www.neuronewsinternational.com




www.neuronewsinternational.com



A legacy of neurovascular innovation, clinical evidence and more with Carsten Schroeder, Terumo Neuro president and CEO
2-3 6
SOFIA: unparalleled safety and excellent outcomes in acute stroke care with Dheeraj Gandhi (Baltimore, USA)
WEB: the safest device ever studied in brain aneurysm treatment with Laurent Spelle (Paris, France) and Adam Arthur (Memphis, USA)
4-5 7
LVIS EVO: how physician feedback fuelled the latest evolution in coil-assist stents with René Chapot (Essen, Germany)
The past year has been an incredibly eventful and productive period for Terumo Neuro. In September 2024, the company officially announced a full rebrand from the MicroVention™ moniker it had operated under for many years, followed by the opening of a brand new, state-of-the-art research and development (R&D) centre in the USA earlier this year. Last July, Terumo Neuro also announced the conclusion of a legal case against multiple former employees over trade secret misappropriation—among other claims—relating to its aneurysm treatment portfolio. Two of the company’s flagship products, the WEB™ device and the SOFIA™ catheter, are in the midst of celebrating major milestones in 2025 as well. Terumo Neuro president and chief executive officer (CEO) Carsten Schroeder sits down with NeuroNews to discuss all of these recent events in addition to providing a window into what the future holds for one of the neurovascular industry’s most established yet also most innovative players.
Could you outline the significance of last year’s rebrand from MicroVention to Terumo Neuro?
MicroVention was started almost 30 years ago in Southern California and—although
the first product the company wanted to make was a stentriever—the first device it actually brought out was an embolisation coil with a reliable detachment system, which was then followed by the Hydrogel coils. In 2006, the company was acquired by Terumo, but
it continued under the MicroVention name until last year. Terumo’s thinking was that, being well-known and having expertise in ischaemic stroke, haemorrhagic stroke and neurovascular access, MicroVention should broadly continue what it was doing.
When I came aboard around five years ago, I said, “that’s all fine—that’s where we come from and it’s our DNA—but our customers are moving into other disease states”. Our customers are thinking about using venous stenting to treat pulsatile tinnitus or idiopathic intracranial hypertension (IIH); they’re moving into oncology treatments with catheters and liquid embolics; there are people working on endovascular treatments for hydrocephalus; there’s the chronic subdural haematoma (cSDH) space—there are many other diseases that will become considerable markets over the next 10 years. So, we felt it was important to signal to our employees, physicians and patients that we want to go beyond ischaemic, haemorrhagic and access. We want to participate in and contribute to these new, evolving areas, and we want to follow the lead of our customers who are heading to those places anyway. That was the main motivation behind the brand change.
But, what has continued over the past five
All rights reserved. Published by BIBA News, London T:+44 (0)20 7736 8788, publishing@bibamedical.com. The opinions expressed in this supplement are solely those of Terumo Neuro and the featured physicians and may not reflect the views of NeuroNews DISCLAIMER: Information provided may not represent the approved indication for use for each country/market. Please refer to the Instruction for Use (IFU) in the specific market/country that you are looking into. The contents included in these interviews express only the clinical perspective of the physicians; they are completely independent and do not necessarily reflect the opinions of Terumo Neuro.
years and will continue moving forward is Terumo Neuro working hand-in-hand with physicians to design tools that allow them to treat their patients. That is what made the company what it is today and that will not change. At every conference, we have tech suites where we demonstrate prototype products that are about to be launched. We have customer visits at our R&D centre in Aliso Viejo, USA almost every week. We always get physician input on our device designs. All of these things will continue but, now, we need to do them across more disease spaces—doing so ourselves, or by working with external partners.
Are there any other reasons why now is a particularly exciting time for the company?
These things have not been done before. We’re also exploring other ideas regarding post-approval studies in other key geographies and, overall, we’ve doubled the budget that goes into this work.
How would you assess the current landscape of endovascular aneurysm treatments?

Carsten Schroeder
Yes, definitely. We have a couple of products that are celebrating significant anniversaries. The SOFIA catheter was launched a decade ago this year and, in October 2025, it will be 15 years since the first ever case with the WEB device as well. And—even 15 years later—we’re now starting to roll the WEB 17 system out in China and we’re currently working to have it approved in Japan too.
In addition, we introduced the LVIS™ EVO™ stent in the USA just last year and, in the past few months, we’ve launched the SOFIA 88 neurovascular support catheter, so we have several new products coming out in addition to the anniversaries of our more established devices. We’re also continuing to invest in R&D and business development at a rate that—I would say—is above the industry average.
