Cullman Regional Starts a Neuroscience Department
 By Jane ehrhardt
By Jane ehrhardt
With the arrival of neurologist Muhammad Siddiqi, MD, on staff, Cullman Regional Medical Center has taken the first step toward creating their own neuroscience department. A daunting goal, neuroscience programs are among the most complex to create, partially due to the host of clinical conditions that call for an array of subspecialties.


The foundation of a solid neuroscience department relies on access to those subspecialists. UAB Medicine lists 78 neurologists who cover specialties from neuromuscular issues, memory and cognitive disorders, neuropathology to vascular neurology, sleep medicine, and neurooncology. Ten neurologists listed epilepsy as their specialty.
“We have to bring in more neurologists with subspecialty training. That is our future plan,” Siddiqi says. “As we see the
patient influx and see what type patients we are getting, that will be our priority.” Cullman Regional has been gathering patient data since Siddiqi arrived two months ago. Prior to that, an outside neurology practice provided services, leaving no hospital-focused data.

“My job is to slowly see where we are busy and where we need to grow based on patient population and the types of disease we are facing,” Siddiqi says, who spent years as part of a team building a neuroscience department at a large hospital in Tallahassee, Florida. At this early point, he sees stroke topping the list of needs for Cullman.
Right now, the hospital can medicate patients after diagnosis in hopes of dissolving the clot as quickly as possible to save brain tissue. But without a neurosurgeon trained in neurovascular procedures on staff, Cullman must transfer patients with large clots to UAB to perform those
Drs. Fulmer and Barlow Rock
By anSley FranCo
Many in the Birmingham medical community know neurosurgeon Ben Fulmer, MD and anesthesiologist Michael Barlow, MD, as the pair that spends hours together every week in the operating room. However, most of us aren’t aware that Fulmer and Barlow also spend some of their evenings and weekends together performing in their band, The Underhills.
Fulmer started playing guitar when he was 15. “I’ve always loved music, and I was trying to get attention from some people, so I figured I needed to pick up a few hobbies, and guitar seemed like the best way to do that,” he said. “My best friend played guitar first, so we played together, and we were a couple of geeky guys. I started playing the drums later when I beat my cousin out of some drums that were put in the

attic because it drove his dad insane.”
After being put on the piano bench by his parents as a kid, Barlow grew fond of music, and he played in a few bands during his school years. “I joined the Underhills to fill in that keyboard spot. I just love music and getting to perform,” he said.
The Underhills started with a group of neighborhood dads who had played in bands in their younger years and wanted to rekindle their musical talent. Nine years ago, Barlow joined the band to play the rhythm guitar and drums. Fulmer entered the following year, playing guitar to round out the sound. “We’re kind of a comedy act masquerading as a band as a bunch of middle-aged dads, but at the same time, when we show up, we want to play well. We try hard to put together something good,” Fulmer said.
The Underhills currently have a bass, (CONTINUED ON PAGE 3)
FOCUS TOPIC ONCOLOGY SERVING A 24 COUNTY AREA, INCLUDING BIRMINGHAM, HUNTSVILLE, MONTGOMERY & TUSCALOOSA NOVEMBER 2022 / $5 www.birminghammedicalnews.com FOLLOW US 866.951.7676 | DYNAMICQUEST.COM BIRMINGHAM HUNTSVILLE | MONTGOMERY MOBILE IT security & peace of mind Our Healthcare IT is just a phone call away—any time, every day
Muhammad Siddiqi, MD examines a patient.
(CONTINUED ON PAGE 3)
The Underhills dressed up as Devo for last year’s Halloween performance.
Welcome Our Newest Provider






Jeffrey Cuomo, MD Sports Medicine and Orthopedic Surgery










Accepting New Patients
Jeffrey Cuomo, MD is a board-certified Orthopedic Surgeon affiliated with Walker Baptist Medical Center in Jasper. He is sports medicine fellowship-trained with over 20 years of experience. He has served the community for over a decade including serving as a team physician for Jasper City and Walker County Schools. Dr. Cuomo has three daughterstwo at the University of Alabama and one in medical school at the University of South Alabama. He loves wakeboarding, hunting and Alabama football.
Sciatica (numbness or pain in or around the lower back, hip or knee)
Shin splints, plantar fasciitis and iliotibial (IT) band pain
2 • NOVEMBER 2022 Birmingham Medical News
Interests Now
Special
Acute and
Arthritic
Arthroscopic
Broken
Concussion
Joint
Knee
Muscle,
Call 205-221-5374 to schedule an appointment with Dr. Cuomo. Visit BBHCareNetwork.com to learn more. VIEW BIO 2950 Highway 78 East • Jasper, AL 35501
chronic tendon injuries
care
surgery
bones or stress fractures
management
replacement surgeries
problems
tendon and joint pain
Musculoskeletal injuries
Nonsurgical orthopedic care
Regenerative medicine
Sports injuries, trauma and sideline care
Cullman Regional Starts a Neuroscience Department,





procedures. “They can go through the leg to remove the clot from the brain,” Sid diqi says. “That’s why you need a neuro surgeon on board.”
In time, the hospital aims to acquire the staff and resources to attain accredi tation from the Joint Commission as a primary stroke center, and ultimately a comprehensive stroke center. Those des ignations confirm that a facility provides the critical elements for long-term success in improved outcomes for stroke patients.

Other units Siddiqi puts at the top of their neuroscience department goals in clude seizures, headaches, multiple sclero sis, and dementia. In his personal specialty, he has seen numerous misdiagnoses so far of headaches as migraines. “There are 24 types of headache,” he says. “If you treat those types of headaches with migraine medicine, it’s not going to work. You need a nerve block. You need a different type of medicine to treat those headaches.”
Memory issues can also be easily mis diagnosed. “The number one cause of loss of memory is depression. It’s called pseudodementia or false dementia,” Sid diqi says. “So memory medications are not going to help these patients.” Siddiqi has recently seen a 32-year-old man pre scribed medication for dementia for mem ory loss when the cause actually lay in his anxiety and depression.
All of these goals require patience and a vast financial investment well be
continued from page 1
yond the staff costs. “Building a neuro science department requires millions of dollars,” Siddiqi says. In equipment, a neurosurgical catheter lab for procedures such as removing clots, inserting stents, and preventing bulging aneurysms from bursting, runs around $3 million. CT brain scanners to detect viable tissue in the penumbra following a stroke cost $2 million. “It takes a lot of manpower and resources to build a department,” he says. “But when you grow, you are seeing more patients, so it eventually pays for itself.”
Cullman Regional already pulls in patients from in-between communities closer to Huntsville, including Madison County, and has experience drawing in patients all the way from Birmingham. One of their orthopedic surgeons still sees a group of patients he had when practic ing in Birmingham. All older patients who are also friends, they ask for appointments to be scheduled on the same day so they can ride together.
“They’re following the quality care,” Siddiqi says. “Distance doesn’t mat ter when you find a good doctor.” With the Birmingham neurology market get ting oversaturated and patients waiting months to get an appointment with a neurologist, he expects to welcome that overflow in Cullman. “You will go to the doctor who listens to you and treats you, even 45 minutes away.”
Drs. Fulmer and Barlow Rock,



continued from page 1
drummer, keyboardist, two guitarists and a lead singer who play a wide variety of music. “We like to fight about what we play more than anything,” Fulmer said. “We don’t want to play the old, tired songs that you’ve heard many other bands play, so we like to play fun, eclectic 1980s MTV rock and roll kind of stuff. We want to surprise people and get the wives dancing. We just try to make every body in their 50’s get loose like in the col lege band parties.”
“We play a lot of songs that you don’t hear bands play often because they aren’t easy. Springsteen’s Born to Run is a hard one to tackle, but we make them our own,” said Barlow.

Since the two joined the band, they have played at The Fennec, Birmingham Country Club, Avondale Brewing Com pany and private parties. “We are all so busy, and it’s hard to get us together in practice to get it all right, so we have to pick and choose where we play,” Fulmer said. The Underhills only perform four to five times a year, but you can always find the band on stage around Halloween time.
“Last year we dressed up as Devo and played at The Fennec downtown, and that was a blast,” Fulmer said.

“One of my most favorite perfor
mances was one Halloween when we per formed at the Saturn, and we all dressed up as Animal House and chose our cos tumes based on characters, we thought best fit our personalities. I thought up to that moment it was our finest moment, the best that we played,” said Barlow.

Though Fulmer and Barlow do not have much disposable time between work and their families, they both un derstand having an outlet is important. “Everybody needs something besides work to do to keep your sanity,” Barlow said. “For me, it’s not just playing music. It’s having friends you have something in common with. I like the relationships in the band and our camaraderie. You get burned out with just working, but if you have this other interest, it gives me something to look forward to.”





