AGSMED

Featuring:
How The Scalpel Will Mould Tomorrow: Surigcal Innovation and Cardiovascular Disease.
The Heart of Healing: A Closer Look at Statins As A Treatment for Cardiovascular Disease
Recent Advances in 3D Printing In Cardiovascular Devices History, Advances and Challenges on Heart Transplantation. PCSK9 Inhibitors as a Replacement for Statins.

March 2024
AGSMedisastudent ledscientific magazine,focusing onupandcoming advancesin medicine.Our primaryaimisto introduceglobal innovationatthe schoollevel,aiding allSTEMorientated pupilsinwidening theirknowledge.

Editor-in-chief:
Hrishik Subramani
Editors:
Alex Glover
Anthony Unugboke
Sivaharishan Sivakanthan
Ayaan Raaza
Queries to : D8GanapathySubramani@ags.bucks.sch.uk
Please feel free to find one of the editors for queries as well.
CONTENTS

PAGE11
PCSK9Inhibitors; WillTheyReplace Statins?
PAGE13
TheTragicFinancial Stateof TheNHS- An EconomicCommentary AsideFromTheTheme
PAGE16OpinionPage Puzzles
Bibliography
HowTheScalpel WillMould Tomorrow: Innovationin SurgerySolving Cardiovascular Disease
Hrishik Subramani
Global health challenges are aplenty; the one thing which almost everyone experiences is illness. Out of all of the major health problems in the world, cardiovascular disease is most widespread in its destruction, with 17.9 million deaths every year, being the leading cause of death globally. However, with the growth of human intelligence and the inevitable growth of advanced technology, I am confident in predicting that most, if not all of these cardiovascular diseases will be near eradication in the future, as new treatment plans emerge. In this article, I will outline a few surgical solutions for CVD and how they have been adapted to create new ones, showing promise for progressive development in the future creating optimism in the scientific communityworldwide.
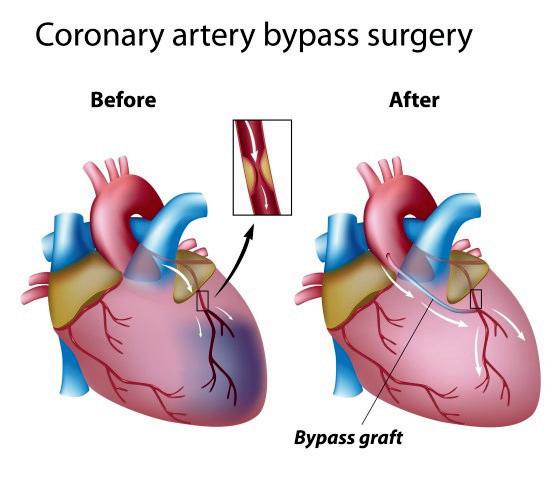
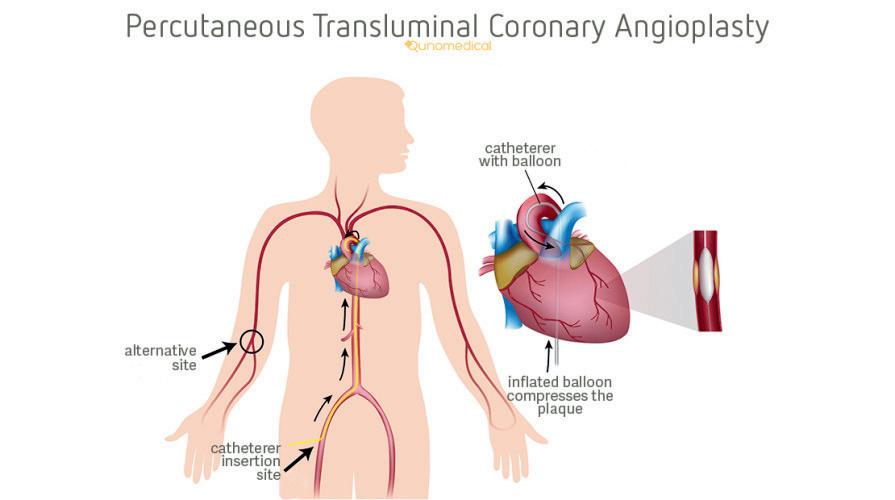
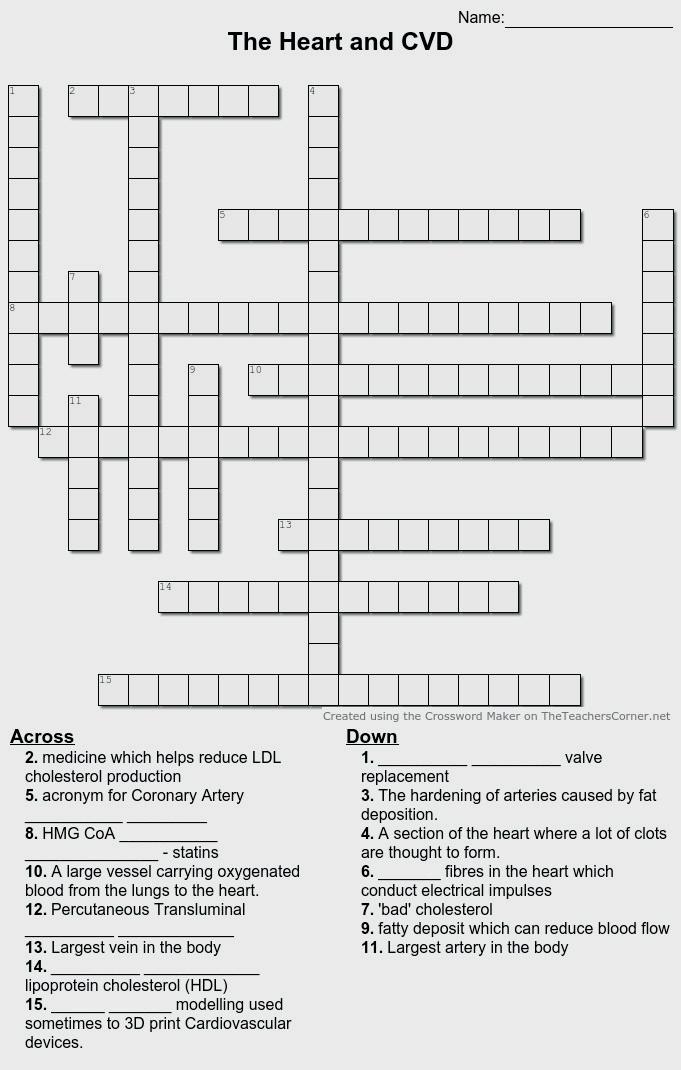
The standard surgical treatments for CVDs today are often Coronary artery bypass grafts(CABG), heart transplants or coronary angioplasties (Percutaneous Transluminal CoronaryAngioplasties-PTCA).
A CABG involves diverting blood flow from narrowed blood vessels supplying the heart to bypass a blockage. PTCA involves inserting a balloonintobloodvesselsand inflating them to create more spaceforbloodflow.
