




By laUra FreeMan
This April, Grandview Medical Center became one of the first in Alabama to offer a new weight loss procedure for bariatric patients called the Endoscopic Sleeve Gastroplasty (ESG), which helps patients eat less and feel full faster. This minimally invasive procedure helps to shorten the length of the stomach by approximately 50 percent and reduce its volume by 75 percent.
Surgeons at Grandview, like Andrew Frey, DO, enter the patient’s stomach using an endoscope to sew a portion of the stomach closed. A small suturing device, attached to the end of an

endoscope or camera, goes through the mouth into the stomach while the patient is asleep. Six to eight stitches are placed in a U shape pattern, starting at the bottom of the stomach, and working towards the top. These internal stitches will reduce capacity and change the shape of the stomach, forming a tube. The procedure is reversible, but the goal is for the stitches to stay permanently.
“We can perform this whole procedure with the endoscope without ever making a cut,” Frey said. “Patients can have it done in an outpatient setting so typically, they’re back to work in two or three days.”
(CONTINUED ON PAGE 3)

By laUra FreeMan
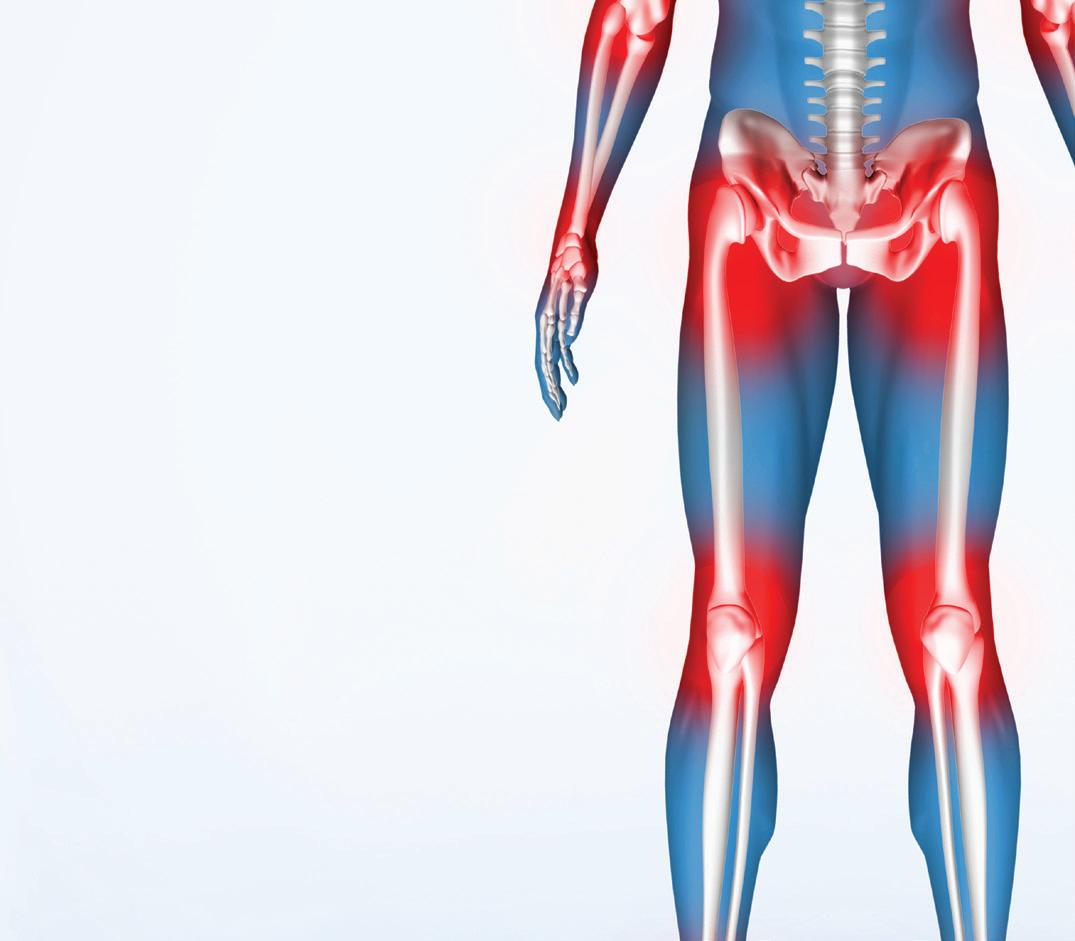
Since the first advances in knee replacement surgery in the 1960s and 1970s, a steady progression of innovations in techniques and technology has continued to improve the procedure and patient outcomes.
The latest step forward is the cementless version of the Oxford unicondyl implant for partial knee replacement by Zimmer Biomet which recently received approval by the FDA. After 20 years of clinical experience and
more than 300,000 procedures across Europe and other regions, the new implant’s success has been impressive.
“With the cementless version, the primary advantage is that there should be less risk of the joint loosening over time. It also removes the possibility of an adverse allergic reaction or sensitivity to the cement,” said orthopedic surgeon Patrick Peavy MD of Alabama Ortho Spine and Sports. “As the incision heals, a natural bond forms with the surrounding tissue, holding the implant in place.”
The precision required for
successfully performing the procedure is a bit more demanding, which is why the initial approval of the implant was granted to only 50 orthopedic surgeons in the United States. In Alabama, that surgeon was Peavy.
“My mentor in Boston was noted for his work in partial knee replacements. I became interested in this option and followed the development of the cementless version,” he said. “It was clear that the advantages were worth the additional training and precision