Another thing that started under my leadership was an increased focus on postapproval clinical work. This is now being seen in a number of poster presentations, journal publications and symposia regarding real-world evidence on our products rather than just premarket data. Traditionally, Europe has tended to do more of that—for example, in the CLEVER study with the WEB device, and the SEALANT study with Hydrogel coils and the LVIS EVO stent—but this was not always the case in the USA. So, we began by taking an existing ischaemic stroke registry, named RESTORE, and ‘boosting’ it to include more than 800 patients across all of the ischaemic stroke products we have available in the USA. And we’re now doing a similar thing on the aneurysm side with the Complex Aneurysm Registry (CAR), where we’re hoping to go up to 900 US patients across all of the options we have for treating aneurysms.
If you look at overall value, coiling is still the single largest market in aneurysm treatment, and it continues to grow slightly. It’s also a highly competitive space and there are a lot of platinum coils on the market. Terumo Neuro has its Hydrogel-coated coils and, to date, there are three randomised trials showing that these devices are superior to regular platinum coils. This is therefore an important part of our portfolio and one that we probably need to talk about a little bit more often. The WEB device has probably sucked the air out of the room there
We felt it was important to signal to our employees, physicians and patients that we want to go beyond ischaemic, haemorrhagic and access.”
slightly because it may be preferable to place one WEB device rather than five, six or seven coils—but, coiling remains a massive market and one that is still growing. That being said, the use of stents, flow diverters and intrasaccular devices continues to grow in popularity, especially among younger physicians in the earlier stages of their career. In 2023, we celebrated the one-year anniversary of US availability of our Flow Redirection Endoluminal Device (FRED™) X flow diverter, and there have been numerous studies and publications on the device over the past two-to-three years. With the WEB device, we’re streamlining our portfolio but also adding new sizes because we’re seeing that—across 10–15 years of data—some sizes are the ‘go-to’
in many cases while others are hardly ever used. So, we’re streamlining that portfolio in accordance with customer preference while bringing out more sizes to give physicians more choice, optimising device selection and placement with the ultimate goal of making procedures quicker, safer and more effective for the patient.
Could you discuss Terumo Neuro’s R&D capabilities and why they are important regarding continued innovation?
We have a purpose-built centre, constructed by MicroVention back in 2016, which has a fully equipped angio suite that—via in-silico models—allows us to test devices under the most realistic conditions that are possible outside of a patient’s body. We have physicians coming in regularly, we give them an anatomical model—usually a challenging one—and then we give them multiple device prototypes and ask them which they prefer. Then, we collate feedback from all of the physicians to inform the final device design. And, of course, we also have manufacturing capabilities, including R&D pilot lines and a machine shop, and all of this is in the same building.
In March this year, we also established the Discovery and Technology Center of Terumo (D-TECT) in Aliso Viejo to further expand our global R&D and innovation capabilities.
What was the significance of Terumo Neuro’s recent legal settlement with Balt?
The medical device industry is centred on intellectual property (IP), through either patents or trade secrets, and it’s my belief that a company needs to protect these types of assets. That’s what we did when we litigated against Balt, and we eventually reached a mutually acceptable settlement. And, we sent out a press release detailing this because we believed that it was important to signal to the world that we take our IP very seriously. If people move from one company to another—which they’re entitled to do— they need to leave behind all of their trade secrets and IP belonging to the company.
We hope that the conclusion of this case sets a precedent, demonstrating that we’re protecting our assets at all costs and that other companies should do the same. As I said at the time, the case highlights our commitment to ethical business practices and the fact that we feel IP protection is foundational in fostering a fair and competitive market, as well as ensuring that groundbreaking medical technologies can continue to evolve and reach the patients who need them.
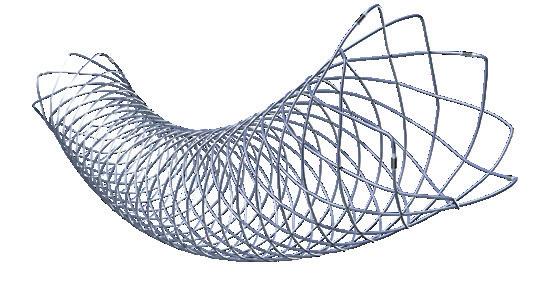
The Woven EndoBridge (WEB™) aneurysm embolisation system, having been introduced as an intrasaccular option for brain aneurysm treatment in 2010, is now a mainstay in the management of these rare but often complex cases. Having played integral roles in evaluations of the device across Europe and the USA, respectively, Laurent Spelle (Bicêtre Hospital, Paris, France) and Adam Arthur (Semmes-Murphey Clinic, Memphis, USA) are perfectly placed to discuss not only the current body of clinical data behind the WEB device, but also its innovative journey over the past 15 years.
THE TWO PROVIDE SIMILAR recollections of their initial WEB device experiences, with Spelle’s very first case— and every subsequent case in Europe—being included within a large-scale registry, and Arthur’s first WEB treatment representing the start of enrolment in the US WEB-IT study.