A sensational new technique being pioneered currently is the minimally invasive heart surgery in either thoracoscopic heart surgery or robot assistedsurgery.Inbothcases,thereisa significant decrease in risks of surgery with lower blood loss, faster recovery, lower scarring and lower chance of infection.
Showing PTCA and CABG Procedures.
In particular, robotic surgical methods paveapathwayforsuccessandgrowth, creatingacrediblegroundforoptimism. With the inevitable evolution of technology, robotic surgery is bound to develop in dexterity and perhaps even automate, decreasing operating time andpossibilityofcomplications.
Fig 1 (above), and Fig 2 (left):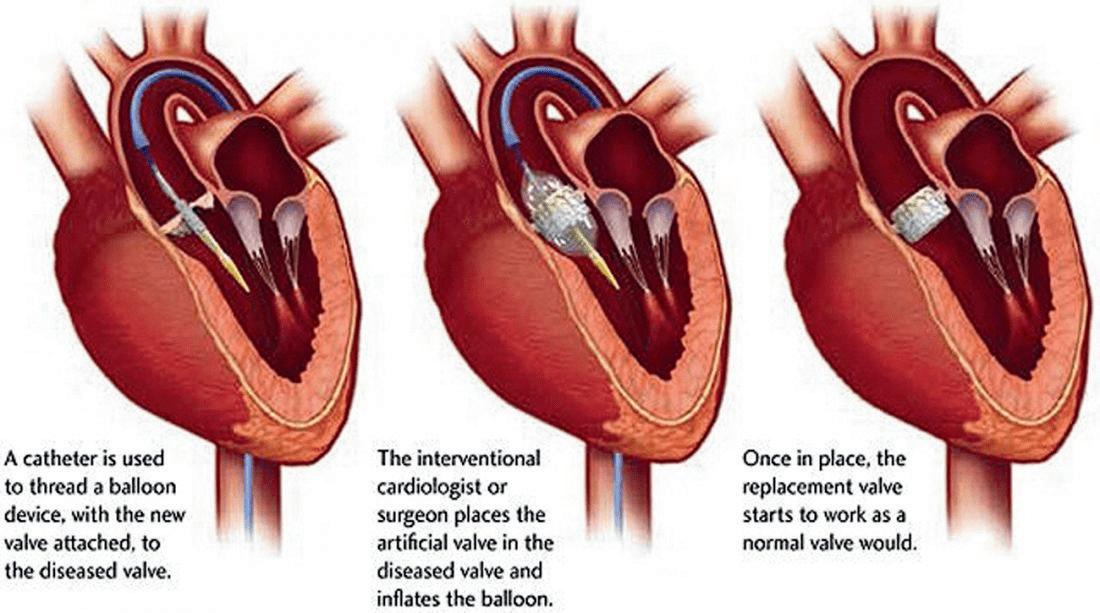
3: Diagram of TAVR
It is not only technology related advancements which encourage optimistic thinking in cardiothoracic surgery and in the treatment of CVD. Novel treatments such as transcatheter aortic valve replacement (TAVR) demonstrate the evolution of care to maximise quality of life and considerrisksforolderpatientsas well. TAVR is another example of minimallyinvasivesurgeryusedto treat aortic stenosis(stiffening of the aortic valve - a cardiovascular disease) which entails the insertion of a new aortic valve using a catheter inserted via the femoral artery or via a small chest incision. This technique grossly reduced surgery time by up to 4 hours and reduced recovery time. Innovation and development on alreadyexistingproceduresshows promise in the future for the resolution of CVD at lightning speeds, saving millions of lives everyyear.
Even within this procedure, there is constant improvement happening every year, with the upgrade of both the valves and the delivery systems. A prime example of this adaptation is the addition of the fabric skirting to the valves to prevent paravalvular leak, which subsequently decreases postoperative morbidity. An issue was found, understood and resolved - a golden cycle of improvement which will be the driving force of care in our future. If this cannot foster hope for a healthier future,thenthereisnothingelsewhichcan.
CVD is a rising global challenge, and with the increased frequency of obesity, fatty foods and multinational corporations promoting them, it is an irrefutable problem of the future. However, with the rate of improvement with surgical solutions for different cardiovascular diseases, it seems to me that this type of long term thinking and advancement in surgery can always find credible solutions and save lives without doubt. In this process, there are also the desirable byproducts of decreased pain, surgery length and recovery time.These display a bright future in global health andhencefosteroptimism.
Fig

TheHeartof Healing:A CloserLookat StatinsAsA Treatmentfor Cardiovascular Disease
Alex GloverBreakthroughs in medical treatments provide hope and victory in the constant fight we have against cardiovascular disease (CVD). The effects of poor lifestyle choices can be reversed through modern treatments and technology - presciptions and medications combat the damage of smoking and alcohol and a lack of exercise no longer leads to irreversible harm to arteries and the heart. In this section I will explain one of the leading treatments of CVD - statins - and the array of ways they help to reduce cholesterollevels.
The build up of fatty acids and cholesterol in arteries (plaque) can be inherited but is also due to the consumption of too much salt and saturated fat, and makes blood vessels narrow and harden, a condition known as atherosclerosis. This reduces the diameter of the lumen of arteries, meaning the oxygen demand of the heart cannot be met due to decreased blood flow. The combination of plaque and the extra water absorbed back into the blood during selective reabsorbtion in the kidneys also increases blood pressure, making deposits prone to suddenlybreakandformaclot.

It is clear that preventing cholesterol formation can dramatically reduce one’s chances of aquiring CVD, therefore various drugs have been developed. First, it may be useful to identify the two main types of cholesterol; low-density lipoprotein cholesterol (LDL) and high-density lipoprotein cholesterol (HDL). LDL is what is known as “bad” cholesterol (because it increases one’s chances of CVDandstrokes),andmakeupmostof the choleterol in your body. HDL absorbs cholesterol and carries it back to the liver, where it is either broken down or excreted, which gives it the nameof“good”cholesterol.
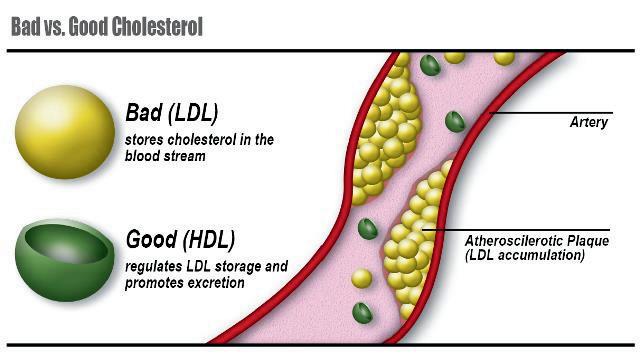 Fig 5: LDL and HDL in an Artery
Fig 4: Statin Prescription
Fig 5: LDL and HDL in an Artery
Fig 4: Statin Prescription
Statins (HMG-CoA reductase inhibitors) reduce the rate of LDL cholesterol production in the liver by blocking an enzyme called HMG-CoA-Reductase. HMGCoA stands for 3-hydroxy-3-methylglutaryl coenzyme A. This results in an upregulation (increase in number) of LDL receptors in the liver, meaning more LDL is taken up from the blood by the liver, leading to low plasma LDL levels. This process can lower LDL cholesterol levels by as much as 55%. Sometimes, if statin treatment alone is not sufficient, ezetimibe may be prescribed as well. Ezetimibe lowersLDLcholesterollevelsbyabout20% by inhibiting the absorption of cholesterol to the liver, leading to a decrease in the amount of cholesterol here, resulting in an up-regulationofLDLreceptors.
