Australian Pain Society Newsletter



Clinical Associate Professor Kylie Bailey
As I write this during National Pain Week, it serves a timely reminder to pause and reflect on the lived experience of chronic pain, and the many challenges faced when navigating life with it. As we all know, it is not only pain that is experienced, but also stigma, social isolation, poor access to appropriate care, and significant financial burden. These barriers make the journey more complex for those living with chronic pain. In this context, our commitment to compassionate, person-centred, and evidencebased care remains imperative. It's a principle I see consistently upheld by the members of the Australian Pain Society (APS) and reflected in our eNewsletter.
Now to the eNewsletter. The APS is celebrating excellence in our professional community and is calling for submissions for The Rising Star and The Distinguished Member awards. If you are a rising star pain researcher, or know someone who has made a considerable contribution (for at least ten years) to the APS and pain research, please consider applying. The APS is also calling for Topical Sessions submissions that are innovative and creative. Travel Grants to attend the Annual Scientific Meeting (ASM) in Adelaide next year are also available, along with a rare opportunity to submit an expression of interest for a preconference workshop prior to the ASM.
The Pain in Childhood Special Interest Group (SIG) journal watch review section provides very interesting summaries of recent paediatric pain publications. They include:
1. The impact of pain on sensory modulation and function
2. The effects of fear of pain on recovery for sports related concussion,
3. A systematic review on psychological pain interventions for children and young people.

Further, the August edition provides two recent publications, one on Motor Proficiency Delay and Chronic Pain in Children, and the other on the Effect of Incentives on Recruiting Limited English with Low Back Pain. Dr Dulce Calado has provided a report on the 2025 Association of Southeast Asian Pain Societies (ASEAPS) congress held in Singapore. There is also information on the Basic Pain Research SIG Pain Hour webinar on objective measurements of pain in rodents.
Finally, the Australian Physiotherapy Association has kindly granted the APS Members access to their InMotion July 2025 edition, called Shifting the Needle on Pain Management. This 13-paged news item collates the highlights of physiotherapy presentations at the APS ASM in Melbourne earlier this year.
We hope you find this edition both informative and supports your work in the pain field.
Until next time, Kylie

Tuesday 2 September 2025
Topical Session Submissions Close
Tuesday 7 October 2025
Rising Star Award Applications Close
Tuesday 28 October 2025
Free Paper/Poster Abstract Submissions Close
Tuesday 18 November 2025
Registrations Open!
APS 2026 will be held from 19 - 22 April 2026 at the Adelaide Convention Centre, SA
Please visit the conference website here: www.dccam.com.au/aps2026
If you have any questions, please contact the APS Conference Secretariat: apsasm@dccam.com.au

Submissions Deadline: Tuesday 2 September 2025
On behalf of the Scientific Program Committee and the Local Organising Committee, we are pleased to advise topical session submissions for APS 2026 are now open.
The deadline for Topical Session submissions is: Tuesday 2 September 2025
We are looking for innovation, so put on your creative thinking caps and think beyond the traditional, formal three speaker format. This is your opportunity to reimagine how we explore topics like pain philosophy, ethics in research and pain, controversial conversations in pain, or go niche by exploring one area from numerous perspectives.
Your session can be a healthy debate, or an in-depth collaborative discussion, or something entirely new. We also encourage sessions to be interactive, such as including an audience poll or awarding prizes.
Proposed symposia that bring together a range of experience levels (early career to senior) and diverse professional expertise will be prioritised.
View the topical session submission guidelines and submit via the conference website.
We look forward to receiving your submissions. Should you have any queries regarding your submission or the process, please contact the Conference Secretariat.

This award showcases rising star pain researchers in Australia. The Rising Star may be awarded annually, subject to the application of suitable candidates.
The Rising Star winner will receive a return domestic airfare, accommodation, and complimentary registration to attend the 46th Annual Scientific Meeting. At the ASM the Rising Star will give a plenary presentation to showcase their work and ideas.
The deadline for Rising Star Award submissions is: Tuesday 7 October 2025
Please click here to view the Rising Star Award Submission Guidelines.
To submit an application, please complete the form online here.
Should you have any queries regarding your submission or the process, please contact the Conference Secretariat: apsasm@dccam.com.au
We look forward to receiving your submission.

Submissions Open Tuesday 1 July 2025
Abstracts will be accepted for Free Communication and Poster presentations. Opportunities to participate in the Rapid Communication Sessions are also available.
The deadline for Abstract submissions is: Tuesday 28 October 2025
Please click here to view the Abstract Submission Guidelines
See below for the three Abstract Submission Portals.
Experimental Studies & Clinical Trials Abstract Guidelines
Clinical Practice & Service Delivery Abstract Guidelines Case Reports Abstract Guidelines
Should you have any queries regarding your submission or the process, please contact the Conference Secretariat: apsasm@dccam.com.au
We look forward to receiving your submission.

The Scientific Program Committee (SPC) and the Local Organising Committee (LOC) invite proposals for a half-day Pre-Conference Workshop for inclusion in the program on Sunday 19 April 2026
We invite APS members to seize this opportunity to present a Pre-Conference Workshop. These 3 hour Workshop slots are rarely available, so don’t miss your chance to contribute to the program. We look forward to receiving your submissions.
To submit your Workshop idea, please download and complete the application form, located on the conference website, and send it to the APS Conference Secretariat via apsasm@dccam.com.au by Monday 1 September 2025
Guidelines
• If accepted, the applicant of the Workshop will be responsible for coordinating all speakers.
• Speakers must be able to present onsite at the Adelaide Convention Centre, SA, on Sunday 19 April. Virtual presentations will not be accepted.
• Workshop speakers will receive complimentary registration for the Workshop only. No further discounted or complimentary registrations to other workshops or the conference are available.
• Further guidelines will be made available to you, if/once your Workshop is accepted.
The accepted Workshop will be included on the APS 2026 conference website, promoted alongside the other six workshops being held on the Sunday, and will be included in the online registration form.

The Board of Directors is seeking nominations from all Australian Pain Society (APS) members for candidates to be considered for the Distinguished Member Award(s). The award will be presented to the recipient at the APS 46th Annual Scientific Meeting (ASM) in Adelaide (19 - 22 April 2026).
Eligibility criteria:
Candidates must be APS members who have had a lengthy career in the field of pain and:
• Made major contribution1 towards the Society, and
• Significantly contributed to the science of pain management, and/or
• Played a significant clinical, educational or research role in the field of Pain Management in Australia
1 Major contributions include, but are not limited to:
• Scientific Program Committee involvement
• Pain research
• APS projects
• Subcommittee involvement
• Board liaison
• Contributions to ASM presentations
Nomination Guidelines:
• A ‘Nomination for Distinguished Member Award’ form must be completed.
• It is desirable that nominees have held continuous APS membership for over 10 years.
• Nominations must include an 800-900 word biography of the nominee. The Board will not consider incomplete nomination forms.
• Unsuccessful nominations are not automatically carried over to subsequent years. A new submission is required for each nomination cycle.
• The nominator must be prepared to present a brief summary of the Distinguished Member biography in the ASM program, or arrange a suitable alternate for the presentation segment.
Submission
• All nominations to be submitted to the APS Secretariat by 31 October 2025.
Notification:
• The APS Board will notify successful nominees by 31 December 2025.
• Distinguished Member recipients are actively encouraged to attend the Annual Scientific Meeting in order to receive their award in person from the APS President.
The nomination form and a listing of past recipients of the Distinguished Member Award, including their biographies, can be found on the APS website.