“We do these stressful jobs, and this is an incredibly different thing than what we do, day in and day out as surgeons,” Ful mer said. “I want to always be able to have a bit of a hand in it showing people a good time. It’s a crazy fun thing to do which is not like my typical day. It’s a privilege.”





Meet Our Nurse Practitioners!



National Nurse Practitioner Week is November 13th-19th and we’re celebrating by highlighting our highly skilled team of Nurse Practitioners! Our team works hard to provide the best pain care to their patients. When you refer to Alabama Pain Physicians, you can rest assured that your patients are in great hands.
Serina Bourassa, CRNP Anna Turner, CRNP Mickey Brown, CRNP
Jessi Barthelemy, CRNP Vanessa Daniel, CRNP Sara Byars, CRNP
David Lee, CRNP Heather Lee, CRNP Lauren Windsor, CRNP
BamaPain.com | 205.332.3160
Birmingham Medical News NOVEMBER 2022 • 3
Boothe Strives to Represent Alabama Physicians Through the Medical Association

 By Marti WeBB Slay
By Marti WeBB Slay
As president of the Medical Asso ciation of the State of Alabama, Julia L. Boothe, MD, MPH, FAAFP, wants to continue building an organization that represents physicians of all kinds, that collaborates with advanced practitioners and provides information that is critical to quality healthcare for Alabama.
Founder of Pickens County Primary Care, Boothe has a particular commit ment to rural health care. The Medical Association has a task force addressing that issue, especially in the Black Belt. “We still have a swath through the mid dle of our state where patients are sig nificantly underserved. We have some different state scholarships which have been out there for years to encourage people to choose primary care in a rural setting,” she said.
Boothe said the closing of rural hos pitals had made it even more difficult for beginning physicians to establish a rural practice. “When I first got out, I didn’t really know how to run a business. In the old days you just hung out a shingle, but with the way insurers are now, it’s more cumbersome. So, I was employed by our
























local hospital. Well, our local hospital closed two years ago, so we don’t have that infrastructure.”


For a list of the scholarships avail able for pre-med students, medical stu dents and resident physicians to help attract them to underserved parts of the state, visit alabamamedicine.org.


Expanding Medicaid has been an effort by the Medical Association in re
cent years. The website says, “Right now, more than 220,000 residents are caught in the state’s health ‘coverage gap.’ They earn too much to qualify for Medicaid and too little to afford private insurance.”
“We were able to get the postpar tum expansion approved and that went into effect earlier this year,” Boothe said. “New mothers now have postpartum coverage for a full year, where in the past they just had a few weeks of care. Our infant mortality and maternal mortality have escalated in recent years, and lot of that is due to not having health care for long after delivery. That was our first step: to get the legislature to expand to that group. We are hopeful we can use that data and information to push for ward so we can expand Medicaid.”
The Medical Association is also addressing the state’s opioid crisis. “It’s been going on for years, but now it’s in every community,” Boothe said. “We are trying to educate not only physicians, but also the public on what’s available, what to look out for and how to screen. Like every area of medicine, we are con stantly learning and evolving, so we’ve got to get that information out.”
“And we’re working on having more
cohesiveness between advanced practice providers such as physician assistants, nurse practitioners and nurse midwives. We know it takes all of us to make the team of health care succeed. The phy sicians in this state can’t see everybody, and we want to make sure it’s a true col laboration.”
The association also advocates and represents physician’s interests with the legislature. “We are one of the top groups legislators respect, and we are trying to build on that,” she said.
Boothe expects to see increased ef forts concerning emergency services around the state, to address gaps as a re sult of so many hospital closures. “A lot of us are dependent on an urban group to cover our areas, and they are getting pulled too,” she said. “In our county, an ambulance used to be gone about an hour to get to the patient, treat them and get them to the hospital. Now it’s pretty much a three-hour minimum to drive out of the county for every transport. And the hospital ERs are having such slow times due to the volume, so they can’t get pa tients off to release the EMS to take other calls. There are times in our county when there is nobody available.”
4 • NOVEMBER 2022 Birmingham
News
Medical
MALPRACTICE INSURANCE An individualized approach to your risk INSPIRIEN.NET 800. 821.96 05 Founded in 2003 by hospitals and physicians in Alabama, we have been dedicated to helping our customers manage the rising cost of malpractice insurance from the beginning. Whether a physician, allied professional, rural hospital or multi-state healthcare facility, we can help.
Tailored Underwriting with a wide range of policy options from fully insured to varied deductibles
Reinsurance backed by AM Best “A” rated partners from Lloyd’s of London
Risk Protection and Prevention Services built in with every policy including IQ 360 Claims, Risk Management, Legal and Underwriting Review
Over 100 years of collective experience in our legal and clinical support team, with many coming from Alabama healthcare facilities. (CONTINUED ON PAGE 7)
Medical Association President Julia L. Boothe, MD, MPH, FAAFP
•
•
•
•
A partner in healthcare law that


KNOWS


all the ANGLES

Waller is proud to be recognized as #1 in the South region in the ABA Health Law Section’s 2019 Law Firm Recognition List.

No representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers. Contact: Colin Luke 205-226-5717.
Driving business, practicing law. wallerlaw.com
Birmingham Medical News NOVEMBER 2022 • 5












6 • NOVEMBER 2022 Birmingham Medical News VIBRANT COMMUNITY. GROWING HEALTH SYSTEM. You work everyday to improve quality of life for your patients. Now it’s time to improve yours. – Modern, updated hospital Advanced robotics technology Full vesting of 403b match after 90 days – Immediate time off accrual – Tuition reimbursement, education starter loans and education partnerships – Free, convenient parking Scan the QR code to learn more about career opportunities at Cullman Regional.
Breast Cancer Screening Update
By laura FreeMan
Advances in breast cancer screening and treatment have made a tremendous difference in outcomes. Between1989 and 2020, death rates have gone down 43 percent. However, for populations most at risk for more aggressive and ear lier malignancies, detection is still often coming too late.
To give more women a better chance to be survivors rather than statistics, guidelines for best practices in screening are being enhanced. New tools and strat egies are aimed at finding these cancers earlier when they are more treatable.
“For women who have no addi tional risk factors or family history of breast cancer, the usual recommenda tion to begin mammography screening at age 40 still stands,” assistant director of UAB’s radiology residency program, Stefanie Woodard, DO said. “However, patients from ethnic backgrounds at greater risk of triple negative cancers, genetic mutations linked to more aggres sive cancers, or earlier changes in breast tissue should begin screening at age 30.”
Although African-American women have a slightly lower overall incidence of breast cancer than non-Hispanic whites, the American Cancer Society data shows that they are 42 percent more likely to die from the disease. Death rates are also higher among Native American, Alaskan Native and Hispanic popula tions. Women with an Ashkenazi Jewish background, descended from Jews who settled in the Rhinelands of western Germany and northern France in me dieval times, are also at higher risk of a BRAC mutation linked to aggressive breast cancer.
“Patients who have a close relative diagnosed with breast cancer should also be referred for early screening,” Woodard said. “If the relative’s cancer occurred at
 Woodard, DO
Woodard, DO
an early age, the patient and her doctor may want to consider beginning screen ing up to ten years before the relative’s cancer was diagnosed so that any changes can be detected as early as possible.”
In addition to weighing genetic in fluences in deciding when screenings should begin, physicians may want to consider age, tissue density and past find ings in deciding which type of screening to order. Woodard’s area of expertise is in breast cancer screening and imaging, a field that has been expanding and is re fining the diagnostic toolbox to provide a more precise screening.
“Breast tissue tends to be denser in younger patients, and ultrasound or breast MRI may offer a clearer, more definitive view,” she said.
MRIs can provide a 3D view and in women with variations in tissue, it can be helpful in distinguishing between fluid-filled cysts, suspicious anomalies and harmless anatomical differences unique to the patient.












“One of the options physicians may want to consider when ordering
Boothe Strives to Represent Alabama
Physicians, continued from page 1
Boothe estimates that only one-third to half of physicians in the state are members of the Medical Association, and she urges everyone to join, in order to make the association more effective.

“We represent all physicians in the state, whether they are a member or not,” she said. “We are working to help people un derstand why the Medical Association is here and what we do. I don’t think some know what we are doing for them. We meet face to face with various insurers each month, where we ask about issues our members have sent to us, including reimbursement issues or an authoriza tion problem and work through those.”
“We want people to be a part of our organization so that all our voices are heard. The best way to do that is to join, talk with us, let us know about your issues. We do our best to represent all the different specialties and bridge the gaps, because we are all in this together. We don’t want the ‘versus’ like urban vs. rural or super specialties vs. primary care. It’s going to take all of us to make health care work, and we know we’ve got things we want to work on for our state, but it takes having all of us at the table.”