With one of the nation’s largest healthcare law practices, Holland & Knight has more than 475 experienced attorneys covering virtually every segment of the healthcare industry, from transactional matters, regulatory compliance and real estate to litigation, government enforcement and public policy issues.
Our dedicated healthcare attorneys and professionals – in Birmingham and throughout the country – have the insight, experience, depth and resources to help promote and protect your interests.
www.hklaw.com
Colin H. Luke, Partner Birmingham, AL | +1.205.226.5717
After the procedure, it’s important for patients to follow a strict diet and exercise regimen. They start out on a liquid diet and progress to a soft diet. Eventually, they will be back to eating a regular diet with healthier portion sizes. To qualify for the ESG procedure, a person needs to have a BMI greater than 30.
“Our patients have often had weight issues their entire life and have tried multiple diets or even medication like GLP-1 with varying degrees of success. ESG gives us another option to treat both their obesity, as well as other comorbid conditions,” Frey said.
Without any incisions, stapling or external scarring, the ESG procedure helps patients lose weight because the quantity of food that can be eaten is restricted, the number of calories the stomach can absorb is reduced and the stomach empties more slowly, making it feel full longer.
“Patients are losing anywhere from 15 to 20 percent of their excess weight one year after undergoing this procedure,” Frey said. Medical studies also show that
Surgeons sew part of the stomach closed with an endoscope.
from page 1

patients typically consumed 59 percent fewer calories.
The ESG procedure was pioneered in 2012 at the Mayo Clinic. Since then, it has grown in popularity.
“What we’re seeing, especially with some of the success of medications, is that patients are looking for increased weight loss, but without surgery,” Frey said. “Alabama, in general, struggles with obesity.
If you pull up census data over the past 30 years, the entire country has become more obese, but Alabama has around a 40 percent prevalence of obesity.”
Over the last five years, Frey has seen a significant increase in bariatric medications on the market. While many of these medications have helped patients, he’s also seen patients coming back to look for more options because of pharmaceutical side effects or because of financial reasons.
“We know that obesity is a disease,” Frey said. “It’s caused by a variety of factors including biology, genetic risk, the environment and the foods that are around us. So our team is trying to address all of this. We have to meet with dietitians, and we have to develop exercise plans. To me, it’s about more than just the pounds the patients are losing. I’m rewarded by them coming off chronic medications, like blood pressure medications or insulin for our diabetic patients, and by increasing their cardiovascular health. That gives them stamina to participate in all aspects of their life.”
continued from page 1
required to perform the procedure. The cementless procedure has been available for a while in Europe and the results have been excellent. Surgeons who have been performing the technique there came to help train the first surgeons here who would be working with the cementless implant.
“I began offering the option to selected patients shortly after FDA approval was finalized. The outcomes have been very good. Patients were pleased when I explained the advantages of the cementless procedure and that it should last longer. What they really get excited about is being able to choose a partial knee replacement rather than having to undergo a total knee surgery. The partial knee procedure only removes the damaged part of the joint. It’s usually less painful and recovery tends to be faster.”
In his practice, Peavy performs both partial and total knee replacements in patients of all ages. “While it’s true that

time tends to increase wear, age isn’t the only factor in determining which procedure would likely offer the best outcome for a particular patient,” he said. “Each case has to be evaluated individually based on the location and severity of the damage.
“Since accidents and sports injuries may damage only part of the knee, it follows that we would see that more in active people who tend to be younger. The partial knee surgery preserves more of the original tissue, so we get more natural movement. In addition to
getting patients back to their lives faster, preserving more healthy tissue could also be an advantage in later life if the patient eventually needs a revision surgery or a full knee replacement.”
Judging by procedures in Europe, there seems to be a positive correlation between good outcomes and the frequency of experience of the surgeon using the technique, with surgeons who do 30 to 40 or more cases per year becoming particularly adept.
As with other joint replacements he performs, Peavy says prehab and rehab
can be a major plus. “If patients have coverage for enough physical therapy visits per year, it would be great if they could do both,” he said. “It’s always good to go into surgery with muscles in the best possible condition and to get patients back on their feet as soon as possible afterward. And after surgery, I usually recommend looking at lower impact activities, but if a patient’s joy in life is running, I’m not going to tell them to give up what matters to them. I tell them to listen to their body. Take reasonable precautions and go enjoy life.”


By Marti WeBB Slay
When Hassan Alkhawam, MD, interventional and structural cardiologist at UAB St. Vincent’s, had a patient needing a new aortic valve, he recognized the patient would be best served with a new valve on the market.
Abbott’s Navitor™ Vision valve is the latest addition to the Navitor transcatheter aortic valve implantation (TAVI) system, a minimally invasive therapy to treat severe aortic stenosis. The valve incorporates three radiopaque markers designed to help physicians deploy it more precisely at the intended depth. The FDA has approved the valve for patients at high or extreme surgical risk.
“Up to 15 years ago, the only treatment for severe aortic stenosis was open heart surgery,” Alkhawam said. “Now we have more options with transcatheter aortic replacement, and in the last 15 years it has been advancing.”
“This newest valve has several benefits due to advanced engineering. It offers better sealing so we don’t have leaking around the valve when there is a lot of calcium, and in the future if we need to access the coronary again, we can do that

easily and put in stents if needed without any difficulty.
“Deploying the valve is more visible in patients with peripheral vascular disease compared to the other valves as well. This valve has three radiopaque markers so when we are deploying the valve, we can see under the x-ray where we are deploying it, so we are able to install the valve in the appropriate position to achieve excellent hemodynamic results. That’s very advanced technology.”
Alkhawam was one member of a

team which included Mustafa Ahmed MD, structural heart director and interventional/ structural cardiologist, and Parvez Sultan, MD, cardiothoracic surgeon. They have now successfully completed two surgeries with the new valve.
The first patient had a lot of calcium in his aortic valve, and since the Navitor valve doesn’t push the calcium, Alkhawam felt it would be a better option over the two older valves on the market. Also, since the surgeons would typically expect high risk
of paravalvular leakage in patients with a lot of calcium, he wanted to use the Navitor valve. It worked.
“We did not have any leak at all,” he said. “We had amazing results for the first case. Also the patient had a lot of blockages in his heart, so he might need a cardiac catheterization in future. With this valve, we will be able to access his coronary in the future without a problem.”
The minimally invasive TAVI procedure typically requires an overnight





















