 by laura Freeman
by laura Freeman
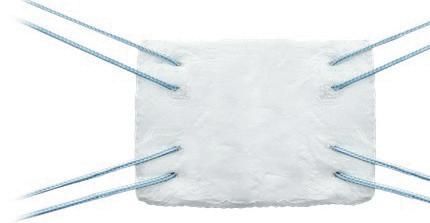
In June of last year, UAB became the first orthopedic surgery program in Alabama to use BioBrace implants to support weakened soft tissue in procedures like ACL and Rotator Cuff repairs, where it can be difficult to achieve and
maintain successful outcomes. Each procedure that was done with BioBrace was tracked in detail as the patients’ healing progressed, and now the results are in and have been published.
“I’ve done more than 50 rotator cuffs in that time and quite a few other soft tissue repairs working with BioBrace, and
the results have been impressive,” Chief of Sports Medicine Amit Momaya, MD said. A surgeon in the UAB Department of Orthopedic Surgery, Momaya is also team physician for UAB Athletics, the Birmingham Bulls hockey team, and Hoover Vestavia Soccer.
In the past, soft tissue support was
Interventional cardiologist Mark Sasse, MD wants to increase awareness about current treatments for deep vein thrombosis (DVT) and prevention of post thrombotic syndrome. “When I was a cardiology fellow, we didn’t have the equipment, the knowledge or the desire to treat DVTs more aggressively,” he said. “DVTs can be neglected, because they are typically treated with only anticoagulant therapy. Physicians
would prescribe anticoagulants, and we thought we did our job. Unfortunately, a signifi cant minority of patients, approximately 20 to 50 percent, develop post-thrombotic syndrome, a chronic disease that occurs after a large unresolved thrombus, even with optimal anticoagulant therapy.
“The symptoms of post thrombotic syndrome can include leg swelling, leg pain, color changes below the knee, venous ulcers and ultimately, disability. The sequelae of post throm-
botic syndrome are difficult to treat.”
Thrombolytic therapy, one of the modalities to treat large DVT, can increase the risk of bleeding. It may not resolve the thrombus completely since some of the thrombus is chronic. There are also options to use balloon angioplasty to disrupt the chronic thrombus. However, this does not usually result in a durable longterm outcome. Aspiration devices have been available for several years but are limited in their ability to extract chronic thrombus.
either synthetic or biologic. BioBrace is both. Its purpose is to help prevent reinjury and to speed healing.
“One of the key differences between BioBrace and other options is that it isn’t just contributing the strength of external materials. It also works with the biology,
(CONTINUED ON PAGE 6)









At the heart of one of the most highly regulated industries in the nation, health care facilities and providers face challenges that draw attention and resources away from their mission to provide quality patient care.
Burr & Forman’s health care team works alongside you to address and anticipate your needs by providing preventative guidance and pragmatic solutions, enabling you to focus on providing care and achieving healthy outcomes.
Birmingham | Mobile | Montgomery
Jessie Bekker
Howard Bogard
Richard Brockman
Kelli Carpenter Fleming
Jim Hoover
Catherine “Cat” Kirkland
Angie Cameron Smith

Compression stockings are another common treatment for DVT. “They improve symptoms, but numerous trials show they don’t change the longterm outcomes for post-thrombotic syndrome,” Sasse said. “They don’t change the pathophysiology because the thrombus is still present.”
The Inari company has now developed the ClotTriever catheter that removes the clot and restores blood flow in the affected vein. “This device has a soft blade at the end of a windsock-like basket, which catches the clot, preventing it from embolizing. We can pull the clot from the vein, out of the body and restore complete blood flow,” Sasse said. “Grandview Medical Center was a participant in the original CLOUT trial proving that patients have reduced risk of developing post-thrombotic syndrome with intervention.
“The procedure can be performed as an inpatient or as an outpatient. We can access the patient from multiple points. From the internal jugular vein access, clots in the inferior vena cava, which resides in the abdominal cavity, can be extracted. In other cases, we place patients in the prone position in the catheterization laboratory and then access the popliteal vein. We put a sheath in the vein
and place wire through the DVT. Then we upsize the small sheath to a much larger sheath so the ClotTriever can be delivered to the affected vein and extract the thrombus.
“It takes a high level of expertise to do the procedure in order to keep the bleeding risk low. Since the venous system is low pressure, we can obtain hemostasis relatively easily and mobilize the patient quickly. Typically, we use the ClotTriever first to extract the thrombus. We can make multiple passes, and if we are happy with the result, we conclude the procedure. If there is residual thrombus, we can use adjunct devices such as balloon angioplasty and aspiration catheters to help extract the rest of the thrombus.”
“If the procedure is outpatient, the patient recovers for three to four hours, and then they are sent home, if there is no bleeding. They resume their anticoagulants immediately. Patients usually achieve resolution of the thrombus in three to six months, but it can take up to year. Residual thrombus after anticoagulation is a risk for reoccurrence of DVT.”
Symptoms of a DVT can be as simple as heaviness or tiredness or just an odd feeling in the legs. Other symptoms are itching or cramps, varicose veins, and redness. “If you are not a pigmented
person, you can see legs turn a copper color below the knee. In darker skinned patients, the skin will get darker and more indurated,” Sasse said. “If a physician suspects DVT, a venous ultrasound is the most expeditious diagnostic test. It’s easy, safe, and widely available.”
Sasse encourages physicians to consider the possibility of a DVT earlier so intervention can be performed before the onset of post thrombotic syndrome. “Cardiology fellowship trained us to be heart and artery doctors,” he said. “We ignored the venous system. When cardiologists observe swelling, edema or leg pain, we think it is a cardiac condition or related to peripheral arterial disease. Patients and physicians can diminish the symptoms of venous disease because it doesn’t appear to be an urgent problem."
Sasse cautions against clinical inertia, or the idea that physicians treat DVTs the way they always have. “Even if we can’t extract all the thrombus, enhanced flow in the vein leads to better patient outcomes,” he said.
Ultimately, extracting a blood clot can result in improved quality of life. “Many patients are miserable from post thrombotic syndrome,” Sasse said. “Given our expertise, we can make people asymptomatic after this intervention.”






















