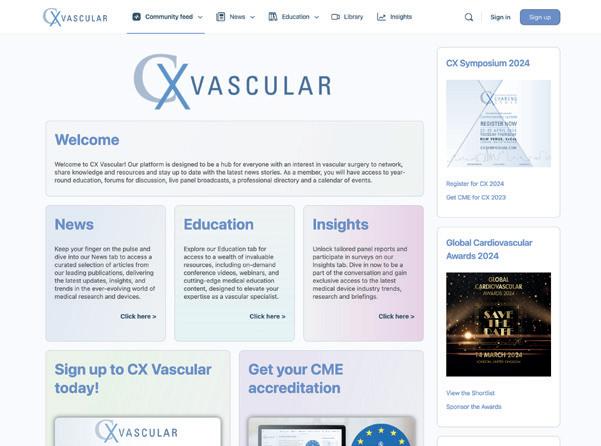
Charing Cross Symposium 2024 preview page 8
World’s first successful geneticallyedited pig kidney transplant performed in USA
A recent attempted transplant of a genetically-edited pig kidney has been successfully carried out for the first time at Massachusetts General Hospital (MGH) in Boston, USA. The transplant team, led by Leonardo V Riella, Tatsuo Kawai, and Nahel Elias (all MGH), transplanted the genetically-edited pig kidney with 69 genomic edits into a living patient after a fourhour-long surgery. The recipient of the transplant—Richard Slayman—a 62-yearold-man living with end-stage-kidney disease (ESKD)—is recovering well and is expected to be discharged soon.
The genetically-edited pig kidney was provided by eGenesis. After five years of collaborative research between the company and MGH—the findings of which were published in Nature in 2023—eGenesis was able to provide a kidney from a pig donor that was genetically-edited using CRISPR-Cas9 technology to add certain human genes to improve its compatibility with the human recipient, as well as remove harmful pig genes. eGenesis also inactivated porcine endogenous retroviruses in the pig donor to eliminate any risk of infection in humans.
The US Food and Drug Administration (FDA) approved an expanded access protocol (EAP) for the transplantation in February 2024, along with an infusion of novel immunosuppressant drugs; tegoprubart, provided by Eledon Pharmaceuticals, and ravulizumab, provided by Alexion Pharmaceuticals.
As MGH stated in a press release about the transplantation, the procedure marks a “major milestone in the quest to provide more readily available organs to patients”. It also added that the successful xenotransplantation of a genetically-edited pig kidney in a living recipient represents is “a historic milestone” as a potential solution to the shortage of organs available for transplantation that is affecting the globe. It state that, according to the United Network for Organ Sharing (UNOS), more than 100,000 people in the USA await an organ for transplant, with 17 people dying each day whilst
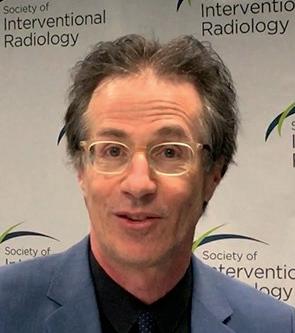
Profile: Gerald Beathard page 10

Dos and donʼts of vascular access at ASDIN page 12
UKKA RaDaR study gives insight into rare kidney diseases page 14
PINCH trial: First blinded RCT finds preoperative forearm exercises increase target vein diameter
In a recent research letter published in the European Journal of Vascular and Endovascular Surgery, a group of researchers—led by Koen van der Bogt (Haaglanden Medical Centre [HMC], The Hague, The Netherlands)—discuss the PINCH trial and its hypothesis that preoperative exercise may result in larger blood vessel diameters at the time of arteriovenous fistula (AVF) creation, aiding in the surgical formation of forearm AVFs. According to this letter, the PINCH trial was able to show a moderate increase in cephalic vein diameter thanks to preoperative arm exercises for six weeks before surgery, with an additional improvement for patients that had an increased pinching force in the same timeframe.
According to figures quoted by van der Bogt et al, rates of radiocephalic fistula (RCF) maturation failure are as high as 30–60%, implying that methods to improve maturation are needed. The current recommendations given by international guidelines to aid in improving RCF maturation are that regular forearm exercise in the first months after AVF creation that, based on small, non-randomised studies, is shown to aid in fistula maturation. However, the PINCH trial shows that doing these exercises preoperatively may in fact yield better results for maturation, due to the increased diameter of blood vessels.
The design of the PINCH trial—which the authors aver has been previously approved by the medical ethics board—was intended to detect a 0.58mm improvement in mean venous diameter in the treatment group (equalling an estimated 66% increase in blood flow) with a power of 80% and an alpha level of 5%. To do so, the researchers determined that they would need 16 patients per group. Due to this, they enrolled 24 patients (to allow for any drop-outs). Predialysis patients or those on haemodialysis through a contralateral central venous catheter scheduled for creation of an AVF were eligible. A standard preoperative arterial and venous duplex was performed in both arms by blinded vascular laboratory technicians.
Patients that were randomly assigned to the intervention (PINCH) group received a real time monitored handgrip training device, which was paired to a game on a tablet device intended to aid in the

exercises. At baseline, patients received instructions and a training schedule containing exercises for 10 minutes, three times daily for a total of six weeks. Van der Bogt et al also state that patients attended weekly supervised physiotherapy sessions, allowing for training to be adjusted based on maximum pinch force for each individual. After six weeks, duplex ultrasound was repeated, and pinch force was assessed. AVF surgery was then performed six–eight weeks after the forearm training began, with follow-up visits that included a duplex ultrasound planned for six weeks post AVF creation. The primary endpoint was increase in cephalic vein diameter after six weeks of forearm exercise.
Whilst 66 patients were eligible, only 48 of the patients recruited gave consent and were randomised. Nine patients withdrew from the study after inclusion, but before starting the training schedule (seven in the intervention and two in the control group). The authors highlighted that patient characteristics showed little to no significant differences between the two groups. Initially, the baseline vascular diameter measurements were found to be larger in the control group, but at six weeks, patients that had been assigned to the intervention group showed a greater increase in cephalic vein diameter at elbow level. The study also found that a subgroup of PINCH patients with increased pinching force showed significantly greater increases in
April 2024 Issue 11 www.renalinterventions.net
In this issue:
Continued on page 2 Continued on page 4
Follow Renal Interventions on all our social media platforms for the latest news, insight and events in kidney care
target vein diameter
the vascular diameter of the cephalic vein at the elbow when evaluated with a tourniquet. As well as this, the authors state that there was an increase in compliance (no tourniquet versus tourniquet) of the cephalic vein at the elbow. There were no differences in the diameter of the cephalic vein at wrist level.
Van der Bogt and the co-authors of this letter state that the PINCH study is “the first blinded randomised controlled trial (RCT) investigating the impact of preoperative forearm exercise on target vein diameter, using directly and remotely supervised exercises”. They argue it shows that responsiveness to forearm exercise relies on adherence to the training programme, with, as they phrase it, a “moderate positive effect on cephalic vein diameter at the elbow and on cephalic vein compliance”.
Preoperative cephalic vein diameter, according to the authors, is a key predictor of AVF maturation. Venous distensibility, resembling vascular compliance, has also shown a significant correlation with AVF maturation. In this study, increased cephalic vein diameter and compliance were clinically significant, potentially improving AVF outcomes, which has to be evaluated in future studies. The current study was not powered to assess AVF maturation directly, one of the limitations of this small RCT, the authors state.
One thing that the authors did draw to the readers’ attention was the physicalfav study, the results of which were published in 2021 in the Journal of Nephrology. This study, which they state is the only other RCT on six to eight weeks of unsupervised upper and forearm exercises before AVF creation—although not a blinded study—reported increased venous and arterial diameters, promoting the creation of more forearm AVFs. They do add that larger baseline vascular dimensions and physical capacity, compared

“There is still more work and research that is needed in this area.”
with patients that participated in the PINCH trial, could explain the more favourable reported outcomes that Ines Aragoncillo Sauco (Gregorio Marañón General University Hospital, Madrid, Spain) et al experienced during the physicalfav trial. Van der Bogt et al state that the results of this earlier trial may suggest that preoperative forearm exercises may be particularly beneficial in patients with adequate baseline strength.
In their conclusion, the authors of the research letter state that “a moderate effect on vasodilation is to be expected from well executed forearm exercises in patients with adequate strength at baseline”. They add, however, that there is still more work and research that is needed in this area. The ideal composition of a training programme, which they say “will be a trade-off between intensity and burden”, should be studied and further established.
To detect a 0.58 mm improvement in mean venous diameter in the treatment group (equalling an estimated 66% increase in blood flow) with a power of 80% and an alpha level of 5%, 16 subjects per group were needed for the study.
The latest stories from the renal world
CROSS-SPECIALTY COLLABORATION: Advocating for the importance of collaboration across the boundaries of specialties for the benefit of renal denervation as a therapeutic intervention, Wei Li (Syracuse VA Medical Center, SUNY Upstate Medical University Syracuse, USA, and Texas Tech University School of Medicine, Lubbock, USA) and Aiyu Zhao (Syracuse VA Medical Center, Syracuse, USA) write together about the origins of renal denervation, the complications that can often accompany it, and the crucial role that multidisciplinary collaboration plays in managing those complications.


● For more on this story, go to page 5
ACHIEVEMENTS AT ASDIN:
At the recent American Society of Diagnostic and Interventional Nephrology (ASDIN) annual scientific meeting in New Orleans, USA (23–24 February 2024), then-president of ASDIN Vandana Due Niyyar outlined some of the society’s achievements over the past year, as well as some of their hopes for what they will accomplish in the year to come. She emphasised the success of the society's leadership in widening the multidisciplinary nature of both ASDIN and their annual meeting, and highlighted how essential the participation of ASDIN members is to its success.

● For more on this story, go to page 6
ANALYSIS OF RADAR DATA:
A new longitudinal analysis of the UK National Registry of Rare Kidney Diseases (RaDaR) recently published in The Lancet explores the impact of rare kidney diseases on chronic kidney disease (CKD). The authors explore the impact of these conditions on rates of kidney failure, and how that can affect the percentages of patients afflicted that are represented in cohorts requiring kidney replacement therapies.

