meaningful change.
GKAS Co-chair Anna Viron, at center, is joined by past president Mina Kim, member Reginald Moncrieff and NYCDS President Dr. Vera Tang, along with dedicated volunteers at Special Olympics Long Island Region Games.
Monica Barrera, D.D.S.
Ninth District cont.
“Frills & Drills Social” celebrating all dentists. It took place at the beautiful St. Andrew’s Golf Club in Hastings-onHudson, where the scenery is almost as good as the hors d’oeuvres.
Less than two weeks later, the 9th hosted its annual “Shredding Day.” Operating from the parking lot of the association’s headquarters, Legal Shred helped members dispose of their files in a HIPAA-compliant manner. This member benefit is greatly appreciated and anticipated by members, who filled every available time slot.
And then there is our “Health is Wealth” summer wellness event, which will again be held at the Hudson River Park in Tarrytown. In this beautiful setting, we welcome members, residents, Touro students and their families to enjoy the amazing cuisine of the Latusion food truck; standing yoga, led by Dr. BJ Mistry; and music along the scenic Hudson River.
Reach Out
Association executives, the Board and Nominating Committee all continue to meet to address issues within the 9th and the profession. We invite members to reach out to us to discuss their concerns. A venue for an exchange of ideas is the September General Meeting, which will take place at Westchester Manor in Hastings-on-Hudson.
Our leaders want to hear from members. Perhaps there’s a committee you wish to join? Talk to us; we’re always interested in adding new people. And, as always, please feel free to reach out to association staff for help, advice or to share your thoughts and concerns, so we can be sure all our members’ needs are met.



NINTH DISTRICT
Casual atmosphere prevailed at Frills & Drills Social in June. Enjoying evening are, from left, Chantal Monegro Tavarez, 9th
President Renuka Bijoor, Lynn and Bill Tepper, Tuoro dental student Raoul Velazquez, Fred Kriegel, dental resident Alexander Constantine.
Frill & Drills, which celebrates all dentists, brought together, from left, Thomas Fuschetto, Amanda Iorio, Lindsey Schiffman, Priyanka Patel.
Catching up at Frills & Drills are, from left, 9th Board member Timothy Leung, President-Elect Bharat Joshi, Gemini MasterPatel, New Dentist Committee Chair Lana Hashim.


























Read, Learn and Earn
Readers of The New York State Dental Journal are invited to earn three (3) home study credits, approved by the New York State Dental Association, by properly answering the following 20 True or False questions, all of which are based on articles that appear in this issue.
When you have completed the questionnaire, return it to the New York State Dental Foundation, along with the appropriate fees: $35/dentists; $25/hygienists. Nonmember fees are: $65/dentists; $45/hygienists. All those who achieve a passing grade of at least 70% will receive verification of completion. Credits will automatically be added to your CE Navigator account.
For a complete listing of online lectures and home study CE courses sponsored by the New York State Dental Association, visit www.nysdentalfoundation.org.
Practicing Dentistry in the Age of Periodontal Risk Management—Page 26-32
1. Detecting periodontal risk factors early may reduce the morbidity of oral and systemic diseases.
q T or q F
2. We live in the age of periodontal risk management.
q T or q F
3. There are no known risk factors associated with periodontal disease.
q T or q F
4. Implant failures among smokers are twice those of nonsmokers.
q T or q F
5. Cannabis does not influence the oral microbiome. q T or q F
q Enclosed is a check for the full amount. Members’ fees are $35/dentists; $25/hygienists. Nonmember fees are $65/dentists; $45 hygienists. (Make checks payable to the New York State Dental Foundation.) Mail to NYSDF, 20 Corporate Woods Boulevard, Suite 602, Albany, NY 12211. Questionnaires must be received within 90 days of Journal publication.
