
t h e h I e d a


t h e h I e d a
F o r a l l h e a l t h I n e d u c a t I o n P r o F e s s I o n a l s

Lee is the Director of HIEDA and has extensive experience in pastoral care Until 2022 he was the Headmaster and CEO at Taunton School in Somerset and prior to this he was the School’s Deputy Head which involved leading the pastoral team and being the Designated Safeguarding Lead Outstanding support for student and staff wellbeing has always been at the heart of his approach and the School was shortlisted for a TES Award for excellence in this area
Lee always worked closely with the School’s medical team which provided excellent support to the community, particularly during the COVID pandemic He is excited to be supporting HIEDA members in delivering the highest quality of care in their own environments
It is a great pleasure to bring to you our first hIeda Journal. curating it has been a very enjoyable experience and it has been a privilege to have been able to work with such outstanding practitioners they have willingly shared their expertise and experiences which I know will be valued by you all
I set out with the objective of compiling a Journal for all health in education professionals and so most of the articles are written by colleagues who have vast experience of leading health centres in educational settings
I very much hope that these articles will provoke reflection on clinical, operational and strategic approaches they may also lead you to thinking about how you might improve your
practice hIeda is very keen to support you should you need advice or cPd
It has been really interesting to see how the authors have approached a subject of their choice they have identified a broad spectrum of interests offering opinions and thoughtprovoking observations I very much hope that there is something for everyone.
health professionals always speak warmly of the community that they serve but it is vital to consider the health professional network as a community in itself In developing this Journal I am aiming to generate a feeling of inclusion this is particularly important for those working on their own or in small teams If we can engender a feeling of belonging and support across
the health in education network then improved service will follow
I very much hope that this Journal will become an integral part of this network allowing members to share concerns, ideas and best practice
I hope that you enjoy reading it

The value of collaboration through communities of practice in international school nursing.
Many nurses take the leap and venture into the world of international school nursing It offers exciting opportunities both personally and professionally I took the leap some 20 years ago, learning over time both the joys and the challenges this environment has to offer one of the most important lessons that remains pertinent to my practice is the benefit of collaboration with other international school nurses
In many countries, school nursing is a specialism, requiring additional training and skills (nMc, 2023a) Many international school nurses come without additional training in public health, and as well as adapting to this new role, in a new country, they are caring for children, young people and their families who are also finding their way in an expat environment
children and young people in international schools have more complex needs, they are exposed to more change, transition and adjustment, increased exposure to different cultures, different languages, bringing increased emotional stress and anxiety (hansson et al, 2011) hansson et al (2011) describe this as ‘context-specific health needs’ For the international school nurse, this requires a different set of skills to meet their needs and provide effective care this includes a greater awareness of cultural diversity, ethical issues, awareness of the impact of transient lifestyles and the phenomenon of third culture kids (hansson et al, 2011) In my own experience, all these aspects resonate with my practice, as much today as they did when I first started working in an international
environment. during this time I have gained a heightened awareness of the impact of globalisation for both students and colleagues and the nuances this brings to our everyday work andrews and Boyle (1999) discuss the need to be ‘culturally competent ’ and ‘contextually meaningful’ in the care we give and this is heightened when working in an international environment, impacting daily nursing practice one way of helping to navigate this is by having a community of Practice (coP) a coP is where “groups of people, who share a concern or a passion for something they do, learn how to do it better as they interact regularly ” (Wenger, 1998) a forum where international school nurses, who sit outside the organised compounds of the local/ national health systems are able to regularly meet to support each other and share good practice
creating safe environments where nurses can build these open relationships and learn together is invaluable, particularly for international school nurses who often work in isolation For many this is the first time they have practised independently, working as an autonomous practitioner having a like-minded community that shares the same experiences is one way of bridging this gap of isolation Being part of a coP gives the opportunity to foster positive relationships with other international school nurses, provides a common support network where practice can be explored thus providing and enabling opportunities for continuing professional development (cPd), reflective practice, clinical supervision, safeguarding practice and sharing and pooling of resources.

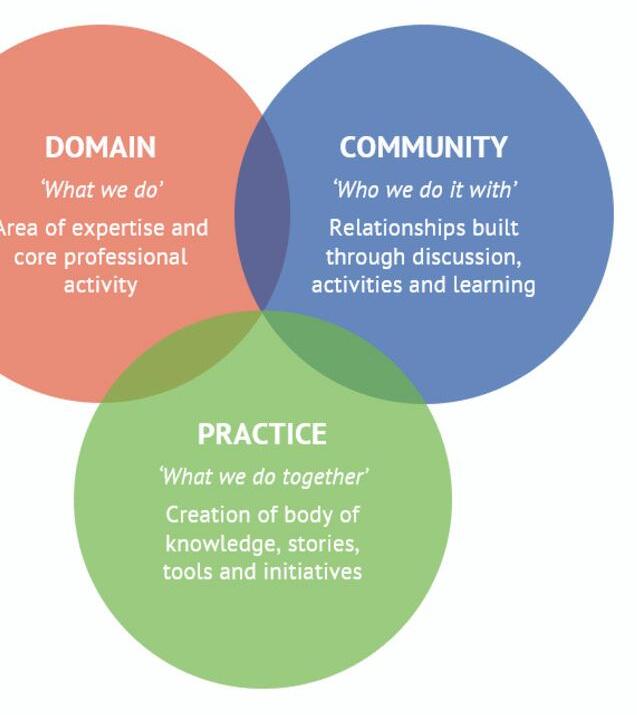
It is the strategic structure of having a defined coP that moves common support systems from ad hoc, take it or leave it, to purposeful, accessible networks that ultimately contribute positively to best practice a coP is not an abstract conception, rather it is quantifiable It can consist of in-person or virtual networking, contact and support via emails and/ or social media platforms for communication and varied accessibility to meet individual needs which are all part of today ’s professional toolkit in an organised and structured manner.
Oa coP is not a new concept, however, revisiting the approach provides a scaffold on which international school nurses can ensure their practice continues to be safe, effective and contemporary effective communication and collaboration are fundamental to nursing (nMc, 2023b), for many it facilitates required cPd and/ or professional registration needs It creates a cohesive learning environment, where international school nurses are able to take responsibility for their own professional learning and practice, leading to a greater sense of professional identity (heemsker et al, 2021) Being part of a like-minded group also builds one’s own self identity, increasing self worth through shared values and beliefs this connection with colleagues, building a network of familiar faces, is invaluable for self care, mental health and wellbeing as with any practice, it requires willingness and commitment from its members and a shared responsibility to make the coP a functioning and useful environment (ranmuthuglalaet al, 2011) With the ultimate aim of providing children, young people and their families with the best possible level of care, focusing on how we effectively collaborate within our practice, our individual contribution within the wider domain is vital to the continued development and progress of international school nursing
andrews, M M , and Boyle, J s (1999) transcultural concepts in nursing care Philadelphia: lippincott, Williams and Williams
hansson, a , clausson, e , and Janlöv, a (2012) International school children’s health needs: school nurses’ Views in europe the Journal of school nursing 28(2) 144-152
heemskerk, W M , dauphin, s l M , van dorst, M a , Bussmaker, M , Wallner, c (2021) a learning community within nursing practice: the value created by the activities and interactions during the early stage of community development nurse education in practice Vol 57, nov
nMc (2023a) standards of proficiency for specialist community public health nurses (scPhn) available at: https://www nmc org uk/standards/stan dards-for-post-registration/standardsof-proficiency-for-specialist-communitypublic-health-nurses2/ 11/11/23
nMc (2023b) the code available at: https://www nmc org uk/standards/code /read-the-code-online/ 11/11/23
ranmuthugala, G , Plumb, J J , cunningham, F c et al (2011) how and why are communities of practice established in the healthcare sector? a systematic review of the literature BMc health services research, 11,273
university of oxford (2023) communities of practice available at: https://pod.admin.ox.ac.uk/communitie s-of-practice 11/11/23
Wenger, e (1998) communities of Practice learning, Meaning, and Identity cambridge university Press

“During this time I have gained a heightened awareness of the impact of globalisation for both students and colleagues and the nuances this brings to our everyday work.”