● For more on this story, go to page 14

Renal Interventions
April 2024 – Issue 11
Nicholas Inston | Editorial Board: Ziv Haskal, Stephen Hohmann, Robert Jones Publisher: Stephen Greenhalgh | Content Director: Urmila Kerslake | Editorial contribution: Jocelyn Hudson, Will Date, Eva Malpass, Jamie Bell and Bryan Kay | Advertising: Rav Pankhania rav@bibamedical.com Subscriptions: subscriptions@bibamedical.com | News or advertising queries: Published by: BIBA News, which is a subsidiary of BIBA Medical Ltd BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788 | BIBA Medical, North America, 155 North Wacker Drive, Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323 Printed by: Print Tech Solutions. Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address. © BIBA Medical Ltd, 2024. All rights reserved. If you have comments on this issue or suggestions for upcoming editions, write to georgeb@bibamedical.com Introduction 2
linkedin.com/company/renal-interventions/
Editor-in-chief:
PINCH trial: First blinded RCT finds preoperative forearm exercises increase
News In Brief
from page 1
Continued
mm 0.58 increase in blood flow 66% a power of 80% alpha level 5%
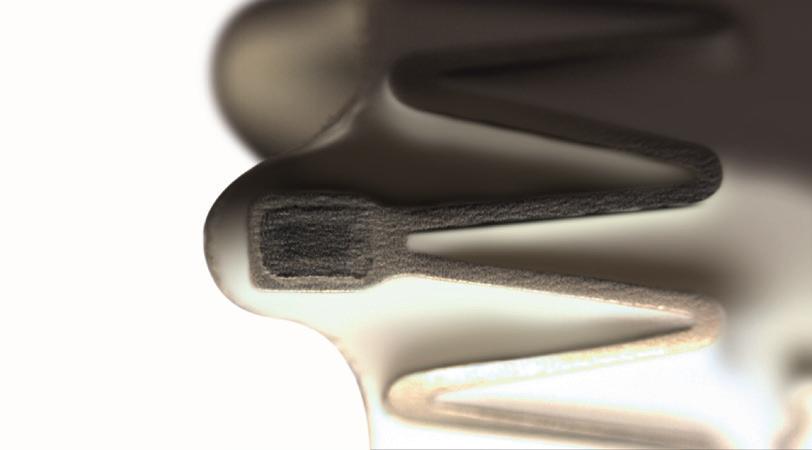
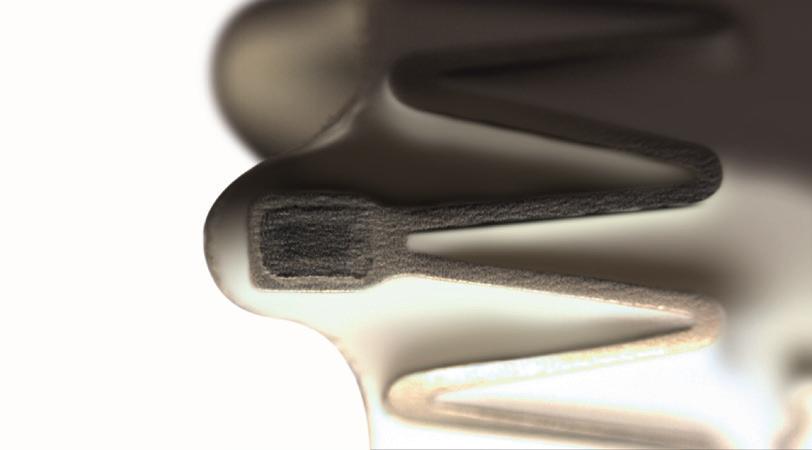
Example of the PINCH real time monitored handgrip training device
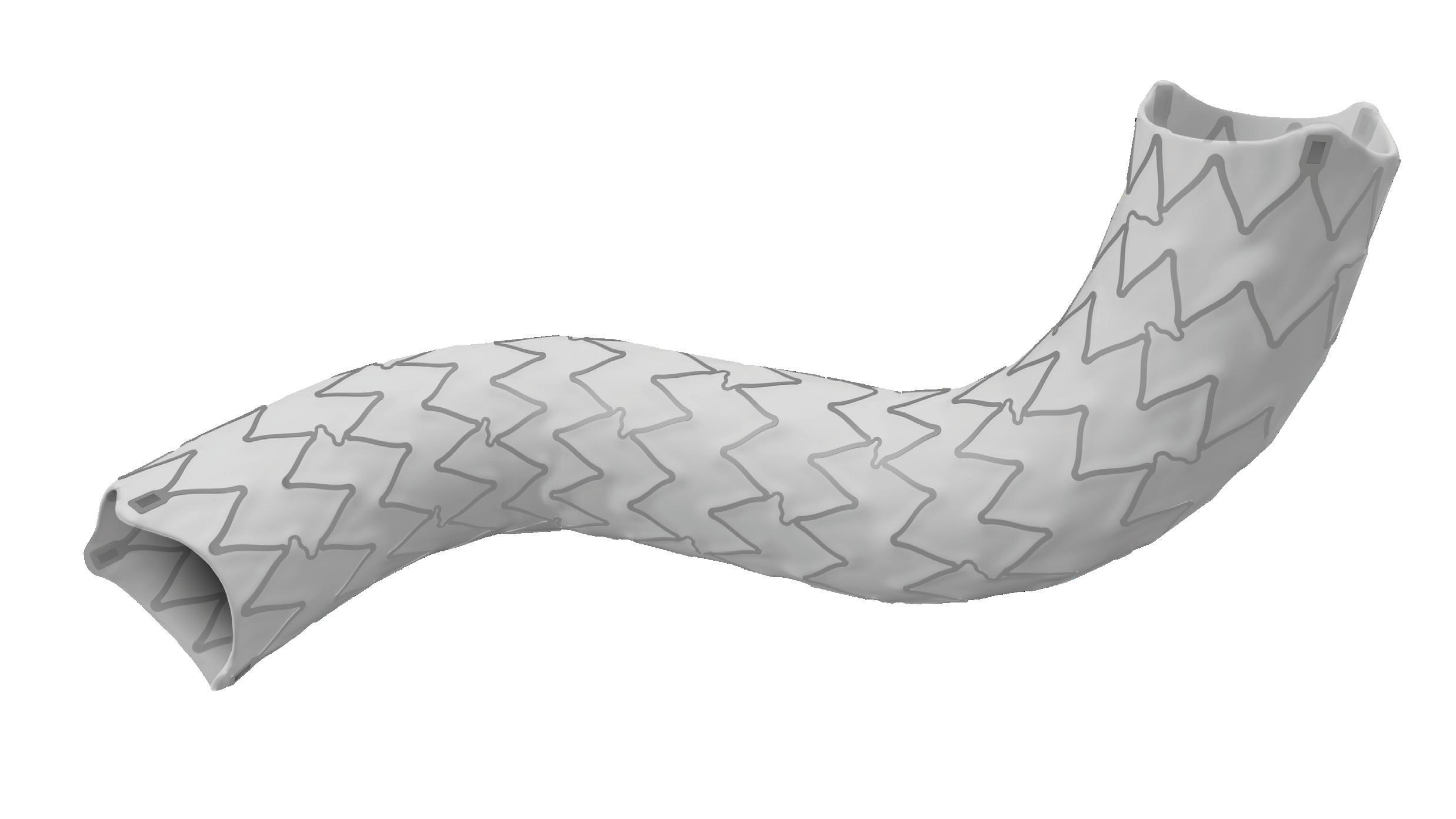
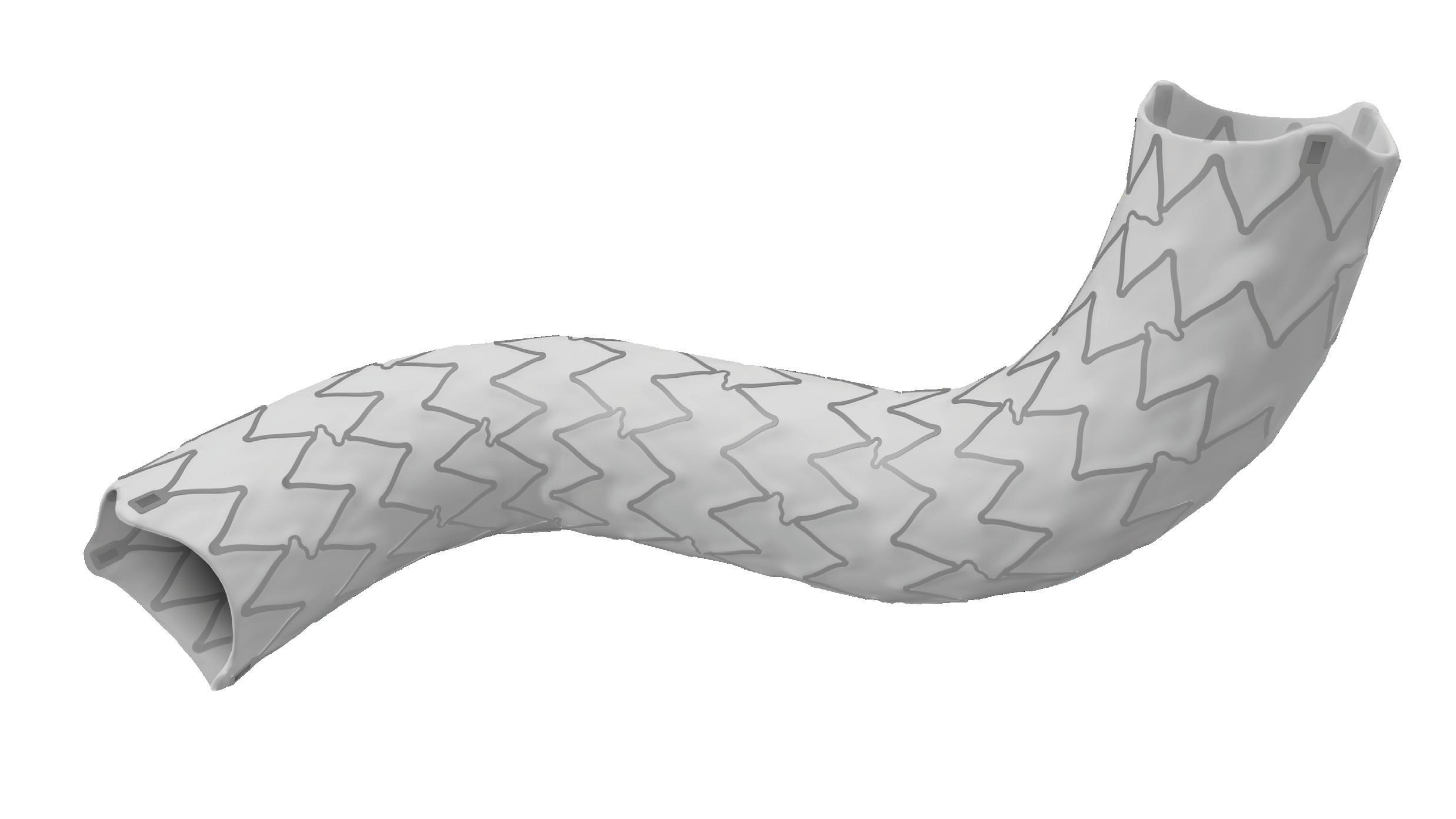
High flexibility
To arrive and treat the most angled arteries
Enhanced visibility
Unique stent with radiopaque markers to facilitate the implantation

Smallest profiles
6F introducer compatibility up to 8mm*
TechCover
Proprietary technology to encapsulate the stent into an inner and outer ePTFE layer
*6F up to 8x17 mm and 7F from 8x27mm up to 10 mm.
www.ivascular.global iCover BX ePTFE covered stent The visibility you deserve
World’s first successful genetically-edited pig kidney transplant performed in USA
Continued from page 1
waiting for an organ. The organisation also adds that kidneys are the most common organ needed for transplant, and ESKD rates are estimated to increase 29–68% in the USA by 2030, according to research published in the Journal of the American Society of Nephrology.
The recipient of the transplant has been living with type-2 diabetes and hypertension for several years, and had previously received a human kidney transplant in December 2018, after undergoing dialysis for seven years prior to the transplantation. The transplanted organ began to show signs of failure after five years, leading to the patient resuming dialysis in May 2023, which lead to him experiencing recurrent dialysis vascular access complications that necessitated regular hospital visits for dialysis maintenance.
Slayman said in a statement: “I have been a Massachusetts General Transplant Center patient for 11 years and have the highest level of trust in the doctors, nurses, and clinical staff who have cared for me. When my transplanted kidney began failing in 2023, I again trusted my care team at MGH to meet my goals of not just improving my quality of life but extending it. My nephrologist, Winfred Williams, and the transplant centre team suggested a pig kidney transplant, carefully explaining the pros and cons of this procedure. I saw it not only as a way to help me, but a way to provide hope for the thousands of people who need a transplant to survive. I want
to thank everyone at MGH who has cared for me, especially Williams, Kawai, the surgeon who performed my first kidney transplant and now this one, and Riella, who has orchestrated the logistics behind this new transplant. They have supported me during every step of the journey, and I have faith they will continue to do so.”
Commenting on the importance of the landmark procedure, Kawai stated: “The success of this transplant is the culmination of efforts by thousands of scientists and physicians over several decades. We are privileged to have played a significant role in this milestone. Our hope is that this transplant approach will offer a lifeline to millions of patients worldwide who are suffering from kidney failure”.
The transplant team highlighted the importance of collaboration for the advancement of new treatments, with Elias saying that: “This seminal transplant could not be possible without collaboration and effort from multiple teams and specialists at MGH including physicians, surgeons, scientists, anaesthesiologists, and nurses. They participated in coordinating the patient’s care in preparation for the transplant, seeing him through the surgery, and caring for him postoperatively.”
Summarising what has been achieved by their team, Riella said: “Seventy years after the first kidney transplant and six decades following the advent of immunosuppressive medications, we stand on the brink of a monumental breakthrough in transplantation. At MGH alone, there are over 1,400 patients on the waiting list for a kidney transplant. Some of these patients will unfortunately die or get too sick to be transplanted due to the long waiting time on dialysis. I am firmly convinced that xenotransplantation represents a promising solution to the organ shortage crisis.”
This advertorial is sponsored by Alio
“Seventy years after the first kidney transplant and six decades following the advent of immunosuppressive medications, we stand on the brink of a monumental breakthrough in transplantation.”

Significant milestones of the Alio SmartPatch™ to enable remote monitoring of patients with chronic kidney disease
With one in three people living with diabetes and one in five with hypertension, the risk of chronic kidney disease (CKD) is increasing across the globe. Around 700 million people are estimated to have CKD. That number increases to 850 million people including acute kidney injury, which translates to more than 10% of the global population. This increasing incidence warrants a significant need for renal replacement therapy—it is expected around 5.4 million people will require dialysis or transplant by 2030 with 15–20% of the patients dying within the first 12 months of starting dialysis.
Afunctioning dialysis access is an essential aspect of treating patients with CKD and end-stage kidney disease (ESKD). Timely dialysis access (haemodialysis arteriovenous fistula/graft [AVF/G] or peritoneal dialysis catheter insertion), preserving the function of AVF/G with early diagnosis of failure, and a patient engaged surveillance of the dialysis access are challenges faced by patients and their clinical team. Despite the use of surveillance strategies, point-of-care ultrasound, and other advances, most care is delivered at specialist centres, requiring patients to travel to centres repeatedly for diagnostic and therapeutic interventions. Remote patient monitoring (RPM) is key to enhancing dialysis access surveillance. With continuous measurement of dialysis access status, RPM can provide more insight into the access pathophysiology, improving patient engagement towards their care. Furthermore, it enables access surveillance without the constraints faced by healthcare providers, such
as trained staff, frequency of in-centre visits, timely review, and early alert to the patients’ clinical state. A solution with the ability to measure key information for CKD and ESKD patients remotely and proactively is paramount to address this unmet need.
Alio SmartPatch™ is such a solution—a wearable biosensor and US Food and Drug Admin istration (FDA)-cleared, non-invasive, wireless medical device that remotely monitors the patient’s dialysis access with timely notifica tions for healthcare providers to intervene.
The Alio remote monitoring platform combines this differentiated, multisensor wearable SmartPatch with a provider-based portal for sequential tracking of patients' physiological metrics. These metrics include basic vitals, haematologic parameters, and potassium, as the world’s first to measure abnormal serum potassium indicator. The SmartPatch operates in conjunc

