
























































































This publication is dedicated to the residents and fellows of Bascom Palmer Eye Institute – past, present, and future. May you enjoy rewarding careers in service to your patients, institutions, and communities, while contributing to our understanding of vision disorders and diseases.
Bascom Palmer Eye Institute gratefully acknowledges the many Bascom Palmer physicians, alumni, and employees who contributed to this publication.
A special thank you to Steven J. Gedde, M.D., chair of Bascom Palmer’s 60th anniversary committee, for his invaluable contribution and unwavering support. Thank you also to chapter editors: Eduardo C. Alfonso, M.D., Douglas R. Anderson, M.D., Hilda Capó, M.D., John G. Clarkson, M.D., William W. Culbertson, M.D., Harry W. Flynn Jr., M.D., Thomas E. Johnson, M.D., Carol L. Karp, M.D., Byron L. Lam, M.D., Richard K. Lee, M.D., Ph.D., Richard K. Parrish II, M.D., and Vittorio Porciatti, D.Sc.
Thanks as well to our donors large and small. Bascom Palmer’s success in patient care, vision research, medical education, and community service would not be possible without the generosity of our friends who have provided support to the Institute since its founding.
This book draws on Twenty-Five Years of Vision, a history of Bascom Palmer Eye Institute written by Todd Ellenberg in 1987, The Chief, a biography of Edward W. D. Norton, M.D., written by John T. Flynn, M.D., in 2002, and Bascom Palmer Eye Institute: 50 Years of Vision written in 2012 by Richard Westlund.
Bascom Palmer Eye Institute, part of UHealth – University of Miami Health System, serves as the department of ophthalmology for the University of Miami Leonard M. Miller School of Medicine in Miami, Florida. U.S. News & World Report has ranked Bascom Palmer as the #1 ophthalmology program in the United States, an honor it has received for the 21st time since the publication began its annual rankings 33 years ago. Ophthalmology Times has also ranked the Institute as the best overall program in the United States numerous times, and Bascom Palmer’s ophthalmology residency program is ranked the best training program in the United States by Doximity, an online professional network for U.S. physicians.


In addition to its international reputation as one of the premier providers of eye care in the world, Bascom Palmer is the largest ophthalmic care, research, and educational facility in the southeastern United States. Each year, more than 285,000 patients with nearly every ophthalmic condition are treated, and more than 19,000 surgeries are performed.
In addition to treating patients at five locations in Florida (Miami, Palm Beach Gardens, Naples, Plantation, and Coral Gables), Bascom Palmer faculty members also staff the Miami Veterans Affairs Medical Center, Jackson Memorial Hospital, and Nicklaus Children’s Hospital. Additionally, the Institute has a long-standing relationship with community physicians in treating patients from the West Palm Beach Veterans Medical Center. The sponsored research enterprise at Bascom Palmer has grown from $3.8 million in 2004 to $16.6 million in 2021. For additional information, please visit www.bascompalmer.org.
Editor’s Note:
Endpapers of a book are typically beautifully decorated patterns or illustrations.
In honor of Bascom Palmer’s 60th anniversary, chose to display the history of the Institute’s signature magazine, Images, from its first issue in 1981 to the latest issue in January 2022. While I have had the pleasure of producing and editing Images for 20 years, would like to recognize and thank my predecessor, Debra Durant, who brought Images to light at its inception.
Marla Bercuson
Author
Richard Westlund
Editor
Marla Bercuson
Executive Director, Business Operations
Bascom Palmer Eye Institute
Kim A. Foster
Kim A. Foster Graphic Design
Elizabeth Lane Lawhorn Synapse
Printing Darren Taylor Miami Print Inc.
Photo Credits
Alexander Rodriguez Project Specialist Bascom Palmer Eye Institute
Donna Victor Photography Bascom Palmer Eye Institute Archives
Marketing Support
Natali Latorre Director, Marketing Healthcare Bascom Palmer Eye Institute
Jessica Fleitas Manager, Communications Bascom Palmer Eye Institute
Miami Hits A Million. That was the headline in 1962, the year the Magic City welcomed its one-millionth permanent resident, the year Bascom Palmer Eye Institute officially opened its doors as South Florida’s first academic center dedicated to vision care. Prospects for the burgeoning metropolis at the edge of Biscayne Bay were unlimited—and no man saw that more clearly than Edward W. D. Norton, M.D., founding director of Bascom Palmer. With his wit, charm, and uncompromising vision, he attracted talented clinicians and researchers who quickly began making major contributions to virtually every field of ophthalmology.
Six decades later, Bascom Palmer is one of the world’s leading eye institutes, known for excellence in vision research, clinical care, ophthalmic education, and community service. And much like our hometown, we have experienced growth. We have opened multiple locations throughout South Florida to provide our patients with convenient access to care. We have developed robust telehealth and virtual education services to connect with patients and vision professionals almost anywhere in the world. Furthermore, our scientists and clinicianresearchers are making important discoveries that hold the promise of better treatments in the future.
As we celebrate our 60th anniversary, I want to thank our devoted physicians, employees, trainees, philanthropic donors, and the leadership of the University of Miami for your deep commitment to excellence in every aspect of our operations. Thanks to your support, we can look forward to the future with great confidence.

Copyright @2022
Bascom Palmer Eye Institute ISBN 9780984944217
All rights reserved. No part of this book may be reproduced in any form or by any means without the prior, written permission of Bascom Palmer Eye Institute.
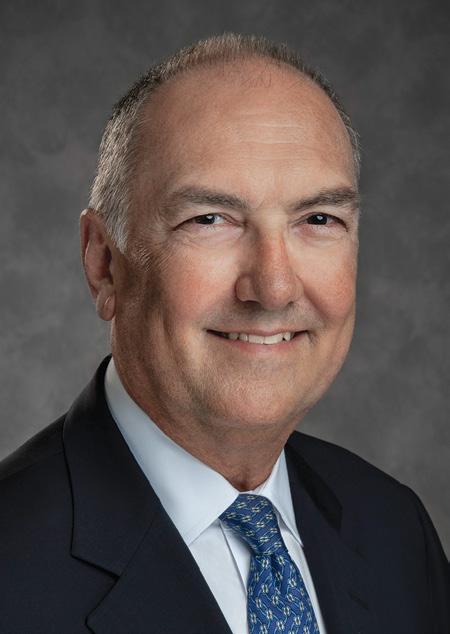
Eduardo C. Alfonso, M.D.
Kathleen and Stanley J. Glaser Chair in Ophthalmology Chair, Department of Ophthalmology, University of Miami Miller School of Medicine
Director, Bascom Palmer Eye Institute

Since its founding in 1962, Bascom Palmer Eye Institute at the University of Miami Miller School of Medicine has made multiple distinctive contributions to vision care in South Florida and around the world. By developing innovative diagnostic and treatment procedures, training generations of skilled professionals, and delivering compassionate clinical care, Bascom Palmer’s clinicians, scientists, trainees, and staff members have touched the lives of millions of patients around the world.
“For six decades, we have been dedicated to delivering the best possible vision care to patients and finding effective treatments for blinding diseases,” said Eduardo C. Alfonso, M.D., director and chair of Bascom Palmer Eye Institute, and the Kathleen and Stanley J. Glaser Chair in Ophthalmology. “We are also committed to serving our diverse South Florida community and beyond to promote equitable access to excellent vision care.”
Guided by the vision of founding director Edward W.D. Norton, M.D., the Institute has grown from a modest program with two full-time faculty members to the largest ophthalmic care, research, and educational facility in the southeastern United States, providing care to more than 285,000 patients annually.
Norton and his successors have all been committed to advancing the Institute’s mission: “To enhance the quality of life by improving sight, preventing blindness, and advancing ophthalmic knowledge through compassionate patient care, innovative vision research, and education.”
One indicator of their success is Bascom Palmer’s #1 ranking as the nation’s best in ophthalmology by U.S. News & World Report – the 21st time, and the 19th consecutive year that the Institute has received the top ranking since the publication began
surveying U.S. physicians for its annual “Best Hospitals” rankings 33 years ago.

Bascom Palmer’s multidisciplinary research program has also grown through the decades and covers a broad spectrum, from the most basic investigations of molecules, cells, and tissues involved in the sense of vision, to the development of devices for new clinical applications, including telehealth, artificial intelligence, and computer-augmented vision to transform vision diagnostics and personalized vision correction.
Reflecting on his 42-year career at Bascom Palmer, Paul F. Palmberg, M.D., Ph.D., professor of ophthalmology, said, “It is wonderful to see the fulfillment of Dr. Norton’s dream of a world-class center for clinical care, teaching, and research and to see the torch of empowerment passed from generation to generation.”
A longtime dream
Back in 1923, Bascom Headon Palmer, M.D., opened one of Miami’s first ophthalmology practices. Palmer was the first surgeon in Florida to perform corneal transplants. He was also an active volunteer with the Miami Lighthouse for the Blind and helped create community outreach programs.
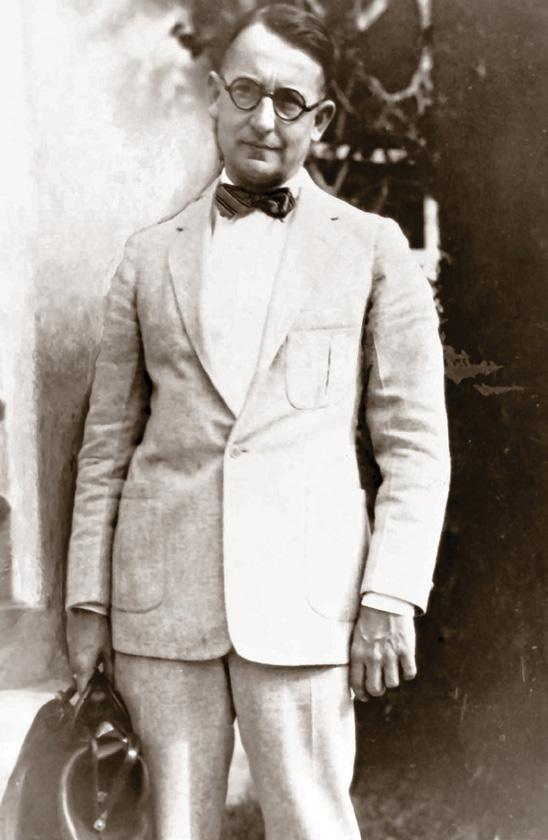
In 1943, amid World War II, Palmer began discussing the feasibility of establishing an eye clinic in Miami dedicated to saving sight and preventing blindness. Five years later, the Miami Lighthouse purchased land for the proposed clinic. However, there were no funds available for design or construction.
In 1952, the University of Miami established a School of Medicine, and at Palmer’s urging, created the division of ophthalmology in the department of surgery for the 1954-55 school year.
“Miami will eventually be home to an ophthalmology institute in a medical center second to none in the nation.”
– Bascom H. Palmer, M.D.
“Dr. Curtin was also known as the conscience of Bascom Palmer Eye Institute. Whenever Dr. Norton faced an ethical dilemma, he would turn to Dr. Curtin for advice.
Dr. Norton himself was a man of the highest integrity, and he knew a discussion with Dr. Curtin would provide a consensus of two honest men.”
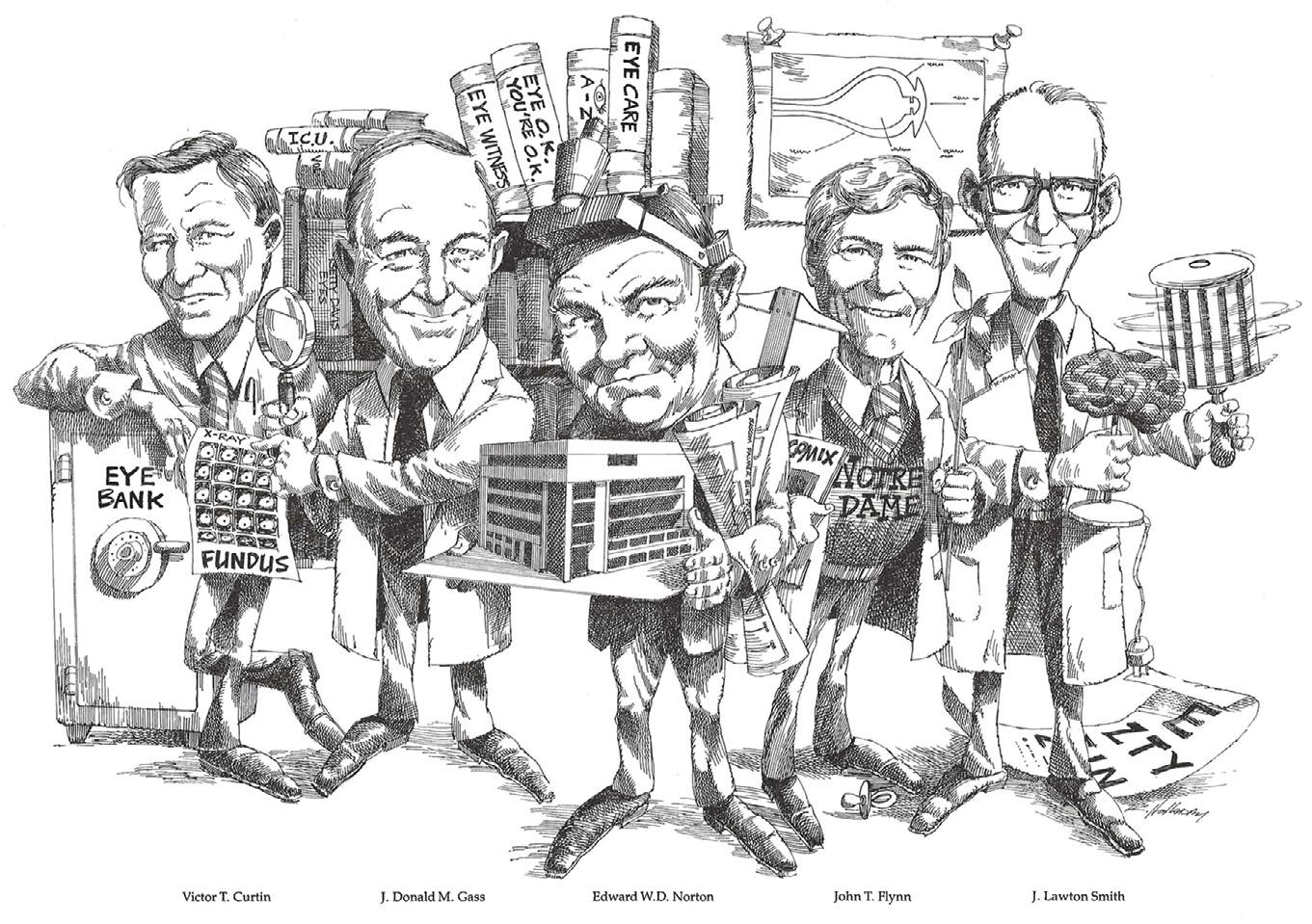
The founding five ophthalmologists were (left to right) Lawton Smith, M.D., John Flynn, M.D., Donald Gass, M.D., Edward Norton, M.D., and Victor Curtin, M.D.

Before Palmer died on September 4, 1954, he outlined his hope that Miami would eventually be home to “an ophthalmology institute in a medical center second to none in the nation. It will be a clinic where both the indigent and others may be treated. It will serve this community as a clearinghouse for research and reliable information on the care of the eyes and the conservation of sight.”
The arrival of “The Chief”
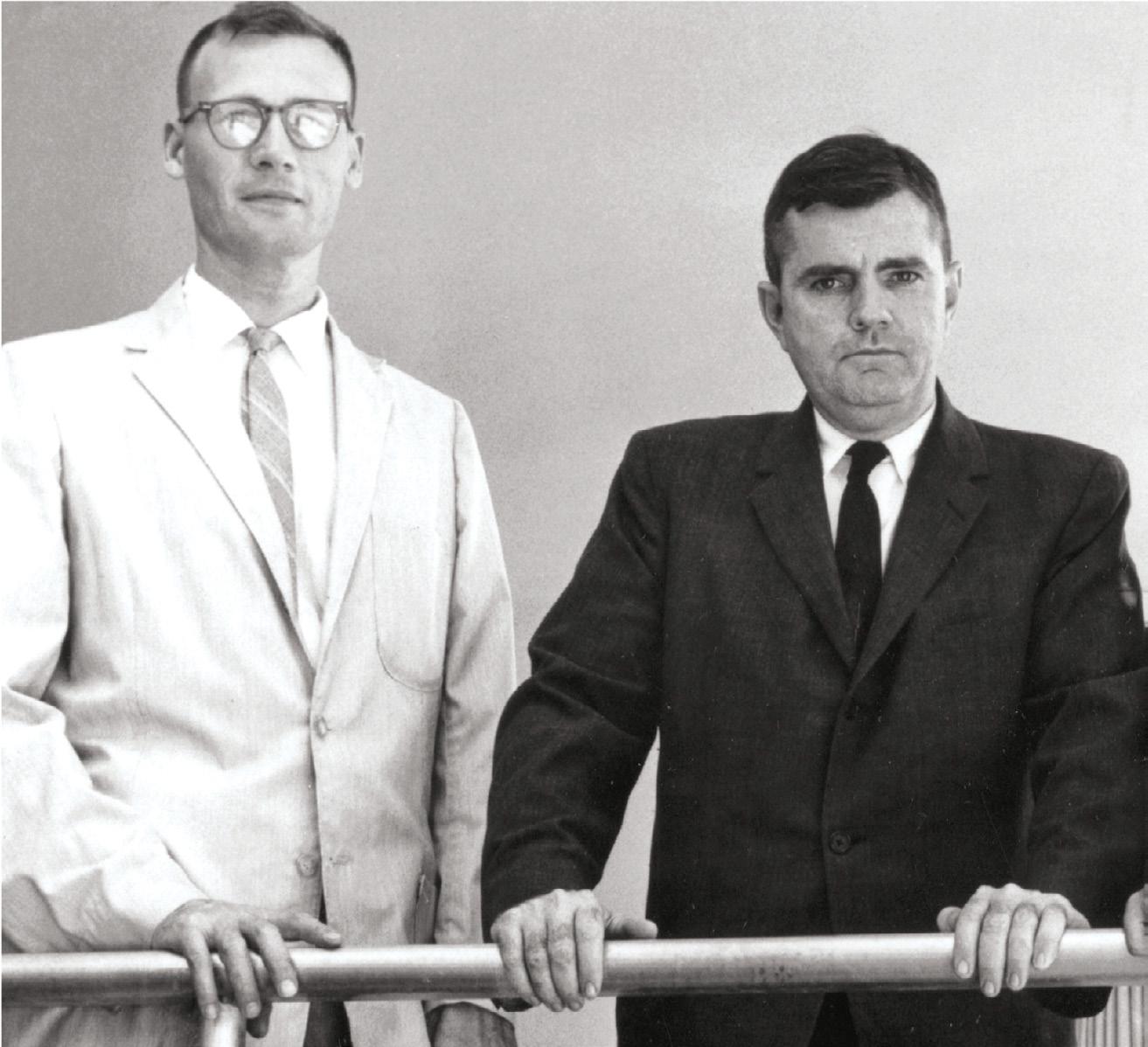
In December 1957, upon his first visit to the University of Miami, Norton said, “When I looked at the city of Miami, I realized this city had great potential and I thought that we could develop a very good department here.” A month later, John Farrell M.D., chair of the department of surgery at the young school of medicine, selected the 35-year-old Norton, an excellent neuroophthalmologist, master retinal surgeon, and assistant professor of surgery at Cornell Medical Center, to be the chief of the division of ophthalmology at an annual salary of $10,000. Norton would be known as “The Chief” throughout his career.
Driven by a desire to make a lasting contribution to the field of ophthalmology,
Norton set to work to build a nationally recognized ophthalmology program and an eye clinic that would fulfill a long-standing community dream. Joining Norton in this quest was Victor T. Curtin, M.D., who had completed his residency with Norton at Cornell from 1955-1958. Curtin and Norton took and passed their Florida medical boards together in 1958.
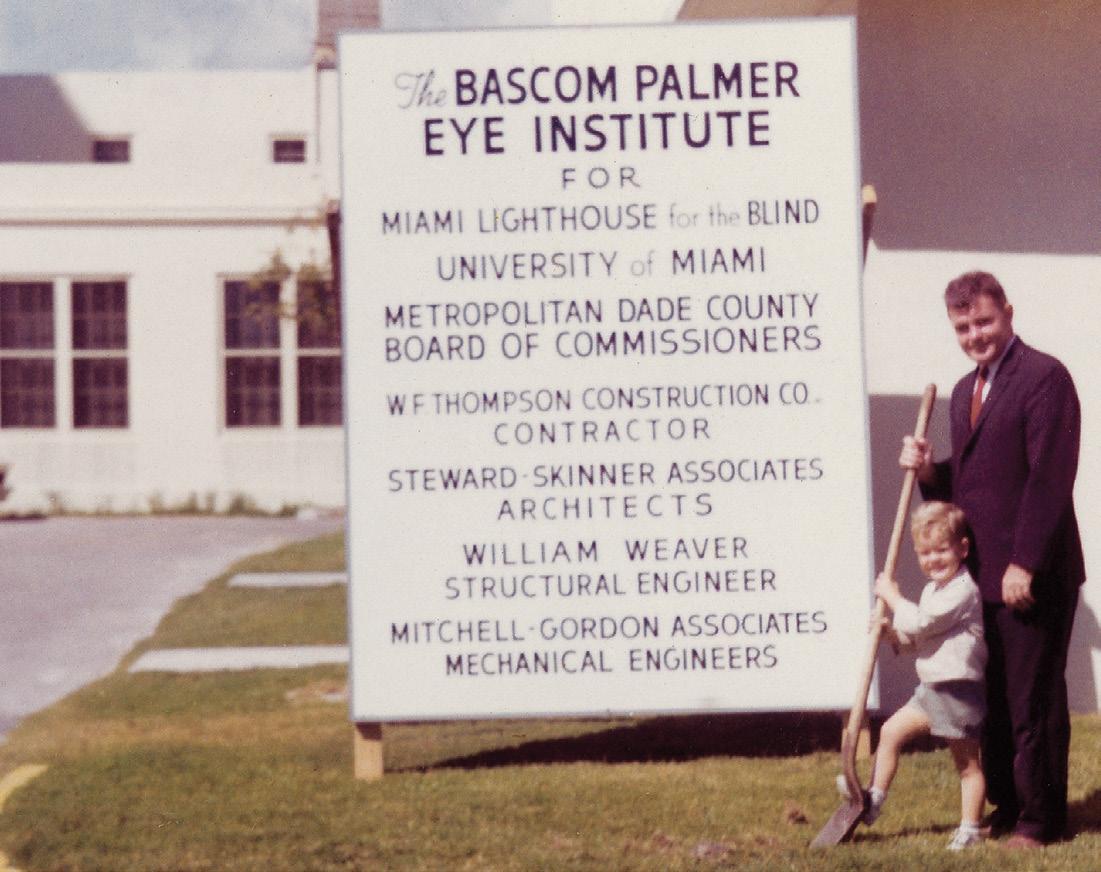
Along with his clinical and teaching responsibilities, Norton soon established a close relationship with the Miami Lighthouse, which set aside $200,000 in 1959 to build an eye institute. Norton also became friends with leaders of the Florida Lions Club, which led to the formation of the Florida Lions Eye Bank.
While the donation from the Miami Lighthouse had increased to $305,000 by 1961, the construction bid on the project was $510,378 – $200,000 more than they had in hand. To obtain the balance, Norton and Kenneth Whitmer, M.D., a longtime Miami ophthalmologist, paid a visit to Claude Hemphill, a founder and chair of the CIT Finance Corporation in Tampa. He agreed to donate the needed funds on the condition that construction begin immediately. The ground was broken on March 6, 1961, and
work began the next week. It took less than a year to complete the four-story medical building, designed by Miami architects John Skinner and Harold Stewart.
When Bascom Palmer Eye Institute opened its doors on January 21, 1962, no one could have foreseen that it would become one of the world’s leading centers. At that time, there was no hospital dedicated to only eye surgery in Florida or anywhere else in the Southeast United States. The largely voluntary faculty members of the University of Miami School of Medicine’s division of ophthalmology had only one operating room at Jackson Memorial Hospital available for eye surgery, three half-days per week. There were no specialized surgical tools for residents, and the operating room was neither configured nor lighted for eye surgery. It was hardly an ideal situation for clinical care, medical education, or research. However, “The Chief” focused on building a center that would offer the highest level of clinical care and bring advanced treatments to the South Florida region. Under Norton’s leadership, Bascom Palmer attracted a remarkable collection of talented
ophthalmologists who flourished in the Miami sunshine. In less than a decade, the new department of ophthalmology had become a national center of medical excellence.
– Douglas Anderson, M.D. These first ophthalmologists became known as Bascom Palmer’s “founding five” as they were the initial clinical faculty members for several years before others joined the team.
“Dr. Norton chose quality people and then let them decide where they could make the greatest contribution,” said Douglas Anderson, M.D., a professor emeritus of ophthalmology. “When I arrived in 1969, he told me that my job would be to become the best ophthalmologist of which I was capable.”
For the first three years, Norton and Curtin were the only full-time faculty members in the department of ophthalmology. They would discuss cases and bounce ideas back and forth. Throughout their long professional partnership, Norton relied on Curtin to handle a variety of administrative projects while also seeing patients, interviewing residency candidates, and maintaining the department’s high standards.
As a researcher, Curtin tracked ocular tumors in patients with small or medium melanomas. “Rather than remove the eye right away, our study found that monitoring the tumor was a better strategy,” he said. “So, we were able to preserve vision in many patients.” Throughout his life, Curtin was devoted to better treatments of retinal diseases and advancing ophthalmic pathology.
J. Lawton Smith, M.D., Norton’s choice for the third faculty member, focused his practice on diagnosing neurological disorders and soon became one of the nation’s top neuro-ophthalmologists. An exceptional teacher, he organized the nation’s first clinical postgraduate educational session devoted to neuro-ophthalmology in 1963 and continued the annual Bascom Palmer Neuro-Ophthalmology Course for more than 15 years.
J. Donald M. Gass, M.D., who joined the faculty in 1963, studied diseases of the macula and became a pioneer in the emerging field of fluorescein angiography, a technique in which intravenously injected dye allows the blood vessels in the eye to be
photographed in detail. Known as the “Father of Macular Diseases,” Gass conceptualized how macular holes form, creating the foundation for surgery on a formerly untreatable condition.
In his nearly 40 years at Bascom Palmer, Gass revolutionized the diagnosis and treatment of more than a dozen macular and vitreoretinal disorders. He also wrote the Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment, one of the most important ophthalmological texts. In a fitting tribute to his career, in 1999, the Association of Cataract and Refractive Surgeons named Gass as one of the 10 most influential ophthalmologists of the 20th century. His knowledge of chorioretinal diseases is unparalleled in the history of ophthalmology.
After joining the faculty in 1965, John T. Flynn, M.D., launched a treatment program for amblyopia (“lazy eye”) in pediatric patients. He studied retinopathy of prematurity (ROP), known in the 1960s as retrolental fibroplasia, a condition that can lead to blindness in serious cases. He developed an international five-stage classification for ROP and the first accepted therapy for the disorder. Supported by a $1.2 million grant awarded by the National Eye Institute, he published a major study in 1984 examining the various risk factors for the condition. Noting his lifelong research interest in this condition, Flynn said in 2011, “I’m still working on ROP.”
These first ophthalmologists became known as Bascom Palmer’s “founding five” as they were the initial clinical faculty for several years before others joined the team.
In addition to experts in clinical care and teaching, Norton launched the department of ophthalmology’s laboratory research program soon after his arrival. In 1960, from the University of Miami’s department of psychology, he recruited Thorne Shipley, Ph.D., an expert in binocular and color vision whose research focused on neuro-physiology.


Two years later, Norton hired Duco I. Hamasaki, Ph.D., a researcher focused on neurophysiology who soon became known for his electrophysiological single-cell studies and his work on retinal pigments. Shipley and Hamasaki were laboratory scientists who rounded out the five clinicians as the initial faculty members and laid the foundation upon which the Institute’s basic science research program was built. As Hamasaki said, “I came to Bascom Palmer because Dr. Norton had a strong commitment to research, as well as teaching and patient care.”
As future chair, John Clarkson, M.D., said, “Perhaps the most remarkable thing about those early days was Dr. Norton’s ability to choose that first group of faculty members. All of them were extraordinary clinicians and educators. Through the years, our advances in clinical care, research, and education have all begun by selecting people with skills and integrity who always put the patient first.”
Throughout the 1970s, Bascom Palmer attracted new faculty members who would
go on to leave their mark on the field of ophthalmology as clinicians, researchers, educators, and administrators. In 1972, Bascom Palmer hired its first female faculty member, Mary Lou Lewis, M.D., who had just completed her fellowship in vitreoretinal diseases. “Bascom Palmer was a great place to work, but a few patients were uncomfortable because I was a woman,” said Lewis. “I received a lot of support from the staff.”
During the 1970s, Lewis primarily performed retinal detachment and vitreoretinal surgeries. In 1979, she began work on the Macular Photocoagulation Study, evaluating whether laser surgery could improve the vision in patients with macular degeneration. “Lasers are now passé because it is easier to treat the condition medically with injections,” said Lewis, who retired in 2001.
For Bascom Palmer, the 1970s was a decade of remarkable growth. It became evident that the Institute had outgrown its original

building and would need a new and much larger eye hospital. In these early years, one of Norton’s many priorities was raising funds to build this new center. He reached out to Anne Bates Leach, a resident of Palm Beach and a grateful patient of the Institute. She contributed more than $1.5 million and received additional support from her friends in the Southern Dames of America, including Celeste Sanford, who donated more than $1 million to the hospital fund.
With that private-sector support and bond money from the University of Miami, about $6 million was available to build a state-ofthe-art, seven-story facility on a 1.54-acre site at 900 NW 17th Street. Norton hired Hilario Candela, FAIA, lead architect of the Miami architectural firm Spillis Candela. The exterior of the building was designed with poured concrete and steel that reflected the mid-century modern architectural style with curves that softened the interior. Norton and Candela were able to work collaboratively with the leadership of the City of Miami and its mayor Maurice A. Ferre, the Public Health Trust, and with the leadership of the University of Miami, including its president Henry King Stanford to accomplish this seminal project in the history of the Institute.

Three years after breaking ground, the new Anne Bates Leach Eye Hospital opened in July 1976. George Blankenship, M.D., did the first procedure in the hospital’s new operating rooms that October. “The entire faculty loved the new hospital,” said Lewis. “It had well-designed examining rooms, and the operating suites were very well equipped. It provided a very nice, welcoming atmosphere for our patients.”
When the hospital opened, floors one and two were used for outpatient clinics, floors three and floor were uncompleted shell space, and floors five and six were dedicated to surgery and patient beds, while Bascom Palmer’s ophthalmic library was designed for the lower level. The hospital was originally licensed for 100 beds. Today as ophthalmic care has shifted to fewer hospitalizations, and most surgeries are performed on an outpatient basis, the facilities have been transformed accordingly to serve patients in a state-of-the-art facility.
With the opening of the Anne Bates Leach Eye Hospital, the Institute’s original building was renamed the William L. McKnight Vision Research Center. McKnight, a grateful patient and retired chair of the 3M Company, had donated $2.5 million for vision research.

One of the major advancements of the early 1980s was the completion of the Edith and Earl Retter Education Center, a stateof-the-art teaching facility connected to the eye hospital by an enclosed skywalk. Other projects included the renovation and expansion of two floors of the McKnight Vision Research Center, expanding the Ophthalmic Biophysics Laboratory, and creating the Ophthalmic Microbiology Laboratory. In 1983, the Florida Lions Eye Bank and Ocular Pathology Laboratory moved from the McKnight building to the third floor of the eye hospital where they remain today. A new capital campaign to expand the Institute’s research facilities brought further progress. “In the early 1980s, I asked Dr. Norton how additional researchers could be accommodated, and his reply astonished me,” said Palmberg. “He said, ‘When our building was constructed in 1962, we made sure that the foundation could support expansion to eight stories, and we already have funds for the work.’”
On October 17, 1985, the ground was broken for the $5.5 million expansion of the McKnight Vision Research Center. Taking part in the ceremony was Evelyn McKnight, whose $4 million gifts in honor of her husband helped to fund the addition of four floors to the original building. The expansion project increased the building’s total space to 70,000 square feet. However, no additional structural work was needed because of Norton’s foresight. Upon its completion, the building was rededicated as the Evelyn F. and William L. McKnight Vision Research Center. In 1985, Charlotte Breyer Rodgers, an heir to the Breyer’s Ice Cream founder, donated more than $5 million to establish a professorship in ophthalmology and the Charlotte Breyer Rodgers Research Pavilion in the McKnight Vision Research Center. Northwest 10th Avenue, the street between the eye hospital and the research center, became a pedestrian mall. Rodgers also created an endowment fund to establish a flower garden between the two buildings, now fondly known as “The Breyer Patch.”

Another major gift came from James L. Knight, chair emeritus of Knight-Ridder Newspapers, Inc. He contributed $5 million to complete the addition of the McKnight Center in 1988 and to further endow its vision research activities.
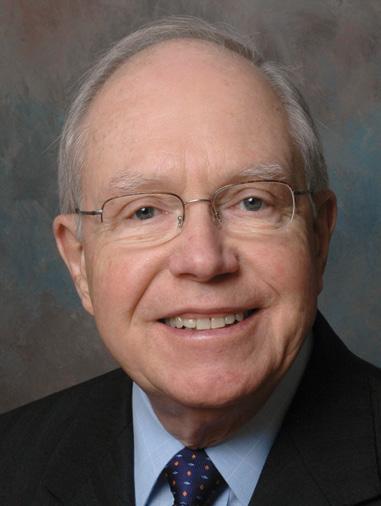
Following Norton’s 1991 retirement, Clarkson, a graduate of the Institute’s training programs, became the Institute’s second chair. After graduating from the University of Miami School of Medicine, he completed his ophthalmology residency at Bascom Palmer, became chief resident, and joined the faculty in 1975. Under Clarkson’s leadership, the Institute steadily attracted more women residents, fellows, and faculty members. “By the time I became chair, more than half of our residents were women,” he said. “That reflects a positive change – not just in our program, but medicine nationally as well.”
Recognizing the national shift to a managed care system, Clarkson developed the Bascom Palmer Eye Care Network, including ophthalmologists and optometrists who would provide primary care in their offices and refer patients to Bascom Palmer for more complicated issues. He also led a $10 million capital campaign to complete the interior of the hospital’s fourth floor, which included expanded services for children, glaucoma, and oculoplastics.
Among the first contributors were William and Norma Horvitz, who had a special interest in pediatric eye care. “We hope that more children will have the opportunity to receive earlier ophthalmic treatment and thus avoid some of the vision miseries of later life,” they said at the time. By the mid1990s, more than 7,000 children were treated
each year at the newly renamed William and Norma Horvitz Children’s Clinic, including many referrals from the Caribbean and Latin America.
In 1994, Bascom Palmer for the first time was ranked “Best in Ophthalmology” in the United States by ophthalmologists surveyed by U.S. News & World Report for its annual Best Hospitals issue. Shortly after learning of that honor, Norton died at age 72. Reflecting on his mentor, Clarkson said, “Dr. Norton saw himself as a gardener. His role was to till the soil, plant the seeds, pull the weeds, and stand back and watch the luxuriant growth. Right from the start, Dr. Norton inspired openness and trust. That transparency and integrity created a foundation that allowed Bascom Palmer to grow in reputation and strength.”
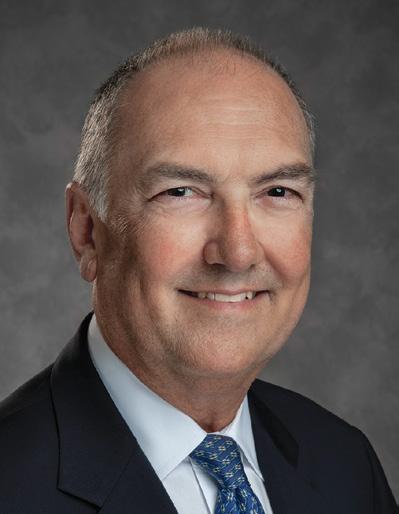
Two years later, Clarkson became dean of the medical school, while continuing to see ophthalmology patients. Glaucoma specialist Richard K. Parrish II, M.D., who had completed a fellowship in 1982 before joining the faculty, succeeded him. “We’re excellent, but how can we become even better?” he asked at the time. “That will come by making decisions in the best interest of our patients, the acquisition of medical knowledge, and society at large,” he said.
Parrish’s priorities included improving the Institute’s computer network and taking advantage of the rapidly evolving Internet to connect with ophthalmologists in other countries. “I foresee having real-time interactive videos so that whether you’re in Maracaibo or Madrid, you’ll be able to key in Bascom Palmer and find out what’s being presented at Grand Rounds or in our courses for practicing physicians.”
Responding to the changing healthcare landscape, Parrish also recognized the
importance of building new networks, including the Institute’s first satellite facility in Palm Beach County. On November 17, 1996, Parrish, Clarkson, and other faculty members celebrated the grand opening of Bascom Palmer Eye Institute of the Palm Beaches. More than 240 Bascom Palmer friends and benefactors attended the reception in the 5,000-square-foot medical leased office made possible by major gifts from the Walter G. Ross Foundation and The Jewish Guild for the Blind.
In 1999, Parrish, who holds the Edward W. D. Norton Chair in Ophthalmology, stepped down as Institute chair to spend more time on his glaucoma research, residency education, and clinical care, as well as editing a comprehensive reference textbook, the Bascom Palmer Eye Institute Atlas of Ophthalmology, a collaborative effort of the entire faculty published in 2000.



From 1999 to 2001, Richard K. Forster, M.D., served as Bascom Palmer’s interim chair as a nationwide search was underway. Forster, who completed a residency in ophthalmology and served as chief resident at Bascom Palmer in 1970, said, “My focus was to maintain our culture and values. We continued to provide the best possible patient care, educate physicians, residents, and medical students, and maintain our ongoing research without missing a beat.”
While Forster enjoyed his two-year tenure, the corneal and external diseases specialist said he was happy to return to clinical responsibilities, including regular trips to treat patients in Palm Beach Gardens. “It was a good two years,” he said, “and we kept Bascom Palmer moving forward.”
Into the 21st century
In 2001, Carmen Puliafito, M.D., M.B.A., was
selected to lead Bascom Palmer into the new century. An author, inventor, teacher, surgeon, and researcher, Puliafito was the founding director of the New England Eye Center and chair of the department of ophthalmology at Tufts University. A vitreoretinal specialist, he was a co-inventor of optical coherence tomography (OCT), which produces clear images of retinal tissue during a non-invasive examination.
As the first chair from outside the Institute, Puliafito became an agent of change, advancing Bascom Palmer’s missions of clinical care, education, vision research, and community service. Under his leadership, the size of Bascom Palmer’s clinical faculty doubled to 70, including more women and minorities. For instance, Hilda Capó, M.D., became Bascom Palmer’s first Hispanic female professor of ophthalmology in 2002. As a pediatric ophthalmologist, she emphasized preserving the vision of Bascom Palmer’s youngest patients.
Along with recruiting faculty members, Puliafito expanded Bascom Palmer’s residency program from six to seven physicians a year. In 2002, the Institute was named “Best Residency (Teaching) Program” by Ophthalmology Times, which annually ranks the top ophthalmology programs in the United States. He also strengthened Bascom Palmer’s research program by attracting more grants and private donations. “We succeeded in regaining Bascom Palmer’s core research grant from the National Eye Institute,” he said. “Over the next few years, we moved into the top ten in terms of NIH research grants. We also recruited eight scientific researchers and established a Center for Molecular Ophthalmology.”
Under Puliafito’s direction, Bascom Palmer regained the No. 1 ranking in U.S.
Bascom Palmer’s core research grant from the National Eye Institute. Over the next few years, we moved into the top ten in terms of NIH research grants. We also recruited eight scientific researchers and established a Center for Molecular Ophthalmology.”
“We’re excellent, but how can we become even better? That will come by making decisions in the best interest of our patients, the acquisition of medical knowledge, and society at large.”
– Richard Parrish II, M.D.John Clarkson, M.D.
“We succeeded in regaining
– Carmen Puliafito, M.D.Richard Parrish II, M.D. Carmen Puliafito, M.D. Richard Forster, M.D.
World Report’s rankings of eye hospitals in 2004, three years after his arrival, and it has maintained that position every year since.
With growing patient volume, he planned a major renovation of the Anne Bates Leach Eye Hospital. That resulted in significant improvements throughout the hospital, including expansion of the surgical suites, remodeling of the retina, cornea, glaucoma, and children’s centers, and creation of a new lobby, as well as additional patient waiting areas. “Our goal is to serve our patients and to bring safe and effective treatments to them as soon as possible,” said Puliafito.
In 2004, the Vision Van was donated to Bascom Palmer by the Josephine Leiser Foundation, thanks to the generosity of a longtime patient who dreamed of providing free eye care to the medically underserved. It has been used to bring mobile eye care services to communities throughout South Florida as well as emergency assistance to victims of natural disasters.
The next year, a gift from Estelle and George G. Rosenfield led to the creation of the Imaging and Macula Center. Containing the most up-to-date and advanced ophthalmic photography equipment, the center allowed the Institute’s ophthalmologists to perform advanced diagnostic procedures.

