


Lewis, S., BSN, Morse, E., DNP, MPH, & Phillippi, R.D., PhD Belmont University Doctor of Nursing Practice Program
• A Step Ahead Foundation (ASAF) partners with clinical providers across Middle Tennessee to expand access to long-acting, reversible contraceptive methods (LARC).
• Accurate client tracking from initial contact to service delivery is essential to understanding service utilization, improving care coordination, and sustaining access to LARC.

Current workflow does not reliably capture patients' transitions across intake, scheduling, service delivery, and billing. Specifically, there is:
• No actionable insight into whether clients ultimately receive care
• Limited ability to evaluate missed opportunities for care or close gaps associated with care coordination
• There is no structured, time-sensitive follow-up process for missed appointments
This quality improvement project used the IHI Model for Improvement to strengthen client tracking from first phone call through billing and reimbursement. Specifically, the project aimed to:
• Identify what changes could improve tracking accuracy and reduce misclassified no-shows
• Test changes through workflow observation, key partner feedback, and a small 4-week pilot study.
Phase 1 – April–June: Discovery
• Retrospective review of utilization and billing data
• Identification of tracking gaps and misclassification patterns regarding "no-shows"
• Clarified operational definition of “true no-show”
Key Finding: 43% of individuals who called ASAF and scheduled appointments did not appear in the system as having received services.

Phase 2 – June–July: Workflow Mapping
• Identification of pilot site (partner clinic that serves the highest number of women who are uninsured)
• Observation of clinic workflow and documentation
• Mapping transitions from intake → scheduling → service delivery → billing

Phase 3 – August–October: Co-Design + Pilot
• Development of a standardized tracking process
• Drafting data capture and information sharing expectations
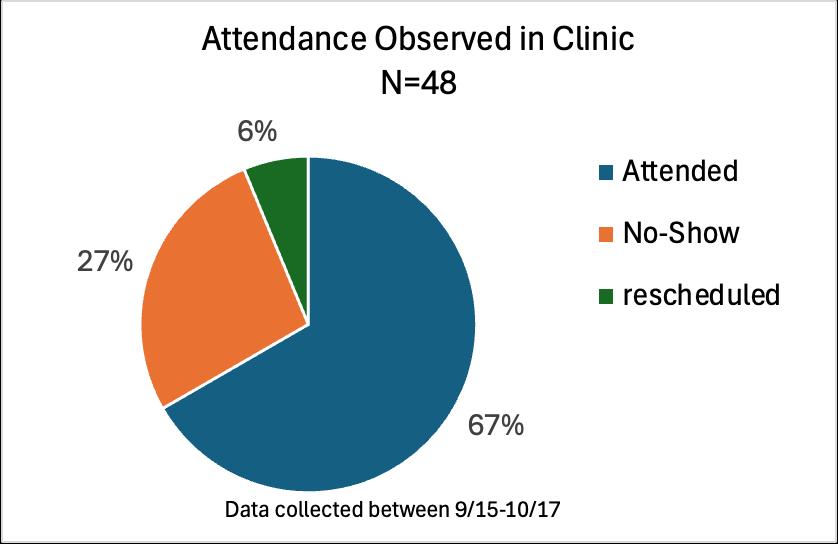
• Tracking "true no-shows" for discrete 4-week period at the pilot site
Key Finding:
Nearly 1/3 of clients scheduled appointments that they neither attended nor rescheduled, highlighting the need for timely and proactive follow-up.
True no-show rates are high among uninsured and underinsured clients, who experience greater structural barriers to accessing LARC.
Key Finding:

Documentation gaps occurred most often during handoffs between service delivery → billing.
Appointment attendance (or nonattendance) is not tracked or reported directly. Billing is a lagging indicator of patient attendance.
• More consistent and complete data collection improves equity, billing accuracy, and operational decision-making.
• Implementing a standardized tracking workflow is needed to ensure care coordination across multiple partner sites.
• Establishing a timely follow-up pathway for missed appointments will reduce preventable loss to follow-up among vulnerable clients.
• A central care coordination champion will be essential to promoting accountability and continuity.