The Australian Pain Society (APS) is pleased to announce the availability of several Travel Grants for members to present their research at our Annual Scientific Meeting (ASM).
Travel Grants are awarded as follows:
• PhD students (up to the value of $500)
• A single dedicated Travel Grant for a Pain in Childhood (PinC) SIG member ($500)
• A single dedicated Travel Grant for a Basic Pain Research (BPR) SIG member ($500)
• If funds permit, further travel grants may be offered to nurses, allied health professionals, and other post-graduate students.
This Travel Grant program is designed to encourage contribution to, and participation in the ASM, and is made possible through an allocation of a capped pool of APS operating funds.
Full eligibility criteria and Terms and Conditions are available on the Travel Grants webpage.
Professor Michael Cousins AO Travel Grant
In honour of Professor Michael Cousins AO, the APS is pleased to announce a single, dedicated Travel Grant for an Allied Health Practitioner (AHP) member to present their research abstract at our Annual Scientific Meeting (ASM).
The Professor Michael Cousins AO Allied Health Practitioner Travel Grant includes:
• Complimentary ASM registration at the relevant early bird rate
• $500 towards ASM travel and accommodation expenses
To be considered for any Travel Grant:
a. an EOI for a Travel Grant must be indicated when your abstract is submitted; AND
b. a Travel Grant Application form must be submitted to aps@apsoc.org.au by 5pm AEDT on 30 November 2025 – no exceptions.
Yanfei Ban
Yanfei is currently a PhD student at The University of Queensland (UQ). His interests include α-conotoxins as novel non-opioid analgesics for neuropathic pain relief.
Moments at APS 2025
I am sincerely grateful to the Australian Pain Society (APS) for awarding me the Travel Grant, which enabled me to attend the 2025 Annual Scientific Meeting (ASM). As a current PhD student researching novel analgesic drug discovery and their mechanisms of action in neuropathic pain models, this opportunity was invaluable for my academic and professional development.
Receiving the Travel Grant greatly alleviated the financial burden of attending the meeting. It helped cover essential costs, including airfare and accommodation, which would otherwise have made participation challenging. With this support, I was able to fully engage in the conference, present my research, and interact with leaders in the field.
At the meeting, I presented my preclinical research on the precise mechanisms of pain relief provided by α-conotoxins, which target GABAB and α9α10 nicotinic acetylcholine receptors. Although my work was accepted as a poster, I was also given the opportunity to deliver a short oral presentation at the Basic Pain Research (BPR) Special Interest Group (SIG) pre-conference workshop (PCW). This was an unexpected but extremely valuable opportunity to showcase my findings to a broader audience. Several researchers expressed interest in my project, and we had insightful discussions on the challenges associated with investigating such mechanisms in complex pain models. These conversations were not only intellectually stimulating but also inspiring.
This was my first time attending an APS scientific meeting, and I found the experience exceptional. APS demonstrated outstanding organisational proficiency and responsiveness. The events were well co-ordinated, and the conference team was consistently supportive, providing quick responses to queries and offering helpful guidance. I was particularly impressed by the collaborative and welcoming atmosphere throughout the meeting.
One of the most memorable aspects of the ASM was meeting a fellow researcher whose work closely aligns with mine. We exchanged ideas about experimental design and methodologies, and our discussion extended to broader issues in neuropathic pain research. This exchange has left a lasting impression and opened the door for future intellectual collaboration.
I was also fortunate to connect with a potential collaborator with expertise in electrophysiology. As my research currently focuses on in vivo pharmacology, this connection could be instrumental in helping me further interpret and validate my findings through electrophysiological techniques.
Among the many excellent sessions, my favourite was the BPR SIG PCW. It provided a rich overview of neuropathic pain mechanisms, with a particularly engaging discussion on immuneneural crosstalk in chronic constriction injury models. The insights I gained from this workshop will undoubtedly influence my future work.
Looking ahead, I am excited about the prospect of returning to the APS ASM next year. I hope to continue building on the momentum from this year and aim to deliver a full oral presentation. Participating in APS has been a pivotal experience in my journey as a young researcher, and I am thankful for the support and opportunities it has provided.
Declaration: I would like to express my sincere thanks to my advisory team—Emeritus Professor Maree Smith, Associate Professor Richard Clark, and Dr Andy Kuo—for their invaluable support and guidance. I am also grateful to Dr Orada Sriwatananukulkit and Dr Xiaosa Wu for their generous assistance throughout the project. I am supported by an international PhD scholarship from UQ. Funding for this study was provided by the NHMRC. The Centre for Integrated Preclinical Drug Development (CIPDD) is financially supported by National Collaborative Research Infrastructure Strategy (NCRIS) funding awarded by Therapeutic Innovation Australia, along with co-investment funds from UQ and the Queensland Government.
Martjie Venter
Martjie is a PhD candidate in the Centre for Pain IMPACT at Neuroscience Research Australia and the University of New South Wales. Her research focuses on the translation of evidence-based treatments for chronic low back pain, from research to clinical practice.
Reflections from APS 2025 in Melbourne
I am very grateful to the Australian Pain Society (APS) for awarding me a Travel Grant to attend this year’s Annual Scientific Meeting (ASM) in Melbourne. The grant covered the cost of getting to and from the conference which made the trip much more accessible for me as a PhD student. Without that support, attending would have been a lot more difficult, so I truly appreciate the opportunity.
At the conference, I presented some of my work using mediation analysis to help optimise the RESOLVE intervention for chronic low back pain in real-world clinical settings.
RESOLVE provided participants with non-drug strategies, such as mental movement, physical movement and sensory training. My aim is to better understand how the intervention works so that it is easier to implement. The presentation seemed to be well received, it was great to have conversations with researchers and clinicians who were interested in how this kind of analysis can inform practical decisions. It was encouraging to see others engaged and thinking about how they can apply this method in their own contexts.
This was my second APS meeting, I also attended the 2023 conference in Canberra. Both have been excellent in their own ways. What really stood out to me about the ASM, especially when compared to other conferences I have been to, is the strong sense of community. There is something special about the way clinicians, researchers and industry partners come together with a shared focus on improving outcomes for people living with pain. It does not feel siloed, people are approachable, conversations feel genuine and there is a real spirit of collaboration.

That atmosphere makes it so much easier to connect and share ideas. The gala dinner was also a highlight; it was a fun and relaxed way to catch up with colleagues and revealed some impressive dance moves from the pain community!
One of the highlights for me this year was meeting some of my collaborators from the University of South Australia in person. Remote work is so useful but being able to chat faceto-face was much better. We had some great conversations about future directions, so I am excited to keep building on that collaboration.
There were plenty of standout sessions, but one that really stood out to me was the workshop on Gabapentinoids. It covered some of the growing concerns around the use of these medications for low back pain, including issues of effectiveness and safety. I thought the presenters delivered the workshop well and prompted some important conversations that are perhaps much overdue.
Looking ahead, I am already excited to attend the next APS ASM in Adelaide in 2026. What I am looking forward to most is reconnecting with the people I met this year and hearing how their research has progressed. As I mentioned earlier, there is such a great sense of community at the APS conferences that I have attended, and I am excited to keep being a part of that. It is so motivating being around people who have similar goals to improve the lives of people in pain through their research.
Overall, I left this year’s conference feeling energised, with a growing list of ideas and new connections across Australia. Thanks to the APS for making this possible. See you next year!
Declaration: Martjie is supported by a University Postgraduate Award from the University of New South Wales and a PhD TopUp Scholarship from Neuroscience Research Australia.

At the 2025 Australian Pain Society’s 45th Annual Scientific Meeting, some of the profession’s leading lights presented groundbreaking research aimed at transforming pain care through more inclusive, evidence-based and system-aware approaches. Together, their work highlights the evolving role of physiotherapy in helping to tackle complex pain challenges across diverse populations. Melissa Mitchell reports.
Delivering the Australian Pain Society’s pre-conference physiotherapy workshop, sponsored by the APA, Dr Alicia Rayner explored physiotherapy management of tension-type headache and migraine.
Dr Alicia Rayner FACP laid down a challenge to physiotherapists—reconsider how you are assessing and managing tension-type headaches and migraines. These conditions, Alicia said, are often viewed in silos, as either purely musculoskeletal or purely medical, when in reality they frequently present as persistent pain conditions with significant overlap. The message from the Specialist Musculoskeletal Physiotherapist (as awarded by the Australian College of Physiotherapists in 2022) is clear—physiotherapists have a crucial role to play in identifying, understanding and managing primary headaches, particularly when viewed through a pain science and central sensitisation lens.

Alicia encouraged clinicians to see both tensiontype headaches and migraines as primary headaches, underpinned by a sensitised nervous system. These conditions share many features with other nociplastic pain presentations such as fibromyalgia or irritable bowel syndrome and benefit from an approach that extends beyond joint or soft tissue treatment, she said. Migraines, for instance, often involve widespread sensory hypersensitivity, disrupted sleep, fatigue and cognitive difficulty—hallmarks of central sensitisation that physiotherapists are well placed to address.
Among the tools available to physiotherapists, Alicia highlighted exercise as one of the most effective and underutilised interventions. She pointed to research recommending three sessions of moderate-intensity exercise per week to reduce migraine frequency and intensity. Exercise not only activates the endogenous pain inhibition system but also improves sleep, mood and overall wellbeing. For those with sensitised systems, Alicia said, graded exposure is recommended, along with patient-led pacing to avoid flare-ups and build confidence in moving.
Manual therapy also has a role, Alicia said, particularly in treating tension-type headaches, which make up the bulk of primary headache presentations. These are typically bilateral, mild to moderate in intensity and not aggravated by physical activity. Alicia said that many patients misclassify their headache type, often attributing their pain to cervicogenic sources, when in fact their symptoms align more closely with tensiontype headache or migraine. In these cases, manual therapy may reduce musculoskeletal input and stress-related tension, offering relief even if it’s not addressing a biomechanical cause directly.
Alicia also addressed the complex relationship between migraine and neck pain. While neck pain may accompany migraine, Alicia urged clinicians to be cautious about assuming causality.
‘Cervicogenic headache is rare,’ Alicia says. ‘But we often treat the neck and the headache improves, leading us to draw conclusions that may not be accurate.’ Instead, she encouraged clinicians to view neck pain as one of many symptoms of central sensitisation rather than a driver of headache in most cases.
Alicia provided practical tools for diagnosis, including the FLINDA (Frequency, Location, Intensity, Nature, Duration and Autonomic signs) (coined by Alastair Flett) framework. This structured questioning helps clinicians uncover patterns and characteristics that differentiate tension-type headaches from migraines and supports more accurate diagnosis. This is especially important because patients often under-report or misclassify their symptoms. She said that a migraine does not have to be severe or unilateral to meet diagnostic criteria. Moderate bilateral headaches with nausea and sensory sensitivity may still qualify.
In discussing common triggers, Alicia introduced the DEEPH (Dietary, Emotional, Environmental, Physical, and Hormonal) (devised by Alastair Flett) method, highlighting the multifactorial nature of headache and migraine. Patients with migraine often experience a cyclical sensitivity to stimuli, which can be modulated through lifestyle education and support. Alicia stressed the importance of helping patients recognise patterns in their symptoms, reinforcing the therapeutic value of headache diaries and self-monitoring.
Alicia would like to acknowledge Dr Alastair Flett FACP for his role in headaches and pain and changing our understanding of these conditions.
Alicia emphasised the need to rule out red flags, including signs of vascular events or medication overuse headache or significant changes in headache presentation during pregnancy. New or worsening headaches should always prompt further investigation, she said. Once serious pathology is excluded, physiotherapists are well positioned to lead conservative, non-pharmacological care for these patients.
Treating primary headache, Alicia said, isn’t about curing a condition. It’s about helping people live better with it. Through education, movement and an understanding of pain mechanisms, physiotherapists can provide meaningful support. ‘We’re not just treating the headache,’ Alicia said. ‘We’re helping patients understand their condition, feel empowered and regain control over their lives.’