One of Puliafito’s priorities was expanding Bascom Palmer’s geographic reach in the South Florida region. In 2004, Bascom Palmer leased medical office space at Naples


Community Hospital and in Plantation in keeping with the Institute’s long–time commitment to serving the region. He also led a $22 million capital campaign to build a permanent facility in Palm Beach Gardens.
Located on a 7.4-acre campus on PGA Boulevard in the PGA National development, the Bascom Palmer Eye Institute at Palm Beach Gardens opened in 2006. The campus included the Maltz Center, a 40,000-squarefoot patient care facility made possible with the generous support of Milton and Tamar Maltz, and the Frankino Pavilion, an adjacent 10,000-square-foot ambulatory surgical center, made possible with support from Connie and Sam Frankino.
“This state-of-theart medical facility is the University of Miami’s first major construction project outside Miami-Dade County,” said Donna Shalala, president of the University of Miami at the time. “It reflects our commitment to serving the region’s fast-growing population while continuing to provide the finest academic medical programs in the state.”
In 2007, Puliafito left Bascom Palmer to become dean of the Keck School of Medicine at the University of Southern California. Eduardo Alfonso was named interim chair,
and the national search concluded that the strongest candidate was already at Bascom Palmer. “Dr. Alfonso embodies the best of Bascom Palmer’s tradition,” said Forster, who served on the search committee. “He’s a fine individual with the skills to ensure a bright future for our Institution.”
A native of Cuba, Alfonso grew up in Puerto Rico before moving to the United States to attend college and medical school completing both degrees at Yale University.
In 1984, he completed his residency in ophthalmology at Bascom Palmer before completing fellowships in ophthalmic pathology, cornea and external diseases, and ophthalmic research at the Massachusetts Eye and Ear Infirmary of Harvard University. He joined the Bascom Palmer faculty in 1986. A specialist in corneal transplants and corneal infections, Alfonso has been a world leader in the development and clinical applications of artificial corneas, a significant issue for patients in developing nations without readily available donor transplant tissue as well as in the diagnosis and treatment of severe corneal infections.
Under Alfonso’s leadership, Bascom Palmer continues to move forward with an aggressive agenda of internal and external growth. “We will always continue to improve all of our systems to provide better patient care, nurture our researchers, and enhance our educational programs,” he said.
This ambitious agenda included a three-day global scientific meeting held in February 2012, when Bascom Palmer
celebrated its golden anniversary. Nearly 650 ophthalmologists from around the world, including 300 Bascom Palmer alumni, attended the conference at the Biltmore in Miami. With 180 distinguished presenters, topics in the ever-changing field of ophthalmology ranged from research breakthroughs in cataract surgery and gene therapy to targeted goals of new clinical trials on the treatment of glaucoma and optic nerve diseases.
Alfonso has focused on growing the philanthropic endowment to support the growth of faculty and staff, the facilities, and the educational, research, and community service programs. Remodeling of the Anne Bates Leach Eye Hospital by converting administrative offices into additional clinical space has led to the establishment of the Shirley and L. Jules Arkin Laser Vision Center, the Cornea Imaging Center, the Samuel and Ethel Balkan International Pediatric Glaucoma Center, and multiple upgrades to existing clinical space. Advancements
in 2015 included an expansion of clinical space at the Plantation center which included the new Ocular Surface Center. That year featured the opening of the new Bascom Palmer Eye Institute at Naples, a $25 million state-of-the-art, award-winning clinical care and ambulatory surgery center where an extensive array of clinical and surgical services, research clinical trials, and medical education seminars are offered. In 2017, Bascom Palmer opened at the Lennar Foundation Medical Center in Coral Gables.
In 2019, the third building on Bascom Palmer’s Palm Beach Gardens campus, a $15 million project, was opened – the Lois Pope Center for Retinal & Macular Degeneration Research. The Center is equipped with the latest research, diagnostic and imaging technology, and training facilities. It serves as the premier hub of national and international clinical research studies on new treatments for retinal and macular diseases. Bascom Palmer also increased its care of patients in the Middle East and began construction of a new eye center in Abu Dhabi, slated to open in 2023.
Also continuing to grow are Bascom Palmer’s laboratory and vision research facilities located within the McKnight Vision Research Center and the Stem Cell Institute. These include: The Adrienne Arsht Hope for Vision Laboratory; Ophthalmic Biophysics Center; Artificial Intelligence and Computer Augmented Vision Laboratory; Miami Integrative Metabolomics Research Center; William Thode Ocular Microbiology Center; Dr. Nasser Ibrahim Al-Rashid Orbital Vision Research Center; Dr. Lola Gisela Rais de Lerner Clinical Trials Unit; and the Mark
J. Daily Inherited Retinal Diseases Center. The Institute has maintained robust support for its research programs from the National Institute for Health and the National Eye Institute (NIH/NEI), and foundations like Research to Prevent Blindness, Fight for Sight, and others.
The establishment of the EPIC Kaleidoscope Electronic Health Record System in 2012 was a major investment that has led to a marked improvement in clinical care, research, and education. Bascom Palmer pioneered the module for eye care and has been one of the early adopters, resulting in collaborative clinical research with vision institutes worldwide. In addition, a significant level of collaboration has existed with the American Academy of Ophthalmology’s Intelligent Research in Sight (IRIS) Clinical Registry, which has tracked clinical outcomes, thus identifying areas for continued clinical improvement.
Philanthropy fuels the Institute’s educational mission. The total remodeling of the Edith and Earl Retter Education Center was made possible by a gift from the family of Dr. José Berrocal. The Global Center for Ophthalmic Education was also established with gifts from the Braman Family Foundation. To continue to support both the education and academic missions in perpetuity, the Institute’s endowment has grown by more than 50% in the last ten years. During that same time period, the number of endowed chairs held by faculty members has grown from eight to 18 endowed chairs and one professorship. The education and leadership missions of the Institute have also been evident in regional, national, and
international organizations including the International Council of Ophthalmology, the Pan American Association of Ophthalmology, the American Academy of Ophthalmology, the Association for Research in Vision and Ophthalmology, the Florida Society of Ophthalmology, the Miami Ophthalmological Society and many other specialty groups and societies.
Through Bascom Palmer Eye Institute’s leadership role at the University of Miami, the Miller School of Medicine, and the University of Miami Health System, major achievements have been attained. For example, the centralization of key clinical administrative operations included the implementation of the electronic health record EPIC and Kaleidoscope – its eye care module, and the consolidation of hospital licenses into one single hospital system – the University of Miami Hospital and Clinics, thus changing the Anne Bates Leach Eye Hospital from a hospital to a center. The Bascom Palmer Eye Institute gained recognition by the University of Miami Board of Trustees as an Institute at the University and a Translational Institute at UHealth, the other being the Sylvester Comprehensive Cancer Center.
For Bascom Palmer, the COVID-19 pandemic posed perhaps the biggest challenge the Institute faced in six decades. In March 2020, the rapid spread of the coronavirus forced a shutdown of nonemergency clinical services to patients, the suspension of research activities, and cancellation of the in-person educational
programs. The Institute responded with new resilient and effective protocols to protect patients, physicians, and staff while continuing to provide all of its services, most importantly, emergency eye care.

Supported by technology staff members, Bascom Palmer’s physicians began offering telehealth consultations and assessments, followed by “hybrid” visits, to maximize patient safety and minimize in-person clinical services. “Through emergency surgery, timely clinic visits, video conferences, and old-fashioned phone calls, our physicians continued providing the best possible patient care despite the many challenges of COVID-19,” said Alfonso.
The pandemic also affected the Institute’s research program, forcing a temporary halt to clinical trials and some laboratory projects. However, many scientists and clinicians made significant contributions to timely COVID-19 studies regarding the impact of the virus on optical tissues.
In training and medical education, faculty members took advantage of the worldwide move to video platforms to offer new learning programs such as virtual Grand Rounds “attended” by physicians, residents, and medical students from throughout the U.S. and beyond.
Looking back on the crisis, Alfonso said, “I am very proud of our team’s resiliency and ability to adapt to changing conditions. The pandemic allowed us to critically examine our processes and develop new ideas, instruments, and protocols that will serve patients, education, and research now and into the future.”

“I am very proud of our team’s resiliency and ability to adapt to changing conditions. The pandemic allowed us to examine our processes critically and to develop new ideas, instruments, and protocols that will serve patients, education, and research now and into the future.”
– Eduardo Alfonso, M.D.The real heroes during the COVID-19 pandemic included Bascom Palmer’s physicians, residents, fellows, nurses, technicians, and the other staff members who continued to provide the best possible patient care despite the many challenges of the pandemic.
For 60 years, Bascom Palmer’s doctors on the vitreoretinal service have been leaders in the field. Their unparalleled level of innovation includes developing the Vitreous Infusion Suction Cutter; performing the world’s first pars plana vitrectomy; paving the way for improvements in the diagnosis and treatment of retinal detachments, diabetic retinopathy, and macular holes; and revolutionizing the treatment for neovascular and exudative eye diseases by pioneering the use of intravitreal bevacizumab therapy and optical coherence tomography.
Harry W. Flynn Jr., M.D., has led the service for the past 25 years –its excellence continues.
Back in 1957, internationally renowned calypso singer Harry Belafonte was having trouble with his vision. He sought out Edward Norton, who was the only retinal surgeon in New York City to use the new binocular indirect ophthalmoscope, which allowed for detailed examination of the interior of the eye. The retinal surgery was a success and Belafonte later would visit Norton in Miami for vision checkups and fundraising events to support Bascom Palmer.
“For Dr. Norton, patient care and safety were paramount,” said Wayne E. Fung, M.D., (fellow 1968). Fung, the recipient of a lifetime achievement award from the American Academy of Ophthalmology, spent more than 50 years in San Francisco as a renowned ophthalmologist. “The Chief would treat his patients with care and compassion, regardless of social or economic status.”
Through the decades, Bascom Palmer has stayed on the leading edge of clinical care, treating patients of all ages with care and compassion. “Our goal is to deliver the best possible vision care to patients throughout our diverse South Florida community and around the world,” said Eduardo Alfonso. “We are committed to equity in healthcare, and our team is reaching out to marginalized neighborhoods to provide screening and access to appropriate vision care.”
Delivering excellent clinical care is a team effort, adds Michael Gittleman, Bascom Palmer’s chief administrative officer. “In addition to having great faculty, our staff is second to none,” he said. “From our nurses and therapists to our patient schedulers, maintenance workers, and technology professionals, we focus on supporting our clinicians, researchers, and educators, while delivering an excellent experience to our patients and families.”
Altogether, Bascom Palmer has about 1,200 faculty and staff members in the Institute’s South Florida facilities. “We believe in
opening the door to career opportunities,” said Gittleman. “Many of our nurses and technicians have been with us for more than 20 years, as we provide support for their journeys in health care.”
Bascom Palmer is committed to excellence in every area of vision care, with a focus on seven subspecialty services: cornea; retina; glaucoma; pediatric ophthalmology and adult strabismus; neuro-ophthalmology; oculoplastics; and ocular oncology.
“Our physicians and researchers have been on the leading edge of vision care for six decades,” said John Clarkson. “Their remarkable contributions to ophthalmology have been instrumental in preventing blindness, halting disease progression, and restoring vision for patients throughout South Florida and around the world.”

Diagnostic, treatment, and vision preservation services are provided at five

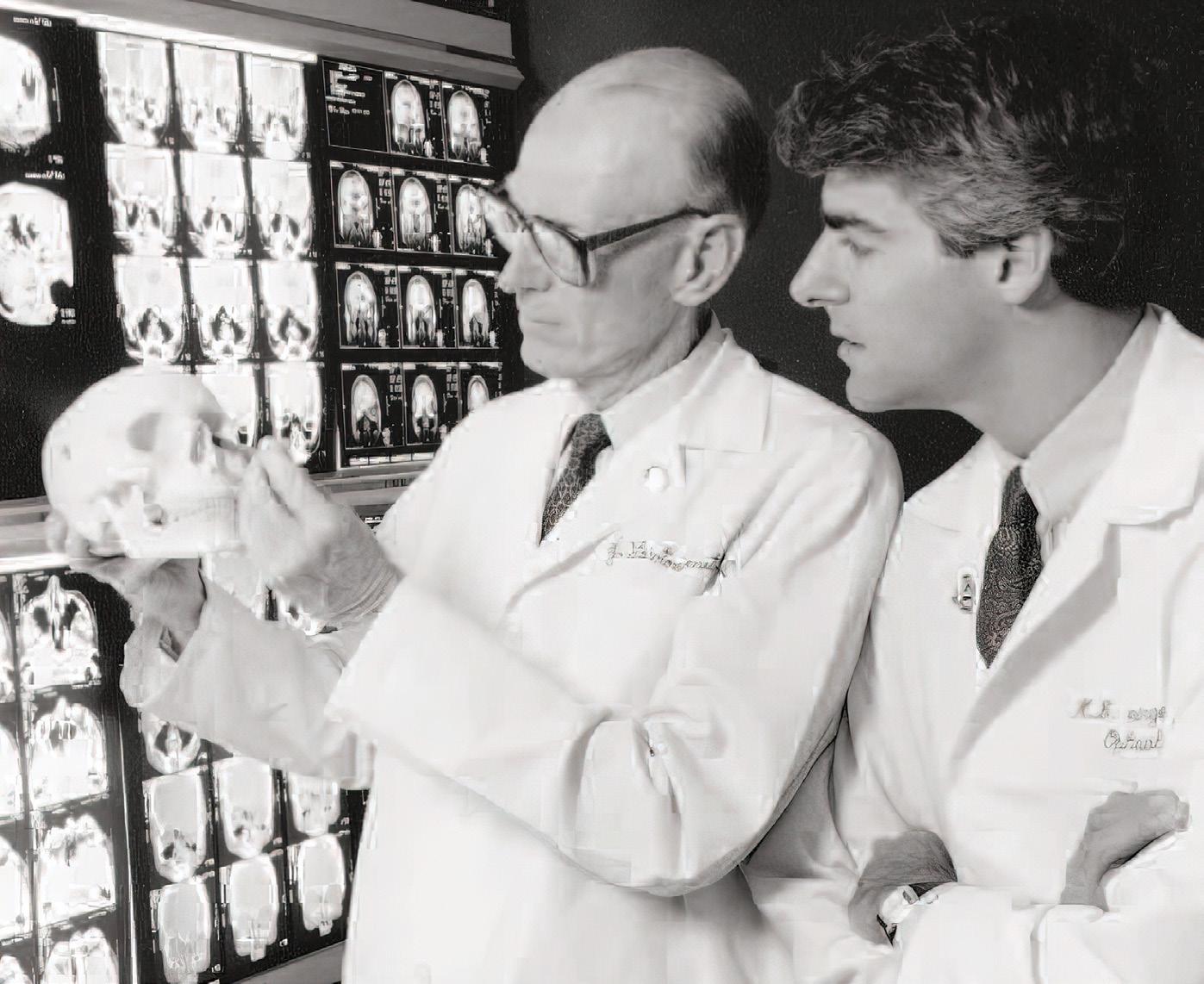
In 1989, a patient with a particularly difficult pterygium required a surgical procedure that involved surgeons from three different subspecialties. On the left is pediatric ophthalmologist, John Flynn, M.D.. Behind him is oculoplastic specialist, Jan Kronish, M.D., and corneal specialist, Eduardo Alfonso, M.D., is on the right. A medical student observes from the background.

locations in Florida, including the Institute’s Miami flagship eye center located at the University of Miami Miller School of Medicine campus, Palm Beach Gardens, Naples, Plantation, and Coral Gables. Bascom Palmer’s doctors also treat veterans and their family members at the Miami VA Hospital, adults and children at the Jackson Health Care System, and young patients at Nicklaus Children’s Hospital in Miami.
In recent years, Bascom Palmer has also expanded its telehealth program, allowing patients to be seen in the comfort of their homes, increasing accessibility to care. “The COVID-19 pandemic accelerated our drive to provide virtual care,” said Gittleman. “Now, we are continuing to come up with new ideas and approaches to better serve patients from home.”
Bascom Palmer’s cornea and external disease specialists have decades of experience in treating damage to the corneal tissues and optical surfaces. “Our faculty are involved at the highest level of national and international developments in diseases and surgery of the cornea,” said service director William W. Culbertson, M.D., (fellow 1979), the Lou Higgins Chair in Ophthalmology. “As a result, we are ready and able to provide the latest and most appropriate treatments to all of our patients.”
For example, several surgical options are available for treating cataracts, which can develop from normal aging, an eye injury, disease, or other causes. Once the cataract
is removed and a new lens put into place, patients typically regain all the benefits of normal vision.
“As cataract surgery evolves as significant technology, femtosecond laser-assisted cataract surgery is now providing greater precision compared with manual techniques and may be better for patients overall,” said Culbertson, who has been at the forefront of vision correction surgery since its earliest days.
Under Culbertson’s direction, Bascom Palmer has made significant contributions to corneal transplant techniques, including partial transplants involving only a thin membrane and layer of cells.

Laser surgery, eyeglasses, or contact lenses with an appropriate prescription can correct nearsightedness, farsightedness, astigmatism, or other refractive errors. The Institute’s specialists also offer advanced approaches to treating dry eye, tear disorders, and conditions affecting the iris, and eyelids, such as keratoconus, pterygium, endophthalmitis, and Fuch’s Dystrophy.
Edward Norton had a strong interest in treatments for retinal and vitreous diseases, including diabetic retinopathy. Working with the newly formed National Eye Institute, part of the National Institutes of Health (NIH), he helped organize the Diabetic Retinopathy Study, the first major clinical trial in ophthalmology. This study showed the benefit of panretinal photocoagulation in reducing blindness in diabetic patients. The Diabetic Retinopathy Vitrectomy Study demonstrated the value of early vitrectomy in Type I diabetic patients. George W. Blankenship Jr., M.D., led the Institute’s efforts in the management of patients with diabetic retinopathy for nearly 20 years. At Bascom Palmer, he served as principal investigator on the NIH-sponsored Diabetic Retinopathy Study, the Early Treatment Diabetic Study, and the Diabetic Vitrectomy Study, each of which demonstrated a beneficial effect of treatment.
Vascular diseases, genetic disorders, aging, and cancer can lead to the degeneration of light-sensitive retinal tissues, including the macula that provides central vision, or the
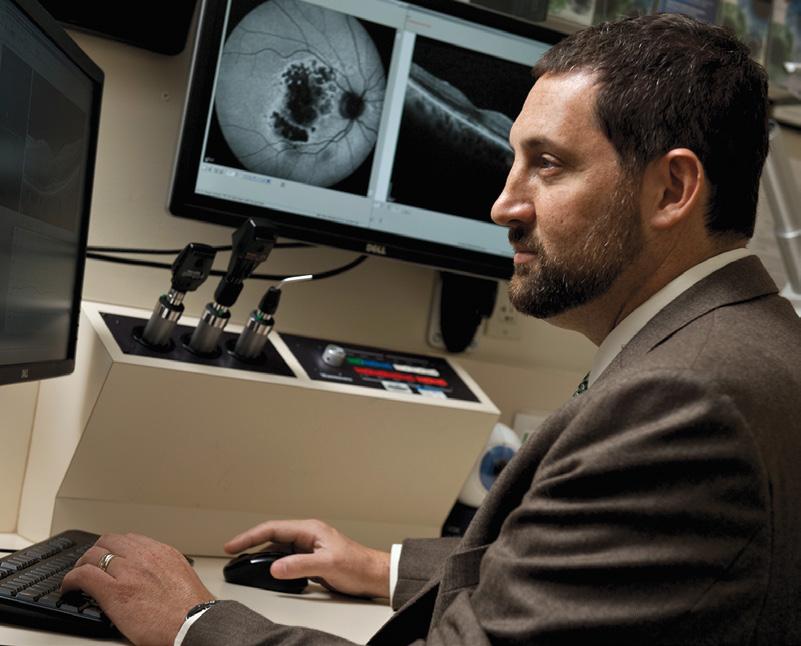
surrounding cells that provide peripheral vision. Through the years, the Institute’s retinal specialists, including Philip J. Rosenfeld, M.D., Ph.D., (Fellow 1996), have made major advancements in treating age-related macular degeneration (AMD) –including pioneering the use of anti-VEGF medications to maintain vision – as well as conditions like diabetic retinopathy and retinitis pigmentosa.
“Advances in optical coherence tomography (OCT) have been very effective in evaluating macular diseases and response to treatment,” said service director Harry W. Flynn Jr., M.D., professor of ophthalmology and the J. Donald M. Gass Chair in Ophthalmology. “OCT has been particularly helpful in understanding the value of antiVEGF treatments for wet AMD and diabetic macular edema.”
Another clinical advancement is the use of small-gauge vitrectomy instruments, which allow for suture-less surgeries, said Flynn. “We participated in clinical case series, which showed significant patient benefits including less pain, shorter procedures and quicker recovery times.”
The Institute’s retinal specialists have evaluated various antifungal agents to manage endophthalmitis, an infection of the eye’s inner fluids and tissues. “Our ocular microbiology laboratory led by Dr. Darlene Miller is essential in our research. Our group has also reported that the combination of vitrectomy with scleral buckling had better outcomes for rhegmatogenous retinal detachment than vitrectomy alone,” said Flynn.
For more than five decades, Bascom Palmer has been a leader in developing better treatments for glaucoma, a blinding disease that still holds many secrets. “The focus of our research over the years has been finding therapies to improve patient care,” said professor of ophthalmology Richard Parrish, who leads Bascom Palmer’s glaucoma service.
“Each year we treat nearly 40,000 patients who have advanced glaucoma,” said Parrish.

“We carefully review medications and surgical procedures to determine the most effective approach for individual patients.” The Institute’s specialists perform comprehensive glaucoma screenings to determine the nature of the underlying disease and the extent of vision loss. Treatments include prescription eye drops to decrease intraocular pressure by reducing the amount of fluid the eye produces or by increasing the outflow of fluid from the eye. Oral prescription medications may also reduce pressure inside the eye.
Laser therapy can be an effective strategy for opening clogged drainage channels inside the eye, releasing fluid build-up. Another option is filtering surgery to create a new passage for drainage. To enhance filtering surgery, tiny drainage devices or “aqueous shunts” may be inserted to keep the surgically created opening from closing. “We also have extensive experience in minimally invasive glaucoma surgery to lower eye pressure and prevent disease progression,” said Parrish.
“Our faculty are involved at the highest level of national and international developments in diseases and surgery of the cornea. As a result, we are ready and able to provide the latest and most appropriate treatments to all of our patients.”
– William Culbertson, M.D.
William Culbertson, M.D.
George Blankenship, M.D.Richard Parrish II, M.D.
Bascom Palmer’s resources, vast experience, and extremely dedicated team of specialists provide our youngest patients a major advantage.”
– Craig McKeown, M.D.“These procedures are indicated in certain types of glaucoma and work by using microscopic-sized equipment and tiny incisions.”
Bascom Palmer is also a world leader in the diagnosis and treatment of pediatric glaucoma with a team led by Alana Grajewski, M.D., (fellow 1989), a professor of clinical ophthalmology, holder of the Kolokotrones Chair in Ophthalmology, and director of the Samuel and Ethel Balkan International Pediatric Glaucoma Center. Although this disease most commonly affects the elderly, childhood glaucoma (from birth to 18 years of age) affects one in 5,000 children. With the clinical team’s expertise in this rare vision condition, families come to the Institute from throughout the U.S. and many international locations.
Children’s eye care needs are different from those of adults. Early diagnosis and treatment of childhood eye diseases and disorders significantly affect a child’s physical, emotional and social development.
Bascom Palmer’s pediatric ophthalmologists work closely with other ophthalmology experts to diagnose and treat infants, children, and adolescents with a wide range of vision conditions.
“We are a team of experienced, dedicated, and compassionate pediatric ophthalmologists with access to advanced technology,” said service director Hilda Capó, a professor of clinical ophthalmology and the John T. Flynn Chair in Ophthalmology. “Our goal is to provide comprehensive evaluations and the most up-to-date treatments to improve the vision and quality of life of children and adults. We take great pride in using our expertise to deliver top-quality care to our patients.”
Since the 1960s, Bascom Palmer has been treating children with amblyopia, strabismus (misalignment of the eyes), retinopathy of prematurity, cataracts, optic nerve anomalies, tumors of the eye, and other vision disorders. The Institute provides compassionate care to children and advises and educates parents and other family members who come to the William and Norma Horvitz Children’s Clinic, designed specifically for our youngest patients.

“Children with certain medical conditions, such as intellectual disabilities, developmental delay, Down syndrome, or behavioral issues benefit greatly from a comprehensive eye examination by a pediatric ophthalmologist,” said Capó. “Our pediatric team also evaluates adults with strabismus and double vision who may benefit from surgery.”
“For many conditions, early intervention with the appropriate course of treatment is essential for a successful outcome,” said Craig A. McKeown, M.D., professor of clinical ophthalmology. “Bascom Palmer’s resources, vast experience, and extremely dedicated team of specialists provide our youngest patients a major advantage.”
From the days of early faculty members like Norton and Smith, Bascom Palmer’s neuro-ophthalmologists have been treating challenging conditions that affect both the eyes and the brain. In the early years, they recruited and trained a world-class neuroophthalmology team, including Noble David, M.D., Joel Glaser, M.D., (fellow 1967), Norman Schatz, M.D., (fellow 1966), John McCrary,
M.D., (fellow 1967), and Robert B. Daroff, M.D., a pioneer in the field of ocular motor research at Bascom Palmer. This is chronicled in The Golden Age of Neuro-Ophthalmology at the Bascom Palmer Eye Institute written in 2002 by Joel Glaser in the Journal of Neuroophthalmology.
“We treat a variety of patients spanning a large spectrum of vision problems, some of which are life-threatening,” said service director Byron L. Lam, M.D., (fellow 1991), professor of ophthalmology, and the Robert Z. & Nancy J. Greene Chair in Ophthalmology.
“We have extensive experience in diagnosing complex issues, such as disorders of the optic nerve and central nervous system, and treating tumors of the optic nerve, orbit, and brain with visual implications.”
Many neuro-ophthalmology patients come to Bascom Palmer with unexplained vision loss. A careful and comprehensive assessment could identify a nutritional, inflammatory, or metabolic problem affecting the optic nerve, brain, or eye. For instance, inflammatory and infectious disorders can affect the visual pathway. Other patients have vision problems related to inherited retinal diseases or eye movement disorders, such as double vision or abnormal eye alignments.”
“We work closely with other subspecialists to provide coordinated care for these types of conditions,” said Lam. “We also offer the latest treatments for problems like optic nerve inflammation, thyroid eye disease, and macrovascular decompression causing facial spasms.”
“At Bascom Palmer, we have the ability to collaborate with our colleagues in neuroophthalmology as well as colleagues in other clinical specialties at the University of Miami, including neurology, neurosurgery, endocrinology, and rheumatology, who are all experts in the field to determine the best plan for each patient. We are not just helping our patients with their vision, we are delivering compassionate patient care at the same time,” said Joshua Pasol, M.D., (fellow 2007) an associate professor of clinical ophthalmology.
Under the direction of David T. Tse, M.D., who joined the Institute’s faculty in 1986, Bascom Palmer was one of the first academic centers to create a dedicated oculoplastic medical and surgery service. Tse pioneered the use of adjuvant intraarterial chemotherapy for the management of adenoid cystic carcinoma of the lacrimal gland, a treatment that has significantly improved the prognosis of this aggressive cancer. Now, the specialists
“For many conditions, early intervention with the appropriate course of treatment is essential for a successful outcome.Hilda Capó, M.D. Byron Lam, M.D. J. Lawton Smith, M.D., and Mitchell Strominger, M.D., examine a skull. “Alas, poor Yorick!”
“Our oculoplastic surgery group is wonderful and is on the cutting edge of clinical and basic science research. Our doctors continually learn from each other, honing their surgical skills and continuing to improve and develop novel techniques for the benefit of their patients.”
– Thomas Johnson, M.D.
treat conditions of the orbit (bony socket containing the eye, eyelids, and surrounding structures), the lacrimal system (tear glands and ducts), the eyelids, and the face. Disease processes range from cancer to trauma to serious infections. Treatment often requires a multidisciplinary approach. All age groups are treated, from newborn infants to the elderly.
Tse, a professor of ophthalmology and the Dr. Nasser Ibrahim Al-Rashid Chair in Ophthalmology, also led a team that created a 3-D printed prosthesis in 2014 for a woman who could not afford a traditional orbital-facial prosthesis. By scanning the undamaged side of her face and merging the image with her orbital defect, the software application merged the scans and sent them to a 3-D printer, which created a facial and ocular prosthesis with colored pigments matching the patient’s skin tone.
Service director Thomas E. Johnson, M.D., (fellow 1993), professor of clinical ophthalmology, joined the Bascom Palmer faculty in 1992 and helped build the service to enjoy a reputation as the country’s best. “Our oculoplastic team is a wonderful and collaborative group on the cutting edge of clinical and basic science research,” said Johnson. “Our doctors continually learn from each other, honing their surgical skills, and continuing to improve and develop novel techniques for the benefit of their patients.”
Today, the Institute has the nation’s largest ophthalmic plastic surgery team, performing medical, reconstructive, and cosmetic procedures on the delicate anatomy of the orbit, face, and eyelids. Professor of clinical ophthalmology, Wendy W. Lee, M.D., (fellow 2004), has developed Bascom Palmer’s multispecialty aesthetic center that offers cosmetic treatments that vary from the least invasive topical treatments to injectables, lasers, and surgery.
“Our team has performed pioneering work for many types of conditions and treatments,” said Johnson. “We use our imagination, experience, and skills to find solutions to problems, no matter how difficult or complex.”
While primary ocular cancers are rare, they can occur within the eye, on the eye’s surface, in the skin cells around the eye, or in glands that produce tears. Secondary eye cancers resulting from tumors from other parts of the body that have spread to the eye occur more frequently.
Bascom Palmer’s ocular oncology experts take a holistic approach to eye cancer care and research. “We are in a unique position to support our patients from the initial diagnosis through surgery, medication or radiation treatment and follow-up care if issues arise later in life,” said specialist Zelia M. Correa, M.D., Ph.D. “No other ocular oncology center in the U.S. has the same resources and ability to provide coordinated support to patients whose disease may have spread beyond the eye.” Correa follows J. William Harbour, M.D., (fellow 1995), as director of the ocular oncology service. Bascom Palmer has comprehensive oncology treatment for intraocular tumors with Correa, ocular surface tumors with Carol Karp, M.D., and orbital and lid tumors managed by the oculoplastic service.

While a Miami man was hammering in his workshop, a metal splinter flew up into his eye. “A doctor near his home told him the eye was lost because it was bleeding and had become infected,” said Kenneth L. Fan, M.D., M.B.A., (chief resident 2022). “By the time he reached Bascom Palmer’s Emergency Department, his vision was almost gone, but our team has seen many injuries like this. We were able to save his eye and even restore his vision to 20/40. Helping patients with emergency blinding conditions is what keeps us going every day.”
From traumatic injuries to lifethreatening tumors, swollen blood vessels, viral infections, and unusual diseases, patients who need emergency eye care turn to Bascom Palmer – one of the few U.S. hospitals with a specialized eye emergency

department. A unique medical resource for patients from throughout South Florida and beyond, the Bascom Palmer Eye Institute Emergency Department also provides exceptional training for ophthalmology residents, who learn surgical procedures and medical treatments for an exceptionally wide range of eye problems.
“The Emergency Department is a jewel for Bascom Palmer,” said Kara M. Cavuoto, M.D., (resident, fellow 2012), associate professor of clinical ophthalmology and director of the Emergency Department, which is located at Bascom Palmer’s Miami center. “We are open 24/7/365 and typically see 75 or more adult and pediatric patients a day – more than 25,000 each year.
Patients receive a diagnosis, emergency care, and treatment of eye problems from a trained ophthalmic team of board-certified physicians, fellows, residents, registered nurses, ophthalmic technicians, and optometrists. “We are the gatekeepers,” said Fan. “We never know who is going to walk through our doors. It might be someone who lives nearby or a patient who has flown all night to see one of our specialists.”
“The Emergency Department is a jewel for Bascom Palmer. We are open 24/7/365 and typically see 75 or more adult and pediatric patients a day – more than 25,000 each year.”
– Kara Cavuoto, M.D.Beginning in the 1990s, Bascom Palmer expanded its South Florida footprint, based, in part on population studies indicating projected growth in Collier and Palm Beach counties. Drs. Norton and Clarkson focused initially on Palm Beach County, home to many Bascom Palmer patients and donors.
Since its early days, Bascom Palmer physicians have provided care to residents of Palm Beach County. Under Clarkson’s visionary leadership, the Ophthalmology Research Foundation (ORF) purchased seven acres of land in Palm Beach Gardens in 1996 as a future site for a permanent satellite campus.
In 1996, Parrish hired David S. Greenfield, M.D., (fellow 1995), to be the medical director of Bascom Palmer Eye Institute of the Palm Beaches. “Our goal was to provide clinical and surgical care to a wider region,” said Greenfield, who is now a professor of ophthalmology, the Douglas R. Anderson Chair in Ophthalmology, and vice chair for academic affairs for the department of ophthalmology.

Today, the doctors at Bascom Palmer’s campus at Palm Beach Gardens serve about 50,000 patients and perform 3,000 procedures annually. “Our volume probably exceeds most ophthalmology programs around the country,” said Greenfield. “We also host a multidisciplinary fellowship program, as well as elective rotations by medical students from the UM Miller School, Florida Atlantic University, Yale University, and other institutions.” The current medical director is Jorge A. Fortun, M.D., an associate professor of clinical ophthalmology and retina and vitreous diseases specialist.
Bascom Palmer Eye Institute at Naples first opened in 2004 in an office at Naples Community Hospital. “Initially, we had several specialists driving over from Miami to see patients,” said Stephen G. Schwartz, M.D., M.B.A., professor of clinical ophthalmology and medical director. “Through the years, we continued to grow and serve our community.”

“Our services include retina, cornea, glaucoma, oculoplastics, and neuroophthalmology,” said Kendall E. Donaldson, M.D., M.S., (resident, fellow 2004), professor of clinical ophthalmology and medical director. “We also have a dry eye and a pediatric cornea service.”
While Plantation’s patients have their surgery done in Miami, they appreciate being able to take care of their pre- and post-operative visits closer to home, added Donaldson. “We consider ourselves an extension of the main Institute just 25 miles away. “
Bascom Palmer’s newest location is in the Lennar Foundation Medical Center on the University of Miami’s Coral Gables campus. The 200,000-square-foot LEED-certified ambulatory center provides area residents with easy access to vision care.
“Our Coral Gables location delivers the same extraordinary care provided at all of Bascom Palmer’s world-class eye care centers, with full diagnostic services,” said medical director Rahul S. Tonk, M.D., (fellow 2017), a specialist in cornea and external diseases, cataract, and LASIK.

As patient demand for the Institute and advanced subspecialty care increased, philanthropic donors supported the construction of a dedicated center on U.S. 41, a few miles north of downtown Naples. That is now the professional home of eight fulltime physicians. Bascom Palmer’s surgery center in Naples, is under the medical direction of Allister Gibbons, (fellow 2015), an associate professor of clinical ophthalmology “We offer our patients the benefits of an academic medical center, including access to retinal clinical trials,” said Schwartz. “We also provide telehealth services to our community and hope to expand our facility to serve more patients from Southwest Florida.”
Since opening in 2004, Bascom Palmer Eye Institute at Plantation has provided Broward County patients with convenient access to vision care. It is a 12,000-square-foot facility in the Miller School’s multidisciplinary office center, where 35,000 patients are seen annually.
Like the other medical directors, Donaldson continues to see a steady increase of patients, like a woman in her 60s who was having pain and swelling in her left eye. “She had a LASIK treatment a decade ago, followed by cataract surgery several years later,” Donaldson said. “We used OCT to examine her eye and found a cleft between the LASIK cap and the underlying cornea. We were able to replace the corneal lining, her swelling disappeared and she now sees 20/20 in her eye.”
One of the major sources of endowment support for Bascom Palmer is the Ophthalmology Research Foundation, Inc. (ORF). The ORF is recognized by the IRS as a 501(c)(3) supporting organization. Initially funded partially through faculty donations, the ORF was incorporated with the sole purpose of supporting the University’s department of ophthalmology. For more than 50 years, the ORF has supported the department’s mission.
The ORF’s governing board is led by the department chair, and all board members are faculty members of the department of ophthalmology. Funds from the ORF have provided support for vision research and have financed the purchase of property to provide medical center patient and staff parking as well as clinical facilities and surgical centers in Palm Beach Gardens and Naples.
The ORF was established by Drs. Norton, Curtin, and Gass, with the assistance of Gaby Kressly, the department’s administrator. The Ophthalmology Research Foundation continues as an enduring contribution both now and in the foreseeable future.
With more than 50,000 samples of eye tissue dating back to the 1960s, the Bascom Palmer Florida Lions Ocular Pathology Laboratory provides a unique resource for studying cancers of the eye. Led by medical director Sander R. Dubovy, M.D., professor of ophthalmology and pathology, the Institute’s pathology lab analyzes more than 3,000 new biopsy specimens each year. Dubovy holds the Victor T. Curtin Chair in Ophthalmology.
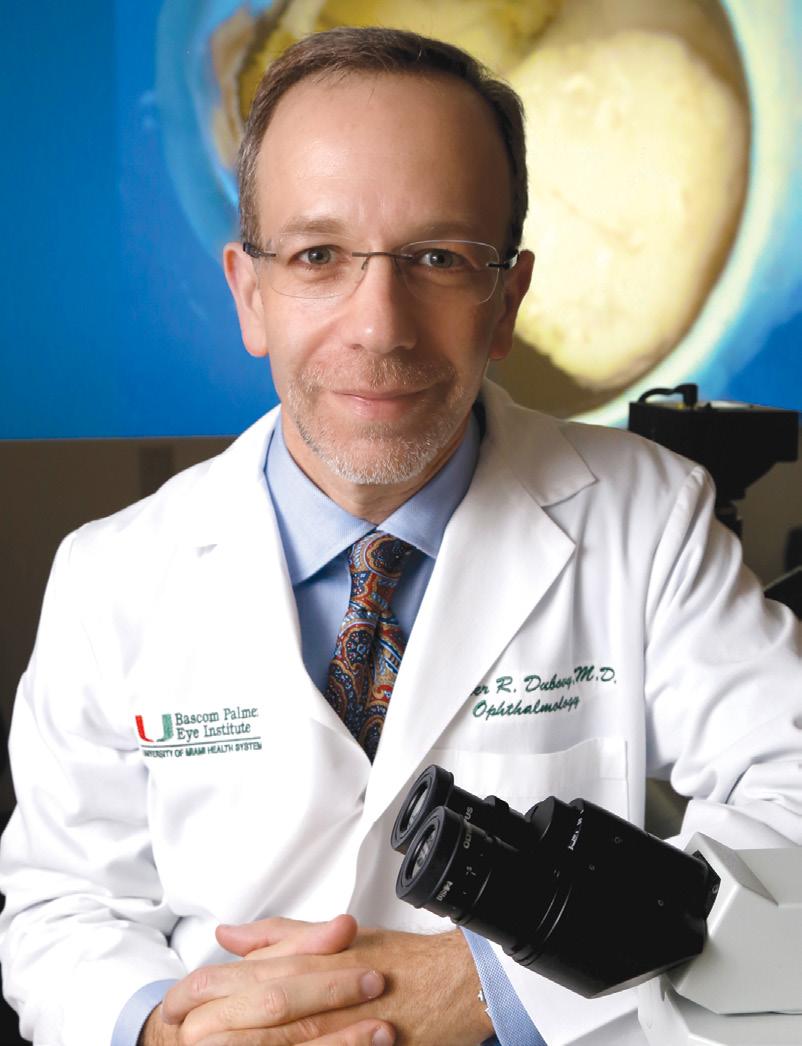
“We are one of the busiest ocular pathology laboratories in the country,” said Dubovy, a retina specialist who is one of the few U.S. physicians board-certified in both ophthalmology and pathology. “We continue to expand by investing in new equipment, adding additional staff as needed, and most importantly, training young physicians through our pathology fellowship program who will become the next generation of ocular pathologists.”
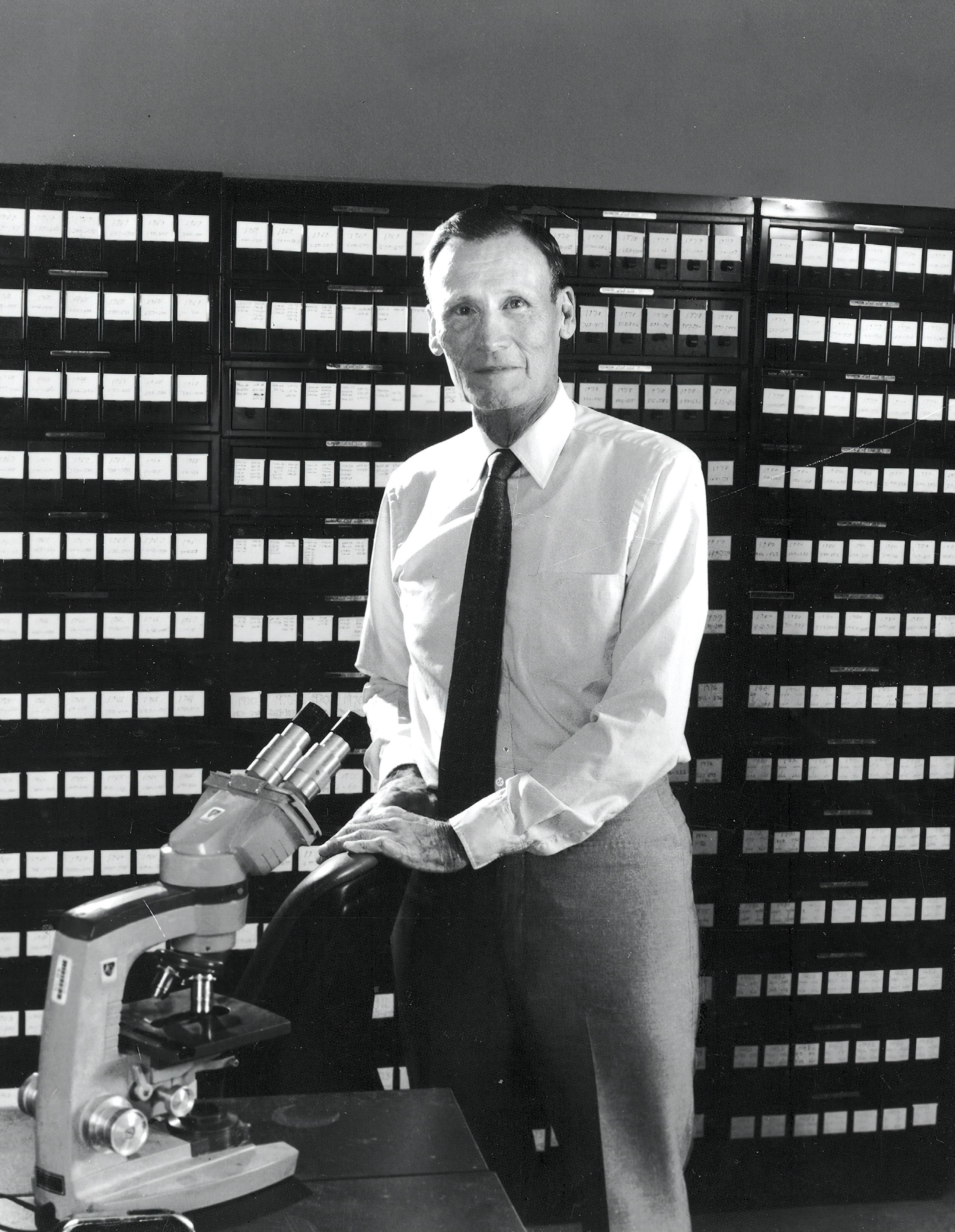
Victor Curtin founded Bascom Palmer’s ocular pathology laboratory in 1962 in a unique association with the Florida Lions Eye Bank. He started the laboratory’s collection of specimens and remained a consultant to the Eye Bank for 57 years until his death in 2016. That historical perspective is particularly important for oncology patients who return for further treatment since past and present specimens can be easily compared.
Through searches of the laboratory database for rare ophthalmic conditions, Dubovy and his colleagues have been able to assemble and publish case studies that have shed new light on the diagnostics, pathophysiology, and clinical outcomes of several disease entities. Since the pathology laboratory team processes the specimens within the Institute, Bascom Palmer clinicians can get results very quickly.
Also celebrating its 60th anniversary, the Florida Lions Eye Bank was founded in 1962 in cooperation with the Lions Clubs of Florida and Bascom Palmer Eye Institute. Realizing the importance of an eye bank, founding chair Edward Norton requested the first eye bank in the State of Florida be located within the Institute. Bascom Palmer and the Eye Bank have evolved side by side for six decades.
“The Florida Lions Eye Bank’s mission is to recover, process, and distribute corneal and scleral tissue for sight-saving transplant surgery,” said Elizabeth Fout-Caraza, executive director. “To make this happen, we rely upon the selflessness of the individuals and their families who choose to donate their eyes upon their death.” Since 1962, nearly 65,000 corneas have been provided for transplant, restoring sight to tens of thousands of recipients.
With the opening of Bascom Palmer, Victor Curtin, became the first medical director of the Eye Bank, serving in that volunteer role through 1996. With the support of the medical examiners in Dade and Broward counties, the supply of donor corneas increased rapidly and it became one of the largest eye banks in the country in terms of sending out tissues. For many years, the Eye Bank would send out 2,000 corneas annually for free – mostly to recipients in Florida.
In 1983, in gratitude for Curtin’s dedication, the South Florida Lions endowed $500,000 toward a chair at Bascom Palmer in his name; the funds were matched to create a $1 million contribution. “It was a complete surprise to me,” said Curtin at the time. “It is an honor to be remembered in this way.” Today, Dubovy is the Eye Bank’s medical director.
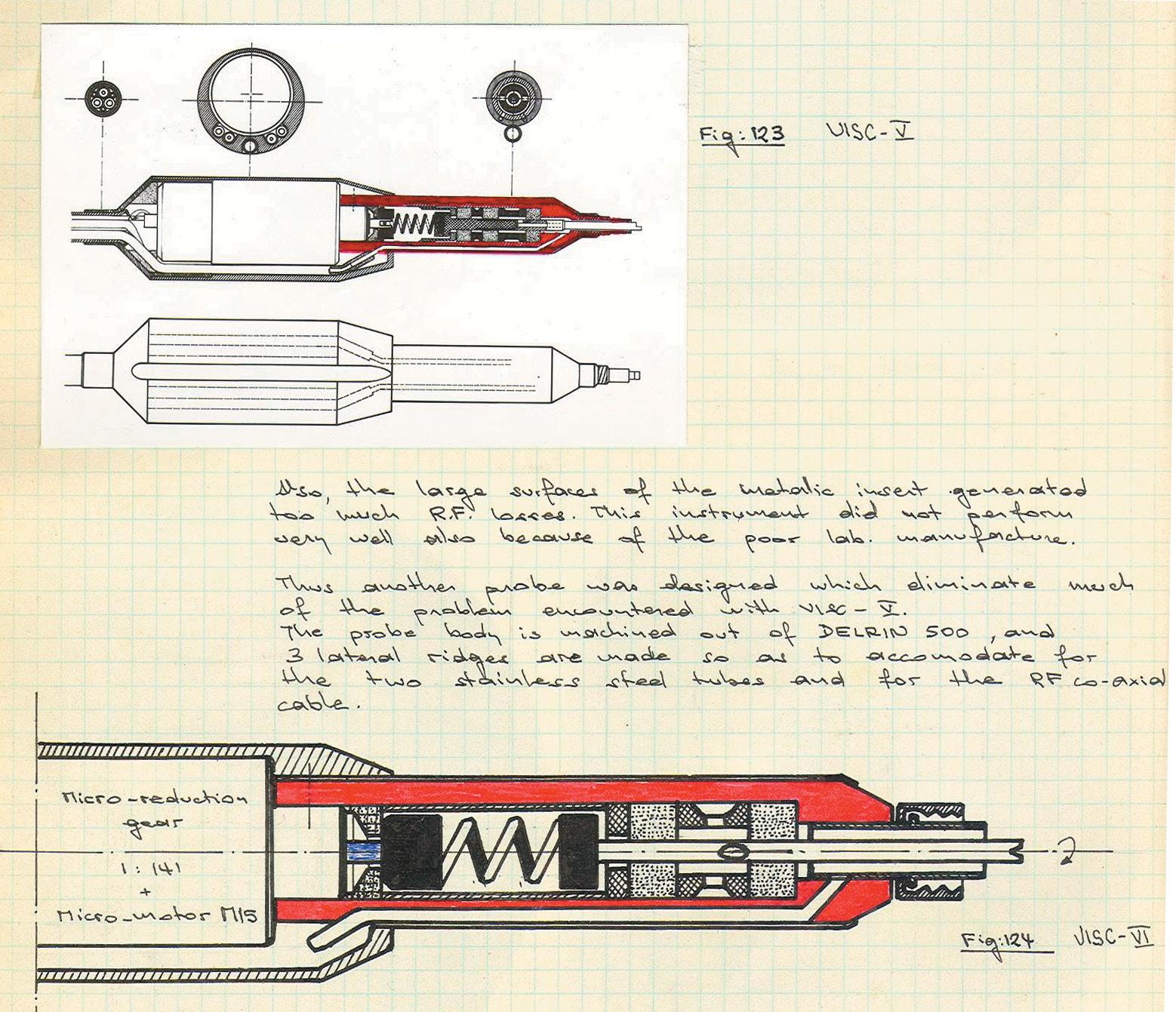
To date, more than 350 surgical instruments and clinical devices have been developed by Bascom Palmer’s Ophthalmic Biophysics Center, with many more in the works. Shown here is a drawing of one of the most notable devices – the Vitreous Infusion Suction Cutter (VISC), designed for the first vitrectomy.
Under the dynamic leadership of Dr. Edward Norton and the chairs who followed him, Bascom Palmer Eye Institute is one of the world’s foremost academic medical centers for scientific discovery and clinical innovation.