For more information about the Medical Association and its programs, or to join, visit alabamamedicine.org.

for patients at higher risk and those who have issues that might make getting a clear image difficult is a contrast en hanced digital mammogram (CEDM),´ Woodard said. “It’s much like a regular mammogram, but with dye to make dif ference in tissue clearer. It is faster, less expensive and less stressful than an MRI for patients who may be a bit claustro phobic. It could also provide the infor mation needed to avoid the worry and expense of an unnecessary follow-up procedure.”
“Mammogram technicians are welltrained to work with each patient’s in dividual anatomy to get a clear image. Since large breasts aren’t dense, they aren’t usually a problem as long as all tissue can be included in the images. Implants can also usually be shifted to allow traditional mammography. If the patient’s breasts are angled outward with tissue farther back toward the arm, tech nicians may include a third view on each side to make sure everything is visible.”
Although breast cancer is usually considered a disease of women, it can occur in men, which is an important point to keep in mind in evaluating symp toms in the chest area of male patients. Another consideration physicians are seeing more often is breast care in trans
sexual patients who are transitioning.
“A female to male transition with top surgery that removes all breast tissue also reduces the risk of breast cancer. A male to female transition with hormones over an extended period would create a need for regular screening,” Woodard said.
In addition to regular screenings, it can make a big difference for a patient when her provider explains what her lifetime risks of breast cancer are. Not everyone has a grandmother or great aunt to ask about family history. Basic genealogy genetic tests like 23 and Me or Ancestry may be able to provide clues to some mutations, but there are many other genetic, health and lifestyle factors that can influence risk.
That’s where a new type of clinic usually found at a larger medical cen ter may be able to help. “UAB has a breast cancer risk evaluation clinic that can combine current health data with biomarkers, personal history, family his tory, if known, and even genetic testing to give patients a better sense of their risks and the factors they can change for the better. This gives patients and their physician a starting point for developing a screening plan and working toward a healthier future,” Woodard said.
WE USE THE PERSONAL TOUCH.
how we make a difference in your debt collection. After 25 years, we know the best way to recover overdue balances is hands-on. No automation, no robots, just a personal outreach and connection.
Birmingham Medical News NOVEMBER 2022 • 7
DiRecManagement.com
It makes all the difference.
That’s
Call Nathan Ryan today and discover
can help
your
how we
improve
bottom line 251.344.6660 x298
JEFFCO
ONCOLOGY
ENDORSED BY
MEDICAL SOCIETY
Stefanie
The Disparity Dilemma
Why Are African American Women More Likely to Die from Breast Cancer?
 By laura FreeMan
By laura FreeMan
According to American Cancer So ciety figures, African American women are slightly less likely to have breast can cer—but if they do develop the disease, they are 42 percent more likely to die from it. The question is why.






“It’s a combination of biology, access to health care, and a whole range of eco nomic and social factors,” Erica StringerReasor, MD said. An assistant professor at UAB, she works in hematology and on cology, focusing on translational research in the treatment of highly aggressive women’s malignancies, including triple negative and HER2+ breast cancer, as well as high-grade ovarian cancer.
“African-American women are more likely to develop triple negative and other highly aggressive types of breast cancer that are harder to treat and faster to kill,” she said. “Many live in areas where ac cess to health care is difficult and they may not have the financial resources to take off work and travel long distances for regular screenings that might detect the cancer early when it is more treatable.
“Another factor is likely to be the
overall health of African-American pa tients at the time they are diagnosed. There are often co-morbidities that put these women in a weaker position to fight the disease. They are at high risk of devel oping hypertension, diabetes, obesity and a rage of unknown and untreated or un dertreated conditions. This again stems from lack of access to basic healthcare. They may not have insurance through their work or be able to afford individual insurance or direct payment for care.
“Lifestyle factors can also contrib ute to risk. African-Americans are more likely to smoke. Food choices are influ enced by cultural traditions of high fat and high salt foods. Healthy foods are expensive and may not be readily avail able to people who don’t have a grocery store nearby.”

Timely treatment and monitoring for recurrence can also stack the odds for or against a patient. If symptoms are ig nored too long due to cost concerns, lack of awareness of their importance or of family history, cancer can gain a foothold that is difficult to overcome.
Another problem in beginning treat ment is knowing which treatments are
Erica Stringer-Reasor, MD
most likely to work for which cancers and which people. The unfortunate fact is that African-Americans have been seriously underrepresented in clinical trials for new medications and treatments. Although a trial can give a physician data on how well a treatment worked for participants, it can’t give a definitive answer whether the same results will hold true for patients who weren’t represented in the trial.



“We know that some medications, such as blood thinners, work very dif ferently in people with different genetic backgrounds. To be sure we are giving African-American patients the most ef
fective and safest treatment for the type of breast cancer they have, we need Afri can-American participants in those trials equal to their percentage in the overall population,” Stringer-Reasor said.
Unfortunately, efforts to recruit more African-Americans to participate in clini cal trials have been difficult. There is the lingering image of research that exploited African-Americans early in the last cen tury that is beginning to be resolved, but the difficulties of distance and economics have to be overcome to make participa tion easier.
“Part of that can be managed by working with health care partners in the communities where people live,” Stringer-Reasor said. “If the study re quires a blood draw, that would be easier to do in the local doctor’s office or health department than having to drive a hun dred miles every time.”
Awareness of trials is another area where we can do better. On diagnosis, every patient should be given access to current listings of clinical trials they may qualify for that might be beneficial for their condition.

“We make a point to get the word
Healthy is a fee ling we should all indulge.
Discover a renewed definition of skin care in a lavish, immersive environment. After all, health is a hard thing to overdo.
8 • NOVEMBER 2022 Birmingham Medical News TOTALON1ST.COM 1927 1ST AVE N, WOODWARD BUILDING, 1ST FLOOR
(CONTINUED ON PAGE 10)
ONCOLOGY
Exercise and Nutrition for Breast Cancer Survivors
By Jane ehrhardt
About 30 percent of all cancer di agnoses in females are breast cancer. Of those 287,850 new cases of invasive breast cancer annually, according to the American Cancer Society, about 85 per cent will survive for at least five years. That means that, right now, around 3.8 million women are breast cancer survi vors in the U.S.
What many may not know is the impact of weight, diet, and exercise on the chance of recurrence of their cancer. The Chan meta-analysis in 2014 delved into 82 follow-up studies covering over 200,000 survivors and found that women who increase their BMI by one category post-diagnosis, such as overweight to obese, increase their mortality risk up to 30 percent in the higher category.
“Many gain weight because of the chemo. Also, some forms of hormonal treatment can cause weight gain,” says Wendy Demark-Wahnefried, PhD, RD, a professor of Nutrition Sciences at UAB and Associate Director of Cancer Pre vention and Control at the O’Neal Com prehensive Cancer Center.
Exercise can mitigate that risk. “Re searchers have found that doing more physical activity reduced the risk of dying
in survivors from breast cancer by 40 per cent, even if they had not exercised before diagnosis,” says Laura Q. Rogers, MD, MPH, a professor at UAB Heersink School of Medicine department of medicine.

A 2014 meta-analysis parsed out the amount of exercise to show that one, two, and three hours of brisk walking after a breast cancer diagnosis reduced the risk of dying from any cause by 13, 24, and 34 percent, respectively, and dying from breast cancer specifically by 6, 11, and 16 percent. “The take-home message is, try to do at least two to three hours per week, but even doing one hour a week is beneficial,” Rogers says.
Exercise also mitigates the high risk




of mortality breast cancer survivors face from cardiovascular causes. “Survivors are more likely to die from cardiovascu lar disease than breast cancer,” DemarkWahnefried says. A 2022 study in the Journal of Clinical Oncology of 13,642 women broke down the increased risk by their treatment. The highest risk of heart failure/cardiomyopathy was in survivors who received both anthracyclines and trastuzumab, though women who re ceived radiation therapy and aromatase inhibitors were also at increased risk over women without breast cancer.
Diet can help bolster the survivor’s system against the effects of treatment. For instance, alcohol increases the activ
Welcoming our newest Nurse Practitioner
ASHLEY BOLER, CRNP
MEDICAL WEST CARDIOLOGY

Medical West is proud to welcome Ashley Boler , CRNP, to our team of medical professionals. Ashley is a board-certified Nurse Practitioner specializing in cardiovascular care. She received her Bachelor of Science in Nursing degree from Capstone College of Nursing at The University of Alabama and her Masters of Science in Nursing from The University of Alabama at Birmingham. Ashley is now seeing patients at Medical West’s Cardiovascular Services Health Center.

