
Serving a 24 County Area, Including Birmingham, Huntsville, Montgomery & Tuscaloosa




By SteVe SPenCer
After receiving his PhD from MIT in 2002, followed by post-doctoral work at the University of Washington (UW), Matt Kaeberlein joined the UW faculty, where he focused his research on the biology of aging. Over time, he came to understand that most chronic diseases were associated with aging, and exacerbated by lifestyle, and after nearly 20 years in academia, he wanted to put his findings into practice.
“Our current healthcare system is largely reactive,” Kaeberlein said. “It’s good at fixing sick people. I wanted to work on something to keep people healthy in the first place.”
Kaeberlein met with Dave Sabey, the founder of Sabey Corporation, a large commercial real estate firm. Sabey had


already helped found the P4 Medicine Institute which uses a model structured around personalized, preventative, predictive, and proactive healthcare. The two men spent time talking about the fric-


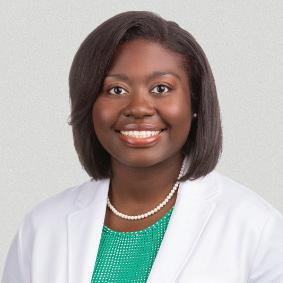
By Laura Freeman
In a time when many physician practices are being purchased by equity groups, and physicians often find themselves employees of a hospital or a business owned by someone else, is it still possible to be successful in your own pri-
vate practice?
Brittney Anderson MD, FAAFP, is a real life example of a family doctor who is building an independent career in modern medicine. Since opening her solo practice, Anderson Family Care, in Demopolis three years ago, her appointment book has been full and she has also navi-

tion points in today’s healthcare system, thinking through the countless problems with the aim of using science-based practices to help people optimize their health.
With this in mind, in September 2023, they launched OptiSpan in Seattle. “We want to build an evidence-based, implementable toolkit that we can give to providers,” Kaeberlein said. “So we set up our own clinic, not so much to earn revenue, but rather to gain experience so that we could build the platform. We wanted to find out if there were interventions or modifications that could give us 80 percent of the benefit for 20 percent of the cost, which could be steps toward population-level proactive healthcare programs. And we’ve learned a lot.”
When a person joins the OptiSpan program, they come to the clinic
gated the business side of private practice.
“I started my career working in a group practice, but I had the nagging feeling that it wasn’t what I was meant to do,” Anderson said. “I wanted to be
(CONTINUED ON PAGE 4)









At the heart of one of the most highly regulated industries in the nation, health care facilities and providers face challenges that draw attention and resources away from their mission to provide quality patient care.
Burr & Forman’s health care team works alongside you to address and anticipate your needs by providing preventative guidance and pragmatic solutions, enabling you to focus on providing care and achieving healthy outcomes.
Alabama Health Care Team
Birmingham | Mobile | Montgomery
Jessie Bekker
Howard Bogard
Richard Brockman
Kelli Carpenter Fleming
Jim Hoover
Catherine “Cat” Kirkland
Garrett Lucey
Angie Cameron Smith

for Gateway Day, which lasts about six hours. “We do broad comprehensive blood work,” Kaeberlein said. “There’s a metabolic collection, biomarkers of inflammation, of cardiovascular health, kidney health, liver health, toxins, and hormones.
Then we do an ultrasound for screening. It’s not a diagnostic tool, but it picks up things like significant plaque in the arteries, kidney or liver problems.
“The goal of our diagnostics is, first, to find out if the person has any serious problems that need immediate attention, and we often find things like prediabetes. Second, we want to establish their current health baseline.
“To get a detailed look at how someone is functioning physically, we do an exercise assessment that includes VO2 max, flexibility, and strength. We get a DEXA scan, which gives us information on muscle mass, fat mass, and bone density. Then we collect urine for urinalysis, and we do multi-genome sequencing.
“ We also do a cognitive assessment, and oral screening. We do this because oral health is both a predictor and a cause of other problems. We have a tool that can image the inside of a mouth, and we have a dentist who reads those images and can make recommendations if there’s any problem there.”
OptiSpan providers will also ar-
range a whole body MRI for people who want it. This helps with cancer detection, as well as quantitative brain imaging. Information on the size and volume of different parts of the brain can be predictive for cognitive impairment. If the team detects any problems from the workups, they’ll refer out for more indepth procedures.
Gateway Day clients also spend several hours meeting with a physician. After that, they’ll meet with a coach to get information about the person’s lifestyle.
The OptiSpan program is structured around what they call the four pillars of health span. Eat – nutrition; move – exercise; sleep; connect - mindfulness and relationships. Kaeberlein and the team believe these components of health are all equally important.
“We use wearables to help with this,” Kaeberlein said. “Everyone gets a sleep tracker so we can assess the quality of their sleep. We also track heart rate variability. And everyone gets a continuous glucose monitor for at least their first 28 days with us. We do this in part to educate people. When someone sees in real time how certain foods and alcohol, as well as exercise and sleep affect their glucose metabolism, we hope that it will give them an incentive to remodel their behavior toward healthier habits.”