 ROSIE MACMANUS
ROSIE MACMANUS
The importance of clinical supervision has long been recognised in several fields acknowledging that the best patient outcomes arise from having staff who feel supported and valued although the concept of clinical supervision was first seen in the fields of psychotherapy and the counselling services it became practice in nursing in the late 1980s and its importance has gradually become recognised
clinical supervision is now explicitly discussed by cQc, nMc, GMc and the rcn as a recognised tool for increasing patient and staff safety however, it is not mandated and access to supervision is often limited or fluctuating
Within the education sector, supervision is commonly used for safeguarding leads and their deputies, but rarely accessed by the nursing team there are, of course, several reasons for this time is often top of the list for barriers to accessing clinical supervision, alongside budgetary constraints and nurses not knowing how to access appropriate supervision. however, given the positive benefits derived from clinical supervision, such as stress reduction, greater staff retention and safer practice, there is a strong argument for making clinical supervision mandatory for all health care professionals
clinical supervision for the school health care team should follow the same principles as supervision for the safeguarding team. It should be independent of the workplace, and not led by the employee’s line manager – although the employer may fund this service It should not form part of an annual appraisal but should be an independent process offered at regular intervals throughout the year,
either individually or in group sessions staff should be given time to attend these sessions away from the workplace and most importantly it should be confidential this last point can often cause some concern for line managers Whilst there are times that this confidentiality might be broken, it is important that the clinical supervision session is a safe space for the supervisee to talk freely through elements of their practice clinical supervision sessions can also be used as part of the revalidation process
the process of clinical supervision starts with an individualised contract between the supervisor and the supervisee the contract will detail a number of housekeeping matters such as:
• how often supervision will take place;
• When and where;
• the format the supervision will follow;
• What will be documented and how it will be kept;
• confidentiality and when it can be broken;
• a review date;
• how the supervisee should prepare for the session
clinical supervision sessions are typically guided by a model and there are a number of these available examples include Proctor ’s three-function model and models that focus on restorative and resilience-based processes a supervisor will generally choose their preferred model, and in discussion with the supervisee, agree that this will form the structure of the session It is important to ensure that the model suits the needs of the supervisee and should be changed if it does not
remember, clinical supervision is not a time to shoehorn the supervisee into something that is not appropriate for them as this is their time to work through issues that are relevant to them –they must be able to easily access the process a supervisor may choose to use different models for individual and group sessions
clinical supervision has a foundation in reflective practice through reflection, nurses can review their positive and negative experiences and assess how and why they occurred, how they impacted the individual and how practice can be improved if necessary the nMc highlights the benefits of reflective practice, again observing that individuals are supported in a multidisciplinary environment this enables practice and service improvements which ultimately leads to reassurance for service users that health care professionals are continuously learning and improving care
a popular model of reflection is Gibbs reflective cycle this model provides six pages for the supervisee to work through, logically encouraging the supervisee to explore their feelings around the issue being discussed It provides a framework to analyse the situation leading to the development of an action plan, positively driving practice forward
the role of the supervisor is to coach the supervisee through this process by offering non-judgemental guidance at each stage there will, of course, be time for the supervisee to check correct practice and procedure with the supervisor but, ultimately, the supervisor is the vehicle and the supervisee is the driver on the road to improved practice
the provision of clinical supervision ensures that employers are meeting their duty of care to the wellbeing of all staff and it is closely linked to increased patient safety, higher levels of job satisfaction and retention ensuring that employees not only feel valued and supported but are able to offer the highest level of clinical care to service users this leads to the best outcomes for the pupils in their care

 ALEX GILLEY - LEAD NURSE, RADLEY COLLEGE
ALEX GILLEY - LEAD NURSE, RADLEY COLLEGE
The pitch-side nurse in schools; the role, the ethos, the evolution.
The RCN talk of school nurses delivering both universal and targeted services while working across education and health In my eleven years of being a lead nurse in a boarding school, the changes I have seen in school nursing are vast; the role used to be viewed as one that was centred around a stereotypical caricature of a nurse who puts a plaster on a knee, or gives a paracetamol for a headache with a pat on the head; both scenarios were put to me when I said I was leaving acute medicine to become a lead nurse in a school, along with “you will be so bored”
Far from it! a steep learning curve of injury management, concussion recognition and a plethora of childhood illnesses, not to mention the ever evolving childhood immunisation programme and rise in mental health concerns all of this said, I don’t think any role in the team has developed as much, or as publicly, as the role of the pitch-side nurse I am approached frequently about this position by other schools who want to know the answers to a number of questions including: what is the job description? how does it work? What does that nurse do when they are not pitch-side? My predecessor had the extraordinary vision, along with an emergency nurse practitioner who was already in a nursing role in the school health centre, to create a role for a “First aid and sports health coordinator ” (Fashc) over the years there have been many conversations about the ambiguity of the title, which doesn’t really recognise the clinical aspect of the role, but we still haven’t settled on a suitable alternative the Fashc would provide continuity at the pitches, being pitch-side for every rugby match alongside a GP, and attending all rugby training sessions

In its infancy, the role gave continuity at the pitches, but also support to the GPs in attendance as an emergency nurse practitioner (enP), advanced training in injury assessment and radiology requesting (IrMer) training had been undertaken in a&e this meant that an x-ray could be ordered by the Fashc at the school health centre when the pupil was injured, saving a lot of time in the local minor injuries unit
the extended a&e training, along with specific pitch-side training, also meant that the Fashc was able to carry out an annual update with all the GPs and sport coaches covering neck injuries and immobilisation of fractures this swiftly developed into the Fashc becoming a first aid trainer for the entire school this added a further layer of trust between the coaches and pitch-side nurse, along with better integration of the health centre with the wider school community
In addition to rugby, football and hockey were soon recognised as sports that carried significant injury risk, so the Fashc started attending all football and
hockey matches over the years, the role has also developed away from the pitches there is a lot more administration and liaising with physiotherapists, the rehab team and coaches, along with external sporting teams and academies this is all in conjunction with reviewing pupils who are injured, updating and managing the “off games” list, managing pupil, parental and coaches expectations along with supporting the wider health centre team in their injury assessment and management It has become a significant role, carrying enormous expectation while performing a large part of the role in full view of the spectators at the pitches; high pressure in every way
around four years ago, the GPs felt that they needed to step away from the pitch-side role their indemnity insurance was increasing hugely and there were fewer GP’s feeling comfortable in the role, despite the presence of the Fashc after a review of the pitch-side service, it was decided that the GP would be replaced by a specialist/advanced skills paramedic along with an additional paramedic this third clinician was added due to the increase in the number of matches that were being played in any given block fixture.
It was felt that paramedics possess the emergent care skills that sport related injuries require including the ability to immobilise, to manage multiple patients, to triage and to act within the scope of a professional practice



Given the connection we still had with a&e we were fortunate enough to already have good working relationships with some paramedics, two of whom became members of our pitchside team this added a new dynamic to the Fashc role she was now coordinating external clinicians, ensuring they were aware of our school policies and procedures, and it was mutually beneficial as this also gave the opportunity to learn from the paramedics and develop further confidence in primary care outside of the clinical setting
In the last six months our school has employed a sports therapist to oversee the rehabilitation of pupils the role is managed jointly by our director of sport and the First aid and sports health coordinator due to the clinical nature of the role While this expands the job description of the role, it also further demonstrates the pivotal nature of the Fashc in the management of injured pupils
everything in life can, will and must move forward the role has developed and progressed so much but the constant remains the positive impact of the presence of the First aid and sports health coordinator at the pitches this positive impact is felt by staff, by pupils, by parents and by all in the health centre the continuity of good clinical care, of compassion and of commitment is so important and key to the success of the role