By Miranda a. Franco and Beth PitMan
The Center for Medicare and Medicaid Innovation (CMMI) recently released a statement on its plans to unveil a new strategy focused on “improving the health of Americans through disease prevention via evidencebased practices, empowering individuals with information to make informed decisions, and promoting choice and competition.” Established under the Affordable Care Act, CMMI’s primary role is to test new ways of providing and reimbursing health services. The center runs temporary pilot programs aimed at improving patient care and reducing costs, with the ultimate goal of incorporating successful approaches into broader Medicare and Medicaid policies. Currently, CMMI oversees 23 models and receives $10 billion in mandatory funding each decade to develop, test and evaluate different experiments.
The announcement from CMMI suggests that the Trump Administration is putting its own stamp on value-based care. Early signs of this shift became clear with the recent cancellation of several
payment models, many of which had supported primary care. Some of these models were nearing their completion, while others had only recently launched.
Specifically, CMMI announced plans to discontinue the Primary Care First (PCF), Mak ing Care Primary (MCP), the mandatory ESRD Treatment Choices (ETC) and the Maryland Total Cost of Care (TCOC) models.
A bit of background on these models:
• PCF (2021-2026): A voluntary model offering an innovative payment structure to support advanced primary care, prioritizing clinician-patient relationships and improved health outcomes for patients with complex chronic needs.
• MCF (2024-2034): A 10.5-year model focused on improving care management and coordination, helping primary care clinicians form partnerships with specialists and community resources to address patient health needs.
• ETC (2021-2027): A mandatory model designed to increase home dialysis and kidney transplants for Medicare beneficiaries with End Stage Renal Disease, while reducing expenditures and
maintaining care quality. The model will be formally terminated through future rulemaking.
• Maryland TCOC (2019-2026): A Maryland-specific model aimed at achieving fixed savings for Medicare beneficiaries’ total cost of care. It will transition to the States Advancing AllPayer Health Equity Approaches and Development (AHEAD) Model in January 2026, pending state discussions.
CMMI aims to end these models early, by Dec. 31, 2025. The Centers for Medicare & Medicaid Services (CMS) stated in its press release that participants in these models will receive follow-up communication regarding the modelspecific winddown.
Additionally, the Medicare $2 Drug List and Accelerating Clinical Evidence models will not move forward as previously announced. CMMI also stated that it is “considering options” to reduce the scope of the Integrated Care for Kids (InCK) model.
These terminations signal the administration’s growing focus
Our team of 15 board-certified physicians specializes in minimally invasive procedures to capture the latest in treatments with the most e ective outcomes for each patient.
WE ARE LEADERS SPECIALIZING IN:
• Chest pain & hypertension
• Peripheral Artery Disease
• Cutting-edge therapies
• Watchman & treatment of AFIB
• Venous disease & procedures
• Interventional cardiology including TVAR, TCAR, and EVAR procedures
on regularly assessing whether demonstration models are achieving expected cost savings while maintaining or improving quality of care. CMMI estimates that ending these models will save taxpayers roughly $750 million, though it has not detailed how these savings will be achieved. More updates are expected in the near future.
Accordingly, providers involved in other demonstration models should prepare for potential changes, particularly if CMMI continues with its new strategy regarding innovation center demonstrations. Notably, CMMI has confirmed that it plans to continue with other active models, including the Accountable Care Organization (ACO) Primary Care Flex (PC Flex) model.
Drawing on insights from the first Trump Administration, many anticipate a more contentious stance on mandatory models and a likely pivot toward payercentric payment reforms. Also notable will be the influence of new leadership at the U.S. Department of Health and Human Services (HHS). Abe Sutton, the director of CMMI and former policy advisor to the U.S. Domestic Policy Council, as well








































MANDATORY multi-factor authentication (MFA)
MANDATORY biannual vulnerability scans
MANDATORY annual penetration tests
MANDATORY encryption of all ePHI
MANDATORY network segmentation
MANDATORY asset and network inventory
MANDATORY log retention The HIPAA Security Rule is












By anSley Franco
Three months ago, Judy Corbett, MD, was attending a medical convention in Nashville, looking for tools she could bring back to her Gulf Coast GYN and aesthetics clinic in Foley, Alabama. That’s when she came across a booth offering a 10-minute demo of a non-invasive treatment for mental wellness. Curious, she sat down to try it.
“Even with just a 10-minute demo, I could feel the difference that occurs from this technology. It’s a sense of peace that is absolutely beneficial to mental clarity, sleep, and overall mood and anxiety. After personally experiencing that, I knew I wanted to bring that to my patients,” Corbett said.
The treatment she tried is ExoMind, a device that uses transcranial magnetic stimulation (TMS) to help improve mental and emotional health. TMS isn’t new, it has been used in psychiatry for over 20 years, mainly to treat major depressive disorder. However, this version is designed to be faster and more accessible than traditional TMS methods.
The device quickly identifies a person’s motor threshold, or the lowest
level of stimulation needed to cause a visible muscle twitch. Once that’s established, it delivers targeted magnetic pulses to the dorsolateral prefrontal cortex and aims to encourage the brain to rewire itself, a process known as neuroplasticity.
The idea is that this stimulation helps shift the brain’s chemical balance, particularly between dopamine and serotonin, which can impact mood, anxiety and sleep.
While the research behind devices like ExoMind is still growing as it was launched early this year, more providers across different specialties are taking an interest in treatments that don’t require medication or invasive procedures. For Corbett, the firsthand experience was enough to start exploring how mental wellness tools like this could fit into her broader approach to care.
“Yearly checkups of women’s wellness and annuals are proactive measures to look for breast cancer or cervical cancer or other illnesses,” she said. “But wellness is really so much more than that. It’s an opportunity for someone to have a better quality of life, more longevity of life, to remain active as they age. I am 62 so I truly appreciate that aging does happen and being able to
We have two clinic locations, in Birmingham and Bessemer, so patients have the option to choose the closest location for them.
We’ve made referring easy by contacting and scheduling patients quickly and keeping you informed on their treatment plan.
We provide a comprehensive treatment plan for patients, offering the most up-to-date and innovative treatment options.

