




By JAne ehrhArDt
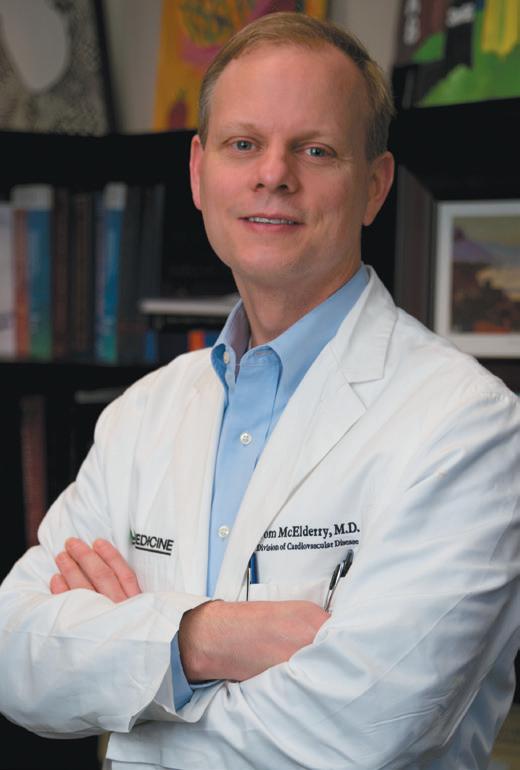
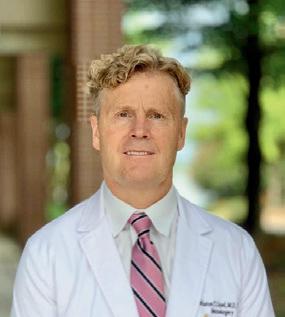
Electrophysiologist Tom McElderry, MD, with the UAB Cardiovascular Institute, became the first physician in the world to utilize a new vascular closure system to help stop the bleeding for procedures that need a larger venous access site.
The procedure using the Vascade MVP XL mid-bore venous closure system took place in mid-June, and the device achieved full market release on August 15. McElderry, also the co-director of the UAB Heart and Vascular Center, worked with the engineers at Haemonetics to produce the new device, which is an extension of the original Vascade MVP meant for smaller openings that has been
in use since 2019.
The device uses a collapsible disc technology with a collagen patch to close the venous access post-surgery. When the sheath, through which the instruments reach the surgical site, is removed from the vein, the collagen patch is applied and serves as a plug, causing less discomfort for the patient.
McElderry collaborated with the engineers in a series of experiments deploying collagen in preclinical models. The larger opening presented the team with two challenges. “We had to work on getting the collagen right—the volume that would consistently achieve hemostasis at the vessel,” McElderry says. “And we had to minimize the friction between the col-
lagen and the delivery system so that we could consistently deliver the collagen at the desired location.”
The use of collagen in the Vascade system has been a significant improvement over prior closure techniques. Before Vascade, closure was accomplished by putting direct pressure on the area or a stitch system. “The older ways of managing this could be uncomfortable for the patient,” McElderry says. “Surgeons would put a suture through the skin that needed to be removed later. It’s called a figure-of-eight suture, which can be uncomfortable while the stitch is in and then during the removal process. Patients had to lay immobile for six hours with a 10-
(CONTINUED ON PAGE 3)



By steve sPencer
In his 2015 State of the Union, President Obama announced the Precision Medicine Initiative with the goal of one day being able to tailor medical treatments to the individual based their genetic and health data. From that vision, the National Institutes of Health (NIH) created the All of Us Research Program. In order to accelerate medical research, the program aimed to build a database of health information on 1,000,000 people, and as of August has exceeded that with over 1,277,000 participants and counting.
People who join the program start by filling out a questionnaire that includes their name, where they live, along with basic questions about their health, lifestyle, and fam-








At the heart of one of the most highly regulated industries in the nation, health care facilities and providers face challenges that draw attention and resources away from their mission to provide quality patient care.
Burr & Forman’s health care team works alongside you to address and anticipate your needs by providing preventative guidance and pragmatic solutions, enabling you to focus on providing care and achieving healthy outcomes.
Alabama Health Care Team
Birmingham | Mobile | Montgomery
Jessie Bekker
Howard Bogard
Richard Brockman
Kelli Carpenter Fleming
Jim Hoover
Catherine “Cat” Kirkland
Garrett Lucey
Angie Cameron Smith