tion with a hub data relay system and an end-toend cloud software data path.
The SmartPatch also contains a microphone, and when placed over the AVF/G access, it collects a 15-second, reviewable acoustic recording of the AVF/G access. Alio has developed an automated, machine-learning method of analysing the acoustic sample. In the proof-of-concept study comprising of 692 reads from 28 patients, Alio’s prediction algorithm was able to detect patency of AVF/G (flow or no flow) with sensitivity of 79.3% and specificity of 95.3%. Further studies are planned to evaluate the impact on clinical practice, patient engagement, and cost-effectiveness in delivering a remote surveillance of dialysis access.
The Alio SmartPatch and its ability to measure patency of AVF/G offers a unique opportunity to deliver patient-centred, personalised monitoring of CKD and ESKD patients through frequent remote monitoring. With additional metrics under development, the Alio team looks ahead to offering a comprehensive, proactive and predictive renal failure care solution for patients and healthcare professionals.
References:
1. Francis A, Harhay M N, Ong, A C M, et al. Chronic kidney disease and the global public health agenda: an international consensus. Nature Reviews Nephrology. 2024; 3 Apr. doi: 10.1038/s41581-024-00820-
6. Online ahead of print. PMID: 38570631.
2. Whittaker D R, Miller F, Shimasaki N, et al. Development of a machine-learning based, remote-monitoring system for the automated detection of the periodic acoustic signal associated with the bruit of an AV access. Journal of Vascular Surgery. 79; 4, 26S. April 2024.
3. Miller F, Murray J, Budhota A, et al. Evaluation of a wearable biosensor to monitor potassium imbalance in patients receiving hemodialysis. Sensing and Bio-Sensing Research. 2023; 40:2214-1804.
4 April 2024 – Issue 11 Xenotransplantation
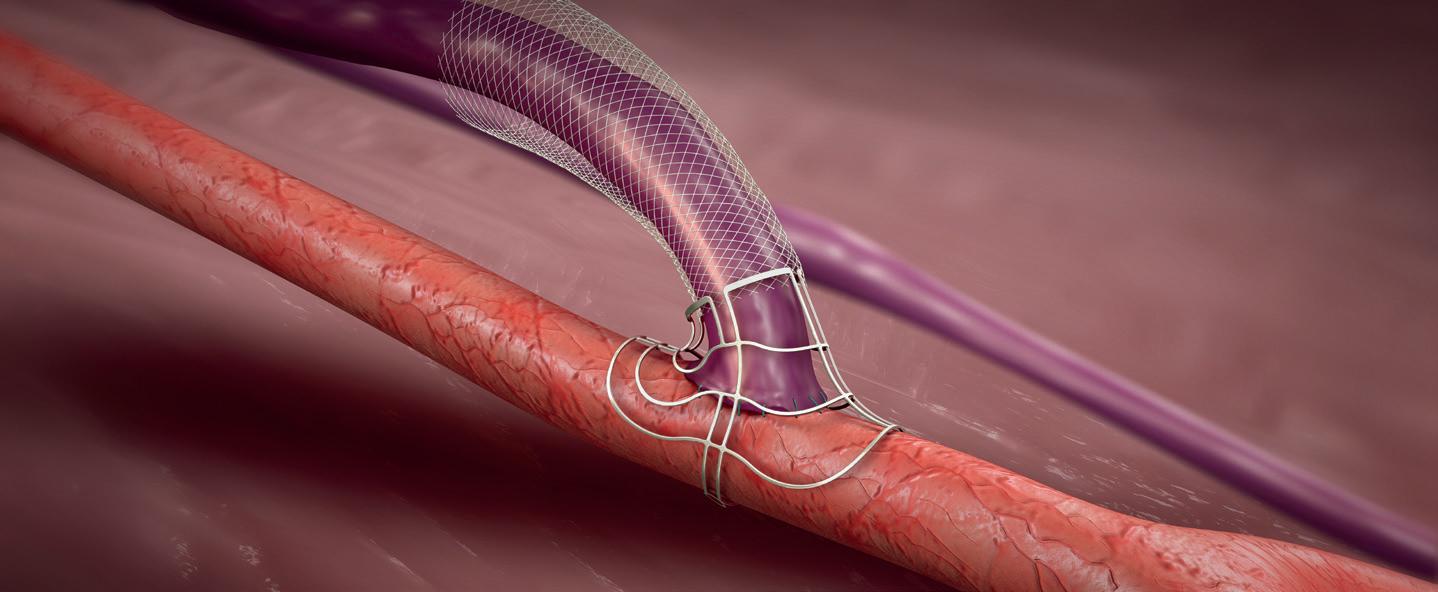
Below: The kidney xenotransplantation being performed
SmartPatch
Point of View
Wei Li & Aiyu Zhao


Renal denervation: Bridging specialty boundaries with better collaborations
Wei Li (Syracuse VA Medical Center, SUNY Upstate Medical University Syracuse, USA, and Texas Tech University School of Medicine, Lubbock, USA) and Aiyu Zhao (Syracuse VA Medical Center, Syracuse, USA) write together about the origins of renal denervation (RDN), the complications and challenges that can often accompany the new therapeutic intervention, and the importance of multidisciplinary collaboration to combat these issues effectively.
Hypertension leads to stroke, heart attack, heart failure, kidney damage, and many other health problems. A reduction of 10mmHg in systolic blood pressure (SBP) is associated with substantial risk reductions: 28% for heart failure, 27% for stroke, 17% for coronary disease, 5% for chronic kidney failure, and 13% for mortality.1 In the USA, despite the availability of medications and lifestyle intervention advocacy, nearly 50% of adults are affected by hypertension.2,3 The US Surgeon General’s call-to-action has underscored the role of social and economic factors as root causes of health inequities, notably impacting certain populations, including non-Hispanic Blacks2 and US veterans, who experience hypertension prevalence rates ranging from 71% to 87%.4 Among them, a majority (66%) were considered to have uncontrolled hypertensions, according to the Veterans Health Administration guideline.4
The concept of RDN originated in 1953 with open surgical splanchnicectomy for severe primary hypertension.5 The initial generation of minimally invasive catheter-based RDN in 2014 failed to show significantly lower office or 24-hour ambulatory SBP compared with sham treatment.6 However, with further animal and clinical studies, two newer generation of percutaneous endovascular RDN devices have recently demonstrated that RDN significantly reduced office and 24-hour ambulatory blood pressure (BP) compared with sham treatment and subsequently received US Food and Drug Administration (FDA)’s approvals in November 2023.
Initially explored within interventional cardiology, RDN is now garnering interest from a broader range of medical specialties, including nephrology, radiology, and vascular surgery. Each specialty contributes unique perspectives and expertise to RDN. Cardiologists provide insights into hypertension’s cardiovascular implications, while nephrologists offer valuable insights into renal physiology and blood pressure regulation, and have suggested that
adults with hypertension and chronic kidney disease be treated with a lower target systolic blood rpessure (SBP) of <120mmHg.7 Interventional cardiologists, radiologists, and vascular surgeons play pivotal roles in RDN’s imageguided procedures.
Like any other minimally invasive technologies, RDN poses challenges and potential complications, especially when intervening in normal renal arterial anatomies, often in working-age patients. Variations like accessory renal arteries or aberrant branching patterns can complicate procedures, increasing the risk of adverse events such as renal artery dissections, occlusions, perforations, and bleeding. These complications may lead to life-threatening sequelae, necessitating open surgical reconstructions.
To mitigate challenges and minimise adverse events, implementing RDN programmes through a collaborative care models is key. Multidisciplinary teams, including physicians and allied healthcare professionals, should collaborate to assess patient suitability and care priority, perform RDN procedures, and coordinate post-procedural care. This patient-centred approach leverages diverse expertise to optimise treatment outcomes and evaluate long-term efficacy.
Given the developmental journey of the current RDN technology, it certainly serves as a catalyst opportunity for interdisciplinary research and future innovation, stimulating cross-specialty dialogue and collaboration. Cross-specialty joint research initiatives can explore the mechanistic underpinnings of RDN, elucidating its effects on sympathetic tone, renal function, and cardiovascular outcomes. Collaborative efforts also extend beyond clinical research to encompass technological advancements, such as smaller profiles of delivery systems, less invasive imaging modalities, and biomarker discovery, aimed at optimising RDN procedures and patient selection criteria.
RDN is within the realm of endovascular intervention where the adoption of RDN necessitates comprehensive education and training programmes spanning the above specialties. Collaborative efforts in medical education empower practitioners to further standardise the trainings of RDN procedures. Furthermore, interdisciplinary training programmes foster a culture of mutual learning and collaboration, equipping healthcare professionals with a holistic understanding of RDN’s clinical applications and implications across these specialties.
While RDN holds promise, its adoption may exacerbate the above existing health inequities among the current hypertension populations due to disparities in access to care, socioeconomic factors (such as private or government/public health insurances), and geographic locations. Vulnerable groups may face barriers to accessing this advanced therapeutic option for uncontrolled primary hypertension. Addressing these factors requires a multifaceted approach involving healthcare providers, community stakeholders, and policy and law makers to ensure equitable access to RDN and comprehensive hypertension management among underserved and vulnerable populations, including veterans.
Overall, RDN represents more than just a new therapeutic intervention; it embodies a major paradigm shift towards collaborative care delivery that affects one of the most prevalent health issues. By uniting specialists across disciplines, RDN will likely exemplify the transformative power of interdisciplinary collaboration in advancing medical science and improving patient outcomes in general. As we embrace the opportunities presented by RDN, let us continue to foster collaborative endeavours that transcend disciplinary boundaries and drive innovation in cardiac, imaging/radiological, vascular, and renal medicines.
Affiliations and disclosures:
Wei Li is an associate professor and endovascular and vascular surgeon and the founding programme director of a surgeon-led future interventional nephrology fellowship programme. He is also a consultant for W. L. Gore & Associates, the principal investigator of studies at Becton, Dickinson, and Company (BD) and Recor Medical.
Aiyu Zhao is a chief of nephrology, dialysis program medical director, and facility dialysis programme committee chair, and board-certified hypertension specialist (CHS). She has no relevant financial disclosures.
References
1. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. The Lancet. Mar 5 2016;387(10022):957-967. doi:10.1016/S0140-6736(15)01225-8
2. Muntner P. The US surgeon general’s call-to-action to control hypertension: ntroduction to an American Journal of Hypertension compendium. Am J Hypertens. Mar 8 2022;35(3):211-213. doi:10.1093/ ajh/hpab188
3. Swaminathan RV, East CA, Feldman DN, et al. SCAI position statement on renal denervation for hypertension: patient selection, operator competence, training and techniques, and organizational tecommendations. Journal of the Society for Cardiovascular Angiography & Interventions. 2023/11/01/ 2023;2(6, Part A):101121. doi:https:// doi.org/10.1016/j.jscai.2023.101121
4. Yamada M, Wachsmuth J, Sambharia M, et al. The prevalence and treatment of hypertension in Veterans Health Administration, assessing the impact of the updated clinical guidelines. J Hypertens. Jun 1 2023;41(6):995-1002. doi:10.1097/hjh.0000000000003424
5. Smithwick RH, Thompson JE. Splanchnicectomy for essential hypertension; results in 1,266 cases. J Am Med Assoc. Aug 15 1953;152(16):1501-4. doi:10.1001/jama.1953.03690160001001
6. Bhatt DL, Kandzari DE, O’Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. Apr 10 2014;370(15):1393-401. doi:10.1056/NEJMoa1402670
7. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. Mar 2021;99(3s):S1-s87. doi:10.1016/j.kint.2020.11.003
April 2024 – Issue 11 5 Renal Denervation
for mortality for heart failure 28% for chronic kidney failure 5% for coronary disease 17% stroke 27% 13%
A reduction of 10mmHg in systolic blood pressure (SBP) is associated with substantial risk reductions
ASDIN president outlines society’s achievements from the past two years and its goals moving forward
At this year’s American Society of Diagnostic and Interventional Nephrology (ASDIN) annual scientific meeting (23–25 February 2024, New Orleans, USA), outgoing president Vandana Dua Niyyar (Emory University, Atlanta, USA) used her president’s address to explore what the future looks like for ASDIN and the society’s plan for action.
The leadership of ASDIN has been working hard, according to Niyyar, and focusing on their mission “to promote excellence in dialysis access care to improve outcomes for patients with kidney disease”. She averred that the leadership convened an in-person strategic planning retreat to review the current state of the organisation, identify opportunities for growth and capitalise on their strengths while acknowledging and addressing strategies to mitigate their weaknesses. “Our goal was, for this coming year, to identify and prioritise three to five mission-critical objectives, assign champions, give them measurable outcomes and provide them with the resources to succeed in achieving these targets,” she stated. These objectives were as follows:
• To ensure that the patient perspective is incorporated into every aspect of ASDIN’s strategy and plan.
• To focus on the individual needs and provide personalised attention to each individual category of ASDIN membership including nephrologists, interventional nephrologists, interventional radiologists, vascular surgeons, dialysis nurses, dialysis technicians, and administrators.
• To work with ADSIN’s associates to develop educational curricula with didactic and hands-on workshops for nephrology technicians and nephrology nurses, with the ultimate goal of ensuring that every dialysis unit can have ASDIN-certified expert cannulators.
• To engage with the leadership of large dialysis organisations and explore value propositions for both sides.
Once the ASDIN leadership had these goals in mind, Niyyar stated, they then “went out and did the work of ASDIN”, which she summarised in two words as collaboration and individualisation.
One thing that Niyyar ensured was highlighted early during her address was ASDIN’s work towards improving certification, in particular the work of the haemodialysis vascular access certification (HVAC) committee and the endovascular arteriovenous fistula (endoAVF) committee. “The [HVAC] committee,” she averred, “is continuing its work supporting new certification programmes,
in collaboration with International Society of Nephrology (ISN).
The outgoing president also highlighted the importance of continuing the creation and dissemination of new knowledge. ASDINs research committee had, according to Niyyar, “completely revamped the way we look at research,” stating that they “are now awarding annual US$25,000 grants for research”. The education committee had also been very active, she said, engaging with general nephrologists through the American Society of Nephrology (ASN), medicine residents through the American College of Physicians (ACP), and “reviewing multiple requests for endorsements for educational materials and meetings”.
One question that ASDIN was attempting to address was where trainees could find the necessary training that they need. “The training and workforce committee sent out an electronic survey to all ASDIN members,” said Niyyar. Based on the responses received, she stated that
industry sponsors, and that this year, ASDIN is “proud to say” that they had self-funded 20 travel grants to support fellows. Another key facet of ASDIN’s attempt to engage with new generations was the social media committee; Niyyar stated that they had “been working with the renal fellow network” on their interventional nephrology series—which are now available online—and had also collaborated with medical journals to create visual abstracts for easy dissemination to everyone with interest in interventional nephrology. “Our surgical partners have also been very active,” added Niyyar, “promoting a comprehensive holistic approach, making sure that we incorporate the surgical perspectives and engage the younger residents, not just from vascular surgery, but general surgery as well.”
streamlining the review process so it’s faster and more efficient and continuing timely processes of the multitude of applications that we receive”. Continuing, she added that “we founded the [endoAVF] committee last year, and we have certified 10 individuals so far. But as I keep emphasising, it is a living document, and as we get to version 2.0 and hopefully further, we’ll make sure that we maintain stringent quality criteria and make changes to our certification process as we evolve”. Niyyar also highlighted ASDIN’s work in improving training for both peritoneal dialysis (PD) and ultrasound. She shared that the PD committee had been focusing on identifying current training programmes and promoting more PD insertion training that would also help increase the number of patients dialysing at home, especially in light of the US Health and Human Services (HHS) initiative. Niyyar emphasised the increasing role of the USA in nephrology and highlighted the continued work of the ultrasound committee in certification in three key “nephro-centric” areas—kidneys, dialysis access and volume assessment, as well as the online library of training modules created by members of the ultrasound committee, and webinars
“If we can see how much work is being done by just 25% of ASDIN members, how about if every single one of our members was actively involved?”
they “then created a comprehensive list that’s now available on the ASDIN website, where you can get information about the centre, the number of procedures performed, the kind of procedures that are performed and—since a lot of the nephrologists are IMGs [international medical graduates]—we have information about the visa requirements, as well as the opportunities for jobs after training”.
Another key aspect of continuing to grow, according to Niyyar, is engaging the next generation of interventional nephrologists. She lauded the fact that ASDIN had 20 travel grants last year, thanks to
One final point that Niyyar wanted to address was the participation of ASDIN members. “When you look at all the work that is being done [by ASDIN], you would assume that the majority of the membership is actively involved. I was curious about this question, and when I looked at the data, I could see that only 25% of our members are involved.” She continued, asking: “If we can see how much work is being done by just 25% of ASDIN members, how about if every single one of our members was actively involved?”
Drawing the 2024 presidential address to a close, she ended by entreating the members of ASDIN to become more involved in the societies’ activities. “I really would request everyone to make sure that, if you can, please participate, because you can never underestimate the power of one. One voice can make a difference. If you are at all doubtful, I share this quote from Margaret Mead that I got from my mentor Prabir Roy-Chaudhury (University of North Carolina, Chapel Hill, USA); ‘Never doubt that a small group of thoughtful, committed citizens can change the world. Indeed, is the only thing that ever has.’ ASDIN has precedence in this area too. We have literally— both ASDIN and the field of interventional nephrology—revolutionised the way we do dialysis access in this country. Not only has ASDIN broken the glass ceiling, it has shattered it.”