To schedule an appointment, scan the QR code or call (205) 481-7557.
ity of aromatases in the fat stores which is a suspected mechanism for breast cancer. “Aromatases produce internal sources of estrogen in post-menopausal women. We do not want high levels of estrogen, be cause breast cancer is a hormone-driven cancer. Anything that’s going to stimulate estrogen is not a good thing,” DemarkWahnefried says.
Lignans also reduce estrogen in free circulation in the body. A type of plant estrogen and a fat soluble antioxidant, lignans are found in foods such as flax seeds, sesame seeds, kale, broccoli, whole grains, and legumes, including soybeans. A review of 21 studies from the Ger man Cancer Research Center found that postmenopausal women with high lignan intakes were 14 percent less likely to de velop breast cancer. “Lignans bind to sex hormones and because breast cancer is a hormone-driven cancer, these lignans may be able to interfere with that path way,” Demark-Wahnefried says.
Many areas of optimum care for survivors remain unclear. All agree that a healthy diet of fruits, vegetables, whole grains, and lean meat is desired, and being overweight is bad. “Lose it slowly, though, like a half pound a week, because it looks like faster weight loss may actually cause
Medical West Cardiovascular Services Health Center
995 9th Avenue SW, Suite 407 Bessemer, AL 35022
P: (205) 481-7557
F: (205) 424-5585
Birmingham Medical News NOVEMBER 2022 • 9
ONCOLOGY
Wendy Demark-Wahnefried, PhD, RD
Laura Rogers, MD, MPH (CONTINUED
ON PAGE 10)
The Disparity Dilemma,
continued from page 8
out,” Stringer-Reasor said. “When a patient is diagnosed, we give them contact information with phone num bers and websites they can check for lists of the latest trials. We also do out reach, working with churches and civic organizations to have health days with speakers and we hand out informative flyers. We want to help people under stand the importance of breast cancer screenings and how they can get it done free or at low cost.”
“We want African-Americans to understand how important it is that we are well represented in trials so we will have solid answers on how well we can expect treatments to work for us. It’s a legacy we can give back to our community. It’s also a way to get access to the cutting edge treatments that might be the answer to changing the outcome of our illness, or at least giving us longer and better quality time with our families.”
Exercise and Nutrition for Survivors,
continued from page 9
too much stress on the body, which reacts with more inflammation. That may counteract the benefits of losing weight,” Rogers says.
Weight loss does reduce fatigue and can improve physical function ing, but it is not yet clear what its impact on breast cancer survival is. “We know gaining weight is bad. We don’t know if losing weight will help. That is what the BWEL trial will answer,” Demark-Wahnefried says.
The Breast Cancer Weight Loss ran domized phase III trial is expected to release their findings within a year on whether weight loss in overweight and obese survivors helps prevent breast cancer from recurring.
“There’s probably not ever going to be one single nutrient or food or exercise that makes all the difference to a breast cancer survi vor. There’s no magic bullet,” Rog ers says. The impact is made with an overall adjustment. To that end, Rogers and Demark-Wahnefried have created a year-long study called Amplify, now accessible at AmplifyMyHealth.org, where sur vivors find resources, information, and support for making the lifestyle changes to hopefully live longer and feel better. As Rogers says, “Noth ing can replace feeling better.”
More Hard Times for Hospitals
By tyler layne and Jay GreathouSe
about three-quarters of the outstanding amount had been repaid but it isn’t a dif ficult leap to imagine that much of the remaining repayment burden is borne by the smaller healthcare systems and inde pendent hospitals mentioned above.

ties and having the tough conversations and evaluating the current situation now can reap the benefits for years to come. With that in mind, before acting, hospital management and boards should make the following considerations:
Steep inflation, staffing shortages, supply chain disruption, the continuing impact of COVID-19 and other factors are putting financial pressures on hospi tals the likes of which we have not seen before. The grim reality is that the cur rent financial condition of the hospital industry is worse than it was in 2008 at the peak of the Great Recession.
Last year, hospital coffers were bol stered with federal COVID-19 relief funds, including the benefits of payroll tax deferrals and the Accelerated and Advance Payments Program imple mented in early 2020 by the Centers for Medicare & Medicaid Services. While the largest hospital systems were able to use these funds and programs to conserve cash for a potential downturn, many smaller systems and independent hospitals were forced to spend most or all of the funds they received. These hos pitals now face a liquidity crisis as funds are depleted while expenses remain high and the cost to borrow capital is growing ever more expensive.
One big cause of the downturn is required repayments for the Medicare loan program. Providers must repay the amount in 29 months, a time frame that ended this summer for those that received the advance payments in early 2020. The repayment period should end for pro viders by the end of 2022. As of May,
Higher expenses, largely driven by increased labor and supply costs, and the resulting squeeze on operating margins are other factors dragging down cash on hand. Hospital costs have been rising as inflationary pressures, workforce short ages, supply chain disruptions, and phar maceutical expenses combine to drive up overall operating costs. To make matters worse, there is no additional federal fi nancial support for hospitals in the fore seeable future.
It isn’t difficult to see that hospital leaders across the country are at a cross roads. While communities and their hospitals are unique, all U.S. hospitals – particularly standalone, general acute care facilities and small- to medium-sized non-profit hospital systems – face many similar challenges, including decreasing inpatient census, decreasing revenues, a move toward a value-based business model, and capital-intensive needs, such as physician and nurse recruitment, infor mation technology and facility improve ments. In light of the growing challenges standalone community hospitals and small- to medium-sized systems face, the expectations and challenges for boards, management teams, and elected officials have grown significantly.
While hospitals and smaller health systems undoubtedly face unprecedented challenges today, these times also present unique opportunities if tackled swiftly and proactively. The process can seem daunting, but management teams, boards and community leaders are tasked with preserving healthcare in their communi
• Remember your duties to the mission of the hospital or system and the provision of high-quality care in the geographic area served by the hospital or system.
• Identify the ideal end game and several alternatives and work backwards to assess what actions need to be taken in the near- and long-term to succeed.
• Think long-term in tandem with the short-term fixes that the hospital or system may need. Repeated short-term fixes may jeopardize long-term goals.
• Revisit your strategy regularly as facts and circumstances are fluid, and options and end games may materialize or become unavailable.
• Surround yourself with experts who have helped management and boards with creative financial, operational, and legal decision-making to preserve care.
• Make a plan to communicate with your constituents, including physicians and the public, and follow through on that plan regularly.



• Identify potential roadblocks and work proactively to address them. Being reactive lengthens the process and lessens the prospects for success.
• Address regulatory compliance and ensure that day-to-day operations are as unaffected as possible by the strategic decision-making being undertaken.




Tyler Layne is a partner at Waller where his legal practice focuses on advising healthcare clients in restructuring matters
Jay Greathouse is a partner at Waller where he advises not-for-profit and investor-owned healthcare clients in acquisitions and divesti tures and complex joint ventures.

practice in rural Alabama
10 • NOVEMBER 2022 Birmingham Medical News ARMSA is administered by the Alabama Office of Primary Care and Rural Health and is supported by the Office for Family Health Education & Research, UAB Marnix E. Heersink School of Medicine For details visit https://aohw.org/2021-armsa or email ARMSA@uabmc.edu Apply for ARMSA today! Answer the call
We’re
•
• internal
•
•
Earn $50,000 a year! ARMSA
to
The Alabama Rural Medical Service Award (ARMSA) incentivizes primary care physicians and NPs to practice in rural, medically-underserved areas in Alabama. Eligible PCPs receive $50,000 a year and NPs receive $30,000 a year for up to 3 years as a service loan payable by years of service. PCP and NP must not have practiced in the rural area within 3 years of October 1, 2021.
looking for NPs in family medicine and for physicians in the primary care fields of:
family medicine
medicine
general pediatrics
internal medicine/pediatrics





















Birmingham Medical News NOVEMBER 2022 • 11 Call 205-221-5374 to make an appointment. Scan the QR Code or visit BBHCareNetwork.com to learn more about Dr. Prevost. Welcome Our Newest Provider Mark Prevost
Spinal Orthopedic Surgery Mark Prevost
MD is an Orthopedic Spine Surgeon and is affiliated with
Baptist Medical Center
He returns home to
after completing his medical education and training in
and
offers the latest technology in spine surgery. Areas of Interest Minimally Invasive Spine Surgery Disc Replacement Lateral/Anterior/Posterior Lumbar Fusion Anterior Cervical Fusion Kyphoplasty Epidural Steroid Injections
II, MD
II,
Walker
in Jasper, AL.
Jasper
Alabama
Texas. Dr. Prevost