For six decades, Bascom Palmer’s clinicians and researchers have made major contributions to virtually every aspect of vision: retinal diseases, corneal transplants, glaucoma, and cancers of the eye and orbit. Norton himself was an innovator who found a new way to treat partial tears of the retina. He would inject a gas bubble into the eye to unroll the loose retinal flap, so it could be reattached safely – a breakthrough that helped surgeons treat other types of retinal detachments.
“Many things we do in patient care today we learned to do as a result of the research conducted by preceding generations,” said Norton in a 1984 interview. “Therefore, this generation has an obligation to make its own contributions for future generations.”
On April 20, 1970, Bascom Palmer retinal specialist Robert Machemer, M.D., (fellow 1968), performed the world’s first pars plana vitrectomy on a Miami patient who had not seen with his right eye for five years. Until then, ophthalmologists had considered the vitreous body forbidden territory because of the risk of causing a retinal detachment. Machemer’s successful procedure opened the door to many new types of treatment for retinal tears, detachments, scar tissue, macular holes, vitreous hemorrhage, traumatic injuries, and other conditions. “For a young researcher, Bascom Palmer offered an ideal environment, where credit was given to any individual who made a discovery,” said
Machemer in a 2007 interview. “It was in this supportive environment that the new art of vitreous surgery evolved.”
In fact, Bascom Palmer was a natural home for this revolutionary eye surgery, as Norton and volunteer faculty member David Kasner, M.D., (honorary alumnus), had been engaged in clinical research on the vitreous throughout the 1960s. In his curiosity about ocular anatomy, Kasner created an anatomy laboratory in his garage in Coral Gables. He became interested in creating eyes embedded in plastic that could be used for anatomical demonstrations. In the process, he discovered that the application of acrylic chemicals to partial cadaver specimens that he obtained from the Florida Lions Eye Bank turned the vitreous white and opaque. Kasner was teaching cataract surgery at the Miami V.A. Hospital located at the Biltmore Hotel in Coral Gables to Bascom Palmer’s residents including Gordon Miller, M.D., (resident, fellow, chief resident 1966). Miller brought to Kasner’s attention the first
“Many things we do in patient care today we learned to do as a result of the research conducted by preceding generations. Therefore, this generation has an obligation to make its own contributions for future generations.”
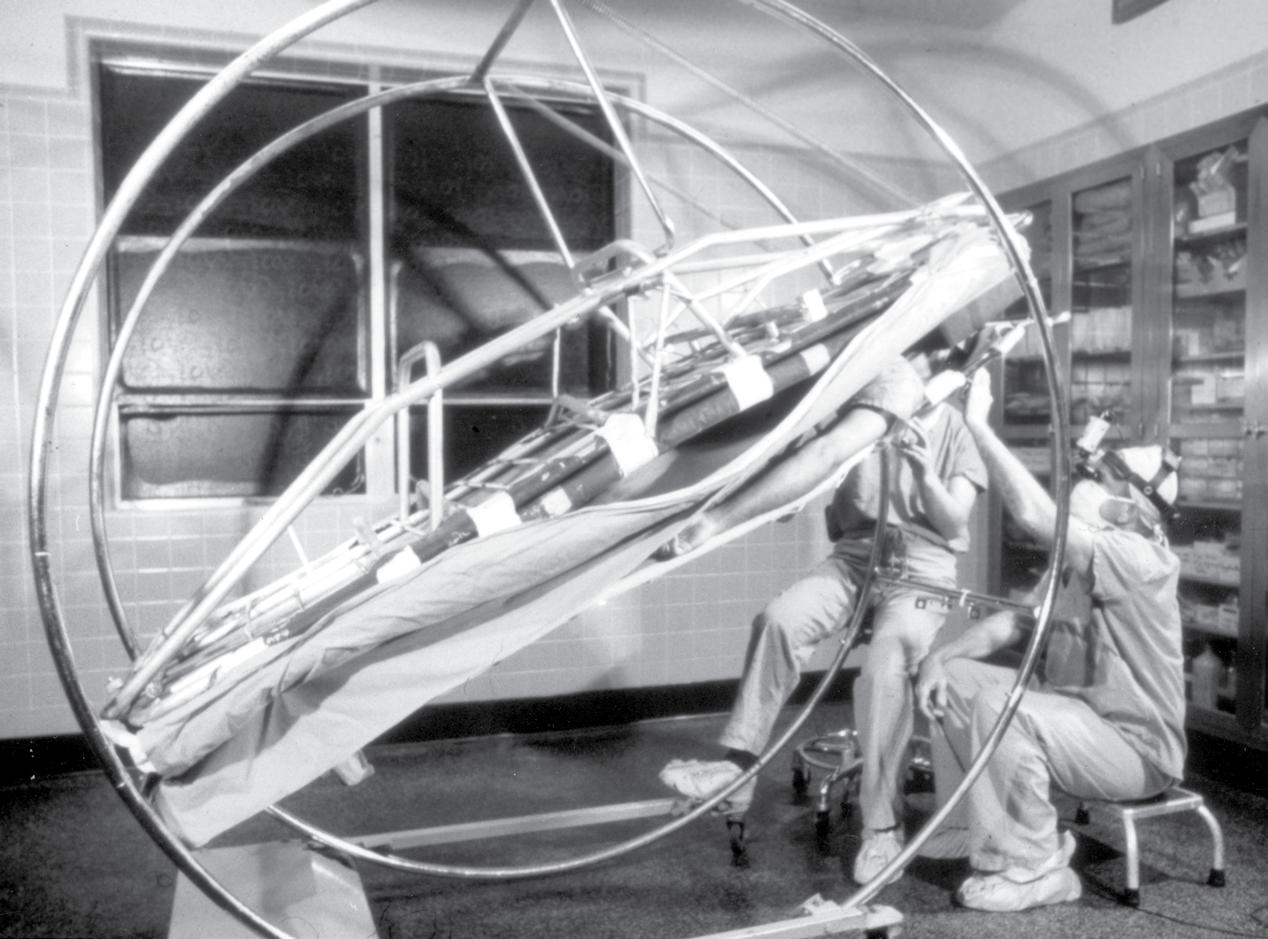
– Edward Norton, M.D.In the early 1970s, Bascom Palmer’s Ophthalmic Biophysics Center made this rotating table for retinal detachment surgery. Gas was injected into the eye and the patient remained face down during the surgery.
patient, and eventually a second who had lost vision because of an accumulation of a cloudy protein (amyloid) in the vitreous cavity. After getting the approval from Norton to proceed, Kasner and Miller utilized Kasner’s technique for manually removing vitreous material from the eyes of those patients resulting in a significant improvement in vision for both eyes. “This was something that has previously been considered taboo in ophthalmology,” said Jerome P. Fisher, M.D., (resident 1980). “The two doctors then published what is believed to be the first case reports of planned therapeutic vitrectomy in the ophthalmic literature,” he added. This was the precursor
and stimulus to the development of the modern automated vitreous surgery subsequently pioneered by Machemer. Back in 1969, Machemer met Jean-Marie Parel, Ph.D., Ing. ETS-G, a Swiss-born biomedical engineer who was developing motorized microsurgical instruments in Melbourne, Australia. They conceived the idea for an instrument (later called the vitreous infusion suction cutter or VISC) that could be introduced through the pars plana to aspirate, cut, and remove the diseased vitreous while maintaining the shape of the eye through the continuous infusion of saline solution. “It provided the foundation for doing intraocular microsurgery while preventing the collapse of the eye,” said Parel, research associate professor and holder of the Henri and Flore Lesieur Chair in Ophthalmology.
Two decades later, retinal specialist William E. Smiddy, M.D., holder of the M. Brenn Green Chair in Ophthalmology, contributed to the development of vitrectomy for the treatment of macular holes, which occur in the central part of the retina.
Today, retina specialists collectively perform thousands of vitrectomies each year thanks to this Bascom Palmer innovation.
Throughout the 1970s, biomedical research and development blossomed at Bascom Palmer. Under Parel’s leadership, the Ophthalmic Biophysics Center (later named for benefactor Walter G. Ross) began developing new equipment to advance clinical care. For instance, Parel developed the first modern programmable eye for a patient mannequin, with features like a sensor that would close the iris in response to light. “We were able to mimic conditions like retinopathy of prematurity,” Parel said. “A student could recreate an intravenous injection and use fluorescein angiography to see the changes in real-time.”

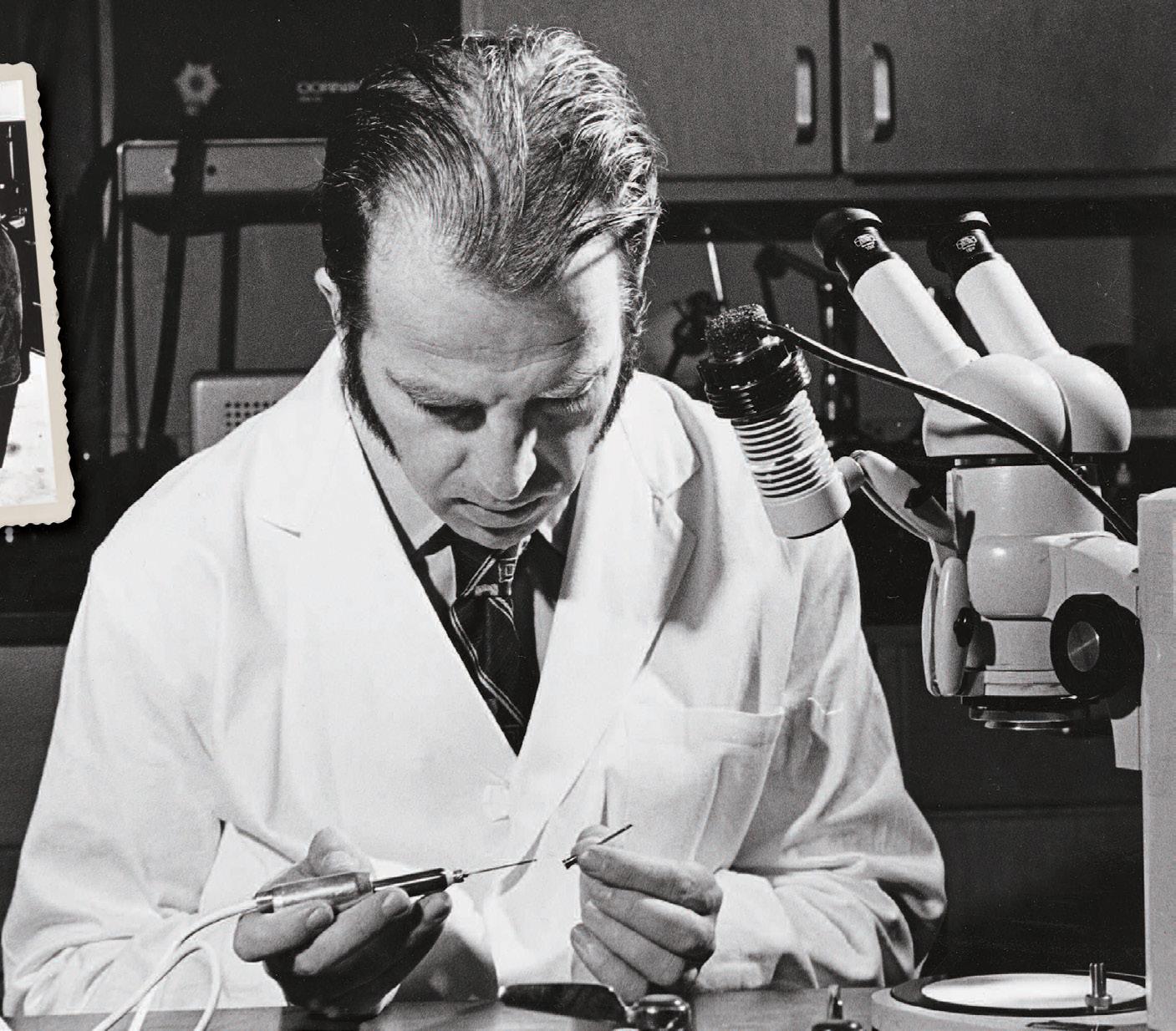
In the 1980s, Parel’s team designed the world’s smallest motorized scissors, which were used to cut retinal membranes that obscure vision. Parel also worked closely with John Clarkson in developing a “nextgeneration” fluid control system that improved surgical precision in vitrectomies. Later in that decade, Parel worked with Norton and Francisco E. Fantes, M.D., (resident, fellow 1987), who created the Fantes ordinal grading scale for assessing corneal hazing – on a study of the accommodative power of soft polymer lenses.
Through the decades, Parel and his team have invented or improved more than 350 devices, and at one point, Parel alone had more patents than the rest of the entire faculty of the UM medical school. “Dr. Norton had a view of the future so far-reaching it was unbelievable,” said Parel. “He recognized how biophysical engineering could make a huge difference in ophthalmology. He was much more interested in the instrumentation than many of his peers.” The OBC closely collaborates with Fabrice Manns, Ph.D., (research fellow 1997) a professor of biomedical engineering
and ophthalmology, and Marco Ruggeri, Ph.D., a research assistant professor of ophthalmology, as well as every other scientist at Bascom Palmer who needs technology support. In return, these gifted scientists help the OBC by sharing their knowledge and practical know-how that ultimately benefits patient care.

In 1973, Robert W. Knighton, Ph.D., (fellow 1979, research professor emeritus), joined the research faculty and began studying how to improve clinical imaging of the tissues of the eye. He took over the clinical electrophysiology research program, exploring how to improve electroretinograms (ERGs) that provided clearer diagnostic images to ophthalmic surgeons. “In the early days of vitrectomies, the physicians needed ways to assess the retina when it was screened by dense blood in the vitreous body,” he said. “It took brighter and brighter flashes of light to get an ERG to see if the retina was functioning,” he said.
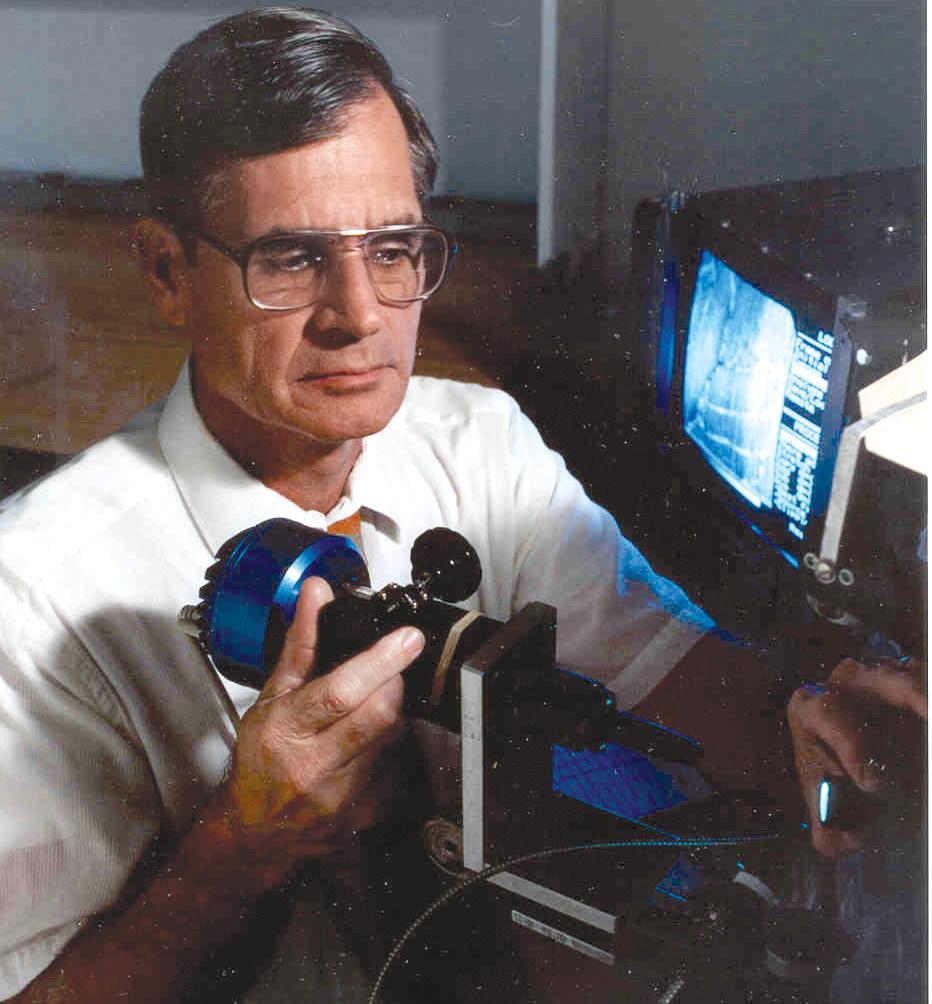
Meanwhile, clinicians and scientists in Bascom Palmer’s research laboratories were studying glaucoma and a wide range of other vision-impairing conditions. Shortly after joining the faculty in 1969, Douglas R. Anderson, M.D., divided his time between clinical care and groundbreaking scientific research. He showed how a rise in intraocular pressure (IOP) could damage the optic nerve – one of the most important discoveries in the field, as it was the first demonstration of physilogic abnormality in response to elevation of pressure in the eye. Anderson also contributed to the use of visual field testing to detect early optic nerve changes in glaucoma patients. Early in his career, he also worked closely with Ralph Kirsch, M.D., a member of the voluntary faculty, in reviewing photos of the optic nerves in his patients. After five years of work, Anderson mounted images taken by Bascom Palmer photographer Freddy Gonzalez and presented their findings at the 1975 meeting of the American Academy of Ophthalmology. Their paper won a gold medal, and Anderson later wrote an authoritative textbook on visual fields. Anderson, now a professor emeritus of
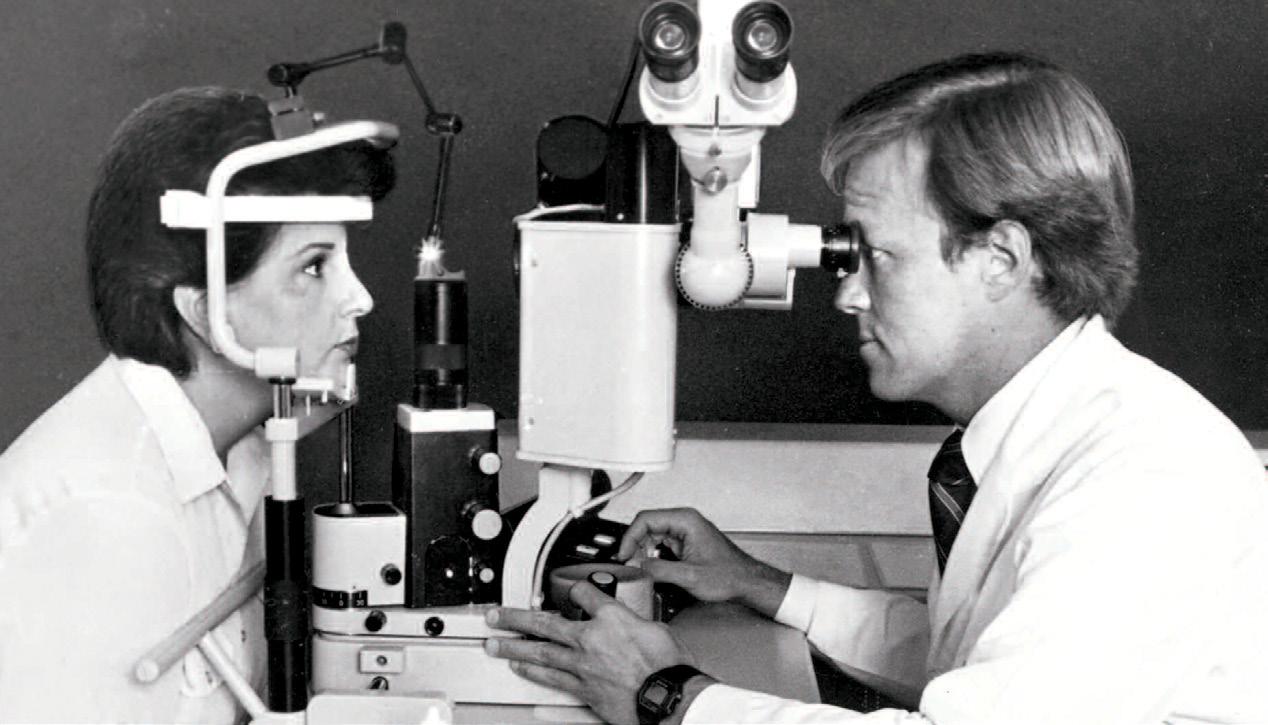
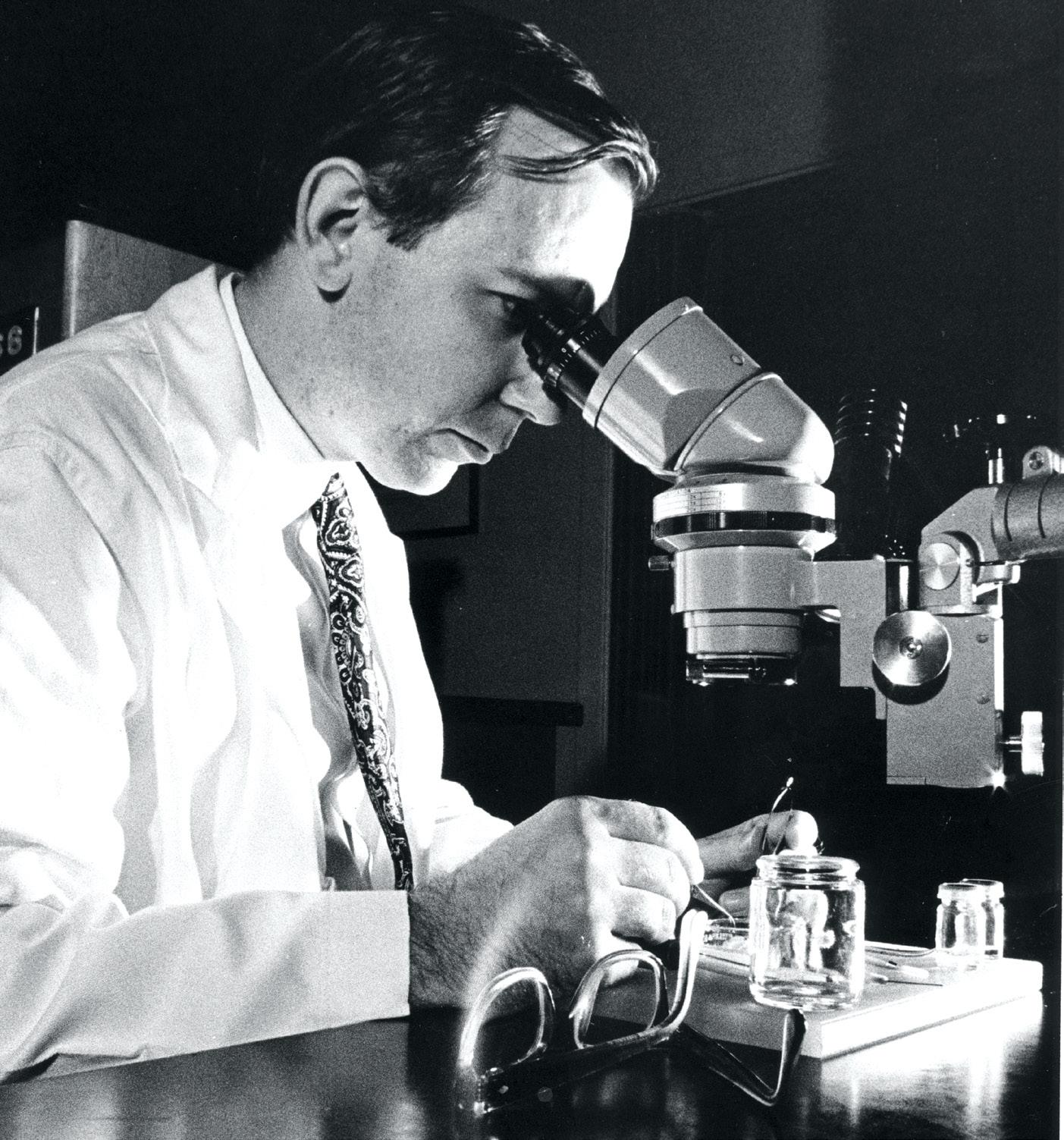
ophthalmology, served 47 years on Bascom Palmer’s faculty.

In 1978, Bascom Palmer’s ophthalmic biophysics center added a laser research laboratory led by Parel and Hanspeter Loertscher, a Swiss scientist who developed the infrared YAG laser earlier in the decade. Parel and Sidney H. Mandelbaum, M.D., (fellow 1982), clinically led the lab, which is credited for the development of a non-contact laser trephination technique for corneal transplantation.
Meanwhile, Bascom Palmer’s clinicians were quick to put this advanced technology to clinical use. In 1982, they performed approximately 4,000 laser procedures. Ophthalmologists began using the excimer laser to reshape the cornea in a procedure known as photorefractive keratectomy.
In 1988, Clarkson directed a multicenter central vein occlusion study funded by the National Eye Institute that analyzed whether early photocoagulation (laser) therapy was the best treatment to prevent further complications and loss of vision. The findings, published in 1993, confirmed the importance of frequent follow-up examinations, including an undilated slit-lamp examination of the iris in all patients with recent onset of central vein occlusion.
Meanwhile, Knighton was conducting laboratory research on the retinal nerve fiber layer, which is damaged by glaucoma at an early stage well before the loss of visual sensitivity. His work led the way to better explanations of why some nerve bundles worked better than others did. “There is a huge benefit to being a researcher in a clinical department,” said Knighton. “You can interact with the physicians and learn what would be most useful to them. Later on, you can see the results of your laboratory work being put into practice in the patients’ eye clinics.”
Soon after David Tse joined the Bascom Palmer faculty in 1986, he was faced with an extremely challenging case. A 21-year-old patient, Steve Downey, was facing a deadly
cancerous tumor in the tear-producing lacrimal gland that extended into his brain. “Based on actuarial data at that time, 80 percent of all patients with this lethal orbital tumor would die within ten years,” said Tse. “We decided to try something new in order to save this young man’s life.”
Tse had developed an innovative approach to deliver high concentrations of chemotherapy directly to the tumor, shrinking it before surgery. “This protocol has produced a survival rate of more than 80 percent, a dramatic improvement over surgery alone,” said Tse. Within a year, Downey’s adenoid cystic carcinoma was gone. “Short-term and long-term, Dr. Tse saved my life,” said Downey a decade ago.
In the early 1980s, Parel began studying the biochemistry of the eye in hopes of finding a better approach to cases of advanced diabetic retinopathy, a condition that occurs when a retinal membrane grows back after surgical removal. Collaborating with Richard Parrish, Parel began developing a system to insert a controlled-release drug called 5-fluorouracil (5-FU) into the eye. The medication is often used in chemotherapy to inhibit cellular growth. Using the OBC’s
resources, Parel created tiny implants made from biodegradable synthetic polymers that released drugs at a constant rate for several days, weeks, or months, depending on the desired outcome. Eventually, the body would absorb the biodegradable implant.
The 5-FU also held the promise of more effective treatments for some glaucoma patients. Ophthalmologists frequently perform a glaucoma filtration procedure called a trabeculectomy to open a new exit passage for the fluid inside the eye, thereby lowering the pressure. However, the body’s natural healing defenses sometimes respond by closing the passage. Administering 5-FU or other medication following the
trabeculectomy can help keep the passage open so the eye drains properly.
After studying the effectiveness of 5-FU in the laboratory, Parrish began using 5-FU for glaucoma surgery in a randomized clinical trial funded by the National Eye Institute called the Fluorouracil Filtering Surgery Study. The study demonstrated that using 5-FU resulted in substantially higher success rates in terms of controlling intraocular pressure.
“Dr. Norton gave me the time to do the research,” Parrish said. “That gave me the tremendous satisfaction of contributing to the advancement of glaucoma surgery.” Parrish and others were stimulated to undertake research on surgery for glaucoma. He and Anderson encouraged Elizabeth A. Hodapp, M.D., now an associate professor of clinical ophthalmology, to write her 1993 book, Clinical Decisions in Glaucoma, which displays her astuteness and logical thinking, as well as her effective straight-forward succinct manner of teaching. The book is frequently cited in the literature, with regard to an often-used set of criteria for classifying the severity of visual loss in patients with glaucoma, “the HAP criteria,” (or the HodappAnderson-Parrish criteria.)
After joining the faculty in 1980, glaucoma specialist Paul Palmberg discovered that color photographs could replace a more invasive diagnostic technique in some
diabetic patients. The findings convinced the National Institutes of Health to launch the Diabetes Control and Complications Clinical Trial. Palmberg served for a decade on the monitoring committee for the trial, which found that tightly controlling blood sugar – guided by frequent home monitoring by diabetic patients – significantly lowered the risk of retinal and kidney damage.
“My participation in glaucoma surgery innovation to avoid and fix hypotony maculopathy and bleb problems, resulted in my coining of the term ‘target pressure’ in 1988,” said Palmberg, who helped write the American Academy of Ophthalmology’s first Preferred Practice Pattern for Primary Open-Angle Glaucoma. He shared the World Glaucoma Prize in 2000 for showing that glaucoma damage could be halted with consistently low intraocular pressures.

In the 1980s, vitreoretinal specialist and professor, Janet L. Davis, M.D., M.A., (fellow 1987), an internationally recognized expert in uveitis, focused on the treatment and disease mechanisms of ocular inflammations and infections. She quickly became a leader in the fight to save sight in AIDS-related eye disease. “I was involved in taking care of HIV patients with ocular infections and participated in national research protocols for treatment,” said Davis. “We also have made real progress in treating uveitis since I began my practice.” Davis holds the Leach Chair in Ophthalmology.
After joining the faculty, William Culbertson worked closely with Davis in setting up one of the nation’s first uveitis clinics. In 1993, he identified the herpes virus as a cause of acute retinal necrosis, a devastating infection that can affect the retina and vitreous and lead to optic neuropathy. Thanks to this work, medications and laser treatments are now available to control this severe inflammation of the eye.
More recently, Culbertson pioneered a new surgical technique for corneal transplants for patients with Fuchs dystrophy. Working
in collaboration with Juan F. Batlle, M.D., (resident, fellow, chief resident 1984), in the Dominican Republic, he focused on transplanting just the back membrane and cells of the cornea. “The benefits include better vision without large amounts of astigmatism or nearsightedness,” he said. Currently, Culbertson is working with Jeffrey L. Goldberg, M.D., Ph.D., (resident, fellow 2010, former faculty), Eduardo Alfonso, and Guillermo Amescua, M.D., (fellow 2012), in transplanting cells tagged with magnets to direct them to the appropriate place in the cornea.
In addition to specializing in uveitis, agerelated macular degeneration, and other vitreoretinal diseases, Thomas A. Albini, M.D., a professor of clinical ophthalmology, is well-published on the risks of alternative, unproven “stem cell” therapies for eye disorders. His findings in 2017 led to significant changes in U.S. federal policy.
Sonia H. Yoo, M.D., a surgeon in corneal and refractive surgery, and holder of the Greentree Hickman Chair in Ophthalmology, has investigated the use of lasers to break cataracts to facilitate their removal and has been involved in numerous studies aimed at improving the outcomes of patients undergoing cataract and refractive surgery. For example, advanced intraocular lens designs allow surgeons to correct for nearsightedness and far-sightedness with a single implant. “Many technologies are on the horizon that will bring cataract surgery to the next level,” she said.
Carol L. Karp, M.D., (fellow 1994), pioneered a medical treatment for ocular surface squamous neoplasia – cancers that grow on the surface of the eye. While studying the effectiveness of interferon on other diseases, Karp became interested in the drug’s antiviral and anti-neoplastic properties. She designed a protocol to study the drug in patients with ocular surface tumors, curing them of their cancer without surgery.
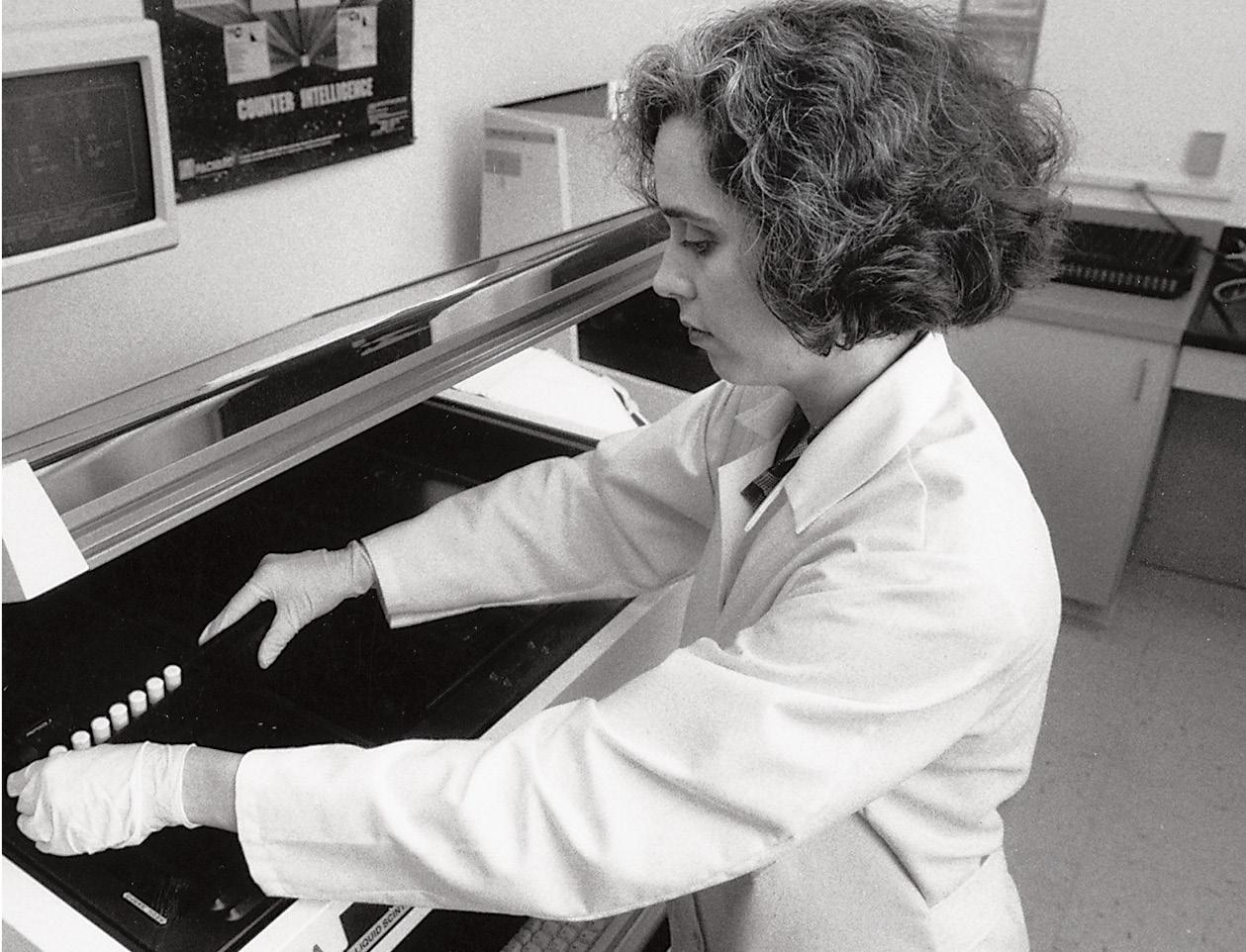
“The results were dramatic from the very first patient,” said Karp, holder of the Richard K. Forster Chair in Ophthalmology and the Dr. Ronald and Alicia Lepke Professorship in Corneal and External Diseases. Karp’s work helped to change the standard of care for the treatment of ocular surface tumors.
When she suspects squamous cell or melanoma cancer, she can do optical biopsies using ultra-high-resolution optical coherence tomography techniques developed by Jianhua (Jay) Wang, M.D., Ph.D., professor
of ophthalmology and of electrical and computer engineering. Wang’s research focuses on the development of advanced ophthalmic imaging and its applications in eye research. “We can look at the cell patterns to determine the type of cancer and track the progress of treatment until the cancer is eradicated,” Karp said.
Since the 1990s, Bascom Palmer has been a leader in curing squamous cell cancers without surgery. “We use medications compounded by our pharmacy that are very effective in curing many of these cancers,”
she said. “We also offer surgical options for treating squamous tumors, that don’t respond to medications. Other tumors, such as ocular surface melanomas and lymphomas are managed with advanced surgical approaches and other treatments in partnership with our colleagues at Sylvester Cancer Center for a comprehensive approach to treating our patient’s disease.”
Douglas Anderson and Stephen Drance, O.C., M.D., led the highly impactful Normal Tension Glaucoma Study. This landmark multicenter randomized clinical trial demonstrated the benefit of lowering intraocular pressure in the treatment of normal tension glaucoma. This pioneering study set the standard of care in the clinical practice of glaucoma. Before this study, there were differing opinions about whether IOP was involved in producing glaucomatous optic nerve damage when the pressure was in the statistically normal range. Patients who had their IOP lowered by 30% experienced slower rates of visual field loss than those who were observed without treatment in the study. The trial was sponsored by the Glaucoma Research Foundation and represented a tremendous collaborative effort among glaucoma specialists to address an important clinical question.
In the 1990s, Bascom Palmer was one of 21 U.S. eye centers selected to participate in



the Ocular Hypertension Treatment Study sponsored by the National Eye Institute of the National Institutes of Health. With Parrish as the study co-chair, the study found that eye drops to treat elevated pressure could be effective in delaying the onset of glaucoma. Bascom Palmer’s glaucoma researchers also took part in the nationwide Advanced Glaucoma Intervention Study (AGIS), which examined outcomes of laser and surgical glaucoma treatment. As a member of the AGIS Monitoring Committee, Palmberg suggested analyzing the relationship between pressure and vision loss. “We now have medical and surgical ways of achieving the needed reduction in eye pressure in nearly all cases, and we have learned how to avoid or to fix most complications of surgical treatment,” he said. “That’s great news for patients.”
Revolutionizing AMD treatment Rosemary Kohler began losing her eyesight in the early 2000s from age-related macular degeneration (AMD). Fortunately, Philip J. Rosenfeld, M.D., Ph.D., (fellow 1996), professor of ophthalmology, was quickly able to stabilize her eyesight. Rosenfeld had spent two decades seeking more effective treatments for the “wet” form of AMD. When he began studying this disorder at Bascom Palmer in the 1990s, AMD treatment involved thermal laser photocoagulation and photodynamic therapy to destroy abnormal blood vessels; however, he felt there had to be a better approach.
Over the years, he tested Retaane®, Macugen® and Lucentis® , various medications that target the body’s vascular endothelial growth factor, a protein associated with the formation of abnormal blood vessels in the affected eyes. While these treatments proved to be effective in many patients, Rosenfeld kept searching.
In early 2005, Kohler became one of Rosenfeld’s first patients to participate in his clinical study of Avastin®, a drug similar to Lucentis that had been approved for use in treating colon cancer. Drawing on his medical insights, Rosenfeld felt Avastin could also be effective in repairing damaged blood vessels in the retina.
“Not only did Avastin halt the progression of wet AMD in his patients, many even regained vision just a few days or weeks after treatment.,” said Carmen Puliafito, a coprincipal investigator with Rosenfeld. “It was truly a revolutionary advancement.”
Bascom Palmer’s director of pharmacy services, Serafin Gonzalez, PharmD, and his staff assisted Rosenfeld’s work. A specialist in ophthalmic compounding, Gonzalez was the first to compound bevacizumab (generic Avastin) for intraocular injection and his protocol is currently used worldwide.
Ophthalmologists around the globe quickly put Rosenfeld’s findings into practice and honored him for his contributions. “I am honored to receive recognition, but what is even more important is that patients all over the world can now see because of these drugs,” said Rosenfeld.
In the ophthalmic plastics service, Thomas Johnson helped advance a surgical procedure called optic nerve sheath fenestration, which relieves built-up pressure around the optic
“Not only did Avastin halt the progression of wet AMD in his patients, many even regained vision just a few days or weeks after treatment. It was truly a revolutionary advancement.”
– Carmen Puliafito, M.D.
nerve that can lead to permanent vision loss and blindness. In this proceedure, one of the muscles controlling the movement of the eye is disconnected, allowing the surgeon to rotate the eye and gain access to the optic nerve. A window is then cut into the optic nerve sheath, allowing the excess fluid to escape. The results are immediate, often restoring most of the vision that was lost, and halting further vision loss.