6 ASDIN April 2024 – Issue11
ASDIN
Vandana Dua Niyyar giving her presidential address
New
algorithm aims to
provide clearer guidance on high AV access blood flow management
At the most recent American Society of Diagnostic and Interventional Nephrology (ASDIN) annual scientific meeting (23–25 February 2024, New Orleans, USA), Gerald Beathard (University of Texas Medical Branch, Galveston, USA) closed out the first session with a presentation titled “Inflow enigma—balloon or bowtie?”
“WE DIAGNOSED CASES WITH WHAT WE refer to as outflow stenosis,” Beathard began, “however this is actually an imbalance between the inflow and outflow.” The total outflow capacity of an access, he states, is inadequate to handle the inflow volume. This relative inadequacy of the access outflow capacity in comparison to inflow blood volume results in “increased outflow resistance and a proportional increase in intraluminal pressure”.
The point at which this occurs, however, depends on two variables, according to Beathard. “These two variables are the inflow blood flow—or Qa—and the outflow luminal diameter.” Each of these can vary considerably, he stated. “There’s a reciprocal relationship between the percent reduction in outflow luminal diameter and Qa.” This means that, as Beathard framed it, a 15% reduction in luminal diameter with a Qa of 4,000 mL/min, can cause a development of a mega-fistula and hyper pulsatility, whereas if you only have a Qa of 800mL/ min, you may have to have a 60–70% reduction in outflow luminal diameter in order to generate the same clinical picture. The adverse effects of
high access blood flow, he stated, can include eccentric ventricular hypertrophy, dilatation of heart chambers, and pulmonary hypertension. It can also cause “haemodialysis dialysis access related distal ischaemia (HAIDI), aneurysmal dilatation of the AV [arteriovenous] access, and also decrease dialysis clearance efficiency because of an increase in cardiopulmonary recirculation.”
Continuing the presentation, Beathard moved on to examine studies that have explored this topic. “Most studies that have dealt with excessive flow and flow reduction have waited until the patient is having serious problems—such as heart failure—before he is treated.” Beathard, however, feels that the basic principle of medi-
Comparing AVG materials and outcomes needs further examination with promise of new technologies on horizon
At the most recent ASDIN annual scientific meeting (23–25 February 2024, New Orleans, USA), Victoria Teodorescu (Emory School of Medicine, Atlanta, USA) gave a presentation as part of the “Cut, Suture, and Action in ASDINville” session, in which she explored the various options for materials used in arteriovenous grafts (AVGs) and the comparative outcomes of each of these options.
BEGINNING HER PRESENTATION, SHE OUTLINED the main features of polytetrafluoroethylene (PTFE) grafts, stating that PTFE is a “ubiquitous material” used for dialysis access grafts, and that there have been some variations developed, with “one of the first [variations] being tapered, where the graft goes from four to seven millimetres [with the] smaller end at the artery”. The aim of this, she averred, is to reduce the incidence of steal. However, citing a meta-analysis of five studies, she stated that over 4,000 patients showed “no differ-
ence in steal, no difference in either primary or secondary patency, or in the infection rate”. Despite this, the authors did send a “word of caution”, stating that this was a relatively small number of studies, despite the large number of patients, and that “there was limited stratification of outcomes”. Symptomatic steal, Teodorescu stated, occurs in a “very, very small number” of patients and this may explain the authors’ caution.
Continuing, Teodorescu moved on to examining heparin-bonded grafts. “[Heparin-bonded grafts] sound enticing [as an option to] reduce the episodes of thrombosis,” she postulated, but stated that, despite appearances, in a prospective randomised trial of 160 grafts, whilst there was a small amount of improved patency early on in the heparin-bonded grafts compared to standard grafts, in the later period of time, there was no difference between the two.
One option that Teodorescu appeared to be in favour of was “quick-stick” grafts. She stated that she feels that these grafts could be “an advantage”. On average,
cine is to treat things before the disease happens, taking a “prophylactic approach,” which he stated is “something that we should consider in these cases”.
With that in mind, Beathard stated that he thinks that it is “critically important” that access flow measurement be a part of the evaluation of all of these cases, prior to planning treatment, and then, using this information, a bimodal approach be taken; angioplasty for cases with a low or normal Qa, and flow reduction as primary treatment for cases with an elevated Qa.
In order to better manage the issues that arise from high access blood flow, Beathard, along with colleagues from various centres, have developed an algorithm that will help to simplify the decision process of which modality to use when managing this issue in AV access. “We developed [this algorithm],” he stated, “so that if you take major flow, access flow that it is in the 800 and 1500 mL/min range, management should be individualised based upon individual patients, comorbidities and situation. If it’s 800 mL/min or less, then [use] angioplasty.” If that is successful, he adds, blood flow after angioplasty should be measured to see if flow reduction is needed as a secondary procedure. This algorithm, which he presented at the 2024 ASDIN annual scientific meeting, is pending publication in the Journal of Vascular Access
Teodorescu stated, “for the quick-stick graft compared to almost one procedure for the standard graft over the same period of time, there was, as expected, no difference in steal,” but that the big advantage to these grafts is a shorter time to cannulation. Quick-stick grafts, on average, took six days to cannulate, whereas the standard graft took almost a month. Of course, what goes along with this, she adds, is “less catheter-related complications”. However, she added that there are recently published case reports that show that these grafts can de-laminate.
Drawing her presentation to a close, Teodorescu moved on to discussing bovine carotid artery grafts. “These,” she averred, “have been introduced a while back, and initially, there were very good reports of both assisted and secondary patency.” A larger study that she used as an example, as she framed it, negated the good results of primary patency, as it only had 32% at a year, but there was a very good secondary patency of 78%.
In her conclusion, Teodorescu stated that there are several conduits available to create access, although the options are “dependent on patient characteristics”. Adding her final thoughts, she stated that she was “wondering whether, with the new advent of technology coming—especially bioengineered grafts—if we’ll be able to say something different over time”.
7 April 2024 – Issue 11 ASDIN ASDIN
Beathard et al's new alogrythm Critical inflow-outflow imbalance Measure access blood flow (Qa) Clinical judgement > 800– <1500 PTA-primary Qa – <800mL/min Flow reduction– primary Qa – >1500mL/min Routine follow-up Stent-graft or Surgical intervention Measure access blood flow (Qa) Flow reduction Target 800 to 1000mL/min Qa >1500mL/min No No Yes Yes Success
CX 2024 promises “not
only the complex, new, innovative, but also the everyday”
in vascular access and renal interventions
With the 2024 Charing Cross Symposium (23–25 April, London, UK) rapidly approaching, Renal Interventions spoke to Nicholas Inston (University Hospitals Birmingham, Birmingham, UK) and Kate Steiner (East and North Herts NHS Trust, Stevenage, UK) about the Vascular Access Masterclass, what they feel the highlights are, and which controversial topics will be addressed.
One thing that both Inston and Steiner made sure to highlight was the fact that the programme this year will be heavily focussed on controversies, and the fact that the issues that arise in vascular access do so on a global scale. When speaking on what she felt merited close attention, one of the first things that Steiner spoke of was the Great Debate, which will be taking place on Tuesday morning. The motion—endovascular arteriovenous fistulas (endoAVFs) are a failed experiment—will be hosted by Inston and moderated by Narayan Karunanithy (Guy’s and St Thomas’ NHS Trust, London, UK), and is a debate that Steiner says she is sure “will be controversial”. She also said that, whilst she is “very much against the motion”, she feels that it will “be really interesting to see if that changes at the end of the debate”.
Steiner is not alone in her belief that this will be a programme highlight, as Inston also highlighted the importance of addressing endoAVFs and their role in vascular access. “This technology has been around for about 10 years,” Inston averred, “first in an experimental setting, but now, fully into the clinical arena”. According to Inston, however, the issue arises from the fact that “we don’t really know yet where we should be using these fistulas. Should these be for everybody? Should these be for a select few? Should there be actually certain indications in certain patients? Or actually, are we not using them in a wide enough application?” This will be the focus of the Great Debate, with input from, as Inston puts it, “the experts who’ve done some of the highest volumes of these cases in the world”.
Another feature of the programme that both Steiner and Inston highlighted was the focus on drug-coated balloons (DCBs). Whilst addressing how variations in reimbursement can lead to differences in standard of care on a global level, Steiner referred to DCBs, stating that “in the UK, these drug-coated technologies are reimbursed via high-cost device tariff. This doesn’t happen globally, and they can therefore add a significant expense to a procedure, which is then reimbursed, and the reimbursement may not be reflected in the tariff for that procedure. So again, we see this can create differences in pathways and can lead to inequalities in care globally”. The afternoon of day one will give several opportunities to address these drugcoated technologies, with a session addressing whether or not we know which DCB to use and the ABISS trial, as well as a podium-first


session dedicated solely to the topic of which DCB to use.
Addressing the same topic, Inston stated that “one of the approaches to managing stenoses in vascular access historically has been a mechanical approach—that’s your balloons and, over the last few years in peripheral vascular disease and in vascular access, using pharmacological appli-
Case study
cations [that] have also come into our armamentarium”. What he means by that, Inston expands, is that “drug eluting or drug-coated balloons are now commonplace,” despite the fact that “there’s been a lot of controversy about these”. Inston added that “there’s been some number of studies on these, [but] the results are not exactly consistent, and what we want to do is actually try and pick this apart and try and look at what information, what data we can use from that to apply to a patient population, to be able to use these things in an appropriate fashion.”
Another aspect of the programme that Inston highlighted was the fact that it is not just vascular access that will be the topic of discussion, but also renal interventions. “This session is not just about vascular access,” Inston stated. “This is also about management of the patient with renal failure. And for a lot of us who do intervention and surgery, we will be presented with patients with kidney problems, particularly in the vasculature, and this might include nutcracker syndrome, this might include renal arteries, but also the issue of renal denervation, particularly for hypertension, is coming back into the clinical arena. We’re
CX 2024 vascular access masterclass to feature realworld case studies for audience debate Come
A key feature of the Vascular Access and Renal Interventions programme for this year’s Charing Cross (CX) International Symposium are the case studies that will be presented for the audience to discuss, debate, and decide on the best course of action throughout the duration of the event.
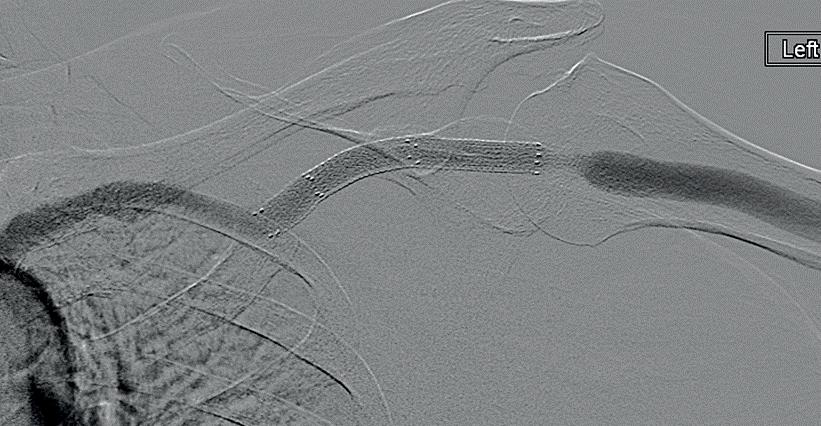
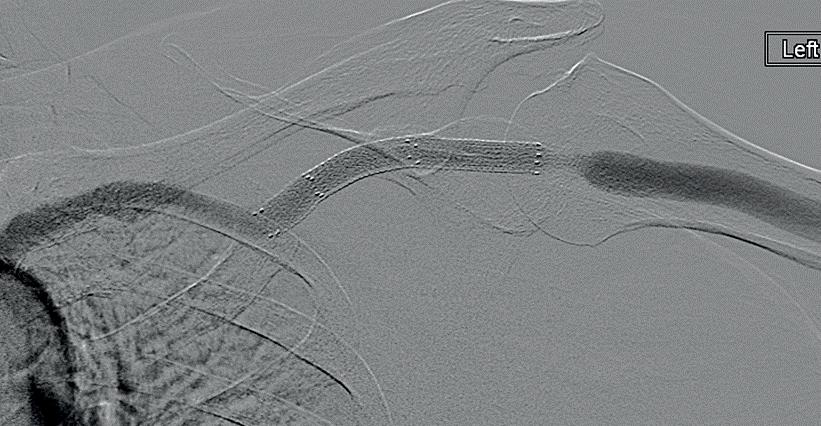
Starting at 10:30 on day one of the CX International Symposium (23 April 2024), the session will be chaired by Nicholas Inston (University Hospitals Birmingham, Birmingham UK), and will feature several case studies, which the audience will then be asked to pitch what they feel is the most suitable treatment for each example. A second session by the same name, chaired by Kate Steiner (East and North Herts NHS Trust, Stevenage, UK) will take place at 16:10 later the same day. As a taster of what can be expected, we have included a case study below, featuring all of the information that will be provided to the audience to allow them to make a well-informed decision.
What would you do for this 57-year-old woman with a left brachiocephalic arteriovenous fistula?
Six weeks prior to this venogram, she had had recurrent cephalic arch stenoses treated with balloon angioplasty, and on the last intervention, the lesion lateral to stent graft had some recoil during balloon angioplasty. She is having dialysis for four hours, three
April 2024 – Issue 11 8 Charing Cross Symposium CX Preview
Kate Steiner
Nicholas Inston
us
next
to the vascular access masterclass and tell
what you would do
Image proved by Nicholas Inston with the patient's consent
going to discuss all of these things and present the cutting-edge up-to-date research on this.”
Another aspect of the programme that is vital, Inston stated, is making sure to address “not only the complex, the new, the innovative, but also the everyday”. To do so, there is a session in which Inston will be presenting cases to international experts and asking them “what would you do?” According to Inston, the panel of global experts “don’t know about these cases yet, but they’re going to have to be on the spot, tell us what they would do and, in fact, debate with their colleagues on stage and with you in the audience as to whether they do it right or they do it wrong”.
Steiner also made sure to highlight the wider coverage of the programme: “The other sessions that we have which are going to be great are the case presentations and discussions in the presentation zone that will be a really good opportunity for people to, in a smaller forum, ask the experts, and we’ve got a really good programme for that.” As well as this, she also put focus onto a workshop examining the maturation of surgical and endoAVFs, with vascular access nurses, sonographers, and patients present for the hands-on workshop.
Both Inston and Steiner were clear that controversies take centre stage in this year’s vascular access and renal interventions programme; with a great debate on whether endoAVFs were a “failed experiment” or not, examinations of global discrepancies in treatments, and debates on the best course of action for specific cases, it is sure to be, as Inston put it, a “really strong” programme with “some big highlights”.
Highlights of Vascular Access and Renal Interventions Masterclass programme
As well as the programme features mentioned above by Nicholas Inston (Birmingham, UK) and Kate Steiner (Stevenage, UK), there is a wide range of highlights to the Vascular Access and Renal Interventions Masterclass programme that you should be sure to catch at this year’s Charing Cross (CX) International Symposium (London, UK).
One of the key features of this year’s focus on controversies will be the Great Debate, which will be discussing the motion that Endovascular AVFs are a failed experiment. Anchored by Inston and moderated by Narayan Karunanithy (London, UK), this will be taking place at 09:10 on day one of CX (Tuesday 23 April).
As well as this, there will also be a roundtable that will bring together experts from around the globe to discuss international approaches to vascular problems and how that can impact on both the exciting to the everyday. Also moderated by Inston, who will be joined by panel of experts inlcuding Robert Shahverdyan (Hamburg, Germany), Robert Jones (Birmingham, UK), Shannon Thomas (Sydney, Australia), Raphael Coscas (Paris, France), and Maarten Snoeijs (Maastricht, Netherlands), this will be held at 14:50 on day one of the symposium. There will also be a podium first presentation of the five-year outcomes of IN.PACT AV Access trial, given by Andrew Holden (Auckland, New Zealand) at 12:30 on day one of the symposium, a presentation addressing whether nutcracker syndrome is real or not from Paul Crowe (Birmingham, UK) that will kick off a series of presentations on the syndrome in the afternoon of day one, an examination of the current approaches to treating renal artery aneurysms from Robert Morgan (London, UK), and much more.
To see the full programme for the Vascular Access and Renal Interventions Masterclass, visit cxsymposium.com/cx-events-2024.