In December, Medtronic landed the first FDA approval for a catheter system that delivers a new form of ablation treatment for atrial fibrillation (AFib). “It allows for the energy delivery to be faster which can help reduce complications, and there are signals that it is more effective,” says Macy Smith, MD, cardiac electrophysiologist with Alabama Cardiovascular Group at Grandview Medical Center, which has been part of the clinical trials on the new approach since its early stages.
To date, the most common type of ablative procedure for AFib is a form of thermal ablation where Radiofrequency (RFA) energy produces heat to form scar tissue on the areas of atrial heart tissue that are out of sync with the heart’s rhythm. The new approach, called pulsed field ablation (PFA) offer a non-thermal (not caused by changes in heat) approach. PFA uses microsecond pulses of high-voltage electrical fields to create small holes in the cells and selectivity deactivates them.


Most of the three to six million AFib patients in the U.S. treat their condition with oral medications, but approximately four percent require interventional techniques, including catheter ablation and surgical ablation. “Ablation has become a cornerstone for the treatment of AFib because the medicines don’t work that well long-term,” Smith says. With the aging U.S. population, the number of AFib patients is projected to reach 16 million by 2050.
With at least four PFA catheter systems having now passed through pivotal

trials in the U.S., more PFA devices will likely be hitting the market soon. Boston Scientific already received the FDA nod for their system in January, and Johnson &
Johnson is expected to not be far behind.
In Europe, PFA has been approved for several years. “They’ve done tens of thousands of cases, and it appears to be safer and at least as effective, potentially more effective, than traditional catheter ablation” Smith says. “We’ll know more in the coming years once we do more cases.
“With the PFA system the risk to surrounding tissues is lower than with traditional catheter ablation. When you use thermal energy, there’s a small, but real risk of collateral damage to nearby tissues.”
One of the primary but minimal risks with ablation is damaging the esophagus, which sits right behind the left atrium, a primary spot for AFib problem tissue. “However, with PFA you can ablate in close proximity with other structures with a very low chance of any damage there,” Smith says. European PFA outcomes have reported zero esophageal injuries.
“The energy delivery is fast and easily reproducible so you can shorten steps, making it faster. And usually faster is safer,” Smith says. “A conventional
(CONTINUED ON PAGE 6)
When physicians, scientists and researchers with extraordinary talent and passion are given the technology, the facilities, and the support, they achieve great things. The discoveries, innovations and clinical trials happening today will help shape the future of treatments and lead to cures.










April 19 9 am – 3 pm




















We’ve been dedicated to helping our customers manage the rising costs associated with risk from the beginning, and we do it in one of the most challenging insurance markets: healthcare. As a result, we know we have what it takes to rethink risk—the way it’s managed, financed, and leveraged—in a way that can help any organization achieve its goals.
blood and the body’s own healing factors. It reabsorbs, so eventually it becomes tissue and doesn’t have to be removed,” Momaya said.
Offered by the Conmed Corporation, the biocomposite design of the BioBrace reinforced bioinductive implant is made with two distinct materials. The first is a highly porous type I collagen sponge matrix with pores sizes to rapidly engage with the body’s healing systems. It is reinforced with microfilaments made of resorbable poly (L-lactide) (PILLA)
Although it is bioinductive, it is also durable enough to allow suturing and cannula passing. It is designed to be placed between the repaired tendon and bone, providing a scaffold for new tissue growth. It promotes cellular infiltration







continued from page 1
and the development of new blood vessels. The implant is FDA indicated to reinforce soft tissue where weakness exists and is available in two sizes.
“We’re also finding it helpful in quite a few other applications that involve soft tissue, such as Tommy John surgery, Achilles and ankle repairs, some types of knee injuries and other types of shoulder and joint conditions that can benefit from soft tissue augmentation,” Momaya said.
By augmenting weak tissue and giving it a protective shield to help it withstand unexpected jolts and movements that could reinjure the repair, the hope is that the implant will give the tissue an opportunity to become stronger and speed healing time.
In some surgeries, the implant also
seems to reduce pain and improve the odds for a better overall outcome and return to function. “These types of injuries can be quite painful and have a negative effect on patient’s lives, especially when surgeries don’t achieve a good outcome or when reinjury sends them back to the same difficult position where they have to start over,” Momaya said. “What we’ve seen in our experience with BioBrace so far is that it really does seem to be helping with outcomes, prevent reinjuries and get better results the first time.
“As research and new applications develop over time, I’m looking forward to seeing how this new tool and other new tools we are working on now will be able to help our patients.”














continued from page 4









catheter procedure takes me around 90 minutes, whereas a PFA takes less than an hour, and that’s with a learning curve on board. Once you get beyond that, it’s a significant change.”
The shortened time between the two ablation processes derives from the faster delivery of energy over a potentially wider area with PFA which means less ablation lesions have to be performed.
The size of the ablation area generated by the PFA depends on the platform used. There are variable basket and flower shapes generating the fields which allow the device to adapt to individual patient anatomies. “With the wider fields, they can potentially ablate around an entire pulmonary vein with one application,” Smith says. “That’s not possible with the thermal catheter, which limits the surgeon to touching the tissue in small spots.
“PFA has fewer steps and is easier to perform so there is less of a learning curve, making training for the new technique less of a time commitment for surgeons.”
The shorter PFA procedure time means less time under anesthesia, which can lessen the drug’s post-operative effects. PFA patients are also spared the common chest pains caused by the irritated tissue from the thermal procedure.
With multiple devices having attained FDA approval, PFA systems are now breaking onto the market. Grandview expects to begin performing pulsed field ablations this month. “Over time, I think PFA will phase out catheter ablation,” Smith says. “Real world data will tell us in the coming years. But I expect it to completely change the landscape of ablation for atrial fibrillation.”




