




If there is a medical situation that compares to feeling like you’re living under the sword of Damocles, finding that you have an aortic aneurysm is one of them.
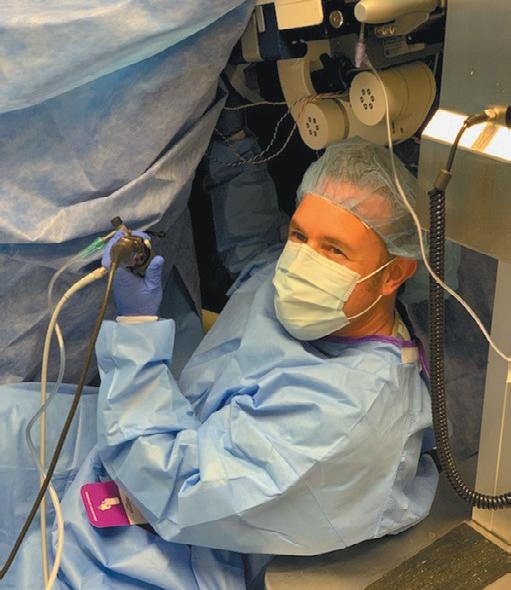
“An aneurysm diagnosis naturally brings with it a sense of urgency. No one wants to live under constant, life threatening danger. However, in managing the condition and hopefully correcting it, there are situations where patience is a priority,” said Adam Beck, MD, Director of UAB’s Division of Vascular Surgery & Endovascular Therapy.
Beck is also a member of the UAB Cardiovascular Institute. In November he was first in
the United States and second in the world to use the new LumiGuide, a second generation 3D device guidance solution powered by Fiber Optic RealShape Technology (FORS).
“The light technology reduces procedure time and the need for fluoroscopy. We are no longer limited to relying on just x-ray or ultrasound for complex visualization of internal arterial anatomies. It allows us to see in real time what’s going on inside what can be very complex and irregular structures. This helps us stay on the cutting edge of endovascular aortic repairs.”
Perhaps the most difficult skill in managing these vascular anomalies effectively is learning how to recognize when it’s better to do some-

 By marti WeBB slay
By marti WeBB slay
Anesthesiologists are now playing a bigger patient assessment role prior to surgery. “It’s becoming imperative that anesthesiologists practice more than just intraoperative anesthesia, but that they move into the preoperative space as well, especially in a tertiary referral center like UAB,” said Chris Godlewski, MD, MSHA, associate professor in the UAB Department of Anesthesiology & Perioperative Medicine. “It can be a challenge to take care of some patients, given the burden of comorbidities and the extent of surgery they may be having.
“The upshot of this is that Anesthesi-
ologists have expanded into the perioperative surgical home concept. We now have a process in which the patient’s medical history is reviewed, and they are often seen by an anesthesia provider prior to the day of surgery. We order lab studies, initiate pathways for things like sleep apnea and postoperative nausea, collect critical information and intervene when necessary to try to ensure the patient isn’t going to get cancelled the day of surgery, and to make sure the anesthesiologist has all the necessary information. This allows the patient to proceed through the peri-operative period as safely as they can.
“To help with this process, my colleague Dr. Jeff Simmons has built a robust
www.birminghammedicalnews.com

Preoperative Assessment, Consultation, and Treatment Clinic. It is constantly updated with the latest perioperative guidelines with the goal being the safest surgical experience possible.”
Prior to surgery, it can be helpful for the anesthesiologist to see many of the studies that historically only specialists would evaluate. “We can tailor our anesthetic plan as a result of those studies,” Godlewski said. “From an anesthesia perspective, we have to consider the entirety of the patient’s medical and surgical history. We may obtain cardiac catheterization reports, echocardiograms, and pulmonary function tests and put it (CONTINUED






