In 2006, Eduardo Alfonso unraveled the mystery behind a worldwide outbreak of fungal corneal infections among users of soft contact lenses associated with the use of a contact lens solution. Working with the U.S. Centers for Disease Control, Alfonso and his colleagues notified ophthalmologists around the world about the findings, reducing the number of new keratitis cases. A global product recall was prompted by his findings.
“Our laboratory team saw an increase in the number of cases of this unusual infection – something a non-ocular laboratory might have missed,” said Alfonso. “Had it not been for our specialized laboratory resources under the direction of Dr. Darlene Miller, we would not have been able to alert the world to this epidemic.” Miller is a research professor of ophthalmology and scientific director of the ocular microbiology laboratory.
During the COVID-19 pandemic, the expertise of Darlene Miller, D.H.Sc., and her
team in the ocular microbiology laboratory was again evident. The current tests for COVID-19 use nasal and sputum swabs to check for respiratory infections, but Miller notes, “while the risk of transmission from the eye is small, the virus has been documented in tears and conjunctiva swabs.”

A study with a worldwide impact on glaucoma care was co-chaired by Steven J. Gedde, M.D., (fellow 1996), professor of ophthalmology, and holder of the John G. Clarkson Chair in Ophthalmology. The multicenter, randomized “Tube Versus Trabeculectomy (TVT) Study” launched in 2006 compared the safety and efficacy of a tube shunt implantation with trabeculectomy in patients with prior ocular surgery.
“Our collaborative study found a higher success rate with the tube shunt surgery,” said Gedde in announcing the five-year findings in 2012. “That prompted a shift in practice patterns throughout the ophthalmology community.” The outcome of the TVT Study prompted a second five-year trial. The Primary Tube Versus Trabeculectomy (PTVT) Study began in 2016 and involved glaucoma patients without prior ocular surgery.
“Both procedures showed a similar IOP reduction,” said Gedde, who presented the five-year results at the 2021 AAO meeting. “There was no difference in failure rates, and late-onset complications were similar. Before this study, tube shunts were reserved for the most challenging cases. Now, the findings suggest that tube shunts may be an appropriate choice as an initial glaucoma procedure.”
While therapeutic interventions for glaucoma typically focus on reducing intraocular pressure, the disease continues to progress in a subset of patients despite adequate control of IOP.

David Greenfield served as a principal investigator for the multicenter randomized “Low-pressure Glaucoma Treatment Study,” and for the past three decades, his research
has advanced the understanding and treatment of normal-pressure glaucoma. LoGTS was a prospective, randomized clinical trial that investigated visual field outcomes in normal pressure glaucoma patients treated either with a topical betaadrenergic antagonist (timolol maleate 0.5%) or an alpha2-adrenergic agonist (brimonidine tartrate 0.2%).
The patients randomized to treatment with brimonidine were significantly less prone to develop visual field progression compared to those treated with timolol despite similar intraocular pressure levels during the course of the study. There was also a trend towards less frequent optic disc hemorrhage in the eyes treated with brimonidine. This was the first randomized clinical trial to demonstrate the possibility of a pressure-independent treatment effect on visual function in patients with glaucoma.
At Bascom Palmer, specialists in ocular surface disorders are leading the way in clinical care, with a wide spectrum of personalized treatments to preserve and restore patient’s vision, according to Amescua, an associate professor of clinical ophthalmology and medical director of the ocular surface program. “Our researchers have developed special medications, biological therapies, and photodynamic treatment while gaining a better understanding of this important, but often neglected, aspect of vision care,” Amescua said.
have access to advanced automated equipment for imaging and treatment for dry eye syndromes and ocular surface diseases.
Anat Galor, M.D., (fellow 2008), professor of ophthalmology, focuses on the peripheral nerves serving the eye, as well as the brain itself, as some eye medications can increase the sensitivity of nerves serving the ocular surface. “One of the biggest challenges we face is when a patient has an ocular surface that looks perfect but still experiences pain or dryness in the eye,” said Galor. “We may need to run tests of the nerves, and are researching to find new treatment modalities to combat ocular pain.”
Bascom Palmer professor John R. Guy, M.D., was one of the world’s leading experts in the field of neuro-ophthalmology at the time of his death in 2020. He was known for his pioneering gene therapy research for the treatment of Leber hereditary optic neuropathy (LHON), as well as his research on optic neuritis, multiple sclerosis, and other diseases caused by mutations in mitochondrial DNA.
Guided by Byron Lam, founding medical director of Bascom Palmer’s Center for Hereditary Eye Diseases, Bascom Palmer’s team continues to be at the forefront of the fast-growing field of gene therapy – as well as virtually every other field in ophthalmology.
Bascom Palmer’s surgical team, led by Janet Davis, has performed more than 100 subretinal gene therapy procedures for inherited retinal diseases such as retinitis pigmentosa and choroideremia.
For example, in 2018, with his sight steadily worsening due to a blinding inherited condition, 9-year-old Creed Pettit became the first patient to undergo a landmark gene therapy surgery at Bascom Palmer. Creed was diagnosed at age 2 with Leber congenital amaurosis, a disease caused by an RPE65 genetic mutation. His family came to Bascom Palmer to find a treatment for his condition.
Audina M. Berrocal, M.D., (fellow 2001), a pediatric retinal surgeon and professor of clinical ophthalmology, injected Luxterna®, a product developed by Spark Therapeutics that makes the photoreceptor cells on the retina produce a protein that people with the RPE65 genetic mutation lack.
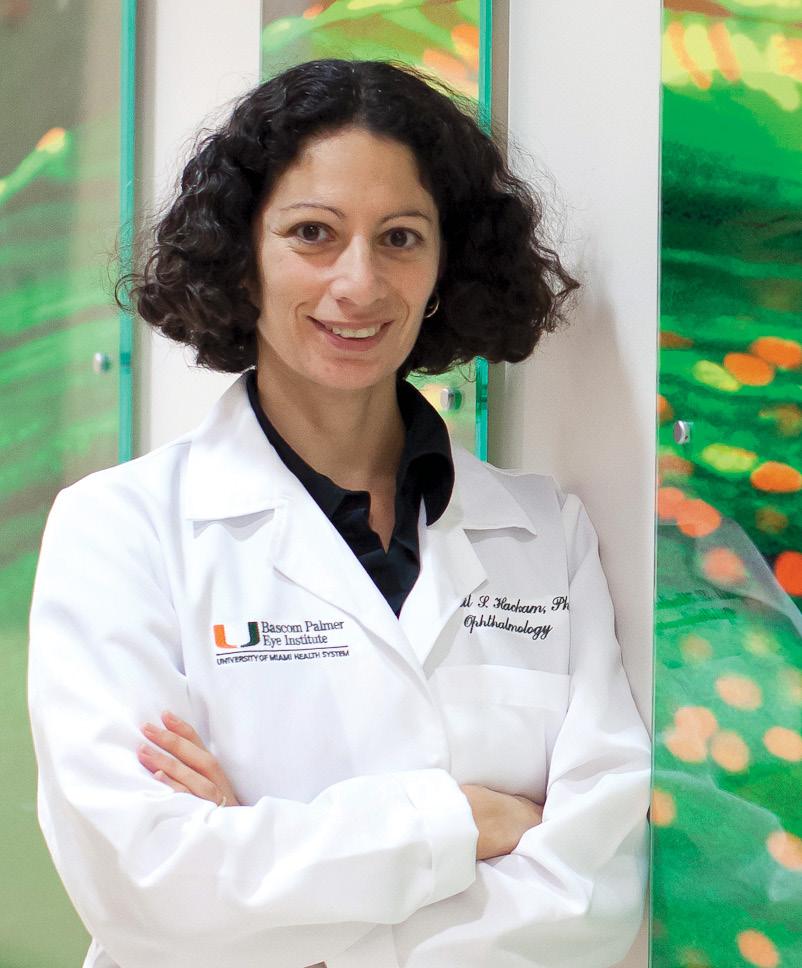
Professor of clinical ophthalmology Ninel Z. Gregori, M.D., (fellow 2006) has also been involved in pivotal clinical trials focusing on gene therapy for inherited retinal diseases as well as embryonic stem cell-derived RPE cell transplantation for age-related macular degeneration and Stargardt disease. She performed the first Argus II retinal prosthesis implantation in Florida.
“From its foundation, our Institute’s success has been inspired and sustained by novel bench-to-bedside and clinical research,”
said Vittorio Porciatti, D.Sc., vice chair and director of research, and holder of the James L. Knight Professorship in Ophthalmology. “Using the advanced tools of the 21st century, including genetics, cellular biology, molecular diagnostics, biotechnology, imaging, and artificial intelligence, our researchers are poised for another exciting decade of discoveries to prevent and cure eye diseases.”
In the past decade, Bascom Palmer’s scientists have continued to explore new fields. For instance, Porciatti pioneered a non-invasive electrophysiological tool called PERG (pattern electroretinography) to identify problems with the optic nerve neurons before they die – a critical step in treating LHON to prevent loss of vision.

Another scientist and professor of ophthalmology, Sanjoy K. Bhattacharya, Ph.D., is using mass spectrometry to study the structural and functional damage that occurs to the trabecular meshwork and optic nerve in glaucoma. “Our combined proteomic and lipidomic approach is providing new insights into the pathophysiology of glaucoma,” he said.
Valery I. Shestopalov, Ph.D., a professor of ophthalmology and molecular cell biologist – whose research projects in the retina investigate cellular and molecular mechanisms underlying injury, loss of

functionality, and death of retinal ganglion cells – was one of 57 U.S. researchers honored by President George W. Bush in 2004 with the Presidential Early Career Awards for Scientists and Engineers. His research projects on the retina investigate cellular and molecular mechanisms underlying injury, loss of functionality, and death of retinal ganglion cells, which is a fundamental clinical problem and the cause of blindness in many human diseases.
With research supported by the National Institutes of Health and private foundations, Abigail S. Hackam, Ph.D., research professor of ophthalmology, is investigating new treatments to protect the retina in agerelated macular degeneration, as well as glaucoma and inherited diseases. One focus is on specifically modifying the retinal damage responses in order to halt disease progression and promote tissue repair and regeneration. Several years ago, she found that a diet enriched with grapes had a beneficial impact, and is now looking at repurposing growth factors to stimulate the development of new nerve fibers called axons in laboratory models.
“One of the great things about Bascom Palmer is the wide-ranging expertise of the faculty,” said Hackam, the Institute’s director of laboratory research. “There are many collaborative studies underway involving innovative approaches to imaging, medical therapies, and surgical procedures.”
Bascom Palmer’s tradition of innovation shows no signs of letting up, despite the challenges posed by the COVID-19 pandemic. “Reduced laboratory time slowed progress of ongoing experiments but allowed our scientists to produce more papers and grant submissions using available data,” said Porciatti.
Responding to the pandemic, the Institute’s Ophthalmic Biophysics Center team developed a web-controlled robotized slit-lamp useful for remote patient examinations from anywhere in the world and useful in a pandemic. Other
innovations include an instrument to assess light sensitivity of patients undergoing gene therapy and an instrument to treat patients with corneal infections. Under development are an optical system to visualize aqueous humor scleral outflow, subminiature implants releasing medications to treat glaucoma, a biocompatible titanium keratoprosthesis (artificial cornea) for patients not amenable to cornea transplant, and several diagnostic instruments.
“In the next few years, the Institute will be promoting highimpact research such as gene therapy, stem cell therapy, and gene editing therapy,” said Porciatti. “Our other priorities include developing new technology such as biomaterials, drug delivery vehicles, and imaging instruments. Our key strengths include our faculty, residents, and fellows. Our ability to bring scientists and clinicians together for the benefit of patients will continue to drive innovation throughout the Bascom Palmer Eye Institute.”
Audina Berrocal, M.D., with 9-year-old Creed Pettit in 2018,who said, “I could see a rainbow for the first time,” following his gene therapy surgery.
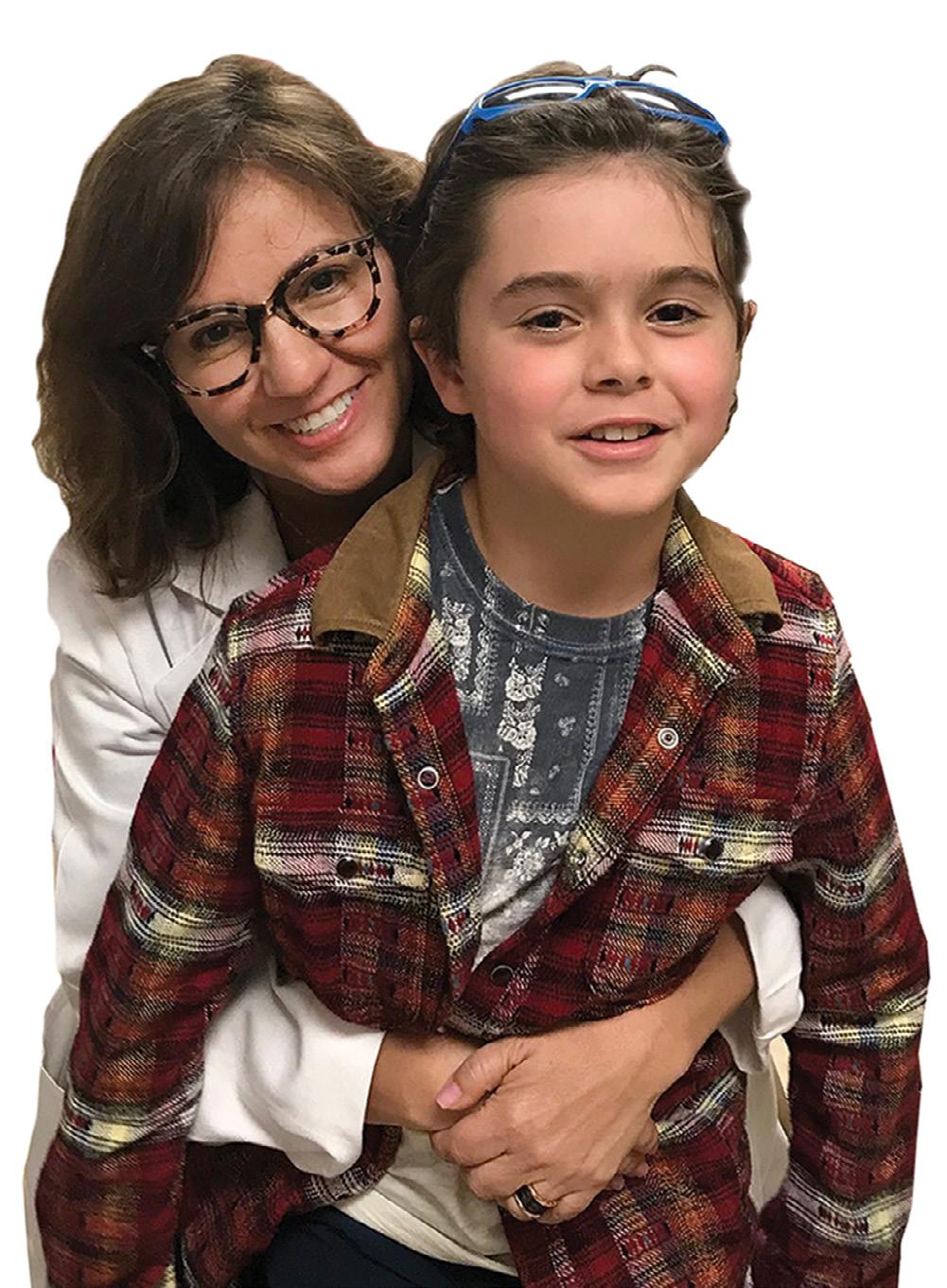
1966
1969
1974 Richard K. Forster, M.D., pioneers the use of intraocular antibiotics for endophthalmitis.

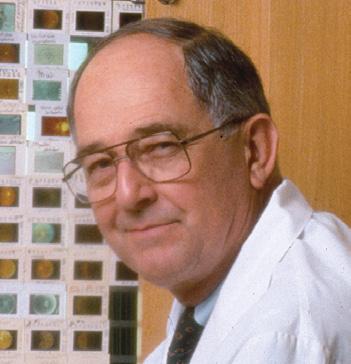
Bascom Palmer Eye Institute’s story dates back to the 1920s when Bascom H. Palmer, M.D., opened one of Miami’s first ophthalmology practices. His dream was to establish an eye clinic dedicated to saving sight and preventing blindness. Looking to the future with hope, he predicted Miami would eventually be home to an ophthalmology institute second to none in the nation.
The opening in 1962 of Bascom Palmer Eye Institute, named in honor of Dr. Bascom Palmer, was the first step in the long journey to the Institute’s global leadership in ophthalmology. Under the dynamic 33-year leadership of Edward W.D. Norton, M.D., and the chairs who followed him, Bascom Palmer has become one of the world’s foremost academic centers for scientific discovery and clinical innovation.
As Bascom Palmer Eye Institute looks ahead to the next 60 years, it will continue to be guided by Dr. Norton’s words, “The patient’s needs always come first.”
1970
performs the world’s first pars plana vitrectomy for retinal detachment.
1970 Biomedical engineer JeanMarie Parel, Ph.D., begins a 50-year journey of inventing or improving more than 350 ophthalmic instruments
1974 John T. Flynn, M.D., discovers the appropriate amount of oxygen to be used in incubators will save the retina and vision of infants with retinopathy of prematurity.


1976 Douglas R. Anderson, M.D., discovers that elevated intraocular pressure impairs axonal transport in the optic nerve and is affected by glaucoma
1984 Richard K. Parrish II, M.D., introduces the drug 5-Fluorouracil (5-FU) to prevent the growth of scar tissue following glaucoma surgery.
1988 Paul F. Palmberg, M.D., Ph.D., redefines glaucoma treatment throughout the world by determining the proper “target pressure” in the eye.
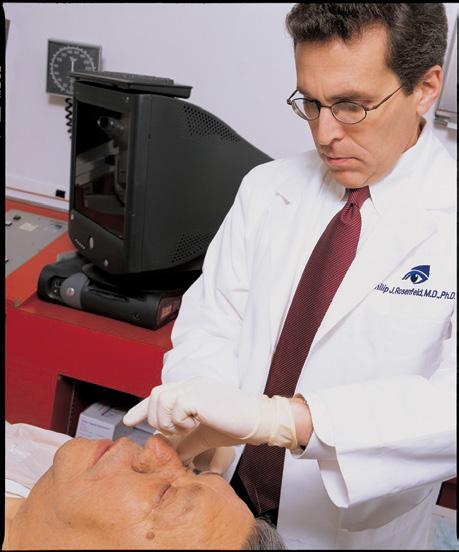
1991 William Smiddy, M.D., is among the first physicians to perform surgery to close a macular hole
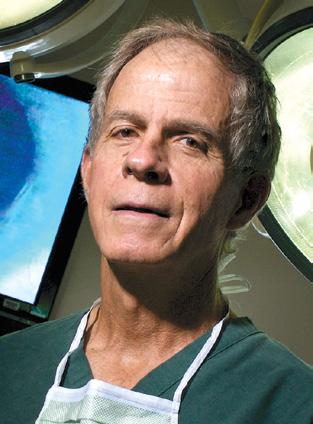
1993 William W. Culbertson, M.D., identifies the herpes virus as a cause of acute retinal necrosis, a devastating infection of the retina.
1994 U.S. News & World Report names Bascom Palmer the #1 eye hospital in the country, an honor it receives time and time again.
1998 William W. Culbertson, M.D., performs the first successful posterior lamellar endothelial transplantation.
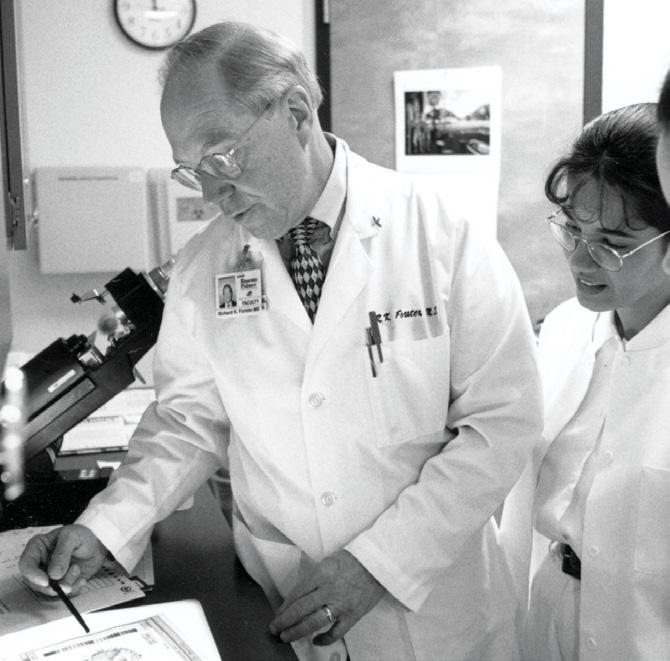
2001 Carmen A. Puliafito M.D.’s, inventive work in retinal imaging using optical coherence tomography gives ophthalmologists around the world new diagnostic and treatment tools.
2006 Philip J. Rosenfeld, M.D., Ph.D., pioneers the treatment for the wet form of age-related macular degeneration using a cancerfighting drug named Avastin®, forever changing the course of treatment for this blinding disease


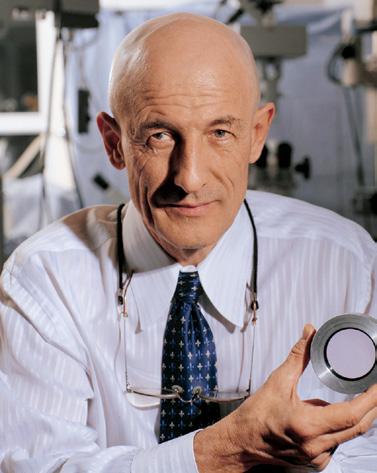
2006 Eduardo C. Alfonso, M.D., unravels the mystery behind a world-wide outbreak of fungal infections among contact lens users.
2011 Byron Lam, M.D., discovers a key gene of retinitis pigmentosa
2013 Guillermo Amescua, M.D., performs the first mother-son corneal transplant in South Florida history


2015 Janet L. Davis, M.D., and Ninel Z. Gregori, M.D., perform the first “Bionic Eye” implantation procedure in Florida.

2016 Alana Grajewski, M.D., performs life-changing pediatric glaucoma surgery that restores sight to a blind toddler from Brazil.
2018 Led by Audina Berrocal, M.D., a Bascom Palmer surgical team using leading-edge gene therapy for an inherited eye disorder, restores sight to a 9-year-old boy.
2020 Bascom Palmer’s new developments in telemedicine make eye care safer and more efficient for patients during the COVID-19 pandemic.

1986 David T. Tse, M.D., introduces the use of intra-arterial chemotherapy to treat lethal lacrimal gland cancer
1999 Carol L. Karp, M.D., pioneers the use of interferon for treatment of ocular surface squamous neoplasia

2014 John Guy, M.D., pioneers gene therapy techniques for treating Leber Hereditary Optic Neuropathy
2022 Bascom Palmer’s Artificial Intelligence and Computer Augmented Vision Laboratory, led by Mohamed Abou Shousha, M.D., Ph.D., is leading the way to transform vision diagnostics and personalized vision correction.

In 1973, three years after Robert Machemer performed the world’s first pars plana vitrectomy at Bascom Palmer, top retinal surgeons from around the globe gathered at Key Biscayne, Florida for the meeting of the prestigious Club Jules Gonin. Edward Norton invited Jean-Marie Parel to demonstrate the new VISC system that Machemer and Parel had conceived. After Parel and the Bascom Palmer’s Ophthalmic Biophysics Center produced 13 automated VISC systems, Norton gave the equipment to the retinal specialists attending the meeting and soon launched a training program for ophthalmologists who wanted to perform vitrectomies using this new equipment.

“Dr. Norton felt this was the best way to help patients around the world,” said Parel. “The patients could not all come to Bascom Palmer, but we could train the top clinicians to begin doing these procedures in their own countries.
Soon afterward, Norton gave the handdrawn VISC designs and a prototype to a West German surgical instrument company rather than patent the system. Before long, several manufacturers had entered the market. “The technology companies had the funds to accelerate development far beyond our capabilities,” added Parel.
This is just one early example of how the tradition of unselfish sharing of information has enabled Bascom Palmer to gain an international reputation for ophthalmology leadership in education – a role that the Institute’s scientists, clinicians, and educators have embraced through the decades.

At its inception, Bascom Palmer had only two faculty members. Therefore, Norton relied on volunteer ophthalmologists from the community to teach medical students

and ophthalmology residents. “Gradually, the voluntary faculty grew to include many former residents and fellows who remained in private practice in South Florida after completing their training at Bascom Palmer,” said Jerome (Jerry) P. Fisher, M.D., (resident 1980), president of the Bascom Palmer Alumni Association. From its earliest years,
when ophthalmology was a division of the medical school’s department of surgery, private practitioners contributed their time and expertise to teaching students about the diagnosis and treatment of disorders of the eye. “After the founding of Bascom Palmer, Dr. Norton continued to foster a mutually beneficial relationship with the community ophthalmologists who helped teach residents and fellows and provided the referral source for many patients,” Fisher added. “Dr. Norton encouraged community physicians to bring in patients with interesting or unusual eye illnesses to Grand Rounds on Thursday mornings, or to staff clinics for the physicians-in-training.”
In addition to David Kasner, who taught cataract surgery to residents for more than
“Bascom Palmer played a pivotal role in the advance of intraocular lenses, and Dr. Norton was a great ally in what has been called one of the world’s greatest medical innovations as far as improving the quality of life.”
– Norman Jaffe, M.D.
30 years, Richard Shugarman, M.D., was another notable community physician who taught hundreds of residents and fellows throughout his 50-year affiliation with the Institute. Serving as a volunteer faculty member, his involvement in the resident contact lens clinic was legendary.
Harry Horwich, M.D., taught pediatric ophthalmology to residents; Richard Tenzel, M.D., (honorary alumnus), one of Florida’s first oculoplastic surgeons, donated his time for 25 years to teaching oculoplastic surgery; and Ralph Kirsch, M.D., (honorary alumnus), taught residents about glaucoma and cataract surgery.
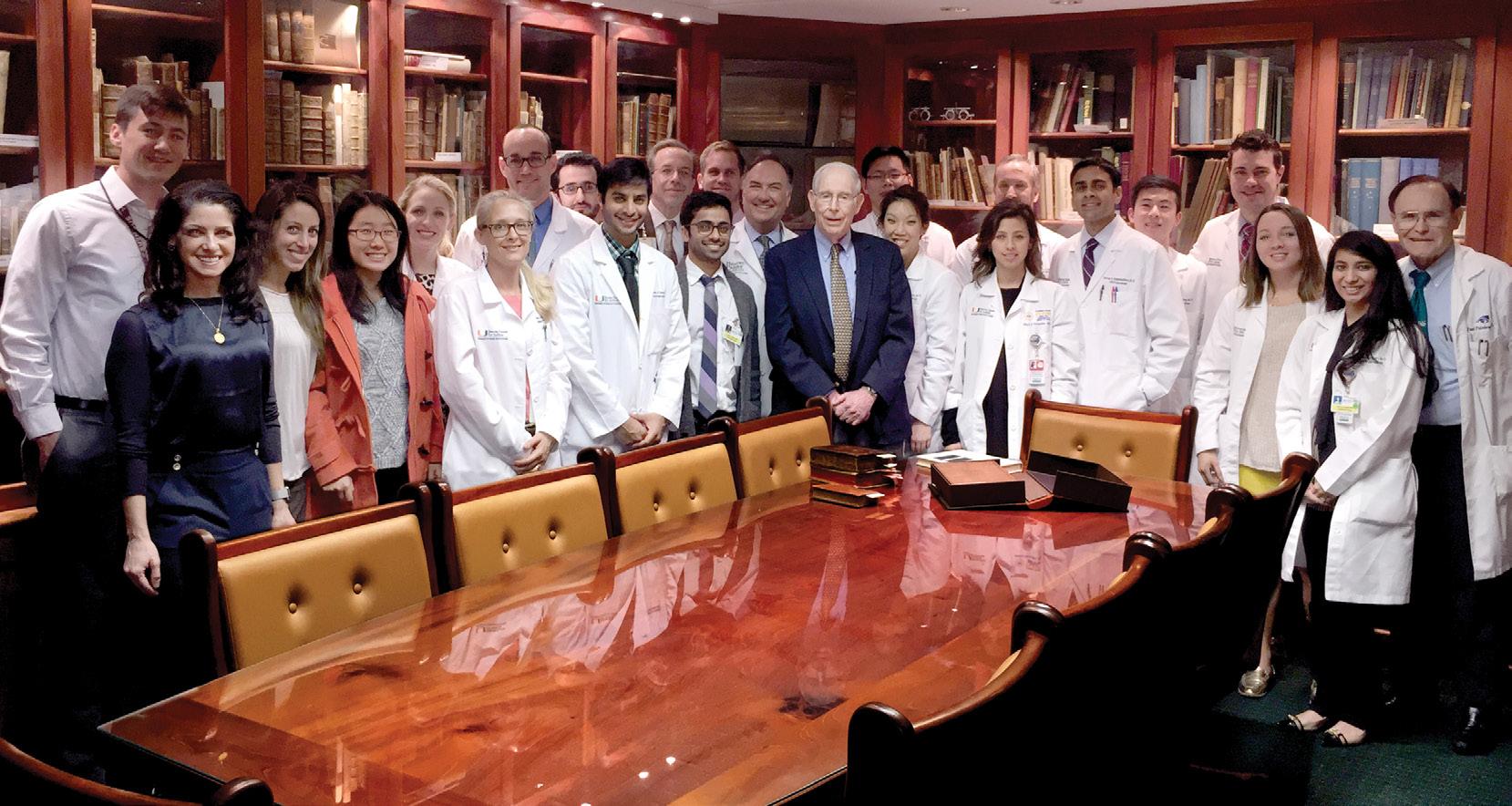
In addition, Gordon Miller, David J. Singer, M.D. (fellow 1969), and Myron Tanenbaum, M.D., (resident 1985), provided oculoplastics training for residents rotating through the Miami V.A. Hospital. Al Smith, M.D., and members of his group of pediatric ophthalmologists at Miami Children’s Hospital (now called Nicklaus Children’s Hospital) provided assistance in the pediatric ophthalmology clinics, and Wilson (“Bill”) Wallace, M.D., (resident, chief resident 1974), and William R. Stiles, M.D., (resident 1974), drove each week for decades from Boca Raton to attend Grand Rounds and assist residents in the clinics. Another voluntary faculty member, Henry M. Clayman, M.D., (resident 1972, former faculty), made himself available to the residents at Grand Rounds and in the clinic during his active practice as well as in his retirement, always sharing his knowledge with the house staff.
Since the 1960s, Bascom Palmer’s clinicians and scientists have been wellrecognized leaders in clinical care. To take just one example, cataract specialist Norman S. Jaffe, M.D., was one of Bascom Palmer’s early attending physicians and voluntary faculty members. He had a special interest in cataract extractions and wrote a textbook in 1972, Cataract Surgery and its Complications that went through six editions.
Jaffe was also one of the first U.S. physicians to use intraocular lenses in cataract surgery, implanting the first ones on December 4, 1967. “I did six cases and five
more the following day,” he recalled. “These 11 patients were so excited to have a lens rather than aphakic spectacles.”
At the time, lens implants were a controversial topic in academic medicine, as some ophthalmologists felt the implant would create ongoing problems. After 243 implant cases were completed in Miami, Norton asked the local ophthalmologists in private practice to begin a two-year moratorium on new procedures to determine whether there were any complications.
After the two-year moratorium, the Bascom Palmer physicians found that the implants gave much better vision than the prior “Coke bottle bottom” lenses without ongoing problems. When the favorable report was presented, ophthalmologists around the world resumed the procedure with rigid guidelines for lens implants. Jaffe became president of the new American Intraocular Lens Society in 1974 and Norton chaired a 1975 symposium on lens implants for the American Academy of Ophthalmology (AAO), even though he was not a cataract surgeon himself.
The so-called Miami Study of Intraocular Lens Implants became a landmark, giving the implant credibility and respectability. “Nowhere else had there been a study where physicians would stop doing a certain procedure at the request of an academic medical center,” said Jaffe. “Bascom Palmer played a pivotal role in the advance of intraocular lenses, and Dr. Norton was a great ally in what has been called one of the world’s greatest medical innovations as far as improving the quality of life.”
Bascom Palmer’s Crown Jewel
Building a library of ophthalmology was always a central focus of Norton’s vision. He often said, “Without a library, each generation must start from scratch. By studying the literature of the last half of the nineteenth and the first three-quarters of the twentieth century, one can readily appreciate the accelerated evolution of knowledge and easily predict that a similar process will continue at an ever-increasing rate into the 21st century.”
Bascom Palmer’s ophthalmic library was established shortly after the Institute first opened in 1962. Although at the time if offered little more than a handful of ophthalmological books transferred from the University of Miami School of Medicine’s Library, Norton envisioned it as ultimately becoming a repository for all ophthalmic literature – the most complete ophthalmological collection in the world. Thanks to his commitment, generous contributors, and the energy and dedication of Reva Hurtes – the founding library director who served from 1962-2004 – Norton’s vision has been fulfilled.
Through the years, more than 15,000 books have been collected, including rare and historical texts dating back to the 1400s, some not found anywhere else in the world. The Dr. and Mrs. Ralph Kirsch Rare Book Room, known as the crown jewel of Bascom Palmer, preserves 3,000 books dating from 1496 to 1900, including an exceptionally rare copy of the second edition of Georg
Bartisch: Ophthalmodouleia Das ist Augendienst (1686), published 103 years after the original edition. A 1613 book on depth perception with drawings by Peter Paul Rubens, as well as books on optics by Johann Kepler (1611), Rene Descartes (1664), and Sir Isaac Newton (1704), are also in the collection. In addition to modern textbooks, the Norton Library includes more than 250 ophthalmic journals and old periodicals from around the world including Germany, Great Britain, Italy, and France – some dating from the 1880s.
In 1987, on the 25th anniversary of the Institute, the library was formally dedicated and named the Mary and Edward Norton Library of Ophthalmology.
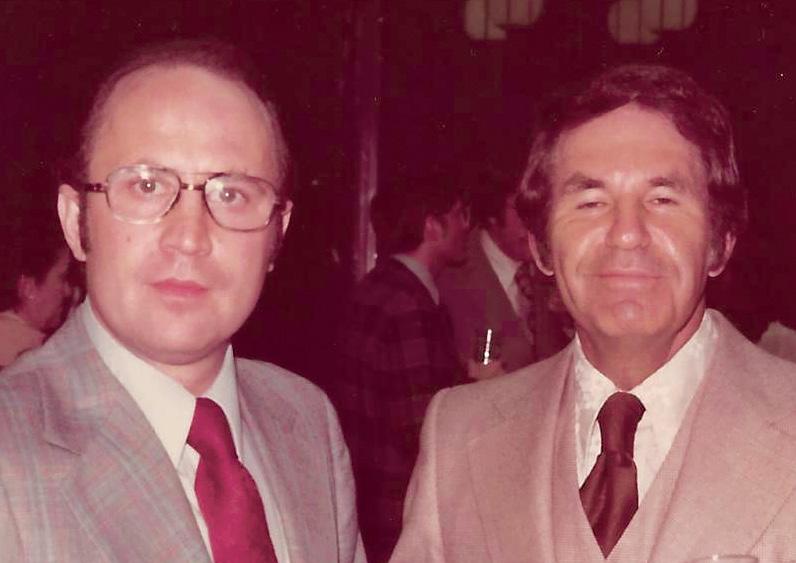
The library is undergoing extensive renovation. Upon completion, the library will comprise the Rare Book Room, Global Center for Ophthalmic Education, offices for the residency education and continuing medical education teams, study rooms for residents

and fellows, and a conference room. This Norton Library for the 21st century will be a place where our doctors can gather for individual and group study, in a peoplecentric, technology-rich environment.
In 1980, Bascom Palmer dedicated the Edith and Earl Retter Education Center. The Retters, patients of Drs. Gass and Norton, donated $800,000 toward the construction of a state-of-the-art teaching facility. “Education typically is not as well supported as research,” said Richard Forster. “This gift provided a major step forward for our entire program and helped expand the Institute’s educational mission of advancing ophthalmic knowledge.”
Shortly after the center opened, Coral Gables ophthalmologist James C. Major Sr., M.D., (resident, chief resident 1963), said, “I can bring interesting and unusual patients to Grand Rounds. This benefits our group because it increases our professional exposure to rare and unusual cases.”
In 2011, the Berrocal family graciously provided the leading gift to completely renovate the center’s auditorium. To honor the ophthalmology legacy started by José A. Berrocal, M.D., Bascom Palmer’s first fellow, (fellow 1964), the 180-seat conference hall

was renamed in his honor. The sophisticated closed-circuit TV system allows real-time images of diagnostic and surgical procedures from the operating room to be transmitted to the observers in the auditorium.
For more than 40 years, the center has been home to the Institute’s Grand Rounds, held regularly on Thursday mornings for Bascom Palmer’s faculty, residents, fellows, and South Florida physicians, regularly attracting more than 100 ophthalmologists.
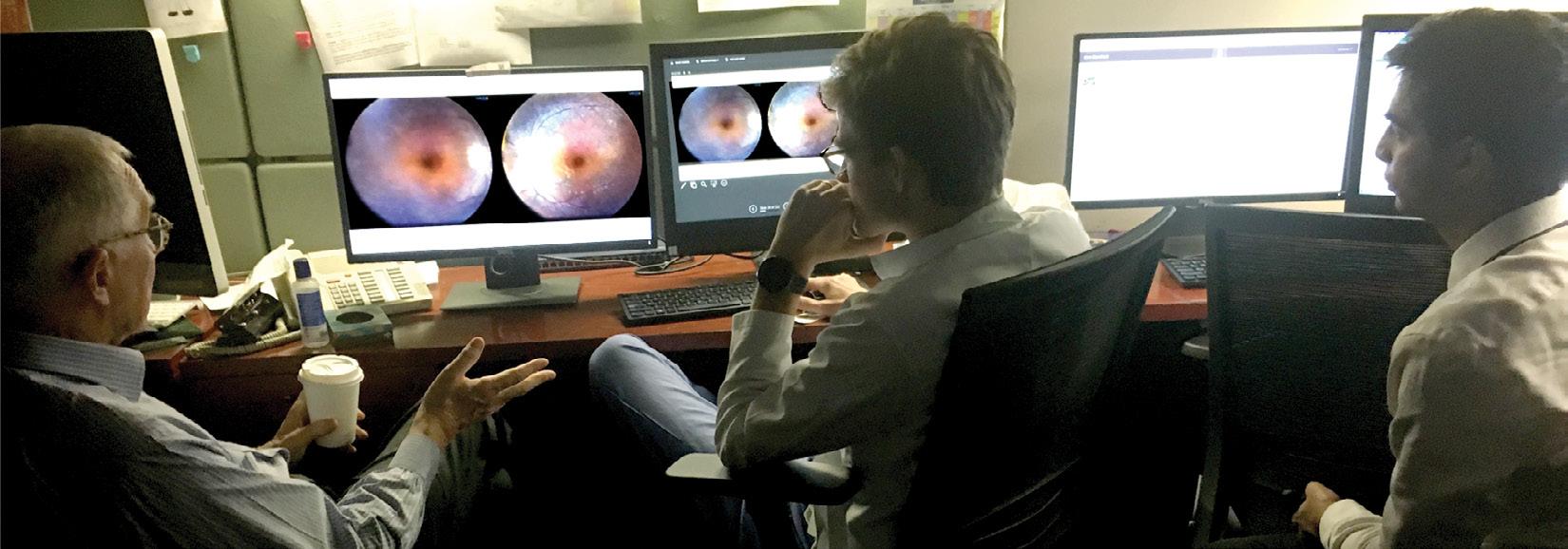
Through the decades, the Institute has continually expanded its robust calendar of events in the education center. Under the leadership of Steven Gedde, the Institute’s year-round calendar of in-person, online and hybrid events, including Grand Rounds, continuing medical education courses, an esteemed distinguished lecture series, and the popular Inter-American Course in Clinical Ophthalmology (CURSO), continues to grow.
Growing up in the Midwest, Julia Hudson, M.D., (resident 2022), set her sights on becoming a doctor. After earning her medical degree at the University of Pennsylvania, she chose Bascom Palmer for her residency training in ophthalmology. “There are several things that set Bascom Palmer apart from
the other great U.S. residency programs,” said Hudson.