 VICKY PIEKARZ - NHS GP Practice Business Manager, CQC Specialist Advisor, Healthcare Advisor to Independent Schools
VICKY PIEKARZ - NHS GP Practice Business Manager, CQC Specialist Advisor, Healthcare Advisor to Independent Schools
Vicky qualified as a Physiotherapist in 2003, but transitioned into management in 2009, gaining a wide range of leadership and healthcare management experience within the military, NHS, private healthcare, and boarding education sector From previous roles as a specialist advisor for the CQC inspecting Primary care settings, she has a strong background in providing consultancy and mentoring for individuals and teams looking to enhance or assure the quality of their healthcare provision She is passionate about how the governance can underpin the consistency behind safe and effective care, but balanced alongside a keen interest in team-working psychology, which truly underpins the actions of healthy and supportive team environments to influence change
The challenges and barriers in maintaining quality in school healthcare.
For all healthcare professions working within a school environment, it can be a lonely and strange world Most find their way into the sector coming from large hospitals, GP practices, community care and the social care sector, all heavily immersed in a world where colleagues and other departments speak the same “healthcare language” and with an innate understanding of the highs and lows this comes alongside the governance elements of service improvement primarily coming from a ‘top down’ approach to keep nudging everyone in the right direction of travel Whereas in schools and the boarding sector, step outside the doors of the treatment room, and the language and chatter is primarily “teaching” so how do we fit in, what are the challenges, what are the risks and what makes healthcare in education, and boarding, vulnerable?
In this article, I share my observations and reflections from a journey into the education sector and a story that seemed to resonate with many others that I have met My aim is to bring transparency to a hidden world, to bring reassurance to some that their experiences are not unusual, or perhaps create an article that drives chatter toward future change
Firstly, we must consider the notable impact of the regulatory standards in the education sector which really opens up healthcare teams to the greatest risk Within the education sector, an oFsted or IsI inspection will assess medical support under the larger pastoral and welfare umbrella, but by no means does this allow the inspectorate a full and comprehensive deep-dive into the weeds of how good quality healthcare is upheld, nor a level of understanding in comparison to the rigour of healthcare specific inspections
the care Quality commission (cQc), who regulate, monitor, and inspect all health and social care providers in england (care homes, hospitals, private clinics, dentists, home based care, community GP services, mental health services, hospices, ambulance services – the list goes on), however, omits healthcare sites in schools unless there are special educational needs one could argue that without a cQc type regulatory deep-dive and analysis of all the safety processes, care pathways, governance, and staff knowledge, it is very difficult to quantify or assure how safe, effective, responsive, caring, or well-led the healthcare delivery in schools actually is this is especially the case when caring for young people who probably have very little exposure to benchmark what may be considered effective or safe medical care basics It could also be argued that with the increasing and evolving healthcare needs of children and young people of today, the level of risk that medical teams are exposed to is also slowly growing
the core responsibility og providing high quality medical outputs falls primarily on the individual medical professionals working within a school environment For the regulated professions (GPs, nurses, Physios, Psychologists, Paramedics) the concept is that they work to adhere to their own regulatory body standards which should create an innate awareness and ingrained individual duty to comply and be vigilant towards ethical ‘codes of conduct ’ or ‘Professional standards of Practice’ that duty, however, still lies with the individual to recognise, reason, and rightly report if there are breaches in those standards
to add a further level of complexity, not all healthcare professions are regulated by law, meaning that their professional title is also not protected For roles such as healthcare assistants, sports therapists, and counsellors, it is optional to choose to affiliate themselves with an accredited body recognised by the Professional standards authority if that is, their level of training meets the registration criteria therefore, without sufficient supervision there could be a dilution of the desire to recognise and report breakdowns in care quality other factors that conversely constrain a healthcare professional in reporting breaches in standards also need to be openly recognised often these individuals are working alone and behind closed doors so reporting issues takes courage a strong psychologically safe team culture, where reported issues are welcomed as learning opportunities and not seen as a sign of inferior practice, is vital this can often be very difficult if the direct team manager is not a medical profession themselves, perhaps with a differing level of reactive response to the significance of a scenario, either by under-response (dismissal) or heightened response (panic) the manager may have different boundaries on what is deemed a risk and not hold the vision or solution to fine-tune healthcare improvements
Within a traditional hierarchical education environment, sometimes the medical teams are not empowered to sufficiently steer the direction to a solution, nor have the time for new projects although the issue may be discussed within the teams, the problem continues if there is no determination to take accountability and drive the solution there is therefore a danger that future team appetite to report subsequent, or enduring, risk events in a continual improvement cycle is slowly quashed. In time, this can result in a demotivated team, a negative and destructive blame-culture and any evolution is blocked
the relationships between school medical team staff working alongside each other, often in very small teams, makes speaking up to report care quality issues intrinsically challenging those working in healthcare are primarily ‘caring’ individuals, constantly trying to do their best for others, so creating conflict or unrest is not a default cognitive response rather than speak up, the risk is to continue to do what has always been done, working with a cognitive dissonance to keep the peace, or avoiding creating extra work for the team to address
In the larger healthcare sectors where communication teams continually disseminate clinical reminders, updates, new awareness campaigns and changes to practice, the school sector healthcare teams are distant to this and hence it poses a risk that it becomes normal to unquestionably do what has always been done
despite the lack of cQc interrogation, all healthcare sites in an education setting should do all they can to uphold the high standards of clinical governance maintained in any healthcare site this includes holding clear documented evidence of policies, care pathway, and standards to which all staff must adhere evidence of audits, surveys or quality review projects to evidence a continual review of outcomes must be retained capturing issues, errors, complaints and risks should be a natural process as should the review of this documentation evidence of ongoing staff education, peerreview, reflection, and appraisal should be available In small teams, especially if working alone, it is important that these standards do not slip and a high focus is placed on maintaining them.
the ‘dry administrative’ clinical governance churn, however, does not sit high on the ‘exciting’ list for many that went into a career focused on ‘people-based care’ appraisals are often heavily focused on very specific clinical training or personal cPd objectives for the individual, whereas the bias should probably be weighted towards improving all pillars of team clinical governance to ensure all are engaged in the journey to improving the wider business outputs of quality assurance
the deep-rooted momentum must lie within fostering a wider team culture of psychological safety where the shared values and vision is to be always vigilant and looking to improve quality there cannot be an optional approach to excellence, nor can it be a one-off appraisal objective no healthcare team should ever say they have ‘no issues’ I often observe in healthcare that the ‘daily moans’ or frustrations simply become part of the daily normal whereas they should be seen as sparkling gems crying out for a resolution. these quality improvement observations should always be captured, documented and not forgotten another observation that potentially constrains the resolution is within the ‘language’ used to convey the problem and facilitate the solution those that work in healthcare are ‘people’ people, so relaying a problematic scenario often involves an anecdotal recap of a situation Without diffusing its worth, the language to engage (or convince) hierarchy, managers or governors should focus more sharply on defining the risk, and clear suggested options for resolution the story should be the secondary headline With a clear risk defined, the appropriate prioritisation and time allocated to drive the solution can be defined the remaining question, therefore, focuses on who is leading the solution For historically hierarchical led sectors (both in teaching and healthcare) the model for any quality improvement project has a wealth of momentum when lead from the ‘bottom-up’ rather than relying solely on the one at the top to find the resolution With clear boundaries, the medical teams themselves should be empowered to sufficiently steer their own solutions alongside the appropriate support and guidance to ensure a harmonious outcome for all parties
Finding a clear and obvious mitigation to the risk can also be challenging It is important that there are open channels of communication to engage with differing opinions and ideas solutions and out-the-box thinking can be found from many avenues and not always those from a medical background Whilst the networking chatter may provide a concept solution it could be that putting pen to paper to revise policies, new instructions, flow charts or guidance may suit the strengths of others within the team, favouring those with a more logical, data, process driven mindset By recognising and utilising all of the team members’ strengths, and collaborating to establish the solution the quality improvement cycle continues to evolve and thrive
“Nurturing h gives power an to our pup