Dr Emma Karran spotlighted urgent equity gaps in pain research, introducing a globally developed dataset designed to draw attention to disparities.
Tackling the persistent under-representation of marginalised groups in pain research, Dr Emma Karran argued that inequities in pain outcomes often remain invisible due to incomplete or superficial collection of sociodemographic data. To address this, she led a major international project designed to identify which equity-relevant data should be collected.
Emma, a senior research fellow from the University of South Australia with a background in physiotherapy, education and research into the social determinants of health, made the case that pain research often fails to account for the broad societal and contextual factors that influence pain experiences and treatment outcomes. Traditional data collection tends to

prioritise basic descriptors such as age, sex and education, often conflating gender and sex and omitting key details such as place of residence, cultural identity or financial security.
Emma explained that this narrow scope can obscure meaningful differences in how pain is experienced and managed across different populations.
To build a more equitable evidence base, Emma and her team launched a three-year pain research project, ‘Identifying Social factors that Stratify Health Opportunities and Outcomes (ISSHOOs) in pain research’. The project aims to produce global consensus on a standardised, equity-relevant dataset for inclusion in all human adult pain studies. The dataset will help researchers more accurately describe study populations and interpret findings through a health equity lens.
The ISSHOOs project unfolded in several stages. It began with two scoping reviews examining how social determinants of health are currently captured in both clinical and research settings. The findings were mapped against the PROGRESS-Plus framework—a tool widely recognised in health equity research. This provided the foundational categories for the subsequent consensus process.
A three-round Delphi study followed, enlisting 168 global participants including pain researchers, clinicians, equity experts and individuals with lived experience of persistent pain. More than one-third of participants had firsthand experience with chronic pain, underscoring the project’s commitment to inclusivity. The Delphi process invited these contributors to evaluate, suggest and prioritise items for inclusion in a minimum dataset.
Despite the careful design of this consensus process, Emma acknowledged a key limitation. Certain groups—such as people from lower socio-economic backgrounds, rural communities and minoritised cultural or sexual identities—were under-represented. To counter this, the team conducted targeted supplementary data collection, recruiting 55 additional participants from historically under-represented groups. This ensured that the dataset was more reflective of diversity often missing from pain research.
The final consensus process, Emma said, identified two datasets. Set A, the minimum dataset, includes eight items: age, sex, gender, place of residence, race/ethnicity/culture, education level, financial status and work status. These items (each including a question and a set of response options) are considered essential for describing study participants in a way that supports equity-focused interpretation and application of research findings. Set B, the extended dataset, contains 30 optional items from which researchers can select a subset to suit their specific research questions and study context. These include housing conditions, health literacy, access to healthcare and experience of discrimination.
Emma emphasised that the datasets are not intended as rigid templates but as adaptable tools that can guide culturally sensitive research. Each item is accompanied by preambles for participants and detailed instructions for researchers to ensure clarity, appropriateness and transparency in data collection. For example, Emma said, sex and gender are explained simply but respectfully, taking into account the diverse legal and cultural contexts in which research may occur.
Emma went on to outline the broader benefits of using this dataset. More comprehensive demographic data
can support subgroup analysis, highlight treatment disparities and improve findings. Harmonised data also enables better comparisons across studies and contributes to systemic reviews with an equity lens. Emma said that Set B’s context-rich variables may help generate new hypotheses about how social environments influence pain and its management.
However, Emma was candid about the project’s limitations. While it offers a significant advance in standardising equity data in pain research, it does not directly address structural and systemic drivers of health inequity such as institutional racism or economic policy. The dataset’s relevance for paediatric populations is also limited at this stage because the complexities of adapting it for children require further investigation.
Despite this, Emma’s work provides a powerful blueprint for shifting how pain research is conceptualised and conducted. It invites researchers to engage more deeply with questions of who is studied, who is left out and how these choices shape the evidence base that informs clinical practice and policy.
As health equity continues to gain prominence across disciplines, this project is also a reminder that meaningful change begins with the basics—asking better questions, listening to more voices and collecting data that matters most. If pain researchers want to serve all people, their research must first see them.

Chronic pain and access to pain care are not experienced equally across Australia. Physiotherapist and PhD candidate Sophie Shephard presented a powerful challenge to the ‘metrocentric’ assumptions embedded in pain policy.
Pain care in rural and remote Australia, Sophie Shephard MACP argued, is shaped by deeply entrenched systemic inequities that go beyond workforce shortages or geographic isolation. While 28 per cent of Australians live outside major cities, rural populations shoulder a disproportionate burden of disease, including significantly higher rates of chronic pain.
However, Sophie said, rural pain inequity cannot be solved by parachuting urban solutions into rural areas. Instead, she advocated for a systems-level understanding of pain management that recognises the influence of place, power and policy.

Central to Sophie’s presentation was the concept of ‘urbanormativity’—the tendency to view urban settings as the ideal model for healthcare delivery and rural settings as somehow lacking or backward. As a consequence, pain services, policies and even clinical research are predominantly shaped by urban norms, rendering rural voices invisible. This is compounded by what Sophie calls an ‘epistemic injustice’—a process by which rural people are devalued as knowers or excluded from the development or dissemination of knowledge that affects their care.
Sophie highlighted the importance of adopting a framework that allows for a nuanced understanding of rural health systems. Drawing on a model by Lisa Bourke and colleagues in the 2012 paper Understanding rural and remote health: a framework for analysis in Australia, Sophie described five interrelated domains that shape rural health outcomes: geographic isolation, rural locale, local health responses, broader health systems and social structures, all underpinned by power. These domains interact to create a complex picture of rural health and pain care, where distance and infrastructure are just the beginning of the challenge. Social processes, expectations around participation in care, informal community-based health responses and the influence of political and economic structures all have a role to play, Sophie says.
Geographic isolation, for example, includes environmental barriers such as mountain ranges, flood zones or unsealed roads. Rural locales are socially shaped by tightly knit community networks and longstanding community knowledge—assets frequently ignored in urban-centric planning. Health services in these settings are often pieced together through formal and informal supports and yet
these responses are rarely recognised or funded appropriately, she argued.
Broader health systems including state and federal policies, funding structures, professional standards and institutional priorities are often designed without meaningful rural input. These systems continue to reproduce inequities through omission and lack of insight, Sophie said. This was reinforced by preliminary findings from Sophie’s systematic review of chronic pain interventions, evaluated in rural Australian cohorts. Despite a search strategy designed to be as broad and inclusive as possible, the review identified only 10 studies, of which two genuinely focused on the rural context. Strikingly, all bar one failed to report individual participant place of residence, relying instead on the location of service delivery.
While this is not uncommon, Sophie said, it undermines any understanding of whether the interventions were truly accessible or appropriate for rural populations. Without data on participant residence, it is impossible to understand who is actually being reached—particularly in a health system as centralised as Australia’s, where service location alone tells us little about travel burden, accessibility or the extent to which rural communities are excluded in practice.
Compounding this invisibility, the reviewed studies also failed to report on other critical intersectional aspects of participant identity such as income, education level, cultural or linguistic background and Aboriginal or Torres Strait Islander background.
Sophie encouraged the audience to ‘problematise’ how rural pain management is typically framed. For
example, while it is common to frame the problem of rural pain care as the result of a lack of trained workforce and resources to support best practice pain management, this assumes that metropolitan models of best practice are universally applicable. Reframing the problem—by asking instead whether urban models are fit for purpose in rural contexts—potentially leads to very different solutions. Sophie advocated for bottom-up, community-led approaches that are flexible, innovative and grounded in the local realities of rural life.
The shift in thinking is not just theoretical, Sophie said. It has real implications for how pain care is designed and delivered. She argued that even the most efficacious pain interventions may prove ineffective if they cannot adapt to the context in which they are implemented. Pain, like health, is an emergent product of complex systems. Solutions that fail to account for local realities may ultimately fail the people they are designed to help.
Rural people are not passive recipients of care, Sophie argued, and nor should their communities be viewed through a deficit lens. Instead, the pain sector must embrace a systems-based understanding of rural health that values lived experience, recognises the complexities of place and elevates local knowledge and leadership.

Physiotherapist and researcher Associate Professor Ebonie Rio delivered a compelling case for re-imagining how clinicians understand, assess and treat tendon pain.
Far from being passive cables that connect muscle to bone, tendons are metabolically active tissues with cells (tenocytes) that constantly communicate and remodel in response to load and their environment. Highlighting the capabilities of tendons, Ebonie Rio MACP, an APA Titled Sports and Exercise Physiotherapist, said that in the lower limbs especially, tendons act like springs, storing and releasing energy to power movement efficiently. Whether leaping in sport or simply stepping off a kerb, humans rely on the spring-like action of tendons throughout life.
Yet despite their critical function, tendons are vulnerable to injury and the consequences can be complex. Ebonie explained that tendon injury can

affect a really broad group of people, from elite athletes to sedentary older adults, office workers and people with chronic illness such as diabetes and HIV. Despite this prevalence, Ebonie said, there is no specific International Classification of Diseases code for tendinopathy, making it difficult to track its true incidence or burden on the health system.
One of the central themes of Ebonie’s talk was the need to improve diagnostic clarity. Ebonie described four distinct categories of tendon injury: tendinopathy, peritendon irritation, bursitis and rupture. Each has a unique presentation, response to load and treatment pathway. For instance, while tendinopathy is driven by high-speed tensile loading, peritendon issues are provoked by movement and friction and bursae-related pain may be triggered by footwear or compression. Understanding these differences, Ebonie said, is essential for delivering appropriate care.
Ebonie advocated for a move away from palpation and imaging as primary diagnostic tools. She noted that pain during tendon palpation is common but often unhelpful for distinguishing clinical diagnosis. Similarly, imaging frequently shows abnormalities in people without symptoms, which makes it an unreliable guide. Instead, she recommended a load-based functional assessment to determine whether pain is localised and increases in response to progressively challenging loading tasks—hallmarks of tendinopathy.
But the tendon story doesn’t end in the tissues. Ebonie delved into the central nervous system changes that accompany chronic tendon pain. People with tendinopathy exhibit alterations in the motor cortex, changes in excitability and inhibition, and asymmetries in strength and motor control. These adaptations, she said, can pose a heavy
cognitive burden, akin to pressing both the brake and the accelerator while trying to move. Yet other aspects of neural function, such as body schema and body modulation, appear to remain intact.
This brain–body link has significant implications for treatment. According to Ebonie, while current rehabilitation protocols often restore basic strength, they rarely challenge or retrain the motor cortex. To truly optimise function and prevent recurrence, clinicians may consider how they integrate neuroscience—targeted methods that engage the brain during movement, she said.
One simple yet powerful tool Ebonie championed was externally paced strength training using a metronome. Patients concentrate and coordinate, promoting changes in cortical activity. Ebonie said that compared to unstructured, self-paced movements, externally paced exercises deliver both muscular and neural benefits.
Equally important is the language clinicians use. The words chosen in the clinical setting shape patients’ expectations, beliefs and engagement with treatment. Outdated or nocebic terms such as ‘tendonitis’ or ‘degenerative tendon’ imply inflammation or damage, fuelling fear and passivity, Ebonie argued. More accurate terminology such as ‘tendinopathy’ helps frame the condition as a load-related issue that improves with active rehabilitation.
Ebonie set out a clear hierarchy of intervention effectiveness. Passive therapies, she said, consistently underperform. Effective treatment requires building sufficient muscular capacity and motor control through targeted loading, with education and reassurance to reduce fear and build confidence.
She also encouraged clinicians to tailor interventions to the individual and their specific tendon injury. For example, people with gluteal tendinopathy benefit from reducing compression by avoiding crossed legs or prolonged standing on one hip. Individuals with Achilles insertion issues need to avoid stretching and instead benefit from heel lifts or load modification. Bursae-related pain (for example, the superficial bursae) is often improved by changing footwear or reducing the friction or compression from shoes.
Ebonie also touched on the increased incidence of tendon rupture following the COVID-19 pandemic, theorising that changes in physical activity patterns may have played a role. Tendons that rupture usually have underlying pathology but no pain and these changes in behaviour combined with asymptomatic changes may have contributed to the post-pandemic spike, she said.
Ebonie concluded by urging clinicians to embrace a more nuanced and responsive approach to tendon care. She emphasised the importance of accurate language, load management tailored to the individual and rehabilitation that addresses strength and motor control and central nervous system adaptation. By shifting focus from damage and dysfunction to capability and adaptability, practitioners can help patients better understand their condition, engage more confidently with treatment and, ultimately, return to the activities that matter to them.