Earlier this year, the U.S. Department of Health and Human Services (HHS) Office of Civil Rights (OCR) published its 2024 Final Rule governing healthcare conscience protections, “Safeguarding the Rights of Conscience as Protected by Federal Statutes.” The Final Rule dictates the protections and enforcement procedures surrounding the rights of healthcare providers and entities to be free from discrimination associated with their decisions to participate or refrain from participating in procedures based on their conscience. The 2024 Final Rule took effect March 11, 2024.
The conscience protections are statutorily authorized under the “Church Amendments” and the “Coats-Snowe Amendment,” which provide different, but related, protections. The Church Amendments prohibit public officials and authorities from imposing certain requirements that run contrary to a person’s or entity’s religious beliefs or moral convictions pertaining to abortion, sterilization and other healthcare services involving certain federal funds. The Coats-Snowe Amendment provides conscience protections for healthcare entities related to
abortion provision or training, referrals for such abortion or training, and accreditation standards related to abortion. These protections are also implicated under Medicare and Medicaid statutes, the Weldon Amendment and provisions included in the Affordable Care Act (collectively, the “federal healthcare conscience protection statutes”).
HHS first authorized rulemaking associated with the conscience protections in 2008; however, it quickly determined that the regulations were overbroad, and new regulatory requirements were published in 2011. The 2011 Final Rule eliminated some of the specific definitions and processes articulated in the 2008 Final Rule, but retained provisions designating OCR as the recipient for complaints of violations of the conscience protections. In 2018, HHS once again issued a Proposed Rule aiming to reinstate some of the 2008 Final Rule’s provisions. That updated Final Rule, adopted in 2019, included specific definitions for relevant terms, imposed procedural requirements and detailed enforcement procedures. The 2019 Final Rule has been the subject of multiple challenges, and multiple district courts have declared it impermissible. As such, HHS has been operating under the 2011 Final Rule since its publishing.
(CONTINUED ON PAGE 15)








The Section of Cardiac Critical Care Medicine within the Division of Pediatric Cardiology at the University of Alabama at Birmingham has an immediate opening for recruitment of a BE/BC cardiac intensive care faculty member to join our current team of 7 faculty members in the CVICU. Entry or mid-level candidates are encouraged to apply.
The ideal candidate will provide care for children in our 20 bed state-of-the-art pediatric CVICU located within The Benjamin Russell Hospital for Children at Children’s of Alabama. They will work in close collaboration with our multidisciplinary team of cardiovascular surgeons, anesthesiologists, perfusionists, cardiologists and nurses. Individuals’ board eligible in critical care/cardiology/NICU/anesthesia with additional 1-2 years of training or experience in cardiac critical care will be considered. A history of excellent communication and evidence of exceptional clinical and teaching skills are a must. Preference will be given to individuals with a strong interest/experience in scholarly activities and clinical/ translational research. Start-up resources for faculty development, research and teaching are available where appropriate.
The Pediatric and Congenital Heart Center of Alabama performs over 400 surgical cases/ year and has active programs in heart failure, transplant, and mechanical circulatory support. There are over 500 children/year with acquired and congenital, medical and surgical heart disease admitted to our CVICU. This includes all preoperative neonates with surgical cardiac disease and high risk patients from our busy interventional and electrophysiology programs.
Birmingham is the largest city in Alabama, with a metropolitan population over 1 million. The city is thriving with a growing restaurant and arts scene, charming neighborhoods, and many outdoor park and entertainment spaces. Birmingham is well located in the Southeast with easy access to lakes, mountains, and gulf beaches. Diversity is a defining feature of Birmingham’s past, present, and future. At UAB, we are committed to capitalizing on what makes Birmingham and the University trailblazers in moving inclusion forward. We are invigorating conversations, fostering civic engagement, widening perspectives, stimulating innovation and connecting people.
In alignment with UAB School of Medicine’s mission to reflect the diversity of our community and meet the needs of our diverse population, candidates are required as part of the application process to provide a statement that is up to one page single-spaced describing their contributions to promote diversity and inclusion.
For more information regarding UAB Department of Pediatrics and/or Section of Cardiac Critical Care Medicine, visit www.uab.edu/pediatrics.
Successful candidates must be a licensed MD, DO, or MD/PhD. Rank, salary and tenure status are commensurate with training and experience. UAB is an Affirmative Action/ Equal Opportunity Employer. All inquiries will be kept confidential.
Interested applicants should create a candidate profile at the following link: https://uab.peopleadmin.com/postings/20824
UAB is an Equal Opportunity/Affirmative Action Employer committed to fostering a diverse, equitable and family-friendly environment in which all faculty and staff can excel and achieve work/life balance irrespective of irrespective of, race, national origin, age, genetic or family medical history, gender, faith, gender identity and expression as well as sexual orientation. UAB also encourages applications from individuals with disabilities and veterans. A pre-employment background investigation is performed on candidates selected for employment. In addition, physicians and other clinical faculty candidates who will be employed by the University of Alabama Health Services Foundation (UAHSF) or other UAB Medicine entities must successfully complete a pre-employment drug and nicotine screen to be hired.
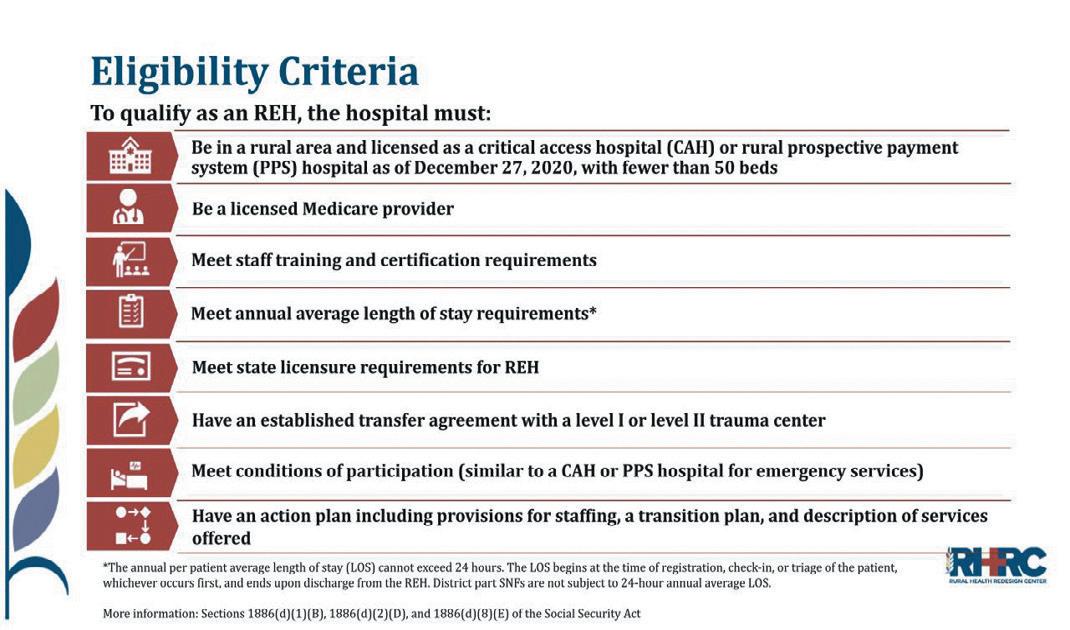
When Rural Emergency Hospital (REH) designation took effect on January 1, 2023, Bob Bernstein, principal at Medovation Health, and the hospital leadership of Bullock County Hospital in Union Springs, Alabama, began investigating the process to achieve that
designation.
Medovation Health had assumed contract management of financiallydistressed Bullock County Hospital in 2022, and moving to become an REH seemed to make sense. “REH has the potential to be a savior for rural healthcare,” Bernstein said. “When care is
(CONTINUED ON PAGE 11)