pound sandbag over the access site on the leg to allow for some healing of the opening into the vein.
“With the collagen-based devices, the post-procedure immobility time drops to two hours. The Vascade device delivers collagen right on top of where the sheath enters the blood vessel, so that it stops the bleeding at that site. It’s a more consistent closure, so we find less oozing and bleeding after the procedure. It also absorbs into the body over a period of weeks, requiring no post-operative removal.”
Besides the obvious positives of the shorter immobility time, the early am-
bulation after the procedure also helps older patients. “A lot of our patients have low back pain and having to lay for long periods of time makes that worse,” McElderry says.
Another advantage for patients is the same-day discharge on almost all procedures. “That even includes the procedures we’re doing later in the afternoon,” McElderry says. “Because of the truncated bed rest, they’re able to leave the hospital even if we don’t finish their procedure until five or six o’clock at night.”
Those same-day releases made the most difference during the COVID pandemic, when hospitals were inundated
with patients needing longer-term care. The original Vascade became available the year before COVID hit.
“There is a real need for closure of larger access sites now because there’s been an increase in several procedures, including pulse field ablation and the Watchman implant for left atrial appendage occlusion, that need larger sheaths,” McElderry says.
He and his partners have performed hundreds of these two procedures with the Vascade MVP XL in the last three months, which is engineered for closure following procedures requiring 10-12F sheaths (up to 15F in outer diameter).
continued from page 1
McElderry’s involvement in the progression of the collagen-based closure system will continue as the national primary investigator for an upcoming study to expand the indication for even larger sheath sizes.
He says that his time helping to devise the Vascade MVP XL was particularly satisfying. “It was absolutely fun working with the engineers,” he says. “And it’s always rewarding when it’s something that you worked on for so long, and worked on in the experimental environment, that you’re able to take to the patients and see the benefits.”
ily medical history. All of Us also asks for their medical records. Then they visit a participating clinic – UAB is partnering with All of Us in Alabama. There, nurses will take their weight, and measure their height, hips, and waist, as well as their blood pressure and heart rate. They will also give blood samples which All of Us will use to sequence their genome.
All the information collected is secure. Participants in the database are deidentified so that no name is connected to an individual’s data. The program has strict policies to prevent misuse of data, and has Certificates of Confidentiality from the U.S. government which will help fight legal demands to give out any potentially identifying information.
“The participants get some information on their ancestry, and reports on physical traits they’re likely to have based on their genome,” said Roger Smalligan, MD, MPH, who is Regional Dean at the UAB School of Medicine Huntsville and the site PI in Huntsville. “We run the entire list of actionable genes on every participant. There are currently about 60 different genes that are associated with risk for specific conditions. If someone has one of these genes, we will let them know, and they can decide whether or not to receive this information. We have a genetics counselor who people can talk to if they’d like help with this.”
Of course, simply having data doesn’t mean anything. It’s what you do with it that counts, and researchers are already starting to make use of it. “With this wealth of information, the potential studies are only limited to researchers’ imagination,” Smalligan said. “One example is with the G6PD deficiency. This results from mutations in the G6PD gene, and can lead to severe anemia, an enlarged spleen, and jaundice. We had always thought that a single defect was the main cause of this, but researchers using the All of Us database found 118 new variations that are also important risk factors for the disease.

Roger Smalligan, MD, MPH
“Some researchers are using this information for neuro degenerative disease like Dementia. We know a lot about these diseases already, but so far, the available medications haven’t been as impactful as we would like. If we can discover genetic precursors for dementia, we could attack it earlier. That would be a big help.”
It’s important to note that All of Us has an ongoing relationship with study participants, following them over a 10year period, and the program is continually coming up with ideas to source more information. For example, All of Us recently offered Fitbits to a number of participants. Program administrators mailed them the Fitbits, and taught them how to use it. Fitbits can gather information on activity, sleep, heartrate, and stress, and all that data is synched to the entire database.
Likewise, the NIH and All of Us recently rolled out a joint project to study the impact of diet on health. The program sends specific meals to the people who sign up, along with a schedule that includes breakfast, lunch and dinner. Program nurses will draw blood so researchers can look for correlations. With a level of detail that can include a person’s lifestyle, medical history, their genome, along with all the information obtained from a Fitbit, now including
diet, investigators can drill down to a granular level of research.
“When you feed all this data into an AI system, you’ll probably discover a number of unexpected correlations, and new findings,” Smalligan said. “And the potential studies that researchers can design with this data are unlimited. It’s really whatever a researcher can dream up.”
This has the potential to bring enormous value to the healthcare system. Currently, two patients with the same condition may respond differently to the same drug so physicians often have to try several prescriptions before finding the right one. Findings from the All of Us data will help healthcare providers prescribe the most effective drug at the outset, resulting in better health for the patient and lowering costs for the system.
For Alabamans who want to participate in All of Us, go to www.joinallofus.org/southern where you’ll find information on the program, and a link to sign up.





















By Ansley FrAnco
Christopher DeGroat, MD, an interventional cardiologist with Cardiology Specialists of Birmingham and St. Vincent’s, recently became the first in Alabama to perform the BTK scaffold procedure, a new drug-eluting resorbable scaffold that treats blocked arteries below the knee in people with peripheral artery disease (PAD), which can help prevent amputations.
DeGroat’s interest in finding solutions to PAD began three years ago when he saw a patient with a mild foot wound and referred him to a vascular surgeon. After he learned that the patient had their leg amputated, his career shifted.
“If you look at the morbidity and mortality of below-the-knee critical limb ischemia, 60 percent of people die at five years. So the outcomes are terrible. At that point in my career, I decided that I didn’t want to deal this with for my patients’” DeGroat said.
He found that there are limited options for below-the-knee intervention for people facing amputation or having debilitating pain. Vascular surgery has a poor long-term latency rate, and balloon
angioplasties show great results immediately, but have similar outcomes to surgical procedures down the line. Through LinkedIn, DeGroat found the BTK scaffold procedure and began training.
The procedure involves using a bioresorbable scaffold, usually to treat PAD in the belowthe-knee arteries. PAD is characterized by narrowed arteries, often due to plaque, that reduces blood flow to the limbs.


DeGroat’s patient, 72-year-old
Larry Chafin, a Vestavia resident, had leg pain for about six to seven years before seeing a physician who told him he had a 90 percent blockage in his legs. This is a common situation, according to DeGroat, since many people will ignore symptoms until the pain and/or numbness becomes too much to neglect any longer. Chafin’s cardiologist recommended him to DeGroat, and after two BTK scaffold procedures, one on each leg, Chafin quickly noticed results.
“The immediate result was getting


blood down to my feet because my toes were turning blue, so that was a relief,” Chafin said. “Right off the bat, some of the swelling has been relieved in my legs. When I do walk now, they still hurt, but I feel them. I feel the blood tingling going through, trying to go through my legs.”
When DeGroat completed this BTK scaffold procedure, only 500 had been done nationwide. DeGroat said this procedure is important for Alabamians.
“Unfortunately in the South, at times we struggle with getting some of these technologies in and giving our patients the same standard care as other parts of the country, especially in some of the rural areas,” DeGroat said.
Some risk factors for peripheral artery disease are high blood pressure, diabetes and obesity. Alabama ranks in the top five states of people with these risk factors.
DeGroat said he has seen an increase in peripheral arterial referrals, especially from northern Alabama and Atlanta. He hopes other community hospitals can continue to obtain new technologies to help the rural populations.
“The number one thing I hope to do is to make people aware of how prevalent PAD is,” DeGroat said. “I joke among patients that you only care about two things: feeling good and living a long time. And this is one technology that has shown that potentially does both of those things.”
We have two clinic locations, in Birmingham and Bessemer, so patients have the option to choose the closest location for them.
We’ve made referring easy by contacting and scheduling patients quickly and keeping you informed on their treatment plan.
•
•
•
•
• Visit alamedical.org/insurance for more details.
• Contact our Insurance Coordinator to start saving! (334) 954-2514 abeesley@alamedical.org
We provide a comprehensive treatment plan for patients, offering the most up-to-date and innovative treatment options.