continued from page 1
The movement component of the program isn’t as simple as saying that all exercise is good. “There are certain people for whom a particular type of exercise is most beneficial,” Kaeberlein said. “For example, we measure our clients’ flexibility, stability, and strength so depending on where you fall in these areas, you may focus more on one specific type of exercise.
“One thing that’s more common than expected is that there is a subset of middle-aged women who are extremely lean. Often they do a lot of cardiovascular exercise, and you assume they’re in great health. But when we do a body composition, we find that they are under-muscled, and often have a bit of visceral adipose which causes inflammation and metabolic disease. They might be eating a healthy diet, but a certain amount of muscle is needed for the body to regulate glucose, so these women are often pre-diabetic.
“So we give them a resistance training workout program, prescribe a little testosterone, and tell them to back off on the cardio, at least until you get the body composition where it needs to be. And we put them on a diet that has enough protein and calories to build muscle.
“We recently had a woman with this phenotype who looked healthy. But testing showed she had very high lipid levels.
We found a history of micro strokes in her brain, not enough to impair cognitive function or brain health, but warning signs that if this did not get fixed, it was going to get serious quick. We put her on the resistance training program, coupled with testosterone, along with a lipid lowering therapy. We successfully lowered the lipids. So things are going in the right direction, but I don’t want to say she’s 100 percent out of the woods. It’s ongoing. We update clients’ biomarkers quarterly. For someone like this lady, we’ll do the DEXA every quarter.”
Ultimately, the OptiSpan team wants to promote longevity and optimize healthspan through proactive strategies rather than reactive treatments. They aim to redefine healthcare by shifting the focus from treating disease to preventing it entirely.
The last century revolutionized global life expectancy through vaccines, antibiotics, and medical innovations. This century will be defined by optimizing healthspans for all people. The question isn’t just how long we can live, but how well.















like the doctors I grew up with in Prattville, and those I shadowed when I was studying rural medicine, and they were all in private practice. I wanted the freedom to be the kind of doctor I wanted to be and to make decisions based on what was best for my patients.
“Of course, a lot of responsibility comes with that independence. In a solo private practice, it isn’t just your career to think about. Your staff depends on your success for their paycheck and the stability of their livelihood. You have to do the work of running a business as well as being a doctor.
“So I started out with a plan to be successful. I built office hours and business hours into my day so that what needs to be done gets done. To last, a practice has to be profitable, so I did the work up front to confirm that there was demand, learned how to work with insurance, and did the marketing—you never stop marketing. Families change, some move away, and others move into the area.
“But you also have to know your limits. Once your list is full, you can’t keep taking on new patients without adding capacity. There are a limited number of hours in every day. You can’t make more by taking the business side of your work home with you. When I go home every night, I leave the office behind. My patients deserve a doctor who is rested, alert
and able to focus on them.”
Anderson’s interest in healthcare started early, but it was during a trip to Ghana in college that she realized what she wanted to do with her life.
“While I was in Africa, I got malaria and became very ill,” she said. “They took me to a local clinic for help. While I was there, a father brought in his daughter. They had travelled so far to get care. So my first thought was to become a doctor practicing in Africa. But my father pointed out that right here in the rural South, there are so many people who have to travel long distances to get access to health care, especially in the Black Belt.
“So I decided to practice here, where I could provide better access to underserved populations. When I come to work, I know I’m meeting a real need as a family practice doctor. My patients are terrific. I get to see the whole family and watch the kids as they grow. I also have a wonderful staff. It’s so important to choose the right people, make sure they have the training and resources they need, and treat them right. They should know they are valued, respected and appreciated.”
Managing growth so that capabilities match the need is also an important part of designing a successful practice. “Adding a physician’s assistant has been a game changer. I can make better use of
my time. Still, the demand from people in the area who need a family practice doctor are more than I can manage alone. So in November, another physician will be joining me. As you can imagine, a lot goes into choosing the people you want to work with, and setting up an infrastructure where you can work well together,” Anderson said.
Another aspect of teamwork that has to be considered in private practice, especially in a rural area, is having resources you can call on when patients need more specialized care. “Our local hospital is part of the UAB system, and there’s the wonderful MIST system and telemedicine I can call on when I have an unusual case,” she said. “I’ve also built a strong relationship with specialists and hospitals in both Tuscaloosa and Birmingham.
“Now that the local hospital had to close down maternity care, I refer pregnant patients to out of town obstetricians. I can deliver a baby if necessary, but it’s good to have an obstetrician and NICU available, if needed.
“I know when those babies come home, I’ll be looking after them. I like children, but I wouldn’t want to be a pediatrician all day, every day. Being a family practice doctor, I see patients in all age groups, with just about any kind of condition you can imagine. I think variety helps prevent burnout. A specialist tends
With so many medical liability insurers having sold out to Wall Street, there’s an important question to ask. Do you want an insurer that’s owned and led by physicians, with $7.3 billion in assets, and a financial award program that’s paid more than $175 million in awards to retiring members? Or do you want an insurer that’s focused on paying its investors?
Join us and discover why our 90,000+ members give us a 93% satisfaction rating when it comes to exceptional service.
to get very good on a narrow focus, but the tradeoff is that you see a lot of the same thing.
“In family practice, every day is different. In a rural area where poverty is high and access to care is low, patients can have a variety of extra issues complicating their health.”
This is especially true in an area with a high density of populations that have long been underrepresented in clinical studies. In southwest central Alabama, both ethnicity and economics can influence the frequency and type of conditions a physician may see, as well as which medications are likely to be needed.
To help other physicians interested in private practice, Anderson does a twice weekly podcast called Physicians Hanging a Shingle that covers key topics.
“It takes a certain mindset, and you need the planning and systems in place to get things done and stay profitable,” she said. “You are your patients’ physician and the CEO of your own business.”
In addition to running her practice, Anderson serves as chair of the Alabama Academy of Family Physicians and Vice Speaker of the Medical Association of the State of Alabama.
“Private practice is definitely doable and very rewarding,” she said. “You just have to have a solid plan and follow it.”
By Laura Freeman
Cardiovascular Associates has been making history in heart health for almost 80 years. Now the practice is entering a new era of growth encouraged by the renaissance of Baptist Health, a five-hospital system in central Alabama that is undergoing a revitalization following the purchase of 80 percent of its shares by nonprofit Orlando Health.
“This is an exciting time for us,” Practice Chairman John (Tom) Eagan, MD said. “We were working on plans for enhancing our practice and expanding outreach when the new owners came on board last fall. From our first meetings, we could see our mission and their vision were very much aligned. Like us, their focus is excellence in patient care and they are interested in expanding community-based health services so patients don’t have to travel long distances to access state-the-art cardiovascular care.
“The new management for Baptist Health has been very supportive in helping us update technologies and seeing that we have the resources we need. Cobranding to communicate a shared identity known for quality care makes sense.