At a Mississippi hospital, a patient diagnosed with advanced kidney cancer needed a prescription, but the $26,950 price tag for a 30-day supply of pills placed the life-saving drug out of reach. However, because the hospital qualified for the federal 340B program, they were able to cover the patient’s cost.
Enacted as part of the Public Health Service Act of 1992, the 340B program was designed to assist specific healthcare entities in reaching more patients, expanding access to affordable medications, and providing essential healthcare services to a broader patient population, regardless of their insurance status or ability to pay.
The government defines the covered entities to include nonprofit hospitals, such as critical access hospitals, freestanding cancer hospitals, and children’s hospitals. Clinics of all types can qualify as well, including those treating HIV and family planning. “They have to provide some type of care in the community that’s considered a safety net,” says Heather Brooks, RPh, the vice president of operations and services at ProxsysRX, a Birmingham-based company that partners with covered entities nationwide to

provide pharmacy services and properly manage their 340B programs.
The government, and therefore taxpayers, contribute nothing to the plan. The funding source relies solely on the drugmakers providing outpatient drugs to covered entities at reduced prices. “Using a prescribed formula, manufacturers calculate the 340B ceiling prices which change every quarter, and are based on the Average Manufacturer Price (AMP) minus the Unit Rebate Amount (URA) from the quarter before,” Brooks says.
In return for the deep discount, the pharmaceutical manufacturers’ products gain access to the Medicaid and Medicare Part B prescribers, which include nearly 86 million and 31 million individuals, respectively. According to HRSA,

340B covered entities purchased $53.7 billion in covered outpatient drugs in calendar year 2022.
The hospitals sell the outpatient drugs through a contract pharmacy. The pharmacy fills the patients’ prescription, notably with the patient paying below the usual price or even for free—or charges their insurance company the full price. The covered entity then receives the monies collected minus whatever pharmacy dispensing fees they agreed to.
Those monies have opened the way for these safety-net institutions to save lives and provide care not seen in their communities before. For instance, a rural hospital that’s part of a small Louisiana health system serves a very low income population and provides care to all who walk through their doors. The labor and delivery unit often cares for uninsured patients, and runs as a net loss to the facility. Their 340B program revenue keeps that unit open. Otherwise, those mothers would be forced to deliver at home or would have to drive over 60 miles away.
A large health system in Alabama uses their 340B savings to fund a pharmacy for patients with HIV. The pharmacy extends the 340B discount to patients who need extra help by providing free or discounted prices.



The pharmacies generate revenue as well, which is defined by the contract they agree to with the covered entity. Generally that includes a fee per prescription filled and, in some cases, a percentage of the revenue. Thse profits have been notable enough to entice 71 percent of pharmacies owned by the top four pharmacy chains—Walmart, CVS, Rite Aid, and Walgreens—to join the 340B program.
The success of the program has spurred its growth. According to HRSA, discounted prescription drugs purchased wholesale under the 340B program grew 22.3 percent to $53.7 billion from 2021 to 2022. The number of pharmacies participating in 340B has exploded as well, from 601 in 2009 to 26,885 in 2022, according to a study published in Health Affairs Scholar
This burgeoning growth and having no say in the program’s definition of covered entity has riled drug manufacturers who see that potential profit eaten into. “Not only do they have to give the government a rebate on drugs for Medicaid purchases and claims, but they also have to extend a discount to covered entities,” Brooks says. “And over time, the government has added more and more entity types to that bucket.”