#1
#2
Average resolution time = 47 minutes
We’re not talking response time, but the actual minutes it takes to solve your IT issue. The industry average is around 8 hours.
90-day client rating = 100% (460 responses)

Our HERO is the ambitious Practice Manager whose life is wrapped up in the success of the business – income, mortgage, retirement, even the kids’ college. They have a sense of humor but are constantly thinking about ways to improve their business, maximize productivity, and MANAGE RISK. They’re passionate about their business and take it personally when a competitor, hacker, or employee threatens their mission to improve the world.
We’re not about passing the blame. We fi nd solutions.









Apathetic or complacent US businesses who are willing to accept UNLIMITED RISK by ignoring today’s threats. Business owners who think, “it won’t ever happen to me.” Foreign Governments seeking footholds in the US or leverage. Cybercriminals who believe that all Americans are rich and therefore justified targets. Global crime syndicates who employ thousands in an Enterprise organizational structure. IT and Cybersecurity companies who take advantage of unwitting customers with Projects and Hourly Billing. The Cybersecurity industry as a whole, which has bored and confused the entire US public into a state of wanton vulnerability, while the hackers get better every day.
Practice Managers who are mature enough to understand that THEY OWN ALL THEIR COMPANY’S RISK, and who are willing to have routine, honest, and candid discussions about CYBER RISK MANAGEMENT and CYBERSECURITY / REGULATORY COMPLIANCE. They understand that by getting buttoned up and taking RISK seriously, they can maximize productivity, retire earlier, and send the kids to college debt-free. We are for HAVING FUN while making clients SAFER FROM CYBERCRIME. You know, CybertechnoLOLogy!
When you book a discovery, you also give Hand in Paw a boost in their mission to bring hope, healing, and unconditional love that only therapy animals and their handlers can provide. Help us reach our goal to donate $20,000 by year’s end to aid Hand in Paw in their services.



The solo “IT Guy” who doesn’t have the time, desire, or skills to keep up with ever-changing threats and subsequent countermeasures. Technology companies that baffle their customers into spending money on things they don’t need. MIND-NUMBING CYBERSECURITY TRAINING AND CONTENT that BORES AND CONFUSES NORMAL PEOPLE INTO NEVER GETTING ANY SAFER FROM CYBERCRIME. ANTIcybertechnoLOLogy.


CybertechnoLOLogist www.sipoasis.com



By lAurA FreemAn
Not long ago, surgery was primarily done in hospital operating rooms. This began to change as an aging population developed more chronic conditions that needed attention at the same time that many community hospitals were having to close their doors, which funneled more patients into city hospitals. Administrators faced a challenge in trying to schedule procedures for patients who were in pain, but whose conditions were not life-threatening.
Fortunately, advances in treatment and technology have expanded the types of care that could be completed in a day with the patient likely to go home the same night. This made ambulatory surgery centers (ASC) a new option that has quickly become a thriving alternative. As of June 2023, there were 5,828 ambulatory surgery centers in the United States, which was an increase of five percent over the previous year. The outlook for growth continues to be strong.
“Advances in surgical techniques are dramatically expanding the types of procedures that can be safely done in an outpatient setting,” Kelly Fowler, Administrator of Surgical Institute of Ala-
bama, said. “Medicare is shifting toward approving more acute conditions for treatment in ambulatory surgery centers, which is creating opportunities for continuing growth.
“We are already doing total joint replacement and spinal surgeries for patients who are happy that they don’t have to spend time in the hospital. They are up within a couple of hours, ready to start rehab, and they can go home the same day.
“Traditionally, most of the ASCs in our state have been multi-specialty, but we also have several that perform only eye surgery or gastroenterology procedures. As we see expansion into cardiology, urology and other specialties, I believe we will see more single-specialty surgery centers set up to handle these specific types of procedures.”
As technologies continue to evolve, ASCs can anticipate a growing demand from cardiology, bariatric surgery, colorectal surgery and higher acuity procedures from a wide range of specialties. ASCs that want to attract a following in a particular specialty may need to invest in specialized technologies. The revolution in robotics, imaging, optics and AI will likely affect future needs. There may also be regulatory requirements such as certificates of



need that will have to be addressed.
A number of hospitals have also opened their own outpatient centers for same day surgery patients. ASCs can free up hospital-based operating rooms and patient beds to handle trauma and sudden illnesses that don’t allow predictable scheduling. This also gives hospitals the opportunity to concentrate on more complex procedures that require longer recovery time and to make major investments in more sophisticated technologies.
In turn, ASCs can provide access and help avoid frustrations for patients who might otherwise see their wait for a minor procedure repeatedly extended due to emergencies that take priority. At 3:30 pm, even the most understanding patient who hasn’t been able to eat or
drink since midnight can become cranky with another delay. This could affect the review they give on care quality questionnaires that can affect reimbursement.
In contrast, ASCs doing the same types of procedures over and over are set up for efficiency. They can also shift staff early in the day to streamline admissions and handle routine paperwork and discharges later. This efficiency allows ASCs to offer cost advantages compared to hospital-based procedures, which is good for the coverage provider and the patient’s out of pocket costs.
An NIH study showed that 30-day outcomes in the sample reviewed were equal to or better than those for in-patient procedures. Patient satisfaction scores are also high.
(CONTINUED







By Beth neAl PitmAn
This article is Part 2 of a two-part series on the information blocking disincentives for healthcare providers that took effect on Aug. 1, 2024, following publication of the final rule in July by the U.S. Department of Health and Human Services (HHS).
In August, HHS finalized information blocking disincentives for healthcare providers that continue the agency’s commitment to encouraging permitted access to and exchange of electronic health information. The final rule specifically focuses on establishing disincentives for healthcare providers found by the HHS Office of Inspector General (OIG) to have committed information blocking.
The final rule maintains several noteworthy aspects from the proposed rule:
• Scope. Disincentives apply to healthcare providers, including hospitals, physicians, dentists, certain therapists and other eligible professionals participating in Medicare and Medicaid programs, and is not limited to persons regulated by the Health Insurance Portability and Accountability Act (HIPAA) or healthcare providers using certified Health Information Technology (IT).