“Every single patient being treated with WEB was enrolled in a clinical study,” Spelle says. “This was a new concept, but I think we should recognise that this is the way to do it.”
Following its CE-mark approval in 2010, the WEB device went on to be rigorously evaluated within a number of European studies—most notably, WEBCAST and WEBCAST2, as well as the French Observatory study. Five-year follow-up data from more than 160 aneurysm patients across those investigations ultimately showed no occurrences of bleeding or rebleeding, zero instances of WEB-related morbidity or mortality, and a 77.9% rate of adequate occlusion.
“Never in the history of the field of interventional neuroradiology has a device been so extensively studied, through numerous clinical trials, in order to continuously shape its technical development,” Spelle comments. “And, each time there was a technical evolution of WEB, the new designs were assessed in new clinical studies.”
While the vast majority of patients enrolled in these initial studies were those with unruptured aneurysms, subsequent research demonstrated the WEB device’s utility in ruptured cases too. CLARYS—in which all 60 European participants were ruptured aneurysm patients—found no instances of WEB-related morbidity or mortality, zero rebleeding occurrences, and an adequate occlusion rate of 87%, out to one year. Speaking as the study’s principal investigator (PI), Spelle describes these as “very important” results that highlight the
WEB device’s ability to protect against future rebleeding and, thus, have established the device as a viable option in ruptured aneurysms.
More recently, the CLEVER study—evaluating the newer-generation WEB 17 system across 163 European patients (ruptured aneurysms, 36.8%)—observed 0% rates of rebleeding and WEBrelated morbidity or mortality at one year, in addition to adequate occlusion rates of 86.5% and 82.4% for ruptured and unruptured aneurysms, respectively. In Spelle’s view, these data indicate that the WEB device can be deployed safely and effectively in ruptured aneurysm patients.
The other key piece of prospective, multicentre data on the WEB device comes from WEB-IT, which was launched in 2014 once the device arrived on US soil and saw Arthur himself enrol the first handful of patients as PI for the study.
presented for the first time in 2022—showed an adequate occlusion rate of 96.4% and a retreatment rate of 15.5% at five years. A complete occlusion rate of roughly 58% was also maintained at both one and five years of follow-up.
According to Arthur, WEB-IT’s fiveyear results are “absolutely remarkable”— especially given the known treatment challenges and significant rupture risk associated with wide-neck bifurcation aneurysms. He goes on to note that data on both safety and effectiveness in the study surpass anything previously seen regarding devices used to treat brain aneurysms.


“WEB intrasaccular therapies were fundamentally new—it really is not the same as deploying a stent, flow diverter or coil,” he notes.
“So, those first cases enrolled in Memphis were the first time that any of the WEB-IT physicians had put a WEB into a patient’s head.”
Having enrolled 150 patients (ruptured aneurysms, 6%), WEB-IT found a 0.7% rate of overall morbidity at one month, in addition to no WEB-related mortality and a one-year adequate occlusion rate of 84.6%. More long-term data from the study—
“Of those patients who were enrolled in WEB-IT, not a single one has gone on to experience the thing that they were most worried about, which is rupture of their aneurysm or re-rupture of an initially ruptured aneurysm,” Arthur adds. “With 148 patients over five years of follow-up, that’s incredible.”
With no clinical cases through which to gain experience with the WEB device prior to the start of this study, Arthur and many of his US colleagues utilised flow models to hone their understanding of the device, and its characteristics, before using it to treat patients. He comments that WEB-IT was one of the first investigational device exemption (IDE) studies to have utilised model-based simulation in such a comprehensive way and, in his view, may pave the way for these approaches to become more widespread moving forward.
“When discussing WEB-IT’s outstanding results and safety record, people sometimes say, ‘that’s not real-world data because you guys practised in models, and you were very selective and careful’,” he notes. “And, I guess, if the worst criticism someone’s going to throw at the study is that the results were so outstanding because we practised and we were really careful, then I’ll take it!”
Commenting on how WEB-IT contributes to the overall body of evidence on the WEB
Never in the history of the field of interventional neuroradiology has a device been so extensively studied […] in order to continuously shape its technical development.”
Laurent Spelle
device, Spelle states that the device has consistently demonstrated a “very good” safety profile—adding that, in terms of effectiveness, adequate occlusion rates of at least 80% “remain stable” at both one- and five-year follow-up across all of the major studies conducted to date.
In Spelle’s view, the difference between the WEB device he first implanted in 2011 and the ones available across the world today is “night and day”, which speaks to Terumo Neuro’s efforts to continue innovating for the benefit of both patients and physicians. Among the most noteworthy stages of this “tremendous technical evolution” include switching from a dual-layer to a single-layer design to improve navigability; the use of drawn filled tube (DFT) wires to ensure full visibility on imaging; and a considerable reduction in the calibre of microcatheter used to deliver more low-profile iterations of the device.