12 • NOVEMBER 2022 Birmingham Medical News your practice management SOLUTION a e i d i n g e s . W e a g e m p l e x w i n g t i v e i o n s , o u r o v e n y o u ' r e t i n g , v e r y o t u r n L e t u s k a s s o u f h e a l t h c a r e . c o m 2 0 5 - 5 5 8 - 2 5 0 0
Proposed Rules Could Impact
How Healthcare Providers Handle Medical Waste


















 By: anGie CaMeron SMith
By: anGie CaMeron SMith

In August 2022, the Alabama De partment of Environmental Manage ment (“ADEM”) published proposed changes to its rules for public comment. Specifically, the rules affect how a health care provider stores medical waste. If the proposed rules go into effect, many healthcare providers will either need to change the frequency with which they have medical waste picked up or they will need to obtain a permit as a storage facility. Consequently, it is important to understand how the rule changes might impact a practice, facility or provider.
WHAT IS MEDICAL WASTE?
Medical waste is defined by ADEM rules as “a solid waste or combination of solid wastes, which because of its in fectious characteristics, may either (a) cause, or significantly contribute to, an increase in mortality or an increase in serious irreversible or incapacitating re versible illness or (b) pose a substantial present hazard or potential hazard to human health or the environment when improperly treated, stored, transported, disposed, or otherwise managed.”
Additionally, a medical facility or person who produces or generates medi cal waste is a “Medical Waste Genera tor” under ADEM rules. This includes hospitals, nursing facilities, clinics, di alysis clinics, blood banks, dental offices, surgical clinics, medical buildings, health maintenance organizations, home health agencies, physician offices, laboratories, emergency medical services, veterinary clinics, research and manufacturing fa cilities. Under the current rules, where more than one person (e.g., doctors with separate medical practices) is located in the same building, each individual busi ness entity is a separate generator.
What are the changes to the rules?
As a Medical Waste Generator, healthcare providers are already re quired to provide information to ADEM

Jefferson
Answering Service
about its operations, including a written plan on the management of the waste it produces. Under the new rules, a Medi cal Waste Generator will be required to register with ADEM, but there does not appear to be any fee associated with the registration. However, the changes to the rules create additional burdens by requiring a formal management and training program.
The proposed rules require a Medi cal Waste Generator to develop a train ing program for facility personnel whose “duties have a direct effect on medical waste management and/or medical waste accumulation.” There is no fur ther explanation or identification as to which personnel that applies, but the training program requires “classroom or on-the-job training” that teaches com pliance with ADEM rules on handling medical waste. This new training will add additional regulatory requirements for healthcare providers already subject to significant scrutiny for infection con trol and occupational safety measures.
Under the Generator rule, a health care provider cannot store medical waste beyond seven calendar days unless the waste is refrigerated, and then, it can only store the waste for 30 days. If a health care provider does store it beyond seven days unrefrigerated or for longer than 30 days refrigerated, the healthcare provider then becomes a “Storage facility” under ADEM’s rules. Many healthcare pro viders do not generate enough medical waste to warrant waste transport pick-up on a weekly basis nor do they store their medical waste in refrigerated storage con tainers. Therefore, many providers will become storage facilities.
As a Storage Facility, Proposed Rule § 335-17-4-.01 Storage of Untreated Waste states that those healthcare pro viders with no ability to refrigerate waste and who are unable to have waste trans ported from their facility or office within seven calendar days will be required to
obtain a permit from ADEM as a Stor age Facility. If a healthcare provider is able to refrigerate its medical waste but stores it longer than 30 days, it also is considered a Storage Facility. Unlike registration as a Generator, a Storage Facility registration comes with an ini tial fee of $2,630, and requires local government approval involving a hear ing and public comment in that local jurisdiction. See ADEM Proposed Rules §§ 335-17-8-.02 and 335-17-8-.03. One helpful provision is that storage of med ical waste begins after a shipping con tainer is prepared for shipment, and under existing rules, storage does not begin when it is placed in a container at the point of generation, such as a pa tient’s room, operating room or lab.
These new rules will likely result in many healthcare providers changing the way in which they store medical waste by either creating a means to refrigerate medical waste or paying for more frequent transport pickups. Either option chosen will not be inexpensive. In addition to the potential financial impact on the health care provider, the transport companies with whom those providers contract will likely be unable to meet an increase in de mand that these rules will generate.
WHAT’S NEXT?
The rules were published in the Alabama Administrative Monthly on September 1, 2022, and public com ments could be submitted to the agency through October 13, 2022. There was also a public hearing held at ADEM on October 13, 2022, to allow for ad ditional presentations or comments from interested stakeholders. Several organizations and associations repre senting healthcare providers in the state submitted public comments in opposi tion to the proposed rule because of the potential impact. One organization requested that ADEM submit an eco nomic impact statement before adopting the rule. Under Alabama law, if a party negatively affected by the rule change requests an economic impact analysis, the agency must prepare and submit a business impact analysis.
The earliest ADEM could consider adoption of these rules would be at the December 9, 2022 meeting.
Angie C. Smith is a Partner at Burr & Forman LLP practicing exclusively in the firm’s Health Care Practice Group. Angie may be reached at (205) 458-5209 or acsmith@burr.com.
Birmingham Medical News NOVEMBER 2022 • 13 Expect more from your lab 205-918-7156 • southeastlabs.com • Local testing • Accurate billing • Industry-leading turnaround times • EMR/EHR connectivity • Lower cost to your patients Let us create a customized laboratory solution for your practice At Southeast Clinical Lab, we give you more— CONTACT MARY WHITEHEAD 205-933-8601
Exclusively for medical professionals, The Service has provided reliable, caring service to physicians and their patients for over 30 years. • Change your schedule from computer, tablet or smartphone • Operator follow-ups with patient to confirm calls are returned • All calls recorded • Messages delivered via pager, text, phone, fax or email • HIPAA-compliant secure messaging After 6 months of scrutiny by trade industry judges, the Service beat call centers throughout North America & the U.K. with our distinguished customer service rapport, accuracy, & response time. Award of Excellence! Winner of the International ATSI 2018 – 2022
County Medical Foundation Trust
Rallying Around Clinical Trial Programs




 By lynne Jeter
By lynne Jeter
For the last three years, clinical trials have grown by 25 percent, yet participant pay remains arbitrary and inconsistent among studies.
“It’s almost like mismatched supply and demand curves,” said Gunnar Esiason, a patient advocate living with cystic fibrosis and a patient-facing strategist at Atlanta-based Florence Healthcare. “It’s time to talk about paying clinical trial participants more.”
Esiason, who has been involved in several clinical trials, likens clinical trial participants to medical pioneers.
“Together, we step into medicine’s frontiers, but we do so inside a culture that dismisses the value of patients,” he emphasized.

Participating in a trial can be like working for a company that hasn’t invested in its employees in a long time, explained Esiason, whose role at Florence Healthcare entails working with internal teams to set product and market priorities and speaking externally to the market to advocate for closing gaps in clinical trial processes.


“Of course, in this case, the employees are clinical trial participants,” he said. “The pay is low despite the time required to participate in research – and the growing number of trials that need participants. Increasing trial participant pay might be a path toward alleviating the participant supply crunch in trials hungry for patients. One key benefit of increasing pay for patients could be substantial: namely, speeding up clinical trials through a more competitive enrollment process.”


More than 80 percent of clinical trials fail to enroll on time, leading to costs of anywhere from $600,000 to $8 million daily and prompting trials to last twice as long. Moderately increasing pay has been shown to “motivate participation without being an unjust inducement,” said Esiason.







“In other words, patients are encouraged to participate–but not coerced to do so,” he said. “If increasing participant pay can accelerate trial enrollment, then a safe and effective drug can reach market faster and therefore leave products in the pre-revenue stage for shorter periods of time. The return on investment for study sponsors who increase participant pay should be clear to see from a business perspective.”









From a patient perspective, even a
marginal improvement on time to accessing new drugs is celebratory. Patients pay the cost of delay with their health.
“In the latest trial that I participated in, I narrowly fit the inclusion criteria for participation, while a close friend with cystic fibrosis didn’t,” said Esiason. “My health saw explosive improvement overnight, making it clear I was receiving the medication, and not the placebo, during the study. My friend, on the other hand, went in the other direction. After falling outside the trial’s inclusion criteria, she slipped into end-stage disease and sadly passed away. She missed the drug’s approval by a matter of months. Time matters not only for trial participants, but also the community of patients who rely on clinical trial outcomes.”
Patient compensation is typically based on the complexity of trials, independent of therapeutic focus, said Catherine Gregor, MBA, CCRP, chief clinical trial officer for Florence Healthcare.