• There remains a large gap in healthcare providers for which there is no current disincentive and we expect to see OIG and ONC address this gap.
• Healthcare providers will not be penalized for information blocking conduct attributed to a Health IT developer.
• There will be no “double” penalty for providers who may participate in multiple CMS payment programs, such as the Medicare Access and CHIP Reauthorization Act (MACRA), Merit-Based Incentive Payment System (MIPS) program
and Affordable Care Organizations (ACO) shared savings program.
• Impact. Facilities required to report Promoting Interoperability may see the greatest financial impact in Medicare reimbursement reductions. Hospitals will have a 75 percent reduction in the market basket update, and critical access hospitals will see a reduction from 101 percent to 100 percent of reasonable cost reimbursements. HHS estimated the impact in the range of $30,406 to $2,430,766. The AHA issued strong objections to the disincentives noting that the actual penalties may be higher by as much as three times and will have a disproportionate, inequitable and potentially destructive impact on hospitals.
• HHS estimated that the median group disincentive for MIPS clinicians will be $4,116, with a range of $1,372 to $165,326. Participation in MIPS is voluntary.
• Disincentives for ACOs and participants will result in removal from or denial of participation in the ACO for at least one year and receipt of related incentives. As noted by AHA, the ACO disincentive will negatively impact other ACO participants in the ACO
and community beneficiaries of the ACO activities.
• Attestations of no information blocking are required reporting in the MIPS and Promoting Interoperability programs. Providers found to be information blockers may also be subject to False Claims Act enforcement.
• Process. OIG is responsible for investigating and determining instances of information blocking. The OIG’s Information Blocking site includes specific resources for more detail. After a determination of information blocking, OIG will refer the healthcare provider to the appropriate agency, in this case the CMS, to impose the appropriate disincentives. During the investigation and prior to a determination of information blocking, OIG will coordinate with the appropriate agency (CMS in this case) regarding the potential referral for imposition of disincentives. The proposed OIG enforcement priority structure (which is not binding) was maintained in the final rule, which includes:
• resulted in, are causing, or have the potential to cause patient harm
• significantly impacted a provider’s
At UAB Medical West, our number one priority is to offer quality, convenient care for those in West Jefferson County, AL. Currently offering emergency care, two health centers in your community, and a brand new state-ofthe-art hospital just down the interstate, UAB Medical West is committed to being here for you and your entire family. It’s one more way we can offer quality, compassionate care near you.


By lAuren Johnson
Insurance companies have been gradually expanding the use of prior authorizations for routine medical care, which is bogging down physicians with paperwork and delaying care for patients.
Amanda Williams, MD, president of the Medical Association of the State of Alabama and a psychiatrist at Gardenia Cove Mental Health in Montgomery, is hoping insurance companies will hear their requests to improve the process and create a sensible system.
“We’re trying to come up with all these different ways to make the practice of medicine more sustainable,” Williams said. “We’ve had so many physicians burning out. Alabama has a huge workforce shortage of physicians, so we’re trying to do anything we can to make it more rewarding and fulfilling to be a physician. Most people didn’t go into medicine to fill out a bunch of paperwork and fight with insurance companies to get a patient what they need.”
Prior authorization started as a requirement for rare or expensive treatments, but now it’s required for almost
anything that the insurance company could pay for, including medical procedures, medications, diagnostic tests, surgeries, follow-up care, and more. This time-consuming process slows everything down, causing frustration for patients and physicians.
“The more insurance companies deny and put roadblocks up, the less likely it’s going to be for them to have to pay for these things. I have multiple patients who have given up on it and paid cash for some of their medications because they need them and they don’t feel like fighting with their insurance company anymore,” Williams said.
Williams found a survey that reported one-third of Alabama doctors spend almost an entire workday each week filling out prior authorization paperwork, following up with phone calls and fighting denials. This leaves doctors with less time to see patients.
“It’s a nationwide issue,” Williams said. “Obviously, every region and every state has their own particular problems, but for Alabama physicians, this has come up over and over again as one of the key frustrations in the practice of medicine.”


Right now, the system is redundant and creates more hoops for physicians to jump through to provide medical care to patients. If the prior authorization is automatically denied, there is an appeal process that involves more paperwork and sometimes doctors must redo forms they’ve already filled out.
“Even once they’ve been approved, especially for chronic conditions, you have to repeat the prior authorization again,” Williams said.
If a patient changes insurance companies or if an insurance company changes their policy, there can be a gap
in care while doctors redo the paperwork again to get it approved.
“Some of the things that they’re requiring prior authorization for are cheap. It’ll be a medication that, if you pay with GoodRx, you can get it for next to nothing, and we’re still having to spend all this time to do a prior authorization,” Willaims said. “Some of it’s just a waste of healthcare dollars, on their end and on our end.”
In this new campaign, physicians are asking for timely responses, within 24 hours for urgent cases and within 48 hours for less urgent cases. They’re asking to remove the repetition of prior authorizations for patients with chronic conditions. If something is approved, they ask that the insurance company not change the decision later to a denial. They’re asking for all the forms to be electronic, removing the excess paper and the use of fax machines. They’d also like the insurance companies to publicly report the data of approvals versus denials, and if something is denied, they’d like to have a peer-to-peer evaluation with someone who has clinical knowledge of the treatment or medication
(CONTINUED ON




















