Health report






Sponsored by Delivering


Delivering change and adding value through transformation programmes in healthcare








Sponsored by Delivering


Delivering change and adding value through transformation programmes in healthcare


Minister of State with Responsibility for Mental Health and Older People, Mary Butler TD, outlines progress made on the delivery of Sharing the Vision, Ireland’s national mental health strategy.
Sharing the Vision: A Mental Health Policy for Everyone is Ireland’s ambitious national mental health policy to enhance the provision of mental health services and supports across a broad continuum from mental health promotion to specialist mental health delivery during the period from 2020 to 2030.
An unprecedented level of funding, totalling, €1.149 billion was allocated to the overall mental health budget in 2022. This trend was continued in Budget 2023, with €1.2 billion allocated to mental health services. This record budget will allow us to continue to improve mental health services to the benefit of all, through the implementation of Sharing the Vision and Connecting for Life, Ireland’s national suicide prevention strategy.
The vision embodied in Sharing the Vision is to create a mental health system that addresses the needs of the population through a focus on the requirements of the individual. This mental health system should deliver a range of integrated activities to promote positive mental health in the community; it should intervene early when problems develop; and it should enhance the inclusion and recovery of people who have complex mental health difficulties. Service providers should work in partnership with service users and their families to facilitate recovery and reintegration through the provision of accessible, comprehensive, and community-based mental health services.
As Minister of State for Mental Health, the full realisation of Sharing the Vision from policy to practice, to ensure real improvements in mental health service delivery, is a fundamental priority.
I was pleased to establish the National Implementation and Monitoring Committee (NIMC) in 2020 to drive Sharing the Vision forward and ensure robust policy implementation oversight and governance. NIMC is independently chaired by John Saunders, and is supported by a Reference Group of Service Users and Family Members and Specialist Groups. As the HSE has responsibility for the majority of the policy recommendations there is also a HSE Implementation Group (HIG) that reports to NIMC.
So far, the following specialist groups have been set up to address the implementation of complex recommendations: Youth Mental Health Transitions Specialist Group; Primary Care Specialist Group; Acute Bed Capacity Specialist Group; Digital Specialist Group; and Women’s Mental Health Specialist Group.
“As Minister of State for Mental Health, the full realisation of Sharing the Vision from policy to practice, to ensure real improvements in mental health service delivery, is a fundamental priority.”
Developed in collaboration with key stakeholders, Sharing the Vision Implementation Plan 2022-2024 – the first of three implementation plans –provides detailed three-year plans for each of the policy’s 100 recommendations, including setting milestones to be met each year, and detailing the inputs and outputs necessary for implementation. The plan ensures the continued momentum needed for a successful policy implementation.
Since Q3, 2021 a Policy Implementation Status Report has been published each quarter, alongside NIMC’s Quarterly Report Analysis. The Status Report provides an overview of progress as well as a brief status update for each of the 100 recommendations. The Reference Group also provides feedback to the status reports, bringing the service user and family member perspective.
Two years into the 10-year policy, the vast majority of the 100 recommendations are in implementation stage, with any implementation challenges being closely monitored by NIMC.
Some of the significant developments to date include:
• Continued phased implementation and evaluation of national clinical programmes in mental health. This includes dual diagnosis, early intervention in psychosis, eating disorders, ADHD in adults, and selfharm. The clinical programmes are at the heart of service improvement.
• The opening of a new purpose-built forensic campus in Portrane, County Dublin that enables the provision of a modern forensic mental health service and provides a network of forensic facilities to allow proper and timely intervention.
Delivering change and adding value through transformation programmes in healthcare

• Following extensive consultation with stakeholders and a public consultation, the review of the Mental Health Act 2001 was completed and a General Scheme setting out extensive planned amendments to the Act was published in July 2021. A Mental Health Bill is now being drafted by the Office of Parliamentary Counsel in line with this General Scheme. Work on the Bill is ongoing, and I plan to introduce it into the Oireachtas as early as possible in 2023.
• The expedition of developments in online mental health supports and service provision. These initiatives exemplify the whole-of-population approach to mental health service developments that Sharing the Vision promotes. Specific examples include 24-hour text support and guided online therapy.
• Review and service improvement in children and adolescent mental health services (CAMHS) to align with the recommendations arising from the Maskey Report (2022).
• Continued development of the recovery approach and the further embedding of the lived experience expertise into service provision through the ongoing development and roll out of initiatives, including peer support working, recovery education, and the individual placement service.
• The Sláintecare Implementation Strategy and Action Plan (2021-2023) and the Women’s Health Action Plan (2022-2023), both of which were published by the Department of Health, and the work of the Taskforce for Mental Health and Addiction Challenges for Persons Coming to the Attention of the Criminal Justice System. All of which align to the recommendations of Sharing the Vision
Mental health is not a matter for the health sector alone.
The reform promised by Sharing the Vision cannot be achieved without measures being taken by other government departments and state agencies, as well as by the Department of Health, for example, the Comprehensive Employment Strategy for People with Disabilities, and the National Housing Strategy for Disabled People 2022-2027, as aligned strategies to Sharing the Vision
We will continue to build on innovation and progress achieved already and maintain the momentum necessary to put policy into practice and provide better mental health services for us all.

medicine.
The right treatment for the right person at the right time: this is the promise of personalised medicine, a paradigm shift in healthcare with transformative potential for patients, practitioners, and the public, writes Mairéad O’Driscoll, Chief Executive of the Health Research Board (HRB).
In order to explore what this might mean for Ireland, the HRB National Conference recently brought together stakeholders from across the health ecosystem to discuss the future of personalised medicine, with a number of key takeaways emerging.
Firstly, personalised medicine is far from blue-sky thinking: from treating cancer to managing neurological conditions like epilepsy, research in genomics is already informing tailored treatment paths that are improving patients’ lives. The shift is from a ‘one-size-fits-all’ approach to diagnosis and treatment to one that combines molecular profiling, medical imaging, and lifestyle data, for example, to enable earlier and more precise diagnosis, select personalised therapies, or predict predisposition to disease and target prevention strategies.
Already a prominent fixture on the European research landscape, personalised medicine is climbing the policy agenda here in Ireland too. Important developments in recent months include:
• Ireland joined the European ‘One Million Genomes’ initiative, aiming to securely link genomics databases to advance personalised medicine;
• a citizens’ jury has met on the future use of genomics, highlighting key issues around genomics in medicine;
• the first National Strategy for Genetics and Genomics, which sets out a vision and roadmap for genomics in Ireland; and
• co-funded by the HRB, a new Digital Europe project is set to advance a European genomic data infrastructure.
With these wheels now in motion, the time is right for Ireland to capitalise on this momentum.
To truly deliver on the promise of personalised medicine, however, we must go beyond research alone. The real potential lies not only in new medical treatments, but in transforming how we deliver healthcare more broadly: from diagnosis, to treatment, to disease prevention. Unlocking the benefits for society will require systemic change.
This can only happen if every stakeholder in the health ecosystem has a seat at the table: from government departments and agencies, health system professionals, industrial and academic research, and – crucially –patients and the public. We reached out to over 50 community groups ahead of our recent conference, asking people from all walks of life to share their views on personalised medicine. While attitudes were generally positive, concerns were raised around topics like data protection, access, and equity. One contributor used the term ‘co-creation’ of healthcare to describe the benefits of moving to a personalised approach. As we consider how to get there as a society, it will be essential not just to listen to citizens’ views but to bring the public on board as co-creators of this new future of healthcare.
For more information please contact Gillian Markey, HRB Communications Manager: E: gmarkey@hrb.ie W: www.hrb.ie

At Grant Thornton, we understand that our clients within the healthcare sector operate in increasingly complex and demanding environments with constant pressures to improve access, enhance quality, and ensure patient safety, writes Elaine Daly, Partner –Head of Business Consulting at Grant Thornton.
Appropriately responding to these pressures is vital in order to achieve better patient outcomes, and effectively control operating costs. As the healthcare needs of the Irish population are continually evolving, in line with changing lifestyles and demographics, this will influence future healthcare requirements.
Healthcare is a core component of Grant Thornton’s day-to-day business operations. Our team of healthcare consultants offer numerous services to healthcare organisations so they can meet today’s challenges and also
Grant Thornton’s firm-wide health sector service offering is spearheaded by Elaine Daly, Partner – Head of Business Consulting for Grant Thornton Ireland. Daly is also the lead for business consulting globally which facilitates collaboration and the sharing of best Delivering

position themselves to adapt to emerging trends. We have worked with organisations operating in all areas of healthcare, including community services, acute services, national care programmes, healthcare technology, and many more public and private organisations.

practice across the Grant Thornton global network.
Daly joined Grant Thornton in 2006 having previously worked in business consulting for two other leading Irish advisory firms. She holds over 20 years’ experience and has worked with numerous clients within the health and life sciences sectors, supporting organisations to transform and develop innovative ways of working.
Grant Thornton has experience in working across major healthcare transformation programmes and projects in order to deliver change and add value in line with strategic policies and in tandem with organisational requirements. We seek to support clients to seize opportunities for economic improvement, operational efficiency, and effectively implement value-based healthcare.
Our healthcare consultants possess a unique blend of skills and experience. We bring together teams with clinical and non-clinical backgrounds, who have experience in delivering pan-European healthcare engagements.
As a team, we coordinate regularly with our client delivery teams and, where necessary, our wider firm-wide subject matter specialists to ensure agility of response and consistently high levels of service. As project managers, our team is proactive and independently calls out issues to keep everyone on track.
The result of working with our healthcare consultants is a framework for a range of services, strategies, and solutions that can help healthcare providers optimise operations, improve the patient experience, expand capabilities, and prepare for a strong future.
Elaine Daly Partner – Head of Business Consulting
Grant
Thornton
T: 01 3805 895
E: elaine.daly@ie.gt.com

Our team is passionate about implementing effective improvements within the healthcare industry, and seeks to support clients with the following capabilities:
Programme and project management: Grant Thornton can provide programme and project management services to help organisations strategically plan and react to changes within the healthcare industry. Grant Thornton has experience in developing business cases, maintaining project plans and managing wide-ranging initiatives from initiation to deployment.
We help our clients bring innovation from concept to reality in a safe and measured way. We do this using proven best practice approaches in programme and project management. Our healthcare project managers have experience in leading and overseeing large healthcare projects.
Operational excellence: Grant Thornton help clients develop and implement process improvements using methodologies including lean six sigma. Our teams possesses extensive experience in supporting healthcare organisations to adapt, transform and achieve their goals. We support organisations on their operational excellence journey by providing expert advice and solutions. Our healthcare consultants have significant clinical experience in designing operating systems and clinical pathways.
Change management: Grant Thornton has proven expertise in developing and redesigning target operating models (TOM) by reviewing organisations’ current “as-is” and “to-be” states. We have experience in conducting change management programmes and projects in key areas across clinical and non-clinical settings.
We work as a transformational change partner assisting with stakeholder management and engagement to help healthcare organisations develop the required working practices and sustain new behaviours. We use proven methodologies that enable healthcare organisations to transform seamlessly.
Financial improvement: Grant Thornton has experience in engaging with multi-disciplinary teams across differing healthcare functions to successfully implement financial improvement plans.
At Grant Thornton, we understand that delivering financial improvement in healthcare requires responsive, patient centric solutions, which encapsulate people, processes and technology.