“First of all, this is a very welcoming center with plenty of support from faculty and fellows,” she said. “In addition, we get a rich exposure to a high volume of very diverse patients, seeing unusual conditions. Bascom Palmer also allows us to follow our patients from start to finish, preparing us for successful practices in the future.”
Under Gedde’s remarkable 22-year tenure as Bascom Palmer’s residency program director, the program has established a worldwide reputation for excellence, attracting a growing pool of highly qualified candidates. “For 60 years, education has been an integral part of our mission,” he said. “The success of our residency program is the result of a collaborative effort among a very talented faculty who are deeply committed to teaching the next generation of ophthalmologists, as well as our leadership team, which provides unwavering support for medical education.”
With its deep commitment to education and training, Bascom Palmer has often received the #1 ranking of ophthalmology residency programs in the United States by Doximity, the largest community of healthcare professionals in the country, and by Ophthalmology Times. In recent American College of Graduate Medical Education (ACGME) surveys, 100 percent of residents and 100 percent of faculty members were “very positive” (highest rating) in evaluating the program.
In 2021, Chris Raif Alabiad, M.D., (resident, fellow 2010), succeeded Gedde as the residency program director with
Jayanth Sridhar, M.D., (resident 2014), as associate director. Both have been actively engaged with residents for many years while developing innovative approaches to ophthalmic education.
“Our program has a long tradition of excellence, said Alabiad, a professor of clinical ophthalmology and assistant dean for student affairs at the Miller School. “We have great opportunities to blend virtual and digital learning tools with clinical, laboratory, and classroom instruction. We must be ready to adapt our residency training to new conditions since we never know what lies ahead in the future.”
Sridhar, an associate professor of clinical ophthalmology, added, “We have brilliant students and it is a privilege to serve as associate director.” Sridhar has developed an educational retina podcast, Straight from the Cutter’s Mouth, that has attracted a worldwide ophthalmic audience. He also hosts Experts InSight, a podcast for the American Academy of Ophthalmology.
Each year, Bascom Palmer welcomes seven new residents to the program. In
the past, residents spent their first year after graduating from medical school (“internship”) at a program of their choice, and then matriculated into the Bascom Palmer Eye Institute’s ophthalmology residency program for their second, third, and fourth years of post-graduate ophthalmology training. In 2021, the program transitioned to an integrated format where the seven incoming residents spend their internship year at Jackson Memorial Hospital/University of Miami as part of the internal medicine department. During this exciting year, the residents spend three months learning ophthalmology under the supervision of Bascom Palmer Eye Institute faculty both at the Institute and at the Miami Veterans Affairs Hospital. Thereafter, they will spend the next three years completing an ophthalmology residency training program at Bascom Palmer.
“The learning curve for ophthalmology is very steep, and this allows our new trainees to learn from attending physicians and residents while being exposed to the different fields of ophthalmology,” Sridhar said. “We were pleased to grow our program and now have 28 residents in our Bascom Palmer family.”
One of the program’s special features is an international elective that allows residents to gain firsthand experiences about delivering vision care in underserved regions of the world. “Before the pandemic, our residents traveled the world to such locations as India, Ethiopia, Guatemala, Ecuador, Argentina, and Haiti,” said Gedde.
“Additionaly, closer to home, our residents have also organized outreach programs to provide free screening eye examinations in
underserved areas of South Florida while working with and mentoring University of Miami students for volunteerism and what is often their first exposure to hands-on ophthalmology,” Gedde added.




Meanwhile, the Institute’s residency program has been at the forefront of deploying virtual learning tools, even before the COVID-19 pandemic led to a worldwide transition in medical education. For instance, Bascom Palmer had already introduced a multifaceted surgical curriculum – including simulation training – to assist residents in transitioning to “live” patients.
Other highlights in recent years include revising the didactic lecture series, expanding the social services department, developing a formal mentoring program where incoming residents are paired with upper-level residents and faculty members, and establishing regular conferences with residents and faculty that focus on optimizing patient care and safety.
For several years, Alabiad has been involved in the Miller School’s transition to the NextGen curriculum, which includes virtual learning tools, and “flipped classroom” experiences where students do their homework before attending a class. He has been a leader in introducing simulation training, as well as building collaborative international educational relationships.
“We are actively working with professionals in Mexico and Europe to create validation studies for these simulations as we bring them into our program,” he said.
Looking ahead, Alabiad plans to build on the program’s strong foundation to provide high-quality relevant training to today’s residents. “We want to maintain the highest
level of ethics and professionalism while building a diverse medical workforce to serve our multicultural patient population,” he said. “Our other goals include providing our residents with laboratory and clinical research experiences to help them lay the groundwork for future medical breakthroughs.”
Five years ago, Bascom Palmer launched the Master of Science in Vision Science and Investigative Ophthalmology (MVSIO), a unique graduate degree focused on basic and translational eye research. Like other Bascom Palmer educational programs, the MVSIO attracts students from throughout the U.S. and beyond and had seven graduates last year.
“Our MVSIO program prepares students of different backgrounds for an academic career as physician-scientists or researchers as well as developing entrepreneurial and management skills that can lead to rewarding careers in the private sector,” said Sanjoy K. Bhattacharya, Ph.D., professor of ophthalmology and graduate program director.

“The program’s curriculum includes laboratory research with experimental models, advanced computing and analytic tools, such as analyzing big data sets to identify drug targets and molecules that will respond to those targets,” said Bhattacharya. “For researchers, we discuss how to obtain federal grants and manage funding streams for long-term continuity in the laboratory,” he added. “We also focus on navigating the regulatory issues related to investigational drugs and devices.
One of the Institute’s goals for the master’s degree program is to support entrepreneurs who can bring vision discoveries from the bench to the patient, said Bhattacharya. Toward that end, Bascom Palmer collaborates with UM’s Herbert Business School to develop financial, marketing, and management skills. Students in the MVSIO program also benefit from access to a diverse professional network, including attorneys, financiers, accountants, and other specialists.
Bhattacharya also founded a researchindustry translation program for UM Miller School of Medicine doctoral students in all specialties. “We invite business executives and other leaders from Palm Beach, Broward, and Miami-Dade counties to take part in student-run roundtables,” he said. “This helps our students build presentation skills while planting seeds for future commercial partnerships. The students also learn how to write applications for National Institutes
Health grants.”
To develop a robust and diverse pipeline of future vision specialists, Bascom Palmer offers educational opportunities to medical students as well as undergraduates and students in high school.
“Medical students from the Miller School of Medicine, as well as other institutions, rotate at our program,” said Gedde. “During the pandemic, our team developed a remote program where students could view eye surgeries while a faculty member narrated the procedure.”
For graduate, undergraduate, and high school students interested in medical research, Bhattacharya has also incorporated learning opportunities into his laboratory studies on the regeneration of axons, the tiny nerve cell fibers that send signals to muscles. “When there is severe damage to the spinal column, the ability to move hands, fingers, arms, or legs may be lost,” he said. “If the optic nerve is damaged due to glaucoma or trauma, for example, the result can be loss of vision or blindness.”
Nerve regeneration has been one of the holy grails of medicine for the last 275 years, said Bhattacharya. In 2020, Bhattacharya began holding regular weekend sessions with business school faculty members to
show students how to use natural language processing tools to digitize the findings in written studies printed in different languages from the 1750s to the 1990s. About 35 to 40 students take part in those study sessions, which have already resulted in two scholarly papers published in the journal Annals of Eye Science. Other students are sifting through molecular studies related to neural degeneration in digital format from 1990 to 2022.
“This student research helps advance our understanding of nerve regeneration in different species,” said Bhattacharya. “We are now collaborating with 15 other laboratories worldwide, combining varied data sets in a multiomics approach that hopefully will lead to new insights and potential treatments in the future.” Bhattacharya also created the Miami Integrative Metalobomics Research Center which is doing cuttingedge work encompassing collaboration of interdisciplinary investigators within the University as well as other major institutions, making Bascom Palmer one of the top centers for mass spectrometry in the eye.
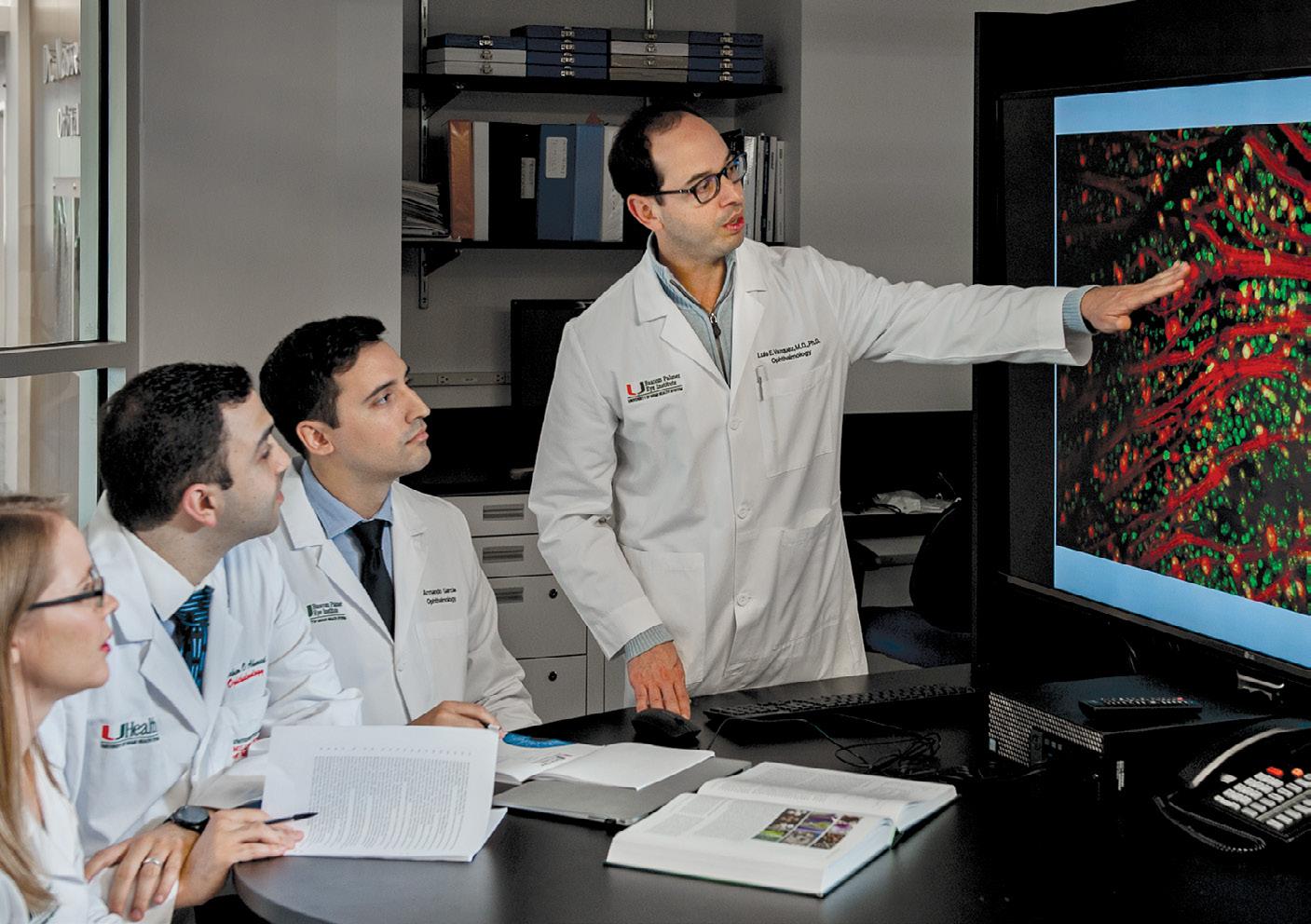
In 2019, Bascom Palmer launched the Global Center for Ophthalmic Education, incorporating all aspects of ophthalmic education, including continuing medical education (CME), residency and fellowship programs, Grand Rounds, observerships, a distinguished lecture series, and international collaborations.
“The global center coordinates our many educational offerings and supports Bascom Palmer’s professional learning at every level in virtually any location,” said Maria Serrano Brosco, executive director. “We were also able to pivot to virtual platforms to continue our educational leadership despite the challenges of the COVID-19 pandemic.”
One recent development was the launch of bascompalmerlearn.org. This new portal provides free access to a wide range of vision-related content, including CME courses, ophthalmic images, surgical videos, lectures, and courses for medical students.


As of early 2022, just one year after its launch, the portal had 14,000 users in more than 100 countries with 110,000 unique page views. “We are fortunate to have the financial support to offer so much content free-ofcharge to eye care professionals around the world,” said Serrano.
Lectures, images, and videos are posted to the portal regularly, including residents’ daily case presentations. “We want to communicate Bascom Palmer’s latest clinical
and scientific information to the ophthalmic community and take advantage of our location to advance education throughout the Americas and beyond,” Serrano said.
As the pandemic recedes, Bascom Palmer is planning to relaunch its in-person meetings, lectures, and other programs.
“We will undoubtedly offer them in a hybrid format so learners can also attend virtually,” added Serrano. “By keeping the online component, we will continue to meet the evolving needs of students, trainees, and vision professionals from Europe, Asia, Africa, Australia, and the Americas.”
“Bascom Palmer also partners with ophthalmic societies and institutions around the world, including the Colombian Society of Ophthalmology and the Pan-American Association of Ophthalmology,” said Serrano. “That multiplies the Institute’s impact on all aspects of vision care.”
Medical education is one of the most important and successful components of the Institute’s mission. Today, there are 48 chairs of academic medical center programs in the U.S. and beyond who have trained at Bascom Palmer. To take just one example, Robert Machemer left Bascom Palmer in 1978 to become chair of Duke University’s department of ophthalmology.
educational programs disseminate medical knowledge around the world and help elevate the quality of care delivered to patients.”
– Steven Gedde, M.D.
“Many of our resident and fellow graduates become leaders in academic institutions, where they train future generations of ophthalmologists,” said Gedde. “Our educational programs disseminate medical knowledge around the world and help elevate the quality of care delivered to patients.”
One of those international leaders is Martine Jager, M.D., Ph.D., (fellow 1990). Now a professor of ophthalmology at Leiden University Medical Center in The Netherlands, Jager in 2007 became the first non-U.S. president of the Association for Research in Vision and Ophthalmology (ARVO), the largest eye and vision research organization in the world.
“After I had finished my training in Amsterdam to become an ophthalmologist, I realized I wanted to combine clinical care with research,” Jager said. “I visited Bascom Palmer and attended Grand Rounds, and was astounded at the level of the faculty.” Reflecting on her cornea fellowship, Jager said, “At Bascom Palmer, I learned to look not just at the cornea, but everything around it, and to listen to the patient to identify the problem. Today, I teach my residents to do the same thing. They need to investigate all the parts of the eye as well as the ocular surface. I believe in the Bascom Palmer philosophy of treating the person – not just the eye.”
In the 1970s, Mizuo Matsui M.D., (research fellow 1972), was the first ophthalmologist to perform vitrectomies in Japan, and later became president of the Japanese Ophthalmological Society. “There is a strong tradition at Bascom Palmer of training the leading vitreous surgeons of the world,” said William Smiddy, a specialist in macular diseases and diabetic retinopathy. “Many of today’s department chairs and senior ophthalmologists around the world completed their training and fellowships here in the 1970s and 80s.” Smiddy is recognized worldwide for his extensive, high-quality clinical research regarding complications of anterior segment surgery.
John C. Merritt, M.D., (fellow 1975) who was Bascom Palmer’s first Black fellow, joined the faculty of Howard University College of Medicine in 1975, where he later became the chair of the division of ophthalmology within the department of surgery. Merritt was a pioneer in the medical use of marijuana as a treatment for glaucoma.
Noting the ongoing influence of the Institute’s graduates, former director John Clarkson said, “The esprit de corps that exists at Bascom Palmer is widely recognized by other institutions with an eye toward transferring our culture as an added benefit of hiring a faculty member.”
Bascom Palmer faculty members have also been active volunteer leaders in regional, national and international ophthalmology associations. Presidents of the American Academy of Ophthalmology (AAO) include Norton in 1980 and George Blankenship in 2001. Douglas Anderson, David Greenfield, and Kuldev Singh (fellow 1992) have served as presidents of the American Glaucoma Society, as has Donald L. Budenz, M.D., M.P.H., (fellow 1992, former faculty), who is now chair of the department of ophthalmology at the University of North Carolina at Chapel Hill.
Richard Parrish, a member of the Academia Ophthalmologica Internationalis, is the editor-in-chief of the American Journal of Ophthalmology and served as president of the American Ophthalmological Society. In 2021, the American Glaucoma Society recognized Parrish for his lifetime contribution to the Society and the field of ophthalmology.
Three of Bascom Palmer’s current faculty members have also served as president of the Florida Society of Ophthalmology, including Stephen Schwartz, Krishna Kishor, (fellow 2007), and Sarah Wellik, (fellow 2005) Wellik, a professor of clinical ophthalmology, is director of the glaucoma service at Bascom Palmer’s practice at Plantation.
Eduardo Alfonso served as president of the Pan-American Association of Ophthalmology (PAAO), an international organization with members from more than 35 countries in the Western Hemisphere. Carol Karp is now the
48 graduates of Bascom Palmer’s training programs have become ophthalmology department chairmen at medical schools and teaching hospitals throughout the world.
University of Miami
John Clarkson, M.D. Richard Parrish II, M.D. Eduardo Alfonso, M.D.
Baylor College of Medicine Dan Jones, M.D.
Boston University Stephen Christiansen, M.D.
Case Western Reserve University Douglas Rhee, M.D. Cleveland Clinic Froncie Guttman, M.D.
Columbia University Stanley Chang, M.D.
Cornell University Donald D’Amico, M.D.
Duke University Edward Buckley, M.D. Robert Machemer, M.D.
Emory University Thomas Aaberg Sr., M.D.
Greater Baltimore Medical Center
Charles Wilkinson, M.D.
Louisiana State University Jayne Weiss, M.D.
Medical College of Georgia Malcolm Luxenberg, M.D.
Medical College of Wisconsin Dale Heuer, M.D.
Mount Sinai Health System James Tsai, M.D.
Pennsylvania State University George Blankenship, M.D. David Quillen, M.D.
Saint Louis University
Oscar Cruz, M.D.
Stanford University
Mark Blumenkranz, M.D. Jeffrey Goldberg, M.D.
Temple University
Jeffrey Henderer, M.D.
University of Alabama Lanning Kline, M.D.
University of Arkansas John Shock, M.D.
University of Chicago William Mieler, M.D.
University of Florida William Driebe, M.D. Sonal Tuli, M.D.
University of Louisville Joern B. Soltau, M.D.
University of Illinois Jose Pulido, M.D
University of Nebraska Raymond Records, M.D.
University of North Carolina Donald Budenz, M.D.
University of Oklahoma Gregory Skuta, M.D.
University of Texas Southwestern J. William Harbour, M.D.
University of Virginia Brian Conway, M.D. University of Washington Philip P. Chen, M.D.
Wayne State University
Gary Abrams, M.D. Yale University James Tsai, M.D.
Universidade Federal de São Paulo, Brazil
Ana Hofling-Lima, M.D.
University of Ottawa Steven Gilberg, M.D.
Queen’s University, Ontario, Canada Martin van Hove, M.D.
Hospital Dr. Elias Santana, Dominican Republic Juan Batlle, M.D.
University of Erlangen, Germany Freidrich Kruse, M.D.
University of Lubeck, Germany Horst Laqua, M.D.
University of Barcelona, Spain Elena Barraquer, M.D.
Uppsala University, Sweden Per Soderberg, M.D.
Chuang-Gung Memorial Hospital, Taiwan
Ray Jui-Fang Tsai, M.D. Baskent University, Turkey Dilek Dursun, M.D.
“Our
president-elect of the organization. Alfonso was also honored with the University of Monterrey’s Catedra Laboris designation, akin to an honorary chair, after signing a cooperation agreement with the Fundación Ojos para México (the Eye Foundation for Mexico) to promote ophthalmic research, knowledge-sharing, and student outreach. More recently, he received the prestigious 2020 Claes H. Dohlman, M.D. Award presented by the Cornea Society and Eye Bank Association of America, and has just begun a three-year initial term commitment on the board of directors of the National Alliance for Eye and Vision Research and the Alliance for Eye and Vision Research (NAEVR/AEVR) after having completed a two-cycle appointment on the NIH/NEI National Advisory Board.
Additionally, John Clarkson served as president of the Macula Society and the American Ophthalmological Society, and CEO of the American Board of Ophthalmology, the independent, nonprofit organization responsible for certifying the nation’s ophthalmologists. Furthermore, Janet Davis served as chair of the American Board of Ophthalmology in 2016.
Bascom Palmer faculty members are also leaders in supporting diversity in ophthalmology as well as fostering an inclusive culture of belonging and opportunity for all. Raquel Goldhardt (fellow 2010), an associate professor of clinical ophthalmology, chairs the Institute’s diversity, equity, and inclusion initiatives.
In 2020, the AAO recognized Elizabeth Hodapp as an “unsung hero of ophthalmology.” Nominated by her colleagues, she was honored for quietly serving the underserved, mentoring the next generation of ophthalmologists, and sharing her skills with the world.
With a worldwide alumni network of hundreds of ophthalmologists who have completed residencies and fellowships at the Institute, Bascom Palmer faculty members conduct collaborative scientific projects and clinical trials with their counterparts around the globe.
One example is Juan Batlle, (resident, fellow, chief resident 1984), who studied the prevention of blindness. Since then, he has been engaged in numerous collaborative projects world-wide and has transformed eye care and education in the Dominican Republic and Latin America.
William Culbertson collaborated with him in clinical studies during the early 2000s on a new form of cataract laser surgery, which soon afterward was approved by the U.S. Food and Drug Administration (FDA). Batlle also collaborated with Jean-Marie Parel in clinical trials of an innovative micro-drainage shunt in glaucoma patients, which is currently awaiting FDA approval.
Bascom Palmer has a long history of providing medical education and training to Latin American physicians. In 1979, Norton and former faculty member Don H. Nicholson, M.D., launched the InterAmerican Course in Clinical Ophthalmology (CURSO) to provide physicians in Latin
America and the Caribbean with the latest information on the diagnosis and treatment of vision diseases and disorders.
Now in its 43rd year, and currently directed by Eduardo Alfonso, Carol Karp, and Paul Palmberg, the course material is presented with simultaneous English-Spanish translation. One of the CURSO highlights is the annual Francisco E. Fantes, M.D. Distinguished Lecture, named in memory of the dedicated and beloved Bascom Palmer physician and educator.
“Training doctors from other countries is one of the most important things that have been done here,” said Norton.
Today, CURSO continues to be the largest meeting in the United States held for Spanish-speaking ophthalmologists. Topics span the entire field of ophthalmology with particular emphasis on practical clinical education.
“Our last in-person CURSO was in the fall of 2019, just before the pandemic,” said Karp. “We had more than 800 attendees who heard presentations from 30 faculty members from
Bascom Palmer and other institutions. It was a wonderful, interactive, educational, and social meeting.” During the pandemic, CURSO attracted many more attendees in its virtual education platform.
When training or consulting with physicians in other parts of the world, Bascom Palmer is committed to global leadership. As Gedde said, “I believe there is tremendous potential to positively impact patient care through education. Graduating residents and fellows can elevate the quality of patient care that is delivered in their local communities. As they educate other physicians, they participate in the global dissemination of scientific and clinical knowledge. Since its founding, Bascom Palmer has certainly made a powerful impact on ophthalmology. I am confident it will continue to do so for the next sixty years and beyond.”
More than 800 ophthalmologists from Latin America and the Caribbean attended CURSO in 2019.

In times of need, Bascom Palmer responds. Bascom Palmer’s three medical relief teams of doctors and ophthalmic technicians traveled to the Gulf States following Hurricane Katrina rendering care to victims of the deadly storm as well as to members of the National Guard.
Bailey Peterson, O.D., an optometrist at Bascom Palmer at Naples, knows that better vision can change a child’s life. “Last year, Bascom Palmer’s school eye screening program in Collier County identified a 9-yearold girl from Guatemala with double vision,” she said. “Her family didn’t realize she had a problem and couldn’t pay for treatment. Our pediatric ophthalmologist performed the surgery the child needed and we were able to give her normal vision and change the trajectory of her life.”
Thanks to philanthropic support from the Naples Children & Education Foundation, there were hundreds of other success stories for the screening program, which reached approximately 15,000 kindergartenaged through 8th-grade students in Collier County’s Title 1 schools. Following the vision screening, approximately 25 percent of the children received full eye exams and two pairs of glasses. Students who needed tertiary care came to Bascom Palmer for further testing and treatment. The program teaches parents and teachers the importance of glasses and overall eye care. “If a child cannot see the teacher or the classwork, it is very difficult to learn,” Peterson said.
Today, Bascom Palmer’s vision professionals are making a difference in communities throughout South Florida and around the world. In another example, Michelle Falcone, M.D., (resident 2020), an assistant professor of clinical ophthalmology at Bascom Palmer at Palm Beach Gardens and a specialist in pediatric ophthalmology and strabismus, is planning a school screening program in Palm Beach County modeled after the Collier County initiative.
“Philanthropy funds our service mission,” said chair Eduardo Alfonso. “Last year, we received $23 million from donors to support these and other high-impact programs that make a huge difference for children and families in our region.”
One of Bascom Palmer’s most powerful programs is the “33136 Initiative,” designed to improve the health and well-being of residents in the low- and moderate-income neighborhoods living in zip code 33136, the area surrounding the University of Miami’s Miller School of Medicine campus and Jackson Memorial Hospital. The project will give the Institute’s specialists a better understanding of how to address preventable vision loss in underserved neighborhoods.
“From its inception, Bascom Palmer’s mission has included providing impeccable care to the Miami community,” said Zubair Ansari, M.D., (resident 2018), assistant professor of clinical ophthalmology and medical director of community clinical services. “Through the years, our faculty and staff members have been building on that tradition, and this program focuses on the challenge of addressing vision loss in our back yard.”

Treating patients in Louisiana during the Hurricane Katrina relief mission


The multidimensional 33136 project includes vision screening, education, preventive care, and clinical services, as well as opportunities to participate in research studies. “We want to keep our community as healthy as possible,” said Ansari. “We hope that this model can be translated for other chronic health conditions, such as heart disease or diabetes.”
“Our faculty and residents work with the University of Miami medical students for community vision screening,” said Richard K. Lee, M.D, Ph.D., (resident, fellow 2004), an associate professor of ophthalmology, holder of the Walter G. Ross Distinguished Chair in Ophthalmic Research, and Bascom Palmer’s associate medical director of community clinical services. Lee and Goldhardt, an associate professor of ophthalmology, are co-faculty advisors of the medical school’s Ophthalmology Interest Club. “Health fairs give the students an opportunity to gain firsthand experience in conducting eye examinations while learning from their mentors at Bascom Palmer.”
Although community health fairs were canceled during the height of the COVID-19 pandemic, in-person vision screenings safely resumed outdoors and at indoor sites with adequate space and ventilation.
Along with detecting ocular disease, the Institute’s service programs also provide opportunities to contribute to research studies, added Lee. For instance, medical students Elaine Han, M.D., and Ryan Nolan, M.D., were co-authors with Lee, a glaucoma
specialist, on a 2020 paper, “The Role of Telemedicine in Population-Based Glaucoma Vision Screening,” published in Glaucoma Today. One of the takeaways from their study was the growing importance of telemedicine in providing timely access to vision care in a variety of settings, including urban and rural clinics. Along with Richard Parrish, Lee also published the only study assessing the incidence and severity of glaucoma in the Haitian population through community health fairs in Little Haiti, a neighborhood of Miami.
For nearly 20 years, one of Bascom Palmer’s most important assets has been the Vision Van – a 40-foot, custom-designed mobile eye clinic for screening and clinical care. Donated by the Joesphine S. Leiser Foundation, it has traveled throughout Florida and around the world to help people in need of eye care.

After Hurricane Katrina devastated the Gulf Coast in September 2005, Bascom Palmer’s doctors and staff members traveled with the Vision Van on a three-week relief mission, treating first-responders and hurricane victims, and dispensing more than $100,000 worth of eye medications, prescription glasses, sunglasses, and contact lenses to those in need at no cost.
The Institute’s team spent 18 days in New Orleans and Baton Rouge, treating hundreds of patients in areas where there were no medical facilities. Lt. General Russel Honoré, commander of Joint Task Force Katrina, presented Bascom Palmer with a medallion honoring its medical service.
After a devastating earthquake hit Haiti on January 12, 2010, Bascom Palmer quickly mobilized a response team. The first Bascom Palmer team arrived 48 hours after the earthquake with ophthalmic equipment and supplies, offering general medical aid and eye surgery in a University of Miami field hospital in Port Au Prince that Thomas Johnson and other volunteers helped establish. In the ensuing months, Bascom Palmer physicians, nurses, technicians, and employees brought medications, eyeglasses, and medical instruments to Haiti and provided critical ophthalmic and trauma care.
When northern Japan was hit by the Tohoku earthquake and tsunami in March 2011, Bascom Palmer offered help to the ophthalmologists in Japan. The Japanese government then arranged for the Vision Van to travel to the hard-hit Sendai region aboard the world’s largest air transport – an Antonov 124, arranged by Michael Kelley, director of strategic operations at Bascom Palmer. Once on the scene, Richard Lee joined forces with doctors and staff from Keio University, Iwate University, Tohoku University, and the Japanese Ophthalmological Society in a special eye rescue mission.
Lee provided training to Japanese ophthalmologists who volunteered to use the Vision Van for emergency vision screenings and eye treatments and to provide more than 1,000 ready-made eyeglasses for people who lost or broke their lenses.


“We appreciated Bascom Palmer’s support in the healing of Japan,” said Kazuo Tsubota, M.D., chief of the department of ophthalmology of the Keio University School of Medicine in Tokyo and a former classmate of Eduardo Alfonso. Based on their experience using the Vision Van, a team of Japanese ophthalmologists built a mobile clinic that has subsequently been used to help victims of natural disasters in Asia.
Closer to home, in 2017, the Vision Van traveled to Key West after Hurricane Irma destroyed many communities in the Florida Keys, providing support to first-responders and other patients with eye emergencies. Eye injuries are very common after a disaster, as
are lost eyeglasses. Restoring eye health is a priority, because when people can’t see, they are at high risk for other injuries, as their whole environment becomes unfamiliar. In addition, closed pharmacies mean that people quickly run out of medications and need antibiotics for acute eye injuries.
In 2020, with funding from The Salah Foundation and Canon U.S.A., Bascom Palmer obtained a smaller, second Vision Van able to go to schools, churches, and other locations in Miami-Dade and Broward counties. “This smaller van gives us the added flexibility to bring our optical instruments and our volunteers to neighborhoods in need of eye screening or care,” said Ansari. “We look forward to expanding our outreach and building more partnerships with local organizations in the future.”
Bascom Palmer’s annual mission trip to the Galapagos Islands has provided eye care to thousands of residents.


Shown here with a group of children are Raquel Goldhardt, M.D., Richard Lee, M.D., Ph.D., and the government head of Isabela Health from the Galapagos Ministry of Health.
Bascom Palmer’s outreach programs extend far beyond South Florida. For instance, the Institute has a longstanding relationship with physicians in Haiti through Project Medishare, a University of Miami Miller School of Medicine initiative that has brought more than 7,000 medical professionals to Haiti since its devastating 2010 earthquake.
Through the UM partnership, Lee initiated a laser therapy program to reduce the intraocular pressure in glaucoma patients, helping to save their vision. “Many glaucoma patients in Haiti have neither access nor economic resources to pay for glaucoma medications,” he said. To improve glaucoma care, Lee is also translating the findings from the Bascom Palmer glaucoma study of Haitian-Americans in Miami into outreach programs in Port-au-Prince.
In 2007, Bascom Palmer introduced an international elective rotation in which its residents spend two weeks providing eye care abroad. “We have generous donors who provide support for our residents’ international educational experience,” said Steven Gedde. “In many cases, they are supervised by Bascom Palmer alumni. When a resident has a terrific experience, he or she passes that enthusiasm along to our next class of residents.” For example, Michael Feilmeier, M.D., (resident 2009) now on the faculty at the University of Nebraska, traveled to Nepal for the Himalayan Cataract Project and later became involved in developing an ophthalmology program in Cap-Haitien, Haiti.
Just before the COVID pandemic, Johnson, an oculoplastic and reconstructive specialist, flew to Haiti in January 2020 to remove a large orbital tumor that was threatening the life of an 11-year-old girl. “I arrived in the morning, performed the surgery, and returned to Miami that evening with a biopsy of the tumor ready to be examined by our pathology laboratory,” Johnson said. “Fortunately, her tumor was not malignant and she has been getting follow-up therapy in both Haiti and the neighboring Dominican Republic. I hear from the family often and she’s now doing fine.”
In the remote Galapagos Islands, located 600 miles off the coast of Ecuador in the Pacific Ocean, a new Bascom Palmer humanitarian initiative is bringing badly needed vision screening and eye care services to more than 3,000 residents. With the help of the Ecuadorian Society of Ophthalmology and the non-governmental Ecuadorian organization Intercultural Outreach Initiative, a “generous donation of optical equipment has allowed residents of the island of Isabela to be screened for vision problems and referred to doctors on the Ecuadorian mainland for more advanced care,” said Lee.
Through the years, Bascom Palmer’s faculty have also traveled around the world in the ORBIS Flying Eye Hospital, a converted DC-10 aircraft equipped with operating,
recovery, and laser treatment rooms, and a 48-seat classroom where healthcare professionals gather for lectures, discussions, and live broadcasts of surgical procedures by visiting faculty members.
Operated by a global nonprofit organization dedicated to saving sight in underdeveloped countries, the ORBIS Flying Eye Hospital has invited Drs. Eduardo Alfonso, Carol Karp, Johnson, Lee, and other Bascom Palmer specialists to provide humanitarian vision care. “I try to take part in as many of their trips as I can,” said Johnson, whose more than 15 transcontinental itineraries have included Ethiopia, Ghana, Cameroon, China, Mongolia, Bangladesh, Armenia, Bulgaria, Nigeria, Kenya, Peru, Paraguay, and El Salvador.
Although the ORBIS aircraft was grounded during much of the COVID-19 pandemic, Johnson provided remote consultations through the organization’s online program CyberSight. “I was recently asked to advise on a complex patient in Africa with extensive skin cancer of the face and eyelid,” he said. “The local doctors had done a nice job of putting the eyelid together but were concerned about residual cancer. I suggested low-dose radiation to the eye, followed by close monitoring, and since then there has been no sign of recurrence.”
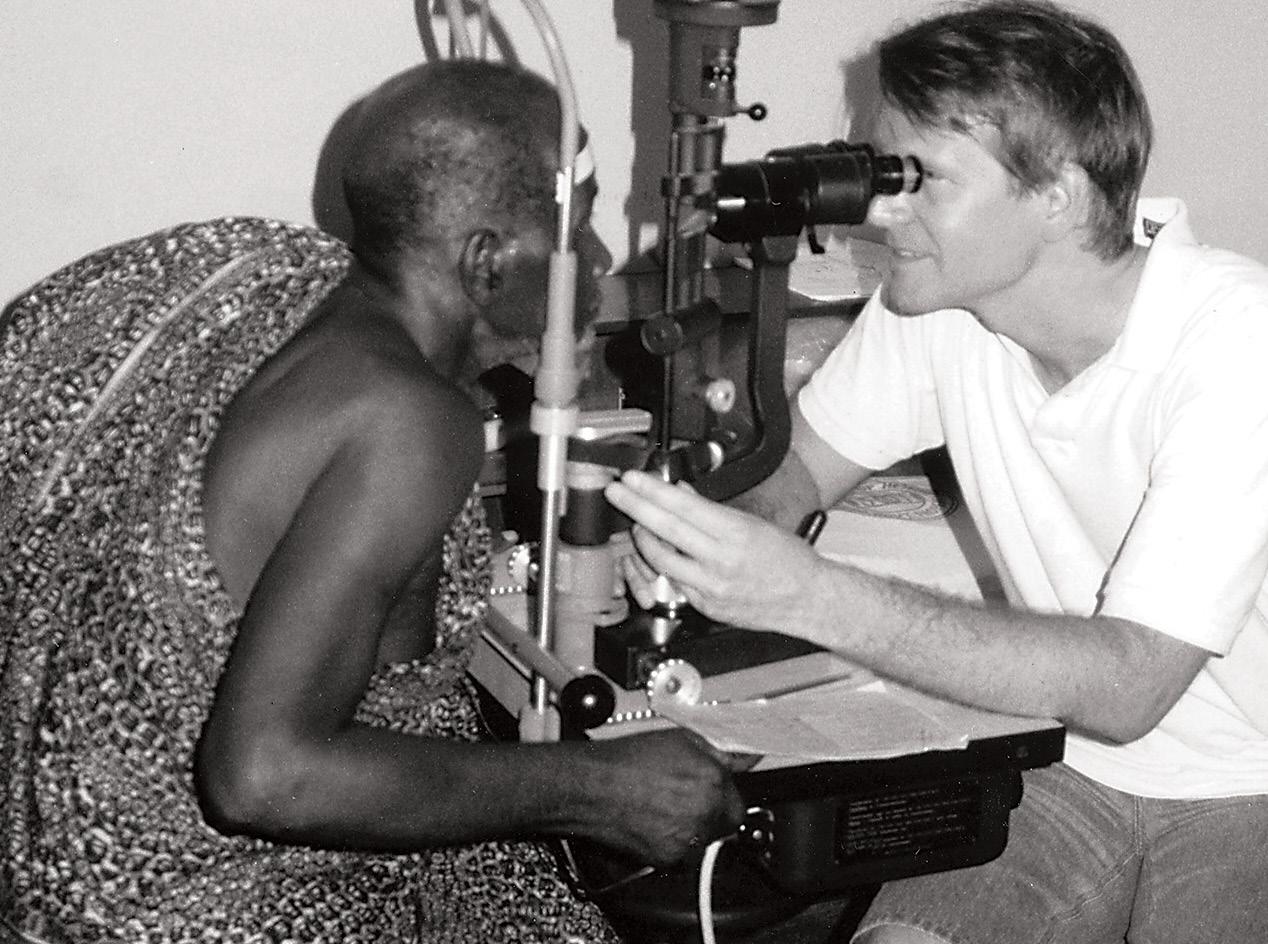
Similar to ORBIS but using trains as surgical operating rooms, Drs. Lee, Goldhardt, Carol Karp, Sandor Dubovy, and Bascom Palmer alumni including Michael Banitt (fellow 2009, former faculty) and Robert Chang (fellow 2009), volunteer with Lifeline Express, an organization that carries ophthalmologists through underserved regions of China and Mongolia to provide advanced training to rural ophthalmologists.
Reflecting on his experiences, Johnson said, “Bascom Palmer has always been supportive of my international travel since I began volunteering with ORBIS in the 1990s. There is no question that service will continue to remain at the heart of Bascom Palmer’s mission.”
“There is no question that service will continue to remain at the heart of Bascom Palmer’s mission.”
– Thomas Johnson, M.D.
Little did Dr. José A. Berrocal know when he became the first fellow to train under Dr. Edward Norton in 1964, that 28 and 37 years later, his two daughters, Maria (left), and Audina “Nina” (right), would also graduate from Bascom Palmer’s fellowship program. Bascom Palmer has had the wonderful privilege of training many members of the same family. Parents and children, spouses, and siblings make up this very special and distinct group.