offer solutions for not just how we look as we age, but how we feel as we age, is very exciting.”
The ExoMind treatment protocol consists of six 24-minute sessions, typically done once a year. During each session, patients lie down while the device is placed on the scalp to deliver targeted magnetic stimulation. According to Corbett, the process is calming, and many patients even fall asleep during the treatment. Afterward, no recovery time is required so patients can immediately return to their daily routines.
The therapy has received FDA


clearance for use in treating symptoms of depression, anxiety, obsessive-compulsive disorder, brain fog and excessive eating behaviors. For Corbett, one of the most noticeable personal benefits was improved sleep. “ExoMind is not gonna cure every mental condition or mental illness, but in conjunction with appropriate care, can significantly improve the quality of treatment,” she said.
Mental health remains a widespread concern. According to the National Health Interview Survey, about 20 percent of adults in the U.S. received some form of mental health treatment in 2020. That includes 16.5 percent who reported taking prescription medication for mental health reasons. Women were more likely than men to seek treatment, with higher rates of anxiety and depression across the board.
Corbett has seen a wide range of patients respond to ExoMind, some managing diagnosed conditions like PTSD, others overwhelmed by the demands of daily life.
“I have a gentleman struggling with PTSD who says that this has been lifechanging for him. I have patients who
(CONTINUED ON PAGE 10)

Legal matters influence most business decisions in your practice.


We take that complex, time-consuming pressure off you, so you can focus on what matters and make the best decisions for you and your patients.


















stay in the hospital. “We go through the femoral artery to deploy the valve. Usually it takes around 30 to 35 minutes on average, and the patients stay overnight. Next day, if everything is good, they go home,” Alkhawam said.
Patients can perform most usual daily activities once they return home but may not drive or lift more than 10 pounds for a week following surgery.




If you suffer from allergies or other ear, nose, throat or hearing problems, we don’t want you to treat your healthcare lightly or ignore symptoms that could lead to more serious issues. Call us now for a complete evaluation with one of our 15 board certified physicians, 5 highly trained and licensed PAs, or 16 clinical audiologists — all available to serve your needs at any of our 10 locations.

continued from page 4
Since the valve is new there’s not a great deal of long-term data, but Alkhawam said they expect the valves to last at least eight years, if not longer. “And after eight years, if they need something else, most likely, we can put another valve inside the old valve. We don’t have to open the chest,” he said, “but that’s a case-bycase decision.”
Alkhawam encourages referring physicians to understand the benefits of the Navitor valve and to know the team at St. Vincent’s has successfully completed Navitor TAVI on patients who may otherwise not have been candidates for valve replacement.
“If they have severe aortic stenosis, they are considered high risk, and they have a lot of calcium in the aortic valve with a risk for paravalvular leak, or if there is a chance they will need to access coronary in future, this valve is a great choice,” he said. “We have every technology in the United States available right now in Birmingham.”
as an advisor to the secretary of HHS during the first Trump Administration, was known for focusing on market-based solutions. After his time in government, Sutton worked at an investment firm, and his background in private sector investment may lead him to prioritize the rapid scaling of high-performing models, as well as influence his perspective on long-term model timelines. Further, equity under his purview may be more focused on rural health equity.
A new CMMI approach could also build on concerns raised by HHS Secretary Robert F. Kennedy Jr., who highlighted the high rates of chronic diseases such as diabetes, cancer, asthma and obesity, linking their prevalence to escalating national healthcare costs. Additionally, support for initiatives such as Medicare Advantage, championed by voices such as incoming CMS Administrator Dr. Mehmet Oz, could further influence CMMI’s push for more market-driven solutions.
It’s also worth noting that CMMI has faced substantial criticism from
continued from page 6
Republicans – highlighted in a House Committee on Energy and Commerce hearing on June 2024 – for issues such as program complexity and limited cost savings. Despite these critiques, CMMI’s model flexibility is significant compared with other CMS demonstration authorities – with a broader latitude in scale, the ability to act mostly nationwide, its exemption from budget neutrality requirements and the lack of time limits. Given this scope, CMMI is likely to remain central to policy efforts under the Trump Administration.
CMMI’s new strategic vision may contain valuable indicators for what stakeholders could expect next. These new imperatives could present opportunities or challenges. Providers, payers and innovators have the chance to adjust their models to offer and finance care that aligns with both federal directives and the evolving needs of their patient populations.
struggle with just being a mom and working and struggling financially and all the different stressors that we deal with,” Corbett said.
Patients visiting Corbett’s Baldwin GYN and aesthetics practice often seek help managing stress and anxiety without the need for sleep aids or prescription nerve medications. While the once-a-year model works for many, individuals with more severe mental health diagnoses may require more frequent sessions. A full round of six ExoMind treatments costs
continued from page 8
$3,000. Corbett’s practice offers both short-term and long-term financing plans to make the therapy more accessible. For Corbett, integrating ExoMind into the practice isn’t about replacing traditional mental health care, it’s about expanding the toolkit. While more research is still needed, tools like ExoMind suggest a growing shift toward accessible, non-invasive support for mental health, meeting patients where they are, both physically and emotionally.





















