Also, statins can sometimes slightly increase HDL cholesterol levels. HDL is mainlycomposedofcholesterylesters(CE) and triglycerides (TG). Cholesteryl ester transfer proteins (CETP) transfer CE from HDL in exchange for TG. It is thought that statins reduce the rate of this transfer, meaning HDL is not modified and fewer chlolersteryl esters are released (which could then accumulate in cells). This is another way that the risk of atherosclerosis and CVD is reduced. However, evidence remainslimited.
Lastly, statins have been shown to decreasethromboplastinlevels(anenzyme releasedwhenbloodvesselsaredamaged) in the blood, meaning less prothrombin is converted to thrombin and therefore less fibrinogen is converted to fibrin to form a clot. Therefore statins significantly downregulate the blood coagulation cascade,meaningone’schancesofhaving CVD or a stroke, for example, reduce greatly. This is what gives statins the nickname“bloodthinners”.
However, statins come with side effects. Headaches, dizziness, feeling sick, tired and physically weak, muscle pains, sleeping problems, digestive system problems and having a low blood platelet count are common side effects. More rarely, statins can cause hair loss, memory problems, pins and needles, inflammation oftheliver&pancreasandskinproblems.
Despite having various side effects attached to them, statins remain a highly effectivetreatmentinreducingone’sriskof CVD. They lower LDL cholesterol levels, sometimes increase HDL cholesterol levels and decrease a person’s chances of a blood clot. It is clear that these advantages significantly outweigh the drawbacks, which leads me to believe that this form of treatment will continue to be used for the foreseeablefuture.
 Fig 6 (above): Skeletal Formula of HMG-CoA Reductase and Fig 7 (right): The Coagulation Cascade
Fig 6 (above): Skeletal Formula of HMG-CoA Reductase and Fig 7 (right): The Coagulation Cascade
RecentAdvancesin 3DPrintingin Cardiovascular Devices
Anthony UnugbokeIntroduction.
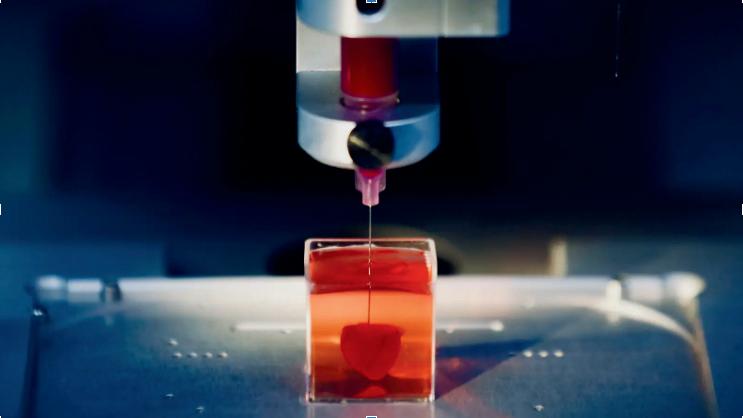
In recent years 3D printing has rapidly developed as a useful process, serving a numerous range of both medical and nonmedical purposes in industry. A particularly promising development is the medical capacityfor3Dprintingtobeusedintreatment of patients with cardiovascular disease. It is abletointegratethetechnologiesofcomputeraided design and material processing to construct different structures. Due to the complexity of cardiovascular structure and the uniqueness of different cardiovascular diseases, the application of 3D printing can open up a new way for the diagnosis and treatment of complex cardiovascular diseases. This development is especially hopeful as it servesasabridgebetweentraditionalmedical imaging,anatomyandmedicaldevices.
The need for personalised treatment of CVD.
The familiar, traditional methods of treating CVD includes the application of cardiovascular medical devices (vascular grafts, stents etc). However the size of devices prepared by traditional preparation technology is limited. It cannot accurately match the unique lesion (injury) environment and organ size of each patient. Additionally many postoperativecomplicationshavebeenassociatedwiththe usage of these cardiovascular devices. For example, the materials currently used in vascular grafts have poor blood compatibility which can lead to platelet adhesion - this resultsinthenarrowingofthevascularlumenwhichcauses strokes. These unavoidable complications have led to ineffective treatments or surgical failure with many of these traditionally manufactured devices. This overbearing issue naturally spurred an innovative response among medical researchers with regards to the individual designs of cardiovascular devices, culminating in the advent of 3D printing technology that has enabled personalised treatment. Therefore, the combination of 3D printing technology with medical imaging technology and anatomy is crucial for the precision medicine of cardiovascular diseases.
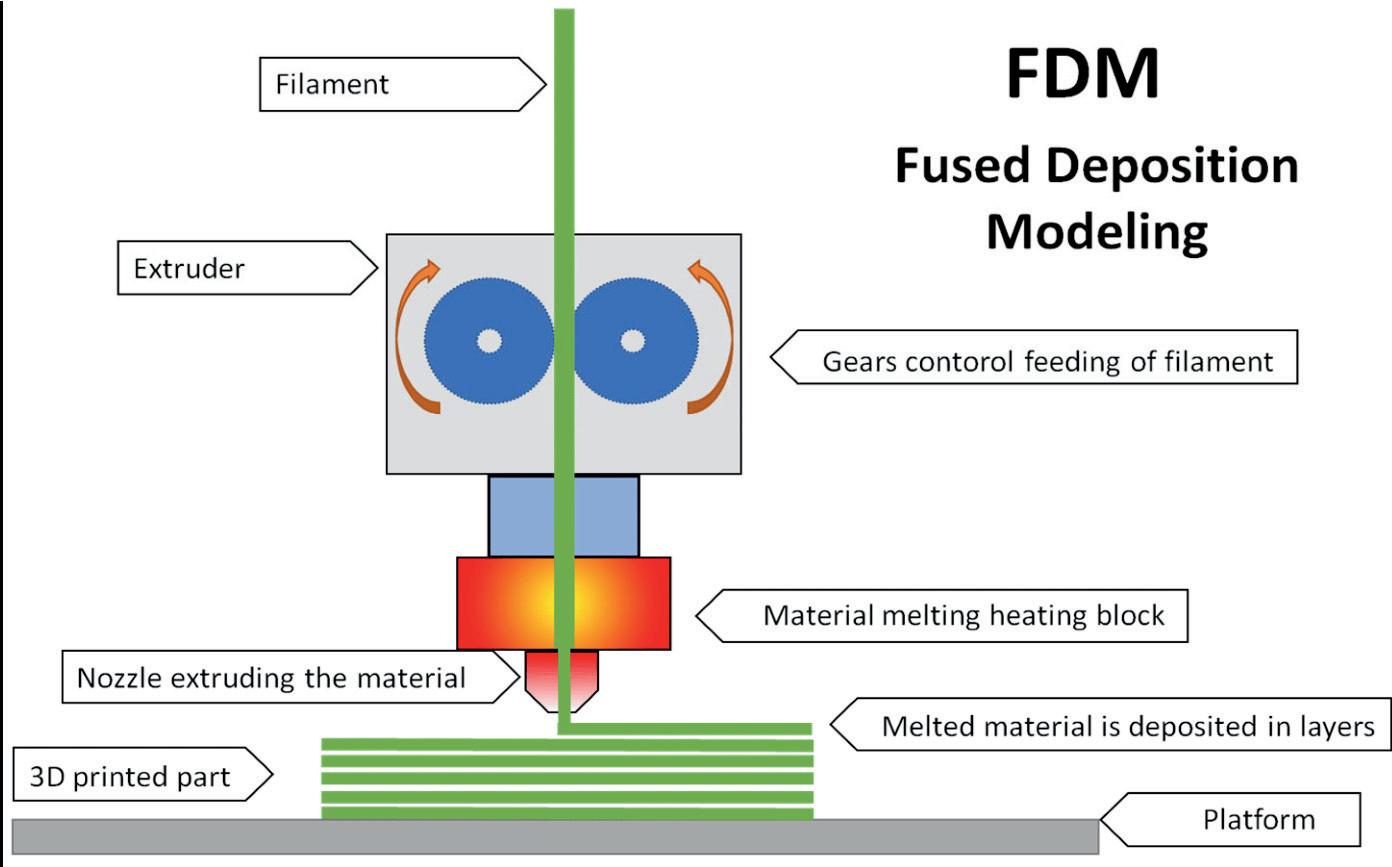
There are many methods available for the 3D printing of cardiovascular devices. I will touch upon the process of Fused-Deposition Modelling, as its essence is very simple to grasp.