Now, whenever you see the name Cardiovascular Associates, you’ll also see consistent identification with Baptist Health.
“We’ve also just taken the latest step in our outreach plan by opening a new office in Cullman. For now, we have physicians and some of our staff from other offices seeing patients on alternating days. Eventually, we plan to recruit physicians and staff who will be based in Cullman full-time.”
Future plans also include expanding staffing in other offices. Additional

improvements range from basic updates in the clinic environment to technology upgrades and new equipment, including a new dedicated in-office CT for the Colonnade office scheduled to be installed this fall.
“Orlando Health is doing a great job by using the expertise from both the Alabama and Florida locations to mutually benefit patients and physicians,” Eagan said. “They had a cardiovascular seminar for primary and other referring physicians in Florida, and invited several
of our physicians to speak about the latest developments in the field. When it is our turn to hold a seminar, we can call on their best people.”
Considering the challenges now facing healthcare, there is much to be said for joining forces with partners known for strength, stability and a forward perspective.
Practice Administrator Kevin McIntyre says the internal response he is seeing from staff has been good. “We’re getting a lot of positive feedback,” he said. “Working day to day, our staff sees the small improvements that cumulatively make things better for their patients and their work environment, and they are excited about the bigger improvements like the new dedicated CT. It will give us ultra-fast, ultra-accurate diagnostic data right here in the office.”
Eagan said the word at Baptist Health hospitals in and around Birmingham has been very positive since the change of ownership. “The new leadership started by getting the infrastructure aligned with the quality we want patients to expect, he said. “It began with the basics, like new paint where needed, fixing




By marti WeBB SLay
When neuroscientist Lindsey Smith, PhD, was recovering from breast cancer surgery, she was given instructions to exercise and eat well, but accessible information about how to do that effectively was lacking.
“When I asked my physician what I could do to keep this from coming back, he said, ‘eat right and exercise,’ and that was it. As you can imagine, I needed more information. I was dealing with a completely shattered nervous system, my life had been turned upside down, and it was a lot to manage.”
She decided to take her experience in higher education along with her background in neuroscience, the neuroendocrine system, and pathology, and develop an educational, neuroscience-based program that would have helped her at the time. The result was Synaptic Harbor, which offers neuroscience-based tools for peak performance and well-being.
“It was a combination of my stubbornness and my need for knowledge, structure, and efficiency. So that’s what I began dedicating my time to,” she said. “Initially it was a personal pursuit.”
Smith grew up with an interest in mind-body holistic practices, but pursued a conventional biomedical research-

based education, earning her doctorate in neuroscience from UAB and specializing in brain plasticity, synaptic physiology, learning and memory, hormones and behavior, and later, digital pathology.
Returning to her roots, she explored mind-body tools through modern neuroscience, finding several were backed by research and have emerging clinical relevance. Her primary focus is soundbased tools. “These practices work,” she said. “We have brain scans, cellular and molecular data in health and disease, and evidence of long-term functional brain changes.”
Smith leverages this data to create sound-based integrative learning programs and assistive tools that enhance brain plasticity and stress resilience at
the cellular level. “This brain-body education empowers people with practical neuroscience knowledge, helping them understand how daily choices shape their brains over time and offering actionable frameworks for positive brain change,” she said.
She offers free sound baths through Jefferson County libraries. Participants relax on yoga mats and are immersed in tones from crystal singing bowls and other idiophonic instruments. These hour-long sessions use soothing sounds, guided imagery, and meditation to foster stress resilience and teach about the nervous system, promoting restorative non-sleep, deep rest. She uses the baths to teach stress management and mental resilience techniques, helping participants learn how to achieve healthier lives, better stress control, and improved sleep.
“I want to expand what people currently know,” she said. “Diet and exercise are just two of six key factors. When you look at all the latest data, there is a sixpart Venn diagram of what it takes to live a healthy life and for your brain to age well.”
The other factors are sleep, environmental toxin exposure (especially endocrine disruptors), relationships, and stress.
“The Harvard Study of Adult Development, one of the longest studies on
adult life, showed that loneliness and not having a support system is just as bad for your health as smoking,” Smith said. “And the one I focus on the most, because it undermines all the others, is stress. Stress affects cellular health, brain function, diet, exercise, social ties, and sleep. It is one of the six major contributors to people not thriving, but its role as an influencer of our habits is often overlooked. If we are stressed we probably aren’t reaching out to our support systems as much, we are coping with late night snacks, nicotine, or habits that undermine our sleep quality. The majority of Americans report symptoms of stress, according to the American Psychology Association, with nearly half of adults reporting that stress negatively impacts their behavior. Most importantly, stress-resilience is not a trait we are born with. It is a skill we build, and that’s where neural plasticity comes in.
“Habit change is essential, particularly with chronic illness. When you undergo a cancer diagnosis, you have to make lifestyle changes. But most people have no roadmap for how to do that.”
Smith has developed a fuel vs. friction framework to identify what supports or hinders progress in these six areas, aiding stress resilience and positive habit adoption.
For almost 20 years, Seven Corners Healthcare has been managing the medical needs of nearly 40,000 inmates across the country and providing seamless support for you to succeed. Valued partnerships with practices, doctors, physician assistants and more include:




Live answering and 24/7 support
Dedicated account managers so you always know who you’re working with
Customized processes and technology for an individualized experience





By Jessie L. Bekker and Katie Griffith
Alabama’s age of medical consent is rising from 14 to 16 beginning October 1, following the passage of amendments and additions to existing age of consent state laws in the 2025 legislative session. For medical practices, the change will require parent or guardian involvement during two additional years of childhood, unless an exception applies—and providers should be aware that, even once a child reaches age 16, parents and guardians will maintain certain rights to access their child’s records.
The Age of Consent Law and It’s (Several) Exceptions
While the general rule will require that minors under 16 have a parent or guardian’s permission to obtain health care services, the law provides several exceptions to the minimum age requirement. Minors can make their own medical decisions, regardless of age, if they:
• Have graduated from high school;
• Are emancipated;
• Are married or divorced;
• Are pregnant, may be pregnant or

want to prevent pregnancy;
• Require diagnosis of or treatment for a sexually transmitted infection, drug dependency or alcohol toxicity;
• Require diagnosis of any reportable disease;
• Have children; or
• Do not depend on a legal guardian and live apart from a parent (or other individual acting in place of a parent).
Providers can act without parental consent if they suspect abuse, neglect, exploitation or an imminent threat to the minor.