Budget 2023 delivered a record investment of over €23 billion pledged to Ireland’s health and social care services. The investment comes as free GP care is extended to all children aged six and seven, the phased rollout of Sláintecare continues, and the State struggles to address its lack of hospital beds.
Budget 2023 allocated €23 billion to the Department of Health, comprising €22.240 billion in current expenditure, including a 5.6 per cent increase in core spending, and €1.177 billion in capital expenditure, including a 10.7 per cent increase in core health capital expenditure.
This level of funding will deliver record levels of health funding in absolute terms for the third year in a row, although it must be noted that inflation reached as high as 9.2 per cent in Ireland during 2022 according to Central Statistics Office data. This allocation renders the Department of Health the second-best funded department in current expenditure, with only the Department of Social Protection receiving more funding for gross current expenditure (€23.387 billion), and the third-best funded department by capital
expenditure, with the Department of Housing, Local Government and Heritage (€3.516 billion) and the Department of Transport (€2.622 billion) receiving more in gross capital expenditure. The Department of Health thus accounts for 29.4 per cent of current expenditure and 9.7 per cent of capital expenditure.
Notable health measures to be taken through the increased funding delivered by the Budget include the expansion of free GP care to all children aged six and seven by the end of 2022, with eligibility also to be further extended from 1 April 2023 to people in households earning the median household income of €46,000 per annum or less. The Government has stated that this will mean that “almost half of the population will have access to free GP care” and that “these measures will be supported by a significant package of additional capacity supports to GP practices”.
“Giving someone a doctor visit card will not automatically translate into an accessible service when that service is already struggling to cope with current demand.”
Irish Medical Organisation
Other measures include the removal of VAT on defibrillators, the announcement of public funding of IVF treatment from September 2023 onwards, a €47 million plan to invest in increased GP access to diagnostic services in fields such as echocardiography, spirometry, and natriuretic blood tests, and a once-off €100 million fund to address energy costs within the health sector during the winter of 2022/23.
The budgetary measures have received a demur reaction from medical practitioners, with John Farrell, chairman of the Irish College of General Practitioners (ICGP), saying that the provision of expanded free GP will “inevitably mean longer waiting times for patients’ appointments with GPs, at a time of huge workforce and workload pressures”. A recent survey by the ICGP found that just one-fifth of GP practices stated that they have the capacity to take on new patients. This sentiment was echoed by the Irish Medical Organisation, which stated: “Giving someone a doctor visit card will not automatically translate into an accessible service when that service is already struggling to cope with current demand.”
December 2022 saw the Government reach “landmark” agreement on a proposal from Minister for Health Stephen Donnelly TD on a public-only hospital consultant contract. The contract will include: basic pay of between
€209,915 and €252,150 on a six-point scale; a 37-hour week with an 8am to 10pm Monday to Friday and 8am to 6pm Saturday schedule; consultants will continue to receive additional remuneration of up to €38,000 per annum for on-call duties and overtime as applicable; a “highly flexible contract that enables consultants opt for a variety of different work patterns including less than whole time”; work sharing; compressed hours; flexible start and finish times; supporting consultants to participate in medical education training and research and enabling a greater focus on research and education in line with other jurisdictions; and consultants will be permitted to engage in off-site private practice in a similar fashion to Britain’s NHS.
Speaking after the approval of the contract, Donnelly stated that its introduction “will be a landmark in delivering universal healthcare” and “will maintain the momentum of reform and improvement in our health services”. The Irish Hospital Consultants Association, a negotiating body within the agreement, has stated that the agreement will not help to reduce waiting lists unless other issues are addressed, namely the filling of over 900 current permanent consultant vacancies.
In his statement welcoming the agreement of the Sláintecare contract, Donnelly, who took office in May 2020,
also noted that 900 additional acute beds have been delivered since January 2020 and that 16,200 staff have been recruited over the “last two years”, including 4,600 nurses and midwives, 2,650 health and social care professionals, and 1,750 doctors and dentists.
While noting that this was the “highest level of recruitment in the history of our health service” and that 1,300 consultants had been recruited over the last 10 years, Donnelly also stated that “our ratio of consultants to population in Ireland has historically been far too low”; the OECD’s Health at a Glance: Europe 2022 report shows that the State has 3.5 practicing doctors per 1,000 of population as of 2020, beneath the EU27 average of 4.0.
As the reshuffling in the Cabinet takes effect, Donnelly’s tenure as Minister of Health has seen an increase in National Treatment Purchase Fund (NTPF) waiting lists; from over 776,000 patients in figures released in February 2020, the last figures released before the onset of the Covid pandemic and the agreement of the tri-party coalition, to 841,748 patients in October 2022. The October figure, however, marked a reduction from 853,014 in September 2022. With this figure having begun to decrease as the Taoiseach’s office rotates from Fianna Fáil to Fine Gael, the former will hope to have initiated a long-term trend of reductions in the waiting lists during its tenure.

Delivering change and adding value through transformation programmes in healthcare
Contextualising Department of Health policy direction, Health in Ireland: Key Trends 2022 is a guide to the significant trends in health and healthcare over the past decade. Highlighting progress as well as persistent challenges in delivering accessible, timely, and efficient healthcare, the report explores demographics, population health, hospital and primary care, and health service employment and expenditure.
Census 2022 indicates that the population of the State is 5,123,536, representing a 7.6% increase on Census 2016
The population has grown by 10.5% since 2013
The largest change (35%) was observed in the 65+ age cohort
Total Fertility Rate has fallen to 1.7, representing the 6th highest fertility rate in the EU
Life expectancy at birth for women in 2020 was 3.6 years longer than for men
In 2021, 81.7% of males and 81.3% of females perceived their health as being good or very good
In the EU, an average of 71.1% of males and 67% of females perceived their health as being good or very good
In 2021, 48% of males and 48.1% of females aged 65+ reported suffering from a chronic illness or a health problem
Between 2012 and 2021, age-standardised death rates for all causes decreased by 15.8%
The age-standardised death rate for cancer has declined by 15.3%
Death rates from suicide decreased by 15.1% between 2020 and 2021
Total public expenditure on health increased by 69.5% between 2012 and 2021
HSE non-capital total allocation has increased by 8.1% between 2020 and 2021
Acute hospitals accounted for 33.3% of HSE gross non-capital expenditure in 2021
Public capital expenditure on health increased by 11.7% between 2020 and 2021
Total public and private health expenditure in the State was €26.5 billion in 2020

Delivering change and adding value through transformation programmes in healthcare
Inpatient discharges from publicly funded acute hospitals decreased by 3.5% between 2012 and 2021
Average length of stay increased by 12.3% to 6.1 days between 2012 and 2021
The number of beds for day cases has increased by 19.1% to 2,440 between 2012 and 2021
The number of day cases has increased by 11% to 1,016,146 between 2012 and 2021
The number of adults waiting for 12 months or longer for an elective procedure (from August 2021 to August 2022) has increased by 3,000
The total number of people on outpatient waiting lists has increased to over 629,446 (in August 2022)
206 transplants were carried out in the State in 2021
80% of ECHO ambulance calls were responding to in under 19 minutes
55% of DELTA ambulance calls were responded to in under 19 minutes
Admissions to psychiatric hospitals and units decreased by 13.5% between 2012 and 2021
The proportion of the population in possession of a medical card increased by 31.2% to 30.8% between 2012 and 2021
The number of GP only visit cards increased to 530,378 between 2012 and 2021
The number of people registered for the Drugs Payments Scheme decreased by 2.3% between 2012 and 2021
Average annual attendances to a GP were 3.3 visits per annum
The proportion of the population covered by private health insurance increased from 42.8% to 45.1% between 2017 and 2021
The proportion of blood donors in the population declined to 1.5% in 2021
Whole time equivalents employed in the public health services increased by 4.9% to 132,323 between December 2020 and September 2021
Nurses represent 31% of total staff employed
Hospital consultants employed by the public health service increased by 43.5% between 2012 and 2021
Non-consultant hospital doctors increased by 51.7% between 2012 and 2021
In 2021, there were 4.05 practicing doctors per 1,000 of the population in the State; above the
3.7


Ireland can move from a laggard to a digital health leader in Europe by 2025 if available digital solutions are embraced, says Martin Curley, the HSE’s Head of Digital Transformation and Open Innovation.
Expanding on a popular theory by MIT’s Michael Schrage that innovation is not something that innovators do but what customers adopt, Curley says that momentum built up over the pandemic must be maintained if Ireland is to fulfil its potential as a leader in digital health.
The HSE’s Head of Digital Transformation and Open Innovation regards the Covid-19 pandemic as a catalyst for digital innovation but stresses that many of the solutions implemented had previously existed.
“What happened with Covid as a catalyst was that the adoption curve dramatically accelerated and shifted left. We experience around a decade’s worth of adoption happening in a matter of weeks,” he explains.
Curley identifies two reasons for big bang adoption. The first, he says, is that necessity is the mother of invention. “We had no choice,” he states.
“Within 48 hours of Covid being in Ireland we had developed a remote monitoring solution for Covid-19 which kept patients at home or allowed them to discharge early. That was phenomenally successful and empowered patients.
“Similarly, the demand for electronic prescriptions existed for more than a decade. Within two-and-a-half weeks, and with some secondary legislation progressing through the Dáil, electronic prescribing was here and is routinely used today.”
The second factor flagged by Curley was decreased resistance to innovation.

Despite being a top 12 economy, with the top 10 MedTech companies, top 10 pharma companies, and top 10 tech companies, Ireland is ranked 80th in the CEOWORLD Magazine Health Care Index, which rates healthcare systems relative to factors that contribute to overall health.
Outlining his thesis for circumventing resistance to innovation, Curley points to Ireland’s Digital Health Strategy and Action Plan: Stay Left, Shift Left, 10X, which he says is increasingly getting global attention.
“Stay left is the idea that we can keep people well using digital technology to manage healthcare from home. Shift left is about moving patients as quickly as possible from acute care to community care to care at home, using digital technology.”
Curley observes that the application of digital technology within healthcare, an information-intensive industry, allied with exponential innovation methodology – or Open Innovation 2.0 – enables 10X returns.
“10X better, 10X cheaper, 10X faster, and 10X higher volume,” he states.
“One of the key design patterns is design for adoption. Designing solutions so that they are easy to adopt. That means solutions need to have a lot of utility, there needs to be evident value from it, the user experience has to be good, and they have to be ubiquitous.”
"The demand for electronic prescriptions existed for more than a decade. Within two-and-a-half weeks, and with some secondary legislation progressing through the Dáil, electronic prescribing was here and is routinely used today.”
Martin Curley, the HSE’s Head of Digital Transformation and Open Innovation
Unlike in the past, when risk-adverse clinicians or patients resisted clinical innovations and effectively acted as obstacles to change, Curley believes that the administrative side of the health system is the epicentre of resistance to digital innovation.
However, Curley has adopted German philosopher’s Arthur Schopenhauer’s three stages of truth theory to digital health innovation, which is that “all truth passes through three stages. First, it is ridiculed. Second, it is violently opposed. Third, it is accepted as being self-evident.”
In practice, he articulates, Open Innovation 2.0 hinges on a “shared vision” whereby a community works together to create shared value.
In association with various clinicians, Curley is involved in a number of ‘living labs’ – pilots for disruptive digital technology innovation in a clinical setting – around Ireland. Based on their success to date, several of these living labs have already scaled up.
Regardless, the HSE’s Head of Digital Transformation and Open Innovation believes that Ireland now faces a challenge to maintain momentum.
“The innovation momentum built up over Covid-19, where teams were autonomous, empowered, and highly motivated could be a new normal for our health service. We know how to do it and we have clinically proven solutions but there are blockages in the system.
“We as a society and an economy actually have to make an explicit decision as to whether we aggressively embrace these new digital health solutions.
“By embracing digital health innovation we can move from being the laggard in Europe to being a digital health leader by 2025 and can improve our digital health exports by a factor of 10,” he concludes.