Fused Deposition Modelling (FDM) uses a thermo-melting material as a moulding material to construct the model. Under the control of the computer program, the extrusion nozzle moves according to the pre-set trajectory.
The thermo-melting material is heated in the sprinkler so that its temperature is slightly above the melting point.
The melt is extruded from the nozzle to complete the deposition of a single layer.
After the material is extruded from the nozzle, the temperature drops and begins to solidify. Above this layer, the nozzle quickly deposits the next layer, and the latter layer fuses with the previous layer.
After this repeated stacking of layers, the three-dimensional printing is completed according to the pre-set graphics.
Currentapplicationfor3Dprintingcardiovasculardevices.
A clear example of how 3D printing can improve the manufacture of already existing cardiovascular devices is apparent in the 3D printing of vascular stents. Vascular stents are a cardiovascular device which can support the narrowed blood vessels and resume bloodstream. As aforementioned the stent sizes currently used in clinics are limited and non-specific to patients. 3D printed stents can be individually designed according to the patient's specific lesion environment and vessel size, so as to achieve the purpose of precision medicine. Moreover, various complex structures of vascular stents can now be prepared via this method allowing for adaptability to different diseases & injuries.
Futureprospectsfor3Dprintingcardiovasculardevices.
Despite the great progress of 3D printed devices in the treatment of cardiovascular diseases, 3D printing also has inherent limitations associated with cardiovascular applications. I believe there are two main reasons we have clearly not seen the mass popularisation of 3D printing techniques in manufacturing cardiovascular devices and hence are still relying on traditional methods.
1.
Due to the unique mechanical and biological properties of cardiovascular tissues, only a limited variety of materials can be applied via 3D printing techniques.
2.
Due to the necessary high demand of the biosafety, sterility and storage of cardiovascular devices, clinical translation will remain to be a severe challenge. The challenge is exemplified due to the complexity in structure of 3D printed devices.
Based on the previously mentioned limitations, further effort clearly needs to be devoted to develop novel printable materials, which fit for various cardiovascular applications. With emerging advanced biomaterials and various new strategies for 3D printing technology, I strongly believe that 3D printed cardiovascular devices with high precision and high personality will be developed in the future.
History,Advancesand Challenges onHeartTransplantation
PAGE10
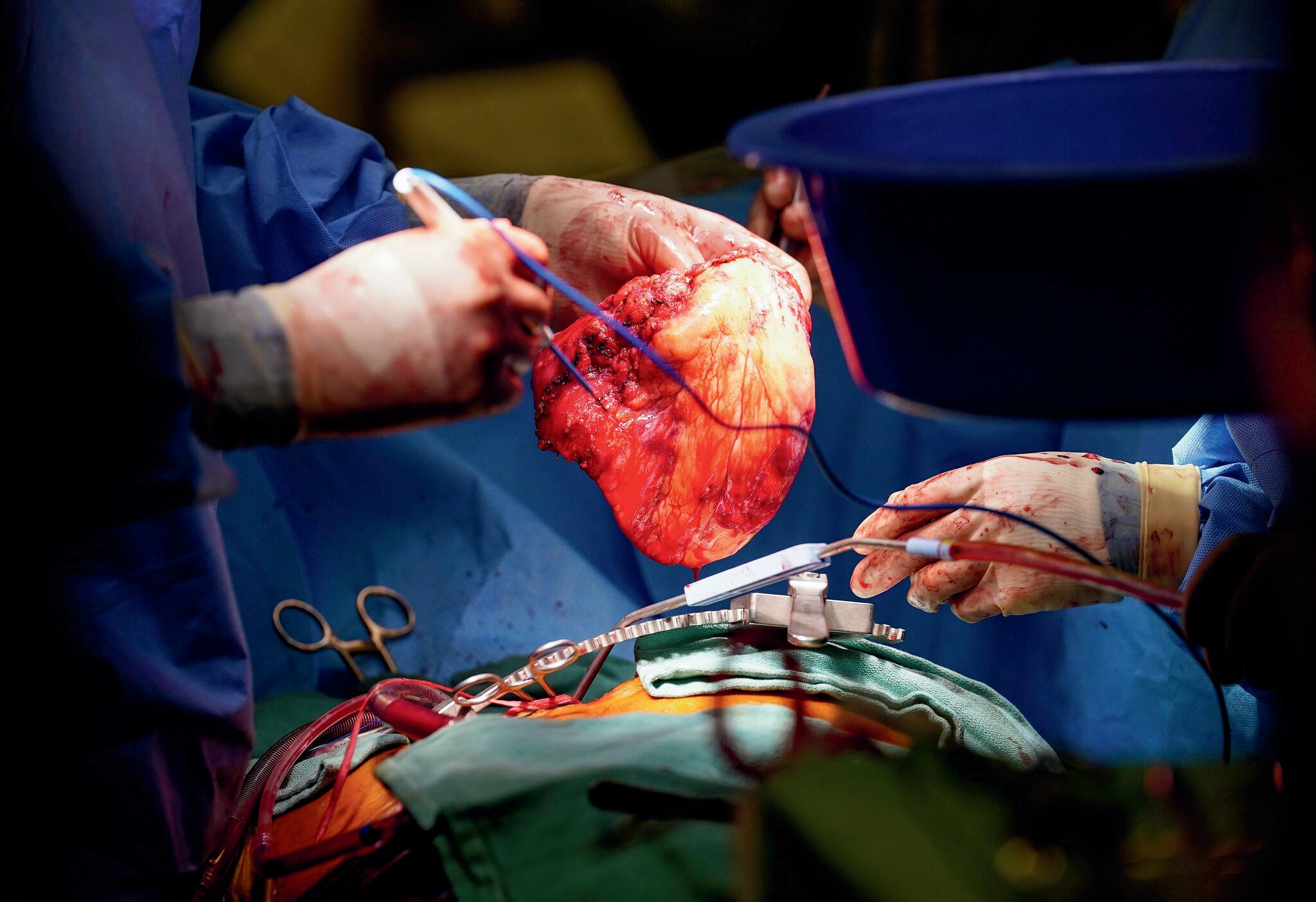
Since the first successful heart transplantation in 1967, Louis Washkansky who was 53 years old when he was dealing with heart failure, in recent years, there has been many significant advancements however, there has been a continuation of challenges that we still deal with today. In 1954, Kidneys became the first organ to be successfully transplanted, followed by pancreas and liver transplants .