Certain current provisions of the law will stay in place, including a section allowing providers to treat minors without parental consent if getting consent would delay treatment or put the minor’s life, health or mental health at increased risk. The law will also continue to permit parents or legal guardians, with the input of a mental health professional, to authorize mental health treatment for minors up to age 19, the age of legal adulthood in Alabama, if care is necessary and appropriate. In those cases, the minor’s consent is not needed to provide care.
Notably, while some of these excep-
When physicians, scientists and researchers with extraordinary talent and passion are given the technology, the facilities, and the support, they achieve great things. The discoveries, innovations and clinical trials happening today will help shape the future of treatments and lead to cures.
tions exist today, others are new, including the permission granted to providers to act if they suspect abuse, neglect, exploitation or an imminent threat. The new law also specifically allows providers to provide pregnancy prevention services without parental involvement; until now, the law has only addressed diagnosis and treatment of pregnancy.
Finally, providers will maintain protection from liability when treating a minor (without the necessary consent) in good faith under the false representation that the minor could legally consent to treatment by him or herself.
Though the law will allow some minors to make their own health care decisions—whether under an exception to parental or guardian consent or once aged 16—their parents or guardians will nonetheless, in most cases, have the right to access their child’s medical records. New provisions of the law grant parents and guardians the ability to access a mi-







Healthcare organizations need access to external resources to support their strategic vision. Our team of professional healthcare advisors have extensive experience and specialized education to serve a broad spectrum of needs in the healthcare community. As your advisor, we focus on learning your values and goals and work with your team to develop an effective strategy specific to your organization.

























BIRMINGHAM | UAB St. Vincent’s Birmingham
805 St. Vincent’s Dr, Ste 100 | Birmingham AL 35205
CULLMAN | 1301-A Bridge Creek Dr NE | Cullman AL 35055
HOOVER – HWY. 150 | 2321 John Hawkins Pkwy. Ste 113 | Hoover AL 35244
HOOVER – HWY. 280 | 5406 US Hwy 280 East, Ste D106 | Hoover AL 35242
GARDENDALE | 323 Fieldstown Road, Ste 105 | Gardendale AL 35071
PELHAM | 3143 Pelham Pkwy | Pelham AL 35124 TRUSSVILLE | UAB St. Vincent’s Trussville | 7201 Happy Hollow Road | Trussville, AL 35173
continued from page 5
roofs, plumbing and parking decks, and replacing worn furniture with comfortable new seating. It may seem like a small thing, but when people aren’t feeling well, a pleasant place to see their doctor makes a difference.”
As routine updates and maintenance are completed around the system, Eagan expects phased in upgrades and
Through Synaptic Harbor, Smith offers educational services, including a December Masterclass, “The Brain Rewired: From Synapse to Self-Discovery.” While she targets her information for the lay public, she says it can also be helpful
expansion to begin. “When equipment is state-of-the-art and the environment is welcoming, it’s easier for us to do our best work for patients—in our offices and in the hospitals where we perform procedures,” he said. “Positive changes similar to what we’re seeing in heart health are likely to be seen in other specialties associated with Baptist Health.”
continued from page 6
to physicians, as they help guide their patients to healthier lifestyle choices.
More information about the Masterclass and other services Synaptic Harbor offers can be found on the website www. synapticharbor.com.
nor’s information upon request to the provider controlling the information, unless the provider suspects abuse or neglect of the child or the release of information is prohibited by a court order, a law enforcement officer investigating the parent or guardian related to a crime against the minor, or federal law regarding the confidentiality of substance use disorder (SUD) treatment records. This access right runs until the minor reaches the age of 19, regardless of who consents to the treatment.
Absent these limited circumstances, providers will be in violation of the new law if they deny access to a minor’s medical records to his or her parent or guardian. Providers should not delay access by parents or guardians to a minor’s medical records by requiring the written consent of a minor.
Providers should make note of the
continued from page 8
new consent age requirement prior to treatment. As a result of the new requirements, a 15-year-old patient, for example, who previously consented to his or her own medical treatment will need a parent or guardian’s involvement come October 1, unless an exception applies. Practices should also revisit their policies around intake paperwork for minors. Generally, the person who consents to treatment—whether a minor or a parent/ guardian on his or her behalf—should complete treatment consent forms and patient authorizations related to medical records. However, practice policies should also reflect the access rights parents and guardians maintain to a minor’s health information until the minor reaches the age of 19, even when the minor can legally act alone, subject to limited exceptions.
Jessie Bekker is an Associate at Burr & Forman LLP practicing exclusively in the firm’s Health Care Practice Group. Jessie may be reached at (205) 458-5275 or jbekker@burr.com. Katie Griffith is a law student at Cumberland School of Law.