Capó, remembers her early days at Bascom Palmer in the 1990s. “I was pregnant and a senior physician told me that raising a child would be the most important thing in my life,” she said. “It showed me that the people at the Institute were concerned about me as a person and a future mother – not just as a clinician.”
Today, one of Capó’s three children, Daniela Reyes-Capó, M.D., is following in her mother’s footsteps as a third-year resident at Bascom Palmer and will be moving on to a fellowship in corneal diseases at Baylor College of Medicine. “My daughter is very independent and has rotated with my colleagues here,” said Capó. “But this year she asked me to be her faculty discussant at Grand Rounds and presented a case of a woman with double vision. She called it ‘Double Trouble,’ referring to our mother-daughter bond, and to the double vision of her patient. I am very proud of her work.”
During her tenure, Capó has advised more than 100 residents. She said seeing Daniela go through the training program gave her a fresh perspective. “This is a great program, and our residents make it look easy,” she said.

“However, I could see firsthand how hard my daughter was working to build her clinical skills, and I can appreciate the preparation that goes into providing great patient care.”
For six decades, Bascom Palmer has been a welcoming home for generations of family members and alumni who share a commitment to clinical and research excellence. As Erin M. Shriver, M.D., who completed a fellowship in ophthalmic plastic and reconstructive surgery in 2008 and
now practices at the University of Iowa, said, “Whether you stay in the Miami area after your training or go elsewhere in the country, you will always be part of the Bascom Palmer family.”
Bascom Palmer’s dedication to providing compassionate holistic patient care has its roots in the Institute’s supportive culture for physicians, trainees, nurses, and other staff members. That includes valuable mentoring programs for residents and new faculty members beginning their professional careers.
“Bascom Palmer is about family,” said Eduardo Alfonso. “We value individuals from all backgrounds and foster an inclusive culture of belonging and opportunity for all. Our core values of diversity, integrity, responsibility, excellence, compassion, creativity, and teamwork provide the foundation for welcoming diverse voices, perspectives, and ideas.”
As president of the Bascom Palmer Alumni Association, Jerry Fisher helps the Institute’s national and international graduates stay connected with their peers. “Our Institute is known for the strong feeling of collegiality among our trainees and faculty,” he said. “Our alumni family continues to benefit from the diversity of people from different cultures and experiences who have trained at Bascom Palmer.”
That was certainly the case for S. William “Bill” Clark III, (resident 1983), now in a private comprehensive ophthalmology practice in Waycross, Georgia, and an associate professor at Emory University in Atlanta. “When I came here in 1980, the founding five faculty members were approaching the pinnacle of their careers, so I was surrounded by brilliant doctors and eager residents and fellows,” said Clark.
“Outside of the academics, Bascom Palmer had a family culture, and the annual softball game pitting faculty and fellows against residents was a high point,” Clark said. “I can tell you that the Chief and Don Gass could throw some mean pitches. John Flynn was an aggressive shortstop and Victor Curtin could hit the ball a mile. Back then, all the Residents Days skits were live productions with many voices showcasing rewritten songs and great wit shown in the nuances.”
In those earlier years, the Residents Days program directors were “volunteers” from the Institute’s alumni, including Fisher, Gordon Miller, Bill Wallace, Lee Duffner, M.D., (resident 1969), Jan W. Kronish, M.D., (resident, chief resident 1989), and Patrick E. Rubsamen, M.D., (resident, fellow, chief resident 1991,
former faculty). “The goals of the program, as defined by Drs. Norton and Curtin, were to give residents and fellows the opportunity to write and present scientific papers and defend those presentations,” said Fisher. “This was good practice for future academic presentations.”
In 1964, José Berrocal was the first fellow to train under Edward Norton. Following his fellowship, he chose to go into private practice in his native Puerto Rico, as the island’s first retina specialist.

A generation later, his daughters, Maria H. Berrocal, M.D., and Audina “Nina” Berrocal, M.D., completed fellowships at Bascom Palmer in 1992 and 2000 respectively. Maria entered practice with her father and became an assistant professor at the University of Puerto Rico. Nina joined the Bascom Palmer faculty in 2002 as a specialist in vitreoretinal diseases and pediatric clinical care, serving as medical director of the retinopathy of prematurity service. Many of her patients are premature babies, born as young as 23 weeks of gestation.

“My dad and Dr. Norton were very good friends,” said Nina. “The Norton family would come to Puerto Rico in the summer, and their kids would spend time with us. My sister and I got to know Victor Curtin and Donald Gass as well. We would visit the Nortons on our trips to Miami.”
Maria trained under Gass, learning the latest retinal surgery techniques from one of the field’s most highly regarded teachers. “Being able to consult with the best ophthalmologists on every aspect of a



patient’s eye was one of the best things about my education at Bascom Palmer,” she said. “It’s also very service oriented – the patient still comes first in everything.”
Nina agrees, calling Bascom Palmer a mecca for ophthalmology training. “It’s a pleasure to work with colleagues who are at the top of their fields,” she said. “At the same time, they are still humble about their work and love to teach students.”
Five years ago, Brian Tse, M.D., (fellow 2016), assistant professor of clinical ophthalmology, joined his father, David Tse, in Bascom Palmer’s ophthalmic plastic and reconstructive surgery service. “Growing up, Brian was able to understand the role of a physician and the value of research in advancing vision care,” said Tse. “After an initial interest in orthopedics, he decided to go into ophthalmology and specialize in ophthalmic plastic surgery. He is also working in the laboratory, studying the optic nerve to find new treatment options for patients with injuries or disabling diseases. It is very rewarding to work with him.”

Charles W.G. Eifrig, M.D., (resident, fellow, chief resident 2003), is also a member of a family of ophthalmologists. His father, David, was a retina specialist in North Carolina and his older brother, David Jr., became an ophthalmologist later in life. “Now, my oldest daughter, Gabriela, also wants to be an ophthalmologist,” he added.
Now in private practice in Laguna Hills, California, Efrig said, “My time at Bascom
Palmer was invaluable – it made my career. The collegial atmosphere, combined with intense teaching and the volume of patient challenges gave me exceptional clinical and surgical experience.”
Even though cockfighting has been illegal in Florida since 1986, as a resident, Eifrig recalls a memorable and unusual case wherein he treated a two-year-old girl whose family took her to a cockfight in Miami. “One of the roosters’ heel spurs ripped her eyeball
Thomas M. Aaberg Sr., M.D. Fellow 1969
Thomas M. Aaberg Jr., M.D. Resident, Fellow, Chief Resident 1995
Juan F. Batlle, M.D. Resident, Chief Resident 1985
Juan F. Batlle Logroño, M.D. Fellow 2015

Jose A. Berrocal, M.D. Fellow 1964
Maria H. Berrocal, M.D. Fellow 1992
Audina M. Berrocal, M.D. Fellow 2001, Faculty
Hilda Capó, M.D. Faculty
Daniela P. Reyes-Capó, M.D. Resident 2022
Stanley Chang, M.D. Fellow 1979
Jonathan S. Chang, M.D. Resident, Fellow, Chief Resident 2014
Stephen Fransen, M.D. Fellow 1990
Sara Fransen Grace, M.D. Resident, Fellow 2016
Wayne E. Fung, M.D. Fellow 1968
Anne E. Fung, M.D. Fellow 2005
Alexander Irvine, M.D. Fellow 1970

W. David Irvine, M.D. Resident, Chief Resident 1992
Scott Jaben, M.D. Chief Resident 1982
Korey Jaben, M.D. Resident 2015
James C. Major Sr., M.D. Resident, Chief Resident 1963
James C. Major Jr., M.D. Resident, Fellow, Chief Resident 2009
Mark S. Mandelcorn, M.D. Fellow 1974
Efrem D. Mandelcorn, M.D. Fellow 2010
Donald G. Puro, M.D., Ph.D. Resident 1980
Cynthia Puro Nix, M.D. Resident, Fellow 2010
Stephen R. Russell, M.D. Resident, 1986
Jonathan Russell, M.D., Ph.D. Resident, Fellow, Chief Resident 2021
Joel S. Sandberg, M.D. Resident 1974
Amy C. Schefler (Sandberg), M.D. Resident, Fellow, Chief Resident 2010, Former Faculty
Arthur L. Schwartz, M.D. Fellow 1973
Kenneth S. Schwartz, M.D. Fellow 2003
Richard Tenzel, M.D. Honorary Alumnus
Jack Tenzel, M.D. Resident 1987
David Tenzel, M.D. Fellow 1990
David T. Tse, M.D. Faculty
Brian C. Tse, M.D. Fellow 2016, Faculty
and ruptured the globe,” he said. “I did the emergency repair and later corrected a retinal detachment. I have kept in touch with the family and talked with her when she was 18. She wound up with 20/40 vision and was very appreciative of the care she got at Bascom Palmer.”
Through the years, many professional spouses have worked side by side at Bascom Palmer. “It is very easy to work together and we do not need to schedule meetings. We can easily catch up to discuss research projects, grant applications, and publications,” said Hong Jiang, M.D., Ph.D., (fellow 2011), associate professor of clinical ophthalmology and neurology, who is married to Jay Wang, M.D., Ph.D., scientific co-director of the Experimental Imaging Laboratory and expert in the development of advanced ophthalmic imaging and its applications in eye research.
“Dr. Alfonso once mentioned that we are a marvelous combination for clinical research as Jay is a basic scientist and I am a clinician,” said Jiang. “We usually relax at home, but oftentimes, we chat about research ideas while doing exercises or driving.”
Working together, the husband-and-wife team focuses on the microvasculature and microstructure of the eye as a window of the central nerve system. Their research, funded by grants from the National Institutes of Health, National Multiple Sclerosis Society, and Florida Department of Health, explores changes in the eye in age-related dementia.
Rong Wen, M.D., Ph.D., professor of ophthalmology, and Yiwen Li, M.D., research assistant professor of ophthalmology, were
Juan F. Batlle, M.D. Resident, Chief Resident 1985
Ivan R. Batlle, M.D. Resident 1989
Maria H. Berrocal, M.D. Fellow 1992
Audina M. Berrocal, M.D. Fellow 2001, Faculty
Christopher H. Blodi, M.D. Resident 1983, Former Faculty
Barbara A. Blodi, M.D. Resident, Fellow 1992
Jeffrey L. Goldberg, M.D., Ph.D. Research, Fellow 2010, Former Faculty
Roger A. Goldberg, M.D., M.B.A. Resident 2012
Brandon Lee, M.D. Fellow 2011
Bradford Lee, M.D. Resident 2013, Former Faculty
Pedro Schuchovski, Ph.D. Research Fellow 1989
Plinio Schuchovski, Ph.D. Research Fellow 1989
Jack R. Tenzel, M.D. Resident 1987
David B. Tenzel, M.D. Fellow 1990
classmates in medical school. “We worked as ophthalmologists in different hospitals and patient care was one of the issues we discussed over dinner tables,” said Wen.
“When we moved to the U.S., I started working in retinal research, while Yiwen brought her experience in neuroscience to retinal cell biology. It is wonderful to work together in the same field, and we share ideas, results, frustration, and failures both in the office and at home.”

The goal of Wen’s research is to understand the biology of the retina and photoreceptors, the physiopathology of retinal diseases, and to translate the bench research to patient care. Li’s research focuses on the neuroprotective treatment of retinal neurons using neuroprotective agents.
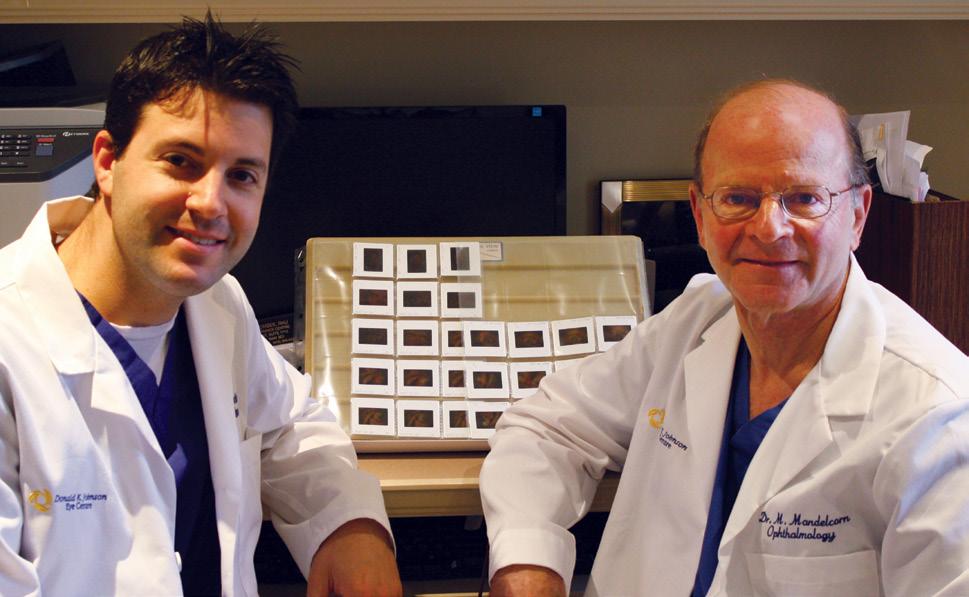
Vittorio Porciatti enjoyed working with his wife, Lori Ventura, M.D. (fellow 1986), who is retired from the faculty. “We met at the Association for Research in Vision and Ophthalmology conference in Fort Lauderdale in 1995, after being introduced by common Italian friends,” he said. “It was a wonderful experience and highly successful in terms of National Institutes of Health grants and publications. But we rarely discussed work issues at home.”

Yunhee Lee, M.D., former assistant professor of clinical ophthalmology, recalls meeting her husband, Steven Gedde, when she interviewed for a faculty position in 2001. “I was working at the New England Eye Center in Boston, and was asked to move to Miami to open a refractive surgery service in the new Palm Beach Gardens facility,” she said. “Steve was very kind and collegial, and before long we began dating and were married. We have different specialties, but
Melissa Meldrum-Aaberg, M.D. Resident, Fellow 1993
Thomas M. Aaberg Jr., M.D. Resident, Fellow, Chief Resident 1995
Nika Bagheri, M.D. Fellow 2018
Jayanth Sridhar, M.D. Resident 2014, Faculty
Barbara A. Blodi, M.D. Resident, Fellow 1992
Justin L. Gottlieb, M.D. Fellow 1995
Zelia M. Correa, M.D. Faculty
J. William Harbour, M.D. Fellow 1995, Former Faculty
Lena A. Dixit, M.D. Fellow 2016
Oliver G. Fischer, M.D., M.S. Fellow 2016
Fumino Ara Iwata, Ph.D. Research Fellow 1993 Takshi Iwata, Ph.D. Research Fellow 1991
Hong Jiang, M.D., Ph.D Fellow 2011, Faculty
Jianhua “Jay” Wang, M.D., Ph.D., M.S. Faculty
Anne L. Kunkler, M.D. Resident 2022
J. Daniel Diaz, M.D. Fellow 2022
Yunhee Lee, M.D. Faculty
Steven J. Gedde, M.D. Fellow 1986, Faculty
Yiwen Li, M.D. Faculty
Rong Wen, M.D., Ph.D Faculty
Arlanna N. Moshfeghi, M.D., M.P.H. Fellow 2006, Former Faculty
Andrew A. Moshfeghi, M.D., M.B.A. Fellow 2006, Former Faculty
Sarah P. Read, M.D. Resident, Fellow, Chief Resident 2018
Daniel S. Choi, M.D. Resident, Fellow 2018
Anita Shirodkar Shane, M.D. Resident, Fellow, Chief Resident 2012
Thomas S. Shane, M.D. Resident, Fellow, Chief Resident 2012
Rhea (McDonough) Siatkowski, M.D. Resident, Fellow 1999 R. Michael Siatkowski, M.D. Fellow 1993, Former Faculty



Kavitha R. Sivaraman, M.D. Fellow 2015
Fred B. Chu, M.D. Fellow 2015
Lori M. Ventura, M.D. Fellow 1986, Former Faculty Vittorio Porciatti, D.Sc. Faculty

Kimberly G. Yen, M.D. Resident 2000
Michael T. Yen, M.D. Resident 2000
we enjoy going to professional conferences together. Working in the same building makes it easy to bring up a cup of coffee or go out to lunch together. The days we can do that are always happy ones.” Lee continues to teach residents and fellows in the Bascom Palmer Emergency Department.
From “The Chief” to today Bascom Palmer’s tradition of kindness and care began in the 1960s with the inspirational leadership of Edward Norton, known to generations of trainees and faculty as “The Chief.” Norton’s daughter, Patricia “Patti” Norton, joined the Institute’s staff in 2016 and serves as manager of clinical business operations. “She has been part of the Bascom Palmer family since the day she was born,” said Alfonso.
Norton’s lasting influence extends well beyond his family members. Scott Jaben, M.D., (resident, fellow, chief resident 1982), recently retired from private practice in Charlotte, North Carolina, recalls working with Norton and the early faculty members.
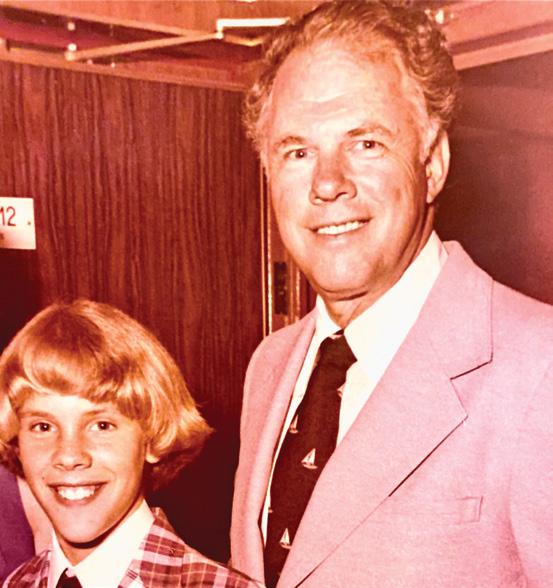
“As residents, we would commend Dr. Norton for what he created at Bascom Palmer,” Jaben said. “He instilled confidence in me, and my personal and professional growth during those years was tremendous.”
That tradition has continued under Alfonso, who was a first-year resident at the Institute when Jaben was chief resident. Fastforward to 2015, when Jaben’s daughter Korey also completed a residency at the Institute.

“She had a tremendous education and gained great experience at Bascom Palmer,” said Jaben, adding that Korey is now a glaucoma specialist at the Veterans’ Administration hospital in Charleston, South Carolina, providing virtual care to her patients.
“We have stayed in close touch with our Bascom Palmer extended family through the years,” added Jaben, whose family recently endowed Bascom Palmer’s Founders’ Lecture Series dedicated to his advisor, John Flynn, as well as Donald Gass and Lawton Smith. “I practiced ophthalmology for 40 years, and every day I was deeply appreciative of my experience at Bascom Palmer.”
Founding chair Edward Norton, his wife, Mary, and five children established a warm and welcoming professional culture that has been one of the distinguishing characteristics of Bascom Palmer through the decades. Here, daughter Patricia (“Patti”) Norton (center in brown dress) is surrounded by members of the Norton family during Bascom Palmer’s 50th anniversary celebration.



David Tse has a bold vision for the future. After decades of treating patients who have lost their eyes to injury or disease, Tse is studying how to tackle the impossible: performing a whole eye transplant. “I want Bascom Palmer to be the first eye center in the world to achieve this ‘moon shot’ goal,” he said. “All of Bascom Palmer has focused on this challenge.”
Currently, Tse is working with colleagues like Sanjoy Bhattacharya and Daniel Pelaez and many others to address the incredibly difficult challenge of joining one optic nerve to another so the visual signals from a transplanted eye can flow smoothly into the patient’s brain. “We are looking at molecular and biological approaches to overcoming the scar tissue that forms a barrier at the end of the nerve,” he said. “This is one
example of how our clinicians and researchers work together on big, bold ideas that could transform ophthalmology in the future.”
Today, Bascom Palmer’s professionals focus on finding new ways to diagnose, treat, and prevent vision diseases and disorders. “Our physicians and scientists are using largescale clinical databases, artificial intelligence, advanced imaging technologies, and therapies to benefit our patients,” said Eduardo Alfonso.
“Every day, our researchers collaborate with colleagues at the Miller School of Medicine, sharing ideas and insights, and launching new laboratory and clinical research initiatives that have led to advancing personalized health care, and studying the patients from their genetic makeup to the environmental diseases that affect health and disease.”
Jorge Fortun, M.D., uses new 3-D technology that enhances and magnifies the stereoscopic image and allows surgeons to clearly visualize all aspects of surgery.
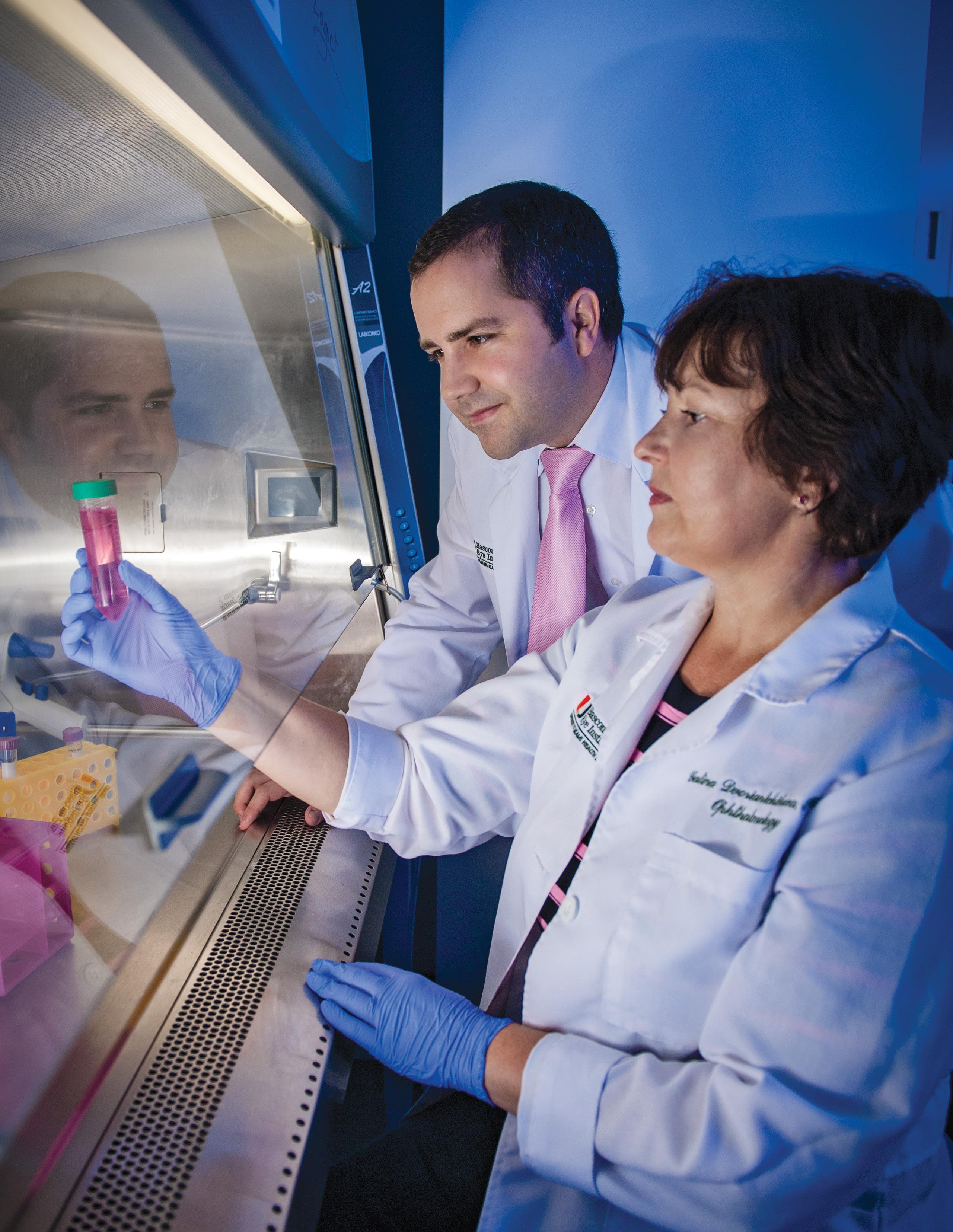
Natali Townsend, O.D., (left), leads Bascom Palmer’s rapid virtual eye care team as they provide quick eye care to patients for common eye conditions.
several years and has been markedly sped due to the pandemic. Vision and eye care lends itself to telehealth or virtual care because digital functional testing of vision and images of the eye can be transmitted to specialists from anywhere.
In addition, Bascom Palmer Eye Institute is validating new paradigms of clinical care by integrating virtual care into in-person testing. The Institute has developed bold new programs such as Bascom Palmer Optical Express, rapid virtual eye care, as well as opening eye and vision testing centers throughout South Florida and beyond. These new models of clinical care have increased access, reduced costs, and improved patient satisfaction.
“With these new facilities and virtual eye care, we are committed to making personalized vision care as accessible as possible for the South Florida community.”
– Eduardo Alfonso, M.D.
Within the next few years, the Institute will be expanding its South Florida footprint with new locations in UHealth’s medical centers at SoLé Mia in North Miami and Downtown Doral. “These state-of-the-art facilities will bring our services closer to residents of Aventura, Miami Gardens, Doral, Miami Springs, and other northern and western Miami-Dade communities,” said Alfonso. “With these new facilities and virtual eye care, we are committed to making personalized vision care as accessible as possible for the South Florida community.”
Increasing access to care and evolving the paradigms of clinical care drive Bascom Palmer to embrace technological advances so that one day, maintenance of vision health will be available to the patient in personalized devices like smartphones or even implantable aids.
Internationally, Bascom Palmer is also expanding its clinical facilities, including a 70,000-square-foot multidisciplinary eye center scheduled to open in 2023 in Abu Dhabi, the capital of the United Arab Emirates.
Recognizing the growing importance of telemedicine and virtual healthcare, a project to make Bascom Palmer’s specialty vision care available locally, nationally, and around the world has been in effect for


Bascom Palmer is investing significantly in scientific and clinical research with three primary areas of focus:
• Preventative therapies, such as identifying cellular and genetic biomarkers of disease, developing gene therapy, cellular therapy, and advanced surgical procedures.
• Regenerative treatments, such as stem cells transplants, tissue transplants, and retinal implants.
• Biotechnology, bringing together multiple disciplines in medicine, engineering, artificial intelligence, big data, and new biomaterials.
“These exciting programs will spur innovation and discovery, support interdisciplinary collaborations with other Institutes, and create further opportunities for philanthropy,” said Alfonso. “They will also attract graduate students and talented investigators to Bascom Palmer, as we recruit new doctors and scientists in keeping with the growth of our research, clinical and educational programs.”
Alfonso said the Institute plans to remain on the leading edge of tapping the data in electronic health records (EHR) for research as well as clinical care. “We will be able to look more closely at patient populations to address issues related to epidemiology and public health,” he said. “Drilling into the EHR data will also allow us to deliver more personalized care, leading to better outcomes for patients.”
Attracting young researchers
Vittorio Porciatti also expects significant progress in the next five years. “We have a very diverse research portfolio that combines our strengths in scientific discovery and clinical care,” he said. “Our professionals are experts in many disciplines and they eagerly share ideas while collaborating on new strategies and tactics to improve patient care.”
“Bascom Palmer’s research priorities are promoting high-impact research (gene therapy, stem cell therapy, and gene editing therapy), developing new technology (including biomaterials, drug delivery, instruments for imaging, electrophysiology, surgery, and artificial vision), generating interdisciplinary collaborations, and using artificial intelligence to take advantage of large data sets.
Porciatti is also proud of Bascom Palmer’s record in recruiting talented young researchers in all areas of vision care. For instance, Stefan Kurtenbach, Ph.D., (research fellow 2017), a research assistant professor, is studying how genomic aberrations and epigenetic changes foster tumor development, Molecular biology of eye diseases and regenerative ophthalmology are the drivers for Daniel Pelaez, a research associate professor. “We harness the power of stem cells, advanced biomaterials, tissue engineering, and molecular genetics to replace cells and tissues and restore the functions that are lost to disease or trauma,” he said. The two main areas of research in
the Pelaez laboratory are molecular biology of eye diseases and regenerative ophthalmology with ongoing projects focused on the optic nerve, retinal neurons, and lacrimal gland regeneration.
Cornea and external disease specialist, Alfonso L. Sabater, M.D., Ph.D., (research fellow, fellow 2017), assistant professor of ophthalmology, is looking for new strategies to protect and regenerate the cornea.
“Corneal damage due to multiple causes can be slowed and even reversed by a variety of approaches,” he said. “These include activating cell survival and proliferation signaling, blocking strategic cell death.”
Giovanni Gregori, Ph.D., a research associate professor of ophthalmology, is focused on the clinical applications of medical image processing. His research
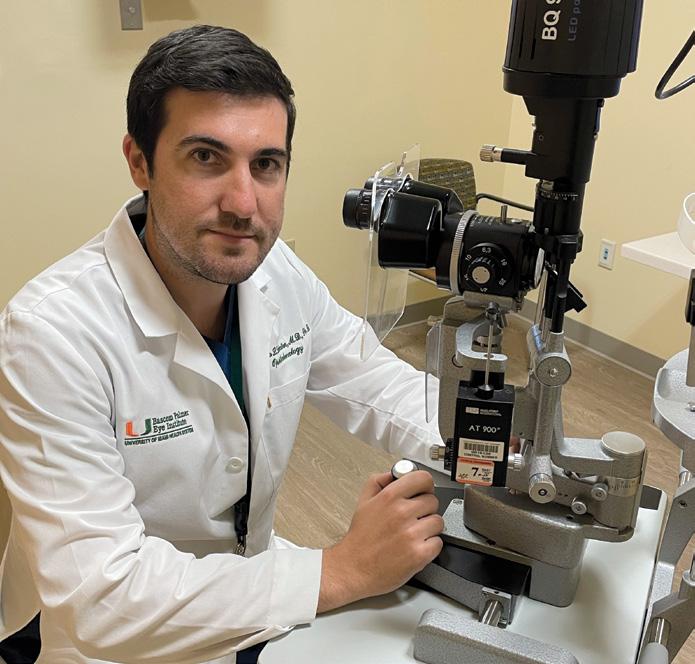
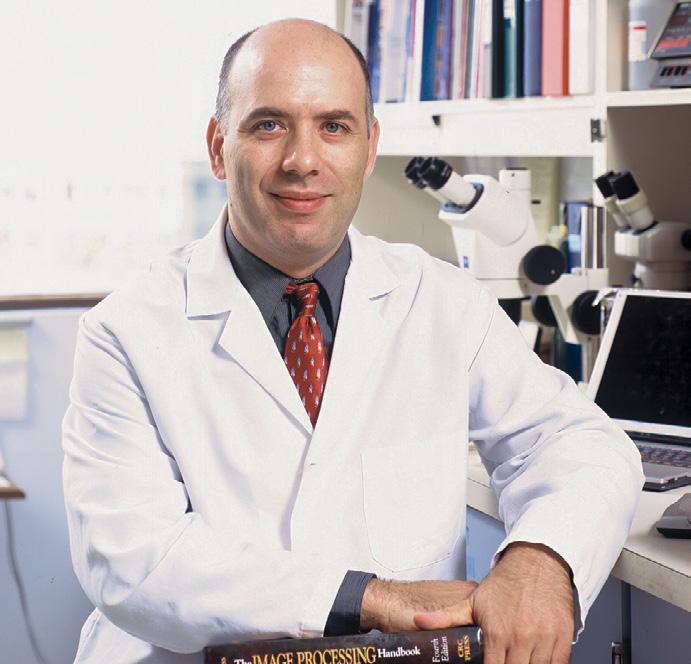

group has been a leader in the development of quantitative tools for the analysis of retinal images in particular those acquired using optical coherence tomography. And, the ongoing studies in the laboratory of Dmitry Ivanov, Ph.D., explore the signaling cascades and the epigenetic mechanisms involved in ocular development and neuronal regeneration in the adult retina. Since 2015, the National Alliance for Eye and Vision Research has recognized and hosted early-stage investigators from around the United States to exhibit the results of their cutting-edge vision research. Included among the impressive NAEVR emerging vision scientists are Pelaez, Sabater, Kurtenbach, Mohamed Abou Shousha, Swarup Swaminathan, Luis Vazquez, M.D., Ph.D., (fellow 2014), and Florence Cabot, M.D., (fellow, research fellow 2019). Emerging scientists also visit members of Congress to thank them for their essential support of the National Institutes of Health and National Eye Institute.
Multidisciplinary collaborations To provide leading-edge care to patients
with ocular surface tumors, Carol Karp collaborates closely with researchers and clinicians at Sylvester Comprehensive Cancer Center of the University of Miami Miller School of Medicine. “We have an active partnership that includes monthly research meetings for eye cancer,” she said. “We share ideas as well as the latest research findings. This seamless connection benefits our patients. For instance, we have new treatments for ocular melanomas, including checkpoint inhibitors. As a result, we can treat patients more aggressively, saving many lives.”
Glaucoma specialist Swarup S. Swaminathan, M.D., (resident 2018), assistant professor of clinical ophthalmology and the Mary Lee and Richard E. Bastin Chair in Ophthalmology, has developed novel statistical models for disease progression using the resources of the UM Institute for Data Science and Computing. “While most patients with glaucoma progress at a slow rate, a small percentage of patients progress at a fast rate and can rapidly develop a visual disability,” he said. “It is vital to understand a patient’s rate of progression, so treatment can be appropriately initiated or augmented.”
Swaminathan received a Mentoring for the Advancement of Physician Scientists
grant from the American Glaucoma Society for this study, which was also supported by grants from the National Eye Institute and the National Institutes of Health.


In the cornea field, William Culbertson has another vision-saving project in the works in collaboration with Guillermo Amescua and Ellen Koo, M.D., both cornea and cataract specialists. Koo is committed to improving the field of corneal transplantation and eye banking. She has also pioneered innovations in the surgical techniques of Descemet Membrane Endothelial Keratoplasty and Descemet’s Stripping Endothelial Keratoplasty.
“Rather than perform a corneal transplant, we are taking a cellular biology approach to restoring vision,” said Culbertson. “We grow replacements for the defective cells, put magnetized nanoparticles in the new cells, and use magnets to pull them to the back of the cornea.”

In glaucoma as well as retinal, corneal, and neuro-ophthalmic care, the Institute’s researchers are using powerful 21st-century technologies to advance the frontiers of vision care. “To understand the drivers of glaucoma, we are analyzing large-scale clinical databases, developing artificial intelligence algorithms, deploying advanced imaging technologies, and studying family genetics,” said Richard Parrish.
One of the most exciting advances in glaucoma research is just getting underway, and once again, Bascom Palmer is at the forefront. In 2018, the American Academy of Ophthalmology launched the nation’s first comprehensive eye disease clinical registry with Bascom Palmer as one of four U.S. institutions to be selected for the IRIS Registry Analytic Center Consortium, which is taking the lead in applying the patient data to current vision problems.
“Statistical analysis of the best treatments for glaucoma is essential because there is a wide variation in the severity of the disease and physicians use different therapies,” said Elizabeth A. Vanner, Ph.D., the Institute’s
director of biostatistics. “Bascom Palmer is fortunate to have a strong biostatistics program that receives grant support from our donors.”
Vanner said it takes extensive work to translate the administrative data uploaded from providers into clinical data for research purposes. For instance, an electronic health record may indicate a visual field assessment was performed on a patient with glaucoma, but not give the results. Alternatively, the records might not indicate whether a certain medication was given to the right or left eye – a challenge for research since glaucoma may advance faster in one eye than the other. “While there are shortcomings, the Intelligent Research in Sight (IRIS) Clinical Registry opens the door to new types of research studies, including large-scale studies that require extensive computing power,” Vanner said.

For example, Peter Chang, M.D, (fellow 2010), professor of clinical ophthalmology, has launched several glaucoma studies using the IRIS Registry data, including a comparative analysis of laser trabeculoplasty and surgical procedures to open a fluid drainage passage based on 79,332 patients/ eyes with primary open-angle glaucoma.
“We know that lasers can have a positive impact, but without access to the registry, it was difficult to determine the real-world impact,” said Chang, whose two papers from the study covered patient responsiveness to laser treatments and the duration of that response. “That indicates laser therapy is
Mohamed F. AbouShousha, M.D., Ph.D.
a very viable alternative, particularly for patients who may find it difficult to adhere to a medication regimen.”
revolutionary technology brings together lightweight 3-D headsets with artificial intelligence algorithms in a cloud-based platform that provides real-time information about the immediate surroundings. While in development, more than 100 patients had tested the prototype digital glasses on a visual “obstacle course” in the laboratory with excellent results.
“Artificial intelligence is creating a revolution in ophthalmology, and Bascom Palmer is at the forefront,” said Abou Shousha, associate professor of clinical ophthalmology and director of the Artificial Intelligence and Computer Augmented Vision Laboratory in the Institute’s William L. and Evelyn F. McKnight Vision Research Center.

Bascom Palmer also has an extensive gene therapy program with ophthalmologists, surgeons, genetic counselors, and research scientists studying various forms of inherited eye diseases. For instance, Byron Lam, the Institute’s medical director of clinical research, is the principal investigator of a clinical trial for X-linked retinitis pigmentosa (XLRP), which causes blindness in about one in 15,000 men.
– Mohamed F. AbouShousha, M.D., Ph.D.
Another important finding was that laser trabeculoplasty reduced the need for medications in patients with relatively normal eye pressure, Chang said. Because clinical trials typically enroll patients with high intraocular pressure, clinicians would not have known the potential benefits of laser treatments in this second group of patients without the IRIS Registry data. “Since it takes six to eight weeks for a laser treatment to be apparent, it is difficult for practitioners to make comparative assessments,” he added. “Having access to this nationwide database gives us better information to guide our clinical decisions.”
Another IRIS Registry study is being led by Adam L. Rothman, M.D., (fellow 2020), an assistant professor of clinical ophthalmology who was awarded a 2020 Research to Prevent Blindness and AAO grant. His current project involves investigating the change in eye pressure following cataract surgery.

A team of Bascom Palmer clinicians and scientists led by Mohamed Abou Shousha, M.D., Ph.D., (fellow 2011), has developed digital smart glasses that can dramatically expand an individual’s field of vision. This
To advance this technology for screening, diagnosing, and treating visual field disorders, the Institute spun off Heru, a medical technology company. Heru’s first diagnostic application for visual field exams was listed with the U.S. Food and Drug Administration in 2020 and is now being used by vision specialists throughout the U.S.
“Heru’s technology was developed through decades of research, innovation, and clinical validation within the accelerator program at Bascom Palmer,” said Alfonso. “Its full technology suite is focused on improving the quality of life for people with visual defects.”
“Introducing a functional copy of the affected gene using an engineered viral vector can correct the underlying cause and induce a longlasting therapeutic effect,” said Lam, whose work is supported by Hope for Vision, a nonprofit organization dedicated to promoting retinal research. “I have tremendous hope in the doctors and scientists doing this life-changing work and am confident that RP is one step closer to being treated,” said founder Betti Lidsky.
Lam and Rong Wen now serve as directors of the Adrienne Arsht Hope for Vision Center of Retinal Degeneration Research at Bascom Palmer. Their work is supported by Adrienne Arsht Hope for Vision funds and by the National Eye Institute/ National Institutes of Health.

“Working collaboratively with our colleagues at the University of Miami, Bascom Palmer now has the most robust genetics research program in the nation,” added Alfonso. “That talent has already enabled us to identify specific genes involved in glaucoma and retinal degenerative diseases.”
Reflecting on 60 years of visionary leadership, Alfonso said Bascom Palmer is committed to pursuing bold ideas in research, delivering excellent clinical care, and educating future generations of vision professionals. “Our
professional team – as well as our alumni around the world – are proud to continue Dr. Norton’s legacy of providing compassionate patient care and investing in world-class scientific discovery and clinical innovation,” he said. “Our vision is to transform global ophthalmology and change lives – one patient at a time.”
Wen, M.D., Ph.D.
Audina Berrocal, M.D.Byron Lam, M.D.
“Our vision is to transform global ophthalmology and change lives –one patient at a time.”
– Eduardo Alfonso, M.D.
“Artificial intelligence is creating a revolution in ophthalmology, and Bascom Palmer is at the forefront.”
Since the founding of the Institute, people have always been our strength. Meet the Bascom Palmer faculty members as of June 1, 2022.









































Arindel S. Maharaj, M.D., Ph.D.
Associate Professor of Clinical Ophthalmology










Jaime D. MartinezMartinez, M.D. Assistant
























Richard M. Awdeh, M.D.
James Banta, M.D.

Juan Batlle, M.D.
Stanley Braverman, M.D.
Jerome Fisher, M.D.
Gilbert Grand, M.D.
Daniel Hutter, M.D.
J. William Harbour, M.D.
Maja Kostic, M.D., Ph.D.
Aarup A. Kubal, M.D.
Anup A. Kubal, M.D.
Ajay E. Kuriyan, M.D., M.S.
Van Lansingh, M.D., Ph.D.
John J. Martin, M.D.
Sotiria Palioura, M.D.
Nimesh Patel, M.D.
Anna V. Quan, M.D.
Jonathan F. Russell, M.D.
Felix Sabates, M.D.
Juliana Sallum, M.D.


Joseph A. Singer, M.D.
Huda Sheheitli, M.D.




Myron Tanenbaum, M.D.
Nancy Thomas, M.D.


Joseph Trentacoste, M.D.
Anil Vedula, M.D.
Daniel Vu, M.D.
Roberto Warman, M.D.
Mark A. Werner, M.D.