all together in package. This allows us to be much more safe and effective than the traditional letter from a consulting physician stating ‘cleared for surgery.’”
Godlewski said not being evaluated by an anesthesia provider until the day of surgery can sometimes lead to delays and cancellations. “It can be a scramble to collect and review results at the last minute,” he said. “The more information we have, the more smoothly the process goes. And it allows us to take better care of the patient and customize the anesthetic. Technology and pharmacology have evolved, so rather than a one-size-fits-all approach, we can be highly specific with what we give the pa-
tient to safely address their health issues and hone in on the best possible outcomes. In a complicated patient, we have the ability to mitigate substantial risk when we are able to evaluate them prior to the day of surgery.”
There are questions which are specific to a given surgery, but there are also many questions that are important regardless of which surgery a patient is having. “There are certain things that catch our attention no matter what the surgery is,” Godlewski said. “One big factor is cardiac status. Do they have heart failure? Have they had heart attacks or stents? Are they having chest pains, shortness of breath or irregular heart rhythms? If so, have they been
from page 1
seeing somebody and has it been investigated enough that on the day of surgery we aren’t seeking more information?
“There are other concerns as well. Do they smoke? Have they had strokes? Blood clots? Bad heartburn or reflux? How well is their diabetes being controlled? All of these factors can have a substantial impact on the patient’s perioperative course and are considered in the anesthetic plan.”
The answers to these questions can determine not only the course of anesthesia, but also where the patient can or should have the surgery. “A patient with severe cardiovascular disease is often better served having surgery at a larger hospital
because of the increased level of care that may be required,” he said. “Our specialty has become sophisticated in our ability to do this,” he said. “Having folks on the other end giving us this information in a timely fashion is critical. One of our stumbling blocks can be when the patient’s time to surgery is short. Sometimes the clinic on the other end -- who we need information from -- doesn’t get us the information quickly enough. Obtaining those test results are crucial because we can’t do anything with the information if we don’t have it. That can absolutely lead to their surgery being postponed or cancelled. It plays a bigger part than people know.”
continued from page 1 thing and when it’s better to do nothing. Being able to see what’s happening inside the artery should help.
“Most aneurysms have an annual risk of rupture of around five percent,” Beck said. “If repair has a higher risk, your chance for a good outcome may be better if you do nothing to the aneurysm itself, but instead work on keeping hypertension, weight and other co-morbidities under control.
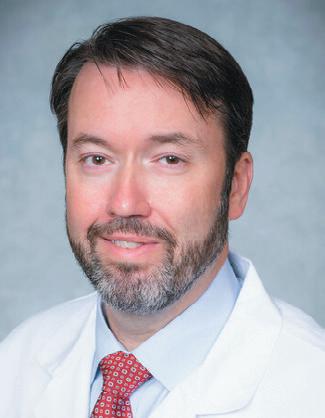 Adam Beck, MD
Adam Beck, MD
“You have to bear in mind that risks
are cumulative and change over time. With aging and additional illnesses, eventually it may be time for surgery.
“In November, what began as a remarkable first-use scenario for the U.S. allowed us to navigate an aortic aneurysm repair using this incredible new tool. It was so successful we’re now using it to do several procedures a week. UAB is rapidly becoming a regional referral center for repairs like these. As we con-


tinue to progress in developing tools and expertise to repair these types of vascular problems, we’re hoping that instead of fear, more people will be able to look forward a long, healthy life.”
The aorta is one of largest and most important great vessels in the body. It is critical to carrying the blood flow that nourishes so many essential body functions. From the heart, the aorta curves upward and branches to supply the brain. It extends downward to bring oxygen and nutrients to the organs of the torso. From there, it divides into the major arteries of the legs and feet, making movement and human activity possible. Unfortunately,
although the body depends on this vascular powerhouse for so many of the key functions in life, it doesn’t always supply the quality of materials and perfection in workmanship to sustain it.
“The areas where we are most likely to find trouble are often in the torso near the kidneys,” Beck said. “It may be a malformation or flaw first noticed in early childhood, or a weakness that looks like a balloon blown up too many times that may show up in aging. We are still seeing far too many aneurysms, but with major advances like this, we are headed in the right direction for dealing with them.”