Please charge my: q VISA q MasterCard q American Express
#
NYSDA Member? q yes or q no
Local/State Dental Society
6. Osteoporosis is usually asymptomatic until a fracture occurs.
q T or q F
7. Treatment of gingivitis and periodontitis during pregnancy is not associated with decreased risk of adverse pregnancy outcomes.
q T or q F
8. About two-thirds of patients over the age of 65 have periodontal disease.
q T or q F
9. Calcium chanel blockers may cause gingival hyperplasia.
q T or q F
10. Risk assessment empowers dentists and dental hygienists to identify potential problems early on and provide proactive interventions for cases that are susceptible to disease or disease progressions.
q T or q F
Orofacial Manifestations of Highly Active Antiretroviral Therapy (HAART) and Pre-Exposure Prophylaxis (PrEP)
Page 33-39
1. A range of orofacial side effects has been associated with both highly active antiretroviral therapy (HAART) and pre-exposure prophylaxis (PrEP).
q T or q F
2. Untreated human immunodeficiency virus (HIV) will never lead to acquired immunodeficiency syndrome (AIDS).
q T or q F
3. There is no definitive cure for HIV.
q T or q F
4. PrEP is a broadly applicable preventive measure.
q T or q F
5. HAART and PrEP regimes do not have common medications.
q T or q F
6. Antiretroviral drugs may cause systemic effects, such as reduced bone mineral density and altered kidney and liver function.
q T or q F
7. HARRT-associated oral conditions do not include xerostomia.
q T or q F
8. PrEP users may exhibit chlamydia.
q T or q F
9. Sexually transmitted infections (STI) are of concern among individuals starting PrEP.
q T or q F
10. It is important for the treating dentist to perform a thorough patient assessment, including the patient’s HIV status and current medications (including HAART or PrEP).
q T or q F
To complete the questionnaire online, scan QR code above
Online Rates for 60-day posting of 150 words or less — can include photos/images online: Members: $200. Nonmembers: $300. Corporate/Business Ads: $400. Classifieds will also appear in print during months when Journal is mailed: Jan and July.
FOR SALE
MANHATTAN: Oral Surgery practice at Central Park South. Practice for sale with transition to ownership. Four operatories with windows facing Central Park in exclusive medical condominium building on Central Park South. 20-year-old oral surgery practice with large patient database, complete medical equipment and website. Long-term lease of professional space of approximately 900 square feet. Current oral surgeon retiring. Work in pristine office in prime location. Tremendous growth potential. Contact: nycentralparksouth@gmail.com.
BRONX: Excellent startup practice for sale. General family practice established 17 years ago, conveniently located off main road. Open 4 days/week until 4. 2022 gross collection $399K with 2 operatories and 1 doctor. No advertising done. Digital X-rays, completely paperless with dental software. Growing patient base with room to grow with more days. Excellent opportunity to grow your own practice. To discuss, please call: (347) 661-6638.
BROOKLYN: Central Brooklyn general dental practice for sale. Practice served community for 35 years and features three updated operatories and nearly 2,000 active patients. Recently remodeled, and real estate available for purchase. With minimal advertising, practice draws 20-25 new patients per month and collects $800K annually with nearly $400K in take-home earnings. Doctor open to all transition options and aims to retire within six months offering smooth path for new ownership. Ready to learn more? Contact Headwaters Practice Transitions by email: bailey@headwaterstransition.com. Reference #HNY32625
HUDSON VALLEY AREA: Established for over 40 years, this 2-location oral surgery practice in Hudson Valley area serves 1,380 active patients and brings in 115 limited exams/month with minimal marketing. Ten total operatories. Located just 60 miles from NYC. Ideal expansion opportunity with $1.69M in collections and $230K EBITDA. Real estate available. Contact Kaile Vierstra, Professional Transition Strategies, by email: kaile@professionaltransition.com; or call: (719) 306-8385.
WATERTOWN/THOUSAND ISLANDS: Dental practice for sale in beautiful northern NY. Desirable location approximately 1 hour north of Syracuse in close proximity to Thousand Islands and Canadian border. Modern, well-designed, attractive, standalone building with ample parking. 3,395 square feet. Main floor offers 9 ops with digital X-ray, CBCT, Eaglesoft, Schick Sensors, 3D printing and CEREC. Finished 1,500-square-foot basement includes conference room, laundry/locker room, kitchen and 2 additional offices. Building available for sale or lease. Reputable practice can run 1-2 dentists with gross revenue in excess of $1M annually on 4-day week. Experienced,
highly motivated team of 8 willing to remain after sale. Owner retiring and willing to help with transition. Contact Robert Schonfield, DDS, by phone: (315) 771-4012; or email: rob@docschonfield.com.
NORTHEASTERN NY: Thriving general dental practice near greater Burlington, VT, metro area. 14 operatories, including three hygiene chairs, and serves 4,540 active patients with 45 new patients monthly. Generating $2.7M collections and $507K EBITDA. Ideal for dentists seeking turnkey opportunity. Located in free-standing building with real estate available. Practice combines strong financials with stunning location. Contact Professional Transition Strategies by email: bailey@professionaltransition.com; or call (719) 694-8320. Reference #NY122024.