A strengths-based approach to arthritis and persistent pain in the Aboriginal and Torres Strait Islander population was the focus of a talk by physiotherapist researchers Dr Samantha Bunzli and Jane Linton.
Apresentation by Dr Samantha Bunzli APAM and Jane Linton (Gumbaynggirr) called on physiotherapists to reframe how healthcare systems engage with chronic musculoskeletal pain, particularly in Aboriginal and Torres Strait Islander populations. As part of a program entitled ‘Strengthening pain care with our ways’, Samantha and Jane were members of a research team that advocated for harmonising different paradigms of health. Where Western medicine traditionally focuses on pathology and deficit (what makes people sick), Aboriginal and Torres Strait Islander approaches are rooted in salutogenesis—understanding and fostering the conditions that enable individuals and Communities to live well.

Samantha and Jane began with a video story of Thomas, a former football player living with osteoarthritis whose wellbeing was sustained with regular exercise, cultural connection and social participation. His experience underscored the concept of ‘flourishing’—a holistic view of health as more than the absence of disease. Samantha and Jane described it as a framework that closely aligns with Aboriginal and Torres Strait Islander views on wellness, where cultural identity, Community belonging and connection to Country are critical to managing pain and chronic illness.
This perspective is especially pertinent for physiotherapists, whose scope of practice includes physical rehabilitation, health education and promoting functional independence. Samantha and Jane encourage clinicians to look beyond joint function and physical impairment and consider broader health indicators such as social, emotional and cultural wellbeing. They presented a powerful visual metaphor: the melaleuca tree. The tree and its flowers are culturally significant for some Aboriginal Communities. In their model the tree’s roots represent culture, Country and kinship; its soil signifies historical and systemic influences such as racism and colonialism and the branches are the social determinants of health—housing, employment and access to healthcare. When those conditions are supported, the tree flowers, symbolising a life that flourishes.
Physiotherapists, they argued, are well positioned to support this flourishing by working in partnership with Aboriginal and Torres Strait Islander Communities to provide culturally safe and accessible care. However, access to physiotherapy and other nonpharmaceutical interventions remains inequitable. The research team conducted a systemic review showing that Aboriginal and Torres Strait Islander people are 1.5 times more likely to experience arthritis than other Australians, yet significantly less likely to access primary care services or receive joint replacement surgery. They are, however, twice as likely to be prescribed opioids for pain.
Rather than reinforcing a deficit discourse that frames Aboriginal and Torres Strait Islander communities in terms of disadvantage, the team applied a strengthsbased model that centres Aboriginal and Torres Strait Islander voices and capacities. Through the ‘Stay Moving, Stay Strong’ project they established Community reference groups in Western Australia and Victoria to co-design arthritis education materials. Aboriginal people living with arthritis shaped every aspect of the project, from identifying priorities to reviewing content, ensuring that the resources were culturally relevant, visually engaging and practically useful.
Key themes that emerged from interviews with 31 participants, who experienced all types of arthritis, included the social and emotional toll of arthritis, the importance of Community connection and barriers to accessing care. Participants expressed a strong desire for information that acknowledged their cultural context and responsibilities such as caring for family and maintaining cultural practices. The preferred formats for learning, Samantha and Jane said, were brochures and videos featuring artwork and stories from Aboriginal artists and Community members.
The project culminated in a suite of educational resources for osteoarthritis, rheumatoid arthritis, gout and lupus. The materials were co-designed using accessible language, balanced visual and written content and included links to local Aboriginal medical services. A dedicated website (tinyurl.com/ wncecbr4) hosts four brochures and six videos showcasing lived experiences and personal strategies for managing arthritis. Samantha and Jane said that the response has been overwhelmingly positive.
Evaluation of the program is ongoing, with recent Community feedback affirming the relatability, usefulness and accessibility of the resources. Suggestions for future iterations, Samantha and Jane said, include creating resources specifically for carers and family members, recognising the interdependence of individuals and their Communities in Aboriginal cultures.
The team’s work advocates for a shift in practice towards collaborative, culturally safe and Communitydriven approaches that support Aboriginal and Torres Strait Islander people to thrive on their own terms. By embracing Aboriginal and Torres Strait Islander Community ways of knowing, being and doing, healthcare can become more inclusive, more effective and more connected to the people it serves.
This research, argued Samantha and Jane, stands as a compelling example of how researchers can contribute to social justice and health equity, not only by treating pain but by transforming the systems and assumptions that shape care.
The Staying Moving, Staying Strong project was conducted by a national interprofessional team of Aboriginal and non-Aboriginal health professionals and research leaders. In addition to Jane and Samantha, the research team involved Ngiyampaa woman Brooke Conley; Badimaya, Wajarri, Wilunyu woman Charmaine Green; Ngoonooru Wajarri woman Wanda Flanagan; Whadjuk, Balladong, Gnarla Karla Boodja Nyoongar man Trevor Pickett; Noongar (Wardandi) man Jonathan Bullen; Ivan Lin; Penny O’Brien; and Jennifer Persaud. The project was funded by an Arthritis Australia and Commonwealth Government grant, administered through Arthritis and Osteoporosis WA.


Physiotherapist researcher Dr Nathalia Costa investigated systemic barriers and opportunities to improve low back pain care in Australia.
During her postdoctoral research at the Leeder Centre for Health Policy, Economics and Data at the University of Sydney, Dr Nathalia Costa (now a senior research fellow at the University of Queensland) and her team conducted a qualitative study to explore the perspectives of policymakers, academics, professional association leaders and other key stakeholders on what hinders low back pain (LBP) care in Australia and how to improve it. They used a systems thinking approach—a method that helps make sense of complex problems by examining how different factors and systems interact.
The results, based on 37 in-depth interviews, showed that LBP is a ‘wicked problem’ shaped by a web of

challenges in a complex system. They also indicated some practical steps that could help to improve care.
A central finding from Nathalia’s work is the significant variability in care pathways for patients with low back pain. People receive inconsistent messaging from healthcare professionals, a reflection of divergent clinical philosophies, differences in training and differing care models across private and public settings. This contributes to confusion, mismanagement and uneven health outcomes, particularly in rural and regional areas and for those unable to afford out-of-pocket care.
Funding models also emerged as a major theme. Nathalia and her team’s research showed that the current Medicare fee-for-service model does not adequately support best-practice care. While guidelines advocate for non-pharmacological and non-surgical approaches, these are poorly funded or entirely unfunded. Nathalia said that allied health services, which are often central to evidence-based care, remain under-supported, with limitations such as the five-session cap under chronic disease management plans.
Public understanding of LBP is another critical barrier. The interviews revealed widespread misconceptions including a desire for quick fixes, beliefs that movement can damage the spine and reliance on imaging and medication as primary solutions. The community struggles to navigate a fragmented health system; many consumers are unclear about the roles of different allied health professionals and how to access appropriate care.
Nathalia drew attention to the commercial and systemic forces that reinforce the status quo.
Financial incentives encourage practices that may be low value or even harmful, such as overreliance on imaging or passive treatment modalities. Especially in the private sector, time pressures and financial incentives make it difficult for clinicians to pursue ongoing education or shift to more evidencebased models of care. Interviewees highlighted that some practitioners engage in services not aligned with best practice to meet financial needs and one of them admitted doing this themselves.
Beyond these core challenges, Nathalia’s analysis points to a range of contributing factors that complicate efforts to improve care. These include limited access to conservative management, short consultation times, siloed professional practice, persistent stigma around pain and the neglect of social determinants of health. Many of these barriers are entrenched in broader healthcare structures and policy inertia.
Despite this daunting landscape, Nathalia’s presentation offered a road map for progress. Her interviews revealed strong support for increased collaboration across stakeholder groups. People with lived experience and the community more broadly, clinicians, researchers, advocacy groups, professional associations, academics, universities, private health insurance companies, employers/ workplaces, policymakers, government agencies, departments of health, research funding bodies, lawyers, advisory committees, the pharmaceutical industry and the compensation sector all need to engage in joint problem-solving to address the systemic nature of the issue. Practical suggestions included the creation of summits or working groups to facilitate cross-sector dialogue and the co-design of reforms.
Interviewees also recommended changes to funding mechanisms such as expanding subsidies for allied health, funding multidisciplinary community-based care and restricting Medicare to better align with chronic disease needs. Public health campaigns to improve health literacy and reframe community perceptions of back pain were considered essential, Nathalia said. Other proposals included reforms to the workers compensation sector, more robust information systems and improved workforce training to equip practitioners with the skills needed to deliver guideline-informed care.
A key takeaway is that how we define the problem of LBP influences the solutions that we pursue. Too often, LBP is framed narrowly as a condition to be managed at an individual level. Nathalia advocates for a broader, more inclusive framing, one that embraces complexity, priorities equity and recognises that coherent action across the system is more critical than pinpointing a single solution.
Nathalia’s closing message emphasised the need for research and advocacy that extends beyond traditional academic boundaries. By drawing on stakeholder analysis and cross-sector networks, researchers and clinicians can help monitor government accountability and drive meaningful change. As she noted, solving ‘wicked problems’ like LBP is not about finding one correct answer but about supporting stakeholders to work together towards coherent and sustainable action.
Scan the QR code to watch the presenters discuss their research.


Amy McNeilage
Amy McNeilage is a PhD candidate and senior research officer in The University of Sydney’s Medical School with expertise in qualitative methodology. Her research seeks to identify and mitigate harms associated with opioid and gabapentinoid use.