I work with staff, students and parents to help educate and support pupils in managing their own physical, emotional and mental wellbeing Ensuring support, guidance, education and access is available to students to learn and develop resilience in life skills related to wellbeing From anxiety management, to nutrition, from sleep, to peer mentoring the role covers a wide dimension With a specialist interest in how fundamental sleep health is, in 2020 I trained as a qualified Sleep Practitioner and began the drive to improve sleep health
My career background lies in the health sector with 20 years as a Physiotherapist I had wonderful years working in elite sport with teams such as Harlequins and the England Women’s Rugby Team, as well as working at Guys and St Thomas’ NHS Trust as Clinical Lead for Musculoskeletal Physiotherapy services I began a clinical lecturing role in Physiotherapy at Kings College London After relocating to Dorset, I started working at Canford School, setting up the physiotherapy service, tutoring in a girls Boarding House and teaching PSHE My passion for educating and empowering people drives my work, underpinning which is a belief in holistic and preventative approaches
The aim for any school should be to ensure that the wellbeing of their pupils is integral to the fabric of their school community, not seen as an adjunct to the pupil’s school journey as head of Wellbeing at canford school I advocate an ‘injury prevention’ mindset rather than one of reaction I feel passionately about empowering our pupils with the knowledge and skills to manage their mental, physical and emotional health so that they feel a sense of security, control and independence, to flourish in all aspects of school life whilst mastering wellbeing skills to carry with them into the real world My belief is that our role as educators stems beyond the academic framework and should incorporate the learning of life skills nurturing human skills gives power and dimension to our pupil body
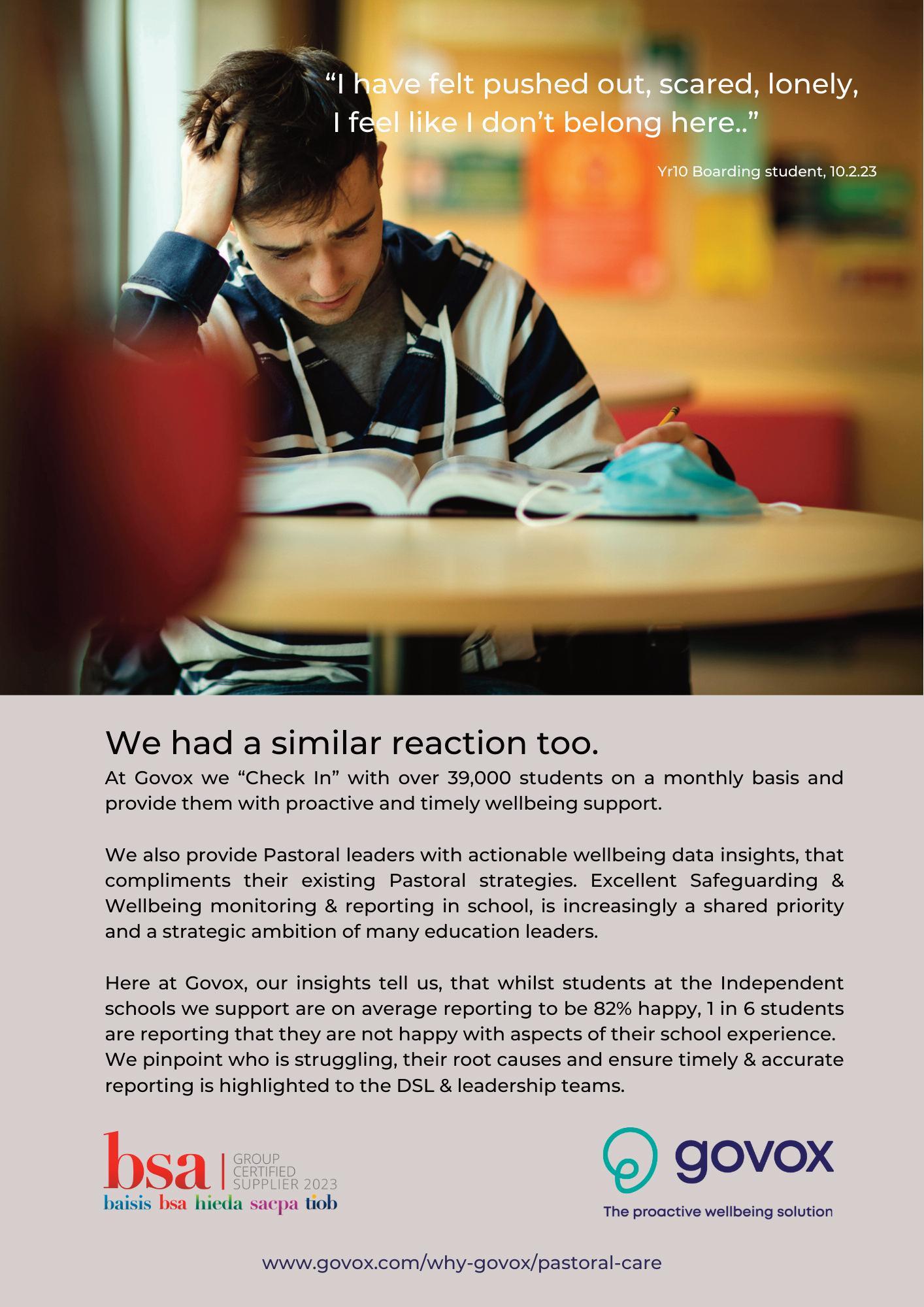
to establish a culture of wellbeing throughout your school community, I would encourage school teams to carry out a deep-dive audit into their wellbeing provision this will help guide where to focus your activity in supporting and promoting wellbeing after completing our school audit, we established the main common themes from pupil, staff, and parent feedback tiredness was one of the top areas of note this did not come as a surprise to me as sleep was an area of health I had already been working on in conjunction with our school counsellor.
We had noticed a trend in those students seeing the school counsellors suffering with mental health problems who were also presenting with extremely poor sleep patterns and sleep health sleep health is so incredibly interlinked with our wellbeing homeostasis our health centre staff had seen an increase in demand from parents for sleep-based medication support such as prescribed Melatonin.
this reflects our society and the systemic culture in being quick to medicate whilst not taking ownership for our behavioral trends or exploring how we can help to manage this aspect of health ourselves Pastoral house staff were encountering more pupils arriving at the school with a history of sleep health issues they were, however, sometimes discovering this when other emotional or behavioral issues came to the forefront
sleep health should be talked about and promoted with the same level of importance as areas such as heart health or bone health our pupils can recite the rainbow of food they should have on their plate or the 10,000 steps they should do in a day to be healthy, but very few know about the depth of sleep health In truly exploring and understanding the benefits of sleep to our physical, emotional and mental health we can see that, fundamentally, sleep underpins all that we do. understanding the complexities and interconnections of school life highlighted how better sleep health supported better outcomes in all areas of a pupil’s school existence some examples relevant for our adolescent pupils include better concentration in the classroom, more patience and tolerance within friendship circles, improved self-esteem and improved mood to name but a few Good sleep health is a superpower that more people should utilise and actively manage more effectively
We embarked on tackling sleep health for our canford community as a key focus to the active promotion of wellbeing as head of Wellbeing, I was mindful of how we can give the most support to the greatest number of pupils and how to go about making the most impact to support my research into sleep health I trained as a sleep Practitioner with the sleep charity I wanted to ensure I