ASTORIA: Dental practice available for quick sale. Mainly restorative, cosmetic and implant office. Charts also available for sale. One block from N train on 36th Ave. Busy area; new buildings; vibrant town only few minutes to Manhattan, Central Park. Office located off main entrance from street. FFS and some good PPOs (out of network). Referring Ortho, wisdom teeth. Grossing $250K on just few hours per week. Asking $145K. Please call to discuss. Contact Teo by phone: (917) 704-3011; or email: serafindental@aol.com.
MANHATTAN: Midtown dental practice for sale. General practice offers prime ownership opportunity. With four operatories and nearly four decades of service, practice operates 3-4 days/week, serving 570 active patients. Collections $1.2M and EBITDA $330K all on fee-for-service basis. Real estate also available for purchase. Enjoy NYC’s vibrant culture and amenities while owning thriving practice. Contact Professional Transition Strategies: bailey@professionaltransition.com; or call (719) 694-8320. Reference #NY62624.
JEFFERSON COUNTY: Great opportunity. Longestablished, profitable practice is must-see. Located minutes from downtown Watertown. Well-equipped 4-operatory practice sits on busy road, with great curbside appeal. Large private parking lot. Practice fully digital with pano X-ray and utilizes Eaglesoft. Revenue $730K with one FT Hygienist. Doctor only works 3 days/week (20 hours max). Seller refers out all endo, ortho and oral surgery. Practice positioned for growth. Primarily FFS, with 2,000 active patients. 2-story building also for sale with vacant apartments upstairs. Contact Dental Practice Transitions Consultant Michael Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY3385.
ONTARIO COUNTY: Long-established, highly productive practice with 2022 revenue of $1.4M. Nestled in backdrop of beautiful Finger Lakes wine-making country. Fully computerized, fully digital office with 7 well-equipped treatment rooms. Utilizes Dentrix Ascend PMS; Planmeca CBCT and digital impression systems added in recent years. 3,500 active patients and combination of insurance and FFS. Strong hygiene program. Well-trained team available for transition. Contact Dental Practice Transitions Consultant Michael Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY3395.
ONEIDA COUNTY: Bright, immaculate, all-digital, 100% FFS practice with great curb appeal. Highly desirable location and convenient access to highways. $900K+ revenue on 4-day workweek. Seller in practice for 30 years and
committed to aiding in very successful transition. Four wellequipped operatories and Dentrix, all in efficiently designed 1,100-square-foot space. Thriving general practice averages 30+ new patients per month. Contact Transitions Sale Consultant Mike Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY3513.
SENECA COUNTY: Charming practice in heart of Finger Lakes region. 45-minute drive to both Rochester and Syracuse city centers. Digital practice offering 3 equipped ops with 2022 revenue $653K on 3 clinical days/week. Softdent, 2D pano and diode laser. 1,700-square-foot practice offers comprehensive dental care in welcoming environment. Fulltime Hygienist and full administrative staff, all with excellent systems and training in place. 50% FFS. Specialties referred out. Real estate also available. Contact Transition Sales Consultant Michael Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY3572.
WESTERN NEW YORK: Fantastic opportunity to own well-established, thriving practice in beautiful area. Practice growing and has loyal patient base made up of 86% insurance and 14% FFS. Fully digital Pan, sensors, intraoral cameras and paperless charting, all integrated with Eaglesoft. Building with off-street parking and additional rental units also for sale or lease. Outstanding staff and established patient base make wonderful opportunity for new owner’s future. Contact Practice Transition Consultant Brian Whalen at (716) 913-2632; or email: brian.whalen@henryschein. com. #NY3665
CAPITAL REGION: Turnkey opportunity for well-established dental practice located in growing and desirable area conveniently located to downtown Albany, Saratoga and Schenectady, with revenue of $800K. Attractive, efficient 2,505-square-foot space with 5 fully equipped treatment rooms. Standalone building offers excellent visibility on busy two-lane main road and also available for purchase. Digital office using Dentrix with pano X-ray upgradable to 3D. Four dedicated full-time employees and three part-time willing to stay after transition. Doctor refers out most specialties on 39-hour week. Must-see opportunity for any interested buyer looking to acquire successful primarily FFS dental practice. Contact Transition Sales Consultant Michael Damon: (315) 430-9224; or email: mike.damon@henryschein.com. #NY3942
NORTHERN NEW YORK: High-grossing, high-tech 7-op operatory general dentistry practice located in standalone building. Located near Canadian border. Beautiful practice offers great visibility and curb appeal. 3,000-square-foot, 100% digital practice utilizes Eaglesoft with CBCT and CEREC. Highly trained, experienced team of professionals awaits, including 3 full-time Hygienists expected to transition with practice. Open 4 days/week with 3,300 active patients and healthy new patient flow. Doctor willing to stay to assist with transition. Great turnkey opportunity. Contact Transition Sales Consultant Michael Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY3673
OSWEGO: General practice for sale. High-visibility, established practice with convenient access to I-81. Growing community, located less than 10 miles from future Micron SemiConductor plant, which will be one of country’s largest. $1.1M revenue on just 28-hour week. 5 well-equipped
operatories, with recent addition of new hygiene room. 100% digital practice with newly added pano X-ray and iTero scanner. Refers out all specialties. Mix of FFS/PPO. Don’t miss out on this growing practice with seller committed to very successful transition. Schedule visit today. Contact Transition Sales Consultant Michael Damon at (315) 430-9224; or email: mike.damon@henryschein.com #NY4023.