“For example, CAR-T cell studies have a higher compensation than firstline chemo,” she said.
While the FDA acknowledges pay as a recruitment incentive, the agency leaves questions around the amount to individual review boards (IRBs). The result is a wide variation in the governance over research participant pay, with IRBs operating independently of each other.
“While the risk of coercion is certainly one worth acknowledging, today’s patients have access to more information about their own health and investigational products than ever before,” said Esiason. “With scientifically sound resources at hand and a broad cultural shift towards patient-centered trial design, patients have plenty of opportunity to critically appraise trials before consenting.”

With technology rapidly advancing to make trials more geographically accessible, it’s time the industry starts to treat patients according to what they are worth to increase trial access and participation, noted Esiason.
“A controlled increase in participant pay is a lever our industry and regulators should examine,” he said.
Even though inadequate pay for clinical trial participants has been an historical issue for decades, practical experience has shown a number of costs endured by participants are not compensated in traditional stipends, such as
14 • NOVEMBER 2022 Birmingham Medical News Birmingham ID & Infusion offers your patients needing antibiotic therapy or long-term biologic infusion therapies a unique outpatient alternative.
Always treated by trained infusion nurse
Supervision by a physician • Intake process completed by our staff • All insurance accepted • Open 7 days a week neurology | gastroenterology | rheumatology | pulmonology | dermatology | nephrology INFUSION THERAPIES FOR William Lapidus, MD Anurag Gandhi, MD Lily Colpitts, MD Bruce Tucker, MD 205-739-2266 BHMINFUSION.COM 4704 CAHABA RIVER ROAD, BIRMINGHAM AL 35243 Near I-459 and Hwy 280 behind the Colonnade OUTPATIENT INFUSION CENTER Provider Enrollment Coding Assistance Charge Entry & Review Claim Submission Payment Posting AR & Claims Appeals Patient Statements Patient Collections Patient Inquiries Analytics & Reporting CONTACT US TODAY 888.874.7084 (ext. 3 for Sales) Unrivaled Accuracy Our team has unparalleled experience, which means our clients collect more in revenue. N o Need to C hange So ftw are We work with countless EHR software platforms, so practices can get the help they need, without overhauling their operations True Customer Service No offshored call centers Our responsive, articulate team operates right here in the U.S. www.thevallettagroup.com | info@thevallettagroup.com Flexible, Comprehensive Revenue Cycle Management Keeping you close when you need it the most You are our focus. 205.838.3888 52 Medical Park Drive East, Suite 401, Birmingham, AL 35235 Simple access to high quality care is just around the corner. Board-certified specialists. 100+ caring sta . No parking fees. Close to home.
•
•
Why it’s time to talk about paying clinical trial participants more money
(CONTINUED ON PAGE 15)
Gunnar Esiason
The Time is Now for Advance Care Planning

 By CraiG Greer
By CraiG Greer
Most people don’t usually think about advance direc tives until a crisis occurs. This often leads to confusion and sometimes conflict if a person has never discussed the types of care they would want if they were unable to speak for themselves.
Advance Care Planning is more than just the legal document called an Advance Directive. True planning is about talking with loved ones and making sure they understand the types of treat ment you would and would not want if faced with a life threatening or life lim iting illness. The birth of the Advance Directive came through the courts. Life support technology outpaced our under standing, which means that if people did not recover, they could still be kept alive. No one knew when it was appropriate to turn off the machines. It had ever dis cussed before.


Today, we have gotten better about the legal document, but we have not im proved our discussions with loved ones about our wishes. Too often this conversa tion only happens when a terminal illness has been diagnosed – and that is the worst possible timing. People avoid the conversa tion out of fear of appearing to give up.
Respecting Choices, a group out of La Crosse Wisconsin, developed a great pro gram for hospitals, medical practices, social workers and churches to use. It encourages advance care planning in three stages.
The first stage is for people over the age of 18 to determine who would make medical decisions for them if they are unable to speak for themselves. This includes a discussion of types of life sup port they may want and under what con ditions. An example: I would want to be on a respirator if there is more than 20 percent chance that I will recover, or I want everything done to keep me alive.
The second stage of advance care planning is for people with a chronic ill ness. For instance, a person with heart failure or COPD can live a long time with good quality of life on medications.
There comes a time when the medications no longer work and it is important to discuss what types of medical treat ment a person might want and a discussion of when they might want to receive only comfort measures instead of aggressive treatments.

The last stage is for those who have been diagnosed with a terminal illness. For these people, it is important to discuss whether or not they would want CPR if their heart stopped beating and other aggres sive interventions such as tube feeding, or a respirator.
Having these discussions while a per son is healthy is never easy, but it is more difficult if faced with a life threatening illness. We should have these discussions periodically throughout our lives as we age and as our health condition changes.
My advance directive was different from my 30’s than it is now that I am in my 60’s. My wife and I have had many conversations over the years and have filled our advance directives out together and we are currently reviewing them again. We also make sure our children know our wishes.
Today, physicians are getting better about asking patients what interventions they would want, but this is a conversa tion that must happen with all members of the family so if and when the time comes, there is clear direction as to the wishes of the patient.
For more than 22 years I worked in hospice and one of the most difficult things to hear from family members is: “I know what I would want, but I don’t know what my ______ would want.”
There are great, free resources available on the internet including Five Wishes, The Conversation Project Starter Kit and much more.
One of the best gifts you can give your family members is the give of con versation. It is a difficult thing to do, but one of the most important conversations you can have with loved ones.





Rallying Around Clinical Trial,

copays, lost wages, childcare expenses, et cetera, said Esiason.
“Questions have always been about how to justify the cost to sponsors in the budget and then how to make sure we are ‘compensating’ and not ‘incentivizing.’ Re cent guidance from the FDA on inclusion and diversity in 2020 and 2022 suggests that sponsors and sites need to evaluate

continued from page 15
the use of compensation to reduce barri ers to recruitment and level the divide in socioeconomic impact,” he added.
Esiason emphasized his gratitude for the community’s willingness to rally around clinical trial programs.
“But clinical trials don’t exist with out us, so we need to demand more from them,” he said.
Birmingham Medical News NOVEMBER 2022 • 15 Now Accepting New Patients (205) 939-3699 AndrewsSportsMedicine.com Now Accepting New Patients (205) 939-3699 AndrewsSportsMedicine.com NOW ACCEPTING New Patients at our Birmingham Clinic (205) 939-3699 AndrewsSportsMedicine.com Christopher M. Beaumont, MD ORTHOPAEDIC SURGEON Hand, Wrist & Upper Extremity Specialist Learn more about Dr. Beaumont
C. Pitts,
MD ORTHOPAEDIC SURGEON Foot & Ankle Specialist Learn more about Dr. Pitts
Charles
Jr.,
Craig Greer is the Director of Special Projects with KanTime Hospice Software.
Craig Greer
Medical Malpractice Premiums Demystified