Promotion of greater equality, diversity and inclusion across healthcare will lead to a stronger health system and improved patient outcomes, writes Suzanne Crowe, President of the Medical Council.
One of the main tenets of the public sector and human rights legislation is promoting equality and we believe, as the Medical Council, that represents both doctors and patients, that this is key to ensuring that medical regulation protects the public and supports registered medical practitioners.
Women in medicine in Ireland: Where do we go next?
Working in a childrens’ hospital as a doctor, I am the product of my mother’s
sacrifices. The result of the sacrifices and compromises made by a generation of women who stayed at home under the conditions of the marriage bar introduced in the 1930s, which was not officially lifted until 1973.
At the end of last year, of the 25,959 doctors on the medical register, 45 per cent were female. In 1994 the figure was only 30 per cent.
When we look at younger doctors, in 2021, there were 9,326 doctors aged between 20 and 35 on the register. Of those, 53 per cent were female and 47
per cent were male. This next generation of women doctors will achieve career development along slightly different pathways to the paths that we took.
Today, there are many women in medicine who balance busy working lives with caring roles at home.
Sometimes compromises can involve delaying having a family until training is finished, or it might be changing specialty to facilitate one partner in the relationship spending more time with family.
45 per cent of our specialist register are female, compared to just 38 per cent 10 years ago. While the numbers of women entering medicine rises each year, this increase is slow to be seen in appointments at a senior level and across different specialties there is still inequality in terms of training opportunities and career progression.
The unequal impact of caring responsibilities on women represents an obstacle to career development and explains why we do not have as many women consultants and professors as we should at this stage.
Tackling these issues will be a legacy that is meaningful for the next generation of patients and doctors of all genders, and the workplace as a whole.
As with many elements of our society, the healthcare sector has much historical hurt and distrust to undo when it comes to those who are in the LGBTQ+ community.
I attended a conference during Pride on this topic and was saddened to hear participants speak about fear and a lack of respect that was the hallmark of healthcare for people who did not follow what was regarded as the ‘traditional norms of our society’.
From the memories came a sense of

hope at how things have changed for the LGBTQ+ community in healthcare access. Healthcare staff from several hospitals described the education and training they have done to facilitate compassionate care to LGBTQ+ people. LGBTQ+ patients need openness, respect, and specific measures to include all aspects of them as patients and partners in their own decisions and care.
Continuing to improve how doctors and healthcare professionals engage with the LGBTQ+ community will help to build understanding. Initiatives like the LGBT Champions programme, established by LGBT Ireland in partnership with the HSE, will be essential to this. The programme empowers participants with the understanding and skills needed to increase the visibility, respect, awareness, and knowledge of the issues facing older LGBTQ+ people.
The number of new doctors who registered with the Medical Council in 2021 was 2,605, which represents a 14 per cent increase on the previous year. Of those, 1,717 were international graduates and 888 were Irish graduates.
In 2021, 8,759 (40.4 per cent) doctors who retained their registration held a non-Irish passport.
According to the CSO, an estimated 622,700 non-Irish nationals are living in Ireland, making up 12.7 per cent of the total population.
The promotion of equality, diversity and inclusion at board level can reduce the possibility of ‘groupthink’ as a greater range of perspectives is brought to the table. Ideally, a board should reflect the stakeholders its decisions impact. This is an area the Medical Council, like many bodies involved in healthcare, is failing on, but it is one we are committed to addressing.
Currently there are no Council members that
could be classified as non-Irish, meaning that for nearly 13 per cent of the potential patient population and 40 per cent of doctors on the register, they are not reflected on a board that makes decisions that have, in some cases, a huge impact on their lives.
We continue to engage with the Department of Health and the bodies that nominate members of the Medical Council, outlining the importance of equality, diversity, and inclusion and the Medical Council’s responsibilities in this area.
All bodies and agencies involved in healthcare delivery, policy, and advocacy need to be more cognisant of the importance of equality, diversity, and inclusion in their work, and with us all playing our part individually and by working together we will in return have a stronger health system and improved patient outcomes.
Suzanne Crowe is President of the Medical Council and works as a consultant in paediatric intensive care in Children’s Health Ireland Crumlin.
The Medical Council is the regulatory body for doctors. It has a statutory role in protecting the public by promoting the highest professional standards amongst doctors practising in Ireland.
T: 01 4983100
E: communications@mcirl.ie
W: www.medicalcouncil.ie
Delivering change and adding value through transformation programmes in healthcare





The HSE has released its winter plan amid expectations of a surge in cases of Covid-19, in addition to the expected pressure the health service will face due to seasonal illnesses.
The HSE is expecting a rise in levels of Covid-19 and has prepared a contingency plan aimed to mitigate the worst excesses of the virus. As such, there will be a projected rise in unscheduled care, which the Department has rationalised will take place for the following reasons:
• a lack of bed capacity to meet demand;
• reduced staffing levels and recruitment challenges;
• scheduled care waiting lists and the impact of delayed and postponed care;
• developments in primary and community care services;
• challenges in integrating patient care across acute and community services;
• increases in population, particularly the ageing population, and increasing numbers of patients requiring health services including refugees and those seeking international protection; and
• the ongoing need for separate Covid-19 and non-Covid-19 pathways and the resulting infection prevention and control requirements in both acute and community services.


The HSE has further made plans for the combatting a potential ‘twin-demic’ of both influenza and Covid-19, although it does state that Covid-19 in Ireland appears to be transitioning to an endemic proportions. The plan will be funded to the tune of around €169 million.
It is to be measured by a set of key performance indicators, including a 97 per cent patient experience time (PET), a 99 per cent PET for over 75s, a delayed transfer of care (DTOC) of 350, a length of stay of 4.8 days, an 8am trolly count of less than 236, and a National Ambulance Service (NAS) turnaround time of 80 per cent. None of these targets have been met to date in 2022.
As outlined by the Department of Health, the Winter Plan identifies key priorities which aim to address the objectives of the of the plan and align with corresponding initiatives at national and local level.
• Delivering additional capacity in acute and community services: To deliver additional acute and community bed capacity and increase staff capacity through the implementation of the Safe Staffing and Skill-Mix Framework and prioritisation of recruitment for existing funded posts to support Winter Plan 2022/23. The HSE also plans to extend the opening hours of several local injury units to operate between 8am and 8pm.
• Improving pathways of care for patients: To implement alternative patient pathways during the winter period to support admission avoidance, patient flow and discharge, including Enhanced Community Care (ECC) supports.
• Rolling out vaccination programmes for flu and Covid-19: To deliver an influenza vaccination programme alongside a Covid-19 vaccination programme, and increase awareness and uptake for these respective programmes.
• Implementing Pandemic Preparedness Plan: To implement the Public Health Plan which

includes the development of a surge and emergency response plan, in the event of a significant surge in Covid-19 infections.
Due to the potentially localised nature of virus control, the HSE has devised local area action plans which are akin to the response to the Covid-19 lockdowns, providing a local approach to different areas based on their need.
The Department has, however, stated that the overall aim is for an integrated response where local and national measures work in tandem.
On the national level, the HSE will:
• implement bespoke integrated local action plans focused on improving USC performance and alleviating seasonal winter pressures;
• deliver new nationally led, locally delivered initiatives, based on best practice, to enhance admission avoidance, patient flow and discharge during the winter period; and

• continue the implementation of the ongoing initiatives funded through the Winter Plan and National Service Plan 2020/21 and 2021/22, including the provision of additional acute and community capacity.
On the local level, as part of the local immediate action plans, the HSE will:
• make available an integrated response fund so that local governance structures can develop initiatives to respond rapidly to newly emerging challenges during winter;
• set KPI targets for each site as part of the plan;
• engage with sites to develop initiatives requiring longer-term investment and implementation to drive improvements in USC activity as part of three-year USC Improvement Programme; and
• establish local integrated governance structures and implementation teams to monitor and report initiative implementation, KPI performance, and proactive responses during the winter period.


As we come to the end of 2022, I have been reflecting on the work my team have accomplished this year to prevent outbreaks of vaccine preventable diseases in Ireland, writes Lucy Jessop, Consultant in Public Health Medicine – National Immunisations Lead for the HSE National Immunisation Office.
The National Immunisation Office is a multi-disciplinary team of 20 within the HSE. We manage vaccine procurement and distribution and development of training and communication materials for the public and health professionals to allow for safe, equitable, and highquality vaccination programmes to be delivered in line with Department of Health Immunisation Policy. During the Covid-19 pandemic, we have also
supported the implementation of the Covid-19 vaccination programme and its many updates by supporting healthcare professionals who are offering Covid-19 vaccines and advocating for their patients to get vaccinated.
In 2021, our work mainly concentrated in supporting the rollout of Covid-19 vaccine, and supporting our routine programmes when capacity allowed. However, 2022 has seen a return to
“normal” work alongside supporting the Covid-19 vaccination programme and additional programmes we did not anticipate in 2021.
In April and May, our work in the development and implementation of mobile solutions ScanVax and TrackVax to support the safe and effective rollout of Covid-19 vaccines in Ireland was recognised with the receipt of IT Project of the Year at the CIO and IT Leader Awards and the award of Best Use of Information Technology at the Irish Healthcare Centre Awards (IHCA).
Our winning continued in June, with receipt of the best short presentation for “Views on Covid-19 vaccination of young children in Ireland: Results from a cross-sectional survey of parents” and receipt of best poster for “Preparation for catch up vaccination for Ukrainian people displaced by war – a descriptive piece” at the RCPI Summer Scientific Meeting.
In November, our team was awarded the Best Case Study, Healthcare Provider Recognition Award at the GS1 Healthcare Conference for ‘TrackVax’ and in December our Communications Manager will travel to India to present about the HPV vaccination programme in Ireland at the South Asia Regional meeting being organised by the Coalition to Strengthen the HPV Immunisation Community and HPV Prevention and Control Board.
This year we also published some important Irish research titled Addressing Vaccine Hesitancy in General Practice: A National Survey of General Practice Nurses and Views on Covid-19 vaccination of young children in Ireland, results from a cross-sectional survey of parents
The Covid-19 vaccination programme continued to evolve and with that so did our materials and messages to
healthcare professionals. The recent introduction of adapted Covid-19 vaccines has not only provided additional protection to people who get vaccinated but meant that all materials required updating to ensure we continue to support vaccinators in providing up to date and accurate information. We implemented a Keep Up to Date digital campaign during the summer to highlight the importance of babies getting vaccinated at two, four, six, 12, and 13 months of age through GP practices as we saw from published data that uptake of vaccines had decreased during Covid-19. With a return to travel we wanted to prevent outbreaks of diseases like meningococcal disease and polio which can make children very sick and leave them with lifelong changes that affect their health.
In October, the seasonal influenza vaccination programme was launched and to date over 800,000 eligible people have come forward to get their flu vaccine this season.
We are also encouraging people over 65 to get their pneumococcal vaccination through a digital campaign and working with health professionals and stakeholder organisations to develop short video messages to ensure people have access to accurate information and come forward to get protected.
We have just finalised plans for implementing the Laura Brennan HPV catch up vaccination programme, which will offer an additional opportunity throughout 2023 to get vaccinated for eligible people who did not previously accept the invitation to get vaccinated. I hope people will avail of this opportunity as the more young people vaccinated and women screened the better the spread of HPV infection can be controlled. Since the programme was introduced in Ireland in 2010 over 500,000 people have received their HPV vaccine course, which will move us closer to the global elimination of cervical cancer.
When planning our work for 2022 we did not anticipate we would also be supporting people who came to Ireland from Ukraine and supporting our colleagues in the HSE in the rollout of a monkeypox vaccination programme.
The declaration of war in Ukraine has resulted in over 50,000 people coming to Ireland from Ukraine. We wanted to support these people with accurate
“Since the programme was introduced in Ireland in 2010 over 500,000 people have received their HPV vaccine course, which will move us closer to the global elimination of cervical cancer.”
information about vaccination programmes in Ireland to try to prevent outbreaks of vaccine preventable diseases. We quickly built relationships with health professionals now living in Ireland from Ukraine and developed bespoke materials which are community focused and address the most common queries using terminology and in a language they understand.
In July 2022, the WHO declared monkeypox a public health emergency of international concern. My team quickly developed materials to support the HSE vaccination programme with input from the community who are being offered the vaccine and ensuring materials were translated into Irish, French, Spanish, and Portuguese to support as many people as possible.
My team and I continue to “rise to the challenge” and look forward to continuing to deliver a high-quality service on behalf of the HSE in 2023.
Lucy Jessop graduated from Cambridge
W: www.immunisation.ie
Social: @hseimm on Twitter and Instagram and National Immunisation Office on YouTube.
University and worked in paediatrics before training in public health medicine in London.
She worked as a consultant in public health in Buckinghamshire for five years, leading on maternal and child health including immunisations. In 2014, she moved to work as a Consultant in Health Protection in Northern Ireland and was the lead for childhood immunisation programmes which included being the Northern Ireland member of the Joint Committee for Vaccinations and Immunisations (JCVI) in the UK.
In 2019, she took up the position of Director of the National Immunisation Office in Ireland, where she leads the implementation and improvement of all the national immunisation programme in line with Department of Health Immunisation Policy. She is a member of the National Immunisation Advisory Committee (NIAC) in Ireland and is a passionate advocate for immunisations across the life course.