ST. LAWRENCE COUNTY: Well-established, highly profitable, 100% FFS general practice with just 52% overhead. Turnkey. Annual revenue $750K+ on 4-day week. Standalone building with large parking lot located right on main road with excellent visibility. Building also available for sale with approximately 3,000 square feet of dedicated dental space. Room to double practice size based on recent clinic vacancy on other half of building. 4 fully equipped treatment rooms in 100% digital practice with Sirona Pan/Ceph imaging. Refers out some endo and oral surgery. Doctor willing to stay for extended period of time. Contact Transition Sales Consultant Michael Damon at (315) 430-9224; or email: mike.damon@henryschein.com #NY4019.
MONROE COUNTY: Looking for well-established, standalone GP practice with wonderful curb appeal? Here it is. Conveniently located in front of Wegmans Plaza, 1,400-square-foot dental space with commercial renters downstairs available for sale or lease. Located in one of Rochester’s fastest growing suburbs. Digital practice offers four fully equipped treatment rooms and 4-day week with 6 days of hygiene. Primarily PPO with FFS. Motivated seller refers out all specialties. Don’t miss out. Contact Transition Sales Consultant Michael Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY4035
SYRACUSE: Long-established, highly visible general practice in desirable neighborhood. $725K+ revenue practice with great curb appeal and ample parking. 2,100-squarefoot leased space just 10 minutes from downtown. Offers 4 well-equipped treatment rooms with ability to add 5th. 100% digital practice and CAD/CAM. Well-trained, experienced team awaits with strong full-time hygiene program. Mix of FFS/PPO. Refers out most specialties. Very motivated seller seeking retirement. To schedule visit, please contact Mike Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY4142
SYRACUSE AREA: Attractive general practice in desirable, vibrant suburb of Syracuse is primed for growth. Situated on busy main road with ample parking. 15 minutes to downtown Syracuse and one mile to Township 5 where shopping, dining and entertainment options abound. Top-rated school district. 4-op digital practice is a must-see with affordable 2,300-square-foot leased space. Room to expand to 2 more ops. Utilizes Eaglesoft PM with Schick sensors and 100% paperless. Refers out most endo, implants, perio and some extractions. Experienced team of professionals await post-transition. PPO-based practice open just 3.5 days per week. Very motivated seller. For more information please contact Mike Damon at (315) 430-9224; or email: Mike.damon@henryschein.com. #NY4235
ONTARIO COUNTY: Long-established, efficiently designed 1,800-square-foot leased space with 4 fully equipped treatment rooms and plumbed room for addi-
tional 5th room. Located in scenic community described as Gateway to beautiful Finger Lakes Region and just 25 minutes from downtown Rochester. Insurance-based practice. Utilizes Eaglesoft PM software. Refers out all specialties. Averages 15-20 new patients per month with zero marketing. Strong hygiene program with practice positioned for growth. For more information, please contact Practice Transition Consultant Mike Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY4198
NASSAU COUNTY: Modern general practice built out less than five years ago in a standalone building. 5 operatories with plumbing in place for 6th, and equipped with state-of-the-art technology, including an iTero scanner, CBCT imaging, and digital X-rays. Located on highvisibility main road. Practice experiencing rapid growth, making it excellent opportunity for doctor just starting out or seasoned practitioner looking to expand their portfolio. For more information, please contact Practice Transition Consultant Jim Higgins at (914) 496-4856; or email: jim.higgins@henryschein.com. #NY4134