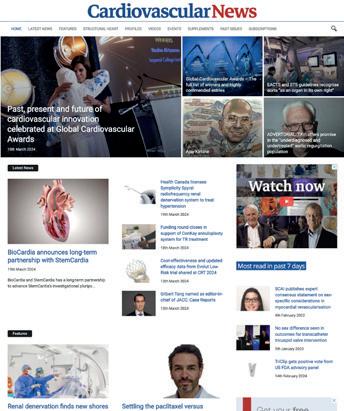
9 April 2024 – Issue 11 Charing Cross Symposium *Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the cardiovascular field Editorially independent Available in print and digital formats and through our social channels Visit cardiovascularnews.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** Subscribe today CX Preview
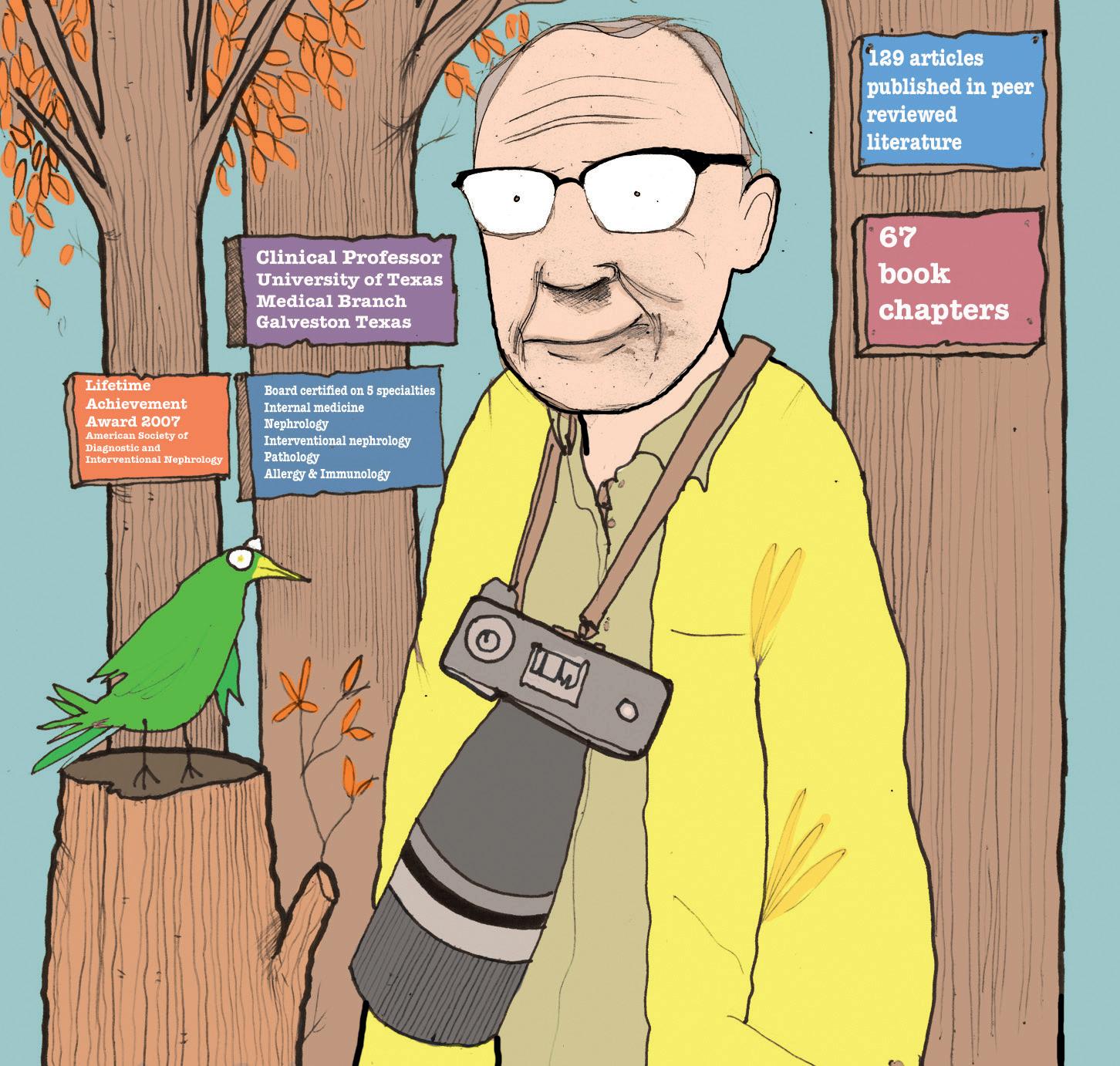
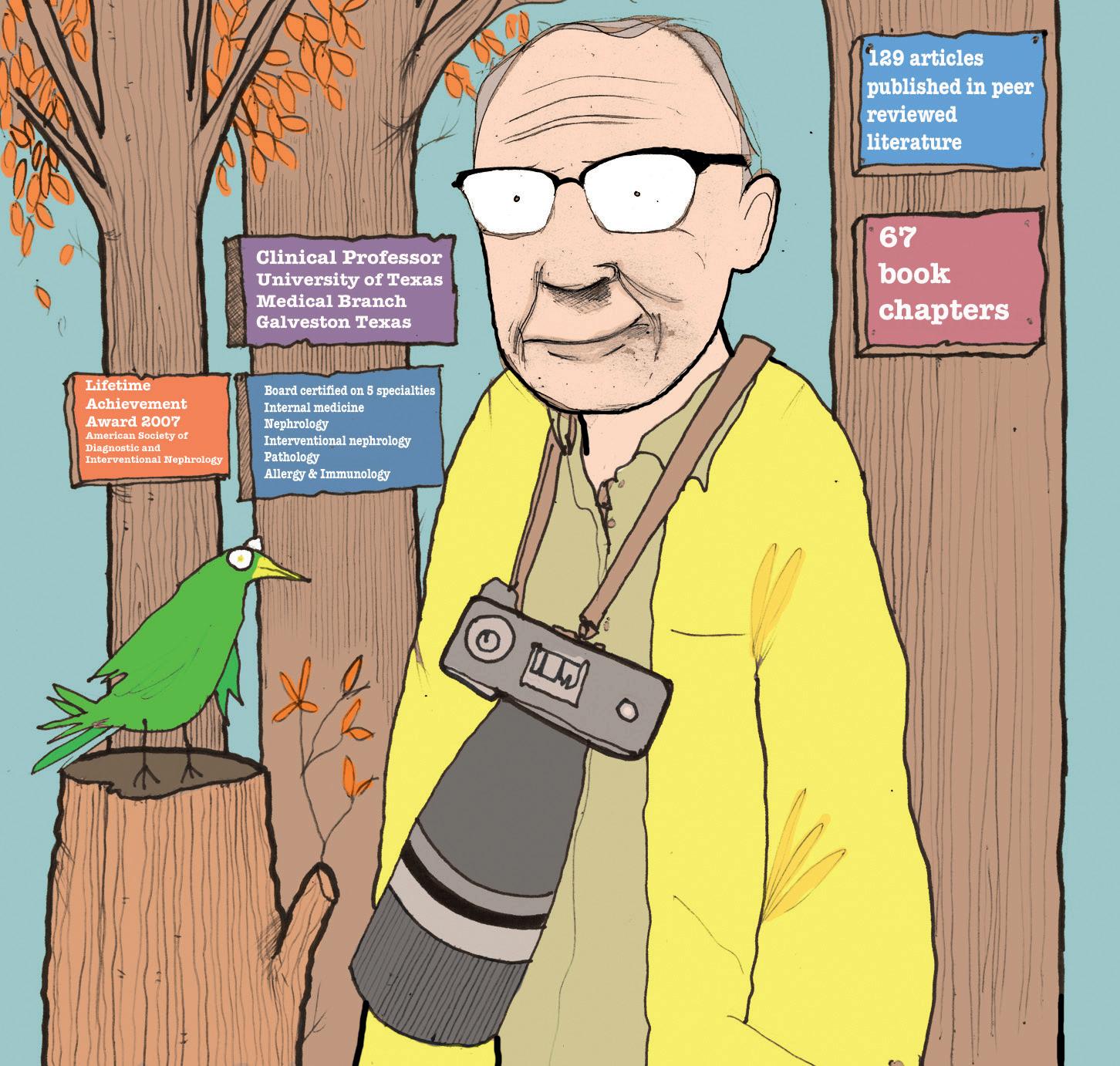
Gerald Beathard
With a career spanning 60 years, a passion for music and photography, and a wealth of experience in teaching and leading the future clinicians of his field, clinical professor at University of Texas Medical Branch (Galveston, USA) Gerald Beathard speaks to Renal Interventions about his career in interventional nephrology (IN), those that helped him at the beginning of his career and what he feels the future of IN should look like.
What drew you to a career in IN? I more or less eased into it over time. I didn’t really think that I was going to engage in a career in IN, but in taking care of dialysis patients in the late 1970s, I was encountering patients who had problems with their vascular access, and nobody seemed to understand what the problem was. This also meant that no one was really addressing it directly. If a patient had a problem with their vascular access, the general approach was that the surgeon would revise it or create a new access.
However, in the 1980s, there was an article published that discussed doing balloon angioplasty on venous structures; prior to that, balloon angioplasty had only been on arteries. It reported angioplasty results on venous structures—some of which were dialysis access—which piqued my interest. I said “that maybe something like that can be done”, and from that I decided that I would start doing angiograms on our patients, by taking regular X-rays of patients with contrast injections, with the needles in place.
Around this time, a cardiologist joined our clinic who was willing to help me start doing dialysis access angioplasties. He called me one day and said that he was going to an arterial angioplasty course and asked if I would like to go. The one-day course consisted primarily of lectures, with a live video demonstrating the technique at the end of the course. Everyone was given a certificate that said we were now qualified to do femoral artery angioplasties. I’d never done one, but I had a certificate that said I was qualified to do it. I came back and applied to the credentials committee to start performing angioplasties on dialysis access, with this cardiologist as my proctor. He showed up for the first case and stayed for a few minutes, and that’s the last time I saw him. After that, I started treating venous outflow stenosis with angioplasty on a regular basis.
Did you have any mentors that helped you during your career?
Early on, the only people that I could say served as mentors were the radiology technologists who worked in interventional radiology where I was doing cases. There was no one that I could turn to that had any experience in handling these kinds of cases. The radiology technologists would tell me what the interventional radiologists were doing, what kind of balloons and guidewires they were using. Along with their guidance, it was more or less trial and error. I did make a few mistakes—nothing major—but I collected data on every case that I did. I also attended a one-day course on dialysis access thrombectomy, after which I started doing thrombectomies.
In Texas, we had a small, informal association of nephrologists, which paid a small fee for Allen Hull (Dallas, Texas) to serve as a lobbyist in Washington, and to represent us in issues involving the Centers for Medicare & Medicaid Services (CMS). At one point, I received a bulk mail-out from CMS implying that they would not pay for venous angioplasty on dialysis access. I contacted Hull regarding this, and he told me that he wasn’t familiar with the procedures that I was doing on dialysis access and that he would check with some associates and get back to me. He later said that those he had spoken to were not familiar with what I was doing and were sceptical as to its value, despite what I had found. He replied that I needed to write a paper reporting my results, providing evidence of its value. Using the data I had collected, I wrote a paper reporting on about 300 cases, and continued performing dialysis access procedures with no reimbursement issues.
What do you think is the most important thing to develop for the next 10 years of IN? I think that we’ve gone through a time where freestanding access centres, being operated by nephrologists, have been very important and extremely valuable to patient care. However, reimbursement has gotten to the point where many of these centres are not financially viable. It
seems that IN is being forced to move into ambulatory surgical centres and hospitals. With this change, I think that the efficiency with which nephrologists were able to do these procedures is suffering. In the freestanding extension of office model, it was not unusual to see a nephrologist do 10–12 cases a day. Working in a hospital, it’s only possible to do less than half of that number. With reimbursement as it is, I think that it’s getting to the point where it’s financially difficult for a nephrologist to practice IN.
I feel that, going forward, we need to develop dedicated centres that can offer the full spectrum of services needed for dialysis access management. With this, we need to have practitioners—not nephrologists necessarily—that can offer the complete range of what is needed for vascular access care in a dialysis centre, ranging from ultrasound evaluation all the way up through surgery. Some centres offer that now; in some instances, this is a single physician, and in others, there are several practitioners—some of them nephrologists, some are surgeons, and some of them are interventional radiologists. I think the future of vascular access is moving in that direction.
You have been referred to as one of the “founding fathers” of ASDIN. What do you think have been some of the bigger achievements as a society?
One of our big achievements is the high quality of interactive meetings that we have recently had (23–25 February 2024, New Orleans, USA) as a society, that has actually become multidisciplinary. When we first started, our meetings were relatively small, and we generally had them in conjunction with either the American Society of Nephrology or the American Kidney Foundation, discussing subjects that were really very basic. Today, we have much more complicated issues being discussed and, crucially, our meetings have become multidisciplinary. If you look at the speaker agenda from our recent annual meeting, we had radiologists, surgeons, and interventional nephrologists on the schedule, as well as nephrologists. We have also expanded so that we have nurses and an associates meeting, for practitioners who are vital to the care of dialysis patients. I think that this type of meeting has been, in my mind, a major accomplishment. Much of this can be attributed to our executive secretary, Mary Lea Nations, who has really done a Herculean job.
The other major issue is the offering of a specialty certification. We have not been able to get the American Board of Medical Specialities to offer certification for IN because they say that the numbers are not large enough to make it financially feasible. However, it’s often essential for a physician to have some type of certification in order to get the necessary practice credentials. The society has developed a robust certification and recertification system to offer this type of recognition.
What advice would you give someone looking to move into the field of IN?
They need to be associated with a programme that is offering this training at a high level of clinical expertise. Unfortunately, there are only a few IN training programmes available. They also need to have a good general nephrology training programme, because most interventional nephrologists also practise a significant amount of general nephrology as well. Radiologists and surgeons also need to have training from someone that can give them the type of insights that they need to understand dialysis, the literature,
Fact file
Current appointment:
Clinical professor, University of Texas Medical Branch, Galveston, USA
Education:
1960–64: Medical School: University of Texas Medical Branch, Galveston, USA
1964–65: Internship: University of Texas Medical Branch, Galveston, USA
Honours (selected):
1986: Physician of the Year 1986, Austin Diagnostic Clinic, Austin, Texas