considered the most up to date evidence-based research when building the foundation to my sleep health initiatives the canford school holistic sleep Programme came to fruition to ensure we were supporting pupil wellbeing in all aspects of school life and to provide better communication and support on sleep health throughout the school
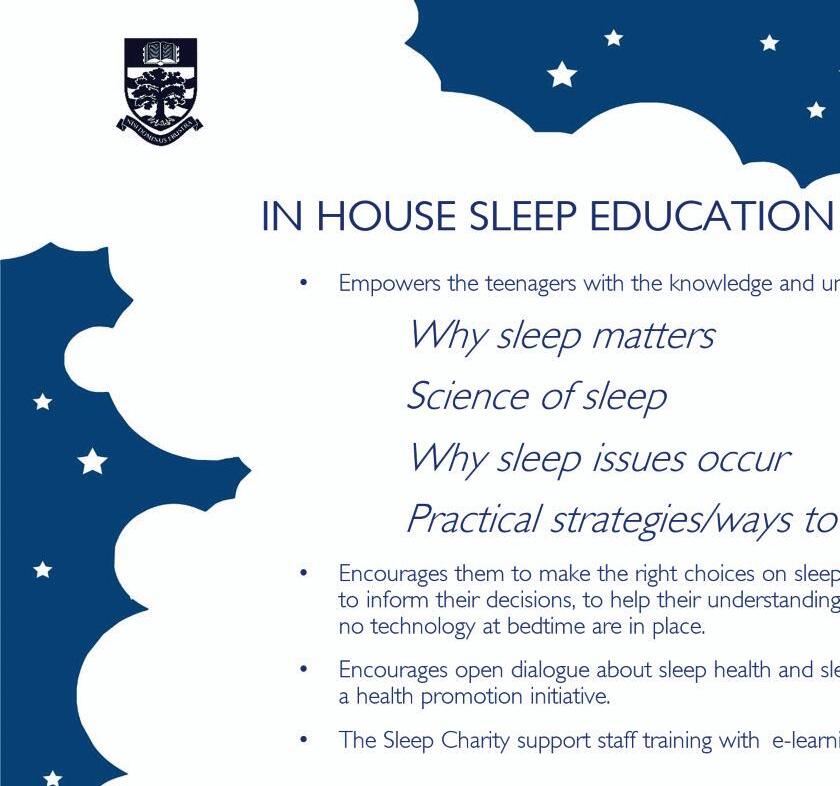
the sleep Programme can be divided into four main areas where changes: pre-medical questionnaire and baseline testing, a transition information leaflet relevant to sleep hygiene for entry level families, sleep champion staff and the In-house sleep education Programme
In the pre-medical questionnaire that goes out to all pupils joining the school, we were already asking for details on physical health information such as teeth, hearing and past medical history We give parents and carers the opportunity to disclose any previous emotional health issues to improve our understanding of the full health picture, we introduced a question on sleep health history, giving people the opportunity to disclose any history of poor sleep health or concerns this information can then be shared with relevant housemasters and housemistresses, with consent, and means that they are on the front foot when keeping an eye on how they settle into busier senior school life It also means that health centre staff have a fuller overall picture of a student ’s health.
the school counsellor can access this information and know if sleep problems are a new aspect of their presentation or if it is a previous issue this is a small change that has made a big difference in supporting individual pupils and raising awareness of how seriously we value sleep health It has even helped housemasters navigate some of the room
allocations to give a better experience to all We are also using the teen sleep Index questionnaire to gain a scoring for sleep health from all of our pupils It gives a baseline score and the aim is to repeat this every half term to gauge patterns in sleep health It can be difficult to quantify wellbeing provision but this tool is one way of analysing improvements in sleep health after intervention from staff
a leaflet based on sleep health was designed as part of the welcome information pack for new students and their families It aims to provide transparency on our sleep hygiene expectations, to share information on phone policies and prevent screen usage before bed to stop stimulation of the brain, whilst also encouraging relaxation and human interactions amongst pupils as part of a structured bedtime routine It gives suggestions on bringing in a teddy or blanket that smells of home, possible use of an eye mask and healthy snack choices for tuck boxes this may seem obvious to those reading this, but it could be valuable to adopt to aid your communication with parents, to help regulate sleep patterns in pupils joining the school and to show that sleep health is valued at the school to reflect our openness about sleep health, and to encourage pupils to talk about it, we trained a sleep champion in every house, either a matron or a tutor It gave pupils a designated member of staff who they knew they could talk to about sleep issues. these staff were supported in their role with an elearning module from the sleep charity as well as in-house training on tools used to support pupils such as sleep diaries It demonstrates the weight we give to wellbeing and active promotion of talking about aspects of health


the In-house sleep education Programme was designed to empower our pupils, through education, to make better and informed choices on managing their sleep health the programme consists of four sessions educating pupils on the importance of sleep health, the science of sleep,
why sleep issues can occur and then practical tools they can use to manage their own sleep health It was made fully relevant to their age for better engagement, showing we support what is important in their lives whilst also teaching them about tools that they could utilise in the future should they encounter changes in their sleep health It is taught in house to make it less formal than the classroom to give a more relaxed environment for them to feel open to asking questions and talking about health It is delivered by a sleep champion and the program is revisited with all year groups so that we can build on their understanding and relevance as they mature this ensures that we get a spiral effect to learning and can embed the understanding more deeply
encouraging open dialogue about sleep health and introducing health and wellbeing initiatives such as this helps reduce risk and prevent the onset of mental, physical and emotional health issues in our pupils at an age where they are open to absorbing information


Sinead’s aim is to improve the health literacy of her pupils and empower them to utilise the variety of health and wellbeing services available to them, should they need She has a passion for health promotion which involves reactively and proactively engaging and educating her pupils and her medical and non-medical colleagues
The role of the school nurse in developing targeted health promotion strategies.
Adolescents are recognised by the department of health (2021) as being a vulnerable demographic who are more likely to suffer from health problems that are mostly considered preventable at a time when young people are experiencing physiological and neurological changes, they have heightened desires to experiment this, coupled with new exposures to alcohol, drugs and sex, can increase potential risk to mental and physical health (World health organisation (Who), 2021a)
additionally, societal influences from friends, family and social media platforms around topics such as body image and sexuality, can also negatively affect young people’s mental health research suggests that poor early health and wellbeing behaviours, such as early sexual initiation and substance use, are not only associated with lower academic achievements but that these experiences can have long-term neurocognitive implications, which can result in behavioural, emotional and social difficulties into adulthood (Who, 2021a)
consequently, Public health england (Phe) (2021a) supports school-based health education programmes to improve adolescents’ health literacy by strengthening attitudes, beliefs, and skills required to maintain lasting healthy lifestyles currently, the Who (2021b) state that a comprehensive approach to adolescent health is often wanting, partly due to a misconception that adolescents are healthy although the healthy child programme outlines evidence-based recommendations to promote and support healthenhancing behaviours for children up to 19 years, there are currently no mandated wellbeing reviews for school-aged children (Phe, 2021a) despite this, schools and school nurses are recognised as being key components in supporting healthy adolescent
development and reducing health risks through the delivery of effective health promotion.
Phe (2021b) suggests that school nurses can identify health and wellbeing needs, support behavioural changes and influence local outcomes by collectively considering current evidence, using professional judgement and listening to the service user voice school nurses are therefore encouraged to use a needs assessment to determine what targeted interventions and information are required
For example, nurses can audit common types of injuries or illnesses that result in pupils visiting the medical centre If there were a great number of pupils attending with head injuries, then it would support a school wide education programme on head injuries, as well as a review of policy and a review of safety procedures around sport for instance a nurse could also send an anonymous questionnaire to their pupils to identify any barriers preventing them from accessing the medical centre or if there are topics that they would like more information on but may not want to attend the medical centre in person For example, if pupils highlight that they are worried about stigma or they are too embarrassed to discuss certain topics the nurses can work on strategies to deliver health information using alternative methods such as signposting credible online resources and advertising external organisations such as MInd and Brook
It would be best practice for school health services to gain regular feedback from pupils and staff to ensure continual positive clinical development In order to engage pupils with school based health interventions, pupils and staff must collaboratively
recognise, react and co-ordinate action therefore, effective health promotion requires strong leadership and communication between the school medical centre, the pastoral leads and senior management teams
In summary, school medical centres should work with pupils and staff to create targeted health promotion strategies in order to engage as many pupils as possible nurses are in a unique position to deliver information in a variety of creative ways that include online, via posters, in classrooms and during consultations By having a comprehensive understanding of adolescent health and recognising the barriers and facilitators of health engagement, nurses can be effective at improving the health literacy of their school pupils
idepartment of health (2021) health visiting and school nursing service delivery model retrieved January 1, 2022, from https://www gov uk/government/publica tions/commissioning-of-public-healthservices-for-children/health-visiting-andschool-nursing-service-delivery-model
Public health england (2021a) healthy child programme 0 to 19: health visitor and school nurse commissioning retrieved May 15, 2022, from https://assets publishing service gov uk/ government/uploads/system/uploads/at tachment data/file/969168/Commissioni ng guide 1.pdf
Public health england (2021b) health visiting and school nursing service delivery model retrieved May 15, 2022, from https://www gov uk/government/publica tions/commissioning-of-public-healthservices-for-children/health-visiting-andschool-nursing-service-delivery-model
World health organisation (2021a)
Adolescent and young adult health Retrieved March 15, 2022, from https://www who int/news-room/factsheets/detail/adolescents-health-risksand-solutions#: :text=Violence%20durin g%20adolescence%20also%20increases %20the%20risks%20of,reproductive%20 health%20problems%2C%20and%20co mmunicable%20and%20noncommunica ble%20diseases
World health organisation (2021b) coming of age: adolescent health retrieved May 15, 2022, from https://www.who.int/newsroom/spotlight/coming-of-ageadolescent-health
 ASHLEY MASON - Paramedic and Health Services Manager at St Peter’s School, York
ASHLEY MASON - Paramedic and Health Services Manager at St Peter’s School, York
The new graduated return to activity and sport (GRAS) guidance.
As far back as 1977 a three week “standdown” from sport was recommended after a concussion over the decades there has been a total transformation in how head injuries in sport are managed approaches designed for professional level sport have translated into everyday practice for grassroots and school sports the rFu’s Graduated return to Play protocol has recently been refreshed to the Graduated return to activity and sport protocol and is the evidence-based way of supporting and managing those with concussion safely back into full contact sport this refresh followed the first uK-wide concussion Guidelines for Grassroots sport, published in april 2023 by the Government and the sport and recreation alliance
this article will focus on the new national guidance and Graduated return to activity and sport (Gras) protocols to help manage concussion in the school setting
W H A T I S C O N C U S S I O N ?
the nhs describe concussion as “the sudden but short-lived loss of mental function that occurs after a blow or other injury to the head It is the most common but least serious type of brain injury ”
W H A T A R E T H E S I G N S ?
the uK concussion Guidelines break down the signs and symptoms into four areas:
• Physical: headaches, dizziness, vision changes;
• Mood: short tempered, sad, emotional;
• Mental processing: not thinking clearly, feeling slowed down;
• sleep: not being able to sleep or sleeping too much
only 10% of people with concussion have a loss of consciousness
C O N C U S S I O N S A S S E S S M E N T T
the new guidelines are supported by three assessment tools the first can be used by nonhealth care professionals, such as teachers and coaches, to make quick, initial decisions on removing players they also highlight red flags and when to call an ambulance the other two tools are for children aged 8-12 years and over 13 and are designed to be used by health professionals they should take place in the first 72 hours and take about 15 minutes to complete
the assessment tool clearly states that it “should not be used by itself to make, or exclude, the diagnosis of concussion” this will be a clinical decision made by the health care Professional taking into account all the circumstances present When assessing a patient and considering concussion, have confidence in yourself and your decision making the concussion Guidelines for Grassroots sport make it clear that even suspected concussion cases should follow the graduated return pathway
It is vital that when discharging a pupil with concussion after initial assessment you explain the red flags to them and their responsible adult. a head injury information sheet should also be provided
the new guidance sets out the two main changes from the old pathway:
1 Importantly this pathway, recognising the value of light physical activity in a player ’s recovery, no longer requires an initial 14-day complete standdown period. a player can start very light physical activity 24-48 hours after their concussion provided that their symptoms are not more than mildly exacerbated after a first week of progressive light exercise, provided symptoms are not more than mildly exacerbated by the activity, the player is able to start non-contact training activities in the second week with resistance training activities also started in this week
2 contact training activities with a predictable risk of head injury can then be introduced in week three (but only if/when the athlete has been symptom free for 14 days)
F I
N A L S I
1 Initial relative rest 24 - 48 hours after concussion;
2 return to daily activities and light physical activities Following 24 - 48 hours initial rest period (min 24 hours after concussion event);
3 aerobic exercise and low-level body weight resistance training start stage 3 when symptoms allow eg mild symptoms are not worsened by daily activities/light physical activities;
4 rugby-specific non-contact training drills and weight resistance training no earlier than day 8;
5 Full contact practice no earlier than day 15;
O N
i
england rugby headcase guidance on concussion
https://keepyourbootson co uk/rugbysafetoolkit/headcase/
uK concussion Guidelines for non-elite (Grassroots) sport
https://www sportandrecreation org uk/policy/resear ch-publications/concussion-guidelines
“Building therapeutic r is seen a improving o young p