With a focus on developing minimally invasive technologies in the diagnosis and treatment of thoracic disease, Dr. Minnich performed the rst electromagnetic navigational bronchoscopy (ENB) and the rst robotic bronchoscopy in the state of Alabama. As a result, he has developed some of the most indepth experience with these surgical technologies in the world, including offering endoscopic thoracic sympathectomy, which is the most effective treatment for hyperhidrosis (excessive sweating).
Visit alabamathoracicsurgery.com for the extensive list of our services and procedures
ability to care for patients
• were of long duration
• caused financial loss to federal healthcare programs or other government or private entities
• Appeals . Neither the 21st Century Cures Act (Cures Act) nor the final rule establishes an administrative appeals process but instead defers to appeal processes available under the authority relied upon by HHS to establish a disincentive (i.e., authority for payments, recoupment, or contracting for Shared Savings Programs, MIPS or Promoting Interoperability).
• Timing . The Cures Act and HHS did not establish a time period for imposition of disincentives after a determination of information blocking has been determined, but defers to the timing requirements in regulatory authority for the agency imposing the disincentive.
• Enforcement Discretion . OIG will not investigate healthcare providers until after the effective date of the final rule and is exercising its enforcement discretion not to make any determination of information blocking, and related referral for imposition of disincentives, on conduct occurring prior to the effective date of the final


continued from page 7
rule. There is, however, no structure allowing OIG to exercise enforcement discretion, as there is with HIPAA, in either waiving or reducing penalties in light of voluntary corrective action or other voluntary remediation.
Anyone can submit an information blocking complaint to the ONC Information Blocking Portal or the OIG Hotline. From April 5, 2021, through August 31, 2024, over 1100 complaints have been received. OIG has determined that 1,059 are possible claims of information blocking, approximately 85 percent were filed by patients (which could also include attorneys on behalf of patients) and more than 90 percent were regarding healthcare providers.
Information blocking regulations have been effective since April 5, 2021, with a lengthy phase-in period. HHS reiterated through the final rule that its imperative to begin enforcement without delay is predicated on the fact that providers have had more than three years to implement an anti-information blocking




program. Providers should take the following steps:
• Review and Update Policies and Processes. Ensure that organizational policies and procedures align with information blocking regulations and promote seamless electronic health information (EHI) exchange. Assure that processes implemented align with policy statements and do not contribute to practices of information blocking.
• Privacy Compliance Integration. Monitor changes in privacy laws and integrate compliance with privacy laws, such as HIPAA’s reproductive healthcare privacy rules and Part 2 Substance Use Disorder privacy law, with processes to mitigate and prevent information blocking.
• Training. Provide comprehensive training to staff members on information blocking, including the definition, exceptions and potential consequences of noncompliance. Particular attention to staff responsible for Health IT, health information management and privacy is important.
• Monitor Compliance. Implement mechanisms to monitor and audit information sharing practices to identify and address any potential issues proactively. Address specific processes





for navigating privacy laws prohibiting or delaying disclosures, such as the recent HIPAA reproductive healthcare privacy rules.
• Health IT Coordination and Contracting. Investigate technology processes that can enable compliance with the Cures Act and assist in flagging and restricting disclosure of sensitive information that is either prohibited from disclosure or requires additional consents or other actions prior to disclosure. Contracts with Health IT vendors should include provisions requiring compliance with the Cures Act and affording healthcare providers with protection in the event the Health IT vendor engages in information blocking conduct.
• Mergers and Acquisitions Information blocking compliance should be incorporated into diligence reviews in transactional matters.
IN CASE YOU MISSED IT Part 1 of Holland & Knight’s series on information blocking disincentives appeared in the September 2024 issue of The Birmingham Medical News.





Indulge in the seemingly improbable luxury of a lavish restorative environment with personalized skin treatment.








By Jim hoover
According to a federal district judge in Mississippi, a cancer center’s investors bought themselves a lawsuit because of a conscious decision not to structure the ownership arrangement in compliance with a safe harbor. A federal district court in Mississippi recently denied a motion to dismiss filed by Magnolia Regional Health Center (MRHC) and its joint venture cancer center partners in a False Claims Act (FCA) lawsuit brought by the cancer center’s former executive director. The relator alleges that MRHC and its physician-investors violated the FCA because of alleged violations of the AntiKickback Statute (AKS) and Stark Law. The alleged violations originate from an alleged illegal kickback scheme inherent in the investment structure. It was clear that although the physician-investors were not required to make referrals to their investment—Magnolia Cancer Center (MCC)—the more they referred, the more they would profit. This was allegedly known at the time of MCC’s offering memorandum.
MCC was a joint venture formed in 2007 between MRHC and several phy-