1993: Brackenridge Hospital, Austin Texas Physician Of The Year Award
2007: American Society of Diagnostic and Interventional Nephrology Lifetime Achievement Award
2008: Establishment of Gerald Beathard Excellence in Academic Achievement Award
2008: Establishment of Gerald Beathard Lectureship
2016: University of Texas Medical Branch Ashbel Smith Distinguished Allumnus Award
2021: Establishment Gerald Beathard Outstanding Nephrology Fellow, Award
Profile 10 April 2024 – Issue 11
Illustration by: Andy Watt / NB Illustration
Q&A
and also how to do these procedures appropriately. If you take something as simple as putting in a dialysis catheter, there are certain things that are not immediately obvious that need to be followed to do it appropriately. A surgeon or radiologist who just has basic training in their specialty is not going to be able to offer the high level of dialysis access management that the patient deserves.
How significant do you think that the patient experience should be in the future of IN? I think the patient’s perspective is very important, and I think that it starts with making strong patient relationships. One of the things that’s happened in the past, that I’m afraid is going to be less of a feature going forward, is many of the interventional nephrologists have been doing procedures on the patients of their practice that they also see in their offices and in the dialysis unit. They have developed a close relationship with these patients. I think having that relationship, where the patient can have a sense of confidence in them as their physician, is extremely important. It’s important to really know the patient, to know things about the
“I think the patient’s perspective is very important, and I think that it starts with making strong patient relationships.”
patient that may not be obvious, and things about their family and social situation. These things can have a significant effect on the patient’s quality of life. Many of the procedures that are performed are for problems that tend to be recurrent. You hope that it’s going to be quite some time in the future, but you’re probably going to see that patient again. I think that if the patient has one bad experience, it’s going to have a very
unfavourable effect on the relationship between the physician and the patient. Unfortunately, it is also going to bleed over into other patients, because the patients in the dialysis unit tend to talk to other patients. I think having a very positive patient-physician relationship is critically important.
What are your interests outside of medicine?
I do a lot of medical writing, but I’m also very interested in outdoor and wildlife photography. I worked for a group called Lifeline—a subsidiary of DaVita—for almost 20 years, developing freestanding access centres around the country. Eventually, we had 78 centres, most of which were decorated with my photographs that I had printed, framed and hung myself. I like to cook and have attended cooking schools in China, Greece, Italy, and Portugal, as well as the USA. I also have a passion for music; I sing in a church choir, and was privileged to sing at both President and Barbara Bush’s funerals because they were held at the church I attend in Houston. That was quite an experience. I’ve also written and published more than 100 Southern Gospel songs.
Profile 11 April 2024 – Issue 11
ASDIN
American Society of Nephrology and Home Dialysis University expand collaboration to enhance home therapies education for nephrology fellows
THE AMERICAN SOCIETY OF NEPHROLOGY (ASN) and Home Dialysis University (HDU) launched a collaboration in 2023 to improve nephrology trainees’ knowledge, proficiency, and exposure to home dialysis therapies. Through the collaboration, ASN provided scholarships to 30 fellows to attend an in-person HDU fellows training course and participate in a virtual longitudinal case-based education series led by renowned experts in peritoneal and home haemodialysis. A recent press release notes that, after a successful first year, ASN and HDU will continue the scholarship programme this year, awarding 45 fellows the opportunity to participate.
ACCORDING TO DATA SHARED IN the ASN press release, home dialysis has been associated with lower cost and equal or better clinical outcomes than facility-based dialysis. In 2021, only 14.1% of Medicare patients receiving dialysis underwent dialysis at home. Despite the higher incidence and prevalence of kidney diseases in Black and Hispanic people when compared to non-Hispanic White people, Black and Hispanic people with kidney diseases are even less likely to be treated with home dialysis.
“The ASN HDU scholarship programme, now in its second year, continues to affirm ASN’s commitment to improving access to home dialysis for all individuals with kidney diseases. Improving education and exposure to home dialysis among nephrology fellows will pave the way for a future kidney medicine workforce to ensure universal access to home dialysis and improve the care of people on dialysis,” said Deidra C Crews, ASN president. Nephrology fellows have long cited a lack of education and exposure to home haemodialysis and peritoneal dialysis during training as a major educational gap, the ASN states. The ASN Task Force on the Future of Nephrology recommends providing additional education to close currently identified gaps in nephrology
ASDIN programme chair highlights the dos and don’ts of vascular access, the importance of home haemodialysis, and new data on the cost of catheters
Dalia Dawoud (Nephrology Associates Medical Group, Azura Vascular Care, Riverside, USA)—the programme chair of the most recent American Society of Diagnostic and Interventional Nephrology (ASDIN) annual scientific meeting (23–25 February 2024, New Orleans, USA)—sat down with Renal Interventions to discuss what she felt were some of the key highlights of the meeting, including the important role that home haemodialysis (HH) plays, new data that have come to light regarding the costs of catheterisation and catheter-related bacteraemia, and what she refers to as the “dos and don’ts” of preservation of vascular access.
RI: For the first time in the history of ASDIN, you have had a whole session dedicated to home haemodialysis. Why is this important, and what are the key strands for people to think about?
Dalia Dawoud: Medicaid and Medicare funding for dialysis has significantly increased, emphasising the importance of delivering a high quality of care that is also cost-effective. HH has emerged as a pivotal focus, consistently showing its cost-effectiveness and positive impact on patient outcomes compared to traditional in-centre haemodialysis.
A significant aspect highlighted in the session was the optimisation of vascular access care for HH. The conventional “fistula first, catheter last” approach can limit access to HH for patients who do not fit the standard criteria for optimal access. This rigid approach fails to
consider the individualised cinical needs of each patient. The session also emphasised the importance of customising care to meet the specific needs of each patient. This involves considering factors like age, multiple comorbidities, shortterm life expectancy, challenging vasculature, and patient preferences. It was stressed that every patient should have the chance to explore HH, even if it means departing from conventional methods.
The key message was unmistakable: Healthcare providers must not accept “no” as the final answer, and they should overcome any obstacles to deliver the highest quality, individualised care when transitioning patients to HH. This approach not only improves patient outcomes and quality of life but also ensures a more effective allocation of healthcare resources.
RI: What can you tell us about the new data
training, establishing individualised pathways to provide opportunities for fellows to explore advanced specialised care and other career goals in more depth, and prioritising diversity, equity, and inclusion as well as promoting healthcare justice in all aspects of nephrology, especially fellowship training.
“I was not comfortable with managing home dialysis patients the way I was with inpatient dialysis,” said 2023 scholarship programme participant Fatima Ayub, University of Arkansas (Fayetteville, USA) for medical sciences and central Arkansas veterans' healthcare system. “The HDU scholarship programme has cleared up a lot of concepts for me and enabled me to be more confident while managing these patients. I am now routinely seeing these patients in our home therapy clinics, implementing all the knowledge I am receiving from our faculty at HDU.”