“The biggest innovation we’ve added is a biologic implant,” says Amit Momaya, MD, chief of sports medicine and surgeon in the UAB Department of Orthopaedic Surgery.
Momaya performed Birmingham’s first bridge-enhanced ACL restoration (BEAR), which is the first surgical treatment that allows the body to repair its own ACL. “ACL repair isn’t novel,” Momaya says. “For years, they tried and failed miserably back in the 80s. The re-tear rates then were upwards of 50 percent, leading to the procedure fading out of use.”
But following several decades of research, including funding from the NIL, the procedure now includes a biologic component made up of various proteins derived from bovine collagen. This essentially allows the ACL stump to heal and reconnect with prior tissue on the wall.
The procedure builds a scaffold of stitching between the ends of the torn tissue with the biologic component secured in the middle. That implant is basically a protein-based sponge injected with the patient’s blood to hold and protect blood flowing in the gap of the
ACL and allows a natural clot to form. The surgery takes between 30 and 45 minutes. After eight weeks, the implant is absorbed as the body generates the collagen and blood vessels to replace it.
One of the major advantages to maintaining the original ACL tissue, versus the more common reconstruction with tendon grafts, is retaining the nerve fibers. “When you’re jumping and landing, those nerve fibers give you appropriate feedback,” Momaya says. “They essentially give your knee balance and tell it where it is in space.”
That native tissue could also lead to less arthritis down the road. Currently, one in three people will suffer from radiographic knee osteoarthritis within ten years of an ACL injury. Up to 80 percent of patients develop arthritis 15 to 20 years after knee surgery. “Animal studies show that keeping the native tissue may reduce arthritis in knees,” Momaya says. “Time will tell in humans over the next 10 years.”
A third obvious benefit to the procedure is not needing a graft, especially when taken from the patient’s own body. “When you do that, you’re robbing Peter to pay Paul,” says Momaya, who has performed around 2,000 knee reconstructions in his
 Amit Momaya, MD
Amit Momaya, MD
career. Removing that tendon tissue from elsewhere in the body creates weakness in that area that was once whole.
The recovery from the procedure takes around nine months, basically the same as a reconstruction. “This is because it still has to go through the maturation of healing the tissue,” Momaya says. “You can’t speed up that process.”
BEAR patients do take longer initially to show improvement. Whereas reconstruction patients may walk out the door after surgery, BEAR patients are allowed only partial weight bearing of about 50 percent for the first two to
four weeks, depending on the meniscus repair. “The flip side is BEAR patients have less pain and get their motion back quicker,” Momaya says.
The decreased pain is because surgeons who use the procedure are able to drill smaller tunnels in the knee. In reconstruction surgery, tunnels run 10mm, but BEAR requires only 3.5mm. “That’s a third of the size, which leads to a dramatic decrease in the pain experience,” Momaya says. The graft is the primary source of additional pain in reconstruction. The third source is the fluid still left in the knee from remnants of the fluid inserted to improve vision during the procedure and the tunnels bleeding for a while.
In studies, the BEAR technique has shown no notable difference from reconstruction surgery in muscle strength, knee joint laxity, or postoperative knee scores. However, it has showed better hamstring strength. BEAR patients also showed faster recovery from symptoms and return to their daily activities.
“My favorite part of this procedure is not having to take a patient’s tissue to revive another part of their body,” Momaya says. “Someday I hope we call that procedure barbaric.”









At the heart of one of the most highly regulated industries in the nation, health care facilities and providers face challenges that draw attention and resources away from their mission to provide quality patient care.
Burr & Forman’s health care team works alongside you to address and anticipate your needs by providing preventative guidance and pragmatic solutions, enabling you to focus on providing care and achieving healthy outcomes.
Birmingham | Mobile | Montgomery
Jessie Bekker
Howard Bogard
Richard Brockman
Kelli Carpenter Fleming
Jim Hoover
Catherine “Cat” Kirkland
Angie Cameron Smith

What if a trusted third party could help your company identify specific vulnerabilities before the hackers do? Cyberattack stories abound, from large corporations like Target and Equifax to various small businesses across Alabama, and the productivity and revenue loss continues to be catastrophic. However, a comprehensive penetration test, ideally performed by an outside cybersecurity expert who is unfamiliar with your network and uninvolved with its design, will often highlight weaknesses in your company’s network and its defenses. During such an exercise, various tools and software are deployed that seek out deficiencies better found by you than a hacker.
Consider a couple pen testing success stories from two well-known companies:
• Penetration testing conducted at the Mayo Clinic identified outdated operating systems on crucial medical equipment and devices. Furthermore, the testing discovered staff with weak and overused passwords. Mayo acted quickly to update its systems and enforce a strict password policy, thereby strengthening its protection significantly.
• Walmart’s testing found unpatched software in use, weaknesses in its Point of Sale system, and poor password hygiene. Walmart immediately patched and updated its POS system to protect customer payments and implemented employee training and password policies.
While the Mayo Clinic and Walmart are large corporations, penetration testing offers benefits to healthcare providers at every size. In fact, for many cybersecurity insurance policies and certain compliance frameworks, annual (or even more frequent) third-party penetration testing is a requirement. Healthcare providers and certain adjacent industries often have certain legal requirements to perform penetration testing at least annually. Discovering open ports, weak user credentials, unpatched applications, and other potentially devastating fissures in your practice’s network allows your team to repair and resolve these problems before the hackers find them. While you may need to dedicate some time and resources to fixing these problems, the cost is minimal when compared to that of an actual breach that takes your entire practice out of operation for weeks or even



