3 minute read
Shoulder Films
patient for free air. A lateral decubitus film will detect these things as well in the patient who is not able to ambulate. In the lateral decubitus, the upper side of the abdomen should be seen in order to evaluate the patient for free air in the abdominal cavity. The AP erect is done on infants weighing up to fifteen pounds.
The urinary tract can be evaluated with a plain film that includes images of the kidneys, ureters, and bladder. IV contrast is used to outline these structures in the supine patient. Images are obtained immediately after the injection and again after ten minutes. A final film is taken after the bladder is filled with contrast or about 25 minutes after the injection of contrast material.
Advertisement
A lateral film is taken in late pregnancy in order to look for cephalopelvic disproportion in the patient with an arrest or possible obstruction of labor. It is used when an ultrasound cannot be performed. An AP or PA of the pelvis can also be obtained for this purpose.
SHOULDER FILMS
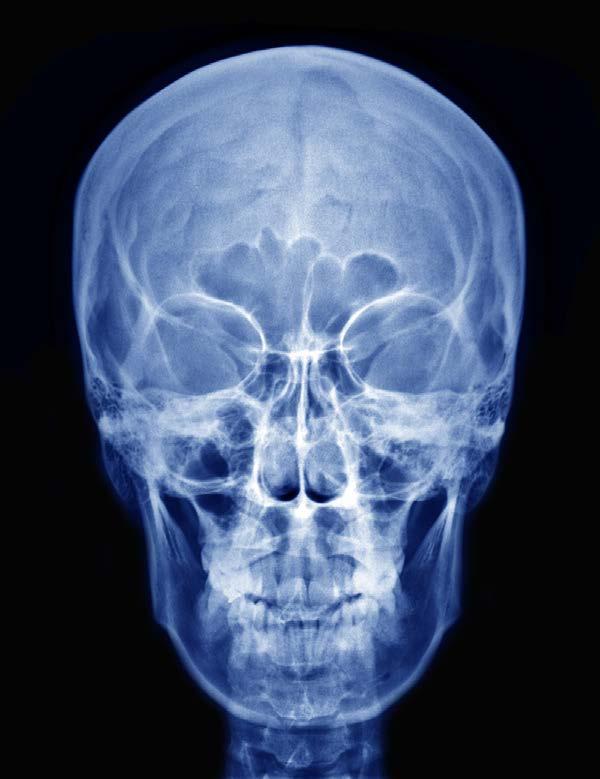
A shoulder film is done to evaluate a person for fractures of the affected area, for shoulder dislocation, or for other bony abnormalities of the shoulder. Soft tissue problems, like calcifications of the rotator cuff muscles can be seen on a plain film of the shoulder. The standard image is of the AP shoulder that can be internally or externally rotated. Figure 7 shows a typical shoulder x-ray:
Figure 7.
You can also get a Y image, which is a lateral image of the scapula, an axial image, or an apical oblique image. The difference is the angle at which the beam is aimed toward the shoulder. These images can help detect subluxations or dislocations of the shoulder. There is a special acromioclavicular or AC image taken at a ten-degree angle from the horizontal, directed upward to view the AC joint. The Y image is called this because the scapula, the scapular spine, and the coracoid process together form a Y shape. In the AC joint view, the bottom of the acromion needs to be aligned with the bottom of the clavicle. If this does not happen, think of an AC subluxation or dislocation. Figure 8 shows this alignment:

Figure 8.
For evaluation of fractures of the proximal humerus, the Neer classification is used. This divides the humeral head into four segments. Segment I is the humeral shaft; segment II is the humeral head; segment III is the greater tubercle where most of the rotator cuff muscles insert; segment IV is the lesser tubercle, where the subscapularis muscle inserts. Figure 9 shows these segments:

Figure 9.
As you can see by the figure, the anatomical neck is located between the two tubercles and the head of the humerus. The surgical neck is below that and is a site for many fractures. Dislocation is noted when any segment moves more than one centimeter or when there is curvature or angulation of a segment more than forty-five degrees.
The Neer classification is determined by the parts that are left after the fracture. In a one-part fracture, there is a simple non-dislocated fracture, while in a four-part fracture, there is dislocation through all four parts of the proximal humerus with four separate fracture segments. More than ninety percent of these are one-part fractures. CT scanning is done in a three or four-part fracture.
Luxation or dislocation involves a disruption in the relationship between two components of the joint. More than 95 percent of shoulder subluxations are anterior. This can be seen in several images of the shoulder joint. Figure 10 shows a dislocated shoulder:

Figure 10.
Traumatic dislocation of the shoulder will often cause an impaction fracture of the humeral head, known as a Hill-Sachs lesion. The lesion will be seen on the posterolateral side of the humerus so it requires internal rotation of the shoulder in order to see it. There is a Bankart lesion, located on the opposite side of a Hill-Sachs