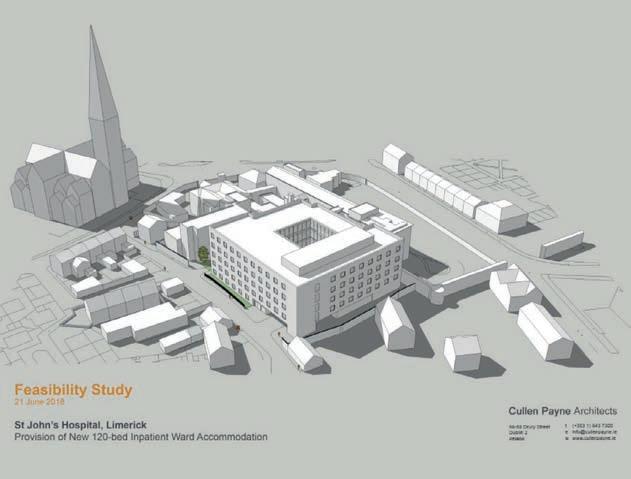
Our strategy, which has been developed with input from our staff, patients, and healthcare partners, lays out a clear five-year plan with a focus on developing and improving our services to patients.
A key pillar of the strategy is building a 150-bed state-of-the-art new unit. The bottom line is that if St John’s can expand its excellence to do more and treat more people, there will be an instant return on this investment.
The strategy was developed by the board following deep consultation with all staff, its partners at the University of Limerick (UL) Hospitals Group, UL, GPs, the St John’s Hospital Patient Partnership Forum, and the wider public. It is built around the hospital’s vision of being a leading provider of healthcare services where innovation and excellence are at the heart of the patient experience.
The proposal addresses the necessary capacity requirement to tackle public waiting lists by accommodating a very
significant proportion of the scheduled care work in the region. It provides solutions to the critical needs associated with the public waiting lists. St John’s already has the sixth busiest endoscopy list and 12th busiest elective surgery list in the country, as well as the busiest LIU in the mid-west region and second busiest in the country.
The strategy is both patient and people/staff centric but very much contingent on the delivery of the new, state-of-the-art 150-in-patient bed facility that will take the hospital from an 89 to 200 bed hospital. The new facility will deliver an additional 31,390 bed days per annum in the Limerick region and meet HIQA and SARI standards for infection, prevention, and control. It will also deliver a safer patient environment,
and an increase in in-patient access by 150 per cent.
Our infrastructure development plan over the next five years forms a key element of our strategy. It will build on the strong foundations that presently exist within our clinical service models and will help to signpost our direction for the future.
Underpinned by the national strategy for healthcare reform, we are evolving our plans to enable us to meet current and future challenges associated with the reform agenda.
The impact of the Covid pandemic on clinical services has resulted in the need to speed up service transformation to achieve fully integrated care through redesign, financial resourcing, and resources to support implementation of the Sláintecare Reforms for Healthcare, working with HSE partners in the acute and community sectors to transform service provision in the mid-west.
Our focus lies on proactively responding to healthcare needs by ensuring we have the capacity to safely deliver services in the post Covid pandemic era, to reduce public waiting lists and speed up where we can on the further development of integrated care pathways between our hospital and the community. Our plans emphasise the connections between the high-quality services we provide while working with our HSE partners to achieve better outcomes, more effectively.
We propose to undertake a programme of building and clinical service developments that will greatly assist in speeding up and enhancing the delivery of care. With an emphasis on transformational change at local level, each element of our plan facilitates the upscaling of services to enhance overall service provision in Limerick and the
mid-west. Our plan has a particular focus on scheduled care, clinical support and recovery services and management of patients with chronic illness who require a step-up from community level care.
There are important levers required to support the progress of each aspect of these developments, the biggest challenge being capital investment. The condition survey of our hospital commissioned by the HSE in 2018 shows a clear and cogent case for serious capital investment in St John’s Hospital. This five-facet survey report on the existing buildings outlines clearly their physical and functional deficiencies which strengthens the case for a new bed block.
Speaking at the strategy launch in July 2022, CEO of St John’s Emer Martin said: “St John’s has made an incredible contribution to healthcare in Limerick for almost two-and-a-half centuries and to this day delivers outstanding results. However, it has also been long since acknowledged that the facilities here are simply not fit for the purpose or the people; our exceptional people who come to work here every day and the patients that they give that exceptional care to. That, essentially, is what this strategy is all about, finding a way to deliver this outstanding care in a modern, high-tech hospital to more people across Limerick and the midwest.
“So, by any measurement, except of course for the facility itself, St John’s is a model hospital, and it makes absolute sense to not only address the shortcomings in the existing hospital but, in doing so, give more people access to this standard of care in the mid-west. We have the capacity on the site to do this and in a region that clearly needs key solutions like this to help address pressures on the system. It’s a win-win for healthcare in the mid-west, for the UL Hospitals Group and the people of the mid-west.”
Martin added: “We recognise that what lies ahead may be challenging but we have the determination, resolve and resilience to fulfil our plan. The bottom line is that if St John’s can expand its excellence to do more, and treat more people, there will be an instant return on this investment.”


• An elective hospital of choice for acute medicine including specialist areas of respiratory, renal and endocrinology services
• To increase our medical assessment unit service to a seven-day service
• Continue to operate the busiest injury unit service in the mid-west
• Develop rapid access clinics in our key speciality areas
• Continue our role as a regional service provider for our clinical recovery and support unit
• Continue our role as a regional service provider for interventional pain treatments
• Enhance our role as a regional service provider for endoscopy and bowel screening
• To further develop our elective surgery including extended stay surgery and as a key provider of diagnostic work, e.g., radiology
• Enhance our role as an exemplary teaching hospital for multidisciplinary staff in conjunction with the University of Limerick and UL Hospitals
St John’s Hospital
St John’s Square, Limerick, V94H272
T: (061) 462 222
W: www.stjohnshospital.ie
• Enhance our role as a leading provider of innovative solutions to healthcare problems in conjunction with the University of Limerick and UL Hospitals Group
Delivering change and adding value through transformation programmes in healthcare

Life expectancy 82.8 years – 1.5 years higher than EU average
Self-perceived ‘bad’ health status: 3.9% of population – fourth lowest in OECD
Infant mortality rate: 3.1 per 1,000 births – 0.1 below EU average
Source: OECD 2022
Cancer deaths: 234 per 100,000 population – eighth highest in OECD
Lung cancer: 18% five-year survival rate – 3% higher than EU average
Prostate cancer: 91% five-year survival rate – 4% higher than EU average
Childhood leukaemia: 88% five-year survival rate – 3% higher than EU average
Sources: OECD 2022 and CSO 2022
32% of population with access to medical card
10% of population with GP visit card
46% of population covered with health insurance
20% with neither health insurance nor medical card
Source: OECD 2022
Suicide rate: 9.4 per 100,000 population
Suicide deaths 2021: 399 – 59 higher than 2020
Male suicide deaths 2021: 302
Female deaths by suicide 2021: 97
Sources: OECD 2022 and CSO 2022
3.3 doctors per 1,000 population – sixth lowest in the EU
25 new medical graduates per 1,000 population – highest in the EU
12.9 nurses per 1,000 population – 4.5 higher than EU average
2.9 hospital beds per 1,000 population – third lowest in EU
Pre-Covid, hospitals ran at 95% occupancy rate, above ‘safe’ classification
Source: OECD 2022
Ireland health spending as a per cent of GDP 2020: 7.1%
OECD average health spending as a per cent of GDP 2020: 9.7%
Health expenditure 2020: €26.5billion – equivalent to €5,284 per person
Source: OECD 2022
Delivering change and adding value through transformation programmes in healthcare

12,553 presentations of self-harm in 2020, affecting 9,550 people
1 in 500 people self-harmed in 2020
1 in 4 people who presented as self-harming had a repeat incident in 2019
68% received an assessment in the presenting hospital 80% received a follow-up recommendation upon being discharged from hospital 11% left hospital before a recommendation of treatment had been made Presentations went down by 12% in March, 22% in April, and 11% in December, coinciding with the introduction of Covid restrictions
Source: National Self Harm Registry 2021