months.
Consider the cost of assuming your network is protected. For example:
• Alabama’s own Norwood Clinic announced in late 2021 that a cyberattack had exposed the records of roughly 228,000 patients. A $2.3 million settlement was reached in January. This settlement doesn’t include the cost of cleaning up the actual breach itself or the downtime in productivity for the clinic.
• In 2019, an extensive ransomware attack hit Tuscaloosa’s DCH Medical Center, extending to Northport and Fayette centers as well. A social engineering scheme focused on employees, convincing them to click on attachments via email,
thus releasing malware and shutting their entire network down. Hospital services and functions were partially paused for 10 days until a decryption key was purchased from the attackers at an undisclosed cost. A lawsuit from a group of patients is ongoing.
When your eight-year old tells you he’s done his homework, do you believe him or do you double check that it’s complete? If your mechanic changes your oil, does he assume he’s put the cap back on or is it part of his protocol to inspect that before he’s done? Do you go to bed believing your doors are probably locked for the night or do you make sure they’re secure? Your company’s network must be given the same thorough consideration. Protecting your business’s most valuable assets means that alerts must be managed, patches updated, and security gaps remedied. If not, you are at a significantly higher risk of attack.
Kristin Shoe is the Director of Marketing at SIP Oasis an IT services company based in Birmingham. She can be reached at (205) 623-1223.


Kidney Disease has long suffered a lack of research funding, lagging behind heart disease, cancer, and others. Consequently, until recently, there has been limited progress made in treatments for the disease. This is especially troubling when considering the immense burden that kidney disease places on patients and their families, not to mention the huge financial burden to the healthcare system.
Happily, we can highlight two areas in kidney disease where we can demonstrate recent meaningful progress. The first has to do with advancements in medication management, and the second is related to care delivery.
First, the past few years have been exciting in Nephrology. We have seen a major increase in the discovery of new medications that achieve great results for patients – and as so often happens, they were kind of discovered by accident. For example, one class of medications was designed for the treatment of diabetes, but is not very strong as a diabetes therapy alone – on the other hand, scientists discovered enormous benefit to patients with kidney disease, keeping

them alive and healthy longer. Another class includes some of the recently popular injectable weight loss drugs – it turns out they are very good for patients with kidney disease as well.
This excitement has compelled the American Society of Nephrology, the American Heart Association, and the American Diabetes Association to work together, for the first time ever, to create guidelines for physicians caring for patients with kidney disease and for those at risk. These guidelines lay out a framework for care that, when applied appropriately, will really be a gamechanger in the world of patients with kidney disease.


As stated, the other area we wish to highlight pertains to care delivery. Patients with kidney disease are some of the most complex and sick people around –on average, they are burdened by more health problems, take more medications, have more doctor’s appointments, and are more economically disadvantaged on average than the general population.
Basically, they are some of our neediest.
But since they are also the most expensive, Medicare and private insurers are motivated to improve matters for these patients in ways that will also result in lower costs to the healthcare system. The result is what some call “value-based care.” We prefer to call it “physiciandriven patient-centered care.”
Through our practice’s partnership with Evergreen Nephrology, we are reaching out to offer more help to patients in the form of better healthcare education, disease prevention, care coordination, dietary education, and general support in an effort to prevent kidney disease from worsening, to prevent hospitalizations, to increase planning and uptake of kidney transplants, and when dialysis is necessary, to focus on home therapies that are often better for quality of life.
The easiest way to describe this process is that we try to do everything we can think of to help patients stay alive, healthy, and out of the hospital so that they can live vibrant and fruitful lives.
Thomas Watson, MD is Board-Certified in Nephrology and Internal Medicine by the American Board of Internal Medicine. He practices with Nephrology Associates.





















































































































































The U.S. Department of Health and Human Services (HHS) and the Centers for Medicare & Medicaid Services (CMS) have started a new effort to educate the public about the Emergency Medical Treatment and Labor Act (EMTALA), sometimes referred to as the “anti-dumping” law. Enacted in 1986, EMTALA was intended to prevent “patient dumping,” a colloquial term for the transfer of uninsured patients to other hospitals or healthcare facilities for strictly financial reasons.

medical screening exam (MSE) and maintaining a central log of those individuals seeking treatment. Hospitals may not delay an appropriate medical screening exam or further medical examination and treatment in order to ask about the individual’s insurance status or payment source.
preliminary injunction in place challenging CMS statements that stabilization may include abortion services.