g trusting, relationships
s vital to outcomes for people.”


U P E R
V I S I O N A N D T R A I
the known elements of decreased funding, reducing school nurse numbers and increasing mental health conditions, combined with an inconsistent approach to adolescent mental health care, contribute to the unique perspective of this literature review
a systematic literature review was conducted the final eight articles were selected with inclusion and exclusion criteria and the research critically appraised General analysis is used to identify themes, recommendations for practice and areas for future research
the themes of relationships, supervision and training, access to school nurses, use of technology and workload were identified following review of the literature the resulting discussions and recommendations for practice are set out below
R E L A T I O N S H I P S relationships between the school nurse and young person were regularly described as important in the literature. Building trusting, therapeutic relationships is seen as vital to improving outcomes for young people relationships between professionals and services is also an important contribution to outcomes for young people this was often focused on individuals and so if that person left their role, the relationship between services could break down other professionals can
A
C C E S S T O S C H O O L N U R S E A N D U S E O F
the use of technology is an important development in school nursing that is becoming more widespread the use of technology not only meets the needs of adolescents but improves access to school nursing for harder to reach young people Mental health is a very common reason for accessing online school nursing services and school nurses need to be trained in how to utilise a new online skillset through the introduction and promotion of an online service, for example chathealth, the school nursing team is subsequently promoted
W O R K L O A D
Workload underpins all the identified themes in the literature. It is well documented that child Protection and other reactive work prevents school nurses from undertaking lower level, preventive work however, a heavy workload causes further challenges as it restricts access to training, something school nurses identify as vital to their role and care of the young people they work with It also means that the school nurses are hesitant to undertake promotional work as they cannot cope with the increased referrals it brings
R E C O M M E N D A T I O N S F O R P R A C T I C E
the most significant and commonly cited theme produced in the literature review was “relationships” It is more and more common to adopt a corporate approach in school nursing, but this does mean that services are limiting the opportunity for relationships to develop By scaling back the corporate approach and ensuring individual school nurses cover local schools, effective working relationships will be formed with school staff, relevant services and most importantly, the young people they work with as young people want technology as an option for meeting their health care needs, the development of an evidence-based app or text service used across all school nursing services will ensure their needs are met with a consistent approach chathealth (2023) is a common choice of text service, however it might be that young people would prefer to use web based or mobile app methods to contact school nurses this additional cost on services and pressure on workloads will be mitigated by using a skill mix model; staff nurses or nursery nurses will make up the majority of the team, with the school nurse scPhn overseeing their work, driving health promotion, initiating online services and continuing to build relationships with the local schools they cover
relationships will also be improved between caMhs and school nursing if caMhs practitioners are able to deliver supervision and case management the research in this review demonstrated that school nurses believe caMhs practitioners are best placed to provide supervision, however the pressures on caMhs service are well known (cQc, 2022) this leads to an identified gap in the research of mental health assessment, intervention and care planning the development of a robust, evidence-based mental health assessment and care planning tool would create a common language between services however, tools need to allow for the creativity of the professional to meet the needs of individual young people; one size does not fit all a tool could be devised with the input of mental health experts, but there would need to be additional research to ensure the content is evidence based this could be done in the form of systematic literature reviews using other services and countries’ approaches to assessment and intervention in adolescent mental health the implementation of the tools needs to be monitored and there must be a review of their effectiveness
I hope you can see how these changes could have a significant impact on the outcomes of young people school nurses are best placed to deliver interventions in school for emerging and mild mental health difficulties, but the recommendations above will ensure their effectiveness, with young people at the heart of everything we do
R E F E R E N C E S
care Quality commission (cQc) (2022) looking at the mental health act between 2021 and 2022 available at:
https://www cqc org uk/sites/defau lt/files/202212/20221201 mhareport2122 easyr ead.pdf (Accessed 08/05/2023)
chathealth (2023) evidence available at:
https://chathealth nhs uk/evidence / (Accessed 08/05/2023)
department of health (doh) (2009) healthy child Programme: From 5-19 Years old available at:
https://assets.publishing.service.go v uk/government/uploads/system/ uploads/attachment data/file/4920 86/HCP 5 to 19 pdf (Accessed 01/04/2023)
Haddad, M., Butler, G. and Tylee, A. (2020) 'School Nurses' involvement, attitudes and training needs for mental health work: a UK-wide cross-sectional study ' , Journal of Advanced Nursing, 66, pp 24712480 Available at: DOI
10 1111/j 1365-2648 2010 05432 x
Membride, H., McFadyen, J. and Atkinson, J. (2015) 'The challenge of meeting children's mental health needs' British Journal of School Nursing 10(1), pp 19-25
Pryjmachuk, S , Graham, T , Haddad, M., and Tylee, A. (2011) 'School nurses' perspectives on managing mental health problems in children and young people', Journal of Clinical Nursing, 21, pp 850-859 Available at: DOI
10 1111/j 1365-2702 2011 03838 x
sherwin, s (2016) 'Performing school nursing: narrative of providing support to children and young people', community Practitioner, april 2016, pp 30-34 available at:
https://pubmed ncbi nlm nih gov/2 7183750/ (Accessed 16/04/2023)
Spratt,J , Philip, K , Shucksmith, J , Kiger A. and Gair, D. (2010) ‘We ae the ones that talk about difficult subjects: nurses in schools working to support young people’s mental health', Pastoral Care in Education, 28(2), pp 131-144 Available at: DOI
10 1080/02643944 2010 482145