In a world of continual change, surviving depends on evolving. That’s as true for healthcare practices as it is for nature.
A generation ago, there were still small practices where one or two independent orthopedic specialists would share an office. Then the mandate for electronic medical records made it imperative to evolve. Only through the strength of numbers and shared costs could a larger practice afford the costs of buying computer hardware and software, plus the staff to operate and maintain it, and the protection to guard data and insure it against cyber attacks threats. The environment demanded that practices be large enough to share the costs.
Today, rising overhead with regulatory and legal pressures are creating a stressful environment for independent practices who must adapt. Some have sold out to equity interests and taken jobs as employees. Others are going to work for hospitals. A few are looking for a better way to evolve and maintain their independence. As of January, several Alabama orthopaedic practices seem to have found that third alternative as members

of the Southern Orthopaedic Alliance.
“It gives us the buying power of a much larger group, but each member retains local control of decision making on compensation, hours and other operational issues,” said alliance president J. Grant Zarzour, MD of Gulf Orthopedics in Mobile.
Seeing how well similar organizations were doing in other states gave Zarzour hope that there was a way for independent practices to succeed while giving patients quality care at appropriate prices.
“That encouraged me to contact other independent practices in the state that I knew were facing the same chal-

lenges and were no more eager than I was to become someone’s employee,” Zarzour said. “Part of my dream when I set out to become a doctor was to work for myself and make my own decisions. I didn’t go through medical school and all that training to have someone else tell me how to practice medicine based on their latest printouts.
“I could read the spreadsheets myself and saw that what we independent practices paid for supplies, insurance, and other services couldn’t be sustained forever, especially when we had little to no bargaining power, no real voice in regulatory matters and we were paying to duplicate a lot of the services other practices
were paying for. If we could share some of these costs and combine our buying power, that could put us in a much better position to go back to spending more time being doctors and less time worrying about whether I should have taken more business classes in college.”
Southlake Orthopaedics in Birmingham was one of the independent practices thinking along the same lines. “When I heard about the alliance Dr. Zarzour was working on, I remembered a colleague in a nearby state who had mentioned joining an alliance,” Christopher Heck, MD, a Southlake physician, said. “To vet the idea, I called my friend to see how it was going. His response was extremely positive. He said that negotiation as a larger group was getting them better prices on supplies and better service, too. Together they were seen as being a big enough client to respond to now rather than a small operation that could be put off. He also said the promise of independence on the local level held true. It was their practice and they decided how many patients they saw and how long they needed to spend with them.
“Doctors tend to be type A people.




continued from page 10
It’s what gets them through medical school and residency, and helps them make difficult decisions in life and death situations. Type A people tend to want to have their own business and build something for themselves. They just aren’t really suited to being employees who are told what to do based on a different set of priorities from people who have all together different training and goals.
“Being part of a practice feels a lot like having my own business. I’m responsible for what I earn based on what I do. If I need to take a few hours off to go to the dentist, I don’t have to ask for permission, but I know the value of making up those hours later.
“To me, the independent practice model works better from both job satisfaction and patient care perspectives. It is the business of physicians, but it is also their calling, so they are looking at quality of patient care and not just profit when topics like increasing case load goals next year come up.”
In addition to Gulf Orthopaedics in the greater Mobile area and Southlake Orthopaedics in Birmingham, Southern Orthopaedic Alliance’s founding members include Alabama Back Institute in Jasper and Anniston Orthopaedics. The alliance is also talking with a number of other practices across the state.
The alliance shares one tax number and a patient-centric approach to care, but each member operates as its own division with autonomy in decision making on local matters.
“So far, it has been everything we
have hoped for,” Zarzour said. “Negotiating together has helped in getting more reasonable prices on supplies and equipment. We’re also in a better position for negotiating services like insurance coverage, including business, malpractice or health coverage for our staff. If we need specialty expertise on changes in Medicare billing, we don’t each have to hire someone. We can pool our resources and hire the best of the best. And in regulatory and governmental matters, we now have a seat at the table.”
Several independent orthopaedic practices have expressed interest in learning more about the alliance and the advantages it can offer.
“We have detailed information on our website, SouthernOrthopaedicAlliance.com, and they are always welcome to call me and we can arrange a time to talk,” Zarzour said. “We look forward to having members in every part of the state. If we need to refer someone in that area, it would be helpful to know who is particularly adept with that type of procedure or condition. It always feels better referring patients, their families and friends to people we trust.
“We get to know each other pretty well in our regular video meetings and we stay in touch with updates when things are happening that our members need to know about. We have experts working for us who spent a lot of time in business classes so we can spend more time with our patients, which is where we’d rather be.”
continued from page 8
delivered closer to home, treatable conditions are identified earlier, and with telemedicine and mobile diagnostics, patient compliance soars. It’s a win for everyone.”
REHs are required to provide 24hour emergency and observation services and can elect to furnish other outpatient services. An REH cannot have inpatient beds, except those furnished in a distinct unit licensed as a skilled nursing facility. Facilities designated as an REH receive enhanced Medicare payments for certain outpatient services and additional monthly payments.
While Bernstein gives high marks to all the agencies involved, both state and federal, for being helpful in pursuing this new process, Medovation Health has hit a few bumps in the road in their effort to achieve REH designation.
The biggest stumbling block has been the federal requirement to eliminate all inpatient beds. Bullock County Hospital has more than 30 inpatient psychiatric beds, and with the short -