 By Stephanie dozier
By Stephanie dozier


In general, few people re ally like, understand, or want to spend money on insurance, but it could be the one thing keeping the doors open after an unforeseen event. There are many kinds of insurances that healthcare organizations should consider, but cost is often a key factor in prioritizing this protective cover.
As a medical professional liability insurer, we can share some insight on what goes into the cost, or “premium,” of insurance policies. There are three basic categories driving cost: market conditions (global reactions in the indus try), exposure (risks to be covered), and experience (history of losses).
MARKET CONDITIONS
Market conditions refers to the overall view of a particular product line and is typically cyclical in nature. It is often described as “hard and soft” mar kets. Social and general inflation drive this market reaction. The soft market is when premiums are low, and competi tion is fierce between carriers. The pre miums are generally low because losses are down and therefore, the majority of carriers are operating profitably, which attracts competition, further driving down premiums. The hard market is when premiums are high and there is less competition as non-specialty carri ers exit the line of business.
Hard markets usually occur when losses overall are increasing, creating the need for insurers to set aside more reserves to cover claims, as well as re spond to the increasing costs for rein surance (insurance for high losses). The two factors that contribute to loss activ ity are frequency (how many claims are occurring) and severity (the value of the claims). There are times in the market where frequency is an issue, but severity remains low. Then there are times when frequency is low, but severity is high. The worst scenario, of course, is when both frequency and severity are high.
The buzz word in the industry is a concept called “social inflation.” Social inflation is being driven by runaway jury verdicts, litigation funding by plain tiff attorneys, as well as an overall anticorporate sentiment. The unpredictable nature of these costs leads to higher premiums. General inflation also plays a role. Just like every other business, insur ance companies are negatively impacted by lower investment returns, increasing labor and supply costs, etc.
EXPOSURE
The type of exposures the healthcare business may have weighs heavily on insurance cost. Exposure can be broken down by classification, type of coverage, and location. Medi cal malpractice is based on classification. For providers, it is linked to their specialty. For healthcare facilities, it is the type of services they offer; e.g. in patient (occupied beds), outpatient (visits), emergency room (visits), labor and deliver (number of deliveries), mental health, re habilitation.
Most professional liability/medical malpractice losses are what are referred to as “long tailed,” while other types of losses like property claims are short term. This refers to the time it takes to settle the loss. Long tail claims typically involve liti gation and therefore are costly and time consuming. They can drag on, sometimes three to five years after the incident oc curred. The location of the exposure also can affect the premium. Things like legal jurisdiction, tort reform availability, as well as access to state patient compensa tion funds are factors to take into consid eration when pricing the risk.
EXPERIENCE
The last variable that contributes to premium pricing is the loss experience of the healthcare entity or provider. Typically, most carriers look at loss his tory going back five to ten years. A loss ratio, or total claims cost divided by pre miums, is used to gauge loss experience. Carriers will have target loss ratios for various types of coverage. In profes sional liability, a client with a 65 to70 percent loss ratio would be favorable. A carrier will want to see loss history, even if it was with another insurer. The main predictor of future losses is analysis of past experience. A longer the history of losses provides a more accurate predic tor of future claims.
Obviously, some of these factors are within control of the insured, while others are not. It will be difficult for a facility to be able to impact market con ditions, but effective risk management to avoid losses (experience) is an opportu nity to materially manage, even offset, rising premiums. Every effort should be made to manage risk well - not just to keep costs down, but more importantly, to protect patients in your care.
Hopefully understanding more about market conditions, exposures, and experi ence demystifies insurance premiums, and helps you as a consumer understand what can lead to fluctuations in premiums.
16 • NOVEMBER 2022 Birmingham Medical News Works for YOU! We Make Sure Your Evaluation is Right, The First Time We offer workers compensation and orthopedic spine solutions that help you get the right evaluation and the right care, every time. Our team can refer to any health system in the state of
Call Our 24/7 Dedicated SpineWorks Hotline Today: 205-202-5715 Fax: 833-673-0476 | www.myspineworks.com Works for YOU! We Make Sure Your Evaluation is Right, The First Time We offer workers compensation and orthopedic spine solutions that help you get the right evaluation and the right care, every time. Our team can refer to any health system in the
of
Call Our 24/7 Dedicated SpineWorks Hotline Today: 205-202-5715 Fax: 833-673-0476 | www.myspineworks.com A warm, caring alternative 205.933.2180 southhealthandrehab.com We deliver a safe and inviting home-like atmosphere for your rehabilitation or LONG-TERM CARE with the assurance of skilled nurses around the clock, along with NP and physician oversight. For post-surgery, our RAPID RECOVERY program targets therapy to face the challenges in returning home and meeting your speci c needs, including daily rehab services and pain management assistance.
Alabama.
state
Alabama.
Stephanie Dozier serves as Vice President of Underwriting for Inspirien.
Stephanie Dozier
We
Our firm works with all types of health care clients on business, regulatory, and litigation matters, covering every aspect of the industry. Burr & Forman’s regional health care group includes over 40 attorneys across the southeast.






Birmingham Medical News NOVEMBER 2022 • 17
the legal services
performed
quality
legal services performed
350 Attorneys. 19 Offices. Results matter.
No representation is made that the quality of
to be
is greater than the
of
by other lawyers.
care
you. Burr.com
about
Kelli Carpenter Fleming
Catherine
Robin
420
Street, Suite
GET-BURR
representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by
Howard
E. Bogard Richard J. Brockman
James A. Hoover
“Cat” Kirkland
B. Mark Lindsey Phillips Angie C. Smith
North 20th
3400, Birmingham, AL (800)
No
other lawyers. Alabama Health Care Team Birmingham, Mobile, Montgomery
Specialists Join Grandview Medical Group
in medical sciences from the University of Kentucky and earned his medical degree from the Alabama College of Osteopathic Medicine. He completed his OB/GYN residency at Beaumont Health in Trenton, Michigan.
John Richardson Jr, MD, cardiothoracic surgeon, has joined Grandview Cardio thoracic Surgeons. He earned his medi cal degree from the University of South Alabama College of Medicine and com pleted his residency in general surgery at the University of South Alabama followed by a fellowship in cardiothoracic surgery at the Medical College of Virginia Hospital in Richmond, Virginia.



Tyler Wahl, MD, MSPH, thoracic sur geon, has joined Grandview Cardiotho racic Surgeons. He earned his medical degree from the University of Alabama at Birmingham School of Medicine and com pleted his residency in general surgery at the UAB of Medicine, followed by a fellow ship in cardiothoracic surgery with focus in thoracic surgery.

cently by the Healthcare Advocate Summit, the premier event created by advocates for advocates for anyone involved in medication patient access, navigation and reimbursement.
Advocates of the Year were named in four categories, with Byars winning the Independent Advocate of the Year, the first award of its kind by the Healthcare Advocate Summit.

BCPAs are patient advocates, cre dentialed by the Patient Advocate Cer tification Board, who help patients and their families navigate the healthcare system. They aid in activities such as communicating with doctors, dealing with insurance companies, scheduling appointments and even finding legal resources.


Byars, one of the first two BCPAs in Alabama, obtained his certification in 2018 and founded Sun Back Moon in 2020 after years of trying to navigate the healthcare system when his daugh ter, Claire, was in cancer treatment.



McIlwain Re-elected to Board of Dental Examiners

Mark McIlwain, DMD, MD was re-elected to the Board of Dental Examiners of Ala bama by his col leagues. McIlwain is a board-certi fied oral surgeon and HighFive Healthcare part ner at Oral and Facial Surgery of the Shoals where he has practiced for 30 years. McIlwain was previously on the Board of Dental Examiners of Alabama from 2020-2021 where he served as board president during the height of the CO VID-19 pandemic.

Drs. Natalya Belotserkovskaya, Benja min “Ben” Rauh, John Richardson Jr, and Tyler Wahl have joined Grandview Medical Group.

Natalya Belotserkovskaya, MD, neurolo gist, earned her medical degree from the University of Alabama School of Medicine at Birmingham. She completed her resi dency training at the University of Cincin nati Department of Neurology and com pleted her neurology fellowship training at the University of Cincinnati.
Benjamin “Ben” Rauh, DO, an OB/ GYN specialist with Grandview Obstetrics and Gynecology, completed his under graduate education at Western Kentucky University. He received a master’s degree

Jeff Byars Named 2022 Independent Advocate of the Year
Board Certified Patient Advo cate (BCPA) Jeff Byars, founder of Sun Back Moon, LLC – Private Pa tient Advocacy & Healthcare Solu tions in Cullman, was named 2022 Independent Advocate of the Year re

“My entire career had been spent in healthcare as both an Emergency Medical Technician and in hospital re imbursement. I thought I was set to navigate the healthcare system with ease,” Byars said. “But when a tumor was discovered in my seven-month-old daughter, I learned how difficult it is to navigate the system. If it was difficult for me with my background, it must be near impossible for someone with no experience with the system. This led me to patient advocacy.”
Children’s of Alabama Announces New Program, Bolstered by $600,000 Donation
Children’s of Alabama has received a $600,000 gift on behalf of The Bill and Pam Smith Family Foundation. This contribution enables Children’s to of fer specialized Nasoalveolar Molding (NAM) services to the region.