By anSLey FranCO
Nearly five years ago, the No Surprises Act laid the groundwork for a significant shift in healthcare business practices in the form of increased data transparency. For physicians, administrators and hospital leaders, access to clear financial information is no longer a luxury. It is becoming a necessary tool for negotiating contracts, evaluating partnerships and planning for long-term stability.
“The value for physicians and administrators is that the information is available to understand what everyone’s allowables are. This gives us the opportunity to work from a position of knowledge when we engage in contract negotiations or when considering joining an accountable care organization. This is applicable in numerous situations,” President and CEO of e3c3 Consulting Cameron Cox said.
E3c3 works with independent practices and health systems across the country, advising them on regulatory compliance, revenue cycle management and strategic planning. For Cox, transparency is more than a buzzword. It is

a practical way for physicians to understand where they stand in the marketplace, allowing them to make decisions without being left in the dark.
Adam Garner, business development officer at After Transparency, agrees. His company helps hospitals and provider groups make sense of the complex financial information they receive. After Transparency gathers data, organizes it and makes it usable for decision makers who need to understand not just what the numbers say, but how to act on them.
“It levels the playing field. It gives information to providers that they didn’t

know before. And carriers have had this for a while,” Garner said. “Providers have never known what they were getting paid in comparison to their competitors.”
To explain the importance of data transparency, Cox compared it to choosing between gas stations. Drivers can see prices from the road and decide where to fill up based on affordability. In the medical world, providers now have similar visibility. They can see whether the facility down the road is being reimbursed more for the same procedure, which allows them to take the information to the insurance company.
“The thought process is that openness will create competition, which will be healthy, and will drive up reimbursement for providers, while lowering costs and increasing options for the patient,” Garner said.
In Alabama and across the Southeast, independent physicians can feel the weight of negotiating with large insurers. Blue Cross and Blue Shield of Alabama remains the state’s dominant carrier, which can make transparency even more important. Understanding allowable amounts and reimbursement trends helps physicians evaluate whether contracts are sustainable. “This data transparency empowers physicians to realize that maybe ‘I’m worth more than you say I am’,” Garner said. “Those are the assumptions. We’ll see how that plays out.”
Both Garner and Cox believe that the shift toward transparency is still in its early stages. Regulations have forced insurers and hospitals to publish more information, but the process of turning raw data into actionable knowledge remains a challenge, in part because of the enormous scale of the data. That’s where
(CONTINUED










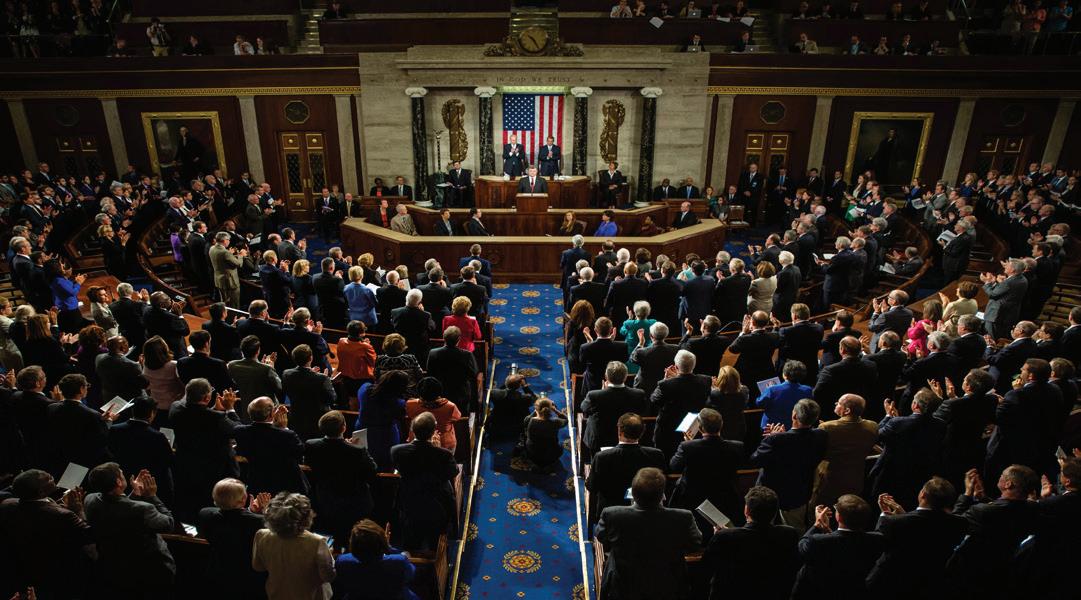
By aBBey manSFieLd ruBy and Jane eLizaBeth FeiSt
The One Big Beautiful Bill Act (OBBB), signed into law by President Donald Trump on July 4, 2025, is expected to impact skilled nursing facilities (SNFs) and the post-acute industry –though by how much remains to be seen. For SNF owners, operators and lenders, understanding the potential effects of the OBBB is key for strategic planning and financial stability in the coming years.
The OBBB makes significant changes to Medicaid, Medicare and the Affordable Care Act (ACA). The nonpartisan Congressional Budget Office (CBO) estimated that a previous iteration of the bill would result in cuts of nearly $1 trillion from Medicaid spending over the next 10 years and that 11.8 million Americans are projected to lose coverage by 2034 as new requirements take effect. Though the actual impact remains to be seen and will vary from state to state, to compensate for the changes, states may cut Medicaid services, tighten eligibility and redetermination requirements, and/ or reduce Medicaid provider payments.
Though senior living (independent living, assisted living) runs on a mostly private-pay model, SNFs rely largely on Medicare and Medicaid. Post-acute and long-term care services are expensive because of the high level of medical care provided – the national median cost of SNF care in 2024 was more than $111,000 per year for a shared room and nearly $128,000 per year for a private room. Private long-term care insurance averages more than $2,200 per month, and preexisting conditions can be an obstacle to qualifying.
Medicare (the federal health insurance for people ages 65 and older) is not designed as a long-term care program.
Medicare Part A covers up to 100 days of SNF care, but only after a qualifying hospital stay of at least three days. The first 20 days are covered at 100 percent, and days 20 to 100 require a coinsurance cost – the amount is $209.50 per day, or $16,760 for the full 80 days, in 2025.
Medicaid (a joint state and federal program for low-income and disabled Americans) covers 100 percent of SNF care, including costs associated with room and board, meals, skilled nursing care, medications and rehabilitation services. Medicaid eligibility requirements vary by state but include financial (income and asset) limits, as well as medical need guidelines.
Researchers from a Brown Univer-

sity School of Public Health study identified 579 U.S. nursing homes at high risk of closure in light of the OBBB’s changes. Most high-risk facilities were concentrated in urban areas and states such as Illinois (93 high-risk facilities), Texas (66), Ohio (41), Missouri (39) and Georgia (37).