“One recent improvement was bringing WEB 17 onto the market,” Spelle says, highlighting the latest addition to Terumo Neuro’s intrasaccular portfolio, which became available in Europe in the late 2010s and gained US Food and Drug Administration (FDA) approval in 2021. “Those devices are really useful in treating smaller, shallower aneurysms.”
“Terumo Neuro and its predecessors— MicroVention and Sequent Medical—have, from my perspective as a physician-
scientist, done a truly fantastic job in developing good clinical practices and very high-quality evidence that allows us to really talk about the safety and effectiveness of WEB,” Arthur adds.
Here, Arthur professes that, as someone who expected flying cars to be readily available by now, no amount or pace of innovation is likely to ever truly satisfy him. Nonetheless, he commends the talented team of engineers at Terumo Neuro for the way they have continued to iteratively improve the WEB device since its inception—a point that Spelle agrees with, also recognising Sequent Medical’s efforts to drive clinical research forward and willingness to incorporate feedback from physicians during the early stages of device development.
While a handful of alternative intrasaccular technologies are currently being developed and studied by other neurovascular companies, the WEB device remains the only device of its kind approved

for intracranial aneurysm treatment in the USA, and thus stands as the “clear leader” within this segment, according to Arthur. In Europe, it’s a similar story; Spelle notes that the WEB device retains a “very dominant” position in this market, due in no small part to the fact that—based on proven clinical safety data and angiographic occlusion outcomes—it is the only intrasaccular device currently being reimbursed for aneurysm treatments across a number of countries.
“I think competition is a healthy thing, so
I would love to see the companies making those other devices generate a lot of great clinical evidence,” Arthur comments. “But, even if you’re the president of one of those companies, you’re not going to say, ‘we have evidence that rivals the clinical data on WEB’, because they don’t.”
Despite this position of strength—but, perhaps unsurprisingly, given Terumo Neuro’s perpetual appetite for innovation and progress—Spelle and Arthur are both hoping to see the company advance the WEB device’s capabilities even further in the coming years. According to Spelle, an improvement in the complete occlusion rates seen thus far may bring tangible benefits for patients, and Arthur feels that optimising the device’s suitability to “the extremes” of aneurysm sizes—very small and very large alike—would be welcomed by many neurointerventionists.
Nonetheless, the WEB device remains as many physicians’ go-to treatment option for wide-neck bifurcation aneurysms—as demonstrated by its usage across thousands
Of those patients who were enrolled in WEB-IT, not a single one has gone on to experience the thing that they were most worried about, which is rupture of their aneurysm or rerupture of an initially ruptured aneurysm.”
Adam Arthur
of clinical cases to date. Spelle feels that the device offers a “very quick and very efficient” approach that can be utilised in almost all of these types of cases, while Arthur posits simply that “this is the safest method of treatment for cerebral aneurysms that has ever been studied, period”.
Much like the WEB™ embolisation system in aneurysm care, the SOFIA™ family of neurovascular catheters are among the most established and long-trusted devices on the landscape of acute ischaemic stroke treatment. Their legacy spans a full decade—following CE-mark approval in 2015 and US Food and Drug Administration (FDA) clearance in 2018, they have been utilised in more than 500,000 procedures across 170 countries. And, with new data and the latest technological advances currently contributing to a surge in the uptake of aspiration-based thrombectomy treatments, the SOFIA catheter’s usage is likely to expand even further in the near future.
AS AN EARLY ADOPTER OF THE technology in the USA, Dheeraj Gandhi (University of Maryland School of Medicine, Baltimore, USA) has played a significant role in this journey. He estimates having used SOFIA catheters in at least 800 cases since it became available to him.
“For me, what stood out about this device, first of all, was its trackability,” he says. “It’s very supple and, if need be, we can curve the tip of the catheter—that’s something we’ve used a lot in certain difficult anatomies. And, as my experience has grown, I’ve become very fond of this device. It not only adds speed, control and versatility in getting through challenging anatomies but— even more important, for me—is having a trustworthy device that doesn’t lead to issues like vessel perforations or dissections. And, on that front, I think SOFIA has an unparalleled safety record.”
Gandhi also highlights the fact that— while it is important to adapt thrombectomy treatments to each individual patient—the SOFIA catheter represents his “go-to device” in the vast majority of acute stroke patients with internal carotid artery (ICA), M1 and more proximal M2 occlusions.