JEFFERSON COUNTY: Well-established, spacious, 3,500-square-foot general practice in beautiful, historic building. 7 equipped treatment rooms with 8th op plumbed. Utilizes Dentrix PM software. FFS/PPO and only in-network with 2 insurances. Strong hygiene program with dedicated team ready to stay after transition. All specialties referred out. $837K revenue and positioned for continued growth. Stunning property also for sale includes 4 fully occupied residential apartment units. Doctor looking to stay for extended period. For more information, please contact Practice Transition Consultant Mike Damon at (315) 430-9224; or email: Mike.damon@henryschein.com. #NY3719
LIVINGSTON COUNTY: Wonderful opportunity to own well-established, thriving GP practice residing in beautiful, historic building with great curb appeal. $1.8M practice located in heart of town center in Western NY. Located less than 1 hour from downtown Rochester. 3,0000-square-foot clinical space offers 5 updated treatment rooms. Additional 1,500-square-foot space upstairs for apartment rental. Building for sale. 100% digital practice utilizing Dentrix software and other technologies. 60% FFS/40% PPO mix. Must see. Schedule visit today. For more information please contact Mike Damon by email: Mike.damon@henryschein. com; or call (315) 430-9224. #NY4251
ONEIDA COUNTY: Excellent opportunity to purchase bustling $1.2M general practice. Located in high-traffic shopping plaza in attractive Utica suburb. Great visibility on main boulevard with ample free parking. 4,500-square-foot space houses 9 fully equipped operatories. Utilizes Dentrix and 100% digital practice with 3D Pan/Ceph. Robust hygiene program and affordable lease. Primarily PPO practice. Contact Practice Transition Consultant Mike Damon at (315) 430-9224; or email: mike.damon@henryschein.com. #NY4269
ONEIDA COUNTY: Wonderful opportunity to own profitable, efficiently run practice with beautiful 2-bedroom apartment upstairs. Located on main road with attractive curb appeal. Attractive standalone building and immaculate 3,200-square-foot space offers 5 well-appointed treatment rooms. 100% FFS, digital office utilizes Dentrix. Open 4
days/week. Refers out most specialties. Building for sale. For more information, please contact Practice Transition Consultant Mike Damon by phone: (315) 430-9224; or email: Mike.damon@henryschein.com. #NY4277.
CHEMUNG COUNTY: Wonderful opportunity to own 100% FFS general practice housed in attractive standalone building. Great visibility on busy main road with ample parking and less than one mile from major interstate. Just 10-minute drive to nearby regional airport. Well-designed 2,500-square-foot space offers 6 fully equipped operatories with modern A-dec equipment in relaxing atmosphere. Digital practice utilizes Eaglesoft PM and CBCT. Well-trained, experienced team of professionals, including 2 full-time hygienists expected to transition with practice. Building available for purchase. For more information, please contact Practice Transition Consultant Mike Damon by phone: (315) 430-9224; or email: mike.damon@henryschein.com. #NY4297
CAPITAL DISTRICT AREA: Wonderful opportunity to own thriving $1.7M general practice. Residing in remodeled brick building with main street visibility and off-street parking, practice located in vibrant college town within 1 hour of Albany. Well-designed 2,800-square-foot space has much to offer. 6 treatment rooms equipped with updated A-dec equipment. 100% digital, 100% paperless practice utilizes latest technologies. 60% FFS/ 40% PPO mix. No Medicaid. Experienced team of professionals expected to stay on after transition. Building for sale too. Contact: Mike Damon, Practice Transition Consultant (315) 430-9224 Mike.damon@henryschein.com.