Victor M. Villegas, M.D.
William Zambrano, M.D.
Isidoro Zarco, M.D.
Midhat Abdulreda, Ph.D.
Steven Gayer, M.D.
David Lee, M.D.
Arnold M. Markoe, M.D.
Fabrice Manns, Ph.D.
Keyvan Nouri, M.D.
Judith D. Post, M.D.
Robert Quencer, M.D.
Konstantinos Sarantopoulos, M.D.
Mustafa Tekin, M.D.
Gaofeng Wang, Ph.D.
Ramzi Younis, M.D.























































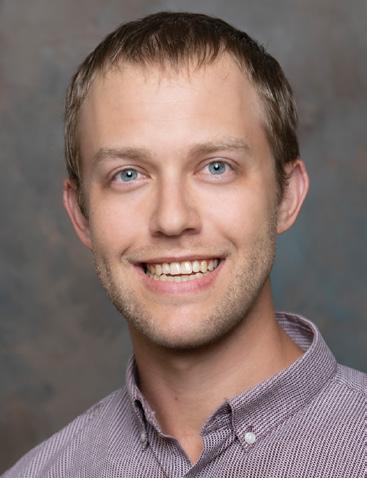



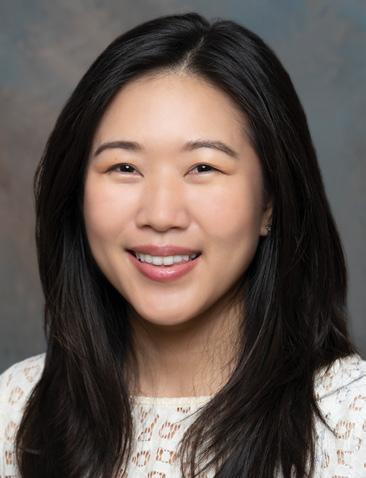







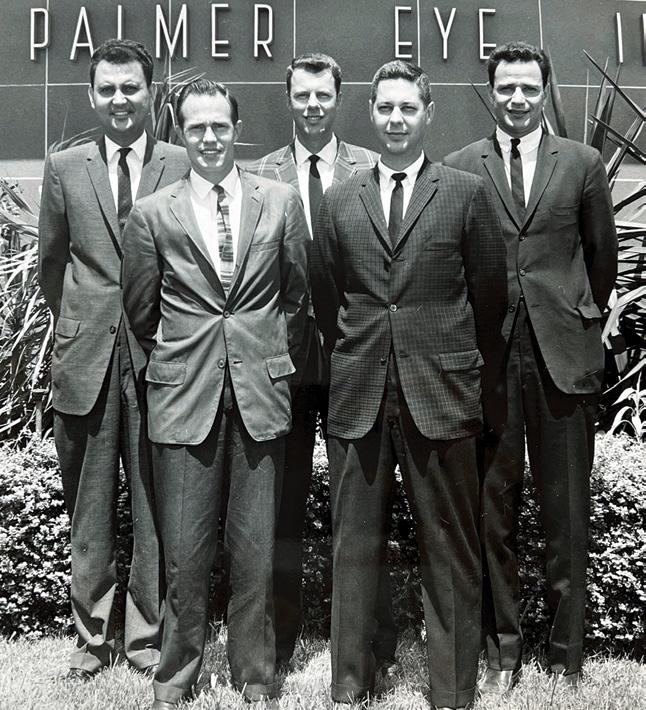
These photographs of residents and fellows may not represent the year of graduation.
1969 1963 1960 1970
Thomas M. Aaberg Sr. Fellow 1969

Thomas M. Aaberg Jr. Resident, Fellow, Chief Resident 1995
Ashkan M. Abbey Resident 2013
Richard L. Abbott Fellow 1978
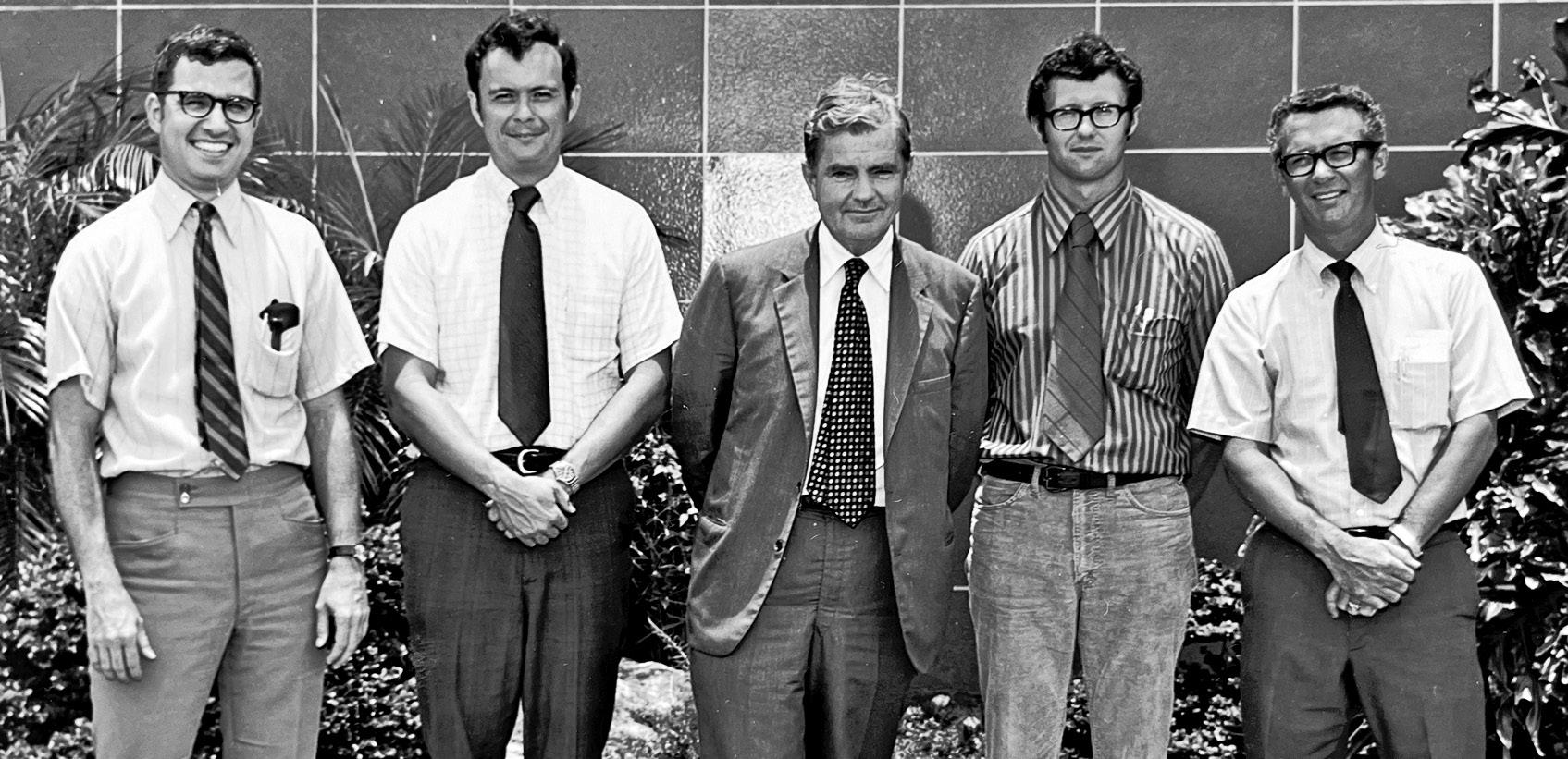
Amany Abdelaziz Research Fellow 2011
Mohamed F. Abou Shousha Fellow 2011, Faculty
Gary W. Abrams Fellow 1978
Adele Abri Research Fellow 2004
Ali Abri Research Fellow 2004
Fawzi D. Abukhalil Fellow 2020
Ana Carolina Acosta Research Fellow 2005
Eldad Adler Fellow 2014
John C. Affeldt Fellow 1983
Shruti Aggarwal Fellow 2019
Dan Agness Fellow 1979
Sumayya Ahmad Fellow 2016
Byung-Joon Ahn Fellow 2008
Chris R. Alabiad Resident, Fellow 2010, Faculty
Luma Al-Attar Resident, Fellow, Chief Resident 2005, Former Faculty
Thomas A. Albini Faculty
Vicente Alcaraz Fellow 1981
Brian D. Alder Fellow 2014
William V. Aldred Resident 1981
Paul Alecce Resident 1959
George Alexandrakis Resident 2000
Eduardo C. Alfonso Resident 1984, Faculty, Chair
Sulaiman Alhumaid Fellow 2020
Tayyeba K. Ali Fellow 2015
Elias Aliprandis Fellow 2005
Arthur W. Allen Fellow 1975
Kyle J. Alliman Resident, Fellow 2010
Zaina N. Al-Mohtaseb Fellow 2014
Zakeya M. Al-Sadah Fellow 2018
Nabih Al-Sheikh Fellow 2002
Nayef K. Alshammari MVSIO 2021
Diego S. Altamirano Research Fellow, Fellow 2021
Rene Altamirano Resident 1958
Gustavo M. Alvira Fellow 1986
Wallace L.M. Alward Fellow 1987
Mohamed Aly Research Fellow 2006
Rosario Amato Research Fellow 2019
Guillermo Amescua Fellow 2012, Faculty
Arezo Amirikia Fellow 1999
Scott R. Anagnoste Fellow, Chief Resident 2000
Apostolos G. Anagnostopoulos Research Fellow, Fellow 2021
Jean-Louis Anctil Fellow 1981
Douglas R. Anderson Honorary Alumnus, Faculty Emeritus
Roger A. Anderson Fellow 2008 Warren Anderson Fellow 2007
Lee S. Anderson Fellow 1982
Roberto Andreu Resident 1986
Husam Ansari Fellow 2007
Zubair A. Ansari Resident 2018, Faculty
Bertrand M. Anz Resident 1979
Rachid Aouchiche Fellow 1976
Antonio V. Aragon Fellow, Chief Resident 2001
Jaime Arango Resident 1961
Martha L. Araujo Cali Fellow 1989
Ahmad A. Aref Fellow 2011
Roberto Arguello Resident, Fellow 1983
Donald Arkfeld Fellow 1979
Jodie A. Armstrong Former Faculty
Claudia Arroyave O’Brien Fellow 2001
Luiz G. Assis Research Fellow 1986
Geetha K. Athappilly Fellow 2010
Richard M. Awdeh Fellow 2009, Faculty
Juan A. Ayala Haedo Fellow 2016
G. William Aylward Fellow 1994
Susan E. Azar Fellow 2011
Hassan A. Aziz Resident, Fellow 2015
Amy Babiuch Fellow 2010
Austin Bach Fellow 2018
Brian Bachynski Fellow 1985
Paul D. Baciu Fellow 2017
Nika Bagheri Fellow 2018
Frank Bajandas Fellow 1975
M. Livia Bajenaru Former Faculty
Evelyn L. Baker Resident 2003
Norman Ballin Resident 1964
Michael R. Banitt Fellow 2009, Former Faculty
Tanuj P. Banker Fellow 2017
James T. Banta Resident 2003, Former Faculty
Anita Barikian Fellow 2020 Derek L. Barker Fellow 2004
Charles C. Barr
Resident, Chief Resident 1979
Elena Barraquer Research Fellow 1989
Debra A. Barrett Resident 1991
Michael Barricks Resident, Fellow 1976
Keith Barton Fellow 1996
Norma B. Barton Fellow 1980
James V. Bastek Fellow 1983
Edgar Batista Resident 2004 Kenneth Batko Fellow 1980
Ivan R. Batlle Resident 1989
Juan F. Batlle
Resident, Fellow, Chief Resident 1984
Lisa Battat Fellow 1999
Joseph O. Beauchamp Resident 1968 Bruce H. Becker Fellow 1977
Carmine Bedotto Resident, Chief Resident 1970
1977
William E. Benson
Fellow 1975 Matthew S. Benz Resident, Fellow, Chief Resident 2003
Leonard Berg Fellow 1964
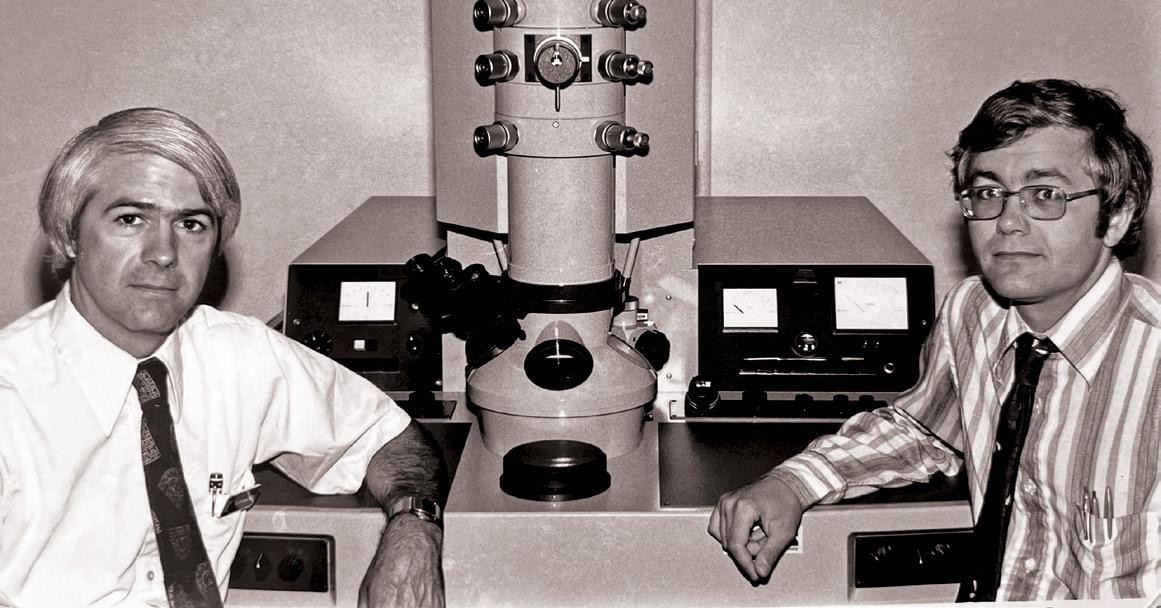
Jose A. Bermudez Magner Fellow 2015
Audina Berrocal Fellow 2001, Faculty
Jose A. Berrocal Fellow 1964
Maria H. Berrocal Fellow 1992
Dana Beyer Resident 1982
Swetangi D. Bhaleeya Fellow 2012
Sanjoy Bhattacharya Faculty Namita Bhardwaj Fellow 2016
Anjali M. Bhorade Fellow 2004
Christian DJ Billotte Research Fellow 2002
Elena Bitrian Faculty
Alan Bird Fellow 1969
Charles J. Blair Fellow 1969
George W. Blankenship Jr. Former Faculty 1989
Nathan W. Blessing Resident, Fellow 2018, Faculty
Lauren S. Blieden Fellow 2012
Barbara A. Blodi Resident, Fellow 1992
Christopher F. Blodi Resident, Former Faculty 1983
Louis Blumenfeld Fellow 1996
Mark S. Blumenkranz Fellow 1980
Donald D. Bode Fellow 1982
Dan Boghen Fellow 1972
George T. Boozalis Fellow 1992
Francois Borruat Fellow 1993
Mark D. Borup Resident 1992
Remi Bougaran Research Fellow 1998
Eileen Bowden Fellow 2020
Charles (Brad) Bowman Resident 1993
James Boynton Fellow 1976
Reagan Bradford Fellow 1985
Puneet S. Braich Fellow 2017
Peter J. Branden Fellow 1991
Robert A. Braunstein Fellow 1979
Bruce Brauston Resident 1962
R. Larry Brenner Resident 1969
Roy Bresky Resident 1970
Dean C. Brick Fellow 1980
Jonathan W. Briggs Fellow 2002
Gregory S. Brinton Resident 1980
Roy D. Brod Fellow 1988
James Brown Fellow 1975
Reay H. Brown Fellow 1983
David J. Browning Fellow 1986
Nancy M. Buchser Fellow 2009
Edward G. Buckley Fellow 1983
Donald L. Budenz Fellow 1992, Former Faculty
Michael J. Bueche Fellow 1993
1980 1978
1978
Helmut Buettner
Resident 1975
Frank Buffam Fellow 1976
George Bullwinkel Resident 1967
Walter E. Bundy Resident 1977
Michelle R. Butler Fellow 2013
Carlos Buznego Resident 1991
Florence A. Cabot
Fellow, Research Fellow 2019, Faculty
Christine E. Callahan Fellow 2004
David G. Callanan Fellow 1992
Natalia F. Callaway Resident 2018
Andrew S. Camp Resident 2016
Randy V. Campo Resident 1981
Ana P. Canto Fellow 2013
Salvatore Cantolino Fellow 1970
Hilda Capó Faculty
Andrew R. Carey Research Fellow 2015
Thomas J. Carlow Fellow 1972
Mont J. Cartwright Fellow 1987
Anthony Castelbuono Fellow 2001
Lourdes A. Casuso Resident, Fellow 2002
Brian Cavallaro Fellow 1999
John Cavender Fellow 1972
Kara M. Cavuoto Resident, Fellow 2012, Faculty
Elizenda Ceballos Fellow 2001
Colleen M. Cebulla Resident, Fellow 2009
Haci Celik Fellow 2019
James Cerasoli Resident 1969
Joseph G. Chacko Fellow 2005
You-Ching Chan Research Fellow 1990
Jonathan S. Chang
Resident, Chief Resident, Fellow 2014
Robert T. Chang Fellow 2009 Stanley Chang Fellow 1979
Ta Chen Peter Chang Fellow 2010, Faculty
Tom S. Chang Fellow 1994
Victoria S. Chang Fellow 2016, Faculty
Warren Chang Fellow 1998
Rolando A. Chanis Fellow 1974
Daniel L. Chao Resident 2014
Pascal Chapon Research Fellow 2000 Steve Charles Resident 1973
Amina Chaudhry Fellow 2020
Nauman Chaudhry Fellow, Chief Resident 1999
Muhammad Z. Chauhan MVSIO 2019
Anuj Chawla Fellow 2015
Percival Chee Resident 1968
Gene W. Chen Fellow 2012 Jei-Yuan Chen Research Fellow 1990 Jenny Chen Fellow 2018
1979 1981
1981 1981
Jessica L. Chen
Fellow 2012
Masako Chen Fellow 2021
Philip P. Chen Fellow 1996
Royce W. Chen Fellow 2014
Sachin (Shawn) Chhabra Fellow 2008
Fred Y. Chien Fellow 2008
Iain Chisholm Fellow 1976 Mark Chiu Resident 1986
James Chodosh Fellow 1993
Catherine J. Choi Fellow 2018
Daniel S. Choi Resident, Fellow 2018
Gabriel T. Chong Fellow 2011
Christopher Chow Fellow 1996
Jessica H. Chow Fellow 2012
Stephen P. Christiansen Fellow 1991
Murray D. Christianson Fellow 1980
Nancy Christmas Resident 1999
David H. Chu Fellow 2010
Fred B. Chu Fellow 2015
Elaine L. Chuang Fellow 1985, Former Faculty
Yunsuk Chung Research Fellow 2011
Daniel S. Churgin Resident 2016
Gerhard W. Cibis Fellow 1977
Joseph M. Civantos Resident 1993
Steven Civiletto Resident, Chief Resident 1979
Bill Clark Resident 1983
Hollis W. Clark Fellow 1986
Robert Clark Fellow 1971 W. Lloyd Clark Resident 1999
John G. Clarkson Resident, Chief Resident 1975, Chair, Faculty Emeritus, Dean Emeritus
Henry M. Clayman Resident 1972, Former Faculty
Charles E. Clevenger Resident, Chief Resident 1964
Michael Cobo Resident, Chief Resident 1980
Steven M. Cohen Fellow 1994
Vanessa Collao MVSIO 2022
Claudia Colomine Fellow 2003
Howard Conn Fellow 1982
Brian P. Conway Fellow 1976
Jane C. Cook Fellow 2019
Ghassan Cordahi Fellow 1999
Richard Corey Resident 2001
George F. Corrent Fellow 1988, Former Faculty
Kathy Corser Honorary Alumna
Rafael T. Cortez Fellow 1978
John A. Costin Fellow 1979
Andrew J. Cottingham Fellow 1975
Thomas Coulter Resident 1971
1982 1983
Scott W. Cousins Fellow 1987, Former Faculty
Stephen S. Couvillion Resident, Fellow, Chief Resident 2007
Ashley M. Crane Resident, Fellow, Chief Resident 2019
Shelley A. Cross Fellow 1982
Benjamin M. Crowder Resident 1970
John I. Crowder
Resident, Fellow 1963
Oscar A. Cruz Fellow 1992
Vanessa Cruz-Villegas Fellow 2003
William W. Culbertson Fellow 1979, Faculty

Jay J. Culotta Fellow 1984
Victor T. Curtin Honorary Alumnus, Faculty Emeritus
Philip L. Custer Fellow 1984
David L. Cute Fellow 2008
Oscar Cuzzani Fellow 1980
Charles K. Dabbs Resident 1988
Mark Daily Resident 1977
Elizabeth A. Dale Fellow 2015
Melvyn Damast Fellow 1972
Donald J. D’Amico Fellow 1982
Deborah Darnley-Fisch Resident, Fellow 1989
Sonal Dave Resident 2007
Helen A. Davis Resident 1982
Janet L. Davis Fellow 1987, Faculty

Ronald Prince Davis Resident, Fellow 2010
Dale G. Davis Fellow 1971
1983
Daniel Dawson Fellow 2006
Delia DeBuc Faculty
Vincent P. De Luise Resident 1981
Gil De Venecia Resident 1960
Peter DeBry Fellow 2001
Derek W. Delmonte Fellow 2011
David R. DeMartini Fellow 1983


Anna Maria Demetriades Fellow 2010
Yuqing Deng Research Fellow 2018
Patrick Dennehy Fellow 1988
Avnish A. Deobhakta Resident 2012
Manishi A. Desai Fellow 2008
Daniel Desjardins Fellow 1985
Gilles Desroches
Fellow 1980
Eric Dessner Fellow 2008
Amr Dessouki Fellow 2000
Vasilios F. Diakonis Fellow 2015
J. Daniel Diaz Fellow 2021 George Dinter Resident 1969
Alberto G. Distefano Fellow 2016
Richard D. Dix Former Faculty Lena A. Dixit Fellow 2016
Erin Doe Fellow 2000 Bernard H. Doft Resident 1978
Kendall E. Donaldson Resident, Fellow2004, Faculty
1983 1983 1984
Matthew B. Donovan Fellow 2021
Rishi R. Doshi Fellow 2013
Mark J. Douglas Fellow, Chief Resident 2001
Richard Dreyer Fellow 1984
William T. Driebe Fellow 1984
Daniel B. Driscoll Resident, Fellow 2011
Sander R. Dubovy Faculty
Joseph Ducharme Fellow 1998
Bernard Duchesne Research Fellow 1996
Kathleen M. Duerksen Resident 1989
Eric R. H. Duerr
Resident, Fellow2020, Former Faculty
Lee R. Duffner Resident 1969
Jyoti R. Dugar Fellow 2013
Pravin U. Dugel Fellow 1993
Jacob S. Duker Resident 2020
Dilek Dursun Fellow 2001
Daliya Dzhaber Fellow 2021
William W. East Resident, Chief Resident 1974
Jose J. Echegaray Fellow 2020
Daniel Eichenbaum Resident 1973
Charles W. Eifrig Resident, Fellow, Chief Resident 2003
Aziza El Aouni Research Fellow 1997
Norman Ellerman Resident, Chief Resident 1964
Erika M. Ellis MVSIO 2018
Matthew E. Emanuel Fellow 2014
Andres Emanuelli Fellow 2012
Geoffrey Emerick Fellow 1998
Mazen Eneyni Fellow 1996
Benjamin P. Erickson Resident, Fellow 2016
Jonathan Erickson Fellow 2011
Edgar M Espana Research Fellow 2005
Diego G. EspinosaHeidmann Research Fellow 2005
Thomas F. Essman Fellow 1994
Gathline Etienne Fellow 2013
Jonathan R. Etter Fellow 2010
Sheikh M. Faheem Fellow 2018
Scott M. Fair Fellow 2020
Manuel Falcão Research Fellow 2010
Michelle M. Falcone Resident 2020, Faculty
Frank Fankhauser Research Fellow 1993
Lilia Fannin Fellow 2001
Francisco E. Fantes
Resident, Fellow 1987, Former Faculty
Michel E. Farah Research Fellow 1984
Bradley K. Farris Fellow 1986
Herbert P. Fechter Fellow 2003
Michael R. Feilmeier Resident 2009
Daniel K. Ferguson
Resident, Fellow 2005
Viviana Fernandez Research Fellow 2005
Luis Fernandez-Vega Fellow 2018
Renato Ferreira Pires Research Fellow 2000
John Fileta Fellow 2015
Edward Fineberg Resident 1975
M. Elizabeth Fini Former Faculty
Jeffrey L. Fischer Resident 1996
Oliver G. Fischer Fellow 2016
Barron C. Fishburne Resident 1995
Jerome P. Fisher Resident 1980
Daniel Fishkoff Resident 1961
Jane Fishler Resident, Fellow 2012
Steven J. Fliesler Former Faculty
Richard Flindall Fellow 1970
Robert A. Flores Fellow 1993
Harry W. Flynn Jr. Faculty
John T. Flynn
Honorary Alumnus, Former Faculty
Alan G. Fong Fellow 2016
Jerry G. Ford Fellow 1996
Richard K. Forster Resident, Chief Resident 1970, Interim Chair, Faculty Emeritus
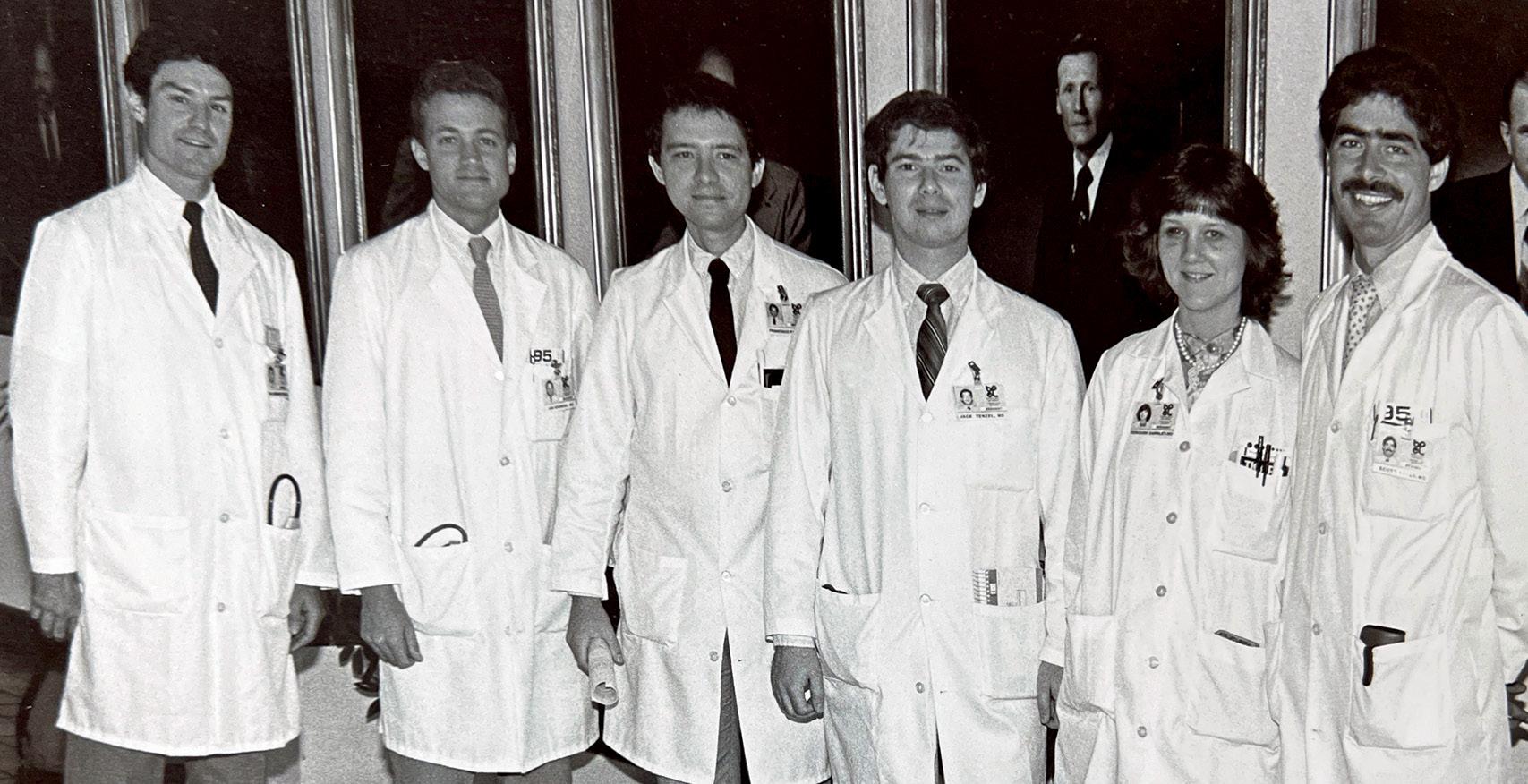
Jorge A. Fortun Faculty
Robert E. Foster Fellow 1993
Benjamin J. Fowler Resident 2021
Gregory M. Fox Resident, Fellow 1992
Martin J. Fox Fellow 1983
Stephen Fransen Fellow 1990
John W. French Fellow 2012
Beth R. Friedland Resident 1984
Tadashi Fujino Fellow 1967
Eriko Fujiwara Research Fellow 2000
Masakatsu Fukuda Research Fellow 1989
Dwain G. Fuller Fellow 1975
Anne E. Fung Fellow 2005
Wayne E. Fung Fellow 1968
Walter Gager Fellow 1968
Jaime R. Gaitan Resident, Fellow 2008
Anna Galanopoulos Fellow 1997
Steven L. Galetta Fellow 1988
Paul Gallogly Resident, Fellow, Chief Resident 2008
Anat Galor Fellow 2008, Faculty Mark S. Gans Fellow 1986
Gail L. Ganser Resident 1996
Armando L. Garcia MVSIO, Fellow 2019
Thomas W. Gardner Fellow 1984
Robert B. Garoon Fellow 2018
J. Donald M. Gass
Honorary Alumnus, Former Faculty
1984 1986
1986 1987 1988
Morgan Gaunt Pansegrau
Fellow 2008
Sandrine Gautier Research Fellow 1997
Gregg S. Gayre Resident 1999
Steven J. Gedde Fellow 1996, Faculty
Edward C. Gelber Fellow 1975 Henry Gelender Fellow 1977
Mohamed Gendy Research Fellow 2009
Mathew K. George Fellow 2012
Mark P. Ghassibi Fellow 2017
JoAnn A. Giaconi Fellow 2003
Allister Gibbons Fellow 2015, Faculty
Steven Gilberg Fellow 1992
Walter Gilbert Fellow 1968
Arthur Gillman Resident 1960
Joel S. Glaser Resident, Fellow 1967, Former Faculty
David G. Godfrey Fellow 1999
Kong Yong Goh Fellow 1995
Jeffrey L. Goldberg Resident, Fellow 2010, Former Faculty
Roger A. Goldberg Resident 2012
Brian E. Goldhagen Fellow 2015, Faculty
Yochanan Goldhammer Fellow 1974
Raquel Goldhardt Fellow 2010, Faculty
David A. Goldman
Resident, Fellow, Chief Resident 2007, Former Faculty
James M. Goldman Fellow 2007
Subba R. Gollamudi Fellow 1992
Daniel Gologorsky Resident 2017
Luri Golubev Research Fellow 2009
Michel Gonvers Fellow 1977
Christine R. Gonzales Resident 1999
Marco A. Gonzalez Resident, Fellow 2015
Roy A. Goodart Fellow 1979
Todd Goodglick Fellow 1993
Margot L. Goodkin Fellow 2009
James Goodwin Fellow 1976
Justin T. Gottlieb Fellow 1995
Sara F. Grace Resident, Fellow 2016
Alana L. Grajewski Fellow 1989, Faculty
David J. Grasic Fellow 2020
Sean M. Gratton Fellow 2014
Trevor Gray Fellow 1997
Stuart N. Green Fellow 1979
Paul B. Greenberg
Former Faculty
David S. Greenfield Fellow 1995, Faculty
Anthony B. Greer Fellow 2015
Giovanni Gregori Faculty
Ninel Z. Gregori
Resident, Fellow 2007, Faculty
Michael G. Gressel Fellow 1984
Kevin W. Greuloch Fellow 2004
Michael R. Grimmett
Former Faculty
Baird S. Grimson Fellow 1977
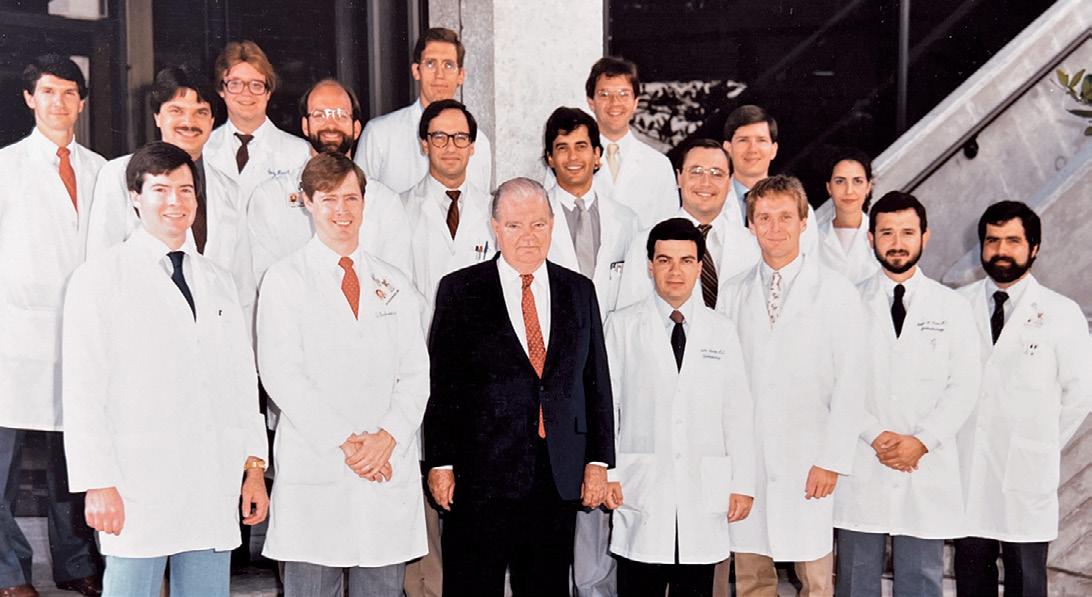
Davinder S. Grover Fellow 2010
R.K. Guerry Resident 1976 Matthew G. Guess Fellow 2005
James H. Guildford Fellow 1988
Medhat F. Guirgis Fellow 2001
Nishi Gulati Fellow 2011
Manasa Gunturu Fellow 2019
Anita Gupta Fellow 2009, Former Faculty
Isha Gupta Fellow 2020
Nisha Gupta Fellow 2016
Joseph R. Gussler Fellow 1994
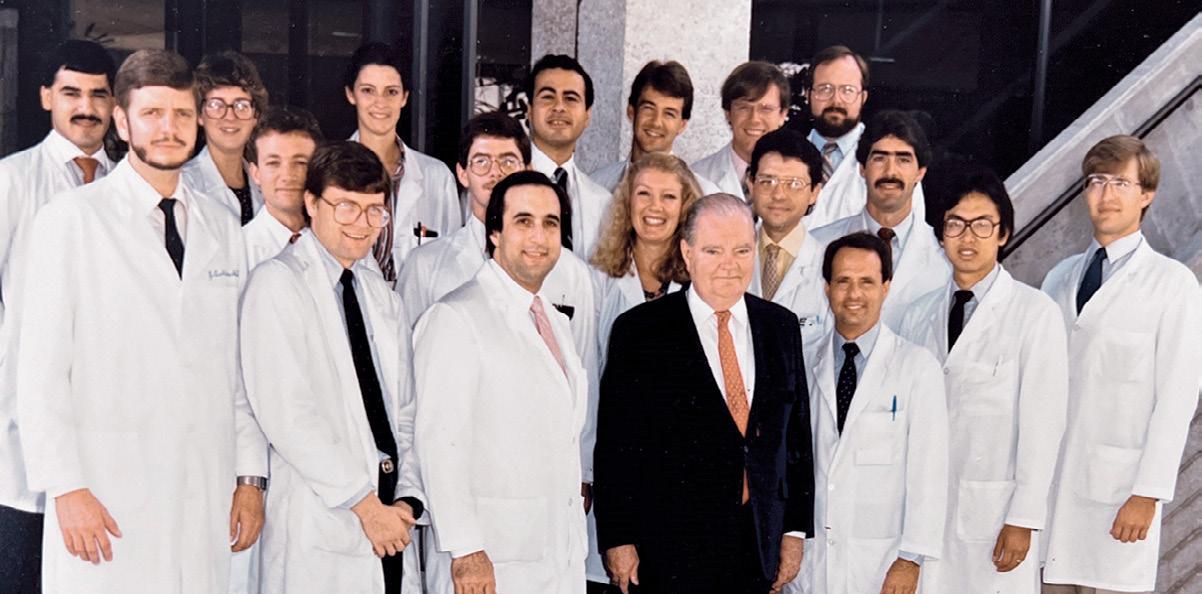
Froncie A. Gutman Fellow 1965
John R. Guy Former Faculty
Jeffrey R. Haag Fellow 1984

Ranya Habash Former Faculty
Takahiko Hachiya Research Fellow 1992
Abigail S. Hackam Faculty
O. Bruce B. Hadden Fellow 1975
Luis J. Haddock Resident 2012, Faculty
Eduard A. Haefliger Research Fellow 1986
Ivan O. Haefliger Fellow 1994
Payman Haft Resident, Fellow 2009
Robert Haimovici Resident 1990
Bryan C. Hainline Fellow 2008
Amy B. Halikman Fellow 1991
Duco I. Hamasaki Faculty Emeritus
Harry A. Hamburger Fellow 1984
Latif M. Hamed Fellow 1989
Ralph Hamilton Resident 1981
William M. Hammonds Fellow 2006
Eric D. Hansen Resident, Fellow 2021
Kara H. Harbick Resident, Fellow 2002
J. William Harbour Fellow 1995, Former Faculty
David Hardy Fellow 1998
Luxme Hariharan Fellow 2014
Russell Harner Resident, Fellow 1972
Thomas W. Harper Resident, Fellow, Chief Resident 2009
Michael S. Harris Fellow 1985
Kristen L. Hartley Resident, Fellow, Chief Resident 2007
Ben J. Harvey Fellow 2012 Ardita Hasalami MVSIO 2021
Bahareh Hassanzadeh Fellow 2015
Andy Hay Resident 1991
J. Timothy Heffernan Fellow 1988
David Heidemann Fellow 1987
Thomas J. Heigle Resident 1996, Former Faculty
1988
Todd W. Heilskov
Resident 1990
Jeffrey Henderer Resident 1998
Amanda D. Henderson Fellow 2016
Chris R. Henry
Resident, Fellow, Chief Resident 2016
Ginger L. Henson Rattan Resident, Fellow 2009
Angela M. Herro Fellow 2015
Jonathan Herschler
Former Faculty
Leonard Hershkowitz Fellow 1975
Dale K. Heuer Fellow 1984
George Hilton Fellow 1967
Akil Hinds Research Fellow 2019
John W. Hinkle Resident 2019
Louis K. Hirsch Fellow 2017
Joanne W. Ho Fellow 2021
Tony W. Ho Fellow 1992
Brian Hoar Fellow 1976
Jubran Hoche Fellow 1985
Elizabeth A. Hodapp Faculty
Joseph Hoffman Resident 1985
Rodrigo Hoffmann Research Fellow 2009
Ana L. Hofling-Lima Research Fellow 1984
Richard Hoft Fellow 1988
Ambika S. Hoguet Fellow 2014
Simon P. Holland Fellow 1987
John H. Holly Resident 1963
Gary Hopen Fellow 1983
Tsugihiko Horiuchi Fellow 1975
Patrick Hostyn Research Fellow 1992
Samuel K. Houston Resident 2013
Cleve Howard Fellow 1980
Hugo Y. Hsu Fellow 2004
Andrew J.W. Huang
Resident, Fellow 1991
Gintien Huang Fellow 2015
Linda Y. Huang Fellow 2016
Suber S. Huang Fellow 1990
Xiang Run Huang
Former Faculty
Jennifer I. Hui Resident, Fellow 2008, Former Faculty
Jan Hummer Resident, Fellow, Chief Resident 1997
David M. Hunter Resident 1970
Steven Hunter Resident 1979
Saunders Hupp Resident 1984
Reva Hurtes Honorary Alumna
Rehan M. Hussain Fellow 2019
Judy D. Hustead Resident 1988
William L. Hutton Fellow 1973
Camille M. Hylton Fellow 2004
Maggie Hymowitz Fellow 2011
1989 1989
Takeshi Ide Research Fellow 2008
Azra Idrizovic Fellow 2016
Nauman Imami Fellow 1997
George Inana Faculty Emeritus
Alfonso Iovieno Research Fellow 2009 Alexander Irvine Fellow 1970
W. David Irvine Resident, Chief Resident 1992
Blake A. Isernhagen Fellow 2015
Hacer Isildak Fellow 2018
Ryan F. Isom Resident, Fellow, Chief Resident 2013
Charles Israel Fellow 1971
Dmitry V. Ivonov Faculty
Fumino Iwata Research Fellow 1993
Takeshi Iwata Research Fellow 1991
Haneen Y. Jabaly-Habib Fellow 2004
Korey A. Jaben Resident 2015
Scott L. Jaben Resident, Fellow, Chief Resident 1982
Robert L. Jack Fellow 1973
Don J. Jackson Fellow 1982
David J. Jacobs Fellow 2011
Samuel G. Jacobson
Former Faculty
Gary Jaffe Resident 1982
Martine J. Jager Fellow 1993
Valerie Jallet Research Fellow 1995
Sulayman E. Jallow Fellow 1981
Brien P. James Fellow 1977
O. Edward James Resident 1971
Glen D. Jarus Fellow 1983
Golnaz Javey Fellow 2009
Hong Jiang Fellow 2011, Faculty
Vishak J. John Fellow 2013
John C. Johnson Fellow 1976
Katherine E. Johnson Resident 2007
Mark W. Johnson Fellow 1990
Robert N. Johnson Fellow 1988
Thomas E. Johnson Fellow 1993, Faculty
Dan B. Jones Resident, Chief Resident 1969
David T. Jones Resident 1998
Wesley Jones Resident 1972
Brian C. Joondeph Fellow 1989
Karen M. Joos Fellow 1994
Eugene E. Joyce Resident 1967
Anna K. Junk Faculty
Peter K. Kaiser Fellow 1997
Manish Kalaria Fellow 2007
Nicholas H. Kalvin Resident 1966
Aditya Kanesa-thasan Fellow 2020
Se Wo Kang Research Fellow 1998
1991 1991 1990
Tracy A. Kangas
Fellow 1995 Mary B. Kansora Fellow 2018
Andrew A. Kao Fellow 2011
Namrata Kapoor Fellow 2009
Carol L. Karp
Fellow 1994, Faculty Louis Kasner Fellow 1996
Oscar Kasner Fellow 1988
Hirohiko Kato Research Fellow 1995
Hasan M. Kattan
Fellow 1990
Harold Katz Fellow 1984
Raananah Katz Resident, Fellow 1981
Matthew D. Kay Former Faculty
Edward Kazarian Fellow 1978
Gary M. Keoleian Fellow 1991
Gerard N. Kervick Fellow 1990
Sara Khandan Fellow 2018
Pooja Khator Fellow 2006
Sherif S. Khedr Fellow 2017
Kay T. Khine Fellow 2018
Earl Kidwell Fellow 1978
Gerhard Kieselbach Research Fellow 1999
Jeremy Z. Kieval Fellow 2009
Brian T. Kim Fellow 2013
Daniel K. Kim Fellow 1989
Elma E. Kim Fellow 2011
Hanna Y. Kim Fellow 2013
Judy E. Kim Resident 1994
Michael Kim Fellow 2000
Richard U. Kim Fellow 2002
Tyson N. Kim Fellow 2019
Won I. Kim Fellow 2009
Nancy M. Kirk Resident 1982
Krishna S. Kishor Fellow 2007, Faculty
John W. Kitchens Fellow, Chief Resident 2005
Jane Kivlin Fellow 1981
Atsuko Kiyosawa Research Fellow 2010
James W. Klein Fellow 1976
Lee I. Klein Resident 1986
Ronald Klein Resident 1976
Lanning B. Kline Fellow 1979
Robert M. Knape Fellow 2012
Robert W. Knighton Fellow 1979, Faculty Emeritus Anne Ko Former Faculty Audrey C. Ko Resident 2015
Marcus J. Ko Fellow 2014
Akira Kobayashi Research Fellow 1992
Bruce Kohrman Fellow 1989
Gregg Kokame Fellow 1988
Hiroyuki Kondo Research Fellow 1997
Wei Kong Research Scholar 2009
Ellen Koo Faculty
Eubee B. Koo Resident 2019
Aaleya F. Koreishi Fellow 2005
Ilyse S. Kornblau Fellow 2019
Helen L. Kornmann Fellow 2014, Former Faculty Andrea N. Kossler Resident, Fellow 2012
Maja Kostic Fellow 2020
Nikisha Kothari Resident 2017
Jaclyn L. Kovach Fellow 2007, Faculty
Martina Kralinger Research Fellow 2000
Joel H. Kramer Resident 1971
Kenneth Krantz Fellow 2006
Rohit Krishna Fellow 1999
Jan W. Kronish Resident, Chief Resident 1989 Friedrich E. Kruse Research Fellow 1991