Among the wealth of clinical data accrued on SOFIA catheters over the past decade, the prospective, multicentre SOFAST study is a key source supporting its safety and efficacy. Enrolling 108 large vessel occlusion (LVO) patients with anterior-circulation ischaemic strokes presenting within eight hours of symptom onset, and conducted across 13 US institutions, the study evaluated first-line
aspiration thrombectomy using the SOFIA 6Fr catheter.
“We found that the overall cohort of patients had a 97% rate of TICI [thrombolysis in cerebral infarction] ≥2b revascularisation,” notes Gandhi, who was the study’s principal investigator. “Moreover, SOFIA alone—when used as a first-line device—was associated with an 87% rate of TICI ≥2b revascularisation. Another impressive finding was that three out of four patients had a firstpass effect [FPE], which we know is a very important metric in terms of predicting outcomes.”
with historical data.
“A lot of companies have made very innovative devices in this space but, for me, the proof is in the pudding,” he adds. “The overall results we saw in SOFAST are almost unbeatable. We can compare them to historic studies—either registries or randomised controlled trials—and, when we look at FPE rates, the majority of those studies range from 35–45%. So, having FPE rates of 75% for TICI ≥2b and 70% for TICI ≥2c is a huge jump forward.”
“There is an increasingly large number of operators starting to use aspiration as their first option,” Gandhi continues. “Earlier on in my career, I mostly used stentrievers. However, two things made me more wary of that technique: the endothelial disruption that might occur from dragging the stent retriever, and the time it was taking to open up the blood vessel.”
Utilising aspiration thrombectomy as a first-line approach, according to Gandhi, can help alleviate both of these concerns; using a catheter removes the need to cross the clot and thus reduces the potential risk of distal embolisation, and it also upholds the ‘time-is-brain’ mantra by minimising device dwell times and significantly shortening the duration of the procedure. These are the key factors Gandhi cites in encouraging fellow neurointerventionists to consider a more aspiration-led paradigm in stroke thrombectomy.

Here, Gandhi reiterates the almost “unparalleled” safety results seen with the SOFIA catheter, reporting only one symptomatic intracranial haemorrhage, zero instances of emboli in new territories (ENT), and a serious adverse event (SAE) rate of 2.8%.
“These procedures are remarkably dependent on the devices, and their safety and operational capabilities—some of the early trials in stroke thrombectomy were negative because the devices used were antiquated,” he continues. “We have also learned over the years that simplicity can be beautiful and, with SOFIA, we often don’t even require a microcatheter or wire, and that’s why the rate of clot engagement—in a very short window of time—is extremely high.”
Gandhi draws attention to the average times to clot engagement and revascularisation in SOFAST, which were 12 and 17 minutes, respectively—both “very impressive” figures in comparison
“It is incumbent on us—especially when there are new, prospective studies coming out—to be willing to make that shift in order to achieve better outcomes,” he states. “And we haven’t stopped innovating after SOFAST. At our centre, it is very common these days to get sub-10-minute revascularisations, and I’ve done a number of cases within five minutes from groin puncture to complete revascularisation.”
On the subject of innovation, Terumo Neuro is currently building upon the longstanding legacy of its 0.07-inch inner diameter (ID) SOFIA 6Fr catheter with the launch of a 0.088-inch ID version of the device.
Commercial availability of the SOFIA 88 catheter—recently described by Ameer Hassan (Valley Baptist Neuroscience Institute, Harlingen, USA) as “truly one of the best products in this category”—was announced in the USA in May, followed by an official launch in the EMEA (Europe, the Middle East and Africa) region in June.

LVIS has entered the building: a closer look at the coil-assist stent backed by physician feedback and “spirit of innovation”
Having been introduced in Europe in 2019 before debuting in the USA just last year, the LVIS™ EVO™ intraluminal support device is one of the newer additions to Terumo Neuro’s portfolio of haemorrhagic stroke therapies. With thousands of units sold in Europe already and ever-increasing uptake on the other side of the Atlantic, the popularity of the LVIS EVO stent continues to grow—as does clinical evidence on its benefits as an adjunctive tool in the treatment of intracranial aneurysms. René Chapot (Alfried Krupp Krankenhaus, Essen, Germany) discusses his first-hand experiences with the LVIS EVO stent as an early adopter of the device who also played a notable role in its development.
CHAPOT HAS BEEN USING THE LVIS EVO stent “extensively” since its European introduction, deploying the device in hundreds of aneurysm cases to date—predominantly alongside coils when embolising unruptured wide-neck aneurysms ranging from 4–10mm in diameter.
He describes the device as an “evolution” of older braided coil-assist stents, commenting that the more open and ultimately more optimised braid angles seen in the LVIS EVO stent’s mesh structure are an important contributing factor in its ability to open and expand “very well”, even within smaller neurovasculatures and tight curves. On this front, Chapot notes that the quality of a given stent plays a “major role” in dictating what is technically feasible once the device has been implanted; “an unexpanded stent is always at risk for some ischaemia to occur”, he avers.