age of mental health beds in the state, they were loath to close them. They hoped the solution would be to create a separate legal entity that would create a psych hospital in the facility that contracted services to the REH, but they were unable to achieve that goal because of regulations, cost and other legal barriers.
“BCH was the first to pursue REH and appears to still be the only active application in the state,” Bernstein said. “Our goal is to convert by May 1. It is likely that others will follow now that the process is better-defined.”
Medovation Health has enlisted the aid of the Rural Health Redesign Center (RHRC) and the Rural Emergency Hospital Technical Assistance Center (REH-TAC) to help with the process.
“The Rural Emergency Hospital designation works best to help hospitals that have low inpatient census,” said Anna M. Anna, RN, BSN, MHA, BC-NE, RHCEOC, program direc -
(CONTINUED ON PAGE 15)
Medicare reimburses about $60 per patient per month for 20 minutes of staff time of chronic care management on patients with 2 or more high risk conditions. Tasks your staff already performs qualify for that reimbursement,

The U.S. Food & Drug Administration (FDA) released new proposed draft guidance in February that would change the FDA’s outlook on the engagement of a data monitoring committee (DMC) in clinical trials.
A DMC, also often referred to as a data and safety monitoring board or an independent data monitoring committee, consists of individuals with specialized knowledge who review emerging data from an ongoing trial to determine whether the trial should be modified, continued or stopped. The FDA recommended in its 2006 Guidance titled “Guidance for Clinical Trial Sponsors: Establishment and Operation of Clinical Trial Data Monitoring Committees” the use of DMCs “in situations in which safety concerns may be unusually high” (for example, where treatment administration is particularly difficult, the study population was inherently vulnerable or the study was performed in high morbid-

ity or mortality populations). Historically, DMCs were used in large, randomized, multicenter trials sponsored by federal agencies, like the National Institutes of Health (NIH). However, in recent years, study sponsors have employed DMCs in new categories; now, DMCs may oversee modestly sized trials to entire clinical development programs, rather than a single trial. While optional in these settings, DMCs are required for use in emergency research where informed consent is not

obtained from all research subjects.
Below is a summary of the draft guidance, including considerations in determining whether to use a DMC, the DMC’s relationship to other clinical trial groups, like Institutional Review Boards (IRB), and operational considerations when employing a DMC.
The FDA’s new draft guidance specifically notes that DMCs are not appropriate for use in all clinical trial settings. For example, DMCs might be impractical for short-term trials, while the FDA highly recommends their use when trial subjects are at serious morbidity or mortality risk, or where causality assessment is based on single risk factor.
DMCs, unlike other review groups, are “the only oversight group that has access to accumulating unblinded safety and efficacy data.” The FDA’s guidance

foresees a DMC’s interactions with other trial review groups as follows:
IRB . While an IRB is responsible for evaluating a trial to determine whether risks to subjects are minimized and such risks are “reasonable in relation to anticipated benefits,” an IRB typically only reviews blinded data and significant new information about a trial.
Steering committees take on several roles, including recruitment and loss to follow-up and demographic inclusion, but like an IRB, typically only reviews blinded data. Where a steering committee and a DMC are used, the FDA recommends a clear delineation between each respective group’s roles and responsibilities in the study.
Other Committees . The FDA’s guidance document describes the recommended relationship between a DMC and other types
(CONTINUED ON PAGE 14)
UAB Medical West, as a community hospital, knows how important it is to have quality care close to home. That’s why we’re thrilled to open our brand new state-of-the-art facility right off of I-459 at Exit 1 this August. In addition to our current services, the new facility will allow us to offer robotic surgery, more beds in our Intensive Care Unit and Operating Room, and the newest state-of-theart imaging technology including 3-D mammography. It’s just one more way we can continue to bring the highest quality of care to the communities in West Jefferson County. For more information about our services near you, visit us online at medicalwesthospital.org.
Immerse in a restorative setting of self-care with personalized treatment for exceptional skin health. Because healthy is a feeling we should all indulge.







continued from page 12



















With a focus on developing minimally invasive technologies in the diagnosis and treatment of thoracic disease, Dr. Minnich performed the rst electromagnetic navigational bronchoscopy (ENB) and the rst robotic bronchoscopy in the state of Alabama. As a result, he has developed one of the largest surgeon experiences with these technologies in the world, which includes offering the most effective treatment for hyperhidrosis (excessive sweating) --- endoscopic thoracic sympathectomy.