I felt incredibly fortunate to be selected as a delegate for the 2024 painSTAR Pain School for Translation and Research, held over five inspiring days in the beautiful Barossa Valley in November. I applied with the goal of expanding my network, improving my research communication and leadership skills, and learning from interdisciplinary experts and consumers on how to make my work more impactful. painSTAR exceeded all expectations – and left me feeling energised, motivated, and better equipped to contribute to the pain research community.
The event was impeccably organised, from the engaging program and fun social activities to the excellent catering (with plenty of sugary



snacks to keep us going!) and beautiful accommodation with sunrise views over the vineyards. Although the schedule was full, I managed to squeeze in a few early morning birdwatching walks by the creek, including my first ever sightings of a musk lorikeet, rainbow bee-eater, and a grey currawong (we mostly have the pied ones in Canberra!).
One of the biggest highlights for me was the opportunity to present my own PhD work in such a genuinely supportive environment. I felt more relaxed than ever during my talk, thanks to the warmth and encouragement of both faculty and fellow delegates. The feedback I received was insightful and constructive, and I left with new ideas and renewed confidence in how I frame and share my research.
Professor Jeff Mogil’s workshop on giving better talks completely shifted how I think about preparing and delivering talks. For example, he encouraged us to pare back the detail and instead focusing on storytelling and clarity. I have already put this into practice in subsequent presentations (including at the


Australian Pain Society [APS] conference in April in Melbourne), and I am seeing a tangible difference in how my work is received.
Equally valuable was the grant writing session with Associate Professors Tasha Stanton and Wendy Imlach. Their generous sharing of experiences helped to demystify a process that can often feel daunting. I now feel I have a better grasp of how to approach grant applications strategically – and with a little more confidence.
Beyond the structured sessions, painSTAR created a strong sense of community. The social activities were a perfect balance to the intensive program. I particularly enjoyed my first-ever ‘paint and sip’ experience, which was equal parts silly and fun. This was such a great way to get to know fellow attendees outside of a research context. The final night’s pitch presentations were also a standout: creative, entertaining, and seriously impressive given the limited prep time.
Since returning home, painSTAR’s impact has continued. It came at the perfect time – just as I was entering the second half of my PhD – and provided a much-needed boost of energy and motivation. I have been drawing on insights from the week as I start to draft my thesis.
Attending the APS Annual Scientific Meeting in Melbourne this year felt especially rewarding –reconnecting with painSTAR alumni and faculty made the conference experience feel richer and more collaborative. It was a great reminder
of the community that painSTAR is helping to foster, and how valuable those connections can be. This is particularly so when introducing early career researchers to the wider APS network in such a welcoming and supportive way.
I am incredibly grateful to the organisers, faculty, and fellow delegates for making painSTAR so memorable. I look forward to paying it forward by continuing to contribute to the pain research community in Australia and beyond.
Declaration: Amy McNeilage has nothing to declare.

The Australian Pain Society (APS) is a multidisciplinary association whose purpose is to advance pain management through education, research, and advocacy for transformational improvements in clinical care. Our vision is that all people will have optimal pain management throughout life.
Cops for Kids (CFK) is a South Australian based charity focused on supporting initiatives that strive to improve the lives of children in that state. Part of the CFK mandate includes the provision of funds for research to assist in the care of sick children and/or enhance the life quality of a child.
APS is pleased to announce our partnership with Cops for Kids is continuing with an eighth Clinical Research Grant Program
In brief, the award is to enable clinical research meeting the following criteria:
• Achieve a meaningful conclusion in one year
• Conducted in Australia and must be relevant to the South Australian population
• The applicant must be an Australian citizen or permanent resident
• The applicant and their supervisor (if applicable) must be members of the Australian Pain Society and its Pain in Childhood Special Interest Group

• The funded project can be related to any aspect of a childhood pain complaint - including theoretical, mechanistic, diagnostic, treatment, epidemiological and/ or sociological approaches; and
• The grant funding of $40,000 (inclusive of GST) will be paid quarterly in arrears upon the submission and acceptance of a combined Progress Report-Acquittal Form
Further information about the Clinical Research Grant can be obtained from the APS Secretariat.
Mentoring available:
To assist with the grant application process and any general queries, past CFK grant recipients have generously offered to conduct several informal online ‘drop in’ sessions on the following dates and times:
a. Thursday 07AUG25 at 1:30-2pm AEST, register here
b. Wednesday 20AUG25 at 1:30-2pm AEST, register here
Clinical Research Grant Application forms are available online and must be submitted by: 5pm AEST on Wednesday 10 September 2025.
By Dr Carolyn Berryman, APS Pain in Childhood SIG Chair-Elect
In 2023 I was fortunate to be awarded the Cops for Kids (CFK) Clinical Research Grant #6. The funding allowed the national group of researchers I was leading to connect with adolescents and their families to investigate what barriers adolescents faced when seeking care for chronic pain. Our discoveries led to a far deeper understanding of the gaps in service delivery. We identified the needs and wants of the adolescents and their families which highlighted the need for care and service delivery development in young people’s pain. Of importance, adolescents often reported feeling invalidated and unheard, their care was fragmented across different healthcare sectors, and communication with other important sectors such as schools was unreliable. Accessibility to care was limited, and many families expressed their desire for increasing the capacity of healthcare professionals to manage chronic pain in their local community.
Based on the findings from the CFK Clinical Research Grant #6 I then worked closely with investigators in primary care, the Department of Education and the local health networks to develop a Medical Research Future Fund (MRFF) grant. We then submitted under the 'Multidisciplinary Models of Primary Care Stream 4' and were fortunate enough to be successful with this proposal. The MRFF grant provides five years' worth of funding to iteratively develop service delivery and care, co-designed with key interest holders, and


BLOG WEB
to run an implementation trial of the final product. We have just advertised the first PhD project related to the grant and are developing our protocols for each work package. The MRFF grant proposal shifts the focus of care to community based wellness hubs with a central tertiary hub for more complex care. To further strengthen our study, we have a committed advisory board which comprises of an extensive and experienced team of international researchers. We have also made connection with the director of a similar scheme that is currently rolling out in Finland.
The Cops for Kids Clinical Research Grant has connected me with an outstanding group of clinician researchers in paediatric pain and really supported my development as a lead researcher. The CFK funding enabled pilot data to support our successful MRFF grant bid. It has been a life changing event for me.
I recommend you consider applying for the CFK#8 grant and take advantage of the mentoring sessions generously offered to assist with the application process.
Clinical Research Grant Application forms are available online and must be submitted by: 5pm AEST on Wednesday 10 September 2025.
Thursday 21 August 2025, 12-1pm AEST (via Zoom)
The purpose of our Basic Pain Research Special Interest Group (BPR SIG) is to share, improve, and promote scientific knowledge and understanding of the mechanisms of nociception and pain. Our focus spans all levels of investigation, from molecular and cellular analyses to preclinical and clinical research.
This forum will provide an informal platform to promote and share our research and insights, from early career researchers (ECRs) (including students) and senior colleagues.
Session 13: Innovations in objective pain measurement in rodent models
Summary:
Join us for this month’s BPR Pain Hour, featuring two exciting talks on emerging technologies for objectively measuring pain in preclinical rodent models. These presentations will highlight novel approaches to analysing behaviour and facial expressions, offering new insights into pain research.
Talk 1: Decoding Pain-Related Behaviour in Rodents Using BlackBox
Dr Barkai will share his work on developing algorithms to quantify pain-related behaviours in rodents using the BlackBox platform, a tool designed to enhance the precision and scalability of behavioural pain assessment.
Talk 2: Painface – Facial Expression Analysis in Rodent Pain Models
Professor Zylka will present Painface, a system for evaluating pain in rodents through facial expression analysis. He will discuss its development and potential to improve objectivity in preclinical pain studies.
The invited speakers:
• Dr Omer Barkai, Lab of Clifford Woolf, Department of Neurobiology, Harvard University, USA
• Professor Mark Zylka, Department of Cell Biology and Physiology, University of North Carolina-Chapel Hill, USA
All are welcome to attend, including postgraduate students.
Please be advised that the speakers and most of the audience may not have clinical or healthcare backgrounds. Therefore, they may not be able to provide advice about managing pain from a healthcare perspective.
We look forward to seeing you there, please register here.
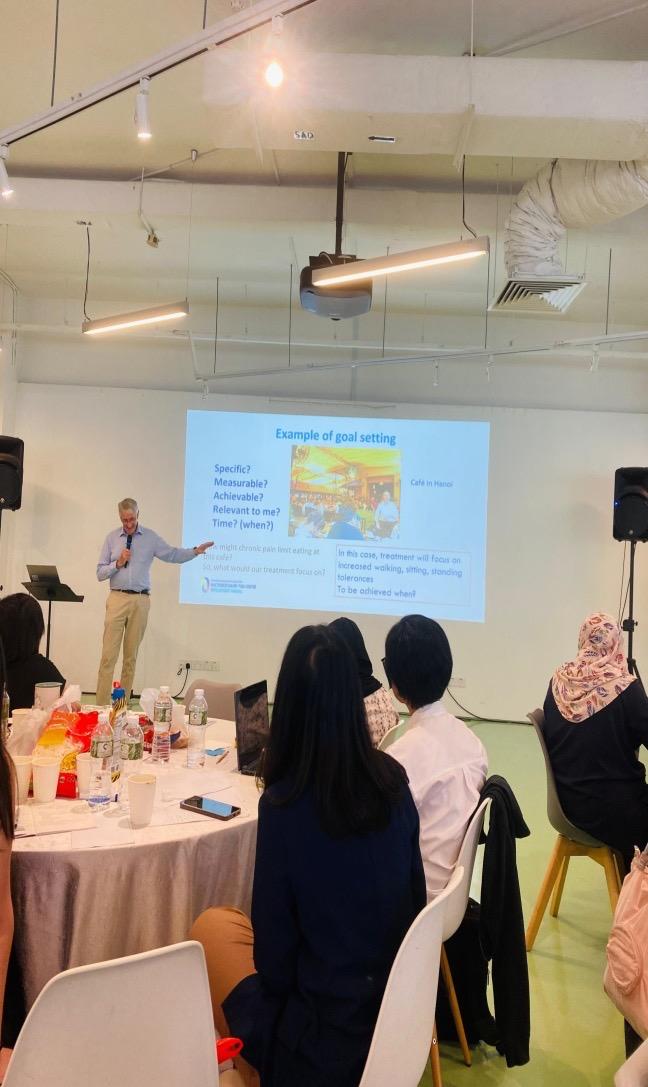
By Dr Dulce Calado, Timor Leste
From April 27th to May 4th, 2025, I had the privilege of participating in the Pain Management Camp and the Association of Southeast Asian Pain Societies (ASEAPS) congress held in Singapore. This opportunity was not just a professional development experience; it was a deeply personal journey that further affirmed my commitment to advancing pain management in my country.
On this occasion I would like to say thank very much to the Australia Society of Anaesthetists (ASA), the Australian Pain Society (APS) and the Australian and New Zealand College of Anaesthetists (ANZCA) for giving me the opportunity to participate and learn more about pain management.
What motivated me to join this training was a blend of both professional responsibility and personal conviction. As a general physician actively involved in the development of pain management services in Timor-Leste, I realise that many patients still feel pain even though they have taken medication. Pain management is an important concept in our hospital system, and I believe that with the right knowledge and collective will, we can offer compassionate care, that respects the dignity of each patient.
Before the training began, my expectation was to deepen my understanding of particularly pain and symptom management, communication skills, and psychosocial support. I also hoped to learn how to better support patients and families emotionally and spiritually, which is often a neglected dimension of care. I am grateful to say that not only were these expectations met, they were significantly surpassed.
All presentations on pain management were very useful and I really learned from them. For me, the most memorable was the presentation by Professor Michael Nicholas on SelfManagement. His talk focussed on teaching patients pain self-management skills. See
below for the key elements he covered. Key elements:
1. Assessment for biopsychosocial contributors to pain, distress, disability.
2. Preparation (re-orientation of expectancies to value self-management).
3. Basic education (addressing patient’s uncertainties about pain).
4. Core self-management skills taught:
• Goal setting (provides motivation/ direction).
• Activity pacing (achieving goals, step by step).
• Exercises (regular, normal movements are important).
• Self-regulation of stress (using relaxation/ meditation)
• Problem-management (to overcome obstacles to living with pain)
The biopsychosocial model teaches us that building good relationships and trust with patients is through clear and good communication. This training greatly influenced the way I view pain management, not just as a medical intervention, but as a compassionate, person centred approach that addresses the whole person: body, mind, and spirit.
My hope is that pain management will be integrated into every level of our health system, available in hospitals and clinics. And I hope that what I have learned and gained from this training can be shared with my colleagues, so that we can work harder and alleviate the suffering of patients. Further, this training reaffirmed my belief that change is not only necessary, it is achievable. It begins with each of us choosing to show empathy, courage, and the willingness to care.