Composed of nitinol-platinum drawn filled tube (DFT) wires, the LVIS EVO stent is fully visible on imaging, Chapot adds, going on to highlight its “very reliable” detachment system and the fact that the ‘finished ends’ seen in earlier iterations of the device have been shortened to address possible concerns over recrossing the stent once it has been delivered.
“So, there are many technical features that make it a very good device,” he posits. “Among braided stents, it’s probably the one that is easiest to handle and has the greatest ability to conform well to the anatomy of the vessel.”
Chapot indicates that—while the LVIS EVO stent can also be crossed with a second device—its use may require the operator to tailor their approach as compared to alternative stenting options, either by treating the aneurysm via balloon-assisted coiling or ‘jailing’ it with a microcatheter before delivering the stent itself. However, in Chapot’s view, this adjustment is made worthwhile by the upsides the LVIS EVO stent offers.
“You adapt your way of working to this,” he comments, “but, if you want to combine the
advantages of using a stent to hold the coils in the aneurysm and the advantages of having a [high metal surface area (MSA)] device—while also removing the need for lifelong antiplatelet therapy—then I would say that, in all aneurysms smaller than 10mm, it is a very good choice.”

In 2022, Chapot and his colleagues in Essen reported their experiences with the LVIS EVO stent in the journal Interventional Neuroradiology, finding that—when deployed in conjunction with the HydroCoil™ embolic system (Terumo Neuro) across a population of more than 100 unruptured aneurysm patients—the device achieved a high and stable rate of complete aneurysm occlusion at one year, and was associated with acceptable rates of immediate and delayed complications.
Additionally, Chapot is a leading figure—alongside co-principal investigator Jonathan Downer (Royal Infirmary of Edinburgh, Edinburgh, UK)—within a more large-scale assessment of this treatment approach. The ongoing, observational SEALANT study has enrolled a total of 206 patients with unruptured but also ruptured (>30 days since occurrence) aneurysms across 19 European sites. Initial safety analyses in SEALANT have shown a 100% rate of good functional status at discharge as well as a 99.5% rate of technical success with the LVIS EVO device.
the procedure] but, rather, how the outcomes look after a longer period of time—and I’m talking about several years rather than a few months of follow-up.”
Along with several other physicians, Chapot was involved in the development and evaluation of the LVIS EVO stent before it even reached the market, with his feedback and firsthand experiences being taken into account while Terumo Neuro was still refining the device’s design. He recalls three “very tough” situations in particular— one aneurysm in Germany, one in Japan, and another in the USA—in which the device was tested, with details of its design being modified marginally until it was shown to perform adequately in these challenging cases.
“I would say this is one of the strengths of Terumo Neuro; to be able to evaluate products based on the requirements of physicians, who are reporting on the potential drawbacks of existing materials, and improving up to the point where those materials become very good,” he says.
“In the end, what makes a treatment successful is a combination of different things, and I expect that this study will confirm a very high level of stability,” Chapot says, touching on the long-term follow-up period (36 months) being observed. “Today, there are a thousand ways to treat an aneurysm, so the question is not what is feasible [regarding
Here, Chapot acknowledges the “spirit of innovation, in every direction”, Terumo Neuro is currently demonstrating, including its more recent introductions in liquid embolics, stentrievers and carotid stents, as well as the “extremely important” work the company is doing to ensure more long-established devices—like the WEB device and the SOFIA catheter—are “constantly renewed”.
“Whenever a company is able to accept there are potential limitations, and work to develop a new device that works better, I have a lot of respect for this because it’s a lot of effort—and also probably expensive—but, in the end, it’s best for the patients and for the physicians,” he concludes.
REFERENCES: 1. Arthur AS, Molyneux A, Coon AL, et al. The safety and effectiveness of the Woven EndoBridge (WEB) system for the treatment of wide-necked bifurcation aneurysms: final 12-month results of the pivotal WEB Intrasaccular Therapy (WEB-IT) Study. J Neurointerv Surg 2019. 2. Pierot L, Moret J, Barreau X, et al. Aneurysm Treatment With Woven EndoBridge in the Cumulative Population of Three Prospective, Multicenter Series: 2-Year Follow-Up. Neurosurgery 2020. 3. Pierot L, Szikora I, Barreau X, et al. Aneurysm treatment with the Woven EndoBridge (WEB) device in the combined population of two prospective, multicenter series: 5-year follow-up. J Neurointerv Surg. 2022. 4. Spelle, L., et al. (2021). "CLinical Assessment of WEB device in Ruptured aneurYSms (CLARYS): results of 1-month and 1-year assessment of rebleeding protection and clinical safety in a multicenter study." J Neurointerv Surg. 5. CLEVER: Clinical evaluation of WEB 0.017 device in intracranial aneurysms. Final results at 1 year. Observational post-market, prospective, multicenter GCP study. Conducted at 17 European sites with a minimum of 160 subjects. Data comes from information presented at ISC 2023. 6. Fiorella D, Molyneux A, Coon A, et al. Safety and effectiveness of the Woven EndoBridge (WEB) system for the treatment of wide necked bifurcation aneurysms: final 5 year results of the pivotal WEB Intra-saccular Therapy study (WEB-IT). J Neurointerv Surg 2023.