sician-investors to treat cancer patients. MCC was voluntarily dissolved in 2020 after a consultant advised them that the structure could possibly be perceived as contrary to the AKS or Stark Law. The relator described a “bombshell” disclosure when he was personally present at the time the former MRHC CFO stated that “MCC had to be dissolved because it violated federal law.” Since the time the relator obtained his position, there were multiple attempts to unwind the joint venture and restructure MCC. However, the complaints regarding the alleged violations
went unaddressed and the structure was not voluntarily dissolved until 2020. Defendants admit the dissolution occurred after a consultant advised them “that the structure could possibly be perceived as contrary to the AKS or Stark laws.”
The relator filed his qui tam lawsuit alleging that certain physicians and medical clinics violated federal statutes including the AKS and the Stark Law, by referring patients to a MCC in which they were investors. The AKS makes it illegal to offer or pay remuneration to induce referrals of individuals for the furnishing of services paid for by a federal health care program. The Stark Law provides that, if a physician has a “financial relationship” with an entity the physician “may not make a referral to the entity for the furnishing of designated health services for which payment otherwise may be made under” Medicare, and “the entity may not present or cause to be presented a claim” to Medicare for such services. The complaint further alleged that, by falsely certifying that their Medicare billings were compliant with the law, the investors violated the FCA.
To be clear, the case is still pending and not close to final. What was before
the court were motions to dismiss the qui tam complaint filed by MRHC and the other investors. The court noted that the complaint contained considerable objective written proof in the record supporting the contention that MCC was unwound based on concerns among its participants regarding its legality. Among such proof was an email in which a physician expressed his concerns about the legality of the venture to the relator: the joint venture was set up in such a way that participating physicians had a financial incentive to refer patients to MCC, since doing so increased their own investment income. Specifically, the physician noted that, while he was not required to refer patients to MCC, “the more I refer, the more I make.”
The court relied heavily on language in the offering memorandum that warned of possible non-compliance with the AKS. The judge opined that the investors made a conscious decision that they were not going to “due diligence” their way out of a good investment (or “kickback scheme”), and it further appeared to the court that, in making that decision, the investors “bought themselves
(CONTINUED ON PAGE 11)




the current lawsuit.” The fact that the physician investors knew that they were “living dangerously” in the interests of investment profits was further confirmed by the offering memorandum’s notation that certain “safe harbors” existed under the AKS which allow physicians to invest in a manner which would give them reassurance that they were complying with the law, but that the MCC would not be structured in a way to comply with an AKS safe harbor. The court did however recognize that the defendants may have affirmative defenses to the alleged Stark law violations.
Although this case is still in its infancy and there are many unknown facts, there several reminders that health care provid-
continued from page 10
ers can take away from the case. First is the importance of complying with the Stark law, which reasonably appears to be called into question. Unlike the AKS, the Stark law requires strict compliance with a Stark exception. Thus, if there is any concern that the business arrangement does not comply with a Stark exception the health care providers should not enter into the arrangement as presented. The arrangement must be compliant with Stark or the health care provider-investors should walk away.
Second, often times investors and management believe relators are the rank and file of the organization trying to make a buck by filing a qui tam lawsuit. However, as is often the case, the relator
is usually another physician or member of management. As a result, compliance concerns or complaints from investors or management should be taken extremely seriously.
Finally, it is interesting to note that MCC decided to dissolve the organization. There may be numerous reasons for such a course of action. However, another alternative is to correct the organizational structure and make a Stark self-disclosure.
Jim Hoover is a health care trial and compliance Partner at Burr & Forman LLP practicing exclusively in the firm’s health care group. Jim may be reached by telephone at (205) 458-5111 or by E-mail at jhoover@burr.com.
continued from page 4







The forecast for ASC growth is not without challenges. “One of the biggest difficulties we face is the fact that to secure anesthesia services we have to pay stipends in addition to what the payer and the patient pay the anesthesia group,” Fowler said. “In the past, the reimbursements they received were enough to cover the cost. Now we have to pay the difference despite the fact that what ASCs receive in reimbursement is significantly less than what hospitals are paid for the same service, despite our record for good outcomes. Anesthesia services are an essential part of the team, and we understand that they need to be reimbursed for the valuable work they do. The key is finding an anesthesia partner to walk this road with you, one who will get creative in how we operationally work together, maximizing throughput and efficiency while looking for new ways to lessen overall costs.
“We also don’t necessarily have the favorable vendor contracts that hospitals tend to have. Although ASCs are known for efficiency and the savings that are helping to keep costs to Medicare and private payers lower, the reality is that costs are growing beyond what we can offset with efficiency and cost containment efforts alone. We have to negotiate contracts and reimbursements with fairness and real-world numbers in mind.
























“Overall, the future for ambulatory surgery centers is looking bright That should be good news for us, for patients and for everyone interested in providing access to efficient, affordable quality surgical care.”
continued from page 8







that is being discussed. Williams believes these changes will ease the administrative burden and make the process less painful for everyone.
“In the midst of this workforce crisis, we’re trying to figure out all the different ways that we can reduce the burdens of healthcare, anything we can do to prevent physicians from either retiring early or decreasing their clinical hours,” Williams said.


To address this issue, she and her team are gathering patient stories and physician stories about their experiences with prior authorization to bring to the insurance companies and leaders across the state. If you have experienced delays in care or if you couldn’t receive treatment because of prior authorization, visit the website www.ALFixPriorAuth. com to share your story.
By meGAn hAys, PhD
Productivity can foster a sense of accomplishment, reducing stress and cultivating a positive workplace environment with greater morale. Many everyday actions can kill productivity, causing us to feel like a failure and become stressed.
By addressing key productivity killers, from mindlessly checking emails to working excessive hours, individuals can enjoy benefits such as improved focus, efficiency and overall productivity. Improving your productivity requires identifying and overcoming common pitfalls that hinder efficiency. Productivity is not just about working hard but about working smart. Avoid mindlessly checking email and other messages
While intended to be a productivity tool, email can be a serious distraction and productivity killer. It is easy to justify checking emails and other messages as work, but that inbox can quickly consume productive work hours. We get drawn into procrastinating by answering emails because of a cognitive bias known as the mere urgency effect. The tendency is to choose completing a five-minute,
time-sensitive task over an important project that requires hours of focused or deep work. Perceived urgency tends to trump importance every time, even when the rewards of the less ‘urgent’ task are objectively greater.
To combat this, I encourage people to set aside specific chunks of time each day to address emails rather than answering each individual email as it comes in. Check your email and other messages in batches. Ideally, put your phone out of sight when you are at your work station. Some tips include avoiding looking at the phone during focused work, putting the phone on Do Not Disturb mode and checking communication apps only at certain times during the day.
Take steps to get sufficient sleep
Research has demonstrated that insufficient sleep impairs cognitive functions such as attention, memory and decisionmaking. Sleep deprivation also increases distractibility, making it difficult to focus and perform tasks efficiently. The cognitive impairment of being awake for 17 or 24 hours is comparable to having a blood alcohol content of 0.05 percent or 0.10