As CORU CEO and Registrar, Ginny Hanrahan approaches the end of her tenure, she has been reflecting on the achievements on the team she leads.
Every day across Ireland, tens of thousands of people benefit from the care and compassion of health and social care professionals. From occupational therapists to optometrists and from social workers to speech and language therapists, there is not an Irish family whose life is not touched by some of these professionals. Other professions regulated by CORU include physiotherapists/physical therapists, dietitians, dispensing opticians, radiographers, radiation therapists, medical scientists, and podiatrists.
For the past 15 years, Ginny Hanrahan has been tasked with ensuring the quality and consistency of that care. As the inaugural CEO and registrar of
CORU, Ireland’s multi-profession health and social care regulator, Hanrahan has overseen the introduction of statutory regulations for a dozen professions, while plans are well underway for adding a further five to that list.
Public protection is a phrase Hanrahan repeats often. “This is the raison d'être,” she explains. “We currently regulate the work of over 24,500 health and social care professionals. Each one of our regulated professionals could have dozens of patients or service users a week. Protecting those people is our mission and this guides everything we do.”
CORU was established in 2005, under the Health and Social Care Professionals Act by Mary Harney who was then Minister for Health to regulate a range health and social care professions, many for the first time. The journey for Hanrahan started in May 2008 when, having been Head of Clinical Services in Dublin’s Beaumont Hospital for over seven years, she took on the role of CORU CEO/Registrar.
“The concept of a multi-profession regulator seemed completely alien to many people. But all I could see was a huge opportunity to improve the experience of patients and services users nationwide by setting statutory standards for the professions to be regulated. I am glad to say my optimism paid off and the results have been quite clear.”
The first major milestone for the fledgling regulator was the opening of the social worker register in 2011. “The vast majority of Ireland’s social workers enhance the lives of those who need their services, but by opening this register we established a legal set of standards, including the first statutory code of professional conduct and ethics for social workers, as a guide to the professionals. In December 2014, we opened the Fitness to Practise function of our regulation, to provide a place for people to turn to if things go wrong.”
Now having repeated the opening of registers 11 times you could forgive Hanrahan for taking the moment for granted, not so she says. “It is the culmination of years of work from the CORU team, countless volunteers and the professions themselves. It sends a powerful message to its service users/patients about the quality of care they can expect to receive. The opening of a register is a huge milestone for us and one we always celebrate.”
Fitness to practice, the process of investigating and adjudicating on complaints, is often seen as the central
pillar of regulation, but Hanrahan says this is not the case. “Clearly it is vital, when things go wrong that we act very swiftly. There have been some difficult and high-profile cases, including striking people off when that has been in the public interest. But I do not like to dwell on these exceptions. The overriding legacy of CORU is the high standards of education, conduct, and ethics that are demonstrated by the vast majority of registrants.”
CORU also has the powers to act against any individual found using one of CORU’s protected titles without registering with CORU. “We expected this be a rare occurrence, but it has happened and has led to criminal convictions. CORU registration is now the ultimate Q-mark for the professions we regulate. To maintain trust in that, we must maintain its utmost integrity.”
Hanrahan, who is due to retire in mid2023, reflects on the achievements of her team over the past decade and a half but is equally focussed on laying the foundations for the future. “We now have 12 regulated professions and more on the way. It is a huge achievement from the entire CORU team which includes an executive staff of 75 and the sterling work of the voluntary Health and Social Care Professionals Council under the leadership of Mo Flynn, as our Chairperson, committees of council and the 12 profession specific registration board members. All of our bodies, have a majority of lay/non-professional members, who bring the voice of the public and service users to any decisions we make.”


Hanrahan is positive about the future and confident that CORU will continue to transform public protection for the people of Ireland. “We are entering a new phase of our work. The professions we are now working with to prepare for their registrations, such as social care workers, psychologists, counsellors, and psychotherapists bring new levels of complexity. It would be easy to class this as challenging, but I can only see the opportunity once again to protect the public by working hard to ensure we get this right. Each profession has one opportunity to get their standards of regulation correct – we achieve these. Under our legislation, we will also be working with the final two professions –orthoptists and clinical biochemists.
Standards of regulation have to be balanced to ensure we do not squash creativity and innovation which is required for the development of work for all professions. We also need to acknowledge the incredible work these
“The vast majority of Ireland’s social workers enhance the lives of those who need their services, but by opening this register we established a legal set of standards and provided a place for people to turn to if things go wrong.”
professions have undertaken during Covid and the demands that have been placed on them to ensure that they continue to be engaged with their profession, but also to mind themselves. The high level of burnout that is being noted in research on many of the people who worked so tirelessly through this period – the need for resilience and kindness in regulation has never been more important, to ensure that safe services are delivered to patients and service users.
The need for regulation too is increasing according to Hanrahan who says that this must be viewed in the wider societal context. “We have an ageing population, increasing numbers of people with disabilities living in the community and their changing care demands. Over 30 other professions are keen to be considered for regulation, including clinical engineers, chiropractors, osteopaths, medical physicists, play therapists, to name just a few. Decisions on the regulation of any professions rests with the government. A risk based approach needs to be taken in relation to any decisions, based on the harm that can be potentially caused by any professional group and whether a higher standard of consumer protection could
be more appropriate for a number of professions.”
Against the backdrop of these societal pressures and with CORU expected to grow to over 40,000 registrants by the middle of the decade. Hanrahan says the model of regulation will need to be reformed. “We have reached the point where ‘what got us here will not get us there’. Our new statement of strategy for 2022-2026 commits us to develop a more sustainable regulatory model that is focused on right touch regulation, always ensuring that regulation is proportionate, consistent, targeted, accountable, and agile.”
While changes lie ahead for how CORU operates, Hanrahan is confident that one thing will not change and that is the why. “CORU will continue to be guided through every change it makes by ensuring it is first and foremost guided by that mission to protect the public.”
T: 01 293 3160
E: info@coru.ie
W: www.coru.ie


As the Sláintecare programme nears its fifth year, its implementation has been curtailed by factors such as the Covid-19 pandemic and high-profile resignations, ultimately stymying the project.
Sláintecare was first proposed in 2017 following an Oireachtas report which outlined the need to establish a universal, single-tier healthcare system which can be accessed by all Irish citizens. The principles of the programme were supported by all the main political parties in the Dáil.
The programme has been curtailed by the Covid-19 pandemic, as well as a lack of pace in delivery which culminated in three high-profile resignations from the programme in 2021, including former Executive Director Laura Magahy, who cited frustration at the slow pace of the implementation of the programme.
Anthony O’Connor also resigned from the council in late 2021, stating in a
letter to Health Minister Stephen Donnelly TD that the original culture of Sláintecare had been “bulldozed” and that the Government’s replacements were “incongruous” with the principles of the reforms.
Whilst originally under the remit of the Department of the Taoiseach, in 2022, the Department of Health approved measures to devolve the implementation of Sláintecare into regional health areas.
On 26 October 2022, the Oireachtas Health Committee heard from Leo Kearns, the chair of the Regional Health Areas Advisory Group who suggested that the regional health area delivery
process is at risk of being curtailed by the daily workload of senior figures in the HSE and the Department of Health.
“It is difficult to see much real progress being made on implementation unless senior leaders in HSE and Department of Health are freed up from some of their ‘business as usual’ responsibilities to devote significant thought and time to this,” Kearns told the committee.
Meeting in June 2022, the Sláintecare Programme Board set out a target of ensuring the delivery of six regional health areas by the end of the year.
The regional health areas are designed to ensure that there can be a localised response per each of the six areas. However, differing local responses are

not a guaranteed success, and there is the potential for there to be a lack of a consistent strategy to underpin developments in the healthcare system throughout the State.
The Sláintecare Implementation Strategy 2021-2023 outlines a vision for healthcare and immediate actions which are consistent with the original Sláintecare report. The implementation strategy’s foreword, written by the former Executive Director Laura Magahy, reiterates a commitment to the vision of a universal single tier healthcare system.
Budget 2023 allocated a record amount (€23.4 billion) in funding to the heath service. However, this is mostly targeted at reducing waiting times within the existing HSE framework, rather than a fundamental reform of the healthcare system.
In his statement on the budget, Health Minister Stephen Donnelly TD made no mention of Sláintecare, and it is unclear specifically how much of the funding in the health budget will be for supporting the reforms as part of the project.
The budget did allocate funds with the aim of eliminating inpatient charges, with the aim of saving patients up to €800 per year. However, the inequality in health outcomes for people who rely on the HSE, compared with those who have access to private healthcare remain significant. The median treatment response time in private healthcare is five days, compared to a 17-day median wait with the HSE.
This is underpinned by an increasing trend in the number of Irish citizens who access private healthcare, with most reporting a higher satisfaction level than those who use the HSE. This suggests that those who can afford to seek private healthcare are doing so amid a perception that the HSE cannot adequately meet their needs.
Figures on health outcomes in Ireland are generally strong, with Ireland recording the highest self-perceived health outcomes in the EU, with 83 per cent stating that they were in good health. However, figures from the Department of Health relating to health outcomes in the State in 2021 reveal
that Ireland has a lower doctor-topatient ratio than both the EU average and the OECD average.
The Department of Health’s Statement of Strategy 2021-2023 does state that one of its five strategic priorities is making access to healthcare fairer and faster, citing the principles of Sláintecare as the means to achieve this.
The percentage of the population who hold a medical card, as of 2020, remains below the figure for 2009, despite 2020 being three years after the launch of the strategy, the stated aim of which is to work towards a universal healthcare model.
Whilst measures have successfully been taken under the aegis of Sláintecare, such as the Sláintecare Integration Fund, which piloted 105 of the 123 intended projects throughout the HSE in 2021, the bigger picture of delivering a universal healthcare system has fallen down the list of priorities for the Government.

A report by the Economic and Social Research Institute (ESRI) has found that there was a decline in perinatal mortality over the 2000s and 2010s, but that this decline was experienced at a much lower rate for unemployed mothers.
The report found that the perinatal mortality rate, which measures the number of stillbirths and infant deaths within one week of birth, declined from 8.3 in 2000 to 5.4 in 2019. However, for unemployed mothers, although there was a decline, the rate was between 1.6 and 2.2 times the rate of mothers in the higher professional group, and this rate remained elevated throughout the last two decades.
Looking at the standardised mortality rates, there was a clear correlation across the board of economic background and health outcomes. There was furthermore a trend whereby health outcomes got worse between 2000 and 2009, before subsequently improving again over the 2010s.
Given that 2009 was measured at the height of the recession and subsequent rise in poverty, one can infer that more poverty results in worse outcomes, and that the uptick in better health outcomes came for those who subsequently had a higher standard of living as Ireland came out of the recession.
The report also found that agricultural workers and farmers are on average over 2.4 and 2.3 times more likely to die of circulatory disease than employers and managers.
It is roughly between 1.7 and 2 times more on average for unskilled-manual, skilled manual and non-manual. There is very little difference between employers and managers and the unknown and higher and lower professional groups.
Whilst the mortality rate fell across the board between 2000 and 2019, the rate at which it fell varies vastly depending on economic background, with mortality for low-earners falling a rate which was considerably smaller than those from an economically prosperous background, resulting in a wider equality gap than existed in 2000.
The report also included analysis of Covid-19 mortality. It showed that, between March 2020 and May 2021, those in disadvantaged socio-economic groups accounted for higher proportions of deaths relative to their shares in the population aged 65 and older.
While the numbers of deaths in non-white groups were very small overall, those with black or Asian Irish ethnicity accounted for slightly higher proportions of Covid-19 deaths than their respective shares who were aged 65 and above.