NAM is a pre-surgical cleft lip and palate therapy designed to reduce the size of the cleft by molding and repo sitioning the nose and mouth tissues prior to surgery. Infants wear a customfitted appliance, similar to an orthodon tic retainer, for an estimated 12 weeks, as long as 23 hours a day. Children tend to adapt well to the treatment, latching onto the appliance like a pacifier. NAM often reduces the number of surgeries needed to repair the lip and palate, and the treatment leads to better outcomes.
“When you have a child with medical complexity, it changes you,” Pam Smith said. “You see the world through a dif ferent lens.”
Bill and Pam Smith’s donation is in spired by their daughter Caroline. Fol lowing her birth in 2019, the Smiths navigated challenges seeking therapy for her cleft palate. At the time, NAM was not available in Alabama, requiring the family to travel back and forth to Children’s Hospital of Philadelphia for treatment.
Three UAB Physicians Join National Academy of Medicine
Drs. Marie-Carmelle Elie, James Markert, and Alan Tita, of the Marnix E. Heersink School of Medicine at UAB, have been invited to join the National Academy of Medicine, one of the high est honors that can be bestowed on a physician.
Marie-Carmelle Elie, MD, a profes
18 • NOVEMBER 2022 Birmingham Medical News GRAND ROUNDS
- MELODY WITH A DOTHAN FAMILY PRACTICE Birmingham 205-631-5969 | Montgomery 334-277-6201 | medisysinc.com PRACTICE MANAGEMENT | CLINICAL EHR | BILLING SERVICES | RCM
Long standing. Committed experts.
Top-level
support.
We have been with MediSYS for more than 25 years. It’s comforting to know MediSYS is always there for us.
Natalya Belotserkovskaya, MD Benjamin Rauh, D0
Tyler Wahl, MD, MSPH
John Richardson Jr, MD
Jeff Byars
Mark McIlwain, DMD, MD
EDITOR & PUBLISHER
Steve Spencer VICE PRESiDENT OF OPERATIONS Jason Irvin
CREATIVE DIRECTOR Katy Barrett-Alley
CONTRIBUTING WRITERS
Jane Ehrhardt, Laura Freeman, Lynne Jeter, Marti Slay
Birmingham Medical News
270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110
AD SALES: Jason Irvin, 205.249.7244
All editorial submissions should be mailed to:
Birmingham Medical News 270 Doug Baker Boulevard, Suite 700-400 Birmingham, AL 35242 or e-mailed to: editor@birminghammedicalnews.com
All Subscription requests or address changes should be mailed to:
Birmingham Medical News Attn: Subscription Department 270 Doug Baker Boulevard, Suite 700-400 Birmingham, AL 35242 or e-mailed to: steve@birminghammedicalnews.com

Cooper Green Adds Patient Portal
Birmingham Medical News is published monthly by Steve Spencer ©2021 Birmingham Medical News, all rights reserved. Reproduction in whole or in part without written permission is prohibited. Birmingham Medial News will assume no reponsibilities for unsolicited materials.
All letters sent to Medical News will be considered Medical News property and therefore unconditionally assigned to Medical News for publication and copyright purposes.
birminghammedicalnews.com
sor and chair of UAB Emergency Medicine, obtained her under graduate degree from Columbia University and her medical de gree from the State University of New York-Downstate with a dis tinction in research, along with an emergency medicine residency at Mount Sinai Medical Center. She is triple board-certified in emer gency medicine and critical care, as well as hospice and palliative care medicine.

While at the University of Medicine and Dentistry of New Jersey-Rutgers and then the University of Florida Col lege of Medicine, Elie launched and lead initiatives that combined emergen cy, critical care and palliative medicine.

James Markert, MD, the James Garber Galbraith Endowed Chair of Neurosur gery, graduated from Harvard University and his medical degree from the Colum bia University College of Physicians and
Surgeons, along with a master’s degree in public health before joining the neuro surgery faculty at UAB in 1995.
Cited by NAM as a world expert on oncolytic viruses, Markert has held positions in the American Association of Neurological Surgeons, Congress of Neurological Surgeons, American Academy of Neurological Surgery and the Society of Neurological Surgeons. He has served as president of the South ern Neurosurgical Society.
Cooper Green Mercy Health Services has added an online patient portal messaging system to help patients manage their health care. The portal allows patients to send a private, se cure message to their health care team and get a response within two business days, and facilitates prescription renewals and lists upcoming appointments. Lab results and health record infor mation are accessible to patients from the portal.
The portal is open to all pa tients of Cooper Green Mercy Health Services. Patients can sign up by sending an email to pa tientportal@cgmhs.org.



Alan Tita, MD, PhD earned his medical degree from the University of Yaoundé 1, Cameroon, followed by resi dency training at Baylor Col lege of Medicine and a fel lowship at UAB. He earned a master’s degree in public health from the University of Leeds, U.K., and a PhD in public health epidemiology from the University of Texas Health Sciences Center.
Tita holds the Mary Heersink En dowed Chair of Global Health and is the director of the Mary Heersink Insti tute of Global Health. As professor of OB/GYN, he also leads the Center for Women’s Reproductive Health. He has as a consultant for the World Health Organization, NIH, and the American Board of Obstetrics and Gynecology.
Providing Services at Grandview Medical Center
Our professional team of doctors, nurses, and staff look forward to seeing you.
Birmingham Medical News NOVEMBER 2022 • 19
FOLLOW US GRAND ROUNDS
BIRMINGHAM (near Super Target) Grandview Medical Center 4600 Hwy 280, Ste 230 Medhelp 280 Bldg, 2nd floor ALABASTER (formerly Shelby Ob-Gyn) 408 1st Street North 205.664.9995 | CWCALABAMA.COM
SAME DAY APPOINTMENTS
Kara Conti, MD | Ashley Duke Gooding, MD | James Head, MD | Jessica Rodriguez, MD Malcolm Simmons, MD | David L. Spangler, MD | George Zaharias, MD
AVAILABLE
Cooper Green hospital.
Marie-Carmelle Elie, MD James Markert, MD Alan Tita, MD, PhD
Living With Diabetes?


















Listen to your heart.

People with diabetes are twice as likely to develop heart disease than those who don’t have this disease. High blood sugar, high blood pressure and high cholesterol levels all raise the risk for heart disease with no obvious symptoms. Don’t take the risk. If you live with diabetes, listen to your heart. Talk to one of our cardiologists to get answers about your heart health.

Call 205-510-5000 to schedule an appointment today. CVAPC.com LEARN MORE NOVEMBER IS AMERICAN DIABETES MONTH
 By Jane ehrhardt
By Jane ehrhardt













































 By Marti WeBB Slay
By Marti WeBB Slay












































 Woodard, DO
Woodard, DO















 By laura FreeMan
By laura FreeMan











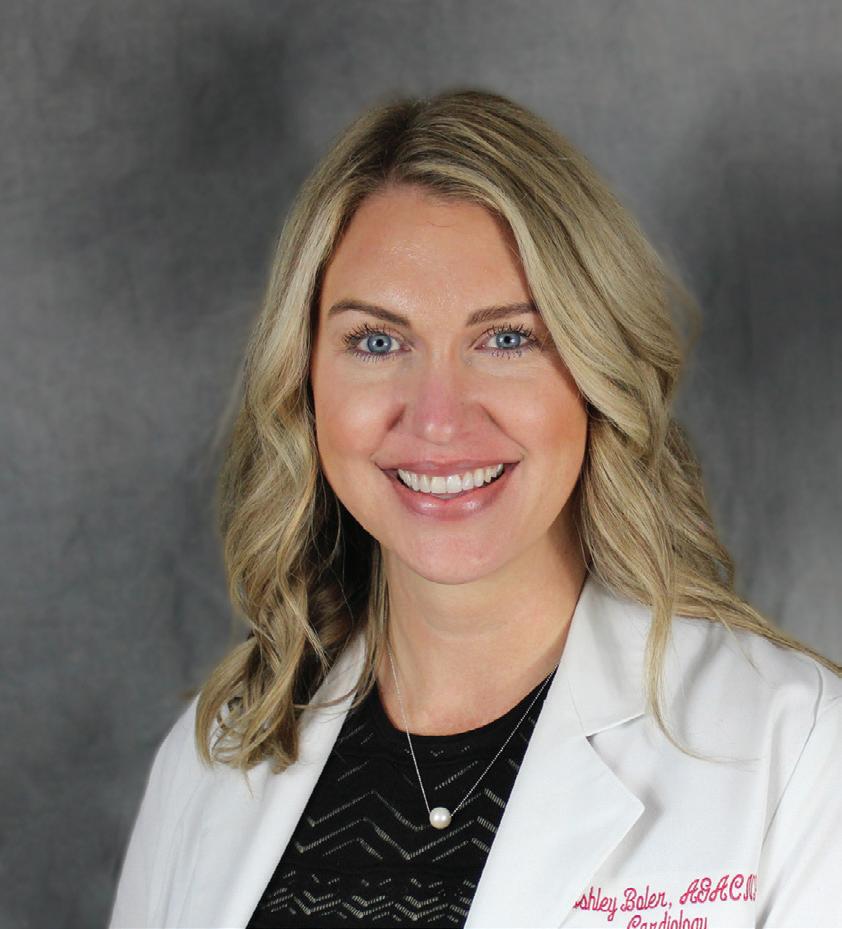





























































 By: anGie CaMeron SMith
By: anGie CaMeron SMith






 By lynne Jeter
By lynne Jeter

























 By CraiG Greer
By CraiG Greer


















 By Stephanie dozier
By Stephanie dozier















