Rural hospitals, many of which also rely on Medicaid, may also be at risk of closure as a result of the OBBB’s changes. Prior to passage of the OBBB, rural hospitals were already experiencing challenges caused by a number of economic factors, including low margins, staffing challenges and high populations of uninsured and underinsured patients, leading to more than 100 U.S. hospital closures in the past decade. Some project



that the OBBB’s changes will add to an already precarious financial situation for many rural hospitals and result in more closures.
When a hospital closes, SNFs may receive patients with more complex needs, potentially affecting staffing and resource allocation within a facility. It can also increase travel distances for SNF patients needing emergency or other specialized care, delaying or hindering access to necessary services that can be critical in life-threatening situations. Rural hospital closures are associated with decreased local labor force and staffing strain. Finally, SNFs are often connected to hospitals – sometimes directly, sometimes through formal preferred provider networks and others through informal referral networks – and the closure of a hospital may result in fewer referrals to a local SNF.
The Centers for Medicare & Medicaid Services (CMS), under the previous administration, promulgated a rule (89 Fed. Reg. 40876) that established minimum staffing standards for long-term care facilities participating in Medicare or Medicaid. The rule, which was slated for implementation starting in 2026 for nonrural facilities and 2027 for rural facilities, garnered criticism because of concerns about exacerbating staffing shortages and labor costs, among others.
The OBBB delays implementation of the rule until 2034.









Physicians, continued from page 11
consulting firms and data platforms can make a difference, especially for independent practices that may lack the resources to do it on their own.
“The challenge with the data is that it’s massive. So, it’s really not available for the layperson. I couldn’t just go through it, even though it’s free,” Cox said. “You can’t do anything with it. It’s larger than the Library of Congress.”
Garner agreed, adding that the first obstacle for any provider is simply obtaining the data. “It is public, but just like Mount Everest is public, you need experts to navigate and get you there.”
Cox says the importance of this work cannot be overstated because the data ultimately affects every provider with a private insurance contract, as well as employers and patients.
Some physicians hesitate when they hear the cost of turning transparency data into a usable format. “Let’s say
it costs you $5,000 to get the data in a format in which I can use it,” Cox said. “They don’t understand the upside to it. Most physicians, when they hear the word expense, think of overhead. When I hear the word expense, I think investment. You can use this information to do different things; it doesn’t have to just be contract negotiations. It can be all kinds of things with regard to your practice.”
Looking ahead, Cox hopes to simplify the data and get it into the hands of every provider. Garner sees the potential for transparency to be used by the patient to determine where the most affordable option for care is based on their insurance.
For Alabama’s physicians, the takeaway is straightforward. Transparency is no longer something to watch from a distance. It is a resource that can be used now, while the healthcare market continues to evolve.
The OBBB is one of the most consequential pieces of legislation in recent congressional history. Though many in the SNF industry are relieved over the 10-year moratorium on the staffing mandate, the bill may mean financial challenges ahead for SNF owners, operators and lenders, particularly for facilities dependent on Medicaid reimbursement.
To prepare for what’s to come, SNF owners and operators should:
• reassess portfolio valuations, particularly for facilities with high Medicaid census
• develop financial models for various potential outcomes, particularly focused on changes in Medicaid reimbursement
• consider direct or indirect dependence on a nearby rural hospital and strategize to mitigate the effects of a closure
• consider opportunities to diversify payer sources and reduce Medicaid dependence
• monitor state-specific changes to Medicaid and consider impact on SNFs in those states
• evaluate geographic diversification in facility acquisition and disposition strategies
• focus on operational excellence and invest in specialized clinical programs to maximize reimbursement rates
• explore artificial intelligence (AI) technologies to aid with predictive analytics, streamline operations and track and analyze compliance data
• SNF lenders should:
• update underwriting criteria to account for the new Medicaid financing realities, including increased scrutiny of borrowers’ payer mix
• consider stricter financial covenants for facilities heavily dependent on Medicaid
• track state-by-state Medicaid environments to determine which may be higher risk for sustained economic performance
The skilled nursing industry has demonstrated remarkable resilience through numerous policy shifts over decades. Facilities that proactively prepare for potential changes while maintaining their focus on quality patient care will be best positioned to navigate the evolving landscape.





























































The Birmingham Heart & Vascular Center, a new outpatient Ambulatory Surgery Center (ASC), is scheduled to open in early 2026 at 46 Medical Park Drive, Suite 310B, just inside the ground level entrance of St. Vincent’s East.
The state-of-the-art facility is jointly owned by UAB, Birmingham Heart Clinic, PLLC (BHC), and U.S. Heart & Vascular. The surgical care facility’s clinical leadership includes ASC board
members Drs. Joshua Cockrell, Jacob Townsend, and Robert Yoe, IV. Project partners include GE HealthCare, Birchfield Penuel Architects, and Robins & Morton.
The ASC will provide a range of cardiology and vascular procedures, including right and left heart catheterizations, loop implants and explants, pacemakers, defibrillators, and stent placements.