EMTALA applies to all hospitals that receive any Medicare funding. The law gives all patients certain rights, regardless of whether they are Medicare beneficiaries or not. Specifically, these rights under EMTALA include:
• Screening: If someone comes to a hospital emergency department asking for care, the hospital must determine whether an emergency exists by providing an appropriate
• Stabilization: For a patient with an emergency medical condition, the hospital must provide treatment as needed to stabilize the patient. If the hospital does not have the capacity to treat the patient and a transfer is appropriate, medically indicated and documented, the hospital must provide the care necessary to ensure, within a reasonable medical probability, that no material deterioration is likely to result from or occur during a transfer. Stabilization includes delivery of the baby and placenta for pregnant patients. There is litigation pending and a
• Necessary transfers: Patients with unstable emergency medical conditions cannot be transferred unless a physician or “qualified medical person” at the hospital decides that the risk of transfer is outweighed by the benefits of treatment at a hospital offering higher levels of care. Hospitals with specialized capabilities and sufficient capacity must accept transfers from hospitals that lack the capability to treat an emergency medical condition.
EMTALA violations can result in civil monetary penalties, civil enforcement, a hospital’s termination from Medicare or a physician’s exclusion from Medicare and Medicaid.
In addition to providing new educational resources to the public, HHS
and CMS plan to provide hospitals and provider associations with EMTALA training materials and discuss best practices with these stakeholders. HHS also plans to establish a team of experts to support hospitals in complying with their EMTALA obligations.
CMS has a new webpage that provides individuals with an explanation of their rights under EMTALA. The site provides instructions regarding how to file a complaint for noncompliance and includes a link to state survey agencies that can receive complaints. In the event this new education initiative leads to more patient complaints regarding potential EMTALA violations, hospitals can lower risks of noncompliance by reviewing their EMTALA compliance programs to ensure that they conform to applicable laws and rules.
Shannon Britton Hartsfield is a partner in Holland & Knight’s Tallahassee, Florida, office.

In the little moments and major milestones of childhood, we are here for our patients and their families – helping, healing, teaching and discovering.


About eight years ago, Luis F. Pineda, MD, published a book of recipes. “Cooking with Cancer was born with the idea of trying to improve the quality of life of cancer patients by providing food they would have some enjoyment in,” says the oncologist, who in addition to board certifications and training in hematology/ oncology, internal medicine, psychiatry, neurology, and pain management, is also a chef.
“The book was about creating recipes that specifically addressed the nature of their suffering,” Pineda says about the over 50 recipes that are freely available for download on the nonprofit Cooking With Cancer website (cookingwithcancer.org). The recipes reflect the findings in studies on the damage caused by chemotherapy to aspects such as taste, flavor, absorption processes, and bowel function.
Olive Chowder, for instance, has an enticing sour and bitter pungency to incite the subdued tasting abilities along with a significant cathartic effect on the gastrointestinal tract. Chayote and Mozzarella Cake uses a green vegetable from Latin America called guisquil that holds
a high content of water to aid with rehydration.
Most dishes are gelatinous, liquid or smooth to ease swallowing. Among the seven completely unique ice-cream dishes is Feta Cheese Ice Cream with Roasted Pepper. The fat and proteins in the cheese offer calories to those fighting weight loss and also serve as building blocks for the intestinal flora destroyed during chemotherapy.
One recipe even supplants the need for expensive treatment for nausea and vomiting, symptoms that are controlled in the brain by the neurotransmitter substance P. A common pre-chemo injection given to block that neurotransmitter costs around $400. “Capsaicin, which is the active component of jalapeno peppers, does basically the same thing,” Pineda says. “So I created Jalapeno Pepper Soup, and prior to chemo, patients eat a bowl. Basically we are pre-medicating with something you cook at home and costs pennies, rather than with an expensive injectable compound. So you see how we use scientific knowledge of taste and flavor together with the chemical compounds in the food, like capsaicin, to control common symptoms of cancer patients.”



Colon cancer is often treated with 5-flourouracil, a chemotherapy drug that dampens the receptors of smell and taste, mostly on the tongue and front part of the mouth. The receptors in the back of the mouth are less affected. “We made a recipe using a special pepper, called a Cobanero or Mayan Lover, that has the capacity to enhance the electrical activity
of those receptors,” Pineda says. For a mild option, the Anaheim Pepper Jell-O with Tamarind Granita has a sweet and bitter taste that excites the overall mouth, preferentially the middle and the back. It bypasses the front of the mouth and the lips, where patients may