By Kelli FleMing
In recent years, we have seen an emerging number of physicians and healthcare providers transitioning to concierge, direct-to-consumer practices. Many providers no longer want to deal with the hassles of billing insurance, obtaining authorizations, responding to audits, etc., all in exchange for a reimbursement rate that those same providers view as insufficient. In addition, many patients are becoming frustrated with unfavorable insurance coverage determinations and increasing premium expenses. Those same patients are wanting a more personalized experience when it comes to their healthcare, and are willing to pay to receive such an experience. As a result, patients are seeking alternative ways to receive and pay for healthcare, and providers are shifting to accommodate patient demand. Hence, the emergence of concierge practices across the country.
While there are a number of legal issues to consider before transitioning a practice to a concierge model, one such consideration relates to whether or not a provider should opt out of Medi-

care. Opting out of Medicare allows a provider to avoid Medicare mandatory claims submission requirements. Under the Medicare regulations, Medicare providers agree to submit claims to Medicare for covered services rendered to Medicare beneficiaries, and if those providers are participating, to accept the Medicare payment rates in exchange for such services. In other words, Medicare has a mandatory claims submission requirement that requires a provider to submit a claim to Medicare when

covered services are rendered to Medicare beneficiaries. However, submitting claims is oftentimes what a concierge practice is aiming to avoid, and opting out of Medicare allows a provider to avoid the Medicare mandatory claims submission requirement. However, opting out of Medicare should not be done without careful consideration.
First, only certain types of provider are allowed to opt out. Specifically, the following provider types may opt out of Medicare: doctors of medicine, doctors of osteopathy, doctors of dental surgery or dental medicine, doctors of podiatric medicine, doctors of optometry, physician assistants, nurse practitioners, clinical nurse specialists, certified registered nurse anesthetists, certified nurse midwives, clinical psychologists, clinical social workers, registered dieticians and nutrition professionals, marriage and family therapists, and mental health counselors. However, the following provider types are not eligible to opt out of Medicare: anesthesiology assistants, chiropractors, occupational therapists, physical therapists, qualified audiologists, and qualified speech language pathologists.
Secondly, opting out is a somewhat “permanent” decision. To opt out a provider must file an opt-out affidavit with its Medicare Administrative Contractor. There are specific guidelines regarding when the affidavit can be filed and when it can take effect. However, opting out cannot be retroactive. Once a provider opts out of Medicare, the opt out status remains in effect for two years. At the end of the two year period, the opt out affidavit automatically renews for another two year period unless the provider provides a cancellation notice at least 30 days prior to the expiration date. During the two year opt-out period, there is very limited ability to terminate the opt out.
Third, the opt out is an “all or nothing” status and applies to all settings in which the provider sees Medicare beneficiaries. In other words, a provider cannot opt out for some Medicare patients but not others. However, an opted out provider may still refer patients to other participating providers for services, and such services, when provided by other participating providers, are covered by Medicare.
Fourth, as the result of the opt out,
(CONTINUED ON PAGE 17)











Warmer weather isn’t the only gift summer brings. Along with the buzz of summer break comes a rush of graduating providers and physicians who are eager to start the next phase of their career.

Summertime is when many healthcare organizations hire a new resource to join their busy team, and physician and provider enrollment with insurance payers is an essential component of the onboarding process. Kassouf’s credentialing specialists can manage the credentialing and enrollment process from start to finish, helping you avoid the headaches this time-consuming project can cause. Our team of experts leverages years of experience to make the process as efficient as possible, while our advanced credentialing software efficiently and accurately completes applications.
Let us manage the enrollment process for you so you can focus on your practice. Contact us today to schedule a software demo and discuss how we can help you with your provider enrollment needs.
“I brag all the time on the great job you all did. To get up and running as quick as we did was truly remarkable, and I believe that was because you guys cared and appreciated our sense of urgency. Honestly, I don’t see how we could have done this on our own. We are truly grateful for you all.”
–Owner & Physician, Obstetrics & Gynecology



By Jane ehrhardt
In the rapidly evolving world of telehealth, a new app is changing the way patients and physicians approach skin cancer detection. CheckMySpot, a tele-dermatology app founded by spouses Michael Webb, MD, a board-certified dermatologist, and Elizabeth Webb, JD, offers a streamlined, asynchronous service that aims to bridge the gap between initial skin cancer concerns and in-person dermatology visits.
Michael Webb emphasized that the app is not a substitute for in-person care, but rather a tool to expedite necessary visits. “This is not virtual dermatology. This is a store-and-forward or asynchronous tele-dermatology,” he says, meaning there is no live interaction between patient and physician.
CheckMySpot does not provide treatment online. Instead, users receive a report within 24 hours from a boardcertified dermatologist evaluating their submitted photos. If a suspicious lesion is identified, the app connects the patient either with their existing dermatologist or with one in the app’s growing preferred referral network.
The development took two years