The Alabama Disability Determination Service (DDS) invites letters of interest from physicians wanting to work part-time as a medical consultant. The work involves reviewing disability claims in the Birmingham or Mobile offices. An Alabama medical license is required.
The DDS is committed to maintaining a diverse workforce; and therefore, the DDS encourages minority applications.
of reviewing bodies, like endpoint assessment committees, clinical site monitors, safety data review entities and adaptation committees. For example, endpoint assessment committees should not review unblinded data, and therefore, should be separate and distinct from the DMC, while safety data review entities should not review efficacy data, a role generally assumed by a DMC.
DMC Composition . The FDA’s guidance notes that a DMC should be established by a sponsor, trial steering committee or both. DMCs are generally comprised of experts in the field of research, including clinicians, biostatisticians, experts in informatics and technology, FDA regulatory experts, and those with DMC experience. Independent statisticians should also perform statistical analyses, though these statisticians should not serve on the DMC in a voting capacity. Per the FDA, “a well-constructed DMC should be equipped to identify unexpected issues and mitigate problems that could otherwise cause risks to subjects or could adversely affect the quality of the data and integrity of the trial” (emphasis added). Moreover, financial and intellectual conflicts of interest should be evaluated, and those who could bias the trial results eliminated from consideration. In a separate section, the FDA outlines the need for independence of the DMC and its members from the study sponsor.
DMC Charter. The FDA’s recommendation includes a list of items to be included on a DMC’s written charter, which should state the purpose of the DMC, its specific goals and the possible
In response, starting in 2019, drug manufacturers began putting forth their requirements, like requiring covered entities report claims data, limiting covered entities to only one contract pharmacy and restricting 340B access to drugs available for the 340B plan because they say the program has gotten too big.
“It’s changed a lot in the last three to four years,” Brooks says. “There’s now a lot of litigation on this program. There have been lawsuits over the definition of patient, the transparency of drug pricing within the program, and the use of contract pharmacies. There’s nothing in the statute saying covered entities have to do any of this, so HRSA is telling the manufacturers to step back in line, and that they have no right to create any requirements or restrictions,” she says.
Despite the recent legal battles, the growing program improves healthcare, quality of life, and employment in a num-
recommendations it might make to the study’s sponsor. The FDA’s guidance sets forth several elements of a complete charter, including the DMC composition, meeting criteria, the DMC’s planned analyses and data confidentiality.
DMC Responsibilities. The FDA sets forth a detailed list of responsibilities a DMC should assume. Broad categories include monitoring: (1) trial conduct, like recruitment rates and participant dropout and the completeness and timeliness of data; (2) results of interim data analyses; and (3) safety, effectiveness, trial futility and the need for trial adaptations. The DMC may also consider external data and make recommendations to the sponsor concerning continuation of the trial.
FDA Reporting. Finally, although the FDA requires that study sponsors report to the FDA findings that a reasonable possibility of serious unanticipated adverse events was tied to the drug’s use, the FDA’s recommendation would also ask sponsors to inform the FDA about all of the DMC’s safety-related recommendations, whether or not serious.
While the draft guidance, if implemented, would supersede the 2006 guidance, its terms would constitute nonbinding recommendations. The FDA is accepting public comments to its draft guidance until April 15, 2024. A copy of the draft guidance can be reviewed by visiting https://www.fda.gov/ regulatory-information/search-fda-guidance-documents/use-data-monitoringcommittees-clinical-trials.
Jessie Bekker is an attorney at Burr & Forman practicing exclusively in the healthcare practice group. Jessie may be reached at (205) 4585275 or jbekker@burr.com.
continued from page 9
ber of local communities. “Between late 2019 and the end of 2023 ProxsysRx’s 340B Support program went from zero to more than $500 million in savings generated for the hospitals and health systems we serve,” Brooks say. “These savings are vitally important to keeping the healthcare safety-net in place in many communities.
“One of my favorite things is to hear about how 340B impacts patients. Last week, a pharmacist in one of our locations told me about a patient who was in tears when insurance would not cover the medication prescribed for her son, who was being discharged from the hospital with a new diabetes diagnosis. The discount provided to the patient through the partnership of the hospital and the pharmacy, and funded by the 340B program enabled that mom to focus on controlling her son’s diabetes, rather than how to pay for the medication.”
continued from page 11
tor of RHRC. “The goal of the REH designation is to help small rural hospitals stabilize and continue to provide current services in emergency care and observation care, as well as to offer and even expand outpatient services to meet the healthcare needs in their community. Hospitals that have general psych or behavioral health are concerned about losing these services for their communities. They may struggle as they try to determine what works best.”
The process for working with RHRC begins with a half hour introductory call, and if the hospital meets eligibility criteria, they are invited to be part of a cohort process to apply for REH status. “If they decide to go through the process, we provide them with technical assistance to help them figure out what it’s like to be an REH hospital and what that means for them. We also work with them on their individual community needs. Transitioning to an REH will be different than their current services, but it’s exciting to think they can grow, and bring more value to the community. And the financial stability that REH status could bring to some of these hospitals will allow them to invest in outpatient care,” Anna said. “They can start thinking diff erently about how they serve their community.”
“We are still learning a lot,” Bernstein said. “CMS came up with a global approach to this, but left implementation in large part to the individual states. How are they going to license it, what is their process going to be? As far as we know, we are still the first to try going online in Alabama so some of the state agencies, particularly ADPH which has licensure responsibility, are appropriately trying to figure out how this conversion jives with their responsibility to public health and building codes and other regulations out there. It’s a complex process.”
“The struggles that we see across the county in rural health care are real,” Anna said. “This is a solution. It may not be the right solution for all of the struggling rural hospitals, but it is the right solution for some of them, to help them survive and continue to meet the needs of their community.”
If you have questions or would like assistance determining feasibly for conversion to REH, contact RHRC at REHSupport@RHRCO.org or Medovation Health at BBernstein@medovatonhealth.com.
The 2024 Final Rule delegates authority to OCR to initiate compliance reviews; conduct investigations; utilize existing enforcement regulations (and withhold funding) for grants, contracts and other programs and services; and make enforcement referrals to the U.S. Department of Justice. Any individual or entity may file a complaint with OCR alleging potential violations of the federal healthcare conscience protection statutes. In other words, the complainant is not required to be the entity whose rights have been violated. Failure to respond to a request for information or to a data or document request will result in a negative inference.
One best practice for achieving compliance with and educating the public on the 2024 Final Rule is by posting and providing notice about the federal healthcare conscience protection statutes. The 2024 Final Rule outlines a model notice in Appendix A, which states, in part:
“You may have rights as a provider, patient, or other individual under these Federal statutes, which prohibit coercion
or other discrimination on the basis of conscience, whether based on religious beliefs or moral convictions, in certain circumstances. If you believe that [Name of entity] has violated any of these provisions, you may file a complaint with the U.S. Department of Health and Human Services, Office for Civil Rights …”
Entities and recipients subject to the 2024 Final Rule should educate personnel by posting this notice on its website, in a prominent and conspicuous physical location, in personnel materials (such as manuals, handbooks, orientation materials and trainings), in employment applications and in postgraduate education materials. Covered entities or recipients should address any complaints or inquires related to the federal healthcare conscience protection statutes and should cooperate fully if OCR initiates an investigation or request for information.