WEB: The WEB™ Aneurysm Embolization System is indicated for use at the middle cerebral artery (MCA) bifurcation, internal carotid artery (ICA) terminus, anterior communicating artery (AComm) complex, or basilar artery apex for the endovascular treatment of adult patients with saccular, wide neck bifurcation intracranial aneurysms with dome diameter from 3 mm to 10 mm and either neck size 4 mm or greater or the dome-to-neck ratio is greater than 1 and less than 2. Contraindications: Patients with known active bacterial infection that may interfere with or negatively affect the implantation procedure. Patients with known hypersensitivity to nickel. PRECAUTIONS: Large bore microcatheters may have a higher probability of developing a thromboembolic event in the parent vessel. The WEB embolization device should be used only by physicians trained in percutaneous, intravascular, and neurovascular techniques and procedures at medical facilities with the appropriate fluoroscopic equipment. The WEB embolization device should be used by physicians who have received appropriate training for this WEB embolization device. Carefully weigh the benefits of treatment vs. the risks associated with treatment using the WEB embolization device for each individual patient based on their medical health status and risks factors for intracranial aneurysm rupture during their expected life time such as age, medical comorbidities, history of smoking, intracranial aneurysm size, location, and morphology, family history, history of prior asymptomatic subarachnoid hemorrhage (aSAH), documented growth of intracranial aneurysm on serial imaging, presence of multiple intracranial aneurysms, and presence of concurrent pathology. The benefits of WEB embolization device use may not outweigh the risks associated with the WEB embolization device in certain patients; therefore, judicious patient selection is recommended. Limit the exposure to X-ray radiation doses to patients and physicians by using sufficient shielding, reducing fluoroscopy times, and modifying X-ray technical factors when possible. The WEB embolization device may create local field inhomogeneity and susceptibility artifacts during magnetic resonance angiography (MRA), which may degrade the diagnostic quality to assess effective intracranial aneurysm treatment. Please only use digital subtraction angiography (DSA) or computed tomography angiography (CTA) to assess intracranial aneurysm occlusion for patient follow-up. Steam shaping 0.021” and greater microcatheters may result in improper WEB embolization device delivery and deployment, depending on the degree of shaping and catheter deflection during WEB embolization device delivery. If repositioning is required, take special care to retract or to advance the WEB embolization device under fluoroscopy, including new road map to confirm catheter position. For full list of precautions, warnings, indications, and complications visit the QR code below. VIA™: The VIA™ Microcatheter is intended for the introduction of interventional devices (such as the WEB device/stents/flow diverters) and infusion of diagnostic agents (such as contrast media) into the neuro and peripheral vasculature. LVIS™ EVO™: The LVIS™ EVO™ Device is Indicated for use with neurovascular embolization coils in patients ≥ 18 years of age for the treatment of wide-neck (neck width ≥ 4 mm or dome to neck ratio < 2) saccular intracranial aneurysms arising from a parent vessel with diameter ≥ 2.0 mm and ≤ 4.5 mm. Contraindications: Use of the LVIS device is contraindicated under these circumstances: Patients in whom anticoagulant, anti-platelet therapy or thrombolytic drugs are contraindicated; Patients with known hypersensitivity to metal, such as nickel-titanium and metal jewelry; Patients with anatomy that does not permit passage or deployment of the LVIS device; Patients with an active bacterial infection; Patients with a pre-existing stent in place at the target aneurysm. Precautions: The LVIS device is provided sterile for single use only. Do not reuse, reprocess or resterilize. Reuse, reprocessing or resterilization may compromise the structural integrity of the device and/or lead to device failure which, in turn, may result in patient injury, illness, or death. Reuse, reprocessing, or resterilization may also create a risk of contamination of the device and/or cause patient infection or cross-infection, including, but not limited to, the transmission of infectious disease(s) from one patient to another. Contamination of the device may lead to injury, illness or death of the patient. Carefully inspect the sterile package and the LVIS device prior to use to verify that neither has been damaged during shipment. Do not use kinked or damaged components, or if the packaging is damaged. See the product label for the device shelf life. Do not use the device beyond the labeled use by date. Exercise caution when crossing the deployed/detached LVIS device with adjunctive devices such as guidewires, catheters, microcatheters or balloon catheters to avoid disrupting the device geometry and device placement. The LVIS device with neurovascular embolization coils may create