from conception to market launch with this latest year of soft launch in Alabama to gather user feedback to heighten the app’s efficacy. A key challenge was ensuring that the submitted photos met the necessary diagnostic standards. To address this, CheckMySpot requires users to view a short instructional video on how to take a high-quality image. If an image does not meet the necessary criteria, users are asked to resubmit the image alongside guidance on how to improve the photo.
To date, CheckMySpot has been downloaded nearly 1,400 times, with over 100 case submissions. Data from the app aligns with broader dermatological research. “Four out of five lesions that doctors see in a clinic visit are benign, and about one out of five are actually something that is suspicious for skin
cancer,” Webb says. “And that pattern has held true in what we see in our service.”
For those who need further evaluation, CheckMySpot’s preferred referral network of board-certified dermatologists is designed to expedite access to care. “When patients don’t indicate who their dermatologist is, we’ll select one in their area who has agreed to see these patients or have them scheduled within a week,” Webb says.
Neither the clinics nor CheckMySpot receives any monetary gain for the referrals. “That’s actually illegal,” Webb says. “But what it does do is provides physicians with an incentive in that they receive a case that helps expedite someone in need of urgent care.”
The app also has the potential to reduce the overall cost burden of skin cancer detection and treatment in the country. “Over $75 billion a year is spent in the U.S. on evaluating skin spots. Roughly $24 billion is spent on skin cancer evaluation and treatments, and that number continues to rise in direct correlation with the increased incidence of all types of skin cancer,” Webb says. By keeping four out of five benign cases out of dermatology clinics and ensuring the malignant ones are seen sooner, CheckMySpot has the
potential to lower healthcare costs both for individuals and insurers.
On a personal level, CheckMySpot users may discover cost savings as well. The app charges $70 per evaluation, an amount designed to align with the national average for copays. “We took an average copay amount, and this is a fee-for-service model. Currently, it is a non-covered service, but it is an eligible medical expense for health savings accounts,” Webb says.
While the cost may not be significantly lower than some insurance copays in Alabama, where the app is only currently available, the indirect savings— for such things as taking time off work, travel expenses, and lost wages—can add up, especially for rural patients, along with the at-home ease for elderly patients. “Your indirect savings is roughly $184,” Webb says, citing published research. CheckMySpot’s mission extends beyond cost and convenience, though. It is also looks to increase awareness of early skin cancer detection. “The majority of people who are seeing spots are seeing them throughout the year, and they’re not aware the clock is ticking,” Webb says. “Every four-week delay to definitive




At Hardware Park, we help bring new ideas to life. As a dynamic hub for real-world product development and NextGen education, we provide the design and engineering expertise, tools, and industry connections essential to turning ideas into reality. Embedded in Birmingham’s thriving startup ecosystem, we’re helping develop breakthrough medical devices — from advancing neurosurgery and fighting the opioid crisis to improving dialysis and restoring sight Tell us about your idea. It’s free, confidential, and you own the idea. Scan the code to get started today


HudsonAlpha Institute for Biotechnology, in collaboration with Phenome Health and the Buck Institute for Research on Aging, has launched a pilot study to explore how genetics and lifestyle influence a person’s risk of developing Alzheimer’s disease and related dementias. The study, called HOPE AD (Healthy Outcomes through Phenomic Explorations for Alzheimer’s Disease), is now enrolling participants at the Smith Family Clinic for Genomic Medicine in Huntsville.
Alzheimer’s disease and other dementias gradually impair memory, function, and quality of life. While there is no known cure, research suggests combining early detection with lifestyle changes may reduce the risk or delay onset.
“Alzheimer’s disease and other dementias begin years before any symptoms appear, so waiting until someone shows signs of memory decline may be too late,”

said Nick Cochran, PhD, HudsonAlpha Faculty Investigator and lead researcher at HudsonAlpha on the study. “This project is a chance to shift from reacting to preventing. We’re exploring whether giving people personalized health information can empower them to make changes that protect brain health.”
The pilot study will enroll 200 healthy adults between the ages of 65 and 75 who have a close family member (parent, sibling, or child) with dementia, but don’t have cognitive impairment themselves. The study uses a “phenomic” approach—capturing detailed data about participants’ health, environment, and lifestyle. This helps researchers paint a fuller picture of dementia risk than genetics alone. Results from the pilot will inform a more extensive study in the coming years.
Eligible participants will be invited to an initial visit at the Smith Family Clinic, where they will undergo routine medical exams, including cognitive testing and wellness assessments, and family history/medical history overviews. All participants will receive valuable clinical results, including:
• APOE status- a well-known gene linked to Alzheimer’s risk
• Polygenic risk score- an analysis that combines multiple genes to provide a more complete picture of disease risk
• pTau217 protein levels- a brain protein, or “biomarker,” known to be elevated in early Alzheimer’s disease
Individuals identified as having elevated risk will be invited to continue with the study through a year-long lifestyle intervention program. The program includes personalized coaching on several factors, including nutrition, physical activity, sleep, and cognitive engagement, all of which have evidence for reducing dementia risk. Researchers will also evaluate how these changes impact health over time.
“HOPE AD is about more than just biological data,” said Meagan Cochran, MS, CGC, Director of the Smith Family Clinic and study co-investigator. “We also want to understand how knowing their risk affects people’s choices. Do they feel more motivated to take action? That’s a crucial part of prevention that we hope this study will help answer.”
The long-term vision for HOPE AD is to help create a new standard of care. By determining what works, HOPE AD aims to develop screening tools and prevention strategies that could one day be used broadly in clinical practice.
“HudsonAlpha has long been a leader in genetics and genomics,” said HudsonAlpha President Neil Lamb,
(CONTINUED ON PAGE 17)

of Medicare, continued from page 12
the provider cannot bill Medicare for services rendered but can directly charge Medicare beneficiaries an agreed upon fee, without a limiting charge. To do so, the provider must enter into a private contract with the beneficiary setting out the terms of the relationship. There are specific requirements regarding what must be included in the private contract, including but not limited to clarification that the patient will pay out of pocket
for services, and that neither the provider nor the patient will submit a claim to Medicare for reimbursement.
Thus, while opting out may make sense for certain providers engaged in concierge medicine, it is a complicated process with implications that must be carefully considered and evaluated.
Kelli Fleming is a Partner at Burr & Forman LLP practicing exclusively in the firm’s Health Care Practice Group. Kelli may be reached at (205) 458-5429 or kfleming@burr.com.
PhD. “HOPE AD represents an exciting next step: using that knowledge to inform care, empower participants, and extend the number of dementia-free years people can enjoy.”
Researchers from both collaborating organizations believe HOPE AD could be a model for how precision health can reshape public understanding of Alzheimer’s prevention.
“Combining HudsonAlpha’s deep expertise in genomics with our experience in phenomic analysis and lifestyle
continued from page 16
behavior interventions could uncover actionable insights that lead to meaningful improvements in Alzheimer’s prevention,” said Jennifer Lovejoy, PhD with Phenome Health.
Study enrollment is open at the Smith Family Clinic for Genomic Medicine. To learn more about the HOPE AD study and see if you’re eligible for enrollment, visit hudsonalpha.org/hopead or call the Smith Family Clinic at 256-327-9640.
continued from page 14