percent, respectively. Many people fall into the trap of sacrificing sleep for work but find themselves working more to make up for lost productivity due to sleep deprivation.
Making sleep a priority and keeping a consistent sleep-wake cycle is important to improving productivity. Guidelines suggest that adults should get at least seven hours of quality sleep per night, but this may vary from person to person. Understanding the link between sleep and job performance can equip people with the information needed to break the pattern of treating sleep like a luxury. The primary goal is to get the amount of sleep you need to feel rested and functional.
Getting better sleep can look like promoting a strong circadian rhythm by waking up around the same time every day, getting bright light exposure within an hour of waking and having a consistent bedtime routine. Bedtime procrastination can contribute to sleep deprivation. I recommend that people set a daily clock-out time for any remaining work tasks at home.
Multitasking is a myth
Multitasking may seem like a time saver, but this is a myth. Trying to do


two or more tasks at once often results in decreased efficiency, increased errors and lower-quality work. A cognitive phenomenon called the switch cost effect is the culprit. This is the extra time it takes the brain to shift its attention from one task to another, resulting in decreased performance. Every time we switch tasks, we need to disengage from the current task and reorient our focus to the new task.
Researchers have demonstrated that the cognitive load associated with task switching can accumulate over time and cost up to 40 percent of productive time. This can be mitigated by focusing on
(CONTINUED ON PAGE 14)

























By chArles hunt ii, mD, FAcs, rvt
As a Cardiothoracic Surgeon who has transitioned to the treatment of Venous Disorders, I have gained appreciation for the destructive nature of venous disease and become more aware of the misconception that saphenous vein reflux disorder and varicose veins are purely cosmetic. Tragically, the arterial system is synonymous with the vascular system. However this neglects the importance of the lymphatic and venous system. Dysfunction of either the lymphatics or venous system can be as equally devastating to a patient. A remarkable aspect of modern venous procedures is that it offers both curative and preventative measures.
In the absence of treatment, saphenous vein reflux disorder can advance to the end-stage symptoms or signs that consist of permanent edema, lipodermatosclerosis, destruction of the lymphatic system, and non-healing venous ulcers. Early intervention prevents these complications from developing.
Medical school and residency taught me that varicose veins were cosmetic. My experience as a vein specialist has demonstrated to me that varicose veins are

a risk factor for spontaneous thrombus formation with potential for propagation into the deep system or pulmonic embolization. Removal of the varicose veins eliminates the risk of superficial thrombophlebitis and subsequent deep vein thrombosis secondary to propagation. The majority of spider veins are truly cosmetic but a subset of spider veins are a bleeding hazard. I have witnessed significant blood loss secondary to prominent spider veins. Two main factors contribute to the bleeding risk. Venous hypertension and lack of sufficient tissue to assist in tamponade of the offending vessel. The vein is designed to withstand approximately 8 to 12 mmHg. A patient with saphenous vein reflux disorder may have
a venous pressure at the ankle of 120 mmHg. As one can imagine even a small puncture with a 120 mmHg of pressure and no overlying tissue can result in terrifying experience for an individual. Anecdotally, I have observed that the majority of cases of spontaneous hemorrhage occurs after a hot bath or shower secondary to vasodilation.
Modern treatment of saphenous vein reflux disorder provides patients with a safe and highly effective and definitive cure and the opportunity to prevent devastating complications.
20 years of experience in vascular medicine. He is the Physician-Owner of Alabama Vein & Restoration Medspa.

























continued from page 12 one task at a time with the least amount of distraction possible.
Practice directing your full attention to completing one task at a time, as opposed to attempting multiple tasks simultaneously. While it can be difficult, turning off your phone and email notifications can help you resist the urge to multitask.
Avoid the always on work culture
Thanks to the always on work culture, there is a common belief that more hours worked equals more productivity and demonstrates greater dedication. This is a dangerous myth that can lead to diminished cognitive function, reduced efficiency, burnout and increased errors. While it is true that putting in extra hours can result in increased output in the short term, there is an inflection point in which working long hours leads to diminishing returns. Do not equate hours worked with productivity. Instead of focusing on the number of hours worked as a badge of honor, I recommend that you prioritize effectiveness and efficiency. This means setting realistic goals, embracing downtime when needed, getting enough rest, engaging in enjoyable activities outside of work and effective time management during work hours. A healthy work environment that values efficiency and
quality output is more productive than one that values long work hours.
Without a plan, individuals risk spending too much time deciding what tasks to tackle next or how to approach them, leading to inefficiency and wasted time.
People fall into the planning fallacy thinking trap, which is the tendency to underestimate the amount of time needed to complete a big task. This is a big reason that to-do lists on their own can be counterproductive. Instead, try making an hour-by-hour plan for each day the night before. This strategy is called timeboxing, and it eliminates the dilemma of not being sure what to do next and increases accountability. This can be done on a phone notepad, a handwritten plan, sticky note or a digital calendar. The key is having a personalized planning system that is integrated into something looked at daily.
Improving your productivity requires identifying and understanding common pitfalls that hinder efficiency. By addressing these common pitfalls, you can improve your focus, efficiency and overall productivity, allowing you to achieve your goals with greater ease.
Megan
Hays, PhD is an Associate Professor and Director of Wellness Education at UAB.
The Association of TeleServices International (ATSI) is the trade association for providers of telecommunications and call center services, including telephone answering and message delivery, across North America and the UK.
At their recent conference in Detroit, ATSI honored Birmingham’s Jefferson County Medical Foundation Trust with the 2024 Award of Excellence. This was the 7th year that Jefferson County Medical
Foundation has received the award. ATSI contracts with independent judges to evaluate message services over a six month period. The scoring criteria includes:
• Response time.
• Courteousness of the representative.
• Accuracy of the call.
• Knowledge of the account.
• Overall impression of the call.
Shelby Baptist Medical Center has cut the ribbon on its new Nursing Education Hall, a project funded by the Baptist Health Foundation. An approximately $20,000 project, the renovated hallway features several hospital rooms and simulation labs where nursing students and staff can advance their healthcare training.
“This space will offer an immersive, hands-on experience,” said Shelby Baptist CEO Holly Dean.
The project was spearheaded by Brookwood Baptist Health Nurse Educator Charman Harper, DNP, RN. Harper went to Dean with the idea and led the way from conception to the ribbon cutting.
The Nursing Education Hall is located on the second floor of the main hospital to the left of the Cardiovascular Unit and is open to all Shelby employees and student nurses.
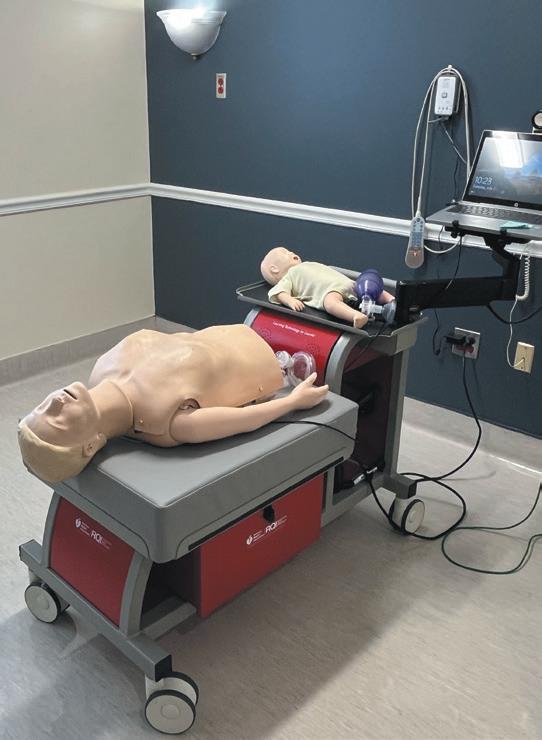
Nursing Education hospital rooms.