local field inhomogeneity and susceptibility artifacts during magnetic resonance angiography (MRA), which may degrade the diagnostic quality to assess effective intracranial aneurysm treatment. The safety and effectiveness of the device has not been established in the treatment of large and giant wide‐neck intracranial aneurysms. The benefits may not outweigh the risks of treatment in patients with wide-neck intracranial aneurysms ≤ 5 mm in size, or reduced life expectancy, in the absence of additional risk factors for intracranial aneurysm rupture. The safety and effectiveness of the device has not been well established in the posterior circulation. Ensure that the specific embolization coil models and sizes used are indicated for the embolization of intracranial aneurysms. Potential Complications: The following potential risks and complications associated with general anesthesia, cerebral angiography, intracranial catheterization, intracranial stent placement or intra-saccular coil deployment have been identified below: Allergic reaction, including but not limited to: contrast dye, nitinol metal, and any other medications used during the procedure; Aphasia; Blindness; Cardiac Arrhythmia; Coil prolapsed or migration into normal vessel adjacent to aneurysm; Complications of arterial puncture including pain, local bleeding, local infection and injury to the artery, vein or adjacent nerves; Cranial neuropathy; Death; Device fracture, migration or misplacement; Dissection or perforation of the parent artery; Headache; Hemorrhage (i.e., intracerebral hemorrhage (ICH), subarachnoid hemorrhage (SAH), or retroperitoneal (or in other locations)); Hemiplegia; Hydrocephalus; Infection; Injury to normal vessel or tissue; Ischemia; Mass effect; Myocardial Infarction; Neurological deficits; Occlusion of non-target side branches; Pseudo aneurysm formation; Reactions to anti-platelet/anti-coagulant agents; Reactions due to radiation exposure; Reactions to anesthesia and related procedures; Reactions to contrast agents; Renal failure; Aneurysm rupture; Stenosis of stented segment; Seizure; Stent thrombosis; Stroke or TIA (Transient Ischemic Attack); Thromboembolic event (T/E); Vasospasm; Visual impairment. Potential Risks Associated with X-ray Exposure: The use of the LVIS device requires fluoroscopy, which presents potential risks associated with X-ray exposure. The risks of angiographic and fluoroscopic X-ray radiation doses to the patient include risks such as alopecia, burns ranging in severity from skin reddening to ulcers, cataracts, and delayed neoplasia that increase in probability as procedure time and number of procedures increase. The probability of adverse event occurrence increases as the procedure time and the number of procedures increase. Operators should take all necessary precautions to limit X-ray radiation doses to patients and themselves by using sufficient shielding, reducing fluoroscopy times, and modifying X-ray technical factors whenever possible. Hydrogel Embolic System: The HydroCoil Embolic System (HES) is intended for the endovascular embolization of intracranial aneurysms and other neurovascular abnormalities such as arteriovenous malformations and arteriovenous fistulae. The HES is also intended for vascular occlusion of blood vessels within the neurovascular system to permanently obstruct blood flow to an aneurysm or other vascular malformation and for arterial and venous embolizations in the peripheral vasculature. The device should only be used by physicians who have undergone pre-clinical training in all aspects of HES procedures as prescribed by MicroVention. For complete indications, contraindications, potential complications, warnings, precautions, and instructions, see instructions for use or visit QR code. SOFIA™: The SOFIA™ Flow Plus Aspiration Catheter with the Gomco™ 405 Aspiration Pump and Terumo Neuro™ Tubing Kit is intended for use in the revascularization of patients with acute ischemic stroke secondary to intracranial large vessel occlusive disease (within the internal carotid, middle cerebral – M1 and M2 segments, basilar, and vertebral arteries) within 8 hours of symptom onset. Patients who are ineligible for intravenous tissue plasminogen activator (IV t-PA) or who fail IV t-PA therapy are candidates for treatment. SOFIA™ Distal Access Catheter: The SOFIA Distal Access Catheter is intended for general intravascular use, including the neuro and peripheral vasculature. It can be used to facilitate the introduction of diagnostic and therapeutic agents. It is not intended for use in coronary arteries.
RX Only: Federal (USA) law restricts this device to sale by or on the order of a physician. For Healthcare Professionals Intended Use Only. Please refer to IFU for the full list of risks, contraindications, warnings, and precautions.
WEB™, SOFIA™, LVIS™, EVO™, HydroCoil™, MicroVention™ and Game-changing Impact™ are trademarks of MicroVention, Inc., registered in the United States and other jurisdictions. All brand names are trademarks or registered trademarks owned by TERUMO CORPORATION, its affiliates, or unrelated third parties. MM2110 07/2025 US ©2025 MicroVention, Inc.