The Department of Justice recently published a notice of proposed rulemaking applicable to healthcare entities covered under Title II of the Americans with Disabilities Act that relates to accessibility to medical diagnostic equipment for disabled individuals. This article discusses those proposed revisions and next steps for covered entities.
Background:
Title II of the Americans with Disabilities Act (“ADA”) mandates that state and local government services, programs and activities be accessible to individuals with disabilities. This includes, but is not limited to, state and local government entities that offer healthcare support, such as public hospitals and entities that received federal funding from The U.S. Department of Health and Human Services (“HHS”). Under Title II, impacted entities must provide reasonable modifications for disabled individuals when necessary to avoid discrimination on the basis of disability unless those modifications would fundamentally alter the nature of the public entity’s service, program, or activity. Failure to comply with Title II can result in significant fines ($75,000 for a single violation), individual legal action, and even loss of federal funding. Further, noncompliance can lead to audits, department oversight and reporting requirements.
Proposed New Rule:
On January 12, 2024, the Department of Justice (“Department”) proposed revisions to the regulations implementing Title II relating to technical standards


and scoping requirements for services and programs related to Medical Diagnostic Equipment (“MDE”). MDE is equipment used in, or in conjunction with, medical settings by healthcare providers for diagnostic purposes. It includes, but is not limited to, examination tables, examination chairs (including chairs used for eye examinations or procedures, and dental examinations or procedures), weight scales, mammography equipment, x-ray machines, and other radiological equipment commonly used for diagnostic purposes by health professionals. The standards cover independent entry, use of, and exit from MDE by disabled individuals.
The Department explained in a press release that the proposed regulations help address shortcomings in healthcare entities providing accessible equipment, diagnostic and medical care to individuals with disabilities. The proposed regulations provide the example of patients with disabilities having to forgo Pap smears because they could not safely transfer from their wheelchairs to a fixed-height exam table, and inaccessible mammography machines contributing to low breast cancer screening rates for patients with disabilities. The Department estimates that this title II
ADA proposed regulation would affect 6,905 public entities.
Key Proposed Changes:
The proposed rule contains a number of important changes for covered entities:
• Adoption of the standards for accessible MDE issued by the Architectural and Transportation Barriers Compliance Board.
• Proposed rule requires at least 20 percent (but no fewer than one unit) of each type of equipment in use in facilities that specialize in treating conditions that affect mobility to meet the MDE standards, and requiring at least 10 percent (but no fewer than one unit) of each type of equipment in use in other facilities to meet the MDE standards.
• Proposed rule does not require entities to make all existing MDE accessible, but requires that programs when viewed in their entirety, be readily accessible to and usable by individuals with disabilities, taken into consideration if retrofitting would create an unduly financial and administrative burden or constitute a fundamental alteration to the MDE. A fundamental alteration means the change would alter diagnosticallyrequired structural or operational characteristics of the equipment and prevent the use of the equipment for its intended diagnostic purpose.
• An entity may comply with MDE standards requirements through such means as reassignment of services to alternate accessible locations; home visits; delivery of services at alternate accessible sites; or any other methods that result in making its services, programs, or activities readily accessible to and usable by individuals with disabilities. In choosing among available methods for meeting the requirements,
a public entity shall give priority to those methods that offer services, programs, and activities to qualified individuals with disabilities in the most integrated setting appropriate.
• The proposed regulation requires that covered entities ensure staff is able to successfully operate accessible MDE, assist with transfers and positioning of individuals with disabilities, and carry out the program access obligation with respect to existing MDE.
• Covered entities should also ensure staff understand the entities’ obligations with regard to MDE and are properly trained to communicate and coordinate with disabled individuals with regard to MDE.
Conclusion
Comments on the proposed regulations closed February 12, 2024, and no final rule has been published to date. All entities that will be impacted by this change should start preparing for its impact. Compliance obligations can be burdensome, and noncompliance can lead to substantial penalties.
Matt Scully is a Partner at Burr & Forman LLP practicing in the firm’s Labor and Employment Group. Matt may be reached at (205) 458-5321 or mscully@burr.com




With more than 20 locations in Central Alabama, UAB Callahan Eye makes nationally recognized, vision-saving care even more accessible. Our state-of-the-art eye exams go well beyond checking prescriptions to include eye health evaluations, eye pressure measurements, and analysis for other serious medical conditions. As trusted vision experts, there’s nothing in our way of improving people's sight.
See the di erence at uabcallahaneye.org.
With more than 20 locations in Central Alabama, UAB Callahan Eye makes nationally recognized, vision-saving care even more accessible. Our state-of-the-art eye exams go well beyond checking prescriptions to include eye health evaluations, eye pressure measurements, and analysis for other serious medical conditions. As trusted vision experts, there’s nothing in our way of improving people's sight.
See the di erence at uabcallahaneye.org.