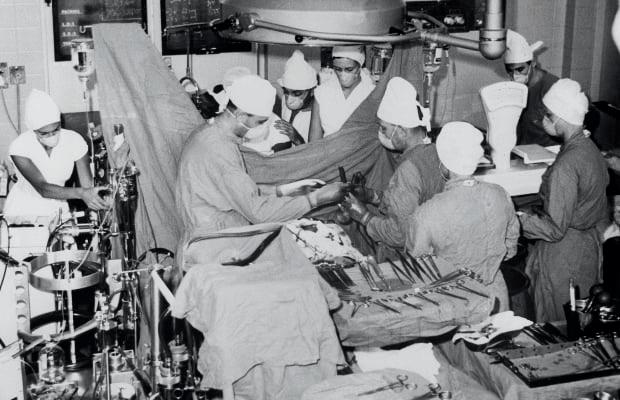
In the late 1970s to 80s, surgeons Terence English and Magdi Yacoub assisted with the first transplant in the UK on Keith Castle, a patient that was known as the ‘great survivor’ . The BHFfunded Heart Transplant Research Group, established by Sir Terrence had a huge impact
on many lives by making the heart transplant a procedure which allows lives of patients to be extended by 10 years. Image on the right was the press conference after the first UK heart transplant in 1968. There still seemed to be ongoing challenges that they were dealing at the time. One of the major problems was the shortage of donor organs since there was a decrease in people who were dying in particular circumstances that their organs were suitable for the procedure and were in good conditions. Furthermore, with more advances in surgical techniques there have been more adapted and overall better methods such as organ preservation, being able to use the tissue type for matching as well as further advances to reducing the likelihood of infections through the intake of antibiotics. Also, having the ability to remove heart from brain dead donors whilst they are on ventilators so that they are in better conditions for heart transplant operations
 Sivaharishan Sivakanthan
Sivaharishan Sivakanthan

on many lives by making the heart transplant a procedure which allows lives of patients to be extended by 10 years. In recent years there has been rapid-evolving technology that has enabled for more heart transplants. In 2022, there was a 95% increase in the number of transplants of machine perfused hearts - machine perfusion is a technique for organ transplantation and in this case hearts were preserved in purpose for it to be transplantation and were preserved in certain conditions. One of the main areas focus for the nation and as part of the UNOS-led collaborative project was the recovery of DCD (donation after circulatory death) donors. Throughout the course, 75% contributed to the overall increase DCD donors and DCD organs transplanted. The report from the NASEM, National Academies of Sciences, Engineering and Medicine recommended that the approach of collaborative work and embracing innovative was significant to the role of maximising organ use and DCD organs.
Important Statistics about Heart Transplants:
In 2022, 42,77 organs transplants were performed in the US with an increase of 3.7% over 2021
Heart transplants increased overall by 21.5% (4,169 in 2022)
DBD heart transplants increased by 4.6% (3,822 in 2022)
DCD heart transplants increased by 68% which was 347 in 2022
The new ‘heart in a box’ perfusion system is one of the many new advances of heart transplants. This is where a donated heart after circulatory death (when the heart is no longer beating) is resuscitated and placed in a portable box which ensures that the heart is warm and metabolically active, according to experts say that it extends the window of transport for up to 12 hours. This has been a huge development from when there was a four hour window and different conditions.
PCSK9Inhibitors
An alternative to Statins?
Ayaan Raza
Earlier in the magazine, we dived into statins, a revolutionary treatment for cardiovascular disease and lowering cholesterol levels. In this section of the magazine we will be looking at PCSK9 inhibitors, answering the question, are these the new alternatives to statins?
What are PCSK9 Inhibitors and what do they do? They are a monoclonal antibody that regulate the number of LDL receptors (primarily located in the liver) you have, and hence reduces the amount of LDL-C (low-density lipoprotein cholesterol) produced, the “bad cholesterol” as previously mentioned. This is important as high LDL Cholesterol levels, levels of which should be below 100 mg/dL, result in increased risk of stroke and heart disease. They work by inhibiting the production of PCSK9 (Proprotein convertase subtilisin/kexin type 9), with increased activity of this protein being associated with high LDL-C levels. This key link between the PCSK9 protein activity and LDL-C levels, led to the development of PCSK9 inhibitors

The monoclonal antibodies against PCSK9 (alirocumab,evolocumab),whichareusedas a treatment for hyperlipidemia, lowered cholesterol levels and the incidence of cardiovasculardiseases.
Hyperlipidemia is one of the most prevalent risk factors of cardiovascular disease (CVD), simply defined as elevated concentrationsoflipidsorfatsintheblood.
However surely statins as previously stated do the same job so why would we use PCSK9 Inhibitors? Many patients may already be on maximally-tolerated statin or ezetimibe (another medicine used in addition to statins useful in lowering cholesterol levels) doses yet have not achieved their cholesterol targets, or may be intolerant to statins and ezetimibe. Patients may also take PCSK9 Inhibitors if they have heterozygous Familial Hypercholesterolaemia (FH), an inherited condition caused by genetic mutation, making your liver less able to remove LDL-C from the blood and hence with higher levels of LDL-C increased risk of heart disease.
There are currently two types of PCSK9 inhibitors commercially available with more in development, Evolocumab (Repatha) and Alirocumab (Praluent) , the only two currently FDA approved. Both of the PCSK9 inhibitors are taken through injection every two to four weeks, followed by blood tests every few months to monitor how well the medication is working and changes in cholesterol levels. For some people PCSK9 inhibitors can be highly effective, research showing it can reduce LDL-C levels by 45-70%. However there are some side effects, most commonly flu like symptoms cold, nausea, as well as muscle pain, fatigue and swelling/itchiness near the injection site. Less commonly, use of PCSK9 Inhibitors may result in kidney and liver problems. Patients with severe kidney and liver will also require adjusted doses. Overall, patients tolerate PCSK9 Inhibitors well.