The Irish Association for Counselling and Psychotherapy (IACP) was honoured in November 2022 to be invited to appear before the Joint Committee on Education, Further and Higher Education, Research, Innovation and Science, as part of its examination of Mental Health Supports in Schools and Tertiary Education.
Lisa Molloy, Chief Executive Officer, had the pleasure to participate in a round table discussion alongside representatives from: the HSE National Mental Health Services, Jigsaw, Spunout, the Psychological Society of Ireland, the Irish Society for the Prevention of Cruelty to Children, and the Irish Council for Psychotherapy.
The IACP has been calling for the introduction of access to school counselling and psychotherapeutic supports for many years, and was delighted with the news of the allocation of €5 million for an in-school counselling pilot for primary schools.
School-based counselling programmes are established in over 60 countries worldwide and are mandatory in 40. They have been operating at secondlevel education very effectively in the United Kingdom for many years.
Following on from the success of school-based counselling at second level, there is now a pilot project in Northern Ireland, called Happy Healthy Minds. The evaluation report of this programme will provide invaluable learning to the Irish Government in determining the model for the primary school pilot here.
The bottom line is that having timely access to professional qualified counsellors and psychotherapists through schools has been proven to be highly effective.
Growing support for this was clearly captured in our last nationally representative general public survey. This survey conducted by Behaviour and Attitudes from April to May 2022 has produced some timely topline results.
These results include a finding that 93 per cent of Irish adults think that counselling and psychotherapy should be made available for children and young people through schools. This is a 5 per cent increase from the already high level of pre-pandemic support of 88 per cent in 2019.
Growing international evidence for the benefits of school-based counselling highlights accessibility, de-stigmatisation and support for children, teachers, and parents and caregivers.
The IACP believes early intervention is critical and access to counselling and psychotherapeutic services through schools, as research indicates, is highly successful with positive outcomes not only for children but also for the wider community.
The IACP represents more than 5,000 members, based in communities nationwide and is the largest counselling and psychotherapy association in Ireland.
T: 01 230 3536
E: ceo@iacp.ie
W: www.iacp.ie



We are moving into a period of unprecedented change and there are many new and existing challenges facing healthcare systems. Our healthcare consulting team has identified seven challenges that will continue to impact healthcare providers into 2023, writes Elaine Daly, Partner –Head of Business Consulting at Grant Thornton.
Demographic change is one of the greatest challenges of our time. As the population ages, healthcare systems will face challenges to meet the needs of an older population. The number of people aged 65 and over in the Republic of
Ireland was estimated at 696,300 in 2019 by the Central Statistics Office and is projected to more than double to 1.56 million by 2051.
The long-term impact of Covid-19 on increased service demand and health outcomes for the older person will evolve
over time. However, there are concerns regarding the impact of delayed access to care and reduced physical and social activity during the pandemic.
Healthcare systems must respond appropriately and adapt their working practices to meet these changes and include specific mechanisms for health promotion, prevention, treatment and rehabilitation suitable for the needs of older people.
47.5 per cent of the Irish population now has private health insurance according to the Health Insurance Authority (HIA). In the context of private health insurance, patient consumerism is more important than ever as medical costs and insurance premiums rise. Consequently, patients actively pursue the best value for their investment whilst also expecting high-quality care. In tandem with this, tolerance for time-consuming processes and delays has declined, with patients now seeking organisational efficiency and a positive experience.
Customers currently have ease of access to digital tools and technologies to make informed decisions surrounding their health and wellbeing. The empowered customer demands a mix of both physical and digital interaction. Within the last few years, the demand for this has grown with patients seeking personalised care outside the hospital setting. A positive patient experience is a key factor for patients when choosing between healthcare providers.
Providing high-quality, sophisticated care has become increasingly challenging and expensive. This can be attributed to several factors, such as the cost of developing new medicines, purchasing of specialised equipment, development of
new facilities, and costs associated with recruiting additional staff.
The onus lies on healthcare providers to understand and respond to issues posed by costs, whilst still delivering highquality care to their patients.
The availability of suitably qualified staff is an increasingly significant problem in Ireland and internationally. Globally, healthcare providers are competing to recruit and retain staff. Burnout is a significant risk, as the challenge of delivering multiple care pathways while reducing waiting lists places a burden on employees. As the labour force ages and service demand increases, the gap between workforce supply and demand is expected to widen.
Consequently, these recruitment difficulties may limit the ability to respond to increased consumer demands and hamper the delivery of core and new service developments.
Breakthroughs in digital innovations are happening at an exponential rate and the challenge is for healthcare leaders to keep pace with these innovations. Healthcare providers must respond to the latest findings and innovations, and ultimately perform cost-benefit analyses of the emerging options to determine how these innovations can best help their clinicians deliver care.
The growth in digital innovations presents an increased risk of serious data breaches. As healthcare functions continue to move online as a result of the pandemic and changing consumer behaviour, it is important to ensure these processes are protected from outside threats. Empowered customers will demand transparency to ensure their data is stored securely and used appropriately.
According to the World Health Organisation (WHO), health infrastructure is one of the largest consumers of energy. Hospitals use twice as much energy per square meter as conventional buildings because they

must accommodate patient needs and adhere to regulatory requirements regarding performance guarantees.
According to a WHO report, the Covid-19 pandemic response has resulted in tens of thousands of tonnes of additional medical waste, placing enormous strain on healthcare waste management systems globally and endangering both human and environmental health. These findings have highlighted the urgent need to improve waste management procedures and energy consumption.
The effects of humans on the environment are growing and the resulting dangers are causing illness and injuries, lowering productivity, and taxing health systems while also degrading quality of life. Improvement in human health and life expectancy over the past 150 years has been largely attributed to the reduction of environmental pollution and developments in hygiene. However, even now, tainted food, water, and air
continue to be significant global causes of pain and demise.
As global warming and extreme weather events increase the hazards to human health, healthcare systems will need to undergo change. Effective action depends on an understanding of the relationship between preventing climate change and human health.
Carbon dioxide and other environmental pollutants produced by healthcare systems are significant. Thus, in order to mitigate further environmental and climate change, efforts must be made to lessen the global impact of healthcare providers and the healthcare sector.
Elaine Daly Partner – Head of Business Consulting
Grant Thornton
E: elaine.daly@ie.gt.com
T: 01 3805 895





Breda Smyth, who became the first female Chief Medical Officer in the State in 2022, and Stephen Mulvany, who has been acting CEO of the HSE since October 2022, are the two most prominent figures in Irish healthcare.
Breda Smyth became the first woman to serve as CMO in the history of the State when she was appointed to the role, originally on an interim basis in July 2022, before being appointed permanently in October 2022.
Smyth has extensive experience leading national programmes across public health, serving as senior responsible owner on the HSE Public Health Reform programme in 2019. She was the national lead on the Health and Positive Ageing Project, and developed and published the Healthy and Positive Ageing for All: Research Strategy 2015–2019 in collaboration with the Department of Health in 2019. She was also the national stroke prevention lead in the Stroke Clinical Programme from 2010 to 2014, leading the pilot opportunistic screening for atrial fibrillation.
Throughout the Covid-19 pandemic, Smyth, who hails from Straide, County Mayo, played a role as a member of the National Public Health Emergency Team (NPHET), the Rapid Testing Expert Advisory Group and as a founding member of the Covid-19 Irish Epidemiological Modelling Advisory Group
Smyth completed her primary degree in medicine (MB, BCh, BAO) in University College Galway (now the University of Galway). She then continued her training in the Royal College of Physicians of Ireland (RCPI), undertook a master’s in Public Health in University College Dublin, a Medical Doctorate in NUI Galway (now the University of Galway) and a post-doctoral fellowship in the University of California, Los Angeles. Smyth was conferred as a member of the Faculty of Public Health Medicine of Ireland in 2005, and, in 2013, was made a fellow of the Faculty of Public Health Medicine in Ireland.
She previously was professor for public health medicine in NUI Galway and a consultant in public health in HSE West.
Following the retirement of her predecessor, Tony Holohan, Smyth was appointed as Chief Medical Officer of Ireland – on an interim basis from 15 June 2022 – by Minister for Health Stephen Donnelly TD.
Outside of work, Smyth is also an accomplished musician and has toured and performed worldwide as a violinist with Michael Flatley’s Lord of the Dance and Feet of Flames which included


performances at the Ryder Cup and the Red Cross for the Royal Family in Monaco.
She released her debut album Basil and Thyme in 2002 and was subsequently nominated as female traditional musician of the year by the Irish Music Magazine in 2003. She hosted the Irish Music Magazine Awards in the National Concert Hall, Dublin in October 2003.
Smyth has also undertaken extensive research including a medical doctorate, on Mortality Inequalities in Ireland from 2000 to 2006 between 2007 and 2009 for which she received the Zachary Johnson Bronze Medal. She was also awarded a post-doctoral fellowship in the University of California, Los Angeles from 1998 to 2001.
Stephen Mulvany assumed the role of Acting Chief Executive Officer of the HSE in October 2022. Prior to this, Mulvany had been Chief Financial Officer since 2014. In that role he was responsible for financial planning, operational planning, and service delivery of the organisation.
His strongest achievements are seen as having ensured that a “strong and integrated financial performance system” was in place, assisting former CEO, Paul Reid, in all strategic and operational matters relating to
budgetary management, forecasting needs, and the securing of funding for health and social care services.
He has worked for over 30 years in the public sector. Alongside his role as Chief Finance Officer, he had served as National Director for Mental Health, regional director for operations in the Dublin North-East region, and working as a hospital networking manager in Ardee, County Louth.
Key focuses of Mulvany’s career in the public sector include stewardship, accountability, financial planning, management, as well as corporate and professional leadership.
Mulvany has held various roles throughout the HSE including Chief Financial Officer, National Director for Mental Health, National Director of Finance and Regional Director of Operations in Dublin North East as well as Hospital Network Manager. Before this he worked for several years in local government.
Mulvany is a certified accountant, having graduated from Griffith College Dublin with a postgraduate diploma in management and application of information technology in accounting, an MSc in management practice, as well as a certificate from the Institute of Directors.


Children’s Health Ireland currently provides paediatric services in Crumlin, Temple Street, Tallaght, and Blanchardstown at Connolly Hospital. The highest number of children and young people is in the eastern region of Ireland where the rollout of the National Model of Care for Paediatrics is well advanced.
New facilities for outpatient and urgent/emergency care in Blanchardstown and Tallaght opened in 2019 and 2021 providing local and convenient paediatric services northwest and southwest of Dublin. Services in both new facilities will continue when the new children’s hospital opens.
Our new children’s hospital building is now over 70 per cent complete.
Taoiseach Micheál Martin TD and Minister for Health Stephen Donnelly TD, visited the new children’s hospital in November 2022. Together with children who attended Children’s Health Ireland
services, they planted the first of 400 trees destined for the four acres of gardens and open spaces planned within the 12-acre grounds of the new children’s hospital.
They visited the most progressed areas in the building – including one of the hospital’s 22 operating theatres, the 60bed critical care unit, and an ensuite inpatient room. The new hospital will provide all services for the sickest children in the State, and some allisland services, as well as supporting local paediatric services currently provided at Crumlin and Temple Street
and the inpatient and day care paediatric services at Tallaght.
Ambitious transformation of healthcare requires long-term planning and implementation. The health policy and plan for paediatrics is based on the 2016 National Model of Care for Paediatric Healthcare Services. This model of care stipulates having an integrated network of paediatric services based on two core principles. The first is that children and young people should be treated as close to their home as is clinically appropriate. The second is that national and highly specialist acute services are consolidated in one children’s hospital co-located with a large academic adult hospital. The development of paediatric services in regional hospitals is an integral part of this model of care.
When looking at services in our hospitals in Children’s Health Ireland, we have many excellent services, while others require continued development especially when it comes to providing timely access to patients. It is important to acknowledge achievements in times of change when things are moving quickly. We want to share some recent milestones in Children’s Health Ireland that have enabled us to continue our vision, mission and values and strive to achieve our strategic objectives.
The new Paediatric outpatient and emergency care unit (ECU) at Children’s Health Ireland (CHI) at Tallaght opened in November 2021. This service recorded 34,994 Emergency Care Unit attendances and 15,000 plus outpatient appointments in 12 months. These figures are a tribute to the efforts of many staff to provide care in these new facilities, providing paediatric care and treatment for local children, young people, and their families.
Significant progress has been made this year to increase the number of spinal surgeries undertaken, up by 152 (54 per cent) on the same period last year. Long waiting times have also been reduced with 32 per cent fewer children waiting greater than 12 months and 24 per cent less waiting greater than four months for inpatient care. An increase in OPD referrals and new additions to the waiting list of 30 per cent means that the impact of this increased activity is not visible when looking at total patients waiting. Capacity projects (theatres, beds, MRIs) coming on stream in early 2023 will continue to improve access to our orthopaedic service. CHI also continued to work with our partners in the National Orthopaedic Hospital Cappagh to extend services provided to our patients with non-complex needs on orthopaedic and radiology waiting lists. We continue to implement our model of care as we work towards the new hospital. Our neonatal service (premature and sick new-born babies) in Children’s Health Ireland at Crumlin marked a major step in November 2022 on the way to delivering the neonatal intensive care unit (NICU) in the new children’s hospital and providing worldclass neonatal care. The unit in CHI at Crumlin has six neonatal high dependency beds for babies with additional care needs. Together with six well-established neonatal high dependency beds in CHI at Temple Street, this will provide long-planned specialised services for a particularly vulnerable group of patients.
Children’s Health Ireland is the ninth cancer centre in the Irish healthcare system, currently providing cancer services for children and adolescents up to 16 years of age as the hub of a network of cancer services. CHI warmly welcomed the launch by the National Cancer Control Programme (NCCP) of a framework for the care and support of adolescent and young adults (AYA) with cancer in Ireland. This framework (20222026) focuses on the specific needs and risks of AYA cancer patients. Children’s Health Ireland has planned for an increase in capacity in the new children’s hospital to meet the implementation of this framework, specifically the change in highest age for admission from 16 years old to 20 years old based on best international evidence on clinical outcomes for young people with cancer.
Children’s Health Ireland and our four academic partners of UCD, TCD, RCSI, and DCU collectively agreed to set up a paediatric academic health sciences centre to drive our vision for integrating health services with research, education,