regarding the costs of catheters?
Dalia Dawoud: For many years, there has been a strong initiative advocating for arteriovenous fistulas (AVFs) as the primary choice for optimal access. This stems from concerns about the substantial costs and poor outcomes associated with catheter-related bloodstream infections, which have led to the perception that catheters are less desirable for this purpose.

“We have to tailor the care of the patient to their individual clinical needs.”
However, recent data suggest that catheters have the lowest access-related costs compared to both endovascular and open AVF interventions, particularly when considering all associated costs with maturation procedures and interventions needed to manage failure of AVFs. It’s important to note that only about 60% of AVFs mature, and approximately a third of all fistulas created require intervention to meet maturation criteria and be suitable for cannulation.
Therefore, while my presentation does not endorse catheters, it emphasises the need for tailored patient care based on individual clinical requirements rather than solely on cost considerations or reported data.
RI : Can you summarise the essence of the dos and don’ts of preservation of vascular access?
Dalia Dawoud: During the session, a key focus was the ethical responsibility of vascular access care providers in distinguishing between routine follow-up appointments that may be unnecessary and the critical, ongoing care required to maintain vascular access. This approach seeks to ensure the highest level of patient care while efficiently managing resources. This topic resonated strongly with the audience, highlighting the importance of managing this balance effectively to avoid compliance issues and ensure optimal patient outcomes.
12 April 2024 – Issue 11 Home Haemodialysis
Dalia Dawoud
This advertorial is sponsored by Laminate Medical Technologies
Physicians
around the world
agree: VasQ is revolutionising AVF outcomes
In medicine, the pursuit of better patient outcomes fuels the quest for innovation. Haemodialysis patients and vascular surgeons seeking consistent, patent vascular access have been discouraged by standard, unsupported arteriovenous fistulas (AVF) functional success rates ranging from 40–72% as reported in landmark studies over the years.1-8 These consistently high rates of failures were assumed to be a natural ceiling to functional success rooted in unavoidable mechanical and haemodynamic factors that arise when you arterialise a vein and lead to poor maturation.
In response, Laminate Medical Technologies created a new device concept by which the surgeon can structurally reinforce the outflow vein using an external vascular support and guide its maturation in a more mechanically and haemodynamically stable configuration. That device, called VasQ™ External Support, was designed specifically to address these two factors of arteriovenous fistula failure that have plagued vascular access surgeons for decades. VasQ is a laser-cut nitinol brace that sits on the artery and sets the angle as well as the baseline diameter of the vein at the level of the anastomosis. The remaining ~2.5 cm of vein is surrounded by a flexible woven nitinol brace that diametrically tapers outward, facilitating a gradual transition of a flow with a more laminar profile through the juxta-anastomotic segment to the outflow vein. To date, this structural reinforcement that guides a more optimal venous remodelling has led to functional success rates randgin between 88–100% across nine studies as well as potential long-term benefits surgical fistula outcomes by providing permanent reinforcement to the artery-vein connection.8-16
Here, five surgeons from across the world who have recently integrated VasQ into their practices offer their unique perspectives—Ari Kramer (Spartanburg Medical Center, Orangeburg, USA), George Blessios (Blessios Medical, New York, USA), Paul Gibbs (Queen Alexander Hospital, Portsmouth, UK), and Yong Enming and Zhang Li (both Tan Tock Seng Hospital, Novena, Singapore). Many medical devices show promising clinical data but can fall short in real-world cases. However, following nearly a decade of work, leading surgeons from across the world agree, VasQ’s clinical data is overwhelmingly positive and adoption of VasQ has helped to consistently improve outcomes as promised, positioning VasQ as a device with the potential to reshape the standard of care for haemodialysis patients worldwide.
Kramer
“As the director and principal surgeon of Vascular Access Surgery at Spartanburg Regional Hospital, I was thrilled to be the first in the USA
to implement VasQ after it was granted US Food and Drug Administration (FDA) de novo status, marking an exciting opportunity for patients seeking improved outcomes from surgical fistulas. Faced with the limitations of traditional methods, especially their disappointing maturation rates and particularly at the wrist, VasQ stood out as an innovative, low-risk solution promising to give my patients the best chance for a usable fistula without as many additional procedures. The transition to this technique was smooth, and its initial performance not only met but exceeded our high expectations, reflecting the device's impressive clinical data. With VasQ, I’ve observed significant improvements in my fistula maturation rates without any complications or patient complaints, signalling a transformative advancement in our practice and a leap forward for patient care.”
Blessios
“When I first heard about VasQ, I was sceptical it would improve my outcomes. I have observed how strict patient selection based on arterial diameter and flow as well as an aggressive follow-up protocol can yield high rates of functional success but was curious if the device had the potential to standardise my surgical technique.17,18 The VasQ US Pivotal Study also interested me in the device’s potential to prevent longer term complications like aneurysm formation. In my first cases at Kaleida Health in Buffalo, USA, I could clearly see and feel the
“The externally supported fistulas simply felt better and gave me more confidence in their potential for success with a reduced need for secondary procedures.”
George Blessios
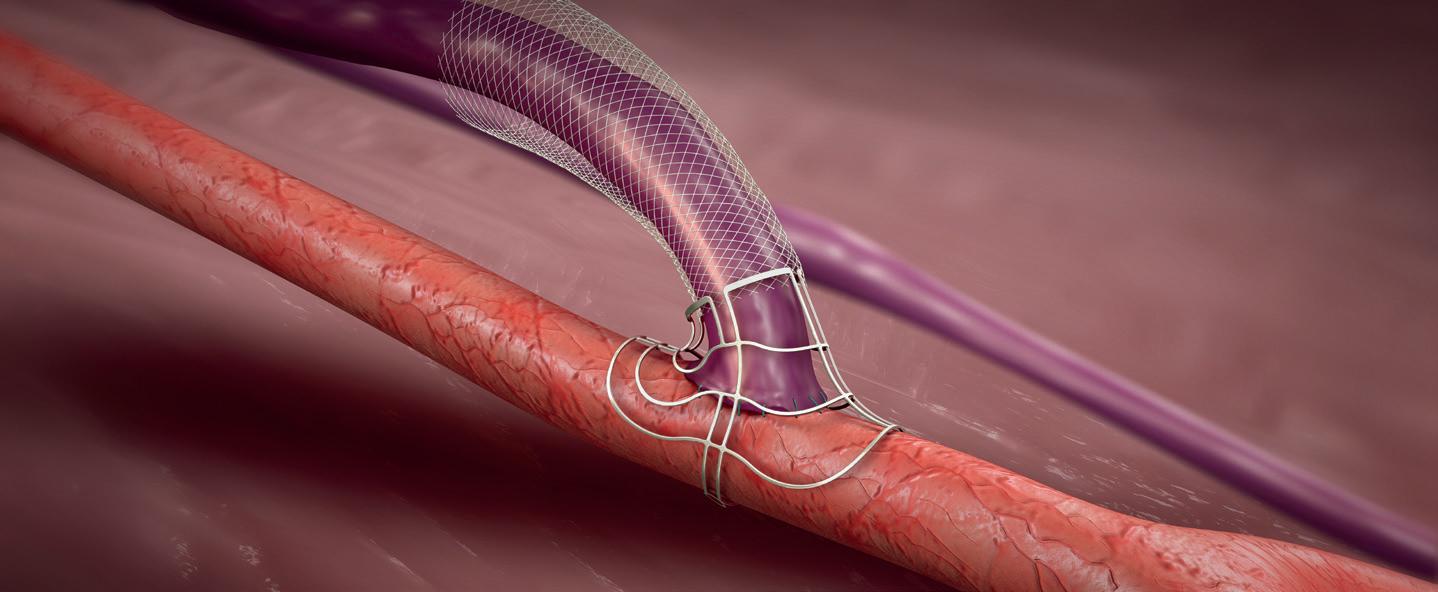
difference with VasQ in place. The externally supported fistulas simply felt better and gave me more confidence in their potential for success with a reduced need for secondary procedures. I am still in the early stages of assessing this technology, but so far the results tell me that this device will likely be the standard for my fistula creations going forward.”
Gibbs





“I became interested in VasQ when I saw the outcome improvements being reported from a variety of vascular access experts at meetings like the Charing Cross (CX) Symposium and Vascular Access Society (VAS) annual congress. As the lead surgeon for vascular access surgery at Portsmouth Hospital, I see many high-risk patients with low probability of fistula success. Having incorporated VasQ into my practice, I would say it has led to more consistency in fistula creation and improved outcomes for my patient population, even when implanted by less experienced surgeons in my centre. Traditionally high-risk patients now have a fighting chance at a sustained, well-functioning fistula with VasQ in place—it’s a game changer for the vascular access community!”
Yong & Zhang
“Our hospital, Tan Tock Seng, has been a pioneer of the VasQ device in Singapore and among the first to implant the device in the country. My colleagues and my interest in VasQ stemmed from its engineering and how it was designed to impact the haemodynamic of the fistula. Our initial results are promising in an Asian population with smaller vessel diameter, with no primary failures or infections so far, and a mean time to cannulation of 68 days. Additionally, all fistulas were considered radiologically mature at one month with only 20% requiring balloon assisted maturation compared to a baseline of 30–40% of fistulas requiring balloon assisted maturation. Implanting VasQ to support our fistulas has helped to reduce the need for balloon assisted maturation in our practice whilst reducing the rate of primary failures.”
VasQ represents more than just a medical device—it embodies a promise of hope and progress for dialysis patients worldwide and the vascular surgeons, nephrologists, and other integral healthcare workers who strive to provide the best possible care to end-stage renal disease (ESRD) patients. With its innovative design and proven efficacy, VasQ stands as a testament to the power of innovation in medicine, offering a glimpse into a future where improved patient outcomes and enhanced surgical techniques are not just aspirations, but tangible realities.
*VasQ is intended for use as an external support for upper extremity arteriovenous fistulas created for vascular access by means of vascular surgery.
References
1. Dember et al JAMA. 2008;299(18):2164-2171
2. Huijbregts et al Clin J Am Soc Nephrol. 2008; 3:14-719
3. Masengu A, et al. Clin Kidney J. 2016 Feb;9(1):142-7
4. Allon et al. Am J Kidney Dis. 2018;71(5):677-689
5. Irish et al. JAMA Intern Med. 2017;177(2):184-193
6. Bleyer et al. J Vasc Surg. 2019; 69:507-15
7. Peden et al. J Vasc Access. 2022 Mar;23(2):265-274.
8. Karydis et al. Am J Kidney Dis. 2019;75(1):45-53
9. Chemla et al. J Vasc


13 April 2024 – Issue 11 Advertorial
Access. 2016; 17(3):243-248
Shahverdyan et al. Semin Dial. 2023;36(2):147-154. 11. Leonardi et al. J Vasc Access. 2021 Jul;22(4):658-665. 12. Publications in progress. Data on file with Laminate. 13. Swiecka, Zippel, Storck GMS 2021 14. Shahverdyan et al. J Vasc Surg. 2022 Jan;75(1):248-254 15. Karydis, Mallios, Mestres, Matoussevitch VAS 2021 16. Dillavou, Ozaki, Hentschel, Lucas VEITH 2021 17. Blessios et al. J Vasc Access. 2020 Jul;21(4):434-439. 18. Blessios et al. J Vasc Access. 2016 Mar-Apr;17(2):124-30
10.
Enming Yong
Paul Gibbs
Li Zhang
George Blessios
Ari Kramer
Laminate
Vascular external support system use found to boost key functional outcomes for surgical arteriovenous fistula creation
Alik Farber (Boston University, Boston, USA) presented the results of a multicentre US study at the 2024 Society for Clinical Vascular Surgery (SCVS) annual meeting (16–20 March, Scottsdale, USA) that shows creating arteriovenous fistulas (AVFs) with a vascular external support system, VasQ (Laminate Medical), decreases the median time to achieve two-needle cannulation by reducing the need to perform maturation procedures.
THE STUDY SET OUT TO ASSESS THE functional outcomes of fistulas created with an external vascular support device as compared with rigorously matched controls of unsupported fistulas for end-stage kidney disease (ESKD) patients by the same surgeons.
Farber focuses on the unreliable trajectory of unsupported fistula functional success that surgeons grapple with: “[AVFs], when they work, are much more durable and much better for patients [than central venous catheters or arteriovenous grafts],” he said. “But to work, they require maturation, which means that the vein that is plugged into the artery needs to grow in diameter and thickness. We are asking the body to do this, but the problem is, this doesn’t work all the time. Sometimes the vein may grow in diameter but not in thickness, or it may not grow in diameter and simply grow in thickness. So, the corollary to that is many surgically created fistulas do not mature; some fistulas require procedures to help with maturation, and these may or may not be successful.
“In the ideal world, the best thing for the ESKD patient is the creation of a fistula that, after a certain period of time, say six weeks, is usable 100% of the time without any other interventions. That’s the predictable ideal, but doesn’t happen very often. So, anything that
improves outcomes to get us closer to that ideal is going to be a very good thing for our patients,” he added bluntly.
One approach to overcoming this quandary is the concept of external support during surgical fistula creation. The VasQ device is a nitinol-based permanent vascular reinforcement implanted around the artery-vein connection. The device is designed to reduce both haemodynamic and mechanical stress to create more functional fistulas. The device, implanted during the surgical creation of either upper arm or forearm fistulas, guides the remodelling in the juxta-anastomotic region to promote outward wall thickening by maintaining the optimal angle, reducing wall tension and facilitating a more stable, laminar flow profile.
“It appears that externally supporting the fistula and making the fistula take an improved angle has promise in increasing functional patency and decreasing the number of interventions to get to maturation,” Farber told Renal Interventions
Six US sites that participated in the VasQ US pivotal study and enrolled more than six patients were eligible to participate in a retrospective chart review of unsupported AVFs to compare them to fistulas that had VasQ support. The cohort for this analysis included 104 ESKD
UKKA RaDaR study provides new insight into the effects of rare kidney diseases on kidney failure
In a recent paper published in March 2024 in The Lancet, Katie Wong (Department of Renal Medicine, University College London, London, UK) et al discuss the results of a longitudinal analysis of the UK National Registry of Rare Kidney Diseases (RaDaR) and what the analysis showed regarding the effects that rare kidney diseases have on chronic kidney disease (CKD).
AS THE AUTHORS STATE IN THEIR ARTICLE, CKD is a major global health challenge that can, if left unchecked, progress to kidney failure. However, the authors highlight the fact that the burden of CKD is not borne equally. Individuals with rare kidney diseases in particular, according to Wong et al, account for 5–10% of people with CKD, but constitute more than 25% of patients receiving kidney replacement therapy. In order to examine the impact of these rare kidney diseases, the authors used the National Registry of Rare Kidney Diseases (RaDaR)—which gathers longitudinal data from patients with these conditions—to study disease progression, as well as outcomes of death and kidney failure.

“The immediate days to first use is typically shorter with VasQ fistulas.”
Alik Farber
patients, with 52 in the unsupported group and 52 in the VasQ group. Both groups were well matched with no significant differences in baseline parameters, including vessel diameter. The researchers evaluated the functional outcomes of time and intervention rate prior to first use, as well as functional success, which was defined as the proportion of fistulas used for haemodialysis at three and six months after AVF creation.
Farber presented the results, which showed a nearly 30-day reduction in median time to first use driven by a significantly lower need for maturation procedures in the VasQ group as compared to the unsupported cohort. Additionally, significantly more fistulas in the VasQ cohort achieved functional success by the threemonth timepoint. The VasQ cohort also showed a trend toward a higher functional success rate at six months, but that finding did not reach statistical significance.
“[We’ve presented] that the immediate days to first use is typically shorter with VasQ fistulas. The ratio of interventions to first use is also significantly less in the VasQ-supported fistulas and the functional success is higher in this group,” commented Farber, adding that the device is relatively easy to place and doesn’t add significant time to the procedure.
Commenting on the results, he said: “The study offers encouraging evidence for the efficacy of an external vascular support of fistulas, especially in lowering intervention rates and shortening the time to achieving functional success.
“I think it’s exciting that there is new clinical science in this space. There’s a huge opportunity that we have with these patients because the maturation rates are currently 50 to 60%, at best. And that’s a pretty small number. So, there’s a considerable need to improve the maturation rates and I applaud Laminate Medical and other companies that are trying to develop ways to address this issue.”
In order to analyse the data, Wong et al recruited people up to the age of 96 years living with 28 types of rare kidney diseases from 108 UK renal care facilities. The primary outcomes of their study were cumulative incidence of mortality and kidney failure in individuals with rare kidney diseases, which they calculated and compared with that of unselected patients with CKD. Cumulative incidence and Kaplan–Meier survival estimates were calculated for the following outcomes: median age at kidney failure; median age at death; time from start of dialysis to death; and time from diagnosis to estimated glomerular filtration rate (eGFR) thresholds, allowing calculation of time from last eGFR of 75mL/min

per 1.73m² or more to first eGFR of less than 30mL/min per 1.73m² (the therapeutic trial window).
According to the authors, 27,285 participants were recruited between 18 January 2010 and 25 July 2022, with a median follow-up time from diagnosis of 9.6 years (interquartile range 5.9–16.7). What the researchers found was that patients enrolled in RaDaR had significantly higher five-year cumulative incidence of kidney failure than 2.81 million UK patients with all-cause CKD, but better survival rates. They also found that median age at kidney failure, median age at death, time from start of dialysis to death, time from diagnosis to eGFR thresholds, and therapeutic trial window all “varied substantially between rare diseases”.
What this study found, they state, was that patients with rare kidney diseases differ from the general population of individuals with CKD. The authors state that, whilst patients with rare kidney diseases have higher five-year rates of kidney failure, they also have a higher survival rate than other patients with CKD stages 3–5, meaning that they are over-represented in the cohort of patients requiring kidney replacement therapy. The authors state that “addressing unmet therapeutic need for patients with rare kidney diseases could have a large beneficial effect on long-term kidney replacement therapy demand”.
“Whilst patients with rare kidney diseases have higher five-year rates of kidney failure, they also have a higher survival rate than other patients with CKD stages 3–5.”