OPEN (Online Pain Education Network) is a new, online training program funded by the Department of Health and Aged Care, alongside philanthropic partners TDM Foundation and Hearts and Minds Investments (HM1).
Developed by leading pain clinicians and researchers from the University of Sydney and Curtin University, OPEN equips healthcare professionals with practical, evidence-based skills to better support Australians living with chronic pain. It's available to GPs, nurses, physiotherapists, psychologists, occupational therapists, allied health professionals, care workers and students.
Grounded in real-world experience, OPEN reflects a person-centred, interdisciplinary approach shaped by clinicians and people with lived experience. Proceeds are reinvested into pain education and research, supporting continuous improvements in care — and advancing the goals of the National Strategic Action Plan for Pain Management.

Chronic




“When I was given the tools to manage my own pain, it was like a dream come true.”
Joe, 35, managing chronic back pain



Sinclair, C, Meredith, P & Strong, J 2020, ‘Pediatric Persistent Pain: Associations Among Sensory Modulation, Attachment, Functional Disability, and Quality of Life’, The American Journal of Occupational Therapy, vol. 74, no. 2, pp. 7402205040-7402205040p11.
DOI: 10.5014/ajot.2020.033308
Reviewer: Luke Macauley, Psychologist, Paediatric Chronic Pain Service, Women’s and Children’s Hospital, Adelaide SA.
Review of article
Study group
114 children/adolescents from ages eight to 18. All participants had persistent pain (>three months) or a specific pain disorder.
Aims
To investigate relationships among sensory modulation, attachment, function, and quality of life in a paediatric population with persistent pain.
Method
Authors employed a cross-sectional quantitative design. Measures used included Functional Disability Index, Pediatric Quality of Life Inventory, and Experiences in Close Relationships Scale-Revised measuring attachment pattern. The Short Sensory Profile 2 or Adolescent/ Adult Sensory Profile as was age appropriate were also administered to measure sensory processing effects on the child’s home, school and community life.
More advanced statistical analyses included stepwise hierarchical multiple regression to determine whether sensory modulation or attachment independently predicted functional disability or Quality of Life (QOL). A second series of regression analyses determined whether anxious or avoidant attachment styles mediated relationships between sensory modulation and disability or QOL.
The authors report a wide range of results based on statistical analyses, though not all hypotheses were supported by the data. Of note, low registration sensory profile – that is a pattern where an individual does not readily notice or respond to sensory input - was correlated positively with both anxious and avoidant attachment, and negatively with emotional, social, and school-related QOL. Anxious attachment was significantly negatively correlated with social and school-related QOL. Likewise, avoidant attachment negatively correlated with school-related QOL. Sensory sensitivity accounted for 31% of variance in disability.
Conclusions
The authors identified a correlation between those who were less aware or responsive to sensory input and higher anxious and avoidant attachment. They related this to a prior study which observed a similar effect in children with a history of trauma. They conclude that “Higher low registration among children and adolescents with persistent pain may be related to previous developmental trauma, which predisposes such children and adolescents to insecure attachment” and possibly persistent pain.
Reviewer's critique & take home message from the article
Strengths:
The authors note that theirs is the first study to demonstrate the independent effect of sensory modulation and attachment on QOL in children with chronic pain. The study is highly detailed in collecting and reporting data and analyses. This has facilitated a thorough examination of a novel hypothesis with good face validity, i.e. clinically/anecdotally observed correlations between variables. The results uniquely describe possible mechanisms of effect relating to
sensory sensitivities associated with chronic pain and attachment. The findings offer good clinical utility in formulating and addressing enmeshment and avoidance behaviours e.g. school avoidance.
Limitations:
The authors acknowledge the likely measurement bias inherent in self-report data collection and parent observation of children’s subjective sensory experiences. They also acknowledge that number of years having experienced pain/disability was not collected in data which likely bears on QOL. Finally, there is recognition that results may be limitedly generalisable to male children/adolescents with pain due to gender imbalance in sample, and that the limited sample size prevented more complex statistical analysis.
Take home message:
The study provides meaningful statistical evidence which sheds light on the hugely impactful role parents and parent-child relationships play in treatment of paediatric
chronic pain. When challenged and/or in pain, children with certain sensory profiles may choose strategies that increase feelings of safety by increasing physical/social/emotional closeness to caregivers, but which also serve as avoidance of opportunities to grow e.g. engage in school. Therapy for chronic pain may be perceived as challenging or provoking by children and/or their parents. Therefore, careful attention towards attachment and sensory profiles is required to address avoidance behaviours underlying chronic pain and encourage individuation from attachment figures. The findings reinforce the need for treating sensory sensitivity to improve participation in daily activities, and the use of attachment-based therapies to support school engagement.
Declaration
This review has been completed independently, ensuring an accurate summary of the referenced article, conducted in accordance with academic standards. The reviewer has nothing to declare.
Arnold, J. T., Franklin, E. V., Baker, Z. G., Abowd, M., & Santana, J. A. (2022). Association between fear of pain and sports-related concussion recovery in a pediatric population. Clinical Journal of Sport Medicine, 32(4), 369–375.
DOI: https://doi.org/10.1097/ JSM.0000000000000951
Reviewers: Jett Swaffer and Alistair Jones, fourth year UniSA Physiotherapy Students, conducting health promotion project out of Paediatric Chronic Pain Service at Women’s and Children’s Hospital
Review of article
Study group
128 paediatric patients aged eight to 18 years who presented to a sports medicine clinic with a primary diagnosis of concussion from September 2018 – March 2020. Participants were included if they presented within two weeks of injury and were symptomatic at the initial visit.
Aims
The aim of the study was to determine if an association exists between fear of pain and recovery time from sports-related concussion in a paediatric population.
Method
This study utilised a prospective observational study. There was no intervention. Study participants who met inclusion criteria were administered the Fear of Pain Questionnaire (FOPQ) at their initial visit. After completing the FOPQ, the patient went through a normal concussion assessment. Patients continued with follow-up visits until there was clinical recovery, defined as resolution of concussion symptoms, resumption of normal daily physical and cognitive activity, and normalisation of physical examination findings to functional levels. Time to clinical recovery was the main outcome measure.
Summary of results
Those with prolonged recovery had significantly higher FOPQ scores (M = 33.12) than those without prolonged recovery (M = 26.16). Average number
of days to recover was 42.57. Seventy-three (57%) patients had a prolonged recovery (> 28 days). Patients with prolonged recovery indicated higher FOPQ scores at their initial sports medicine visit. In addition to being more likely to have a prolonged recovery, younger patients tended to have higher scores for fear of pain due to the stage of brain development when the concussion occurs or age-dependent physiological responses to the concussion.
In conclusion, higher fear-of-pain scores on the FOPQ were prospectively associated with prolonged recovery from concussion in a paediatric patient population. Concussion is a unique injury, as symptoms are exacerbated by physical, cognitive, and emotional stressors, and recovery has a multifaceted trajectory. It is important for clinicians to evaluate and monitor for maladaptive fear avoidance behaviours throughout the recovery process to most effectively treat patients.
Reviewer's critique & take-home message from the article
This study presents a well-designed approach to understanding how fear of pain affects recovery in paediatric patients with concussion. The study could have benefited from more explicit criteria to define recovery to improve the rigour of the methodology. The small study size does limit the generalisability of findings and cannot control for the influence of outliers or confounding variables. Paediatric patients were more likely to have a prolonged recovery from concussion when they had higher fear of pain. Clinicians would benefit from future research investigating whether this finding can be replicated in a larger sample, and whether fear of pain can be effectively modified through educational interventions to potentially reduce recovery time in patients with concussion.
Declaration
This review has been completed independently, ensuring an accurate summary of the referenced article, conducted in accordance with academic standards. The reviewers have nothing to declare.
Sheykhangafshe FB, Farahani H, Dehghani M, Fathi-Ashtiani A. The effectiveness of psychological interventions in the treatment of children and adolescents with chronic Pain: A systematic review. Journal of Child Mental Health. 2024; 11 (1):62-80.
DOI: 10.61186/jcmh.11.1.6
Reviewer: Mon Chamlagai, Provisional Psychologist, Paediatric Chronic Pain Service, Women’s and Children’s Hospital, Adelaide SA
Review of article
Study group
The target group for the study is children and adolescents with chronic pain. In total, the systematic review included 3,252 children and adolescents from 10 countries including United States, Sweden, Canada, United Kingdom, Spain, Germany, Italy, Iran, Lebanon and France.
Aims
To investigate how effective psychological interventions are in treating children and adolescents with chronic pain.
Method