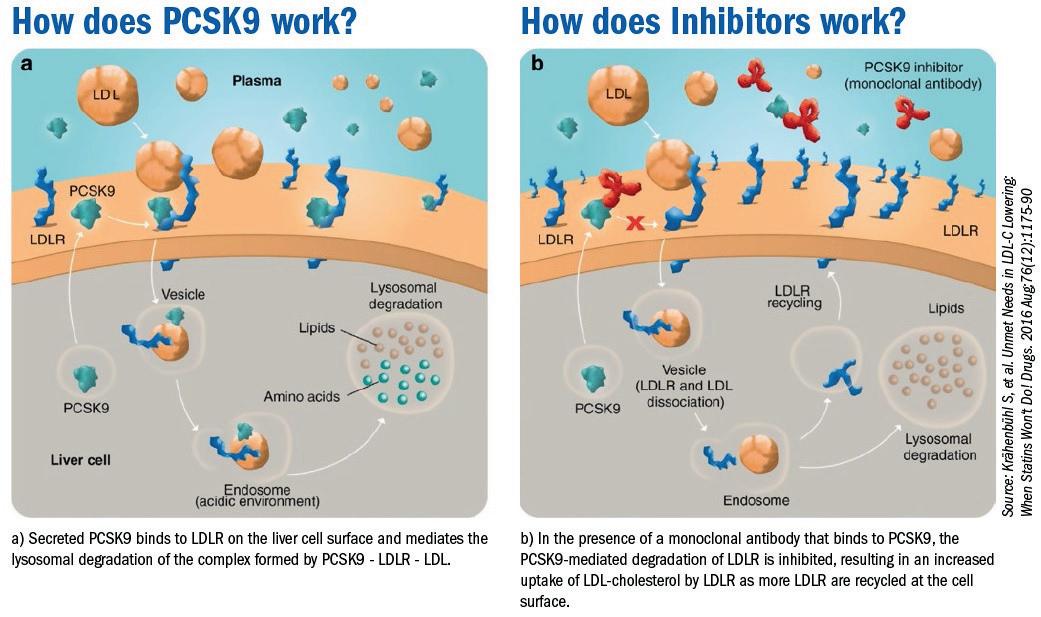
How do PCSK9 Inhibitors actually work? On the outside of the liver cells are LDL receptors which attach to LDL cholesterol as it passes by in the blood. The LDL receptor then takes the cholesterol out of the blood and into the liver to be broken down. Therefore, the more LDL receptors we have the easier it is to keep our LDL blood cholesterol level down. The PCSK9 protein however breaks down the LDL receptors resulting in lower LDL receptor numbers as blood cholesterol levels rise. Therefore PCSK9 Inhibitors stop the protein from working meaning we have more LDL receptors, allowing for more LDL-C to be broken down resulting in decreased LDL cholesterol levels.
Fig 9: Mechanism of PCSK9 and InhibitorsTheTragicFinancialState ofTheNHS: WhatIsTheProblem?
An economic commentary, aside from the main theme about the economic situation of the NHS
Hrishik Subramani
NHS funding is a fairly well discussed topic of contention; it is widely acknowledged that the NHS isn’t getting the money it needs, nor is it getting the right amount of attention and aid it warrants as a pillar of our British society. But how bad is the crisis, and what are the main problems?
The NHS is a vital pillar of British society and stands as one of our most indispensable public services. Being tied to the state, and state funded, a decline in the economy of Britain constitutes insurmountable challenges for the NHS, especially for those who are unable to afford private healthcare.
Currently, the NHS’ money comes from taxation and from National Insurance Contributions as well a small portion from charges for services such as prescriptions and somedentaltreatments,gainingthe entirety of its budget from the Department of Health and Social Care’s budget – which had £155.1 billion for the NHS in 2022/23. There is a growing issue surrounding the funding increase peryear.

Although there has been a noticeable funding increase every year(a vitality considering soaring inflation), the percentage increase per year in the last decade (2010’s) has become less than a third of the average increase in the 2000s- being on average only around 1.7 % per year. This trend of decreasing increases in spending helped to grow a crisis where capacity could not grow in accordance with demand for services. In a country which has an aging and growing populace and where new more expensive treatments rise as preferred options of care, this deficit of funding brews an extraordinary and catastrophic increase in waiting times in A&E, for electives and even for referrals to other clinics. Just to amend these tremendous backlogs, vast sums of money would need to be provided. To start to fix the backlog of electives which could be up to 15 million patients by the end of 2025 would cost £2bn on its own, being in itself a huge logistical operation.
In addition to this, the strikes which have taken course throughout this year, as well as the rising inflation could see the NHS overspending by £7bn in 2024. Just as in previous years the budget has been more of a guideline than an ultimatum due to the essential requirement of certain equipment in a hospital, which save lives and cannot be cut (£87.4>£85.3bn in the fiscal year of 2018/19). Fostered by unfeasible and unrealistic assumptions about the requirements of the NHS, cuts in financial expenditure have to be made and the backlog builds up, leading to more than 23,000 excess deaths in England in A&E.
It is clear to see that the woeful state of the NHS financially is a matter that needs to be addressed urgently. Although I am able to acknowledge the myriad of financial issues which the country is facing due to inflation, strikes, unemployment etc. and the difficulties surrounding managing these, I feel it is the responsibility of the government to take ownership of this issue and take drastic steps to mend it (more than is currently being done), to keep the NHS, as Aneurin Bevan so rightly put, ‘as a testament to the value we place on human life’ rather than a shortcoming of the country, with nothing to show but corridors full of full beds.
Please note that this article is also available on the Studenomics.co.uk website, but is still written in its entirety by the author listed above.

Opinion:
Students have their say
What is your opinion on the use of cannabis internationally for analgesia?
Ibelievethatcannabisshouldbelegalisedin caseswherepatientsfaceseverepain,asthe outweigheddrawbackofwrongfulprescriptionsisbythehugebenefititwillprovide ofalleviatingpainforthosewhoundergothe mostsuffering.
~ManasTannan


Ibelievethekeyiseducationand consent.Similartosmoking,adults shouldbetoldaboutthesideeffectsand othernegativeexternalitiesthatcome fromtheuseofcannabis,andfromthis theyshouldbefreetoauthorisetheuseof cannabisinemergencies.Indoingso,the autonomyofeachindividualhavebeen respected,witheachperson understandingthepotentialrisksthat comewiththepracticeStudiesby Harvarduniversityhaveshownthat placebosarejustaseffectiveascannabis, whichasksthequestionofwhetherthe drugtrulyisworthimplementingintothe medicalindustry.
~AnonymousYear12.
Whilecannabishasitsbenefitsin providinganalgesiaandrelievingpain causedbyseverediseases,the downsidesarefarmoresignificant.Evenif cannabisweretobelegallyprescribed,it wouldbechallengingtodetectallthe blackmarketsthatwouldarisefromsuch anaction,withmedsbeingsoldtoaddicts.