Cooking for Cancer Evolves, continued from page 10

suffer from painful and sometimes disabling sores from a Herpes Simplex infection.
Monosodium glutamate (MSG) is also included in some recipes to intensify taste. “MSG has a bad reputation,” Pineda says. “But it’s coming back, because they have realized that headaches and migraines are not related to the MSG.”
As new discoveries have unfolded over the past decade since the book came out, new recipes continuously appear on the website to reflect that progress. Carbohydrates used to be sought after to help cancer patients regain weight. Studies now show consumption of carbohydrates relates to inflammation, the chronic nature of obesity, and insulin metabolism that now is believed to cause cancer. Basically, Pineda says, cancer loves glucose, as any PET scan using a glucose tracer proves.
Even nutritionists would offer milkshakes to chemo patients in hopes of getting them to eat and regain weight. “By comparison, an article published today shows that people who lose weight during cancer treatment basically live longer and have a better response to the treatments,” Pineda says. “Other studies mirror the benefits of low carb diets, including the popular keto diet. We have studies ongoing at UAB of glioblastoma, prostate and pancreatic cancers showing patients doing

better when they eat less.”
Another new approach to aiding treatment and even prevention of cancer lies with using bacteria and prebiotics to bolster the body’s systems. “Bacteria programs your immune system,” Pineda says. Fiber from vegetables, for instance, feeds the bacteria in the intestine that activate the immune system.
The new recipes incorporate these discoveries by integrating prebiotics, postbiotics, probiotics. “The Creme Brulee With Ginger and Basil puts probiotics into it, kind of like Activia yogurt has probiotics inside it,” Pineda says. The asparagus recipe acts as a prebiotic. Prepared in a way to destroy the cellulose but still remain crunchy, the fiber in the asparagus is very rich, which fortifies the bacteria flora of the intestine. Look for the new edition of Cooking with Cancer to arrive on the site in the next six months.


The slightest errors, delays, and oversights lead most surgeons to miss out on revenue. Surgical Pathways has proven to capture tens of thousands of overlooked dollars per surgeon lost in the complicated prep and process of tracking and billing procedures.
It adds up.
Created and constantly adapted with the input of the surgeons themselves, Surgical Pathways tracks every needed step to prepare, perform, and bill for each surgical procedure. Know in a glance when and who is responsible along the way for anything from pre-certs, medications, and clearance to claims. All automated.
A customizable software that works with your existing EHR/PM system.






On February 15, more than 200 associates, providers, elected officials, first responders, and guests attended a ribbon cutting and open house for the Ascension St. Vincent’s East Freestanding Emergency Department in Trussville. The facility opened it’s doors to patients the next day.
The 12,500-square-foot facility, open 24/7, is located off I-59 at 6670 Green Drive in Trussville. It has 12 treatment rooms, a decontamination treatment area, onsite lab and imaging, including
x-ray and CT, and a helipad for air ambulance transfers.
“Trussville is growing at a rapid rate and we want to put emergency care close to where residents live and work,” says Jason Alexander, CEO, Ascension St. Vincent’s. “We have nine acres, which will allow us to expand in the future.”
Ascension St. Vincent’s is also building a Freestanding Emergency Department in Pelham, which is tentatively set to open by the summer of 2025.
Vulcan Imaging Associates (VIA), a leading radiology practice in Alabama, has acquired Women’s Imaging Associates, an independent tele-mammography practice established by Caroline Reich, MD that offers breast imaging expertise in women’s health services.

VIA is a full-service practice that has a reputation for subspecialty proficiency among referring physicians. This addition unifies two market leading practices to build an unrivaled team of board-certified, fellowship-trained breast radiologists to provide outstanding quality
Eric Blackmancare to both the local communities they serve as well as across the country through partnerships with hospitals, healthcare facilities and other radiology groups.
“We are thrilled to have this opportunity to expand our Women’s Division, continue our growth with Dr. Reich and provide the highest level of quality in breast imaging. This acquisition strengthens our desire to provide the best service possible to the physicians and patients we serve,” said Eric Blackman, CEO of Vulcan Imaging Associates.
SYSTEMEDX, a Birminghamarea provider of medical practice software and medical practice revenue collection services, has hired Mark Lewis as the Chief Sales Officer.
“Mark will be a superb addition to Systemedx. His 27 years of serving medical practices with Practice Management (PM), Electronic Health Records (EHR), and Revenue Cycle Management (RCM) is a testament to his dedication”, said Lisa Warren, CEO of Andrews Sports Medicine.
 Mark Lewis
Mark Lewis
Lewis graduated from Hampden–Syd-
ney College in Virginia with a Bachelor’s degree in Managerial Economics and pursued graduate work in Finance at UAB. His Healthcare professional experience spans almost three and a half decades. He began in finance at Brookwood-Baptist Hospital, moved to United Healthcare Insurance, and then led Sales at MediSYS before joining Systemedx.
Kevin Bonner, the Chief Solution Architect for Systemex, said, “Systemedx has gained a tremendous asset with the hiring of Mark.”