The systematic review included 38 articles out of 973 that were published between January 2001 to July 2024. Databases searched included Google Scholar, EMBASE, psychINFO, Scopus, Proquest and PubMed. Quality assessment was undertaken using a checklist that included the type of research, research objectives, clarity of inclusion and exclusion criteria, adherence to ethical protocols, population and sampling process, data collection tools and data analysis. The results were reported using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis) framework. Some of the key words for the database search included ‘children’ ‘adolescents’ ‘chronic pain’ ‘pain management’ and ‘pain reduction’.
Summary of results
Psychological treatments such as cognitive behavioural therapy, acceptance and commitment therapy, biofeedback-relaxation techniques, mindfulness-based intervention and compassionfocused therapy. These therapies were applied in the treatment of chronic headaches, abdominal pain, irritable bowel syndrome and other pain. These therapies were reported to be effective in reducing pain, stress, anxiety, pain-related disabilities and overall quality of life.
Psychological interventions have been shown to be effective in treating chronic pain symptoms amongst adolescents and children by increasing understanding of mind-body connections in relation to experiences of pain. Further, the development of pain management strategies that address other factors that might be intensifying pain such as sleep and stress have been found to be helpful.
Reviewer's critique & take-home messages from the article
The first shortcoming of the study was that no list of inclusion or exclusion criteria for the articles was reported. This makes it difficult for the reader to draw any conclusions from the data presented as they cannot be confident that all relevant articles were identified. The second shortcoming of this review is that there is no synthesis of the extracted data. Indeed, the report of effectiveness for psychological outcomes arises from grouping the studies together under type of intervention and stating that each study within this type of intervention shows a statistically significant improvement, therefore the overall outcome is that this type of intervention is effective. More confidence in the results of this study would result from a meta-analysis of the grouped studies.
Declaration
Mon Chamlagai declares that she has no conflict of interest.
The Australian Pain Society (APS) is keen to share publications from our members with their colleagues via our eNewsletter. If you’ve had an article accepted or published recently, please contact our Assistant Editor Joanne Harmon via the APS Secretariat (aps@apsoc.org.au) with the title, authors, and reference (i.e., journal, volume, and DOI) of your article and request the submission template. We would love it if you also supply a short commentary (300 words max) to give our readers the gist of the article.
Evaluating the effect of incentives on recruiting people with low back pain with limited English proficiency as part of the COMFORT cluster randomised controlled trial: a study protocol for a study within a trial (SWAT)
Thank you to APS members Dr Stephanie Mathieson, Professor Fiona Blyth and their colleagues Lisa Vizza, Christopher Maher, Rowena Ivers, Andrew McLachlan, Patrick Kelly, Philip Clare, Rachel Thompson, Thomas Lung, Louisa Degenhardt, Sharon Reid, Bradley Martin, Michael Wright, Rawa Osman, Simon French, Kirsten McCaffery, Gabrielle Campbell, Hazel Jenkins, Monika Boogs, Jarrod McMaugh, Carol Bennett, Fiona Stanaway and Christina Abdel Shaheed for sharing the following recent publication.
Article first published online: 17 June 2025
Journal Reference: Vizza L, Maher CG, Ivers R, McLachlan AJ, Kelly PJ, Blyth F, Clare PJ, Thompson R, Lung T, Degenhardt L, Reid S, Martin BC, Wright M, Osman R, French SD, McCaffery KJ, Campbell G, Jenkins HJ, Mathieson S, Boogs M, McMaugh J, Bennett C, Stanaway F, Abdel Shaheed C. Evaluating the effect of incentives on recruiting people with low back pain with limited English proficiency as part of the COMFORT cluster randomised controlled trial: a study protocol for a study within a trial (SWAT). Trials. 2025 Jun 17;26(1):209.
DOI: 10.1186/s13063-025-08852-4
Abstract
Background
Previous research has reported that Australians with limited English proficiency are less likely to be included in clinical trials due to language, literacy, and cultural factors. In the pain field, participants with limited English proficiency are three times more likely to be excluded from research, whereas in low back pain trials, one in five participants are excluded. This low representation can limit the generalisability of research findings to Australia's diverse population, and strategies are required to facilitate the inclusion of participants with limited English proficiency in clinical trials.
This study within a trial (SWAT) embedded within a registered cluster randomised trial (ACTRN12622001505796) will evaluate a strategy to improve recruitment of participants with limited
English proficiency who speak Arabic, Cantonese, Mandarin or Italian.
Methods
This SWAT will evaluate the effect of perparticipant monetary incentive to facilitate the recruitment of participants with limited English proficiency (in Arabic, Chinese and Italian communities) from participating general practices enrolled in the COMFORT trial. In brief, the COMFORT trial will randomise general practices in a 1:1 ratio to either (i) intervention (educational outreach visits to support GPs to provide opioid stewardship for their patients with low back pain with non-drug strategies including heat wraps and patient education about judicious opioid use) or (ii) control (usual care).
In this embedded SWAT, the randomisation schedule will also randomly allocate general practices 1:1 to either (a) SWAT intervention (monetary incentive aimed at enhancing recruitment of individuals with limited English proficiency) or (b) SWAT control (no additional incentive). The SWAT primary outcome will be the proportion of participants with limited English proficiency enrolled into the COMFORT trial in the SWAT intervention versus SWAT control. Data collection, analyses and general study procedures will follow the COMFORT protocol.
Results
The trial is underway and currently recruiting. Ethics approval has been received by The University of Sydney (2023/632).
Conclusions
This SWAT will determine whether a perparticipant monetary incentive facilitates greater recruitment of people with limited English proficiency who speak Arabic, Cantonese, Mandarin or Italian by participating GPs.
Declaration
This SWAT has not received specific external funding; however, it is embedded within the COMFORT trial, which is supported by the National Health and Medical Research Council (NHMRC) of Australia (APP2000989) with coauthors as investigators.
Thank you to APS members Rebecca Fechner and Joshua W Pate and their colleagues Mark Alcock, Kris Rogers, Linsay Rogers, Anna Gollan, Erin Turbitt and Arianne Verhagen for sharing the following recent publication.
Article first published online: 09 May 2025
Journal Reference: Fechner, Rebecca; Rogers, Kris; Rogers, Linsay; Gollan, Anna; Alcock, Mark; Turbitt, Erin; Verhagen, Arianne P.; Pate, Joshua W. The Prevalence of Co-existing Motor Proficiency Delay and Chronic Pain in Children Presenting to a Tertiary Pain Service: A Cross-sectional Observational Study. The Clinical Journal of Pain ():10.1097/AJP.0000000000001297, May 9, 2025.
DOI: 10.1097/AJP.0000000000001297
Abstract
Background and Aims
Chronic pain can profoundly impact children’s physical, social and psychological functioning, with negative effects that can persist into adulthood. The prevalence of motor proficiency delay in children with chronic pain is unknown. We aimed to describe the prevalence of motor proficiency delay in a sample of children and estimate potential predictive factors of delayed motor proficiency from routinely collected selfreport measures.
Methods
We conducted a cross-sectional study of 94 children and adolescents (six-18 years) with chronic pain who attended a tertiary pain clinic in Australia. We assessed their motor proficiency using the Bruininks-Oseretsky test for Motor Proficiency, Second Edition (BOT-2) standardised assessment tool. Participants also completed a suite of routine clinical questionnaires and a self-perception questionnaire. We described the prevalence of motor proficiency delay using descriptive statistics and estimated the extent to which routine demographic and clinical data could explain variation in BOT-2 scores using a multivariable linear model to calculate adjusted R².
Results
Overall, 83% of participants presented with challenges in at least one motor-proficiency subtest (e.g., coordination), and 41% had delayed
total motor proficiency scores. We found that just 9% of the variance in BOT-2 scores could be explained by the covariates in the multivariable prediction model (Adjusted R2=0.09, 95% CI:0.01 to 0.25).
Conclusions
BLOG WEB
Most children presenting to a tertiary pain clinic presented with motor proficiency challenges are unlikely to be identified through routinely collected self-report measures. Given the BOT2 can identify norm-referenced developmental targets, the use of these assessments may enhance clinical formulations and guide developmentally sensitive rehabilitation programs.
Clinical Implications
For children with chronic pain, the BOT-2 may help clinicians understand nuanced developmental factors that influence and/or perpetuate pain, which in turn could assist teams to communicate the needs of children more sensitively and accurately to important stakeholders (e.g., parents, teachers and school staff, coaches and local health practitioners). For example, consider an 11-year-old boy with chronic pain, and challenges with school attendance, academic progress and socialising with peers. A clinical team could present his objective age-referenced scores relating to motor proficiency when collaborating with school, e.g., he has seven-year-old level fine motor skill, and six-year-old level bilateral coordination skills. Discussions with school may include multidisciplinary strategies to curb expectations in class (e.g., his fine motor skill makes written work a challenge) or to scaffold his social and physical participation (e.g., he may need to build skills to engage in age-appropriate outdoor play with peers). Providing such scaffolds at school may reduce the burden on his nervous system and improve his pain experience by building his ability to participate academically, physically and socially. With continued participation and success, a cascade of positive influences and developmental opportunity could follow, including the possibility of improving his developmental level.
Declaration
Rebecca received a start-up grant from the Queensland Children’s Hospital Study, Education and Research Trust Account (SERTA) to conduct this research.