~ GauravBohra

Cannabisisanaddictivedrug,andIfeel apartthatitshouldhavenoplaceinsociety doctors.fromasamedicine,prescribedby However,ifthepublichas accesstoalcohol,theyshouldalsohave accesstoasmallamountofcannabis.
~NiruktAgrawal

Iwouldnotsupportthe internationaluseasmore formalusesofanalgesianeed tobepromoted/provided ratherthanwhatwouldhave beenillegal.
~ JosephAlolawalobaBibliography
All images not referenced below are from Canva, rights go to the respective creators on Canva.
Article One: Surgical treatments of CVD:
1.
The Future of Cardiovascular Surgery | Circulation - AHA/ASA Journals. Available at: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.116.023545(Accessed:15October2023).
2.
New trends in cardiac surgery: Toward a less-invasive surgical ... Available at: https://www.jtcvs.org/article/S00225223(18)33436-6/fulltext(Accessed:15October2023).
NHSchoices.Availableat:https://www.nhs.uk/conditions/coronary-heart-disease/treatment/(Accessed:15October 2023)3.
4.
Top ten public health challenges to track in 2022 - Wiley Online Library. Available at: https://onlinelibrary.wiley.com/doi/full/10.1002/puh2.21(Accessed:15October2023).
5.
Cardiovascular diseases (no date) World Health Organization. Available at: https://www.who.int/healthtopics/cardiovascular-diseases#tab=tab_1(Accessed:15October2023).
6.
Damiano, R.J. (2012) Moderncardiothoracicsurgery:Currentstate-of-the-art&emergingtechnologies, Missourimedicine. Availableat:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6179775/(Accessed:15October2023).
7. Percutaneous transluminal coronary angioplasty (PTCA) - health video: Medlineplus medical encyclopedia (no date) MedlinePlus.Availableat:https://medlineplus.gov/ency/anatomyvideos/000096.htm(Accessed:15October2023).
Neely RC;Leacche M;Byrne CR;Norman AV;Byrne JG; (no date) New Approaches to Cardiovascular Surgery, Current problemsincardiology.Availableat:https://pubmed.ncbi.nlm.nih.gov/25498978/(Accessed:15October2023).
8. Transcatheter Aortic Valve Replacement (TAVR) (2023) Mayo Clinic. Available at: https://www.mayoclinic.org/testsprocedures/transcatheter-aortic-valve-replacement/about/pac20384698#:~:text=Transcatheter%20aortic%20valve%20replacement%20(TAVR)%20is%20a%20minimally%20invasive%2 0procedure,guide%20it%20to%20the%20heart.(Accessed:15October2023).
10.
9. Writer, A.C. (no date) 11globalhealthissuestowatchin2023,accordingtoIHMEexperts, TheInstituteforHealthMetrics and Evaluation. Available at: https://www.healthdata.org/news-events/insights-blog/acting-data/11-global-health-issueswatch-2023-according-ihme-experts(Accessed:15October2023).
11.
Figure 1: MyHeart. (2016). Heart Bypass Surgery Explained In Incredible Pictures • MyHeart. [online] Available at: https://myheart.net/articles/heart-bypass-surgery-explained-in-incredible-pictures/.
12.
Figure2:Hospitals,M.(n.d.).CoronaryAngioplasty(PTCA),Balloonprocedure&stentplacement.[online]BestHospitalsin India | Medicover Hospitals. Available at: https://www.medicoverhospitals.in/procedures/coronary-angioplasty-and-stentsinsertion/[Accessed3Mar.2024].
13.
Figure3:www.wakemed.org.(n.d.).TAVR,WakeMedHealth&Hospitals,Raleigh&WakeCounty,NC.[online]Availableat: https://www.wakemed.org/care-and-services/heart-vascular-care/cardiovascular-surgery/valve-conditions/tavr.
Article Two: Medical Treatments of CVD: www.heartuk.org.uk. (n.d.). Statins. [online] Available at: https://www.heartuk.org.uk/gettingtreatment/statins#:~:text=Statins%20slow%20down%20LDL%2Dcholesterol.(Accessed02/03/24).
1.
2. Feingold, K.R. and Grunfeld, C. (2018). Cholesterol Lowering Drugs. [online] Nih.gov. Available at: https://www.ncbi.nlm.nih.gov/books/NBK395573/.
4.
Centers for Disease Control and Prevention (2017). LDL & HDL: Good & Bad Cholesterol. [online] Centers for Disease ControlandPrevention.Availableat:https://www.cdc.gov/cholesterol/ldl_hdl.htm.(Accessed02/03/24)
3. Pirahanchi, Y., Sinawe, H. and Dimri, M. (2020). Biochemistry, LDL Cholesterol. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK519561/#:~:text=LDL%20receptors%20on%20the%20liver.
6.
5. McTaggart, F. and Jones, P. (2008). Effects of Statins on High-Density Lipoproteins: A Potential Contribution to Cardiovascular Benefit. Cardiovascular Drugs and Therapy, 22(4), pp.321–338. doi:https://doi.org/10.1007/s10557-0086113-z.
7.
Undas, A., Brummel-Ziedins, K.E. and Mann, K.G. (2005). Statins and Blood Coagulation. Arteriosclerosis, Thrombosis, and VascularBiology,[online]25(2),pp.287–294.doi:https://doi.org/10.1161/01.atv.0000151647.14923.ec.
8.
www.sciencedirect.com. (n.d.). Cholesterol Ester Transfer Protein - an overview | ScienceDirect Topics. [online] Available at:
https://www.sciencedirect.com/topics/neuroscience/cholesterol-ester-transferprotein#:~:text=CETP%20transfers%20CE%20from%20HDL[Accessed3Mar.2024]
Figure 5 :Disabled World. (n.d.). Blood Cholesterol: Management and General Information. [online] Available at: https://www.disabled-world.com/health/cardiovascular/cholesterol/.
9. Figure 6 : NEUROtiker, F.I.A. svg by (2007). Skeletal formula of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA). Edited using Inkscape. [online] Wikimedia Commons. Available at: https://commons.wikimedia.org/wiki/File:HMG_coenzyme_A.svg [Accessed 3 Mar. 2024].
10. Figure 7 :Anon, (2019). Coagulation | Theory & Clotting | A Level Biology Revision. [online] Available at: https://alevelbiology.co.uk/notes/coagulation/.
ARTICLETHREE:3DPRINTINGANDCVD
1.
2.
THIRIET, M., DELFOUR, M., GARON, A. (2015). VASCULAR STENOSIS: AN INTRODUCTION. IN: LANZER, P. (EDS) PANVASCULAR MEDICINE. SPRINGER, BERLIN, HEIDELBERG. HTTPS://DOI.ORG/10.1007/978-3-642-37078-6_32
V. DHINAKARAN, K.P. MANOJ KUMAR, P.M. BUPATHI RAM, M. RAVICHANDRAN, M. VINAYAGAMOORTHY, A REVIEW ON RECENT ADVANCEMENTS IN FUSED DEPOSITION MODELING, MATERIALS TODAY: PROCEEDINGS, VOLUME 27, PART 2, 2020, PAGES 752-756, ISSN 2214-7853, HTTPS://DOI.ORG/10.1016/J.MATPR.2019.12.036.