New changes to eligibility criteria will help provide access for more Jefferson County residents who need services at Cooper Green Mercy Health Services Authority.
Approved by the Jefferson County Commission, Cooper Green will evaluate income based on the individual person seeking to enroll, rather than the income of the household in which the person resides. Formerly, Cooper Green followed the federal definition of household income, which compares the sum of all working adults in the household’s in-
come to the Federal Poverty Guidelines. With the change, a person meets the criteria to be enrolled in low- or no-cost plans at Cooper Green, if they make $29,160 a year or less.
This eligibility change coincides with the building of a new Cooper Green facility set to open in early 2025. These requirement changes and the new facility will enable providers to care for more patients than the 6,300 county residents that Cooper Green serves today.
• Patients are scheduled within 24 hours and seen in clinic within 2-4 weeks of referral.
• We keep you informed about the patient’s treatment plan and make sure the loop is closed on your referral.
In 2022, Baptist Health Foundation, in partnership with Baptist Health System, launched their Community Support Fund to provide charitable grants to established 501(c)3 non-profits who are providing healthcare or health related services, and operate within Jefferson, Shelby, Talladega, and Walker counties.
In November of 2023, the Community Support Fund awarded over $350,000 to 38 organizations. One recipient, Birmingham Metro Baptist Association’s
ReMedy program, collects and refurbishes durable medical equipment like wheelchairs and walkers to loan to individuals in need of them. Another grantee was the United Ability JETS program, which provides work-based learning opportunities to students with disabilities.
In 2024, Baptist Health Foundation wants to support more non-profits by addressing access to healthcare, food insecurity, behavioral health, and supporting individuals who find themselves in crisis.
CORRECTION In the February Birmingham Medical News, an article stated that Grandview Medical Center was the first hospital in Birmingham to use Intuitive’s Ion endoluminal system. Actually, UAB has been using the system since August 2021.

VICE
Jason Irvin
CREATIVE DIRECTOR
Katy Barrett-Alley
CONTRIBUTING WRITERS
Jane Ehrhardt, Ashley Franco, Laura Freeman, Lynne Jeter, Marti Slay
270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110
AD SALES:
Jason Irvin, 205.249.7244
All editorial submissions should be e-mailed to: editor@birminghammedicalnews.com Scan

Every student at the UAB Marnix E. Heersink School of Medicine now has access to a portable point-of-care ultrasound unit (POCUS), thanks to $2 million federal grant awarded to the Department of Family and Community Medicine. UAB is one of the first medical schools in the United States to give each of its students access to these devices.
Unlike the dedicated machine on wheels used in labor and delivery units, a POCUS unit fits in a clinician’s pocket and connects to a tablet or smartphone to visualize the results.
“Clinicians can use handheld ultrasound to evaluate almost every major organ system and better visualize suspect-
ed pathology,” said Steven Brown, MD, Assistant Professor in the Department of Family and Community Medicine. “Some even call it the stethoscope of the future.”
“POCUS could be particularly helpful for patients in rural and urban underserved areas, who face significant wait times for appointments or must travel long distances for care,” said Irfan Asif, MD, Chair of the Department of Family and Community Medicine.
In addition to the 600 devices for medical students, the POCUS Initiative includes 100 units for the community preceptors who teach UAB medical students in their clinics. The preceptors will use the units to identify soft-tissue in-
fections, fluid accumulation in the joints and abdomen, gallbladder disease, kidney stones, heart failure, dehydration, and more. The department will educate and train residents and faculty, as well as medical students.
A provider can use handheld ultrasounds to determine whether a softtissue lesion is an abscess or a cyst or a lipoma or a mass; to determine whether a patient has a torn tendon, examine the gallbladder for stones or look at the heart to determine how well it is functioning — all of which could be done without having to send patients out for additional tests and referrals.

After 25 years, we’ve proven the value of the personal touch. No robots, no automation, just a real person reaching
us make a difference in