treatment of a Stage 1 melanoma lowers survival by five percent. We’re looking to empower people to take charge.”
The app’s latest version during this past year of its soft launch, introduced new features to enhance the user experience. “You no longer have to draw a circle around the spot with an ink pen,” Webb says. “Instead you can drag and drop a circle overlay around the spot on your image. Another advancement is the inclusion of autofocus technology to improve image quality. Like when you remote deposit a check with a photo on your phone, you’ll get photo assist that will focus it properly.”




Bruce Korf, MD, PhD, the Distinguished Professor of Genetics at the UAB Heersink School of Medicine Emeritus, talks with Steve Spencer about genomic medicine.
CheckMySpot represents a notable
shift in how patients can take control of their dermatological health, particularly in rural areas where access to specialists is limited. “There’s no substitute for an in-person dermatology visit for a signifi cant lesion,” Webb says. “The point of CheckMySpot is to expedite care and reduce unnecessary clinic visits, which could have a meaningful impact on both patient outcomes and overall healthcare costs. The real mission that we have is getting skin cancers to definitive treatment earlier to improve survival, surgical outcomes, and reduce costs—both directly to a patient and indirectly to the





Listen on Spotify, Apple and Amazon at The Birmingham Medical News Doctor Talk. Or go directly with these

Bruce Korf, MD, PhD, the Distinguished Professor of Genetics at the UAB Heersink School of Medicine Emeritus, talks with Steve Spencer about genomic medicine.

Listen on Spotify, Apple and Amazon at The Birmingham Medical News Doctor Talk Or go directly with these QR codes:

When physicians, scientists and researchers with extraordinary talent and passion are given the technology, the facilities, and the support, they achieve great things. The discoveries, innovations and clinical trials happening today will help shape the future of treatments and lead to cures.

With Alabama facing a maternal health crisis, particularly for women living in rural and underserved areas, Governor Kay Ivey recently signed two bills that aim to provide aid to pregnant women.
The Presumptive Medicaid Eligibility bill allows pregnant women to receive up to 60 days of Medicaid coverage before full application approval, and reduces Medicaid coverage delays,
ensuring earlier access to prenatal care and better health outcomes for mothers and babies.
The Paid Parental Leave for State Employees and K-12 Educators legislation provides up to eight weeks of paid leave for full-time female employees and two weeks for full-time male employees following the birth, adoption or death of a child.
The Poarch Creek Indians have donated $750,000 to Atmore Community Hospital which is near their reservation. Previously, the Tribe donated $1,000,000 to the hospital during the Covid-19 pandemic.
“Rural healthcare is a necessity, not a luxury”, said Tribal Chair and CEO Stephanie Bryan. “We need to have access to a good hospital that is part of our community. We are blessed to be able to support Atmore Community Hospital and the wonderful people who work there and care for us.”
The Poarch Creek Indians are committed to improving the quality of life in Atmore and throughout the State.

Among the Tribe’s beneficiaries are schools, numerous education initiatives, healthcare, charities, and non-profits across the state.
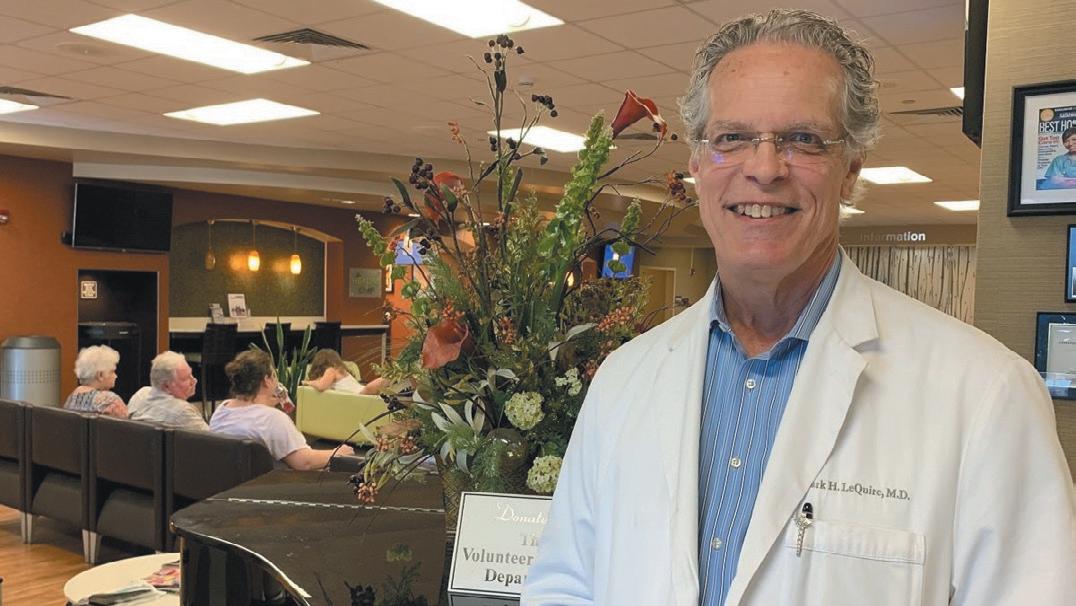
LeQuire, MD
Mark LeQuire, MD, a physician partner with Montgomery Radiology Associates, was sworn in as the new President of the Medical Association of the State of Alabama during the Association’s annual meeting in April. LeQuire, who has practiced for over 30 years, served the past year as Presidentelect of the Medical Association under President Amanda Williams, MD, whose term has expired.
“Being a physician is a calling—one that requires compassion, dedication and a lifelong commitment to our patients'
well-being,” LeQuire said. “Every physician, regardless of specialty, shares a deep responsibility to provide the best possible care, to advocate for our patients and to uphold the highest standards of medicine. I’m honored to lead the Medical Association in its mission to support Alabama’s physicians and improve healthcare for all.”
LeQuire earned his medical doctorate from the University of Alabama’s School of Medicine in 1982. He previously served as Chairman of the Alabama Board of Medical Examiners.
In March construction started on a $150 million tower expansion at Huntsville Hospital.
The five-story, 154,000-square-foot project will add 120 beds, a cardiothoracic intensive care unit, a neuro intensive care unit for neurosurgical and stroke patients, three floors of acute medical space and a new emergency department vehicle entrance.
“Expanding the Madison Street Tower will give us the space to meet the advanced health care needs of North Alabama and southern Tennessee
for decades to come,” said Jeff Samz, president and CEO of the Huntsville Hospital Health System. Additionally, the project will convert 70 existing patient rooms from double occupancy to single occupancy. When the expansion is complete the hospital will have a total of 931 patient beds, up from its current 881 beds.
Robins & Morton, which built the Madison Street Tower in 2006, is serving as the general contract on the project, with Chapman Sisson Architects providing architectural services.