LIVERPOOL SUBURB: Well-established, highly profitable general practice in desirable suburb of Liverpool lets you hit ground running. 4-op, 1,800-square-foot office located on highly trafficked road with spacious parking lot. 100% digital. Utilizes Dentrix PM software and operates primarily PPO. Approximately $800K revenue generated on 3.5day week with most specialty procedures referred out such as Endo, Extractions, Implants and Ortho. Practice growth awaits. Attractive location less than 7 miles from Micron Technologies, future site of what will be NY’s largest semiconductor plant bringing thousands of new jobs. Don’t miss out on wonderful opportunity to own your own practice. Motivated seller. Contact Mike Damon, Practice Transition Consultant (315) 430-9224 Mike.damon@henryschein.com. #NY4394
BINGHAMTON: General practice with revenue of $558K; 4+ ops and 775 active patients. Located on Susquehanna River, practice has water views from both operatories and above apartment. Open Monday thru Thursday, 9-5; closed last week of every month offering ample opportunity for growth and expansion. Minimal competition. Loyal staff and patients. FFS/PPO; no Medicaid. Bulk of specialty referred out. Extremely low overhead with net profit of $320K in 2024. Recently updated equipment and digital scanner. Real estate also for sale with onsite apartment. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#493344. https://ddsmatch.com/practices/493344
ALBANY: Pediatric practice with revenue of $1.17M, 6+ ops and 2,011 active patients. Nestled in heart of NY’s Capital Region, practice benefits from Albany’s thriving,
family-friendly communities, excellent schools and easy access to major highways, making it convenient for families across Capital District, Hudson Valley, and Western Massachusetts. Hours Monday–Thursday, 8–4; ideal for school schedules and working parents. 94% insurancebased, 6% fee-for-service, strong PPO participation and no Medicaid. 2,630-square-foot modern, kid-friendly space with 6 operatories; room for expansion as current footprint allows for 2+ additional ops. Amazing longterm staff. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#484208. https://ddsmatch.com/practices/484208
UTICA AREA: General practice for sale with revenue of $1M; 4 ops and 2,300 active patients. Highly successful FFS dental practice situated in desirable area of Oneida County offering perfect balance of suburban convenience and regional accessibility. Located near major highways. Practice benefits from steady patient flow. Fully equipped with modern, well-maintained dental equipment in excellent condition. 1,100-square-foot real estate available. Strong community reputation with high-retention rate. Long-term team. All specialty procedures are referred out. Open Mon-Thurs. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#483455 https://ddsmatch.com/practices/483455
BUFFALO: General practice with $375K revenue; 2 ops and 2,360 active patients. Well-established practice is rare opportunity. Practice has served loyal patient base over 70 years. Located on main boulevard, offers high visibility and easy access. Seller, operating since 1995, ensures steady demand with appointments booked 4-5 weeks in advance and stable hygiene schedule. Open 4 days/week. Turnkey practice allows for great work-life balance and growth potential. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#477568. https://ddsmatch.com/practices/477568
ROCHESTER: General practice with $351K revenue; 3 ops and 677 active patients. Established starter practice at current location for 41 years and offers significant growth potential. Loyal patient base with some traveling up to an hour for specialty treatment plans, which are all referred out. Currently open 3 days week; potential to expand hours. 80% insurance and 20% FFS payor mix, with no Medicaid. 1,800-square-foot space is 1,000 square feet of clinical, 800 square feet storage. Excellent condition; recently remodeled in 2024. Digital charts and radiography. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#442477. https://ddsmatch.com/practices/442477
SYRACUSE: General practice for sale with $857K revenue, 4 ops and 1,234 active patients. Rare opportunity to acquire well-established general practice in desirable northwest suburb. Located in growing area with charming downtown, practice benefits from excellent school district and low competition. Loyal staff and primarily FFS patients, generating revenue on 3.5 days per week and 10 weeks of vacation. Accepts only one insurance plan, accounting for 30% of revenue. Beautiful stone construction real estate also for sale. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#403119.https://ddsmatch.com/practices/403119
NORTH BUFFALO: General practice for sale with revenue of $1M; 8 ops and 3,970 active patients. Pristine, well-run general practice with significant growth potential. Practice features equipment, including chairs, cabinets, digital pan and sensors, installed in 2017, and Eaglesoft. Associaterun practice; new ownership can achieve immediate results. All specialty work referred out. Assignable lease expiring in 2030. Open Mon -Thurs, 8-5; Friday, 8-1, attracting 60 to 65 new patients monthly. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#399535. https://ddsmatch. com/practices/399535