The Alabama Board of Medical Examiners is offering several new online Continuing Medical Education (CME) courses, now available to licensed physicians in the state.
"The introduction of these online CME courses marks a step forward in our mission to enhance the quality of healthcare in Alabama," said William M. Perkins, Executive Director of the Alabama Board of Medical Examiners.
The initial course offerings include:
• Understanding Collaborative Practice in Alabama
• Supervisory Practice in AlabamaRoles & Responsibilities
• Supervisory Practice in Alabama - The Role of an Anesthesiologist Assistant and Supervising Anesthesiologist


EDITOR & PUBLISHER
Steve Spencer
VICE PRESiDENT OF OPERATIONS
Jason Irvin
CREATIVE DIRECTOR
Katy Barrett-Alley
CONTRIBUTING WRITERS
Jane Ehrhardt, Ashley Franco, Laura Freeman, Lynne Jeter, Marti Slay
Birmingham Medical News
270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110
AD SALES: Jason Irvin, 205.249.7244
All editorial submissions should be e-mailed to: editor@birminghammedicalnews.com
FOLLOW US
Scan to visit birminghammedicalnews.com
The Patient-Centered Outcomes Research Institute, a non-profit that funds clinical effectiveness research, has awarded the UAB Department of Family and Community Medicine with $11.4 million to lead a study into how primary care can help patients with physical disabilities, who also have Type 2 diabetes or other chronic diseases, best manage their health.
The multisite study will compare the effectiveness of digital health coaching, remote patient monitoring and a combination of these options for improving blood sugar levels in people living with physical disabilities, Type 2 diabetes, and at least one other cardiometabolic or cardiorenal comorbidity, such as hypertension, congestive heart failure, coronary artery disease, cancer or chronic kidney disease.

Telehealth programs, including digital health coaching and remote patient monitoring, are increasingly used, especially for those who have limited access to inperson health care. However, more information is needed to demonstrate which option — or a combination of these interventions — is the most effective.
This trial will randomly divide participants into three groups to test different interventions for six months.
The group that receives remote patient monitoring will have a healthcare team checking and managing their blood sugar remotely. Participants will be provided the necessary devices and a mobile WiFi data plan to transmit the data. If a patient’s blood sugar remains elevated for a long period of time, a healthcare provider will offer guidance.
Born and raised in Birmingham, Dr. Armour graduated summa cum laude with a B.S. in Biomedical Sciences from Auburn, and received her doctor of medicine from the UAB School of Medicine. She went on to complete her OB/GYN residency at the University of Oklahoma Health Sciences Center. Dr. Armour practices all aspects of obstetrics and gynecology but holds a special interest in laparoscopic and spectrum robotic gynecology surgery. She focuses on compassionate and personalized care for all her patients.
A second group will receive digital health coaching, which involves oneon-one weekly phone calls with a health coach. This approach offers personalized support for participants on managing Type 2 diabetes, including advice on nutrition, exercise and taking medications. Finally, a third group will receive a combination of both the remote patient monitoring and digital health coaching programs.
This multisite trial will partner with health systems across the Deep South — UAB, the University of Mississippi Medical Center and LSU Health. Alabama, Mississippi and Louisiana currently rank near the bottom of all states for health outcomes, and have some of the country’s highest rates of diabetes and multiple chronic illnesses.



Scan to visit Birmingham Medical News Blog
• Long-term care
• Short-term care
• In-patient physical occupational & speech therapies Serving the Birmingham Community for over 38 Years
• 24/7 admissions
1201 N 22nd
Birmingham, AL 35234 205-251-5271 | Call us today for a tour!


With the nation’s largest healthcare law practice according to Modern Healthcare, Holland & Knight has more than 400 experienced attorneys covering virtually every segment of the healthcare industry, from transactional matters, regulatory compliance and real estate to litigation, government enforcement and public policy issues.
Our dedicated healthcare attorneys and professionals – in Birmingham and throughout the country – have the insight, experience, depth and resources to help promote and protect your interests.