“We are supported by our charity partner, Children’s Health Foundation but none of this is possible without our biggest asset, our staff. They provide the essential factor to make our future possible.”
and innovation to drive better outcomes for patients and attract and retain the best staff.
Minister for Health Stephen Donnelly TD, launched our Healthy Ireland Implementation Plan 2022-2025. Children’s Health Ireland encourages and supports staff, patients, and families to lead healthy lives. By creating a supportive, wellbeing focused working environment, staff are empowered to take personal responsibility for their own health and wellbeing. This in turn will support patients and families with the quality of care they are provided.
We procured our electronic healthcare record (Epic) for our new hospital. It will support safer care, better patient experience and provide a paper light environment as a new Digital Hospital.
We launched our first conference on Global Child Health: Communities Healing the World in Crisis in October. CHI also worked with European Children’s Hospital organisation in providing outreach and supports to the Ukraine crisis. We worked closely with children’s hospitals in Poland to support oncology services for young children from Ukraine.
CHI is proud of the way our staff continue to respond to Covid-19 in 2022 and impacts of high viral rates in communities. The implementation of infection control guidelines across all CHI meant that we maintained our patients’ and staff’s safety through the pandemic, with low infection rates throughout the year. We have seen internationally the high rates of viruses such as RSV in children; our staff are dealing with this challenge through the 2022 winter months.
We are very proud of the staff in Children’s Health Ireland, who despite challenges are making progress in paediatric services. We are supported by our charity partner, Children’s Health Foundation but none of this is possible without our biggest asset, our staff. They provide the essential factor to make our future possible. We are in awe of the care and treatment given to children, young people, and families by staff.
W: www.childrenshealthireland.ie
Delivering change and adding value through transformation programmes in healthcare


With a planned investment portfolio of €5.7 billion under the National Development Plan to 2025, the Irish Government has commissioned analysis of healthcare infrastructure in the State, which has found notable regional disparity in infrastructure capacity and built infrastructure in good but ageing condition.
Two separate reports were published in September 2022 as part of the Government’s Healthcare Capital Investment in Ireland series, the first of which analyses the healthcare infrastructure capacity of the State, the second of which analyses the built infrastructure of healthcare within the State.
Analysis of the healthcare infrastructure capacity in the State found there to be great variation in the distribution of said capacity dependent upon the regional health area. In terms of critical care unit (CCU) beds, regional health areas A
(North Dublin, Meath, Louth, Cavan, and Monaghan), B (Longford, Westmeath, Offaly, Laois, Kildare, and parts of Dublin and Wicklow), and E (Limerick, Tipperary, and Clare) were found to have “significantly more” beds relative to population than areas C (Tipperary South, Waterford, Kilkenny, Carlow, Wexford, Wicklow, part of South Dublin), D (Kerry and Cork), and F (Donegal, Sligo, Leitrim, Roscommon, Mayo, and Galway). In total, the State has 7.7 CCU beds per 100,000 of population, a rate well below the 2020 OECD average of 12, that falls as low as seven per 100,000 in area D and rises as high as 12 per 100,000 in area A.
This disparity is in part explained as being “partially reflective of the presence of national centres of excellence in some regional health areas and the associated higher acuity care provided in these hospitals”. The analysis also notes that the HSE’s multi-year plan Phase 2 looks to deliver 446 CCU beds. The report further states that the number of general hospital beds available per area is “uneven”, with F having 247 beds per 100,000 and C having 207. “The relationship between occupancy and bed capacity in each region is weak, highlighting the need for further analysis of acute care performance,” it states.
In keeping with having the highest rate of CCU beds per population, area A also has the lowest proportion of patients on trolleys per bed, six. All other regional health areas record patients on trolleys per bed in the double figures, ranging from 11 to 13, and areas F, C, and B all report using over 60 trolleys per day.
The number of patients on waiting lists per ambulatory beds available was found to be “highly skewed”, with area F having 36 patients waiting per bed and area E having 12 patients waiting per bed, and other areas ranging from 18-25 patients waiting per bed. Such disparity, the report says, points to the need to facilitate greater inter-regional referrals, and the need to explore the utilisation of day beds on a seven-day basis rather than the current five-day basis.
Levels of access to radiological equipment also varies across areas, with F having 8.4 X-rays per 100,000 population compared to 5.5 in RHA E.
“This may influence the levels of unmet need and delayed discharge in each region,” the report says. 47 per cent of X-ray machines were also found to be over 10 years old, “implying the need for investment and replacement strategy for these assets”.
The second report, an analysis of the healthcare sector’s built infrastructure, found the capital stock of both community and acute facilities to vary significantly, with a “large proportion” of both – 70 per cent of the community estate and 50 per cent of the acute care estate – built over 40 years ago, which “likely has negative associated impacts on maintenance costs, patient safety and efficiency”. The quality of the stock was, however, found to be good in the community care portfolio, where over 90 per cent of all sites received a score of B or above across all four categories measured.
The report notes that €1 billion of the €5.7 billion to be invested is to be spent on the replacement and refurbishment of the HSE residential estate in order to meet Health Information and Quality Authority standards. The majority of this spending will be accounted for by the acute care portfolio, which fares much worse in terms of quality of stock, with
In total, the State has 7.7 CCU beds per 100,000 of population, a rate well below the 2020 OECD average of 12, that falls as low as seven per 100,000 in area D and rises as high as 12 per 100,000 in area A.
Area B (Longford, Westmeath, Offaly, Laois, Kildare, and parts of Dublin and Wicklow)
Area C (Tipperary south, Waterford, Kilkenny, Carlow, Wexford, Wicklow, part of south Dublin)
Area D (Kerry and Cork)
Area E (Limerick, Tipperary, and Clare)
Area F (Donegal, Sligo, Leitrim, Roscommon, Mayo, and Galway)
just 43 per cent of sites having the recommended B rating, and 44 per cent of the portfolio being below the recommended rating for functionality.
€887 million is recommended for spending on acute care settings, with the remaining €121 million to be spent on community care.
The report also notes the portfolio of vacant buildings within the HSE estate, with portfolios of vacant buildings over 20,000m2 in five counties, ranging from 50,000m2 in Galway to 25,000m2 in Dublin. The report states that the HSE is currently engaging with the Land Development Agency on the potential disposal of these portfolios and that “the utilisation of these sites for other purposes where suitable may alleviate
issues around housing and other societal issues”.
In terms of energy efficiency, just 28 per cent of the top 120 energy users within the HSE portfolio exceed a Display Energy Certificate rating of B3, with the report stating that it is “likely that significant investment will be required to achieve carbon abatement targets in the health sector in line with government objectives”.
The report concludes by stating that, along with the aforementioned investment, further research will be needed to determine where to next for health infrastructure, and that the Healthcare Capital Investment in Ireland series will now provide a baseline for such research.

Human health needs to be at the heart of our response to the unfolding climate crisis if we are to succeed in limiting the significant risks to population health. That was the main message to emerge at a major all-island conference on climate change and health in November 2022.
The Joint Public Health Conference on 30 November 2022 attracted close to 1,000 health professionals, researchers, policymakers, and NGOs from across the island and beyond to consider the implications and risks of climate change to our health.
In the wake of COP27, the one-day conference provided a timely opportunity to cast a health lens on the global climate crisis, which has the potential to exacerbate existing health inequalities on the island of Ireland and amplify the pressures on our health and social care systems.
The event was jointly organised by the Institute of Public Health, Public Health Agency, Queen’s University Belfast, Ulster University, University College Cork, and HSE Health and Wellbeing.
In his opening address, Patrick Vallance, Chief Scientific Adviser to the UK Government, said climate change affects us all, is a matter for public health, and is an issue that governments need to act on as a matter of urgency.
Maria Neira, Director of Public Health and Environment, World Health Organization (WHO) also made a strong health argument for addressing air pollution as part of our climate change response. The health community at large, Neira believes, must join forces, harness the health argument for positive change, and highlight the great opportunities and health benefits of taking climate action.
Providing some insights into how health services are striving to become more sustainable, NHS Chief Sustainability
Officer, Nick Watts, said being innovative and open to new ideas is key to making the transition away from carbon, giving an example of using drones to deliver chemotherapy drugs.
In a thought-provoking presentation, John Barry from Queen’s University Belfast outlined his belief that economic drivers, such as consumerism and capitalism, are unsustainable and contribute to socio-economic inequalities and negative health impacts.
The conference was chaired by Jenny Mack, a public health consultant with the Institute of Public Health, who said the successful event helped to focus minds and build new connections across disciplines and policy sectors.
“Climate change is contributing to death, disease, and inequalities across the world and we, on this island, are not immune. Across the globe, we are witnessing more floods, droughts, and heatwaves and we are also seeing the effects closer to home, with recordbreaking temperatures and more extreme weather events than ever before,” Mack says.
“While this all-island conference highlighted the inherent health risks from climate change, it also identified the opportunity to work together and to harness positive health gains through climate action,” Mack adds.
Takeaways from the Healthy Planet Healthy People conference
1. The climate crisis is creating a health crisis.
2. Urgent systemic action is needed to reduce emissions and engage in adaptation to ensure we are preparing for the changing climate.
3. We must seize the opportunity to create a healthy, sustainable, and equitable environment for the natural world, and our health, to thrive.