Spring Hill College has broken ground on the $35 million Annette N. Shelby Health and Science Innovation Center. The facility will expand the college’s nursing and pre-med programs, as well as provide space for new programs like exercise science and other health sciences.
Senator Richard Shelby addressed the crowd at the groundbreaking ceremony. “Annette devoted her life to education, mentorship and public service,” Shelby said about his wife, who died in July. “I am proud to see her legacy live on here at Spring Hill.”
A native of Alabama, Annette
Shelby was the first woman to earn tenure at Georgetown University’s McDonough School of Business, a Jesuit institution.
The center will be 57,000 square feet and will have an anatomage lab, using digital cadavers for training, a high-tech nursing simulation lab space, virtual reality lab and labs dedicated to nursing skills and microscopy. Completion is expected in spring 2027.
The construction is being supported by federal funding, and investments from the city of Mobile and Mobile County.
As a pharmacist, Zach brings exceptional professionalism to MediSYS with a unique insight and experience in healthcare.
• His patient-facing role throughout his career has given him hands-on insights into the healthcare system
• He knows the day-to-day challenges providers face and can provide solutions that truly improve their work ow and patient care.
Contact Zach today to explore a partnership of experience and trust! 256-626-1754


The ability to call them and WORK



with them on high-level matters contributes to our overall success.



— Warren Averett Client

Why entrust your practice to a generalist when you could have an advisor that understands your specific needs and the challenges of the healthcare industry?

Warren Averett is uniquely equipped with experts who have dedicated their careers to helping medical practices thrive. We help physicians make smart personal and business decisions. We’re here for you.



The University of Ala bama at Birmingham named Kenny Shafer as Chief Executive Officer of UAB St. Vincent’s Birmingham, effective September 2nd.
Shafer has over a decade of health system leadership, most recently serving as CEO of John son City Medical Center, a 501-bed hospital that serves northeast Tennessee. During his tenure, he led growth in clinical services and helped elevate the hospital’s recognition for quality, performance and safety.

His leadership was vital to the development of the Ballad Health Trauma Network.
“I am honored to join the UAB Medicine team and to lead a hospital that has such a rich legacy of service,” Shafer said. “My family and I are excited to make Birmingham our new home.”
He has also held key operational roles across the Ballad Health system, including COO of Indian Path Medical Center. He has overseen initiatives to expand access in interventional radiology, trauma and critical care, neurosciences, orthopedics, and cardiovascular surgery.
In this new role, Shafer will oversee daily operations and guide St. Vincent’s Birmingham’s integration within the UAB Health System. He will work closely with its clinical and operational teams to advance its mission.
“Kenny is a thoughtful leader with the ability to elevate care, strengthen teams and deliver results,” said Dawn Bulgarella, CEO of the UAB Health System.
Senate President Pro Tem Garlan Gudger has appointed James Clements, CEO at Cullman Regional Medical Center, to serve on the Alabama Rural Roadmap Initiative (ARRI).







Formed during the 2025 legislative session, ARRI is intended to develop strategies that support growth in Alabama’s rural communities.
“Healthcare services in rural communities are essential for quality of life and economic development,” Clements said. “I’m grateful to Senator Gudger for
selecting me to participate in this initiative and look forward to seeing the impact it will have on our state.”
Over the next year, members of the initiative will assess community needs, coordinate resources, and develop actionable recommendations for the Alabama Legislature to consider. The group’s work will focus on infrastructure, business and entrepreneurship, workforce development and training, rural healthcare, and quality of life.
Crothall Healthcare, which provides support services in areas such as patient transportation, sterile processing, and environmental services, will lay off 52 employees in Montgomery, beginning on September 30, 2025, due to the termination of their contract with Baptist Medical Center East for environmental services and hygiene maintenance. The company has had several layoffs in 2025 due to contract losses and operational challenges.

With one of the nation’s largest healthcare law practices, Holland & Knight has more than 475 experienced attorneys covering virtually every segment of the healthcare industry, from transactional matters, regulatory compliance and real estate to litigation, government enforcement and public policy issues. Our dedicated healthcare attorneys and professionals – in Birmingham and throughout the country – have the insight, experience, depth and resources to help promote and protect your interests.
www.hklaw.com


During our recent clinic relocation, Veritas demonstrated a profound understanding of our requirements.Their exceptional collaboration in identifying the most suitable office for our needs was invaluable, and they attentively listened to our preferences, providing comprehensive insights into our practice’s unique needs. Their meticulous attention to detail and unwavering commitment to client satisfaction are evident in their approach. I highly recommend Veritas to anyone seeking a real estate group. Their exceptional services and unwavering dedication make them a reliable partner for any medical practice.