Anup A. Kubal Fellow 2010
Francois Kuhne Research Fellow 1992
Kaushal M. Kulkarni Fellow 2012
Stephen M. Kulvin Resident 1970
Ajay E. Kuriyan Resident, Fellow, Chief Resident 2016
Joseph Kurstin Resident, Chief Resident 1968
Stefan Kurtenbach Research Fellow, 2017 Faculty
Burton J. Kushner Fellow 1974
Roger P. La Rue Resident 1960
Pierre Laflamme Fellow 1976 Karren Laird Resident 1997
Robert J. Laird Resident, Chief Resident 1975 Geeta Lalwani Fellow 2007, Former Faculty
Byron L. Lam Fellow 1991, Faculty
Horst Laqua Fellow 1976
Eric Larson Resident, Fellow 2003
Michelle Latting Fellow 2020
Alison J. Lauter Fellow 2021, Faculty
Paul R. Layman Resident 1974
Bradford W. Lee Resident 2013, Former Faculty
Brandon W. Lee Fellow 2011 Jennifer W. Lee Fellow 2017 John P. Lee Fellow 1984 Rachel H. Lee Fellow 2021
Richard K. Lee Resident, Fellow 2004, Faculty Steven Lee Fellow 1995 Wendy W. Lee Fellow 2004, Faculty
Wen-Hsiang Lee Former Faculty Yunhee Lee Faculty
John E. Legarreta Fellow 2015
Jean-Marc Legeais Research Fellow 1991 Hana Leiba Fellow 1995
1993 1993
Theodore Leng
Resident 2009
John A. Leon Fellow 1989
Robert E. Leonard Resident, Fellow, Chief Resident 1996


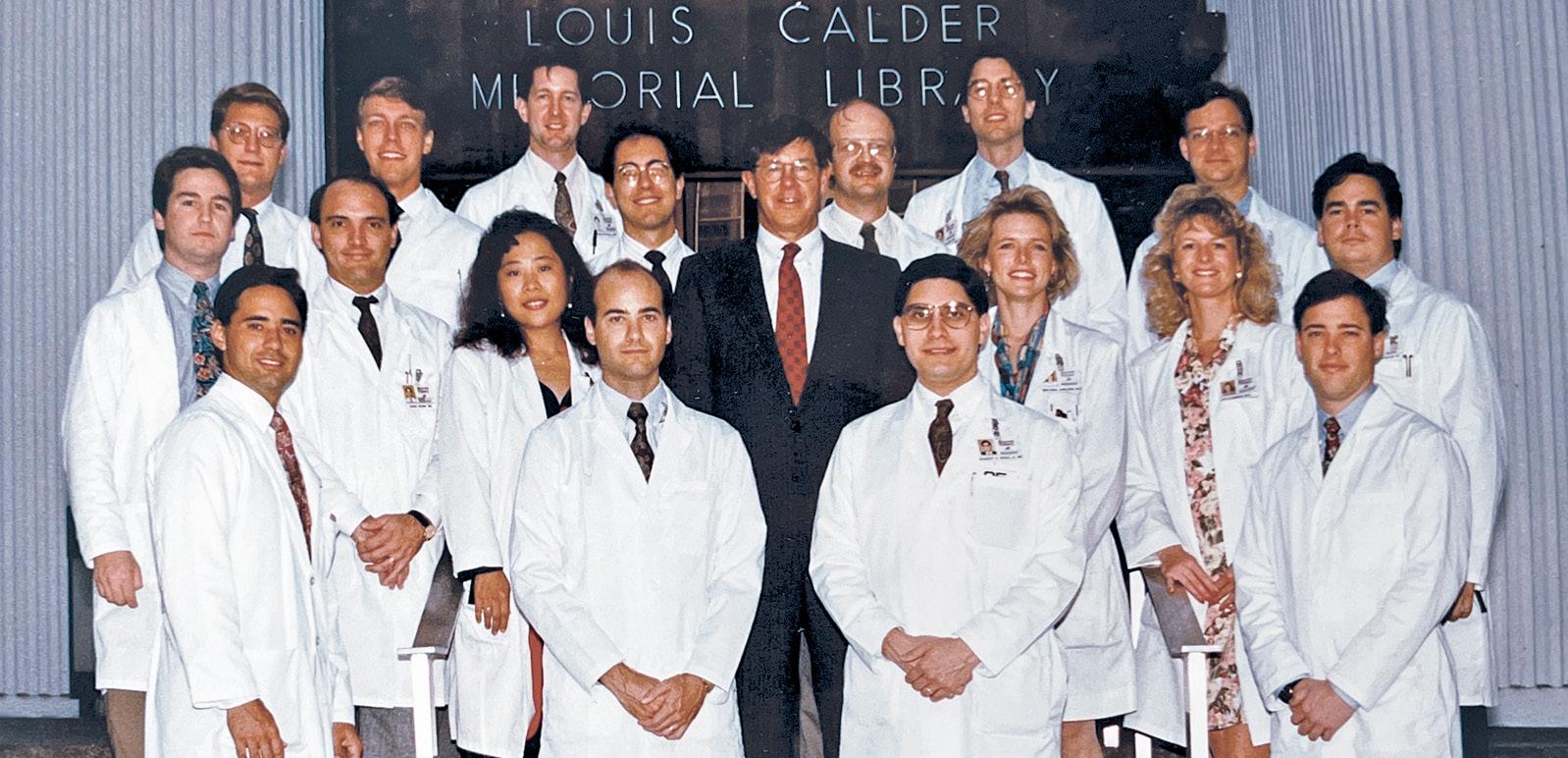
Frederick Lepore Fellow 1980
Ella H. Leung Fellow 2016
Andrew Levada Resident, Fellow 1982
David Levenson Fellow 1965
Ira K. Levine Fellow 1987
Kathrine Leviste MVSIO 2020
Alexandra E. Levitt Resident 2020 Ivor Levy Fellow 1974
James R. Lewis Fellow 1990
Mary Lou Lewis Fellow 1972, Faculty Emerita
Richard A. Lewis Fellow 1975
Kam-Fa Li Research Fellow 1989 Yiwen Li Faculty
Sophie D. Liao Fellow 2014
Douglas Lieb Fellow 2002
Thomas J. Liesegang Resident, Chief Resident 1976
Michele C. Lim Fellow 2000
James Lin Fellow 2019
Richard C. Lin Fellow 2006
John T. Lind Fellow 2009
Ahila Lingappan Resident 2010
Robert Lingua Former Faculty
William J. Lipham Resident 1997
Grant T. Liu Fellow 1993

Stephanie M. Llop Santiago Faculty
Louis A. Lobes Resident 1976
Neal Logan Fellow 1982
Roy Loo Fellow, Chief Resident 2002
Christina Lopez Research Fellow 1996
McGregor N. Lott Fellow 2008
Casey J. Lowrance Fellow 2019
Matthew D. Lowrance Fellow 2013
Jordon J. Lubahn Fellow 2013
Wojciech Lubinski Research Fellow 1992
James G. Luetkemeyer Resident 1993
Brandon J. Lujan Fellow 2008
Susan Luscombe Resident 1980
Rajiv Luthra Former Faculty
Malcolm N. Luxenberg Resident 1966
Deanna P. Lyttle Fellow 2016
Robert Machemer Fellow 1968, Former Faculty
Brian Madow Fellow 2009
James M. Magnusen Fellow 1979
Robert C. Magoon Resident 1963
Arindel S. Maharaj Fellow 2014, Faculty
James C. Major Sr. Resident, Chief Resident 1963
James C. Major Jr. Resident, Fellow, Chief Resident 2009
Nayla Malek Research Fellow 1993
Kim S. Mallick Fellow 1985
John D. Mallonee Resident 1977
Sid Mandelbaum Fellow 1982
Efrem D. Mandelcorn Fellow 2010
Mark S. Mandelcorn Fellow 1974
Fabrice Manns Research Fellow 1997, Faculty
Tomiya Mano Research Fellow 1989
Fabiola Mansur de Carvalho Fellow 1991
Lisa Kay Mao Resident 1992
J. Richard Marion Fellow 1978
Peter Marsh Resident 1997
John J. Martin Fellow 1987
Heidy C. Martinez Fellow 2020
Jose Agustin Martinez Fellow 1993
Jaime D. Martinez-Martinez Research Fellow, Fellow 2020, Faculty
Amy Z. Martino Fellow 2012
Yukihiko Mashima Research Fellow 1991
Steven L. Maskin Fellow 1991
Ben L. Mason Resident, Fellow 2006
Mizuo Matsui Research Fellow 1972
Jared L. Matthews Fellow 2017
Jeffrey J. Mattingly Fellow 2020
Elias C. Mavrofrides Fellow, Chief Resident 2004
John McBeath Resident, Fellow 1978
Catheleen McCabe Resident 2000
Andrew J. McClellan Resident, Fellow, Chief Resident 2017
John A. McCrary Fellow 1967
Brooks W. McCuen Resident 1978
Timothy J. McCulley Fellow 2000
Rhea McDonough Siatkowski Resident, Fellow 1999
Brian McKillop Fellow 1981
Craig A. McKeown Faculty
Adam McLaughlin Fellow 2014
Edward B. McLean Fellow 1972
William McLeish Resident 1989
Alexander R. McLeod Fellow 1973
Fred L. McMillan Fellow 1974
Mario Meallet Fellow 2002
C. Maxwell Medert Resident 2021
Carlos A. Medina Mendez Research Fellow, Fellow 2016
Calvin Mein Fellow 1982
Jerry Meislik Fellow 1978
Melissa Meldrum-Aaberg Resident, Fellow 1993
Alan D. Mendelsohn Fellow 1987
Carlos E. Mendoza-Santiesteban Faculty
John C. Merritt Fellow 1975
1995 1997 1999
Kenneth H. Messner
Fellow 1972
Rike Michels Research Fellow 2004
Ron Michels Fellow 1973
Stephan Michels Research Fellow 2005
Robert C. Mickatavage Resident 1964
William F. Mieler Resident, Chief Resident 1985
Solange Milazzo Research Fellow 2004
Daniel M. Miller
Resident, Fellow, Chief Resident 2006
Darlene Miller
Faculty Gordon R. Miller Resident, Chief Resident 1966

John J. Miller
Resident, Chief Resident, Fellow 2006
Kevin P. Miller Fellow 2018
Michael P. Miller Resident 1996
Kristin Minkowski Fellow 2021
Shahnaz Miri Fellow 2021
James Mitchell Fellow 1981
Atsushi Mizota Research Fellow 1990
Dimple Modi Fellow 2012
Yasha S. Modi Resident 2014
Kenneth Moffat Fellow 1983
Amir Mohsenin Fellow 2015
Antonio Montalbo Fellow 1971
Christina S. Moon Fellow 2013
Jeffrey K. Moore Resident, Fellow, Chief Resident 2004
Renuka Mopuru Fellow 2019
Alexei L. Moraczewski Resident, Fellow 2007
Diany S. Morales Resident, Fellow 1999
Juan Moreno Jarrin Research Fellow 1992
Rebecca Morgan Fellow 1990
Melina I. Morkin Fellow 2019
Jada Morris MVSIO 2021
Robert Morris Fellow 1978
Andrew Moshfeghi Fellow 2006, Former Faculty
Arlanna N. Moshfeghi Fellow 2006, Former Faculty
Stephen J. Moster Resident 2018
Marcus S. Muallem Fellow 2003
Jay Mulaney Fellow 1990
Paul M. Munden Fellow 1992
Wuqaas M. Munir Fellow 2006
Michelle Munoz Former Faculty 1999
Akira Murakami Research Fellow 1992
J. Frank Murchison Fellow 1991
Fernando H. Murillo-Lopez Fellow 1995
Timothy G. Murray Former Faculty
Allie M. Nadelson Fellow 2016
Yasunobu Nagae Research Fellow 1994
Zayna Nahas Fellow 2013
Natsushi Nakagawa Research Fellow 1999
Nambi Nallasamy Fellow 2018
Abed Namavari Fellow 2017
Mohit Nanda Fellow, Chief Resident 1990


Afshan A. Nanji Fellow 2014
Derek Nankivil Research Fellow 2011
Arvind Neelakantan Fellow 2007
Ann G. Neff Fellow 2000, Former Faculty Christine C. Nelson Fellow 1984
Juan A. Nevarez Fellow 1985
David A. Newsome Fellow 1977
Alexander T. Nguyen Fellow 2018
Jackie K. Nguyen Fellow 2006
Quang Nguyen Fellow 1997
Don H. Nicholson Former Faculty
William Nicol Fellow 1969
Neda Nikpoor Resident, Fellow 2017
Cynthia P. Nix Resident, Fellow 2010
Don Noel Fellow 2021
Jila Noorikolouri Fellow 2020
Edward W. D. Norton Founding Chair
Terrence P. O’Brien Faculty
Patrick O’Conner Fellow 1978, Former Faculty
Jeffrey Odel Fellow 1977
Rafael Oechsler Research Fellow 2009
Richard B. Oglesby Resident 1963
Guy E. O’Grady Resident 1971, Former Faculty
Kingsley C. Okafor Fellow 2017
Constance Okeke Fellow 2005
Anne-Marie E. Okoduwa MVSIO 2021
Lisa C. Olmos de Koo
Resident, Fellow, Chief Resident 2010
Karl R. Olsen
Resident, Chief Resident 1986, Former Faculty
John C. Olson Fellow 1982
Cassandra B. Onofrey Resident, Fellow 2002
Avinoam Ophir Fellow 1981
Robert H. Osher Resident, Fellow 1980
Carla J. Osigian Probst Fellow 2017, Former Faculty Angela Oster Resident 1999
Ray T. Oyakawa Fellow 1981
James D. Paauw Fellow 2010
Elba Pacheco Resident 1989
Scott E. Paitker Fellow 1986
Sotiria Palioura Fellow 2015
Paul F. Palmberg Faculty
Joseph Panarelli Fellow 2012, Former Faculty
Anushree M. Pandya MVSIO 2021
Seth M. Pantanelli Fellow 2014
George C. Papachristou Fellow 2013
Jean-Marie Parel Honorary Alumnus, Faculty
Paul W. Park Fellow 2005
Stanley S. K. Park Fellow 2018
D. Wilkin Parke III
Resident, Fellow, Chief Resident 2013
James L. Parker Fellow 1977
Richard K. Parrish II Fellow 1982, Faculty, Chair
Michael Parrott
Resident, Fellow, Chief Resident, 2010

Jacqueline N. Parrotta Fellow 2019
Kambiz K. Parsa Fellow 2006
Joshua Pasol Fellow 2007, Faculty
Neel D. Pasricha Fellow 2021
Heena R. Patel Fellow 2014
Nimesh Patel Resident, Fellow, Chief Resident 2020 Ravi H. Patel Fellow 2016
Umangi A. Patel Fellow 2021
Avinash Pathengay Research Fellow 2011
Jonathan Pederson Fellow 1978
Daniel Pelaez Faculty
Jesse S. Pelletier Fellow 2008
Zhiyou Peng Research Fellow 2017
Zuhair H. Peracha Fellow 2016
Ivonildo C. Pereira Fellow 1989
Gerardo M. Perez Fellow 1986
Victor L. Perez Former Faculty
Diley Perez-Garcia Fellow 2020
Gary A. Pesicka Fellow 1986
Stephen C. Pflugfelder Fellow 1986, Former Faculty
Pittaya Phamonvaechavan Research Fellow 2009
Renata Picciani Fellow 2014
Alejandra M. Piniella Resident 2000
Nathan Pirakitikulr Resident 2021
James C. Pitts Fellow 2016
David E. Poeltl Resident 1992
Timothy Polk Fellow 1995
Samuel E. Poppell Fellow 1982
Vittorio Porciatti Faculty
Sreedhar Potarazu Fellow 1995
Stanley Potter Resident 1959
James O. Powell Resident 1974
Antonio Prado Resident 1994
Carmen A. Puliafito Chair
Jose S. Pulido Fellow 1987
Lutz E. Pullinat Fellow 1994
Donald G. Puro Resident 1980
Hui Qiu Research Fellow 2000
Ann V. Quan Resident, Fellow 2021
Harry A. Quigley Fellow 1977
David Quillen Fellow 1995
Carolyn D. Quinn Resident, Fellow 2005, Former Faculty
Joseph A. Qureshi Resident 2009
Stephen M. Rabinowitz Fellow 1989
Aleksandra V. Rachitskaya Resident, Fellow, Chief Resident 2014
Janet Rader Fellow 1991 Ronald Radius Fellow 1979
Emeline Radhika Ramenaden Fellow 2015
Henry M. Ramseur Resident, Chief Resident 1971
Pradeep Y. Ramulu Fellow 2007
Rumya Rao Fellow 2011
Paul A. Raskauskas Fellow 1991
Siddarth Rathi Fellow 2017
Frederick M. Rauscher Resident, Fellow 2008
Tracy B. Ravin Resident 2003
Sarah P. Read Resident, Fellow, Chief Resident 2018
Raymond Records Fellow 1971
Ashvini K. Reddy Fellow 2013
Rahul Reddy Fellow 2004
Usha P. Reddy Resident 2009
Nelson Redfern Resident 1979
Lawrence T. Reese Fellow 1978
Nidhi R. Relhan Batra Fellow 2018
Ann M. Renucci Fellow 2002
Maria Cecilia Reyes Fellow 2010
Dale S. Reynolds Fellow 1997
Michael G. Reynolds Resident, Fellow 1992
Douglas J. Rhee Fellow 2000
Leonard S. Rich Fellow 1980
Ryan M. Rich Fellow 2008
David W. Richards Fellow 1987
Preston P. Richmond Resident 1986
Ernesto Rios Montenegro Fellow 1970
John P. Ritchey Fellow 1973
Al Rivera Resident 1985
Dennis M. Robertson Fellow 1969
James C. Robinson Fellow 1995
Edward Rockwood Fellow 1986
Jill F. Rodila
Fellow 2004, Former Faculty Marianeli Rodriguez Resident 2017
Andre Romano Research Fellow 2002
Andrew J. Rong Resident, Fellow 2020, Faculty
Robert Rosa Jr. Resident 1994, Former Faculty
Alexandre Rosen Research Fellow 2003
Krista D. Rosenberg Resident, Fellow 2006
Michael L. Rosenberg Fellow 1981 Michael A. Rosenberg Resident 1973
Philip J. Rosenfeld Fellow 1996, Faculty Steven I. Rosenfeld Fellow 1985
2004 2007
George Rosenwasser
Fellow 1988
Daniel Roth Resident 1998
Elena B. Roth Resident 1996, Faculty
Adam L. Rothman Fellow 2020, Faculty
Paul M. Rougraff Resident 1996
Megan A. Rowlands Fellow 2021
Patrick E. Rubsamen
Resident, Fellow, Chief Resident 1991, Former Faculty
Marco Ruggeri Faculty Ryan B. Rush Fellow 2009
Jonathan F. Russell
Resident, Fellow, Chief Resident 2021
Stephen R. Russell Resident 1986
Cullen D. Ryburn Fellow 2020
Steven J. Ryder Fellow 2017
Alfonso L. Sabater Fellow 2018, Faculty
William I. Sabates Fellow 1980
Avinoam B. Safran Fellow 1978
Hady Saheb Fellow 2011
Mark Salevitz Fellow 1995
Ruben F. Salinas-Garcia Resident 1978
Kumar Sambhav Fellow 2019
David B. Samimi Resident 2011
Joel S. Sandberg Resident 1974
Norman Sanders Resident, Chief Resident 1961
Helga Sandoval Fellow 2001
Steven S. Saraf Fellow 2017
Mikio Sasoh Research Fellow 1995
Roger M. Saulson Resident 1989
Tim Saunders Fellow 1986
Peter J. Savino Fellow 1974
Ibrahim Sayed-Ahmed MVSIO 2018
Mohamed S. Sayed Fellow 2018, Former Faculty
Ronald J. Scelfo Resident 1975
Norman J. Schatz Fellow 1966, Faculty
Amy C. Schefler
Resident, Fellow, Chief Resident 2010, Former Faculty
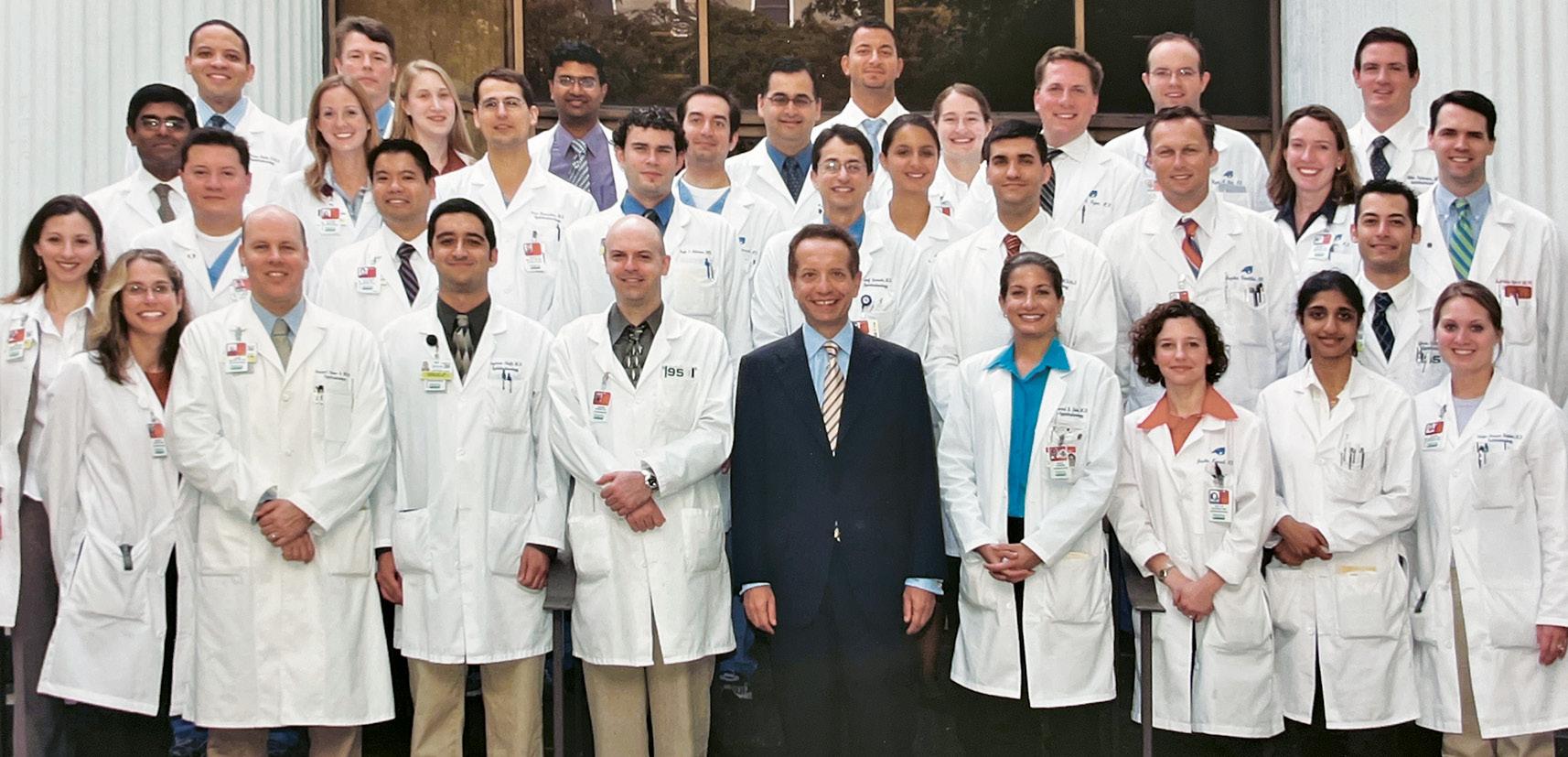
Vivian Schiedler Resident 2005
John J. Schietroma Fellow 1986
Andrew M. Schimel Fellow 2012
Lawrence Schoch Resident 1975
Gerald R. Schultz Honorary Alumnus
Scott Schultz Fellow 2013
Arthur L. Schwartz Fellow 1973
Daniel M. Schwartz Fellow 1989
Geoffrey Schwartz Fellow 2003
Kenneth S. Schwartz Fellow 2003
Lee K. Schwartz Fellow 1980
Marc F. Schwartz Fellow 1986
Stephen G. Schwartz Faculty
Joan Schwoer-Borruat Research Fellow 1992
Ingrid U. Scott Resident, Fellow, Chief Resident 1997, Former Faculty
Kevin R. Scott Fellow 1991
Joseph Scuderi Fellow 1981
Ronald L. Seely Fellow 1971
Ernesto I. Segal Fellow 1991
Tony P. Sellitti Resident 1994
Ausra Pond D. Selvadurai Fellow 2010
Karen Senikowich-Morgan Resident 1984
Robert C. Sergott Fellow 1980
Raymond J. Sever Resident, Chief Resident 1967
Amar P. Shah Fellow 2021
Lavanya Shah Fellow 1994 Milan Shah Fellow 2011
Pulin A. Shah Fellow 2007
Sejal Shah Fellow 2014
Veeral S. Shah Fellow 2013
Neha Shaik Fellow 2019
Valery I. Shestopalov Faculty
Anita R. Shirodkar Shane
Resident, Fellow, Chief Resident 2012
Thomas S. Shane
Resident, Fellow, Chief Resident 2012
James A. Sharkey Fellow 1994
Ashish Sharma Research Fellow 2009
James A. Sharpe Fellow 1973
Lauren J. Shatz Fellow 2003
Hal E. Shaw Fellow 1979
Justin M. Shaw Fellow 2015
Arthur H. Shedden Fellow 1985
Clinton W. Sheets Fellow 2008
Jin-Hui Shen Research Fellow 1994
Bobby J. Shewmake
Resident, Chief Resident 1974
Rebecca A. Shields Resident 2015
Gary Shienbaum Fellow 2013
Hiroyuki Shimada Research Fellow 1989
Paul M. Shipkin Fellow 1979
Thorne Shipley
Former Faculty
John P. Shock Fellow 1971
Erin M. Shriver Fellow 2008, Former Faculty
Maggie F. Shuler Resident 2000
Harold K. Shutt Fellow 1970
R. Michael Siatkowski Fellow 1993, Former Faculty
Nouman Siddiqui Fellow 2005
Joseph Sidikaro Fellow 1983
Ruwan A. Silva Resident 2012
Ariadna Silva-Lepe Fellow 1995
Bernd Silver Resident 1962
Bruce Silverstein Fellow 1995
David W. Sime Resident 1966
2011 2014 2015
David P. Simon
Resident 1975 Gabriel Simon Research Fellow 1993
Mark W. Simon Resident 1993
Brad Simons
Fellow 1998, Former Faculty
Joseph A. Singer Resident 1967
David J. Singer Fellow 1969
Kuldev Singh Fellow 1992
Jack Sipperley
Resident, Chief Resident 1978
Adam B. Sise Fellow 2015
Robert A. Sisk Fellow 2009
Kavitha R. Sivaraman Fellow 2015
Virgil E. Sklar Resident 1984
Ruta J. Skrinska Fellow 1988
Gregory L. Skuta Fellow 1987
Michael Slavin Fellow 1981
Allan R. Slomovic Fellow 1985
Ilya M. Sluch Fellow 2018
William E. Smiddy Faculty
J. Lawton Smith
Honorary Alumnus, Former Faculty
Jess Smith Fellow 1976
Michael P. Smith Fellow 2015



Scott R. Sneed Resident 1987
Lucia Sobrin Resident 2003
Per Soderberg Research Fellow 1995
David A. Sola-Del Valle Fellow 2016
Abraham Solomon Fellow 2001
Joern B. Soltau Fellow 1998
Alice Song Resident 2002
Dae Y. Song Resident 1990
Sabine Sparfel Research Fellow 1992
Kenneth O. Sparks Fellow 1984
John C. Sparrow Resident 1976
Robert H. Spector Fellow 1976
Robert T. Spector Fellow 1983
Frank A. Spellman Fellow 1983
Nehemiah E. Spencer Fellow 2010
Oriel Spierer Fellow 2015
Henry Alex Spratt Fellow 2014
Jayanth Sridhar Resident 2014, Faculty
Lana Srur Faculty
Thomas J. Stafford Fellow 1966
Natalie A. Stanciu Resident, Fellow 2011
Harold Stanley Resident, Fellow 1977
Boris Stanzel Research Fellow 2002
John R. Stechschulte Fellow 1985
Greg E. Stein Fellow 2017
Kimberly E. Stepien Fellow 2007
William Stewart Fellow 1977
William Robert Stiles
Resident 1974
Warren C. Stout Fellow 1985
Jack D. Stringham Resident, Fellow, Chief Resident 2018
Mitchell B. Strominger Fellow 1993
James Stuart Fellow 1964
Doyle Stulting Resident 1981
Rodney Sturm Fellow 1963
Eric Suan Fellow 1991
Brandon K. Suedekum Fellow 2006
Joseph H. Sugg Fellow 2004
Gentaro Sugita Fellow 1978
Leejee H. Suh Fellow 2007, Former Faculty
Kevin K. Suk Fellow 2011
Paul B. Sullivan Fellow 1967 Cathy Q. Sun Fellow 2019
Ivan J. Suñer
Resident 1996, Former Faculty
Jennifer Sung Resident 1998
John Susac Fellow 1973
Swarup S. Swaminathan Resident 2018, Faculty
David E. Swanson Fellow 1980
Zeba A. Syed Fellow 2018
Mary Szatkowski Resident 1980
Homayoun Tabandeh Fellow 1998
Hassan Tahi Research Fellow 2000
Yoshiko Takesue Research Fellow 1993
William L. Taldone Resident 1985
Myron Tanenbaum Resident 1985
Wimolwan Tangpagasit Research Fellow 2009
Yasuo Tano Fellow 1978
Mehdi Tavakoli Fellow 2019
Garth A. Taylor Fellow 1977
Mike Taylor Resident 1965 William Taylor Fellow 1968
Masoud Teimory Fellow 1994
Martin Ten Hove Fellow 1994
David P. Tenzel Fellow 1990
Jack Tenzel Resident 1987
Richard Tenzel Honorary Alumnus Gerald Terris Resident 1958
Despoina Theotoka MVSIO 2020
Benjamin J. Thomas Resident 2013 Matthew A. Thomas Resident 1985
Martin L. Thomley
Resident, Fellow, Chief Resident 1994
Marie Thulliez Research Fellow 2018
Catherine T. Thuruthumaly Fellow 2017
Rollins Tindell Fellow 1981
Donald Tingley Fellow 1990
Aubrey R. Tirpack Fellow 2019
2016
Lisa M. Tom
Fellow 2021
Robert L. Tomsak Fellow 1980
Rahul S. Tonk Fellow 2017, Faculty
Shenandoa Toote MVSIO 2019
Shobha Topgi Fellow 2021
Nicole J. Topilow Resident 2021
Trexler M. Topping Fellow 1978
Justin H. Townsend Resident 2011, Faculty
Michael K. Tracy Fellow 2005
Van Ann Q. Tran Resident 201
Kimberly D. Tran
Resident, Fellow, Chief Resident 2019
Fritis Treffers Research Fellow 1981
Giora Treister Fellow 1976
Joseph Trentacoste Resident 1988
John Trible Fellow 1995
Omer Trivizki Fellow 2020
Jonathan D. Trobe Fellow 1977
James Truitt Resident, Chief Resident 1977 Enoch Tsai Fellow 1973
James C. Tsai Fellow 1994
Ray Jui-Fang Tsai Fellow 1988
Brian C. Tse Fellow 2016, Faculty
David T. Tse Faculty Scheffer C.G. Tseng Former Faculty
Elmer Y. Tu Fellow 1993
David N. Tucker Resident, Fellow, Chief Resident 1973 Sonal Tuli Fellow 2001
Jonathan H. Tzu Resident, Fellow, Chief Resident 2015


Yasutaka Uchihori Research Fellow 1990
Saul Ullman Fellow 1987
Stephen C. Ume Fellow 2006
Lejla Vajzovic Fellow, Resident 2011
Carlos A. Valdes-Lora Resident 1983
Felipe A. Valenzuela Fellow 2017
Stephanie L. Vanderveldt
Resident, Fellow, Chief Resident 2008
Robin Vann Resident 1998
Mylan R. VanNewkirk Fellow 1991
Carlos W. Vazquez Fellow 1998
Luis E. Vazquez Fellow 2014, Faculty

Anil S. Vedula Resident, Fellow 2011
Michaela Velikay-Parel Research Fellow 1996
Nandini Venkateswaran Resident 2019
Lori M. Ventura Fellow 1986, Former Faculty
Angela Verkade Fellow 2020
Alan M. Verm Resident 2001
Nancy F. Vilar Fellow 1998
Franck Villain Research Fellow 1993
2017 2019
Carlos M. Villanueva Fellow 1994
Natalia Villate Fellow 2003
Victor M. Villegas Fellow 2013, Former Faculty
Kateki Vinod Fellow 2016
M. Louella Vivino Fellow 1999
Monika Voigt Research Fellow 2000
Irene Voo Resident, Fellow 2005 David T. Vroman Fellow 2000
Daniel M. Vu Fellow 2020
Edward C. Wade Fellow 1989
Gary R. Wallace Resident 1972
Kenneth Wallace Resident 1972
Wilson Wallace Resident, Chief Resident 1974
Thomas Walsh Fellow 1965
Scott D. Walter Resident 2015
Jianhua (Jay) Wang Faculty
Ming X. Wang Fellow 1997
Ye Elaine Wang Fellow 2019
Roberto Warman Fellow 1987
Yaffa Weaver Brown Resident 1997
Aaron D. Webel Fellow 2019
Stephen M. Weinstock Fellow 1974
Mark A. Weisbrod Fellow 2008
Paul D. Weishaar
Resident, Fellow, Chief Resident 1996
Jayne S. Weiss Resident 1983
Matthew J. Weiss Resident, Fellow 2013
Mark N. Welch Fellow 2013
Roger Welch Fellow 1986
Sarah R. Wellik Fellow 2005, Faculty
John A. Wells Fellow 1965
Rong Wen Faculty
Christina Y. Weng Fellow 2014
Jane C. Werner Fellow 1978
Mark A. Werner Fellow 2006, Former Faculty
Matthew R. West Fellow 2018
Sara T. Wester
Resident, Fellow 2010, Faculty
Carl K. Wetzig Fellow 1981
Garth A. Wilbanks Fellow 1991
Ron Wilbur Resident 1960 Daniel Wilhelm Resident 1965 Charles P. Wilkinson Fellow 1971
Basil K. Williams Resident, Fellow, Chief Resident 2017
Delyse B.Williams Fellow 1989
Frank M. Williams Fellow 1971
John Williams Fellow, Chief Resident 1986 Stu Willner Resident 1965
J. Philip Wilmeth Resident 1985
Deanna K. Wilson Resident 1988
2020 2021
Louis Wilson
Fellow 1966
Tom Wilson Fellow 1976
Timothy W. Winter Fellow 2012
Kirk E. Winward Resident, Chief Resident 1990
Robert S. Wirthlin Resident 2004
Ted H. Wojno Fellow 1983
Thomas Wolf Fellow 1985
George C. Wong Resident 1991
Norman F. Woodlief Fellow 1984
Dana P. Woods Resident 1994
Fasika A. Woreta Fellow 2012
Martha M. Wright Fellow 1991
Tracy M. Wright Fellow 2014
Elaine I. Wu Fellow 2010
Darrell WuDunn Fellow 1995
Charles Wykoff Resident, Fellow, Chief Resident 2010
Katsuya Yagasaki Research Fellow 1988
Tashihiro Yajima Research Fellow 1994
Shalini Yalamanchi Fellow 2011
Mitsumo Yamamichi Research Fellow 1997
Hideo Yamamoto Research Fellow 2010
Akifumi Yamanaka Research Fellow 1995
Uichi Yamanouchi Fellow 1968
Justin J. Yamanuha Fellow 2019
Chung-May Yang Fellow 1991
Nicolas A. Yannuzzi Resident, Fellow, Chief Resident 2020, Faculty


David Yarian Fellow 1979
Kin Yee Fellow 2014
Oliver L. Yeh Fellow 2016
Zohar Yehoshua Fellow 2011, Faculty
Kimberly G. Yen Resident 2000
Michael T. Yen Resident 2000
Joseph Yeung Resident 1974
Michael C. Yim Resident, Fellow 2018
Zhoug Yixiong Research Fellow 2009
Daniel M. Yoder Resident, Fellow 2003
Kenichi Yoshida Research Fellow 2001
Kenichi Yoshino Research Fellow 1994
Ryan C. Young Resident, Fellow, Chief Resident 2016
Sonia H. Yoo Faculty
J. Edward Ysasaga Resident, Fellow, Chief Resident 2002
Hong Yu Faculty Yimin Yuan Research Scholar 2009
Anthony C. Zacchei Fellow 1996
Ihor Zachary Fellow 1974
Charles M. Zacks Fellow 1990
Nicholas Z. Zakov Fellow 1977
Harvey Zalaznick Resident 1977
William Zambrano Resident 1988
Chad C. Zatezalo Fellow 2012
Jill S. Zaveri Fellow 2017
Mike Zein MVSIO 2021
Jeffrey Zervas Fellow 1987
Lucy Y. Zhang Fellow 2017
Xuemin “Rosie” Zhang Fellow 2021
Yan Zhang Research Fellow 2018
Yu Zhao Fellow 2017
Xiao Yi “Ellie” Zhou Fellow 2018
Angela Y. Zhu Fellow 2020 Dagny C. Zhu Fellow 2017
Carol F. Zimmerman Fellow 1989
Jeffrey M. Zink Fellow 2006
Leonid Zlotcavitch Fellow 2020
John V. Zudans Resident 2002
Todd A. Zwickey Fellow 1986























“I predict that Miami will eventually be home to an ophthalmology institute in a medical center second to none in the nation.”
– Bascom Headon Palmer, M.D.
“Dr. (Edward) Norton saw himself as a gardener. His role was to till the soil, plant the seeds, pull the weeds, and stand back and watch the luxuriant growth. He inspired openness and trust. That transparency and integrity created a foundation that allowed Bascom Palmer to grow in reputation and strength.”
– John G. Clarkson, M.D.
“When I arrived at Bascom Palmer in 1969, Dr. Norton told me that my job would be simply to become the best academic ophthalmologist of which I was capable. He explained this his job was to provide the best environment within which that could happen.
– Douglas R. Anderson, M.D.
“Responding to huge demand for the vitrectomy instruments we designed, Bascom Palmer launched a global training program. We knew every patient could not come to us for surgery, so we trained the top ophthalmologists around the world so they could do the procedure in their own countries.”

– Jean Marie Parel, Ing.ETS-G, Ph.D.
“Bascom Palmer’s tradition of excellence drives every aspect of its operation.”
– Eduardo C. Alfonso, M.D.
“The tremendous amount of clinical and pathologic material at Bascom Palmer is essential to the expansion of our research efforts on a national and international level.”
– Sander R. Dubovy, M.D.
“A patient’s problem is an opportunity to innovate.”
– David T. Tse, M.D.
“There is tremendous potential to positively impact patient care through education. Graduating residents and fellows can elevate the quality of care that is delivered in their local communities. As they in turn educate others, they participate in the global dissemination of scientific and clinical knowledge.”
– Steven J. Gedde, M.D.
“I stayed at Bascom Palmer not to be a teacher, but to remain a student for the rest of my life. A day does not pass that I learn far more from the residents, fellows, and my patients than I teach them.”
– Richard K. Parrish II, M.D.
“I could see a rainbow for the first time.”
– 9-year old Creed Pettit following leading-edge gene therapy