3.
YIHONG SHEN, JIE CUI, XIAO YU, JIAHUI SONG, PENGFEI CAI, WANXIN GUO, YUE ZHAO, JINGLEI WU, HONGBING GU, BINBIN SUN, XIUMEI MO, RECENT ADVANCES IN THREE-DIMENSIONAL PRINTING IN CARDIOVASCULAR DEVICES: BENCH AND BEDSIDE APPLICATIONS, SMART MATERIALS IN MEDICINE, VOLUME 5, ISSUE 1, 2024, PAGES 36-51, ISSN 2590-1834, HTTPS://DOI.ORG/10.1016/J.SMAIM.2023.07.001. (HTTPS://WWW.SCIENCEDIRECT.COM/SCIENCE/ARTICLE/PII/S2590183423000364)
4.
5.
WWW.SCIENCEDIRECT.COM. (N.D.). MEDICAL DEVICE - AN OVERVIEW | SCIENCEDIRECT TOPICS. [ONLINE] AVAILABLE AT: HTTPS://WWW.SCIENCEDIRECT.COM/TOPICS/MATERIALS-SCIENCE/MEDICAL-DEVICE [ACCESSED 1 MAR. 2024].
FIGURE 8: PRZEKOP, ROBERT E., EWA GABRIEL, DARIA PAKUŁA, AND BOGNA SZTORCH. 2023. "LIQUID FOR FUSED DEPOSITION MODELING TECHNIQUE (L-FDM)—A REVOLUTION IN APPLICATION CHEMICALS TO 3D PRINTING TECHNOLOGY: COLOR AND ELEMENTS" APPLIED SCIENCES 13, NO. 13: 7393. HTTPS://DOI.ORG/10.3390/APP13137393
ARTICLEFOUR: HEARTTRANSPLANT:
CINDY YOUNG (2023). ANOTHER RECORD YEAR FOR HEART TRANSPLANTS: STEEP INCREASES SEEN IN DCD TRANSPLANTS IN 2022. [ONLINE] UNOS. AVAILABLE AT: HTTPS://UNOS.ORG/NEWS/IN-FOCUS/2022-HEART-TRANSPLANTS-STEEP-INCREASES-INTRANSPLANTS-FROM-DCD-DONORS/#:~:TEXT=RAPIDLY%2DEVOLVING%20PERFUSION%20TECHNOLOGY%20IS [ACCESSED 1 MAR. 2024].
1. EWSNETWORK.MAYOCLINIC.ORG/DISCUSSION/HEART-TRANSPLANT-INNOVATION-NEW-HEART-IN-A-BOX-TECHNOLOGY-PROVIDESGIFT-OF-LIFE-TO-ARIZONA-MAN-AS-COUPLE-PREPARES-TO-CELEBRATE-50-YEAR-ANNIVERSARY/#
2. HTTPS://WWW.BHF.ORG.UK/INFORMATIONSUPPORT/HEART-MATTERS-MAGAZINE/MEDICAL/HISTORY-OF-UK-HEART-TRANSPLAN T3.
ARTICLEFIVE:PCSK9INHIBITORS:
1. Kaddoura, R., Orabi, B. and Salam, A. (2020). PCSK9 monoclonal antibodies: An overview. Heart Views, 21(2), p.97. doi:https://doi.org/10.4103/heartviews.heartviews_20_20.
Heartuk.org.uk. (2019). PCSK9 inhibitors Cholesterol Treatment & any side effects. [online] Available at: https://www.heartuk.org.uk/gettingtreatment/pcsk9-inhibitors.
2. Binod Pokhrel and Levine, S.N. (2019). PCSK9 Inhibitors. [online] Nih.gov. Available at: https://www.n cbi.nlm.nih.gov/books/NBK448100/.3. https://my.clevelandclinic.org/health/drugs/22550-p csk9-inhibitors4. Cleveland Clinic. (2022). PCSK9 Inhibitors: How They Manage Cholesterol and Side Effects. [online] Available at: https://my.clevelandclinic.org/health/drugs/22550-pcsk9-inhibitors.an (2021). PCSK9 inhibitors: an alternative to statins? [online] British Heart Foundation. Available at: https://www.bhf.org.uk/for-professionals/healthcare-professionals/blog/2018/pcsk9-inhibitors.
6.
5. www.biovendor.com. (n.d.). PCSK9 and its Inhibitors: A new approach in lipid lowering therapy | BioVendor R&D. [online] Available at: https://www.biovendor.com/pcsk9-and-its-inhibitors-a-new-approach-in-lipid-lowering-therapy.
8.
7. BritishHeartFoundation(n.d.). Familial hypercholesterolaemia (FH). [online] www.bhf.org.uk. Available at: https://www.bhf.org.uk/informationsupport/conditions/familial-hypercholesterolaemia.
CDC (2020). LDL and HDL Cholesterol: ‘Bad’ and ‘Good’ Cholesterol. [online] Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/cholesterol/ldl_hdl.htm#:~:text=LDL%20(low%2Ddensity%20lipoprotein).
9. Hill, M.F. and Bordoni, B. (2023). Hyperlipidemia. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK559182/#:~:text=Hyperlipidemia%2C%20in%20particular%20elevated%20LDL.
11.
Rosenson, R.S., Hegele, R.A., Fazio, S. and Cannon, C.P. (2018). The Evolving Future of PCSK9 Inhibitors. Journal of the American College of Cardiology, [online] 72(3), pp.314–329. doi:https://doi.org/10.1016/j.jacc.2018.04.054.
10. Figure 9: www.biovendor.com. (n.d.). PCSK9 and its Inhibitors: A new approach in lipid lowering therapy | BioVendor R&D. [online] Available at: https://www.biovendor.com/pcsk9-and-its-inhibitors-a-new-approach-in-lipid-lowering-therapy.
Article6:NHSEconomy: Checking the NHS’s reality: the true state of the health service’s finances. Available at: Your paragr aph text.1.
3.
2. Hoddinott, S. (Jan.2023) The NHS crisis – institute for government. Available at: https://www.instituteforgovernment.org.uk/sites/default/files/2023-01/NHS-crisis-does-government-have-a-plan.pdf?ref=health-policyinsight(Accessed: 30 October 2023).
4.
5.
NHS sinks into £7bn cash crisis as inflation and strikes bite (2023) The Guardian. Available at: https://www.theguardian.com/society/2023/sep/17/nhs-sinks-into-7bn-cash-crisis-as-inflation-and-strikes-bitet (Accessed: 30 October 2023)
The NHS budget and how it has changed (2023) The King’s Fund. Available at: https://www.kingsfund.org.uk/projects/nhs-in-a-nutshell/nhsbudget#:~:text=What%20is%20the%20NHS%20budget,as%20staff%20salaries%20and%20medicines. (Accessed: 30 October 2023).
Ford, J. (no date) The NHS is facing a deepening financial crisis – the BMJ. Available at: https://www.bmj.com/bmj/section%20pdf/724776path=/bmj/347/7916/Observations.full.pdf (Accessed: 30 October 2023)