There’s




EDITOR
Steve Spencer
VICE PRESiDENT OF
Jason Irvin
CREATIVE DIRECTOR
Katy Barrett-Alley
CONTRIBUTING WRITERS
Jane Ehrhardt, Ashley Franco, Laura Freeman, Lynne Jeter, Marti Slay
Birmingham Medical News
270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110
AD SALES: Jason Irvin, 205.249.7244
All editorial submissions should be e-mailed to: editor@birminghammedicalnews.com
Last year, sports medicine providers at UAB partnered with Bama Wellness Advocacy to launch a nutrition program for athletes in Birmingham City Schools, aiming to enhance the performance and well-being of student-athletes.
The pilot program began with the basketball teams at Ramsey and Huffman High Schools, and has been expanded to serve four of the city’s football programs, six of its basketball programs and some of the springs sports teams across Birmingham City Schools.
With registered dietitian, athletes can get counseling on topics like weight loss
and weight gain, education about eating disorders, and dietary recommendations for athletic performance.
“These young athletes are catalysts for change in their communities, specifically when it comes to prioritizing their health,” said James Jones, head athletic trainer for the UAB Department of Orthopaedic Surgery and Birmingham City Schools. “Their impetus for change has already influenced their family and community members to take steps to protect their health, and we hope that impact continues to expand as we grow this program.”
The UAB Emergency Department has earned the first Level 1 Accreditation from the American College of Emergency Physicians which represents the gold standard in emergency care.
A Level 1 emergency department must meet and exceed the program’s 34 common criteria, as well as additional requirements in physician and nurse staffing, in the availability of critical
The Alabama State Senate voted unanimously to pass House Bill 346 which removes the 100 hour minimum service requirement for retired physicians who volunteer at free clinics. The legislation, which has been signed into
personnel and resources for emergency care, and in creating a safe environment for patients and staff.
“Achieving the ACEP Level 1 Accreditation highlights UAB’s commitment to excellence in emergency care,” said Andrew Edwards, MD, professor in the UAB Department of Emergency Medicine.
Over the last few years, UAB
law, is expected to increase participation in the Retired Senior Volunteer Program, allowing more retired doctors to provide care to underserved populations.
Health Insurance from Alfa
House Bill 477 by Rep. David Faulkner, R-Mountain Brook, has been signed into law. The bill allows the Alabama Farmers Federation to offer health coverage plans to its members.
The bill was opposed by over 30 organizations including March of Dimes,

leadership has taken steps to expand its capabilities in emergency medicine.
In 2022, UAB President Ray Watts established the UAB Emergency Medicine Task Force, providing a framework to enhance patient care and operational efficiency. In 2023, Governor Kay Ivey authorized a $50 million appropriation to support the expansion of UAB’s emergency department.
Women’s Foundation of Alabama, American Heart Association, and the American Cancer Society Cancer Action Network. These opponents say lack of enforcement by the Department of Insurance will leave patients with nowhere to turn if their claims are wrongfully denied.
Sponsors of the bill say it will give Alfa members who earn too much to receive subsidies through the healthcare marketplace a chance at more affordable health premiums.
birminghammedicalnews.com







physicians, OB/GYNs, and primary care nurse practitioners to practice in rural, medically underserved areas in Alabama. ARMSA offers $50,000 a year for primary care physicians, with a 3-year maximum award period. The award is a service loan that is payable by years of service.











At the heart of one of the most highly regulated industries in the nation, health care facilities and providers face challenges that draw attention and resources away from their mission to provide quality patient care.
Burr & Forman’s health care team works alongside you to address and anticipate your needs by providing preventative guidance and pragmatic solutions, enabling you to focus on providing care and achieving healthy outcomes.
Alabama Health Care Team
Birmingham | Mobile | Montgomery
Jessie Bekker
Howard Bogard
Richard Brockman
Kelli Carpenter Fleming
Jim Hoover
Catherine “Cat” Kirkland
Garrett Lucey
Angie Cameron Smith