Rich Campbell
Brian Culverhouse
Nancy Ferren
Peter Jameson 205-304-1010 www.veritasmre.com
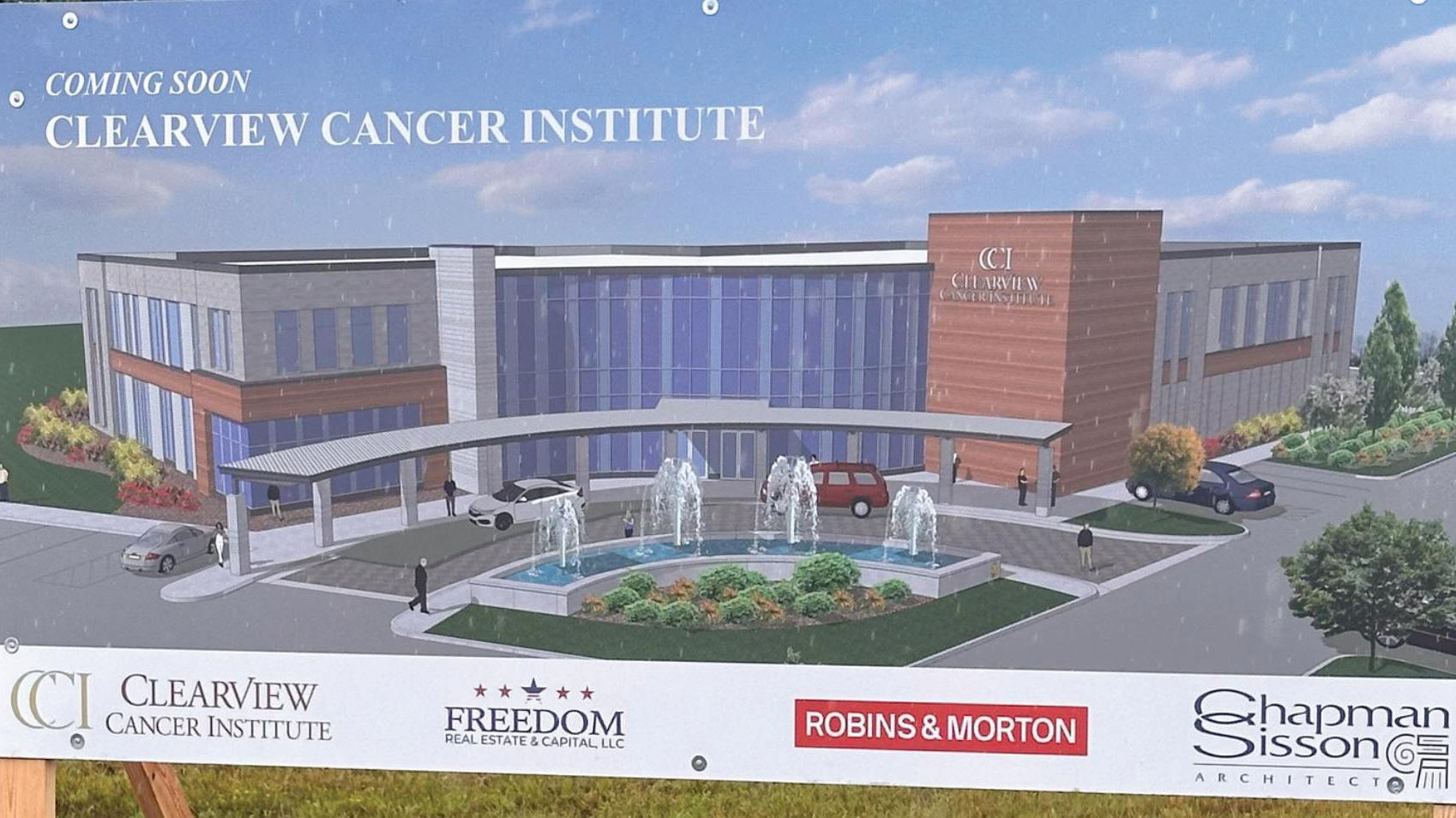
In August, the Clearview Cancer Institute (CCI) broke ground on a new $54 million facility in Decatur, which is slated to open in 2026 on a five-acre site located at 1626 6th Avenue SE. The 57,500-square-foot, two-story cancer center will replace CCI’s current Decatur

facility on 14th Avenue, which the group had outgrown.
The new center will unify Clearview's Decatur-based oncologists, incorporate advanced technology, and provide personalized care for patients with cancer and blood disorders closer to home. Ca-
pabilities will include space for lab work; an expanded radiation area; a large imaging area for MRIs; and extra space for patient care.
Currently, CCI operates 13 cancer treatment locations throughout North Alabama.




the pandemic,

Steve
Katy Barrett-Alley
CONTRIBUTING WRITERS
Jane Ehrhardt, Ashley Franco, Laura Freeman, Lynne Jeter, Marti Slay
Birmingham Medical News
270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110
AD SALES: Jason Irvin, 205.249.7244
All editorial submissions should be e-mailed to: editor@birminghammedicalnews.com

Cullman Regional’s freestanding emergency department in Hartselle has earned The Joint Commission’s Gold Seal of Approval®. Hartselle Health Park ER underwent a rigorous, unannounced onsite review.
The hospital ranks nationally as a
Top 10 percent Performer in several quality metrics by CMS and consistently beats state and national benchmarks for heart attack and stroke related care. Additionally, Cullman Regional is one of only five hospitals in the state with zero central line associated bloodstream infections in the


most recent reporting period.
Since opening in January, Hartselle ER has cared for more than 6,000 patients from south Morgan County and surrounding communities.
Birmingham-based KultureCity, a non-profit that provides services to assist those with sensory processing disorders, has purchased the Powell Avenue Steam Plant, an historic Birmingham landmark.
KultureCity sees it as a space for the City of Birmingham. “That would include a water play area, which the city doesn’t have,” Maha said. “A place for an inclusive play-

ground. On top of that, also developing an amphitheater to push the boundaries of accessibility.”
“We also envision that front space being used as a common area where we can hold events, Christmas markets, Fourth of July events. Imagine a New Year’s Eve party where you’ve got those two beautiful spires, the smoke stacks, that can be used for ball drops.
At Pulmonary Associates of the Southeast, we get your patients in sooner. Because sooner is better when someone is struggling with lung function, sleep, asthma, or other critical care conditions. That’s why we make referrals as easy as possible to get your patients in and on their way to feeling better.
The MedTech Device Center at Hardware Park provides the guidance, engineering expertise and industry connections essential to moving your medical technology ideas from concept to market. As a part of Alabama's technology ecosystem, we are helping bring many breakthrough medical technology concepts to life, from reversing the effects of myopia to revolutionizing bipolar neurosurgery. Your idea could be next. It's free and confidential. Scan the code to get started today.
Fulmer Instruments
In surgery, the need for a more agile, modern tool led to the founding of Fulmer Instruments. Through Hardware Park development partners, Fulmer is creating breakthrough surgical instruments.
Electric Indigo
Hardware Park is working directly with Electric Indigo to help develop glasses that address the soaring myopia epidemic amongst kids and young adults.