Climate change is the single greatest challenge of the 21st century, according to the World Health Organization (WHO). It is not limited to impacts on the environment but has direct and indirect effects on our health and everyday lives.
The direct effects are many. Across the globe, extreme heat, rising sea levels, floods, droughts, and storms have already led to tens of thousands of deaths every year.
The roots of the climate crisis are also exacerbating another public health issue, air pollution. It accounts for approximately seven million premature deaths worldwide every year and is a major risk factor for diseases, including heart disease, lung disease, and stroke.
Indirectly, climate change is also impacting our food and water security, increasing the transmission of infectious diseases, disrupting healthcare systems, and displacing communities.
Despite the scale of the challenge, there are opportunities for positive change and health gains, according to Jenny Mack, a public health medicine consultant at the Institute of Public Health and a member of the Faculty of Public Health.
“The World Health Organization has estimated that the value of health gains from climate action should be around double the cost of mitigation policies at a global level. Moving away from fossil fuel combustion, improving active travel infrastructure, adopting a more sustainable food system – these are just some of the ways that we can improve health outcomes and reduce emissions through climate action,” says Mack.
The consensus in the scientific world is that urgent action is required to reach net zero emissions as quickly as possible, to limit global warming to 1.5°C.
Strong leadership, transboundary working, and a “climate in all policies” as well as a “health in all policies” approach are also vital, Mack adds.
“Inaction is not an option. It is time that we come together - north, south, east, and west - to face this public health emergency as the window of opportunity is closing. We must reduce our contribution to greenhouse gas emissions and make sure that our infrastructure, our health services, and our communities are adapting to our changing climate. There is no time for complacency, we must act now to protect the future of our island and to safeguard the generations to come,” Mack concludes.
Key facts about climate change and health:
• Almost 25 per cent of all estimated global deaths are linked to environmental factors.
• Air pollution is a major health threat on the island of Ireland, contributing to an estimated 1,800 premature deaths each year.
• Northern Ireland has experienced a 2,050 per cent increase in the occurrence of extreme weather events between 2000 and 2019 (from four to 86).
• Around 33,000 people in Northern Ireland live in areas at significant risk of flooding.
• At least 300 communities have been identified as being at significant risk of flooding in Ireland.
• Belfast had the highest carbon emissions per capita of UK capital cities in 2019.
E: jenny.mack@publichealth.ie
W: www.publichealth.ie


Sheila McClelland, CEO of the Nursing and Midwifery Board of Ireland (NMBI) talks about its new data report, the State of the Register2022, which provides information for policymakers and the public to inform workforce planning models, and the overall direction of the organisation in the coming years.
As the regulator for more than 80,000 nurses and midwives in Ireland, NMBI’s mission is to protect the public and the integrity of the professions through the promotion of high standards of education, training, and professional conduct.
Our role is to help nurses and midwives make the right decisions for people using health and social care services through our statutory obligations. These are maintaining a Register of Nurses and Midwives; setting standards for education bodies for nursing and midwifery courses; setting professional standards for nurses and midwives; and considering complaints against nurses and midwives who practise in Ireland.
The Irish healthcare landscape is changing with the rollout of Sláintecare and demographic trends showing an ageing population. These developments mean that we will need more nurses and midwives than ever before working in the Irish health sector. In NMBI, we need to be prepared for the changes and we need to be agile in our response to them. It is important that we plan for the future healthcare workforce through evidence-based data. It is also vitally important that data is available to workforce planners, policymakers and stakeholders across the sector as they respond to changing needs.
When we set out on our digitisation journey as part of a wider government initiative a number of years ago, we did so with the dual aims of making the annual renewal process easier for our registrants and collecting a data set which would assist in future planning for our health services.
Thanks to the digitisation of our annual renewal process and the engagement of our registrants, we can now provide valuable insights into the nurses and midwives registered in Ireland for the first time.
Last October, we published the State of the Register2022, providing a breakdown of the number of nurses and midwives registered in Ireland, what division they are in, their age and gender, and where they are located across the country.
We can see that the number of practising nurses and midwives in the country is increasing. This is driven by the increase in undergraduate numbers and ongoing overseas recruitment of nurses and midwives to work in Ireland.
As of 1 June 2022, there are 81,431 nurses and midwives on the NMBI Register, with 75,871 self-declared as currently practising; and of these, 66,471 state they are patient-facing in their role.
The report also reveals that more than 90 per cent (68,310) of all nurses and midwives registered in Ireland are women, while the majority of new registrants in the past year came from overseas, outside the EU.
The 12 months from 1 June 2021 to 31 May 2022 saw a total of 4,937 applicants joining the register, with 1,555 of these qualified in Ireland, 3,021 from outside of the EU and 361 from EU countries.
The top overseas countries for new registrants were India (2,364), Philippines (391), United Kingdom (250) and Zimbabwe (132).
The report also provides a breakdown of registrants across practice areas:
• General nursing continues to be the most common area of practice, with 54,797 active nurses working in this area.

• The second highest number of nurses practising are psychiatric nurses (7,377).
• There are 3,999 practising intellectual disability nurses and 3,371 practising children’s nurses.
• In the midwives division, there are 9,661 on the Register with 4,561 of these practising and 3,850 in patient-facing roles. However, it is important to note that many of those registered as midwives are also registered and working in nursing divisions of the register. Furthermore, the number of practising midwives increased in the past year.
The full report on our registration figures and statistics is available on www.nmbi.ie.
Following an extensive public consultation last year, we gained valuable insights, suggestions, and practical steps that we can take to improve our focus, efficiency and effectiveness. Thanks to the input from registrants, the public, staff organisations, employers, managers, people using services, advocate groups and other key stakeholders, we have developed our Statement of Strategy 2023-2025
Our aim is to enhance NMBI’s function as a regulator for nurses and midwives
in Ireland and our new strategy sets a clear direction for our organisation over the next three years. We will continue to focus on increased engagement with our registrants, the public and our key stakeholders. Together with the data we now have from the State of the Register, we can develop our education and regulation initiatives. We also look forward to reporting on any changes in the demographics of registrants yearon-year. Our 2023-2025 strategy will be published on www.nmbi.ie in due course.
T: 0818 200 116
E: communications@NMBI.ie W: www.nmbi.ie

Delivering change and adding value through transformation programmes in healthcare

A comparative analysis of European healthcare carried out by the OECD has found Ireland to be performing worse than the European average in unmet healthcare needs, doctors per capita, and hospital beds per capita, but above the average in nurses per capita and ratio of nurses to doctors.
Published on a biannual basis, 2022’s edition of the OECD’s Health at a Glance: Europe allows for an opportunity survey the Irish health system’s performance in the European context.
The OECD defines unmet healthcare needs as there being a time in the previous 12 months whereby people surveyed “felt they needed medical care… but did not receive it”, with a follow-up question then relating to the cause of that unmet need. The report focuses on three reasons: prohibitive costs, excessive travel distance, and overly long waiting lists. The resulting data is then broken down into three categories: those of the lowest quintile of income, the total population, and those of the highest quintile of income.
It is only among those of the highest quintile of income that Ireland performs better than the EU27 average, with 0.5 per cent of Irish high-income earners stating that they had experienced unmet healthcare needs in the previous 12 months, as opposed to a European average of 0.7 per cent of high-income earners. 2 per cent of the State’s total population stated that they had had healthcare needs not met in the previous year, as compared to a European average of 1.8 per cent, and 3.9 per cent of low-income earners in Ireland stated the same, compared to a European average of 3.8 per cent. While Ireland performs worse than the European average in two of the three categories, countries such as France, Slovakia, Romania, Latvia, Finland, Greece, and Estonia all recorded rates worse than the European average in all three categories.
Ireland also performs under the European average with regard to the number of doctors per 1,000 of population. Having had 2.7 doctors per 1,000 in 2010, when the EU27 average was 3.4, the State had 3.5 doctors per 1,000 as of 2020, when the EU27 average was 4.0. Leading countries in this category include Greece (5.8 in 2010 and 6.2 in 2020), Portugal (3.9 in 2010 and 5.5 in 2020), and Austria (4.8 in 2010 and 5.4 in 2020). The share of different categories of doctors in Ireland also differs greatly from the European average, with 25 per cent of Ireland’s doctors being GPs, compared to a European average of 20 per cent, and just 46 per cent of Irish doctors being specialists, compared to an average of 69 per cent.
While Ireland’s number of nurses per capita is ahead of the EU27 average (7.4 and 8.3 nurses per 1,000 population in 2010 and 2020 respectively), the figures for Ireland show that the ratio of nurses to 1,000 population have slightly dropped from 12.9 in 2010 to 12.8 in 2020. Despite this, the State still retains the second-highest level of nurses per capita among the countries surveyed, with only Finland recording a better ratio.
Despite having 12 nurses per 1,000 in population in 2010, Finland has since surpassed Ireland’s ratio, having 13.6 nurses per 1,000 population as of 2020. One possible explanation for the slight fall in nurse ratio in Ireland may be that the remuneration of hospital nurses ratio to the national average wage was 1.2, exactly in line with the European average, but behind countries such as Greece, Hungary, Poland, Czech Republic, Spain, Luxembourg, and Belgium. Such data suggests that, while nursing delivers an above average wage in Ireland and is a common career choice, it does not deliver the remuneration needed to retain and indeed grow the nurses to
population ratio as the Irish population continues to grow.
Given its lower-than-average rate of doctors to population and higher-than-average rate of nurses to population, it is perhaps inevitable that Ireland would have an above average ratio of nurses to doctors, recording a rate of 3.2 as compared to the EU27 average of 2.2. This ratio places Ireland amongst the best performing European states in this regard, on par with Slovenia, and behind only France, Belgium, Finland, and Luxembourg.
Ireland is among the worst performing states in the EU on the metric of hospital beds per 1,000 population as of the 2020 data featured in the OECD’s report, recording a rate of 2.9 beds per 1,000 that places it above only Finland, Denmark, and Sweden.
While data for Ireland’s 2010 rate is not provided, it is notable that all states surveyed – the EU27, Serbia, Switzerland, North Macedonia, Montenegro, Norway, Türkiye, Iceland, and the UK – showed a decrease in beds per 1,000 from 2010 to 2020, except for Bulgaria, Romania, Serbia, and Türkiye. The most pronounced of these falls is that of Finland, which fell from a rate of 5.9 hospital beds per 1,000 in 2010 to 2.8 in 2020.
While the onset of the Covid-19 pandemic since the collation of the 2020 data included will no doubt have led to many of the states increasing the bed to population ratios and arresting the slide that took place throughout the 2010s, the report shows that there remains much work to be done in both Ireland and further afield in Europe.

Date for your diary











Since the launch of Our Public Service 2020 in December 2017 there has been huge progress in the key areas of promoting innovation, digitalising services and improving the development of people and workforce planning. There are currently 370,000 public servants working across different sectors in Ireland, all working to deliver better, more effective services. In 2020 the Covid19 pandemic sharply brought into focus the need for public service organisations to be responsive, resilient and agile. Irelan d’s public services responded well and quickly to change the way they work to deliver services and meet the needs of citizens. A number of reforms already in place under the on-going public service reform agenda greatly facilitated the rapid response to th e challenges emerging from the pandemic — Build to Share ICT infrastructure, the progressive digitalisation of services, a streamlined and centralised Government procurement system, a move to shared services — as well as centralisation of strategic HR capability. Looking to the future, the Making Innovation Real Strategy, the Civil Service Renewal Strategy and Connecting Government 2030 all provide practical roadmaps to build on our culture of innovation. This conference will feature a range of expert speakers who will talk about their innovation journey and look ahead to what’s next as we look to a new future.

Sponsorship and exhibition opportunities
There are a number of opportunities for interested organisations to become involved with this conference as sponsors or exhibitors. This is an excellent way for organisations to raise their profile with a key audience of senior decision-makers from across Ireland’s public services.
For further information on how your organisation can benefit, contact Lynda Millar on 01 661 3755 or email lynda.millar@eolasmagazine.ie
3 The next phase of innovation: What does the future look like?
3 Designing public services for the digital age – Digital by Default;
3 New ways of working; 3 Embedding efficient design techniques in policy; 3 Engaging with the service user – becoming citizen-centric;
3 The delivery of healthcare in Ireland; 3 Integrating innovation into operational and strategic planning; 3 Building resilience into our public service organisations; 3 Innovation as a driver for sustainability;
3 Embracing innovation and technology to transform the delivery of services;
3 All change: planning for the future mobile workforce;
3 Educating our children and young people both now and in the future;
3 Looking at the realities of automation and technology enabled solutions;
3 Sectoral update: health; justice; education; local government;
3 Best practice case studies