Sarah Knight is the mother of two boys with severe food allergies After 20 years as a senior television producer, she left her job to set up The Allergy Team to support families living with food allergy and to provide training and education about allergies for schools Backed by the country’s leading experts, The Allergy Team provides practical solutions to help schools reduce risk and improve the safety and wellbeing of pupils with the condition It also assesses schools who want
You can find out more about The Allergy Team at theallergyteam com/schools
Serious allergic reactions are one of the few medical conditions that can take a pupil from completely well to fighting for their life in minutes
It ’s not surprising then, that some school staff feel very anxious about having students with allergies in their care and might look to excluding a pupil with allergies from some activities, rather than run the risk of including them, and something going wrong
as a business which supports families living with food allergies and works with schools, all too often The Allergy Team hears about this kind of decision making, and the devastating impact it can have on young people
But for me, this is personal too Both my sons have food allergies and I have seen them deflated and frustrated time and time again when they can’t enjoy every aspect of school life in the same way as their peers My eldest has been told he has to have packed lunch rather than eating school dinner with his friends, because the school is too nervous to cater for him and every Pta bake sale, I have to churn out allergy-friendly options otherwise there is nothing for them to enjoy not only do children like mine often feel left out, but their exclusion speaks to my worst fear that schools don’t know how to look after them safely
trips are often the highlight of any school term, discussed in excited giggles in break times, fraught with controversy about who is going to sit next to whom on the coach Imagine being the only child in the class left out of that experience or told you will need to do a different activity to everyone else
While many schools are great at risk assessing and planning trips and residentials to be as inclusive as

possible, others fall short the impact on pupils’ mental health and wellbeing can be devastating and pupils with allergies are twice as likely to be bullied as those without
recently, I was contacted by a mother whose teenage daughter had just quit her school ccF because she had been told she could not join an overnight expedition due to her serious food allergies among the reasons given was that the ration packs provided by the army are not nut free. a few weeks later, I was doing an allergy review at another school and met the staff that ran the ccF activities there they explained that they ask their cadets (without nut allergies) to go through the ration packs and remove the packets of nuts, enabling the pupils with nut allergies to safely go on the trip they use this as an opportunity to discuss food allergy and how serious allergic reactions can be – education, spreading awareness and inclusion, all in one
sometimes it ’s the parents of pupils with allergies who feel nervous about giving permission for their child to go on a trip My eldest son is allergic to egg and milk he has experienced anaphylaxis (a lifethreatening allergic reaction) to traces of these foods in the past and so school trips were high on my worry list for a long time however, I was hugely reassured by a Q&a with Professor Graham roberts, one of the country ’s leading allergy consultants, who has a special interest in supporting adolescents with allergies to become more independent in managing their condition he describes school trips and residentials as the perfect opportunity for pupils with allergies to start taking responsibility, in an age-appropriate way and with the safety net of trusted adults from school

keeping a watchful eye For example, they might have the opportunity to choose food from an unfamiliar menu or to carry their own medication, but still under the safety umbrella of the school
as I explained earlier, it ’s not just big events that can leave pupils with allergies side-lined children with allergies are being excluded from cooking lessons, Pta events, science experiments and match teas after sporting fixtures But it doesn’t have to be this way and school medical teams can play a key part in reminding all staff of practical ways to ensure pupils with allergies can be kept safe and included:
• Plan ahead so you have time to think of alternatives to make activities inclusive For example, if you have a pupil allergic to wheat and you want supplies for junk modelling, ask parents to bring in shoe boxes rather than cereal packets
• Make sure food allergy is included in risk assessment and ensure this takes into account travelling to and from an activity, as well as when you’re there
• If you are taking older pupils on a residential trip, consider training them to recognise the symptoms of an allergic reaction and to administer adrenaline this could be incorporated in general first aid training as well as learning valuable life skills, the pupils will be better placed to support their peers with allergies in other social situations, such as at parties or on trips into town
• take opportunities to remind the whole school of their collective responsibility for reducing risk to pupils with allergies, for example inset days, assemblies or event planning meetings some schools will devolve responsibility to their catering team or school nurses but a whole school approach is vital
• sign up to the Schools Allergy Code and Register launched in collaboration with IsBa the register is a record of schools which have demonstrated that they are adhering to best practice in allergy management and have been assessed by the allergy team. schools who want to join get free mentoring and training for all staff, including how to reduce risk and support wellbeing for pupils with allergies


I have been in Nursing for nearly 40 Years My nursing career has embraced many different types of diverse healthcare environments I also had a career break and became a Teacher of Science for nearly a decade, whilst raising my 4 children as a single parent
I am also a Registered Homeopath and Clinical Hypnotherapist who enjoys teaching Yoga on a weekly basis and enjoys walking my 3 black labradors in the Mendip Hills of North Somerset
A new year: reflections from a health centre.
A L L E R G Y S U P P O R T
september brings the start of another school year and along with the anticipation of a new term comes the flurry and influx of new starters at the school, For us in the health and Wellbeing centre, this means that we must be vigilant in our updates, maintenance and creation of new health care plans for all our students from Pre-Prep to sixth Form one of the key areas that seems to be increasing in prevalence is the number of cases of allergic reactions or food intolerances.
We are currently working very hard with different departments, including admissions, data management and catering, to ensure that the information provided by parents, carers and guardians is acted upon our role is to ensure that the right information is communicated to the correct staff that are working to support the pupils
We have created a new standard for allergy care, together with KIt t Medical, thus securing full coverage around the school as a proactive measure in the event of allergic reactions which might lead to anaphylaxis It is staggering that 20% of serious anaphylaxis incidents that occur in schools across the uK happen to children who do not know that they have allergies there is an estimated one to two children with allergies in every school classroom across the uK
We have a total of six KIt ts in different locations across the campus each KIt t is designed to be seen as well as being easily accessible We have chosen suitable wall mounted locations there is a
clear, easy-access key to unlock the box and each box contains four adrenaline auto-injector pens two of the pens contain 300mcg and two contain 150mcg there are also clear usage instructions for use in an emergency situation
We have just completed our half term health checks for our KIt ts to ensure that there is no complacency and due diligence checks are carried out.
We aim to provide a strong and warm communication channel between the health centre and parents a channel that will encourage and create a pathway which will facilitate easy access for parents, carers and guardians to connect with us in support of their child’s health needs and not just on the physical aspects We can only create a plan if we receive the evidence and supporting information which can sometimes be problematic when working with international health care professionals
sometimes shared data information systems can seem complex and difficult to access, so liaising with our data team to deliver bespoke health care templates has enabled us to ensure that we are making effective and appropriate use of key health information ensuring our data and systems are accurate and compatible with our eMIs so that information is accessible prior to our immunisation sessions has kept the nursing team very busy We have been tirelessly updating and inputting paper records onto the computer can you relate?