Developed by the Australian Pain Society in collaboration with the National Ageing Research Institute, this FREE ‘train-the-trainer’ pain management program is for use by sta in both residential aged care facilities and organisations that provide aged care in the community, as well as NDIS providers.
Eight (8) painACT modules: One for the trainer called “How to use the painACT trainer program”, and seven modules for the trainer to train their sta :
Introduction to pain in aged care
Impact of pain on the person, family and sta
Conversations about pain
Source

Developed by the Australian Pain Society in collaboration with the National Ageing Research Institute, this FREE ‘train-the-trainer’ pain management program is for use by sta in both residential aged care facilities and organisations that provide aged care in the community, as well as NDIS providers.
For more information:
painACT is available on the Australian Pain Society website and consists of: > trainer learning module documents > short training video clips, and > participant handout material apsoc.org.au/painACT-Online-Learning








EXPRESSIONS OF INTEREST ONLINE: www.dccam.com.au/aps2026
Registrations open 18 November 2025
IMPORTANT DEADLINES
Topical Sessions 2 September 2025
Rising Star Award 7 October 2025
Free Papers & Posters 28 October 2025
Early Bird Registration 24 February 2026
Professor Yves De Koninck Yves De Koninck is Professor of Psychiatry and Neuroscience at Université Laval
and interdisciplinary approach to study the pathophysiology of neuromusculoskeletal conditions with the ultimate goal to improve management for patients.
For sponsorship and exhibition opportunities or more information please contact the APS Conference Secretariat: DC Conference & Association Management (DCC&A) P: 61 2 9954 4400 E: apsasm@dccam.com.au
> Online Pain Education Network (OPEN) launched in July 25
Other items of interest for our members:
> Latest opioid data from the Australian Bureau of Statistics: Opioid induced deaths in Australia.
> Australia’s annual overdose report 2024 from the Pennington Institute
> Australian Atlas of Healthcare Variation Series: This series explores how healthcare use in Australia varies depending on where people live. It investigates reasons for variation that may be unwarranted, and provides specific achievable actions to reduce unwarranted variation
> ePPOC: electronic Persistent Pain Outcomes Collaboration: The electronic Persistent Pain Outcomes Collaboration (ePPOC) is an Australasian initiative that aims to improve the quality of care and outcomes for people who experience chronic pain.
> PainHEALTH: painHEALTH‘s aim is to help health consumers with musculoskeletal pain access reliable, evidence-based information and tips to assist in the co-management of musculoskeletal pain. painHEALTH is an initiative of the Department of Health, Western Australia
> Stanford University CHOIR: CHOIR Collaborative Health Outcomes Information Registry
> Opioid Podcasts for GPs: These podcasts are produced by David Outridge GP, and FAChAM Trainee as a project under the auspices of Dr Steven Kelly Staff Specialist in Addiction Medicine, Kullaroo Clinic Gosford. A weekly series from the Hunter Postgraduate Medical Institute (University of Newcastle)
> Airing Pain: Pain resources via an online radio show produced by Pain Concern, a UK registered Charity
> Indigenous Resources: Webpage on the APS website aggregating Indigenous resources
> Tame the Beast: Free educational tool that aims to inspire research-based action in the treatment of chronic pain
> Codeine information hub
NSW Agency for Clinical Innovation resources:
> Brainman and Pain Tool Kit translations
> Pain Management Resources
> Quicksteps to Manage Chronic Pain in Primary Care
> Built into Quicksteps: “How to de-prescribe and wean opioids in general practice”
> A list of helpful apps for consumers and clinicians
> Chronic Pain in the ED
The APS Board is pleased to advise that the updates to our membership system, as voted upon and agreed at the 2025 Annual General Meeting, have now been implemented.
New applicants can now apply online with an electronic signature and no longer require a nominator to co-sign their application form.
We hope these changes will make it easier for potential members to join the Australian Pain Society.
Now is an especially great time to encourage your peers to join the Australian Pain Society with this new streamlined process AND half year membership rates through to 31 December 2025, as follows:
a. Regular A
b. Regular B
c. Regular C
$65
$130
$220
d. Retired $65 Concessional Rate, half year does not apply
e. Student $65 Concessional Rate, half year does not apply
Payments can be made by Credit Card or BPAY.
Did you know that the Australian Pain Society is a registered charity with ACNC? Your donation will help the Society to promote the prevention and control of diseases in human beings associated with pain.
All donations of $2 or more to APS are tax-deductible.
as at 20 July 2025
Miss Talia Barnet-Hepples Physiotherapy
Mr Joel McPhee Physiotherapy
Mr Erfan Nasheri Psychology
Dr Katrina Norris
Psychology
01-03 August 2025
Pharmaceutical Society of AustraliaPSA25
Constructing Excellence
International Convention Centre, Sydney, NSW
08-10 August 2025
Neuromodulation Society of Australia & New Zealand
NSANZ 2025 18th Annual Scientific Meeting
ICC Sydney, NSW
23-30 August 2025
Pain Revolution 2025
Rural Outreach and Cycling Tour
Various venues: Bundaberg, Hervey Bay, Gympie, Maleny, Noosa, Birtinya, Sunshine Coast, QLD
04-06 September 2025
International Association for the Study of Pain (IASP)
NeuPSIG 2025, 9th International Congress on Neuropathic Pain
Urania Berlin e.V., Berlin, Germany
07-09 October 2025
Australia & New Zealand Musculoskeletal Clinical Trials Network
ANZMUSC 2025 Scientific Meeting
University of Queensland City Campus and Customs House, Brisbane, QLD
08-09 October 2025
National Rural Health Alliance, Australian Rural Health Education Network & Federation of Rural Australian Medical Educators
10th Rural & Remote Health Scientific Symposium
Alice Springs Convention Centre, Alice Springs, NT
13-15 October 2025
Australian Association of Psychologists Inc
AAPi Conference 2025
Grand Hyatt, Melbourne, VIC
17 October 2025
Pain Nurses Australia
2025 Annual Professional Day - Pain in Vulnerable Populations
Waterview in Bicentennial Park, Sydney Olympic Park, Sydney, NSW
23-25 October 2025
Australian Physiotherapy Association
Scientific Conference
Adelaide Convention Centre, Adelaide, SA
24-26 October 2025
Faculty of Pain Medicine (FPM)
2025 FPM Spring Meeting
Esplanade Hotel, Fremantle, WA
14-16 November 2025
Royal Australian College of General Practitioners
GP25
TBC, Brisbane, QLD
19-21 November 2025
Australian & New Zealand Spinal Cord Society
ANZCoS 2025: Rivers of Innovation
Brisbane Convention and Exhibition Centre, Brisbane, QLD
18-21 March 2026
New Zealand Pain Society (NZPS)
NZPS26 - The Right Fit
Christchurch Town Hall, Otautahi Christchurch, NZ
19-22 April 2026
Australian Pain Society
2026 Australian Pain Society 46th Annual Scientific Meeting
Adelaide Convention Centre, Adelaide, SA
Vision:
All people will have optimal pain management throughout life.
Purpose:
The Australian Pain Society is a multidisciplinary association whose purpose is to advance pain management through education, research, and advocacy for transformational improvements in clinical care.
Priorities:
In order to achieve our purpose, the Australian Pain Society will provide:
> Membership
> Research
> Education
> Services and resources
> Good governance and operations
> Advocacy




President:
Mrs Bernadette Smith
Psychology Plus
South Burnie TAS
Tel: 03 6431 9959 Fax: 03 6431 995001
President-Elect:
Dr Laura Prendergast
Persistent Pain Management Service
Northern Health
Broadmeadows VIC 3047
Tel: 03 8345 5166 Fax: N/A
Work days Mon & Thu
Secretary:
Mrs Dinah Spratt
Physiotas Physiotherapy
Shearwater TAS 7307
Tel: 03 6428 7500 Fax: 03 6424 7811
Treasurer:
Dr Duncan Sanders
Pain Management Unit,
Sydney Medical School, University of Sydney / Managing Pain Clinic and E3 Physio
Gold Coast QLD
Tel: 07 5620 1234 Fax: 07 3009 042


ACT Director:
Mr Anjelo Ratnachandra
Beyond Pain Pty Ltd
Belmont VIC 3216
Tel: 0400 202 803 Fax: N/A
NSW Director:
Dr Connor Gleadhill
Department of Health and Aged Care
Primary Care Division
Newcastle NSW 2038
Tel: 0405 203 661 Fax: N/A






NT Director:
Dr Amelia Searle
Flinders Medical Centre Pain
Management Unit
Bedford Park SA 5042
Tel: 08 8204 5499 Fax: 08 8204 5440
QLD Director:
Mrs Karla Wright
Fernvale Priceline Pharmacy
Fernvale QLD 4306
Tel: 07 5427 0695 Fax: 07 5427 0698
SA Director:
Ms Heather Gray
Royal Adelaide Hospital
Adelaide SA 5000
Email: heather.gray@sa.gov.au
TAS Director:
Mr Sinan Tejani
Launceston General Hospital
Launceston TAS 7250
Tel: 0469 967 841 Fax: N/A
VIC Director:
Mrs Alison Sim
10 South Sports Medicine
Geelong VIC 3220
Tel: 0488 988 315 Fax: N/A
WA Director:
Ms Jacintha Bell
Lifeworks Occupational Therapy
Mount Lawley WA 6050
Tel: 0451 178 880 Fax: 08 6323 3329





Immediate Past President:
Mrs Joyce McSwan
Gold Coast Primary Health Network
Persistent Pain Program, QLD and PainWISE
Tel: 0412 327 795 Fax: 07 3539 9801
SPC Chair:
Professor Kevin Keay
Department of Anatomy
University of Sydney
Sydney NSW 2006
Tel: 02 9351 4132 Fax: 02 9351 2817
IASP Liaison:
Professor Fiona Blyth AM
Sydney School of Public Health
Faculty of Medicine and Health
University of Sydney
Camperdown NSW 2006
Email: Fiona.blyth@sydney.edu.au
Communications Coordinator:
Mrs Bernadette Smith
Psychology Plus
South Burnie TAS 7320
Tel: 03 6431 9959 Fax: 03 6431 9950
Newsletter Editor:
Clinical A/Prof Kylie Bailey
Sagacity Services
Mount Hutton NSW 2290
Tel: 0447 905 085



Newsletter Assistant Editor:
Dr Joanne Harmon
School of Clinical and Health Sciences
University of South Australia
Adelaide SA 5000
Tel: 08 8302 1442
Scholarship/Grant Selection Subcommittee Co-Chairs:
Emeritus Professor Maree Smith AC
Centre for Integrated Preclinical Drug Development
University of Queensland St Lucia QLD 4072
Professor Luke Henderson
Anatomy & Histology, School of Medical Sciences
Brain & Mind Centre
University of Sydney Camperdown NSW 2006

Secretariat:
DC Conference & Association
Management Pty Ltd
PO Box 637
North Sydney, NSW 2059
Tel: 02 9016 4343
Email: aps@apsoc.org.au
Website: apsoc.org.au