14 April 2024 – Issue 11 AVF creation

Jes S Lindholt & Thomas Emil Andersen
TELEGRAFT: The revolutionary artificial and sustainable graft for haemodialysis and bypass surgery
Jes S Lindholt, Thomas Emil Andersen and Martin Alm write together about TELEGRAFT, a prospective future graft solution that is being developed for the use in home haemodialysis and bypass surgery patients, what the issues are that they hope the graft solution can overcome, and how they intend the graft to do so. With 10% of the worldwide population affected by chronic kidney disease and millions of deaths each year due to lack of access to dialysis units, there is a dire need for innovative and accessible devices which will help patients safely receive dialysis from home.
The unmet need
Artificial blood vessels have been used for more than 50 years when the patient does not have the necessary “spare parts”. However, very few improvements have been made to prevent the most frequent and serious complications, such as stenosing neointimal hyperplasia—scar tissue formation in the sutures between the graft and the native vessel slowing the blood flow, which causes them to close frequently, and problems with infection of the graft, which can occur even years after they have been inserted.
The problems are particularly frequent when they are used for dialysis, where up to 70% fail within a year. If they are used for bypass from the groin to the thigh, half close within five years, and they cannot be used for bypass of smaller blood vessels such as the coronary arteries on the heart.
By setting out to develop a graft solution for the most vulnerable patients—the dialysis patients—who can even use it for safe home dialysis without risking life-threatening bleeding, we are fairly certain that it can quickly also be used for bypasses in atherosclerosis; the potential therefore becomes enormous.
The innovative solution
To combat this unmet need, we are collaborating to develop a special biomimetic and drug-elut-
ing material for artificial blood vessels. The fundamental ideas are to use a special chemical to mimic a naturally occurring chemical found in the blood vessels of bears that is responsible for preventing the vessels from occluding whilst the animals hibernate during winter, as well as paclitaxel and antibiotics, which are intended for a slow internal release to prevent scar tissue formation in the suture line, and an external release on demand to combat impending bacterial infection, respectively.
Blood poisoning arising from vascular prostheses is a frequent and life-threatening complication for dialysis patients. The new technology developed in the project makes it more difficult for the bacteria to attach to the material and thus prevents infections. In addition to that, the Swedish company VERIGRAFT contributes technology to improve integration with the surrounding tissue, thereby ensuring that the blood vessel grows quickly with its surroundings, and which,


combined with a three-layer self-closing silicone wall, enables fast and safe dialysis—so safe that many dialysis patients will be able to look forward to using home dialysis, rather than spending several hours on transport to and staying at a dialysis clinic two to three times a week.
However, we do not believe that the complications can be completely ruled out. Due to this, we are attempting to equip the artificial blood vessels with two diagnostic tools, in the form of pressure gauges that can monitor the blood flow via telemonitoring—thereby warning of impending closure—as well as optical sensors that can pick up signs of incipient inflammation. Today, we usually only discover the complications when it is too late—but with telemonitoring, we get an early warning so that we can make corrections before the problems arise. It is a completely new approach which has enormous potential to reduce patients’ suffering and the costs to the healthcare system.
The (hopefully) upcoming graft is therefore aptly named TELEGRAFT.
Development of the graft started September 2022 and is planned to end February 2027 (54 months). The project is funded by Horizon Europe with a total budget of €5,298,235.75.
Disclosures:

Jes S Lindholt is project coordinator and a professor of Vascular Surgery at Odense University Hospital (Odense, Denmark). Thomas Emil Andersen is an associate professor at the Department of Clinical Microbiology, University of Southern Denmark (Odense, Denmark). Martin Alm is a chemist from the Biomodics ApS (Rødovre, Denmark).

16 Point of View April 2024 – Issue 11 Haemodialysis Graft
Development of the graft started and is planned to end 54 months
Disclaimer: Funded by the European Union. Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or the Health and Digital Executive Agency. Neither the European Union nor the granting authority can be held responsible for them.
September 2022 February 2027



Education, News, Insights
Join the CX Vascular platform today to connect and engage with the global vascular community, share expertise and experiences, and stay up-to-date with the latest education and news in the vascular world. Members will also have access to exclusive content including live discussions on the latest advances in the vascular field and interviews with key thought leaders in the space.
Register now
the community at https://cxvascular.com
Join
Clinical and Industry News

Fresenius Medical Care
launches new educational augmented reality application for kidney replacement therapy
Fresenius Medical Care announced the launch of its new augmented reality (AR) glasses and its accompanying application, Ready4 MultiFiltratePro AR, at the first day of the International Symposium on Intensive Care and Emergency Medicine ([ISICEM], 19–22 March, Brussels, Belgium).
Developed for use with Fresenius’ continuous kidney replacement therapy system MultiFiltratePro, the AR application is comprised of digital learning modules—covering topics such as how to set up the machine, how to activate the citrate pump or how to handle several system components through the AR training—which are then streamed via the use of the AR glasses as the wearer uses the dialysis machine. This, Fresenius states, will allow nursing staff to learn how to use acute dialysis machines within the intensive care wards.
Fresenius hopes that this new AR training resource will allow nursing staff to remain on-site in intensive care units (ICU), which have suffered from shortages globally, by allowing for flexible, ongoing training and education that can take place on site, keeping staff where they are needed most.
Ready4 MultiFiltratePro AR will be launched in select markets as early as Q2 2024, with a limited launch of the MultiFiltratePro taking place in the USA in the latter part of 2024. Once the Safety of Regional Citrate Anticoagulation (SARCA) trial has been completed successfully, Fresenius plans for a full launch of the MultiFiltratePro with the Ready4 MultiFiltratePro AR learning experience in 2025.
Health Canada licenses
Symplicity Spyral radiofrequency renal denervation system to treat hypertension
Medtronic has received a license from Health Canada for its Symplicity Spyral multi-electrode renal denervation (RDN) system.
This is indicated for the management of essential hypertension in patients for whom blood pressure remains uncontrolled despite lifestyle modifications and guideline-driven medical therapy with antihypertensive medications, or when guideline-driven therapy is poorly tolerated.
The Symplicity blood pressure procedure is a minimally invasive technique that uses radiofrequency
ablation to calm the nerves near the kidneys that can become overactive and contribute to high blood pressure. Nearly one in four Canadian adults are affected by hypertension, and it’s estimated that 90% of individuals will develop high blood pressure at some point during their lifetime.
“As we look to improve options to help manage patients with hypertension, we’re encouraged by this latest approval of the Symplicity Spyral renal denervation system,” said Sheldon Tobe, nephrologist and hypertension specialist, Sunnybrook Health Sciences Centre (Toronto, Canada). “There is a big unmet need in Canada for the subset of patients who can’t fully control hypertension with medication and/or lifestyle changes. This innovative procedure will help to fill that gap by potentially helping to improve blood pressure control.”
The Heath Canada licence is based on clinical evidence backing the Symplicity blood pressure procedure.
FLOW trial shows reduction in kidney disease progression in patients with CKD and type 2 diabetes treated with semaglutide 1.0mg
Novo Nordisk has announced via a press release the headline results from the kidney outcomes trial FLOW, coming after the decision to stop the trial early due to efficacy that was announced on 10 October 2023, based on a recommendation from an independent data monitoring committee.
The double-blind trial sought to compare injectable semaglutide 1.0mg with placebo as an adjunct to standard of care for prevention of progression of kidney impairment and risk of kidney and cardiovascular mortality in people with type 2 diabetes and chronic kidney disease (CKD). The trial enrolled 3,533 people with type 2 diabetes and CKD.
The primary endpoint of the trial, which was to demonstrate a statistically significant and superior reduction in kidney disease progression—as well as cardiovascular and kidney death—of 24% for people treated with semaglutide 1.0mg when compared to placebo, was achieved, and superiority of semaglutide 1.0mg versus placebo was confirmed for the confirmatory secondary endpoints.
The combined primary endpoint included five components measuring the progression of CKD and the risk of kidney and cardiovascular mortality. Both CKD and cardiovascular components of the primary endpoint

contributed to the risk reduction. During the trial, it was also noted that semaglutide 1.0mg appeared to have a safe and well-tolerated profile, in line with previous semaglutide 1.0mg trials.
The press release also states that Novo Nordisk expects to file for regulatory approvals of a label expansion for Ozempic in the USA and EU in 2024, and that the full results from FLOW will be presented at a scientific conference later this year.
US FDA grants 510(k) clearance to Fresenius Medical Care’s new haemodialysis system
Fresenius Medical Care recently announced via a press release that it has received 510(k) clearance from the US Food and Drug Administration (FDA) for its new 5008X haemodialysis system, which it hopes will allow it to “bring a new standard of care in dialysis therapy to people living with kidney disease in the USA”.
This new product, Fresenius states, will differ from conventional high-flux haemodialysis by incorporating both diffusion and convection techniques to “eliminate larger molecules and effectively manage fluid replacement through convection” that are already widely used in Europe.
Results from the CONVICE study—a three-year, multinational research study conducted in eight European countries that compared these two types of haemodialysis techniques—were recently published in the New England Journal of Medicine (NEJM) and have demonstrated that patients treated with high-volume haemodiafiltration experienced a 23% decrease in mortality rates when compared to those treated with the more commonly used high-flux haemodialysis.
Fresenius states that, in the USA, there are currently an estimated 160,000 in-centre haemodialysis machines across all service providers that could be replaced to adapt to this “new standard of care”.
MultiOmic Health and Queen’s University Belfast collaborate for future of diabetic kidney disease diagnosis
MultiOmic Health has partnered with the Centre for Public Health at Queen’s University Belfast ([QUB] Belfast, UK) on a collaborative project to develop data-driven diagnostic tools for diabetic kidney disease (DKD). This project, which will take place over two years, is partially funded by a grant awarded by Innovate UK’s £20 million Advancing Precision Medicine programme to MultiOmic.
MultiOmic and QUB plan to use their collective expertise to explore molecular-level differences and similarities in kidney disease amongst patients with type 1 and type 2 diabetes. This project, which started in December 2023, aims to identify diagnostic and prognostic biomarkers for DKD progression, as well as likely complications within specific patient subpopulations.
Chronic kidney disease (CKD), which is common in patients with both type 1 and type 2 diabetes, has an economic cost of £7 billion per year in the UK, including £6.4 billion in direct costs to the National Health Service (NHS),
according to MultiOmic’s press release. With CKD becoming more prevalent in patients with diabetes, they state, this poses a substantial challenge, as it helps to increase the risk of cardiovascular events and kidney failure.
The “one-size-fits-all” approach that is favoured presently, according to MultiOmic, is failing to address specific needs that are tailored to members of a diverse diabetic population. It feels that the solution to these limitations is a data-driven approach that offers a way to improve and advance personalised approaches for DKD management.

Invizius treats first patients in first-in-human phase 1 clinical study of haemodialysis priming solution
Invizius has announced in a press release that the first two patients have been treated with its H-Guard priming solution in the company’s first-inhuman phase 1 clinical study at the National Institute for Health and Care Research (NIHR) Manchester clinical research facility (CRF).
The study, which is investigating the safety and tolerability of Invizius’s lead product, H-Guard, in patients receiving haemodialysis who are vulnerable to dialysis-induced immune activation, which occurs, Invizius states, when a patient’s blood comes into contact with foreign surfaces in the dialysis circuit. This can then lead to excessive inflammation, coagulation, vascular and organ damage, and other deleterious outcomes. The purpose of H-Guard is to prevent this from occurring; it is flushed through the dialysis machine prior to the treatment beginning, with the aim of preventing serious complications by “attenuating the patient’s immune response to the dialysis procedure”.
Following the treatment of these first two patients, the UK Medicnes and Healthcare products Regulatory Agency (MHRA) approved continuation of the study, based off the safety and performance data from these patients. Moving forward, the trial will now recruit up to a further eight patients into the study, which is being led by Sandip Mitra (Manchester Royal Infirmary, Manchester, UK) and co-investigators Leonard Ebah (Manchester Royal Infirmary, Manchester, UK) and Duha Ilyas (Manchester Royal Infirmary, Manchester, UK). Mitra said of the trial that “our aim is to improve the outcomes of patients on dialysis. We are continuing this study to seek more safety and performance data necessary to demonstrate H-Guard’s potential and to direct future clinical applications and testing.”
18 April 2024 – Issue 11
Latest News
Conference Calendar
23–25 April
Charing Cross (CX) Symposium 2024
London, UK cxsymposium.com
29–30 April
Euro Nephrology Summit 2024
Paris, France nephrologycongress.conferenceseries.com/ europe
14–18 May
National Kidney Foundation (NKF)
Spring Clinical Meetings 2024
Long Beach, USA kidney.org/spring-clinical
23–26 May
61st European Renal Association (ERA) Congress
Stockholm, Sweden era-online.org/events/stockholm-2024
28–31 May
Leipzig Interventional Course (LINC) 2024
Leipzig, Germany
leipzig-interventional-course.com/visitors/ linc-2024
31 May–05 June
American Traansplant Congres (ATC) 2024
Philadelphia, USA atcmeeting.org/

10–11 June
International Conference on Renal Medicine and Dialysis (ICRMD)
Barcelona, Spain waset.org/renal-medicine-and-dialysisconference-in-june-2024-in-barcelona
11–13 June
UK Kidney Week 2024
Edinburgh, UK ukkw.org/
14–15 June
Endo Vascular Access (EVA) meeting
Patras, Greece evameeting.org/








*Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the field of renal disease management Editorially independent Subscribe today Available in print and digital formats and through our social channels Visit renalinterventions.net and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription**
board
Meet our editorial
Inston Chairman of the Editorial Board Nicholas Inston is a transplant and vascular access surgeon, and the clinical service lead for renal surgery, at Queen Elizabeth Hospital in Birmingham, UK. Ziv Haskal Board Member Ziv Haskal is a professor of radiology, and an interventional radiologist and interventional oncologist, at the University of Virginia School of Medicine in Charlottesville, USA. Stephen Hohmann Board Member Stephen Hohmann is a vascular and general surgeon at the Texas Vascular Associates clinic in Dallas, USA.
Nicholas
Jones Board Member Robert Jones is an interventional radiologist at Queen Elizabeth Hospital in Birmingham, UK.
Robert
Conference Calendar 19 April 2024 – Issue 11



MEETING PROGRAM DAY 1 SESSIONS SESSIONS DAY 2