SCARSDALE: Multi-specialty practice with revenue of $1.5M; 5 ops and 900 active patients. Rare chance to own well-established, 100% FFS multi-specialty practice in heart of Westchester. Services include family, cosmetic, perio, endo, pedo and non-complex oral surgery. Practice runs efficiently with seller working just 3 days/week and contracted specialists on set schedule. Averaging 20 new patients/month. Spa-like, 2,500-square-foot space with calming atmosphere and ample parking. Loyal, skilled staff willing to stay post-sale. Tech-driven with Softdent PMS and modern equipment. Weekend emergency service potential. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#361773. https://ddsmatch.com/practices/361773
LAKE CHAMPLAIN: General practice with revenue of $945K; 10 ops and 5,311 active patients. Opportunity to own thriving 4,000-square-foot, 10-op dental practice on shores of Lake Champlain. Serving community for 38 years with room for 2–3 providers and strong hygiene program, including 2 full time and 1 part time. Real estate also available. First floor of medical building with lake views. Located in college town near Montreal, Burlington and Lake Placid. High patient demand. All specialties referred out. Open Mon-Thu, 8–5. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#319431. https://ddsmatch.com/practices/319431
ALBANY: Expedited sale. General practice; $2M revenue; 6 ops and 1,750 active patients. Asking $1.15M; real estate separate. Rare opportunity to acquire highly productive, 40-year-established practice in Northeastern Albany. Beautifully maintained, tech-forward office features Cone Beam, CAD/CAM, laser, Seiler microscope, 3D printer, RAYFace scanner and Eaglesoft PMS. Housed in 2,700-square-foot standalone building also for sale. Lab, private office, staff lounge and more. 100% FFS while accepting PPOs (not in-network). Turnkey, modern practice with exceptional care standards and growth potential. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#319294. https://ddsmatch.com/practices/319294
NORTHERN NY: General practice with $501K revenue, 4 ops and 700 active patients. Located near Canadian border in scenic, rural area known for outdoor recreation, practice close to five colleges and excellent schools. Seller specializes in mini dental implants and full-mouth reconstruction. 20 new patients/month. 2,084-square-foot office was renovated in 2022; sits on 0.5 acres and may be available. Equipped with Dentrix, Dexis, Cone Beam, digital pan and radiography. Open Mon–Thurs, 8-4. All special-
ties referred out; growth potential. Practice is 90% FFS; seller pays $2,500 monthly rent. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#308057 https://ddsmatch. com/practices/308057
ITHACA: General practice with $1.7M revenue; 6 ops and 4,432 active patients. Expedited sale under $1M. Located on Cayuga Lake in Finger Lakes region. Thriving practice sits in vibrant Ivy League college town. Established in 2001, generated $1.66M in 2024, with associate who is staying post-sale and 11 weeks of seller vacation. 2,400-squarefoot leased space at $5,031/month. Lab, private office and more. Equipped with Cone Beam, Cerec and fully digital PMS. Excellent condition throughout. Payer mix: 80% insurance, 20% FFS. Open Mon-Fri, 8–5. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#308038. https://ddsmatch.com/practices/308038
UPSTATE: General practice for sale with revenue of $1.7M; 5 ops and 4,141 active patients. Rare opportunity to acquire well-established, tech-driven practice in heart of Upstate NY known for outdoor lifestyle. Loyal staff and patient base, with minimal local competition. Five ops with expansion potential. Perio, OS and Ortho referred out offering strong growth opportunities. 2024 revenue of $1.7M with 60% overhead. All digital Eaglesoft, charts, pan, radiography. Open Mon–Thurs 8-5, Friday 8:30–1. Insurance and FFS mix; limited Medicaid. Seller open to DSO or private transition. 2-story real estate with ample parking also available. Adjusted rent $4,500. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ ddsmatch.com. Ref#295892 https://ddsmatch.com/ practices/295892
LAKE GEORGE: General practice $1M+ revenue; 4 ops and 4,500 active patients. Well-maintained general dental practice just 10 minutes from Lake George in charming town. Surrounded by outdoor recreation, practice draws patients from up to 100 miles away and averages 45 new patients/month. 2,170-square-foot office includes adjacent, fully renovated apartment included in RE purchase. Most specialties referred out; no current marketing or online presence. 30% FFS, 70% insurance. Uses Dentrix and Dexis sensors. All new computer system. Loyal staff will stay. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#292028 https://ddsmatch.com/practices/292028
SOUTHERN TIER: General practice with $1.8M revenue; 6 ops and 1,703 active patients. Established in 1964 and acquired by current owner in 1988, thriving 100% FFS practice located in NY’s scenic Finger Lakes and Wine Country region. Renowned for outdoor recreation, wineries and charm. Averaging 56 new patients/month, features loyal patient base, skilled staff and strong growth. Top dental sleep practice in region, with referrals from four hospitals and OMFS visiting monthly. Seller open to private sale or partnership and willing to assist transition. 5,157-square-foot building also available with expansion potential. Contact Justin Baumann, DDSmatch, by phone: (716) 266-9707; or email: jbaumann@ddsmatch.com. Ref#274575 https://ddsmatch.com/practices/274575
FOR RENT
DOWNTOWN BROOKLYN: Dental space available to rent in downtown Brooklyn office building. Landlord will buildout basic construction with tenant responsible for plumbing, dental equipment, etc. Long-term leases available. Please contact to discuss options. Call Joe Schachter at (646) 529-3632; or email: joe@courtmgmt.com.