We aim to provide the highest standards of pitchside support and are currently working with our medical officer, paramedic and sport physiotherapist to further develop our offering in this area As a nursing team we work together to support and offer gold standard pitch-side care. All our nurses have sports injury qualifications, and are trained in intermediate life support. Having worked within the NHS, we are all very acutely aware that ambulance waiting times may significantly increase during the winter season and so by upskilling our team we can ensure that we offer the highest level of acute care should it be required prior to arrival of an ambulance

We are delighted that we have converted part of the building into a beautiful new space suitable renamed ‘The Wave’. It is a sensorial haven of calm and Zen much needed for not just pupils but anyone who needs to “just be”.
This space boasts Love Island style bean bags, an egg chair, textures and layers of textiles, cushions and furnishings with colours and sounds to enable all who enter to relax. It is a space where you can be close to our designated counselling area and we also hope to create an outdoor garden from our existing patio space. This year we are having a Wishing Tree so that we can release, let go and acknowledge our needs as we work within an ever-changing world.
In an ever-changing world, with so many different forms of communication, it seems more important than ever to be able to meet the emotional and social needs of our pupils and perhaps equip them with a wellbeing toolkit through a different way of assessing their health needs. I was excited when invited to talk to year 7 and 8 to find out what they thought ‘health and wellbeing’ meant to them. They had the language to articulate the whole spectrum of emotions and feelings that they had experienced or witnessed It is so good for pupils to encounter health care professionals before they actually need them. As a diverse team, like many other schools, we offer so much more than our clinical skills and this uniquely positions us to support pupils and staff to navigate the pressures of being human when it seems that life and external expectations expect us to be beyond just that.
 ADAM EUSTACE - SPECIALIST MSK PHYSIOTHERAPIST MSc, PGDip, BSc, MMACP, MCSP, HCPC
ADAM EUSTACE - SPECIALIST MSK PHYSIOTHERAPIST MSc, PGDip, BSc, MMACP, MCSP, HCPC
Adam Eustace is the lead physio at Wellington College and Shrewsbury School, Director of Modus Physiotherapy and Modus Education Adam has been instrumental in developing fully integrated sports management systems within schools, through staff and pupil education seminars, optimised pitch-side care, and access to physiotherapy triage clinics With over 10-years’ experience in the school sector, Adam understands the challenges sports injury management presents to medical teams As a result, Adam has developed the only sports management course tailored to school nursing teams and sports staff through Modus Education, already teaching over 100 schools across the country
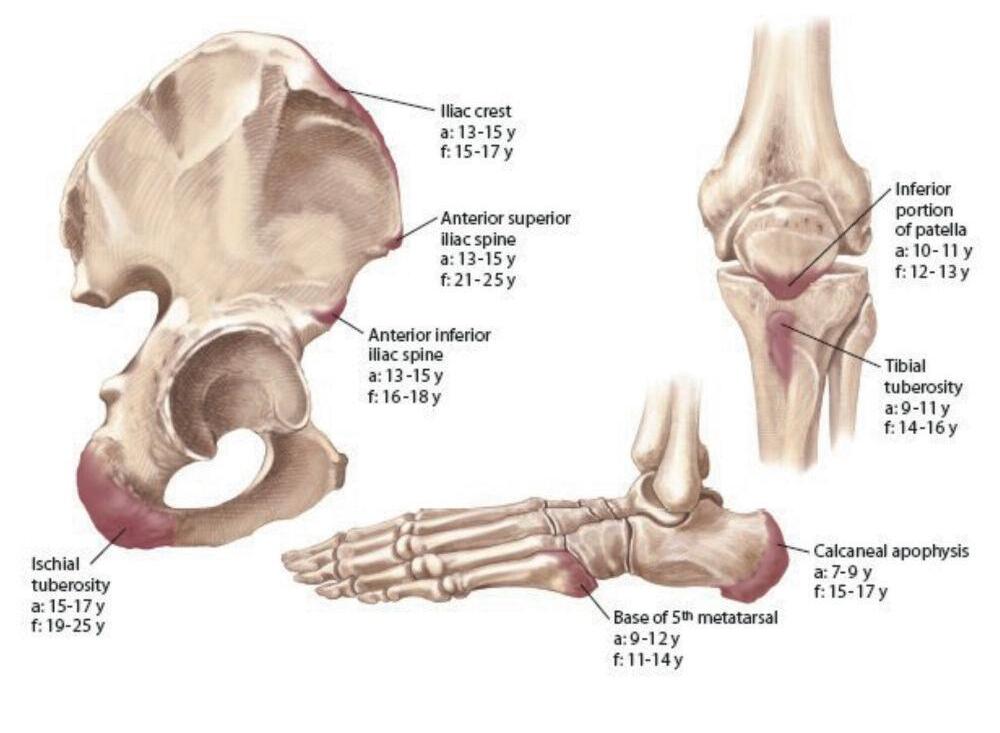
Working within a school health centre, I’m sure we have all seen a child with osgood schlatter ’s and severs diseases, but what about larsen-Johansson disease, thrower ’s elbow, hip apophysitis or even Iselin disease? these are all types of apophysitis injuries which account for around 16% of all adolescent sporting injuries (rossi & dragoni, 2001) In this article we are going to outline what they are, how they may present and how they should be managed
the term ‘apophysis’ is given to a bony protrusion which is not directly attached to its adjacent bone until skeletal maturity is reached the tendon or ligament attachments often found at these sites are often subjected to traction forces during physical activities during times of increased activity or high load, these sites may become irritated leading to an inflammatory reaction termed apophysitis In rare cases a large acute load may even detach the apophysis leading to an avulsion fracture
HoW do tHey PReSent?
though the location of pain may vary dependent on the apophysis affected (see figure 1), one of the key characteristics of an apophysitis is that it has a gradual, insidious onset, and is aggravated by physical activity If a patient complains of pain at an apophysis with an acute or traumatic onset (e g after forcefully kicking a ball, landing from a jump or throwing a ball), then an avulsion fracture must be considered and an x-ray warranted
We will now describe the presentation of two lesser known apophysitis injuries, namely hip and pelvic apophysitis and Iselin disease
apophysitis injuries originating at the hip and pelvic region are often misdiagnosed and mismanaged this is due to a lack of knowledge in their presence and misdiagnosis as tendon injuries

Pain originating at the front of the pelvic region (asIs & aIIs, see figure 2) often results from kicking sports and sprinting; pain at the pubic symphysis
from running, dance and gymnastics; the ischial tuberosity (bony lump you sit on) from sprinting, kicking and repeat bending (as in hockey); and pain along the Iliac crest from distance running.
though the literature states a common onset of these apophysitis injuries between 9 and 15 years of age (Wilson & rodenberg, 2011), they may present in athletes until around 18 years of age
ISELIN DISEASE
this is the least common lower extremity apophysitis, presenting in girls between 8 and 12 years, and boys between 10 to 14 years of age (Frush, 2009) It is caused by the repeat traction force at the base of the 5th Metatarsal (see figure 1) by the peroneal muscles these muscles normally prevent the foot from rolling inwards (inverting), and are more often stressed in sports that require frequent changes in direction, or following an acute ankle injury (e g netball, football, basketball) It rarely presents with swelling in the area, and if present should be referred for an x-ray to assess for an avulsion fracture
HoW SHould tHey Be mAnAGed?
In a health centre setting, initial management should involve educating the patient on what the condition is, and how to reduce the overall loading through activity moderation. as a general rule, if a patient can perform their daily activities (e g stairs, walking, squatting) with minimal pain, they may continue to perform sporting
activities If they are struggling to carry out normal daily activities they should have a period of enforced rest from sport and carry out some light stretches until the symptoms resolve.
In persistent cases (> 4 weeks) or very sporty children, referral to a physiotherapist may be warranted to assess for any factors exacerbating the condition (e g poor movement mechanics, weak or tight muscles, anatomical variations)
WHen SHould i Be conceRned?
thankfully apophysitis injuries are normally selflimiting and can usually be easily managed however, in some instances pain may indicate a more significant pathology this needs further investigation by a physiotherapist or medical professional Presentations which should warrant further investigation might include (but are not limited to):
• acute onset of pain and/or loss of ‘normal function’ (e g unable to bend knee, unable to weight-bear)
• Pain which does not appear to be related to physical activity (e g night pain, resting pain, unremitting pain)
• excessive swelling and/or bruising
• Pain not eased by period of rest
• any presentation of which you are unsure of the pathology

FRIDAY 12 APRIL
FRIDAY 12 APRIL
TUESDAY 16 APRIL
FRIDAY 26 APRIL
THURSDAY 2 MAY
WEDNESDAY 22 MAY
TUESDAY 11 AND WEDNESDAY 12 JUNE
THURSDAY 20 AND FRIDAY 21 JUNE
MONDAY 8 JULY
Audience: Independent and boarding school nurses, matrons, health and wellbeing leads, pastoral staff
our annual conference is the highlight of our events programme and the culmination of another academic year
our focus last year was on anxiety and the importance of inclusion for sufferers this year our focus will be on the everchanging landscape of health care and how we can support everyone, young people and adults, in fulfilling their potential both physically and emotionally We will soon be announcing more detail and information regarding our speakers
hIeda/Bsa Member rate: £215 | hIeda/Bsa additional Full Member Fee: £110 Bsa affiliate Member: £325 | Bsa additional affiliate Member: £140 | non-member rate: £430*
“Fantastic trainers with fabulous knowledge, skills and personalities.”
5th
london W1W 5PF
+44