Our referral process will put the spring back in your step!
• Patients are scheduled within 24 hours.
• Patients are seen in clinic within 2-4 weeks of referral.
• We keep you informed about the patient’s treatment plan.
• We make sure the loop is closed on your referral.
205.332.3160
One of the biggest news stories in the past year has been the emergence of artificial intelligence (AI), the science of creating machines that can think like humans, something that is both exciting and frightening. There are probably numerous ways in which AI can help medical practices work more efficiently, while providing quality care. However, one of the downsides will be in the realm of cybersecurity. In this regard, Britain’s National Cyber Security Centre recently warned that the rapid development in AI will likely contribute to the global rise in ransomware attacks.
With this in mind, let’s take a look at the ways AI is being used to empower cybercrime activity.
Deepfakes involve phony audio and/or visual media that appears to be authentic. A CEO’s voice, for example, might be employed to engage in a phone call to an employee requesting that a large sum of money be wired to an account. The employee fully believes that

his employer is on the other end of the phone.
While hackers in the past have spent hours attempting to guess a user password, AI programs are able to generate vast numbers of password variations using simple algorithms in a short period of time.
Hacking
Hacking attempts by humans cannot begin to compete with those powered by AI. The hacking capabilities of AI programs are exponentially more effective than those of humans.

Criminals have begun to use social engineering once they’ve gained access to a business’s email, posing as business partners or clients, and asking for payment. The use of AI accelerates this process dramatically, and even security professionals are often unable to recognize generated emails.
Advanced Persistent Threats
This type of attack allows information from the targeted network to be gleaned over time, with the breach itself evading detection. AI algorithms automate and enhance this process.

Ransomware attacks are improved and strengthened via AI algorithms.
AI-generated financial transactions
target businesses and evade traditional fraud detection.
Distributed Denial of Service Attacks (DDOS)
AI botnets are powered to attack business websites, overwhelming them with malicious traffic, eventually disabling the site completely.
While the power of AI has dramatically increased the threat potential from cybercriminals, IT security experts are also using AI defensively to protect business networks. New AI-driven cybersecurity solutions are constantly evolving to detect threats in real-time and respond instantly, so it’s important for medical practices to stay aware of the coming threats and solutions.






With the largest healthcare practice in the country, Holland & Knight has more than 400 experienced attorneys covering virtually every segment of the healthcare industry, from transactional matters, regulatory compliance and real estate to litigation, government enforcement and public policy issues.
Our dedicated healthcare attorneys and professionals – in Birmingham and throughout the country – have the insight, experience, depth and resources to help promote and protect your interests.
Kassouf named accounting top regional leader
Kassouf was named a Top Regional Leader in Accounting Today’s annual ranking. The firm placed in the top 20 among Gulf Coast firms, including Alabama, Mississippi, Louisiana, and Florida. Kassouf is one of four Birmingham firms and one of eight Alabama firms to receive the honor.
“We are honored to be named a regional leader in the accounting profession. It’s a reflection of our team’s dedication to helping our clients,” said Kassouf Managing Director Jonathan Kassouf.
The award is based on data such as annual revenue, percentage in revenue change, employee metrics, and fee splits.






The announcement was made during the Biden Cancer Moonshot forum at the White House where leaders from across health care, government, research and other divisions came together to discuss the challenges of increasing access to cervical cancer prevention.
“I am honored with the opportunity to lend my expertise and life experiences to such an important effort,” Scarinci said. “My dedication to cervical cancer elimination is both personal and professional as I truly believe we can eliminate this cancer in my lifetime, as we have done with polio.”
Birmingham-based MainStreet Family Care










EDITOR & PUBLISHER
Steve Spencer
VICE PRESiDENT OF OPERATIONS
Jason Irvin
CREATIVE DIRECTOR
Katy Barrett-Alley
CONTRIBUTING WRITERS
Jane Ehrhardt, Ashley Franco, Laura Freeman, Lynne Jeter, Marti Slay
Birmingham Medical News 270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110
AD SALES: Jason Irvin, 205.249.7244
Grandview Medical Center is beginning a project to expand its Emergency Department. Emergency department visits have nearly doubled since the hospital’s opening to more than 44,000 visits in 2023.
The expansion project will add 3,600-square feet and 10 additional treatment rooms, bringing the total number to 32. Construction is expected to be completed by the end of the year.
Grandview is also planning an inpatient bed expansion project. The proposed project, currently in the regulatory approval process, includes an expansion of Grandview’s Women’s Center, the relocation of inpatient reha-

bilitation to a connected building on campus, and the renovation of space within the hospital to accommodate additional acute care beds.
The proposed inpatient bed expansion project will occur in two phas-


es. The first phase will add postpartum beds to the hospital’s obstetrics unit. Newborn deliveries at the hospital have tripled since 2016 with more than 3,000 births last year. The second phase will add 25 acute care beds on the 10th floor after that space is vacated by the relocation of the hospital’s 17-bed inpatient rehabilitation unit to Grandview Physicians Plaza II, a 140,000-square foot building that opened on the Grandview campus in 2023 and is expected to be fully-occupied by the end of 2025.
After regulatory approvals are received, the bed expansion project is expected to be completed in approximately one year.