DOWNTOWN BROOKLYN HEIGHTS: Modern, turnkey dental office available for rent. Walk in and start practicing. Downtown Brooklyn Heights with views of lower Manhattan. Available now. Fully furnished with 3 ops, A-dec chairs, Nitrous. New server and computers included. Near all trains. Call or text for more information: (347) 712-0778.
BRONX: Prime Morris Park dental/medical space for lease. Currently operated as Pelham Parkway Dental Associates, a 20-year established practice. 5 operatories with potential for 6th with existing plumbing. Space offers reception/ waiting area, wet kitchenette, private office and full unfinished basement. Located near prominent medical campuses of Hutchinson Metro Center, Einstein Medical School and Montefiore Hospital. Morris Park will become main medical hub of the borough, boosted by MTA Metro North Morris Park stop with New Haven line access to Connecticut and Penn Station. Please contact Anthony Mameli, NYS Real Estate Broker, Bronx CRE by phone: (347) 387-9768; or email: anthonym@bronxcre.com.
MIDTOWN MANHATTAN: Newly decorated office with windowed operatory for rent FT/PT. Pelton Crane equipment, massage chair, front desk space available; shared private office, concierge; congenial environment. Best location on 46th Street, between Madison Avenue and 5th Avenue. Please call or email: (212) 371-1999; karenjtj@aol.com.
MANHATTAN: Upper East Side op for rent. Office located at Madison Avenue & 60th Street. Modern, quiet, boutique private practice. Endodontic microscope, 2 digital scanners, materials and instruments available for rent. Inquiries by text: (646) 648-3242; or email: pyondds@gmail.com.
EQUIPMENT FOR SALE
DENTAL OFFICE LIQUIDATION: Entire contents of upscale general dental office for sale. Package consists of thousands of items, many in brand new condition for all specialties at huge discount, including instruments, portable equipment and supplies. Offer only available as bulk purchase. Complete list and photos are available upon request. All items are now warehoused in East Hampton, NY. Arrangement may be made for onsite viewing as well. For more information, contact by email: ddsnow28@aol. com; or call (917) 526-0721 and leave message.
OPPORTUNITIES AVAILABLE
SUFFOLK COUNTY: Southampton. Tooth Ferry Pediatric Dentistry, located in heart of Southampton, seeks warm and caring Pediatric Dentist or general dentist with strong experience treating children. Bright, nautical-themed office thoughtfully designed to help kids feel comfortable while receiving high-quality dental care. With strong presence in community and loyal patient base, practice offers supportive, team-oriented environment dedicated to creating positive dental experiences for every child. Open to both full-time and part-time candidates and offer competitive compensation and benefits package. Please inquire for details. Email: eastendtoothferry315@gmail.com; or call: (347) 891-7263.









New York State Dental Foundation Presents Albert H. Stevenson Award
THE NEW YORK STATE DENTAL FOUNDATION recognizes an outstanding graduating student from each of the dental hygiene schools in the state with the presentation of the Albert H. Stevenson Award. This award is given to a graduating student who displays the leadership qualities and enthusiasm that Dr. Stevenson gave to the field of oral hygiene. Dr. Stevenson proudly communicated the importance of the oral hygiene field and advocated to have dental hygiene recognized as a licensed profession. The dental hygiene profession as it stands today is due, in part, to Dr. Stevenson’s tireless dedication.
The 2025 recipients of the Foundation’s Albert H. Stevenson Award are: Maduri Mathoor, New York City College of Technology; Elisabeth Keeler, Hudson Valley Community College; Sanaa Wade, SUNY Broome; Grace Noto, Monroe Community College; Danielle Harris, Erie Community College; Kate Wright, SUNY Orange; Marjuany Graterol, Hostos Community College; Janet Duffy, State University of New York at Farmingdale; and Noelle Gerace, NYU College of Dentistry.
Kate Wright
Elisabeth Keeler
Danielle Harris
Janet Duffy
Maduri Mathoor
Marjuany Graterol and presenter, Dr. Amarilis Jacobo
Grace Noto
Noelle Gerace and presenter, Dr. Egidio FaroneSanaa Wade and presenter, Dr. Payam Goudarzi